- 1Department of Psychiatry, Faculty of Medicine, University of Alberta, Edmonton, AB, Canada
- 2Addiction and Mental Health, Alberta Health Services, Edmonton, AB, Canada
- 3Department of Public Health, Alberta Health Services, Fort McMurray, AB, Canada
- 4Department of Family Medicine, Faculty of Medicine, University of Alberta, Edmonton, AB, Canada
- 5Department of Psychiatry, Northern Lights Regional Health Centre, Fort McMurray, AB, Canada
The Fort McMurray wildfire was the costliest disaster in Canadian history, with far-reaching impacts. The purpose of this paper is to examine the prevalence and risk factors of elevated generalized anxiety disorder (GAD) symptomatology in residents of Fort McMurray 6 months after the wildfire. Data were collected via random selection procedures from 486 participants. Generalized anxiety disorder symptoms were measured via the GAD-7. The 1-month prevalence rate for GAD symptomatology 6 months after the disaster was 19.8% overall, regression analyses revealed six variables with significant unique contributions to prediction of GAD symptomatology. Significant predictors were: pre-existing anxiety disorder, witnessing of homes being destroyed by the wildfire, living in a different home after the wildfire, receiving limited governmental support or limited family support, and receiving counseling after the wildfire. Participants with these risk factors were between two to nearly seven times more likely to present with GAD symptomatology. In addition, participants who presented with elevated symptomatology were more likely to increase use or problematically use substances post-disaster. This study extends the literature on mental health conditions and risk factors following disasters, specifically in the area of generalized anxiety. Findings and implications are discussed.
Introduction
The 2016 Fort McMurray wildfire was the costliest natural disaster in Canadian history1. The wildfire had far-reaching impacts. It destroyed hundreds of homes and businesses, hundreds of thousands of acres of land, and necessitated the largest evacuation in Alberta's history, relocating thousands of residents of Northern Alberta. The objective of this study was to examine the prevalence of generalized anxiety disorder (GAD) symptoms and associations with sociodemographic, exposure-related, and clinical risk factors in survivors of the fire.
Over 40% of Canadians will be exposed to a major disaster in their lifetime, with the majority reporting significant impact on their ability to function in day-to-day life (1). Although exposure to natural disasters is relatively common, a subset of persons exposed will struggle with clinically significant mental health conditions, such as post-traumatic stress disorder (PTSD), depression, and substance use disorders (2). Research suggests risk factors that may place people experiencing disasters at greater risk of incurring mental health conditions (3). For example, in a survey of veterans who survived Hurricane Katrina in the Gulf Coast of the United States, persons with a pre-existing mental condition, especially PTSD, were nearly 12 times more likely to develop another mental health condition on screening following the disaster (4). However, the relative risk of identified sociodemographic and clinical factors in predicting post-disaster mental health symptomatology such as PTSD symptoms is unclear, with some inconsistencies in results reported which may be related to methodological factors (5).
Most post-disaster research has focused on PTSD and depression, with little research examining prevalence and risk factors associated with the development of post-disaster anxiety symptoms (2). Published research suggests that GAD symptoms are elevated following disasters (6–9). In addition, prevalence rates of GAD tend to remain stable over time rather than showing attenuation, as is often reported in PTSD research (6, 9, 10). Of the existing research, GAD symptoms have been associated with pre-existing mental health conditions as well as exposure to disaster-related variables, such as high typhoon exposure (11, 12). Some variables, such as degree of exposure to the disaster, may confer increased risk for the development of anxiety symptoms, whereas other variables, such as higher income, may exert a protective effect (13). Gene by environment interactions have also been reported, such that specific genetic factors differentially increase the risk of the development of GAD in individuals following disasters (8, 14). Conceptually therefore, genetic, social, environmental, and psychological factors could combine to explain elevated levels of GAD following wildfires. “Feelings of uncertainty” which is a central feature of the disaster experience (15) could be lead to increased anxiety levels post-disasters. Uncertainty around housing, job security, and the stress of dealing with insurance companies as well as concerns related to the long-term damaging physical health effects of the smoke from the wildfires could all culminate in elevated anxiety levels post-disaster. Furthermore, the possibility of recurring wildfires could heighten the uncertainty and increase anxiety levels in the victims. Other studies have suggested increased use of nicotine, alcohol and other substances following natural disasters and that the co-existence of substance use with mental health disorders worsens the outcome for survivors (16–19).
To add to the limited literature related to post-disaster anxiety disorders, our study aims to examine the impact of the 2016 Fort McMurray wildfires on the prevalence of elevated GAD symptoms and examine whether sociodemographic, exposure-related, and clinical factors are associated with elevated symptomatology. Consistent with previous literature regarding mental health conditions following a disaster, we hypothesize that there will be increased prevalence rates of GAD symptomatology in the respondents compared to what they self-report prior to the wildfires. In addition, we hypothesize that sociodemographic, exposure-related, and clinical variables would predict the likely presence of GAD symptoms. Another goal of this study is to investigate the association between likely GAD and substance use. We hypothesize that consistent with the literature on the mental health and substance use effects on victims' post-disasters, we will observe increased substance use in respondents who had likely GAD.
Materials and Methods
Quantitative data were collected using self-administered paper-based questionnaires. Study participants were selected using random selection procedures. Participants completed written informed consent before completing the survey questionnaires. This study was carried out in accordance with the recommendations of the University of Alberta Review and Ethics Board. The protocol was approved by the University of Alberta Review and Ethics Board (Pro00066054). All subjects gave written informed consent in accordance with the Declaration of Helsinki.
