A Commentary on
Comparison of newer hand-held ultrasound devices for post-dive venous gas emboli quantification to standard echocardiography
by Karimpour K, Brenner RJ, Dong GZ, Cleve J, Martina S, Harris C, Graf GJ, Kistler BJ, Hoang AH, Jackson O, Papadopoulou V and Tillmans F (2022). Front. Physiol. 13:907651. doi: 10.3389/fphys.2022.907651
1 Introduction
We read with interest the study by Karimpour et al. (2022) comparing two new portable devices to standard echography on the task of Venous Gas Embolism (VGE) detection in scuba divers. In operating conditions of open water dives, the authors compared portable 2D echograph Butterfly iQ and Doppler ultrasound device O’Dive to a 2D echograph Vivid Q currently used for VGE detection in research. There are however several important aspects of the study that need to be considered.
2 Reporting of VGE grades within the scope of use of each device
It is important to ensure the validity of VGE scores by respecting the scope of use of each detector. In contrast to precordial detectors screening for VGE the whole body’s venous return in one measurement, the subclavian detector O’Dive necessitates two measurements, one under each clavicle, for a single VGE evaluation. The O’Dive VGE score is calculated as the highest score within the two. While other research studies followed the user manual and reported correctly the O’Dive VGE scores (Germonpré et al., 2020) (Balestra et al., 2022), the authors of (Karimpour et al., 2022) gave several results outside its scope of use. The tables 5 and 6, sensitivity, specificity and Spearman rho in Section 3.2 are misleading, being based on one-side only subclavian measurements. The VGE grades from O’Dive are correctly reported only in Table 7 (42.7% sensitivity and 86.7% specificity) and in Spearman rho coefficient for maximum grade.
3 Dives and monitoring information missing
The authors stated the need to obtain more ultrasonic data in the field conditions as a main motivation of their study. For a field study, the reader would like to have an idea about the range of exposures (depth, duration, gases) being monitored. The inter/intra subject variability in low VGE scores observed after shallow dives can be greater and higher scores from provocative dives could be more stable. Indeed, in (Balestra et al., 2022), the results in 6 divers on provocative dives lead to a very good agreement between grades from O’Dive and grades from a portable echography device. In (Karimpour et al., 2022), 74% of VividQ scores within 141 paired ButterflyiQ/VividQ scores were 0 or 1, suggesting non-provocative diving.
To evaluate monitoring difficulty with each device in operating conditions the reader would need 1) the total number of dives that authors attempted to monitor, 2) the number of dives successfully monitored at least once with at least one device, 3) the number of VGE scores obtained with each device, 4) the number of dives with a full set of measurements for each device. Moreover, it would be pertinent to report if for some divers the monitoring was complicated or impossible due to some physiological characteristics. Unfortunately, the only information about monitored dives and divers provided was the number of subjects enrolled in the study.
4 VGE scores included in and excluded from the comparative analysis
The authors excluded from analysis VGE scores from devices when a paired measurement from other device was unavailable. Unfortunately, for O’Dive the authors did not report either number of measurements discarded, or the associated VGE scores. Thanks to the study data communicated by authors, we recovered this information: there were 267 successful measurements with O’Dive and 187 successful measurements with Vivid Q, 40% more O’Dive VGE evaluations were successful compared to Vivid Q. The authors analysed 173 matched pairs of scores from O’Dive and VividQ, thus excluding from analysis 35% of all O’Dive measurements and 7.5% of all Vivid Q measurements. As such a large percentage was excluded from analysis, we summarized in Table 1 the VGE scorings from O’Dive and Vivid Q for both included and excluded data. In particular, we remark that more than half High Bubble Grades (HBG: grades 3 or greater) from O’Dive were excluded from analysis, while it is not the case for Vivid Q.
