- 1Department of Psychiatry and Psychotherapy, Medical University of Vienna, Vienna, Austria
- 2Justizanstalt Göllersdorf, Göllersdorf, Austria
- 3Institut für Suchtdiagnostik Wien, Vienna, Austria
Objective: The impact of substance abuse on violent behavior in patients suffering from schizophrenia is well-known. However, the association between the pattern of substance abuse and certain aspects of criminal behavior like the severity of offense, the previous history of violence and the age at onset of the criminal career is still unclear.
Method: To assess the relationship between substance abuse, schizophrenia and violent behavior we examined healthy non-offenders; healthy offenders; non-offenders suffering from schizophrenia; and offenders suffering from schizophrenia, with respect to different patterns of substance abuse (none, alcohol only, illicit drugs only, and multiple substances).
Results: Healthy offenders as well as offenders and non-offenders suffering from schizophrenia are characterized by increased rates of alcohol and illicit drug abuse. Especially multiple substance abuse appears to lower the threshold of aggression and illegal behavior. This effect is more pronounced in subjects suffering from schizophrenia. In both offender groups the abuse of psychoactive substances is associated with an earlier onset of the criminal career, but has no impact on the severity of the offenses.
Conclusion: Our results point to the need for a differentiated view on the contribution of substance abuse to the criminality of subjects suffering from schizophrenia.
Introduction
During the last 20 years various studies have confirmed a moderate though statistically significant association between schizophrenia and violence (1–9). Most of these studies point in particular to the complex role of co-morbid substance abuse for the development of violent behavior (10–26).
However, the aforementioned association remains unclear for several reasons:
1) Compared with the general population, subjects suffering from schizophrenia exhibit significantly higher rates for substance abuse. This primarily concerns alcohol and cannabis, while opiates and hallucinogens are of minor importance (27–40). Subjects with schizophrenia and co-morbid substance abuse tend to have an earlier onset of schizophrenia than do those without co-morbidity. However, research does not support a link between specific symptoms of schizophrenia and choice of abused drugs (29).
2) Independent of a subject's mental health status, substance abuse is by itself a major criminogenic factor (41–47). A meta-analysis of 30 experimental studies confirms the common knowledge about the influence of alcohol on aggressive behavior (41).
3) Since 1996 the World Health Organization (WHO) has compiled the Global Alcohol Database to provide a standardized reference source of information for a global epidemiological survey of alcohol use and its related problems (48). Since 1999 the United Nations Office on Drugs and Crime (49) publishes the annual World Drug Report. These international health statistics clearly manifest different national prevalence rates for alcohol- and drug abuse. Additionally, interdependencies do exist between several problematic behavioral patterns such as alcohol and drug abuse, violent, and criminal behavior. The weight of these single components varies significantly in different cultures (50). Therefore, the transferability of results from American studies on the association of schizophrenia, substance abuse, and offending behavior to the European situation is limited.
Our study addresses the following questions:
a) Are there differences concerning the prevalence rates and patterns of substance abuse between offenders suffering from schizophrenia and non-offenders suffering from schizophrenia?
b) Are there differences concerning the prevalence rates and patterns of substance abuse between offenders with schizophrenia and healthy offenders?
c) Do the rates of substance abuse in these three groups differ from the rates in healthy controls?
d) Is there an association between substance abuse and patterns of criminal behavior independent of the mental status of the offenders?
Materials and Methods
Sample
In order to assess the impact of the patterns of substances abuse on criminal behavior of male patients with schizophrenia, we used a case-control-study-design with four groups.
One hundred and three male offenders suffering from schizophrenia (OS) according to DSM-IV (51), admitted to the Justizanstalt Göllersdorf, Austria's central institution for the treatment of male mentally ill offenders not guilty by reason of insanity (NGRI).
One hundred and three healthy male offenders (OH), matched for age and severity of offense with the offenders suffering from schizophrenia.
One hundred and three male non-offenders suffering from schizophrenia according to DSM-IV (NoS) matched for age and duration of illness with the offenders NGRI.
One hundred and three male non-offenders without major mental disorders or personality disorders (NoH), matched for age with the other groups. The social stratification and the town/rural distribution of this group are representative for the overall population of Eastern Austria (52).