A targeted sample size of 1,050 was calculated based on an adult population estimates of 60,000 for Fort McMurrary 6 months after the fire, a 95% confidence interval, and a margin of error of ±3% for estimates of the prevalence rates for GAD. Based on this sample size estimate and an assumption of a dropout rate approximating 30%, random selection procedures were used to distribute survey questionnaires to 1,500 adult residents of Fort McMurray. Data were collected in November 2016. Data collection sites were located at various sites within the community and included: a main recreation center, a post-secondary educational institution, a public library, and from three large religious congregations. In each facility, adult residents were randomly approached and invited to participate in the study. Prospective respondents were offered the opportunity to complete the survey forms at the designated data collection points or to take them home and return completed forms within a week to a data collection point. Overall, 1,500 survey forms were randomly distributed during the data collection period. All adult residents who were approached indicated their acceptance of the invitation to participate by collecting the survey forms although not all of them completed and/or returned the completed forms.
A data collection form was designed and used to collect predictive sociodemographic and clinical information, exposure-related data, and support information from respondents. Selected predictive factors were based on a literature review of the factors which have been previously investigated in relations to the mental health effects (depression, anxiety and PTSD) of wildfires and other natural disasters (16, 17, 20–25). The GAD-7 was used to assess GAD symptomatology (26). According to these authors, sensitivity and specificity of the GAD-7 exceed 0.80 at a cut point of 10 or greater “at which threshold sensitivity is nearly maximized”. The cut-off point we used for probable presence of GAD in this study was 10 on the GAD-7.
Substance use was assessed using the Alcohol Use Disorder Identification Test [AUDIT; (27)], the Drug Use Disorder Identification Test [DUDIT; (28)] and the Fagerstrom Test for Nicotine Dependence (29).
SPSS Version 20 (30) was used to analyze data. Univariate analyses with Chi-squares tests were used to ascertain the relationship between predictor variables and GAD symptomatology. Predictor variables that showed statistically significant relationships (p ≤ 0.05, two-tailed) with GAD on univariate analysis and predictor variables that trended toward significance (0.05 ≤ p ≤ 0.1, two-tailed) were then entered into a logistic regression model. Prior to performing the logistic regression analysis, correlational diagnostics were performed to identify