
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Physiol. , 05 May 2023
Sec. Cardiac Electrophysiology
Volume 14 - 2023 | https://doi.org/10.3389/fphys.2023.1125340
This article is part of the Research Topic Future Directions in Conduction System Pacing to Achieve Cardiac Resynchronization View all 9 articles
 Jie Zhang†
Jie Zhang† Feng Li†
Feng Li† Zhi-Yuan Zhang†
Zhi-Yuan Zhang† Fan Yang
Fan Yang Qi Kong
Qi Kong Jia-Yi Chen
Jia-Yi Chen Lei Zhang
Lei Zhang Huan-Huan Liu
Huan-Huan Liu Xu-Fei Chen
Xu-Fei Chen Yu-Heng Ye
Yu-Heng Ye Ru-Xing Wang*
Ru-Xing Wang*Background: The effects of conduction system pacing (CSP) compared with conventional biventricular pacing (BVP) on heart function in patients with heart failure remain elusive.
Methods: PubMed, Embase, Cochrane’s Library and Web of science databases were searched up to 1 October 2022 for pertinent controlled studies. Random or fixed-effect model were used to synthesize the clinical outcomes. Subgroup analysis was performed to screen the potential confounding factors.
Results: Fifteen studies including 1,347 patients were enrolled. Compared with BVP, CSP was significantly associated with shortened QRS duration [WMD -22.51 ms; p = 0.000], improved left ventricular ejection fraction [WMD 5.53%; p = 0.000], improved NYHA grade [WMD -0.42; p = 0.000], higher response rate and lower heart failure rehospitalization rate. CSP resulted in better clinical outcomes in higher male proportion group than lower one compared with BVP. No significant differences of clinical outcomes were observed between left bundle branch area pacing (LBBaP) and his bundle pacing (HBP) except the pacing threshold. The pacing threshold of LBBaP was significantly lower than those in BVP and HBP.
Conclusion: This study suggests that CSP might be superior to conventional BVP for HF patients. In a higher male proportion group, CSP may be associated with more benefits than BVP.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022355991; Identifier: CRD42022355991.
Cardiac resynchronization therapy (CRT) through biventricular pacing (BVP) has been proved to bring out clinical benefits in heart failure (HF) patients with reduced left ventricular ejection fraction (LVEF) and left bundle branch block (LBBB). However, CRT based on BVP was realized through non-physiological fusion of paced wavefronts from the right ventricular (RV) endocardium and left ventricular (LV) epicardium (Ploux et al., 2015). As a result, the super-response rates of BVP was relatively low (only 20%–30%) and a considerable number of patients (30% at most) may not derive clinical benefits from BVP (Ellenbogen and Huizar, 2012), which means we need more effective pacing strategies to deliver CRT. Recently, conduction system pacing (CSP), mainly including his bundle pacing (HBP) and left bundle branch area pacing (LBBaP) has emerged as a promising alternative CRT.
HBP has been established as a feasible pacing strategy to improve cardiac function in several researches and it can provide comparable LVEF improvement to BVP (Upadhyay et al., 2019a). However, the disadvantage of HBP lies in its high and unstable LBBB correction threshold. LBBaP was a novel technique developed by Huang et al. (2017). A series of case reports and observational studies demonstrated the feasibility and safety of LBBaP in HF patients meeting the criteria of CRT (Zhang et al., 2019; Guo et al., 2020; Wu et al., 2021). However, few studies compared the effectiveness between CSP and BVP. The purpose of this study is to determine whether there are differences in clinical prognosis and pacing parameters between CSP and BVP in HF patients who required CRT.
This meta-analysis was performed in accordance with the PRISMA guidelines. We conducted the meta-analysis registration on the PROSPERO platform (CRD42022355991).
A total of four databases (PubMed, Web of Science, Embase and the Cochrane Library) were systematically searched by two independent investigators (J. Zhang and F. Li) up to 1 October 2022. Search keywords included “conduction system pacing”, “His bundle pacing”, “left bundle area pacing”, “left bundle branch pacing” and “biventricular pacing”, and “cardiac resynchronization therapy”. We performed the search by using the keywords alone and following query formula” (conduction system pacing or His bundle pacing or left bundle branch pacing or left bundle branch area pacing) and (Biventricular pacing or cardiac resynchronization therapy)”. Studies reporting comparing outcomes between CSP and BVP were included. We also screened and conducted a manual search of the references of the original and review articles for potential studies not identified before.
The titles, abstracts, and full texts were reviewed by two independent reviewers (J. Zhang and Z-Y Zhang) to select the eligible studies. The inclusion criteria are as follows: 1) randomized controlled trials, retrospective studies or prospective/observational studies. 2) studies comparing pacing outcomes between CSP and BVP in HF patients. 3) studies reporting on pacing outcomes during follow-up, including final QRS duration (QRSd), reduction in QRSd, final LVEF, improvement in LVEF, New York Heart Association (NYHA) grade, reduction in NYHA grade, echocardiographic, clinical CRT response rates and CRT super response rates. According to the references, echocardiographic CRT response was defined as at least 5% improvement of LVEF during follow-up (Guo et al., 2020). Clinical CRT response was defined as decreasing NYHA functional class for at least one grade at the last follow-up. CRT super response rate was defined as a significant improvement in LVEF for at least 20% or final LVEF≥50% (Wu et al., 2021). Review articles, letters, studies without original data, editorials, case reports, animal studies and protocols were excluded.
The data for eligible studies were extracted by two independent researchers (J. Zhang and F. Li) and any disagreements were resolved by a third researcher (R.-X. Wang). The extracted data mainly included study characteristics (such as first author, country, study design, publication year, sample size and follow-up time), patients’ demographic and clinical characteristics.
We use two appraisal tools to assess the study quality. The Cochrane’s Risk of Bias Tool Quality was used for evaluating the randomized controlled studies, and the Newcastle-Ottawa Scale (NOS) was used to assess the quality of non-randomized controlled studies.
We used the weighted mean difference (WMD) for continuous variables and risk ratio (RR) for categorical variables. The 95% confidence intervals (CI) for WMD and RR were calculated. The Stata (Version 16.0) was used for statistical analyses, and p < 0.05 was statistically significant.
The Chi-squared test and I-squared (I2) were used to assess the heterogeneity among studies. If the I2 value was less than 50% and/or p > 0.05 with the Chi-squared test, the between-study heterogeneity is not substantial, and a fixed-effect model was used. Otherwise, we used a random-effect model. Potential publication bias was assessed by the Egger regression asymmetry test. A sensitivity analysis with sequentially omitting one study method was conducted to evaluate the influence of a single study on the overall risk.
