
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Physiol., 17 December 2021
Sec. Exercise Physiology
Volume 12 - 2021 | https://doi.org/10.3389/fphys.2021.782167
This article is part of the Research TopicMethods and Applications in Exercise PhysiologyView all 9 articles
Introduction: The ventilatory threshold (named as VT1) and the respiratory compensation point (named as VT2) describe prominent changes of metabolic demand and exercise intensity domains during an incremental exercise test.
Methods: A novel computerized method based on the optimization method was developed for automatically determining VT1 and VT2 from expired air during a progressive maximal exercise test. A total of 109 peak cycle tests were performed by members of the US astronaut corps (74 males and 35 females). We compared the automatically determined VT1 and VT2 values against the visual subjective and independent analyses of three trained evaluators. We also characterized VT1 and VT2 and the respective absolute and relative work rates and distinguished differences between sexes.
Results: The automated compared to the visual subjective values were analyzed for differences with t test, for agreement with Bland–Altman plots, and for equivalence with a two one-sided test approach. The results showed that the automated and visual subjective methods were statistically equivalent, and the proposed approach reliably determined VT1 and VT2 values. Females had lower absolute O2 uptake, work rate, and ventilation, and relative O2 uptake at VT1 and VT2 compared to men (p ≤ 0.04). VT1 and VT2 occurred at a greater relative percentage of their peak VO2 for females (67 and 88%) compared to males (55 and 74%; main effect for sex: p < 0.001). Overall, VT1 occurred at 58% of peak VO2, and VT2 occurred at 79% of peak VO2 (p < 0.0001).
Conclusion: Improvements in determining of VT1 and VT2 by automated analysis are time efficient, valid, and comparable to subjective visual analysis and may provide valuable information in research and clinical practice as well as identifying exercise intensity domains of crewmembers in space.
Examining the ventilatory profile during incremental exercise to a maximum effort has been used to assess aerobic fitness and monitor and prescribe exercise training in athletes and clinical populations with decades of controversy (Yeh et al., 1983; Poole et al., 2021). Noninvasive measurements of the ventilatory profile are represented commonly as two inflection points: the ventilatory threshold (named as VT1 in this paper) and the respiratory compensation point (named as VT2 in this paper; Whipp et al., 1989; Cannon et al., 2009; Pallarés et al., 2016; Carriere et al., 2019; Galán-Rioja et al., 2020). Determining VT1 and VT2 during an incremental exercise test should be accompanied by a set of universally agreed upon and explicitly defined quality-control criteria (Meyer et al., 1996; Gaskill et al., 2001; Poole et al., 2016; Galán-Rioja et al., 2020). Several VT methods for detecting VT have traditionally been based on a subjective visual analysis, but this is time-consuming, requires 2–3 trained personnel with an independent reviewer and a strict set of criteria to maintain tight quality control (Caiozzo et al., 1982; Yeh et al., 1983; Gladden et al., 1985; Dickstein et al., 1990a; Shimizu et al., 1991).
VT1 is commonly described as the point at which pulmonary ventilation and carbon dioxide (CO2) output begin to increase exponentially (Whipp et al., 1989; Dennis et al., 1992). The ventilatory equivalent method has been used to identify VT1, which is best described as the intensity of activity that causes the first rise in the ventilatory equivalent of oxygen (O2) without a concurrent rise in the ventilatory equivalent of CO2 (Reinhard et al., 1979; Powers et al., 1984). Determining VT1 using the excess CO2 (ExCO2) method requires the intensity of exercise that causes an increase from steady state to an excess production of CO2 (Volkov et al., 1975). Likewise, the V-slope method, also commonly used method, uses points that show an increase in the slope from less than 1 to greater than 1 in the CO2 production (VCO2) by O2 consumption (VO2) data (Dickstein et al., 1990a; Ekkekakis et al., 2008) and in the minute ventilation (VE) by VCO2 data (Beaver et al., 1986) for locating VT1 and VT2, respectively. All computerized methods mentioned require finding the point where the slope changes markedly over the entire scattergram. However, two regression lines skim the slope of data points from left to right and stop as soon as its criterion is satisfied; thus, the algorithm for searching VT1 might estimate lower VO2 compared with the other methods depending on the amount of noise in the data (Ekkekakis et al., 2008). For the severe exercise intensity domain, VT2 is considered the second break point at which the partial pressure of arterial CO2 starts to decline during heavy exercise (Beaver et al., 1986; Nattie and Li, 2012). The 2-line regression model for detecting the slope change in the scattergram also has been used to find VT2 associated with VE and VCO2 (Volkov et al., 1975; Reinhard et al., 1979; Davis et al., 1980; Powers et al., 1984; Brooks, 1985; Beaver et al., 1986). However, a disadvantage, inherent to methods that use regression analysis during maximal exercise, is the possibility that the hyperventilation phase (VT2 starting point) may be partially included in the calculation (Dickstein et al., 1990b).