any strong inter-correlations (Spearman's correlation coefficient of 0.7–1.0 or −0.7–−1.0) among predictor variables. Consequently, “sought counseling after the wildfire' which was highly positively correlated with “received counseling after the wildfire,” (Spearman's correlation coefficient of 0.80) was dropped from the regression model. Furthermore, “on no psychotropic medication” was also dropped from the regression model as it was highly negatively correlated with “on antidepressants before the wildfire” (Spearman's correlation coefficient of −0.80). Using this approach, we avoided multicollinearity. All other variables in the model were not as strongly correlated with each other. Odds ratios from the binary logistic regression analysis were calculated to determine the association between the predictor variables and GAD symptoms, controlling for the other variables in the model. Finally, we used Chi-square tests to ascertain the relationship between GAD symptomatology and substance use. In other to determine the unique contribution of GAD symptomatology to substance use in the respondents independent of their history of a mental health diagnosis and usage of psychotropic medication before the wildfire” we used a logistic regression model to examine the impact of GAD on substance use whilst specifically controlling for pre-existing mental health conditions and use of psychotropic medication before the wildfires.
Results
Results will be presented as follows. First, descriptive characteristics of the sample (e.g., sociodemographic, living situation, exposure to disaster, clinical variables) will be presented. Second, the associations between GAD symptoms and the descriptor variables will be discussed. Third, the results of logistic regression examining significant predictors of GAD symptomatology will be presented, as well as the influence of GAD symptomatology on self-reported substance use.
Descriptive Sample Characteristics
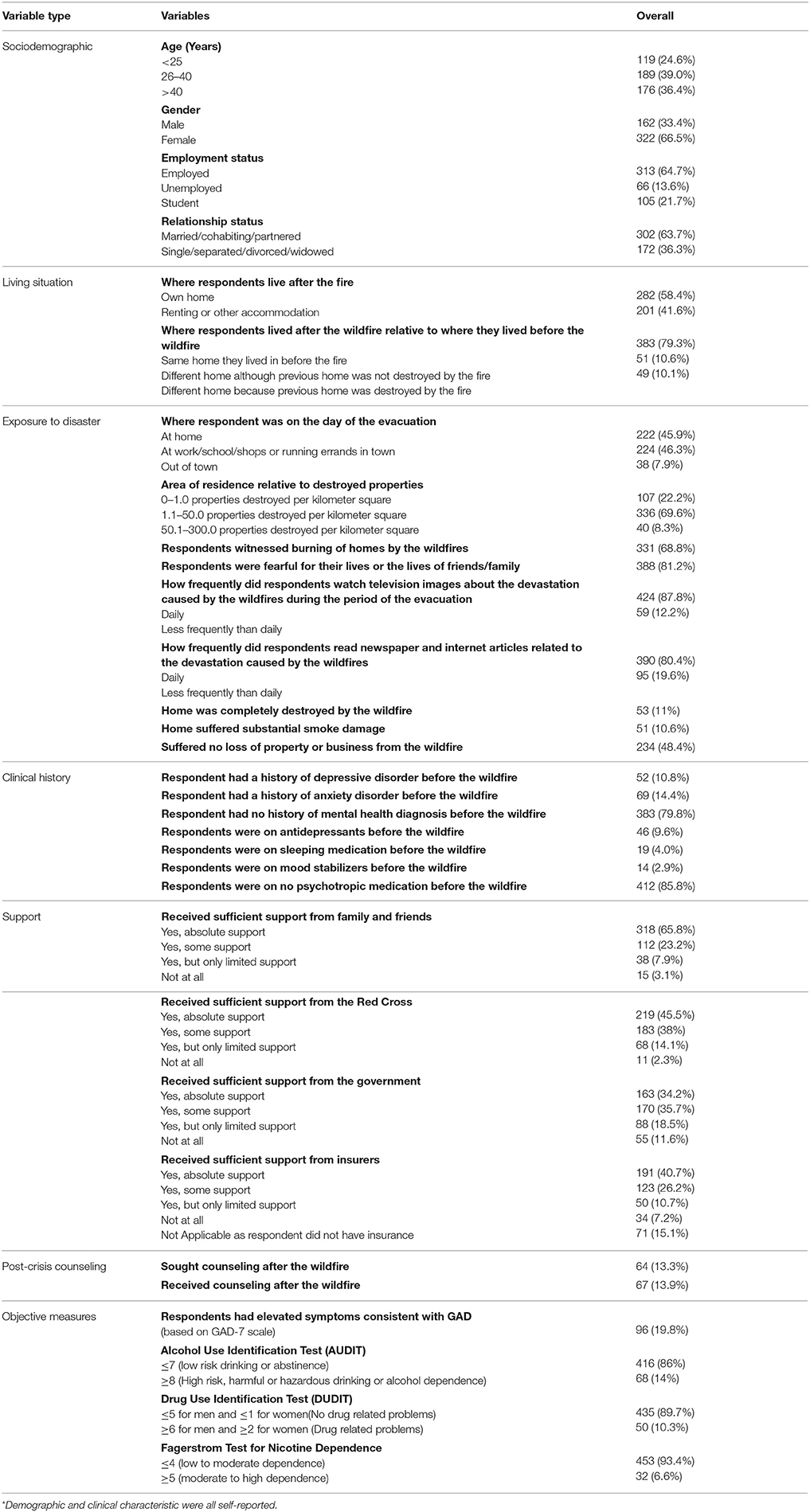
Sample characteristics are as listed in Table 1. The sample was predominantly 26 years of age or older (75%), female (67%), employed or in school (87%), and married, partnered, or cohabiting (64%). Most participants were living in the same home they lived in before the fire (79%). Although many reported no significant loss of property or business due to the wildfire (48%), the majority of participants reported a high degree of exposure to the wildfire. For example, most were in town during the evacuation (92%), witnessed houses burning (69%), and were in close proximity to property destruction (70%). The majority of participants reported daily exposure to media coverage of the wildfire and its effects (i.e., 80, 88%) and 81% feared for their lives or their family members' lives.
