
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Physiol., 26 January 2023
Sec. Exercise Physiology
Volume 14 - 2023 | https://doi.org/10.3389/fphys.2023.1079841
This article is part of the Research TopicPhysical activity and fitness for the Prevention and Management of Bone DiseasesView all 13 articles
A correction has been applied to this article in:
Corrigendum: The effects of Tai Chi on physical function and safety in patients with rheumatoid arthritis: a systematic review and meta-analysis
Background: Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory autoimmune disease that results in the destruction of joints, connective tissues, muscle, tendons and fibrous tissue. Until now, there are no cure therapies.
Objective: We aimed to assess the effectiveness of Tai Chi (TC) on RA patients by meta-analysis.
Methods: The PubMed, Cochrane Library, EMBASE, web of science, China National Knowledge Infrastructure and Google Scholar were searched up to January 2023. We included randomized controlled trials (RCTs) or controlled clinical trials (CCTs) comparing TC to control conditions for RA patients. Review Manager (Version 5.3) software was used to analyze outcomes of time to walk 50 feet, joint tenderness, number of swollen joints or tender joints, handgrip strength, pain, the Health Assessment Questionnaire (HAQ) and withdraws overall.
Results: A total of 351 patients with RA from six RCTs and three CCTs were included for meta-analysis. TC could also significantly decrease withdrawals overall in studies (OR = 0.28, 95% CI 0.12 to 0.67, p = 0.002). No significant treatment effects of physical function were identified of the other outcomes.
Conclusion: Our findings indicated that TC was safe to RA patients, but it cannot improve physical function and pain. However, there is still lack of more evidence.
Systematic Review Registration: [https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=367498], identifier [CRD42022367498].
Rheumatoid arthritis (RA) is a prevalent disease with incidence by 8.2% (Finckh et al., 2022). RA presents a systemic inflammatory autoimmune disease that destroys the joints, connective tissues, muscle, tendons and fibrous tissue. The accurate aetiology of RA is still ambiguous, but it is well known that the development of RA is associated with genetic susceptibility, environmental factors and immune response (Scherer et al., 2020; Testa et al., 2021). RA is often progressive and primarily involves the pain, stiffness and swelling of joints (Han et al., 2004). Some extra-articular manifestations also usually happen, such as cardiovascular disease, respiratory disease, central and peripheral nervous system (Figus et al., 2021). When compared to the general population, those with RA have a 50% greater risk of cardiovascular death (Finckh et al., 2022). RA brings a substantial burden for both the individual and society, because of decline in physical function, quality of life, work capacity and societal participation, and major direct medical costs (Hsieh et al., 2020). Current therapeutic approaches for RA includes pharmacological and non-pharmacological approaches. Pharmacological methods refer to disease-modifying antirheumatic drugs, non-steroidal anti-inflammatory drugs, glucocorticoids and biological drugs (Fraenkel et al., 2021). Regarding non-pharmacological approaches, such as exercise, education, psychological and self-management therapies for RA patients were found to be beneficial in improving non-inflammatory symptoms (mainly functional disability, pain and fatigue) (Roodenrijs et al., 2021). However, no cure is currently available for RA (Nagy et al., 2022).
Recently, several clinical studies and systematic reviews suggested that physical activity attenuates inflammation, cardiovascular risk, psychological health and sleep in RA patients (Metsios et al., 2015; McKenna et al., 2017; Pope, 2020). As a mitigatory therapeutic exercise, Tai Chi (TC) has been practiced for centuries as a martial art in China. At the same time, it has been drawn more and more attention. After introduced to Europe and America, the viewpoints of TC shifted and it is nowadays well-known as a kind of exercise to treat patients with knee osteoarthritis (Wang et al., 2016). TC consists of a series of slow and purposeful movements that involve turning, shifting one’s weight from one leg to the other one, bending and unbending the legs with various arm movement, which is benefit for balance, flexibility, strength and function of human beings (Wu et al., 2004).
In RA, TC appears safe (Christie and Fongen, 2005) and improves pain and functional status of RA (Kirsteins et al., 1991; Wang et al., 2005; Wang, 2008). A review in year of 2004 by Han (Han et al., 2004) suggests that TC is beneficial on lower extremity range of motion for RA patients. However, in Han’s review the three included studies were only up to December 2003. Another review in year of 2019 by Mudano (Mudano et al., 2019) showed that it was uncertain whether TC had any effect on joint pain, activity limitation or function in RA, and important effects cannot be confirmed or excluded since all outcomes had very low-quality evidence. Nevertheless, an overview of systematic reviews suggests that clinical improvement of TC is achieved, although not statistically significant with regard to pain and disease pattern (Imoto et al., 2021). Additionally, a clinical study published in 2020 is not included in any systematic reviews or meta-analysis (Liang, 2020). Thus, the effectiveness of TC for RA is still considered unproven, because of lack of enough convincing evidence. Therefore, the aim of this study was to conduct a systematic review and meta-analysis for exploring effectiveness of TC and summarizing the existing literature.
The work was reported in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (Page et al., 2021) and registered in PROSPERO (registration identification: CRD42022367498; website: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=367498).
