
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry , 27 August 2019
Sec. Addictive Disorders
Volume 10 - 2019 | https://doi.org/10.3389/fpsyt.2019.00579
This article is part of the Research Topic Addiction and Attachment View all 23 articles
Background: Substance use disorders (SUDs) represent a worldwide epidemic with extensive costs to the individual and to society. Occasionally described as an attachment disorder, they have been linked to various impairments in self-regulation and social functioning. However, while there have been significant advances in the development and validation of treatment strategies for SUD in recent years, the components of these treatment approaches have yet to be fully explored. The characteristics of polydrug use disorder (PUD) especially need to be addressed in more detail, as this diagnosis is highly common in individuals seeking treatment, while simultaneously being associated with poor treatment success.
Aim and Scope: This review aims at further exploring the relevance of attachment in PUD and its treatment. To this end, this review provides a concise summary of relevant theories on the development and treatment of SUD in general, including related parameters of attachment, emotion regulation, and neuroscience. Furthermore, several studies focused specifically on PUD are described in more detail. These studies explored the connections between attachment, personality structure, primary and higher emotions (including spirituality), as well as structural and functional neural parameters in inpatients with PUD as well as in healthy controls. Most notably, the described studies highlight that insecure attachment and impairments in personality structure are present in inpatients with PUD. In addition, these characteristics are paralleled by extensive impairments in white matter integrity, especially in tracts connected to facets of emotion regulation.
Conclusions: Based on our findings, we emphasize conceptualization of PUD as an Attachment Disorder, on a behavioral as well as on a neural level. Furthermore, we point out the importance of an integrated bio-psycho-social approach in this research area. Consequently, future studies might more closely focus on the influence of attachment-based interventions on emotion regulation abilities as well as a potentially related neuroplasticity. Neuroplastic changes, which are still rather unexplored, might represent important parameters for the assessment of treatment outcomes especially in long-term SUD treatment.
As it has been suggested that individuals with polydrug use disorder (PUD) differ from individuals with other substance use disorders (SUDs) (1) and that they consequently may need different treatment settings (2), we dedicated five studies to the exploration of attachment and related parameters in inpatients with PUD. In this review, we summarize current theoretical models and empirical results related to the conceptualization of addiction as an attachment disorder before discussing our results on PUD and their implications for future research and clinical practice.
SUDs represent a worldwide public health problem [e.g., Ref. (3)]. As the social, occupational, mental, and physical problems connected to these disorders often persist even after abstinence is achieved, the direct and indirect costs of SUD to the individual and to society are extensive (4). Polydrug use is especially common among drug users worldwide (1). Furthermore, most individuals in treatment for SUD report a PUD (2). As previous studies have suggested numerous differences between PUD and Mono-SUD regarding personality (e.g., impulsivity) as well as etiological (e.g., emotional neglect in childhood) factors (5), it has been suggested that individuals with PUD might even need different treatment settings (2). However, while countless studies have focused on understanding the multifactorial and complex nature of different SUD in order to optimize prevention and treatment, “many challenges remain to understand and treat drug addiction” (p.1) (6).
Bowlby (7) already noted that insecure attachment patterns can help to explain “the many forms of emotional distress and personality disturbances, including anxiety, anger, depression, and emotional detachment, to which unwilling separations and loss give rise” (p. 201). Accordingly, insecure attachment patterns have been extensively discussed as contributing to different facets of personality pathology (8, 9) as well as a large number of other psychiatric diseases, including affective disorders in addition to SUD (10).
Importantly, attachment theory offers the great advantage of not only informing our understanding of the development of psychopathology but also of the development of mental health and well-being. Figure 1 gives a short overview regarding the mechanisms underlying the development and treatment of SUD that will be described in this review.
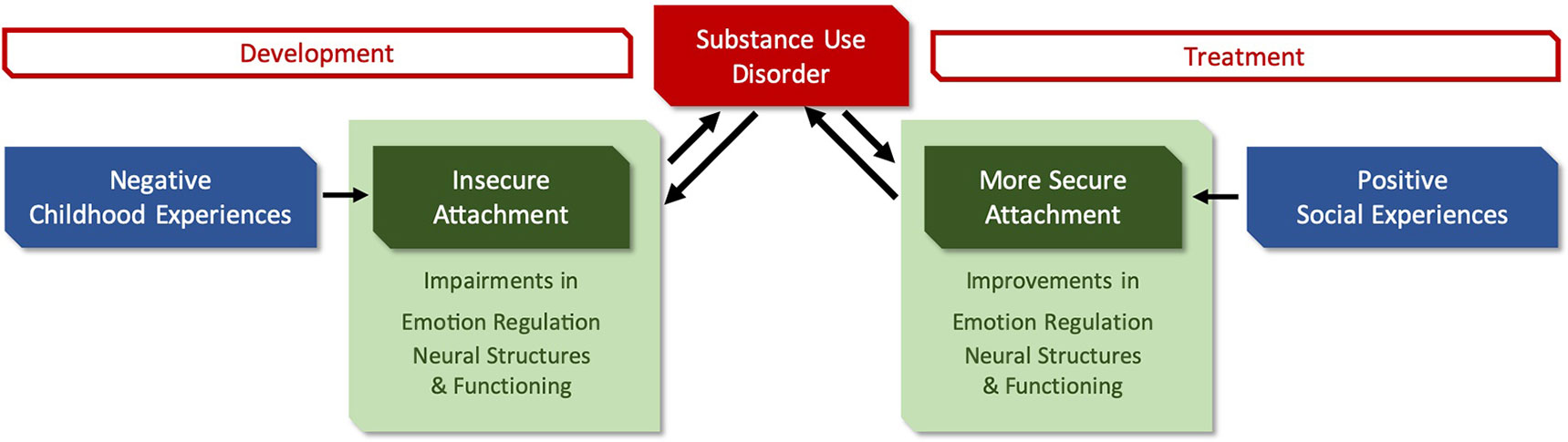
Figure 1 Brief overview of the influence of attachment on SUD. The figure details the role of attachment patterns that form through social experiences, as well as related parameters on the development and treatment of substance use disorders (SUDs).
Consequently, this review aims to describe how insecure attachment (developed in response to negative childhood experiences) leads to diverse vulnerabilities (e.g., impairments in emotion regulation and neural parameters) that may contribute to the development of SUD and that are in turn influenced by the dynamics of SUD. On the other hand, positive social experiences during treatment may promote the development of more secure attachment (including for example improvement in emotion regulation) that supports an increased independence from psychoactive substances (see Figure 1).
In this paper, we will therefore first provide a concise summary of the background relevant for our research on PUD (i.e., attachment theory and its relationship with personality structure, conceptualization of SUD and its relation to attachment in general, neural parameters underlying attachment and emotion regulation, treatment of SUD with a focus on the therapeutic community). Consequently, we will discuss five studies focused on inpatients with PUD undergoing treatment in a therapeutic community setting. Lastly, we will discuss the results of these studies in relation to current research and theoretical models with a special focus on attachment-related parameters (e.g., emotion regulation) and treatment approaches.
As “adaptations to early experiences set the stage for negotiating later experiences” (11), the development of adult psychopathology has to be considered in light of the interactions between earlier experiences, the resulting adaptation, and current contextual parameters (12). Furthermore, most theories of development include the fundamental concept that social relationships both influence and are influenced by the development of psychopathology: Therein, secure attachment is generally thought to act as a protective factor, while insecure attachment is thought to increase the vulnerability for psychopathology [for an overview, see Ref. (13)]. Importantly, however, the possible influence of attachment always has to be considered in the context of other risk factors (14–16) as pathology is unlikely to be caused by a single risk factor.
According to attachment theory, attachment is not a mere secondary drive but has to be seen as a fundamental primary motivation with its own dynamics (17). As it—ideally—establishes a “secure base” from which the individual can explore the world as well as a “safe haven” to retreat to in times of distress (18), the attachment system has an important impact on everyday person–environment interactions (19).
Attachment theory (17, 18, 20) differentiates between a secure attachment style that is established through a sensitive, supportive, and caregiving environment and insecure attachment styles that are the result of an inconsistent, insensitive, or dismissive attachment figure. Mikulincer and Shaver (21) differentiate between two basic attachment dimensions: Anxious attachment and avoidant attachment. Accordingly, secure attachment (low anxious and avoidant attachment) allows the individual to deal with stressful experiences by relying upon mental representations of previously received support or by actively seeking support in the present (22). Individuals with high levels of anxious attachment, characterized by the use of hyperactivating strategies, actively demand support even though they may feel unworthy of love (21). For individuals with high levels of avoidant attachment, characterized by the use of deactivating strategies, they pride themselves on their self-reliance, which in turn can lead to a denial of personal imperfections and weaknesses (23).
Lastly, fearful attachment is defined by high levels of anxious attachment and avoidant attachment (21, 24). While “normal” samples mostly contain individuals with secure attachment (about 70%) (25), individuals with extremely high scores on both anxious attachment and avoidant attachment (i.e., fearful attachment) are most likely to be found in abused or clinical samples [for an overview, see Ref. (26)]. Fearful attachment can furthermore be described as disorganized, since individuals with this attachment style seem unable to develop an organized strategy, whether to rely on hyperactivating or deactivating behaviors to get their attachment needs met [e.g., Ref (22)]. Therefore, rather than enacting and habituating reliable clinging/whining/attention-seeking (hyperactivating) or withdrawing/dissociative (deactivation) behaviors, they simply erupt into some kind of behavior in an effort to relieve stress and may even combine hyper- and deactivation strategies into odd and ineffective responses.
Bowlby, describing the long-lasting effects of attachment across the lifespan (7), has already named early attachment experiences as an important factor influencing personality structure. Essentially, while the internal working models defined by attachment theory have a strong focus on the content and behavioral consequences of mental representations, the concept of personality structure extends this model by adding the complexity of their structural organization and integration. Therefore, individuals with similar attachment patterns might vary regarding the level of integration and differentiation of their internal working models (27, 28). In general, however, more insecure attachment patterns seem to be associated with lower levels of structural integration (i.e., more impairments in personality structure) (29).
A good structural integration is defined by a relatively autonomous self that shows stability as well as flexibility when adequately processing impulses, emotions, and conflicts (30). A moderate structural integration is defined by a tendency towards overcontrolling as well as an increased occurrence of self-destructive impulses. A low structural integration is defined by impaired regulatory functions, which leads to repetitive flooding with intense negative affect as well as (self-) destructive impulses (30). Lastly, a disintegrated structure is defined by the central fear that the sense of self vanishes due to a symbiotic merging of the self and objects (30). Consequently, patients with a low level of structural integration seem to be more likely to experience psychotic symptoms (31), to have a longer duration of mental illness (32), and to be recommended psychiatric instead of psychotherapeutic treatment (33). Conversely, both patients and therapists rate a higher level of structural integration as advantageous for the success of treatment and a change in symptoms (32, 34).
