
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Physiol. , 01 September 2022
Sec. Environmental, Aviation and Space Physiology
Volume 13 - 2022 | https://doi.org/10.3389/fphys.2022.934163
This article is part of the Research Topic Survival in Extreme Environments – Adaptation or Decompensation?, Volume II View all 9 articles
Background: Musculoskeletal conditions are major contributors to years lived with disability. Cold exposure can be a risk factor, but any conclusion is obscure.
Aim: The aim of the present scoping review was to identify the existing evidence of an association between cold exposure and musculoskeletal conditions. The aim also included to consider pain in different regions and their assessment, as well as different measures of cold exposure, effect sizes, and to assess the feasibility of future systematic reviews and meta-analyses.
Eligibility criteria: The studies must have: an epidemiological design, defined cold exposure to come prior to the health outcome, defined exposure and outcome(s), existence of effect estimate(s) or data that made it possible to calculate such an estimate. Further, studies were required to be in English language and published in peer-reviewed journals. Studies that had a specific goal of studying cold exposure as an aggravator of already existing health problems were excluded.
Sources: We searched Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations, Daily and Versions(R), and Embase Classic + Embase for original studies.
Charting method: The included studies were reviewed for study population, measurement of exposure and outcome, and effect size. Each publication was assessed for risk of bias.
Results: The included studies were heterogeneous in populations, measures of cold exposure and musculoskeletal conditions. Most studies used self-reported data. They were mostly cross-sectional studies, only two were prospective and one was a case-control study. Associations were found for different cold exposures and regional musculoskeletal conditions, but the heterogeneity and lack of studies impeded valid synthesis of risk magnitude, or meta-analyses.
Conclusion: The studies identified in this review indicate that cold exposure increases the risk of musculoskeletal conditions. However, there is a need for studies that better assess temporality between exposure and outcome. Future studies should also include better exposure assessment, including both objective measurements and measures of subjective experience of cold exposure. The heterogeneity in measurement of exposure and outcome impeded any meta-analysis.
Musculoskeletal conditions are among the most common causes of severe pain (Woolf and Pfleger, 2003) and are some of the leading contributors to the global burden of years lived with disability (Blyth et al., 2019). As a group, musculoskeletal conditions are estimated to cause 21.3% of the total years lived with disability in the world (Hoy et al., 2015). Most of the musculoskeletal conditions increase with age, and the present population age structure and the predicted increase in longevity imply augmented forthcoming occurrence. In addition, the risk of pain increases with age-related comorbidity, thus the global burden related to pain can be expected to continue to increase (Blyth et al., 2019).
Musculoskeletal conditions are highly diverse regarding aetiology, pathophysiology, anatomy, and impact on physical function. The collective concept entails all complaints related to muscles, joints, tendons, ligaments, and bone structures. The conditions may be systemic or regional. The latter include neuropathic disorders such as radiculopathies with pain or regional entrapment pain [e.g., Carpal tunnel syndrome (CTS)]. Many musculoskeletal conditions are defined by symptoms rather than clinical findings (e.g., low back pain), and pain is the major symptom. However, the aetiology of the pain can be difficult to identify (Treede et al., 2015). Consequently, the differentiation between musculoskeletal conditions and other pain conditions can be difficult. Therefore, pain or regional pain are often used terms.
The majority of studies on risk factors for musculoskeletal pain in the occupational context have explored the impact of job task, physical load, repetitiveness, static strain (NIOSH, 1997), or person related modifiers such as stress, anthropometry, BMI, vitamin status, or genetics (Mills et al., 2019). Concurrent exposures are the rule in epidemiological studies, obscuring any effects of the multitude of risk factors and modifiers not included in the study. The hypothesis claiming to account for the findings include metabolic mechanisms, pathologic muscle physiology, deteriorated blood supply or failing muscular control (Visser and van Dieën, 2006).
Original studies on cold environment as a risk factor for musculoskeletal conditions or pain are rare, and they are divergent in designs, assessment methods and case definitions. The human reaction to cold exposure is relative and relates to differences in temperature and is as such influenced by adaption, acclimatisation, coping and physical status. The impact relates to cold ambient temperature modified by wind chill, humidity, and contact cooling. Various studies use proxies for cold exposure either as measured temperature, estimated cooling effect, isotherms, climate, latitude, and contrasts from season, or outdoor/ indoor exposures.
The aim of the present scoping review was to identify the existing evidence of an association between cold exposure and musculoskeletal conditions. The aim also included to consider pain in different regions and their assessment, as well as different measures of cold exposure, effect sizes, and to assess the feasibility of future systematic reviews and meta-analyses.
This review was planned as a systematic review and registered in PROSPERO (ID: CRD42018108223). However, due to large heterogeneity in the measurement of exposure and outcome it became evident that it was not feasible to perform a systematic review. This will be described and discussed in Results and Discussion. It was therefore carried out as a scoping review. The following eligibility criteria were defined: epidemiological design, defined cold exposure to come prior to the health outcome, defined exposure and outcome(s), existence of effect estimate(s) or data that made it possible to calculate such an estimate. Further, studies were required to be in English language and published in peer-reviewed journals. Studies that had a specific goal of studying cold exposure as an aggravator of already existing health problems were excluded.