A subgroup analysis was also performed according to our previous reported methods (Li et al., 2022). A total of five confounding factors were screened, including study design (multi-center and single-center), CSP sample size (>20 and ≤20), male proportion (>50% and ≤50%), CSP types (LBBaP and HBP), and follow-up (≥12 months and <12 months).
A total of fifteen studies including 1347 HF patients were eligible (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vijayaraman et al., 2019; Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Moriña-Vázquez et al., 2022; Rademakers et al., 2022; Vijayaraman et al., 2022; Wang et al., 2022) the flowchart of study selection is displayed in Figure 1. The baseline characteristics of the eligible studies were presented in Table 1. Four of fifteen eligible studies were randomized controlled studies (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vinther et al., 2021; Wang et al., 2022), and the literature quality was evaluated with the Cochrane’s Risk of Bias Tool (Supplementary Figure S1); meanwhile, the remaining eleven non-randomized studies (Vijayaraman et al., 2019; Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Moriña-Vázquez et al., 2022; Rademakers et al., 2022; Vijayaraman et al., 2022) were evaluated with the Newcastle-Ottawa Scale (NOS) (Supplementary Table S1). The quality of all the studies were good.
All eligible studies (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vijayaraman et al., 2019; Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Rademakers et al., 2022; Vijayaraman et al., 2022; Wang et al., 2022) including 1282 HF patients (633 patients for CSP, and 649 for BVP) reported the final QRSd, the average time of observation was 10.2 ± 7.2 months and thirteen studies (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vijayaraman et al., 2019; Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Rademakers et al., 2022; Wang et al., 2022) reported the shortening of QRSd with a 8.8 ± 5.5 months time of observation. When compared with BVP in the last follow-up, CSP resulted in a narrower QRSd [WMD −22.51 ms; 95% CI (−27.29, −17.72); p = 0.000; I2 = 79.2%] (Figure 2A) and more shortening of QRSd [WMD 26.43 ms; 95% CI (20.49, 32.37); p = 0.000; I2 = 72.9%] (Figure 2B).
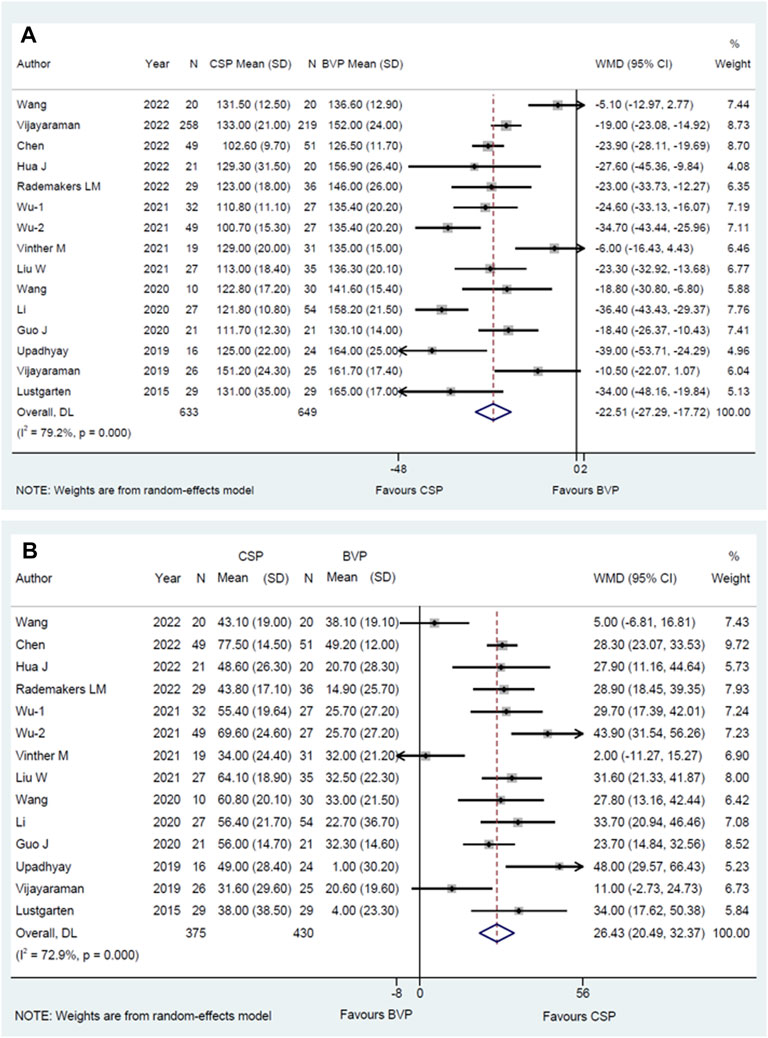
FIGURE 2. Forest plot of final QRSd and shortening of QRSd between CSP and BVP. (A) Final QRSd, (B) shortening of QRSd. CSP, conduction system pacing; BVP, biventricular pacing; WMD, weighted mean difference; CI, confidence interval.
In addition, the significant treatment-covariate interaction was identified in the male proportion subgroup for more shortening of QRSd, including >50% subgroup [WMD 31.94 ms; 95% CI(24.40,39.47); p = 0.000; I2 = 56.6%] and ≤50% subgroup [WMD 20.34 ms; 95% CI (11.57,29.10); p = 0.000; I2 = 79.8%] with p = 0.049 for interaction (Supplementary Table S3). Similarly, the final QRSd of higher male proportion is narrower than the lower one, including >50% subgroup [WMD -26.72 ms; 95% CI (−33.40,-20.04); p = 0.000; I2 = 77.4%] and ≤50% subgroup [WMD −17.09 ms; 95% CI (−24.22,-9.95); p = 0.000; I2 = 80.3%], but it did not reach statistical significance with p = 0.053 for interaction (Supplementary Table S2). The results suggested that CSP tends to bring shorter QRSd in higher male proportion group when compared with BVP.
The WMD and corresponding 95% CI of final LVEF was available from nine eligible studies (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Hua et al., 2022a; Chen et al., 2022; Rademakers et al., 2022; Wang et al., 2022), and the improvement of LVEF was also available from ten studies (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Rademakers et al., 2022; Wang et al., 2022). The average time of observation was 8.4 ± 6.2 months for final LVEF, and 8.8 ± 6.0 months for the improvement of LVEF. When compared to BVP, CSP resulted in higher LVEF [WMD 5.53%; 95% CI (3.70, 7.36); p = 0.000; I2 = 0.0%] (Figure 3A) and a higher improvement in LVEF [WMD 5.45%; 95% CI (3.81,7.09); p = 0.000; I2 = 0.0%] (Figure 3B). The subgroup analysis for the final LVEF and the improvement of LVEF was shown in Supplementary Tables S4, 5.
