
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Physiol. , 22 August 2022
Sec. Clinical and Translational Physiology
Volume 13 - 2022 | https://doi.org/10.3389/fphys.2022.892623
Aim: The aim of the study was to evaluate the potential predictive value of permanent RBBB and LBBB for longer-term prognosis in patients with new-onset STEMI who underwent percutaneous coronary intervention (PCI).
Methods: Patients with new-onset STEMI that underwent emergency PCI at our department from June 2012 to September 2020 were included in the study. Gensini score (GS) was employed to evaluate the severity of coronary lesions. The primary endpoint of the study was the occurrence of major adverse cardiac and cerebrovascular events (MACCEs), the composite of cardiac mortality, recurrence of myocardial infarction, cardiac shock, stroke, stent thrombosis, or revascularization. We also set all-cause mortality as a secondary endpoint.
Results: Out of the 547 patients, 29 patients had new-onset permanent LBBB, 51 patients had new-onset permanent RBBB, and 467 patients had no bundle-branch block (BBB). The occurrence of no BBB, new permanent LBBB, or RBBB was not associated with the severity of coronary artery lesions as evaluated by the GS. After follow-up at an average of 43.93 months, MACCEs occurred in 52 patients. Kaplan-Meier analysis showed that patients with new-onset RBBB were at greater risk for MACCEs compared to those with new onset LBBB (χ2 = 5.107, p = 0.021). Also, an independent correlation was found between new permanent RBBB and LBBB and MACCEs risk. The adjusted hazard ratios (HRs) were 6.862 [95% confidence interval (CI) of 3.764–12.510] for the new-onset permanent RBBB and 3.395 (95% CI of 1.280–9.005) for LBBB, compared to those with no BBB, respectively (both p < 0.05).
Conclusion: New onset permanent RBBB in patients with new onset STEMI who underwent PCI may be correlated independently with increased risk of poor long-term prognosis.
ST-elevation myocardial infarction (STEMI) is the most common type of acute coronary syndrome (ACS), which is more likely associated with worse clinical outcomes and prognosis compared to unstable angina (UA) and non-STEMI (Vernon Stephen Coffey D’Souza et al., 2019). Therefore, it has become a consensus that for any STEMI patient who is admitted to the emergency department exhibiting acute chest pain, a 12-lead electrocardiogram (ECG) must be immediately obtained and interpreted within 10 min. Accumulating evidence suggests that ACS patients presenting with a left bundle branch block (LBBB) or right bundle branch block (RBBB) generally carry a high burden of morbidity and increased risk of mortality (Van de Werf et al., 2008; Widimsky et al., 2012). Accordingly, identification of patients presented with bundle branch block (BBB), especially new onset LBBB, remains of clinical significance and an indication for an urgent reperfusion therapy in current cardiovascular practice (RBB, 2022). Recent studies report that the presence of RBBB in patients with ACS is a high-risk ECG feature and a predictor of poor clinical outcomes (Antman Elliott et al., 2004; Widimsky et al., 2012; Chan et al., 2016; Paul et al., 2020). This reinforces the concept that new onset RBBB in coronary artery disease (CAD), even in the absence of ST elevation, is associated with unfavorable prognosis (Widimsky et al., 2012; Chan et al., 2016).
Previous studies have found that the occurrence of RBBB is more frequent than LBBB, because the Purkinje fibers of the right bundle branch are longer and structurally thinner than those of the left bundle branch (Sorensen et al., 2013; Meyer Matthias et al., 2020). This difference may contribute to the high susceptibility of RBBB to myocardial ischemia compared to LBBB in ACS. Of note, previous studies on RBBB correlated with high-risk of clinical characteristics and mortality yielded inconsistent results regarding the prognostic significance of RBBB (Antman Elliott et al., 2004; Widimsky et al., 2012; Chan et al., 2016; Paul et al., 2020). Furthermore, to the best of our knowledge, it remains debatable whether new permanent RBBB should be used as an independent variable for long-term prognosis of new onset STEMI in patients following primary percutaneous coronary intervention (PCI). Thus, we sought to evaluate the significance of new permanent RBBB and LBBB for long-term prognosis in new onset STEMI patients who underwent PCI.
Patients with new onset STEMI and without previously known CAD who underwent urgent coronary angiography and PCI from Xinjiang Medical University Affiliated Hospital of Traditional Chinese Medicine from June 2012 to September 2020, were selected for the study. STEMI diagnosis was in accordance with the previously published guidelines (Kawashima and Sasaki, 2011). Patients with any of the following clinical conditions were excluded from the study: 1) previous diagnosis of CAD; 2) diagnosis of non-STEMI or unstable angina pectoris with prior revascularization treatments, including percutaneous coronary intervention (PCI) and coronary artery bypass surgery; 3) previous diagnosis of LBBB or RBBB, transient LBBB or RBBB, new-onset STEMI without PCI, LBBB and RBBB combined with impaired atrioventricular conduction, or left posterior hemiblock and left anterior hemiblock with unknown origin, regardless of the persistence of the BBB; 4) pacemaker implantation; 5) atrial septal defect, aortic stenosis, atrial septal defect, dilated cardiomyopathy, hyperkalemia, digoxin toxicity, rheumatic heart disease, cor pulmonale, ventricular hypertrophy, myocarditis or cardiomyopathy, cardiac conduction system degenerative disease, or primary cardiac fibrosis of the cardiac conduction system; or 6) poor compliance to treatment. Due to the nature of retrospective observational studies, the protocol of this work was approved, and the requirement for the informed consent from eligible patients was waived by the Ethics Committee of the local institution. The flowchart of participant enrollment is shown in Figure 1.
