- 1Department of Psychiatry, World Health Organization (WHO) Collaborating Centre for Research and Training in Mental Health, Neurosciences, and Substance Abuse, University of Ibadan, Ibadan, Nigeria
- 2Department of Psychiatry, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
Background: Very little is known about the relationship between spontaneous and treatment-induced motor syndromes in Africans with first episode schizophrenia.
Objective: We investigated the association between spontaneous NSS and EPS, with treatment-induced EPS in a homogenous sample of Black Africans with first episode schizophrenia.
Methods: We examined Xhosa (South Africa) and Yoruba (Nigeria) patients, using the Neurological Evaluation Scale and extrapyramidal symptoms scale before and at 3 months after exposure to low dose flupenthixol decanoate. Pearson's correlations and Linear regression models, controlling for duration of untreated psychosis (D.U.P) and premorbid adjustments, were used in examining associations.
Results: Among 99 participants in the baseline sample, 91 (91.8%) and 20 (20.2%) had at least one definite NSS and EPS, respectively, before exposure to antipsychotics. Treatment-induced EPS were recorded in 34 (38.6%). Spontaneous EPS was associated with treatment-emergent Akathisia in participants with a longer D.U.P (r = 0.75, β = 0.70, p = 0.008). This association was specific for Parkinsonism (r = 0.75, β = 0.85, p = 0.008) and dyskinesia (r = 0.75, β = 1.70, p = 0.008).
Conclusion: Similar to previous findings for tardive dyskinesia in studies implementing longer-term follow-up, spontaneous EPS may also predict short-term antipsychotic-induced EPS such as akathisia. These results may be important for early identification of patients at risk of treatment-induced Akathisia-linked psychomotor agitation in first episode schizophrenia.
Introduction
Early descriptions of schizophrenia include a broad spectrum of neurological examination abnormalities (1) such as Neurological soft signs (NSS) (2) and extrapyramidal syndromes (EPS) (3). Yet, the introduction of antipsychotics has led to a universal tendency to associate EPS with side effects (4) and NSS with neurodevelopmental defects (5).
In other perspective, NSS and EPS are two extremes in the diversity of neuromotor abnormalities in schizophrenia (6) [as NSS are subtle, but demonstrable, impairment in the ability to perform several motor and sensory tests on neurological examination 7, and EPS the more obvious abnormalities of locomotor control, involuntary movements, muscle tone, posture, and support 8). Spontaneous motor syndromes has emerged as a useful descriptor for signs (NSS and EPS) occurring before first exposure to antipsychotics (3, 9).
To date, the three cross-sectional studies of the relationship between NSS and treatment-emergent EPS in never-medicated first-episode schizophrenia have reported conflicting findings (10–12). However, a previous finding of an association between baseline NSS and subsequent development of tardive dyskinesia (TD) (13), across 24 months observation of a multiracial African sample is profoundly important for the prevention of EPS in susceptible patient populations. In this regard, some prior studies conducted in other multiracial samples suggest that persons of African ancestry may have a higher latent risk for motor syndromes (3, 14, 15). Yet, very little is known about the relationship between spontaneous and treatment-emergent motor syndromes in native (Black) Africans with first episode schizophrenia.
In the present study, which is based on a homogenous sample of Black Africans with first episode schizophrenia, we investigated the association between spontaneously occurring NSS and EPS, with 3 months treatment-induced EPS after exposure to minimum effective doses of flupenthixol decanoate.
Methods
The present study is part of an investigation of the socio-demographic, clinical, biological, and treatment aspects of schizophrenia (and related disorders) in patients presenting for biomedical treatment for the first time as out- or in-patients in psychiatric hospitals and community clinics in Cape-Town South Africa and Ibadan Nigeria. It was conducted by multidisciplinary teams comprising of psychiatrists, mental health nurses, and social workers at the two locations, and funded by the New Partnership for Africa's Development through the Department of science and Technology of South Africa. Ethical approval was obtained from the University of Ibadan ethics committee and the Stellenbosch University Faculty of Medicine and Health Sciences Human Research Ethics Committees. Participants provided written, informed consent before interviews were conducted.
