
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry , 06 November 2018
Sec. Psychological Therapy and Psychosomatics
Volume 9 - 2018 | https://doi.org/10.3389/fpsyt.2018.00567
This article is part of the Research Topic Reducing the Mortality Gap in People with Severe Mental Disorders: The Role of Lifestyle Psychosocial Interventions View all 19 articles
 Isabella Berardelli1
Isabella Berardelli1 Valentina Corigliano1
Valentina Corigliano1 Michael Hawkins2
Michael Hawkins2 Anna Comparelli1
Anna Comparelli1 Denise Erbuto1
Denise Erbuto1 Maurizio Pompili1*
Maurizio Pompili1*Over the past years, there has been a growing interest in the association between lifestyle psychosocial interventions, severe mental illness, and suicide risk. Patients with severe mental disorders have higher mortality rates, poor health states, and higher suicide risk compared to the general population. Lifestyle behaviors are amenable to change through the adoption of specific psychosocial interventions, and several approaches have been promoted. The current article provides a comprehensive review of the literature on lifestyle interventions, mental health, and suicide risk in the general population and in patients with psychiatric disorders. For this purpose, we investigated lifestyle behaviors and lifestyle interventions in three different age groups: adolescents, young adults, and the elderly. Several lifestyle behaviors including cigarette smoking, alcohol use, and sedentary lifestyle are associated with suicide risk in all age groups. In adolescents, growing attention has emerged on the association between suicide risk and internet addiction, cyberbullying and scholastic and family difficulties. In adults, psychiatric symptoms, substance and alcohol abuse, weight, and occupational difficulties seems to have a significant role in suicide risk. Finally, in the elderly, the presence of an organic disease and poor social support are associated with an increased risk of suicide attempt. Several factors may explain the association between lifestyle behaviors and suicide. First, many studies have reported that some lifestyle behaviors and its consequences (sedentary lifestyle, cigarette smoking underweight, obesity) are associated with cardiometabolic risk factors and with poor mental health. Second, several lifestyle behaviors may encourage social isolation, limiting the development of social networks, and remove individuals from social interactions; increasing their risk of mental health problems and suicide.
Several well-established psychosocial factors and lifestyle behaviors including life satisfaction, economic adversities, family environment, major life and occupational stressor(s), substance and alcohol abuse, medical conditions, cigarette smoking, being sedentary, underweight or obese, and diet are considered prominent factors in the development of severe mental disorders and suicide risk. Psychiatric patients, including patients affected by schizophrenia, bipolar disorder, schizoaffective disorder and depressive disorder, have higher mortality rates and higher suicide risk compared to the general population (1, 2). Increased mortality is probably also due, besides psychiatric impairment and psychotropic medication use, to unhealthy lifestyle behaviors including poor diet, excessive smoking, alcohol use, and lack of exercise. These unhealthy lifestyle behaviors can increase the development of many physical diseases including overweight, obesity, metabolic syndrome, diabetes, cardiovascular disease, cerebrovascular disease, hepatitis, amongst other medical conditions (3, 4).
Suicide has been described as a multi-faceted construct in relation to psychiatric symptoms, medical conditions, and lifestyle risk factors (5–7). Moreover, lifestyle behaviors are involved in the pathogenesis of medical and severe psychiatric disorders such as depression and psychosis (8, 9), increasing the risk of suicide (10).
Recently, considerable attention has been paid to the concept of life satisfaction and well-being as psychosocial indicators of mental health (11). It has been hypothesized (12, 13) that life satisfaction and meaning in life can help people overcome adversity. Factors associated with optimal well-being and life satisfaction included prudent lifestyle behaviors such as healthy eating, adequate sleep, physical activity, avoiding tobacco, and limiting alcohol consumption (14). Few studies have revealed that suicide ideation is related to psychiatric symptomatology, lifestyle behavior, and lower life satisfaction (15, 16). Koivumaa-Honkanen et al. (17) in a study of 29,067 Finnish adults found that unhappiness was associated with an increased risk of suicide. This group also reported that unhappiness was associated with older age, male gender, sickness, living alone, smoking, heavy alcohol consumption, physical inactivity, and belonging to intermediate social class.
In the past few decades, a lot of progress has been made to identify public health strategies for the prevention of mental health and suicide. Although the approach to suicide has always involved clinical aspects, especially the assessment and the treatment of depression (18), it seems necessary to consider also risk factors that can be identified and modified through specific lifestyle interventions.
Based on data demonstrating how lifestyle behaviors may be involved in both the genesis of severe psychiatric disorders and in increasing suicide risk (19), we aimed to provide a narrative review synthetizing existing published literature on lifestyle interventions and suicide prevention in psychiatric patients behavior. Additionally, we provide a review of the literature on lifestyle interventions promoting mental health reducing suicide risk in the general population and in patients with psychiatric disorders.
Lifestyle behaviors and interventions may differ at different life stages of life. Given this, we reviewed lifestyle behaviors and interventions associated with suicide risk in three age group categories: adolescents and young people (age 16–30), young adults and adults (age 30–65), and older adults and elderly (age >65).
We searched the relevant databases including MEDLINE, ISI Web of Knowledge – Web of Science Index, Cochrane Reviews Library and PsychoINFO for papers published from January 2000 to March 2018.
The following keywords were used: “lifestyle intervention,” “life satisfaction”, “diet,” “physical activity,” “nutrition,” “cholesterol,” “diabetes,” “lifestyle behaviors,” “cigarette smoke” matched with “suicide risk,” “healthy population,” “mental disorders,” “schizophrenia,” “psychotic disorders,” “bipolar disorder,” “depression,” “adolescents,” “adults,” and “elderly.” Inclusion criteria were: studies adopting psychosocial interventions for promoting changes in lifestyle behaviors, studies aiming to improve patients' physical status (evaluated in terms of body mass index – BMI, level of physical activity, smoking status, etc.) and studies that assess the association between lifestyle behaviors and psychiatric disorders and suicide risk. Only papers written in English were included. Studies included in this narrative review were those that examined suicide and lifestyle interventions in adolescence, young adults or adults and the elderly. Studies in which the age group investigated was not clearly defined were excluded from this review.
Randomized controlled trials, clinical controlled trials, pilot studies, cohort studies and reviews were considered eligible for the review process. In addition, the reference lists of all included studies and of relevant existing systematic reviews were checked for possible studies. Papers were screened by an independent researcher (IB) and assessed for eligibility by a senior expert (MP).
Suicidal ideation and suicide attempt are relatively common in this phase of life; with completed suicide being the second most common cause of death in adolescents (20).
It has been described that 10–20% of adolescents suffer from a mental disorder (21). Adolescence is often associated with elevated levels of anxiety, stress, and adverse life events, which may lead to maladaptive feelings of hopelessness, personal failure, and suicidal ideation (22). While positive coping strategies, efficacious problem-solving skills, and general life satisfaction are considered protective for suicide (23). Common severe psychiatric disorders in adolescents include depression, anxiety disorders, behavioral problems (e.g., oppositional defiant disorder or conduct disorder), early psychosis, eating disorders (e.g., anorexia nervosa and bulimia nervosa) and addictive disorders (24), all risk factors for suicidal behavior in adolescents (25, 26).
Unhealthy lifestyle behaviors may impact mental health and suicidal behavior by influencing emotions and judgement. Studies have demonstrated that adolescents with first-episode psychosis have a high prevalence of tobacco, alcohol and cannabis use, selective dietary habits, lower physical activity, and lower level of activity during leisure time (27–30). Other studies have demonstrated a close relationship between cannabis use, hypomania, mania, and suicide risk in adolescents (31, 32). Furthermore, a relationship between weight, social relations, and depressive symptoms has been described (33); stressing the link between lifestyle behavior, mental health and suicide risk.
