- 1Department of Acupuncture and Moxibustion, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2The Affiliated Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
Background: Acupuncture has been extensively applied to manage irritable bowel syndrome (IBS) in clinical practice in China. Some randomized controlled trials (RCTs) have demonstrated their efficacy, but it has rarely been compared with first-line antispasmodics to verify their effectiveness. Therefore, we compare acupuncture with antispasmodics in the treatment of IBS by using an adjusted indirect treatment comparison meta-analysis.
Methods: Embase, OVID Medline, and the Cochrane Central Register of Controlled Trials databases were searched from inception to 14 March 2022, with no language restrictions. RCTs comparing antispasmodics or acupuncture with placebo or one of the antispasmodics were enrolled. The primary outcome of interest was the improvement of abdominal pain. And the secondary outcomes of interest were the relief of global IBS symptoms and adverse events. The random-effects model was utilized to pool data. The effect size was measured by standardized mean difference (SMD) or relative ratio, and the effectiveness of acupuncture and different antispasmodics were ranked by P-scores.
Results: Thirty-five RCTs (n = 5,190) were included. The analysis showed that cimetropium, drotaverine, acupuncture, and pinarverium were superior over placebo in relieving abdominal pain; cimetropium (SMD, −3.00 [95%CI, −4.47 to −1.53], P-score = 0.99) ranked the most effective. In pairwise comparisons, acupuncture had a greater improvement than most antispasmodics except cimetropium and drotaverine in relieving abdominal pain, although the between-group difference was statistically insignificant. In the analysis of continuous outcome in the relief of global IBS symptoms, the result showed that pinaverium was more effective (SMD, 1.72 [95%CI, 0.53 to 2.92], P-score = 0.90) than placebo. Trimebutine and acupuncture had greater improvements than placebo, but no significant difference was shown between groups. In pairwise comparisons, acupuncture was more effective than pinaverium (SMD, −1.11 [95%CI, −1.94 to −0.28]) in relieving global IBS symptoms. In the analysis of adverse events, acupuncture had a lower adverse event rate than most of the other antispasmodics.
Conclusion: Cimetropium, drotaverine, and acupuncture were all better than placebo in improving abdominal pain. Acupuncture was preferred over pinaverium in relieving global IBS symptoms, and acupuncture had lower adverse events than most antispasmodics.
Introduction
Irritable bowel syndrome (IBS) is a commonly functional gastrointestinal disorder characterized by abdominal pain associated with changes in stool form and/or frequency (Drossman and Hasler, 2016). The relative surveys had shown IBS prevalence was 16.8%. Participants suffering from IBS were characterized by a higher prevalence of psychiatric diagnosis and sleep disturbances, higher levels of job strain and isostrain as well as by lower levels of workability compared to non-affected subjects (Buselli et al., 2021). Because the mechanisms of IBS are multifactorial and complicated (Ford et al., 2020), IBS is challenging to manage and has a significant impact on social functioning and quality of life (Frändemark et al., 2018). The previous evidence showed that after 1 and 7 years, over 50% of patients with IBS had the same symptoms and a further one-quarter of patients reported consistent mild IBS symptoms (Agréus et al., 2001). At the same time, based on a burden of disease study, it was reported that the costs directly attributable to IBS in the USA were estimated at US$1 billion and indirect costs were as high as $50 million (Everhart and Ruhl, 2009). Currently, the Rome IV criteria recommend that the choice of treatment should focus on the major symptomatology. According to predominant bowel habits, the pharmacological therapies include soluble fiber (Galica et al., 2022), antispasmodic drugs (Annaházi et al., 2014), central neuromodulators (Fadgyas Stanculete et al., 2021), intestinal secretagogues (Brenner et al., 2018), drugs acting on opioids, or 5-HT receptors (Jones et al., 2021), or minimally absorbed antibiotics (Li et al., 2016). Because antispasmodics were available for all subtypes of IBS, and accumulating evidence showed that antispasmodics can effectively and safely regulate gastrointestinal motility disturbances, improve bowel habits, and relieve abdominal pain/discomfort (Ruepert et al., 2011; Martínez-Vázquez et al., 2012). The international clinical practice guidelines recommended that antispasmodics were considered as the first-line therapy for IBS (Moayyedi et al., 2019).
In China, acupuncture has been extensively applied to manage gastrointestinal diseases in clinical practice. The relative evidence reported that acupuncture can regulate the bowel characteristics and frequency of stool for IBS (Manheimer et al., 2012a). Nevertheless, throughout the past 20 years, the studies of acupuncture concentrated primarily on the specific effect of acupuncture vs. sham acupuncture. Although previous trials investigated the impact of acupuncture on IBS, the majority of trials compared acupuncture with a placebo, and only a minority of them directly compared acupuncture with conventional treatments such as antispasmodics. Three randomized controlled trials (RCTs) which compared acupuncture with pinaverium showed that acupuncture seemed to be more effective in alleviating abdominal pain, improving stool frequency, and reducing the recurrence rate for the management of IBS (Li et al., 2012; Pei et al., 2020). However, the relative study between acupuncture and other antispasmodics such as cimetropium or drotaverine was scarce.
Regarding that antispasmodics have been conventionally prescribed as the first-line drug for IBS (Quigley et al., 2016), it is essential to compare acupuncture and antispasmodics to verify the effectiveness of acupuncture. Therefore, we conducted an adjusted indirect meta-analysis to compare acupuncture with antispasmodics in order to confirm whether acupuncture was equally effective to antispasmodics in the management of IBS.
Methods
Study source
We searched the following three electronic databases from inception to 14 March 2022: Embase, OVID Medline, and the Cochrane Central Register of Controlled Trials (CENTRAL). RCTs comparing antispasmodics or acupuncture with placebo or one of the antispasmodics were included. Furthermore, Clinical registries (Clinicaltrials.gov) and published systematic reviews were also searched for any missed RCTs. Besides, we did not limit the language type in our search. A list of search strategies can be found in Supplementary Table S1.
