
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 18 February 2020
Sec. Child and Adolescent Psychiatry
Volume 10 - 2019 | https://doi.org/10.3389/fpsyt.2019.00933
This article is part of the Research Topic Strengthening Child and Adolescent Mental Health (CAMH) Services and Systems in Lower-and-Middle-Income Countries (LMICs) View all 16 articles
Background: In low- and middle-income countries, rates of common mental health disorders are found to be very high among children and adolescents while individuals, particularly in these countries, face barriers to mental health care. In the recent years, randomized controlled trials (RCTs) have been conducted that implemented and tested different psychological and psychosocial treatment approaches to treat common mental disorders. This review aims to analyze psychological interventions among children and adolescents in low- and middle-income countries.
Methods: RCTs carried out in low- and middle-income countries on psychological and psychosocial interventions for children and adolescents with symptoms of trauma- and stressor related disorders, depression or anxiety were identified in bibliographic databases. Databases were systematically searched until December 14, 2018. Effect sizes indicating differences between treatment and control groups at post-test were computed using a random-effects model. Outcomes were symptoms of depression, anxiety and posttraumatic stress disorder (PTSD).
Results: Thirteen studies with a total of 2,626 participants aged between 5 and 18 years were included. Treatments varied between studies and number of treatment sessions ranged from 1 to 16. The pooled effect size, combining outcomes of depression, anxiety and PTSD of psychological or psychosocial intervention versus care-as-usual or a control conditions yielded a medium effect (g = 0.62; 95% CI: 0.27–0.98). Heterogeneity was very high (I2 = 94.41; 95% CI = 80–91). The beneficial effect of interventions increased after excluding outliers (g = 0.72; 95% CI: 0.37–1.07), while heterogeneity remained high (I2 = 86.12; 95% CI = 87–94).
Conclusion: High quality RCTs investigating the effect of psychological and psychosocial interventions on PTSD, depression and anxiety among children and adolescents in low- and middle-income countries are scarce. Results of the available studies may suggest that psychological and psychosocial interventions might be more effective in reducing symptoms of anxiety, depression and PTSD compared to control conditions. Due to very high heterogeneity, this evidence must be considered with caution.
Approximately one third of the total population in low- and middle-income countries are children and adolescents aged below 18 (1). Future projections see a world population shift towards an older age structure (2). Currently many western countries already face high old age dependency ratios, while many low-income countries, are considered as regions with a high “child dependency ratio,” among them most sub-Saharan African countries and parts of Asia. This means that here there are more than 45 children per 100 working age individuals (ages 15 to 64) (2). These individuals, being the majority of the world’s children and adolescents, receive on average less than US$0.01 assistance for mental health (3). Yet, prevalence estimates for youth in low- and middle-income countries range from 8–27% for anxiety symptoms, 0–28% for depressive symptoms, and for posttraumatic stress disorder (PTSD) estimates range from 0.2% to as high as 87% in adolescents who experienced traumatic events (4). Furthermore, results from the Global Burden of Disease study 2013 reveal that for children and adolescents aged 10 to 19, depressive disorders are one of the leading causes of years lived with disability (5).
When comparing prevalence rates of children and adolescents in high income countries to those in low- and middle-income countries, often a large variability has been found which has largely been attributed to methodological limitations, such as that diagnostic categories often have been developed and tested in high income countries (6). These issues impose problems when comparing prevalence rates across societies (6–8).
A number of trials have been conducted to investigate the effect of psychological and psychosocial interventions. In high income countries, psychotherapies have been found to be effective in treating common mental disorders (9, 10). In low- and middle-income countries studies focusing on adult populations have shown that psychological therapies can reduce symptoms of PTSD, depression and anxiety (11). Considering the effectiveness of psychological and psychological interventions for children and adolescents in low- and middle-income settings, meta-analyses which evaluate the evidence of RCTs examining these interventions are still lacking.
The trials that have been conducted with children and adolescents implemented various forms of psychological and psychosocial treatments, such as school-based treatments, parent- and family-focused interventions, psychoeducational and/or supportive interventions, all of which can include components of cognitive behavioral and exposure based techniques, expressive techniques and mind–body oriented skills (12). Although recommendations advise adjusting an intervention to its target group by making cultural adaptions, these are not commonly implemented or are poorly reported (11, 13, 14).
The majority of the reviews that have previously been conducted to test which of these psychological treatments are most effective focused on children and adolescents who witnessed or experienced adverse events through war or humanitarian crisis (11, 13, 15, 16). However, these reviews did not take into account the general population of children and adolescent in low-and middle-income countries. Singla et al. (17)Klasen and Crombag (18) Yatham et al. (4) and Pedersen et al. (19) performed systematic reviews on interventions for youth in low- and middle-income countries, however, these reviews were not conducted as a meta-analysis, therefore, results were not reported with statistical evidence. Likewise, Purgato et al. (12) analyzed focused psychosocial interventions for children in low-resource humanitarian settings. This review was performed as an individual patient data meta-analysis in a limited target group. Results showed a small positive effect of focused psychosocial interventions on PTSD symptoms but not for depression and anxiety (11).
