- 1Centre for eHealth and Wellbeing Research, Department of Psychology, Health and Technology, University of Twente, Enschede, Netherlands
- 2Department of Research, Stichting Transfore, Deventer, Netherlands
- 3Optentia Research Focus Area, North-West University, Vanderbijlpark, South Africa
Background: Treatment of offenders in forensic mental health is complex. Often, these in- or outpatients have low treatment motivation, suffer from multiple disorders, and have poor literacy skills. eHealth may be able to improve treatment outcomes because of its potential to increase motivation and engagement, and it can overcome the predominant one-size-fits-all approach by being tailored to individual patients.
Objective: To examine its potential, this systematic review studies the way that eHealth has been used and studied in forensic mental health and identifies accompanying advantages and disadvantages for both patients and treatment, including effectiveness.
Methods: A systematic search in Scopus, PsycINFO, and Web of Science was performed up until December 2017. Studies were included if they focused on technological interventions to improve the treatment of forensic psychiatric patients.
Results: The search resulted in 50 studies in which eHealth was used for treatment purposes. Multiple types of studies and technologies were identified, such as virtual reality, web-based interventions, and videoconferencing. The results confirmed the benefits of technology, for example, the acquisition of unique information about offenders, effectiveness, and tailoring to specific characteristics, but indicated that these are not fully taken advantage of.
Discussion: To overcome the barriers and obtain the benefits, eHealth has to have a good fit with patients and the forensic psychiatric context. It has to be seamlessly integrated in existing care and should not be added as an isolated element. To bridge the gap between the current situation and eHealth’s potential, further research on development, implementation, and evaluation should be conducted.
Introduction
Forensic mental health treatment focuses on the intersect between psychiatry and the law by dealing with the relationship between, assessment and treatment of mental illness and criminality of people whose behavior has led, or could lead, to offending (1, 2). Besides treatment of psychiatric disorders, a primary goal is to prevent criminal recidivism via addressing offense-related factors such as antisocial behavior or coping skills. These factors should be addressed via interventions and therapies based on evidence-based approaches such as cognitive behavior therapy (3) and the risk-needs-responsivity principles (4). However, developing and implementing such in-person interventions in this complex field has proven to be challenging. For example, meta analyzes on interventions targeting batterers, juvenile offenders, and relapse prevention of offenders found low overall effectiveness on clinical measures (5). These results indicate that there is room for the improvement in interventions in forensic mental health. A solution might be found in the use of eHealth in treatment. eHealth can be defined as technologies such as web-based interventions, apps, wearables, or virtual reality (VR), to improve and support health, well-being, and quality of care (6). Many studies acknowledge eHealth’s added value for general mental health [e.g. references (7–9)] but it is not yet clear what its advantages for forensic mental health treatment could be.
There are multiple complicating factors within forensic mental health that can influence the success of existing in-person interventions. Among other things, the forensic psychiatric population has specific characteristics, such as the low motivation that forensic psychiatric outpatients generally have for their, often mandated, treatment (10). Studies suggest that mandated treatment outcomes are often worse compared with patients without mandated treatment (11). Another complicating factor is that a large share of the forensic population displays psychiatric comorbidity (12, 13), and that not one, but multiple factors cause delinquent behavior and should be addressed in treatment (14). Furthermore, forensic psychiatric patients are often disproportionately poor, unemployed, and have lower literacy rates (15), which might affect their capability of being engaged in and adhering to interventions. Despite the complexity and diversity that the low motivation, low literacy, and comorbidity of forensic psychiatric patients bring to treatment, most interventions have a “one-size-fits-all approach.” Many interventions do not take individual differences into account (16) despite the acknowledgment of the importance of tailoring interventions to specific characteristics of individual patients (17–19). The use of eHealth technology within in-person treatments and interventions, which is referred to as blended care (20), could be a way to increase this required fit between interventions and patients. eHealth has several characteristics that could be of added value for forensic mental health.
First of all, the content, way of communicating and design of technology, can be tailored to subgroups or individual users, based on their characteristics, needs, or context (21). This tailoring or personalization of eHealth interventions creates a better fit between the technology and the individual user and consequently addresses the complexity and diversity of the forensic mental health domain. Tailoring has been proven to enhance user engagement and effectiveness of multiple eHealth interventions (22–25). The use of tailoring prevents the aforementioned one-size-fits all approach of interventions, which does not seem to suit the complex and broad forensic population (17).
Another way to account for the complexity of the target group is by the use of existing protocols, guidelines, and evidence-based theories in interventions, which is advised for forensic and also general mental health (26, 27). However, many existing in-person interventions for forensic mental health care are not theory-based, or treatment integrity by therapists is not always satisfactory (16, 28). Technology offers the possibility to deliver interventions based on theory and guidelines to patients in a standardized way to increase effectiveness, while still being able to tailor its content to individual patients. Consequently, eHealth can standardize care and interventions by incorporating existing guidelines (29).
eHealth has several characteristics that can increase the motivation of forensic psychiatric patients in managing their own care. If patients are motivated, they are more likely to have higher adherence to an intervention, meaning that they use it in the intended way and obtain positive treatment outcomes compared with disengaged and unmotivated patients (30, 31). Patient engagement can be achieved by using innovative, state-of-the-art technologies that appeal to the patient, like serious gaming, wearable technology, or VR (7, 30, 32). Many of these new technologies do not primarily rely on conscious cognitive reflection, but mainly create experiences, which suits the lower literacy and education of the average forensic psychiatric patient. The way an intervention is designed can contribute to adherence as well, for example, via the application of principles from persuasive design (33, 34). Finally, tailoring of a technology can positively impact adherence since it increases the fit with a patient’s needs and wishes and can increase the perceived personal relevance of an intervention (34), which has a positive influence on patient motivation.
Based on research on eHealth in general, many potential benefits of eHealth for forensic mental health can be identified. However, it is not yet clear in how far these advantages are relevant for and actualized in forensic mental health. To determine what the added value of eHealth is, this systematic review aims to provide an overview the current state of affairs of eHealth research in forensic mental health. This is accomplished by studying the types of studies, the studied technologies, and the mentioned advantages and disadvantages. Based on these findings, it can be identified if and how eHealth can have added value for forensic mental health, and domain-specific recommendations can be provided on how it can reach this potential added value. The research questions were generated via the PICOS method. The population was defined as forensic psychiatric patients, and interventions were all types of technologies used in the treatment of forensic psychiatric patients. Because of the explorative nature of this review, we did not address comparators in the research questions. Main outcomes were types of study, types of technology, and advantages and disadvantages. All study designs were included in this explorative review. This leads to the following research questions: [1] What studies are conducted on eHealth technologies used in the treatment of forensic psychiatric patients? [2] Which types of technologies are being researched in the treatment of forensic psychiatric patients? [3] What advantages and disadvantages accompany the different eHealth technologies that are used in the treatment of forensic psychiatric patients?
Methods
Inclusion and Exclusion Criteria
Studies that focused on the use of technological interventions to improve the treatment of forensic psychiatric patients were included. The main goal of the technology had to be related to the quality of treatment or the identification of elements essential for treatment, such as criminogenic needs or responsivity. Since the use of technology had to be of added value for the quality of treatment, technologies purely focused on facilitating the diagnostic process, such as computer-assisted testing, were excluded. Furthermore, forensic psychiatric patients had to be the main target group and primary user, so technologies aiming to solely support the work process of therapists were excluded. Finally, technologies that were not related to treatment, but merely focused on court-mandated monitoring of the patient’s location or assessment for court were excluded. Because of the broad scope and exploratory focus of this study, all study designs were included.
Literature Search
Electronic searches of the databases Scopus, PsycINFO, and Web of Science were conducted in December 2017. An information expert specialized in developing and improving search strategies was involved in the construction of the search strategy. The same search strategy was used in each database. Search terms can be found in Section “Full Electronic Search Strategy” in Appendix. They were divided into two categories: one on treatment within forensic mental healthcare and one on technology. Search terms were identified by studying the search terms of relevant literature, and expert consultation with researchers in forensic mental health. Articles published up until December 2017, written in English, Dutch, or German, were included.