Study selection
Two investigators independently reviewed the abstract and title, and read the full text in detail to identify included articles. The articles met the following criteria: 1) Diagnostic criteria were limited to Rome I, II, III, and IV criteria; 2) RCTs comparing antispasmodics or acupuncture with placebo or one of the antispasmodics were included; 3) Adult patients with IBS were included; 4) The treatment duration and dose range were limitless, but the interventions were provided for at least a week; 5) At least one of the targeted outcome measurement listed below was required to be obtainable: global IBS symptoms, abdominal pain, or adverse events; 6) RCTs with both inflammatory bowel diseases and IBS were included if IBS date were independently showed. We harmonized any disagreements by consensus and finally judged by a third investigator.
Outcome assessments
The primary outcome of interest was the improvement of abdominal pain. And the secondary outcome of interest was the relief of global IBS symptoms. We also assessed the number of treatment-related adverse events for the safety outcome.
Data collection
According to a standardized form, one investigator extracted the descriptive data, which was then verified by another investigator. We abstracted the following data from the included study: author, published year, study design, the proportion of female participants, mean age, diagnostic criteria, IBS subtype, details of interventions and controls, and outcome data. The number of participants and corresponding events was presented with dichotomous data, while continuous data was presented as mean and standard deviation.
Risk of bias assessment
The risk of bias of each RCT was evaluated by the second edition of the Cochrane risk of bias (RoB 2.0) (Sterne et al., 2019). Each study was assessed in five parts with certain questions in RoB 2.0, finally, the overall risk of bias for the study was judged to be low, some concerns or high. Besides, we also utilized the GRADE system to evaluate the confidence level of evidence in this study. And according to the quality assessment of study design, risk of bias, indirectness, inconsistency, imprecision, and other consideration, the evidence was classified into four levels: high quality, moderate quality, low quality, or very low quality.
Data synthesis
We used the frequentist method to conduct this indirect treatment comparison meta-analysis (Rücker, 2012). We plotted net graphs to identify direct and indirect comparisons between acupuncture and different antispasmodics. A random-effects model was applied to compare the included treatments in this meta-analysis. Forest plots were drawn according to the different outcomes, showing acupuncture or antispasmodics vs. placebo, and displaying the effect sizes and their associated 95% confidence intervals (95%CIs). We calculated the relative ratio (RR) for categorical outcomes including the relief responder rate and adverse event rate. If the relative study with zero events in an arm, it was excluded from the analysis (Mills et al., 2013). For continuous outcomes such as the change in abdominal pain and the improvement of global IBS symptoms, we used the standardized mean difference (SMD). If continuous outcomes were evaluated at different time points, they were combined by using a multivariate analysis (Riley et al., 2017). Besides, the effectiveness of acupuncture and different antispasmodics were ranked by the P-scores method (Rücker and Schwarzer, 2015). P-scores were based solely on the point estimates and standard errors of the frequentist network meta-analysis estimates under normality assumption. They measure the mean extent of certainty that a treatment was better than the competing treatments. The consistency of the network was checked by comparing network estimates, indirect, and direct. And we examined the implications of inconsistency through the use of the z-test. In addition, the transitivity assumption in this study was evaluated through the global heterogeneity, which was estimated by calculating the tau-squared statistics and global I2. The global heterogeneity was categorized into three levels of small, large, and very large according to the cutoff point of I2<50%, 50% ≤ I2<75%, and I2 ≥ 75%, respectively. When large heterogeneity emerged, we conducted a design-by-treatment analysis by decomposing Cochran’s Q to identify the reason for heterogeneity (Krahn et al., 2013).
Results
Trial characteristics
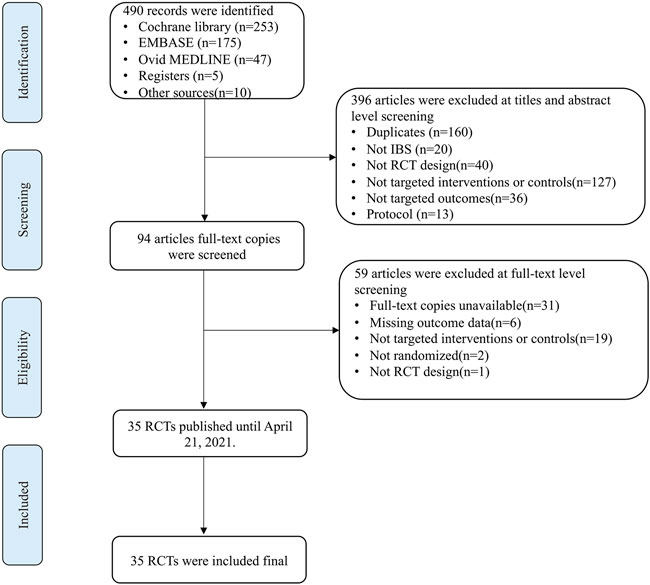
A total of 490 articles were detected in the initial search. 160 duplicate articles were excluded by using Zotero and manual searches. After screening the titles and abstracts, 236 articles were excluded. Then, full-text copies were screened based on the inclusion and exclusion criteria, and 59 articles were further excluded. Ultimately, 35 articles were included in this study. The flow of studies through the selection process is presented in Figure 1.
