- 1LandesEnergieAgentur Hessen, Wiesbaden, Germany
- 2GESIS Leibniz-Institute for the Social Sciences, Department Survey Data Curation, Cologne, Germany
Medical treatments at the beginning and end of human life are highly contested in public discourse. Our study reveals factors shaping the acceptance of social egg freezing (or oocyte cryopreservation) as an assisted reproduction technology (ART) in the general public. Based on the theory of moral contextualism and the literature on medical ethics, we deduce potential factors influencing attitudes toward cryopreservation (for example, the number of oocytes used or the age up to which women plan to use the oocytes). The influence of these factors on individual attitudes is modeled using a factorial design embedded into a web survey. The results show that factors associated with potential harm to the children decrease acceptance of cryopreservation, whereas factors associated with potential harm to the women increase acceptance. The strongest effect has the age at which women plan to use the preserved oocytes.
Introduction
According to a well-known saying, it is never the right time to have a child. Many people, therefore, decide to postpone childbearing despite the risk of declining fertility. The average age of women at first birth continues to increase in wealthy societies. Late childbearing carries the risk of involuntary childlessness for women because fertility strongly declines after age 30 (Wennberg, 2020). Over the last decade, the preventive preservation of women's oocytes has received significant public attention as a possible way for women to extend fertility. Human oocyte cryopreservation was developed to preserve women's fertility threatened by chemotherapy or radiotherapy. The procedure starts with a hormonal ovarian stimulation to collect oocytes from the women. The eggs are then vitrified and can be stored frozen for a long time. For use, the eggs are thawed and fertilized in-vitro before being transfered into the woman's uterus (Walker et al., 2022).
The original limitation of oocyte cryopreservation to medical indications was gradually abandoned in medical practice (Pai et al., 2021). Now, it is used to extend the female fertility span for non-medical reasons, for example, if women lack a partner for childbearing or wish to postpone family formation. Social freezing refers to the use of oocyte cryopreservation for these non-medical motives. The medical literature often uses more neutral terms to describe the practice, e.g., elective (Nasab et al., 2020; Pennings, 2021), non-medical (REF) or planed oocyte cryopreservation (Cremonese et al., 2022).
The rise of oocyte cryopreservation led to controversial scholarly and public discussions about moral and ethical concerns. Some scholars regret that social egg freezing nudges women to adapt their reproductive behavior to the expectations of the neoliberal economy (especially because large U.S. corporations announced to cover the cost of cryopreservation for their employees) instead of adapting the economy to the needs of the women (Bozzaro, 2018). Others stress women's gains in reproductive autonomy (Wennberg, 2020). From a medical ethics perspective, the discussion mostly concerns the success rates for giving live birth from a preserved oocyte, open questions regarding the use of oocytes not used for birth giving, or the cost-effectiveness of the treatments (for a recent overview, see Varlas et al., 2021). From a social science perspective, the discussion about moral implications is broader. Existing research has shown that primarily highly educated wealthy women use social egg freezing because they do not have an appropriate partner for family formation (Baldwin et al., 2014, 2019). Most of the available literature on attitudes toward social freezing focuses on women's disposition to use oocyte cryopreservation (Platts et al., 2021). Less is known about public attitudes toward social egg freezing. This is probably due to the difficulty of including questions on highly specialized medical topics in representative survey studies. We argue that social acceptance is a significant factor in the successful use of cryopreservation because women thinking about or using this technical assistance will be confronted with opinions from their social networks. Recent evidence has shown that the approval of social freezing in social networks increases women's disposition to use it (Caughey and White, 2021).
Existing studies from medical ethics show that acceptance of oocyte cryopreservation is almost universal if used for medical indications but significantly lower for social motivations (Lallemant et al., 2015; Lewis et al., 2016; Wennberg et al., 2016). Although medical professionals tend to support its use for fertility preservation (Goold and Savulescu, 2009; Goldman and Grifo, 2016), social egg-freezing remains contested in public discourses and attitudes (Platts et al., 2021). More in-depth analysis of the reasoning about social freezing revealed a tension between the reproductive autonomy of women and concerns about medical interventions into procreation (Kostenzer et al., 2021). Existing studies also yielded that public attitudes depend on the specific settings of its use: the duration of oocyte preservation (Wennberg et al., 2016) or women's motives for cryopreservation (Lallemant et al., 2015). A systematic study of how the specific settings of the use of social egg freezing influences attitudes and how this interacts with individuals' attributes has not been published yet. Our study fills this gap in the literature.
Moreover, the attitudes correlate with the socio-demographic characteristics of individuals. In particular, older and more religious individuals show lower acceptance of cryopreservation without medical indications (Lewis et al., 2016). No studies have been published on factors influencing attitudes of the general public toward social freezing in Germany. Germany is interesting because the conservative welfare and gender regime produce strongly gendered reproductive norms and behaviors. Despite the claims for growing gender equality, women continue to bear a large part of the childcare work (Neilson and Stanfors, 2014). Traditional gender roles perpetuate gender inequalities by attributing the primary responsibility for childcare to women. Among German women, the belief is widespread that mothers provide better childcare than institutional facilities. Therefore, they feel they must choose between working or childbearing (Rossier et al., 2011). The moral attitudes toward how women use social freezing in Germany are embedded into this traditional family and gender regimes in Germany. We can assume that the public attributes the responsibility for childrens' wellbeing to the (potential) mothers. This responsibility includes the prevention of potential harms to the (unborn) children.
The responsibility for harm is central to our analytical approach to moral attitudes. We argue that attitudes toward social freezing result from individuals' balancing cryopreservation's potential benefits and harms. Thus, attitudes toward cryopreservation depend on how and why it is used and what the perceived consequences are. We address the following two research questions. What factors in the use of oocyte cryopreservation for non-medical indications influence public acceptance? And what social characteristics of individuals are associated with acceptance of cryopreservation?
Our study reveals the mechanisms of moral attitude formation on cryopreservation as a contested form of ART. We show how specific value orientations and moral principles interact with the specific circumstances in the use of cryopreservation when shaping attitudes. Using a factorial survey as an innovative method to assess attitude formation, we embed a quasi-experimental design into a cross-sectional online survey. The factorial survey consists of short descriptions (vignettes) of women that freeze their oocytes to delay childbearing. The descriptions contain a controlled variation of factors expected to influence attitudes. These factors correspond to the experimental treatments. Because the participants' ratings directly respond to this controlled stimulus, a causal interpretation of effects from the vignette factors is possible (Dülmer, 2014a). Therefore, this method allows us to reveal the mechanisms relating specific circumstances in the use of cryopreservation to individuals' attitudes.