After removing duplicates in EndNote, two authors (Saskia M. Kelders and Hanneke Kip) reviewed the titles. Records were included if titles indicated that the article focused on treatment of forensic psychiatric patients, and if there was a possibility that the study used technology for treatment purposes. Because of the possibility of technology not being mentioned in the title, broad criteria were used to prevent the unjust exclusion of relevant articles. Articles were included if at least one of the authors decided that it was relevant. After screening the titles, obtained abstracts were read by two authors (Yvonne H. A. Bouman and Hanneke Kip), using the aforementioned inclusion and exclusion criteria. If technology was not explicitly mentioned in the abstract, did not contribute to treatment, or had a primary user group that did not consist of patients, records were excluded. Records were included if consensus by both authors was reached. Finally, full-text articles were read by one author (Hanneke Kip). Reasons for excluding and doubts about including articles were discussed with other authors (Saskia M. Kelders and Yvonne H. A. Bouman).
Data Extraction
The data extraction process of this systematic review was mostly based on the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions (35). However, a quality assessment was not performed because of the heterogeneity of the included study topics and designs: ranging from explorative qualitative studies to RCTs. The data extraction process started with the generation of an elaborate data extraction form, based on the research questions, that was used to standardize the reporting of relevant information from all obtained studies. The data extraction form contained four categories with their own subcategories: type of study, type of technology, and advantages/benefits, disadvantages/barriers. The data extraction form was filled in by one author (Hanneke Kip), a second author (Yvonne H. A. Bouman) was consulted in case of any uncertainties. In the first phase of the data extraction process, all relevant information was copied literally into the narrative data extraction forms. After that, the information in the table was summarized or made more concise. To answer the first research question, study designs were categorized inductively. We distinguished between experimental, quasi-experimental, quantitative cross-sectional, qualitative, and literature studies. A brief summary of the study goal as described in the articles was added as well. We also indicated whether the effectiveness of an eHealth intervention was assessed by a study and, if this was the case, whether it was more effective, less effective or ineffective, based on a classification for defining intervention effectiveness of Morrison et al. (36). According to this classification, interventions can be seen as more effective if they led to improvements on the majority of outcomes, were at least as effective as comparison groups and more effective than no intervention groups. Interventions are classified as less effective if they led to improvements on a minority of outcome measures or were not as effective as comparison groups, but still more effective than waiting list groups. Interventions classified as ineffective did not lead to any improvements. The second research question was answered by coding the studied types of technologies inductively by comparing the nature of the technologies, resulting in six types of technologies. The results table was structured accordingly. For each study, the used technology, its target group, and its goal were described, using the data extraction forms. To answer the third research question, fragments on advantages and disadvantages literally copied from the articles were coded inductively as well. The first author executed the coding process, which included multiple iterations and constant adaptations, until data saturation was reached. During this iterative process, multiple versions of the code schemes were discussed with all authors and adapted accordingly. This resulted in two code schemes with main and subcodes representing different types of main and accompanying specified advantages and disadvantages.
Results
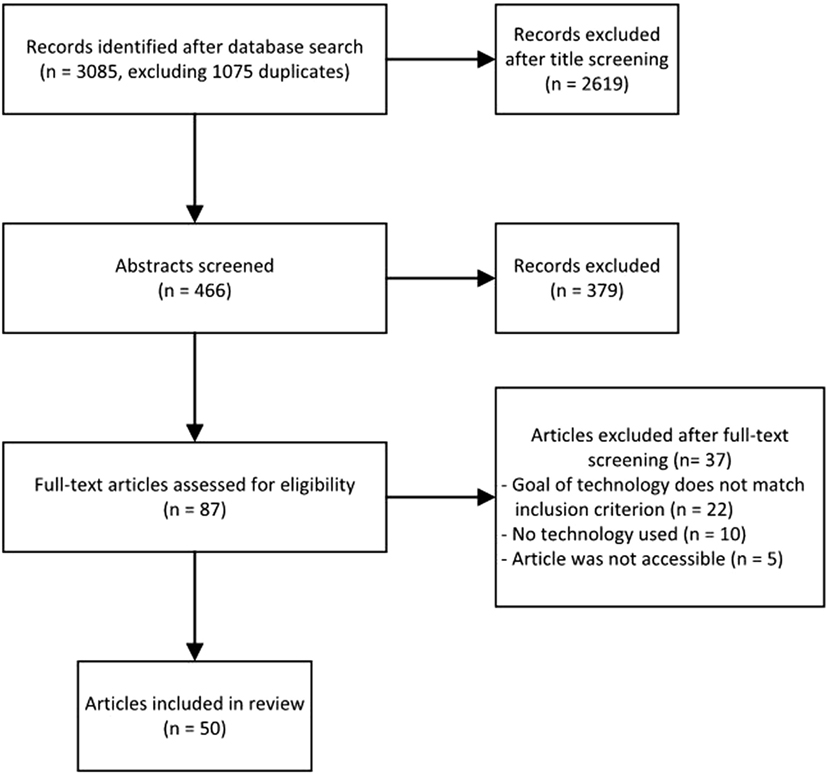
Search Results
The search strategy, the number of included articles, and reasons for full-text exclusion are provided in Figure 1. The main reason for excluding full-text articles was that they did not match the inclusion criteria: the goal of technology was not directly related to treatment, e.g., the mere monitoring of patients for security purposes, or the target group did not consist of patients, e.g., therapists.
The included 50 studies are provided in Table 1, which is structured based on the research questions. The first column provides the authors and year, the second addresses the first research question by providing the study goal, its design and effectiveness based on the design, the third column describes the technology, and the identified advantages and disadvantages are summarized in the last column. This table serves as the backbone of the result section and can be used to identify references.
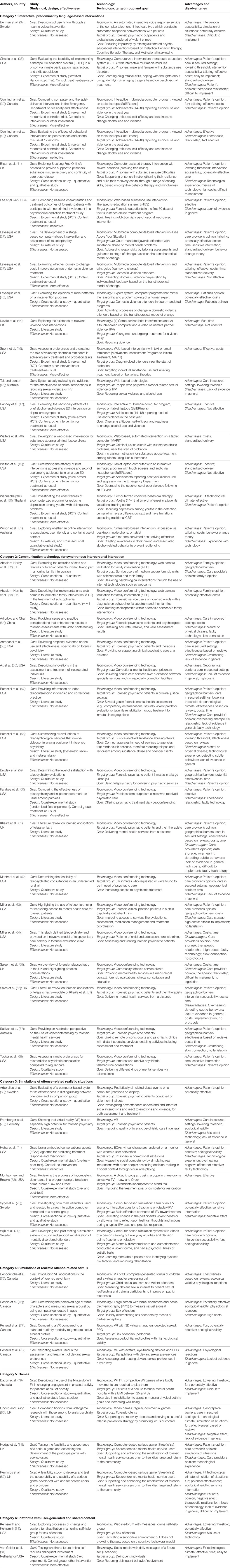
Table 1. Study characteristics, characteristics of technology, and advantages and disadvantages per study.
Study Designs, Research Goals, and Effectiveness
The included studies were categorized based on their study design (see Table 1). The following categories were identified: experimental studies (n = 9), quasi-experimental studies (n = 4), qualitative studies (n = 12), quantitative cross-sectional studies (n = 9), and literature studies (n = 16). There was much variation in research goals.
All included experimental studies used a randomized controlled trial with either two or three groups. The studies aimed to determine the effectiveness of interventions via measuring treatment outcomes such as depressive complaints, alcohol abuse, and attitudes toward violence. Several studies also paid attention to participation and satisfaction with the intervention. The quasi-experimental studies had differing goals: while some determined effectiveness via outcomes such as delinquent involvement, others were more focused on process-related outcomes such as treatment response and progress. Most of the qualitative studies investigated the perspective of the patient via measuring outcomes such as use of the technology, patient preferences, acceptability, or satisfaction with the intervention. Some studies also described and analyzed the development process of eHealth interventions. Studies in the quantitative, cross-sectional category had an especially broad range of research goals. While some determined attitudes and opinions about interventions, others aimed to design and validated realistic stimuli. Further topics that were studied were feasibility, implementation, or potential effectiveness of interventions. Studies focused not only on ready-to-use interventions but also on interventions that were still being developed. The literature studies had in common that they all used scientific literature to provide an overview of the current state of affairs of a specific type of intervention for forensic mental health. However, the included studies ranged from highly structured meta-analyses and systematic reviews to literature reviews and viewpoint papers. Consequently, research goals differed as well: several studies provided a systematic overview of empirical evidence, others provided an overview of existing interventions or technologies, and some focused mainly on the practical applications of technologies in practice.