To our knowledge no recent meta-analysis is currently available that provides results of psychological and psychosocial treatments for children and adolescents in low- and middle-income countries for symptoms of common mental health disorders. This meta-analysis aims to review the effectiveness of psychological and psychosocial interventions for children and adolescents that are focused on the treatment of trauma- and stressor related disorders and depression and anxiety in low- and middle-income countries.
The present review was registered on PROSPERO under the following ID: CRD42019111558. No specific funding was available for this review (20).
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) we predefined our research question in regards to Population, Intervention, Comparison, Outcome and Study (PICOS) Table 1 (21). We included studies that were conducted as randomized controlled trials (RCTs) or cluster randomized controlled trials (cRCTs) in a low- middle-income country as defined by the World Bank (22). Studies had to implement a psychological intervention and an active or non-active comparison group had to be included.
We included children and adolescents below the age of 18 who met diagnostic criteria for any of the anxiety, depressive disorders and/or trauma- and stressor-related disorders (as classified by DSM-5) based on a clinical diagnostic interview or scored above a specified cut-off on a self-report instrument (23). Furthermore, children and adolescents had to be living in low- and middle-income countries defined by the World Bank.
As outcomes we defined measures of symptoms of anxiety, depression or symptoms of PTSD measure by an interview or self-report instrument.
A review protocol was developed based on the PRISMA-statement. A comprehensive search was performed in the bibliographic databases PubMed, Embase.com, and EBSCO/PsycINFO, in collaboration with a medical librarian. Databases were searched from inception until December 14, 2018. The following terms were used as index terms or free-text words (including synonyms and closely related words):
“Developing countries,” “Low- and middle-income countries,” “Anxiety disorders,” “Depressive disorders,” “Children,” and “Adolescents.” The search was performed without restrictions on date, language or publication status. Duplicate articles were excluded. The complete search strings for all databases can be found in Table 2–4. Titles and abstracts were screened by one author based on pre-defined inclusion criteria. The full-texts were then retrieved from the selected studies and rated by two authors. Data then was extracted from the included studies.
Data was extracted on an Excel sheet by two independent researchers. Information on study design, country, assessment instrument, blinding of assessors, type of comparison, type of therapy, treatment provider, fidelity assessment, theoretical background, duration of therapy, number of sessions and format of therapy, in- and exclusion criteria of participants, number of participants, gender, mean age, standard deviation and age range of participants, pre-treatment, post-treatment and follow-up assessment means standard deviations or mean differences and standard deviations of change scores for both intervention and control groups were recorded. Discrepancies were discussed and resolved.
Quality of studies was assessed by two independent reviewers. Version 2 of the Cochrane risk-of-bias tool (RoB 2) was used to perform quality assessment (24). Randomized controlled trials were assessed with RoB 2 for randomized controlled trials, and cluster randomized controlled trials were respectively assessed with RoB 2 for cluster randomized controlled trials. In both, assessments studies were evaluated on the following paradigms: Bias arising from the randomization process; bias arising from the timing of identification and recruitment of individual participants in relation to randomization; bias due to deviations from intended interventions; bias due to missing outcome data; bias in measurement of the outcome, and bias in selection of the reported result. All paradigms inherit specific questions concerning the study that are answered with either “yes,” “probably yes,” “no,” “probably no” or “no information.” These questions guide the decision to evaluate a paradigm, and therewith, the risk of bias in a study with either “low risk,” “some concerns” or “high risk.” The Cochrane tool provides an algorithm to guide the final evaluation into one of the three categories. Questions within the paradigms differ slightly between the assessment for individual randomized trials and cluster randomized trials. Finally, an overall rating of the study was made based on the aforementioned ratings of the five paradigms.
Data analysis was performed with the software Comprehensive Meta-Analysis (CMA) version 3 (25). Data was compiled from Intention to treat samples (ITT) of the studies when available. Completer samples were used when ITT samples were not reported. Standardized mean differences (Hedges’ g) were calculated as a measure of effect size. Hedges’ g is calculated by first subtracting the posttest mean of the treatment group from the posttest mean of the control group and then dividing by the pooled standard deviations of both groups. In this study, this measure was utilized to indicate the difference between the treatment and control condition at post-test. In some studies, mean and standard deviations were not reported but mean change scores were provided. In these cases, Hedges’ g was calculated with the mean change scores and standard deviation differences of each group. If more than one measure of anxiety, depression or symptoms of PTSD was reported, these were all included in the analysis. A random effects model was used due to expected heterogeneity among studies. Heterogeneity was measured with the I2 statistics. We calculated 95% confidence intervals (CI) around I2 (26), using the non-central Chi squared-based approach within the heterogeneity module for Stata (27). To analyze whether characteristics of the studies predicted effect sizes, we performed subgroup analysis. Subgroup analysis was performed using the mixed effects model (28), in which effect sizes within subgroups are pooled according to the random effects model and the difference between subgroups according to a fixed effects model. Subgroup analyses were performed between cluster and individual randomized controlled trials, studies with different risk of bias assessment and between studies with a waitlist control condition and a non-waitlist control condition. Sensitivity analysis was computed in which potential outliers were excluded. Outliers were defined as studies of which the 95% CI of the effect size did not overlap with the 95% CI of the pooled effect size. Finally, publication bias was examined with Duval and Tweedie’s trim and fill procedure and the Egger’s test of asymmetry (29).