Peripheral venous blood samples were drawn, and electrocardiography (ECG) was performed immediately upon admission of patients to the emergency department (ED) or right before the urgent coronary angiography. The blood samples were immediately taken for blood cell counts, biochemical analysis of lipids and glucose metabolism, and renal function analysis. Preoperative evaluation included cardiac echocardiography and ECG. All patients were monitored by ECG for seven consecutive days or received a dynamic electrocardiogram after the operation. ECGs were read by an experienced cardiologist at the ED and reviewed once again at the preparation of this manuscript by another independent and seasoned cardiologist. Standard ECG criteria were used to diagnose LBBB and RBBB (Arslan et al., 2018). New onset permanent LBBB and RBBB were considered if they appeared either on admission or before an urgent coronary angiography, but not at baseline.
After admission, all patients with STEMI were given an emergency coronary angiography and treated with the standard protocols for second generation drug eluting stent placement by experienced and senior cardiologists. Prior to the PCI, loading doses of aspirin and clopidogrel were administered to each patient. The PCI was performed by a group of experienced senior physicians based on the coronary anatomy and clinical conditions of each individual patient. After the PCI, all patients were given the guideline-directed standard treatment regimens, including contemporary antiplatelet therapy and standard-intensity statin therapy, and were followed-up regularly at the clinic after their discharge (Kawashima and Sasaki, 2011). Coronary atherosclerosis was evaluated using the Gensini scoring (GS) system by two experienced cardiologists independently. In case of any disagreements, a third cardiologist would be called in to evaluate the coronary atherosclerosis of the patients, and the final diagnosis was achieved based on the consensus of all three cardiologists.
The average follow-up period was 43.93 months and was conducted either via telephone or at the clinic. At the end of the follow-up, a total of 36 cases were lost to follow up, and 547 patients (93.8%) were followed to the end. The primary endpoint of the study was the occurrence of major adverse cardiac and cerebrovascular events (MACCEs), the composite of cardiac mortality, recurrence of myocardial infarction, cardiac shock, stroke, revascularization, or stent thrombosis. The secondary endpoint was all-cause mortality. Two experienced physicians adjudicated the endpoint events based on a review of medical records. Cardiac mortality was defined as death from any cardiac causes. Recurrence of myocardial infarction was defined as a novel myocardial infarction in the target vessel. Stent thrombosis was confirmed by an angiography. Cardiac shock was defined as a state of hypoperfusion resulting from a low cardiac output due to heart failure. Stroke was divided into fatal and non-fatal ischemic strokes. Revascularization was defined as revascularization involving either targeted or non-targeted vessels. A death from any cause was defined as an all-cause death. Bleeding events were defined as any bleeding event. Patients were censored at the last follow-up, on 24 December 2020, or whichever came first.
The sample size was calculated with the following formula:
Continuous variables are presented as ‘mean ± SD’ for normal distribution; otherwise, medians and interquartile ranges (IQRs) are used. Categorical variables are expressed as percentages. To analyze categorical variables, a chi-square (χ2) test was applied. Multiple group comparisons were performed using ANOVA. The Mann-Whitney U test or Kruskal–Wallis variance analysis was conducted for analyzing non-normal distribution. Multiple logistic regression analysis was employed to study the association of new permanent BBB with the severity of coronary atherosclerosis, as calculated by the Gensini scoring system. The Kaplan-Meier survival curve was employed to analyze the potential predictive efficacy of new permanent RBBB at baseline for the prognosis of new onset STEMI in patients with stent placement. SPSS 23 was used for the statistical analysis, with p < 0.05 indicating statistical significance.
A total of 547 patients with new onset STEMI who underwent PCI were retrospectively included in the study. The risk factors for CAD and baseline blood biochemical profiles of all patients were categorized into three group: no BBB, new onset permanent RBBB, or new onset permanent LBBB (Table 1). We found that patients with LBBB had higher levels of apolipoprotein B and low-density lipoprotein-cholesterol (LDL-C) than those with RBBB and no BBB (all p < 0.05). Patients with new LBBB and RBBB had higher triglyceride than those with no BBB (all p < 0.05).