The paper is organized as follows: We will first present the study's theoretical background and deduce hypotheses from the general framework of moral contextualism. The Section Theoretical background and research hypotheses describes the data and the methods used for empirical analysis. The Section Materials and methods describes the results from the multilevel regression models, and the Section Results discusses the overall results. The paper concludes with recommendations for future research on public attitudes toward cryopreservation.
Theoretical background and research hypotheses
We argue that attitudes toward cryopreservation are not exclusively influenced by considering medical risks and success rates. Rather attitude formation is based on moral considerations and value orientations embedded into general normative frames of individuals. Cross-national studies in sociology have revealed that in contemporary European societies, moral contextualism has become the dominant normative frame for individuals' moral attitudes Dülmer, 2014b; Nunner-Winkler, 2020).
Moral contextualism is best understood by comparing it to moral universalism prevailing in societies where religion is the primary source of morality. Judgments of medical practices and other behaviors depend on religious conceptions of “good” and “bad” set by the church as a moral authority (see Nunner-Winkler, 1997). As long as individuals act according to the moral rules, they are not accountable for the consequences of their behavior. Things happen depending on God's will. Kant's famous example that lying to a murderer is never justifiable (because lying is intrinsically wrong), even if this would save the victim's life, best illustrates the universalist position (Nunner-Winkler, 1997).
In contrast, moral contextualism means that universal rules have the status of prima facie rules wherein they are valid (“you should not harm others”). But moral judgements consider the consequences of behaviors (Dülmer, 2014b). Individuals evaluate the outcomes of behaviors according to the fundamental moral principle of harm avoidance (Nunner-Winkler, 1997). Regarding Kant's example, this means that individuals informing the murderer about the hideout of the victim are partly accountable for the homicide because lying to the murderer is morally acceptable to save human life. Nunner-Winkler summarizes: “A morality that is not derived from God's word but from universally shared human interests can be agreed upon by men of different historical and religious traditions. […] it fulfills the core functions of non-violent conflict regulation and harm minimization” (Nunner-Winkler, 2020, p. 184). Thus, the growth of moral contextualism is driven by continuing secularization in Europe, which leads to the decline of religious morality (Halman and van Ingen, 2015).
Emphasizing the consequences of behaviors with an emphasis on harm minimization has several implications for studying attitudes. First, behaviors harming others for egoistic reasons are unacceptable independently of a universal or contextual moral frame (Dülmer, 2014b; Storm, 2016). Second, behaviors not harming others will be accepted because there are no reasons for condemning them. Third, for attitude formation, individuals balance the potential benefits and harms they perceive related to individual actions or medical technologies. For example, acceptance of euthanasia is higher if requested by a patient suffering from severe pain compared to a patient not suffering from pain because relief from pain is perceived as a benefit of euthanasia (Park and Clery, 2008). Similarly, acceptance of abortion is higher if the pregnancy involves particular medical risks for the mother (Hans and Kimberly, 2014).
We expect that moral contextualism also shapes attitudes toward cryopreservation. If this is the case, individuals would not consider medical technologies to be intrinsically right or wrong. Instead, the moral evaluation depends on the perceived consequences for the women using it and the (un)born children resulting from cryopreservation. This explains why acceptance of oocyte cryopreservation is almost universal for medical indications (e.g., to preserve fertility after cancer treatment).
The objective of cryopreservation is to avoid suffering from involuntary childlessness by widening the fertility span. Therefore, it is not surprising that the dominant view in medical ethics is positive because success rates of subsequent IVF are similar to those without prior cryopreservation (Goold and Savulescu, 2009; Goldman and Grifo, 2016; Walker et al., 2022). In line with moral contextualism, individuals will be more likely to accept cryopreservation for women that would suffer more from involuntary childlessness. Therefore, we expect acceptance of cryopreservation to be higher for women who suffer more from involuntary childlessness (for example, because they have a very strong desire to bear a child; Hypothesis 1).
Medical ethics focus on potential risks of treatments. From this perspective, the higher the success rates of subsequent IVF are, the more acceptable is cryopreservation. One factor influencing the success of IVF is the woman's age when preserving oocytes. Generally, the success rates are higher if women use cryopreservation before fertility declines (Lockwood, 2011; Goldman and Grifo, 2016; Teo et al., 2022). If there is awareness about age-related fertility decline in the general population (Vassard et al., 2016), higher age of women at cryopreservation will trigger the potential harms for women related to the hormonal treatment for collecting the oocytes and the subsequent IVF. Therefore, higher age at cryopreservation is expected to decrease acceptance (Hypothesis 2).
According to moral contextualism, attitudes also depend on the potential harm for children born from IVF after cryopreservation. The literature reveals that the age of women using their preserved oocytes is discussed with respect to consequences for the children. Proponents of cryopreservation argue that the capacity of women to carry children is not limited by menopause. Therefore, cryopreservation is a way to achieve reproductive autonomy (Savulescu and Goold, 2008; Goold and Savulescu, 2009). Critics of this position emphasize that delayed childbearing potentially harms children. For example, there is a discussion about the inferior health outcomes of children born to older mothers (Barclay and Myrskylä, 2016). Moreover, older parents might lack the physical ability to raise children appropriately (Nasab et al., 2020), and delayed childbearing challenges traditional family forms. The conservative welfare regime in Germany supports a model where parents care for children at younger ages and children care for older parents (Goold and Savulescu, 2009). In Germany, health insurances cover the costs for IVF only for married women younger 40.
The actual consequences of late parenthood on children's welfare are discussed in the literature (Sutcliffe et al., 2012), and some countries enacted age limits for accessing ART (Kocourková et al., 2015; Wennberg, 2020). Survey studies yielded a social norm expecting women to bear children before age 40 (Billari et al., 2011). Therefore, the use of cryopreservation conflicts with the social reprobation of delayed childbearing for children's wellbeing. Higher age also increases the health risk of pregnancy and giving birth (Lampinen et al., 2009) which might foster more skeptical attitudes toward late childbearing. In our study, the crucial question is whether the public perceives late parenthood as potential harm to children and mothers. If this is the case, the acceptance of cryopreservation will be lower for women who plan to use their preserved oocytes at later ages (Hypothesis 3).
Another ethical controversy concerns the number of oocytes collected for cryopreservation. The chances of a living birth are higher if more oocytes are preserved because more IVF cycles may be performed. This involves the possibility that surplus oocytes are discarded after successful IVF. In fact, most vitrified oocytes are not used for IVF (Walker et al., 2022). The pro-life position, advocated by Christian churches, considers the destruction of oocytes as harming the unborn life and thus not justifiable (Sallam and Sallam, 2016).
Nevertheless, voluntary egg donation is an alternative usage for frozen oocytes (Tozzo, 2021). It is a pathway to avoid involuntary childlessness for women without their own eggs. It is important to note that whereas the donation of semen is legal in Germany, the donation of oocytes is not. Hence there is no alternative use for cryopreserved oocytes (Gianaroli et al., 2016). If the concern about surplus oocytes influences attitudes, acceptance should decrease with the number of preserved oocytes (Hypothesis 4).