Subjects
The subjects comprised anti-psychotic naïve or minimally treated patients with first episode schizophrenia or schizophreniform disorder (5 subjects had a lifetime exposure to oral anti-psychotics of less than 4 weeks). The diagnosis of the relevant disorder was made according to criteria in the Diagnostic and Statistical Manual for Mental Disorders-Fourth edition (DSM-IV) (16) by the attending psychiatrist at the study locations. Patients were eligible if they were aged between 16 and 45 years and have had less than 4 weeks of oral anti-psychotic exposure during their life time. All eligible patients were informed about the study, and the procedure was explained to them in their home language. We excluded patients with previous treatment of long acting depot antipsychotics, and those meeting DSM IV criteria for current substance abuse. Also excluded were patients with significant physical illnesses (e.g., chronic kidney disease) determined from the result of a full physical examination and appropriate laboratory investigations. Patients with mental retardation were excluded based on clinical history. Additional formal testing of cognitive capacity was not conducted. Participants comprised 81 Yoruba Nigerians, 18 Xhosa South-Africans. Participants did not receive monetary compensation for their participation. They were evaluated as far as possible before antipsychotic medications were prescribed. The following information was obtained from all patients: demographic data, personal history, psychiatric history, medical history, family history.
Measures
The Structured Clinical Interview for the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)- Patients edition (SCID-P) (17) was used in the recruitment of patients. The SCID-P provides for a standardized assessment that generates DSM-IV diagnoses using a semi-structured interview.
Assessment of Neuromotor Abnormalities
Tests assessing NSS and EPS (described below) were administered by independent raters (all psychiatrists) of African (AO, BC, and OE), and Asian (LA) descent after a 3 weeks training at the Tygerberg Hospital, Cape-Town, South Africa. Assessments were conducted in English and/or the home language of participants. The inter-rater reliability (IRR) conducted after training ranged from kappa = 0.62–0.82.
Neurological soft signs
NSS were evaluated using the Neurological Evaluation Scale (NES) (18). The NES is a well validated tool for neurological assessments in first episode schizophrenia. The scale includes “functionally meaningful” sub-scales which reflect signs of Motor co-ordination (tandem walk, rapid alternation, finger-to-thumb opposition, and finger-to-nose test), Sensory integration (audiovisual integration, stereognosis, graphesthesia, extinction, and right-to-left confusion tests), and Motor sequencing (first-ring, the first-edge-palm, Ozeretski, and rhythmic tapping tests). The other signs assessed by the NES include cerebral dominance, short-term memory, frontal release signs and eye movements. The NES items are scored with reference to the descriptive anchors provided on a three-point scale (no abnormality = 0; mild, but definite impairment = 1; marked impairment = 2) with the exception of “suck” and “snout” reflexes which are scored 0 or 2. In this study, a neurological abnormality was defined as the rating of 2 on any item (except cerebral dominance) on the NES. Each item was assessed according to a fixed order. For the present study, we considered the initial assessment of NSS before introduction of antipsychotics.
Extrapyramidal syndromes
EPS were sassed using the Extrapyramidal Symptom Rating Scale (ESRS) (19). The ESRS was designed to rate three main types of EPS: Parkinsonism, dystonia and dyskinetic symptoms. The measure also includes one question to cover akathisia. These categories of EPS are measured assessed in three components of the ESRS. A questionnaire and behavioral scale which includes subjective questions covering the categories of EPS as follows: Questions 1–5 and 7 (Parkinsonism), 6 (Akathisia), 8 (Dystonia), and 10–11 (Dyskinesia). The status of each EPS is rated as 0 (if absent), 1 (mild), 2 (moderate), and 3 (severe). The questionnaire component of the ESRS helps to differentiate subjective akinesia from depressive symptoms related to the anti-adrenaline effects of some antipsychotic drugs. But they also help to differentiate akathisia from anxiety and psychotic agitation. Also included in the ESRS are sections for physical examination covering Parkinsonism, dystonia, and dyskinetic movements as well as sections for clinical global impression items. The status of EPS on clinical examination is rated as 0 (if normal), 1 (very mild), 2 (mild), 3 (moderate), 4 (moderately severe), 5 (severe), 6 (extremely severe). In line with previous studies (20, 21), EPS was considered as present in this study where there was a rating suggesting mild but definite extrapyramidal sign or symptoms in the questionnaire scale (representing self-reported EPS) or clinical examination (representing observed EPS) components of the ESRS. The ESRS was administered before exposure to antipsychotics, followed by 2 weekly ESRS assessments throughout the duration of the study.