Cold exposure was defined by search terms addressing temperature, climate, region and cold effects, while health outcome was defined by concepts on musculoskeletal conditions subclassified by body regions. The search string developed in Medline and EMBASE is presented in Figure 1. Databases searched were Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations, Daily and Versions(R), and Embase Classic + Embase. We used controlled vocabulary search terms (MeSH- and Emtree-index), whenever applicable. In addition, we used search fields, with title, abstract and keyword heading, as the preferred fields to search. Our search was performed with a time limit set for publications between the years 1980 and 2022. The search was last updated in February 2022. The identified publications were first assessed as titles and abstracts by reviewers ACH, MS, and TN for eligibility, and the approach from the preferred reporting items for scoping reviews statement was followed (Tricco et al., 2018). The number of studies at each stage of the process are shown in Figure 2. Based on the inclusion criteria, 46 studies were selected and considered in full text by four of the reviewers in a plenary session (ACH, MS, TN, and EHF). Any disagreement concerning eligibility for inclusion was resolved through joint discussion. Of the 46 titles, 17 were selected for inclusion (Figure 2). No studies were identified from other sources like reference lists of included studies.
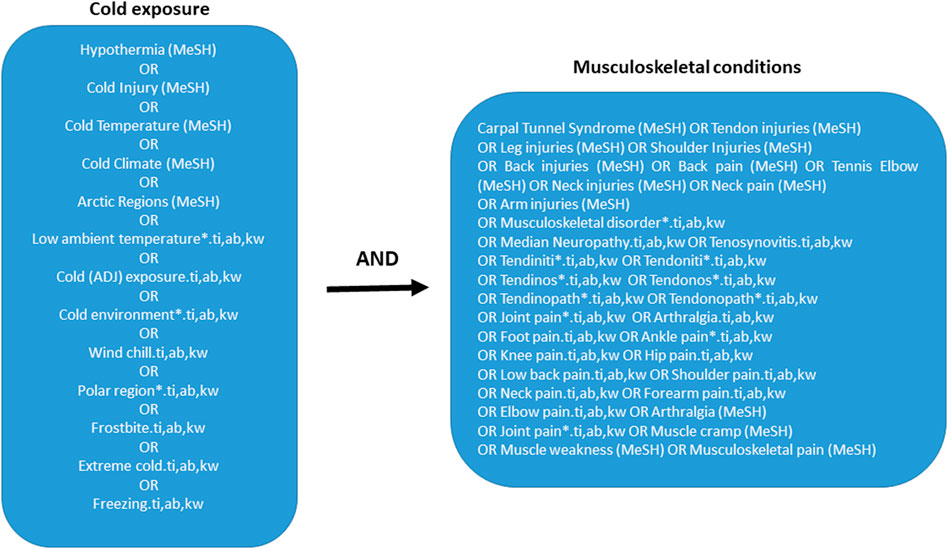
FIGURE 1. Systematic literature search of February 2022 in the following databases: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations, Daily and Versions(R), and Embase Classic + Embase. 1980 to Present. Medline subject headings; ti, titles; ab, abstracts; kw, keywords.
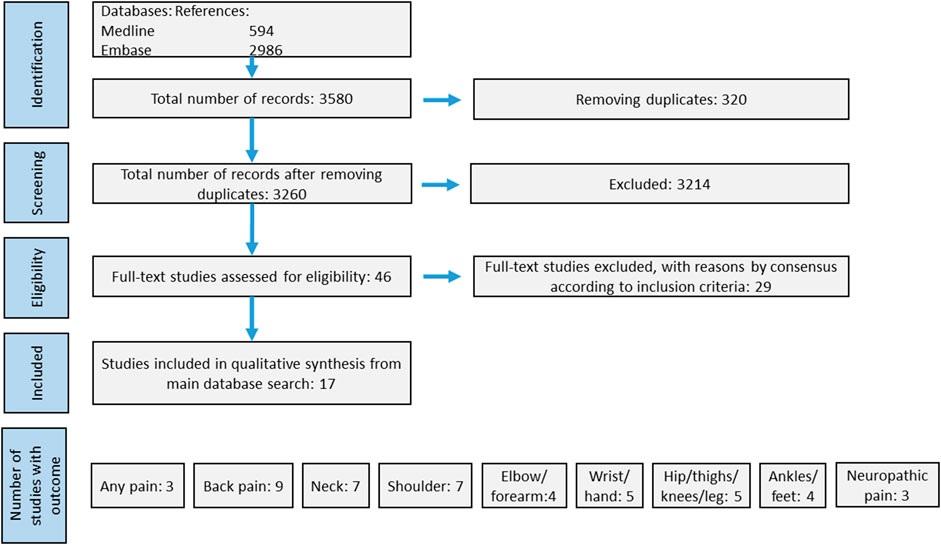
FIGURE 2. Prisma flow-chart displaying the literature search history. Of totally 3,580 references, we included 17 studies.