The effectiveness of an individual intervention was assessed via an experimental or quasi-experimental study by 13 of the 50 studies. Ten of them found that an intervention was as at least as effective as a comparison group and more effective than no intervention groups on most of the outcomes. Three studies found no proof for effectiveness.
Types of Technology
To provide an oversight of the studied eHealth interventions, we created a categorization of the technologies described in the included articles, based on the way its content was presented and communicated to the user. This resulted in six types of technology.
Category 1: Interactive, Predominantly Language-Based Interventions
This type of technology aims to change offense-related cognitions or behavior, mostly via language-based information, assignments, or exercises (n = 17). Their content can be delivered via multiple modalities, e.g., written text, videos, or audio, and is often based on theory or existing, evidence-based therapies. The system also reacts on input of the user. Multiple technologies are used in this category, but most included interventions were delivered via a computer or tablet. A broad range of populations was targeted, among others juvenile offenders (27), domestic violence offenders (27, 43), prisoners in general (41), alcohol abusing, violence-involved adolescents (39, 40, 47), and substance abusing prisoners (38). Several web-based interventions were based on theoretical frameworks such as motivational interviewing, the transtheoretical model, cognitive-behavioral therapy or social cognitive theories. These interventions used different ways of delivering content, such as videos, avatars, telephones, tailored written feedback, and emails.
Category 2: Communication Technology for Synchronous Interpersonal Interaction
This type refers to the use of technology to enable a patient to directly communicate with a care provider, regardless of location (n = 17). The patient always interacts with another human being, and not the technology itself. The main goal of these synchronous communication technologies is to provide an alternative for in-person interaction, so multiple modalities such as sound, video, or text are used. All included studies examined video conferencing technology, which is a two-way interactive video and audio communication system. However, despite using the same technology, these studies did differ in the goal and target group: their focus ranged from, for example, video conferencing in forensic mental health in general (54, 57, 63, 64, 67) to specific target groups, for example, substance abusing patients (58), inmates with psychiatric problems (56, 59, 62, 68), or both schizophrenic patient and family (52, 53).
Category 3: Simulations of Offense-Related Realistic Situations
This type of technology focuses on the use of simulations in the treatment of forensic psychiatric patients (n = 6). In these simulations, visualized scenarios of possible events are presented to patients. The goal of this type of technology is to explore attitudes or behavioral responses to offense-related situations that are viewed as realistic and personally relevant by the user. Some studies used videos with real actors and authentic situations in which the user had to decide on behavioral reactions (69, 73, 74), while others simulated situations via virtual embodied conversational agents to conduct a dialog with prisoners (71), existing popular crime drama series (72), or VR (70).
Category 4: Simulations of Offense-Related Realistic Stimuli
This type of technology presented realistic depictions of stimuli related to the offense of forensic psychiatric patients (n = 4). The goal of using these stimuli is to elicit behavioral, emotional, cognitive, and/or physiological responses of the patient who are relevant for treatment. These stimuli are not interactive, so they do not respond to the actions of the patient, and are not situations. All included studies primarily focused on sex offenders by presenting computer-animated virtual characters depicting realistic naked human beings of several age categories and genders, via either VR or large screens (75–78).
Category 5: Games
This type of technology entails both the usage of existing, commercial games for treatment purposes, and serious games developed specifically for the treatment of forensic psychiatric patients (n = 4). Game elements are always present: the user has to improve his own achievement, or is competing with other users. Studies examined existing, commercial games to improve the recovery process or meet physical activity goals (79, 80), but a serious game specifically developed for rehabilitation purposes was described as well (81).
Category 6: Platforms with User-Generated and Shared Content
This sixth type refers to technologies in which patients can create and react on content, and add and share existing content (n = 2). These platforms can be freely accessible to anyone, e.g., social media, or an approved account can be required, e.g., private forums. The goal of these platforms is for users to share and read material like experiences or opinions to support them in refraining from delinquent behavior. Two studies focused on these kinds of platforms: one was a web-based self-help group for sex offenders (83), the other one made use of social media to reduce delinquent behavior (84).
Advantages
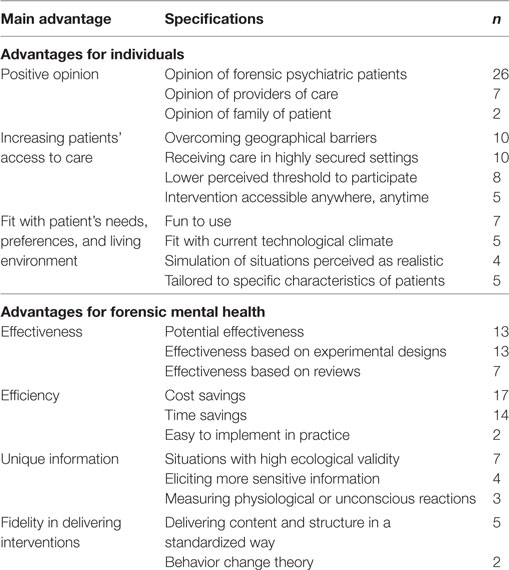
Types of advantages and disadvantages of eHealth technologies were extracted from the included studies via inductive coding. We identified main codes and accompanying subcodes based on relevant fragments from the article, which are provided in Table 2. The subcodes that were found in each article can be found in Table 1.
Several types of advantages were relevant for individual people who are in contact with the technology. Multiple articles mentioned the positive opinion about an eHealth intervention of people who were using or in direct contact with it. This opinion could entail positive attitudes, a high satisfaction or high acceptance of an eHealth intervention before, during or after its use. Studies also indicated that technology can increase patients’ access to care which makes it easier for them to receive treatment. This can be related to overcoming actual physical barriers to receiving care such as traveling distance, or access to care in highly secured settings. The subjective threshold to following treatment can be influenced by technology as well, for example, via privacy and anonymity, or the possibility of accessing an intervention from home and 24/7. Technology also offers new opportunities to involve loved ones in treatment. Another advantage is that technology can closely fit patients’ needs, preferences, and living environment. Patients can find specific technologies fun to use, e.g., serious games or VR, or technology can be developed in such a way that it is automatically tailored to specific characteristics. Also, compared with in-person treatment, technology is better able to create situations that are perceived as realistic and personally meaningful by patients.
Besides individual advantages, studies also described the added value that technology can have for forensic mental health. An important advantage is that eHealth interventions can be as effective as or even more effective than care as usual in reaching their intended goals. Included studies of a more observational nature indicated that the intervention they studied had a lot of potential to be effective, but no definite conclusions could be drawn based on their preliminary qualitative or quantitative results. The included experimental and quasi-experimental studies were able to provide some more insight into effectiveness, and reported mainly positive effects, as can be seen in Table 1. eHealth interventions can also increase the efficiency of forensic mental health care, which refers to practical advantages for forensic settings. Time and costs were claimed to be saved, for example, because eHealth can take away some of the work of therapists, an eHealth intervention can be quicker than in-person care, and many eHealth interventions are easily scalable, so multiple patients are able to follow an intervention at the same time without an increase of labor of care providers or a decrease in safety of patient, provider, or society. However, none of the studies that made statements about reduced costs and time conducted a systematic cost-effectiveness analysis. Studies also stated that eHealth technology can provide unique information that cannot or is difficult to elicit via in-person interventions. Technology was said to create situations with a high ecological validity, in which behavioral reactions can be observed and trained as they occur. Furthermore, it can be used to collect non-verbal information about physiological or unconscious reactions via the use of, e.g., biofeedback, eye-tracking, or measuring sexual arousal. A final advantage is related to fidelity: via technology, interventions can be delivered exactly as was intended, without error or unintended deviations from the desired situation. The standard procedures, structure, content, and evidence-based methods of an intervention can be delivered to patients in a standardized way, meaning that every patient gets the same treatment.