The search strategy was made by two reviewers (HYW and QW). They searched the following electronic databases (up to January 2023): PubMed, Cochrane Library, EMBASE, web of science, China National Knowledge Infrastructure and Google Scholar. The search strategy included “Tai Chi,” “Tai-Chi Chuan”, “Taiji” and “rheumatoid arthritis”. HYW manually screened conference proceedings (such as the International League of Associations for Rheumatology, the Chinese Rheumatology Association, and Chinese Journal of Rheumatology) and files from our department as supplemental material. Details of the English search strategy were shown in the Supplementary Appendix S1.
All studies searched were imported into Endnote X9. Firstly, two reviewers (HYW and QW) screened the titles and abstracts relevant to TC for patients suffering from RA independently. Then still independently these two reviewers read full articles and identified whether the study to be included or not according to the following inclusion criteria. Disagreements were solved by JHW. All the reviewers were trained together to fully understand the inclusion criteria, exclusion criteria and using method of Endnote software before starting selection.
Participants were adults (16 years of age and older) suffering from RA. Patients were diagnosed by rheumatologists or clinicians in the department of rheumatology.
The eligible trials should be TC therapy which compared with no therapy, usual care, sham therapy or any active treatment. Different types of TC protocol and co-interventions were allowed. Additionally, there were no limitations of the frequency of TC exercise, time of every intervention or the duration of trials.
1 Main outcomes (physical function): Time to walk 50 feet, joint tenderness, number of swollen joints or tender joints, handgrip strength, pain and HAQ.
2 Additional outcome (safety): Withdrawals overall.
Randomized controlled trials (RCTs) and controlled clinical trials (CCTs) were considered whether published or not in this review. Studies were included without language limitations.
The risk of bias was assessed using Review Manager software (Version 5.3.5, The Nordic Cochrane Centre, Copenhagen; available from: http://community.cochrane.org) and the 2011 revised Guidelines and Handbooks for Systematic Reviews in the Cochrane Back Review Group (Cumpston, 2011) by two reviewers (HYW and GWW). This handbook recommended seven quality criteria, each of which was rated with yes, no or unclear. Details of seven quality criteria were as follows: Random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias) and other bias. Disagreements were solved by a third party (YRW). A study would not be excluded even with a high risk, but it might degrade our confidence to recommend this cure strategy.
Two reviewers (HYW and QW) extracted data from the included studies independently by a pre-pilot standardized form, which included first authors’ last names, publication years, types of studies, characteristics of interventions and participants (included TC and comparison groups), outcome measures of effectiveness (efficacy of functional and clinical outcomes) and safety (withdrawals overall), methodological qualities, allocation concealments and durations of studies. Disagreements were solved by a third investigator (JHW) with discussion.
The extracted data were divided into two parts: characteristics of studies were shown in a table, outcome measures of effectiveness and side effects were imported into the Review Manager software for performing meta-analysis. The outcomes of effectiveness data in the TC and control groups were used to estimate the mean difference (MD) and 95% confidence intervals (CIs). The outcomes of safety data were in terms of odds ratio (OR). All reported values were two sided and p < 0.05 was considered to be statistically significant. All the data was performed on the Review Manager software by one reviewer (HYW).
Regarding the methodological (methodology of included studies) and clinical (clinical characteristics of the participants) heterogeneity, we evaluated as not homogeneous due to different intervention periods and various countries of subjects. Based on these, random-effect model was used to perform the analysis.
After searching the electronic databases, websites (Google Scholar) and paper sources, we collected 425 articles. However, in the electronic databases 106 articles were excluded based on titles and abstracts after duplicates removed, only 13 records were screened by reading full texts. Among these, three studies did not include control group (Uhlig et al., 2005; Uhlig et al., 2010; Waite-Jones et al., 2013), the variable is auricular acupressure in one study (Lee et al., 2012), and participants were same in one study (Wang et al., 2005) with another included study (Wang, 2008). Regarding the websites results, the first three hundred records were evaluated, but there were no studies that could be included. In addition, two studies were found in paper journals, but did not meet the inclusion criteria. Finally, as two independent CCTs in the same article (Kirsteins et al., 1991), nine trials from eight articles included were analyzed (Van Deusen and Harlowe, 1987; Kirsteins et al., 1991; Zhu et al., 1999; Lee, 2005; Lee and Jeong, 2006; Wang, 2008; Shin et al., 2015; Liang, 2020). The difference lies in the frequency of TC intervention (details in Figure 1).