Various forms of SUD, including PUD, have been linked to impairments in the cognitive control of emotions [for an overview, see Ref. (35)].
Importantly, deficiencies in emotion processing and regulation are a known “liability spectrum that underlies many different mental disorders” (p. 154) (36). Developing the capacity for healthy interpersonal affect regulation requires the development of a secure attachment style, as individuals with secure attachment are willing and able to acknowledge and communicate their emotions (37). Therefore, the primary function of adult attachment relationships may be seen in the social regulation of emotions (38).
Consequently, the use of psychotropic substances has been connected to anxious attachment (39, 40), avoidant attachment (41, 42) and disorganized attachment (39, 43, 44). This indicates that the deprivation of developmental needs generally can result in vulnerabilities that in turn lead to misguided attempts at self-repair, leaving the individual “constantly searching for something ‘out there’ that can be substituted for what is missing ‘in there’” (p. 7) (45). This coincides with the psychodynamic point of view that substance abuse “represents a failure to negotiate the transition from helplessness to competence in the social world” (p. 2004) (10). Importantly, the conceptualization of SUDs as an “Attachment Disorder” does recognize that SUDs are not a one-dimensional phenomenon: While substance abuse is initially used by the individual to deal with difficulties in interpersonal relationships, it consequently gradually increases the impairments in “an already fragile capacity for attachment” (p. 2) (45).
Although numerous neurobiological studies in the past few decades focused on attachment in nonhuman animals, such research in humans is relatively limited (46). Consequently, neural circuits underlying attachment are as yet relatively unknown (47). In addition, one has to keep in mind that the attachment behavioral system is highly unlikely to be related to a singly, dedicated attachment circuit, as this higher-order construct makes use of multiple subsystems (e.g., emotion, memory, perception, motivation) (46). In light of these multiple subsystems involved in attachment, it may even be suitable to “think of the entire human brain as an attachment system” (p. 244) (46).
As one of the most important brain structures associated with emotion (48), the amygdala reacts to both unconditioned and conditioned signs of threat (46) and is highly sensitive to facial social signals (49, 50). Together with the hippocampus that is involved in the formation of associations between internal states and environmental stimuli (51), the amygdala consequently enables the identification and consolidation of important interactions with attachment figures as well as emotionally salient situations (46).
Strongly connected to these brain structures, the prefrontal cortex plays an important role in motivation as well as emotion regulation (46, 52, 53). In detail, the prefrontal cortex seems to be connected to attachment through the encoding of “automatic” (conditioned through threat related stimuli) responses to the attachment figures as well as the “effortful” modulation of cognitive operations involving the attachment figures (46).
While secure attachment is generally thought to be associated with less reactivity to distress, insecure attachment seems to be connected to increased neural activation throughout the brain under conditions of distress (e.g., pain or threat) (46). Furthermore, individuals with avoidant attachment seem less able to profit from the presence of others in times of distress but rather tend to perceive them as an additional burden (46). Among these processes, social affect regulation can be seen as a bottom-up mechanism, while affect regulation without support from others can be seen as a top-down mechanism. These top-down mechanisms include effortful cognitive and attentional emotion regulation strategies, such as suppression or cognitive reappraisal, that rely heavily on the prefrontal cortex (46).
In the literature on SUD, various terms are used to describe the relation between a psychotropic substance and its user. Consequently, a SUD can be described as chronic, relapsing disorders defined by 1) the compulsive seeking and taking of psychotropic substances, 2) a loss of control regarding these behaviors, as well as 3) the emergence of withdrawal symptoms that include negative emotions (e.g., irritability, anxiety) when these behaviors are unfruitful.
While similar criteria for SUD can be found in Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) (54) and International Classification of Diseases in 10th revision (ICD-10) (55), conceptual and diagnostic changes have been made in the DSM-V (56): Here, the criteria for substance abuse and substance dependence have been merged into one continuum of SUDs, ranging from mild to moderate to severe, based on the number of criteria met.
Diverse pathways and multiple, interacting processes may lead to SUD, with the individuals abusing or dependent on one or more of these substances consequently representing a highly heterogeneous group: Differences might be present, for example, in social development, comorbidity, neurobiological processes and genetics (57). The importance of applying a developmental perspective—as provided for example by attachment theory—to the study of SUD is underlined by various aspects: Epidemiological data reveal characteristic age-related trajectories for SUD, progressing from the typical onset of substance use and SUD during adolescence to peak rates in young adults and to a decline in later life (58).
Regarding the development of a PUD, developmental progression may not only apply to the stages of use—ranging from occasional use to dependence—but also across substances: For example, individuals often seem to progress from “gateway” substances (e.g., tobacco, alcohol, cannabis) to the use of other psychotropic substances (59–62). This progression might be attributed to several factors, including a common propensity to use psychotropic substances, a sensitization for the use of other substances due to the use of a previous substance, or a connection to a social network that promotes the use of several substances (61, 63, 64).
Several studies using magnetic resonance imaging (MRI) techniques have reported altered brain morphology in various SUDs [for an overview, see Ref. (65)]: Regarding gray matter, impairments have particularly been reported in the frontal lobes, the amygdala, and the insula. Regarding white matter, impairments have especially been reported in the genu and the corpus callosum as well as in prefrontal regions. In general, these impairments seem to be relevant for various cognitive dysfunctions relevant in SUD (e.g., increased impulsivity and impaired executive functions) [for an overview, see Ref. (65)]. However, there is still some debate as to how and to what extent SUDs are connected to impairments in white matter integrity (66, 67). For example, impairments in self-regulation and executive functions, connected to dysfunctions or pathologies in the frontal lobes, represent a risk factor not only for SUD but several psychiatric disorders (68). Regarding white matter tracts, a healthy development is necessary for an efficient communication between brain regions, higher order cognitive functioning, as well as several complex behaviors (69). Consequently, substance abuse is likely particularly harmful during adolescence, when white matter is still developing (66, 70–72).
In general, neural impairments connected to SUD seem to be especially prevalent in the above described structures related to attachment and emotion regulation (e.g., in the amygdala or the prefrontal regions).
Most specialists for the treatment of SUD (intuitively) recognize the importance of attachment in addiction, independent of whether interpersonal problems are the cause or the consequence of drug use (45). However, before an attachment to treatment (e.g., a therapeutic alliance) can be established, individuals with a SUD must first become detached from the substances they abuse (45). Therefore, the consideration of attachment theory in the treatment of SUD highlights the importance of the therapeutic alliance (73).
While there have been significant advances in the development and validation of psychosocial treatment strategies for SUD in the past few decades, the parameters for the success of these approaches have yet to be fully explored. A meta-analytic review by Dutra and colleagues (74) found moderate effect sizes for psychosocial treatments, but these effect sizes varied considerably dependent on the SUD and the treatment strategy under study; although individuals with Cannabis Use Disorder appeared to profit considerably from psychosocial interventions, individuals with PUD seem to profit the least. Drop-out rates were high (around one third) across all psychosocial interventions, but approximately the same percentage of participants achieved posttreatment and/or clinically significant abstinence (74).
Since the establishment of opioid substitution in the 1960s, this treatment strategy for opioid use—that is highly prevalent in PUD (75)—went hand-in-hand with psychosocial interventions. Accordingly, international clinical guidelines list psychosocial rehabilitation as crucial in this area (76). However, while several randomized controlled trials and systematic reviews conclude that opioid substitution is just as effective or even more effective when provided on its own, some large outcome studies have concluded that treatment providers with a higher frequency and quality of psychosocial interventions are better able to achieve positive outcomes [for an overview, see Ref. (76)].
Contrary to the classic psychodynamic developmental model, attachment-oriented treatment does not equate mental health and maturity with independence (45, 73). In line with Bowlby (20), normal development is seen as a movement from immature dependence towards mature interdependence and mutuality (73). Consequently, group therapy has been an important component of the treatment for SUD ever since the establishment of Alcoholics Anonymous (AA) in the 1930s (73). This can be attributed to the interpersonal conception of group therapy (human beings are always considered as social and as being situated in relation to others) that is more likely to promote attachment than other treatment strategies (73).
Interestingly, spirituality is also considered to be a helpful factor in the treatment of SUD (77). While it is closely connected to the AA program, it has also been incorporated in other treatment strategies (78, 79). This is not surprising, given that the relationship between believers and a higher power (e.g., God or other divine figures) frequently fulfils the criteria of an attachment bond and can consequently be assumed to enable similar psychological advantages (80). As the sense of having a secure attachment bond with a higher power is associated with higher spiritual well-being (81), spirituality can be conceptualized as the “ability to experience and integrate meaning and purpose in existence through a connectedness with self, others or a power greater than oneself” (p. 117) (82). Consequently, more secure attachment seems to be related to lower levels of mood pathology in general and in individuals with SUD (81, 83).
As an extension of group therapies, therapeutic communities were established in the 1960s as long-term (several months) residential programs for individuals with SUD (84). According to their conceptual groundings, the extent of impairments in psychological dysfunction and social deficits is more important than a certain pattern of drug use. Considering “community as method,” the most important psychological treatment goals are to restructure the negative patterns of behavior, thinking and feeling using self-help, mutual self-help, and social learning (84). A long-term stay within this caregiving, abstinence promoting environment should encourage alternative emotional experiences and, consequently, stimulate a kind of subsequent maturation of former inadequate attachment patterns (45).
While several studies report high levels of PUD in patients with SUD as well as a greater SUD severity in patients with PUD (e.g., 2, 85), comparatively few studies consider a wide range of drug types and/or classes, thereby neglecting the issue of polydrug use and PUD (86). Furthermore, the different definitions of polydrug use applied in SUD research often make it difficult to compare studies (87). These tendencies may lead to research results that provide little relevant information for clinicians involved in SUD treatment programs. On the other hand, explicit evaluations of polydrug use could have a high clinical as well as public health relevance (60).
In general, especially adolescents with self-perceived low social standing and lower parental socioeconomic status seem to be at risk to develop this pattern of drug use (88). Therein, polydrug use seems to be more prevalent in young men than young women (89, 90) and comorbid mental disorders seem to be more prevalent in young adults with PUD compared to those with another SUD (91). Importantly, while polydrug use is highly prevalent in individuals with opioid use disorder, individuals with this pattern of drug use also show a high prevalence of comorbid posttraumatic stress disorder (PTSD) (75). Therein, PTSD and PUD may be connected by “an ‘additive’ self-medication model” (p. 39) (92). In addition, the number of polysubstance opioid overdoses seems to be increasing in certain areas (93) and SUD persistence rates seem to be consistently higher in PUD than in other SUD (94). These recent findings further underline the need for addressing polydrug use and related characteristics in SUD research and clinical practices.
