- 1Department of Psychological Medicine, University of Otago, Wellington, New Zealand
- 2Wakefield Obesity Surgery, Wakefield Hospital, Wellington, New Zealand
- 3Department of Psychiatry, University of Oxford, Oxford, United Kingdom
Background: Bariatric surgery is seldom accessed by people with serious mental illness, despite high rates of obesity in this population. It is sometimes assumed that patients with complex psychiatric histories will have poor post-surgical weight loss or exacerbation of psychiatric symptoms, although this is unsubstantiated.
Objectives: A qualitative descriptive study to explore personal experiences and the impact of bariatric surgery on physical and mental well-being and life-quality in individuals with serious mental illness.
Methods: Nine adults with a history of bariatric surgery and concurrent severe depressive disorder, bipolar disorder, or schizoaffective disorder were interviewed about their experiences of bariatric surgery and its outcomes using semi-structured interview schedules. Data were transcribed and inductive thematic analysis undertaken.
Results: Five broad themes emerged: (1) surgery was highly effective for weight loss, and resulted in subjective improvements in physical health, quality of life, and mental health described as being able to live a life; (2) recovering from surgery was a tough road, notably in the post-operative period where negative sequelae often anteceded benefits; (3) post-operative support was important, but sometimes insufficient, including from families, mental health services, and surgical teams; (4) most considered surgery life-changing, recommending it to others with mental illness and obesity, two had different experiences; (5) participants considered it discriminatory that people with mental illness were not referred or declined weight loss surgery.
Conclusions: Participants benefited from bariatric surgery and felt it should be offered to others with mental illness, but with additional care and support.
Introduction
People living with serious mental illness (SMI), including psychotic disorders and bipolar disorder, have a high prevalence of obesity—nearly twice the rates of the general population (1, 2). There is convincing evidence that SMI in general and certain antipsychotic medications in particular, are associated with high risks of metabolic syndrome—a constellation of cardiovascular risk factors including abdominal obesity, dyslipidemia, hypertension, and hyperglycemia (3–5). This contributes to the elevated mortality from cardiovascular diseases (1), with the presence of SMI itself being a risk for adverse cardiac outcomes over and above that predicted by other established risk factors (6). Obesity and its correlates are major contributors to the dramatic reduction in life expectancy in this group (7, 8). This means evidence-based interventions for weight loss need to be carefully considered, researched, and promoted for those with SMI. Unfortunately, this important research base is limited.
Lifestyle and pharmacological interventions have been shown to result in modest weight loss in people with SMI—on average 3 kg (9–12), but data are inconsistent (13, 14) with little long-term cardiometabolic follow-up.
In the general population, bariatric surgery has superior weight loss outcomes compared with other interventions for severe obesity, resulting in substantial improvements in comorbid conditions (15, 16) and quality of life (15, 17). While less severe conditions such as anxiety, mild to moderate depression, and binge eating disorder are common amongst bariatric surgery patients with a corresponding body of research (18–20), the eligibility of people with more severe psychiatric conditions is controversial (21–23) and research in this group is surprisingly scant.
It is often assumed people with complex psychiatric histories will have poor post-operative weight loss and higher complication rates, which may result in their not being referred or being declined surgery (24, 25). In a survey of mental health professionals conducting bariatric surgery eligibility evaluations, 91.2% identified “psychiatric issues” as “clear contraindications” to weight loss surgery (25).
In fact, what research there is suggests that those with SMI have comparable weight loss and complication rates to controls although unsurprisingly people with SMI may require more postoperative support (26–31). In a systematic review of eight eligible studies of bariatric surgery in people with schizophrenia or bipolar disorder, Kouidrat and colleagues reported favorable weight loss outcomes (32). However most included studies focused solely on physical endpoints like weight loss without assessing changes in mental state (32). Research investigating the subjective peri-operative experiences of patients with SMI is distinctly absent. This study aims to examine the personal experiences of bariatric surgery on physical and mental health, and on quality of life in patients with a history of SMI.
Materials and Methods
Participants
We included participants who had undergone bariatric surgery within 15 years and had active diagnoses of bipolar disorder, psychotic disorder, or severe depressive disorder at the time of the surgery, identified by ICD or DSM diagnosis (in the medical records) or by medication use (therapeutic doses of mood stabilizer and/or antipsychotic medication), with subsequent confirmation on interview. All had been assessed as having stable symptoms at the time of surgery, competent to consent, and capable of complying with postoperative care.
This study received ethical approval from the University of Otago Human Ethics Committee (Health), ref H17/116.
Consent to participate in the study and for publication of data was obtained from all participants.
Recruitment and the Interviewing Process
Patients were recruited through convenience sampling from patient records or snowballing techniques. They were contacted by researchers via postal invitations containing study information, or via telephone, and invited to participate. After obtaining written informed consent, SG conducted semi-structured interviews face-to-face or telephonically, if preferred by participants. Interviews were conducted in and by a university department of psychological medicine.