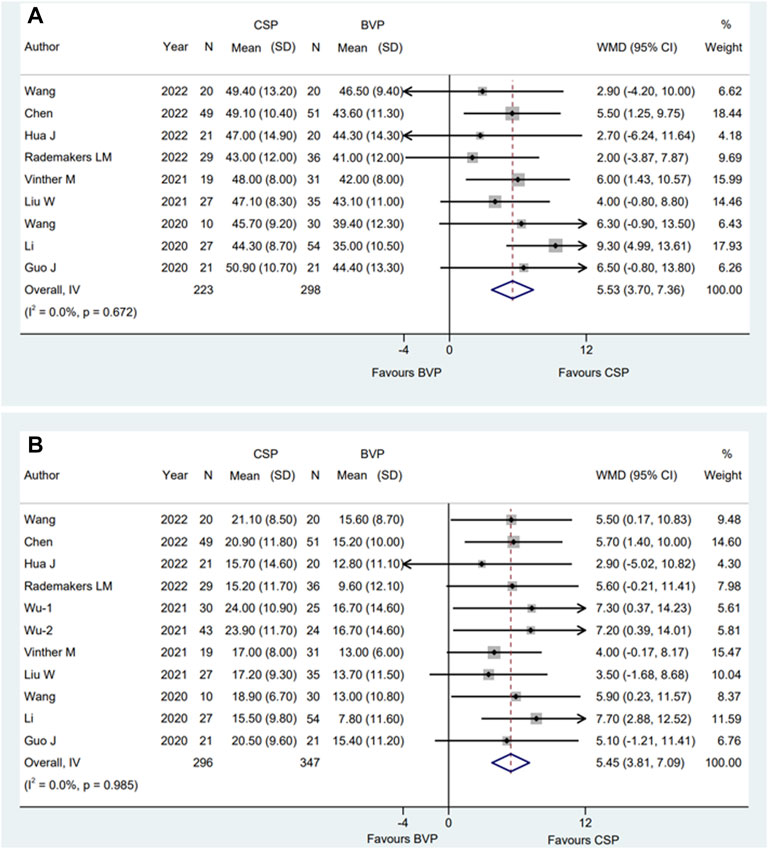
FIGURE 3. Forest plot of final LVEF and improvement of LVEF between CSP and BVP. (A) Final LVEF, (B) improvement of LVEF. CSP, conduction system pacing; BVP, biventricular pacing; WMD, weighted mean difference; CI, confidence interval.
All articles selected involving a total of eight eligible studies (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Rademakers et al., 2022) who reported final NYHA and nine (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Vinther et al., 2021; Wu et al., 2021; Hua et al., 2022a; Rademakers et al., 2022; Wang et al., 2022) reported the changes of NYHA. the average time of observation was 8.8 ± 6.6 months for final NYHA, and 8.4 ± 6.2 months for the improvement of NYHA. We used random-effect model to evaluate NYHA and the pooled results showed that compared with BVP, CSP was associated with significantly improved final NYHA grade [WMD −0.42; 95% CI (−0.63, −0.20); p = 0.000; I2 = 69.9%] (Figure 4A) and a higher change of NYHA [WMD 0.37; 95% CI (0.16, 0.58); p = 0.001; I2 = 56.3%] (Figure 4B).
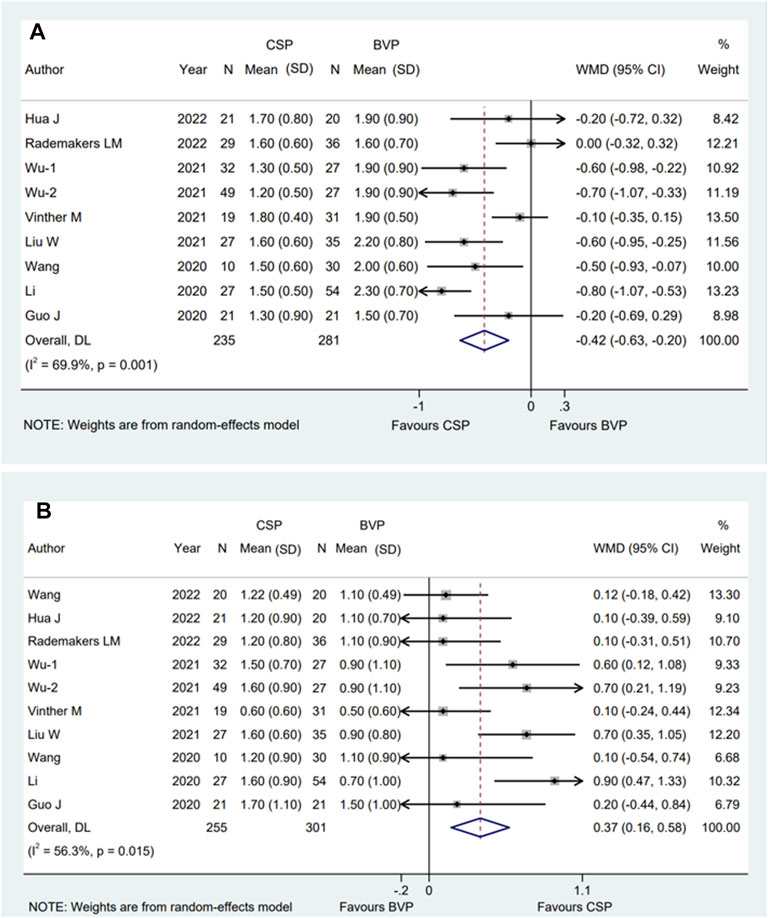
FIGURE 4. Forest plot of final NYHA grade and improvement of NYHA grade between CSP and BVP. (A) Final NYHA grade, (B) improvement of NYHA grade. CSP, conduction system pacing; BVP, biventricular pacing; WMD, weighted mean difference; CI, confidence interval.
The subgroup analysis showed that multi-center subgroup [WMD −0.73; 95% CI (−0.94, −0.52); p = 0.000; I2 = 0.0%] was significantly associated with improved NYHA class when compared with single-center group [WMD −0.32; 95% CI (−0.54, −0.10); p = 0.004; I2 = 56.9%] with p = 0.008 for interaction. The similar results also occurred in male proportion subgroup [>50% subgroup; WMD −0.63; 95% CI (−0.81, −0.45); p = 0.000; I2 = 14.6%, and ≤50% subgroup; WMD −0.20; 95% CI (−0.45, 0.05); p = 0.110; I2 = 52.4%, p = 0.007 for interaction]. Moreover, in the CSP sample size subgroup, the WMD was −0.26 [95% CI (−0.64, 0.12); p = 0.184; I2 = 59.7%] in the ≤20 group. In HBP group, the WMD was −0.38 [95% CI (−0.97, 0.20); p = 0.199; I2 = 85.7%] (Supplementary Table S6).