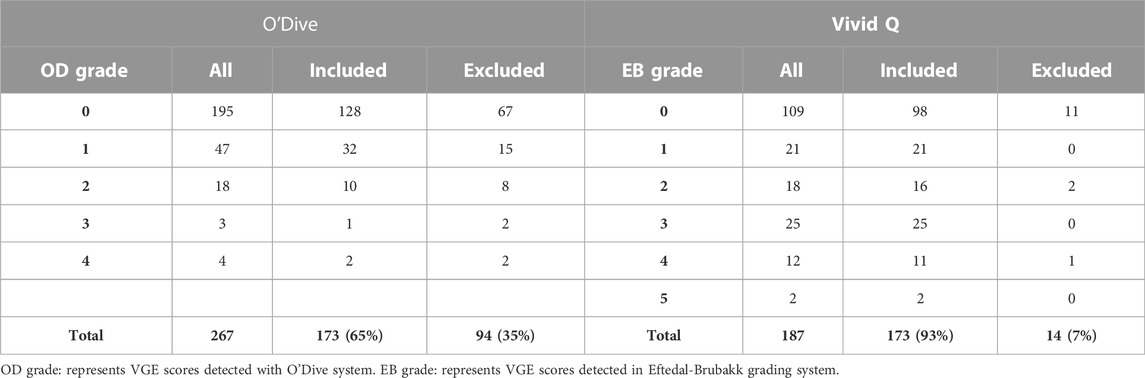
TABLE 1. Number of VGE measurements included in comparative study and excluded measurements from O’Dive and Vivid Q.
5 Equivalence of VGE scores from echographs and doppler detectors
It would be interesting to identify if the difference in VGE scores between Vivid Q and O’Dive comes from the measurement site (subclavian vs. precordial), the technology (Doppler vs. echography) and/or their respective scoring systems. In contrast with classical results (Eftedal and Brubakk, 1997; Brubakk et al., 2001), a recent study (Fichtner et al., 2021) indicates that the EB grades from echography are probably no longer equivalent to Spencer grades from Doppler VGE when evaluation is done at the same measurement site. In (Fichtner et al., 2021), Doppler Spencer grades were systematically lower than echography EB grades, for both precordial and subclavian measurements.
VGE is usually used in research studies to evaluate the DCS risk. Most of historical data relating VGE and DCS risk covers Doppler VGE scored on Kissman-Masurel or Spencer scale (Gardette, 1979) (Vann et al., 1982) (Eatock, 1984) (Sawatzky, 1991) (Hugon et al., 2018), with the two main results for 2D echography EB grades all prior to 2007 (Eftedal et al., 2007) (Doolette, 2016). If the equivalence between scales is lost because of a significant improvement in echograph resolution in VGE detection, the relevance of the additional bubbles detected by echography in DCS risk evaluation should be investigated.
6 Conclusion
For medical research, very sensitive VGE detection with a state-of-the-art medical echograph should be preferred when logistics, budget and the availability of a trained technician allow.
Non-etheless, newer devices are opening the way of easy and large-scale studies in the field allowing for wider-ranging investigation of the influence of diverse physiological and external conditions on variability of VGE and decompression risk.
The conclusion (Karimpour et al., 2022) on weak sensitivity of O’Dive compared to Vivid Q based on incorrect (single-side measurements) device usage and unspecified data selection (35% of O’Dive measurements discarded vs. 7% for Vivid Q) in the context of non-provocative diving is unfounded. The conclusion on usability of Butterfly iQ (specificity 85.6%) in studies interested in specificity should also be extended to O’Dive provided its even higher specificity (86.7%).
We also suggest the necessity to reconsider the equivalence of EB vs. Doppler Spencer grades because of the increased sensitivity of echographs (Recommendation 13 of (Mollerlokken et al., 2016)) and to evaluate its importance in DCS risk quantification.