In terms of clinical history, most participants reported absence of a mental health condition prior to the wildfires (80%), with few on psychotropic medication prior to the wildfire (86%). On objective measures, one-fifth of the sample had elevated GAD symptoms (GAD-7, 20%), and a minority reported high levels of substance use (7–14%). A minority sought counseling after the fire (13%), with nearly all of those who sought counseling receiving it. Most participants reported receiving some or absolute support from a variety of sources, including family and friends (89%), the Red Cross (84%), the government (70%), and insurance companies (67%).
Associations Between Sociodemographic, Clinical, Exposure-Related, and Support Variables and Elevated GAD Symptoms
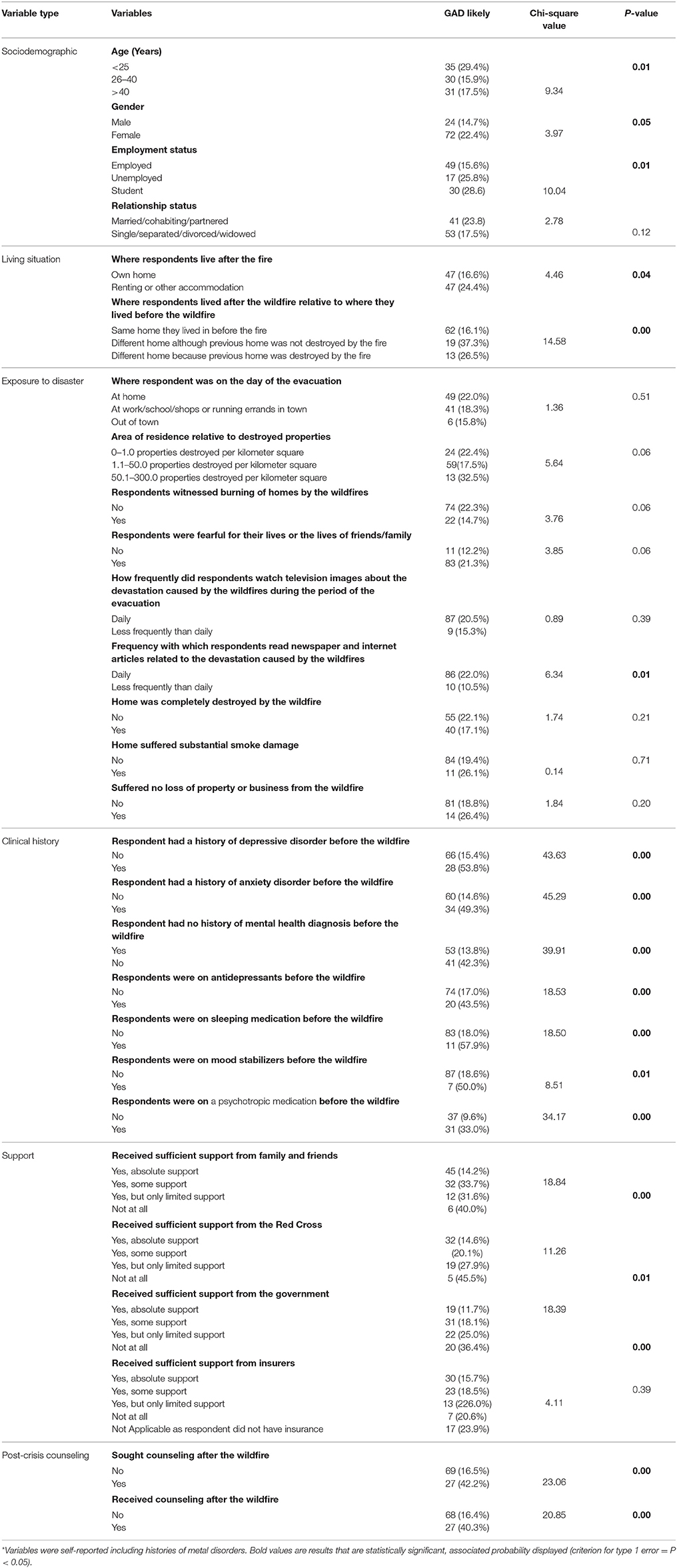
Chi-square analyses (see Table 2) suggested that persons with elevated GAD symptomatology were more likely to be young, female, staying in rental or other accommodation, and living in a home after the wildfire that was different than the home they were living in prior to the wildfire. Participants with elevated GAD symptoms were more likely to read wildfire-related media. In terms of clinical variables, participants with elevated GAD symptoms were more likely to have a history of a mental health condition or have been taking psychotropic medications prior to the wildfire. They were more likely to seek counseling, and less likely to report receiving adequate support, both informal and formal.
Predictors of Elevated GAD Symptoms
The results of the Chi-square analysis were used to inform the selection of variables to be included as potential predictors in a logistic regression analysis. Specifically, nineteen of the variables identified via Chi-square analysis (see Table 2) with significant p-values (p ≤ 0.5) or p-values that were trending or approaching significance (p-values of 0.05–0.1), were entered into a logistic regression model. Note that the variable “sought counseling after the wildfire” was not included in the model, because it was highly correlated with the variable “received counseling after the wildfire” (Spearman correlation = 0.80). Given the high level of conceptual and statistical similarity, this variable was considered redundant and was eliminated.
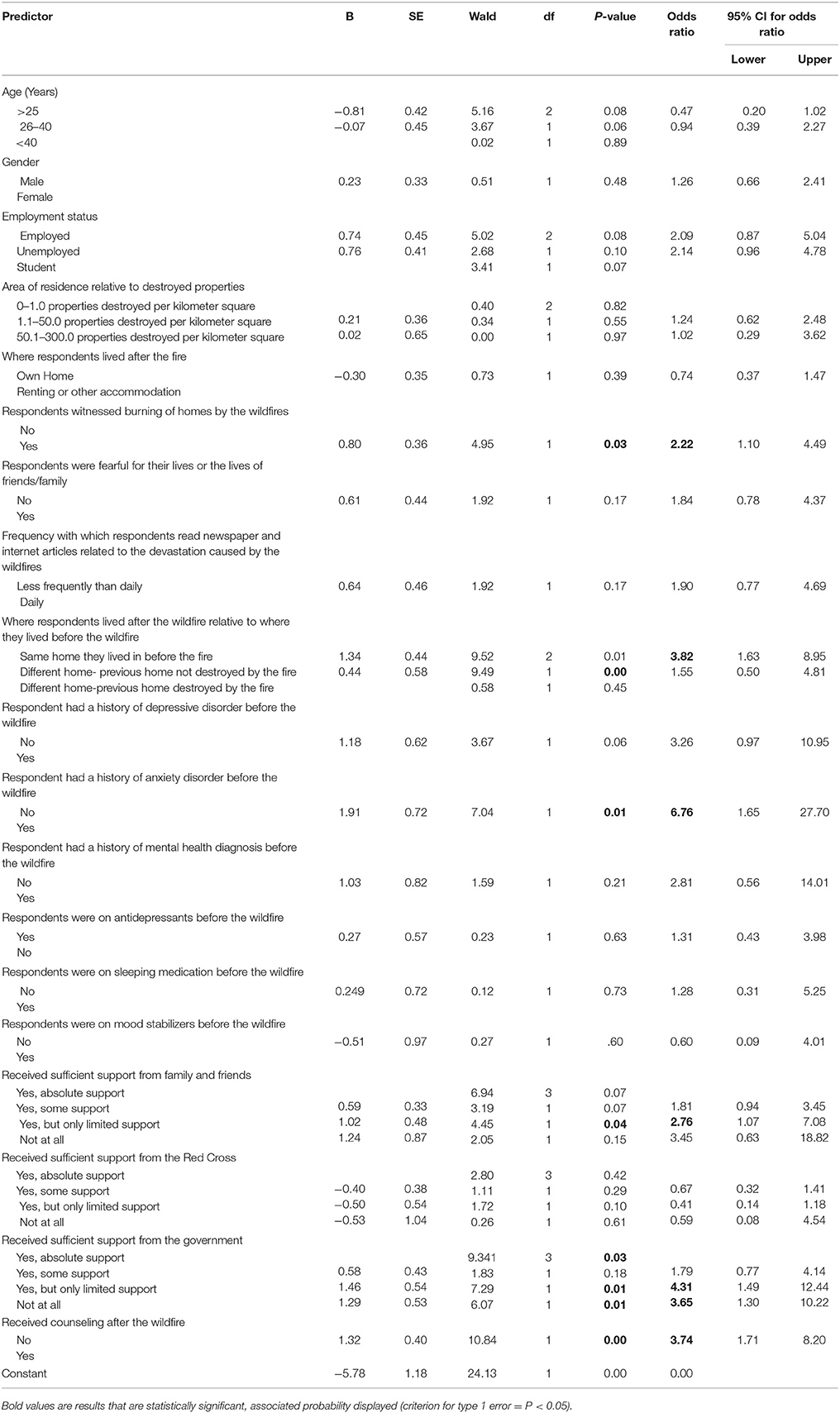
See Table 3 for regression results. The full model including all nineteen predictors was statistically significant, χ2 (29, N = 486) = 106.05, p < 0.00, which suggested that the model was able to distinguish between participants with elevated GAD symptoms vs. those who did not report elevated symptoms. The model as a whole explained ~21–33% (Cox and Snell R2, Nagelkerke R2, respectively) of the variance in GAD-7 symptomatology and correctly classified 84% of cases.