Exercise countermeasures are the only known way for maintaining muscle mass, strength, and cardiorespiratory fitness in crewmembers during spaceflight. It is important for exercise prescriptions to be optimized to maintain astronauts’ fitness to avoid premature physical and cognitive fatigue during performance of high-risk, mission-critical tasks. Additionally, more women are now flying into space, yet few studies about sex-specific physiologic differences in the astronaut population have been explored during and after spaceflight. A reliable and automated detection of VT1 and VT2 for prescribing exercise domains can help to quickly identify and guide individualized exercise prescriptions for the purpose of maintaining and enhancing crewmembers’ performance of submaximal extravehicular activities (EVAs) over long durations. We believe that determining both VT1 and VT2 using the proposed novel automated method and their associated absolute and relative work rates can provide valuable information regarding crewmembers’ ability to exercise (e.g., buffering capacity, lactate kinetics) on the International Space Station (ISS) and to perform EVAs and lunar exploration. Understanding where VT1 and VT2 occur can assist in prescribing exercise intensity above or below those points. Therefore, in this study, we determined the accuracy of our novel automated analysis by comparing the computerized results with subjective visual identification. We also aimed to characterize absolute and relative work rates at VT1 and VT2 and to identify if there are any differences in those values between female and male crewmembers.
This study protocol was reviewed and approved by the NASA Johnson Space Center (JSC)‘s Institutional Review Board and in agreement with the Declaration of Helsinki. All participants in the study provided signatures confirming their informed consent. Data were collected from 2013 to 2019. Astronaut participants in these data were active astronauts in flight training at JSC. Exact training status, e.g., amount of time spent in physically training, is not known. A total of 109 peak cycle tests were obtained from a large astronaut database (74 males and 35 females) and used to examine the ventilatory thresholds at VT1 and VT2. The data set was separated into groups of female and males for the sex difference study (Pescatello et al., 2014). See Table 1 for mean participant characteristics and statistical significances for the overall and sex differences.
Cardiorespiratory fitness (peak VO2) was determined by a progressive, incremental graded cycle ergometer stress test to volitional exhaustion. Our graded exercise protocol was developed to measure peak VO2 and VT at JSC. The protocol has two versions; a nominal protocol and a light protocol conducted on the LODE Excalibur sport cycle ergometer (Lode BV, Groningen, Netherlands). The nominal protocol consisted of a cycling warm-up at 50 W for 3 min followed by stepwise increases of 25 W every minute until test termination. The light protocol consists of the same timed wattage increases (i.e., 3 min warm-up then 1-min increases), but the wattage starts at 45 W and with 15 W increases. Participants were assigned the nominal or light protocol based on body weight. Participants were assigned the light protocol if they weighed less than 65 kilograms. Eight participants fell in this category. We observed that aerobic response was sufficiently fast to adjust to the 15 or 25 W workload increases within the 1-min stage time.
Participants were instructed to maintain a cadence of 75 revolutions per minute (RPM) throughout testing. Respiratory gases were sampled per 10-s interval and analyzed using the ParvoMedics TrueOne® 2400 metabolic cart. After a 30-min warm-up, O2 and CO2 gas were calibrated using known gases (16% O2, 4% CO2) and air flow was calibrated with a 3-L syringe. To ensure accuracy of indirect calorimetry, gas and flow calibration was conducted prior to every exercise test and consisted of ambient and standard gas calibration along with flow meter calibration. Calibration was accepted if new calibration parameters were within +/− 3% of previous values. Additionally, maintenance procedures were followed in accordance with manufacturer guidelines. The rating of perceived exertion (RPE; Borg scale 6–20) was measured every 2–3 min during the exercise test. Heart rate (HR) was determined from 12-lead electrocardiogram recordings throughout the test (CardioSoft CASE®, GE Healthcare, WI, United States). The test was considered to be maximal when at least 4 of 5 following criteria were met: (1) a respiratory exchange ratio (RER) of ≥1.10, (2) a plateau in VO2 with increasing workloads, (3) workload volitional fatigue (a fall of 10 RPM), (4) exercise peak HR that was within 10 beats of the age-predicted maximal HR [207–(0.67 × age)] (Gellish et al., 2007), and (5) RPE at or greater than 19. All participants reached at least 4 of the listed criteria.
In summary, exercise variables in this study were work rates (W), %Wmax (%), HR (beat/min), RER (VO2:VCO2), and VE (L/min) at the ventilatory thresholds (VT1 and VT2) and peak VO2 in absolute (L/min) and relative to body weight (ml/kg/min) expressions. The first 3 min of warm-up were excluded in data analysis.
Detection of abrupt change in data distribution has been considered as one of the important practical problems arising in various applications (Riedel, 1994). In this study, we used a parametric global optimization method (Lavielle, 2005), which was implemented as a MATLAB function, named findchangepts (MATLAB® R2020a, The MathWorks, Inc., Natick, MA, United States). Though the parametric global optimization method identifies a data point change most significantly over the entire scattergram, it could be common during the determination of thresholds to find that some data are indeterminate and inter-method differences are unavoidable in nature (Gaskill et al., 2001). To provide a valid and reliable process, Gaskill et al. (2001) recommended to average the combined multiple methods used to identify ventilatory threshold (Gaskill et al., 2001). Thus, we identified VT1 using the mean of ExCO2 and V-slope (Figure 1A) and detected VT2 using the mean of the excess minute ventilation (ExVE) method (Kim et al., 2020) and V-slope (Figure 1B). Figure 1C shows the combined VT1 and VT2 corresponded to gas exchange data: VE/VO2, ventilatory equivalent for O2 (blue dots); VE/VCO2, ventilatory equivalent for CO2 (red dots); PETO2, end-tidal pressure of O2 (green dots); end-tidal pressure of CO2, PETCO2 (pink dots). Finally, we identified the work rate associated with VT1 and VT2 and compared absolute and relative sex difference.