High symptom of any personality disorder in adolescence have negative repercussions on functioning over the subsequent 10 to 20 years. For instance, elevated Borderline Personality Disorder (BPD) symptoms in adolescence have been shown to be an independent risk factor for substance-use disorders during early adulthood, alcohol consumption, psychopathology, health risk behaviors, and suicide risk (34–37). Prevention and early intervention for BPD are necessary not only for reduction on psychiatric symptoms but also for improving psychosocial functioning and decreasing substance abuse, which are known risk factors for suicide.
Im et al. (38) examined 370,568 students with the aim of recognizing risk factors for suicidal ideation in adolescents found that low sleep satisfaction, high stress, alcohol consumption, smoking, and sexual activity, were significant lifestyle factors associated with suicidal ideation. Lee et al. (39) in a sample of 860 adolescents confirmed the relationship between several lifestyle behaviors and suicide risk including sleep disturbance, internet game addiction, and interpersonal factors (e.g., family conflicts and peer problems). A recent systematic review of 17 studies recognized that, in adolescents, a diagnosis of binge eating disorder was predictive of suicidality, while a high body mass index (BMI) was not (40). Substance-use disorders, including alcohol use disorder, are considered one of the most important risk factors associated with suicide risk during adolescence (41, 42). Moreover, it has been reported that the more the number of substances abused the higher the suicide risk (43). Borges et al. (44) in a recent trial on 1,071 young Mexicans reported that the use of cannabis before age 15, high frequency of cannabis use and another recent substance-use disorder increased the risk of suicide. Park et al. (45) collected data from 68,043 adolescents with the purpose of investigating the undesirable effects of frequent use of caffeinated energy drinks. Their results indicated that energy drink consumption was associated with sleep dissatisfaction, severe stress, depressive mood, suicidal ideation, suicide plan, and suicide attempt. Similarly, Kim et al. (46) in a study of 121,106 Korean adolescents confirmed that severe stress, inadequate sleep, and low school performance were associated with more energy drink consumption and suicide attempts.
Evidence suggests that sedentary lifestyle may impact emotional and mental health in adolescents (47). A systematic review on this topic found a strong relationship between sedentarism, depressive symptomatology, psychological distress, and suicide ideation in adolescents (48). In this regard, Lester et al. (49) demonstrated that participation in sports reduced the incidence of suicidal ideation.
Internet use has a mixed effect on children and young people's well-being. On one hand, internet users may develop a social support that may be artificial. On the other hand, it exposes adolescents to cyberbullying and meeting strangers online (50). In recent years, there has been an increased interest in the relationship between internet use, cyber-bullying, and suicide (51). A recent systematic review of 51 articles investigated the relationship between internet use and self-harm/suicidal behavior. This review demonstrated that internet addiction and elevated levels of internet use, were associated with a higher suicide risk (52). John et al. (53) highlighted that compared to non-victims of cyberbullying, victims of cyberbullying had a greater risk of both self-harm and suicidal behaviors. Rodelli et al. (54) evaluated the associations between physical activity, sport participation, healthy diet, higher sleep duration and lower levels of smoking and lower levels of alcohol use, and suicidal ideation when faced to cyberbullying. Results showed that cyberbullying victimization was associated with higher suicidal ideation while increased physical activity, sleeping longer, healthy diet and lower levels of smoking were associated with lower suicidal ideation. Moreover, a systematic review on the role of web technologies, mobile solutions, social networks, and machine learning in the prevention of suicide risk highlighted that many of these methods can help prevent suicide (55).
The potential role of family relationships (conflict, negative relationship with parents, other) as a risk factor for suicide was evaluated in 36,757 French adolescents (56). Results from this study demonstrated that negative relationships with parents and parental discord was significantly associated with suicide risk and/or depression in adolescents regardless of gender. The role of family interventions in the prevention of mental illness, substance abuse, and suicide ideation and attempts have been evaluated (57). The author suggested that family interventions could be useful in the prevention of suicidal ideation and behavior in both adolescents and parents.
In adults, the relationship between lifestyle behavior, severe psychiatric symptoms, and suicide risk is well documented (58, 59). Recent literature has demonstrated that behavioral lifestyle interventions help patients with serious mental illnesses lose weight and reduce cigarette smoking. Behavioral lifestyle interventions also helped patients achieve changes in fasting glucose levels in patients taking antipsychotic medications (60); simultaneously reducing the possibility of developing medical conditions; indirectly reducing the risk of suicide.
Studies have demonstrated that adult psychiatric inpatients who had attempted suicide presented higher levels of sedentarism and higher tobacco use compared to psychiatric patients who did not attempt suicide (61, 62).
Research reporting on the relationship between suicide, obesity, total serum cholesterol, and dietary patterns is controversial (63). Research examining the relationship between lipid profile and suicide attempts have shown that compared to non-attempters, suicide attempters had lower cholesterol levels (64, 65). More recently, a case control study of a Mexican population found a positive association between lower cholesterol levels and suicide attempt (66). Although the mechanism behind hypocholesterolemia and suicide has not been elucidated, it has been hypothesized that altered cholesterol at synaptic lipid rafts cause a decrease in serotonin transmission, neurotransmitter implicated in the pathophysiology of suicide (67, 68). A recent systematic review and meta-analysis of 11 studies evaluating lipid profile in suicide attempters and non-attempters in people with bipolar disorder failed to clarify the relationship between LDL-cholesterol, triglycerides and suicide in these patients. Shrivastava et al. (69) in a naturalistic cross-sectional cohort study of 60 patients with early psychosis, found that low levels of cholesterol were present only in the group of patients with severe suicidality. Similarly, Messaoud et al. (70) found a positive association between low plasma cholesterol level and suicidal behavior in patients with major depressive disorder.
Studies on the associations between depression, suicidal behavior, glucose levels or insulin resistance are scarce. Higher glucose levels have been associated with dysthymia (71) and higher HbA1c concentrations have been associated with psychotic depression (72). Koponen et al. (73) in 448 patients aged 35 years old found that patients with depression and suicidal behavior had higher blood glucose concentrations at baseline and at 2 h in the oral glucose tolerance test (OGTT).
Although dietary habits have been linked to depression, only few studies have examined the association between dietary patterns and suicide risk (74, 75). Li et al. (75) found that a dietary pattern comprise of vegetables, fruits, potatoes, soy products, mushrooms, seaweed and fish was associated with a decreased risk of suicide. Mukamal et al. (74) reviewed retrospectively the dietary information of 6,803 adults describing the differences in eating habits between suicide attempters and non-attempters. Results indicated that male attempters presented low consumption of vegetables and female attempters presented insufficient fruit consumption. It was further observed that female attempters ate significantly less fish and sea food compared to female non-attempters. Finally, results showed that fruits, vegetables, and meat were significantly under-consumed in those individuals with a history of suicide attempt.
The relationship between body mass index (BMI) and suicide risk in adult seems controversial. A study by Perera et al. (63) supported the hypothesis of an inverse association between BMI and completed suicide, where underweight was associated with an increased risk of completed suicide while obesity and overweight were associated with a decreased risk of suicide in comparison to people of normal weight. Contrarily, Branco et al. (76) stressed that obesity was associated with a higher prevalence of suicide risk, especially in women. Kim et al. (77) on 6,022 nationally representative sample of Korean adults aged 18 to 74 found that being underweight was associated with higher suicide risk and obesity was associated only with risk of suicide ideation but not with suicide attempt. In the same study, underweight individuals were more likely to report severe level of perceived stress (OR, 1.7; 95% Cl, 1.26–2.17) and life dissatisfaction (OR, 1.3; 95% Cl, 1.07–1.68) compared to obese individuals.
A strong relationship exists between well-being and physical activity, sports activities and level of fitness (78, 79). Physical activity and sports activities are considered protective lifestyle behaviuors against stress, depression and other unhealthy behaviors linked to medical illness. In particular, sport activities improve coronary functioning and reduce obesity prevalence (61, 80). Physical activity could be effective in reducing mental health disorders and suicidal behaviors through biological and psychosocial mechanisms; for example, releasing endorphins, increasing serotonin and norepinephrine synthesis, increasing the sense of mastery, self-esteem and social interaction (81). Vancampfort et al. (82) in a recent metanalysis showed that in adults, low physical activity was associated with higher suicide risk. Adams et al. (83) demonstrated that vigorous/moderate physical activity was associated with a positive perceived health and modestly associated with psychiatric symptoms and suicidal ideation reduction; confirming the link between physical activity and well-being.