While this review focuses mainly on PUD, the reported mechanisms related to attachment and emotion regulation as well as their neural correlates may be largely seen as liabilities relevant to SUD in general. In line with this, recent findings suggest that treatment strategies should target these broader liabilities instead of focusing on specific SUD (95). However, several studies also highlight the need for a closer examination of the characteristics and treatment requirements of individuals with PUD (92, 96, 97).
Based on the above described theoretical and empirical background, our research group conceptualized five studies—three of which used (f)MRI—that aimed at further exploring attachment and related parameters in PUD. A concise overview on the methods and results of each study can be found in Table 1. Additional information on the presented studies (e.g., statistical analyses, sample characteristics) can be found in the related publications (98–102) or obtained from the authors.
Regarding attachment and neural parameters in PUD, two studies focused on the relevance of potential impairments in white matter integrity, while one study explored neural activation patterns during a novel emotion regulation task. The aim was to gain new insights into the bio-psycho-social interactions underlying PUD.
As previous studies indicated that a drug substitute (e.g., Methadone) could artificially alter the attachment status so that insecure individuals would appear secure (10, 103), our first study (100) explored whether inpatients with PUD, who were either abstinent or in maintenance treatment, differed regarding white matter structure (assessed by means of diffusion tensor imaging) as well as cognitive ability, attachment style, and personality/mood pathology.
In the first study (100), the sample of 49 men included inpatients with a PUD who were either abstinent (PUDa; n = 18) or undergoing maintenance therapy (PUDm; n = 15) as well as a control group of healthy students (CG; n = 16). In addition to the Adult Attachment Scale (AAS) [Ref. (104, 105), and the Brief Symptom Inventory (BSI-18) (106), participants completed the Neuroticism Extraversion Openness Five Factor Inventory (NEO-FFI) (107) assessing Extraversion, Agreeableness, Conscientiousness, Neuroticism, Openness to Experience, and the 16-Item Inventory of Personality Organization (IPO-16) (108) assessing Identity Diffusion, Primitive Defense, and Reality Testing as potential impairments in personality structure. Lastly, the Wonderlic Personnel Test (WPT) was used as a rough screening instrument for intelligence (109). White matter integrity was assessed through diffusion tensor imaging (DTI) that is based on the directionality and rate of diffusion of water within tissue. Consequently, a higher fractional anisotropy indicates for example that diffusion is restricted by the myelin sheaths of axons (110).
Regarding personality characteristics, PUD showed a higher amount of insecure attachment, a higher total amount of impairments in personality structure, indicating a higher risk for personality disorders (108), as well as higher amounts of neuroticism and agreeableness. Regarding white matter integrity, group differences in FA and radial diffusivity (RD) were generally more pronounced between CG and PUDa than between CG and PUDm, with both clinical groups showing widespread reductions in FA and increases in RD mainly in the same white matter tracts (mostly the superior corona radiata and the superior longitudinal fasciculus of the right hemisphere) (100). In general, lower FA and higher RD indicate a higher probability for white matter impairments (111). Interestingly, more insecure attachment and more impairments in personality structure were related to lower FA (r = -.36 to -.41) and higher RD (r = .31; all p < .05) over all participants.
The results of the first study (100) indicate that impairments in white matter structure are present in inpatients with PUD and that these impairments are paralleled by a higher amount of mood and personality pathology. In line with the conceptualization of SUD as “Attachment Disorders” (112) and in accordance with previous work (42), substituted inpatients with PUD seem to show the highest amount of anxious attachment.
Contrary to our assumptions, no significant differences in white matter integrity between abstinent and substituted inpatients with PUD were found. However, differences in white matter parameters were more pronounced between abstinent inpatients with PUD and healthy controls than between substituted inpatients with PUD and healthy controls (100). This may indicate that white matter integrity deteriorates more under abstinence, as the brain struggles to regain homeostasis (100). As impairments in the superior corona radiata and the superior longitudinal fasciculus have also been observed in adolescent substance abusers, they may be partly premorbid or a very early occurrence in SUD (66). Furthermore, impairments in the superior corona radiata and the superior longitudinal fasciculus appear to be linked with impaired decision-making (113), while impairments in the superior corona radiata can also be linked to higher risk taking in adolescents (69).
In the second study (99), we focused on the superior corona radiata and the superior longitudinal fasciculus, as deficiencies in these tracts have been linked to SUD in several studies (66, 100, 114). In addition, we hypothesized that higher amounts of existential fear and despair would be connected to more insecure attachment and decreased spiritual well-being in inpatients with PUD (115). Furthermore, following the concept of a severity continuum in SUD (56), we differentiated between non-drug-using controls, recreational drug-using controls, and inpatients with PUD.
In the second study (99), the sample of 59 men included inpatients diagnosed with PUD (PUD; n = 19) as well as controls with recreational drug use (RUC; n = 20) and non-drug-using controls (NUC; n = 20). All participants completed the Adult Attachment Scale (AAS) [Ref. (104, 105), the Multidimensional Inventory for Religious/Spiritual Well-Being (MI-RSWB) (116) and the Wonderlic Personnel Test (WPT) (109) as well as the Brief Affective Neuroscience Personality Scale (BANPS) (117) assessing the primary emotions SEEKING, SADNESS, FEAR, ANGER, CARE, and PLAY (118).
Regarding behavioral parameters, PUD showed higher levels of attachment related Anxiety than NUC and RUC as well as higher levels of negative primary emotions than NUC. No differences were found regarding the other variables. To explore possible connections between the behavioral parameters and white matter integrity, a regions-of-interest (ROIs) analysis including the superior longitudinal fasciculus and the superior corona radiata of both hemispheres focused on fractional anisotropy (FA), the most widely used DTI parameter (111). Here, PUD showed a lower FA compared to NUC and RUC in the right and left superior longitudinal fasciculus as well as a lower FA compared to NUC in the right and left superior corona radiata. Furthermore, FA in the right superior corona radiata was related to more secure attachment (r = .58) and less FEAR (r = -.46; both p < .05) (99).
While the second study (99) also supports the presence of white matter impairments and insecure attachment in inpatients with PUD, some additional insights could be gathered, as increased levels of certain primary emotions also seem to be connected to diminished white matter integrity. As in previous research (119, 120), inpatients with PUD in this study demonstrated a higher amount of ANGER, FEAR, and SADNESS compared to non-using controls (99). However, no differences were found regarding SEEKING, which previously has been theorized to be pathologically abridged in SUD (121, 122). This may be attributed to the fact that the inpatients with PUD in this study were enrolled in a therapeutic community (123, 124) during data acquisition. This treatment approach is theorized to act like a substitution drug, thereby balancing the abridged SEEKING dimension that would otherwise heighten drug craving and the possibility of relapse (121, 125). In addition, the high level of SADNESS in inpatients with PUD may underline the close connection between SUD and depression (10). The tentative connections between attachment, primary emotions, religious/spiritual well-being, and white matter integrity in inpatients with PUD that were found in this study (99) are in line with the notion of including religious/spiritual aspects in addiction treatment. As stated before, this may allow for more secure attachment experiences and could consequently increase the ability for emotion regulation (45, 115, 124).
In the third study (101), we aimed to generate new information regarding impaired emotion regulation abilities in SUD by the exploratory use of an fMRI paradigm focusing on cognitive reappraisal. This strategy refers to a deliberate re-interpretation in order to modulate emotional impact (126).
The third study (101) tested 34 right-handed men, divided into two groups, one clinical inpatient group (PUD; n = 18) diagnosed with PUD and one group of healthy controls (HC; n = 16) who reported very little or no experience with illegal substances. Cognitive reappraisal capacity was assessed outside the scanner with the Reappraisal Inventiveness Test (RIT) (127) as well as with the similar Reappraisal Generation Task (RGT) during fMRI: In each test, subjects are instructed to empathize with anger-eliciting situations and to consequently generate different reappraisals in order to downregulate anger. In addition, participants completed the Emotion Regulation Questionnaire (ERQ) (128), German version by Abler and Kessler (129), the OPD Structure Questionnaire (OPD-SQ) (130) assessing impairments in personality structure with four dimensions (131) that each comprises a self-related and an object-related subdomain: 1) Perception; 2) Regulation; 3) Communication; 4) Bonding, as well as the Adult Attachment Scale (AAS) [Ref. (104, 105), the Brief Symptom Inventory (BSI-18) (106), and the Wonderlic Personnel Test (WPT) (109).
Group comparisons revealed several differences with generally large (eta2 > .14) effect sizes (132) between PUD and HC: PUD reported more impairments in personality structure, mood pathology, and insecure attachment. Concerning emotion regulation, PUD reported a less frequent use of reappraisal but a more frequent use of suppression. Regarding cognitive reappraisal, PUD showed lower fluency and flexibility of ideas as well as more induced anger than HC. In line with this, their reappraisals during fMRI were rated as less effective than those of HC. Regarding the reappraisal-related neural activation, remarkably similar patterns were observed for both PUD and HC: They included a rather left-lateralized network of inferior, superior, and middle frontal gyri, supplemental motor areas, as well as pre- and postcentral gyri.
A consequent conjunction analysis on voxels significantly activated in PUD and HC showed in more detail that both groups activated the left inferior and superior frontal gyri, the right cerebellum, as well as the right middle temporal cortex. No group differences in neural activation were found.
The results of the third study (101) not only underlined our previous findings of insecure attachment and impaired personality structure in SUD but also highlighted the prevalence of impaired emotion regulation abilities in PUD. Although we did not find the expected differences in neural activation patterns during cognitive reappraisal between inpatients with PUD and healthy controls, the pattern of neural activation assessed for both groups highlights the crucial role of the frontal cortex and therefore of executive functions in this emotion regulation strategy (127, 133). Considered together with the poorer behavioral results in cognitive reappraisal in inpatients with PUD, the discrepancy between neural and behavioral results may point towards a third parameter connecting these two levels (101): As our previous two studies (99, 100) found extensive white matter impairments in inpatients with PUD, efforts in cognitive reappraisal could generate the required activation in gray matter structures in inpatients with PUD, but white matter impairments may prevent an adequate interaction between these gray matter structures, which could result in a lower capacity for cognitive reappraisal. In addition, as the contrary strategies underlying different types of insecure attachment—hyperactivating strategies in anxious attachment and deactivating strategies in avoidant attachment (134)—appear to be connected to different or contrary patterns of neural activation during emotion regulation (135), a mixture of these patterns could mask possible differences to healthy controls (101). Importantly, the various possible mechanisms of cognitive reappraisal in SUD need to be explored in more detail in future studies, as reappraisal may be directed at the meaning or the self-relevance of a potentially emotion-eliciting situation in order to increase or decrease negative or positive emotions (136). Furthermore, there is some indication that cognitive reappraisal is only adaptive when dealing with uncontrollable stress (where the only option is self-regulation) but not controllable stress (where the situation can be influenced) (137).