Psychiatric Assessment
The severity of the baseline psychopathology was evaluated by administering the Positive and Negative Syndrome Scale (PANSS) (22). The model of the PANSS adopted in this study (23) included five factor analysis derived domain for “positive symptoms” (delusions, hallucinations, unusual thought content, suspiciousness, and grandiosity), “negative symptoms” (lack of spontaneity, blunted affect, emotional withdrawals, apathetic social withdrawals, motor retardation, poor rapport and active social avoidance), “disorganization” (stereotyped thinking, poor attention, disorientation, conceptual disorganization and difficulty in abstraction), “excitement/hostility” (poor impulse control, excitement, hostility, and uncooperativeness), and “emotional distress” (anxiety, depression, guilt, and tension). The PANSS five factor solution (23) was adopted for this study based on its stability and superior validity when compared to the older three factor model (22).
The overall clinical status was assessed using the Clinical Global Impression (CGI-Severity) (24), while pre-morbid adjustment was explored using the Pre-morbid Adjustment Scale (PAS) (25). These measures have been used for the assessments of African patients with schizophrenia in previous studies (26).
Duration of untreated psychosis (D.U.P) was defined as the period in months from the onset of psychotic phenomena to first presentation for biomedical treatment. Onset of psychosis was defined as the presence for 1 week or more of psychotic symptoms with marked deterioration of functioning.
In all cases, pre-morbid functioning was the retrospective rating of patients' functioning up to 6 months before the defined onset of psychosis.
Treatment
After ruling out hypersensitivity by administering 1 milligram (mg) of oral flupenthixol after the first assessment of clinical and outcome characteristics, flexible doses of deep intramuscular flupenthixol injections starting from 5 or 10 mg in 2 or 4 weekly intervals were administered, with increases by 5 mg for up to a maximum of 30 mg depending on age, tolerability or response. Depot antipsychotic was chosen for this study to rule out covert non-adherence, a common phenomenon in first episode schizophrenia (27).
Statistical Analysis
Descriptive statistics such as mean, median and standard deviations were used to summarize quantitative variables, while frequencies and proportions were used for discrete variables. Spontaneous motor syndromes were those occurring before first exposure to flupenthixol decanoate (28). Emergent EPS was determined after exposure to flupenthixol decanoate and censoring participants meeting criteria for spontaneous EPS. The frequency and severity of spontaneous motor syndromes (NSS and EPS) are presented along with their subcategories.
For the relationship between spontaneous motor syndromes and treatment-emergent EPS, we first conducted a Pearson correlation between spontaneous NSS and EPS total scores with the scores for treatment-emergent EPS. Where significant correlation coefficients were observed, the relevant spontaneous motor syndrome scores (NSS or EPS) were entered as independent variables into separate linear regression models. Given previous observations that the frequency and severity of motor syndromes in schizophrenia may be affected by both premorbid adjustments and D.U.P (20), we conducted sub-group analyses controlling for types of D.U.P (</≥12 months) and premorbid adjustment (</≥mean for the entire sample).
Analyses were conducted using Stata version 13.0 (29). Values of p < 0.05 were considered significant.