The 17 studies were examined by four authors (ACH, MS, TN, and EHF) in full text for obtaining type of epidemiological design, assessment of cold exposure and musculoskeletal condition. Further, the number of included subjects, incidence or prevalence, as well as association measures as odds ratio (OR), relative risk (RR) or incidence rate ratio (IRR) and confidence intervals (CI) were extracted by one author (EHF). Any missing effect estimate were calculated using the inbuilt risk-ratio/odds-ratio calculator in STATA 16. Exposure measures were classified either as using measured temperature or proxy for it, or self-reported cold exposure. The method of collecting outcomes was either by questionnaire or by a clinical examination. The outcomes were categorized according to regions. In addition, carpal tunnel syndrome (CTS) and lumbar radiculopathy were categorized as neuropathic pain.
To make it easier for the reader to judge the validity of the estimates provided we included an assessment of the included studies. The studies were assessed by the reviewers using a score system developed for this review (Supplementary Table S1). Sub-scores for method, exposure, and outcome were added up to a total score, a higher score meaning less risk of bias. Maximum points for the outcome sub-score were different for regional pain and neuropathic pain, leading to a potential maximum total score of 21 and 24, respectively (Supplementary Table S1). Any disagreements between the authors were resolved and concluded in joint sessions including four of the authors.
Out of 2,770 unique hits, 46 studies were assessed in full text (Figure 2). A total of 17 studies were identified as eligible for inclusion (Table 1). One of the studies provided data that contained what appears to be a logical flaw, there were more participants not working due to musculoskeletal pain than participants having musculoskeletal pain (Altuntas and Cankaya, 2020). We therefore chose to not calculate and present any effect estimates from this study.
Six of the studies recruited from the general population (Pope et al., 1997; Raatikka et al., 2007; Bodin et al., 2012; Farbu et al., 2019; Farbu et al., 2021a; Stjernbrandt and Farbu, 2022), one study recruited cases and controls from a clinic (Yagev et al., 2007), and the remaining 10 studies comprised of specific working populations, such as construction workers (Burstrom et al., 2013), miners (Skandfer et al., 2014), food processing workers (Piedrahı́;ta et al., 2004; Sormunen et al., 2009; Altuntas and Cankaya, 2020), store workers (Chiang et al., 1990; Dovrat and Katz-Leurer, 2007; Ghani et al., 2020), army recruits (Milgrom et al., 2003) or factory workers (Pinar et al., 2013). The number of participants ranged from 162 to 118 258 (Tables 2, 3).
There were two main categories of exposure measure: temperature and self-reported exposure to cold conditions. Seven studies used temperature as a measure of cold exposure. The measures were heterogenous, ranging from categories based on contact with frozen items (Chiang et al., 1990), to categories based on seasons (Milgrom et al., 2003), ambient air temperature measured at the workplace (Piedrahı́;ta et al., 2004; Dovrat and Katz-Leurer, 2007; Ghani et al., 2020), self-reported number of years worked in an environment below 9°C (Altuntas and Cankaya, 2020), or different regions by latitude, implying different mean temperatures between the regions (Burstrom et al., 2013). Regarding level of exposure, one of the ten studies using self-reported exposure used weekly average time of cold exposure (Raatikka et al., 2007), while many self-reported cold exposures were specified with a certain minimum time of cold exposure per day, or week. For example, cold environment at the workplace >4 h pr day (Bodin et al., 2012), temperature at workplace <10°C ≥ 20 h a week or wearing wet clothes >5 h a week (Skandfer et al., 2014), working ≥25% of the time in cold environment (Farbu et al., 2019; Farbu et al., 2021a). One study used never, occasional or always exposed to cold environment at work (Pope et al., 1997), and two used self-reported cold environment at the workplace without assessing the duration or frequency of exposure (Yagev et al., 2007; Pinar et al., 2013). Another study assessed self-reported exposure to outdoor or cold environment and participants reported on a numerical rating scale from 0 (Do not agree) to 10 (Fully agree) for both occupational exposure and leisure time exposure. Only one study specified cold environment with a temperature threshold (Skandfer et al., 2014), while in one study participants were not asked about the environment, but the perceived cooling of different body parts (Sormunen et al., 2009). Most of the studies focused on occupational exposure. However, in one study participants were asked specifically about leisure time cold exposure as well as occupational exposure (Stjernbrandt and Farbu, 2022), and one used total time exposed to cold during a week (Raatikka et al., 2007). The studies using season or geographical regions also include differences in leisure time exposure (Milgrom et al., 2003; Burstrom et al., 2013).