After identifying 2,249 articles in bibliographic databases, records were de-duplicated and 1,505 titles and abstracts were screened for inclusion. Thereafter, the full-text was retrieved from 126 articles and 1,379 articles were excluded. From the 126 reviewed full-texts, 13 studies were included in the meta-analysis. Reasons for excluding articles to a large extent were due to the lack of a screening assessment or criteria within the studies to ensure that individuals with symptoms of either anxiety, depression or PTSD were recruited. Other reasons to exclude articles were study design, outcome, second report on data included, research not conducted in a LMIC, no psychological treatment or publication type [See PRISMA flow diagram (21), Figure 1]. Seven studies were excluded based on publication type, as the way in which the study was published, e.g. as an abstract, did not provide sufficient data for the meta-analysis.
A total of 13 studies were included in the analysis. In all studies combined, 1,227 participants were enrolled in a psychological intervention and 1,398 participants were enrolled in a control group. One study only recruited girls. Twelve of the studies included in this review were conducted in Asia and Africa, with one study conducted in Southeastern Europe (Kosovo). Out of the studies included, seven were randomized controlled studies, and six were cluster-randomized controlled studies. The number of participants randomized in each study ranged from 15 to 221. The participants included in the studies were aged between 5 and 18 years. Outcomes for depression were reported in ten studies, anxiety in four studies and PTSD in nine studies. Solely one study reported multiple outcomes, for the outcome that was investigated (30). In that study depression was measured with three different outcomes which were all included in this meta-analysis. Psychological treatment was compared to a wait-list control condition in eight studies, four studies compared treatment to a control group and one study utilized treatment as usual (TAU) as a control group which referred to community services available in Zambia (31). The number of treatment sessions ranged from 1 to 16. One study implemented an intervention within an individual format, namely trauma focused CBT (TF-CBT), while the other studies utilized interventions within a group format. These interventions included: 1) Teaching recovery techniques (TRT), which is based on CBT with a focus on symptoms of PTSD wherein individuals are taught coping skills and relaxation techniques with the aim of gradually desensitizing individuals’ phobic avoidance behavior (32), 2) Interpersonal therapy (IPT), 3) Creative play for reducing symptoms of depression, which is facilitated through the expression of thoughts and feelings by art, music, roleplays, games, and discussions (33), 4) Mind body skills group, which also incorporates verbal and nonverbal self-expression activities with the goal to provide individuals with a coping tool to deal with experienced trauma (34), 5) Didactic therapy for the management of stress with coping and appraisal strategies, cognitive behavioral techniques and didactic presentations with work sheets on regulation of emotion and behavior (35), 6) Bibliotherapy, with the aim of reducing depressive symptoms by generating insight into ways of thinking and behaving and replacing maladaptive behavior through reading in a therapeutic setting (30), 7) Spiritual hypnosis, which included reinterpretation the meaning of the traumatic event and expressing emotions (36), 8) (37) CBT, Crisis intervention that encourages the discussion and sharing of traumatic experiences and was facilitated by the use of drawing, games, role-play and talking (38), and 9) School-based interventions which included components of CBT including exposure and creative expressive elements such as drawing and games (39–42). Characteristics of the included studies are also depicted in Table 5.
The risk of bias was assessed separately for individual and cluster randomized controlled trials. Within the individual randomized trials, two studies were rated with an overall high risk of bias. This rating was provided due to: the lack of providing clear description of the plan of analysis, the lack of indicating how many participants completed the interventions, and potential deviations from intended interventions due to awareness of treatment condition and due to a lack of information provided on the analysis used to estimate the effect of assignment to intervention. Other studies were most likely not devoid of the awareness of treatment conditions, however, combined with the aforementioned issues these studies received an overall rating of “high risk.” The major shortcomings within the randomization process and outcome measurement was that not enough information was provided to apprehend how studies randomized. In respect to the outcome measures, the major shortcoming was that assessors were not blinded. Furthermore, two studies received an overall risk of bias rating of “some concerns” due to: randomization process, deviations from intended interventions, measurement of the outcome measure and no comprehensive reporting of analysis plan and actual analysis. Three studies received an overall rating that was considered as signaling “low risk” of bias. Within the risk of bias for cluster randomized trials, four studies received an overall risk of bias rating considered as potentially incorporating “some risk.” This rating was given due to: considerations within the randomization process, no clarity whether outcome data was missing, measurement of the outcome data and potential selection of results. For graphic representation see Figure 2 for cluster randomized- and Figure 3 for individual randomized trials.
This effect of psychological interventions for all outcomes was (g = 0.62; 95% CI: 0.27–0.98) with very high heterogeneity (I2 = 94.41; 95% CI: 80–91). After excluding outliers, the effect size increased to g = 0.72 (95% CI: 0.37–1.07), with very high heterogeneity (I2 = 86.12; 95% CI: 87–94). Five studies were defined as outliers and were excluded (See Figure 4).