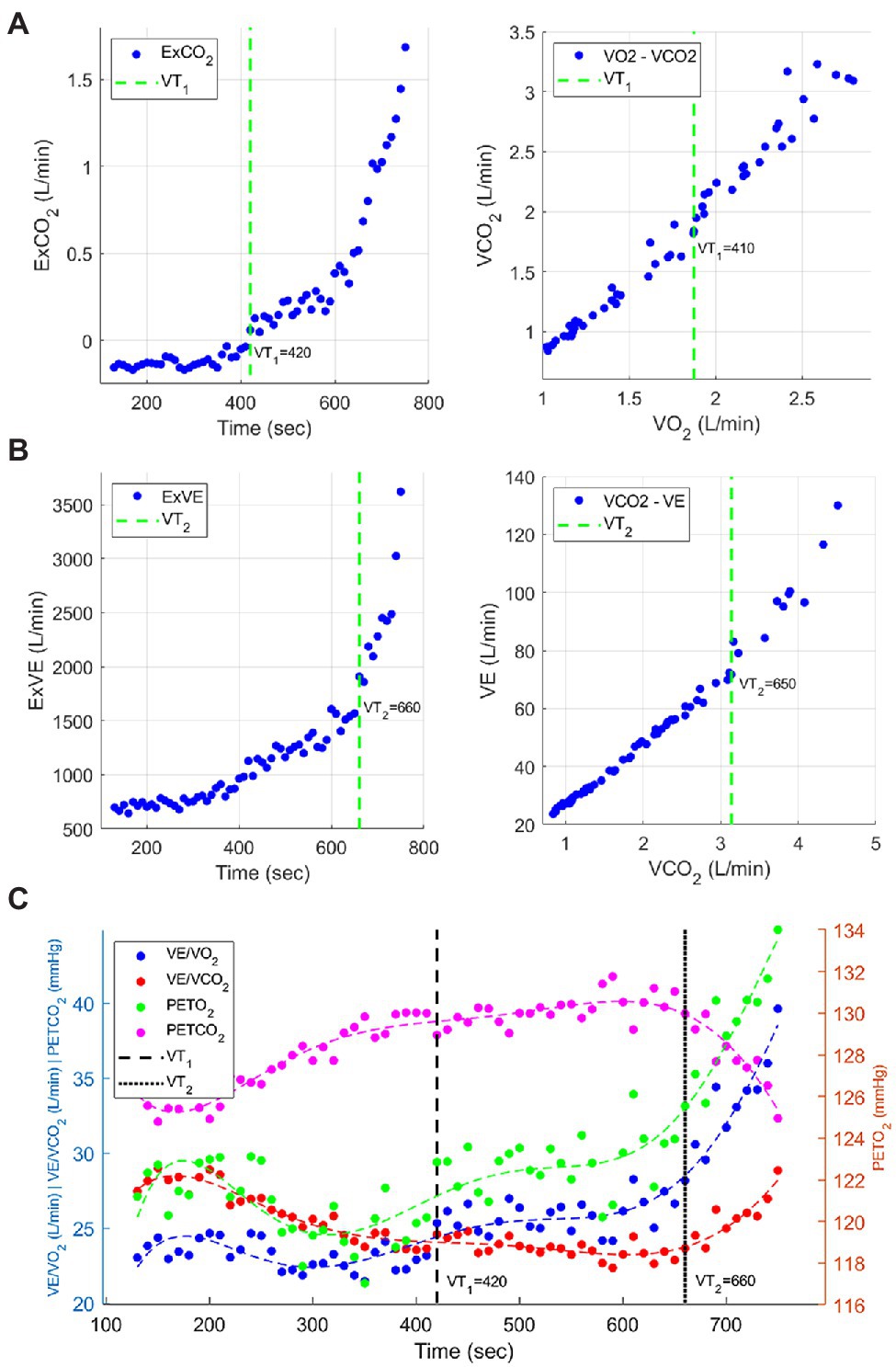
Figure 1. Example of determination of VT1 and VT2. (A) left: ExCO2, right: V-slope for VT1. (B) left: ExVE, right: V-slope for VT2. (C) The combined VT1 and VT2 corresponded to gas exchange data: VE/VO2, ventilatory equivalent for O2 (blue dots); VE/VCO2, ventilatory equivalent for CO2 (red dots); PETO2, end-tidal pressure of O2 (green dots); end-tidal pressure of CO2, PETCO2 (pink dots).
The ExVE is the method we proposed to identify the intensity of exercise that caused an increase from steady state to excess VE (Kim et al., 2020). Anaerobic exercise triggers a cascade of metabolic reactions in the human body (Beaver et al., 1986). At high intensity of exercise, the high-energy demand triggers a breakdown of glucose and a reduction of pyruvate. These metabolic processes produce lactate faster than the body can metabolize it. Bicarbonate buffers hydrogen H+ as a countermeasure when lactate flux increases faster than removal. As exercise intensity increases above this point, VCO2 increases and systemic pH in the bloodstream decreases as the H+ from the bicarbonate is not sufficiently buffered (Myers and Ashley, 1997). This decrease in blood pH triggers carotid bodies, chemoreceptor cells located in the carotid artery, to further increase VE. Therefore, VT2 can be determined as the point in time where VE increases to compensate for VCO2 being greater than VO2, while end-tidal CO2 levels are reduced (Pallarés et al., 2016). We reformulated the typical ExCO2 concept [(e.g.,VCO22/VO2)−VCO2)] (Volkov et al., 1975; Gaskill et al., 2001) to the ExVE form such as (VE2/VCO2)−VE.