Most of the studies used several different outcomes. The outcome measures could roughly be divided into neuropathic (Table 2) or musculoskeletal pain (Table 3). The neuropathic outcomes were clinically verified carpal tunnel syndrome in two studies (Chiang et al., 1990; Yagev et al., 2007), and self-reported lumbar radiculopathy in one (Stjernbrandt and Farbu, 2022). 15 of the studies included musculoskeletal pain as outcome. Two of these studies included a diagnosis verified by clinical examination; one used achilles paratendinitis and another rotator cuff syndrome (RCS) (Milgrom et al., 2003; Bodin et al., 2012). A total of 14 studies used self-reported musculoskeletal pain, either pain in general or at different sites. Six studies used questions from the Nordic Questionnaire to assess the 12-months prevalence of pain, either at multiple sites (Piedrahı́;ta et al., 2004; Altuntas and Cankaya, 2020; Ghani et al., 2020), or at specific sites such as low back (Dovrat and Katz-Leurer, 2007; Skandfer et al., 2014) or shoulder (Bodin et al., 2012). In some of the studies participants were asked about pain that reduced work ability (Burstrom et al., 2013; Altuntas and Cankaya, 2020) or caused a disadvantage in daily activities (Sormunen et al., 2009). In one study participants were asked about shoulder pain lasting more than 24 h during the last month (Pope et al., 1997), and two studies specified that the pain should have lasted 3 months or more (Farbu et al., 2019; Farbu et al., 2021a), thereby more specifically assessing chronic pain. In one study participants were asked to report repeated musculoskeletal pain believed to be caused by cold temperature (Raatikka et al., 2007).
The risk of bias in the included studies was assessed by a scoring system developed for this review (Supplementary Table S1). The total score is presented in Tables 2, 3. The sub scores on exposure, outcome and method are presented in Supplementary Table S2. Most of the studies had less than half of the possible maximum scores, indicating a higher risk of bias. Fourteen of the studies had cross-sectional design, two were cohort studies (Milgrom et al., 2003; Farbu et al., 2021a) and one was a case-control study (Yagev et al., 2007).
There were several different outcomes in many of the studies, and consequently a total of 85 effect estimates were extracted from the included studies (Tables 2, 3). Most of the estimates in the included studies showed an association between cold exposure and pain, either neuropathic or musculoskeletal pain (Tables 2, 3). However, not all were statistically significant, many of the estimates had wide confidence intervals and the estimates between studies varied.
The two studies on CTS found increased odds for cold exposure, either measured as self-reported cold environment at work (Yagev et al., 2007), or as handling frozen food (Chiang et al., 1990). In one study, the highest tertile of occupational cold exposure had significantly increased odds for lumbar radiculopathy, but not the highest tertile of leisure time cold exposure (Table 2) (Stjernbrandt and Farbu, 2022).
Among the studies using pain in general as an outcome, a prospective cohort study found a significantly increased risk of having any musculoskeletal complaints after 7–8 years (Farbu et al., 2021a). However, there were no significantly increased risks of severe or widespread musculoskeletal complaints. This contrasts the earlier findings from a cross-sectional analysis from the same authors showing a significant association between cold exposure and pain at ≥3 sites, but not for pain at 1–2 sites. A significant association between cold exposure and general musculoskeletal pain was also found in a sample of workers from a Turkish ammunition factory (Pinar et al., 2013), as well as between cold exposure and pain believed to be caused by cold exposure in a general population in Finland (Raatikka et al., 2007).
Most studies found cold exposure to be significantly associated with back pain (Table 3). The associations were found using self-reported exposure, subjective experience, geographical regions, and measured temperature at the workplace (Table 3). The results for upper back (including 4 cases) (Piedrahı́;ta et al., 2004) and back pain lasting ≥3 months (Farbu et al., 2019) were not statistically significant. One study did not find any association between leisure time cold exposure and back pain (Stjernbrandt and Farbu, 2022)
Six of the seven studies using neck pain as an outcome found statistically significant associations between cold exposure and neck pain. The associations were found using self-reported exposure, subjective experience, geographical regions and measured temperature at the workplace (Table 3). Three of the studies consisted of reasonable large sample sizes from 6,533 to 118 258. Even though one study found a statistically significant association for occupational cold exposure, the association for leisure time cold exposure was not significant (Stjernbrandt and Farbu, 2022). Another study that did not find a statistically significant association had asked participants for head/neck pain the participants believed to be caused by cold exposure (Raatikka et al., 2007).
A total of seven studies included shoulder pain as outcome. One study of French employees showed that being exposed to cold >4 h per day was positively associated with self-reported shoulder pain in women, but not with clinically diagnosed RCS. The results for men were not reported because the authors did not find a statistically significant higher prevalence of shoulder pain with or without RCS among the 149 men exposed to cold environment (Bodin et al., 2012). Two other studies found a significant association for men, but not for women (Pope et al., 1997; Raatikka et al., 2007). One study found that those working in cold environment ≥25% of the time had significantly increased odds for shoulder pain lasting ≥3 months (Farbu et al., 2019).
Four studies included pain in elbows, forearms, or arms as outcomes (Piedrahı́;ta et al., 2004; Raatikka et al., 2007; Farbu et al., 2019; Ghani et al., 2020). Even though all four studies found increased odds for cold exposure, only one was statistically significant. Studies of pain in the wrist, hands or fingers also consistently found increased odds for pain for cold exposure, but not all associations were statistically significant (Table 3). One study found significantly higher odds for pain in wrist or fingers believed to be caused by cold with increasing cold exposure among women, but not among men (Raatikka et al., 2007).
Among the five studies using hip, knees, thighs, calves or leg, two studies found associations: one between working in cold environments ≥25% of the time and pain in the leg lasting ≥3 months or more (Farbu et al., 2019), and one found significant associations between cold store work and pain in the hip/thighs and knees (Ghani et al., 2020).