For the changes of NYHA, the subgroup analysis showed that CSP sample size >20 group [WMD 0.49; 95% CI (0.24,0.74); p = 0.000; I2 = 51.4%] was significantly associated with a higher improvement of NYHA class when compared with sample size ≤20 group [WMD 0.11; 95% CI (−0.10,0.32); p = 0.315; I2 = 0.0%] with p = 0.023 for interaction. Similar to what we observed in Final NYHA, the difference also shown in the male proportion subgroup [>50% group; WMD 0.54; 95% CI (0.24.0.85); p = 0.000; I2 = 53.4%, ≤50 group; WMD 0.18; 95% CI (0.01,0.36); p = 0.043; I2 = 0.0% p = 0.045 for interaction]. Moreover, in HBP group, the WMD was 0.37 [95% CI (−0.21,0.96); p = 0.210; I2 = 74.5%] (Supplementary Table S7).
LV lead pacing threshold, one of the lead parameters, was used for analysis in BVP group. The pacing threshold was measured in different units, so we used the most frequently used unit V at 0.5 ms (V/0.5 ms) from three studies (Wang et al., 2020; Wu et al., 2021; Chen et al., 2022) for analysis, the average time of observation of the three studies was 10 ± 3.5 months. When compared to BVP group, LBBaP group provided a lower pacing threshold with a WMD of −0.60V/0.5 ms [95% CI (−0.80, −0.41); p = 0.000; I2 = 75.6%]. Conversely, compared with BVP group, HBP group was associated with a higher pacing threshold with a WMD of 0.59 V/0.5 ms [95% CI (0.24, 0.94); p = 0.001)] (Figure 5).
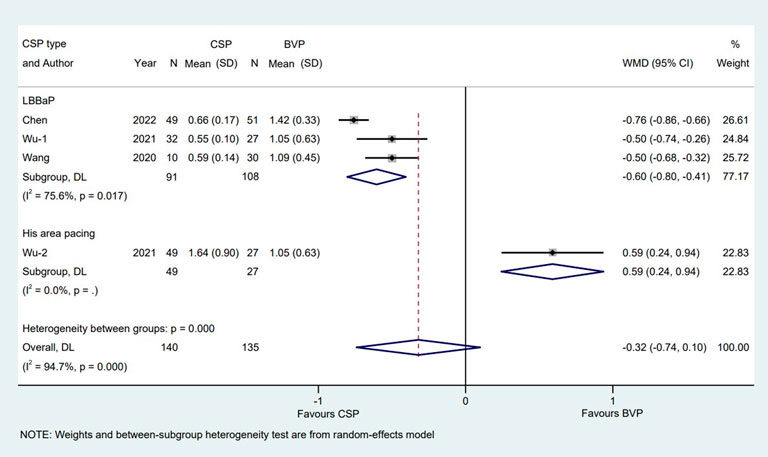
FIGURE 5. Forest plot of pacing thresholds between LBBaP, HBP and BVP LBBaP: left bundle branch area pacing; HBP, his bundle pacing; BVP, biventricular pacing; WMD, weighted mean difference; CI, confidence interval.
There is a total of five studies (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Vinther et al., 2021; Rademakers et al., 2022) reported clinical response rate, eight (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Chen et al., 2022; Moriña-Vázquez et al., 2022; Rademakers et al., 2022; Wang et al., 2022) reported echo response rate and five (Li et al., 2020; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Moriña-Vázquez et al., 2022) for super response rate. The average time of observation was 6 months, 7.3 ± 3.0 months and 13.2 ± 6.6 months for clinical response rate, echo response rate and super response rate individually. Pooled results with fixed effect model showed that compared with patients who received BVP, patients who received CSP were more likely to achieve clinical CRT responses [RR:1.14; 95% CI (1.03,1.28); p = 0.014; I2 = 0.0%] (Figure 6A), echocardiographic CRT responses [RR:1.22; 95% CI (1.13,1.32); p = 0.000; I2 = 47.5%] (Figure 6B) and super CRT responses [RR:1.83; 95% CI (1.47,2.28); p = 0.000; I2 = 4.1%] (Figure 6C). There were no statistical differences between subgroups when it comes to clinical (Supplementary Table S8) and super CRT response rate (Supplementary Table S10). Subgroup analysis suggested that male proportion (%) > 50 group [RR:1.39; 95% CI (1.23,1.57); p = 0.000; I2 = 0.0%] had a higher echo CRT response rate than male proportion (%) ≤ 50 group [RR:1.07; 95% CI (0.97,1.19); p = 0.170; I2 = 0.0%] with p = 0.001 for interaction (Figure 7).