Interviews were audiotaped and transcribed verbatim within 4 days of being conducted. Data were entered into NVivo qualitative data analysis software (NVivo, version 10, QSR International).
Analysis
Data were analyzed using thematic analysis (33). Thematic analysis is an established method for identifying, reporting, and analyzing patterns within data, with minimal organization and description of the data in rich detail. Patterns are identified iteratively through a careful process of data familiarization, data coding, theme development, and review (33).
We used an inductive, realist approach to data analysis, in which we reported the experiences, meanings, and the reality of participants (34). The inductive approach involves coding the data without trying to fit it into a pre-existing coding frame or the researcher’s analytic preconceptions. We selected this thematic approach a priori, as those of us designing the interview (SEP, MH, SR) and conducting the analysis (SEP, MH, SR, and AT) were theoretically agnostic about bariatric surgery. We have backgrounds in psychiatry with limited experience of obesity surgery and wanted to be guided by our participants’ experiences. We selected a strongly data-driven approach as the most appropriate method to explore personal experiences and the impact of bariatric surgery on physical and mental well-being and quality of life.
Two researchers (SEP and MH) independently read and coded transcripts; codes were examined and iteratively condensed into groups capturing similar themes, each with a number of subthemes. These themes and sub-themes were then reviewed by members of the wider team (SR and AT). To achieve saturation of themes, we moved back and forth between data collection and analysis, ensuring the fit between data and the conceptual work of analysis and interpretation. Interviews completed early in the study informed subsequent data collection, and analysis.
Results
Participants
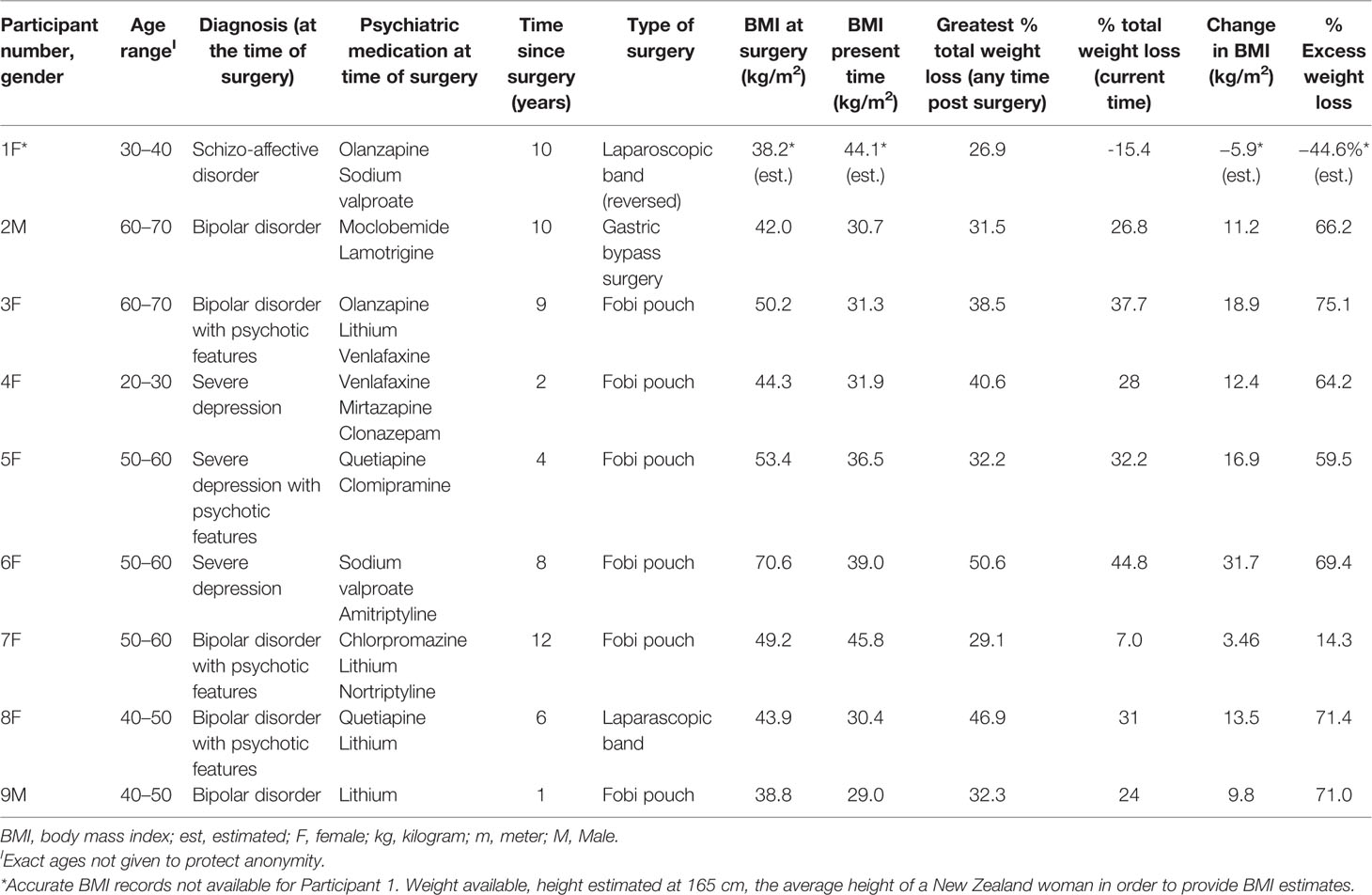
Sixteen potentially eligible patients were identified from patient databases (n = 13) and snowballing techniques (n = 3). Nine responded affirmatively and met eligibility criteria. Demographic characteristics are summarized in Table 1. On average, 7 years had passed since surgery. Primary psychiatric diagnoses included bipolar disorder (n = 5), schizoaffective disorder (n = 1), and severe depressive disorder (n = 3), with psychosis in five. All were prescribed psychotropic medication: antipsychotics (n = 5); mood stabilizers (n = 7); and antidepressants (n = 6).