In patients with schizophrenia, the evidence suggests that increasing physical exercise promotes wellbeing, and improves mental health in these patients (84). Dietary habits and levels of physical activity were evaluated in 428 people with schizophrenia spectrum disorders and increased waist circumference demonstrating that in these patients the intake of fiber, vegetables, fruit, and fish were insufficient and these patients also had low levels of physical activity. Furthermore, negative symptoms were associated with poor diet and less physical activity (85).
The positive relationship between smoking and suicide risk in adult patients with psychotic disorders has been evaluated in a systematic-review and a meta-analysis of observational studies on this topic (86). The same authors, in a randomized study, investigated the effect of smoking reduction on suicidality on 255 patients with a psychotic disorder. This author found that smoking reduction, besides the positive effects on physical health, had a protective effect on suicidal ideation in people with psychosis (87). Bhatt et al. (88) characterized and identified risk factors for suicide attempt in patients with psychiatric disorders. Findings from this study indicated no significant differences on demographic characteristics between psychiatric inpatients who attempted suicide and psychiatric inpatients who did not attempt suicide. The only risk factors for suicide in psychiatric patients found in this study were the presence of impulsivity and borderline personality symptoms. Howard et al. (89) in a recent population-based cohort study on 12,888 subjects (6,456 men, 6,432 women) investigated the relationship between chronic disease conditions, smoking habits, alcohol consumption, depressive symptoms, personality type, and other psychological parameters and suicide found that male sex, obesity, smoking, and living alone were associated with depression and with risk of suicide.
Several studies have focused on the role of occupation and work stressors on suicide risk. Research on this topic has shown that work characteristics and personal resources are linked to depression and suicide attempts (90). A study on 2,855 employees demonstrated that job autonomy, task variety, work-family conflict, family-work conflict, and job dissatisfaction contributed to suicide attempts (89). Furthermore, Kerr et al. (91) showed that poor interpersonal relationships, unemployment, debt and financial difficulties contribute to an increased risk of suicide in the general population. A recent study of 2,027 employed patients in primary care setting examined the association between workplace and suicidal ideation (92). Suicidality was significantly associated with work intensity in men and with work-related emotional demands in women.
Alcohol and substance abuse can worsen psychological well-being and contribute to suicide risk (93). Consumption of alcohol immediately prior to suicide is common (94, 95), with an estimated 37% of deaths from suicide having positive blood alcohol concentrations on toxicology screening indicating acute alcohol consumption before death (96). Bowden et al. (97) in a large cohort study of 2,803,457 residents of Wales, UK, highlighted the relationship between emergency alcohol-related hospital admission and the increased risk of suicide. A recent systematic review of 108 studies explored the associations between substance use and suicide risk in low- and middle-income countries (98) demonstrated an association between alcohol use, intoxication and pathological use of alcohol, tobacco, cannabis, illicit drugs and non-medical use of prescription drugs and suicide risk. Furthermore, Choi et al. (99) examined blood alcohol concentration (BAC) among suicide decedents aged 50 years or older. This study showed that alcohol problems prior to suicide, relationship problems and death/suicide of family/friends were associated with greater odds of having a positive BAC. This study also found that alcohol intoxication was linked to more violent means of suicide.
Over 20% of adults aged 60 and over suffer from a psychiatric or neurological disorder. In the elderly, severe mental disorders present differently than in younger adults. The most common mental and neurological disorders in this age group are depression and dementia. However, anxiety disorders, schizophrenia and psychotic disorders, and substance use problems are also prevalent (100). A body of literature supports the association between late-life suicide ideation and various risk factors including depression and hopelessness (101, 102), while subjective well-being and meaning in life have been identified as protective factors for suicide in older adults (101). Innamorati et al. (103) in a study using psychological autopsy interviews studied 117 old-old adults who died by suicide and compared them to 97 young-old adults (6,574 years), 98 middle aged (50–64 years) suicide victims, and 117 psychiatric outpatients 75 years and older without a history of suicidal behaviors. They found that, in the elderly, unlike others stages of life, loneliness and lack of social support, were associated with risk of suicide. Physical illness, chronic severe pain, debilitating disease, and diagnosis of a terminal illness are common antecedents to suicide in older adults (104). Lee et al. (39) after analyzing age and sex-related features and suicide risk in the elderly stressed that the only stable risk factor for suicide in this age group was the negative perception of one's own health status.
Difficulties in interpersonal relations, social interactions, and social participation have been also linked to suicidal ideation and suicidal intent in the elderly (105). Mogensen et al. (106) reported that in the elderly, suicide risk appeared highest during the 6 months following the loss of a close relative and McLaren et al. (107) observed that widowhood was associated with suicidal ideation both in men and women. A longitudinal study on the importance of social support while adjusting to loneliness in bereaving elderly persons (108) and other studies examining on the importance of social supports reported that primary prevention programs designed specifically to increase social relations could decrease suicide risk (109). Older people are at risk for health decline and loss of independence that can affect social interactions negatively. Clark et al. (110) evaluated the effectiveness of lifestyle interventions in promoting well-being in independently living older people and Lapierre et al. (111) in a systematic review of 19 studies focusing on lifestyle programs for older adults, highlighted that psychoeducational programs and decreasing social isolation in this age group are effective interventions in the prevention of suicide. More recently, Okolie et al. (112) considered telephone counseling for vulnerable older adults and community-based programs incorporating education, gatekeeper training, depression screening, and group activities, as valid therapeutic options in preventing suicidal ideation. Lifestyle interventions in the areas of social interaction (113), personal goals (114), coping, and adaptive behavior (113), emotional flexibility (115), social skills (116), self-esteem (117), sense of belonging (118), reasons for living (119), hope (120), meaning in life (101, 121), religion or spirituality (122) could became promising directions to prevent suicide in older adults.
Several studies have demonstrated the importance of a balanced diet to prevent depression (123, 124) and of sleep-based interventions to prevent suicide (125). Considering that hypnotics use in the elderly has been associated with an increased risk of suicide (126), behavioral treatment of insomnia represents an efficacious alternative to pharmacotherapy in this age group (127). O' Rourke et al. (128) studied specific predictors of suicide in a sample of 220 older adults affected by Bipolar Disorder (BD). Alcohol misuse, medication non-adherence, and cognitive impairment were found to be direct predictors of suicide in these patients, while sleep disturbances acts as a risk factor on suicide ideation via depressive symptoms. Contrary to what happens in other age groups, a link between smoking prevalence and suicide rates in the elderly has not been observed (129).
In this article, we reviewed a growing body of literature demonstrating a relationship between lifestyle behaviors, mental health, and suicide risk (Table 1) in differing stages of life (Table 2) and in severe psychiatric disorders (Table 3). Our review suggests that enhancing protective factors and reducing risk factors known to increase suicidal behaviors (75, 130–132) could help prevent suicide in some individuals. Given the high comorbidity between psychiatric disorders and medical illnesses that result from unhealthy lifestyle behaviors, lifestyle interventions to reduce medical diseases, and increase patient's well-being are urgently needed.
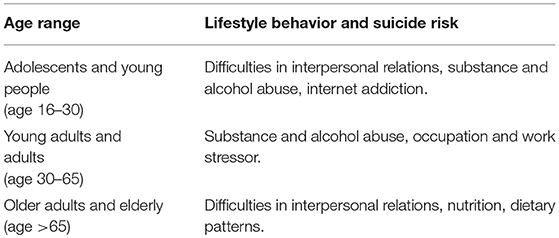
Table 2. Common Lifestyle behaviors implicated in suicide risk in different age ranges (based on results of studies included in this review).