The protocol of the study was approved by the ethic commission of the Medical University Vienna. All patients gave written informed consent in accordance with the Declaration of Helsinki.
Instruments
All subjects underwent the Structured Clinical Interview for DSM Disorders (SCID 1 + 2). The Inter-rater reliability tested for 25 patients was very satisfying (Cohens' alpha = 0.98). We distinguished three types of harmful substance abuse:
1) Alcohol
2) Illicit Drugs
3) Multiple substances (abuse of alcohol, benzodiazepines or illicit drugs)
The assignment to social classes was done according to Kleining and Moore (53). The pattern of criminal behavior was defined by three factors: (1) severity of the offense according to the categorical classification of Taylor (54): “minimal” (verbally aggressive; carrying a weapon which was not used; minimal accidental damage of property), “moderate” (actual bodily harm; using an offensive weapon but without causing injury; damage to property when it was the main intent), “moderately serious” (grievous bodily harm; damage to property when this was extensive and could have threatened life), and “serious” violence (life actually endangered and victim detained in hospital more than 24 h; victim died). (2) number of previous convictions, (3) age at first conviction.
Statistics
The frequency of substance abuse was analyzed by means of Chi-Square Tests, associations between the patterns of violent behavior (severity of offense, number of previous convictions, age at onset of the criminal career) and the different types of substance abuse (none, alcohol only, illicit drugs only, multiple substance abuse) by means of One-Way ANOVA (df = 3).
Results
The social and clinical data of the four groups are listed in Table 1. Compared to the reference group (NoH), both offender groups grew up in low social milieus. As to be expected, patients suffering from schizophrenia mostly were singles at the time of the interview (NoS) or at the time of the offense (OS). Only 4.9% of the healthy reported a life-time history of total substance abuse. In contrast both offender groups (OH, OS) showed very high rates of (comorbid) substance abuse (OH: 70%, OS: 71.8%). However, high rates were also found in the non-offending patients suffering from schizophrenia (NoS: 55.3%).
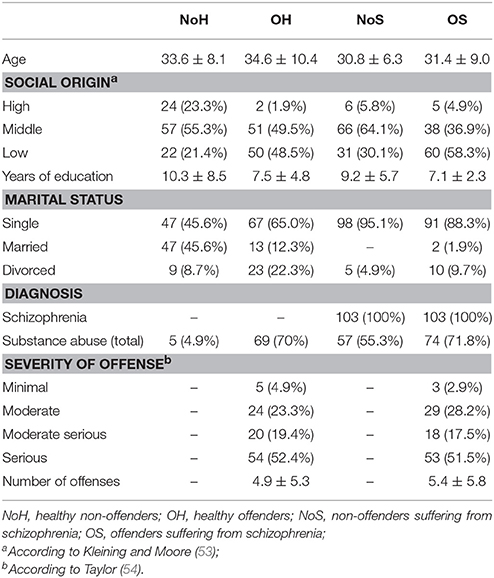
Table 1. Social, clinical, and offense-related data of healthy non-offenders (n = 103), healthy offenders (n = 103), non-offenders suffering from schizophrenia (N = 103), and offenders suffering from schizophrenia (n = 103).
Table 2 shows the patterns of abused substances in the four groups. Only 5 subjects of the NoH group reported periods of alcohol abuse, no single subject used illicit drugs beyond the experimental stage. In contrast, the other three groups showed statistically significantly higher rates for nearly all kinds of substance abuse. Especially the high rates of multiple substance abuse in both offending groups were striking. Interestingly, the highest prevalence of only illicit drug abuse was found in the NoS group. While the illicit drug abuse in both groups of patients suffering from schizophrenia was limited to cannabis abuse, 7.8% of the healthy offenders also reported a history of cocaine abuse and 4.8% reported opiate addiction.
