- 1Department of Biotechnological and Applied Clinical Sciences (DISCAB), University of L’Aquila, L’Aquila, Italy
- 2Department of Mental Health, ASL 1, L’Aquila, Italy
- 3Department of Mental Health, Psychiatric Service of Diagnosis and Treatment, ASL, Rieti, Italy
- 4Department of Systems Medicine, Tor Vergata University of Rome, Rome, Italy
Several studies investigated the role of resilience as a mediating factor for psychopathological phenotypes. The aim of the current study is to explore the putative role of resilience as a mediator between different vulnerability factors and depressive symptoms. One hundred and fifty patients with a major depressive disorder diagnosis have been evaluated on the basis of humiliation (Humiliation Inventory), adverse past family experiences (Risky Family Questionnaire), hopelessness (Beck Hopelessness Scale), and resilience (Resilience Scale for Adult) scores. A multiple regression analysis and a bootstrapping method were carried out to assess the hypothesis that resilience could mediate the relationships between these risk factors as predictors and hopelessness as a dependent variable. Our results show that resilience has a mediating role in the relationship between several risk factors that are specifically involved in interpersonal functioning and hopelessness. The main limitations of the study are the cross-sectional nature of the study, the use of self-report instruments, the lack of personality assessment, and the consideration of the resilience as a unique construct. The understanding of the mechanisms through which resilience mediates the effects of different interpersonal risk factors is crucial in the study of depression. In fact, future prevention-oriented studies can also be carried out considering the mediating role of resilience between interpersonal risk factors and depressive symptoms.
Introduction
Depression is one of the most disabling mental disorders, showing a heterogeneous clinical presentation (1) and it is related to different risk factors such as biological, psychological, and environmental (2). The relationship between risk factors for depression is complex, involving several interconnected pathways which can eventually shape the clinical presentation and outcome of depressed patients (3, 4).
Risk factors for depression include negative interpersonal experiences, such as enduring humiliation and early exposure to a dysfunctional familial environment. Farmer and McGuffin (5) studied the relationship between humiliation and depression showing that humiliating events may have a role in the onset of depression. Indeed, humiliating experiences, such as discrimination, social isolation, and rejection could trigger a depressive episode (6, 7). In fact, the enduring fear of being humiliated is considered one of the pathogenic negative beliefs in depression (8). Moreover, early humiliating experiences, such as bullying and peer victimization, are associated with hopelessness, depression, and suicidality (9).
Early adverse family experiences are a major risk factor for depression (10). Growing up in families characterized by conflicts, violence, and a cold, unsupportive and neglectful parental style results in a higher probability of childhood trauma (11), disruption of psychosocial functioning (12), and depressive symptoms. Specifically, lack of a supportive family during childhood could prevent the development of positive beliefs about one’s own self, others, and the future, increasing the likelihood of hopelessness (13).
Hopelessness can be defined as the negative expectations about future situations and events which could involve the self and the others (14). People who have these negative expectations think they cannot solve their problems, they never reach their goals (14), and that there will be more negative than positive times in their future (15). Beck considers hopelessness as the third component of his cognitive negative triad of depression which already involves the self and the world/environment (16, 17). Hopelessness is often reported in depressed and schizophrenic patient’s cases (18).
Hopelessness can be related to the interpersonal dynamics, as an inadequate parenting style. In particular, the parents use parental tactics, such as guilty or withdrawal of affection to manipulate the child’s emotional and psychological state. As a consequence, children who live with these parents can believe that they have no personal control regarding school activities, and they consider negative events as uncontrollable and overwhelming (19, 20). Moreover, hopelessness can also be related to personality characteristic as emotional instability (21). In the previous case, we can define hopelessness as “learned helplessness” (19–21).
The above-mentioned risk factors could have a direct effect on depressive symptoms; however, they could indirectly affect depression acting through a third mediating variable such as resilience which refers to positive adaptation, or ability to maintain or regain mental health, despite experiencing adversity. Its nature is dynamic throughout the lifespan and interacts with major domains of life functioning, such as intimate relationships and attachment (22). Resilience represents a protective factor against the development of psychiatric symptoms acting as a mediator in the relationship between risk factors and depressive symptoms. Several cross-sectional studies analyzed the mediating role of resilience in the relationship between risk factors and depression, in both clinical (23) and non-clinical populations (24, 25). For example, stigma and avolition were found to be connected to depression by the mediation of resilience in a population of schizophrenic patients (23). The relationship between stress and anxiety and depression in a non-clinical sample is partially mediated by resilience (24). Moreover, the self-perceived competence, considered a personal resilience factor, has been found to be a mediator (but not a moderator) of the relationship between stressful life events and depression in a sample of 9-th grade students during a two-wave longitudinal study. In fact, the direct effect of negative events on depressive symptoms diminished after controlling for self-perceived competence (25). However, resilience has been also considered as a moderator of the effect of risk factors on depressive symptoms. For example, resilience has shown a moderating effect on depressive symptoms severity in individuals exposed to childhood abuse or traumas (3). In addition, social resilience, but not familial resilience, has been found to moderate the effect on depression in adults with a history of familial childhood abuse (26).