Figure 2 shows the code of the procedure how we generated the input data, how we applied the findchangepks function to detect each changepoint location, and how we finally determined VT1 and VT2. For example, we specified “Statistic” as “std” because the “std” option detects a significant change that occurs while the standard deviation of input data distribution increases after ventilatory thresholds. Also, we specified “MaxNumChanges” as “1” to return the index of the most significant change point in the scattergrams (see green dashed lines in Figures 1A,B). The algorithm for searching might be more robust and less influenced by unexpected peak noise at the initial or end time range. It has been reported that VT1 and VT2 commonly lie at exercise intensities between 50 and 65% of VO2 and between 75 and 87% of VO2, respectively (Beaver et al., 1986; Pallarés et al., 2016; Cerezuela-Espejo et al., 2018; Galán-Rioja et al., 2020). Thus, it is recommended to use a specific range of the input signals only, for example, trimming half of the signal length (i.e., from 30th percentile to 80th percentile for VT1, from 50th percentile to 100th percentile for VT2).
For the validation study, three trained evaluators independently and randomly evaluated the graphs of the data to determine VT1 and VT2 values. For each determination, graphs were visually evaluated for the assessment of change in data distribution. Specifically, for VT1, evaluators assessed the intensity of activity that causes the first sustained rise in the VE/VO2 without a concurrent rise in the ventilatory VE/VCO2 (Figure 3A). The rise in VE/VO2 is in concurrence with RER reaching 1.0. For VT2, evaluators assessed increase in both the VE/VO2 and VE/VCO2 (Figure 3B). This rise in VE/VO2 and VE/VCO2 is in concurrence with a decrease in PetCO2 (5). A detailed protocol to maintain tight quality control over determination of VT1 and VT2 values was developed and included the following rules: (1) if, after concurrently viewing all graphs, an evaluator still thought that the VT value was indeterminate, then data for that subject were rejected. If the evaluators thought that data were usable, they then chose what they thought to be the most representative value. (2) The values determined by the three independent investigators were then compared by a fourth independent investigator. If the values determined by the evaluators were within 1 exercise stage (50 W or less than 15%), then values for the 3 investigators were averaged. (3) If values were within 15% of either of the initial investigators, then the VT values were averaged. Comparison values greater than 15% were removed from the analysis. (4) The appearance time of VT needed to be after the 75 W (after 4 min) warm-up of the exercise test or the data were rejected and were considered to be indeterminate. The data reported for the visual identification method include only those participants whose data met all the criteria. Evaluators rejected 57 for VT1 and 28 for VT2 based on our criteria. For the accurate comparison between the visual analysis and the automated analysis, we only used the paired matches.
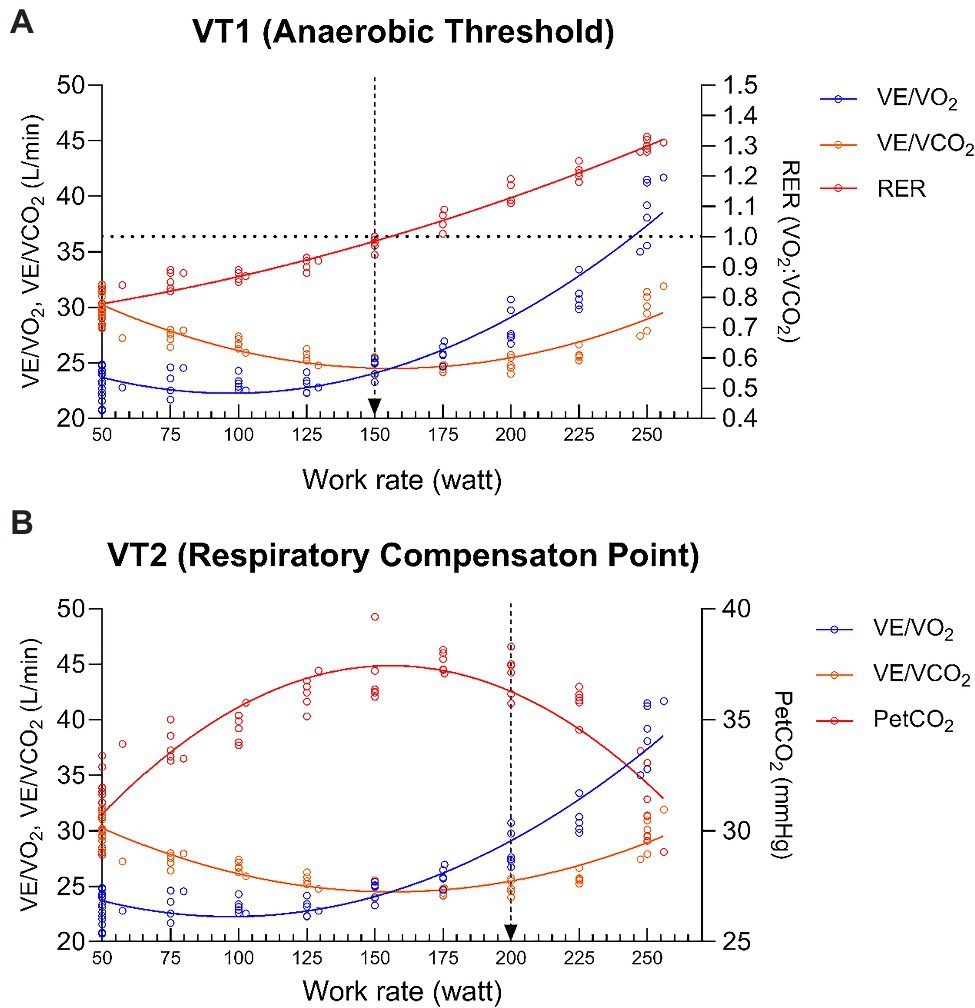
Figure 3. Visual determination of VT1 (A) and VT2 (B). The arrows designate the choice of VT1 and VT2 in these sample graphs from one subject.