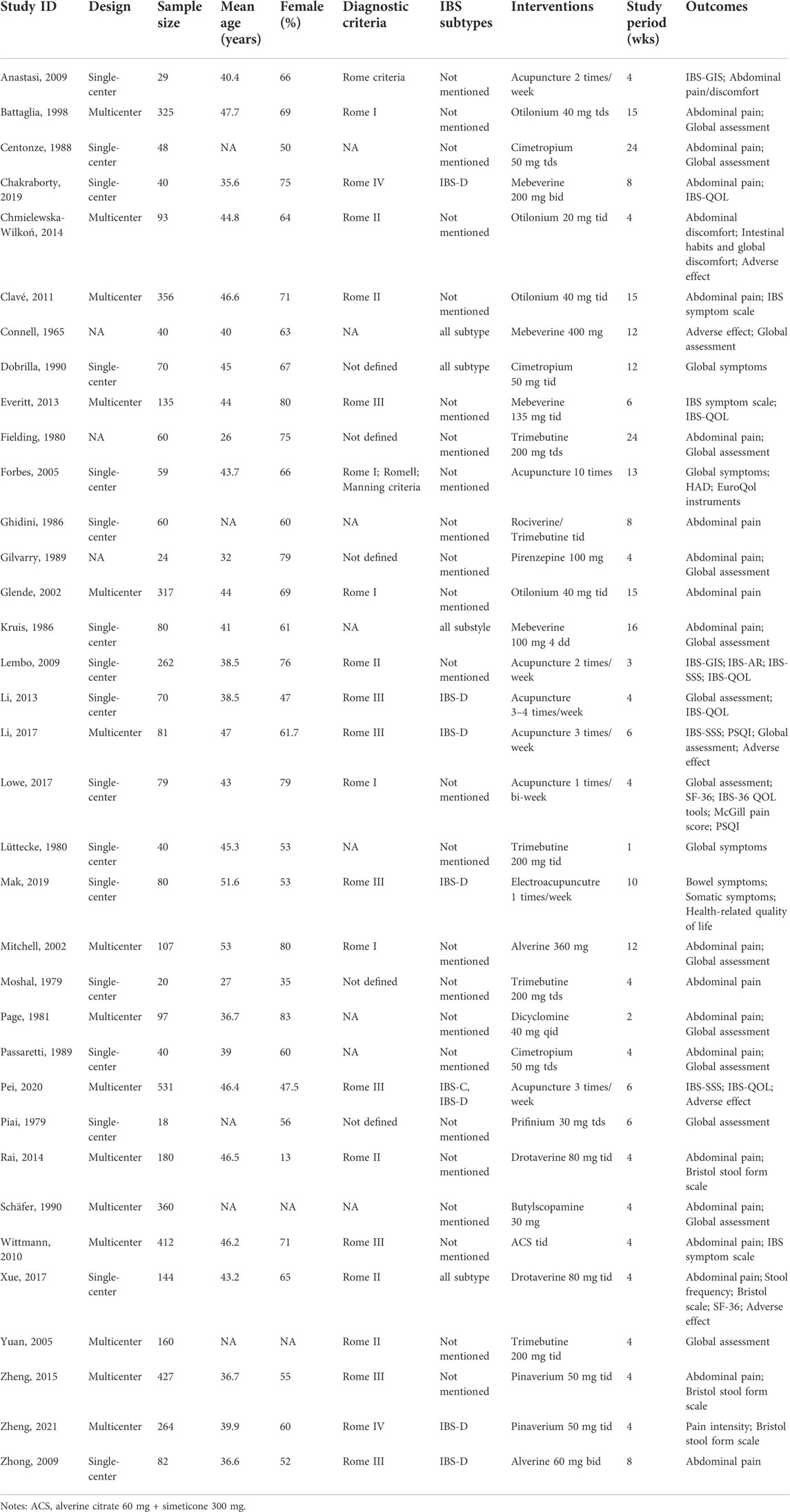
In the 35 articles, 27 assessed the effects of antispasmodics (3,999 participants), and 8 RCTs assessed acupuncture (1,191 participants). The median age of included participants was 35.6 years (range, 26–51.6 years), and the percentage of females was 59%. The detailed characteristics of interventions, controls, and outcomes of the included 35 articles are shown in Table 1.
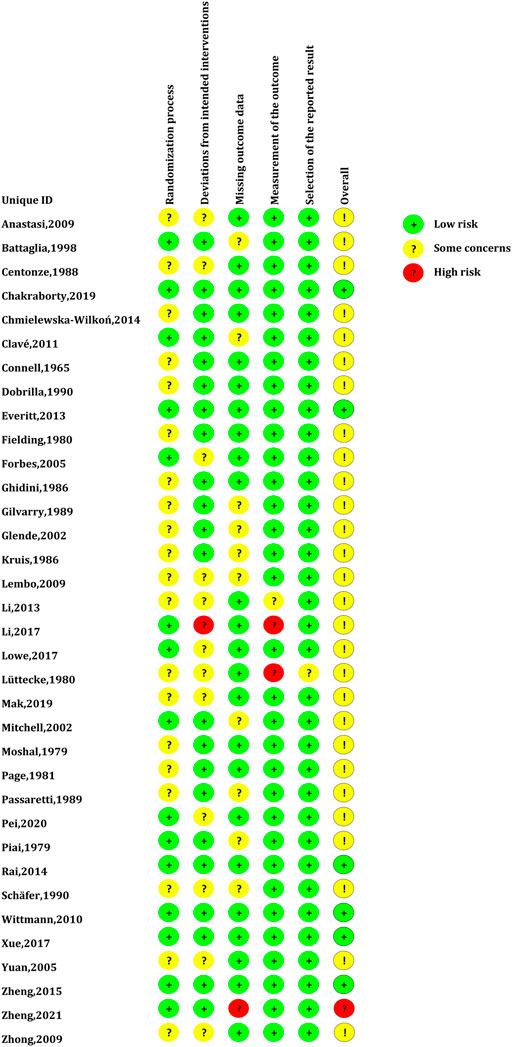
The global risk-of-bias assessment demonstrated that there were 6 RCTs (17.14%) with a low risk of bias, 28 (80%) RCTs with a moderate risk of bias, and 1 RCT (2.86%) with a high risk of bias. The risk of bias assessment for individual RCT is presented in Figure 2.
GRADE assessment demonstrated that the comparative quality of acupuncture vs. antispasmodics was very low for the improvement of abdominal pain and global IBS symptoms, and the adverse events were of low quality. The summary of findings is shown in Supplementary Table S2.