Participants described significant mental illnesses that started early in adult life and pre-dated surgery.
“I would have been 19–20 [when diagnosed] and it was very severe and I was [responding to command hallucinations] … floridly psychotic and I stopped eating, I stopped showering, I stopped doing everything [8].”
Participants reported significant functional impairment that impacted on activities of daily living, relationships, and ability to work.
“I was quite ill mentally. And I wasn’t leaving the house. Slept most of the day and most of the night. And was in a really bad place [4].”
Prior to surgery, seven of the nine participants had been hospitalized for mental health crises, with two in long-term inpatient care. One participant had received long term care from forensic mental health services. Five had histories of suicide or self-harm attempts.
Weight Prior to Surgery
Prior to surgery participants had an average body mass index (BMI) of 48 kg/m2 (Table 1). Psychotropic medication was viewed as a major causal factor for weight gain.
“I’d spent a year in [hospital] and they put me on quetiapine and quetiapine is a shocking weight gainer. And I put on … I got to 130 kg, I mean I was heavy [8].”
“I was on olanzapine. I’d always had really low weight. I weighed 60 or 50 kg and then it went up to 104…and it kept going up [1].”
All described functional impairment and obesity-related physical health issues, including diabetes, obstructive sleep apnea, and impaired mobility. Participants had tried multiple weight loss strategies, which they found ineffectual.
Surgery
Participants thought carefully about surgery before proceeding. All self-funded surgery, in most cases with financial support from relatives, after having been declined or believing they were ineligible for publicly funded surgery.
“My parents paid for it … they felt it was worth it to help me because I was in such a bad place [4].”
Two participants traveled several hundred kilometers to providers that accepted patients with stable SMI.
“I got turned down from the [public hospital] in town here [because of] … my psychiatric problems … I was a bit annoyed really. Because I’m just a human like the next woman that wants helps with their obesity … [3].”
The type of bariatric surgery included laparoscopic gastric bypass surgery (n = 1), laparoscopic adjustable gastric banding (n = 2), and open Fobi pouch gastric bypass (n = 6). One participant subsequently had a gastric band removal.