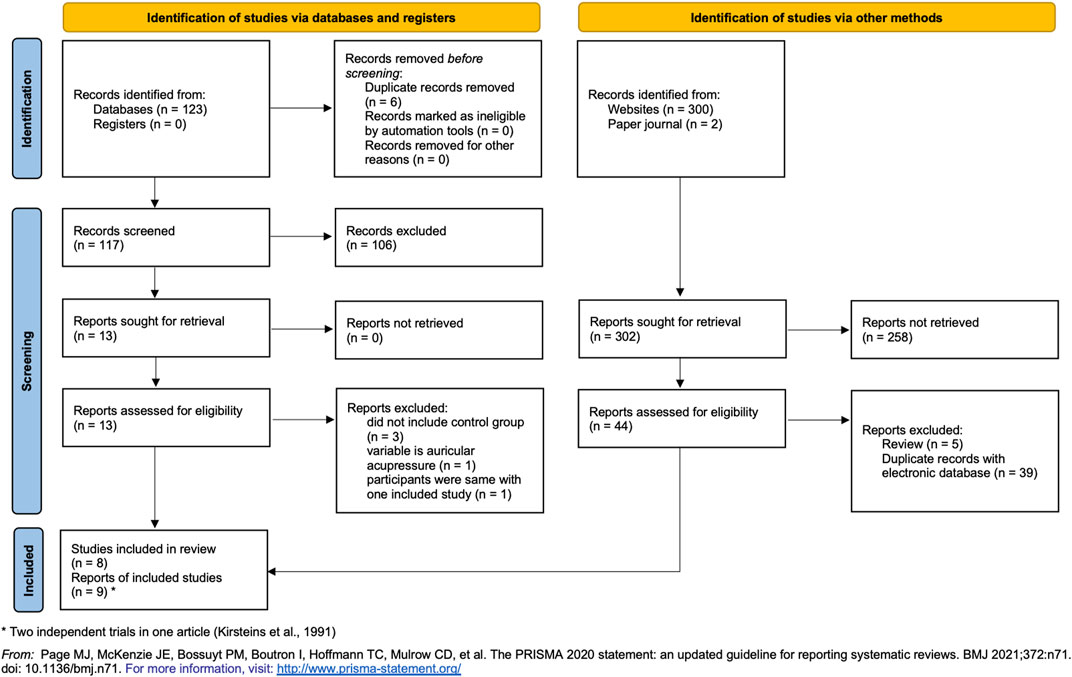
FIGURE 1. Flowchart of trial selection process. * Two trials in one article (Kirsteins et al., 1991).
The recruited articles were published from 1987 to 2020 years. The sample size ranged from 20 (Wang, 2008; Liang, 2020) to 68 (Zhu et al., 1999). All studies were single-center studies, while only one study was a multicenter one (Kirsteins et al., 1991). 351 RA participants were analyzed in this review. All patients satisfied the American College of Rheumatology 1987 revised classification criteria for RA. The frequency of TC was twice weekly (Kirsteins et al., 1991; Wang, 2008), once a week (Van Deusen and Harlowe, 1987; Kirsteins et al., 1991; Lee, 2005; Lee and Jeong, 2006; Shin et al., 2015) or once a day (Zhu et al., 1999; Liang, 2020). The duration of TC was 6 weeks (Lee, 2005), 8 weeks (Van Deusen and Harlowe, 1987; Zhu et al., 1999), 10 weeks (Kirsteins et al., 1991) and 12 weeks (Wang, 2008; Shin et al., 2015; Liang, 2020). The control groups were adopted usual activities without TC, advice about lifestyle, rest at home or oral the same medicine of TC group. The time to walk 50 feet was described in three studies (Kirsteins et al., 1991; Wang, 2008), joint tenderness in three studies (Kirsteins et al., 1991; Wang, 2008), the number of swollen joints in four studies (Kirsteins et al., 1991; Wang, 2008; Shin et al., 2015; Liang, 2020), the number of tender joints in two studies (Wang, 2008; Shin et al., 2015), handgrip strength in three studies (Kirsteins et al., 1991; Wang, 2008), pain in three studies (Lee, 2005; Lee and Jeong, 2006; Wang, 2008), HAQ in two studies (Wang, 2008; Shin et al., 2015; Liang, 2020), withdrawals overall during the study (Van Deusen and Harlowe, 1987; Kirsteins et al., 1991; Zhu et al., 1999). No studies described patients’ cost (details in Table 1).
The final results were shown in the form of summary (Figure 2) and graph (Figure 3). All studies had low risks of attrition bias, reporting bias and other bias. Selection bias of random sequence generation was high in four studies (Kirsteins et al., 1991; Zhu et al., 1999; Lee and Jeong, 2006) and was low in the other five studies (Van Deusen and Harlowe, 1987; Lee, 2005; Wang, 2008; Shin et al., 2015; Liang, 2020). Selection bias of allocation concealment was high in six studies (Kirsteins et al., 1991; Zhu et al., 1999; Lee and Jeong, 2006; Shin et al., 2015; Liang, 2020), unclear in two studies (Van Deusen and Harlowe, 1987; Lee, 2005) and low in one study (Wang, 2008). Performance bias of blinding of participants and personnel was high in seven studies (Kirsteins et al., 1991; Zhu et al., 1999; Lee, 2005; Lee and Jeong, 2006; Wang, 2008; Liang, 2020) and was low in the other two studies (Van Deusen and Harlowe, 1987; Shin et al., 2015). Detection bias blinding of outcome assessment was high in all the included studies.

FIGURE 2. Risk of bias graph. Review authors’ judgements about each risk of bias item presented as percentages across all included studies.