The improvement of abdominal pain
This analysis contained 9 RCTs (n = 2086), and assessed eight treatments in total; 4 RCTs evaluated the effectiveness of antispasmodics, and 5 RCTs assessed acupuncture. The result showed that cimetropium (SMD, −3.00 [95%CI, −4.47 to −1.53], P-score = 0.99, global I2 = 82.2%, Figure 3A) was ranked as the most effective treatment. Drotaverine, acupuncture, and pinarverium were superior to placebo (Figure 3A). In pairwise comparisons, cimetropium was better than most other treatments in relieving abdominal pain, except drotaverine. Compared with antispasmodics, acupuncture had a greater improvement than most antispasmodics except cimetropium and drotaverine in relieving abdominal pain, but the between-group difference was not significant (Figure 3B).
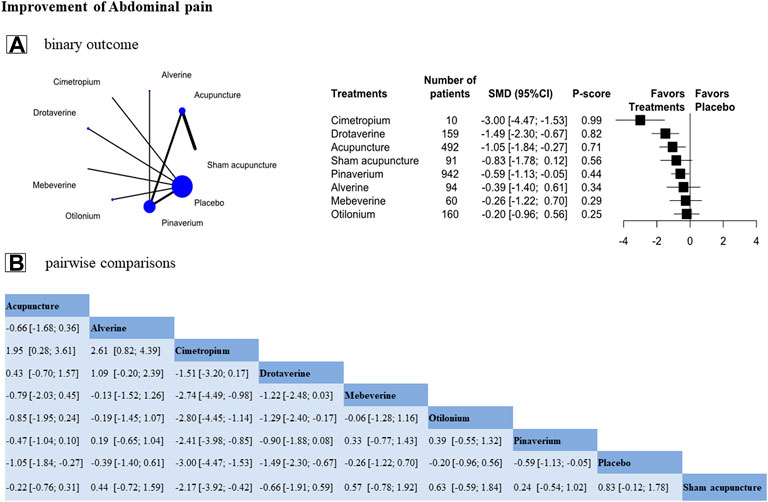
FIGURE 3. Individual-level comparison of the improvement of abdominal pain. Footnote: Individual-level analysis results (A) and the pairwise comparisons results (B) are shown in this figure (A): The geometry of the networks is shown on the left. The size of the blue nodes corresponds to the number of participants assigned to treatments. The right shows the forest plots using placebo as a reference. Direct comparison was linked by a line between two treatments; the thickness of the lines corresponds to the number of trials that studied the treatment. P-scores are used to rank the effectiveness of each treatment. Treatments with the highest p values are the most effective. Standardized mean difference (SMD) > 0 means this treatment superiority over placebo (B): A comparison estimate and its 95% confidence intervals (95% CI) are in the cell between column-defining treatment and row-defining treatment. The upper triangle shows pairwise comparisons of column-defining treatment vs. row-defining treatment. The lower triangle shows pairwise comparisons of row-defining treatment vs. column-defining treatment. For abdominal pain in the upper triangle, SMD>0 favors row-antispasmodics, SMD<0 favors column-acupuncture.
The relief of global IBS symptoms
We analyzed 16 RCTs (n = 2,307) on binary outcomes in relieving the symptoms of global IBS and assessed 13 treatments in total (Figure 4A). The result showed that drotaverine (RR, 2.17 [95%CI, 1.13 to 4.14], P-score = 0.82, global I2 = 47.4%, Figure 4A) was ranked as the most effective treatment. Drotaverine and cimetropium were better than placebo in relief of global IBS symptoms, and acupuncture also had a greater relief than placebo, but no significant between-group difference was noted (RR, 1.67 [95%CI, 0.84 to 3.32], P-score = 0.69, Figure 4A).
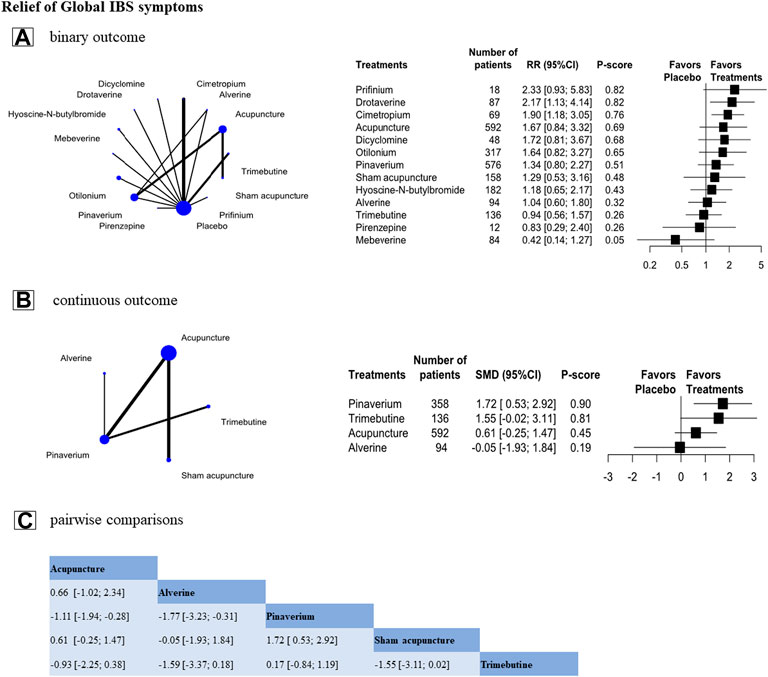
FIGURE 4. Individual-level comparison of the relief of Global IBS symptoms. Footnote: Individual-level binary and continuous outcomes analysis results (A,B) and the pairwise comparisons of continuous outcome results (C) are shown in this figure (A,B): The geometry of the networks is shown on the left. The size of the blue nodes corresponds to the number of participants assigned to treatments. The right shows the forest plots using placebo as a reference. Direct comparison was linked by a line between two treatments; the thickness of the lines corresponds to the number of trials that studied the treatment. P-scores are used to rank the effectiveness of each treatment. Treatments with the highest p values are the most effective. (A): Standardized mean difference (SMD) > 0 means this treatment superiority over placebo. (B): Relative ratio (RR) > 1 means this treatment superiority over placebo (C): A comparison estimate and its 95% confidence intervals (95% CI) are in the cell between column-defining treatment and row-defining treatment. The upper triangle shows pairwise comparisons of column-defining treatment vs. row-defining treatment. The lower triangle of shows pairwise comparisons of row-defining treatment vs. column-defining treatment. For the global IBS symptoms in the upper triangle, SMD>0 favors row-antispasmodics, SMD<0 favors column-acupuncture.