However, only six of 19 predictors made unique contributions (i.e., witnessing of homes burning, place of residence after the wildfire, pre-existing anxiety disorder, perceived support from the government or family/friends, post-crisis counseling). Odds ratios varied from 2.22 (witness of homes burning) to 6.76 (pre-existing anxiety disorder). Participants who witnessed homes burning were approximately twice as likely to have elevated GAD symptoms on self-report, whereas persons who were relocated were nearly four times as likely to present with GAD symptoms. Perceived lower levels of support was also a predictor of GAD symptoms, specifically that persons receiving limited informal support (family and friends) were nearly three times as likely to report elevated GAD symptoms and those receiving limited governmental support were approximately four times more likely to report elevated anxiety symptoms. Participants who received post-crisis counseling were four times more likely to report elevated anxiety symptoms. Participants with a pre-existing anxiety disorder were nearly seven times more likely to report elevated GAD symptoms post-wildfire.
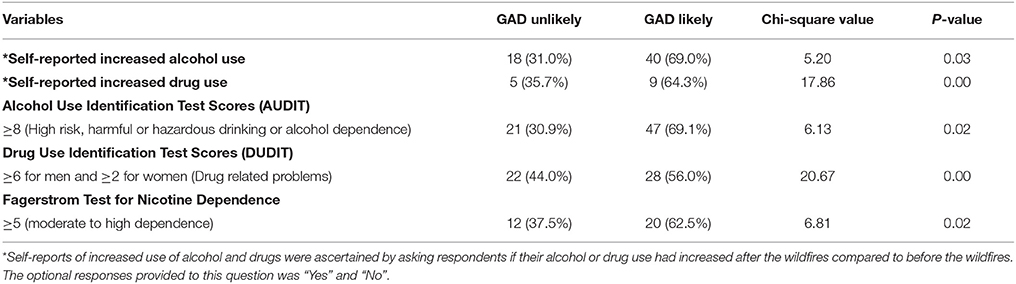
Not only was a pre-existing anxiety disorder a risk factor for elevated GAD symptoms, but participants with elevated anxiety symptoms post-wildfire were also significantly more likely to report increased or problematic levels of substance use (i.e., alcohol, drug, and nicotine, see Table 4).
Table 4 suggests there was statistically significant elevation in the levels of alcohol, nicotine and substance use as measured by self-reports and standardized rating scales in respondents who had likely GAD compared to respondents who did not have GAD.
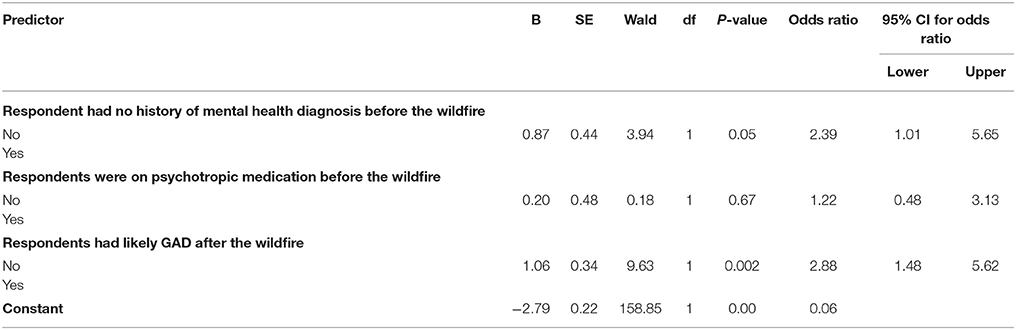
In order to determine the unique contribution of likely GAD to substance use in the population 6 months after the wildfire independent of a prior mental health diagnosis or use of psychotropic medication before the wildfire, we entered the three factors into a logistic regression model. The full model including all three predictors was statistically significant, χ2 (3, N = 486) = 25.35, p < 0.00, which suggested that the model was able to distinguish between participants with drug related problems vs. those who did not have drug related problems. The model as a whole explained only 5.2–10.8% (Cox and Snell R2, Nagelkerke R2, respectively) of the variance in drug related problems and correctly classified 89.9% of cases.