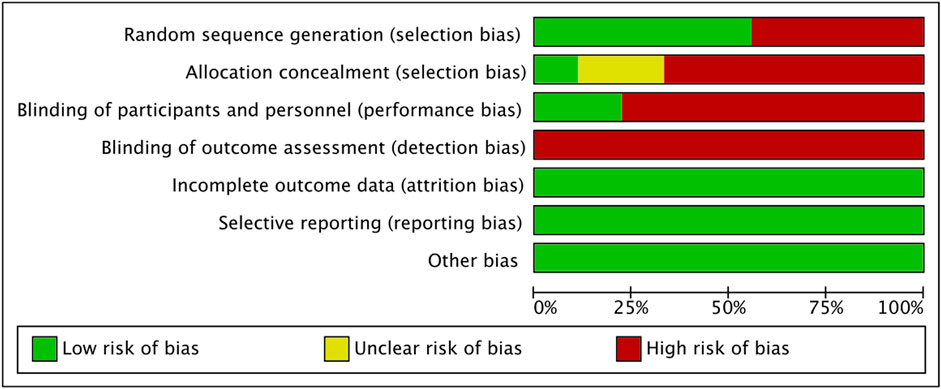
FIGURE 3. Risk of bias summary. Review authors’ judgements about each risk of bias item for each included study.
Regarding the risk of bias of individual studies, four trials (tow trials from one study) were considered with high risk (Kirsteins et al., 1991; Zhu et al., 1999; Lee and Jeong, 2006). In contrast, two studies were rated as medium risk (Lee, 2005; Liang, 2020) and three studies as low risk (Van Deusen and Harlowe, 1987; Wang, 2008; Shin et al., 2015).
We collected the data from three studies (Kirsteins et al., 1991; Wang, 2008) together and acquired evidence that TC therapy could not significantly improve time to walk 50 feet, with MD 0.17 (95% CI −1.06–1.40) in a random effect model (Figure 4). Tow independent CCTs were from one article (Kirsteins et al., 1991).
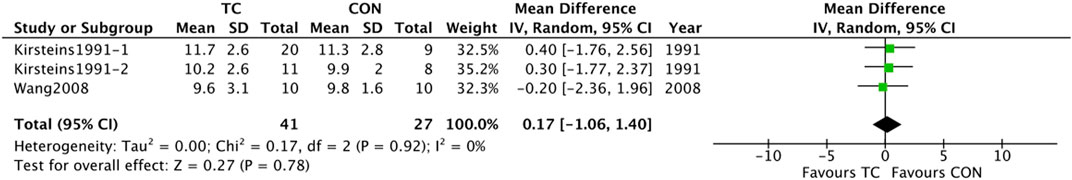
FIGURE 4. A Forest plot of the meta-analyses compared TC group with control group for changing in time to walk 50 feet.
The data from three studies (Kirsteins et al., 1991; Wang, 2008) were collected together and evidence was acquired that TC therapy could not significantly improve joint tenderness, with MD -0.01 (95% CI −0.32 to 0.29) in a random effect model (Figure 5). Tow independent CCTs were from one article (Kirsteins et al., 1991).
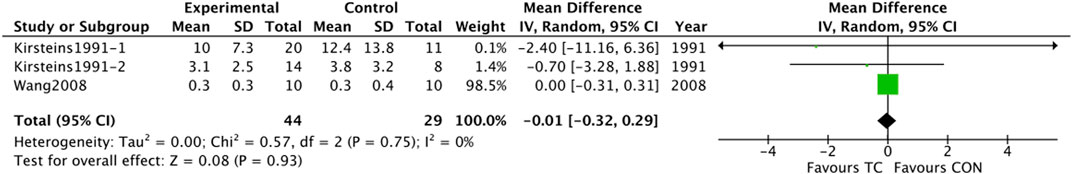
FIGURE 5. A Forest plot of the meta-analyses compared TC group with control group for changing in joint tenderness.
The data were collected from five studies (Kirsteins et al., 1991; Wang, 2008; Shin et al., 2015; Liang, 2020) suggested that TC therapy could not significantly improve number of swollen joints, with MD 0.50 (95% CI −2.09 to 3.10) in a random effect model (Figure 6). Tow independent CCTs were from one article (Kirsteins et al., 1991).
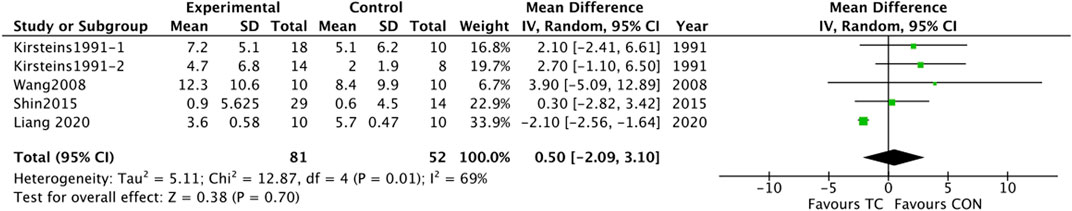
FIGURE 6. A Forest plot of the meta-analyses compared TC group with control group for changing in number of swollen joints.
The data from two studies (Wang, 2008; Shin et al., 2015) together indicated that TC therapy could not significantly improve number of tender joints, with MD 0.41 (95% CI −5.18 to 6.01) in a random effect model (Figure 7).