In the analysis of continuous outcome in relieving the symptoms of global IBS, we included eight RCTs (n = 1,072) and assessed 4 treatments (Figure 4B). The result showed that pinaverium was more effective (SMD, 1.72 [95%CI, 0.53 to 2.92], P-score = 0.90, global I2 = 89.7%, Figure 4B) than placebo. Trimebutine, acupuncture, and alverine were not superior to placebo (Figure 4B). However, in pairwise comparisons, acupuncture was preferred over pinaverium in relieving global IBS symptoms (SMD, −1.11 [95%CI, −1.94 to −0.28]). But compared to other antispasmodics, acupuncture had a non-significantly in relieving the symptom of global IBS (Figure 4C).
Adverse events
The analysis contained 17 RCTs (n = 2,412); 15 RCTs evaluated the effects of antispasmodics, and 2 RCTs assessed acupuncture. The individual-level analysis-assessing 10 treatments-demonstrated that acupuncture had similar adverse event rate to placebo (RR, 0.30 [95%CI, 0.01 to 8.89], P-score = 0.17, global I2 = 0%, Figure 5A), and trimebutine (RR, 28.36 [95%CI, 1.74 to 461.19], P-score = 0.96), cimetropium (RR, 5.53 [95%CI, 1.46 to 20.94], P-score = 0.84), dicyclomine (RR, 4.21 [95%CI, 2.17 to 8.16], P-score = 0.81) had higher adverse event rate than placebo (Figure 5A). In pairwise comparisons, acupuncture had a significantly lower adverse events rate than most other treatments (Figure 5B).
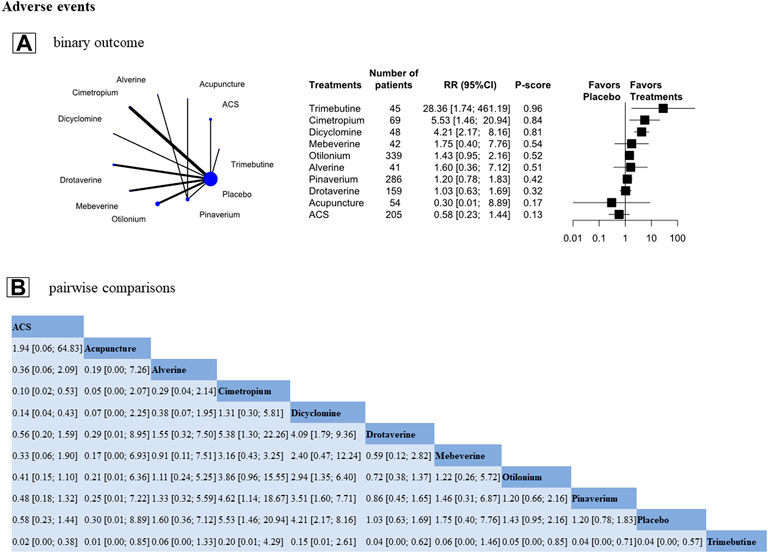
FIGURE 5. Treatment-related adverse events. Footnote: Individual-level analysis results (A) and the pairwise comparisons results (B) are shown in this figure (A): The geometry of the networks is shown on the left. The size of the blue nodes corresponds to the number of participants assigned to treatments. The right shows the forest plots using placebo as a reference. Direct comparison was linked by a line between two treatments; the thickness of the lines corresponds to the number of trials that studied the treatment. P-scores are used to rank the adverse events rate of each treatment. Treatments with the highest p values are the most adverse events. (A): Relative ratio (RR) > 1 means this treatment high over placebo (B): A comparison estimate and its 95% confidence intervals (95% CI) are in the cell between column-defining treatment and row-defining treatment. The upper triangle shows pairwise comparisons of column-defining treatment vs. row-defining treatment. The lower triangle of shows pairwise comparisons of row-defining treatment vs. column-defining treatment. For the adverse events in the upper triangle, RR > 1 favors row-antispasmodics have a higher adverse events, RR < 1 favors column-acupuncture has a lower adverse events.
In the antispasmodics, the main common adverse events were dry mouth, heartburn sensation, sleepiness, nausea, headache, flatulence, dizziness, or weakness. And the adverse events of acupuncture were slight hematoma around the site of needling and stabbing pain. These conditions were mild, and no medical care was necessary.
Discussion
As far as we know, this study first used an adjusted indirect treatment comparison method to respond to the clinical issue: Is acupuncture as equivalent as antispasmodics in terms of improving abdominal pain and global IBS symptoms? In this meta-analysis, we found that acupuncture and some antispasmodics (e.g., cimetropium, drotaverine) were better than placebo in improving abdominal pain. In pairwise comparisons, acupuncture was preferred over pinaverium in relieving the symptom of global IBS, and acupuncture had a significantly lower adverse events rate than most other antispasmodics.
The evidence from previous studies about acupuncture for IBS is relatively lacking and contradictory. On one hand, a Cochrane systematic review including17 RCTs reported that the effective rate of acupuncture for IBS was better than pharmacological interventions (Manheimer et al., 2012a), but the pharmacological interventions were sundry and included Chinese herbal formula, probiotics, pinaverium bromide, and sulfasalazine, etc. Another systematic review similarly confirmed that at 6-month follow-up, acupuncture was more beneficial for overall symptoms of IBS compared to standard medical treatment (Amsallem et al., 2021). The recent research was validated again and reported that acupuncture may be a more effective treatment than PEG 4000/pinaverium bromide in terms of improving the symptoms of IBS (Pei et al., 2020). Our study partially confirmed this result and showed acupuncture had more beneficial effects than pinaverium in relieving the symptom of global IBS, but compared to other antispasmodics, acupuncture had non-significantly benefits. We considered that this difference may be related to the fact that we did not include other pharmacological interventions except for antispasmodics. On the other hand, another previous study indicated that acupuncture achieved favorable therapeutic benefits, but no statistically significant difference was noted between acupuncture and sham acupuncture (Manheimer et al., 2012b; Lowe et al., 2017). In this study, we also found that acupuncture can improve IBS global symptoms compared with sham acupuncture, but the between-group difference was not significant (SMD, −0.22 [95%CI, −0.76 to 0.31]). Besides, the previous relative study showed that non-specific effects may lead to statistically significant results in the treatment of IBS (Kaptchuk et al., 2008).