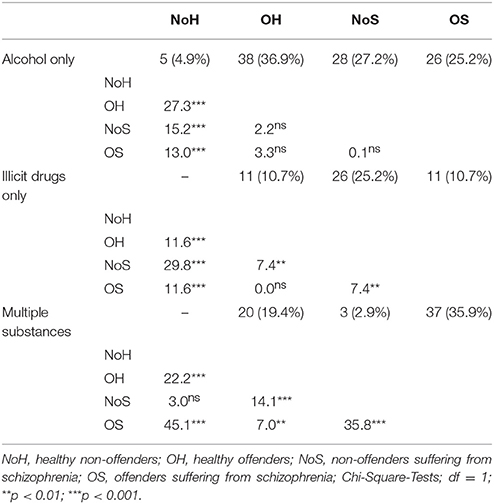
Table 2. Patterns of lifetime substance abuse in healthy non-offenders (n = 103), healthy offenders (n = 103), non-offenders suffering from schizophrenia (N = 103), and offenders suffering from schizophrenia (n = 103).
Finally we compared the relationship between the different types of substance abuse and the patterns of criminal behavior of the two offender groups, which showed substantial similarities (Table 3). By means of One-way ANOVA we found no association between the pattern of substance abuse and the severity of the index-offense. In both offender groups subjects without any substance abuse showed the lowest number of previous convictions. In the OH group all kinds of substance abuse were associated with higher rates of previous convictions, in the OS group alcohol and multiple substance abuse—but not illicit drug abuse alone—was associated with higher rates of previous convictions. The association between psychoactive substance use and the age at first conviction was obvious in both groups. Illicit drug abuse alone or in combination with alcohol was related to earlier onset of criminal behavior.
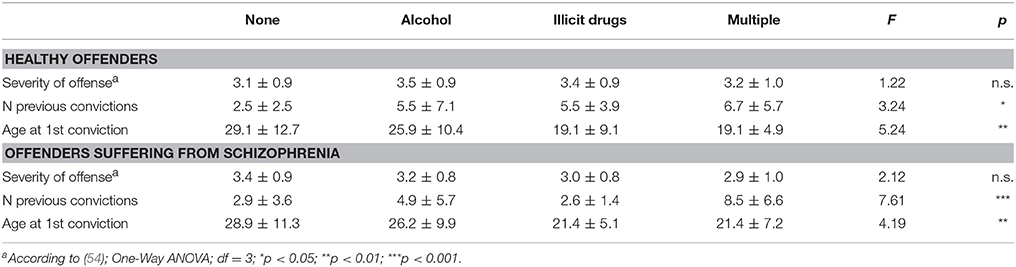
Table 3. Criminal behavior and substance abuse of healthy offenders (n = 103) and offenders suffering from schizophrenia (n = 103).
Discussion
Comparison of the four groups shows that a statistically significantly higher prevalence of substance abuse is associated with both psychiatric illness and offending behavior (Table 2). Only 4.9% of the healthy controls reported a history of alcohol abuse, which is lower than the prevalence rates reported in studies by WHO (48) and UNODC (49). This may be due to the fact that one of the inclusion criteria for the control group was the absence of a DSM-IV Axis I disorder and, especially, of any personality disorder.
Non-offending patients with schizophrenia differ from the other groups by a relatively high prevalence of illicit drug abuse (25.2%) which is nearly exclusively confined to cannabis. This is in line with previous findings of studies on the use of cannabis in schizophrenic patients (40, 55, 56). During the last 20 years three main hypotheses were put forward to explain the increased cannabis use of patients with schizophrenia: (a) cannabis abuse triggers the outbreak of schizophrenia (57), (b) cannabis abuse follows the outbreak of schizophrenia (patients claim improved well-being and coping with stress, facilitation of social interaction, improvement of depression, better control of psychotic symptoms, and reduction of the side-effects of the anti-psychotic medication), and (c) cannabis abuse and schizophrenia reinforce each other.
Compared with the offenders suffering from schizophrenia, significantly fewer cases of multiple substance abuse were identified among the non-offenders suffering from schizophrenia (35.9 vs. 2.9%; Table 2). In addition, the patterns of substance use varied to a large extent: while all of the mentally ill offenders consumed alcohol in addition to the abuse of cannabis or benzodiazepines, the illicit substance abuse of five of the healthy offenders also included opiates or cocaine. While illicit substance abuse alone was not a strong predictor of illegal behavior, the combination of illicit drugs and alcohol appears to stimulate criminal behavior especially in patients suffering from schizophrenia. This result is in line with studies pointing to an association between alcohol abuse and aggressive behavior in mentally ill as well as in healthy subjects (42, 57, 58). According to Giancola and Parrott (44), alcohol significantly strengthens the relation between stimulant drug use and aggression among men. The increased aggressiveness under alcohol is probably caused by three interacting mechanisms (59): (a) disinhibition, (b) aggravation of aggressive impulses, and (c) behavioral disorganization.