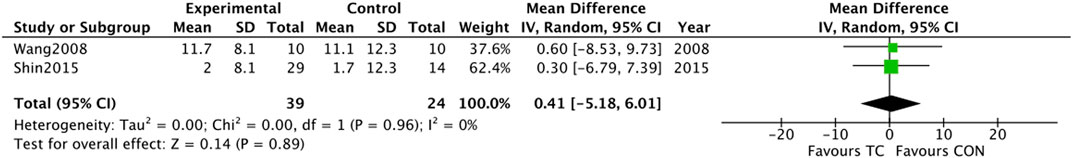
FIGURE 7. A Forest plot of the meta-analyses compared TC group with control group for changing in number of tender joints.
After the collection of the data from three studies (Kirsteins et al., 1991; Wang, 2008), the results showed that TC therapy could not significantly improve handgrip strength, with MD −0.08 (95% CI −0.26 to 0.10) in a random effect model (Figure 8). Tow independent CCTs were from one article (Kirsteins et al., 1991).
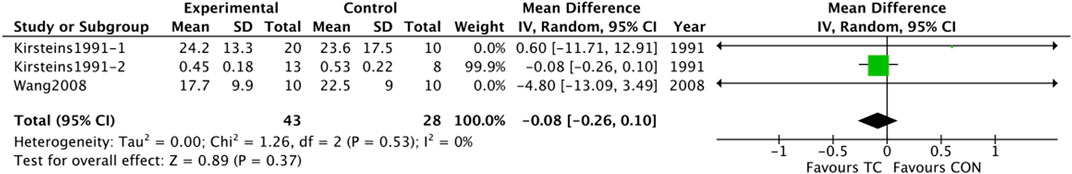
FIGURE 8. A Forest plot of the meta-analyses compared TC group with control group for changing in handgrip strength.
The data from three studies (Lee, 2005; Lee and Jeong, 2006; Wang, 2008) showed that TC therapy could not significantly improve pain, with MD −0.88 (95% CI −1.99 to 0.23) in a random effect model (Figure 9).
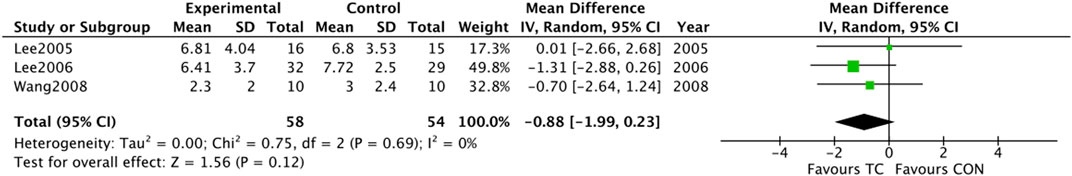
FIGURE 9. A Forest plot of the meta-analyses compared TC group with control group for changing in pain.
After the collection of the data from three studies (Wang, 2008; Shin et al., 2015; Liang, 2020), the results showed that TC therapy could not significantly improve HAQ, with MD −0.19 (95% CI −0.70 to 0.33) in a random effect model (Figure 10).
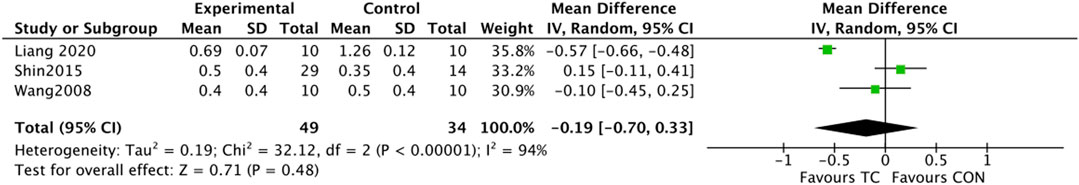
FIGURE 10. A Forest plot of the meta-analyses compared TC group with control group for changing in HAQ.
The data from four studies (Van Deusen and Harlowe, 1987; Kirsteins et al., 1991; Zhu et al., 1999) was combined and provided evidence that TC therapy could significantly improve withdrawals overall during the study, with OR 0.28 (95% CI 0.12–0.67) in a random effect model (Figure 11). Tow independent CCTs were from one article (Kirsteins et al., 1991).
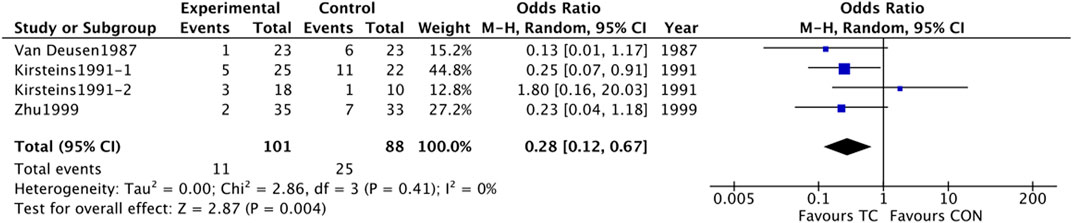
FIGURE 11. A Forest plot of the meta-analyses compared TC group with control group for changing in withdrawals overall.