The above result indicated that sham acupuncture maybe not be an inert control for IBS. Therefore, the comparison between acupuncture and positive drugs seems to be necessary and able to clearly define the effectiveness of acupuncture for IBS in the future. However, it is worth noting that the GRADE assessment demonstrated that the quality of acupuncture vs. antispasmodics was low for the improvement of abdominal pain and global IBS symptoms. But it does not mean that there is a problem with this research itself, and it is mainly caused by the risk of bias in the included literature, the diversity of antispasmodics, and the nature of indirect comparisons.
As we all know, the mechanisms of IBS are complicated. Relative studies reported that the possible mechanisms included the brain-gut axis, gastrointestinal motility, the immune system, visceral hypersensitivity, and neurotransmitters (Yaklai et al., 2021; Qi et al., 2022). In this study, the result showed that cimetropium, drotaverine, acupuncture, and pinaverium were effective in improving global IBS symptoms. At present, antispasmodics were medications with anticholinergic or calcium channel blocking effects (Annaházi et al., 2014; Chey et al., 2015), which can inhibit intestinal wall contraction and regulate intestinal transport time by improving visceral hypersensitivity and intestinal motility (Martínez-Vázquez et al., 2012; Camilleri, 2018). Some evidence showed that drotaverine had antispasmodic effects on intestinal smooth muscle by inhibiting calcium calmodulin complex and phosphodiesterase enzyme system (Rai and Nijhawan, 2021); Cimetropium was mediated by antagonizing acetylcholine in intestinal smooth muscle muscarinic receptors to achieve antispasmodic effect; Pinaverium was an L-type calcium-channel blocker, which can inhibit calcium influx and prevent colonic smooth muscle cell contractions (Annaházi et al., 2014). However, due to the characteristics of multi-link and multi-target of acupuncture, there is still a lack of in-depth understanding of the mechanisms associated with acupuncture in the treatment of IBS. Relative studies had confirmed that acupuncture can improve visceral hypersensitivity and intestinal motility by regulating the Epac1-Piezo 2 axis and reducing 5-HT and 5-HTR expressions (Zhao et al., 2016; Guo et al., 2022) and regulate the brain-gut axis and nervous system by affecting neurotransmitters including 5-HT, substance P, calcitonin gene-related peptide, nitric oxide, and norepinephrine. In addition, IL-18, IL-23, TNF-α, mast cells, and other immune cells and inflammatory factors may be also involved in the regulation of IBS by acupuncture (Wu et al., 2008; Ma et al., 2014).
Compared to the mechanisms of antispasmodics and acupuncture in the treatment of IBS, we found that both of them can improve intestinal hypersensitivity and intestinal motility. But the mechanisms of acupuncture are relatively complicated and diverse. Several challenges should be resolved before acupuncture was implemented into regular clinical practice. Firstly, A further revelation about these mechanisms of action about acupuncture is of importance to the clinical practice. Secondly, compared to the other pharmacological treatments, acupuncture is a complicated intervention and its therapeutic effects are affected by a series of factors such as needling sensation, acupuncture manipulation, acupoint specificity, psychological factors, and needle duration (Shi et al., 2012). Currently, the parametrization of acupuncture and acupoint selection for the treatment of IBS vary in diverse literature, and until now, there are no relevant studies to explore an optimal, and standardized acupuncture treatment strategy for IBS. Therefore, it is extremely important to use all the above influencing factors for clinical practice to evaluate the true effectiveness of acupuncture for IBS in future studies.
There are some limitations in our study. Firstly, we compared acupuncture with the majority of antispasmodics on the basis of indirect estimates. While the indirect estimates borrowed their power from a variety of sources including direct comparisons of antispasmodics vs. acupuncture, antispasmodics vs. placebo, and acupuncture vs. placebo. It may lead to inaccurately represent the difference between acupuncture and antispasmodics. However, the comparison between pinaverium and acupuncture is consistent for the direct and indirect estimates, which indicated to some extent the credibility of the indirect evidence. Secondly, the analysis of continuous outcomes in the relief of global IBS symptoms and abdominal pain showed slightly greater heterogeneity, the variety of antispasmodics such as different types, dosages, usages, and duration of treatment and different acupuncture prescriptions maybe contribute to the statistical heterogeneity. Thirdly, in order to minimize the selectivity bias of the literature, our inclusion definitions ranged from Rome I to Rome IV. The inclusion criteria are relatively broad, which may lead to cloud the interpretation of data. Fourth, most studies lacked follow-up information for antispasmodics, and we did not evaluate the prolonged effect of acupuncture vs. antispasmodics in the treatment of IBS. But relative studies indicated that acupuncture can continue to improve overall symptoms of IBS lasting for 1–3 months after one-course treatment (Lowe et al., 2017; Mak et al., 2019; Pei et al., 2020). These findings suggested that acupuncture might have a long-term effect and be beneficial in maintaining a sustainable alleviation of IBS symptoms.
Conclusion
Cimetropium, drotaverine, and acupuncture were all better than placebo in improving abdominal pain. Acupuncture was preferred over pinaverium in relieving global IBS symptoms, and acupuncture had lower adverse events than most antispasmodics.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
HZ and S-GY designed the study. Y-ZS, Q-FT, and DQ collected and organized the study data. HZ, Y-ZS, and MC analyzed and interpreted the data. Y-ZS and Q-FT wrote the first draft of the manuscript. All authors revised the manuscript and approved it for publication.