Results
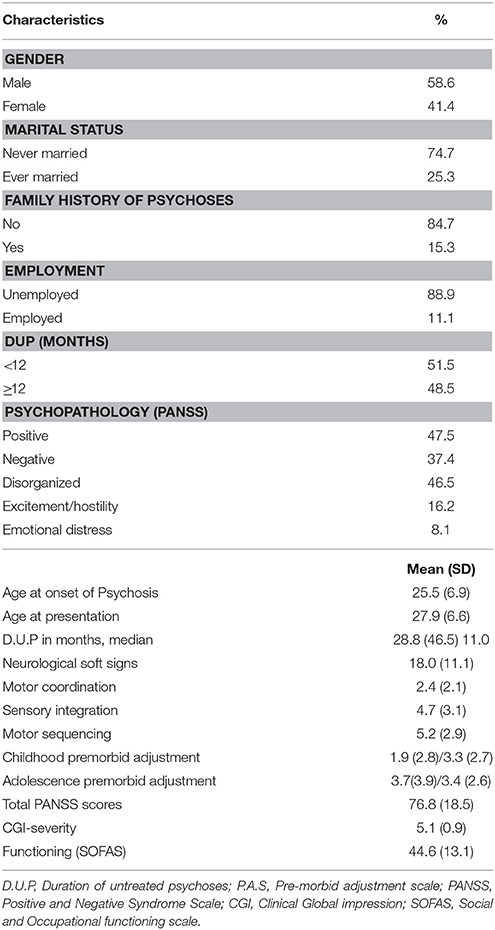
A total of 99 participants met study inclusion criteria and underwent full baseline assessments (Figure 1). Table 1 shows the baseline characteristics of the study sample. Never married and unemployed young men, who were between the ages of 18 and 32 years at onset of psychosis, predominated in the sample. They were mostly markedly ill with prominent positive and disorganization psychopathologies. The median D.U.P was approximately 2.5 years (Table 1).
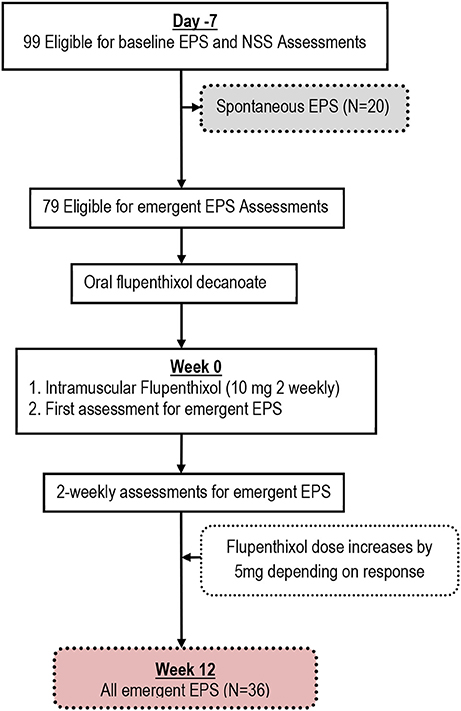
Figure 1. Flow chart showing Spontaneous and Emergent Extrapyramidal Syndromes (EPS) in the study of Black Africans with first episode schizophrenia.
Table 2 describes the frequency and severity of spontaneous motor syndromes and their relationship with 3-months treatment-emergent EPS. About 91.8 and 20.2% of participants had at least one definite spontaneous NSS and EPS respectively. The only spontaneous motor syndrome not recorded in the sample was dystonia. Newly emergent EPS was recorded in 34 (38.6%) participants within 3 months of exposure to antipsychotics. Whereas the overall domain scores of spontaneous motor syndromes were not associated with treatment emergent EPS, spontaneous dyskinesia was significantly associated with treatment emergent akathisia (r = 0.55, β = 1.65, p = 0.008). Table 2 also presents the distribution of doses of flupenthixol decanoate. Antipsychotic dose was not associated with treatment emergent motor syndromes.