Despite the potential role of resilience as mediator between interpersonal depressive risk factors and hopelessness, previous studies did not consider this topic in depth even beyond the field of clinical depression (23). Therefore, the aim of this study is to investigate the putative role of resilience as a mediator between humiliation, adverse early family experiences, and hopelessness in a sample of depressed subjects. We previously reported that depression, resilience, humiliation, and adverse early family experiences are connected to each other. In particular, resilience has negative relation with humiliation, adverse early family experiences, and depression, showing a buffering effect in clinical and non-clinical samples (7, 27, 28). Therefore, we hypothesized that the relationships between adverse early family experiences and humiliation (as predictors) and hopelessness (as outcome) could be significantly mediated by resilience.
Materials and Methods
Participants
One hundred fifty consecutively admitted patients [70 males, 80 females; mean age 41.3 + 10.6 (SD); age range 19–64] for an index depressive episode were recruited from a psychiatry unit. All had a primary diagnosis of major depressive disorder (ICD-10, code F32) made by three senior psychiatrists (AR, FP, and MB). The patients were recruited at the admission and were currently being treated for depression with a homogeneous pharmacological treatment. No patients were treated with a psychotherapy approach. All patients have been hospitalized for a period of 10–14 days. The recruited patients were considered to be “severe cases” because they showed a score >2 in the depression subscale of the Brief Symptom Inventory, according to the results reported in a previous study based on an inpatient population (29). Patients with bipolar disorder, dementia, psychotic symptoms, and other diagnosis were excluded from the study. The questionnaires were administered to patients using a randomized presentation to avoid the order effect after 7 days from the admission. Eligible and available subjects provided written informed consent after receiving a complete description of the study and having an opportunity to ask questions. They then completed the self-report questionnaires in a light and quiet room. The average time to complete the questionnaires has been 23 minutes. The Ethics Committee for Medical Research of the University of L’Aquila (Italy) approved all recruitment and assessment procedures.
Measures and Procedures
Hopelessness was assessed using the Italian version of the Beck Hopelessness Questionnaire (30). It consists of 20 items assessing the prevalence of hopeless thoughts in the past week (31). Participants rated their degree of hopelessness responding “True” or “False” to the questions (item example: “I can’t imagine what my life would be like in ten years”). Evidence of convergent validity of the scale has emerged from findings of negative associations with measures of hope (Hope Scale) and positive future thinking [Life Orientation Test; (32)]. The alpha reliability was 0.92.
Humiliation was assessed using the Italian version of the Humiliation Inventory (7). It consists of 32 items grouped in two dimensions: 20 items assessing the Fear of Humiliation and 12 items assessing the Cumulative Humiliation [item example: “At this point in your life, how much do your fear being scorned?”; (33)]. Participants rated their humiliation experiences on a 5-point Likert scale from 1 (not at all) to 5 (very much). We used the Humiliation total score only has been used and the alpha reliability was 0.97.
Early adverse family experiences were assessed using the Italian version of the Risky Family Questionnaire [RFQ; (34)]. It is composed of 13 items measuring the family background characterized by familial strife, a restrictive parenting style, and chaotic or neglectful parenthood [item example: “How often would you say there was quarreling, arguing, or shouting between a parent and you?”; (35)]. Participants rated aspects of their family environment on 5-point Likert scales ranging from 1 (not at all) to 5 (very often). Alpha reliability was 0.70.
Resilience was assessed using the Italian version of the Resilience Scale for Adult [RSA; (36)]. RSA is a 33 items scale measuring six factors of resilience and a total score (37), four personal factors (Perception of Self, Planned Future, Structured Style, and Social Competence) and two interpersonal factors (Family Cohesion and Social Resources). RSA total score only has been used for this study. Participants rated their resilience on 7-point semantic differential scales (item example: “My close friends and my family: appreciate my qualities □ □ □ □ □ □ □ despise my qualities”). The alpha reliability is 0.83.