Two studies sought to explore parameters of attachment and personality structure in patients at the beginning of treatment for SUDs. Given the high rates of drop-outs [e.g., Ref. (74)] and the often-discussed differences between SUD [e.g., Ref. (2)], the results of these studies may help improve treatment adherence and consequently treatment outcomes.
As there is still some debate about whether various forms of SUD differ regarding their association with insecure attachment [e.g., Ref. (42)] and impairments in personality structure [e.g., Ref. (138)], we examined these parameters in inpatients with either a PUD or an Alcohol Use Disorder (AUD) in comparison to a non-drug-using control group (98).
In the first study (98), 66 inpatients diagnosed with AUD, 57 inpatients diagnosed with PUD, as well as 114 non-drug-using control subjects (CS) completed the Attachment Style Questionnaire (ASQ) [Ref. (139, 140), and the Borderline Personality Inventory (BPI) (141).
Compared to CS, inpatients with AUD or PUD showed higher levels in every facet of borderline personality structure and the attachment facet “Relationships as Secondary” as well as lower levels in every other facet of attachment. These differences were especially distinctive in the area “Confidence in Self and Others” (eta2 = .22), which indicates secure attachment and in the total amount of borderline pathology (eta2 = .30), respectively. No differences could be observed between AUD and PUD inpatients. Separate correlation analyses revealed that attachment and personality structure were unrelated in each group.
While the results of this study (98) confirmed that SUDs are linked to deficient attachment (42, 100) and increased borderline pathology (100, 142), they furthermore indicate that impairments in those areas are similar for AUDs and PUDs. However, although psychodynamic theory closely links early attachment experiences to personality structure (7), no distinctive link between impairments in those areas could be observed. Interestingly, inpatients with a SUD showed lower levels in several facets of attachment deficiencies (e.g., Need for Approval) than healthy controls (140). However, we argue that lower and higher than average levels in these areas could be considered problematic as they might indicate rigid patterns in interpersonal experiences. Correspondingly, from a psychodynamic perspective, one of the major therapeutic aims is described as “greater flexibility in interpersonal relationships and an enhanced capacity to meet interpersonal needs” (p. 99) (143). The increased borderline pathology we detected in inpatients with an SUD (98) suggests that impairments in personality structure can be present independent of comorbid personality disorders. In line with research on the dual diagnosis of SUD and personality disorders (142), we therefore support a dimensional approach in the study and treatment of personality pathology with an SUD.
Building on Study 4, a second study (102) focused on the role of attachment in treatment adherence during the first 6 weeks of a residential treatment program.
One hundred twenty-two inpatients (34 female), diagnosed with AUD (n = 66) or PUD (n = 57), were tested at treatment entry. After 6 weeks, the 47 inpatients remaining in treatment were tested for a second time. Both times participants completed the ASQ [Ref. (139, 140).
Using all ASQ subscales, agglomerative cluster analysis on the total sample suggested a two-cluster solution: Cluster I was defined by higher scores in “Confidence in Self and Others,” while Cluster II was defined by higher scores in “Need for Approval” and “Relationships as Secondary.” Further analyses showed that inpatients in Cluster I were more likely to drop out of treatment during the first 6 weeks. In hierarchical regression analyses predicting treatment adherence, with the control variables sex and psychiatric comorbidity at Step 2, attachment security (Cluster I vs Cluster II) added approximately 6% of variance at Step 3.
The results of the fifth study (102) indicate that self-reported secure attachment might be linked to lower treatment adherence in patients with SUDs. This unexpected finding might be attributed to the influence of self-reflection, with a lower ability for self-reflection resulting in more secure self-appraisal but also to an increased likelihood of treatment drop-out. In line with this, self-report measures of adult attachment—in comparison to attachment interviews—are considered to be more likely influenced by distorted self-images while insufficiently assessing repressed information (144).
Consequently, self-reported attachment security may be attributed to an idealized self-view defined by primitive defense mechanisms (e.g., splitting or denial) (102). Furthermore, our findings potentially reflect a unique attribute of therapeutic communities (124) that threatens such narcissistically distorted self-appraisals: In patients with this form of self-appraisal, the high amount of group cohesion potentially leads to increased cognitive dissonances that consequently increase the likelihood of treatment drop-out (123). The reduction of narcissism in the therapeutic community might also explain the decrease in Confidence in Self and Others after 6 weeks of treatment (102). This is also part of the concept of the therapeutic community itself, as patients are encouraged to explore their interpersonal deficits (124). Furthermore, the decrease in Confidence in Self and Others likely also mirrors the decline of an initial euphoria experienced when entering treatment and being sober after severe substance use (102).
While the application of attachment theory always implies a developmental approach, this article focused on the basis from which individuals diagnosed with a PUD might progress towards recovery. Furthermore, although research focused on attachment already contributed important insights into the characteristics of our social nature, “an important enterprise for the future is to consider how attachment is differentiated from, and integrated with, other features of development” (p. 25) (145).
Consequently, the characteristics and treatment requirements connected to PUDs especially need to be addressed in more detail, as this diagnosis is highly common in individuals seeking treatment while simultaneously being associated with poor treatment success [e.g., Ref. (2)]. Several important conclusions regarding SUD—particularly PUD—and their treatment can be drawn from the original research presented above.
Although the completion of treatment is closely linked to favorable treatment outcome, it is more likely for a patient to drop out of treatment than to complete it: According to a systematic review by Brorson and colleagues (146), the most consistent risk factors for dropping out were cognitive deficits, younger age, personality disorders, and low treatment alliance. Conversely, the effects of treatment are dose related: While more and longer treatments usually lead to a better outcome, disruptions in attachment to the program or the clinical staff increased the likelihood of relapse and drop out (73). Considering the largely insecure attachment status of inpatients with PUD (98–102) may consequently improve treatment adherence.
As mentioned above, the primary function of adult attachment relationships may be seen in the regulation of emotions (38). The regulation of emotions through social interactions is a key function of the attachment system, as the quality of the attachment bond influences emotional functioning and regulation capabilities as well as styles of interpersonal relating from childhood on into adulthood (46, 147). While impairment in cognitive reappraisal, an explicit emotion regulation strategy, seems to be relevant in PUD (101), implicit, i.e., automatic and largely unconscious emotion regulation strategies, may be of even greater relevance, as they are likely more closely connected to the mental representations of self and others included in attachment and personality structure (148).
Furthermore, future studies on PUD may also consider the connections between boredom and substance use: Boredom, which is connected to an emptiness stemming from social isolation as well as a lack of attachment to others (149), represents a critical factor in relapse (149) among others through its connection to increased risk-taking behaviors (150). Boys and colleagues (151) found that close to 90% of young (16–22 years) poly-substance users consumed illicit substances to enhance an activity with 83% consuming the substances to decrease boredom.
Interestingly, while the studies on PUD described in detail above (98–102) focused on inpatients in therapeutic communities, the relation between attachment and psychological distress can also be found in SUD outpatients (152): Here, an insecure attachment is again more common than in healthy controls. Furthermore, fearful attachment appears to be associated with higher levels of psychological distress. Importantly, psychological treatments with a directive, reflective, or supportive orientation appear to result in more patients having a secure attachment style by the end of treatment (152).
While the consideration of different emotions and their role in SUD is of great importance, the absence of these emotions or of their perception has to be considered as well: For example, a recent study (153) found that insecure attachment also seems to be associated with dissociation and alexithymia in individuals with SUD. As they inhibit the identification and verbalization of emotions, dissociation and alexithymia also impair the communication with others and thus the mutual understanding (153).
A change from insecure to secure attachment style might therefore be considered an important goal in SUD treatment, as it could prevent patients from applying defense strategies involving substance use to regulate their emotions and interpersonal relationships (152).
Given that a meta-analytic review by Dutra and colleagues (74) found that individuals with PUD—compared to other SUD—appear to profit the least from treatment interventions, more research on the characteristics and treatment requirements of individuals with PUD is still very much needed. Therein, attachment theory provides a bio-psycho-social model for human behaviors and experiences in relation to the regulation of stress and emotion in social situations (154). Following this approach, the presented results (98–102) underline the conceptualization of PUD as an “Attachment Disorder” as well as the value of the bio-psycho-social perspective in this research area. As the influence of attachment always has to be considered in the context of other risk factors (13), exploring and integrating the clinical characteristics of individuals with PUD are of vital importance for future research on treatment approaches. For example, polydrug use can frequently be found in connection to sexual behaviors (155–158). However, few studies to date seem to have explored the role of sexual behaviors in PUD (159) and no study seems to have explored their romantic relationships.
In addition. the above described studies on inpatients with PUD (99, 100) highlight the fact that insecure attachment and other behavioral impairments in inpatients with PUD are paralleled by extensive impairments in white matter integrity (99, 100), most notably in tracts connected to facets of emotion regulation (e.g., impaired decision-making and higher risk taking behavior) (69, 113). Consequently, a potential neuroplasticity during the treatment of SUD in general—and the long-term stay in a therapeutic community in particular—should be explored in future research.
Furthermore, the results of the above described studies (98, 100, 101) suggest that future research on the treatment for SUD would benefit from the assessment of personality structure and related psychodynamic interventions. Therein, Kohut’s (160) theory that a specific substance can be seen as a “replacement for a defect in the psychological structure” matches with the widespread impairments in personality structure found in inpatients with PUD (101). Furthermore, the influence of traumatic experiences in childhood on the amount of addictive behaviors displayed in young adulthood (161) seems to be mediated by impairments in personality structure and insecure attachment (162–164).
While the above described studies on inpatients with PUD focused on primary emotions and certain emotion regulation strategies (99, 101), there is vast potential for additional contributing factors in PUD related to emotions and their regulation. Among emotion regulation processes, social affect regulation can be seen as a bottom-up mechanism, while affect regulation without support from others can be seen as a top-down mechanism. These top-down mechanisms include effortful cognitive and attentional emotion regulation strategies, such as suppression or cognitive reappraisal, that rely heavily on the prefrontal cortex (46). Consequently, an examination of the neural correlates of bottom-up mechanisms in PUD would generate further important insights.
The importance of research on SUD—and especially PUD—as well as the need for evidence-based effective treatment strategies is further underlined by the consideration of transgenerational effects: For example, in a recent study by Tuhkanen and colleagues (165), only 7% of infants born to mothers with recent or current substance use showed no neurological impairments during their first days of life.
As different definitions of polydrug use are applied in SUD research, the comparison and integration of results can be difficult (87). These tendencies may lead to research results that provide little relevant information for clinicians involved in SUD treatment programs. On the other hand, explicit and systematic evaluations of polydrug use could have a high clinical as well as public health relevance (60). Consequently, the possibility of concurrent use of other substances should always be taken into consideration, even when only the use of one particular psychotropic substance is the focus of a study (57). For example, while polydrug use is often considered a barrier in the prevention of hepatitis C virus (HCV) transmission in individuals who inject prescription opioids, research on the underlying mechanisms is relatively sparse (166).