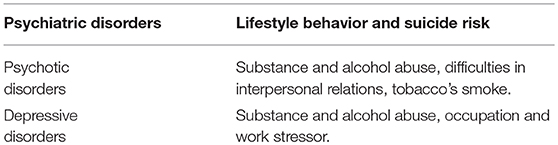
Table 3. Common Lifestyle behaviors implicated in suicide risk in psychiatric disorders (based on results of studies included in this review).
The relationship between lifestyle behavior and suicide is complex and multifactorial. Unhealthy lifestyle behaviors can directly increase the risk of suicide; at the same time increasing the risk for many medical diseases. It is well known that medical illnesses are associated with disability, social isolation and associated with an increased risk of suicide. Sedentary behaviors, underweight, obesity, cigarette smoking, and alcohol abuse are associated with cardiometabolic risk factors, poor mental health, and severe psychiatric disorders. These factors contribute to an increased risk of suicide. Sedentary behaviors, weight issues and fewer social supports contribute to social isolation, limiting the development of social relationships, which increase the risk of developing mental health problems and suicide. Adopting healthy lifestyle behaviors are indispensable for both, improving health and for the prevention of suicide at any stage in life.
Studies included in this article showed different lifestyle behaviors in different lifestages. In adolescent and young adults there are multiple important risk factors for suicide including psychosis, depression, low sleep satisfaction, high stress, substance abuse, alcohol consumption, smoking, sexual activity, internet addiction, interpersonal factors, personality disorders, anxiety or conduct disorders, eating disorders, and aggressive, irritable and antisocial tendencies (38, 39). Though it has been demonstrated that school-based suicide prevention programs increase knowledge on suicide without really preventing suicidal behaviors (133), it seems necessary to consider prevention programs that identify substance abuse, educational competencies (literacy, study skills, time management), educational environment, school programs, social interactions, academic attainment, cognitive progress, emotional control, behavioral expectations, physical and moral development, and encouragement of active engagement in sports.
In adults, lifestyle interventions on smoking, heavy alcohol consumption, physical inactivity, BMI, sedentarism, and eating habits should play a significant role in suicide prevention (17, 65). Effective lifestyle prevention programs in adults can be developed through screening programs identifying and assessing at-risk groups. These programs should include lifestyle training, psychoeducation, support/skills training and crisis response and referral resources (134). In patients with severe psychiatric disease, strategies that promote exercise and sport activities, that reduce caffeine consumption and other health-adverse behaviors are particularly important for the reduction of psychotic symptoms, depression, anxiety, low self-esteem, and life dissatisfaction, factors that increase suicide risk. Gallego et al. (135) suggested that in patients with either schizophrenia spectrum disorders or affective disorders, physicians should be alert for the presence of a previous suicidal attempts and financial or relationship losses, factors that can increase suicidal risk. Furthermore, psychiatric hospitalization, a close psychiatric follow up, collaboration with family would be important strategies in reducing the risk of suicidal behavior in patients affected by severe psychiatric disorders.
Finally, in the elderly, difficulties in interpersonal relations, social isolation and the consequences of physical disability can represent targeted and specific points for intervention. The concomitant presence of depressive symptoms and stressing life events including loneliness and physical illness should be considered warning signs for suicidal risk (136). In the elderly, innovative strategies should promote positive aging, involve family and community gatekeepers, and use telecommunications to identify older adult at risk of suicide (112). Psychosocial interventions influence depressive symptoms and considering that mental illness is one of the most significant factors in suicide; psychosocial interventions should be part of suicide prevention programs in the elderly. Further trials are warranted, especially for the most promising type of interventions for preventing suicide, that is, social activities (137, 138).
When interpreting the results of this review, several limitations should be considered. First, this is a narrative review, therefore, studies were subjectively selected, which could have led to selection bias. Second, we only selected articles in English leaving relevant articles in other languages out of our review. Finally, we did not draw a distinction between gender and risk factors for suicide.
Lifestyle behavior is of paramount importance for suicide prevention as maladaptive maneuvers (such as drinking or drug abuse) as to face increased psychological pain and distress consistently reduce cognitive skill to solve source of suffering. Furthermore, reduced quality of life as observed by impairment of some psychiatric disorders can be worsened by low exercise, excessive smoking, poor diet, and determinants associated with pharmacological treatment. Community mental health with proper programs such as assertive community treatment, psychoeducational family treatment, social skills training, and psychosocial therapies are important interventions that can incorporate education on lifestyle and ultimately reduce suicide risk.
IB and VC searched the literature and provided first draft. MH, AC, and DE independently reviewed the paper and added relevant information. MP provided the intellectual impetuous and supervised the entire process of development of the paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascularmortality in persons with schizophrenia. Curr Opin Psychiatry (2012) 25:83–8. doi: 10.1097/YCO.0b013e32835035ca
2. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. (2013) 10:425–48. doi: 10.1146/annurev-clinpsy-032813-153657
3. De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry (2011) 10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x
4. Smith DJ, Langan J, McLean G, Guthrie B, Mercer SW. Schizophrenia is associated with excess multiple physical-health comorbidities but low levels of recorded cardiovascular disease in primary care: cross-sectional study. BMJ Open (2013) 3:e002808. doi: 10.1136/bmjopen-2013-002808
5. Zhang J, Xiao S, Zhou L. Mental disorders and suicide among young rural Chinese: a case-control psychological autopsy study. Am J Psychiatry (2010) 167:773–81. doi: 10.1176/appi.ajp.2010.09101476
6. Tousignant M, Pouliot L, Routhier D, Vrakas G, McGirr A, Turecki G. Suicide,schizophrenia, and schizoid-type psychosis: role of life events and childhoodfactors. Suicide Life Threat Behav. (2011) 41:66–78. doi: 10.1111/j.1943-278X.2010.00002.x
7. Park S, Lee Y, Youn T, Kim BS, Park JI, Kim H, et al. Association between level of suicide risk, characteristics of suicide attempts, and mental disorders among suicide attempters. BMC Public Health (2018) 18:477. doi: 10.1186/s12889-018-5387-8
8. Bruins J, Jörg F, Bruggeman R, Slooff C, Corpeleijn E, Pijnenborg M. The effects of lifestyle interventions on (long-term) weight management, cardiometabolic risk and depressive symptoms in people with psychotic disorders: a meta-analysis. PLoS ONE (2014) 9:e112276. doi: 10.1371/journal.pone.0112276