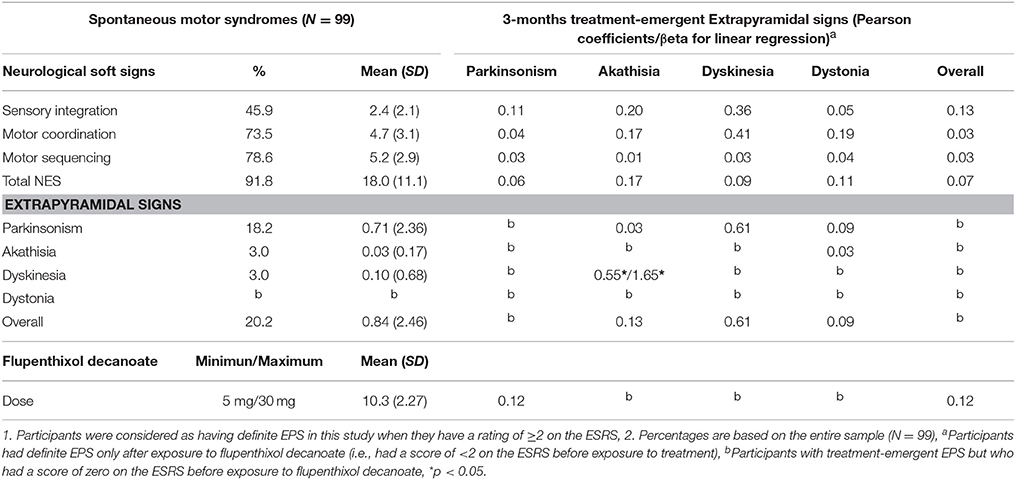
Table 2. Association of spontaneous motor syndromes with 3-months treatment induced extrapyramidal signs (EPS) assessed using the Extrapyramidal Symptom Rating Scale (ESRS) after exposure to flupenthixol decanoate in Black Africans with first-episode schizophrenia.
The results of analyses controlling for D.U.P and premorbid adjustment is presented in Table 3. Spontaneous EPS was associated with treatment-emergent Akathisia in participants with a longer D.U.P (r = 0.75, β = 0.70, p = 0.008). This association was specific for Parkinsonism and dyskinesia (Table 3). Conversely, spontaneous motor sequencing NSS was associated with treatment-emergent dystonia (r = −0.99, β = 1.89, p = 0.014).
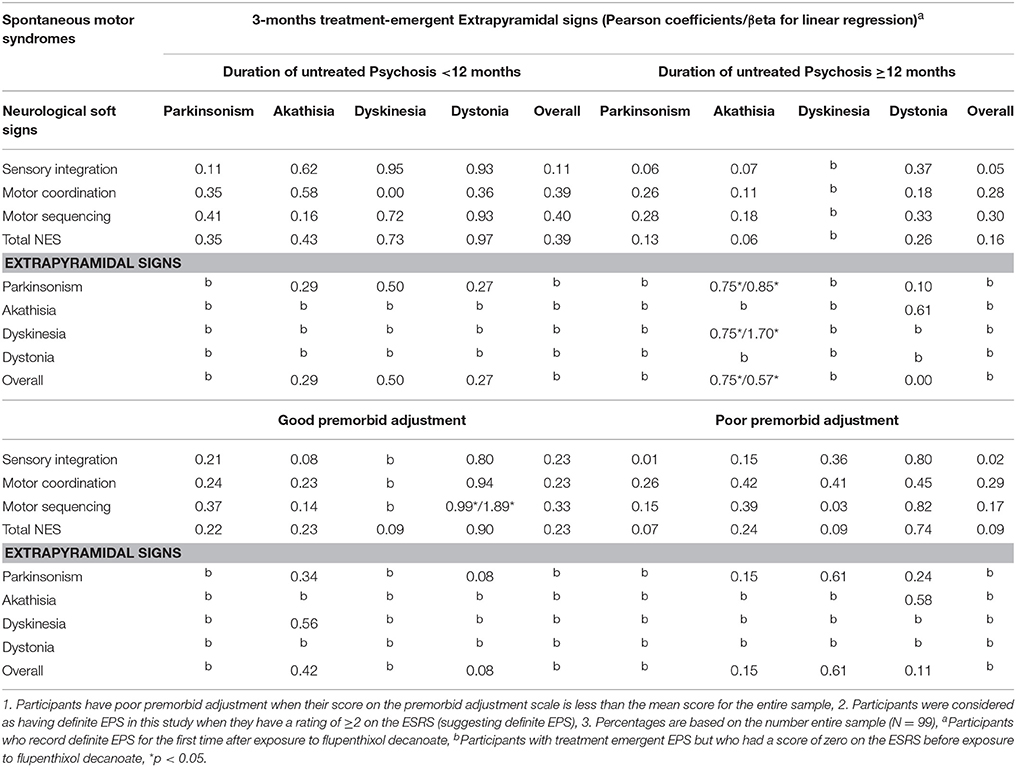
Table 3. Relationship of spontaneous and 3-months treatment induced motor syndromes adjusted by duration of untreated psychosis and Premorbid adjustments in Black Africans with first-episode schizophrenia.