Themes
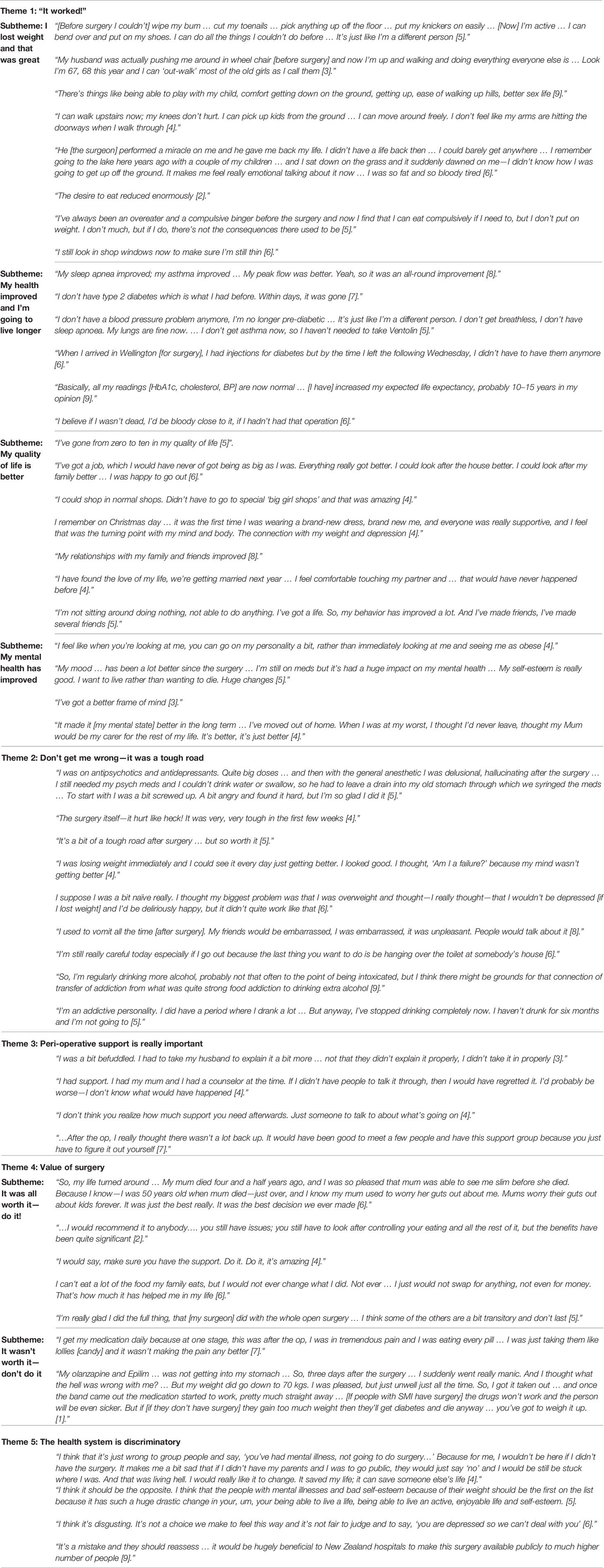
We identified five major themes as follows: [1] Surgery was highly effective across multiple domains extending beyond weight loss; [2] the post-operative period was challenging; [3] support was important and needed to be multidisciplinary; [4] most people thought surgery was life-changing and recommended it to others with SMI and obesity; [5] it was considered discriminatory that people with SMI were not referred or actively discouraged from weight loss surgery. These themes are explored below, and supporting quotes appear in Table 2.
Theme 1: It worked!
Seven participants (78%) reported the operation was successful, improving their health and lives in the medium to long term (“being able to live a life”). This was the predominant theme, shared by the majority, with strong convergence in accounts. Most reported profound improvements across multiple areas (classified as subthemes)—weight loss, broader physical health, quality of life and mental health. Two people had differing experiences, which are discussed in Theme 4.
Subtheme 1(a): I lost weight and that was great
All nine participants lost weight after surgery. The average greatest percentage weight loss was 36.25%. The average current percentage weight loss was 27.2%. Eight participants weighed significantly less now than prior to surgery. The participant who had a gastric band removal had regained weight. Weight loss had profound effects, allowing people to achieve things they considered important, but could not formerly manage:
“[Before surgery I couldn’t] wipe my bum … cut my toenails … pick anything up off the floor … put my knickers on easily … [Now] I’m active … I can bend over and put on my shoes. I can do all the things I couldn’t do before … It’s just like I’m a different person [5].”
“He [the surgeon] performed a miracle on me and he gave me back my life. I didn’t have a life back then … I could barely get anywhere … It makes me feel really emotional talking about it now … I was so fat and so bloody tired [6].”
Subtheme 1(b): My health improved and I’m going to live longer
All but two participants reported net positive improvements in physical health (e.g. “hugely beneficial,” “an all-round improvement”). Eight participants reported improvements in obesity-associated morbidities such as sleep apnea, asthma, pre-diabetes, or diabetes. Most described requiring fewer medications or lower doses, particularly antihypertensive and diabetic control medications.
“When I arrived [for surgery], I had injections for diabetes, but by the time I left the following Wednesday, I didn’t have to have them anymore [6].”
People believed their health gains would extend their lifespan:
“Basically all my readings [HbA1c, cholesterol, BP] are now normal … [I have] increased my expected life expectancy, probably 10–15 years in my opinion [9].”
“I believe if I wasn’t dead, I’d be bloody close to it, if I hadn’t had that operation [6].”
Subtheme 1(c): My quality of life is better
Seven participants said their quality of life had improved, describing improvement in vocational, functional, and social domains.
“I’ve gone from zero to ten in my quality of life [5]”.
“I’ve got a job, which I would have never got being as big as I was. Everything really got better. I could look after the house better. I could look after my family better [6].”
Improvements in self-confidence, self-esteem, and self-image, led to positive changes in social life and overall quality of life. Many felt personal and family relationships improved.
“I’m not sitting around doing nothing, not able to do anything. I’ve got a life. So, my behavior has improved a lot. And I’ve made friends, I’ve made several friends [5].”