351 participants were included in this meta-analysis from nine trials. Three of them were CCTs and six were RCTs in total. All patients were diagnosed by rheumatologists or clinicians in department of rheumatology. We used the collective data to perform a meta-analysis and found that TC could significantly improve the withdrawals overall during the study. Available data suggested that TC was not linked closely with serious adverse events. However, TC cannot improve physical functions of RA patients. Additionally, the included studies were assessed as having a relative high risk of bias. Four trials with high risk might greatly reduces the credibility of the results. Two studies rated with medium risk and three studies with low risk might have relatively small impact on the confidence of the results. Therefore, the confidence in the findings were seriously reduced.
RA is a second common form of arthritis. However, treating strategy is limited and medications are frequently toxic (Nagy et al., 2022). Therefore, RA patients turn to complementary and alternative therapies often (Zhao et al., 2017). The value of regular physical activity is well documented in the management of RA (Hu et al., 2021; Roodenrijs et al., 2021). Physical activity for patients with RA needs to be sustainable and enjoyable, however most of them have less physically active than the general population in fact (Hu et al., 2021). In addition, A systematic review about efficacy of occupational therapy-related interventions for adults with RA concluded strong evidence to support the use of aerobic exercise, such as TC (Siegel et al., 2017).
Recently, TC has been applied with substantial benefits in patients with RA. Intensity in TC is low and equivalent to walking 6 km/h and produces a secondary increase in heart rate (Jin, 1992), which comprised rhythmic movements and emphasis on body balance and coordination (Song et al., 2010). There are different kinds of actions, such as bend knees slightly, keep arms below the shoulder level, forward or backward strides, and turn around while shifting the center of gravity (Song et al., 2007). Although TC has lots of styles and flexible action details, it can be assumed that the major function of TC is similar. TC is considered safe in patients with RA, especially long-standing and dramatically physically inactive individuals (Kirsteins et al., 1991). This is the same with the withdraw overall outcome in our meta-analysis. TC could decrease the percentage of dropouts in trials.
Studies had demonstrated a favorable effect or tendency to improve physical function (Chen et al., 2016). A study indicated that the positive effects of TC were attributed to increases in the muscle strength and endurance of the lower extremity (Song et al., 2010). It may also help to improve body balance and stabilize the weighted joints thereby reducing the risk of falling (Wang, 2009). Additionally, another review about TC treating RA concluded that there were positive effects on a selected range of motion outcomes (Han et al., 2004). However, investigators thought that TC had no effectiveness of TC treating RA in another meta-analysis (Lee et al., 2007). Our results also showed TC cannot improve physical function of RA patients.
The primary limitation of this review is the small total number of eligible trials. Therefore, the results of the studies might or might not apply to the majority of RA patients; there were not enough studies for conclusive judgment, especially the side effects of TC. TC only could be assumed with a low risk of injury as a treatment method. In addition, we tried our best to search relevant articles in different ways, but we could not make sure that all the relevant studies were included. So, the bias from selecting the studies for inclusion in a meta-analysis could not be avoided.
The results of our systematic review and meta-analysis have provided the newest evidence on TC for the treatment of RA. It suggests that TC is a safe method to exercise for RA patients as the lower withdrawals overall. However, TC cannot improve physical function of RA patients. In addition, as the high risk of bias of included studies, the confidence in the findings was seriously reduced. More high-quality clinical studies are needed to further update the results.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Write manuscript, HW; search articles, HW and QW; assess risk of bias, HW and GW; finish the Table and Figures, QW; data analysis, HW and QW; solve disagreements, JW and YW; study design, YW.
Shanghai Huangpu Science and Technology Commission Scientific Research project to HW [grant numbers HKQ201903]. “Clinical research-oriented talents training program” in the Affiliated Hospital of Shanghai University of Traditional Chinese medicine to YW [grant number 2023LCRC01].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2023.1079841/full#supplementary-material
CCTs, controlled clinical trials; CIs, confidence intervals; HAQ, health assessment questionnaire; MD, mean difference; OR, odds ratio; RA, rheumatoid arthritis; RCTs, randomized controlled trials; TC, Tai Chi.
Chen, Y. W., Hunt, M. A., Campbell, K. L., Peill, K., and Reid, W. D. (2016). The effect of tai chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: A systematic review and meta-analyses. Br. J. Sports Med. 50 (7), 397–407. doi:10.1136/bjsports-2014-094388
Christie, A., and Fongen, C. (2005). Thai Chi may be safe though ineffective for rheumatoid arthritis. Aust. J. Physiother. 51 (4), 267. doi:10.1016/s0004-9514(05)70013-1
Cumpston, M. (2011). Assessing risk of bias in included studies. Available from: http://training.cochrane.org/resource/assessing-risk-bias-included-studies.