Table 5 suggests that likely GAD made a unique statistically significant contribution to the model. With an odds ratio of 2.88, respondents who had likely GAD were about three times more likely to present with a drug related problem compared to respondents who did not have a likely GAD when controlling for a mental health diagnosis and use of psychotropic medication before the wildfire.
Separate logistic regressions models however showed that likely GAD did not make unique statistical contributions to either hazardous drinking/alcohol dependence or moderate to high nicotine dependence when controlling for the presence of a mental health diagnosis and use of psychotropic medication before the wildfire.
Discussion
This paper examined the prevalence and risk factors for GAD symptoms following the costliest natural disaster in Canadian history (Fort McMurray wildfire). Overall, the prevalence of generalized anxiety symptoms was high, with approximately one fifth of the sample reporting elevated symptomatology on self-report. This is approximately eight times higher than the rates of GAD in general Canadian population which was 2.5% in 2012 (31). Although the specific prevalence rate for GAD in our study population is unknown, it would be reasonable to assume it would not be much different from that of the general Canadian population. Furthermore, only about 14% of our study population self-reported a life time history of an anxiety disorder and only 9.6% were on an antidepressant. The prevalence rates for GAD symptomatology noted in our study are therefore significant, considering that the participants in the study were generally relatively high-functioning, with a minority endorsing pre-existing mental health conditions and the majority receiving support, with few relocations and direct property loss reported.
Clear risk factors emerged for elevated GAD symptomatology. Persons with elevated symptoms were more likely to be young, female, staying in rental or other accommodation, relocated to a different home, be exposed to media coverage relating to the wildfire, have pre-existing mental health conditions, and be receiving inadequate support.
Of the variables examined, the most salient predictors of elevated GAD symptomatology including witnessing of homes burning, relocation after the wildfire, a pre-existing anxiety disorder, level of perceived support from the government or family/friends, and whether post-crisis counseling was received. The presence of these variables was associated with an increased risk of GAD symptomatology, ranging from a two-fold (witness of homes burning) to a nearly seven-fold (pre-existing anxiety disorder) increased likelihood of elevated GAD symptoms. Increased social support has been reported in previous studies to protect against the mental health effects of post-natural disasters. In a longitudinal evaluation in a rural community sample in northern China after an earthquake, the group that received more support showed a general improvement in post-disaster well-being from 3 to 9 months(21). Similarly, another study reported that lower social support was associated with higher post-disaster psychological distress (32). Furthermore, the literature suggest that communal coping is protective against the mental health effects of the trauma associated with wildfires (15). The findings reported in these studies are consistent with our study results which suggest that increased support from Government, family and friends for victims could be protective against GAD after wildfires.
Our study data are also consistent with studies of mental health following other disasters, which have reported grossly increased prevalence rates as well as predictors of symptomatology that relate to pre-existing mental health conditions and exposure-related variables (32–35).
Our study suggested that elevated GAD symptoms were associated with increased or problematic substance use.
This paper extends the literature by demonstrating associations between GAD symptoms and these variables. GAD symptoms are often not the subject of examination post-disaster, yet they are highly prevalent and associated with relatively more persistence over time and far-reaching effects than other conditions.
The results of this paper suggest that post-disaster, it is important to screen residents for not only post-traumatic stress disorder and depression, but also (GAD). Results also suggest that healthcare systems, public health decision-makers, and governments should work to implement supportive measures post-disaster to mitigate mental health symptomatology.
Limitations are often unavoidable when working within the constraints of post-disaster conditions. There are therefore limitations of the study that merit mention. First, random sampling methods were used, thus the method of data collection was not systematic at a population level. Second, the sample of respondents was not fully representative of the community (e.g., over 66% of our respondents were female even though they comprise < 45% of the Fort McMurray population and we were unable to collect data from all categories of Fort McMurray inhabitants such as the workers in remote camps). Third, likely GAD was identified via screening measure self-report as opposed to a formal diagnostic interview. It is therefore possible that some respondents had anxiety associated with other mental health effects of wild fires including PTSD and Major Depressive Disorder rather than a GAD, Fourth, although we aimed for a sample of 1050 participants we were able to collect data from 488. This increased the margin of error of estimates (i.e., ±4.5% at 95% confidence intervals rather than the estimated ±3% margin of error). Notwithstanding these limitations, our study being one of the few studies to examine the mental health effects of the costliest natural disaster in Canadian history adds to the literature by documenting potential predictive factors for GAD symptomatology after wildfires. Knowledge of these factors would be helpful for policy makers when formulating social and clinical programs to mitigate the mental health effects of natural disasters.
Conclusions
The results of the study suggest prevalence of (GAD) symptoms are grossly elevated following a natural disaster. There are risk factors that increase risk of elevated symptomatology. Specifically, a pre-existing anxiety disorder, witnessing the burning of homes during a wildfire, exposure to wildfire media coverage, relocation, and a perceived lack of governmental support or support from family/friends provide unique contributions to the prediction of elevated anxiety disorders following a wildfire. Substance use is also higher in persons with (GAD) symptoms. Policy implications include screening for generalized anxiety following disasters as well as provision of support to help mitigate the prevalence and impacts of post-disaster anxiety.