Finally, the public debate about social freezing focuses on economic constraints on women's reproductive choices. Postponing childbearing using oocyte cryopreservation allows women not to jeopardize their professional development by taking maternity leave (Lallemant et al., 2015). The concern was that business corporations persuade women to put their own advancement above the wellbeing of the unborn child. Studies on users of cryopreservation revealed that career advancement is among the least cited motives for the treatment but among the most frequently cited motives in studies from the general public (Platts et al., 2021). This finding suggests that economic motives dominate the public reasoning about social freezing much more than its use.
Moral contextualism assumes that exposing others to health risks for egoistic motives is unacceptable. However, postponing parenthood for career reasons is considered an egoistic motivation in Germany (Haker, 2016), mirroring Germany's traditional gender regime where women are considered responsible for child care. Less materialistic motives might also be perceived as egoistic, such as women's wishes for self-realization before motherhood. We expect that motives perceived as egoistic will lower acceptance of social freezing (Hypothesis 5).
Although the lack of a partner is the most important reason for using cryopreservation (Baldwin et al., 2015; Jones et al., 2020; Pennings, 2021; Platts et al., 2021), we do not consider it as a factor predicting attitudes in our study. As Pennings (2021) underscores, the lack of a partner is a demographic phenomenon because many highly educated women will not find a suitable partner. From a perspective of moral sociology, there is no potential harm from the partnership status at the time of preservation. Partnership and marital status are more important for attitudes toward the use of preserved oocytes for IVF and are less important for the decision to preserve oocytes. Some countries, for example, restrict access to IVF to married and/or different-sex couples (Gianaroli et al., 2016). Modeling these options would excessively complicate the empirical analysis. By focusing on attitudes toward decisions of single women, our results are closest to the real-world situations that women experience and, thus, most useful for transfer into medical counseling. This said it is important to bear in mind that there are many more motives for using cryopreservation that are not covered in the experimental part of our study. The present study, however, is not about women's decision-making but the public moral judgements of hypothetical behaviors.
Besides moral contextualism, an individual's value orientations influence attitudes. Religious value orientations are associated with lower levels of acceptance (Lewis et al., 2016) because Christian churches in Europe reject procedures that potentially harm unborn life, in particular the destruction of oocytes, zygotes or embryos. In addition, they object to the separation of sexuality and reproduction (Sallam and Sallam, 2016). If religious people are obedient to the church as a moral authority, they should consistently reject cryopreservation (Hypothesis 6).
In contrast to religious values, self-expression values emphasize an individual's autonomy in life choices (Welzel, 2013). The idea of reproductive autonomy and any means to realize it—such as the use of cryopreservation—is fully compatible with this value orientation. Therefore, we expect that self-expression values are associated with higher acceptance levels (Hypothesis 7).
Lastly, we expect individuals who have a normative preference against late parenthood to be less accepting of cryopreservation since they have concerns about the wellbeing of children (Hypothesis 8). The normative preference against late parenthood might shape how the age of women using preserved oocytes influences individual attitudes (see Hypothesis 5). A strong normative preference against late parenthood will lead to a stronger rejection of women using cryopreserved oocytes later. In contrast, for individuals who are tolerant of late parenthood, we do not expect the age at using cryopreserved oocytes to reduce acceptance (Hypothesis 9).
Materials and methods
The factorial survey
We used a factorial survey (Auspurg and Hinz, 2015) as an innovative method to study the circumstances of oocyte cryopreservation that influence an individual's acceptance. Due to the controlled variation of the treatments and the evaluation of more than one vignette per participant, the effects are unbiased (Auspurg and Hinz, 2015). Moreover, Auspurg and Hinz showed that the multidimensionality of factorial surveys protects against biases due to socially accepted responses (Auspurg et al., 2014; Auspurg and Hinz, 2015).
Every participant rates several vignettes that contain short texts describing different women using cryopreservation to preserve fertility. The vignettes systematically vary with respect to the circumstances (i.e., factors) we expect to influence acceptance. Therefore, each vignette describes a different situation. The descriptions are colloquial, avoiding medical terminology (see Figure 1). An introductory text states that all women are healthy and completely aware of the procedure and that there are no medical objections to either cryopreservation or later IVF. Moreover, the introduction (see Appendix 2) describes cryopreservation as reproductive technology. Thus, all participants have the same information about the procedure (i.e., that egg cells are collected and vitrified, IVF is performed after warming the cells, and surplus eggs are destroyed if they are not needed).
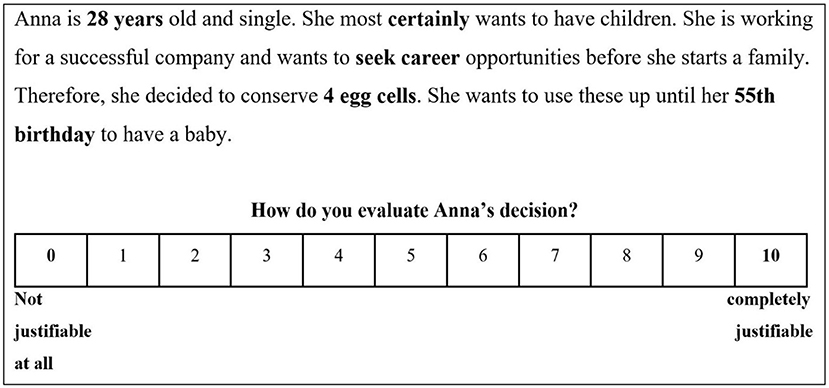
Figure 1. Sample vignette from the factorial design. The elements that change across vignettes are printed in bold. The original questionnaire was in German.
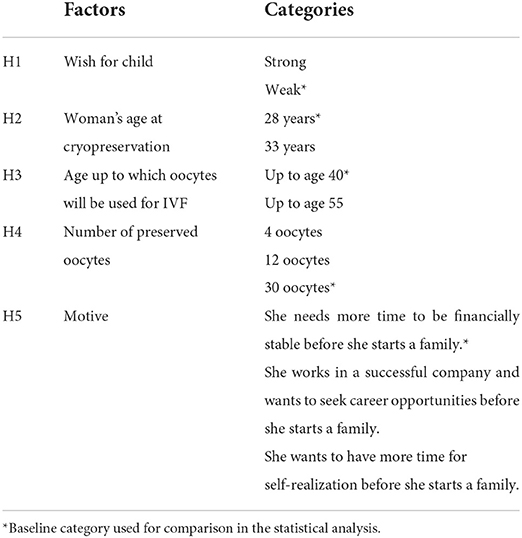
We defined one vignette factor for each of the five circumstances we expect to influence attitudes toward cryopreservation. We selected the different categories of the factors to accentuate the conflict between benefits and harms without becoming unrealistic when combined into a single vignette.