9. Sarris J, O'Neil A, Coulson CE, Schweitzer I, Berk M. Lifestyle medicine for depression. BMC Psychiatry (2014) 14:107. doi: 10.1186/1471-244X-14-107
10. Sharifi V, Eaton WW, Wu LT, Roth KB, Burchett BM, Mojtabai R. Psychoticexperiences and risk of death in the general population: 24-27 year follow-up of the Epidemiologic Catchment Area study. Br J Psychiatry (2015) 207:30–6. doi: 10.1192/bjp.bp.113.143198
11. Bray I, Gunnell D. Suicide rates, life satisfaction and happiness as markers for population mental health. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:333–7. doi: 10.1007/s00127-006-0049-z
12. Shmotkin D. Happiness in the face of adversity: reformulating the dynamic and modular bases of subjective well-being. Rev Gen Psych. (2005) 9:291–325. doi: 10.1037/1089-2680.9.4.291
13. Shrira A, Palgi Y, Ben-Ezra M, Shmotkin D. How subjective well-being and meaning in life interact in the hostile world? J Pos Psych. (2011) 6:273–85. doi: 10.1080/17439760.2011.577090
14. Prendergast KB, Schofield GM, Mackay LM. Associations between lifestyle behaviours and optimal wellbeing in a diverse sample of New Zealand adults. BMC Public Health (2016) 16:62. doi: 10.1186/s12889-016-2755-0
15. Chiu HF, Dai J, Xiang YT, Chan SS, Leung T, Yu X, et al. Suicidal thoughts and behaviours in older adults in rural China: a preliminary study. Int J Geriatr Psychiatry (2012) 27:1124–30. doi: 10.1002/gps.2831
16. Voracek M. National intelligence, suicide rate, and subjective well-being. Percept Mot Skills (2009) 109:718–20. doi: 10.2466/pms.109.3.718-720
17. Koivumaa-Honkanen H, Honkanen R, Koskenvuo M, Kaprio J. Self-reported happiness in life and suicide in ensuing 20 years. Soc Psychiatry Psychiatr Epidemiol. (2003) 38:244–8. doi: 10.1007/s00127-003-0625-4
18. Mercy JA, Rosenberg ML. Building a foundation for suicide prevention: the contributions of Jack, C. Smith Am J Prev Med. (2000) 19:26–30. doi: 10.1016/S0749-3797(00)00170-7
19. De Rosa C, Sampogna G, Luciano M, Del Vecchio V, Pocai B, Borriello G, et al. Improving physical health of patients with severe mental disorders: a critical review of lifestyle psychosocial interventions. Expert Rev Neurother. (2017) 17:667–81. doi: 10.1080/14737175.2017.1325321
20. Lunde I, Myhre Reigstad M, Frisch Moe K, Grimholt TK. Systematic Literature Review of Attempted Suicide and Offspring. Int J Environ Res Public Health. (2018) 15:E937. doi: 10.3390/ijerph15050937
21. Brooks TL, Harris SK, Thrall JS, Woods ER. Association of adolescent risk behaviours with mental health symptoms in high school students. J Adolesc Health (2002) 31:240–6. doi: 10.1016/S1054-139X(02)00385-3
22. Serafini G, Muzio C, Piccinini G, Flouri E, Ferrigno G, Pompili M, et al. Life adversities and suicidal behaviour in young individuals: a systematic review. Eur Child Adolesc Psychiatry (2015) 24:1423–46. doi: 10.1007/s00787-015-0760-y
23. Montross LP, Zisook S, Kasckow J. Suicide among patients with schizophrenia: a consideration of risk and protective factors. Ann Clin Psychiatry (2005) 17:173–82. doi: 10.1080/10401230591002156
24. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
25. McGinty J, Sayeed Haque M, Upthegrove R. Depression during first episode psychosis and subsequent suicide risk: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. (2017) 195:58–66. doi: 10.1016/j.schres.2017.09.040
26. Orri M, Galera C, Turecki G, Forte A, Renaud J, Boivin M, et al. Association of childhood irritability and depressive/anxious mood profiles with adolescent suicidal ideation and attempts. JAMA Psychiatry (2018) 75:465–73. doi: 10.1001/jamapsychiatry.2018.0174
27. Myles N, Newall HD, Curtis J, Nielssen O, Shiers D, Large M. Tobacco use before, at, and after first-episode psychosis: a systematic meta-analysis. J Clin Psychiatry (2012) 73:468–75. doi: 10.4088/JCP.11r07222
28. Pawełczyk T, Trafalska E, Pawełczyk A, Kotlicka-Antczak M. Differences in omega-3 and omega-6 polyunsaturated fatty acid consumption in people at ultra-high risk of psychosis, first-episode schizophrenia, and in healthy controls. Early Interv Psychiatry (2017) 11:498–508. doi: 10.1111/eip.12267
29. Sormunen E, Saarinen MM, Salokangas RKR, Telama R, Hutri-Kähönen N, Tammelin T, et al. Effects of childhood and adolescence physical activity patterns on psychosis risk-a general population cohort study. NPJ Schizophr. (2017) 3:5. doi: 10.1038/s41537-016-0007-z
30. Oluwoye O, Monroe-DeVita M, Burduli E, Chwastiak L, McPherson S, McClellan JM, et al. Impact of tobacco, alcohol and cannabis use on treatment outcomes among patients experiencing first episode psychosis: data from the national RAISE-ETP study. Early Interv Psychiatry (2018) doi: 10.1111/eip.12542. [Epub ahead of print].
31. Leite RT, Nogueira Sde O, do Nascimento JP, de Lima LS, da Nóbrega TB, Virgínio Mda S, et al. The use of cannabis as a predictor of early onset of bipolar disorder and suicide attempts. Neural Plast. (2015) 2015:434127. doi: 10.1155/2015/434127
32. Marwaha S, Winsper C, Bebbington P, Smith D. Cannabis use and hypomania in young people: a prospective analysis. Schizophr Bull. 44:1267–74. doi: 10.1093/schbul/sbx158
33. Brewis AA, Bruening M. Weight Shame, Social connection, and depressive symptoms in late adolescence. Int J Environ Res Public Health (2018) 15:E891. doi: 10.3390/ijerph15050891
34. Chanen, A. M., and McCutcheon, L. (2013). Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br J Psychiatry 54(Suppl.):s24–9. doi: 10.1192/bjp.bp.112.119180
35. Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. J Pers Disord. (2005) 19:466–86. doi: 10.1521/pedi.2005.19.5.466
36. Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: prognosis for functioning over 20 years. J Child Psychol Psychiatry (2008) 49:933–41. doi: 10.1111/j.1469-7610.2008.01930.x
37. Oldham JM. Borderline personality disorder and suicidality. Am J Psychiatry (2006) 163, 20–6. doi: 10.1176/appi.ajp.163.1.20
38. Im Y, Oh WO, Suk M. Risk factors for suicide ideation among adolescents: five-year national data analysis. Arch Psychiatr Nurs. (2017) 31:282–6. doi: 10.1016/j.apnu.2017.01.001
39. Lee H, Seol KH, Kim JW. Age and sex-related differences in risk factors for elderly suicide: Differentiating between suicide ideation and attempts. Int J Geriatr Psychiatry (2018) 33:e300–e306. doi: 10.1002/gps.4794
40. Conti C, Lanzara R, Scipioni M, Iasenza M, Guagnano MT, Fulcheri M. The relationship between binge eating disorder and suicidality: a systematic review. Front Psychol. (2017) 8:2125. doi: 10.3389/fpsyg.2017.02125
41. Galaif ER, Sussman S, Newcomb MD, Locke TF. Suicidality, depression, and alcohol use among adolescents: a review of empirical findings. Int J Adolesc Med Health (2007) 19:27–35. doi: 10.1515/IJAMH.2007.19.1.27
42. Pompili M, Serafini G, Innamorati M, Biondi M, Siracusano A, Di Giannantonio M, et al. Substance abuse and suicide risk among adolescents. Eur Arch Psychiatry Clin Neurosci. (2012) 262:469–85. doi: 10.1007/s00406-012-0292-0
43. Kokkevi A, Richardson C, Olszewski D, Matias J, Monshouwer K, Bjarnason T. Multiple substance use and self-reported suicide attempts by adolescentsin 16 European countries. Eur Child Adolesc Psychiatry (2012) 21:443–50. doi: 10.1007/s00787-012-0276-7