Data Analysis
Descriptive statistics were calculated for all variables considered. We also implemented a correlational analysis considering age and hopelessness and adverse early family experiences in order to explorer the hypothetical effect that adverse early family experiences can have in different phases of individual’s development. The relationship between humiliation and adverse early family experiences as independent variables, hopelessness as a dependent variable, and resilience as a mediating variable was assessed using a mediation approach with bootstrapping method in two different mediational models, one for each independent variable.
Results
Descriptive statistics are reported in Table 1.
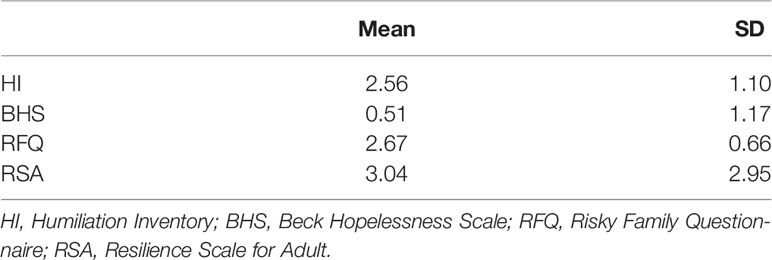
Table 1 Means and standard deviations of humiliation, hopelessness, risky family, and resilience (N = 150).
The above-mentioned correlational analysis (not tabulated analysis) showed that age did not significantly correlate hopelessness but slightly to RFQ (r = −0.21; p < 0.01).
In the first mediation model, humiliation was positively associated with hopelessness (B = 0.07, t (144) = 5.46, p = 0.001) and negatively related to resilience (B = −0.006, t (144) = −4.66, p = 0.001). Resilience was negatively associated with hopelessness (B = −3.89, t (144) = −5.14, p = 0.001). Because both the a-path and b-path were significant, mediation analyses were tested using the bootstrapping method with bias-corrected confidence estimates (38, 39). In the present study, the 95% CI of the indirect effects was obtained with 5000 bootstrap resamples (40). The mediation analysis confirmed that resilience mediated the relation between humiliation and hopelessness (B = 0.02; CI = 0.01 to 0.04). In addition, results indicated that the direct effect of humiliation on hopelessness slightly changed (B = 0.05, t (144) = 3.66, p = 0.003) when controlling for resilience, thus suggesting a small mediation effect. Figure 1 displays the results of the first model.
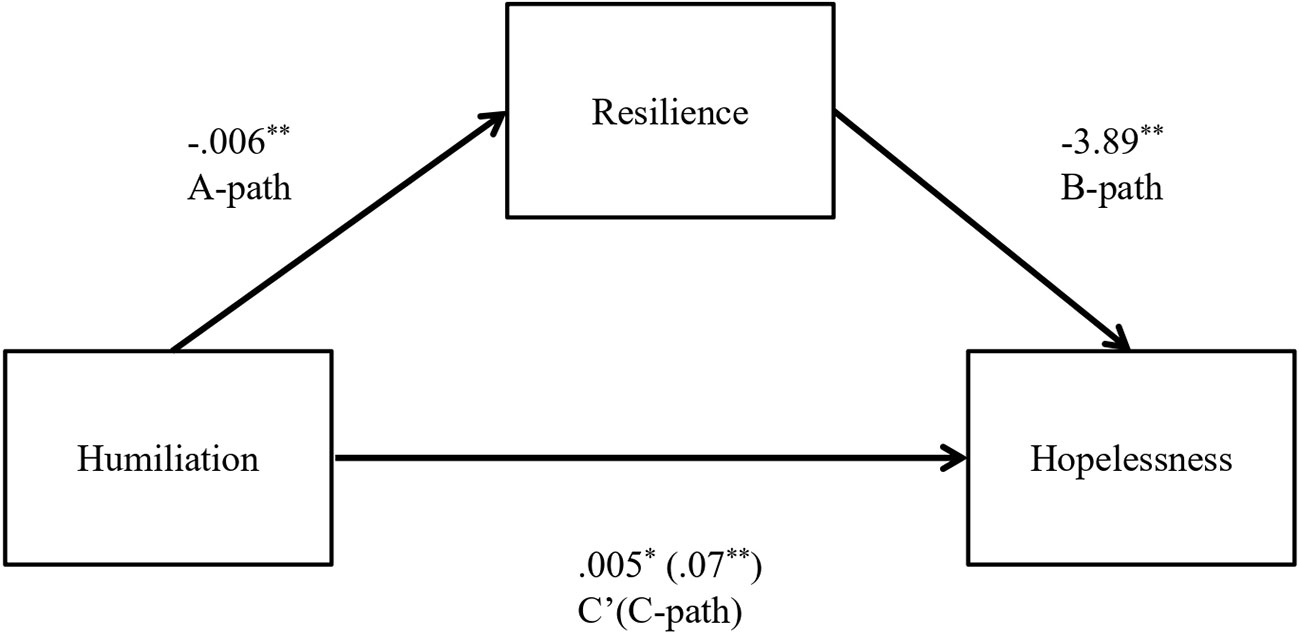
Figure 1 Indirect effect of Humiliation on Hopelessness through Resilience. Note. The unstandardized regression factors are reported. *p < 0.01, **p < 0.001.