Independent t tests were used when examining subject characteristics and sex comparison of exercise variables for VO2, W, HR, RER, and VE values at VT1 and VT2.
The mean differences of the subjective analysis and the automated analysis were examined using independent t test to test for differences between measures. The Bland–Altman analysis (Giavarina, 2015) assessed the limits of agreement between VT1 and VT2. Formal equivalence testing was conducted with the TOST approach with predefined equivalence bounds of ±25 (Schuirmann, 1987). The data were also analyzed by the intraclass correlation coefficients (ICC) to examine the relationships between the subjective analysis and the automated analysis.
For each subject, absolute VO2, relative VO2, W, HR, RER, and VE were determined at VT1 (average of V-slope for VT1 and ExCO2 methods), VT2 (average of V-slope for VT2 and ExVE methods), and peak, a 2-way factorial ANOVA was then used to examine main effects and interactions (VT × Group) for the sex difference study. If significance was found, the appropriate Holm-Sidak multiple comparison post hoc test was performed.
Data were analyzed and figures generated using MATLAB R2020a (The MathWorks, Inc., Natick, MA, United States) and GraphPad Prism (version 8.4.3, La Jolla, CA, United States) with statistical significance set at p < 0.05. Equivalence testing was conducted with the TOSTER package in the R statistical software (R: A Language and Environment for Statistical Computing, R Core Team, R Foundation for Statistical Computing, Vienna Austria, 2019).1 All data are reported as mean ± SD.
Males and females were matched for age but different for mass and height (Table 1). Mean exercise variables for the overall subjects and sex difference are reported in Table 2. At peak, VT1, and VT2, females had lower absolute O2 uptake, W, and ventilation and relative O2 uptake compared to men (p ≤ 0.04). HRs and RERs were not different at peak exercise for either group. However, HRs and RERs were lower in the male group compared to the female group at VT1 and VT2 (p ≤ 0.02).
Exercise intensities at VT1 and VT2 relative to peak VO2 and peak W for the combined analysis in all subjects and sex differences are reported in Figure 4. In the combined analysis, VT1 occurred at 58% of peak VO2 and VT2 occurred at 79% of peak VO2 (p < 0.0001). Work rates at VT1 and VT2 were 50 and 69% of peak W (p < 0.0001). For the sex difference comparison, VT1 and VT2 occurred at a greater relative percentage of their peak VO2 for females (67 and 88%) compared to males (55 and 74%), main effect for group; p < 0.001. However, no differences were found for group expressed as a relative percentage of peak W. Both sexes had VT1 at 50% and VT2 at 70% of peak W (p ≥ 0.40).
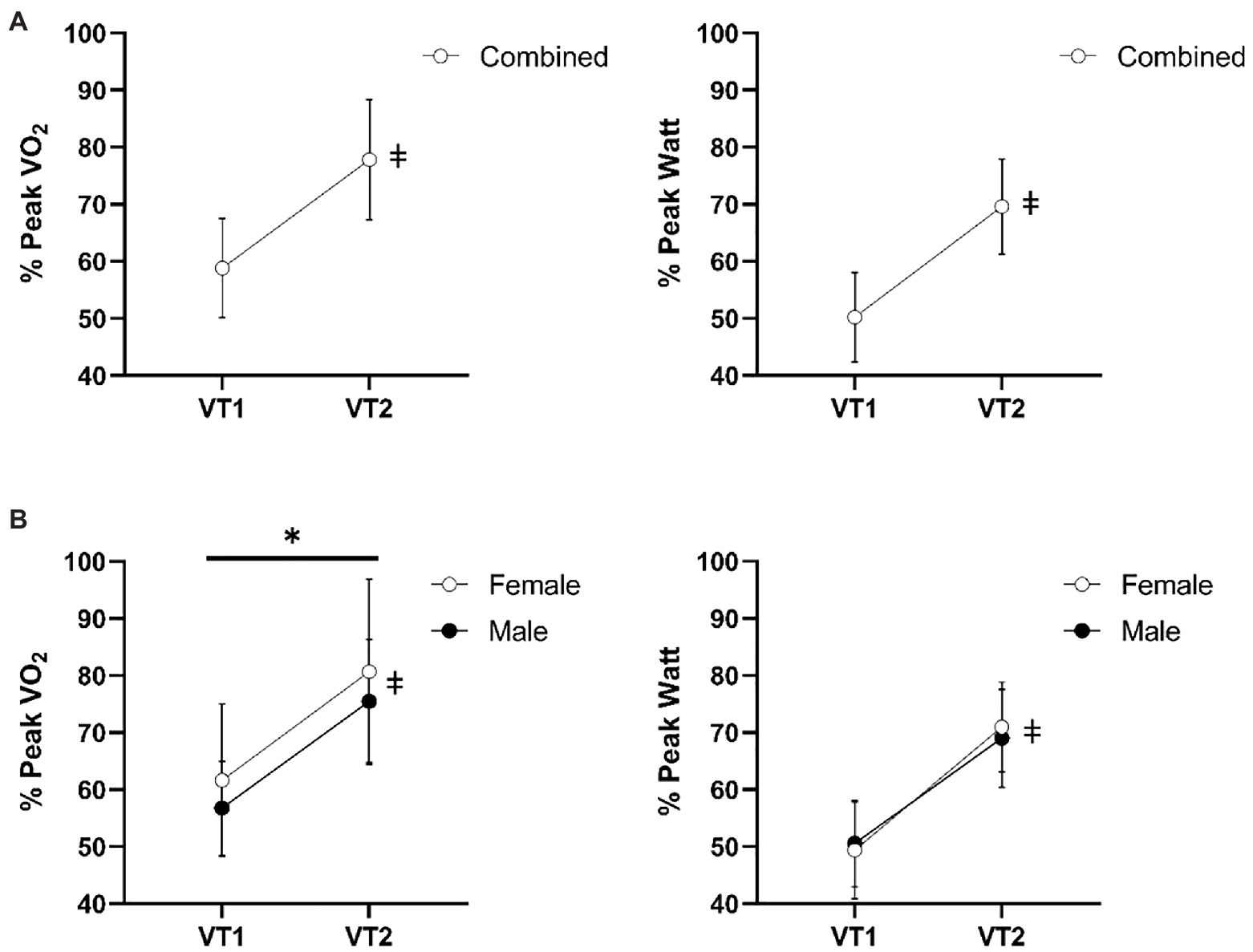
Figure 4. Exercise intensities at VT1 and VT2 relative to peak VO2 and peak W for the combined analysis (A) and sex differences (B). *Indicates group main effect differences P < 0.001. ǂ indicates significant main effect difference between VT1 and VT2 p < 0.0001. Data reported as means ± SD.