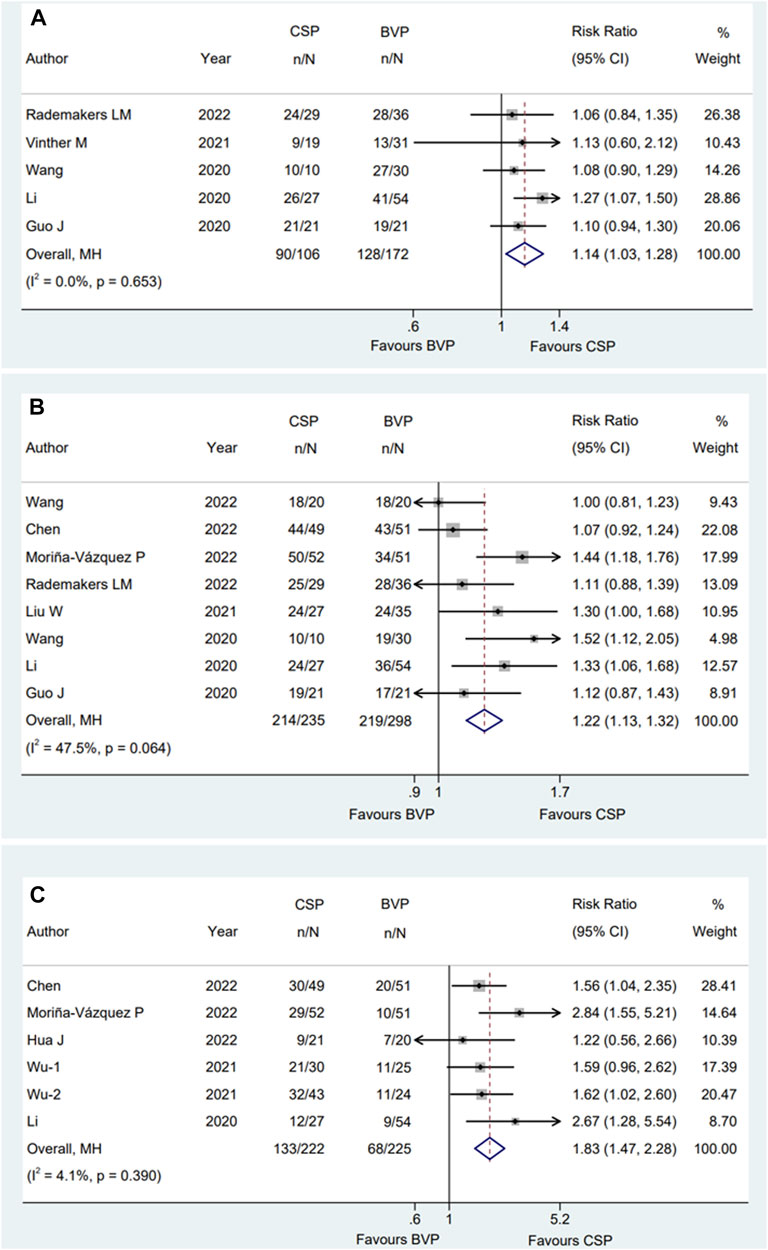
FIGURE 6. Forest plot of clinical response rate, echo response rate and super response rate between CSP and BVP. (A) Clinical response rate, (B) echo response rate, (C) super response rate. CSP, conduction system pacing; BVP, biventricular pacing; RR, risk ratio; CI, confidence interval.
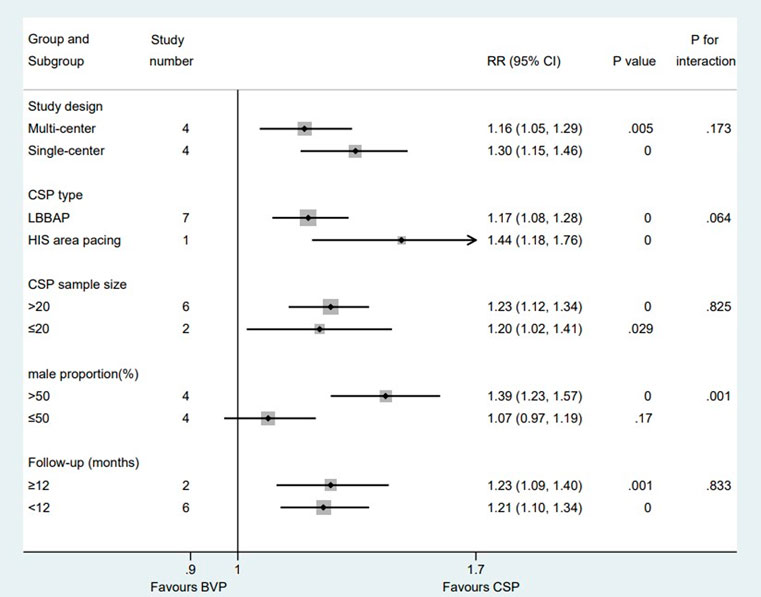
FIGURE 7. Subgroup analysis of echo response rate between CSP and BVP. Subgroup analysis was performed based on five confounding factors. CSP, conduction system pacing; BVP, biventricular pacing; RR, risk ratio; CI, confidence interval.
Publication bias was not found from Egger’s test for all primary outcomes, sensitivity analysis of these outcomes was largely similar (Supplementary Table S11).
The data of all-cause death, complication and HF rehospitalization was presented in Supplementary Table S12. The average time of observation was 11.0 ± 7.1 months, 10.8 ± 7.4 months and 11.4 ± 7.6 months for all-cause death, complication and HF rehospitalization. The rate of all-cause death in CSP group (53/639 [8.3%]) is similar to that of BVP group (55/615 [8.9%]) [RR:0.81; 95% CI (0.58,1.14); p = 0.230]. The incidence of complications in CSP group (14/614 [2.3%]) is lower than that in BVP group (25/531 [4.7%]) but this did not reach statistical significance [RR:0.56; 95% CI (0.29,1.07); p = 0.079]. A total of 140 HFH (heart failure rehospitalization) occurred during the follow-up period. Pooled results with fixed effect model showed that there was a significant decrease in HFH in CSP group (51/571 [8.9%]) compared to that in BVP group (89/540 [16.5%]) [ RR:0.45; 95% CI (0.33,0.62); p = 0.000].
In this meta-analysis, a total of fifteen eligible studies were enrolled to evaluate the clinical outcomes between two different pacing types (conduction system pacing vs biventricular pacing) for HF patients, and the main findings are as follows: 1) CSP is superior to conventional BVP for HF patients in terms of the clinical benefits, efficacy and prognosis; 2) CSP might be associated with more benefits than BVP In a higher male proportion group; 3) LBBaP may offer advantages over HBP for CRT due to a similar electromechanical resynchronization but lower pacing thresholds.
In order to further analyze the advantages of CSP, we conducted a subgroup analysis of five confounding factors. For the first time, we found that CSP had better efficacy (including shorter QRSd, higher echo response rate, and lower NYHA grade) with higher male proportion subgroup. Moreover, NYHA grade is lower in multi-centered groups than single-centered group and CSP sample size>20 groups were superior to that in ≤20 groups in terms of improvement of NYHA. Interestingly, CSP did not lead to lower NYHA grade and higher echo response rate than BVP (p > 0.05) in subgroups with lower male proportion, which is consistent with our findings that CSP tends to result in better cardiac function in male patients. In the CSP sample size ≤20 subgroup, CSP brings the final NYHA grade and improvement of NYHA similar to BVP, probably due to the inherent limitations of studies with small population included. Additionally, there was no statistical difference between HBP group and BVP group in final NYHA grade and improvement of NYHA, the reason for that might be that there are only two studies included and the population was too small to cause significant difference.
The controversies still remained on the efficacy of CRT for HF patients with different gender. The SMART-AV RCT showed a similar CRT response between male and female HF patients (Howell et al., 2021), while an Adapt Response RCT including 1,569 (43.3%) women patients with CRT indication found that the baseline characteristics and living quality between women and men were different, which may result in differences in clinical outcomes (Wilkoff et al., 2020). Waard et al. reported that women have significant reduced rates of death and HF hospitalization compared with men receiving CRT-D. what’s more, men were more likely to develop ventricular arrhythmias than women (de Waard et al., 2019). Whereas, our study showed that compared with BVP, male patients might contribute to better outcomes in CSP.