Datasets are Available on Request
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Author Contributions
VA conceived and designed the study, supervised data collection, analyzed the data and jointly drafted the initial manuscript with MH. MH contributed to the study design and analysis and jointly drafted the initial manuscript with VA. MJ participated in analyzing the data, reviewing and editing the initial draft of the manuscript. JO, ED, BN, IA, SM, and SC participated in data collection, reviewing and editing the initial draft of the manuscript. MB, PC, AG, and X-ML contributed to data interpretation and editing the initial draft of the manuscript. All authors approved of the final draft of the manuscript before submission.
Funding
The study was funded by the Department of Psychiatry, Faculty of Medicine, University of Alberta. MJ was supported by graduate scholarships from the Killam Trust and from Alberta Innovates Health Solutions.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Mr. Ike Omege for his assistance with data collection.
Footnotes
1. ^Fort McMurray wildfire: 3.6B in damage, says Insurance Bureau of Canada | Globalnews.ca., (n.d.). Available online at: https://globalnews.ca/news/2808805/fort-mcmurray-wildfire-cost-of-damage-from-alberta-disaster-to-be-released/ (Accessed March 5, 2018).
References
1. Ibrahim D. Canadians' experiences with emergencies and disasters, 2014. Juristat Canad Centre Justice Stat. (2016) 1. Available online at: https://www150.statcan.gc.ca/n1/pub/85-002-x/2016001/article/14469-eng.htm (Accessed November 22, 2017).
2. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health (2014) 35:169–83. doi: 10.1146/annurev-publhealth-032013-182435
3. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981-200(2016) 1 Psychiatry (2002) 65:207–39. doi: 10.1521/psyc.65.3.207.20173
4. Sullivan G, Vasterling JJ, Han X, Tharp AT, Davis T, Deitch EA, et al. Preexisting mental illness and risk for developing a new disorder after hurricane katrina. J Nerv Mental Dis. (2013) 201:161–6. doi: 10.1097/NMD.0b013e31827f636d
5. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull (2003) 129:52–73. doi: 10.1037/0033-2909.129.1.52
6. Acierno R, Ruggiero KJ, Galea S, Resnick HS, Koenen K, Roitzsch J, et al. Psychological sequelae resulting from the 2004 Florida hurricanes: implications for postdisaster intervention. Am J Public Health (2007) 97(Suppl. 1):S103–8. doi: 10.2105/AJPH.2006.087007
7. Ghafoori B, Neria Y, Gameroff MJ, Olfson M, Lantigua R, Shea S, et al. Screening for generalized anxiety disorder symptoms in the wake of terrorist attacks: a study in primary care. J Trauma Stress (2009) 22:218–26. doi: 10.1002/jts.20419
8. Koenen KC, Amstadter AB, Ruggiero KJ, Acierno R, Galea S, Kilpatrick DG, et al. RGS2 and generalized anxiety disorder in an epidemiologic sample of hurricane-exposed adults. Depression Anxiety (2009) 26:309–15. doi: 10.1002/da.20528
9. Varner S, Langhinrichsen-Rohling J, Bell TR. Persisting generalized anxiety disorder and physical health symptoms 18 months after the deepwater horizon oil spill: a community sample: anxiety and physical symptoms in a community sample post oil spill. J Commun Psychol. (2016) 44:1011–26. doi: 10.1002/jcop.21824
10. Pietrzak RH, Tracy M, Galea S, Kilpatrick DG, Ruggiero KJ, Hamblen JL, et al. Resilience in the face of disaster: prevalence and longitudinal course of mental disorders following hurricane Ike. PLoS ONE (2012) 7:e38964. doi: 10.1371/journal.pone.0038964
11. Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, et al. Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. J Trauma Stress (2009) 22:180–8. doi: 10.1002/jts.20404
12. Berenz EC, Trapp SK, Acierno R, Richardson L, Kilpatrick DG, Tran TL, et al. Pretyphoon panic attack history moderates the relationship between degree of typhoon exposure and posttyphoon PTSD and depression in a Vietnamese sample: research article: panic, PTSD, and depression. Depress Anxiety (2013) 30:461–8. doi: 10.1002/da.22096
13. Dorahy MJ, Rowlands A, Renouf C, Hanna D, Britt E, Carter JD. Impact of average household income and damage exposure on post-earthquake distress and functioning: a community study following the February 2011 Christchurch earthquake. Br J Psychol. (2015) 106:526–43. doi: 10.1111/bjop.12097
14. Amstadter AB, Koenen KC, Ruggiero KJ, Acierno R, Galea S, Kilpatrick DG, et al. NPY moderates the relation between hurricane exposure and generalized anxiety disorder in an epidemiologic sample of hurricane-exposed adults. Depress Anx. (2010) 27:270–5. doi: 10.1002/da.20648
15. Afifi WA, Felix ED, Afifi TD. The impact of uncertainty and communal coping on mental health following natural disasters. Anx Stress Coping (2012) 25:329–47. doi: 10.1080/10615806.2011.603048
16. Chou FH, Wu HC, Chou P, Su CY, Tsai KY, Chao SS, et al. Epidemiologic psychiatric studies on post-disaster impact among Chi-Chi earthquake survivors in Yu-Chi, Taiwan. Psychiatry Clin Neurosci. (2007) 61:370–8. doi: 10.1111/j.1440-1819.2007.01688.x
17. Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry (2014) 71:1025–31. doi: 10.1001/jamapsychiatry.2014.652
18. Bianchini V, Roncone R, Giusti L, Casacchia M, Cifone MG, Pollice R. PTSD growth and substance abuse among a college student community: coping strategies after 2009 L'aquila earthquake. Clin Pract Epidemiol Ment Health (2015) 11:140–3. doi: 10.2174/1745017901511010140
19. Maremmani AGI, Maiello M, Carbone MG, Pallucchini A, Brizzi F, Belcari I, et al. Towards a psychopathology specific to substance use disorder: should emotional responses to life events be included? Compr Psychiatry (2018) 80:132–9. doi: 10.1016/j.comppsych.2017.10.001
20. Jones RT, Ribbe DP, Cunningham P. Psychosocial correlates of fire disaster among children and adolescents. J Trauma Stress (1994) 7:117–22. doi: 10.1002/jts.2490070112
21. Wang X, Gao L, Zhang H, Zhao C, Shen Y, Shinfuku N. Post-earthquake quality of life and psychological well-being: longitudinal evaluation in a rural community sample in northern China. Psychiatry Clin Neurosci. (2000) 54:427–33. doi: 10.1046/j.1440-1819.2000.00732.x
22. Marshall GN, Schell TL, Elliott MN, Rayburn NR, Jaycox LH. Psychiatric disorders among adults seeking emergency disaster assistance after a wildland-urban interface fire. Psychiatr Serv. (2007) 58:509–14. doi: 10.1176/ps.2007.58.4.509
23. Papanikolaou V, Adamis D, Mellon RC, Prodromitis G. Psychological distress following wildfires disaster in a rural part of Greece: a case-control population-based study. Int J Emerg Ment Health (2011) 13:11–26.