For depression symptoms, psychological interventions yielded a medium effect size (g = 0.43; 95% CI: 0.06–0.80) with high heterogeneity (I2 = 94.06; 95% CI: 85–93). Three outliers were detected and excluded, which led to a decrease in the effect size (g = 0.21; 95% CI: −0.05–0.48) with a heterogeneity of I2 = 80.11 (95% CI: 88–95).
For anxiety symptoms, psychological interventions showed a small effect for psychological treatments (g = 0.18; 95% CI: 0.06–0.29) with high heterogeneity (I2 = 96.46; 95% CI: 95–98). The effect of psychological treatments for anxiety dropped to g = 0.06 (95% CI: −0.06–0.17) with low heterogeneity after excluding one outlier (I2 = 0.0; 95% CI: 0–73).
The outcomes for psychological therapies on PTSD symptoms indicated a medium effect size (g = 0.43; 95% CI: 0.10–0.77) with heterogeneity (I2 = 92.86; 95% CI: 86–94). After excluding three studies, which were defined as outliers, the effect size increased to g = 0.50 (95% CI: 0.17–0.83) with high heterogeneity (I2 = 85.54; 95% CI: 91–96) (see Table 6 and 7).
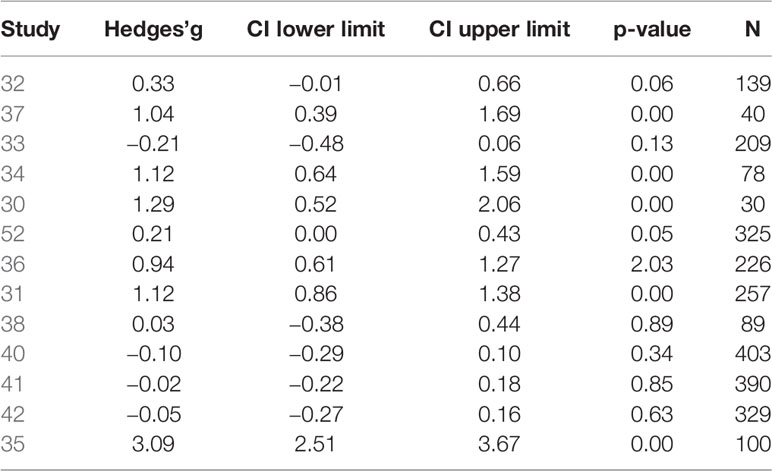
Table 6 Combined outcomes of psychological and psychosocial interventions compared to control conditions.
Examination of the funnel plot indicated significant publication bias. Duvall and Tweedie’s trim and fill procedure suggested that four studies be imputed as a result of publication bias, which resulted in a decreased effect size of g = 0.16 (95% CI: −0.23 ~ 0.56). Furthermore, Egger’s test was significant with an intercept of 7.36 (95% CI: 2.49 ~ 1.87, p = 0.01).
Effect sizes were significantly smaller when waitlist control group was used, (six studies) compared to studies using another control condition (seven studies; p = 0.05). Subgroup analysis also showed that individually randomized studies (seven studies) had significantly higher effect sizes than cRCTs (six studies; p < 0.005). Lastly, studies with high risk of bias (two studies), some risk of bias (six studies) and low risk of bias (five studies) were compared. These results indicated that quality of study was not significantly associated with effect size (p = 0.43).
This meta-analysis reviewed the effect of psychological interventions on symptoms of depression, anxiety, and PTSD in children and adolescents in low- and middle-income countries. Thirteen studies with a total of 2,626 participants fulfilled the predefined inclusion criteria and were included in the analysis. Notably, interventions within the included studies varied greatly from each other. They targeted different symptoms (e.g., anxiety, depression or PTSD) and utilized different treatment approaches with variations in session frequency. Most of the interventions were low-threshold interventions such as school-based interventions. However, some were also more specialized mental health interventions, such as TF-CBT and IPT. Due to very high heterogeneity the results of our meta-analysis should be interpreted with caution.
The result for all pooled outcomes showed a medium to large effect for psychological interventions compared to control conditions. Also, for the outcomes separately a beneficial effect of intervention could be observed. Interventions had a positive effect on the reduction of symptoms of depression (with moderate effect size). Previously, mixed results have been found for the effect of interventions on depression. While Morina etal. (15) report a small to medium effect, Purgato etal. (11) did not find any effect. Further, in the present review a beneficial intervention effect was also found for the treatment of PTSD symptoms. Several other studies have reported a beneficial effect of psychological interventions on symptoms of PTSD (11, 15, 43). Moreover, the included interventions had a positive effect on the treatment of anxiety. However, the observed effect was small. In line with our findings, previous studies in low- and middle-income countries have found some- to no beneficial effect for symptoms of anxiety (11, 43). It is not surprising that the effect for anxiety found in this review was small considering the low number of studies examining anxiety. In addition, the interventions included in this review rarely specifically targeted symptoms of anxiety with evidence-based treatment approaches for anxiety such as exposure (44). The only studies which, to our knowledge, aimed to target anxiety with elements of exposure techniques were school-based interventions, however, it remains unclear how exposure was conducted in these group-based interventions. For all outcomes combined and for symptoms of PTSD, the effect size increased after removing outliers. For symptoms of anxiety and depression, the positive effect of treatment decreased when controlling for outliers.