The incidence rates of clinical outcomes during the follow-up (43.93 ± 24.56 months) for patients with new-onset STEMI who underwent PCI based on no BBB, with new permanent RBBB or LBBB are shown in Table 2 (all p < 0.05). The results indicate that patients with new permanent RBBB were vulnerable to all-cause mortality, cardiac mortality, revascularization, stroke, and cardiac shock than those with LBBB and no BBB (all p < 0.05); those with LBBB had higher incidence of cardiogenic shock than those with no BBB (p < 0.05); and those with no BBB had lower incidence of MACCEs than those with new permanent LBBB and RBBB (p < 0.05).
The baseline characteristics of participants according to the GS tertiles (first GS tertile <48, n = 182; second GS tertile: 49–84, n = 183; and third GS tertile ≥85, n = 182) are presented in Table 3. Age, high-density lipoprotein cholesterol, apolipoprotein AI, prevalence of diabetes mellitus, and hypertension were significantly different among the three GS tertiles (all p < 0.05). However, new permanent RBBB, new onset LBBB, and no BBB indicated no statistical differences with respect to GS based on the observed CAG findings (p > 0.05). Multivariate logistic analyses demonstrated that age (OR: 1.015, p = 0.033), high-density lipoprotein cholesterol (OR: 0.354, p = 0.003), apolipoprotein AI (OR: 0.481, p = 0.023), the prevalence of diabetes mellitus (OR: 1.499, p = 0.031), and incidence of hypertension (OR: 1.528, p = 0.009) were independently associated with the severity of coronary lesions in new onset STEMI patients (Table 4).
The Kaplan-Meier analysis showed that the incidence of MACCEs differed significantly among groups of patients with no BBB, with new onset permanent RBBB and LBBB, and with new onset STEMI who underwent PCI (χ2 = 80.231 p < 0.001, Figure 2). Pairwise comparisons further indicated that patients with new permanent RBBB had a higher incidence of MACCEs than those with new permanent LBBB (χ2 = 5.107, p = 0.021, Figure 2). Likewise, patients with new permanent RBBB had a higher incidence of MACCEs than those with no BBB (χ2 = 81.253, p < 0.001, Figure 2). Patients with new permanent LBBB had a higher risk of developing future MACCEs than those with no BBB (χ2 = 7.783, p = 0.005, Figure 2). Moreover, there was a significant difference in all-cause mortality among those with no BBB and with new onset permanent RBBB and LBBB groups (χ2 = 86.558, p < 0.001, Figure 3). Furthermore, pairwise comparisons demonstrated that patients with new permanent RBBB had a higher incidence of all-cause mortality than those with new onset permanent LBBB (χ2 = 4.131, p = 0.042, Figure 3). Patients with new onset permanent RBBB had a higher risk of future all-cause mortality than those with no BBB (χ2 = 87.812, p < 0.001, Figure 3). Univariate Cox regression analysis indicated that age, systolic and diastolic blood pressure, higher GS, unprotected left main coronary artery (UPLMCA) lesions, RBBB, and LBBB were all potential predictors of MACCEs (Table 5, all p < 0.05). Subsequent multivariate analysis showed that new permanent RBBB and LBBB were independently correlated with a high risk of MACCEs and adjusted HRs of 6.862 (95% CI, 3.764–12.510) and 3.395 (95% CI, 1.280–9.005), respectively, compared to patients with no BBB (both p < 0.05, Table 5; Figure 4). Age (HR: 1.031, 95% CI: 1.006 to 1.057, p = 0.017), UPLMCA (HR: 2.364, 95% CI: 1.213 to 4.606, p = 0.011), and increase of the GS (third tertile vs. First tertile, HR: 3.557, 95% CI: 1.410 to 8.969, p = 0.007) were all independent risk factors for MACCEs in new onset STEMI patients post-PCI (Table 5; Figure 4). Univariate Cox regression analysis indicated that age, systolic blood pressure, higher GS, RBBB, and LBBB were all potential predictors of MACCEs (Table 6, all p < 0.05). The results of a subsequent multivariate analysis demonstrated that new permanent RBBB was independently correlated with an increased risk of all-cause mortality with an adjusted HRs of 24.537 (95% CI: 9.104–66.132), compared to patients with no BBB (p < 0.05, Table 6). Likelihood estimates revealed that systolic pressure (HR:1.027, 95% CI: 1.008 to 1.046, p = 0.004) was an independent predictor of all-cause mortality in new onset STEMI patients post-PCI (Table 6; Figure 5).
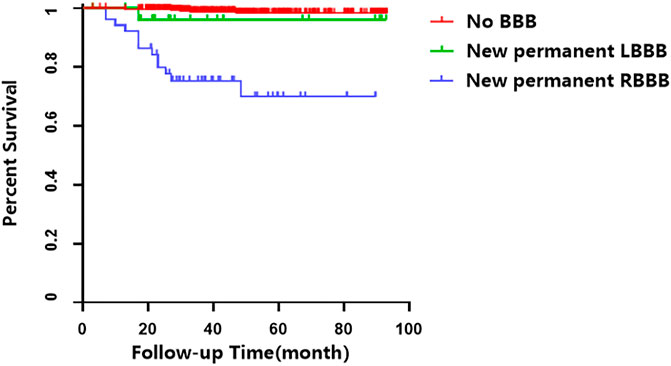
FIGURE 3. Cumulative survival analysis of all-cause mortality in patients with STEMI who underwent PCI.