44. Borges G, Benjet C, Orozco R, Medina-Mora ME, Menendez D. Alcohol, cannabis and other drugs and subsequent suicide ideation and attempt among young Mexicans. J Psychiatr Res. (2017) 91:74–82. doi: 10.1016/j.jpsychires.2017.02.025
45. Park S, Lee Y, Lee JH. Association between energy drink intake, sleep, stress, and suicidality in Korean adolescents: energy drink use in isolation or in combination with junk food consumption. Nutr J. (2016). 15:87. doi: 10.1186/s12937-016-0204-7
46. Kim SY, Sim S, Choi HG. High stress, lack of sleep, low school performance, and suicide attempts are associated with high energy drink intake in adolescents. PLoS ONE (2017) 12:e0187759. doi: 10.1371/journal.pone.0187759
47. Teychenne M, Costigan SA, Parker K. The association between sedentarybehaviour and risk of anxiety: a systematic review. BMC Public Health (2015) 15:513. doi: 10.1186/s12889-015-1843-x
48. Hoare E, Milton K, Foster C, Allender S. The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phyc Act. (2016) 13:108. doi: 10.1186/s12966-016-0432-4
49. Lester D. Participation in sports teams and suicidal behaviour: an analysis of the 1995 national college health risk behaviour survey. Percept Mot Skills (2014) 119:38–41. doi: 10.2466/06.15.PMS.119c13z5
50. Robertson L, Skegg K, Poore M, Williams S, Taylor B. An adolescent suicide cluster and the possible role of electronic communication technology. Crisis (2012) 33:239–45. doi: 10.1027/0227-5910/a000140
51. Messina ES, Iwasaki Y. Internet use and self-injurious behaviours among adolescents and young adults: an interdisciplinary literature review and implications for health professionals. Cyberpsychol Behav Soc Netw. (2011) 14:161–8. doi: 10.1089/cyber.2010.0025
52. Marchant A, Hawton K, Stewart A, Montgomery P, Singaravelu V, Lloyd K, et al. A systematic review of the relationship between internet use, self-harm and suicidal behaviour in young people: the good, the bad and the unknown. PLoS ONE (2017) 12:e0181722. doi: 10.1371/journal.pone.0181722
53. John A, Glendenning AC, Marchant A, Montgomery P, Stewart A, Wood S, et al. Self-Harm, suicidal behaviours, and cyberbullying in children and young people: systematic review. J Med Internet Res. (2018) 20:e129. doi: 10.2196/jmir.9044
54. Rodelli M, De Bourdeaudhuij I, Dumon E, Portzky G, DeSmet A. Which healthy lifestyle factors are associated with a lower risk of suicidal ideation among adolescents faced with cyberbullying? Prev Med. (2018) 113:32–40. doi: 10.1016/j.ypmed.2018.05.002
55. Franco-Martín, M. A., Muñoz-Sánchez, J. L., Sainz-de-Abajo, B., Castillo-Sánchez, G., Hamrioui, S., and de la Torre-Díez, I. (2018). A systematic literature review of technologies for suicidal behaviour prevention. J Med Syst. 42:71 doi: 10.1007/s10916-018-0926-5
56. Consoli A, Peyre H, Speranza M, Hassler C, Falissard B, Touchette E, et al. Suicidal behaviours in depressed adolescents: role of perceived relationships in the family. Child Adolesc Psychiatry Ment Health (2003) 7:8. doi: 10.1186/1753-2000-7-8
57. Brent D. Prevention Programs to Augment Family and Child Resilience Can Have Lasting Effects on Suicidal Risk. Suicide Life Threat Behav. (2016) 46(Suppl. 1):S39–47. doi: 10.1111/sltb.12257
58. Diaz FJ, James D, Botts S, Maw L, Susce MT, de Leon J. Tobacco smoking behaviours in bipolar disorder: a comparison of the general population, schizophrenia, and major depression. Bipolar Disord. (2009) 11:154–65. doi: 10.1111/j.1399-5618.2009.00664.x
59. Bostock EC, Kirkby KC, Taylor BV. The Current Status of the Ketogenic Diet in Psychiatry. Front Psychiatry (2017) 8:43. doi: 10.3389/fpsyt.2017.00043
60. Green CA, Yarborough BJ, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. Am J Psychiatry (2015) 172:71–81. doi: 10.1176/appi.ajp.2014.14020173
61. Andriessen K, Krysinska K. Can sport events affect suicidal behaviour? A review of the literature and implications for prevention. Crisis (2009) 30:144–52. doi: 10.1027/0227-5910.30.3.144
62. Poorolajal, J., and Darvishi, N. (2016). Smoking and suicide: a meta-analysis. PLoS ONE 11:e0156348. doi: 10.1371/journal.pone.0156348
63. Perera S, Eisen RB, Dennis BB, Bawor M, Bhatt M, Bhatnagar N, et al. Body mass index is an important predictor for suicide: results from a systematic review and meta-analysis. Suicide Life Threat Behav. (2016) 46:697–736. doi: 10.1111/sltb.12244
64. Diaz-Sastre C, Baca-Garcia E, Perez-Rodriguez MM, Garcia-Resa E, Ceverino A, Saiz-Ruiz J, et al. Low plasma cholesterol levels in suicidal males: a gender- and body mass index-matched case-control study of suicide attempters and nonattempters. Prog Neuropsychopharmacol Biol Psychiatry (2007) 31:901–5. doi: 10.1016/j.pnpbp.2007.02.004
65. Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P. Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies. J Psychiatry Neurosci. (2016) 41:56–69. doi: 10.1503/jpn.150079
66. Segoviano-Mendoza M, Cárdenas-de la Cruz M, Salas-Pacheco J, Vázquez-Alaniz F, La Llave-León O, Castellanos-Juárez F, et al. Hypocholesterolemia is an independent risk factor for depression disorder and suicide attempt in Northern Mexican population. BMC Psychiatry (2018) 18:7. doi: 10.1186/s12888-018-1596-z
67. Bartoli F, Di Brita C, Crocamo C, Clerici M, Carrà G. Lipid profile and suicide attempt in bipolar disorder: A meta-analysis of published and unpublished data. Prog Neuropsychopharmacol Biol Psychiatry (2017) 79 (Pt B):90–5. doi: 10.1016/j.pnpbp.2017.06.008
68. Mathew B, Srinivasan K, Pradeep J, Thomas T, Mandal AK. Suicidal behaviour is associated with decreased esterified cholesterol in plasma and membrane fluidity of platelets. Asian J Psychiatr. (2018) 32:105–9. doi: 10.1016/j.ajp.2017.11.023
69. Shrivastava A, Johnston M, Campbell R, De Sousa A, Shah N. Serum cholesterol and Suicide in first episode psychosis: a preliminary study. Indian J Psychiatry (2017) 5:478–82. doi: 10.4103/psychiatry.IndianJPsychiatry_185_17
70. Messaoud A, Mensi R, Mrad A, Mhalla A, Azizi I, Amemou B, et al. Is low total cholesterol levels associated with suicide attempt in depressive patients? Ann Gen Psychiatry (2017) 16:20. doi: 10.1186/s12991-017-0144-4
71. Ceretta LB, Réus GZ, Abelaira HM, Jornada LK, Schwalm MT, Hoepers NJ, et al. Increased prevalence of mood disorders and suicidal ideation in type 2 diabetic patients. Acta Diabetol. (2012) 49(Suppl. 1):S227–34. doi: 10.1007/s00592-012-0435-9
72. Han SJ, Kim HJ, Choi YJ, Lee KW, Kim DJ. Increased risk of suicidal ideation in Korean adults with both diabetes and depression. Diabetes Res Clin Pract. (2013) 101:e14–7. doi: 10.1016/j.diabres.2013.06.012
73. Koponen H, Kautiainen H, Leppänen E, Mäntyselkä P, Vanhala M. Association between suicidal behaviour and impaired glucose metabolism in depressive disorders. BMC Psychiatry (2015) 15:163. doi: 10.1186/s12888-015-0567-x
74. Mukamal KJ, Kawachi I, Miller M, Rimm EB. Body mass index and risk of suicide among men. Arch Intern Med. (2007) 167:468–75. doi: 10.1001/archinte.167.5.468
75. Li Y, Zhang J, McKeown RE. Cross-sectional assessment of diet quality in individuals with a lifetime history of attempted suicide. Psychiatry Res. (2009) 165:111–9. doi: 10.1016/j.psychres.2007.09.004
76. Branco JC, Motta J, Wiener C, Oses JP, Pedrotti Moreira F, Spessato B, et al. Association between obesity and suicide in woman, but not in man: a population-based study of young adults. Psychol Health Med. (2017) 2:275–81. doi: 10.1080/13548506.2016.1164870