In the second model, adverse early family experiences were positively associated with hopelessness (B = 0.23, t (144) = 4.20, p = 0.001) and negatively related to resilience (B = −0.02, t (144) = −4.44, p = 0.001). Resilience was negatively associated with hopelessness (B = −4.25, t (144) = −5.53, p = 0.001). As observed for the first model, both the a-path and b-path were significant. Results of the mediation analysis confirmed a mediating role of resilience in the relation between adverse early family experiences and hopelessness (B = 0.10; CI = 0.05 to 0.16). In addition, results indicated that the direct effect of adverse early family experiences on hopelessness changed (B = 0.13, t (144) = 2.41, p = 0.02) when controlling for resilience, thus suggesting a robust mediation. Figure 2 displays the results of the second model.
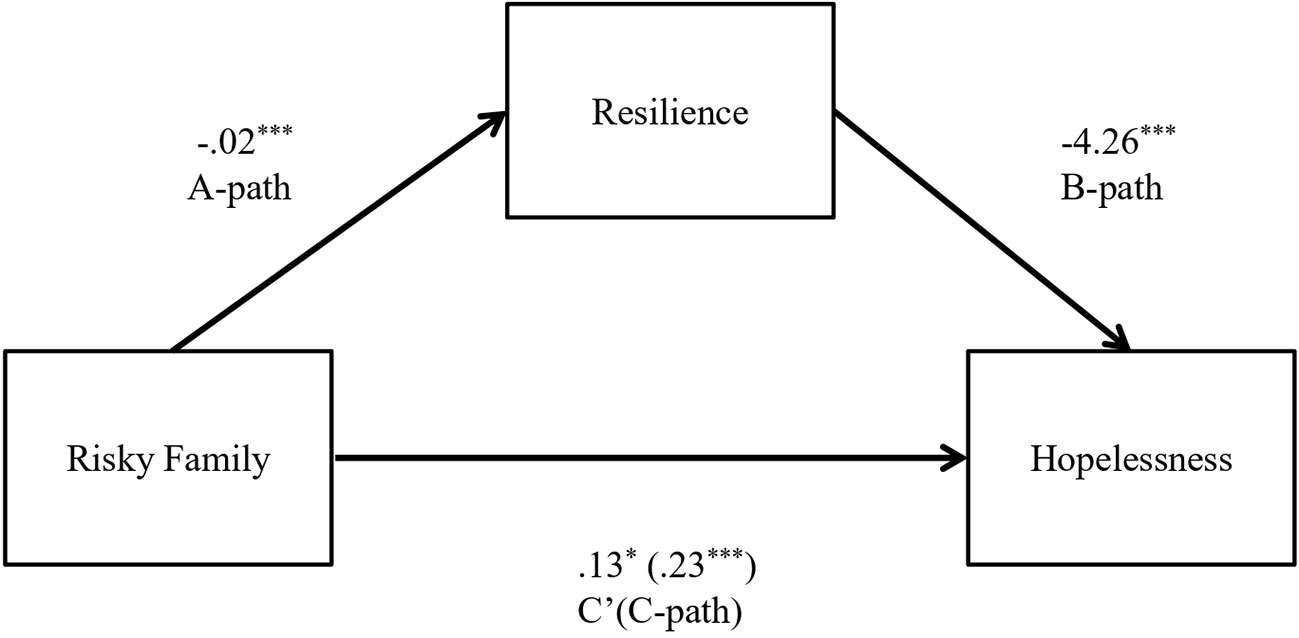
Figure 2 Indirect effect of Risky Family on Hopelessness through Resilience. Note. The unstandardized regression factors are reported. *p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
To the best of our knowledge, this is the first study investigating the putative role of resilience as mediating variable between humiliation, adverse early family experiences (independent variables), and hopelessness (dependent variable) in a sample of depressed patients.
Hopelessness has been considered either a proxy measure of depression or an increased risk factor of suicidality or a moderator of some risk factors toward depression (41).
Adverse early family experiences represent a risk factor that is associated with different mental health disorders throughout the lifetime, including mood disorders, personality disorders, conduct disorders, and psychoses (13). Childhood trauma increases the risk of depression disorders, inappropriate emotion regulation (4), and violent behaviors (42).