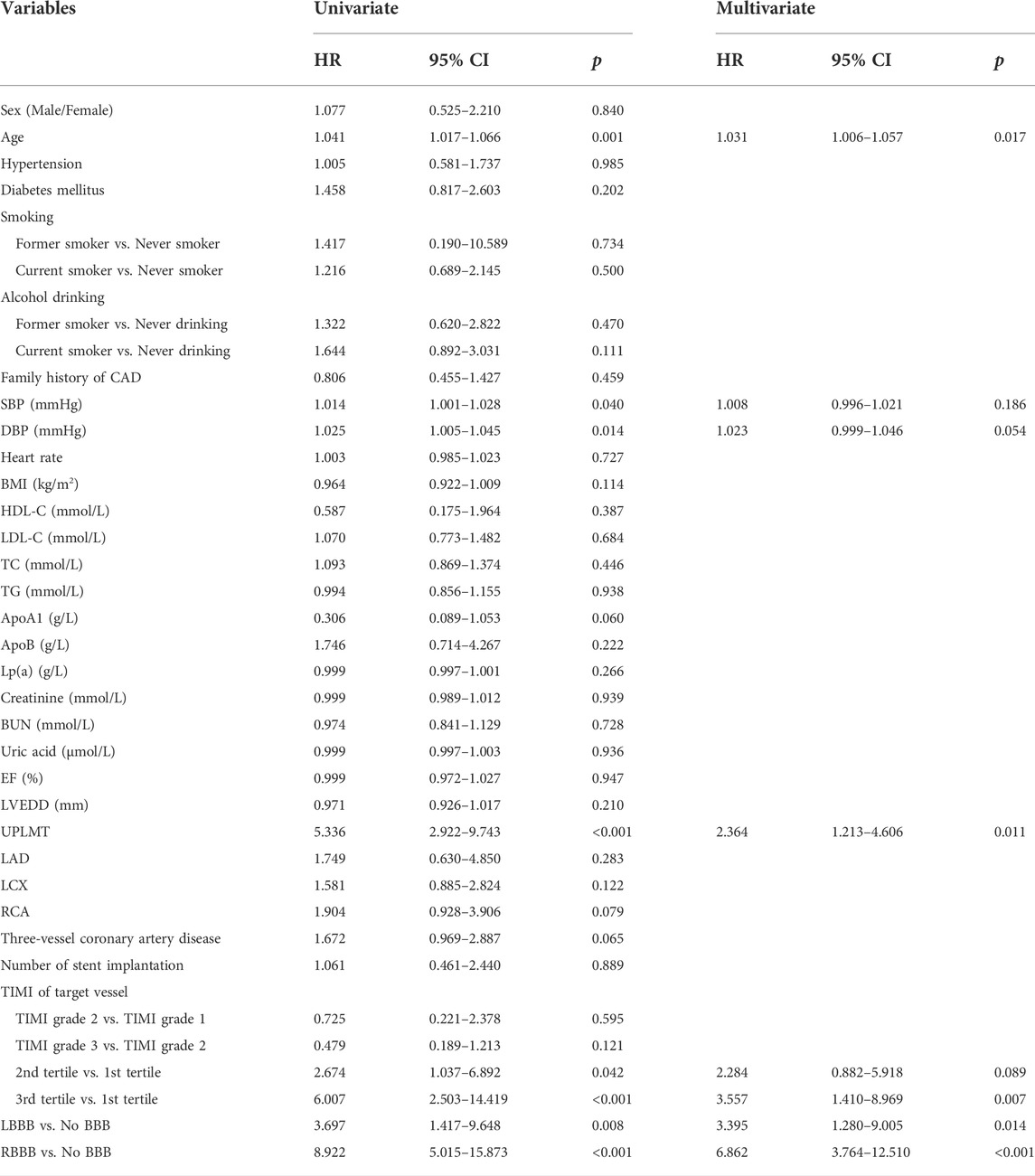
TABLE 5. Potential predictors for the incidence of MACCEs in patients with new onset STEMI who underwent PCI.