77. Kim H, Jeon HJ, Bae JN, Cho MJ, Cho SJ, Lee H, et al. Association of body mass index with suicide behaviours, perceived stress, and life dissatisfaction in the Korean general population. Psychiatry Investig. (2018) 15:272–8. doi: 10.30773/pi.2017.06.28
78. Pate RR, Trost SG, Levin S, Dowda M. Sports participation and health-related behaviours among US youth. Arch Pediatr Adolesc Med. (2000) 154:904–11. doi: 10.1001/archpedi.154.9.904
79. Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: The evidence. Can Med Assoc, J. (2006) 174:801–9. doi: 10.1503/cmaj.051351
80. Babiss LA, Gangwisch JE. Sports participation as a protective factor against depression and suicidal ideation in adolescents as mediated by self-esteem and social support. J Dev Behav Pediatr. (2009) 30:376–84. doi: 10.1097/DBP.0b013e3181b33659
81. Brosnahan J, Steffen LM, Lytle L, Patterson J, Boostrom A. The relation between physical activity and mental health among Hispanic and non-Hispanic white adolescents. Arch Pediatr Adolesc Med. (2004) 158:818–23. doi: 10.1001/archpedi.158.8.818
82. Vancampfort D, Hallgren M, Firth J, Rosenbaum S, Schuch FB, Mugisha J, et al. Physical activity and suicidal ideation: A systematic review and meta-analysis. J Affect Disord. (2018) 225:438–48. doi: 10.1016/j.jad.2017.08.070
83. Adams TB, Moore MT, Dye J. The relationship between physical activity and mental health in a national sample of college females. Women Health (2007) 45:69–85. doi: 10.1300/J013v45n01_05
84. Bassilios B, Judd F, Pattison P, Nicholas A, Moeller-Saxone K. Predictors of exercise in individuals with schizophrenia, A test of the transtheoretical model of behaviour change. Clin Schizophr Relat Psychoses (2015) 8:173–82. doi: 10.3371/CSRP.BAJU.030113
85. Jakobsen AS, Speyer H, Nørgaard HCB, Karlsen M, Hjorthøj C, Krogh J, et al. Dietary patterns and physical activity in people with schizophrenia and increased waist circumference. Schizophr Res. (2018) S0920-9964(18)30168-3. doi: 10.1016/j.schres.2018.03.016
86. Sankaranarayanan A, Mancuso S, Wilding H, Ghuloum S, Castle D. Correction: smoking, suicidality and psychosis: a systematic meta-analysis. PLoS ONE (2015) 10:e0141024. doi: 10.1371/journal.pone.0141024
87. Sankaranarayanan A, Clark V, Baker A, Palazzi K, Lewin TJ, Richmond R, et al. Reducing smoking reducessuicidality among individuals with psychosis: Complementary outcomes from aHealthy Lifestyles intervention study. Psychiatry Res. (2016) 243:407–12. doi: 10.1016/j.psychres.2016.07.006
88. Bhatt M, Perera S, Zielinski L, Eisen RB, Yeung S, El-Sheikh W, et al. Profile of suicide attempts and risk factors among psychiatric patients: a case-control study. PLoS ONE (2018) 13:e0192998. doi: 10.1371/journal.pone.0192998
89. Howard M, Krannitz M. A Reanalysis of Occupation and Suicide: Negative Perceptions of the Workplace Linked to Suicide Attempts. J Psychol. (2017) 151:767–88. doi: 10.1080/00223980.2017.1393378
90. Hsu CY, Chang SS, Yip PSF. Subjective wellbeing, suicide and socioeconomic factors: an ecological analysis in Hong Kong. Epidemiol Psychiatr Sci. (2018) 10:1–19. doi: 10.1017/S2045796018000124
91. Kerr WC, Kaplan MS, Huguet N, Caetano R, Giesbrecht N, McFarland BH. Economic recession, alcohol, and suicide rates: comparative effects of poverty, foreclosure, and job loss. Am J Prev Med. (2017) 52:469–75. doi: 10.1016/j.amepre.2016.09.021
92. Younès N, Rivière M, Plancke L, Leroyer A, Blanchon T, Da Silva MA, et al. Work intensity in men and work-related emotional demands in women are associated with increased suicidality among persons attending primary care. J Affect Disord. (2018) 235:565–73. doi: 10.1016/j.jad.2018.04.075
93. Darvishi N, Farhadi M, Haghtalab T, Poorolaja J. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS ONE (2015) 10:e0126870. doi: 10.1371/journal.pone.0126870
94. Bedford D, O'Farrell A, Howell F. Blood alcohol levels in persons who died from accidents and suicide. Ir Med J. (2006) 99:80–3.
95. Kaplan MS, Huguet N, McFarland BH, Caetano R, Conner KR, Giesbrecht N, et al. Use of alcohol before suicide in the United States. Ann Epidemiol. (2014) 24:588–592.e1-2. doi: 10.1016/j.annepidem.2014.05.008
96. Cherpitel CJ, Borges GL, Wilcox HC. Acute alcohol use and suicidal behaviour: a review of the literature. Alcohol Clin Exp Res. (2004) 28(5 Suppl):18S−28S. doi: 10.1097/01.ALC.0000127411.61634.14
97. Bowden B, John A, Trefan L, Morgan J, Farewell D, Fone D. Risk of suicide following an alcohol-related emergency hospital admission: an electronic cohort study of 2.8 million people. PLoS ONE (2018) 13:e0194772. doi: 10.1371/journal.pone.0194772
98. Breet E, Goldstone D, Bantjes J. Substance use and suicidal ideation and behaviour in low- and middle-income countries: a systematic review. BMC Public Health (2018) 18:549. doi: 10.1186/s12889-018-5425-6
99. Choi NG, DiNitto DM, Sagna AO, Marti CN. Postmortem blood alcohol content among late-middle aged and older suicide decedents: associations with suicide precipitating/risk factors, means, and other drug toxicology. Drug Alcohol Depend. (2018) 187:311–8. doi: 10.1016/j.drugalcdep.2018.02.034
100. Almeida OP, Hankey GJ, Yeap BB, Golledge J, Norman PE, Flicker L. Mortality among people with severe mental disorders who reach old age: a longitudinal study of a community-representative sample of 37892 men. PLoS ONE (2014) 9:e111882. doi: 10.1371/journal.pone.0111882
101. Heisel MJ, Flett GL. Does recognition of meaning in life confer resiliency to suicide ideation among community-residing older adults? A longitudinal investigation. Am J Geriatr Psychiatry (2016) 24:455–66. doi: 10.1016/j.jagp.2015.08.007
102. Szanto K, Galfalvy H, Vanyukov PM, Keilp JG, Dombrovski AY. Pathways to late-life suicidal behaviour: cluster analysis and predictive validation of suicidal behaviour in a sample of older adults with major depression. J Clin Psychiatry (2018) 79:11611. doi: 10.4088/JCP.17m11611
103. Innamorati M, Pompili M, Di Vittorio C, Baratta S, Masotti V, Badaracco A, et al. Suicide in the old elderly: results from one Italian county. Am J Geriatr Psychiatry (2014) 22:1158–67. doi: 10.1016/j.jagp.2013.03.003
104. Lutz J, Fiske A. Functional disability and suicidal behaviour in middle-aged and older adults: a systematic critical review. J Affect Disord. (2018) 227:260–71. doi: 10.1016/j.jad.2017.10.043
105. Fässberg MM, van Orden KA, Duberstein P, Erlangsen A, Lapierre S, Bodner E, et al. A systematic review of social factors and suicidal behaviour in older adulthood. Int J Environ Res Public Health (2012) 9:722–45. doi: 10.3390/ijerph9030722
106. Mogensen H, Moller J, Hultin H, and Mittendorfer-Rutz E. Death of a close relative and the risk of suicide in Sweden-A Large Scale Register-Based Case-Crossover Study. PLoS ONE (2016) 11:e0164274. doi: 10.1371/journal.pone.0164274
107. McLaren S, Gomez R, Gill P, Chesler J. Marital status and suicidal ideation among Australian older adults: the mediating role of sense of belonging. Int Psychogeriatr. (2015) 27:145–54. doi: 10.1017/S1041610214001501
108. van Baarsen B. Theory of social support and self-esteem on adjustment to emotional and social loneliness following a partner's death in later life. J Gerontol B Psychol Sci Soc Sci. (2002) 57:S33–42.