Independent t tests for the comparison between the subjective analysis and the automated analysis found no difference for VT1 (p > 0.05) and VT2 (p > 0.05). Figure 5 illustrates the Bland–Altman plot. Bias for VT1 was 7.08 ± 12.2 W with the 95% Limits of Agreement from −16.99 to 31.06 W. Bias for VT2 was −2.2 ± 12.7 W with the 95% Limits of Agreement from −27.0 to 22.7 W. For VT1 and VT2 combined, the equivalence test was significant, t(132) = −9.389, p < 0.0001, given equivalence bounds of −25 and 25 (on a raw scale) and an alpha of 0.05. For VT1 and VT2 individually, the equivalence tests also were significant, t(51) = −4.513, p < 0.0001 and t(80) = 5.812, p < 0.0001, respectively, given equivalence bounds of −25 and 25 (on a raw scale) and an alpha of 0.05. Equivalence testing showed that the automated and visual measures were statistically equivalent (p < 0.0001) in all ways, each VT1 or VT2 and combined. Finally, a high degree of reliability was found between the subjective analysis and the automated analysis. The ICC between the subjective analysis and the automated analysis were 0.821 for VT1 and 0.830 for VT2 with a 95% confidence interval.
The advantages of a computerized method include faster, objective, and automated data analysis as well as improvements in reproducibility and repeatability. The aim of this study was to provide a novel, reliable, and computerized method for automatically identifying VT1 and VT2. We demonstrated that our method was able to determine ventilatory thresholds comparable to the visual analysis accomplished by 3 trained evaluators. We also determined the associated work rates expressed as absolute and relative submaximal VO2 and W and reported that sex differences exist for VT1 and VT2.
Others have compared various computerized methods for determining VT1 and demonstrated that regression-based methods provide considerably different results (Ekkekakis et al., 2008). For example, VT1 values detected by using 2 regression lines were significantly lower with weaker correlations compared to other computerized methods. Additionally, Pearson correlation coefficients in VO2 (L/min) between ExCO2 and V-slope for VT1 were 0.517 and 0.526 (i.e., a moderate positive relationship) in each sample group. In this study, Pearson correlation coefficient in VO2 (L/min) detected by ExCO2 and V-slope for VT1 using the parametric global optimization method was 0.81 (i.e., a strong positive linear relationship), which is a stronger correlation coefficient compared to using 2 regression lines (Ekkekakis et al., 2008). We also found that the strong positive relationship for Pearson correlation coefficient between computerized methods for determining VT2 (ExVE and V-slope for VT2) between ExVE and V-slope for VT2 means that the parametric global optimization method. In support of these, we found no difference between the subjective visual method by 3 trained evaluators and our automated method. Our novel and automated protocol may increase the methodological consistency in both research and clinical practice.
It has been reported that maximal aerobic capacity is associated with VT1 (59 to 65%) and VT2 (84 to 87%) and that maximal lactate steady state corresponds to VT2 (Pallarés et al., 2016; Cerezuela-Espejo et al., 2018). We found that when comparing to peak work rate, VT1 and VT2 were associated with 50 and 70% of peak W, respectively. These differences may be because of age and fitness of our study participants’ steady state vs. progressive exercise test. When we examined the ventilatory points in relation to peak VO2, the female group had greater relative VO2 associated with VT1 (67%) and VT2 (88%). Beaver et al. (1986) reported that VT1 occurred at 55% of peak VO2 and VT2 occurred at 75% of peak VO2 (Beaver et al., 1986) and a recent meta-analysis reported that VT1 occurs at 50 to 60% of peak VO2 (Galán-Rioja et al., 2020). These values are similar to ours as we report the whole sample was at 58 and 79% of peakVO2 for VT1 and VT2, respectively. As noted earlier, these differences in VT2 for the female group may be because of sensitivity of the carotid body ventilatory drive caused by body temperature, blood osmolarity, pH, K+, H+ buffering by bicarbonate, and the change in partial pressure of O2 (Galán-Rioja et al., 2020).