Subtheme 1(d): My mental health improved
Most participants, with one notable exception, reported improvements in their long-term mental health following surgery, relating to indirect effects, such as greater self-confidence and social connections. Physical changes gave people a greater sense of identity, and the hope they could be viewed on their own merits, rather than stigmatized as overweight psychiatric patients.
“I feel like when you’re looking at me, you can go on my personality a bit, rather than immediately looking at me and seeing me as obese [4]”.
The sense of regeneration was reflected in the recurring phrase “different person,” with positive effects cited on mental health and wellbeing.
“It made it [my mental state] better in the long term … I’ve moved out of home. When I was at my worst, I thought I’d never leave, thought my Mum would be my carer for the rest of my life. It’s better, it’s just better [4]”.
Theme 2: Don’t get me wrong—it was a tough road
All participants described considerable challenges in the post-operative period, including pain, difficulties with dietary adaptions, gastrointestinal side effects and, for two participants, mental state instability.
“I was on antipsychotics and antidepressants. Quite big doses … and then with the general anesthetic I was delusional, hallucinating after the surgery … To start with I was a bit screwed up. A bit angry and found it hard, but I’m so glad I did it [5].”
The negative sequelae anteceded the benefits of surgery, and patients described the post-operative period as difficult.
“The surgery itself—it hurt like heck! It was very tough in the first few weeks [4].”
Some participants reported mismatches between their expectations and the reality of their mental health in this period. The gastrointestinal side effects of the surgery often had social implications, which caused social discomfort. Participants gradually learnt what foods they could not tolerate, adjusting eating habits and portion sizes accordingly, which required long-term commitment. In the medium term, two participants reported an increase in alcohol consumption, which they identified as a “transfer” of addictive tendencies from eating to another outlet.
“I’m an addictive personality. I did have a period where I drank a lot … But anyway, I’ve stopped drinking completely now [5]”.
Theme 3: Peri-operative support is really important
Participants strongly endorsed the importance of psychosocial support after surgery.
“It was hard, but I had the right kind of support and that made it—not better—but I could get through it [4].”
People valued the support of families, friends, surgical and mental health teams. Support was practical (helping out with ADLs after surgery, financial assistance), social (having company at appointments, support groups), psychological (talking therapies), and psychiatric (monitoring of mental state, medication adjustments as necessary). Participants felt that their mental health care was not well integrated with their perioperative bariatric care.
“…After the op, I really thought there wasn’t a lot of back-up. It would have been good to meet a few people and have this support group because you just have to figure it out yourself [7].”
Theme 4: The value of surgery
4(a): It was all worth it—do it!
While acknowledging the post-operative challenges (which were significant as discussed above), seven participants were strongly positive about the overall value personal value of surgery (“miracle,” “the best,” “amazing”). They reflected on the life-changing impacts surgery had for them and family members.
“So, my life turned around … It was the best decision we ever made [6].”
These participants all recommended surgery to others with SMI and obesity.
“I would recommend it to anybody … you still have to look after controlling your eating and all the rest of it, but the benefits have been quite significant [2].”
“…I would not ever change what I did. Not ever … I just would not swap for anything, not even for money. That’s how much it has helped me in my life [6].”
Theme 4b: It was not worth it—don’t do it
Despite losing weight, two patients considered surgery was not a net success for them. For one [1], this related to post-operative deterioration in mental state, and for another [7], there were various surgical complications commencing with a bile leak (related to coincidental cholecystectomy) requiring percutaneous drainage, and a small bowel perforation requiring further surgery almost two years after her gastric bypass. While she achieved weight loss and resolution of her diabetes, she felt the complications outweighed the benefits.
The other patient experienced a postoperative relapse in mental state, which she attributed to changes in absorption of antipsychotic medication, and which required inpatient care. After an extended period of poor psychiatric control, she opted to have her laparoscopic band removed. She thought people with SMI were in a difficult bind, based on her experience.
“[If people with SMI have surgery] the drugs won’t work and the person will be even sicker. But if [if they don’t have surgery] they gain too much weight then they’ll get diabetes and die anyway … you’ve got to weigh it up [1].”
Theme 5: The health system is discriminatory
Surgery was self-funded, which people found expensive. While bariatric surgery is available through the public health system in New Zealand, no participants could access this funding. They felt people with SMI were being excluded either overtly or covertly and this was discriminatory.
“I think that it’s just wrong to group people and say, ‘you’ve had mental illness, not going to do surgery…’ Because for me, I wouldn’t be here if I didn’t have the surgery … I would really like [these attitudes] to change. It saved my life, it can save someone else’s life [4].”
Participants expressed gratitude to their families for their support and to their surgeon for accepting them for obesity surgery after others had declined them on the basis of their SMI. They felt that their surgeon had seen them as people, whereas the public system viewed them as cases of mental illness.