Author contributions
MA and BA contributed to conception and design of the study. MA performed the statistical analysis. MA wrote the first draft of the manuscript. BA and MA contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
Authors AM and AB are employed by Azoth Systems, the company that developed and markets the O'Dive Doppler ultrasound technology. AB is the founder and president of Azoth Systems and AM is in charge of statistical processing and analysis in the company.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Balestra C., Guerrero F., Theunissen S., Germonpré P., Lafère P. (2022). Physiology of repeated mixed gas 100-m wreck dives using a closed-circuit rebreather: A field bubble study. Eurorean J. Appl. Physiology 122, 515–522. doi:10.1007/s00421-021-04856-5
Brubakk A. O., Eftedal O. (2001). Comparison of three different ultrasonic methods for quantification of intravascular gas bubbles. Undersea Hyperbaric Med. 28 (3), 131–136.
Doolette D. J. (2016). Venous gas emboli detected by two-dimensional echocardiography are an imperfect surrogate endpoint for decompression sickness. Diving Hyperbaric Med. 46, 4–10.
Eatock B. C. (1984). Correspondence between intravascular bubbles and symptoms of decompression sickness. Undersea Biomed. Res. 11, 326–329. doi:10.28920/dhm48.3.132-140
Eftedal O., Brubakk A. O. (1997). Agreement between trained and untrained observers in grading intravascular bubble signals in ultrasonic images. Undersea Hyperbaric Med. 24 (4), 293–299.
Eftedal O. S., Lydersen S., Brubakk A. O. (2007). The relationship between venous gas bubbles and adverse effects of decompression after air dives. Undersea Hyperbaric Med. 34 (2), 99–105.
Fichtner A., Brunner B. P., Pohl T., Grab T., Fieback T., Koch T. (2021). A Doppler ultrasound self-monitoring approach for detection of relevant individual decompression stress in scuba diving. Intern. Emerg. Med. 17 (1), 173–180. doi:10.1007/s11739-021-02802-z
Gardette B. (1979). Correlation between decompression sickness and circulating bubbles in 232 divers. Undersea Biomed. Res. 6, 99–107.
Germonpré P., Van der Eecken P., Van Renterghem E., Germonpré F. L., Balestra C. (2020). First impressions: Use of the azoth systems O’Dive subclavian bubble monitor on a liveaboard dive vessel. Diving Hyperbaric Med. 50 (4), 405–412. doi:10.28920/dhm50.4.405-412
Hugon J., Metelkina A., Barbaud A., Nishi R., Bouak F., Blatteau J. E., et al. (2018). Reliability of venous gas embolism detection in the subclavian area for decompression stress assessment following scuba diving. Diving Hyperbaric Med. 48 (3), 132–140. doi:10.28920/dhm48.3.132-140
Møllerløkken A., Blogg S. L., Doolette D. J., Nishi R. Y., Pollock N. W. (2016). Consensus guidelines for the use of ultrasound for diving research. Diving Hyperbaric Med. 46 (1), 26–32.
Sawatzky K. D., Thesis M. Sc. (1991). The relationship between intravascular Doppler-detected gas bubbles and decompression sickness after bounce diving in humans. Toronto: York University.
Keywords: decompression sickness, decompression stress, diving, bubble, Doppler
Citation: Asya M and Axel B (2023) Commentary: Comparison of newer hand-held ultrasound devices for post-dive venous gas emboli quantification to standard echocardiography. Front. Physiol. 13:1074436. doi: 10.3389/fphys.2022.1074436
Received: 19 October 2022; Accepted: 19 December 2022;
Published: 05 January 2023.
Edited by:
Pieter-Jan A. M. Van Ooij, Royal Netherlands Navy, NetherlandsReviewed by:
Caterina Guiot, University of Turin, ItalyCopyright © 2023 Asya and Axel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Barbaud Axel, YXhlbC5iYXJiYXVkQGF6b3RoLXN5c3RlbXMuY29t
 Metelkina Asya
Metelkina Asya Barbaud Axel
Barbaud Axel