It has been reported that microgravity affects females and males differently (Mark et al., 2014). It is important to better understand these sex differences as the female representation in the astronaut corps is increasing, meaning more women will be eligible to fly in space than ever before. Under the microgravity environment, one of the sex-specific differences in exercise response is orthostatic intolerance caused by plasma volume loss and cardiovascular adjustments (Goel et al., 2014). Females generally have smaller body size, lower absolute, and relative aerobic fitness and are weaker in upper and lower body strength, which have implications for risk of fatigue and injury from muscle strains during EVA and emergency egress (Harm et al., 2001). Thus, understanding exercise countermeasures and the adaptations between sexes is of high relevance for the astronaut population. Our data are similar to others that report sex differences in gas exchange threshold for VT1. In this study, we also showed that VT2 differences occurred between males and females. This may be because of differences in breathing adjustments to chemosensitivity, thermoregulation, and menstrual cycle hormones (Beaver et al., 1986; Kilbride et al., 2003; Hayashi et al., 2012).
Others have suggested using exercise work rates above and below the ventilatory breakpoints for VT1 and VT2 for the prescription of exercise training to define exercise domains such as moderate, heavy-and severe exercise intensity domains (Beaver et al., 1986; Nattie and Li, 2012). This gives an individualized approach to prescribe exercise specific to the metabolic demands. Previous exercise training countermeasures during spaceflight or analogues have used a relative percentage of peak VO2 (e.g., continuous cycle exercise for 30 min at 75% of peak VO2 and interval treadmill sessions of 30 s to 4 min at nearly maximal intensity; Moore Jr et al., 2014; Ploutz-Snyder et al., 2018). However, the responses to these exercise prescriptions still have high variability for maintaining fitness. For example, Moore et al. reported that astronauts who have higher initial aerobic capacities are more prone to loss of cardiorespiratory fitness; however, the reason is unknown and may be because of the frequency, intensity, time, and progression of the exercise prescription (Moore et al., 2014). Our data suggest that sex should be considered when prescribing exercise countermeasures and the prescriptions could be further individualized by prescribing based on VT1, VT2, and peak VO2.
Notably, we acknowledge a limitation with our study. This includes not obtaining arterial lactate samples and blood gasses to confirm the metabolic and ventilation breakpoints. Further validation should include these measurements.
In summary, the new automated method has been shown to identify inflection points in each of the variables used to reliably determine VT1 and VT2. Furthermore, we show that sex influences the VT1 and VT2 in members of the US astronaut corps. Detection of both VT1 and VT2 and their associated absolute and relative work rates may provide valuable information regarding crewmembers’ ability to exercise on the ISS and to perform EVAs and lunar exploration. Lastly, accurately tracking fitness pre-, in-, and post-flight is of importance for guidance on the efficacy of exercise training prescriptions as countermeasures.
The datasets presented in this article are not readily available because the study dataset are not publicly available due to privacy laws and other restrictions. Requests to access the datasets should be directed to KK, a3lvdW5namFlLmtpbUBuYXNhLmdvdg==.
The studies involving human participants were reviewed and approved by NASA Johnson Space Center. The patients/participants provided their written informed consent to participate in this study.
KK: conceptualization, methodology, software, data curation, writing – original draft, writing – review and editing, and visualization. ER: methodology, validation, formal analysis, data curation, writing – original draft, and writing – review and editing. BP and DF: validation and writing – review and editing. MY: validation, formal analysis, writing – original draft, and writing – review and editing. MD: investigation, resources, writing – review and editing, supervision, project administration, and funding acquisition. All authors contributed to the article and approved the submitted version.
This work was supported by the NASA Habitations System Account.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Beaver, W. L., Wasserman, K., and Whipp, B. J. (1986). A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 60, 2020–2027. doi: 10.1152/jappl.1986.60.6.2020
Brooks, G. A. (1985). Anaerobic threshold: review of the concept and directions for future research. Med. Sci. Sports Exerc. 17, 22–34.
Caiozzo, V. J., Davis, J. A., Ellis, J. F., Azus, J. L., Vandagriff, R., Prietto, C., et al. (1982). A comparison of gas exchange indices used to detect the anaerobic threshold. J. Appl. Physiol. 53, 1184–1189. doi: 10.1152/jappl.1982.53.5.1184
Cannon, D. T., Kolkhorst, F. W., and Buono, M. J. (2009). On the determination of ventilatory threshold and respiratory compensation point via respiratory frequency. Int. J. Sports Med. 30, 157–162. doi: 10.1055/s-0028-1104569
Carriere, C., Corrà, U., Piepoli, M., Bonomi, A., Merlo, M., Barbieri, S., et al. (2019). Anaerobic threshold and respiratory compensation point identification during cardiopulmonary exercise tests in chronic heart failure. Chest 156, 338–347. doi: 10.1016/j.chest.2019.03.013
Cerezuela-Espejo, V., Courel-Ibáñez, J., Morán-Navarro, R., Martínez-Cava, A., and Pallarés, J. G. (2018). The relationship between lactate and ventilatory thresholds in runners: validity and reliability of exercise test performance parameters. Front. Physiol. 9, 1–10. doi: 10.3389/fphys.2018.01320
Davis, J. A., Whipp, B. J., and Wasserman, K. (1980). The relation of ventilation to metabolic rate during moderate exercise in man. Eur. J. Appl. Physiol. Occup. Physiol. 44, 97–108. doi: 10.1007/BF00421087
Dennis, S. C., Noakes, T. D., and Bosch, A. N. (1992). Ventilation and blood lactate increase exponentially during incremental exercise. J. Sports Sci. 10, 437–449.