First, the potential harm of suffering from involuntary childlessness was modeled by the strength of the wish for a child. We compared a woman who is unsure whether she wants to have a child to a woman who is sure about her desire.
The second factor is the woman's age at cryopreservation. The baseline category for this dimension is a woman at age 28 when the probability of subfertility remains low and the average quality of the oocytes is high. This increases the likelihood of a successful IVF later on. The second value is age 33 when a decline in fertility has started (Johnson and Tough, 2012).
The third factor is age up to which women plan to use preserved oocytes for IVF. It models potential risks for mothers and children due to late pregnancy and childbearing. The baseline category is age 40 since this is, on average, the acceptable age limit perceived by the general public for motherhood in Europe (Billari et al., 2011). Thus, it should not raise concerns compared to a woman who plans to use the preserved oocytes up to 55. At this age, a natural conception is virtually impossible.
The fourth factor models the potential harm to unborn life as the number of preserved oocytes. The baseline category here is 30. If pro-life arguments are relevant for individual attitude formation, a high number of oocytes should reduce acceptance of cryopreservation because it increases the probability that surplus oocytes will be discarded. Situations where 12 and 4 oocytes are preserved, are compared to the baseline category.
Finally, the fifth factor is the woman's motive for preserving oocytes. We distinguish three different motives. The baseline category is a woman who wants to reach financial stability for her family before having a child. This motive is not considered egoistic because material security is important in ensuring children's wellbeing. Other motives represent more egoistic orientations when other life goals such as career and self-realization are preferred over childbearing.
Table 1 summarizes the five factors modeled in the vignettes and all categories associated with those factors.
All women described in the vignettes are without a partner, so questions of partnership status and marital status do not confound acceptance. Figure 1 shows a sample vignette. Participants rated the vignettes on an 11-point scale, ranging from 0 = not justifiable at all to 10 = completely justifiable.
This scale is well-established in international survey programmes (e.g., the questionnaire of the European Values Study).
The total number of possible combinations of the five vignette factors is (2*2*2*3*3) 72. Beck and Opp suggest that participants should not rate more than 20 vignettes (Beck and Opp, 2001). Therefore, it is necessary to draw a sample that preserves the characteristics of the full factorial design (Dülmer, 2015): the factors are uncorrelated (i.e., orthogonality), and the categories occur with the same frequency (i.e., the design is balanced). A balanced design maximizes the precision of parameter estimates due to maximum variance within each factor (Auspurg and Hinz, 2015). Due to the orthogonality of the factors, unobserved heterogeneity is excluded by design in the factorial part of our data analysis. We used D-efficiency as a measure for selecting an appropriate number of vignettes (Auspurg and Hinz, 2015; Dülmer, 2015). The highest D-efficiency (=98.3995) was reached with a sample of 12 vignettes. Every participant rated the same 12 vignettes. The order of the vignettes was randomized in the survey. For the regression models, we transformed all factors into dummy variables.
Operationalization of the social factors
We also considered the characteristics of the individuals in the data analysis. The question wordings for all independent variables can be found in Appendix 3. Religiousness (Hypothesis 6) is measured by the frequency of church attendance (or mosque or synagogue attendance for Muslims and Jewish people, respectively). Answers range from 0 = no attendance to 5 = at least weekly attendance (M = 1.07, SD = 1.07).
Participants' self-expression values (Hypothesis 7) are measured according to Welzel (2010). The index includes the following three dimensions: post-traditional morality (i.e., the acceptance of abortion, divorce, and homosexuality), attitudes toward gender equality (in terms of family income, parenting, and domestic work) and priority for autonomy in education. This last dimension is operationalized using a question on preferences for educational goals. A composite score is computed from the three subscales with a range from 0 = “low on self-expression values” to 3 = “high on self-expression values” (M = 2.5069, SD = 0.34).
Another individual factor is the normative preference against late motherhood (Hypothesis 8). We used a simple measure adapted from the European Social Survey that asks participants at which age they consider women too old to bear a child (see also Billari et al., 2011). Answers ranged from 31 years to 75 years (M = 45.34, SD = 5.53). Eventually, we included participants' sex (69% women) and age (min. = 15, max. = 87, M = 39.9 SD = 14.54) as control variables in the regression analysis.
Data collection
We collected data from 775 German-speaking people older than 18 from a non-commercial non-probability online access panel in Germany. The panel was an actively managed data collection infrastructure accessible free of charge after a positive peer-review of the research design. Participants self-selected into the panel via social media postings and mailings. Registration and participation in the panel are free and participants did not receive incentives for participating in our study. The sample is not representative of the German population. There are more women (69% women), higher educated (56% completed tertiary education), and younger (mean of 40 years) persons in the sample than the general population in Germany (51% women; mean age 44 years; 21% completed tertiary education)1. Therefore, the overall level of acceptance of cryopreservation should not be generalized. Due to the quasi-experimental nature of the factorial survey, the effects found for the vignette part of the study are unlikely to be biased. The advantage of the panel we used is that there is significant variation in the demographic characteristics of participants, covering a large age span and different educational and religious backgrounds. Therefore, we argue that the data give a more reliable assessment of public opinion toward cryopreservation than samples recruited from websites specialized in ART topics or at ART centers. Moreover, the controlled variation of the vignette factors ensures a high internal validity of the design, which allows for a causal interpretation of the vignette factor estimates without assuming that the estimates are equal in a random sample.
Seven hundred and forty nine survey participants rated at least one vignette, and 731 participants rated all 12 vignettes. The 26 people who did not rate any vignette were removed from the analysis. In all, 727 participants completed the questionnaire. After the list-wise deletion of missing values on individual-level variables, data from 596 participants were analyzed. The data for this study are freely available for replication or reuse (Forke, 2016).
Statistical analysis
Because each participant rated 12 vignettes, the dataset is hierarchically structured. The vignette ratings are the first level nested in participants (i.e., the second level). Therefore, multilevel regression analysis (MLA) is the appropriate method for simultaneously analyzing variation within (explained by vignette factors) and between (participants' characteristics) participants (Snijders and Bosker, 1999).
Moreover, MLA allows for estimating how participants' characteristics moderate the effects of the vignette factors (cross-level interaction effects). An appropriate model specification requires testing whether the effects of vignette factors have significant variance across study participants (Dülmer, 2015). To test this, we used the likelihood ratio tests. All analyses were performed with STATA 13.
Results
Our data suggest that most survey participants are aware of some ARTs. All participants in our sample had previously heard of IVF, and only 4% had never heard of social freezing before.