109. Erlangsen A, Nordentoft M., Conwell Y, Waern M, De Leo D, Lindner R, et al. Key considerations for preventing suicide in older adults: consensus opinions of an expert panel. Crisis (2001) 32:106–9. doi: 10.1027/0227-5910/a000053
110. Clark F, Jackson J, Carlson M, Chou CP, Cherry BJ, Jordan-Marsh M, et al. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: results of the Well Elderly 2 Randomised Controlled Trial. J Epidemiol Community Health. (2012) 66:782–90. doi: 10.1136/jech.2009.099754
111. Lapierre S, Erlangsen A, Waern M, De Leo D, Oyama H, Scocco P, et al. A systematic review of elderly suicide prevention programs. Crisis (2011) 32:88–98. doi: 10.1027/0227-5910/a000076
112. Okolie C, Dennis M, Simon Thomas E, John A. A systematic review of interventions to prevent suicidal behaviours and reduce suicidal ideation in older people. Int Psychogeriatr. (2017) 29:1801–24. doi: 10.1017/S1041610217001430
113. Heisel MJ, Duberstein PR, Talbot NL, King DA, Tu XM. Adapting Interpersonal psychotherapy for older adults at risk for suicide: preliminary findings. Prof Psychol Res Pr. (2009) 40:156–64. doi: 10.1037/a0014731
114. Lapierre S, Dub,é M, Bouffard L, Alain M. Addressing suicidal ideations through the realization of meaningful personal goals. Crisis (2007) 28:16–25 doi: 10.1027/0227-5910.28.1.16
115. Brandtstädter J, Rothermund K. Intentional self-development: exploring the interfaces between development, intentionality, and the self. Nebr Symp Motiv. (2002) 48:31–75.
116. Hinrichsen GA, Hernandez NA. Factors associated with recovery from and relapse into major depressive disorder in the elderly. Am J Psychiatry (1993) 150:1820–5. doi: 10.1176/ajp.150.12.1820
117. Chatterton L, Hall PL, Tarrier N. Cognitive therapy for low self-esteem in the treatment of depression in an older adult. Behav and Cogn Psychother. (2007) 35:365–9. doi: 10.1017/S1352465807003608
118. McLaren S, Gomez R, Bailey M, Van Der Horst RK. The association of depression and sense of belonging with suicidal ideation among older adults: applicability of resiliency models. Suicide Life Threat Behav. (2007) 37:89–102. doi: 10.1521/suli.2007.37.1.89
119. Malone KM, Oquendo MA, Haas GL, Ellis SP, Li S, Mann JJ. Protective factors against suicidal acts in major depression: reasons for living. Am J Psychiatry (2000) 157:1084–8. doi: 10.1176/appi.ajp.157.7.1084
120. Snyder CR, Rand KL. The case against false hope. Am Psychol. (2003) 58:820–2; authors' reply 823–4 doi: 10.1037/0003-066X.58.10.820
121. Edwards MJ, Holden RR. Coping, meaning in life, and suicidal manifestations: examining gender differences. J Clin Psychol. (2001) 57:1517–34. doi: 10.1002/jclp.1114
122. Dervic K, Oquendo MA, Grunebaum MF, Ellis S, Burke AK, Mann JJ. Religious affiliation and suicide attempt. Am J Psychiatry (2004) 161:2303–8. doi: 10.1176/appi.ajp.161.12.2303
123. Farioli Vecchioli S, Sacchetti S, Nicolis di Robilant V, Cutuli D. The role of physical exercise and omega-3 fatty acids in depressive illness in the elderly. Curr Neuropharmacol. (2018) 16:308–26. doi: 10.2174/1570159X15666170912113852
124. Wang J, Um P, Dickerman BA, Liu J. Zinc, Magnesium, Selenium and Depression: A Review of the Evidence, Potential Mechanisms and Implications. Nutrients (2018) 10:E584. doi: 10.3390/nu10050584
125. Qian Y, Sun L, Zhou C, Ge D, Zhang L. The association between suicidal ideation and sleep quality in elderly individuals: A cross-sectional study in Shandong, China. Psychiatry Res. (2017) 256:453–7. doi: 10.1016/j.psychres.2017.07.017
126. McCall WV, Benca RM, Rosenquist PB, Riley MA, McCloud L, Newman JC, et al. Hypnotic medications and suicide: risk, mechanisms, mitigation, and the FDA. (2017) Am J Psychiatry. 174:18–25. doi: 10.1176/appi.ajp.2016.16030336
127. Bishop TM, Simons KV, King DA, Pigeon WR. Sleep and suicide in older adults: an opportunity for intervention. Clin Ther. (2016) 38:2332–9. doi: 10.1016/j.clinthera.2016.09.015
128. O'Rourke N, Heisel MJ, Canham SL, Sixsmith. Predictors of suicide ideation among older adults with bipolar disorder. PLoS ONE (2017) 12:e0187632. doi: 10.1371/journal.pone.0187632
129. Shah A. A replication of a possible relationship between elderly suicide rates and smoking using five-year data on suicide rates? A cross-national study J Inj Violence Res. (2010) 2:35–40. doi: 10.5249/jivr.v2i1.44
130. Knox KL, Litts DA, Talcott GW, Feig JC, Caine ED. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the US Air Force: cohort study. BMJ (2003) 327:1376. doi: 10.1136/bmj.327.7428.1376
131. Owens C, Lambert H, Donovan J, Lloyd KR. A qualitative study of help seeking and primary care consultation prior to suicide. Br J Gen Pract (2005) 55:503–9.
132. Moskos MA, Olson L, Halbern SR, Gray D. Utah youth suicide study: barriers to mental health treatment for adolescents. Suicide Life Threat Behav. (2007) 37:179–86. doi: 10.1521/suli.2007.37.2.179
133. Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, et al. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health (2016) 59:S49–S60. doi: 10.1016/j.jadohealth.2016.06.020
134. Motohashi Y, Kaneko Y, Sasaki H. Community-based suicide prevention program in Japan using a health promotion approach. Environ Health Prev Med. (2004) 9:3–8. doi: 10.1265/ehpm.9.3
135. Gallego JA, Rachamallu V, Yuen EY, Fink S, Duque LM, Kane JM. Predictors ofsuicide attempts in 3.322 patients with affective disorders and schizophreniaspectrum disorders. Psychiatry Res. (2015) 228:791–6. doi: 10.1016/j.psychres.2015.05.024
136. Pompili M, Innamorati M, Masotti V, Personnè F, Lester D, Di Vittorio C, et al. Suicide in the elderly: a psychological autopsy study in a North Italy area (1994-2004). Am J Geriatr Psychiatry (2008) 16:727–35. doi: 10.1097/JGP.0b013e318170a6e5
137. Madhusoodanan S, Ibrahim FA, Malik A. Primary prevention in geriatric psychiatry. Ann Clin Psychiatry (2010) 22:249–61.
Keywords: suicide, suicide attempts, suicidal thoughts, lifestyle behavior, lifestyle intervention, suicide prevention
Citation: Berardelli I, Corigliano V, Hawkins M, Comparelli A, Erbuto D and Pompili M (2018) Lifestyle Interventions and Prevention of Suicide. Front. Psychiatry 9:567. doi: 10.3389/fpsyt.2018.00567
Received: 23 July 2018; Accepted: 18 October 2018;
Published: 06 November 2018.
Edited by:
Michael Noll-Hussong, Universitätsklinikum des Saarlandes, GermanyReviewed by:
Giuseppe Carrà, Università degli Studi di Milano Bicocca, ItalyCopyright © 2018 Berardelli, Corigliano, Hawkins, Comparelli, Erbuto and Pompili. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maurizio Pompili, bWF1cml6aW8ucG9tcGlsaUB1bmlyb21hMS5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.