To investigate the association of specific characteristics of the studies with treatment effectiveness, three subgroup analyses were performed in this review. Within the subgroup analyses that were performed, studies utilizing an individual randomization process were compared to studies utilizing cluster randomization. Results show that individual randomized controlled trials showed a higher effect size compared to cluster randomized trials. An explanation may be higher statistical power to detect differences within individual randomized controlled trials. Furthermore, a significant difference in effect size was found between waitlist control condition and non-waitlist control condition, such as treatment-as-usual or no waitlist. Interestingly, interventions of studies implementing non-waitlist condition were found to be more effective than studies utilizing a waitlist condition. This result is not in line with previous studies (10, 45–47) that showed that the effect of psychotherapy is frequently overestimated when treatments are compared to a waitlist control group. Potentially this result may be explained due to the fact that individuals within the waitlist condition were expecting to receive support and therefore experienced a slight relief in symptoms whereas the non-waitlist condition did not experience this and therefore, more pronounced differences between treatment group and control group could be observed. The number of studies included in the subgroup analysis was small, again, also here conclusion must be taken with caution.
Unfortunately, due to the lack of studies with interventions provided in an individual format, no subgroup analysis could be conducted to analyze whether individual therapy is more effective than group therapy. Interestingly, only one study examined an individually delivered intervention, whereas all other studies evaluated interventions for children and adolescents delivered in group format. Given the lack of health care professionals and the high number of individuals in need of treatment, the group format often is considered as a cost-effective and non-invasive solution. Yet, group interventions may also have disadvantages. For example, stigma and shame may become major barriers hindering individuals from sharing private thoughts and experiences related to symptoms of psychological distress. In addition, it may be more challenging to perform evidence-based strategies such as imaginal or in vivo exposure in group sessions than in individual sessions (48).
A number of limitations must be noted. Only a total number of thirteen studies was included. Not all of these studies assessed all three outcomes. Hence, when looking at anxiety, depression and symptoms of PTSD separately, the number of studies was even smaller and potentially underpowered. This was also particularly was the case for subgroup analysis. Furthermore, heterogeneity was very high for all outcomes. Studies differed in regard to their methods. Different screening measures were used and time of post-assessments varied. Interventions between studies were very different regarding their session frequency, intensity and content. Therefore, high heterogeneity unfortunately may be inevitable and some issues in aggregating and comparing the data of these different studies must be noted. Moreover, one study (35) included in the analysis reported effect sizes that were exceptionally high, which may suggest that results were overestimated. However, this study was excluded within the sensitivity analysis. Additionally, indications for publication bias were observed, which potentially indicates that the true effect size of psychological treatment may be lower than observed. Lastly, the subgroup analysis on quality of studies did not indicate an association between risk of bias and outcome. Yet, more than half of the studies included were classified as either containing some concerns in regard to risk of bias or containing high risk of bias. As also this subgroup analysis was underpowered, the quality may have still had an effect on outcome. These considerations should be taken into account in light of the results found in this review.
The lack of studies implementing and evaluating psychological and psychosocial interventions for children and adolescents in low- and middle-income countries is striking. Considering, that approximately more than half of the world population lives in low-income and lower-middle-income countries (49) and children and adolescents comprise almost half of the populations in these countries, the number of studies we found on children and adolescents is shockingly low. Evidently, more focus needs to be set upon this population, forging more studies to implement effective interventions in this group. Recommendations for interventions include the cultural adaption of an intervention to its target group before it is implemented (50). In most of the studies included in this review, it was unclear if and how the interventions were culturally adapted. To increase effectiveness and acceptability of interventions, cultural adaption should be carried out. Next to cultural adaption, attention should also be given to caregivers when providing children and adolescents with mental healthcare. To our understanding, in none of the interventions were caregivers included. Yet, studies have shown that caregivers play an important role in increasing or reducing the risk of mental illness in children and adolescents (19, 51). Promising interventions that could be implemented have already been constructed, examples of such interventions are KIDNET and EASE (52–54). Narrative exposure therapy (NET) has been evaluated in several high quality trials and has been shown to be effective in treating PTSD in adults (55). KIDNET is a narrative exposure therapy for children, which also has been shown to be effective in reducing symptoms of PTSD and increasing levels of functioning (54). EASE was developed for young adolescents and is the adapted version of the World Health Organization (WHO) developed intervention Problem Management Plus (PM+; WHO, 2016). PM+ is a psychological intervention to reduce psychological distress in populations affected by adversities and is delivered by non-professional helpers (56).
This review suggests that psychological and psychosocial interventions may be effective in reducing symptoms of depression, anxiety, and PTSD for children and adolescents. Results must, however, be considered preliminary since the evidence is not yet strong enough to draw definite conclusions. Due to the large heterogeneity between studies, particularly in regard to the methodological approaches, the combined results of the selected studies must be viewed with caution.