Figure 2 shows that cryopreservation for social indications is highly controversial in the sample. Approximately 15% of the vignettes have been rated as “always justifiable,” and 12% have been rated as “never justifiable.” Each intermediate category gathers 6–9% of the ratings. Of the 731 participants who rated all 12 vignettes, 40 consistently rated all vignettes with the lowest (rejecting cryopreservation) and 44 with the highest (accepting cryopreservation) values. Most participants (604) varied their ratings. Eighteen participants did not rate all vignettes but at least one. The mean rating of the vignettes was 5.14 (SD = 3.4), which is very close to the scale midpoint.
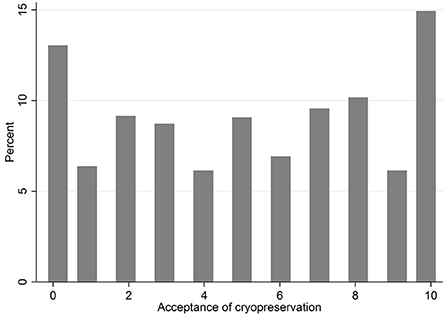
Figure 2. Distribution of vignette ratings in the study sample (author's computation). All participants are included that rated at least one vignette. Number of study participants = 749, Number of vignette ratings = 8,839.
As a preliminary step for MLA, we estimated the intraclass correlation coefficient (ICC), which distinguishes the parts of the variance in the vignette ratings within and between individuals. ICC = 0.696 indicates that almost 70% of the variance in the vignette ratings is due to variation between the participants.
As a second step, we test for significant variation of the regression coefficients of the within part of the model (i.e., the vignette part). The coefficient for “woman's age at using oocytes” varies significantly across participants. Therefore, we specified this factor as a random component to correctly model the effect variation across all participants. All other factors are estimated as fixed effects (i.e., the coefficients are the same for all participants).
Figure 3 shows the unstandardized regression coefficients from the multilevel analysis and their confidence intervals from the full model. Appendix 1 also reports the coefficients and standard errors.
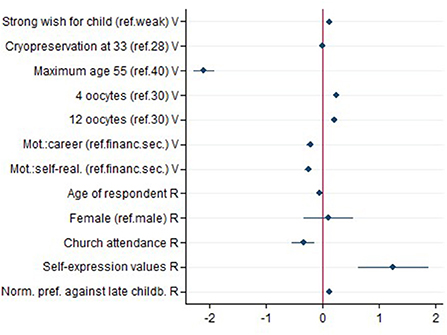
Figure 3. Unstandardized regression coefficients from the multilevel regression model (author's estimation). The dependent variable is acceptance of oocyte cryopreservation. The coefficients for the vignette factors are marked by a V. R marks predictors at the participant level. The bars represent the confidence interval at the 95% level. Number of observations at the participant level = 596. Number of observations at the vignette level (vignette ratings) = 7,152.
Because all variables of the vignette part of the study are dummy coded and have the same variance, the effect sizes are comparable. The regression model shows that acceptance is higher for women having a strong wish for a child (b = 0.124, p < 0.001; Hypothesis 1). In contrast, women's age at cryopreservation has no significant effect on acceptance (Hypothesis 2). The strongest effect in the vignette part of the study is the age up to which a woman plans to use preserved oocytes for IVF. For a woman planning IVF up to age 55, acceptance is, on average, two scale points lower (b = −2.094, p < 0.001) compared to a woman planning IVF up to age 40 (Hypothesis 3).
As expected, a smaller number of preserved oocytes increases acceptance. Compared to the preservation of 30 oocytes, 12 oocytes increase acceptance by 0.21 (p < 0.001) scale points, and preserving 4 oocytes increases acceptance by a quarter scale point (b = 0.25, p < 0.001; Hypothesis 4).
Egoistic motivations decrease acceptance. The effect size for pursuing a career before parenthood (b = −0.218, p < 0.001) was smaller than for self-realization (b = −0.251, p < 0.001). The difference between the two egoistic motives is insignificant, indicating that participants do not differentiate further between egoistic motives (Hypothesis 5).
Regarding the participants' characteristics, our analysis shows that attending church more frequently is linked to lower acceptance (b = −0.340, p < 0.001; Hypothesis 6). In addition, we estimated the interaction effects between individual religiosity and all vignette factors (not reported here). The estimates show that individual religiosity did not moderate the vignette factors. The effects of the vignette factors for regular church goers were not weaker than the effects for participants not attending church. Religious individuals are also sensitive to the circumstances in the use of cryopreservation and do not reject its use categorically. Postmaterialist value orientations have a positive influence on acceptance (b = 1.248, p < 0.001; Hypothesis 7). The effect sizes are not comparable, given the different scales of the participant-level indicators.
Eventually, participants without a normative preference against late childbearing are more accepting of cryopreservation (b = 0.118, p < 0.001; Hypothesis 8). Moreover, we expected the normative preference (participant level) to moderate the effect of the age at which women plan to use their preserved oocytes (vignette level). This interaction effect is significant (b = 0.071, p < 0.001, see Model 3 in Appendix 1). Figure 4 shows the predicted values for acceptance of cryopreservation depending on the maximum age at IVF (40 vs. 55 years) and the normative preference against late childbearing (Hypothesis 9).
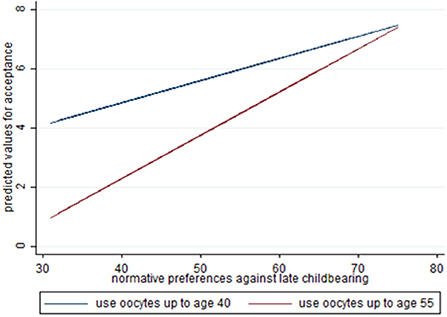
Figure 4. Predicted values for acceptance of cryopreservation depending on the maximum age at realization of parenthood (40 vs. 55 years) and the normative preference against late childbearing (31 to 75 years). The conditional effects plot shows the moderation of the vignette factor age at realization of parenthood effect by the the normative preference against late motherhood at the participant level.
The lower the participants set the age limit for childbearing, the more pronounced was the difference in acceptance of a woman planning to use cryopreserved oocytes up to age 40 compared to age 55. The difference in the vignette ratings for women planning to use oocytes up to age 40 or up to age 55 decreases with more liberal views about delayed childbearing.
Discussion
Whereas, Lallemant et al. (2015) and Wennberg et al. (2016) found high levels of support for cryopreservation in Denmark, Sweden and the UK, our results suggest that it is highly contested in Germany. This might partly be due to the legacy of the conservative gender regime and traditional gender roles placing the primary responsibility for childrens' wellbeing on women. Regarding the factors shaping attitudes toward cryopreservation, our analysis shows that the theoretical frame of moral contextualism provides a sound base to explain the individual level variation in attitudes toward cryopreservation within the context of the German gender regime. The results from the vignette part of the study show that public attitudes depend on the circumstances of its use. Individuals evaluate the consequences in line with the moral principle of harm avoidance and thus form their attitudes accordingly. Our results confirm the basic assumptions of moral contextualism about taking the consequences of medical technologies into account when forming attitudes.