Figus, F. A., Piga, M., Azzolin, I., McConnell, R., and Iagnocco, A. (2021). Rheumatoid arthritis: Extra-articular manifestations and comorbidities. Autoimmun. Rev. 20 (4), 102776. doi:10.1016/j.autrev.2021.102776
Finckh, A., Gilbert, B., Hodkinson, B., Bae, S. C., Thomas, R., Deane, K. D., et al. (2022). Global epidemiology of rheumatoid arthritis. Nat. Rev. Rheumatol. 18 (10), 591–602. doi:10.1038/s41584-022-00827-y
Fraenkel, L., Bathon, J. M., England, B. R., St Clair, E. W., Arayssi, T., Carandang, K., et al. (2021). 2021 American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 73 (7), 1108–1123. doi:10.1002/art.41752
Han, A., Robinson, V., Judd, M., Taixiang, W., Wells, G., and Tugwell, P. (2004). Tai chi for treating rheumatoid arthritis. Cochrane Database Syst. Rev. 3, CD004849. doi:10.1002/14651858.CD004849
Hsieh, P. H., Wu, O., Geue, C., McIntosh, E., McInnes, I. B., and Siebert, S. (2020). Economic burden of rheumatoid arthritis: A systematic review of literature in biologic era. Ann. Rheum. Dis. 79 (6), 771–777. doi:10.1136/annrheumdis-2019-216243
Hu, H., Xu, A., Gao, C., Wang, Z., and Wu, X. (2021). The effect of physical exercise on rheumatoid arthritis: An overview of systematic reviews and meta-analysis. J. Adv. Nurs. 77 (2), 506–522. doi:10.1111/jan.14574
Imoto, A. M., Amorim, F. F., Palma, H., Lombardi Júnior, I., Salomon, A. L., Peccin, M. S., et al. (2021). Evidence for the efficacy of tai chi for treating rheumatoid arthritis: An overview of systematic reviews. Sao Paulo Med. J. 139 (2), 91–97. doi:10.1590/1516-3180.2020.0346.R1.18112020
Jin, P. (1992). Efficacy of Tai Chi, brisk walking, meditation, and reading in reducing mental and emotional stress. J. Psychosom. Res. 36 (4), 361–370. doi:10.1016/0022-3999(92)90072-a
Kirsteins, A. E., Dietz, F., and Hwang, S. M. (1991). Evaluating the safety and potential use of a weight-bearing exercise, Tai-Chi Chuan, for rheumatoid arthritis patients. Am. J. Phys. Med. Rehabil. 70 (3), 136–141. doi:10.1097/00002060-199106000-00005
Lee, E. N. (2005). Effects of a tai-chi program on pain, sleep disturbance, mood and fatigue in rheumatoid arthritis patients. J. Rheumatic Health 12 (1), 57–68.
Lee, H. Y., Hale, C. A., Hemingway, B., and Woolridge, M. W. (2012). Tai chi exercise and auricular acupressure for people with rheumatoid arthritis: An evaluation study. J. Clin. Nurs. 21 (19-20), 2812–2822. doi:10.1111/j.1365-2702.2011.04058.x
Lee, K. Y., and Jeong, O. Y. (2006). The effect of Tai Chi movement in patients with rheumatoid arthritis. Taehan Kanho Hakhoe Chi 36 (2), 278–285. doi:10.4040/jkan.2006.36.2.278
Lee, M. S., Pittler, M. H., and Ernst, E. (2007). Tai chi for rheumatoid arthritis: Systematic review. Rheumatol. Oxf. 46 (11), 1648–1651. doi:10.1093/rheumatology/kem151
Liang, C. (2020). Study on intervention of Tai chi combined with whip movement in patients with rheumatoid arthritis. Master: Shanxi University.
McKenna, S., Donnelly, A., Fraser, A., Comber, L., and Kennedy, N. (2017). Does exercise impact on sleep for people who have rheumatoid arthritis? A systematic review. Rheumatol. Int. 37, 963–974. doi:10.1007/s00296-017-3681-x
Metsios, G. S., Stavropoulos-Kalinoglou, A., and Kitas, G. D. (2015). The role of exercise in the management of rheumatoid arthritis. Expert Rev. Clin. Immunol. 11 (10), 1121–1130. doi:10.1586/1744666X.2015.1067606
Mudano, A. S., Tugwell, P., Wells, G. A., and Singh, J. A. (2019). Tai Chi for rheumatoid arthritis. Cochrane Database Syst. Rev. 9 (9), Cd004849. doi:10.1002/14651858.CD004849.pub2
Nagy, G., Roodenrijs, N. M. T., Welsing, P. M. J., Kedves, M., Hamar, A., van der Goes, M. C., et al. (2022). EULAR points to consider for the management of difficult-to-treat rheumatoid arthritis. Ann. Rheum. Dis. 81 (1), 20–33. doi:10.1136/annrheumdis-2021-220973
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 88, 105906. doi:10.1016/j.ijsu.2021.105906
Pope, J. E. (2020). Management of fatigue in rheumatoid arthritis. RMD Open 6 (1), e001084. doi:10.1136/rmdopen-2019-001084
Roodenrijs, N. M. T., Hamar, A., Kedves, M., Nagy, G., van Laar, J. M., van der Heijde, D., et al. (2021). Pharmacological and non-pharmacological therapeutic strategies in difficult-to-treat rheumatoid arthritis: A systematic literature review informing the EULAR recommendations for the management of difficult-to-treat rheumatoid arthritis. RMD Open 7 (1), e001512. doi:10.1136/rmdopen-2020-001512