The amount of heterogeneity detected in this meta-analysis certainly limits the conclusions that can be taken from this review. The issues which have contributed to the amount of heterogeneity are the considerably small number of RCTs found that could be included and the variability between the studies found. To allow for a more effective meta-analyses in this field, it is of primary necessity that these issues be addressed. It would be beneficial if research designs and measures are unified across treatment studies (57). Furthermore, researchers should perform complete and transparent reporting on methodological characteristics, and avoid bias that may distort the results (58).
Finally, considering the high prevalence of these common mental health disorders in low- and middle-income countries and the issue of scarce specialized treatment for mental health in these countries, it is essential that psychological treatments be continuously implemented for children and adolescents. Efforts should be made to investigate whether psychological interventions with individual therapy are more effective than group therapies among children and adolescents with high quality trials. Also, when an intervention is to be implemented, considerations should be made as to whether cultural adaption is required first and whether caretakers can and should be included in the intervention.
JU led the conduction of the meta-analysis. CA-S was the second rater for full-text ratings, extracted data as a second rater and assessed risk of bias as a second rater. PC advised and supervised the conduction of the meta-analysis. RV was in charge of creating the search string and performing the search in bibliographic databases. MS advised and supervised the conduction of the meta-analysis. All authors were actively involved in writing the article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. UNICEF. The State of the World’s Children State of the World’s Children. UN (2016). Available at: https://www.un-ilibrary.org/children-and-youth/the-state-of-the-world-s-children-2016_4fb40cfa-en.
2. Population Reference Bureau. (2018). “World Population Data Sheet 2018.” 2018. http://www.worldpopdata.org/.
3. Lu C, Li Z, Patel V. Global child and adolescent mental health: the orphan of development assistance for health. PloS Med (2018) 15(3):e1002524. doi: 10.1371/journal.pmed.1002524
4. Yatham S, Sivathasan S, Yoon R, Da Silva TL, Ravindran AV. Depression, anxiety, and post-traumatic stress disorder among youth in low and middle income countries: a review of prevalence and treatment interventions. Asian J Psychiatry (2018) 38:78–91. doi: 10.1016/j.ajp.2017.10.029
5. Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, El Bcheraoui C, Moradi-Lakeh M, et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet (London England) (2016) 387(10036):2383–1. doi: 10.1016/S0140-6736(16)00648-6
6. Kieling C, Rohde LA. Going global: epidemiology of child and adolescent psychopathology. J Am Acad Child Adolesc Psychiatry (2012) 51(12):1236–37. doi: 10.1016/j.jaac.2012.09.011
7. Achenbach TM, Rescorla LA, Ivanova MY. International epidemiology of child and adolescent psychopathology i: diagnoses, dimensions, and conceptual issues. J Am Acad Child Adolesc Psychiatry (2012) 51(12):1261–72. doi: 10.1016/j.jaac.2012.09.010
8. Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. “Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization world mental health surveys”. J Am Med Assoc Am Med Assoc (2004) 291(29):2581–90. doi: 10.1001/jama.291.21.2581
9. Cuijpers P. Four decades of outcome research on psychotherapies for adult depression: an overview of a series of meta-analyses. (2017) 58(1):7–19. doi: 10.1037/cap0000096
10. Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Huibers MJH. “How effective are cognitive behavior therapies for major depression and anxiety disorders? a meta-analytic update of the evidence. World Psychiatry (2016) 15(3):245–58. doi: 10.1002/wps.20346
11. Purgato M, Gross AL, Betancourt T, Bolton P, Bonetto C, Gastaldon C, et al. Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. Lancet Global Health (2018) 6(4):e390–400. doi: 10.1016/S2214-109X(18)30046-9
12. Purgato M, Gastaldon C, Papola D, van Ommeren M, Barbui C, Tol WA. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev (2018) 2018(7):e390–400. doi: 10.1002/14651858.CD011849.pub2
13. Jordans MJD, Tol WA, Komproe IH, De Jong JVTM. Systematic review of evidence and treatment approaches: psychosocial and mental health care for children in war. Child Adolesc Ment Health (2009) 14(1):2–14. doi: 10.1111/j.1475-3588.2008.00515.x
14. Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet (2007) 370(9591):991–1005. doi: 10.1016/S0140-6736(07)61240-9
15. Morina N, Malek M, Nickerson A, Bryant RA. Psychological interventions for post-traumatic stress disorder and depression in young survivors of mass violence in low- and middle-income countries: meta-analysis. Br J Psychiatry (2017) 210(04):247–54. doi: 10.1192/bjp.bp.115.180265
16. Jordans MJD, Pigott H, Tol WA. Interventions for children affected by armed conflict: a systematic review of mental health and psychosocial support in low- and middle-income countries. Curr Psychiatry Rep (2016) 18(1):1–15. doi: 10.1007/s11920-015-0648-z
17. Singla DR, Kohrt BA, Murray LK., Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low- and middle-income countries. Annu Rev Clin Psychol (2017) 13(1):149–81. doi: 10.1146/annurev-clinpsy-032816-045217
18. Klasen H, Crombag Anne Claire. “What Works Where? a systematic review of child and adolescent mental health interventions for low and middle income countries. Soc Psychiatry Psychiatr Epidemiol (2013) 48(4):595–1. doi: 10.1007/s00127-012-0566-x
19. Pedersen GA, Smallegange E, Coetzee A, Hartog K, Turner J, Brown FL, et al. A systematic review of the evidence for family and parenting interventions in low- and middle-income countries: child and youth mental health outcomes. J Child Family Stud (2019) 28(8):2036–55. doi: 10.1007/s10826-019-01399-4
20. Uppendahl JR, Sijbrandij M, Cuijpers P, De Vries R. “Psychological interventions for trauma- and stressor-related disorders and depression and anxiety among children and adolescents in low and middle income countries: a meta-analysis.” (2019).