Disadvantages
Besides advantages, disadvantages were identified as well. They are mentioned and explained in the Table 3 and the accompanying text below.
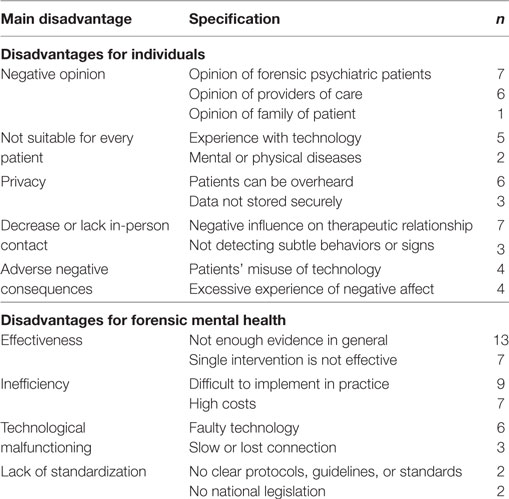
Table 3. Main and specified disadvantages of eHealth and amount of studies they were mentioned by (n).
Disadvantages for individual people were identified in the included studies. First of all, negative opinions of people directly involved with an eHealth intervention were reported. Studies found that attitudes about the technology were negative, or that the acceptance of a technology was low. It was also mentioned that not all technologies can be used by every type of patient, for example, if they have hallucinations or are physically incapable of using the system. Patients might also have low eHealth literacy because they lack knowledge and skills to use specific technologies, or they might be used to commercial products and are underwhelmed by an eHealth intervention. Another issue for individual patients is related to privacy and the confidentiality of sensitive information. Insecurely stored data can be accessed by unauthorized parties, or, especially in the case of communication technologies, patients might be overheard by staff or other patients. Furthermore, it was proposed that a decrease or lack of in-person contact between patient and therapist when using technology could have a negative impact on the therapeutic relationship, since both parties might perceive a greater emotional distance. Communication via technology can also make it harder or impossible to detect subtle but relevant behaviors or other signs such as fidgeting under the table or smell. eHealth interventions can also give rise to some adverse negative consequences: patients might misuse the technology, for example by using VR stimuli of children to arouse themselves, or technology can arouse excessive, unwanted negative affect in a patient.
eHealth can also have disadvantages for the domain of forensic mental health. The section on advantages already provided insight into the effectiveness of eHealth. However, studies also mentioned the lack of evidence of effectiveness, either for an entire domain, one intervention, or a specific outcome. Reviews often indicated that there is not enough evidence for a type of eHealth technology, for example, teleconferencing or VR. It was said that too little studies were conducted to make statements about their effectiveness. Besides these more general statements, some experimental studies also found that a single eHealth intervention was not effective in general, or on specific outcome measures. eHealth can also be inefficient when its development, implementation, or long-term use have practical negative consequences for an organization. Development, start-up costs, and maintenance of technology were often said to be costly, and insurance companies did not cover these costs. Also, several studies indicated that implementation in practice is difficult because of multiple reasons, such as unawareness of the existence of eHealth by stakeholders, too much reliance on the time and efforts of staff, or lack of physical space to set up a system. Furthermore, technological malfunctioning can negatively affect the quality of an eHealth intervention: software might contain bugs, equipment can fail, it can be too outdated to use, or the connection might be lost or be too slow. Finally, an observed disadvantage for eHealth is the lack of standardization: clear protocols, guidelines, and national legislation to optimize and standardize the use of eHealth in practice are insufficient or non-existent.
Combination of Results
Table 4 combines the results provided in Table 1 to create an overview of the study design, effectiveness, advantages, and disadvantages for each of the six identified types of technology.
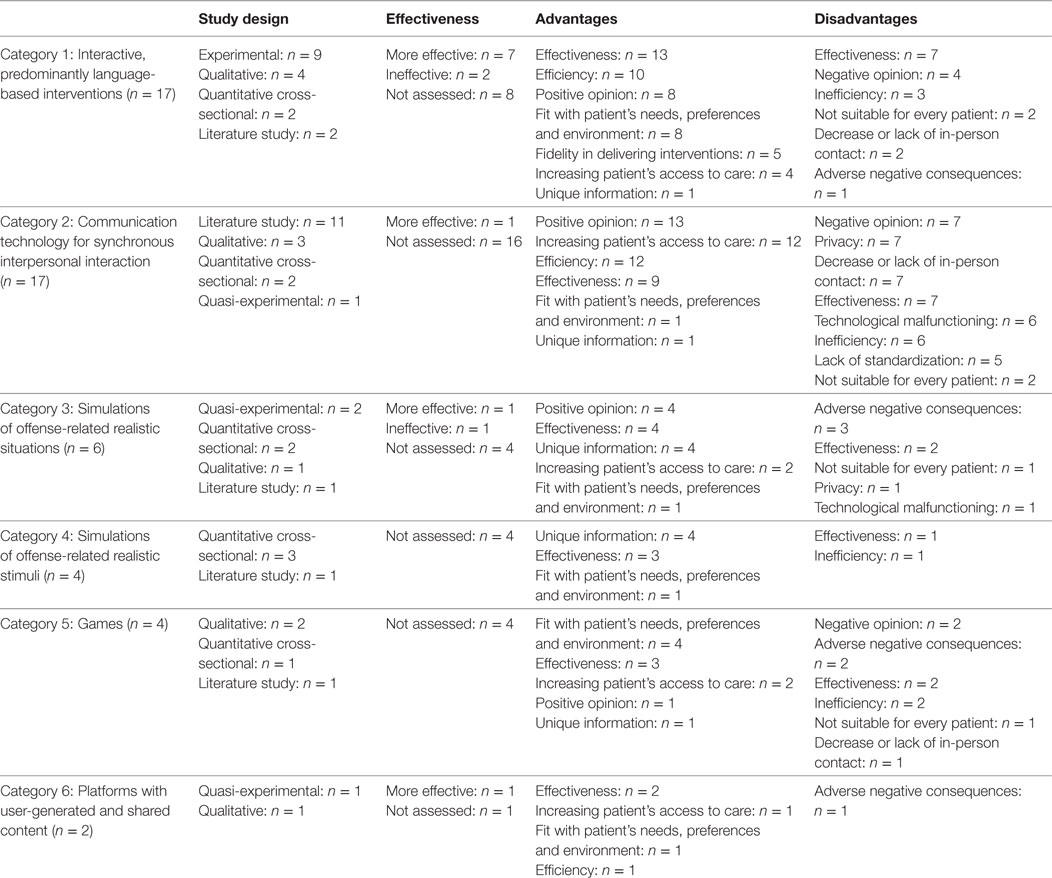
Table 4. Study design, effectiveness, advantages, and disadvantages categorized per type of technology.
The table shows that all experimental studies were conducted on interactive, language-based interventions, and most of these studies found that an eHealth intervention is as effective as or even more effective than a control intervention. Effectiveness was found most as both an advantage and disadvantage, and fidelity in delivering content and structure is mentioned only by these studies. The second category on teleconferencing contains almost all literature studies. These reviews mostly include studies on telepsychiatry in general, whereby the authors related their findings to forensic psychiatry. Opinions of individuals were found most in this category, as both an advantage and disadvantage. Compared with other categories, a lot of these studies paid attention to the increased access to care for patients. Technologies that simulate situations were studied in various ways. Overall, positive opinions and the unique possibilities of these interactive technologies were identified more often than in most other categories, just as the adverse negative consequences of a technology. No studies on effectiveness were conducted on technologies that simulated realistic stimuli, the fourth category. The possibility of technology to create and acquire unique information was acknowledged by all four included studies. The fifth category, games, also contains no studies on effectiveness. Most advantages and disadvantages were related to the individual patient, with all studies mentioning the advantage of the fit between the patient and the technology. The final category, platforms with user-generated content, comprises only two studies, of which one found evidence for effectiveness.