As expected, individuals tend to be more accepting of cryopreservation for women who have a strong desire for motherhood because they would suffer more from involuntary childlessness. On the other hand, individuals are less accepting if women preserve their oocytes without a definite wish for a child.
The age of the women at cryopreservation had no effect on acceptance, although higher age was expected to reduce acceptance. This finding probably reflects the lack of knowledge about increasing subfertility starting at age 30 (Lampic et al., 2006; Bunting and Boivin, 2008; Wennberg, 2020) and suggests individuals are not aware that success of cryopreservation is more likely if oocytes are collected and preserved at a younger age.
The results show that the strongest effect on acceptance of cryopreservation is the age at which women plan to use their eggs. This finding confirms the results from existing studies showing that a longer duration of oocyte storage is related to lower acceptance levels, especially for social indications (Wennberg et al., 2016). Our results suggest that this is due to social objections regarding delayed childbearing (Billari et al., 2011; Kim and Cho, 2021). The moderation of the vignette effect by the normative preference against late motherhood at the participant level underscores the importance of individuals normative orientations for the resulting attitudes. Women's plans for delayed childbearing only reduce acceptance for individuals who are not tolerant of late parenthood. The presence or absence of a preference against delayed childbearing is among the most important factors influencing attitudes toward cryopreservation (directly via the effect of the individual level and indirectly as a moderator for the vignette factor). Late parenthood itself and as a consequence of cryopreservation is perceived negatively in Germany. Why late parenthood is perceived as harmful for children and why this perception is especially strong in Germany should be the subject of further research relating gender role attitudes to moral evaluations of social freezing. This finding might also be specific to the German situation with the strong prevalence of traditional gender roles shaping the normative expectations about “good motherhood.” A comparison of attitudes between different types of gender regimes might show whether or not this finding can be generalized to other social contexts.
Participants were also sensible to concerns about the use of surplus oocytes. This is often crucial in ethical discussions about cryopreservation and other ART (Benagiano et al., 2011; Varlas et al., 2021). If a lower number of oocytes is collected for preservation, acceptance is generally higher but a lower number of oocytes reduces the chance of a life birth (Wennberg, 2020). The pro-life position claims that oocytes should be protected against destruction, which may influence attitudes. In Germany, the donation of oocytes (e.g., to infertile couples or for scientific research) is prohibited. A relevant question here is whether additional options for using surplus oocytes (e.g., for research purposes) would increase acceptance. In other European countries egg donation is a legal medical practice. We would expect this possibility to reduce concerns about surplus oocytes in attitude formation.
The results confirm that delaying parenthood for career reasons is perceived as egoistic. Even more egoistic but not significantly different is the motive of self-realization. Acceptance is higher only for women who postpone family formation because of concerns about financial stability. Therefore, the negative perception of women's career in relation to family formation in Germany should be given further attention.
In addition to the moral evaluation of the circumstances of the individual use of cryopreservation, value orientations explain the variance in the attitudes toward cryopreservation. Our results confirm findings from existing studies that found individual religiosity to be among the social factors associated with lower levels of acceptance for cryopreservation (Lewis et al., 2016). Interestingly, the effects of the vignette part of the study do not differ between religious and non-religious participants. Although the overall level of acceptance is lower for religious individuals, they do not categorically reject cryopreservation. Religious participants are also sensitive to the specific circumstances of the use of cryopreservation.
Moreover, individuals emphasizing values of autonomy and self-determination have higher levels of permissiveness.
This study has limitations regarding the generalization of the results to the general population in Germany because participants were recruited through an online access panel. Furthermore, the study did not address the role of the partner and the women's marital status when forming attitudes toward cryopreservation. Especially for women who have not voluntarily chosen to be without a partner, or women whose partner wishes to postpone childbearing, acceptance might be higher because the women's responsibility for childlessness is limited. For marital status, we argue that this is more important for attitudes toward IVF using cryopreserved oocytes. More research is needed to understand how attitudes toward IVF and cryopreservation are linked. Finally, an individual's knowledge about age-related fertility loss and the success rates of IVF were not part of the study but could moderate how the different factors modeled on the vignettes influence attitudes.
Conclusion
The aim of our analysis was to study how moral principles and value orientations shape attitude formation in the case of cryopreservation. We analyzed the factors in the use of oocyte cryopreservation and the social factors that are associated with acceptance of oocyte cryopreservation. We used a factorial survey as a quasi-experimental design to test hypotheses deduced from moral contextualism. Thus, we studied how differences in specific settings influence acceptance of cryopreservation.
Our results indicate that delayed childbearing is an important factor of concern. A social norm against late motherhood exists, which fosters rejection of cryopreservation if it is used to postpone childbearing until age 55. Information of prospective users should not be limited to age-related fertility decline and risks of cryopreservation and IVF (Daniluk and Koert, 2016). More information about the consequences of delayed childbearing for children and families, including potential social objections against late parenthood, are needed.
It is an open question whether objections against late parenthood also decrease acceptance of oocyte cryopreservation in other countries or whether these objections are specific to Germany with its long-term tradition of conservative family policies that favor traditional gender roles. This relates to the negative perception of women's career when compared to family formation, too. Comparative studies and studies that take the role of men and fathers into account could shed more light on this question.
Moral contextualism proved to be an appropriate frame for studying attitudes toward cryopreservation. More research is needed on other factors that potentially influence acceptance, such as marital status. Our study focuses on factors at the time of cryopreservation. Further studies should also address the circumstances at the time of IVF after warming the oocytes and how the options for using surplus oocytes from cryopreservation (e.g., oocyte donation) influence public acceptance.
Data availability statement
The original contributions presented in the study are publicly available. This data can be found at: http://doi.org/10.7802/1378.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AF designed the questionnaire, collected, and analyzed the data. PS supervised the design and analysis and wrote the introduction, theory, discussion, and conclusion section of the article. All authors contributed to the article and approved the submitted version.
Funding
The publication of this article was funded by the Open Access Fund of the Leibniz Association.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpos.2022.995009/full#supplementary-material
Footnotes
1. ^Data retreived from the demographic database of the Federal Statistical Office of Germany: https://www-genesis.destatis.de/genesis/online (accessed September 19, 2022).
References
Auspurg, K., and Hinz, T. (2015). Factorial Survey Experiments. London: SAGE. doi: 10.4135/9781483398075
Auspurg, K., Hinz, T., Liebig, S., and Sauer, C. (2014). “The factorial survey as a method for measuring sensitive issues,” in Improving Survey Methods: Lessons From Recent Research, eds U. Engel, B. Jann, P. Lynn, A. Scherpenzeel, and P. Sturgis (Routledge; Taylor & Francis Group), 137–149.