21. Moher D, Liberati A, Tetzlaff J, Altman DG, Group The PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
22. The World Bank. Classifying Countries by Income. World Development Indicators. (2019) http://datatopics.worldbank.org/world-development-indicators/stories/the-classification-of-countries-by-income.html.
23. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Am Psychiatr Assoc DSM Library. Fifith Edition (2013). doi: 10.5555/appi.books.9780890425596.x00pre
24. Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev 10 no. Suppl 1 (2016) 29–31.
25. Borenstein M, Hedges L, Higgins J, Rothstein H, Biostat, Englewood N. Comprehensive Meta-Analysis Version 3. (2013) Englewood, NJ: Biostat.
26. Loannidis JPA, Patsopoulos NA, Evangelou E Uncertainty in Heterogeneity Estimates in Meta-Analyses. (2007). BMJ Clin Res Ed 335(7626):914–6.
27. Orsini N, Bottai M, Higgins J, Buchan I. HETEROGI: Stata Module to Quantify Heterogeneity in a Meta-Analysis. (2005) Statistical Software Components. Boston College Department of Economics. https://ideas.repec.org/c/boc/bocode/s449201.html
28. Borenstein M, Hedges LVJ, Higgins PT, Rothstein HR. Introduction to meta-analysis. (2009). Chichester, UK: John Wiley and Sons.
29. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-Analysis. Biometrics (2000) 56(2):455–63. doi: 10.1111/j.0006-341X.2000.00455.x
30. Jacob J, De Guzman RG. Effectiveness of taking in the good based-bibliotherapy intervention program among depressed filipino female adolescents. Asian J Psychiatry (2016a) 23:99–107. doi: 10.1016/j.ajp.2016.07.011
31. Murray LK., Skavenski S, Kane JC, Mayeya J, Dorsey S, Cohen JA, et al. Effectiveness of trauma-focused cognitive behavioral therapy among trauma-affected children in Lusaka, Zambia: a randomized clinical trial. JAMA Pediatr (2015) 169(8):761–69. doi: 10.1001/jamapediatrics.2015.0580
32. Barron I, Abdallah G, Heltne U. Randomized control trial of teaching recovery techniques in rural occupied palestine: effect on adolescent dissociation. J Aggression Maltreatment Trauma (2016a) 25(9):955–73. doi: 10.1080/10926771.2016.1231149
33. Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF., et al. interventions for depression symptoms among adolescent survivors of war and displacement in Northern Uganda. Jama (2007) 298(5):519. doi: 10.1001/jama.298.5.519
34. Gordon JS, Staples JK., Blyta A, Bytyqi M, Wilson AT. Treatment of posttraumatic stress disorder in postwar kosovar adolescents using mind-body skills groups: a randomized controlled trial. J Clin Psychiatry (2008) 69(9):1469–76. doi: 10.4088/JCP.v69n0915
35. Zafar H, Khalily M. Didactic therapy for management of stress and co-morbid symptoms of depression and anxiety in pakistani adolescents. Pakistan J Psychol Res (2015) 30(1):131–149.
36. Lesmana CBJ, Suryani LK, Jensen GD, Tiliopoulos N. A spiritual-hypnosis assisted treatment of children with ptsd after the 2002 bali terrorist attack. Am J Clin Hypnosis (2009) 52(1):23–4. doi: 10.1080/00029157.2009.10401689
37. Bella-Awusah T, Ani C, Ajuwon A, Omigbodun O. Effectiveness of brief school-based, group cognitive behavioural therapy for depressed adolescents in South West Nigeria. Child Adolesc Ment Health (2016) 21(1):44–0. doi: 10.1111/camh.12104
38. Thabet AA, Vostanis Panos, Karim Khalid. Group crisis intervention for children during ongoing war conflict. Eur Child Adolesc Psychiatry (2005) 14(5):262–69. doi: 10.1007/s00787-005-0466-7
39. Jordans MJD, Komproe IH, Tol WA, Kohrt BA, Luitel NP, MacY RD, et al. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. J Child Psychol Psychiatry Allied Disciplines (2010) 51(7):818–26. doi: 10.1111/j.1469-7610.2010.02209.x
40. Tol WA, Komproe IH, Susanty D, Jordans MJD, Macy RD, De Jong TM. School-based mental health intervention for children affected by political violence in indonesia. Jama (2008) 300(6):655. doi: 10.1001/jama.300.6.655
41. Tol Wietse A., Komproe Ivan H., Jordans Mark J D, Vallipuram Anavarathan, Sipsma Heather, Sivayokan Sambasivamoorthy, et al. Outcomes and Moderators of a Preventive School-Based Mental Health Intervention for Children Affected by War in Sri Lanka: A Cluster Randomized Trial. World Psychiatry (2012) 11(2):114–22. doi: 10.1016/j.wpsyc.2012.05.008
42. Tol WA, Komproe IH, Jordans MJD, Ndayisaba A, Ntamutumba P, Sipsma H, et al. School-based mental health intervention for children in war-affected burundi: a cluster randomized trial. BMC Med (2014) 12(1):56. doi: 10.1186/1741-7015-12-56
43. Gillies Donna, Taylor Fiona, Gray Carl, O’Brien Louise, D’Abrew Natalie. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database Syst Rev (2012) (12). doi: 10.1002/14651858.CD006726.pub2
44. Parker ZJ, Waller G, Gonzalez Salas Duhne P, Dawson J, Parker Z. Treatment of anxiety disorders: a meta-analysis. Int J Psychol Psychol Ther (2018) 18(1):111–141.