When looking at all mentioned advantages, effectiveness was stated in studies on all categories, just as the fit of the technology with the patient. However, efficiency was not identified in studies on technologies that simulated situations and stimuli, while the majority of these studies mentioned unique information as an advantage. Overall, less disadvantages then advantages were identified, so most of the disadvantages were stated only once or twice per type of technology. Effectiveness and adverse negative consequences are present in five categories, most other disadvantages are found in less categories. Finally, most of the mentioned disadvantages are complementary to the advantages, for example, both positive and negative opinions were identified in studies on teleconferencing, indicating that this is an important topic for studies on these types of technology.
Discussion
This systematic review provided an overview of the research on eHealth technologies that are used in the treatment of forensic psychiatric patients. The 50 included studies showed a broad range of eHealth technologies that were studied using different research methods, ranging from RCTs to exploratory qualitative studies. Most studies on effectiveness were conducted on language-based interventions, while most exploratory studies focused on technologies that provided an experience and made less use of language. Despite these differences, many publications mentioned the same type of advantages. The opinions of patients and therapists were positive, access to care was increased, the technology fitted the patient, interventions were—or were expected to be—effective and efficient, technology was said to increase fidelity of treatment, and offered new possibilities and information. Disadvantages were that not everyone was enthusiastic about and able to use technology, there were concerns about privacy, in-person contact could decrease, technology could have unintended negative consequences, not every study found strong proof of effectiveness and efficiency, technology could contain errors, and many settings did not have regulations or protocols for eHealth. When comparing the advantages to the disadvantages, it becomes clear that there is a lot of potential and much has been achieved at this point in time, but there are also many opportunities that are not used.
Important advantages of technology were related to technology being able to deal with the complex nature of the forensic psychiatric population. Technology can take the low literacy and education level of forensic psychiatric patients into account (15) by not relying primarily on language and cognitive reflection; it can create real-life, interactive situations in which skills can be trained (56, 70, 74, 77), or information on reactions can be gathered via physiological measures which can be integrated in treatment (27). However, most of these types of technologies are not thoroughly studied, so more studies on technologies such as VR or wearables that monitor arousal are required to determine whether they actually have added value for forensic psychiatric patients.
When looking at the use of technology in practice, many studies reported positive attitudes of both patients and care providers. A positive attitude increases the motivation to actually use a technology in the intended way (30). However, none of the studies paid attention to matters related to the use of technology such as engagement and adherence, despite the knowledge that treatment motivation and completion is low in forensic psychiatric patients (10). Research into the manner in which technology is used by patients and suitable methods to increase their engagement and adherence is required to gain more insight into how and why technology can motivate forensic patients. A way to increase adherence is via persuasive design (33, 34), which was recommended by one of the included studies (48). A specific persuasive element that multiple studies did mention as an advantage is tailoring (18, 27, 38, 40, 58). Tailoring has been recommended as a way to overcome the current predominant “one-size-fits-all” approach in forensic mental health by increasing the fit between the technology and the user (19, 51). Research has shown that tailoring is of added value for eHealth in general [e.g. Ref. (22)], but most interventions for forensic mental health did not use this specific possibility. To conclude, more research needs to be conducted on the interrelationships between technology and treatment motivation, and ways to increase engagement and adherence such as tailoring need to be identified.
Most included experimental and quasi-experimental studies found promising results for web-based interventions. In the majority of the included studies, web-based interventions were as effective as and, in some cases, more effective than in-person interventions. However, many technologies were not studied as extensively as this category, so to create a thorough evidence base for all categories, more evaluation studies are recommended (58, 60, 76). A more specific recommendation provided by several studies was to determine what types of interventions work best for which type of patients, and which mechanisms of change contribute to these differences between individuals (47, 48, 59, 76, 83). Insight in these mechanisms enables better tailoring of interventions to specific groups of patients. These kinds of recommendations are in line with recent visions on eHealth evaluations in general (85, 86), which stress the importance of determining what works best for whom to gain more insight into the working mechanisms.
A final advantage that was mentioned by several included studies is the possibility to incorporate existing guidelines and treatment approaches in eHealth interventions. Blended care, a format in which the use of eHealth is combined and integrated with in-person care, is an especially promising possibility (20). However, only one included study recommended that it should be examined how to best implement computer-delivered interventions in real world settings (48). Most studies did not pay attention to the implementation and integration of eHealth in existing care pathways. For eHealth to be as effective and efficient as possible, it needs to fit the context in which it is used seamlessly: technology should not be used as a separate, standalone tool, but has to be embedded within the current situation (87), among other things via integration in evidence-based treatment approaches such as cognitive behavior therapy and the risk-need-responsivity model. Especially studies on telepsychiatry stressed the need for protocols, standards, and guidelines to achieve this.
Based on the results of this review, it becomes clear that an issue important for eHealth in general also applies to forensic mental health: despite promising studies that show potential, there still is a large gap between potential and current practice, and most interventions fail to have actual clinical benefit in real world settings (86). To bridge this gap and achieve eHealth’s potential, it is essential to create a good fit between the technology, the people involved, and the existing context with its treatments approaches or interventions.
A way to increase the fit between technology, people, and their context is by conducting a good development process (88, 89). Not many of the included studies discussed the development of their interventions. The ones who did discuss it pointed out the importance of iterative development with continuous evaluation cycles (37, 53, 59) and the incorporation of opinions, preferences, and characteristics of people (37, 54, 57, 71, 81, 82). This is in line with recent insights into eHealth development, which state that a good development process requires iterative, evidence-based strategies that acknowledge the complex interrelations between people, technology, and the health-care context (85, 86). These strategies should be derived from multiple disciplines, such as persuasive design, human-centered design, participatory development, business modeling, engineering, and psychology (87). Interventions should not be developed in an expert-driven, non-iterative way (86), but this seemed to be the case for most of the included interventions. Also, due to a virtual absence of insight into the development process, little knowledge on the most optimal way to develop eHealth that fits with forensic mental health practice is present. Consequently, more studies on eHealth in forensic mental health should apply, describe, and critically evaluate development methods.
Implementation was another essential activity to which not much studies paid attention, despite the fact that research and practice have shown that it is a very important yet difficult endeavor (90). Some studies made recommendations for the implementation: they mentioned the necessity of accounting for resistance by patients and therapists, creating an infrastructure for dissemination, and financing (27, 42, 48, 53, 55). The importance of these kinds of activities has indeed been acknowledged by other studies and can be accounted for via using approaches such as business modeling (91) and participatory development (92).
Strengths and Limitations
The main strength of this study is that it used a systematic approach based on the Cochrane guidelines to provide a broad and extensive overview of the current state of research on eHealth interventions in forensic mental health. Despite the thorough execution of this review, it has several limitations. First of all, time between the development and evaluation of a technology and the publication of a study might take up to a couple of years (85), which causes that the most recent interventions and studies that are being conducted at the moment could not be accounted for in this review. Furthermore, because the goal of this systematic review was to provide an overview of the current state of affairs of research, all available studies were included, regardless of their quality and type of results. Consequently, not all results of included studies might be valid or reliable and thus it cannot be guaranteed that all advantages and disadvantages mentioned by these studies are factual and objective. Some advantages and disadvantages mentioned in the articles were based on qualitative results or non-systematic observations combined with reasoning based on existing literature. Again, more research is required to determine whether they can be objectively observed in forensic mental health care. We recommend that a systematic review specifically focused on effectiveness is executed in the near future, when more experimental studies on this increasingly studied topic have been published.
Conclusion
Based on the results of this review, we conclude that eHealth has many actual and potential advantages for forensic mental health. Some especially promising advantages are tailoring, effectiveness—which was mostly examined in web-based interventions—and, specifically relevant for non-language-based technologies, the acquisition of unique information via the use of technology. However, most interventions did not yet fully benefit from the possibilities of the different types of available technologies. To take eHealth in forensic mental health to the next level, it is important to ensure that the use of technology has actual added value for the patient and treatment. eHealth technology needs to be integrated in in-person treatment instead of using it as a separate addition to care, and it needs to closely fit the needs and preferences of both patients and therapists. Consequently, to achieve the benefits and overcome the barriers, eHealth should be developed in such a way that there is a good fit between technology, people, and the context.