Discussion
The present study is based on a homogenous sample of native (Black) Africans with first episode schizophrenia or schizophreniform disorder. Our main finding was that spontaneous EPS was associated with treatment emergent akathisia. This relationship was especially evident when considering spontaneous dyskinesia and Parkinsonism in patients with a longer D.UP. We also found an association between spontaneous motor sequencing NSS and treatment-emergent dystonia in patients with better premorbid functioning.
Our finding suggesting that spontaneous motor syndromes may predict treatment-emergent EPS are largely in keeping with previous studies (10–12). Whereas we found that spontaneous EPS is associated with treatment-emergent Akathisia, prior studies implementing a longer term follow-up of up to 24 months have demonstrated this relationship for treatment-emergent dyskinesia (13). Compared with dyskinesia, akathisia is an earlier onset antipsychotic induced EPS (30). We have implemented a short-term (3-months) follow-up in the present study. This relatively short period of antipsychotic exposure may have been insufficient to demonstrate large increases in dyskinesia in our sample. For example, we found only 5 participants with treatment-emergent dyskinesia the present study. This relatively small number may have been insufficient to power a significant relationship for dyskinesia even if it exists in our sample. Even so, our finding with respect to akathisia is important as it shows that, as with dyskinesia, spontaneous EPS may also predict the emergence of earlier onset antipsychotic-induced EPS. This finding may also be of value for the prevention of akathisia-linked psychomotor agitation in clinical samples through the early identification of susceptible patients. A future longer-term follow-up of our sample will be needed to investigate whether as in other populations, spontaneous motor syndromes predict treatment emergent dyskinesia in Black Africans with first episode schizophrenia.
Our finding of an association between spontaneous motor sequencing NSS and treatment-emergent dystonia in patients with better premorbid functioning was unexpected and must be interpreted with caution. However, it is feasible that such unpredictable findings suggest that there are more complex relationships between the diverse neuromotor abnormalities in schizophrenia. For example, it is plausible that spontaneous and emergent motor syndromes represent distinct, and potentially different, aspects of schizophrenia. This proposition is in keeping with the findings of distinct structural and functional changes (in the basal ganglia, pre-frontal and temporal cortices, as well as the cerebellum) in relation to the clinical spectrum of neuromotor abnormalities in schizophrenia (31, 32). Even so, the aforesaid association between spontaneous motor sequencing NSS and treatment-emergent dystonia in patients with better premorbid functioning may well have occurred by chance.
Strengths and Limitations
This study is based on a homogenous sample of Black Africans with first episode schizophrenia. Given previous observations that race may be important in determine putative risk for neuromotor abnormalities in schizophrenia (14, 15), the evidence provided by the present study is important for better understanding of the nature of neuromotor disturbances of schizophrenia. Prior information on neuromotor abnormalities in schizophrenia, including their evolution in relation to treatment has been based on mostly Caucasian or Mixed population (10, 12, 21). A key limitation of the present study is that the ESRS, which we have used for the ascertainment of EPS, does not provide a robust evaluation of all EPS and is more weighted toward Parkinsonism compared with, for example, Akathisia.
Conclusion
Spontaneous EPS is predictive of treatment-emergent akathisia during a relatively short period of follow-up. The findings overlap with those of a previous 24 months longitudinal observation in a mixed population of Africans where, given the long period of observation, the relationship between spontaneous motor syndrome and treatment-induced dyskinesia was discernible. The result of the present study is of value for prevention of akathisia-linked psychomotor agitation in clinical samples through the early identification of susceptible patients. A future longer-term follow-up of our homogenous sample of Black Africans with first episode schizophrenia will investigate whether as in other populations, spontaneous motor syndromes predict treatment emergent dyskinesia in this population.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was made possible by grants from the New Partnership for Africa's Development, and Lundbeck International.