There were four studies using ankle and/or foot as outcomes (Piedrahı́;ta et al., 2004; Raatikka et al., 2007; Farbu et al., 2019; Ghani et al., 2020). One of the studies with the highest score in the critical appraisal found a higher incidence of achilles paratendinitis among military recruits trained in winter compared to summer (Milgrom et al., 2003), and one study reported an association between hours exposed to cold environment and pain in ankles or feet believed to be caused by cold exposure (Raatikka et al., 2007). One study found no association between cold exposure and pain in the foot lasting ≥3 months (Farbu et al., 2019).
Taken together, the limited evidence available indicates that cold exposure increases the risk of musculoskeletal conditions. The studies on cold exposure as a risk factor for CTS had the least risk of bias and found strong associations (OR of 3.52 and 9.39), but they were limited in size. Associations between cold exposure and back, neck and shoulder pain were found in several studies with reasonable large sample sizes. However, the studies included in this review are in general at risk of being biased. The majority was cross-sectional and only two studies were prospective, in addition to one case-control study. One of the prospective studies attained the outcome 7–8 years after the measurement of exposure and did not include information about the status of exposure at follow-up. Further, most included studies use self-reported exposures or outcomes, and were done in specific populations.
Measuring cold exposure is difficult. One used definition of cold environment at work is an ambient temperature <10°C (International Organization of Standardisation, 2008). However, contact with cold surfaces, cold liquids, draughts, humidity, and amount of clothing also affects the heat loss of an individual. The level of physical activity, and consequently heat production, might lessen the need for protection against the cold. The lack of an association for leisure time exposure might indicate that the setting of the exposure is of importance. The possibility to mitigate the negative effects of cold exposure by wearing more clothes or terminate the exposure might be higher when it is a leisure time activity. Another possibility is that cold exposure might not be a risk factor for musculoskeletal conditions, and that the association between occupational exposure and pain could be confounded by other risk factors. Workers that are exposed to cold might be more exposed to other known concurrent risk factors for pain like heavy lifting, vibration, and awkward working positions. Some of the studies try to take other occupational risk factors into account, but good measurement of all possible confounders and the statistical strength to satisfactorily adjust for these is difficult to achieve. Occupation is also considered as a marker of socioeconomic position, which again is found to be related to pain and other risk factors for pain such as level of physical activity, smoking, obesity, and poor health (Poleshuck and Green, 2008; Mills et al., 2019). Consequently, some studies could be confounded, and even studies with a comprehensive adjustment for other risk factors could be vulnerable to residual confounding.
The discussed heterogenous measurements of exposure, as well as for outcomes, impedes any meta-analysis. The estimated effect size would not be interpretable. On the other side, associations were found using many different measures of cold exposure and in many different countries. These convergent results strengthen the hypothesis that cold exposure increases the risk for musculoskeletal conditions. Another finding that strengthens the hypothesis is that some of the included studies found a dose-response relationship between cold exposure and pain (Pope et al., 1997; Raatikka et al., 2007; Sormunen et al., 2009; Burstrom et al., 2013; Stjernbrandt and Farbu, 2022). One study also found a dose-response relationship for frequency of feeling cold and chronic pain (Farbu et al., 2019). Two of these studies use a subjective measure of cold exposure, i.e., feeling cold or cooling, and the self-reported exposure in several of the other studies could be influenced by the subjective experience. A study of workers in the fishing industry could not find any simple relationship between the ambient temperature and the frequency of feeling cold and feeling cold often was associated with musculoskeletal pain (Bang et al., 2005). Thus, the subjective experience of the environment might be an important marker for the cold exposures’ effect on the body, but a poor marker of the thermal environment. On the other side, the experience of pain and the environment, as well as having pain, could very well be closely connected (Sundstrup et al., 2015; Farbu et al., 2021b). The central sensitization associated with pain could increase the risk of feeling cold or cooling, and the likelihood of reporting a cold environment. Consequently, the cross-sectional studies using self-reported exposure could be vulnerable to reverse causation.
The limited evidence indicating that cold exposure is a risk factor for pain or chronic pain identified in this review could be supported by literature that did not meet our inclusion criteria. One study noted that a colder temperature at the working place was the only notable difference between two groups with different incidence of tenosynovitis in food-processing workers (Kurppa et al., 1991), and other studies have found associations between different environmental complaints and pain (Hildebrandt et al., 2002; Magnavita et al., 2011; Sundstrup et al., 2015). A case-control study found an association between working in a cold environment and having rheumatoid arthritis (Zeng et al., 2017). Further, several experimental studies have found that cold temperature might affect neuromuscular function. For example, cold temperature caused decreased muscle power and contraction velocity (Racinais and Oksa, 2010), it increased stiffness of tendons (Alegre et al., 2016), as well as decreased nerve conductivity (Racinais and Oksa, 2010). A more direct association is found in individuals experiencing non-freezing cold injury, a neuropathic condition causing pain and sensory disturbances (Vale et al., 2017). The possible nerve swelling caused by cooling could be part of the explanation of the association between cold exposure and CTS (Ulaşli et al., 2014). These findings could indicate that cold exposure cause structural changes which increases the risk of pain. In addition, many report that their pain condition is aggravated by weather (Timmermans et al., 2014) and that cold temperature causes pain. Further, the findings that weather affects pain tolerance indicates that the climatic environment can be of importance for how and when we feel pain (Farbu et al., 2021b).