Author Contributions
HK, YB, and SK designed the study and wrote the protocol. HK conducted literature searches. HK and SK screened the titles, while HK and YV screened the abstracts and analyzed the data. HK wrote the first draft of the manuscript and YB, SK, and LG-P contributed to and have approved the final manuscript.
Conflict of Interest Statement
All authors declare that they have no conflicts of interest. The reviewer ND and handling editor declared their shared affiliation.
Funding
Funding for this study was provided by Stichting Vrienden van Oldenkotte. They had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
References
1. Arboleda-Flórez J. Forensic psychiatry: contemporary scope, challenges and controversies. World Psychiatry (2006) 5(2):87–91.
3. Landenberger NA, Lipsey MW. The positive effects of cognitive-behavioral programs for offenders: a meta-analysis of factors associated with effective treatment. J Exp Criminol (2005) 1(4):451–76. doi:10.1007/s11292-005-3541-7
4. Andrews DA, Bonta J. Rehabilitating criminal justice policy and practice. Psychol Public Policy Law (2010) 16(1):39. doi:10.1037/a0018362
5. Babcock JC, Green CE, Robie C. Does batterers’ treatment work? A meta-analytic review of domestic violence treatment. Clin Psychol Rev (2004) 23(8):1023–53. doi:10.1016/j.cpr.2002.07.001
6. van Gemert-Pijnen JEWC, Kip H, Kelders SM, Sanderman R, Kelders SM, Kip H, et al. Introducing eHealth. In: van Gemert-Pijnen JEWC, editor. eHealth Research, Theory and Development: A Multi-Disciplinary Approach. Abingdon, UK: Routledge (Forthcoming).
7. Aardoom JJ, Dingemans AE, Van Furth EF. E-health interventions for eating disorders: emerging findings, issues, and opportunities. Curr Psychiatry Rep (2016) 18(4):1–8. doi:10.1007/s11920-016-0673-6
8. Huguet A, Rao S, McGrath PJ, Wozney L, Wheaton M, Conrod J, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One (2016) 11(5):e0154248. doi:10.1371/journal.pone.0154248
9. Morland LA, Greene CJ, Rosen CS, Kuhn E, Hoffman J, Sloan DM. Telehealth and eHealth interventions for posttraumatic stress disorder. Curr Opin Psychol (2016) 14:102–8. doi:10.1016/j.copsyc.2016.12.003
10. Drieschner KH, Boomsma A. The treatment motivation scales for forensic outpatient treatment (TMS-F) construction and psychometric evaluation. Assessment (2008) 15(2):224–41. doi:10.1177/1073191107311650
11. Perron BE, Bright CL. The influence of legal coercion on dropout from substance abuse treatment: results from a national survey. Drug Alcohol Depend (2008) 92(1–3):123–31. doi:10.1016/j.drugalcdep.2007.07.011
12. Bloem O, Bulten B, Nijman H. Psychopathologie onder gedetineerden. In: Groen NH editors. Handboek Forensische Geestelijke Gezondheidszorg. Utrecht: De Tijdstroom (2011). p. 153–62.
13. Goethals KR, Vorstenbosch ECW, van Marle HJC. Diagnostic comorbidity in psychotic offenders and their criminal history: a review of the literature. Int J Forensic Ment Health (2008) 7(2):147–56. doi:10.1080/14999013.2008.9914411
14. Tervoort MGA. Behandelbaarheid. In: Groen H, Drost M, Nijman HLI, editors. Handboek Forensische Geestelijke Gezondheidszorg. Utrecht: De Tijdstroom (2011). p. 137–52.
15. Greenberg E, Dunleavy E, Kutner M. Literacy Behind Bars: Results from the 2003 National Assessment of Adult Literacy Prison Survey. NCES 2007–473. Washington, DC: National Center for Education Statistics (2007).
16. Whitaker DJ, Morrison S, Lindquist C, Hawkins SR, O’Neil JA, Nesius AM, et al. A critical review of interventions for the primary prevention of perpetration of partner violence. Aggress Violent Behav (2006) 11(2):151–66. doi:10.1016/j.avb.2005.07.007
17. Birgden A. Therapeutic jurisprudence and responsivity: finding the will and the way in offender rehabilitation. Psychol Crime Law (2004) 10(3):283–95. doi:10.1080/10683160410001662771
18. Levesque DA, Johnson JL, Welch CA, Prochaska JM, Fernandez AC. Computer-tailored intervention for juvenile offenders. J Soc Work Pract Addict (2012) 12(4):391–411. doi:10.1080/1533256X.2012.728107
19. Polaschek DLL. Many sizes fit all: a preliminary framework for conceptualizing the development and provision of cognitive-behavioral rehabilitation programs for offenders. Aggress Violent Behav (2011) 16(1):20–35. doi:10.1016/j.avb.2010.10.002
20. Wentzel J, van der Vaart R, Bohlmeijer ET, van Gemert-Pijnen JEWC. Mixing online and face-to-face therapy: how to benefit from blended care in mental health care. JMIR Ment Health (2016) 3(1):e9. doi:10.2196/mental.4534
21. Oinas-Kukkonen H, Harjumaa M. Persuasive systems design: key issues, process model, and system features. Commun Assoc Info Syst (2009) 24(1):28.
22. Alley S, Jennings C, Plotnikoff RC, Vandelanotte C. Web-based video-coaching to assist an automated computer-tailored physical activity intervention for inactive adults: a randomized controlled trial. J Med Internet Res (2016) 18(8):e223. doi:10.2196/jmir.5664
23. Broekhuizen K, van Poppel MN, Koppes LL, Kindt I, Brug J, van Mechelen W. Can multiple lifestyle behaviours be improved in people with familial hypercholesterolemia? Results of a parallel randomised controlled trial. PLoS One (2012) 7(12):e50032. doi:10.1371/journal.pone.0050032
24. Brouwer W, Kroeze W, Crutzen R, de Nooijer J, de Vries NK, Brug J, et al. Which intervention characteristics are related to more exposure to Internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res (2011) 13(1):e2. doi:10.2196/jmir.1639
25. Lustria MLA, Cortese J, Noar SM, Glueckauf RL. Computer-tailored health interventions delivered over the web: review and analysis of key components. Patient Educ Couns (2009) 74(2):156–73. doi:10.1016/j.pec.2008.08.023
26. Schleg S, Bürger C, Schmidt L, Herbst N, Voderholzer U. The potential of technology-based psychological interventions for anorexia and bulimia nervosa: a systematic review and recommendations for future research. J Med Internet Res (2015) 17(3):e85. doi:10.2196/jmir.3554
27. Levesque DA, Ciavatta MM, Castle PH, Prochaska JM, Prochaska JO. Evaluation of a stage-based, computer-tailored adjunct to usual care for domestic violence offenders. Psychol Violence (2012) 2(4):368–84. doi:10.1037/a0027501
28. Hoogsteder LM, van Horn JE, Stams GJJ, Wissink IB, Hendriks J. The relationship between the level of program integrity and pre-and post-test changes of responsive-aggression regulation therapy (Re-ART) outpatient: a pilot study. Int J Offender Ther Comp Criminol (2016) 60(4):435–55. doi:10.1177/0306624X14554828
29. Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med (2011) 8(1):e1000387. doi:10.1371/journal.pmed.1000387
30. Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J, et al. eHealth for patient engagement: a systematic review. Front Psychol (2015) 6:2013. doi:10.3389/fpsyg.2015.02013
31. Bornkessel A, Furberg R, Lefebvre RC. Social media: opportunities for quality improvement and lessons for providers – a networked model for patient-centered care through digital engagement. Curr Cardiol Rep (2014) 16(7):1–9. doi:10.1007/s11886-014-0504-5
32. Crutzen R, Ruiter RA, de Vries NK. Can interest and enjoyment help to increase use of Internet-delivered interventions? Psychol Health (2014) 29(11):1227–44. doi:10.1080/08870446.2014.921300
33. Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res (2012) 14(6):e152. doi:10.2196/jmir.2104
34. Short CE, Rebar AL, Plotnikoff RC, Vandelanotte C. Designing engaging online behaviour change interventions: a proposed model of user engagement. Eur Health Psychol (2015) 17(1):32–8.
35. Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. (Vol. 4). Hoboken, NJ: John Wiley & Sons (2011).
36. Morrison LG, Yardley L, Powell J, Michie S. What design features are used in effective e-health interventions? A review using techniques from critical interpretive synthesis. Telemed E Health (2012) 18(2):137–44. doi:10.1089/tmj.2011.0062
37. Berman AH, Farzanfar R, Kristiansson M, Carlbring P, Friedman RH. Design and development of a telephone-linked care (TLC) system to reduce impulsivity among violent forensic outpatients and probationers. J Med Syst (2012) 36(3):1031–42. doi:10.1007/s10916-010-9565-1
38. Chaple M, Sacks S, McKendrick K, Marsch LA, Belenko S, Leukefeld C, et al. Feasibility of a computerized intervention for offenders with substance use disorders: a research note. J Exp Criminol (2014) 10(1):105–27. doi:10.1007/s11292-013-9187-y
39. Cunningham RM, Walton MA, Goldstein A, Chermack ST, Shope JT, Bingham CR, et al. Three-month follow-up of brief computerized and therapist interventions for alcohol and violence among teens. Acad Emerg Med (2009) 16(11):1193–207. doi:10.1111/j.1553-2712.2009.00513.x
40. Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham CR, Blow FC, et al. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics (2012) 129(6):1083–90. doi:10.1542/peds.2011-3419
41. Elison S, Weston S, Davies G, Dugdale S, Ward J. Findings from mixed-methods feasibility and effectiveness evaluations of the “breaking free online” treatment and recovery programme for substance misuse in prisons. Drugs Educ Prev Policy (2016) 23(2):176–85. doi:10.3109/09687637.2015.1090397
42. Lee JD, Tofighi B, McDonald R, Campbell A, Hu MC, Nunes E. Acceptability and effectiveness of a web-based psychosocial intervention among criminal justice involved adults. Health Justice (2017) 5(1):3. doi:10.1186/s40352-017-0048-z
43. Levesque DA, Driskell MM, Prochaska JM, Prochaska JO. Acceptability of a stage-matched expert system intervention for domestic violence offenders. Violence Vict (2008) 23(4):434–45. doi:10.1891/0886-6708.23.4.432
44. Neville FG, Goodall CA, Williams DJ, Donnelly PD. Violence brief interventions: a rapid review. Aggress Violent Behav (2014) 19(6):692–8. doi:10.1016/j.avb.2014.09.015
45. Spohr SA, Taxman FS, Walters ST. The relationship between electronic goal reminders and subsequent drug use and treatment initiation in a criminal justice setting. Addict Behav (2015) 51:51–6. doi:10.1016/j.addbeh.2015.07.005
46. Tait RJ, Lenton S. Online alcohol interventions, sexual violence and intimate partner violence: a systematic review. Internet Interv (2015) 2(2):152–60. doi:10.1016/j.invent.2015.03.001
47. Ranney ML, Goldstick J, Eisman A, Carter PM, Walton M, Cunningham RM. Effects of a brief ED-based alcohol and violence intervention on depressive symptoms. Gen Hosp Psychiatry (2017) 46:44–8. doi:10.1016/j.genhosppsych.2017.01.008
48. Walters ST, Ondersma SJ, Ingersoll KS, Rodriguez M, Lerch J, Rossheim ME, et al. MAPIT: development of a web-based intervention targeting substance abuse treatment in the criminal justice system. J Subst Abuse Treat (2014) 46(1):60–5. doi:10.1016/jjsat2013.07.003
49. Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA (2010) 304(5):527–35. doi:10.1001/jama.2010.1066
50. Wannachaiyakul S, Thapinta D, Sethabouppha H, Thungjaroenkul P, Likhitsathian S. Randomized controlled trial of computerized cognitive behavioral therapy program for adolescent offenders with depression. Pac Rim Int J Nurs Res (2017) 21(1):32–43.
51. Wilson HJ, Palk G, Sheehan MC, Wishart D, Watson B. Steering clear of driving after drinking: a tailored e-health intervention for reducing repeat offending and modifying alcohol use in a high-risk cohort. Int J Behav Med (2017) 24(5):694–702. doi:10.1007/s12529-017-9664-1
52. Absalom-Horby V, Hare DJ, Gooding P, Tarrier N. Attitudes of relatives and staff towards family intervention in forensic services using Q methodology. J Psychiatr Ment Health Nurs (2012) 19(2):162–73. doi:10.1111/j.1365-2850.2011.01770.x
53. Absalom-Hornby V, Gooding P, Tarrier N. Family intervention using a web camera (e-FFI) within forensic services: a case study and feasibility study. Br J Forensic Pract (2012) 14(1):60–71. doi:10.1108/14636641211204478
54. Adjorlolo S, Chan HC. Forensic assessment via videoconferencing: issues and practice considerations. J Forensic Psychol Pract (2015) 15(3):185–204. doi:10.1080/15228932.2015.1015363
55. Antonacci DJ, Bloch RM, Saeed SA, Yildirim Y, Talley J. Empirical evidence on the use and effectiveness of telepsychiatry via videoconferencing: implications for forensic and correctional psychiatry. Behav Sci Law (2008) 26(3):253–69. doi:10.1002/bsl.812
56. Ax RK, Fagan TJ, Magaletta PR, Morgan RD, Nussbaum D, White TW. Innovations in correctional assessment and treatment. Crim Justice Behav (2007) 34(7):893–905. doi:10.1177/0093854807301555
57. Batastini AB, McDonald BR, Morgan RD. Videotele conferencing in forensic and correctional practice. In: Myers K, Turvey CL, Myers K, Turvey CL, editors. Telemental Health: Clinical, Technical, and Administrative Foundations for Evidence-Based Practice. Amsterdam, Netherlands: Elsevier (2013). p. 251–71.
58. Batastini AB, King CM, Morgan RD, McDaniel B. Telepsychological services with criminal justice and substance abuse clients: a systematic review and meta-analysis. Psychol Serv (2016) 13(1):20–30. doi:10.1037/ser0000042
59. Brodey BB, Claypoole KH, Motto J, Arias RG, Goss R. Satisfaction of forensic psychiatric patients with remote telepsychiatric evaluation. Psychiatr Serv (2000) 51(10):1305–7. doi:10.1176/appi.ps.51.10.1305
60. Farabee D, Calhoun S, Veliz R. An experimental comparison of telepsychiatry and conventional psychiatry for parolees. Psychiatr Serv (2016) 67(5):562–5. doi:10.1176/appi.ps.201500025
61. Khalifa N, Saleem Y, Stankard P. The use of telepsychiatry within forensic practice: a literature review on the use of videolink. J Forens Psychiatry Psychol (2008) 19(1):2–13. doi:10.1080/14789940701560794
62. Manfredi L, Shupe J, Batki SL. Rural jail telepsychiatry: a pilot feasibility study. Telemed J E Health (2005) 11(5):574–7. doi:10.1089/tmj.2005.11.574
63. Miller TW, Clark J, Veltkamp LJ, Burton DC, Swope M. Teleconferencing model for forensic consultation, court testimony, and continuing education. Behav Sci Law (2008) 26(3):301–13. doi:10.1002/bsl.809
64. Miller TW, Burton DC, Hill K, Luftman G, Veltkemp LJ, Swope M. Telepsychiatry: critical dimensions for forensic services. J Am Acad Psychiatry Law (2005) 33(4):539–46.