References
1. Reiter PJ. Extrapyramidal motor disturbances in Dementia Preacox. Acta Psychiatr Neurol. (1926) 1:281–310. doi: 10.1111/j.1600-0447.1926.tb11031.x
2. Heinrichs DW, Buchanan RW. Significance and meaning of neurological signs in schizophrenia. Am J Psychiatry (1988) 145:11–8. doi: 10.1093/schbul/sbi028
3. Pappa S, Dazzan P. Spontaneous movement disorders in antipsychotic-naive patients with first-episode psychoses: a systematic review. Psychol Med. (2009) 39:1065–76. doi: 10.1017/S0033291708004716
4. Fann WE. Tardive dyskinesia and other drug induced movement disorders. In: Fann WE, Smith RC, Davis JM, Domino EF, editors. Tardive Dyskinesia: Research and Treatment. Jamaica, NY: Spectrum Publications (1980). p. 216–32.
5. Whitty PF, Owoeye O, Waddington JL. Neurological signs and involuntary movements in schizophrenia: intrinsic to and informative on systems pathobiology. Schizophr Bull. (2009) 35:415–24. doi: 10.1093/schbul/sbn126
6. Peralta V, Cuesta MJ. Neuromotor abnormalities in neuroleptic-naive psychotic patients: antecedents, clinical correlates, and prediction of treatment response. Compr Psychiatry. (2011) 52:139–45. doi: 10.1016/j.comppsych.2010.05.009
7. Ojagbemi A. Neurological soft signs. In: Ziegler-Hill, V Shackelford, TK, editors. Encyclopedia of Personality and Individual Differences. 2017 ed. Springer International Publishing (2017). p. 1–5.
8. Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. 7th ed. Extrapyramidal Syndrome: Saunders, an imprint of Elsevier Inc. (2003). Available online at: https://medical-dictionary.thefreedictionary.com/extrapyramidal+syndrome.
9. Cuesta MJ, Sanchez-Torres AM, de Jalon EG, Campos MS, Ibanez B, Moreno-Izco L, et al. Spontaneous parkinsonism is associated with cognitive impairment in antipsychotic-naive patients with first-episode psychosis: a 6-month follow-up study. Schizophr Bull. (2014) 40:1164–73. doi: 10.1093/schbul/sbt125
10. Compton MT, Fantes F, Wan CR, Johnson S, Walker EF. Abnormal movements in first-episode, nonaffective psychosis: dyskinesias, stereotypies, and catatonic-like signs. Psychiatry Res. (2015) 226:192–7. doi: 10.1016/j.psychres.2014.12.048
11. Peralta V, de Jalon EG, Campos MS, Basterra V, Sanchez-Torres A, Cuesta MJ. Risk factors, pre-morbid functioning and episode correlates of neurological soft signs in drug-naive patients with schizophrenia-spectrum disorders. Psychol Med. (2011) 41:1279–89. doi: 10.1017/S0033291710001856
12. Peralta V, Basterra V, Campos MS, de Jalon EG, Moreno-Izco L, Cuesta MJ. Characterization of spontaneous Parkinsonism in drug-naive patients with nonaffective psychotic disorders. Eur Arch Psychiatry Clin Neurosci. (2012) 262:131–8. doi: 10.1007/s00406-011-0219-1
13. Emsley R, Turner HJ, Oosthuizen PP, Carr J. Neurological abnormalities in first-episode schizophrenia: temporal stability and clinical and outcome correlates. Schizophr Res. (2005) 75:35–44. doi: 10.1016/j.schres.2004.06.014
14. Morgenstern H, Glazer WM. Identifying risk factors for tardive dyskinesia among long-term outpatients maintained with neuroleptic medications. Results of the Yale Tardive Dyskinesia Study. Arch Gen Psychiatry (1993) 50:723–33.