Pain is one of the most prominent symptoms of musculoskeletal conditions, and pain is an experience and a feeling, it is subjective in nature, and it seems to vary over time (Glette et al., 2020; Farbu et al., 2021b). Measuring it is therefore inherently difficult. In addition, the reporting of pain seems to be affected by the society the individual lives in (Zimmer et al., 2021). To further complicate it, the correlation between clinical findings and pain can often be poor (Dieppe and Lohmander, 2005), meaning a clinically verified diagnosis is not a good measure of an individual’s pain. Thus, the best measure of outcome might be dependent on the causal hypothesis about the association: does cold exposure increase the risk of experiencing pain or does it cause structural changes which again increases the risk of pain?
The results presented in this review are vulnerable to possible publication bias. Some of the included studies do not have a specific aim of investigating cold exposure as a risk factor. Other studies that also included cold exposure as one of many risk factors may have chosen to not report the estimates due to non-significant results. To which extent this is present is not known.
Another limitation is the use of odds ratios as an effect measure, as it has no intuitive interpretation. OR is “overestimated” if interpreted as relative risk, and this bias increases with increasing prevalence (Szklo and Nieto, 2018). The prevalence of the outcomes in the included studies ranged from under 10% to over 80%, and direct comparison of the ORs between studies is precarious. These problems also complicate the communication of the results, and the translation into the clinic.
Some of the included studies had few participants and did not have sufficient power. For example, one study calculated a prevalence ratio based on only 2 cases (Piedrahı́;ta et al., 2004), and another study found an RR of 151 with 100 participants in each group (Ghani et al., 2020). This estimate is only possible if the number of events in one group is less than one or higher than 100. Nevertheless, many studies calculated many estimates. A total of 85 estimates were extracted from 16 studies, but none of the included studies adjusted for multiple testing.
The results in some of the included studies might also be affected by the healthy-worker effect (Hernán et al., 2004). Many studies use occupational exposure, and it might very well be that those vulnerable to cold exposure or developing pain already have changed their occupation. This could lead to an underestimation of the effect.
Another limitation is that many of the studies included questions on aches, stiffness, or trouble in certain regions of the body. Thus, even though we have used the term regional pain in this review, some participants might have had other symptoms than pain. Further, our list of musculoskeletal conditions was not exhaustive.
Although the evidence for cold exposure per se as a causal factor for musculoskeletal conditions is uncertain, it is in many instances relatively easy and cheap to prevent by means of better or more clothing. The association between perceived climatic environment and pain indicates that the person’s own experience of the climate might be a good indicator of cold exposure and the need for protective measures. There is a need for prospective studies, and future research should clearly state their aim and hypothesis, restrain from testing multiple hypotheses at the same time, be sufficiently powered, and try to incorporate both objective and subjective measures of the environment. Future studies could also include an assessment of important aspects of pain like intensity and duration.
ER, ACH, MS, TN, and EHF worked out the search-terms and inclusion criteria. ER refined and carried out the search, produced the figure presenting the full electronic search strategy and revised the methodology together with TN and EHF from PRISMA SR to PRISMA ScR. ACH, MS, and TN read titles and abstracts. ACH, MS, TN and EHF read all full texts considered for inclusion and jointly identified design and measurements of exposure and outcome. EHF extracted the effect estimates. TN, MS, and EHF wrote the first draft. All authors revised the manuscript.
This work was supported by Helse Nord Grant HNF1345-17. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2022.934163/full#supplementary-material
Alegre L. M., Hasler M., Wenger S., Nachbauer W., Csapo R. (2016). Does knee joint cooling change in vivo patellar tendon mechanical properties? Eur. J. Appl. Physiol. 116 (10), 1921–1929. doi:10.1007/s00421-016-3444-5
Altuntas Y. D., Cankaya T. (2020). Effects of working years in cold environment on the musculoskeletal system and carpal tunnel symptoms. Agri Derg. 32 (3), 120–127. doi:10.14744/agri.2020.35651
Bang B. E., Aasmoe L., Aardal L., Andorsen G. S., Bjornbakk A. K., Egeness C., et al. (2005). Feeling cold at work increases the risk of symptoms from muscles, skin, and airways in seafood industry workers. Am. J. Ind. Med. 47 (1), 65–71. doi:10.1002/ajim.20109
Blyth F. M., Briggs A. M., Schneider C. H., Hoy D. G., March L. M. (2019). The global burden of musculoskeletal pain-where to from here? Am. J. Public Health 109 (1), 35–40. doi:10.2105/ajph.2018.304747
Bodin J., Ha C., Chastang J. F., Descatha A., Leclerc A., Goldberg M., et al. (2012). Comparison of risk factors for shoulder pain and rotator cuff syndrome in the working population. Am. J. Ind. Med. 55 (7), 605–615. doi:10.1002/ajim.22002
Burstrom L., Jarvholm B., Nilsson T., Wahlstrom J. (2013). Back and neck pain due to working in a cold environment: A cross-sectional study of male construction workers. Int. Arch. Occup. Environ. Health 86 (7), 809–813. doi:10.1007/s00420-012-0818-9
Chiang H. C., Chen S. S., Yu H. S., Ko Y. C. (1990). The occurrence of carpal tunnel syndrome in frozen food factory employees. Gaoxiong Yi Xue Ke Xue Za Zhi 6 (2), 73–80.