Furthermore, the results of different studies on attachment in adults are also often hard to compare or to summarize (148). In general, self-report measures—as used in the presented studies (98–102)—are thought to be limited in their ability to assess all areas of attachment patterns, as they solely rely on conscious attitudes and behaviors (144). However, they are also considered to be more focused on current attachment patterns in various relationships, while the Adult Attachment Interview (167) solely focuses on the relationship with the parents.
As inpatient participants in the described studies were enrolled in a therapeutic community at the time of data acquisition (98–102), this may have influenced the results in various areas. Among others, the decline in reported attachment security after the initial treatment phase (102) could also—at least partly—be attributable to this treatment approach. However, to date, hardly any empirical studies have investigated the role of attachment theory and related parameters (e.g., therapeutic alliance) for the conceptual framework and success of the therapeutic community [e.g., Ref. (168)]. Consequently, further research is very much needed to explore these mechanisms.
The high levels of comorbid mental disorders in inpatients with SUD in general [for an overview, see Ref. (169)] and PUD in particular also have to be considered in the interpretation of research results. Conversely, deficiencies in emotion processing and regulation are a known “liability spectrum that underlies many different mental disorders” (p. 154) (36). Internationally, this high risk of co-occurrence appears in both directions: While between 40% and 50% of individuals with a SUD also have at least one other psychiatric diagnosis, other psychiatric diagnoses also show a high rate of comorbid SUD [for an overview, see Ref. (169)]. The question of how co-occurring psychiatric disorders influence the participation and outcome of treatment in SUD has also not yet been fully answered (170). Overall, treating co-occurring affective and personality disorders as diagnoses in their own right generally seems to lead to better outcomes than only treating SUD and an integrated treatment approach can therefore be considered evidence based (170).
In line with this, maltreatment, and especially cumulative abuse, during childhood is associated with several related mental disorders, including SUD and PUD (171, 172). Therefore, a more extensive assessment of traumatic experiences might reveal different profiles among individuals with SUD that could profit from different treatment strategies.
While our research highlights the presence of white matter impairments in inpatients with PUD (99, 100), we did not specifically investigate possible influences of the number of abused substances or the intensity of abuse. This may be an interesting area for future research, as recent findings suggest that some neural impairments may be related to specific substances while others are related to the amount of poly drug use (173).
Lastly, many different approaches may have been taken to explore the current theoretical and empirical literature on PUD from an attachment perspective. Therein, different types of reviews are known to have specific strengths and weaknesses (174).
The focus on PUD is now more important than ever, given that the diversification of certain products (e.g., nicotine, marijuana, prescription drugs) in recent years seems to have contributed to an increased polydrug use in adolescents (88, 89). In turn, polydrug use is strongly associated with later SUD and related health issues (175, 176).
The studies on PUD described above and in additional publications (98–102) clearly highlight the importance of attachment and related parameters in PUD as well as their bio-psycho-social integration. Future studies might more closely focus on the influence of attachment-based interventions on emotion regulation abilities as well as a potentially related neuroplasticity.
While recovery represents an important paradigm in the treatment of SUD, the definition of recovery has been extended beyond a reduction in use or sustained abstinence and now also includes the enhancement of global well-being as well as a reintegration into a prosocial community. To date, few studies have incorporated this broadened definition of recovery into their design (79). The most commonly used outcome measure, i.e., treatment retention and abstinence from the primary psychotropic substance (177), might not be able to fully assess the effects of psychosocial interventions, e.g., changes in emotion regulation and other attachment parameters. Especially in long-term inpatient PUD treatment settings (e.g., therapeutic communities), neuroplastic changes, which are still rather unexplored, might represent important additional parameters for the assessment of treatment outcomes.
MH-R and H-FU conceptualized the study. MH-R wrote the draft. H-FU proofread the manuscript. Both authors gave their consent for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to acknowledge the work of Nikolas Bonatos for making helpful and invaluable critical comments about the manuscript.
1. United Nations Office on Drugs and Crime. World Drug Report 2014. United Nations publication (2014). Sales No. E.14.XI.7
2. Weigl M, Anzenberger J, Busch M, Horvath I, Türscherl E. Bericht zur Drogensituation 2015. Wien: Gesundheit Österreich (2015).
5. Martinotti G, Carli V, Tedeschi D, Di Giannantonio M, Roy A, Janiri L, et al. Mono- and polysubstance dependent subjects differ on social factors, childhood trauma, personality, suicidal behaviour, and comorbid Axis I diagnoses. Addict Behav (2009) 34:790–3. doi: 10.1016/j.addbeh.2009.04.012
6. MacKillop J, de Wit H. The Wiley-Blackwell Handbook of Addiction Psychopharmacology. Oxford: Wiley-Blackwell (2013). doi: 10.1002/9781118384404
7. Bowlby J. The making and breaking of affectional bonds. I. Aetiology and psychopathology in the light of attachment theory. An expanded version of the fiftieth maudsley lecture, delivered before the royal college of psychiatrists, 19 November 1976 . Br J Psychiatry (1977) 130:201–10. doi: 10.1192/bjp.130.5.421
8. Brennan KA, Shaver PR. Attachment styles and personality disorders: their connections to each other and to parental divorce, parental death, and perceptions of parental caregiving. J Pers (1998) 66:835–78. doi: 10.1111/1467-6494.00034
9. Nakash-Eisikovits O, Dutra L, Westen D. Relationship between attachment patterns and personality pathology in adolescents. J Am Acad Child Adolesc Psychiatry (2002) 41:1111–23. doi: 10.1097/00004583-200209000-00012
10. Zellner MR, Watt DF, Solms M, Panksepp J. Affective neuroscientific and neuropsychoanalytic approaches to two intractable psychiatric problems: why depression feels so bad and what addicts really want. Neurosci Biobehav Rev (2011) 35:2000–8. doi: 10.1016/j.neubiorev.2011.01.003
11. Stovall-McClough KC, Dozier M. Attachment states of mind and psychopathology in adulthood. In: Cassidy J, Shaver PR, editors. Handbook of attachment. New York/London: Guilford Press (2016). p. 715–38.
12. Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol (2009) 21:1311–34. doi: 10.1017/S0954579409990174
13. DeKlyen M, Greenberg MT. Attachment and psychopathology in childhood. In: Cassidy J, Shaver PR, editors. Handbook of attachment. New York/London: Guilford Press (2016). p. 639–66.
14. Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Dev Psychopathol (1996) 8:597–600. doi: 10.1017/S0954579400007318
15. Greenberg MT, Speltz ML, Deklyen M, Jones K. Correlates of clinic referral for early conduct problems: variable- and person-oriented approaches. Dev Psychopathol (2001) 13:255–76. doi: 10.1017/S0954579401002048
16. Keller TE, Spieker SJ, Gilchrist L. Patterns of risk and trajectories of preschool problem behaviors: a person-oriented analysis of attachment in context. Dev Psychopathol (2005) 17:349–84. doi: 10.1017/S0954579405050170
17. Bowlby J. Attachment and loss, Vol. 2: Separation: anxiety and anger. New York: Basic Books (1973).
19. Sheinbaum T, Kwapil TR, Ballespí S, Mitjavila M, Chun CA, Silvia PJ, et al. Attachment style predicts affect, cognitive appraisals, and social functioning in daily life. Front Psychol (2015) 6. doi: 10.3389/fpsyg.2015.00296
21. Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. New York: Guilford Publications Inc (2007).
22. Mikulincer M, Shaver PR, Pereg D. Attachment theory and affect regulation: the dynamics, development, and cognitive consequences of attachment-related strategies. Motiv Emot (2003) 27:77–102. doi: 10.1023/A:1024515519160
23. Mikulincer M. Attachment style and the mental representation of the self. J Pers Soc Psychol (Gott) (1995) 69:1203–15. doi: 10.1037/0022-3514.69.6.1203
24. Bartholomew K, Horowitz LM. Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol (1991) 61:226–44. doi: 10.1037//0022-3514.61.2.226
25. Granqvist P. Religion as Attachment: the Godin Award Lecture. Arch Psychol Relig (2010) 32:5–24. doi: 10.1163/157361210X487177
26. Shaver PR, Clark CL. The psychodynamics of adult romantic attachment. In: Masling JM, Bornstein RF, editors. Empirical perspectives on object relations theory. Washington: American Psychological Association (1994). p. 105–56. doi: 10.1037/11100-004
27. Diamond D, Blatt SJ. Internal working models and the representational world in attachment and psychoanalytic theories. In: Sperling MB, Berman WH, editors. Attachment in adults: Clinical and developmental perspectives. New York: Guilford Press (1994). p. 72–97.
28. Levy KN, Blatt SJ, Shaver PR. Attachment styles and parental representations. J Pers Soc Psychol (1998) 74:407–19. doi: 10.1037//0022-3514.74.2.407
29. Schauenburg H. Zum Verhältnis von Bindungsdiagnostik und psychodynamischer Diagnostik. In: Schneider W, Freiberger HJ, editors. Was leistet die OPD? Empirische Befunde und klinische Erfahrungen mit der Operationalisierten Psychodynamischen Diagnostik. Bern: Huber (2000). p. 196–217.
30. OPD Task Force. Operationalized psychodynamic diagnosis OPD-2. Manual of diagnosis and treatment planning. Kirkland: Hogrefe and Huber (2008).
31. Uzdawinis D, Edel MA, Özgürdal S, Von Haebler D, Hauser M, Witthaus H, et al. Operationalisierte psychodynamische diagnostik (OPD) bei patienten im schizophrenen prodromalstadium—Eine explorative studie. Z Psychosom Med Psychother (2010) 56:150–62. doi: 10.13109/zptm.2010.56.2.150
32. Rudolf G, Grande T, Oberbracht C, Jakobsen T. Erste empirische Untersu- chungen zu einem neuen diagnostischen System: Die Operationalisierte Psychodyna- mische Diagnostik (OPD). Zeitschrift für Psychosom Medizin und Psychoanal (1996) 42:343–57.