45. Cuijpers P, Cristea IA, Ebert DD, Koot HM, Auerbach RP, Bruffaerts R, et al. Psychological treatment of depression in college students: a metaanalysis. Depression Anxiety (2016) 33(5):400–4. doi: 10.1002/da.22461
46. Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-Analysis. Acta Psychiatr Scand (2014) 130(3):181–92. doi: 10.1111/acps.12275
47. Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosomatics (2009) 78(5):275–84. doi: 10.1159/000228248
48. Miller-Graff LE, Campion K. Interventions for posttraumatic stress with children exposed to violence: factors associated with treatment success. J Clin Psychol (2016) 72(3):226–48. doi: 10.1002/jclp.22238
49. The World Bank. Classifying Countries by Income. World Development Indicators. (2019) http://datatopics.worldbank.org/world-development-indicators/stories/the-classification-of-countries-by-income.html.
50. Harper Shehadeh M, Heim E, Chowdhary N, Maercker A, Albanese E. Cultural adaptation of minimally guided interventions for common mental disorders: a systematic review and meta-analysis. JMIR Ment Health (2016) 3(3):e44. doi: 10.2196/mental.5776
51. Panter-Brick C, Grimon M-P, Eggerman M. Caregiver-child mental health: a prospective study in conflict and refugee settings. J Child Psychol Psychiatry (2014) 55(4):313–27. doi: 10.1111/jcpp.12167
52. Sijbrandij M, Acarturk C, Bird M, Bryant RA, Burchert S, Carswell K, et al. Strengthening mental health care systems for Syrian Refugees in Europe and the Middle East: integrating scalable psychological interventions in eight countries. Eur J Psychotraumatol (2017) 8(sup2):1388102. doi: 10.1080/20008198.2017.1388102
53. Schauer M, Neuner F, Elbert T. Narrative exposure therapy for children and adolescents (KIDNET). In: Evidence-Based Treatments for Trauma Related Disorders in Children and Adolescents Landolt M, Cloitre M, Schnyder U, editors (Cham: Springer International Publishing). (2017). doi: 10.1007/978-3-319-46138-0_11
54. Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7- to 16-year-olds: A randomized controlled trial with traumatized refugee children. J Traumatic Stress (2010) 23(4):437–45. doi: 10.1002/jts.20548
55. Lely JCG, Smid GE, Jongedijk RA, Knipscheer JW., Kleber RJ. The effectiveness of narrative exposure therapy: a review, meta-analysis and meta-regression analysis. Eur J Psychotraumatol (2019) 10(1):1550344. doi: 10.1080/20008198.2018.1550344
56. Brown F, Steen F, Taha K, Aoun M, Bryant R, Jordans M, et al. Early adolescent skills for emotions (EASE) intervention for the treatment of psychological distress in adolescents: study protocol for randomised controlled trials in Lebanon and Jordan. (2019) 20(1):545. doi: 10.1186/s13063-019-3654-3
57. Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, et al. The Lancet Psychiatry Commission on Psychological Treatments Research in Tomorrow’s Science. Lancet Psychiatry (2018) 5(3):237–86. doi: 10.1016/S2215-0366(17)30513-8
Keywords: low- and middle- income countries, children, adolescents, posttraumatic stress disorder, depression, anxiety, meta-analysis, psychological therapy
Citation: Uppendahl JR, Alozkan-Sever C, Cuijpers P, de Vries R and Sijbrandij M (2020) Psychological and Psychosocial Interventions for PTSD, Depression and Anxiety Among Children and Adolescents in Low- and Middle-Income Countries: A Meta-Analysis. Front. Psychiatry 10:933. doi: 10.3389/fpsyt.2019.00933
Received: 15 July 2019; Accepted: 25 November 2019;
Published: 18 February 2020.
Edited by:
Manasi Kumar, University of Nairobi, KenyaReviewed by:
Garumma Tolu Feyissa, Jimma University, EthiopiaCopyright © 2020 Uppendahl, Alozkan-Sever, Cuijpers, de Vries and Sijbrandij. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jana R. Uppendahl, ai5yLnUudXBwZW5kYWhsQHZ1Lm5s
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.