65. Saleem Y, Taylor MH, Khalifa N. Forensic telepsychiatry in the United Kingdom. Behav Sci Law (2008) 26(3):333–44. doi:10.1002/bsl.810
66. Sales CP, McSweeney L, Saleem Y, Khalifa N. The use of telepsychiatry within forensic practice: a literature review on the use of videolink–a ten-year follow-up. J Forensic Psychiatr Psychol (2017) 28:1–16. doi:10.1080/14789949.2017.1396487
67. Sullivan DH, Chapman M, Mullen PE. Videoconferencing and forensic mental health in Australia. Behav Sci Law (2008) 26(3):323–31. doi:10.1002/bsl.815
68. Tucker W, Olfson M, Simring S, Goodman W, Bienenfeld S. A pilot survey of inmate preferences for on-site, visiting consultant, and telemedicine psychiatric services. CNS Spectr (2006) 11(10):783–7. doi:10.1017/S1092852900014905
69. Arborelius L, Fors U, Svensson AK, Sygel K, Kristiansson M. A new interactive computer simulation system for violence risk assessment of mentally disordered violent offenders. Crim Behav Ment Health (2013) 23(1):30–40. doi:10.1002/cbm.1849
70. Fromberger P, Jordan K, Müller JL. Anwendung virtueller Realitäten in der forensischen Psychiatrie. Ein neues Paradigma? = Use of virtual reality in forensic psychiatry. A new paradigm? Nervenarzt (2014) 85(3):298–303. doi:10.1007/s00115-013-3904-7
71. Hubal RC, Fishbein DH, Sheppard MS, Paschall MJ, Eldreth DL, Hyde CT. How do varied populations interact with embodied conversational agents? Findings from inner-city adolescents and prisoners. Comput Hum Behav (2008) 24(3):1104–38. doi:10.1016/j.chb.2007.03.010
72. Montgomery J, Brooks MH. Use of a television crime-drama series to promote legal understanding in mentally ill, incompetent defendants: a pilot study. J Forensic Sci (2005) 50(2):465–9. doi:10.1520/JFS2004050
73. Sygel K, Kristiansson M, Furberg R, Fors U. Reactions on display/intimate partner violence (ROD/IPV) – a study of a new interactive computer simulation program for the treatment of men convicted of intimate partner violence. Int J Forensic Ment Health (2014) 13(4):369–80. doi:10.1080/14999013.2014.951104
74. Wijk L, Edelbring S, Svensson AK, Karlgren K, Kristiansson M, Fors U. A pilot for a computer-based simulation system for risk estimation and treatment of mentally disordered offenders. Inform Health Soc Care (2009) 34(2):106–15. doi:10.1080/17538150903014395
75. Benbouriche M, Nolet K, Trottier D, Renaud P. Virtual reality applications in forensic psychiatry. Paper Presented at the Proceedings of the 2014 Virtual Reality International Conference. Laval, France (2014).
76. Dennis E, Rouleau JL, Renaud P, Nolet K, Saumur C. A pilot development of virtual stimuli depicting affective dispositions for penile plethysmography assessment of sex offenders. Can J Hum Sex (2014) 23(3):200–8. doi:10.3138/cjhs.2529
77. Renaud P, Trottier D, Rouleau JL, Goyette M, Saumur C, Boukhalfi T, et al. Using immersive virtual reality and anatomically correct computer-generated characters in the forensic assessment of deviant sexual preferences. Virtual Real (2014) 18(1):37–47. doi:10.1007/s10055-013-0235-8
78. Renaud P, Proulx J, Rouleau J, Bouchard S, Madrigrano G, Bradford J, et al. The recording of observational behaviors in virtual immersion: a new clinical tool to address the problem of sexual preferences with paraphiliacs. Annu Rev Cyberther Telemed (2005) 3:85–92.
79. Bacon N, Farnworth L, Boyd R. The use of the WII fit in forensic mental health: exercise for people at risk of obesity. Br J Occup Ther (2012) 75(2):61–8. doi:10.4276/030802212X13286281650992
80. Gooch P, Living R. The therapeutic use of videogames within secure forensic settings: a review of the literature and application to practice. Br J Occup Ther (2004) 67(8):332–40. doi:10.1177/030802260406700802
81. Hodge P, Davis J, Maiden N, Mann B, Nidsjo A, Simpson A, et al. StreetWise: a valid ecology for a serious game in a secure forensic mental health setting. Paper Presented at the Procedia Computer Science (2015) 63:252–9.
82. Reynolds LM, Davies JP, Mann B, Tulloch S, Nidsjo A, Hodge P, et al. StreetWise: developing a serious game to support forensic mental health service users’ preparation for discharge: a feasibility study. J Psychiatr Ment Health Nurs (2017) 24(4):185–93. doi:10.1111/jpm.12340
83. Kernsmith PD, Kernsmith RM. A safe place for predators: online treatment of recovering sex offenders. J Technol Hum Serv (2008) 26(2–4):223–38. doi:10.1080/15228830802096598
84. Van Gelder JL, Luciano EC, Weulen Kranenbarg M, Hershfield HE. Friends with my future self: longitudinal vividness intervention reduces delinquency. Criminology (2015) 53(2):158–79. doi:10.1111/1745-9125.12064
85. Hekler EB, Klasnja P, Riley WT, Buman MP, Huberty J, Rivera DE, et al. Agile science: creating useful products for behavior change in the real world. Transl Behav Med (2016) 6(2):317–28. doi:10.1007/s13142-016-0395-7
86. Patrick K, Hekler EB, Estrin D, Mohr DC, Riper H, Crane D, et al. The pace of technologic change: implications for digital health behavior intervention research. Am J Prev Med (2016) 51(5):816–24. doi:10.1016/j.amepre.2016.05.001
87. van Gemert-Pijnen J, Peters O, Ossebaard HC. Improving eHealth. Den Haag, Netherlands: Eleven International Publishing (2013).
88. Kushniruk AW, Bates DW, Bainbridge M, Househ MS, Borycki EM. National efforts to improve health information system safety in Canada, the United States of America and England. Int J Med Inform (2013) 82(5):e149–60. doi:10.1016/j.ijmedinf.2012.12.006
89. van Gemert-Pijnen JE, Nijland N, van Limburg M, Ossebaard HC, Kelders SM, Eysenbach G, et al. A holistic framework to improve the uptake and impact of eHealth technologies. J Med Internet Res (2011) 13(4):e111. doi:10.2196/jmir.1672
90. WHO Regional Office for Europe. From Innovation to Implementation. eHealth in the WHO European Region. Copenhagen: Publications WHO Regional Office for Europe (2016).
91. van Limburg M, Wentzel J, Sanderman R, van Gemert-Pijnen L. Business modeling to implement an eHealth portal for infection control: a reflection on co-creation with stakeholders. JMIR Res Protoc (2015) 4(3):e104. doi:10.2196/resprot.4519
92. Beerlage-de Jong N, Wentzel J, Hendrix R, van Gemert-Pijnen L. The value of participatory development to support antimicrobial stewardship with a clinical decision support system. Am J Infect Control (2017) 45(4):365–71. doi:10.1016/j.ajic.2016.12.001
Appendix
A. Full Electronic Search Strategy
Search string #1 on treatments in forensic mental health settings
forensic
violen*
crim*
delinquen*
offend*
maximum secur*
W/3
treatment*
psychiatr*
patient*
setting*
assessment*
diagno*
rehabilitation
parole
probation
therap*
coach*
intervention*
Search string #2 on technology
E-Health
eHealth
M-Health
mHealth
technolog*
device*
platform*
videoc*
tele*
mobile
*phone
SMS;
web*
“virtual Reality”
virtual
“augmented reality”
wearable*
smart*watch*
game*
online
computer
Keywords: eHealth, interventions, technology, forensic psychiatry, offenders
Citation: Kip H, Bouman YHA, Kelders SM and van Gemert-Pijnen JEWC (2018) eHealth in Treatment of Offenders in Forensic Mental Health: A Review of the Current State. Front. Psychiatry 9:42. doi: 10.3389/fpsyt.2018.00042
Received: 19 October 2017; Accepted: 31 January 2018;
Published: 21 February 2018
Edited by:
Katarina Howner, Karolinska Institute (KI), SwedenReviewed by:
Nubia G. Lluberes, Baylor College of Medicine, United StatesNatalie Durbeej, Karolinska Institute (KI), Sweden
Copyright: © 2018 Kip, Bouman, Kelders and van Gemert-Pijnen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hanneke Kip, aC5raXBAdXR3ZW50ZS5ubA==
 Hanneke Kip
Hanneke Kip Yvonne H. A. Bouman2
Yvonne H. A. Bouman2 Saskia M. Kelders
Saskia M. Kelders