CSP mainly consisted of two different types, including HBP and LBBaP. Accumulated clinical studies revealed that patients with HF often have impaired His-Purkinje conduction, frequently manifested as LBBB. With the pacing lead directly implanted in the native conduction system, HBP can completely restore physiologic his-Purkinje conduction, which may be more beneficial to promote remodeling than BVP (Sharma et al., 2018; Upadhyay et al., 2019b; Huang et al., 2019). Arnold et al. (2018) found that compared with BVP, HBP provides greater improvement in hemodynamic parameters and better ventricular resynchronization, which further leads to the improvement of cardiac function. Therefore, His bundle pacing is considered to be a feasible alternative to conventional BVP in symptomatic HF patients. However, several limitations like high LBBB correction threshold and late threshold increase may restrict the wide clinical application of HBP (Hua et al., 2022b). Our meta-analysis included seven studies (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vijayaraman et al., 2019; Vinther et al., 2021; Wu et al., 2021; Moriña-Vázquez et al., 2022; Vijayaraman et al., 2022) delivering HBP-CRT. The pacing thresholds were higher than BVP in five of them (Lustgarten et al., 2015; Upadhyay et al., 2019b; Vijayaraman et al., 2019; Vinther et al., 2021; Wu et al., 2021). Four studies found the improvement in LVEF was superior in patient who underwent HBP to those received BVP (Vinther et al., 2021; Wu et al., 2021; Moriña-Vázquez et al., 2022; Vijayaraman et al., 2022), while there was no difference between HBP and BVP in the His-SYNC pilot trail, it reported similar improvement in LVEF (7.9% vs 5.9%, p > 0.05), this may have been due to high crossover rate (48% of HBP group and 26% of BVP group) between the operation arms and the high proportion of patients with nonspecific intraventricular conduction defects (Upadhyay et al., 2019b). Similarly, HBP did not brought higher improvement than BVP in the study delivered by Lustgarten et al. probably due to this was a crossover design comparison study (Lustgarten et al., 2015), which gives us an inspiration to reduce the crossover rate between different CRT groups.
LBBaP is a new technique aimed at correcting the desynchrony of LBB conduction. It provides an alternative strategy for delivering CSP and can overcome many limitations of HBP. First of all, LBBaP corrects LBBB with a significantly lower pacing threshold than HBP, partly due to it delivers pacing beyond the site of conduction block. In addition, the lead is positioned closer to myocardial tissue, leading to higher R-wave amplitude with LBBaP. secondly, LBBaP has higher implant success rates, and the procedure time for LBBaP lead implantation was shorter than BVP. Thirdly, LBBaP can achieve left ventricular mechanical synchronization similar to that of HBP, but with better pacing parameters (Liu et al., 2021b; Wu et al., 2021; Moore et al., 2022). Recently, Palmisano et al. (2023) conducted a study comparing the long-term risk of device-related complications between CSP and BVP using propensity-matched analysis. The results showed that HBP showed a significantly higher risk of complications than LBBaP, which is another advantage for LBBaP. For the limitations above, HBP still showed some advantages over LBBaP, Ali et al. (2023) found that HBP delivered better ventricular resynchronization than LBBaP because right ventricular activation was slower during LBBaP. We observed that LBBaP had significantly narrower QRSd, more LVEF improvement, better NYHA class and higher CRT response rates than BVP in this meta-analysis. And there is no difference between LBBaP and HBP in clinical benefits and efficacy. Considering the benefits above, LBBaP appears to be a promising method for delivering CRT.
The VENUS trial (Lador et al., 2021) analyzed the primary outcome in two categories: High-volume centers (>20 patients enrolled) versus low-volume centers. Similarly, we divided the researches included into CSP sample size >20 and ≤20 group with reference to the VENUS trial. Our analysis found that in sample size ≤20 subgroup, CSP did not show statistical difference in the narrowing of QRSd and improvement of NYHA class, suggesting that when technical aspects of CSP are not mature, the effect of CSP might not be so significant.
The multicenter trial can enroll a larger number of subjects, cover a wide range of areas and avoid the limitations that may exist in single-center research, facilitating to a significant and credible the study conclusions. Our meta-analysis found that patients in multi-center groups were associated with significantly improved NYHA class compared with single-center group. The advantages of multi-center may account for the difference.
Moreover, the subgroup analysis found that no difference exists in both follow-up subgroups with all clinical outcomes. This may be attributed to the short follow-up period of the articles we included. Only two studies (Hua et al., 2022a; Vijayaraman et al., 2022) were followed up for about 24 months, and the remaining studies ranged from 6 to 12 months. One study found Permanent HBP was safe and effective during long-term follow-up with a median follow up of 3 years (Zanon et al., 2019). While another study revealed that the elevated capture thresholds, loss of His-bundle capture, and lead revision rates of HBP at intermediate follow-up (median 19.5 months) are of concern (Teigeler et al., 2021). The short-term and intermediate-term performance and safety of LBBaP has been proved, the comparison of long-term efficacy and safety between CSP and BVP remains unclear, studies recruiting more patients with longer follow-up periods and needed.
Several potential limitations in our study should be highlighted. First, only four of fifteen eligible studies are RCT studies, and multiple potential confounding factors (such as selection bias and operator bias) might be existed despite of a comparable baseline characteristics between CSP and BVP group. Therefore, we conducted a subgroup analysis for different pacing outcomes between RCT subgroup and non-RCT subgroup, and the primary outcomes between two subgroups (such as the final QRSd, shortening of QRSd, the final LVEF, improvement of LVEF) showed the similar trends with our pooled results (Supplementary Table S13), indicated that our results are relatively robust. However, more randomized trials should be performed to further demonstrate our findings. Second, the number of patients included is relatively small, which means that the patients may not be sufficiently representative. Third, the follow-up was relatively not longer, the long-term (e.g., 3-year, 5-year or 10-year follow-up) effects of CSP on cardiac function and mechanical synchrony need to be confirmed by studies recruiting more patients with longer follow-up periods. Finally, since LBBaP was first developed by Huang’s team, a total eight of twelve eligible studies (Guo et al., 2020; Li et al., 2020; Wang et al., 2020; Liu et al., 2021a; Wu et al., 2021; Hua et al., 2022a; Chen et al., 2022; Wang et al., 2022) were derived from Chinese electrophysiology centers. Difference in proficiency and skills of the electrophysiologists may influence the comparative efficacy of LBBaP versus BVP for CRT.