Humiliation was also considered a risk factor for depression (7, 27), being associated with sense of entrapment, hopelessness, depression, and suicidal behavior.
Resilience is an ideal mediating variable that may influence the effects of risk factors to depressive symptoms (43, 44). Zimmerman et al. (45) hypothesized that resilience could operate through two main models: the compensatory model, in which resilience could additionally “neutralize” the effect of risk factors, acting independently from them, and the protective factor model in which resilience actually influences the effect of a risk factor interacting with it. In support of a “compensatory” effect of resilience toward depression, individuals with higher levels of resilience showed less psychopathological symptoms than individuals with lower levels of resilience (46). However, within a “protective factor model,” resilience could mediate the effect of negative life events towards psychosocial well-being (47).
Our results underlined the role of resilience as an “intervening variable” in determining the variance of hopelessness, but in different ways. In fact, resilience significantly and directly acts on hopelessness in both models, showing a robust mediation role only between adverse early family experiences and hopelessness. The same role has not been found between humiliation and hopelessness, where the mediation effect is smaller than the previous one. Within the model from humiliation to depressive symptoms, resilience seems not to influence the effect that humiliation exerts on the severity of depressive symptoms (e.g. hopelessness). In fact, resilience does not mitigate the effect of humiliation on hopelessness. On the other hand, resilience significantly acts as mediator between adverse early family experiences and hopelessness. These results confirmed a previous study, where a significant negative correlation between adverse early family experiences and resilience in a non-clinical sample was found, with resilience mediating between adverse early family experiences and the general severity symptoms (48). In the current study resilience displays a protective role between adverse early family experiences and hopelessness, not having the same “strength” between humiliation and hopelessness, thus maintaining a compensatory role. One of the reasons for that could be that resilience is mainly activated as a mediator when the independent variable (in this case adverse early family experiences) is strongly correlated to the dependent one (hopelessness). On the contrary, it does not happen between humiliation and hopelessness.
The effect of a confounding variable cannot be understood and studied only by a mediational model. Resilience itself has been addressed within a moderation framework as well. Although moderation and mediation approaches differ, they both underline the role of a “third intervening variable” in determining the variance of an outcome (i.e. dependent) variable (49). For instance, the moderating effect of resilience on suicidal ideation has been observed in patients with depression and/or anxiety disorders (50). Furthermore, resilience mitigates the development of depression during stressful life events (3, 51), coherently with a moderator function.
This study has important implications for a better comprehension of the importance of resilience, prevention, and treatment of interpersonal stressful factors in depression. In fact, protective factors such as resilience may become a potential target of psychological interventions (52, 53). At the same time, depressive symptoms, such as hopelessness, could negatively influence the patient’s outcome (54). Specifically, preventive interventions could improve the life and the resilient skills of children and avoid the development of depression and mental disorders in adulthood. The primary prevention includes efforts to prevent negative interpersonal events so that children grow up with less exposure to adversities. This prevention is focused on the change of the negative characteristics in the interpersonal environments. One example is the positive parenting program that is aimed to provide targeted education in order to support positive parenting (55). Secondary prevention includes interventions after a negative interpersonal event to reduce the immediate and short-term consequences. Interventions such as psychological first aid (PFA) implemented at school may provide the opportunity to identify at risk children early and to avoid severe psychopathology development (56). Finally, the tertiary prevention includes efforts to treat and reduce long-term consequences of negative interpersonal events. Psychotherapeutic interventions as EMDR are widely used for this goal (57). These two last preventive interventions include the improvement of personal and interpersonal resilient factors useful to counteract the negative consequences of interpersonal events (58).
The main limitations of the study are the cross-sectional approach and the use of self-report instruments. Moreover, the age range of the participants is large, and it has to be considered as a limitation. In fact, the adverse early family experiences could have different effects in different phases/ages of the individual’s development and that could influence the results of this study. However, several hypotheses could explain this relationship, but it is not related to the goal of the study. Finally, the lack of a personality assessment has to be considered as a limitation. It is conceivable that personality traits could influence resilience, the adverse past family and humiliation experiences. Furthermore, we use here resilience as unitary construct; therefore, a more refined analysis considering its components should be conducted in order to have an accurate assessment of the outcomes.
In conclusion, our study investigated the role of resilience as mediator variable between interpersonal factors (i.e. humiliation and adverse early family experiences) and depressive symptoms (i.e. hopelessness). Our results showed that resilience is a significant mediator overall between adverse early family experiences and hopelessness. Future research has to study the mediating role of resilience in depth in order to improve the prevention and the treatment of the negative consequences of interpersonal stressful factors in depression.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The study was carried out in accordance with the recommendations of the Ministry of Health of Italy. All the procedures and the research project were approved by the Ethics Committee for Medical Research of the University of L’Aquila (Italy). All subjects gave written informed consent in accordance with the Declaration of Helsinki. The original ethics approval is available and can be submitted upon request.