Dieppe P. A., Lohmander L. S. (2005). Pathogenesis and management of pain in osteoarthritis. Lancet 365 (9463), 965–973. doi:10.1016/s0140-6736(05)71086-2
Dovrat E., Katz-Leurer M. (2007). Cold exposure and low back pain in store workers in Israel. Am. J. Ind. Med. 50 (8), 626–631. doi:10.1002/ajim.20488
Farbu E. H., Höper A. C., Brenn T., Skandfer M. (2021a). Is working in a cold environment associated with musculoskeletal complaints 7–8 years later? A longitudinal analysis from the tromsø study. Int. Arch. Occup. Environ. Health 94 (4), 611–619. doi:10.1007/s00420-020-01606-6
Farbu E. H., Rypdal M., Skandfer M., Steingrímsdóttir Ó A., Brenn T., Stubhaug A., et al. (2021b). To tolerate weather and to tolerate pain: Two sides of the same coin? Tromsø Study 7, 878–886. Pain. doi:10.1097/j.pain.0000000000002437
Farbu E. H., Skandfer M., Nielsen C., Brenn T., Stubhaug A., Höper A. C., et al. (2019). Working in a cold environment, feeling cold at work and chronic pain: A cross-sectional analysis of the tromsø study. BMJ Open 9 (11), e031248. doi:10.1136/bmjopen-2019-031248
Ghani N., Tariq F., Javed H., Nisar N., Tahir A. (2020). Low-temperature health hazards among workers of cold storage facilities in Lahore, Pakistan. Med. Pr. 71 (1), 1–7. doi:10.13075/mp.5893.00857
Glette M., Stiles T. C., Borchgrevink P. C., Landmark T. (2020). The natural course of chronic pain in a general population: Stability and change in an eight–wave longitudinal study over four years (the HUNT pain study). J. Pain 21 (5), 689–699. doi:10.1016/j.jpain.2019.10.008
Hernán M. A., Hernández-Díaz S., Robins J. M. (2004). A structural approach to selection bias. Epidemiology 15 (5), 615–625. doi:10.1097/01.ede.0000135174.63482.43
Hildebrandt V. H., Bongers P. M., van Dijk F. J., Kemper H. C., Dul J. (2002). The influence of climatic factors on non-specific back and neck-shoulder disease. Ergonomics 45 (1), 32–48. doi:10.1080/00140130110110629
Hoy D. G., Smith E., Cross M., Sanchez-Riera L., Blyth F. M., Buchbinder R., et al. (2015). Reflecting on the global burden of musculoskeletal conditions: Lessons learnt from the global burden of disease 2010 study and the next steps forward. Ann. Rheum. Dis. 74 (1), 4–7. doi:10.1136/annrheumdis-2014-205393
International Organization of Standardisation (2008). ISO 15743:2008 Ergonomics of the thermal environment-Cold workplaces-Risk assessment and managment. Geneva: International Organization of Standardisation.
Kurppa K., Viikari-Juntura E., Kuosma E., Huuskonen M., Kivi P. (1991). Incidence of tenosynovitis or peritendinitis and epicondylitis in a meat-processing factory. Scand. J. Work Environ. Health 17 (1), 32–37. doi:10.5271/sjweh.1737
Magnavita N., Elovainio M., De Nardis I., Heponiemi T., Bergamaschi A. (2011). Environmental discomfort and musculoskeletal disorders. Occup. Med. 61 (3), 196–201. doi:10.1093/occmed/kqr024
Milgrom C., Finestone A., Zin D., Mandel D., Novack V. (2003). Cold weather training: A risk factor for achilles paratendinitis among recruits. Foot Ankle Int. 24 (5), 398–401. doi:10.1177/107110070302400504
Mills S. E. E., Nicolson K. P., Smith B. H. (2019). Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 123 (2), e273–e283. doi:10.1016/j.bja.2019.03.023
NIOSH (1997). “A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back,” in Musculoskeletal disorders and workplace factors. Editor B. P. Bernard (NIOSH).