24. Papanikolaou V, Leon GR, Kyriopoulos J, Levett J, Pallis E. Surveying the ashes: experience from the 2007 Peloponnese wildfires six months after the disaster. Prehosp Disaster Med. (2011) 26:79–89. doi: 10.1017/S1049023X11000094
25. Papadatou D, Giannopoulou I, Bitsakou P, Bellali T, Talias MA, Tselepi K. Adolescents' reactions after a wildfire disaster in Greece. J Trauma Stress (2012) 25:57–63. doi: 10.1002/jts.21656
26. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
27. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Identification Test - Guidelines for Use in Primary Care. Geneva: World Health Organization (2001). Available online at: http://apps.who.int/iris/bitstream/handle/10665/67205/WHO_MSD_?sequence=1 (Accessed November 22, 2017).
28. Berman AH, Bergman H, Palmstierna T, Schlyter F. DUDIT (Drug Use Disorders Identification Test) Manual. Stockholm: Karolinska Institute (2003).
29. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The fagerström test for nicotine dependence: a revision of the fagerström tolerance questionnaire. Br J Addict. (1991) 86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x
30. IBM. How to cite IBM SPSS Statistics or earlier versions of SPSS - United States. (2011). Available online at: from http://www-01.ibm.com/support/docview.wss?uid=swg21476197 (Accessed November 22, 2017)
31. Pelletier L, O'Donnell S, McRae L, Grenier J. The burden of generalized anxiety disorder in Canada. Health Promot Chronic Dis Prev Can. (2017) 37:54–62. doi: 10.24095/hpcdp.37.2.04
32. Carr VJ, Lewin TJ, Webster RA, Hazell PL, Kenardy JA, Carter GL. Psychosocial sequelae of the 1989 Newcastle earthquake: I. community disaster experiences and psychological morbidity 6 months post-disaster. Psychol Med. (1995) 25:539–55. doi: 10.1017/S0033291700033468
33. Carr VJ, Lewin TJ, Kenardy JA, Webster RA, Hazell PL, Carter GL, et al. Psychosocial sequelae of the 1989 Newcastle earthquake: III. role of vulnerability factors in post-disaster morbidity. Psychol Med. (1997) 27:179–90. doi: 10.1017/S003329179600428X
34. Carr VJ, Lewin TJ, Webster RA, Kenardy JA, Hazell PL, Carter GL. Psychosocial sequelae of the 1989 Newcastle earthquake: II. exposure and morbidity profiles during the first 2 years post-disaster. Psychol Med. (1997) 27:167–78. doi: 10.1017/S0033291796004278
Keywords: wildfire, major depressive disorder, mental health, anxiety disorder, support, counseling
Citation: Agyapong VIO, Hrabok M, Juhas M, Omeje J, Denga E, Nwaka B, Akinjise I, Corbett SE, Moosavi S, Brown M, Chue P, Greenshaw AJ and Li X-M (2018) Prevalence Rates and Predictors of Generalized Anxiety Disorder Symptoms in Residents of Fort McMurray Six Months After a Wildfire. Front. Psychiatry 9:345. doi: 10.3389/fpsyt.2018.00345
Received: 01 May 2018; Accepted: 09 July 2018;
Published: 31 July 2018.
Edited by:
Gianluca Serafini, Ospedale San Martino (IRCCS), ItalyReviewed by:
Sebastian Trautmann, Technische Universität Dresden, GermanySerafim Carvalho, Cooperativa de Ensino Superior Politécnico e Universitário, Portugal
Copyright © 2018 Agyapong, Hrabok, Juhas, Omeje, Denga, Nwaka, Akinjise, Corbett, Moosavi, Brown, Chue, Greenshaw and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vincent I. O. Agyapong, YWd5YXBvbmdAdWFsYmVydGEuY2E=
 Vincent I. O. Agyapong
Vincent I. O. Agyapong Marianne Hrabok1,2
Marianne Hrabok1,2 Michal Juhas
Michal Juhas Sandra E. Corbett
Sandra E. Corbett Matthew Brown
Matthew Brown Andrew J. Greenshaw
Andrew J. Greenshaw Xin-Min Li
Xin-Min Li