Baldwin, K., Culley, L., Hudson, N., and Mitchell, H. (2014). Reproductive technology and the life course: current debates and research in social egg freezing. Hum. Fertil. 17, 170–179. doi: 10.3109/14647273.2014.939723
Baldwin, K., Culley, L., Hudson, N., and Mitchell, H. (2019). Running out of time: exploring women's motivations for social egg freezing. J. Psychosom. Obstetr. Gynecol. 40, 166–173. doi: 10.1080/0167482X.2018.1460352
Baldwin, K., Culley, L., Hudson, N., Mitchell, H., and Lavery, S. (2015). Oocyte cryopreservation for social reasons: demographic profile and disposal intentions of UK users. Reprod. Biomed. Online 31, 239–245. doi: 10.1016/j.rbmo.2015.04.010
Barclay, K., and Myrskylä, M. (2016). Advanced maternal age and offspring outcomes: reproductive aging and counterbalancing period trends. Popul. Dev. Rev. 42, 69–94. doi: 10.1111/j.1728-4457.2016.00105.x
Beck, M., and Opp, K.-D. (2001). Der faktorielle survey und die messung von normen. Kölner Zeitschr. Soziol. Sozialpsychol. 53, 283–306. doi: 10.1007/s11577-001-0040-3
Benagiano, G., Mori, M., Ford, N., and Grudzinskas, G. (2011). Early pregnancy wastage: ethical considerations. Reprod. Biomed. Online 22, 692–700. doi: 10.1016/j.rbmo.2011.03.008
Billari, F. C., Goisis, A., Liefbroer, A. C., Settersten, R. A., Aassve, A., Hagestad, G., et al. (2011). Social age deadlines for the childbearing of women and men. Hum. Reprod. 26, 616–622. doi: 10.1093/humrep/deq360
Bozzaro, C. (2018). Is egg freezing a good response to socioeconomic and cultural factors that lead women to postpone motherhood?. Reprod. Biomed. Online 36, 594–603. doi: 10.1016/j.rbmo.2018.01.018
Bunting, L., and Boivin, J. (2008). Knowledge about infertility risk factors, fertility myths and illusory benefits of healthy habits in young people. Hum. Reprod. 23, 1858–1864. doi: 10.1093/humrep/den168
Caughey, L. E., and White, K. M. (2021). Psychosocial determinants of women's intentions and willingness to freeze their eggs. Fertil. Steril. 115, 742–752. doi: 10.1016/j.fertnstert.2020.09.150
Cremonese, J., Marcon, M., Oppi, L., Paletti, G., Romolo, V., Tozzo, P., et al. (2022). An update on planned oocyte cryopreservation (POC) in Italy: medical, epidemiological and legal consideration. Int. J. Environ. Res. Public Health. 19:2371. doi: 10.3390/ijerph19042371
Daniluk, J. C., and Koert, E. (2016). Childless women's beliefs and knowledge about oocyte freezing for social and medical reasons. Hum. Reprod. 31, 2313–2320. doi: 10.1093/humrep/dew189
Dülmer, H. (2014a). “Vignetten,” in Handbuch Methoden der Empirischen Sozialforschung, eds N, Baur and J. Blasius (Wiesbaden: Springer), 721–732. doi: 10.1007/978-3-531-18939-0_53
Dülmer, H. (2014b). “Modernization, culture and morality in Europe: universalism, contextualism or relativism?,” in Value Contrasts and Consensus in Present Day Europe, eds W. Arts and L. Halman (Leiden: Koninklijke Brill NV), 251–276. doi: 10.1163/9789004261662_013
Dülmer, H. (2015). The factorial survey design selection and its impact on reliability and internal validity. Sociol. Methods Res. 45, 304–347. doi: 10.1177/0049124115582269
Forke, A. (2016). Faktorieller Survey zur Moralischen Akzeptanz von Social Freezing. GESIS—Leibniz Institut für Sozialwissenschaften.
Gianaroli, L., Ferraretti, A. P., Magli, M. C., and Sgargi, S. (2016). Current regulatory arrangements for assisted conception treatment in European countries. Eur. J. Obstet. Gynecol. Reprod. Biol. 207, 211–213. doi: 10.1016/j.ejogrb.2016.10.002
Goldman, K. N., and Grifo, J. A. (2016). Elective oocyte cryopreservation for deferred childbearing. Curr. Opin. Endocrinol. Diabetes Obes. 23, 458–464. doi: 10.1097/MED.0000000000000291
Goold, I., and Savulescu, J. (2009). In favour of freezing eggs for non-medical reasons. Bioethics 23, 47–58. doi: 10.1111/j.1467-8519.2008.00679.x
Haker, H. (2016). Kryokonservierung von Eizellen. Neue Optionen der Familienplanung? Eine ethische Bewertung. Zeitschr. Med. Ethik 62, 121–132. doi: 10.14623/zfme.2016.2.121-132
Halman, L., and van Ingen, E. (2015). Secularization and changing moral views: European trends in church attendance and views on homosexuality, divorce, abortion, and euthanasia. Eur. Sociol. Rev. 31, 616–627. doi: 10.1093/esr/jcv064
Hans, J. D., and Kimberly, C. (2014). Abortion attitudes in context: A multidimensional vignette approach. Soc. Sci. Res. 48, 145–156. doi: 10.1016/j.ssresearch.2014.06.001
Johnson, J. A., and Tough, S. (2012). Delayed childbearing. J. Obstetr. Gynaecol. Can. 34, 80–93. doi: 10.1016/S1701-2163(16)35138-6
Jones, B. P., Kasaven, L., L'Heveder, A., Jalmbrant, M., Green, J., Makki, M., et al. (2020). Perceptions, outcomes, and regret following social egg freezing in the UK; a cross-sectional survey. Acta Obstet. Gynecol. Scand. 99, 324–332. doi: 10.1111/aogs.13763
Kim, E. J., and Cho, M. J. (2021). The association between assisted reproduction technology (ART) and social perception of childbearing deadline ages: a cross-country examination of selected EU countries. Int. J. Environ. Res. Public Health 18:2111. doi: 10.3390/ijerph18042111
Kocourková, J., Konečná, H., Burcin, B., and Kučera, T. (2015). How old is too old? A contribution to the discussion on age limits for assisted reproduction technique access. Reprod. Biomed. Online 30, 482–492. doi: 10.1016/j.rbmo.2015.01.017
Kostenzer, J., de Bont, A., and van Exel, J. (2021). Women's viewpoints on egg freezing in Austria: an online Q-methodology study. BMC Med. Ethics 22:4. doi: 10.1186/s12910-020-00571-6
Lallemant, C., Vassard, D., Andersen, A. N., Schmidt, L., and Macklon, N. (2015). Oocyte freezing for social indications: how do men and women's views differ? Internet based survey of knowledge, attitudes and intentions in Denmark and United Kingdom. Hum. Reprod. 30, 323.