15. Glazer WM, Morgenstern H, Doucette J. Race and tardive dyskinesia among outpatients at a CMHC. Hosp. Commun. Psychiatry (1994) 45:38–42. doi: 10.1176/ps.45.1.38
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association (1994).
17. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders Clinician Version (SCID-IV). Washington, DC: American Psychiatric Press Inc. (1996).
18. Buchanan RW, Heinrichs DW. The Neurological Evaluation Scale (NES): a structured instrument for the assessment of neurological signs in schizophrenia. Psychiatry Res. (1989) 27:335–50. doi: 10.1016/0165-1781(89)90148-0
19. Chouinard G, Margolese HC. Manual for the extrapyramidal symptom rating scale (ESRS). Schizophr Res. (2005) 76:247–65. doi: 10.1016/j.schres.2005.02.013
20. Honer WG, Kopala LC, Rabinowitz J. Extrapyramidal symptoms and signs in first-episode, antipsychotic exposed and non-exposed patients with schizophrenia or related psychotic illness. J Psychopharmacol. (2005) 19:277–85. doi: 10.1177/0269881105051539
21. Kopala LC, Good KP, Honer WG. Extrapyramidal signs and clinical symptoms in first-episode schizophrenia: response to low-dose risperidone. J Clin Psychopharmacol. (1997) 17:308–13. doi: 10.1097/00004714-199708000-00011
22. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
23. van der Gaag M, Hoffman T, Remijsen M, Hijman R, de Haan L, van Meijel B, et al. The five-factor model of the Positive and Negative Syndrome Scale II: a ten-fold cross-validation of a revised model. Schizophr Res. (2006) 85:280–7. doi: 10.1016/j.schres.2006.03.021
24. Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: United States Department of Health education and Welfare (1976).
25. Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. (1982) 8:470–84. doi: 10.1093/schbul/8.3.470
26. Gureje O, Aderibigbe YA, Olley O, Bamidele RW. Premorbid functioning in schizophrenia: a controlled study of Nigerian patients. Comprehens Psychiatry (1994) 35:437–40. doi: 10.1016/0010-440X(94)90226-7
27. Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry (2011) 168:603–9. doi: 10.1176/appi.ajp.2011.10081224
28. Schooler NR, Kane JM. Research diagnoses for tardive dyskinesia. Arch Gen Psychiatry (1982) 39:486–7. doi: 10.1001/archpsyc.1982.04290040080014
30. Metin B, Metin SZ, Gunduz A, Poyraz BC, Ozmen M, Kiziltan G, et al. Brainstem reflexes are hyperactive in patients with drug-induced akathisia. Neurol Sci. (2017) 38:1683–9. doi: 10.1007/s10072-017-3038-y
31. Gay O, Plaze M, Oppenheim C, Mouchet-Mages S, Gaillard R, Olie JP, et al. Cortex morphology in first-episode psychosis patients with neurological soft signs. Schizophr Bull. (2013) 39:820–9. doi: 10.1093/schbul/sbs083
Keywords: neurological examination, side effects, neurodevelopmental defects, locomotor control, tardive dyskinesia, African ancestry
Citation: Ojagbemi A, Chiliza B, Bello T, Asmal L, Esan O, Emsley R and Gureje O (2018) Neurological Soft Signs, Spontaneous and Treatment Emergent Extrapyramidal Syndromes in Black Africans With First Episode Schizophrenia. Front. Psychiatry 9:172. doi: 10.3389/fpsyt.2018.00172
Received: 18 October 2017; Accepted: 16 April 2018;
Published: 01 May 2018.
Edited by:
Johannes Schröder, University of Heidelberg, GermanyReviewed by:
Karl Bechter, Universität Ulm, GermanyAnna Comparelli, Sapienza Università di Roma, Italy
Copyright © 2018 Ojagbemi, Chiliza, Bello, Asmal, Esan, Emsley and Gureje. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akin Ojagbemi, ZHJha2luamFnYmVtaUB5YWhvby5jb20=; YWtpbm9qYWdiZW1pQGdtYWlsLmNvbQ==
 Akin Ojagbemi
Akin Ojagbemi Bonga Chiliza2
Bonga Chiliza2