33. Schneider G, Lange C, Heuft G. Operationalized psychodynamic diagnostics and differential therapy indication in routine diagnostics at a psychosomatic outpatient department. Psychother Res (2002) 12:159–78. doi: 10.1093/ptr/12.2.159
34. Müller C, Kaufhold J, Overbeck G, Grabhorn R. The importance of reflective functioning to the diagnosis of psychic structure. Psychol Psychother Theory Res Pract (2006) 79:485–94. doi: 10.1348/147608305X68048
35. Jarmolowicz DP, Mueller ET, Koffarnus MN, Carter AE, Gatchalian KM, Bickel WK. Executive dysfunction in addiction. In: MacKillop J, de Wit H, editors. The Wiley-Blackwell handbook of addiction psychopharmacology. Oxford: Wiley-Blackwell (2013). p. 27–61. doi: 10.1002/9781118384404
36. Kret ME, Ploeger A. Emotion processing deficits: a liability spectrum providing insight into comorbidity of mental disorders. Neurosci Biobehav Rev (2015) 52:153–71. doi: 10.1016/j.neubiorev.2015.02.011
37. Fuendeling JM. Affect regulation as a stylistic process within adult attachment. J Soc Pers Relat (1998) 15:291–322. doi: 10.1177/0265407598153001
38. Mikulincer M, Shaver PR. Adult attachment and emotion regulation. In: Cassidy J, Shaver PR, editors. New York/London: Handbook of attachment. Guilford Press (2016). p. 507–33.
39. Fonagy P, Leigh T, Steele M, Steele H, Kennedy R, Mattoon G, et al. The relation of attachment status, psychiatric classification, and response to psychotherapy. J Consult Clin Psychol (1996) 64:22–31. doi: 10.1037/0022-006X.64.1.22
40. Fowler JC, Groat M, Ulanday M. Attachment style and treatment completion among psychiatric inpatients with substance use disorders. Am J Addict (2013) 22:14–7. doi: 10.1111/j.1521-0391.2013.00318.x
41. Caspers KM, Yucuis R, Troutman B, Spinks R. Attachment as an organizer of behavior: implications for substance abuse problems and willingness to seek treatment. Subst Abuse Treat Prev Policy (2006) 1:32. doi: 10.1186/1747-597X-1-32
42. Schindler A, Thomasius R, Petersen K, Sack P. Heroin as an attachment substitute? Differences in attachment representations between opioid, ecstasy and cannabis abusers. Attach Hum Dev (2009) 11:307–30. doi: 10.1080/14616730902815009
43. Riggs SA, Jacobvitz D. Expectant parents’ representations of early attachment relationships: associations with mental health and family history. J Consult Clin Psychol (2002) 70:195–204. doi: 10.1037//0022-006X.70.1.195
44. De Palo F, Capra N, Simonelli A, Salcuni S, Di Riso D. Parenting quality in drug-addicted mothers in a therapeutic mother-child community: the contribution of attachment and personality assessment. Front Psychol (2014) 5:1–13. doi: 10.3389/fpsyg.2014.01009
46. Coan JA. Toward a neuroscience of attachment. In: Cassidy J, Shaver PR, editors. Handbook of attachment. New York/London: Guilford Press (2016). p. 242–72.
47. Coan JA. Adult attachment and the brain. J Soc Pers Relat (2010) 27:210–7. doi: 10.1177/0265407509360900
48. Johansen JP, Cain CK, Ostroff LE, Ledoux JE. Molecular mechanisms of fear learning and memory. Cell (2011) 147:509–24. doi: 10.1016/j.cell.2011.10.009
49. Benuzzi F, Pugnaghi M, Meletti S, Lui F, Serafini M, Baraldi P, et al. Processing the socially relevant parts of faces. Brain Res Bull (2007) 74:344–56. doi: 10.1016/j.brainresbull.2007.07.010
50. Rolls ET. Emotion elicited by primary reinforcers and following stimulus-reinforcement association learning. In: Coan JA, Allen JJB, editors. Handbook of emotion elicitation and assessment. New York: Oxford University Press (2007). p. 137–57.
51. Brasted PJ, Bussey TJ, Murray EA, Wise SP. Role of the hippocampal system in associative learning beyond the spatial domain. Brain (2003) 126:1202–23. doi: 10.1093/brain/awg103
52. Coan JA, Allen JJB. Frontal EEG asymmetry as a moderator and mediator of emotion. Biol Psychol (2004) 67:7–49. doi: 10.1016/j.biopsycho.2004.03.002
53. Ray RD, Zald DH. Anatomical insights into the interaction of emotion and cognition in the prefrontal cortex. Neurosci Biobehav Rev (2012) 36:479–501. doi: 10.1016/j.neubiorev.2011.08.005
54. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Publishing (1994).
55. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992).
56. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. Arlington, VA: American Psychiatric Publishing (2013).
57. Chassin L, Presson C, Il-Cho Y, Lee M, Macy J. Developmental factors in addiction: methodological considerations. In: MacKillop J, de Wit H, editors. The Wiley-Blackwell handbook of addiction psychopharmacology. Oxford: Wiley-Blackwell (2013). p. 5–26. doi: 10.1002/9781118384404.ch1
58. Masten AS, Faden VB, Zucker RA, Spear LP. Underage drinking: a developmental framework. Pediatrics (2008) 121:235–51. doi: 10.1542/peds.2007-2243A
59. Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: further evidence for the gateway theory. J Stud Alcohol (1992) 53:447–57. doi: 10.15288/jsa.1992.53.447
60. Hayley AC, Stough C, Downey LA. DSM-5 cannabis use disorder, substance use and DSM-5 specific substance-use disorders: evaluating comorbidity in a population-based sample. Eur Neuropsychopharmacol (2017) 27:732–43. doi: 10.1016/j.euroneuro.2017.06.004
61. Mayet A, Legleye S, Beck F, Falissard B, Chau N. The gateway hypothesis, common liability to addictions or the route of administration model a modelling process linking the three theories. Eur Addict Res (2016) 22:107–17. doi: 10.1159/000439564
62. McCutcheon JC, Watts SJ. An examination of the importance of strain in the cannabis gateway effect. Int J Offender Ther Comp Criminol (2018) 62:3603–17. doi: 10.1177/0306624X17729433
63. Kandel DB, Yamaguchi K, Klein LC. Testing the gatewat hypothesis. Addiction (2006) 101:470–2. doi: 10.1111/j.1360-0443.2006.01426.x
64. MacCoun RJ. Competing accounts of the gateway effect: the field thins, but still no clear winner. Addiction (2006) 101:473–4. doi: 10.1111/j.1360-0443.2006.01428.x
65. Yang Y, Chefer S, Geng X, Gu H, Xi C, Stein EA. Structural and functional neuroimaging methods: applications to substance abuse and addiction. In: Adinoff B, Stein EA, editors. Neuroimaging in addiction. Wiley Online Library (2011). p. 38–82. doi: 10.1002/9781119998938
66. Baker STE, Yücel M, Fornito A, Allen NB, Lubman DI. A systematic review of diffusion weighted MRI studies of white matter microstructure in adolescent substance users. Neurosci Biobehav Rev (2013) 37:1712–23. doi: 10.1016/j.neubiorev.2013.06.015
67. Batalla A, Bhattacharyya S, Yücel M, Fusar-Poli P, Crippa JA, Nogué S, et al. Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings. PLoS One (2013) 8. doi: 10.1371/journal.pone.0055821
68. Dawes MA, Tarter RE, Kirisci L. Behavioral self-regulation: correlates and 2 year follow-ups for boys at risk for substance abuse. Drug Alcohol Depend (1997) 45:165–76. doi: 10.1016/S0376-8716(97)01359-8
69. Jacobus J, Thayer RE, Trim RS, Bava S, Frank LR, Tapert SF. White matter integrity, substance use, and risk taking in adolescence. Psychol Addict Behav (2013) 27:431–42. doi: 10.1037/a0028235
70. Clark DB, Chung T, Thatcher DL, Pajtek S, Long EC. Psychological dysregulation, white matter disorganization and substance use disorders in adolescence. Addiction (2012) 107:206–14. doi: 10.1111/j.1360-0443.2011.03566.x
71. Bava S, Thayer R, Jacobus J, Ward M, Jernigan TL, Tapert SF. Longitudinal characterization of white matter maturation during adolescence. Brain Res (2010) 1327:38–46. doi: 10.1016/j.brainres.2010.02.066
72. Lubman DI, Yucel M, Hall WD. Substance use and the adolescent brain: a toxic combination? J Psychopharmacol (2007) 21:792–4. doi: 10.1177/0269881107078309
73. Flores PJ. Addiction as an attachment disorder: implications for group psychotherapy. In: Reading B, Weegmann M, editors. Group psychotherapy and addiction. Sussex Chichester: Whurr Publishers Ltd (2004). p. 1–18. doi: 10.1002/9780470713549.ch1
74. Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry (2008) 165:179–87. doi: 10.1176/appi.ajp.2007.06111851
75. Hassan AN, Le Foll B. Polydrug use disorders in individuals with opioid use disorder. Drug Alcohol Depend (2019) 198:28–33. doi: 10.1016/j.drugalcdep.2019.01.031
76. Day E, Mitcheson L. Psychosocial interventions in opiate substitution treatment services: does the evidence provide a case for optimism or nihilism? Addiction (2017) 112:1329–36. doi: 10.1111/add.13644
77. Davis KL, Panksepp J. The brain’s emotional foundations of human personality and the Affective Neuroscience Personality Scales. Neurosci Biobehav Rev (2011) 35:1946–58. doi: 10.1016/j.neubiorev.2011.04.004
78. Hodge DR. Alcohol treatment and cognitive behavioral therapy: enhancing effectiveness by incorporating spirituality and religion. Soc Work (2011) 56:21–31. doi: 10.1093/sw/56.1.21
79. Richardson GB, Blount TN, Hanson-Cook BS. Life history theory and recovery from substance use disorder. Rev Gen Psychol (2019) 23(2):263–74. doi: 10.1037/gpr0000173