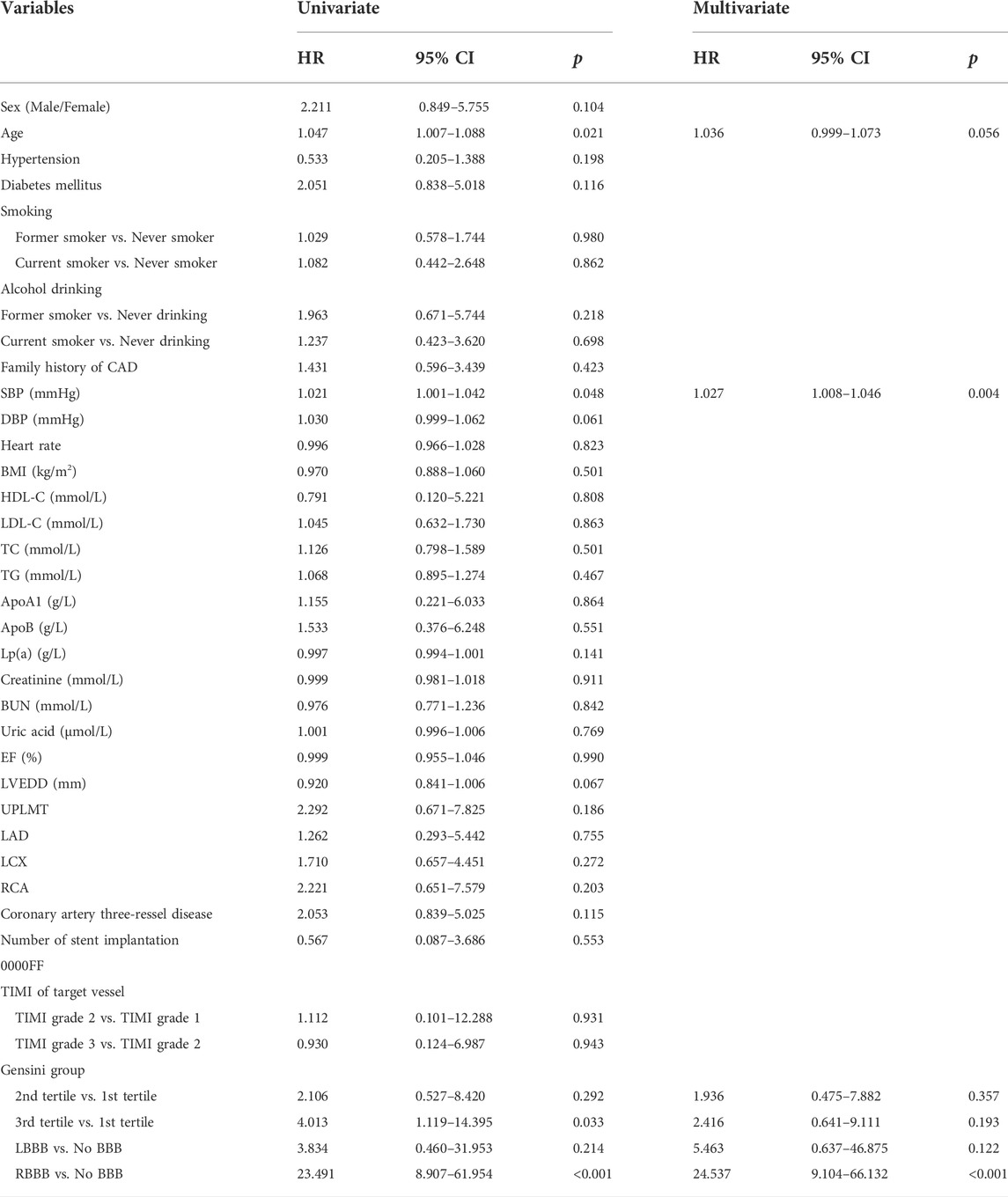
TABLE 6. Potential predictors for the incidence of all-cause mortality in patients with new onset STEMI who underwent PCI.
In this retrospective cohort study, we have drawn the following conclusions: 1) the occurrence of new permanent RBBB and LBBB is an independent predictor for MACCEs in patients with new onset STEMI post PCI; 2) patients with new permanent RBBB are most likely at higher risk for future all-cause mortality and MACCEs than those with new permanent LBBB and with no BBB; 3) having no BBB with new permanent RBBB or LBBB is not associated with coronary artery lesions as evaluated by the GS; and 4) new permanent RBBB in patients with new onset STEMI who underwent PCI had a worse prognosis than those with LBBB or no BBB.