Discussion
This is the first qualitative study, to our knowledge, that explores the experiences of people with SMI following bariatric surgery. For most participants, bariatric surgery was successful across multiple domains—in many instances profoundly so—and they recommended bariatric surgery to others with SMI and obesity. Participants reported an increase in their self-esteem and self-confidence, which enabled them to socialize more frequently and lead to improvements in their personal and family relationships.
The post-operative period was viewed as a tough road, and participants described the need for additional support at this time—practical, physical, and related to their mental health needs. The fact that six participants had “open laparotomy” surgery may have added to this view. This is not so different from the general population undergoing bariatric surgery (35); Jumbe and colleagues recently conducted a qualitative analysis of patients without mental illness, finding patients experienced unmet psychological needs after surgery, which were not well-recognized by health professionals (36).
Obesity is common amongst people with SMI and a major contributor to premature death in this group. In previous research conducted in the same geographical catchment area as this study (37, 38), 74% of the psychiatric inpatients sampled (n = 51) were obese, most with medical comorbidities. They were distressed by their weight, reporting negative feelings about themselves including low personal effectiveness and self-stigmatization. However, none had been referred for bariatric surgery.
The participants in this study viewed the health system as overtly or covertly discriminatory against people with SMI, having experienced barriers to accessing publicly funded bariatric surgery on account of their mental illness.
Limitations
This study has a small number of participants selected by convenience sampling. As is the nature of qualitative studies, it is hypothesis-generating and cannot provide “proof” of the benefits or risks of bariatric surgery, only an account of personal experiences. Those in in our study were a small sample and not representative of the full spectrum of people with serious mental illness. For example, they (or their families) were able to self-fund surgery, meaning they comprised a comparatively socially advantaged group. Furthermore, while five of the participants had psychotic symptoms, none had a primary schizophrenia diagnosis.
Similarly, the number of open surgeries in this group is not typical. More than half our participants had laparotomies, reflecting local practice. However, the majority of contemporary bariatric interventions are performed laparoscopically. The “open laparotomy” technique may be considered a bias, because it may lead to different post-operative experiences.
The qualitative nature of the study means the data comprises personal accounts, not objectives measures, and as such is subject to recall and other biases. Further research is required incorporating the use of validated measures related to well-being, such as quality of life, self-esteem, addictive, depressive and psychotic symptom scales.
Lastly, it is important to recognize that qualitative researchers cannot completely detach themselves from their own personal and professional preconceptions. As noted by Braun and Clark (33), data are not coded in an epistemological vacuum. The researchers who collected and analyzed the data are all health professionals (with mental health expertise), and both the framing of the interview questions and our interpretation of themes may have been influenced by our medical backgrounds.
Conclusions
This small sample with a long follow-up showed the substantial benefit of bariatric surgery accrued to this group with severe mental illness and obesity, which extended beyond physical domains. Overall, bariatric surgery was effective for weight loss, it improved quality of life, and our participants recommended it to others with serious mental illness. Participants would have appreciated more multidisciplinary post-operative support targeted to their mental health needs. Their pathway to undergo surgery was difficult, and the reluctance by gatekeepers to allow access to publicly funded surgery was considered discriminatory.
Obesity and metabolic syndrome are common amongst people with SMI, who should be able to access evidence-based interventions in the same way as other members of the community. Health providers and funders need to carefully consider how to remove the overt and covert barriers that add to discrimination and impede people with mental illness accessing effective treatments for their physical health. There is a clear need for obesity surgery trials which include participants with SMI to explore the risks and benefits of bariatric surgery. Surgical and mental health services need to work together to support the physical and psychosocial needs of patients after bariatric surgery.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The study received ethical approval from the University of Otago Human Ethics Committee (Health), ref H17/116. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SE-P is the principal researcher. SE-P, SR, and MH conceived of the study and designed the protocol and semi-structured interview format. RS provided expert advice on bariatric surgery throughout the study but did not participate in data collection or analysis. SG collected data. SE-P, SR, MH, and AT undertook the thematic analysis. AT assisted with drafting the manuscript. SE-P drafted the first version of this manuscript. All authors provided editorial input and approved the final version of this manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank those people who generously gave their time to participate in this study.