80. Kirkpatrick LA. Attachment, evolution, and the psychology of religion. New York: Guilford (2005).
81. Diaz N, Horton EG, Malloy T. Attachment style, spirituality, and depressive symptoms among individuals in substance abuse treatment. J Soc Serv Res (2014) 40:313–24. doi: 10.1080/01488376.2014.896851
82. Unterrainer H-F, Ladenhauf KH, Wallner-Liebmann SJ, Fink A. Different types of religious/spiritual well-being in relation to personality and subjective well-being. Int J Psychol Relig (2011) 21:115–26. doi: 10.1080/10508619.2011.557003
83. Hiebler-Ragger M, Falthansl-Scheinecker J, Birnhuber G, Fink A, Unterrainer H-F. Facets of spirituality diminish the positive relationship between insecure attachment and mood pathology in young adults. PLoS One (2016) 11:1–9. doi: 10.1371/journal.pone.0158069
84. De Leon G. Therapeutic communities. In: Miller PM, editor. Interventions for addiction. London: Elsevier Inc. (2013). p. 643–53. doi: 10.1016/B978-0-12-398338-1.00066-X
85. John WS, Zhu H, Mannelli P, Schwartz RP, Subramaniam GA, Wu LT. Prevalence, patterns, and correlates of multiple substance use disorders among adult primary care patients. Drug Alcohol Depend (2018) 187:79–87. doi: 10.1016/j.drugalcdep.2018.01.035
86. Jongenelis M, Pettigrew S, Lawrence D, Rikkers W. Factors associated with poly drug use in adolescents. Prev Sci (2019) 20(5):695–704. doi: 10.1007/s11121-019-00993-8
87. Ainscough TS, McNeill A, Strang J, Calder R, Brose LS. Contingency management interventions for non-prescribed drug use during treatment for opiate addiction: a systematic review and meta-analysis. Drug Alcohol Depend (2017) 178:318–39. doi: 10.1016/j.drugalcdep.2017.05.028
88. Bello MS, Khoddam R, Stone MD, Cho J, Yoon Y, Lee JO, et al. Poly-product drug use disparities in adolescents of lower socioeconomic status: emerging trends in nicotine products, marijuana products, and prescription drugs. Behav Res Ther (2019) 115:103–10. doi: 10.1016/j.brat.2018.11.014
89. Zuckermann AME, Williams G, Battista K, de Groh M, Jiang Y, Leatherdale ST. Trends of poly-substance use among Canadian youth. Addict Behav Reports (2019) 10:100189. doi: 10.1016/j.abrep.2019.100189
90. Patrick ME, Kloska DD, Terry-McElrath YM, Lee CM, O’Malley PM, Johnston LD. Patterns of simultaneous and concurrent alcohol and marijuana use among adolescents. Am J Drug Alcohol Abuse (2018) 44:441–51. doi: 10.1080/00952990.2017.1402335
91. Salom CL, Betts KS, Williams GM, Najman JM, Alati R. Predictors of comorbid polysubstance use and mental health disorders in young adults-a latent class analysis. Addiction (2016) 111:156–64. doi: 10.1111/add.13058
92. Kearns N, Cloutier R, Carey C, Contractor A, Blumenthal H. Alcohol and marijuana polysubstance use: comparison of PTSD symptom endorsement and severity patterns. Cannabis (2019) 2:39–52. doi: 10.26828/cannabis.2019.01.004
93. Barocas JA, Wang J, Marshall BDL, LaRochelle MR, Bettano A, Bernson D, et al. Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug Alcohol Depend (2019) 200:59–63. doi: 10.1016/j.drugalcdep.2019.03.014
94. Evans EA, Grella CE, Washington DL, Upchurch DM. Gender and race/ethnic differences in the persistence of alcohol, drug, and poly-substance use disorders. Drug Alcohol Depend (2017) 174:128–36. doi: 10.1016/j.drugalcdep.2017.01.021
95. Franco S, Olfson M, Wall MM, Wang S, Hoertel N, Blanco C. Shared and specific associations of substance use disorders on adverse outcomes: a national prospective study. Drug Alcohol Depend (2019) 201:212–19. doi: 10.1016/j.drugalcdep.2019.03.003
96. Jeffirs SM, Jarnecke AM, Flanagan JC, Killeen TK, Laffey TF, Back SE. Veterans with PTSD and comorbid substance use disorders: does single versus poly-substance use disorder affect treatment outcomes? Drug Alcohol Depend (2019) 199:70–5. doi: 10.1016/j.drugalcdep.2019.04.001
97. Burdzovic Andreas J, Lauritzen G, Nordfjaern T. Co-occurrence between mental distress and poly-drug use: a ten year prospective study of patients from substance abuse treatment. Addict Behav (2015) 48:71–8. doi: 10.1016/j.addbeh.2015.05.001
98. Hiebler-Ragger M, Unterrainer H-F, Rinner A, Kapfhammer H-P. Insecure attachment styles and increased borderline personality organization in substance use disorders. Psychopathology (2016) 49(5):341–4. doi: 10.1159/000448177
99. Unterrainer H-F, Hiebler-Ragger M, Koschutnig K, Fuchshuber J, Tscheschner S, Url M, et al. Addiction as an attachment disorder: white matter impairment is linked to increased negative affective states in poly drug use. Front Hum Neurosci (2017) 11:1–11. doi: 10.3389/fnhum.2017.00208
100. Unterrainer H-F, Hiebler M, Ragger K, Froehlich L, Koschutnig K, Schoeggl H, et al. White matter integrity in polydrug users in relation to attachment and personality: a controlled diffusion tensor imaging study. Brain Imaging Behav (2016) 10:1096–107. doi: 10.1007/s11682-015-9475-4
101. Hiebler-Ragger M, Perchtold CM, Unterrainer H-F, Fuchshuber J, Koschutnig K, Nausner L, et al. Lower cognitive reappraisal capacity is related to impairments in attachment and personality structure in poly-drug use: an fMRI study. In Review (2018).
102. Fuchshuber J, Hiebler-Ragger M, Ragger K, Rinner A, Kapfhammer HP, Unterrainer H-F. Increased attachment security is related to early therapy drop-out in substance use disorders. BMC Res Notes (2018) 11:1–5. doi: 10.1186/s13104-018-3251-7
103. Panksepp J, Knutson B, Burgdorf J. The role of brain emotional systems in addictions: a neuro-evolutionary perspective and new “self-report” animal model. Addiction (2002) 97:459–69. doi: 10.1046/j.1360-0443.2002.00025.x
104. Collins NL, Read SJ. Adult attachment, working models, and relationship quality in dating couples. J Pers Soc Psychol (1990) 58:644–63. doi: 10.1037/0022-3514.58.4.644
105. Schmidt S, Strauss B, Höger D, Brähler E. Die Adult Attachment Scale (AAS)—Teststatistische Prüfung und Normierung der deutschen Version. Psychother Psychosom Med Psychol (2004) 54:375–82. doi: 10.1055/s-2003-815000
106. Franke GH, Ankerhold A, Haase M, Jäger S, Tögel C, Ulrich C, et al. The usefulness of the Brief Symptom Inventory 18 (BSI-18) in psychotherapeutic patients. Psychother Psychosom Med Psychol (2011) 61:82–6. doi: 10.1055/s-0030-1270518
107. Borkenau P, Ostendorf F. NEO-FFI. NEO-Fünf-Faktoren-Inventar nach Costa und McCrae. Göttingen: Hogrefe (1993).
108. Zimmermann J, Benecke C, Hörz S, Rentrop M, Peham D, Bock A, et al. Validierung einer deutschsprachigen 16-Item-Version des Inventars der Persönlichkeitsorganisation (IPO-16). Diagnostica (2013) 59:3–16. doi: 10.1026/0012-1924/a000076
110. Basser PJ. Inferring microstructural features and the physiological state of tissues from diffusion-weighted images. NMR Biomed (1995) 8:333–44. doi: 10.1002/nbm.1940080707
111. Smith SM, Jenkinson M, Johansen-Berg H, Rueckert D, Nichols TE, Mackay CE, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage (2006) 31:1487–505. doi: 10.1016/j.neuroimage.2006.02.024
112. Flores PJ. Addiction as an attachment disorder: implications for group therapy. Int J Gr Psychother (2001) 51:63–81. doi: 10.1521/ijgp.51.1.63.49730
113. Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat Neurosci (2005) 8:1458–63. doi: 10.1038/nn1584
114. Bell RP, Foxe JJ, Nierenberg J, Hoptman MJ, Garavan H. Assessing white matter integrity as a function of abstinence duration in former cocaine-dependent individuals. Drug Alcohol Depend (2011) 114:159–68. doi: 10.1016/j.drugalcdep.2010.10.001
115. Unterrainer H-F, Lewis A, Collicutt J, Fink A. Religious/spiritual well-being, coping styles, and personality dimensions in people with substance use disorders. Int J Psychol Relig (2013) 23:204–13. doi: 10.1080/10508619.2012.714999
116. Unterrainer H-F, Huber HP, Ladenhauf KH, Wallner-Liebmann SJ, Liebmann PM. MI-RSB 48: the development of a multidimensional inventory of religious-spiritual well-being. Diagnostica (2010) 56:82–93. doi: 10.1026/0012-1924/a000001
117. Barrett FS, Robins RW, Janata P. A brief form of the affective neuroscience personality scales. Psychol Assess (2013) 25:826–43. doi: 10.1037/a0032576
118. Panksepp J. Affective neuroscience: the foundations of human and animal emotions. New York: Oxford University Press (1998).
119. Moeller FG, Hasan KM, Steinberg JL, Kramer LA, Dougherty DM, Santos RM, et al. Reduced anterior corpus callosum white matter integrity is related to increased impulsivity and reduced discriminability in cocaine-dependent subjects: diffusion tensor imaging. Neuropsychopharmacology (2005) 30:610–7. doi: 10.1038/sj.npp.1300617
120. Schindler A, Bröning S. A review on attachment and adolescent substance abuse: empirical evidence and implications for prevention and treatment. Subst Abus (2015) 36:304–13. doi: 10.1080/08897077.2014.983586
121. Alcaro A, Panksepp J. The SEEKING mind: primal neuro-affective substrates for appetitive incentive states and their pathological dynamics in addictions and depression. Neurosci Biobehav Rev (2011) 35:1805–20. doi: 10.1016/j.neubiorev.2011.03.002
122. Wright JS, Panksepp J. An evolutionary framework to understand foraging, wanting and desire the neuropsychology of the SEEKING system. Neuropsychoanalysis (2012) 14:5–39. doi: 10.1080/15294145.2012.10773683
123. Chiesa M, Fonagy P. Scientific research, the therapeutic community and psychodynamic psychotherapy. Clin Neuropsychiatry (2010) 7:173–80.
124. De Leon G. The therapeutic community: theory, model, and method. New York: Springer (2000). doi: 10.1891/9780826116673
125. Drummond DC. Theories of drugs craving, ancient and modern. Addiction (2001) 96:33–46. doi: 10.1046/j.1360-0443.2001.961333.x
127. Weber H, Loureiro de Assunção V, Martin C, Westmeyer H, Geisler FC. Reappraisal inventiveness: the ability to create different reappraisals of critical situations. Cogn Emot (2014) 28:345–60. doi: 10.1080/02699931.2013.832152
128. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
129. Abler B, Kessler H. Emotion regulation questionnaire-Eine deutschsprachige Fassung des ERQ von Gross und John. Diagnostica (2009) 55:144–52. doi: 10.1026/0012-1924.55.3.144
130. Ehrenthal JC, Dinger U, Horsch L, Komo-Lang M, Klinkerfuß M, Grande T, et al. Der OPD-Strukturfragebogen (OPD-SF): Erste Ergebnisse zu Reliabilität und Validitt. Psychother Psychosom Medizinische Psychol (2012) 62:25–32. doi: 10.1055/s-0031-1295481
131. Kessler H, Stasch M, Cierpka M. Operationalized psychodynamic diagnosis as an instrument to transfer psychodynamic constructs into neuroscience. Front Hum Neurosci (2013) 7:1–5. doi: 10.3389/fnhum.2013.00718
132. Cohen J. Statistical power analysis for the behavioral sciences. 2. Edition. Hillsdal, NJ: Lawrence Erlbaum Associates (1988).