Previous studies suggested that new onset BBB might indicate a larger territory of AMI involving the proximal branches of the cardiac conduction system or a delayed conduction caused by the severely damaged ventricular myocardium. Either indicator might have concealed the ST-segment elevation (Willems et al., 1985). Current guidelines state that symptomatic patients with new or presumably new LBBB should be treated as STEMI equivalents, which usually is correlated with worse clinical characteristics and prognosis (Neeland Ian et al., 2012). Our data are consistent with the guidelines that emphasize the importance of new LBBB in clinic practice, particularly in patients with successful revascularization (Borja et al., 2018). However, the predictive efficacy of RBBB in ACS remains to be determined (Antman Elliott et al., 2004; Mozid Abdul et al., 2015; Chan et al., 2016; Alkindi et al., 2020; Paul et al., 2020). The inconsistency among previous studies might be caused by the different criteria for patient enrollment and study endpoints. In a previous study, 202,268 primary care patients with no-known significant cardiovascular disease were followed-up for 7.8 years. A previous work found that RBBB was a predictor for pacemaker implantation, a risk factor associated with increased incidence of heart failure in both sexes, and weakly associated with cardiac death in men (Juntao et al., 2018). In a prospective study of 17,437 patients with AMI, results revealed that, although isolated BBB was directly correlated with high-risk clinical characteristics such as three-vessel and left main disease, it could not be used solely to predict increased hospital mortality in AMI patients (Paul et al., 2020). In contrast, in a recent study of 50,974 patients with acute cardiac events, RBBB was found to be independently and significantly correlated with hospital mortality (Mozid Abdul et al., 2015). Likewise, multiple studies have indicated that RBBB is an independent predictor of in-hospital short- and long-term mortality in the context of patients with different types of ACS presentations, including unstable angina and myocardial infarction (McCullough Peter et al., 2005; Widimsky et al., 2012; Chan William et al., 2016; Peter Vibe et al., 2019). Importantly, it is now becoming accepted that RBBB, as a predictor of poor outcomes for ischemic cardiomyopathy, also serves as an independent indicator for the risk of decreased right ventricular ejection fraction (Melgarejo-Moreno et al., 2015). However, it is imperative to optimize the risk stratification in myocardial infarction patients post-PCI, especially for the identification of easily neglected and potential prognostic factors (Sabe Marwa et al., 2016; Yi et al., 2020). Moreover, previous studies failed to address the association between RBBB and prognosis post-PCI.
In our retrospective study, we found no correlations between new permanent LBBB and RBBB and the severity of coronary artery atherosclerosis assessed by GS, which is consistent with prior studies (Wang et al., 2022). Moreover, compared to patients with no BBB, patients with new permanent RBBB were associated with an increased overall risk of MACCEs and all-cause mortality in new onset STEMI patients who underwent PCI, even after adjusting for comorbidities after a long-term follow-up. Therefore, our overall findings are similar to those from the previous reports that new onset RBBB was a high-risk signal for new onset STEMI (Prakriti et al., 2020; Zhu et al., 2022). We also demonstrated that patients with new permanent RBBB were more prone to adverse events, including MACCEs and all-cause mortality compared to those with new permanent LBBB and with no BBB. One possible pathophysiological mechanism for our discovery is that RBBB is more susceptible to dys-synchronized ventricular contractions, resulting in progressive decreased ventricular filling, than LBBB, which in turn leads to an increased risk of developing MACCEs (Figueroa-Triana et al., 2021). Thus, compared to patients with LBBB, this might explain why a new permanent RBBB patient seems more susceptible to ischemic cardiomyopathy (Miller et al., 2015) and at a higher risk for MACCEs and all-cause mortality. In addition, we found that patients with BBB were more likely to have higher levels of triglyceride, while patients with LBBB were more likely to have higher levels of LDL-C and apolipoprotein B. Therefore, patients with BBB had more concomitant risk factors than patients with no BBB, leading to a riskier MACCEs profile. However, the exact underlying mechanisms have yet to be fully understood. In our study, the average duration of follow-up with patients was longer than that in other studies, which might have provided additional prognostic indication of new permanent RBBB in new onset STEMI patients who underwent PCI. Moreover, RBBB is considerably influenced by some non-cardiac factors that may interfere with the predictive value of RBBB (Bussink et al., 2013; Sorensen et al., 2013). Yet, this does not seem to be the case in our study since only new onset STEMI patients with new permanent RBBB or LBBB were included. Based on previous studies and our experience in clinical practice, we found that cardiac ischemic symptoms and the appearance of a new permanent RBBB, especially in the absence of ST-segment elevation, were rather common (Peter Vibe et al., 2019). It is important to mention that these occurrences could be easily misunderstood and overlooked, leading to failed attempts to perform an urgent coronary angiography and, often, disastrous consequences.
First, our work was a retrospective observational study with a relatively small sample size that might have caused selection bias, especially for new onset LBBB and RBBB patients, which could overestimate the predictive value of RBBB and its outcome. Therefore, our findings need to be validated in future prospective and multicenter studies. Second, considering that our study was observational, confounding factors could influence our results, and new onset BBB might have been misclassified in some patients. Although patients did not have any known history of CAD or new onset BBB, our study was not structured to provide insights into the pathophysiology underlying the differences in MACCEs seen with RBBB.
Our study suggests that the occurrence of new permanent RBBB in patients with new onset STEMI may serve as a significant warning sign and be applied as a useful risk stratifier for a new high-risk onset STEMI in patients who underwent PCI.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethical approval was not provided for this study on human participants because this was a retrospective observational study, the ethics committee of the Xinjiang Medical University Affiliated Hospital of Traditional Chinese Medicine granted an exemption from ethics approval. The ethics committee waived the requirement of written informed consent for participation.