This study suggests that CSP might be superior to conventional BVP for HF patients. In a higher male proportion group, CSP may be associated with more benefits than BVP.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
R-XW developed the concept of the study; JZ, FL, Z-YZ designed this study and carried out the data analysis; FL, JZ, and Z-YZ conducted meta-analysis registration in PROSPERO platform with the help from R-XW; JZ wrote the manuscript with help from FL, Z-YZ, FY, QK, J-YC, LZ, H-HL, X-FC, Y-HY, and R-XW provided critical reviews of the paper. All authors have read and approved the final manuscript.
This work was supported by the Natural Science Foundation of China (81770331).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2023.1125340/full#supplementary-material
Ali, N., Arnold, A. D., Miyazawa, A. A., Keene, D., Chow, J. J., Little, I., et al. (2023). Comparison of methods for delivering cardiac resynchronization therapy: An acute electrical and haemodynamic within-patient comparison of left bundle branch area, his bundle, and biventricular pacing. Europace 25, 1060–1067. doi:10.1093/europace/euac245
Arnold, A. D., Shun-Shin, M. J., Keene, D., Howard, J. P., Sohaib, S. M. A., Wright, I. J., et al. (2018). His resynchronization versus biventricular pacing in patients with heart failure and left bundle branch block. J. Am. Coll. Cardiol. 72 (24), 3112–3122. doi:10.1016/j.jacc.2018.09.073
Chen, X., Ye, Y., Wang, Z., Jin, Q., Qiu, Z., Wang, J., et al. (2022). Cardiac resynchronization therapy via left bundle branch pacing vs. optimized biventricular pacing with adaptive algorithm in heart failure with left bundle branch block: A prospective, multi-centre, observational study. Europace 24 (5), 807–816. doi:10.1093/europace/euab249
de Waard, D., Manlucu, J., Gillis, A. M., Sapp, J., Bernick, J., Doucette, S., et al. (2019). Cardiac resynchronization in women: A substudy of the resynchronization-defibrillation for ambulatory heart failure trial. JACC Clin. Electrophysiol. 5 (9), 1036–1044. doi:10.1016/j.jacep.2019.06.007
Ellenbogen, K. A., and Huizar, J. F. (2012). Foreseeing super-response to cardiac resynchronization therapy: A perspective for clinicians. J. Am. Coll. Cardiol. 59 (25), 2374–2377. doi:10.1016/j.jacc.2011.11.074
Guo, J., Li, L., Xiao, G., Ye, T., Huang, X., Meng, F., et al. (2020). Remarkable response to cardiac resynchronization therapy via left bundle branch pacing in patients with true left bundle branch block. Clin. Cardiol. 43 (12), 1460–1468. doi:10.1002/clc.23462
Howell, S., Stivland, T. M., Stein, K., Ellenbogen, K., and Tereshchenko, L. G. (2021). Response to cardiac resynchronisation therapy in men and women: A secondary analysis of the SMART-AV randomised controlled trial. BMJ Open 11 (10), e049017. Published 2021 Oct 27. doi:10.1136/bmjopen-2021-049017
Hua, J., Chen, Y., Yu, J., Xiong, Q., Xia, Z., Xia, Z., et al. (2022). Long-term outcomes of left bundle branch area pacing versus biventricular pacing in patients with heart failure and complete left bundle branch block. Heart Vessels 37 (7), 1162–1174. doi:10.1007/s00380-021-02016-5
Hua, J., Wang, C., Kong, Q., Zhang, Y., Wang, Q., Xiong, Z., et al. (2022). Comparative effects of left bundle branch area pacing, his bundle pacing, biventricular pacing in patients requiring cardiac resynchronization therapy: A network meta-analysis. Clin. Cardiol. 45 (2), 214–223. doi:10.1002/clc.23784
Huang, W., Su, L., Wu, S., Xu, L., Xiao, F., Zhou, X., et al. (2017). A novel pacing strategy with low and stable output: Pacing the left bundle branch immediately beyond the conduction block. Can. J. Cardiol. 33 (12), 1736. doi:10.1016/j.cjca.2017.09.013
Huang, W., Su, L., Wu, S., Xu, L., Xiao, F., Zhou, X., et al. (2019). Long-term outcomes of his bundle pacing in patients with heart failure with left bundle branch block. Heart 105 (2), 137–143. doi:10.1136/heartjnl-2018-313415
Lador, A., Peterson, L. E., Swarup, V., Schurmann, P. A., Makkar, A., Doshi, R. N., et al. (2021). Determinants of outcome impact of vein of marshall ethanol infusion when added to catheter ablation of persistent atrial fibrillation: A secondary analysis of the VENUS randomized clinical trial. Heart rhythm. 18 (7), 1045–1054. doi:10.1016/j.hrthm.2021.01.005
Li, F., Sun, J. Y., Wu, L. D., Zhang, L., Qu, Q., Wang, C., et al. (2022). The long-term outcomes of ablation with vein of marshall ethanol infusion vs. ablation alone in patients with atrial fibrillation: A meta-analysis. Front. Cardiovasc Med. 9, 871654. doi:10.3389/fcvm.2022.871654
Li, X., Qiu, C., Xie, R., Ma, W., Wang, Z., Li, H., et al. (2020). Left bundle branch area pacing delivery of cardiac resynchronization therapy and comparison with biventricular pacing. Esc. Heart Fail 7 (4), 1711–1722. doi:10.1002/ehf2.12731
Liu, P., Wang, Q., Sun, H., Qin, X., and Zheng, Q. (2021). Left bundle branch pacing: Current knowledge and future prospects. Front. Cardiovasc Med. 8, 630399. doi:10.3389/fcvm.2021.630399
Liu, W., Hu, C., Wang, Y., Cheng, Y., Zhao, Y., Liu, Y., et al. (2021). Mechanical synchrony and myocardial work in heart failure patients with left bundle branch area pacing and comparison with biventricular pacing. Front. Cardiovasc Med. 8, 727611. Published 2021 Aug 20. doi:10.3389/fcvm.2021.727611
Lustgarten, D. L., Crespo, E. M., Arkhipova-Jenkins, I., Lobel, R., Winget, J., Koehler, J., et al. (2015). His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: A crossover design comparison. Heart rhythm. 12 (7), 1548–1557. doi:10.1016/j.hrthm.2015.03.048