References
1. Dickerson F, Brown C, Kreyenbuhl J, Fang L, Goldberg R, Wohlheiter K, et al. Obesity among individuals with serious mental illness. Acta Psychiatr Scand (2006) 113(4):306–13. doi: 10.1111/j.1600-0447.2005.00637.x
2. Allison DB, Newcomer JW, Dunn AL, Blumenthal JA, Fabricatore AN, Daumit GL, et al. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. Am J Prev Med (2009) 36(4):341–50. doi: 10.1016/j.amepre.2008.11.020
3. Mitchell AJ, Vancampfort D, De Herdt A, Yu W, De Hert M. Is the prevalence of metabolic syndrome and metabolic abnormalities increased in early schizophrenia? A comparative meta-analysis of first episode, untreated and treated patients. Schizophr Bull (2013) 39(2):295–305. doi: 10.1093/schbul/sbs082
4. Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders—a systematic review and meta-analysis. Schizophr Bull (2013) 39(2):306–18. doi: 10.1093/schbul/sbr148
5. Vancampfort D, Vansteelandt K, Correll CU, Mitchell AJ, De Herdt A, Sienaert P, et al. Metabolic syndrome and metabolic abnormalities in bipolar disorder: a meta-analysis of prevalence rates and moderators. Am J Psychiatry (2013) 170(3):265–74. doi: 10.1176/appi.ajp.2012.12050620
6. Cunningham R, Poppe K, Peterson D, Every-Palmer S, Soosay I, Jackson R. Prediction of cardiovascular disease risk among people with severe mental illness: A cohort study. PloS One (2019) 14(9). doi: 10.1371/journal.pone.0221521
7. Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, Hennekens CH, Lambert M, Leucht S, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry (2008) 69(4):514. doi: 10.4088/JCP.v69n0401
8. Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med Care (2011) 49(6):599–604. doi: 10.1097/MLR.0b013e31820bf86e
9. Caemmerer J, Correll CU, Maayan L. Acute and maintenance effects of non-pharmacologic interventions for antipsychotic associated weight gain and metabolic abnormalities: a meta-analytic comparison of randomized controlled trials. Schizophr Res (2012) 140(1):159–68. doi: 10.1016/j.schres.2012.03.017
10. Kouidrat Y, Amad A, De Hert M. Emerging drugs and indications for cardio-metabolic disorders in people with severe mental illness. Curr Pharm Des (2015) 21(23):3317–24. doi: 10.2174/1381612821666150619093128
11. Praharaj SK, Jana AK, Goyal N, Sinha VK. Metformin for olanzapine-induced weight gain: a systematic review and meta-analysis. Br J Clin Pharmacol (2011) 71(3):377–82. doi: 10.1111/j.1365-2125.2010.03783.x
12. Newall H, Myles N, Ward PB, Samaras K, Shiers D, Curtis J. Efficacy of metformin for prevention of weight gain in psychiatric populations: a review. Int Clin Psychopharmacol (2012) 27(2):69–75. doi: 10.1097/YIC.0b013e32834d0a5b
13. Firth J, Cotter J, Elliott R, French P, Yung A. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med (2015) 45(7):1343–61. doi: 10.1017/S0033291714003110
14. McGinty EE, Baller J, Azrin ST, Juliano-Bult D, Daumit GL. Interventions to address medical conditions and health-risk behaviors among persons with serious mental illness: a comprehensive review. Schizophr Bull (2016) 42(1):96–124. doi: 10.1093/schbul/sbv101
15. Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet (2015) 386(9997):964–73. doi: 10.1016/S0140-6736(15)00075-6
16. Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. J Am Med Assoc (2004) 292(14):1724–37. doi: 10.1001/jama.292.14.1724
17. Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med (2014) 370(21):2002–13. doi: 10.1056/NEJMoa1401329
18. Dawes AJ, Maggard-Gibbons M, Maher AR, Booth MJ, Miake-Lye I, Beroes JM, et al. Mental health conditions among patients seeking and undergoing bariatric surgery a meta-analysis. JAMA (2016) 315(2):150–63. doi: 10.1001/jama.2015.18118
19. Mitchell JE, Selzer F, Kalarchian MA, Devlin MJ, Strain GW, Elder KA, et al. Psychopathology before surgery in the longitudinal assessment of bariatric surgery-3 (LABS-3) psychsocial study. Surg Obes Rel Dis (2012) 8:533–41. doi: 10.1016/j.soard.2012.07.001
20. Kalarchian MA, Marcus MD, Levine MD, Soulakova JN, CourCoulas AP, Wisinski MS. Relationship of psychiatric disorders to 6-month outcomes after gastric bypass. Surg Obes Rel Dis (2008) 4:544–9. doi: 10.1016/j.soard.2008.03.003