133. Rowland J, Hamilton MK, Lino BJ, Ly P, Denny K, Hwang E-J, et al. Cognitive regulation of negative affect in schizophrenia and bipolar disorder. Psychiatry Res (2013) 208:21–8. doi: 10.1016/j.psychres.2013.02.021
134. Shaver PR, Mikulincer M. Attachment theory and research: resurrection of the psychodynamic approach to personality. J Res Pers (2005) 39:22–45. doi: 10.1016/j.jrp.2004.09.002
135. Vrtička P, Bondolfi G, Sander D, Vuilleumier P. The neural substrates of social emotion perception and regulation are modulated by adult attachment style. Soc Neurosci (2012) 7:473–93. doi: 10.1080/17470919.2011.647410
136. Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq (2015) 26:1–26. doi: 10.1080/1047840X.2014.940781
137. Troy AS, Shallcross AJ, Mauss IB. A person-by-situation approach to emotion regulation: cognitive reappraisal can either help or hurt, depending on the context. Psychol Sci (2013) 24:2505–14. doi: 10.1177/0956797613496434
138. Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry (1997) 4:231–44. doi: 10.3109/10673229709030550
139. Feeney JA, Noller P, Hanrahan M. Assessing adult attachment. In: Sperling MB, Berman WH, editors. Attachment in adults. New York: Guilford Press (1994). p. 128–52.
140. Hexel M. Validation of the German Version of the Attachment Style Questionnaire (ASQ) in participants with and without psychiatric diagnosis. Z Klin Psychol Psychother (2004) 33:79–90. doi: 10.1026/1616-3443.33.2.79
141. Leichsenring F. Development and first results of the borderline personality inventory: a self-report instrument for assessing borderline personality organization. J Pers Assess (1999) 73:45–63. doi: 10.1207/S15327752JPA730104
142. Di Pierro R, Preti E, Vurro N, Madeddu F. Dimensions of personality structure among patients with substance use disorders and co-occurring personality disorders: a comparison with psychiatric outpatients and healthy controls. Compr Psychiatry (2014) 55:1398–404. doi: 10.1016/j.comppsych.2014.04.005
143. Shedler J. The efficacy of psychodynamic psychotherapy. Am Psychol (2010) 65:98–109. doi: 10.1037/a0018378
144. Ravitz P, Maunder R, Hunter J, Sthankiya B, Lancee W. Adult attachment measures: a 25-year review. J Psychosom Res (2010) 69:419–32. doi: 10.1016/j.jpsychores.2009.08.006
145. Cassidy J, Jones JD, Shaver PR. Contributions of attachment theory and research: a framework for future research, translation, and policy. Dev Psychopathol (2013) 25:1415–34. doi: 10.1017/S0954579413000692
146. Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev (2013) 33:1010–24. doi: 10.1016/j.cpr.2013.07.007
147. Beckes L, Coan JA. The distress-relief dynamic in attachment bonding. In: Zayas V, Hazan C, editors. Bases of adult attachment: linking brain, mind and behavior. New York: Springer (2015). p. 11–33. doi: 10.1007/978-1-4614-9622-9_2
148. Mikulincer M, Shaver PR. The attachment behavioral system in adulthood: activation, psychodynamics, and interpersonal processes,” In: Zanna M. P. editor. Advances in experimental social psychology, San Diego CA: Academic Press (2003). p. 53–152. doi: 10.1016/S0065-2601(03)01002-5
149. Levy MS. Listening to our clients: the prevention of relapse. J Psychoactive Drugs (2008) 40:167–72. doi: 10.1080/02791072.2008.10400627
150. Patterson I, Pegg S, Dobson-Patterson R. Exploring the links between leisure boredom and alcohol use among youth in rural and urban areas of Australia. J Park Recreat Adm (2000) 18, 53–75.
151. Boys A. Understanding reasons for drug use amongst young people: a functional perspective. Health Educ Res (2002) 16:457–69. doi: 10.1093/her/16.4.457
152. Gidhagen Y, Holmqvist R, Philips B. Attachment style among outpatients with substance use disorders in psychological treatment. Psychol Psychother Theory Res Pract (2018) 91(4):490–508. doi: 10.1111/papt.12172
153. Zdankiewicz-Ścigała E, Ścigała DK. Relationship between attachment style in adulthood, alexithymia, and dissociation in alcohol use disorder inpatients. Mediational model. Front Psychol (2018) 9:1–10. doi: 10.3389/fpsyg.2018.02039
154. Cassidy J. The nature of the child’s ties. In: Cassidy J, Shaver PR, editors. Handbook of attachment. New York/London: Guilford (2016). p. 3–24.
155. Sewell J, Miltz A, Lampe FC, Cambiano V, Speakman A, Phillips AN, et al. Poly drug use, chemsex drug use, and associations with sexual risk behaviour in HIV-negative men who have sex with men attending sexual health clinics. Int J Drug Policy (2017) 43:33–43. doi: 10.1016/j.drugpo.2017.01.001
156. Bourne A, Reid D, Hickson F, Rueda ST, Weatherburn P. T. he Chemsex study: drug use in sexual settings among gay and bisexual men in Lambeth, Southwark and Lewisham. London: Sigma Research, London School of Hygiene & Tropical Medicine (2014).
157. Su S, Mao L, Zhao J, Chen L, Jing J, Cheng F, et al. Epidemics of HIV, HCV and syphilis infection among synthetic drugs only users, heroin-only users and poly-drug users in Southwest China. Sci Rep (2018) 8:1–10. doi: 10.1038/s41598-018-25038-y
158. Surratt HL, Kurtz SP, Buttram M, Levi-Minzi MA, Pagano ME, Cicero TJ. Heroin use onset among nonmedical prescription opioid users in the club scene. Drug Alcohol Depend (2017) 179:131–8. doi: 10.1016/j.drugalcdep.2017.06.034
159. Kraanen FL, Emmelkamp PMG. Substance misuse and substance use disorders in sex offenders: a review. Clin Psychol Rev (2011) 31:478–89. doi: 10.1016/j.cpr.2010.11.006
160. Kohut H. Narzißmus—Eine Theorie der Behandlung narzißtischer Persönlichkeitsstörungen. Frankfurt am main: suhrkamp (1971).
161. Cicchetti D, Handley ED. Child maltreatment and the development of substance use and disorder. Neurobiol Stress (2019) 10:100144. doi: 10.1016/j.ynstr.2018.100144
162. Fuchshuber J, Hiebler-Ragger M, Kresse A, Kapfhammer H-P, Unterrainer HF. Depressive symptoms and addictive behaviors in young adults after childhood trauma: the mediating role of personality organization and despair. Front Psychiatry (2018) 9:1–12. doi: 10.3389/fpsyt.2018.00318
163. Lindberg MA, Zeid D. Interactive pathways to substance abuse. Addict Behav (2017) 66:76–82. doi: 10.1016/j.addbeh.2016.11.016
164. Fairbairn CE, Briley DA, Kang D, Fraley RC, Benjamin L, Ariss T. A meta-analysis of longitudinal associations between substance use and interpersonal attachment security. Psychol Bull (2018) 144:532–55. doi: 10.1037/bul0000141
165. Tuhkanen H, Pajulo M, Jussila H, Ekholm E. Infants born to women with substance use: exploring early neurobehavior with the Dubowitz neurological examination. Early Hum Dev (2019) 130:51–6. doi: 10.1016/j.earlhumdev.2018.12.019
166. Puzhko S, Roy É, Jutras-Aswad D, Artenie AA, Fortier E, Zang G, et al. High hepatitis C incidence in relation to prescription opioid injection and poly-drug use: assessing barriers to hepatitis C prevention. Int J Drug Policy (2017) 47:61–8. doi: 10.1016/j.drugpo.2017.05.027
167. George C, Kaplan N, Main M. Adult attachment interview, third edition. Berkeley: Department of Psychology, University of California.
168. Janeiro L, Ribeiro E, Faísca L, José M, Miguel L. Therapeutic alliance dimensions and dropout in a therapeutic community: “Bond with me and I will stay”. Ther Communities (2018) 39:73–82. doi: 10.1108/TC-12-2017-0036
169. Kavanagh DJ, Connolly JM. Assessment of co-occurring addictive and other mental disorders. In: Miller PM, editor. Evidence-based addiction treatment. Oxford: Elsevier (2009). p. 89–117. doi: 10.1016/B978-0-12-374348-0.00005-7
170. Hesse M. Treating the patient with comorbidity. In: Miller PM, editor. Evidence-based addiction treatment. Oxford: Elsevier (2009). p. 327–43. doi: 10.1016/B978-0-12-374348-0.00017-3
171. Messman-Moore TL, Bhuptani PH. A review of the long-term impact of child maltreatment on posttraumatic stress disorder and its comorbidities: an emotion dysregulation perspective. Clin Psychol Sci Pract (2017) 24:154–69. doi: 10.1111/cpsp.12193
172. Davis JP, Dworkin ER, Helton J, Prindle J, Patel S, Dumas TM, et al. Extending poly-victimization theory: differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abus Negl (2019) 89:165–77. doi: 10.1016/j.chiabu.2019.01.009
173. Kaag AM, Schulte MHJ, Jansen JM, van Wingen G, Homberg J, van den Brink W, et al. The relation between gray matter volume and the use of alcohol, tobacco, cocaine and cannabis in male polysubstance users. Drug Alcohol Depend (2018) 187:186–94. doi: 10.1016/j.drugalcdep.2018.03.010
174. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J (2009) 26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x
175. Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend (2014) 136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011
176. Trenz RC, Scherer M, Harrell P, Zur J, Sinha A, Latimer W. Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addict Behav (2012) 37:367–72. doi: 10.1016/j.addbeh.2011.11.011
Keywords: substance use disorder, attachment, emotion regulation, treatment, polydrug use disorder
Citation: Hiebler-Ragger M and Unterrainer H-F (2019) The Role of Attachment in Poly-Drug Use Disorder: An Overview of the Literature, Recent Findings and Clinical Implications. Front. Psychiatry 10:579. doi: 10.3389/fpsyt.2019.00579
Received: 25 April 2019; Accepted: 23 July 2019;
Published: 27 August 2019.
Edited by:
Carlos Roncero, University of Salamanca Health Care Complex, SpainReviewed by:
Gail Horton, Florida Atlantic University, United StatesCopyright © 2019 Hiebler-Ragger and Unterrainer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Human-Friedrich Unterrainer, aHVtYW4udW50ZXJyYWluZXJAdW5pdmllLmFjLmF0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.