Moore, J. P., de Groot, N. M. S., and O'Connor, M. (2022). Conduction system pacing versus conventional cardiac resynchronization therapy in congenital heart disease. JACC Clin. Electrophysiol. S2405-500X (22), 00863–00865. doi:10.1016/j.jacep.2022.10.012
Moriña-Vázquez, P., Moraleda-Salas, M. T., Rodríguez-Albarrán, A., Arce-León, Á., Venegas-Gamero, J., Fernández-Gómez, J. M., et al. (2022). Cardiac resynchronization therapy in non-ischemic cardiomyopathy: A comparative non-randomized study of his bundle pacing versus biventricular pacing. J. Interv. Card. Electrophysiol. 2022, 1192. doi:10.1007/s10840-022-01192-2
Palmisano, P., Ziacchi, M., and Dell'Era, G. (2023). Rate and nature of complications of conduction system pacing compared with right ventricular pacing: Results of a propensity-matched analysis from a multicentre registry. Heart rhythm. S1547-5271 (23), 00226–6. doi:10.1016/j.hrthm.2023.03.009
Ploux, S., Eschalier, R., Whinnett, Z. I., Lumens, J., Derval, N., Sacher, F., et al. (2015). Electrical dyssynchrony induced by biventricular pacing: Implications for patient selection and therapy improvement. Heart rhythm. 12 (4), 782–791. doi:10.1016/j.hrthm.2014.12.031
Rademakers, L. M., van den Broek, J. L. P. M., and Bracke, F. A. (2022). Left bundle branch pacing as an alternative to biventricular pacing for cardiac resynchronisation therapy. Neth Heart J. 31, 140–149. doi:10.1007/s12471-022-01712-9
Sharma, P. S., Dandamudi, G., Herweg, B., Wilson, D., Singh, R., Naperkowski, A., et al. (2018). Permanent his-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: A multicenter experience. Heart rhythm. 15 (3), 413–420. doi:10.1016/j.hrthm.2017.10.014
Teigeler, T., Kolominsky, J., Vo, C., Shepard, R. K., Kalahasty, G., Kron, J., et al. (2021). Intermediate-term performance and safety of his-bundle pacing leads: A single-center experience. Heart rhythm. 18 (5), 743–749. doi:10.1016/j.hrthm.2020.12.031
Upadhyay, G. A., Vijayaraman, P., Nayak, H. M., Verma, N., Dandamudi, G., Sharma, P. S., et al. (2019). His corrective pacing or biventricular pacing for cardiac resynchronization in heart failure. J. Am. Coll. Cardiol. 74 (1), 157–159. doi:10.1016/j.jacc.2019.04.026
Upadhyay, G. A., Vijayaraman, P., Nayak, H. M., Verma, N., Dandamudi, G., Sharma, P. S., et al. (2019). On-treatment comparison between corrective his bundle pacing and biventricular pacing for cardiac resynchronization: A secondary analysis of the his-SYNC pilot trial. Heart rhythm. 16 (12), 1797–1807. doi:10.1016/j.hrthm.2019.05.009
Vijayaraman, P., Herweg, B., Ellenbogen, K. A., and Gajek, J. (2019). His-Optimized cardiac resynchronization therapy to maximize electrical resynchronization: A feasibility study. Circ. Arrhythm. Electrophysiol. 12 (2), e006934. doi:10.1161/CIRCEP.118.006934
Vijayaraman, P., Zalavadia, D., Haseeb, A., Dye, C., Madan, N., Skeete, J. R., et al. (2022). Clinical outcomes of conduction system pacing compared to biventricular pacing in patients requiring cardiac resynchronization therapy. Heart rhythm. 19 (8), 1263–1271. doi:10.1016/j.hrthm.2022.04.023
Vinther, M., Risum, N., Svendsen, J. H., Møgelvang, R., and Philbert, B. T. (2021). A randomized trial of his pacing versus biventricular pacing in symptomatic HF Patients with left bundle branch block (his-alternative). JACC Clin. Electrophysiol. 7 (11), 1422–1432. doi:10.1016/j.jacep.2021.04.003
Wang, Y., Gu, K., Qian, Z., Hou, X., Chen, X., Qiu, Y., et al. (2020). The efficacy of left bundle branch area pacing compared with biventricular pacing in patients with heart failure: A matched case-control study. J. Cardiovasc Electrophysiol. 31 (8), 2068–2077. doi:10.1111/jce.14628
Wang, Y., Zhu, H., Hou, X., Wang, Z., Zou, F., Qian, Z., et al. (2022). Randomized trial of left bundle branch vs biventricular pacing for cardiac resynchronization therapy. J. Am. Coll. Cardiol. 80 (13), 1205–1216. doi:10.1016/j.jacc.2022.07.019
Wilkoff, B. L., Birnie, D., Gold, M. R., Hersi, A. S., Jacobs, S., Gerritse, B., et al. (2020). Differences in clinical characteristics and reported quality of life of men and women undergoing cardiac resynchronization therapy. Esc. Heart Fail 7 (5), 2972–2982. doi:10.1002/ehf2.12914
Wu, S., Su, L., Vijayaraman, P., Zheng, R., Cai, M., Xu, L., et al. (2021). Left bundle branch pacing for cardiac resynchronization therapy: Nonrandomized on-treatment comparison with his bundle pacing and biventricular pacing. Can. J. Cardiol. 37 (2), 319–328. doi:10.1016/j.cjca.2020.04.037
Zanon, F., Abdelrahman, M., Marcantoni, L., Naperkowski, A., Subzposh, F. A., Pastore, G., et al. (2019). Long term performance and safety of his bundle pacing: A multicenter experience. J. Cardiovasc Electrophysiol. 30 (9), 1594–1601. doi:10.1111/jce.14063
Keywords: left bundle branch area pacing, cardiac resynchronization therapy, biventricular pacing, heart failure, his bundle pacing (HBP)
Citation: Zhang J, Li F, Zhang Z-Y, Yang F, Kong Q, Chen J-Y, Zhang L, Liu H-H, Chen X-F, Ye Y-H and Wang R-X (2023) Conduction system pacing is superior to biventricular pacing in patients with heart failure: Insights from the pooled clinical studies. Front. Physiol. 14:1125340. doi: 10.3389/fphys.2023.1125340
Received: 16 December 2022; Accepted: 26 April 2023;
Published: 05 May 2023.
Edited by:
Christopher Aldo Rinaldi, St Thomas’ Hospital, United KingdomReviewed by:
Maciej M. Sterlinski, National Institute of Cardiology, PolandCopyright © 2023 Zhang, Li, Zhang, Yang, Kong, Chen, Zhang, Liu, Chen, Ye and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ru-Xing Wang, cnV4aW5nd0BhbGl5dW4uY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.