Piedrahı́ta H., Punnett L., Shahnavaz H. (2004). Musculoskeletal symptoms in cold exposed and non-cold exposed workers. Int. J. Industrial Ergonomics 34 (4), 271–278. doi:10.1016/j.ergon.2004.04.008
Pinar T., Cakmak Z. A., Saygun M., Akdur R., Ulu N., Keles I., et al. (2013). Symptoms of musculoskeletal disorders among ammunition factory workers in Turkey. Arch. Environ. Occup. Health 68 (1), 13–21. doi:10.1080/19338244.2011.627893
Poleshuck E. L., Green C. R. (2008). Socioeconomic disadvantage and pain. Pain 136 (3), 235–238. doi:10.1016/j.pain.2008.04.003
Pope D. P., Croft P. R., Pritchard C. M., Silman A. J., Macfarlane G. J. (1997). Occupational factors related to shoulder pain and disability. Occup. Environ. Med. 54 (5), 316–321. doi:10.1136/oem.54.5.316
Raatikka V. P., Rytkonen M., Nayha S., Hassi J. (2007). Prevalence of cold-related complaints, symptoms and injuries in the general population: The FINRISK 2002 cold substudy. Int. J. Biometeorol. 51 (5), 441–448. doi:10.1007/s00484-006-0076-1
Racinais S., Oksa J. (2010). Temperature and neuromuscular function. Scand. J. Med. Sci. Sports 20 (Suppl. 3), 1–18. doi:10.1111/j.1600-0838.2010.01204.x
Skandfer M., Talykova L., Brenn T., Nilsson T., Vaktskjold A. (2014). Low back pain among mineworkers in relation to driving, cold environment and ergonomics. Ergonomics 57 (10), 1541–1548. doi:10.1080/00140139.2014.904005
Sormunen E., Remes J., Hassi J., Pienimaki T., Rintamaki H. (2009). Factors associated with self-estimated work ability and musculoskeletal symptoms among male and female workers in cooled food-processing facilities. Ind. Health 47 (3), 271–282. doi:10.2486/indhealth.47.271
Standardisation I. O. (2008). International organization of standardisation ISO 15743:2008 ergonomics of the thermal environment - cold workplaces- risk assessment and managment. Geneva.
Stjernbrandt A., Farbu E. H. (2022). Occupational cold exposure is associated with neck pain, low back pain, and lumbar radiculopathy. Ergonomics 24, 1–10. doi:10.1080/00140139.2022.2027030
Sundstrup E., Jakobsen M. D., Brandt M., Jay K., Persson R., Andersen L. L., et al. (2015). Central sensitization and perceived indoor climate among workers with chronic upper-limb pain: Cross-sectional study. Pain Res. Treat. 2015, 793750. doi:10.1155/2015/793750
Szklo M., Nieto F. J. (2018). Epidemiology: Beyond the basics. Sudbury: Sudbury: Jones & Bartlett Learning, LLC.
Timmermans E. J., van der Pas S., Schaap L. A., Sánchez-Martínez M., Zambon S., Peter R., et al. (2014). Self-perceived weather sensitivity and joint pain in older people with osteoarthritis in six European countries: Results from the European project on OSteoArthritis (EPOSA). BMC Musculoskelet. Disord. 15, 66. doi:10.1186/1471-2474-15-66
Treede R.-D., Rief W., Barke A., Aziz Q., Bennett M. I., Benoliel R., et al. (2015). A classification of chronic pain for ICD-11. Pain 156 (6), 1003–1007. doi:10.1097/j.pain.0000000000000160
Tricco A. C., Lillie E., Zarin W., O'Brien K. K., Colquhoun H., Levac D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 169 (7), 467–473. doi:10.7326/m18-0850
Ulaşli A. M., Tok F., Karaman A., Yaman F., Dikici O., Oruç S., et al. (2014). Nerve enlargement after cold exposure: A pilot study with ultrasound imaging. Muscle Nerve 49 (4), 502–505. doi:10.1002/mus.23947
Vale T. A., Symmonds M., Polydefkis M., Byrnes K., Rice A. S. C., Themistocleous A. C., et al. (2017). Chronic non-freezing cold injury results in neuropathic pain due to a sensory neuropathy. Brain 140 (10), 2557–2569. doi:10.1093/brain/awx215
Visser B., van Dieën J. H. (2006). Pathophysiology of upper extremity muscle disorders. J. Electromyogr. Kinesiol. 16 (1), 1–16. doi:10.1016/j.jelekin.2005.06.005
Woolf A. D., Pfleger B. (2003). Burden of major musculoskeletal conditions. Bull. World Health Organ. 81 (9), 646–656.
Yagev Y., Gringolds M., Karakis I., Carel R. S. (2007). Carpal tunnel syndrome: Under-recognition of occupational risk factors by clinicians. Ind. Health 45 (6), 820–822. doi:10.2486/indhealth.45.820
Zeng P., Bengtsson C., Klareskog L., Alfredsson L. (2017). Working in cold environment and risk of developing rheumatoid arthritis: Results from the Swedish EIRA case–control study. RMD Open 3 (2), e000488. doi:10.1136/rmdopen-2017-000488
Keywords: cold exposure, cold environment, cold temperature, musculoskeletal conditions, pain, regional pain, scoping review
Citation: Farbu EH, Höper AC, Reierth E, Nilsson T and Skandfer M (2022) Cold exposure and musculoskeletal conditions; A scoping review. Front. Physiol. 13:934163. doi: 10.3389/fphys.2022.934163
Received: 09 May 2022; Accepted: 30 June 2022;
Published: 01 September 2022.
Edited by:
Sanjoy Deb, University of Westminster, United KingdomReviewed by:
Wilton Remigio, Clarkson University, United StatesCopyright © 2022 Farbu, Höper, Reierth, Nilsson and Skandfer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erlend Hoftun Farbu, ZXJsZW5kLmguZmFyYnVAdWl0Lm5v
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.