Although our data did not suggest a link between cannabis use and criminal behavior in general, we must not underestimate other problematic consequences of cannabis abuse such as non-compliance, persistence of psychotic symptoms, and reinforcement of negative symptoms (58).
The influence of substance abuse on the pattern of criminal behavior was very similar in healthy and schizophrenic offenders (Table 3). Our results lead to the conclusion that alcohol and illicit drugs have no influence on the severity of offenses. However, we found a clear association between any kind of substance abuse and the frequency of criminal acting as well as a significant relationship between illicit drugs and an early start of the criminal career, independent of the mental health status of the subjects (60). Our data suggest that the pattern of substance abuse by schizophrenic offenders shows more similarities to that of healthy offenders than to that of non-offenders with schizophrenia. These findings are in line with our own study on family structures and socialization (see also Table 1) (61, 62). Independent of the mental state, dysfunctional family structures and substance abuse are associated with illegal conduct. However, our data must not be understood as an assertion that schizophrenia itself does not account for criminal behavior at all. Although certain psychotic features of schizophrenia, as for example threat-control-override symptoms are not very important for criminal behavior of psychotic patients in general, they are strongly associated with severe aggressive acts, such as severe bodily injury and homicide (63).
Main Findings
In accordance with the literature, high rates of substance abuse in general are associated with both, schizophrenia and offending behavior.
High rates of only illicit substance abuse—especially cannabis—are also found among patients suffering from schizophrenia without any history of offending behavior.
However, the abuse of illicit substances combined with alcohol and the abuse of alcohol only are associated with high rates of criminal behavior among patients with schizophrenia. In particular, the abuse of illicit drugs was found in a subgroup with an early onset of criminal behavior.
Strengths and Limitations
The sample size of the study (103 mentally disorders NGRI and 3 matched control groups) allows to draw robust and differentiated conclusions concerning the impact of substance abuse on criminal behavior in offenders suffering from schizophrenia. However, Eisner (50) stated that the associations between the single features of problematic conduct such as violent and illegal behavior, alcohol and illicit drug use, show substantial cultural variations.
Therefore we have to take into account the globally different rates of criminality and substance abuse. As they are substantially higher in the USA compared to Europe, the results of US-studies apply only partly to European countries. Austria with its low rates of criminality and substance abuse (except alcohol) is in line with most of the other Western European countries. As a consequence, methodologically similar studies in other regions are necessary to investigate the variations of the impact of the culture-specific types of substance consumption on the criminal behavior of patients suffering from schizophrenia.
Author Contributions
TS and HS planned the study and collected the data of the offender groups. TS did the statics and wrote the paper. KR collected the data of both non-offending groups.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Volavka J, Laska E, Baker S, Meisner M, Czobor P, Krivelevich I. History of violent behaviour and schizophrenia in different cultures. Analyses based on the WHO study on determinants of outcome of severe mental disorders. Br J Psychiatry (1997) 171:9–14.