Funding
This study was supported by the National Key Research and Development Program of the Ministry of Science and Technology of the People’s Republic of China (No. 2019YFC1709004), the Sichuan Youth Science and Technology Innovation Research Team (No. 2021JDTD0007), and the Subject Talents Program for Improving Scientific Research Capacity of Chengdu University of Traditional Chinese Medicine (No. BSH2020027).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2022.1001978/full#supplementary-material
References
Agréus L., Svärdsudd K., Talley N. J., Jones M. P., Tibblin G. (2001). Natural history of gastroesophageal reflux disease and functional abdominal disorders: A population-based study. Am. J. Gastroenterol. 96, 2905–2914. doi:10.1111/j.1572-0241.2001.04680.x
Amsallem F., Sanchez S., Armoiry X., Mion F. (2021). Effectiveness of non-pharmacological interventions for irritable bowel syndrome: A systematic review. Evid. Based. Complement. Altern. Med. 2021, 4404185. doi:10.1155/2021/4404185
Annaházi A., Róka R., Rosztóczy A., Wittmann T. (2014). Role of antispasmodics in the treatment of irritable bowel syndrome. World J. Gastroenterol. 20, 6031–6043. doi:10.3748/wjg.v20.i20.6031
Brenner D. M., Fogel R., Dorn S. D., Krause R., Eng P., Kirshoff R., et al. (2018). Efficacy, safety, and tolerability of plecanatide in patients with irritable bowel syndrome with constipation: Results of two phase 3 randomized clinical trials. Am. J. Gastroenterol. 113, 735–745. doi:10.1038/s41395-018-0026-7
Buselli R., Veltri A., Corsi M., Marino R., Necciari G., Baldanzi S., et al. (2021). Irritable Bowel Syndrome prevalence and work ability in a sample of healthcare workers exposed to occupational stress. J. Psychosom. Res. 148, 110566. doi:10.1016/j.jpsychores.2021.110566
Camilleri M. (2018). Management options for irritable bowel syndrome. Mayo Clin. Proc. 93, 1858–1872. doi:10.1016/j.mayocp.2018.04.032
Chey W. D., Kurlander J., Eswaran S. (2015). Irritable bowel syndrome: A clinical review. JAMA 313, 949–958. doi:10.1001/jama.2015.0954
Drossman D. A., Hasler W. L. (2016). Rome IV-functional GI disorders: Disorders of gut-brain interaction. Gastroenterology 150, 1257–1261. doi:10.1053/j.gastro.2016.03.035
Everhart J. E., Ruhl C. E. (2009). Burden of digestive diseases in the United States part II: Lower gastrointestinal diseases. Gastroenterology 136, 741–754. doi:10.1053/j.gastro.2009.01.015
Fadgyas Stanculete M., Dumitrascu D. L., Drossman D. (2021). Neuromodulators in the brain-gut Axis: Their role in the therapy of the irritable bowel syndrome. J. Gastrointestin. Liver Dis. 30, 517–525. doi:10.15403/jgld-4090
Ford A. C., Sperber A. D., Corsetti M., Camilleri M. (2020). Irritable bowel syndrome. Lancet 396, 1675–1688. doi:10.1016/S0140-6736(20)31548-8
Frändemark Å., Törnblom H., Jakobsson S., Simrén M. (2018). Work productivity and activity impairment in irritable bowel syndrome (IBS): A multifaceted problem. Am. J. Gastroenterol. 113, 1540–1549. doi:10.1038/s41395-018-0262-x
Galica A. N., Galica R., Dumitrașcu D. L. (2022). Diet, fibers, and probiotics for irritable bowel syndrome. J. Med. Life 15, 174–179. doi:10.25122/jml-2022-0028
Guo J., Chen L., Wang Y. H., Song Y. F., Zhao Z. H., Zhao T. T., et al. (2022). Electroacupuncture attenuates post-inflammatory IBS-associated visceral and somatic hypersensitivity and correlates with the regulatory mechanism of epac1-piezo2 Axis. Front. Endocrinol. 13, 918652. doi:10.3389/fendo.2022.918652
Jones J., Lembo A., Heidelbaugh J., Kuritzky L., Lacy B. (2021). Management of irritable bowel syndrome with diarrhea: Focus on eluxadoline. Curr. Med. Res. Opin. 37, 567–578. doi:10.1080/03007995.2021.1888705
Kaptchuk T. J., Kelley J. M., Conboy L. A., Davis R. B., Kerr C. E., Jacobson E. E., et al. (2008). Components of placebo effect: Randomised controlled trial in patients with irritable bowel syndrome. BMJ 336, 999–1003. doi:10.1136/bmj.39524.439618.25
Krahn U., Binder H., König J. (2013). A graphical tool for locating inconsistency in network meta-analyses. BMC Med. Res. Methodol. 13, 35. doi:10.1186/1471-2288-13-35
Li H., Pei L. X., Zhou J. L. (2012). Comparative observation on therapeutic effects between acupuncture and Western medication for diarrhea-predominant irritable bowel syndrome. Zhongguo Zhen Jiu 32, 679–682.