21. Boeka AG, Prentice-Dunn S, Lokken KL. Psychosocial predictors of intentions to comply with bariatric surgery guideleines. Psychol Health Med (2010) 15:188–97. doi: 10.1080/13548501003615282
22. Toussi R, Fujioka K, Coleman KJ. Pre- and postsurgery behavioural compliance, patient health, and postbariatric surgical weight loss. Obesity (2009) 17:996–1002. doi: 10.1038/oby.2008.628
23. Simon GE, Arterburn DE. Does comorbid psychiatric disorder argue for or against surgical treatment of obesity? Gen Hosp Psychiatry (2009) 31(5):401–2. doi: 10.1016/j.genhosppsych.2009.05.014
24. Thomson L, Sheehan K, Meaney C, Wnuk S, Hawa R, Sockalingam S. Prospective study of psychiatric illness as a predictor of weight loss and health related quality of life one year after bariatric surgery. J Psychosom Res (2016) 86:7–12. doi: 10.1016/j.jpsychores.2016.04.008
25. Fabricatore AN, Crerand CE, Wadden TA, Sarwer DB, Krasucki JL. How do mental health professionals evaluate candidates for bariatric surgery? Survey results. Obes Surg (2006) 16(5):567–73. doi: 10.1381/096089206776944986
26. Steinmann WC, Suttmoeller K, Chitima-Matsiga R, Nagam N, Suttmoeller NR, Halstenson NA. Bariatric surgery: 1-Year weight loss outcomes in patients with bipolar and other psychiatric disorders. Obes Surg (2011) 21(9):1323–9. doi: 10.1007/s11695-011-0373-6
27. Hamoui N, Kingsbury S, Anthone GJ, Crookes PF. Surgical treatment of morbid obesity in schizophrenic patients. Obes Surg (2004) 14(3):349–52. doi: 10.1381/096089204322917873
28. Shelby SR, Labott S, Stout RA. Bariatric surgery: A viable treatment option for patients with severe mental illness. Surg Obes Relat Dis (2015) 11(6):1342–8. doi: 10.1016/j.soard.2015.05.016
29. Fisher D, Coleman KJ, Arterburn DE, Fischer H, Yamamoto A, Young DR, et al. Mental Illness in Bariatric Surgery: A Cohort Study from the PORTAL Network. Obesity (2017) 25:850–6. doi: 10.1002/oby.21814
30. Fuchs HF, Laughter V, Harnsberger CR, Broderick RC, Berducci M, DuCoin C, et al. Patients with psychiatric comorbidity can safely undergo bariatric surgery with equivalent success. Surg Endosc (2016) 30(1):251–8. doi: 10.1007/s00464-015-4196-8
31. Archid R, Archid N, Meile T, Hoffmann J, Hilbert J, Wulff D, et al. Patients with Schizophrenia Do Not Demonstrate Worse Outcome After Sleeve Gastrectomy: a Short-Term Cohort Study. Obes Surg (2018) 29(2):506–10. doi: 10.1007/s11695-018-3578-0
32. Kouidrat Y, Amad A, Stubbs B, Moore S, Gaughran F. Surgical Management of Obesity Among People with Schizophrenia and Bipolar Disorder: a Systematic Review of Outcomes and Recommendations for Future Research. Obes Surg (2017) 27(7):1880–95. doi: 10.1007/s11695-017-2715-5
33. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
34. Patton MQ. Qualitative evaluation and research methods (2nd edition). Newbury Park, CA: Sage (1990).
35. Bocchieri LE, Meana M, Fisher BL. Perceived psychosocial outcomes of gastric bypass surgery: a qualitative study. Obes Surg (2002) 12(6):781–8. doi: 10.1381/096089202320995556
36. Jumbe S, Meyrick J. Contrasting views of the post-bariatric surgery experience between patients and their practitioners: A qualitative study. Obes Surg (2018) 28(2):2447–56. doi: 10.1007/s11695-018-3185-0
37. Huthwaite M, Elmslie J, Every-Palmer S, Grant E, Romans SE. Obesity in a forensic and rehabilitation psychiatric service: a missed opportunity? J Forensic Pract (2017) 19(4):269–77. doi: 10.1108/JFP-03-2017-0007
Keywords: mental illness, psychosis, obesity, bariatric surgery, qualitative research, discrimination
Citation: Every-Palmer S, Romans SE, Stubbs R, Tomlinson A, Gandhi S and Huthwaite M (2020) Experiences of Weight-Loss Surgery in People With Serious Mental Illness: A Qualitative Study. Front. Psychiatry 11:419. doi: 10.3389/fpsyt.2020.00419
Received: 21 June 2019; Accepted: 23 April 2020;
Published: 12 May 2020.
Edited by:
Christian Huber, University Psychiatric Clinic Basel, SwitzerlandReviewed by:
Umberto Volpe, Marche Polytechnic University, ItalyYoussef Kouidrat, Assistance Publique – Hôpitaux de Paris, France
Copyright © 2020 Every-Palmer, Romans, Stubbs, Tomlinson, Gandhi and Huthwaite. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanna Every-Palmer, susanna.every-palmer@otago.ac.nz
 Susanna Every-Palmer
Susanna Every-Palmer Sarah E. Romans1
Sarah E. Romans1 Richard Stubbs
Richard Stubbs