2. Wallace C, Mullen P, Burgess P, Palmer S, Ruschena D, Browne C. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry (1998) 172:477–84. doi: 10.1192/bjp.172.6.477
3. Arseneault L, Moffitt TE, Caspi A, Taylor PJ, Silva PA. Mental disorders and violence in a total birth cohort: results from the Dunedin Study. Arch Gen Psychiatry (2000) 57:979–86. doi: 10.1001/archpsyc.57.10.979
4. Walsh E, Buchanan A, Fahy T. Violence and schizophrenia: examining the evidence. Br J Psychiatry (2002) 180:490–5. doi: 10.1192/bjp.180.6.490
5. Soyka M, Ufer S. Aggression bei Schizophrenien: prävalenz, psychopathologische und soziodemographische Korrelate. Fortschr Neurol Psychiatr. (2002) 70:171–7. doi: 10.1055/s-2002-24638
6. Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tattan T, et al. Predicting violence in schizophrenia: a prospective study. Schizophr Res. (2004) 67:247–52. doi: 10.1016/S0920-9964(03)00091-4
7. Schanda H, Knecht G, Schreinzer D, Stompe T, Ortwein-Swoboda G, Waldhoer T. Homicide and major mental disorders: a 25-year study. Acta Psychiatr Scand. (2004) 110:98–107. doi: 10.1111/j.1600-0047.2004.00305.x
8. Schanda H. (2006). Untersuchungen zur Frage des Zusammenhangs zwischen Psychosen und Kriminalität/Gewalttätigkeit. Fortschr Neurol Psychiatr. (2006) 74:85–100. doi: 10.1055/s-2004-830290
9. Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. (2009) 6:e1000120. doi: 10.1371/journal.pmed.1000120
10. Eronen M, Tiihonen J, Hakola P. Schizophrenia and homicidal behavior. Schizophr Bull. (1996) 22:83–9. doi: 10.1093/schbul/22.1.83
11. Hiday VA. Understanding the connection between mental illness and violence. Int J Law Psychiatry (1997) 20:399–417. doi: 10.1016/S0160-2527(97)00028-9
12. Mullen PE. A reassessment of the link between mental disorder and violent behaviour, and its implications for clinical practice. Aust NZ J Psychiatry (1997) 31:3–11. doi: 10.3109/00048679709073793
13. Räsänen P, Tiihonen J, Isohanni M, Rantakallio P, Lehtonen J, Moring J. Schizophrenia, alcohol abuse, and violent behavior: a 26-year followup study of an unselected birth cohort. Schizophr Bull. (1998) 24:437–41. doi: 10.1093/oxfordjournals.schbul.a033338
14. Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner HR, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry (1998) 155:226–31.
15. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. (1999) 25:505–17. doi: 10.1093/oxfordjournals.schbul.a033397
16. Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur risk assessment study. Am J Psychiatry (2000) 157:566–72. doi: 10.1176/appi.ajp.157.4.566
17. Brennan PA, Mednick SA, Hodgins S. Major mental disorders and criminal violence in a Danish birth cohort. Arch Gen Psychiatry (2000) 57:494–500. doi: 10.1001/archpsyc.57.5.494
18. Grann M, Fazel S. Substance misuse and violent crime: Swedish population study. BMJ (2004) 22, 1233–4. doi: 10.1136/bmj.328.7450.1233
19. Putkonen A, Kotilainen I, Joyal CC, Tiihonen J. Comorbid personality disorders and substance use disorders of mentally ill homicide offenders: a structured clinical study on dual and triple diagnoses. Schizophr Bull. (2004) 30:9–72. doi: 10.1093/oxfordjournals.schbul.a007068
20. Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry (2004) 161:716–27. doi: 10.1176/appi.ajp.161.4.716
21. Modestin J, Wuermle O. Criminality in men with major mental disorder with and without comorbid substance abuse. Psychiatry Clin Neurosci. (2005) 59:25–9. doi: 10.1111/j.1440-1819.2005.01327.x
22. Joyal CC, Putkonen A, Mancini-Marïe A, Hodgins S, Kononen M, Boulay L, et al. Violent persons with schizophrenia and comorbid disorders: a functional magnetic resonance imaging study. Schizophr Res. (2007) 91:97–102. doi: 10.1016/j.schres.2006.12.014
23. Soyka M, Graz C, Bottlender R, Dirschedl P, Schoech H. Clinical correlates of later violence and criminal offences in schizophrenia. Schizophr Res. (2007) 94:89–98. doi: 10.1016/j.schres.2007.03.027
24. Grann M, Danesh J, Fazel S. The association between psychiatric diagnosis and violent re-offending in adult offenders in the community. BMC Psychiatry (2008) 8:92. doi: 10.1186/1471-244X-8-92
25. Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry (2009) 66:152–61. doi: 10.1001/archgenpsychiatry.2008.537
26. Fazel S, Långström N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. JAMA (2009) 20:2016–23. doi: 10.1001/jama.2009.675
27. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) study. JAMA (1990) 264:2511–8. doi: 10.1001/jama.1990.03450190043026
28. Farrell M, Howes S, Taylor C, Lewis G, Jenkins R, Bebbington P, et al. Substance misuse and psychiatric comorbidity: an overview of the OPCS National Psychiatric Morbidity Survey. Addict Behav. (1998) 23:909–18.
29. Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophr Res. (1999) 35(Suppl.):93–100.
30. Drake RE, Wallach MA. Dual diagnosis: 15 years of progress. Psychiatr Serv. (2000) 51:1126–9. doi: 10.1176/appi.ps.51.9.1126
31. Mueser KT, Yarnold PR, Rosenberg SD, Swett C Jr, Miles KM, Hill D. Substance use disorder in hospitalized severely mentally ill psychiatric patients: prevalence, correlates, and subgroups. Schizophr Bull. (2000) 26:179–92. doi: 10.1093/oxfordjournals.schbul.a033438
32. Duke PJ, Pantelis C, McPhillips MA, Barnes TR. Comorbid non-alcohol substance misuse among people with schizophrenia: epidemiological study in central London. Br J Psychiatry (2001) 179:509–13. doi: 10.1192/bjp.179.6.509
33. Cantwell R, Scottish Comorbidity Study Group. Substance use and schizophrenia: effects on symptoms, social functioning and service use. Br J Psychiatry (2003) 182:324–9. doi: 10.1192/bjp.182.4.324
34. Miles H, Johnson S, Amponsah-Afuwape S, Finch E, Leese M, Thornicroft G. Characteristics of subgroups of individuals with psychotic illness and a comorbid substance use disorder. Psychiatr Serv. (2003) 54:554–61. doi: 10.1176/appi.ps.54.4.554
35. Margolese HC, Malchy L, Negrete JC, Tempier R, Gill K. Drug and alcohol use among patients with schizophrenia and related psychoses: levels and consequences. Schizophr Res. (2004) 67:157–66. doi: 10.1016/S0920-9964(02)00523-6
36. Compton MT, Weiss PS, West JC, Kaslow NJ. The associations between substance use disorders, schizophrenia-spectrum disorders, and Axis IV psychosocial problems. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:939–46. doi: 10.1007/s00127-005-0964-4
37. Korkeila JA, Svirskis T, Heinimaa M, Ristkari T, Huttunen J, Ilonen T, et al. Substance abuse and related diagnoses in early psychosis. Compr Psychiatry (2005) 46:447–52. doi: 10.1016/j.comppsych.2005.03.008
38. Barnes TR, Mutsatsa SH, Hutton SB, Watt HC, Joyce EM. Comorbid substance use and age at onset of schizophrenia. Br J Psychiatry (2006) 188:237–42. doi: 10.1192/bjp.bp.104.007237
39. Mauri MC, Volonteri LS, De Gaspari IF, Colasanti A, Brambilla MA, Cerruti L. Substance abuse in first-episode schizophrenic patients: a retrospective study. Clin Pract Epidemol Ment Health (2006) 23:4. doi: 10.1186/1745-0179-2-4
40. Gregg L, Barrowclough C. Haddock G. Reasons for increased substance use in psychosis. Clin Psychol Rev. (2007) 27:494–510. doi: 10.1016/j.cpr.2006.09.004
41. Bushman BJ, Cooper HM. Effects of alcohol on human aggression: an integrative research review. Psychol Bull. (1990) 107:341–54. doi: 10.1037/0033-2909.107.3.341
42. Hoaken PN, Pihl RO. The effects of alcohol intoxication on aggressive responses in men and women. Alcohol Alcohol. (2000) 35:471–7. doi: 10.1093/alcalc/35.5.471
43. Giancola PR, Saucier DA, Gussler-Burkhardt NL. The effects of affective, behavioral, and cognitive components of trait anger on the alcohol-aggression relation. Alcohol Clin Exp Res. (2003) 27:1944–54. doi: 10.1097/01.ALC.0000102414.19057.80
44. Giancola PR, Parrott DJ. Differential effects of past-year stimulant and sedative drug use on alcohol-related aggression. Addict Behav. (2005) 30:1535–54. doi: 10.1016/j.addbeh.2005.02.011
45. Giancola PR. Influence of subjective intoxication, breath alcohol concentration, and expectancies on the alcohol-aggression relation. Alcohol Clin Exp Res. (2006) 30:844–50. doi: 10.1111/j.1530-0277.2006.00099.x
46. Parrott DJ, Giancola PR. The effect of past-year heavy drinking on alcohol-related aggression. J Stud Alcohol. (2006) 67:122–30. doi: 10.15288/jsa.2006.67.122
47. Giancola PR. The underlying role of aggressivity in the relation between executive functioning and alcohol consumption. Addict Behav. (2007) 32:765–83. doi: 10.1016/j.addbeh.2006.06.015
48. World Health Organisation (WHO). Department of Mental Health and Substance Abuse. Global Status Report on Alcohol 2014. Geneva:WHO (2014).