Li J., Zhu W., Liu W., Wu Y., Wu B. (2016). Rifaximin for irritable bowel syndrome: A meta-analysis of randomized placebo-controlled trials. Med. Baltim. 95, e2534. doi:10.1097/MD.0000000000002534
Lowe C., Aiken A., Day A. G., Depew W., Vanner S. J. (2017). Sham acupuncture is as efficacious as true acupuncture for the treatment of IBS: A randomized placebo controlled trial. Neurogastroenterol. Motil. 29, e13040. doi:10.1111/nmo.13040
Ma X. P., Hong J., An C. P., Zhang D., Huang Y., Wu H. G., et al. (2014). Acupuncture-moxibustion in treating irritable bowel syndrome: How does it work? World J. Gastroenterol. 20, 6044–6054. doi:10.3748/wjg.v20.i20.6044
Mak A. D. P., Chung V. C. H., Yuen S. Y., Tse Y. K., Wong S. Y. S., Ju Y., et al. (2019). Noneffectiveness of electroacupuncture for comorbid generalized anxiety disorder and irritable bowel syndrome. J. Gastroenterol. Hepatol. 34, 1736–1742. doi:10.1111/jgh.14667
Manheimer E., Cheng K., Wieland L. S., Min L. S., Shen X., Berman B. M., et al. (2012a). Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2012, CD005111. doi:10.1002/14651858.CD005111.pub3
Manheimer E., Wieland L. S., Cheng K., Li S. M., Shen X., Berman B. M., et al. (2012b). Acupuncture for irritable bowel syndrome: Systematic review and meta-analysis. Am. J. Gastroenterol. 107, 835–847. quiz 848. doi:10.1038/ajg.2012.66
Martínez-Vázquez M. A., Vázquez-Elizondo G., González-González J. A., Gutiérrez-Udave R., Maldonado-Garza H. J., Bosques-Padilla F. J. (2012). Effect of antispasmodic agents, alone or in combination, in the treatment of irritable bowel syndrome: Systematic review and meta-analysis. Rev. Gastroenterol. Mex. 77, 82–90. doi:10.1016/j.rgmx.2012.04.002
Mills E. J., Thorlund K., Ioannidis J. P. A. (2013). Demystifying trial networks and network meta-analysis. BMJ 346, f2914. doi:10.1136/bmj.f2914
Moayyedi P., Andrews C. N., MacQueen G., Korownyk C., Marsiglio M., Graff L., et al. (2019). Canadian association of gastroenterology clinical practice guideline for the management of irritable bowel syndrome (IBS). J. Can. Assoc. Gastroenterol. 2, 6–29. doi:10.1093/jcag/gwy071
Pei L., Geng H., Guo J., Yang G., Wang L., Shen R., et al. (2020). Effect of acupuncture in patients with irritable bowel syndrome: A randomized controlled trial. Mayo Clin. Proc. 95, 1671–1683. doi:10.1016/j.mayocp.2020.01.042
Qi L. Y., Li H. P., Yang N. N., Li Y. J., Tan C. X., Yang J. W., et al. (2022). Research progress on mechanism of acupuncture and moxibustion in treatment of irritable bowel syndrome. Zhongguo Zhen Jiu 42, 231–236. doi:10.13703/j.0255-2930.20210131-0003
Quigley E. M. M., Fried M., Gwee K.-A., Khalif I., Hungin A. P. S., Lindberg G., et al. (2016). World gastroenterology organisation global guidelines irritable bowel syndrome: A global perspective update september 2015. J. Clin. Gastroenterol. 50, 704–713. doi:10.1097/MCG.0000000000000653
Rai R. R., Nijhawan S. (2021). Comparative evaluation of efficacy and safety of drotaverine versus mebeverine in irritable bowel syndrome: A randomized double-blind controlled study. Saudi J. Gastroenterol. 27, 136–143. doi:10.4103/sjg.SJG_266_20
Riley R. D., Jackson D., Salanti G., Burke D. L., Price M., Kirkham J., et al. (2017). Multivariate and network meta-analysis of multiple outcomes and multiple treatments: Rationale, concepts, and examples. BMJ 358, j3932. doi:10.1136/bmj.j3932
Rücker G. (2012). Network meta-analysis, electrical networks and graph theory. Res. Synth. Methods 3, 312–324. doi:10.1002/jrsm.1058
Rücker G., Schwarzer G. (2015). Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 15, 58. doi:10.1186/s12874-015-0060-8
Ruepert L., Quartero A. O., de Wit N. J., van der Heijden G. J., Rubin G., Muris J. W. (2011). Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2013, CD003460. doi:10.1002/14651858.CD003460.pub3
Shi G. X., Yang X. M., Liu C. Z., Wang L. P. (2012). Factors contributing to therapeutic effects evaluated in acupuncture clinical trials. Trials 13, 42. doi:10.1186/1745-6215-13-42
Sterne J. A. C., Savović J., Page M. J., Elbers R. G., Blencowe N. S., Boutron I., et al. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898. doi:10.1136/bmj.l4898
Wu H. G., Jiang B., Zhou E. H., Shi Z., Shi D. R., Cui Y. H., et al. (2008). Regulatory mechanism of electroacupuncture in irritable bowel syndrome: Preventing MC activation and decreasing SP VIP secretion. Dig. Dis. Sci. 53, 1644–1651. doi:10.1007/s10620-007-0062-4
Yaklai K., Pattanakuhar S., Chattipakorn N., Chattipakorn S. C. (2021). The role of acupuncture on the gut-brain-microbiota Axis in irritable bowel syndrome. Am. J. Chin. Med. 49, 285–314. doi:10.1142/S0192415X21500154
Zhao J. M., Chen L., Zhou C. L., Shi Y., Li Y. W., Shang H. X., et al. (2016). Comparison of electroacupuncture and moxibustion for relieving visceral hypersensitivity in rats with constipation-predominant irritable bowel syndrome. Evid. Based. Complement. Altern. Med. 2016, 9410505. doi:10.1155/2016/9410505
Keywords: acupuncture, antispasmodics, irritable bowel syndrome, treatment comparison, meta-analysis
Citation: Shi Y-z, Tao Q-f, Qin D, Chen M, Yu S-g and Zheng H (2022) Acupuncture vs. antispasmodics in the treatment of irritable bowel syndrome: An adjusted indirect treatment comparison meta-analysis. Front. Physiol. 13:1001978. doi: 10.3389/fphys.2022.1001978
Received: 24 July 2022; Accepted: 21 September 2022;
Published: 06 October 2022.
Edited by:
Hirokazu Fukui, Hyogo College of Medicine, JapanReviewed by:
Zipeng Gong, Guizhou Medical University, ChinaMaria Elena Flacco, University of Ferrara, Italy
Copyright © 2022 Shi, Tao, Qin, Chen, Yu and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Zheng, emhlbmdodWlAY2R1dGNtLmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Yun-zhou Shi
Yun-zhou Shi Qing-feng Tao
Qing-feng Tao Di Qin1
Di Qin1 Min Chen
Min Chen Hui Zheng
Hui Zheng