Author Contributions
AC made substantial contributions to study design, data acquisition, analyses, and interpretation of results; was involved in manuscript drafting and revision; gave final approval of the final version; and agreed to be accountable for all aspects of the work. PS made substantial contributions to study design and interpretation of results; was involved in manuscript drafting and revision. FP made substantial contributions to study design, analyses, and interpretation of results; was involved in manuscript drafting and revision. AR made substantial contributions to study design, analyses, and interpretation of results; was involved in manuscript drafting and revision. VSa made substantial contributions to study design, data acquisition, analyses, and interpretation of results; was involved in manuscript drafting and revision. MB made substantial contributions to study design, analyses, and interpretation of results; was involved in manuscript drafting and revision. DT made substantial contributions to data acquisition and was involved in manuscript drafting and revision. VSo made substantial contributions to data acquisition and was involved in manuscript drafting and revision. RR made substantial contributions to data acquisition, analyses, and interpretation of results; was involved in manuscript drafting and revision. All authors have read and approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet (2015) 386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4
2. Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacology (2004) 29(10):1765–81. doi: 10.1038/sj.npp.1300506
3. Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord (2010) 126(3):411–4. doi: 10.1016/j.jad.2010.04.009
4. Hopfinger L, Berking M, Bockting CL, Ebert DD. Emotion regulation mediates the effect of childhood trauma on depression. J Affect Disord (2016) 198:189–97. doi: 10.1016/j.jad.2016.03.050
5. Farmer AE, McGuffin P. Humiliation, loss and other types of life events and difficulties: a comparison of depressed subjects, healthy controls and their siblings. Psychol Med (2003) 33(7):1169–75. doi: 10.1038/sj.npp.1300506
6. Torres WJ, Bergner RM. Humiliation: its nature and consequences. J Am Acad Psychiatry Law (2010) 38(2):195–204.
7. Collazzoni A, Capanna C, Bustini M, Stratta P, Ragusa M, Marino A, et al. Humiliation and interpersonal sensitivity in depression. J Affect Disord (2014) 167:224–7. doi: 10.1016/j.jad.2014.06.008
8. Neelapaijit A, Wongpakaran T, Wongpakaran N, Thongpibul K. Pathogenic beliefs among patients with depressive disorders. Neuropsychiatr Dis Treat (2017) 10;13:1047–55. doi: 10.2147/NDT.S136212
9. Meltzer H, Vostanis P, Ford T, Bebbington P, Dennis MS. Victims of bullying in childhood and suicide attempts in adulthood. Eur Psychiatry (2011) 26(8):498–503. doi: 10.1016/j.eurpsy.2010.11.006
10. Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull (2002) 128(2):330–66. doi: 10.1037/0033-2909.128.2.330
11. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) Study. Am J Prev Med (1998) 14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8
12. Talevi D, Pacitti F, Costa M, Rossi A, Collazzoni A, Crescini C, et al. Further exploration of personal and social functioning: the role of interpersonal violence, service engagement and social network. J Nerv Ment Dis (2019) 207(10):832–37. doi: 10.1097/NMD.0000000000001036
13. Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE. Early environment, emotions, responses to stress, and health. J Pers (2004) 72(6):1365–94. doi: 10.1111/j.1467-6494.2004.00300.x
14. Beck AT. Depression: Clinical, experimental, and theoretical aspects. University of Pennsylvania Press: Philadelphia (1967). 370 p.
15. Marchetti I. Hopelessness: a network analysis. Cognit Ther Res (2019) 43(3):611–19. doi: 10.1007/s10608-018-9981-y
16. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford Press: New York (1979). 425 p.
17. Bernstein EE, Kleiman EM, van Bork R, Moriarity DP, Mac Giollabhui N, McNally RJ, et al. Unique and predictive relationships between components of cognitive vulnerability and symptoms of depression. Depress Anxiety (2019) 36(10):950–59. doi: 10.1002/da.22935
18. Beck AT, Steer RA, Beck JS, Newman CF. Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide Life Threat Behav (1993) 23(2):139–45.