Scherer, H. U., Haupl, T., and Burmester, G. R. (2020). The etiology of rheumatoid arthritis. J. Autoimmun. 110, 102400. doi:10.1016/j.jaut.2019.102400
Shin, J. H., Lee, Y., Kim, S. G., Choi, B. Y., Lee, H. S., and Bang, S. Y. (2015). The beneficial effects of Tai Chi exercise on endothelial function and arterial stiffness in elderly women with rheumatoid arthritis. Arthritis Res. Ther. 17, 380. doi:10.1186/s13075-015-0893-x
Siegel, P., Tencza, M., Apodaca, B., and Poole, J. L. (2017). Effectiveness of occupational therapy interventions for adults with rheumatoid arthritis: A systematic review. Am. J. Occup. Ther. 71 (1), 7101180050p1–7101180050p11. doi:10.5014/ajot.2017.023176
Song, R., Lee, E. O., Lam, P., and Bae, S. C. (2007). Effects of a Sun-style Tai Chi exercise on arthritic symptoms, motivation and the performance of health behaviors in women with osteoarthritis. Taehan Kanho Hakhoe Chi 37 (2), 249–256. doi:10.4040/jkan.2007.37.2.249
Song, R., Roberts, B. L., Lee, E. O., Lam, P., and Bae, S. C. (2010). A randomized study of the effects of t'ai chi on muscle strength, bone mineral density, and fear of falling in women with osteoarthritis. J. Altern. Complement. Med. 16 (3), 227–233. doi:10.1089/acm.2009.0165
Testa, D., Calvacchi, S., Petrelli, F., Giannini, D., Bilia, S., Alunno, A., et al. (2021). One year in review 2021: Pathogenesis of rheumatoid arthritis. Clin. Exp. Rheumatol. 39 (3), 445–452. doi:10.55563/clinexprheumatol/j1l5l3
Uhlig, T., Fongen, C., Steen, E., Christie, A., and Odegard, S. (2010). Exploring tai chi in rheumatoid arthritis: A quantitative and qualitative study. BMC Musculoskelet. Disord. 11, 43. doi:10.1186/1471-2474-11-43
Uhlig, T., Larsson, C., Hjorth, A. G., Odegard, S., and Kvien, T. K. (2005). No improvement in a pilot study of tai chi exercise in rheumatoid arthritis. Ann. Rheum. Dis. 64 (3), 507–509. doi:10.1136/ard.2004.022483
Van Deusen, J., and Harlowe, D. (1987). The efficacy of the ROM Dance Program for adults with rheumatoid arthritis. Am. J. Occup. Ther. 41 (2), 90–95. doi:10.5014/ajot.41.2.90
Waite-Jones, J. M., Hale, C. A., and Lee, H. Y. (2013). Psychosocial effects of Tai Chi exercise on people with rheumatoid arthritis. J. Clin. Nurs. 22 (21-22), 3053–3061. doi:10.1111/jocn.12327
Wang, C., Roubenoff, R., Lau, J., Kalish, R., Schmid, C. H., Tighiouart, H., et al. (2005). Effect of Tai Chi in adults with rheumatoid arthritis. Rheumatol. Oxf. 44 (5), 685–687. doi:10.1093/rheumatology/keh572
Wang, C., Schmid, C. H., Iversen, M. D., Harvey, W. F., Fielding, R. A., Driban, J. B., et al. (2016). Comparative effectiveness of tai chi versus physical therapy for knee osteoarthritis: A randomized trial. Ann. Intern Med. 165 (2), 77–86. doi:10.7326/M15-2143
Wang, C. (2008). Tai chi improves pain and functional status in adults with rheumatoid arthritis: Results of a pilot single-blinded randomized controlled trial. Med. Sport Sci. 52, 218–229. doi:10.1159/000134302
Wu, G., Liu, W., Hitt, J., and Millon, D. (2004). Spatial, temporal and muscle action patterns of Tai Chi gait. J. Electromyogr. Kinesiol 14 (3), 343–354. doi:10.1016/j.jelekin.2003.09.002
Zhao, S., Otieno, F., Akpan, A., and Moots, R. J. (2017). Complementary and alternative medicine use in rheumatoid arthritis: Considerations for the pharmacological management of elderly patients. Drugs Aging 34, 255–264. doi:10.1007/s40266-017-0443-0
Keywords: physical exercise, arthritis, pain, joint tenderness, swollen joints, health assessment questionnaire
Citation: Wu H, Wang Q, Wen G, Wu J and Wang Y (2023) The effects of Tai Chi on physical function and safety in patients with rheumatoid arthritis: A systematic review and meta-analysis. Front. Physiol. 14:1079841. doi: 10.3389/fphys.2023.1079841
Received: 25 October 2022; Accepted: 17 January 2023;
Published: 26 January 2023.
Edited by:
Esther Ubago-Guisado, Andalusian School of Public Health, SpainReviewed by:
Adérito Ricardo Duarte Seixas, Escola Superior de Saúde Fernando Pessoa, PortugalCopyright © 2023 Wu, Wang, Wen, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junhao Wu, MTU4MDA4MjQ4MzJAMTM5LmNvbQ==; Yiru Wang, d2FuZ3lpcnVlbkAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.