Conceived and designed the study: TZ and BW. Data collection and analyzed the data: YY. Quality control the study and revision: BW, YX, LT, and HJ. Wrote the paper: YY and JW. YY, JW, and BW contributed to the work equally and should be regarded as co-first authors. The manuscript was approved by all above authors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alkindi F., El-Menyar A., Rafie I., Arabi A., Al Suwaidi J., Singh R., et al. (2020). Clinical presentations and outcomes in patients presenting with acute cardiac events and right bundle branch block. Angiology 71, 256–262. doi:10.1177/0003319719892159
Antman Elliott M., Anbe Daniel T., Paul Wayne A., Bates E. R., Green L. A., Hand M., et al. (2004). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction-executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J. Am. Coll. Cardiol. 44, 671–719. doi:10.1016/j.jacc.2004.07.002
Arslan F., Bongartz L., Ten Berg J. M., Jukema J. W., Appelman Y., Liem A. H., et al. (2018). 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: Comments from the Dutch ACS working group. Neth. Heart J. 26, 417–421. doi:10.1007/s12471-018-1134-0
Borja I., James S., Stefan A., Ibanez B., James S., Agewall S., et al. (2018). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC).[J]. Eur. Heart J. 39, 119–177. doi:10.1093/eurheartj/ehx393
Bussink B. E., Holst A. G., Jespersen L., Deckers J. W., Jensen G. B., Prescott E. (2013). Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur. Heart J. 34 (2), 138–146. doi:10.1093/eurheartj/ehs291
Chan William K., Goodman Shaun G., David B., Fox K. A. A., Gale C. P., Chew D. P., et al. (2016). Clinical characteristics, management, and outcomes of acute coronary syndrome in patients with right bundle branch block on presentation. Am. J. Cardiol. 117, 754–759. doi:10.1016/j.amjcard.2015.12.005
Chan W. K., Goodman S. G., Brieger D., Fox K. A. A., Gale C. P., Chew D. P., et al. (2016). Clinical characteristics, management, and outcomes of acute coronary syndrome in patients with right bundle branch block on presentation. Am. J. Cardiol. 117 (5), 754–759. doi:10.1016/j.amjcard.2015.12.005
Figueroa-Triana J. F., Mora-Pabón G., Quitian-Moreno J., Alvarez-Gaviria M., Idrovo C., Cabrera J. S., et al. (2021). Acute myocardial infarction with right bundle branch block at presentation: Prevalence and mortality. J. Electrocardiol. 66, 38–42. doi:10.1016/j.jelectrocard.2021.02.009
Juntao W., Hongxing L., Chunling K., Dong S., Li J., Yu H., et al. (2018). Prognostic value of new-onset right bundle-branch block in acute myocardial infarction patients: A systematic review and meta-analysis. PeerJ 6, e4497. doi:10.7717/peerj.4497
Kawashima T., Sasaki H. (2011). Gross anatomy of the human cardiac conduction system with comparative morphological and developmental implications for human application. J. .Ann. Anat. 193, 1–12. doi:10.1016/j.aanat.2010.11.002
McCullough Peter A., Hassan Sohail A., Vinay P., Sandberg K. R., Nori D. B., Soman S. S., et al. (2005). Bundle branch block patterns, age, renal dysfunction, and heart failure mortality. Int. J. Cardiol. 102, 303–308. doi:10.1016/j.ijcard.2004.10.008
Melgarejo-Moreno A., Galcerá-Tomás J., Consuegra-Sánchez L., Alonso-Fernandez N., Diaz-Pastor A., Escudero-Garcia G., et al. (2015). Relation of new permanent right or left bundle branch block on short- and long-term mortality in acute myocardial infarction bundle branch block and Myocardial Infarction. Am. J. Cardiol. 116, 1003–1009. doi:10.1016/j.amjcard.2015.07.019
Meyer Matthias R., Radovanovic D., Pedrazzini G., Rickli H., Roffi M., Rosemann T., et al. (2020). Differences in presentation and clinical outcomes between left or right bundle branch block and ST segment elevation in patients with acute myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 9, 848–856. doi:10.1177/2048872620905101
Miller B. E., Rajsheker S., Lopez-Candales A. (2015). Right bundle branch block and electromechanical coupling of the right ventricle: An echocardiographic study. Heart Views. 16, 137–143. doi:10.4103/1995-705X.172197
Mozid Abdul M., Mannakkara Nilanka N., Robinson Nicholas M., Jagathesan R., Sayer J. W., Aggarwal R. K., et al. (2015). Comparison of clinical characteristics and outcomes in patients with left bundle branch block versus ST-elevation myocardial infarction referred for primary percutaneous coronary intervention. Coron. Artery Dis. 26, 17–21. doi:10.1097/MCA.0000000000000156
Neeland Ian J., Kontos Michael C., de Lemos James A. (2012). Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J. Am. Coll. Cardiol. 60, 96–105. doi:10.1016/j.jacc.2012.02.054
Paul A., Bhatia Kaku S., Alex Anoop G., Thomson V. S., Mani T., Sharathbabu N. M. (2020). Electrocardiographic predictors of mortality in acute anterior wall myocardial infarction with right bundle branch block and right precordial Q-waves (qRBBB). Can. J. Cardiol. 36, 1764–1769. doi:10.1016/j.cjca.2020.02.065
Peter Vibe R., Morten Wagner S., Jonas G., Pietersen A., Hansen S. M., Torp-Pedersen C., et al. (2019). Clinical implications of electrocardiographic bundle branch block in primary care. Heart 105, 1160–1167. doi:10.1136/heartjnl-2018-314295
Prakriti G., Dawn P., Christopher D. V. (2020). Mortality in patients with right bundle-branch block in the absence of cardiovascular disease.[J]. J. Am. Heart Assoc. 9, e017430. doi:10.1161/JAHA.120.017430
RBB (2022). In addition, some tables seem to be mislabeled (e.g. Table 4 is described as risk factors for severity of coronary lesions but is labeled “Incidence rate of adverse outcomes in new onset STEMI patients”) and critical findings are described incorrectly (e.g. page 9, “The results showed that patients with new permanent RBB had lower all-cause mortality, cardiac mortality,…”). Errors of this type render the manuscript difficult to follow.