Lampic, C., Skoog Svanberg, A., Karlström, P., and Tydén, T. (2006). Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum. Reprod. 21, 558–564. doi: 10.1093/humrep/dei367
Lampinen, R., Vehviläinen-Julkunen, K., and Kankkunen, P. (2009). A review of pregnancy in women over 35 years of age. Open Nurs. J. 3, 33–38. doi: 10.2174/1874434600903010033
Lewis, E. I., Missmer, S. A., Farland, L. V., and Ginsburg, E. S. (2016). Public support in the United States for elective oocyte cryopreservation. Fertil. Steril. 106, 1183–1189. doi: 10.1016/j.fertnstert.2016.07.004
Lockwood, G. M. (2011). Social egg freezing: the prospect of reproductive 'immortality' or a dangerous delusion? Reprod. Biomed. Online 23, 334–340. doi: 10.1016/j.rbmo.2011.05.010
Nasab, S., Ulin, L., Nkele, C., Shah, J., Abdallah, M. E., and Sibai, B. M. (2020). Elective egg freezing: what is the vision of women around the globe? Fut. Sci. 6:FSO468. doi: 10.2144/fsoa-2019-0068
Neilson, J., and Stanfors, M. (2014). It's about time! Gender, parenthood, and household divisions of labor under different welfare regimes. J. Fam. Issues 35, 1066–1088. doi: 10.1177/0192513X14522240
Nunner-Winkler, G. (1997). “Zurück zu durkheim? Geteilte Werte als Basis gesellschaftlichen Zusammenhalts,” in Was Hält Gesellschaft Zusammen? ed W. Heitmeyer (Frankfurt am Main: Suhrkamp), 360–402.
Nunner-Winkler, G. (2020). Moral progress: improvement of moral concepts, refinements of moral motivation. Analyse Kritik 42, 171–190. doi: 10.1515/auk-2020-0007
Pai, H. D., Baid, R., Palshetkar, N. P., Pai, A., Pai, R. D., and Palshetkar, R. (2021). Oocyte cryopreservation - current scenario and future perspectives: a narrative review. J. Hum. Reprod. Sci. 14, 340–349. doi: 10.4103/jhrs.jhrs_173_21
Park, A., and Clery, E. (2008). Assisted Dying and Decision Making at the End of Life. National Centre for Social Research.
Pennings, G. (2021). Elective egg freezing and women's emancipation. Reprod. Biomed. Online 42, 1053–1055. doi: 10.1016/j.rbmo.2021.04.004
Platts, S., Trigg, B., Bracewell-Milnes, T., Jones, B. P., Saso, S., Parikh, J., et al. (2021). Exploring women's attitudes, knowledge, and intentions to use oocyte freezing for non-medical reasons: a systematic review. Acta Obstet. Gynecol. Scand. 100, 383–393. doi: 10.1111/aogs.14030
Rossier, C., Brachet, S., and Salles, A. (2011). Family policies, norms about gender roles and fertility decisions in France and Germany. Vienna Yearbook Popul. Res. 9, 259–282. doi: 10.1553/populationyearbook2011s259
Sallam, H. N., and Sallam, N. H. (2016). Religious aspects of assisted reproduction. Facts Views Vis. ObGyn. 8, 33–48.
Savulescu, J., and Goold, I. (2008). Freezing eggs for lifestyle reasons. Am. J. Bioeth. 8, 32–35. doi: 10.1080/15265160802248492
Snijders, T. B., and Bosker, R. J. (1999). Multilevel Analysis. An Introduction to Basic and Advanced Multilevel Modeling. London: Sage.
Storm, I. (2016). Morality in context: a multilevel analysis of the relationship between religion and values in Europe. Polit. Relig. 9, 111–138. doi: 10.1017/S1755048315000899
Sutcliffe, A. G. (2012). The health and development of children born to mothers in the United Kingdom: observational study using longitudinal cohort data. BMJ 345, 1–10. doi: 10.1136/bmj.e5116
Teo, U. L., Kakkar, P., and El-Toukhy, T. (2022). Current perspectives on social oocyte freezing. J. Obstet. Gynaecol. 42, 370–378. doi: 10.1080/01443615.2021.1904220
Tozzo, P. (2021). Oocyte biobanks: old assumptions and new challenges. BioTech. 10:4. doi: 10.3390/biotech10010004
Varlas, V. N., Bors, R. G., Albu, D., Penes, O. N., Nasui, B. A., Mehedintu, C., et al. (2021). Social freezing: pressing pause on fertility. Int. J. Environ. Res. Public Health 18:8088. doi: 10.3390/ijerph18158088
Vassard, D., Lallemant, C., Nyboe Andersen, A., Macklon, N., and Schmidt, L. (2016). A population-based survey on family intentions and fertility awareness in women and men in the United Kingdom and Denmark. Ups. J. Med. Sci. 121, 244–251. doi: 10.1080/03009734.2016.1194503
Walker, Z., Lanes, A., and Ginsburg, E. (2022). Oocyte cryopreservation review: outcomes of medical oocyte cryopreservation and planned oocyte cryopreservation. Reprod. Biol. Endocrinol. 20:10. doi: 10.1186/s12958-021-00884-0
Welzel, C. (2010). How selfish are self-expression values? A civicness test. J. Cross-Cult. Psychol. 41, 152–174. doi: 10.1177/00223022109354378
Welzel, C. (2013). Freedom Rising. Cambridge, UK: Cambridge University Press. doi: 10.1017/CBO9781139540919
Wennberg, A. L. (2020). Social freezing of oocytes: a means to take control of your fertility. Ups. J. Med. Sci. 125, 95–98. doi: 10.1080/03009734.2019.1707332
Keywords: oocyte cryopreservation, assisted reproduction (ART), moral attitudes, moral contextualism, factorial survey
Citation: Forke A and Siegers P (2022) More benefit or harm? Moral contextualism shapes public attitudes towards social egg freezing. Front. Polit. Sci. 4:995009. doi: 10.3389/fpos.2022.995009
Received: 15 July 2022; Accepted: 07 October 2022;
Published: 28 October 2022.
Edited by:
Jonathan Lewallen, University of Tampa, United StatesReviewed by:
Luciana Caenazzo, University of Padua, ItalyHelga Kristin Hallgrimsdottir, University of Victoria, Canada
Copyright © 2022 Forke and Siegers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pascal Siegers, cGFzY2FsLnNpZWdlcnNAZ2VzaXMub3Jn
 Anna Forke
Anna Forke Pascal Siegers
Pascal Siegers