49. United Nations Office of Drug and Crime. World Drug Report 2016. New York, NY: United Nations Publication (2016).
50. Eisner M. Gewalt und andere Formen von Problemverhalten. Ähnlichkeiten und Unterschiede in internationaler Perspektive. J Konflikt Gewaltforschung (2001) 3:44–67.
51. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Press Inc. (1994).
53. Kleining G, Moore H. Soziale Selbsteinstufung (SSE). Kölner Z Soziol Sozialpsychol. (1968) 20:502–52.
54. Taylor PJ. Motives for offending among violent and psychotic men. Br J Psychiatry (1985) 147:491–8. doi: 10.1192/bjp.147.5.491
55. Myles H, Myles N, Large M. Cannabis use in first episode psychosis: meta-analysis of prevalence, and the time course of initiation and continued use. Aust NZJ Psychiatry (2016) 50:208–19. doi: 10.1177/0004867415599846
56. Mustonen A, Niemelä S, Nordström T, Murray GK, Mäki P, Jääskeläinen E, et al. Adolescent cannabis use, baseline prodromal symptoms and the risk of psychosis. Br J Psychiatry (2018) 212:227–33. doi: 10.1192/bjp.2017.52
57. Bushman BJ. Effects of alcohol on human aggression. Validity of proposed explanations. Recent Dev Alcohol (1997) 13:227–43.
58. Swartz MS, Wagner HR, Swanson JW, Stroup TS, McEvoy JP, McGee M, et al. Substance use and psychosocial functioning in schizophrenia among new enrolees in the NIMH CATIE study. Psychiatr Serv. (2006) 57:1110–6. doi: 10.1176/ps.2006.57.8.1110
59. Pihl RO, LeMarquand D. Serotonin and aggression and the alcohol-aggression relationship. Alcohol Alcohol. (1998) 33:55–65. doi: 10.1093/oxfordjournals.alcalc.a008348
60. Hodgins S. The etiology and development of offending among persons with major mental disorders. In: Hodgins S, editor. Violence Among the Mentally Ill. Effective Treatment and Management Strategies. Dordrecht: Kluwer (2000). p. 89–116. doi: 10.1007/978-94-011-4130-7_7
61. Stompe T, Strnad A, Ritter K, Fischer-Danzinger D, Letmaier M, Ortwein-Swoboda G, et al. Patterns of socialization in male schizophrenic offenders. Aust NZJ Psychiatry (2006) 40:554–61. doi: 10.1080/j.1440-1614.2006.01838.x
62. Stompe T, Ritter K, Schanda H. Prädiktoren für Gewaltdelikte bei Schizophrenie. In: Stompe T, Schanda H, editors Schizophrenie und Gewalt. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft (2018) p. 91–154.
Keywords: schizophrenia, substance abuse, alcohol, illicit drugs, criminal behavior, violence
Citation: Stompe T, Ritter K and Schanda H (2018) Patterns of Substance Abuse in Offenders With Schizophrenia— Illness-Related or Criminal Life-Style? Front. Psychiatry 9:233. doi: 10.3389/fpsyt.2018.00233
Received: 30 March 2018; Accepted: 15 May 2018;
Published: 12 June 2018.
Edited by:
Athanassios Douzenis, National and Kapodistrian University of Athens Medical School, GreeceReviewed by:
Domna Tsaklakidou, University General Hospital Attikon, GreeceStelios Panagiotis Kympouropoulos, University General Hospital Attikon, Greece
Konstantinos Tasios, National Health System, Greece
Copyright © 2018 Stompe, Ritter and Schanda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Stompe, dGhvbWFzLnN0b21wZUBtZWR1bml3aWVuLmFjLmF0
 Thomas Stompe
Thomas Stompe Kristina Ritter3
Kristina Ritter3 Hans Schanda
Hans Schanda