Sabe Marwa A., Sabe Sharif A., Kenya K., Flamm S. D., Griffin B. P., Kwon D. H. (2016). Predictors and prognostic significance of right ventricular ejection fraction in patients with ischemic cardiomyopathy. Circulation 134, 656–665. doi:10.1161/CIRCULATIONAHA.116.022339
Sorensen J. T., Stengaard C., Sorensen C. A., Thygesen K., Botker H. E., Thuesen L., et al. (2013). Diagnosis and outcome in a prehospital cohort of patients with bundle branch block and suspected acute myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2 (2), 176–181. doi:10.1177/2048872613483591
Van de Werf F., Bax J., Betriu A., Blomstrom-Lundqvist C., Crea F., Falk V., et al. (2008). Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European society of Cardiology. Eur. Heart J. 29, 2909–2945. doi:10.1093/eurheartj/ehn416
Vernon Stephen Coffey D’Souza M., Coffey S., D'Souza M., Chow C. K., Kilian J., Hyun K., et al. (2019). ST-Segment-Elevation myocardial infarction (STEMI) patients without standard modifiable cardiovascular risk factors-how common are they, and what are their outcomes? [J]. J. Am. Heart Assoc. 8, e013296. doi:10.1161/JAHA.119.013296
Wang J., Liu C., Guo F., Zhou Z., Zhou L., Wang Y., et al. (2022). Deceleration capacity improves prognostic accuracy of relative increase and final coronary Physiology in patients with non-ST-elevation acute coronary syndrome. Front. Cardiovasc. Med. 9, 848499. doi:10.3389/fcvm.2022.848499
Widimsky P., Rohác F., Stásek J., Kala P., Rokyta R., Kuzmanov B., et al. (2012). Primary angioplasty in acute myocardial infarction with right bundle branch block: Should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? [J]. Eur. Heart J. 33, 86–95. doi:10.1093/eurheartj/ehr291
Willems J. L., Robles de Medina E. O., Bernard R., Coumel P., FisCh C., Krikler D., et al. (1985). Criteria for intraventricular conduction disturbances and pre-excitation. World health organizational/international society and federation for Cardiology Task Force ad hoc. J. Am. Coll. Cardiol. 5, 1261–1275. doi:10.1016/s0735-1097(85)80335-1
Yi Y., Yanan X., Jun W. (2020). Predictive efficacy of neutrophil-to-lymphocyte ratio for long-term prognosis in new onset acute coronary syndrome: A retrospective cohort study.[J]. BMC Cardiovasc Disord. 20, 500.
Keywords: right bundle-branch block, left bundle-branch block, gensini score, cohort study, major adverse cardiac and cerebrovascular events, ST-elevation myocardial infarction
Citation: Yang Y, Wang J, Wu B, Xu Y, Tang L, Jiang H, Wang B and Zhu T (2022) New permanent bundle-branch block and long-term prognosis of patients with new onset ST-elevation myocardial infarction who underwent percutaneous coronary intervention. Front. Physiol. 13:892623. doi: 10.3389/fphys.2022.892623
Received: 10 March 2022; Accepted: 25 July 2022;
Published: 22 August 2022.
Edited by:
Xiuyun Liu, Johns Hopkins University, United StatesReviewed by:
Yang-Yang Qu, Southeast University, ChinaCopyright © 2022 Yang, Wang, Wu, Xu, Tang, Jiang, Wang and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benfang Wang, YmZ3Njg2NkAxNjMuY29t; Tongjian Zhu, d2h1emh1dG9uZ2ppYW5AMTI2LmNvbQ==
†These authors contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.