19. Sorrenti L, Filippello P, Buzzai C, Costa S. A psychometric examination of the learned helplessness questionnaire in a sample of Italian school students. Psychol Sch (2015) 52(9):923–41. doi: 10.1002/pits.21867
20. Filippello P, Harrington N, Costa S, Buzzai C, Sorrenti L. Perceived parental psychological control and school learned helplessness: the role of frustration intolerance as a mediator factor. Sch Psychol Int (2018) 39(4):360–77. doi: 10.1177/0143034318775140
21. Sorrenti L, Filippello P, Buzzai C, Buttò C, Costa S. Learned helplessness and mastery orientation: the contribution of personality traits and academic beliefs. Nord Psychol (2018) 70(1):71–84. doi: 10.1080/19012276.2017.1339625
22. Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry (2011) 56(5):258–65. doi: 10.1177/070674371105600504
23. Rossi A, Galderisi S, Rocca P, Bertolino A, Rucci P, Gibertoni D, et al. Personal resources and depression in schizophrenia: the role of self-esteem, resilience and internalized stigma. Psychiatry Res (2017) 256:359–64. doi: 10.1016/j.psychres.2017.06.079
24. Anyan F, Hjemdal O. Adolescent stress and symptoms of anxiety and depression: resilience explains and differentiates the relationships. J Affect Disord (2016) 203:213–20. doi: 10.1016/j.jad.2016.05.031
25. Tram JM, Cole DA. Self-perceived competence and the relation between life events and depressive symptoms in adolescence: mediator or moderator? J Abnorm Psychol (2000) 109(4):753–60. doi: 10.1037//0021-843x.109.4.753
26. Powers A, Ressler KJ, Bradley RG. The protective role of friendship on the effects of childhood abuse and depression. Depress Anxiety (2009) 26(1):46–53. doi: 10.1002/da.20534
27. Collazzoni A, Capanna C, Bustini M, Marucci C, Prescenzo S, Ragusa M, et al. A comparison of humiliation measurement in a depressive versus non-clinical sample: a possible clinical utility. J Clin Psychol (2015) 71(12):1218–24. doi: 10.1002/jclp.22212
28. Rossetti MC, Tosone A, Stratta P, Collazzoni A, Santarelli V, Guadagni E, et al. Different roles of resilience in depressive patients with history of suicide attempt and no history of suicide attempt. Braz J Psychiatry (2017) 39(3):216–9. doi: 10.1590/1516-4446-2016-2045
29. Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med (1983) 13(3):595–605. doi: 10.1017/S0033291700048017
30. Beck AT, Steer RA. Manual for the Beck hopelessness scale. Psychological Corporation: San Antonio, TX (1988).
31. Pompili M, Tatarelli R, Rogers JR, Lester D. The hopelessness scale: a factor analysis. Psychol Rep (2007) 100(2):375–8. doi: 10.2466/pr0.100.2.375-378
32. Steed L. Further validity and reliability evidence for beck hopelessness scale scores in a nonclinical sample. Educ Psychol Meas (2001) 61(2):303–16. doi: 10.1177/00131640121971121
33. Hartling LM, Luchetta T. Humiliation: assessing the impact of derision, degradation, and debasement. J Prim Prev (1999) 19(4):259–78. doi: 10.1023/A:1022622422521
34. Benedetti F, Radaelli D, Poletti S, Falini A, Cavallaro R, Dallaspezia S, et al. Emotional reactivity in chronic schizophrenia: structural and functional brain correlates and the influence of adverse childhood experiences. Psychol Med (2011) 41(3):509–19. doi: 10.1017/S0033291710001108
35. Taylor SE, Lehman BJ, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to adult C-reactive protein in the coronary artery risk development in young adult study. Biol Psychiatry (2006) 15;60(8):819–24. doi: 10.1016/j.biopsych.2006.03.016
36. Capanna C, Stratta P, Hjemdal O, Collazzoni A, Rossi A. The Italian validation study of the resilience scale for adults. (RSA) BPA (2015) 63(272):16–24.
37. Hjemdal O, Friborg O, Braun S, Kempenaers C, Linkowski P, Fossion P. The Resilience scale for adults: construct validity and measurement in a Belgian sample. IJT (2011) 11(1):53–70. doi: 10.1080/15305058.2010.508570
38. Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivar Behav Res (2004) 39(1):99. doi: 10.1207/s15327906mbr3901_4
39. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput (2004) 36(4):717–31. doi: 10.3758/bf03206553
40. Preacher KJ, Hayes AF. A symptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods (2008) 40(3):879–91. doi: 10.3758/brm.40.3.879
41. Johnson J, Wood AM, Gooding P, Taylor PJ, Tarrier N. Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev (2011) 31(4):563–91. doi: 10.1016/j.cpr.2010.12.007
42. Talevi D, Imburgia L, Luperini C, Zancla A, Collazzoni A, Rossi R, et al. Interpersonal violence: identification of associated features in a clinical sample. Child Abuse Negl (2018) 86:349–57. doi: 10.1016/j.chiabu.2018.08.017
43. Haeffel GJ, Grigorenko EL. Cognitive vulnerability to depression: exploring risk and resilience. Child Adolesc Psychiatr Clin N Am (2007) 16(2):435–48. doi: 10.1016/j.chc.2006.11.005
44. Rutten BP, Hammels C, Geschwind N, Menne-Lothmann C, Pishva E, Schruers K, et al. Resilience in mental health: linking psychological and neurobiological perspectives. Acta Psychiatr Scand (2013) 128(1):3–20. doi: 10.1111/acps.12095
45. Zimmerman MA, Stoddard SA, Eisman AB, Caldwell CH, Aiyer SM, Miller A. Adolescent resilience: promotive factors that inform prevention. Child Dev Perspect (2013) 7(4):215–20. doi: 10.1111/cdep.12042
46. Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther (2006) 44(4):585–99. doi: 10.1016/j.brat.2005.05.001
47. Faircloth AL. Resilience as a mediator of the relationship between negative life events and psychological well-being. [dissertation]. Georgia Southern University: Statesboro (GA) (2017).
48. Collazzoni A, Stratta P, Tosone A, Rossetti MC, D’Onofrio S, Rossi A. Different roles of resilience in a non-clinical sample evaluated for family stress and psychiatric symptoms. PAID (2016) 100:12–5. doi: 10.1016/j.paid.2015.12.007
49. MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci (2000) 1(4):173–81. doi: 10.1023/a:1026595011371
50. Min JA, Lee CU, Chae JH. Resilience moderates the risk of depression and anxiety symptoms on suicidal ideation in patients with depression and/or anxiety disorders. Compr Psychiatry (2015) 56:103–11. doi: 10.1016/j.comppsych.2014.07.022
51. Hjemdal O, Friborg O, Stiles TC, Rosenvinge JH, Martinussen M. Resilience predicting psychiatric symptoms: a prospective study of protective factors and their role in adjustment to stressful life events. Clin Psychol Psychother (2006) 13(3):194–201. doi: 10.1002/cpp.488
52. Waugh CE, Koster EH. A resilience framework for promoting stable remission from depression. Clin Psychol Rev (2015) 41:49–60. doi: 10.1016/j.cpr.2014.05.004
53. Bitsika V, Sharpley CF, Peters K. How is resilience associated with anxiety and depression? analysis of factor score interactions within a homogeneous sample. Ger J Psychiatry (2010) 13(1):9–16.
54. Pompili M, Innamorati M, Gonda X, Serafini G, Sarno S, Erbuto D, et al. Affective temperaments and hopelessness as predictors of health and social functioning in mood disorder patients: a prospective follow-up study. J Affect Disord (2013) 150(2):216–22. doi: 10.1016/j.jad.2013.03.026
55. Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics (2012) 129(1):e232–46. doi: 10.1542/peds.2011-2663
56. Garner AS. Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics (2013) 132(Suppl 2):S65–73. doi: 10.1542/peds.2013-1021D
57. Shapiro F. Eye movement desensitization and reprocessing (EMDR) therapy: basic principles, protocols, and procedures. Guilford Publications: New York City (2017).
Keywords: resilience, mediator, mediation, hopelessness, humiliation, adverse early family experiences, interpersonal risk factor, depression
Citation: Collazzoni A, Stratta P, Pacitti F, Rossi A, Santarelli V, Bustini M, Talevi D, Socci V and Rossi R (2020) Resilience as a Mediator Between Interpersonal Risk Factors and Hopelessness in Depression. Front. Psychiatry 11:10. doi: 10.3389/fpsyt.2020.00010
Received: 18 November 2019; Accepted: 06 January 2020;
Published: 28 February 2020.
Edited by:
Gabriella Martino, University of Messina, ItalyReviewed by:
Luana Sorrenti, University of Messina, ItalyMarianna Alesi, University of Palermo, Italy
Copyright © 2020 Collazzoni, Stratta, Pacitti, Rossi, Santarelli, Bustini, Talevi, Socci and Rossi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dalila Talevi, ZGFsaWxhLnRhbGV2aUBnbWFpbC5jb20=
 Alberto Collazzoni
Alberto Collazzoni Paolo Stratta
Paolo Stratta Francesca Pacitti
Francesca Pacitti Alessandro Rossi
Alessandro Rossi Valeria Santarelli2
Valeria Santarelli2 Massimiliano Bustini
Massimiliano Bustini Dalila Talevi
Dalila Talevi Valentina Socci
Valentina Socci Rodolfo Rossi
Rodolfo Rossi