Dickstein, K., Barvik, S., Aarsland, T., Snapinn, S., and Karlsson, J. (1990a). A comparison of methodologies in detection of the anaerobic threshold. Circulation 81, 38–46.
Dickstein, K., Barvik, S., Aarsland, T., Snapinn, S., and Millerhagen, J. (1990b). Validation of a computerized technique for detection of the gas exchange anaerobic threshold in cardiac disease. Am. J. Cardiol. 66, 1363–1367.
Ekkekakis, P., Lind, E., Hall, E. E., and Petruzzello, S. J. (2008). Do regression-based computer algorithms for determining the ventilatory threshold agree? J. Sports Sci. 26, 967–976. doi: 10.1080/02640410801910269
Galán-Rioja, M. Á., González-Mohíno, F., Poole, D. C., and González-Ravé, J. M. (2020). Relative proximity of critical power and metabolic/Ventilatory thresholds: systematic review and meta-analysis. Sports Med., 1–13. doi: 10.1007/s40279-020-01314-8
Gaskill, S. E., Ruby, B. C., Walker, A. J., Sanchez, O. A., Serfass, R. C., and Leon, A. S. (2001). Validity and reliability of combining three methods to determine ventilatory threshold. Med. Sci. Sports Exerc. 33, 1841–1848. doi: 10.1097/00005768-200111000-00007
Gellish, R. L., Goslin, B. R., Olson, R. E., Mcdonald, A., Russi, G. D., and Moudgil, V. K. (2007). Longitudinal modeling of the relationship between age and maximal heart rate. Med. Sci. Sports Exerc. 39, 822–829. doi: 10.1097/mss.0b013e31803349c6
Giavarina, D. (2015). Understanding bland altman analysis. Biochem. Med. 25, 141–151. doi: 10.11613/BM.2015.015
Gladden, L. B., Yates, J., Stremel, R. W., and Stamford, B. A. (1985). Gas exchange and lactate anaerobic thresholds: inter and intraevaluator agreement. J. Appl. Physiol. 58, 2082–2089. doi: 10.1152/jappl.1985.58.6.2082
Goel, N., Bale, T. L., Epperson, C. N., Kornstein, S. G., Leon, G. R., Palinkas, L. A., et al. (2014). Effects of sex and gender on adaptation to space: behavioral health. J. Women's Health 23, 975–986. doi: 10.1089/jwh.2014.4911
Harm, D. L., Jennings, R. T., Meck, J. V., Powell, M. R., Putcha, L., Sams, C. P., et al. (2001). Invited review: gender issues related to spaceflight: a NASA perspective. J. Appl. Physiol. 91, 2374–2383. doi: 10.1152/jappl.2001.91.5.2374
Hayashi, K., Kawashima, T., and Suzuki, Y. (2012). Effect of menstrual cycle phase on the ventilatory response to rising body temperature during exercise. J. Appl. Physiol. 113, 237–245. doi: 10.1152/japplphysiol.01199.2011
Kilbride, E., Mcloughlin, P., Gallagher, C. G., and Harty, H. R. (2003). Do gender differences exist in the ventilatory response to progressive exercise in males and females of average fitness? Eur. J. Appl. Physiol. 89, 595–602. doi: 10.1007/s00421-003-0853-z
Kim, K. J., Buxton, R., Crowell, J., Downs, M., and Abercromby, A. (2020). An automated excess minute ventilation method to detect The respiratory compensation. Med. Sci. Sports Exerc. 52, 37–39. doi: 10.1249/01.mss.0000670404.13236.08
Lavielle, M. (2005). Using penalized contrasts for the change-point problem. Signal Process. 85, 1501–1510. doi: 10.1016/j.sigpro.2005.01.012
Mark, S., Scott, G. B., Donoviel, D. B., Leveton, L. B., Mahoney, E., Charles, J. B., et al. (2014). The impact of sex and gender on adaptation to space: executive summary. J. Women's Health 23, 941–947. doi: 10.1089/jwh.2014.4914
Meyer, K., Hajric, R., Westbrook, S., Samek, L., Lehmann, M., Schwaibold, M., et al. (1996). Ventilatory and lactate threshold determinations in healthy normals and cardiac patients: methodological problems. Eur. J. Appl. Physiol. Occup. Physiol. 72, 387–393. doi: 10.1007/BF00242266
Moore, A. D. Jr., Downs, M. E., Lee, S. M., Feiveson, A. H., Knudsen, P., and Ploutz-Snyder, L. (2014). Peak exercise oxygen uptake during and following long-duration spaceflight. J. Appl. Physiol. 117, 231–238. doi: 10.1152/japplphysiol.01251.2013
Myers, J., and Ashley, E. (1997). Dangerous curves: a perspective on exercise, lactate, and the anaerobic threshold. Chest 111, 787–795. doi: 10.1378/chest.111.3.787
Nattie, E., and Li, A. (2012). Central chemoreceptors: locations and functions. Compr. Physiol. 2, 221–254. doi: 10.1002/cphy.c100083
Pallarés, J. G., Morán-Navarro, R., Ortega, J. F., Fernández-Elías, V. E., and Mora-Rodriguez, R. (2016). Validity and reliability of ventilatory and blood lactate thresholds in well-trained cyclists. PLoS One 11, 1–16. doi: 10.1371/journal.pone.0163389
Pescatello, L. S., Riebe, D., and Thompson, P. D. (2014). ACSM’s Guidelines for Exercise Testing and Prescription. United States: Lippincott Williams and Wilkins.
Ploutz-Snyder, L. L., Downs, M., Goetchius, E., Crowell, B., English, K. L., Ploutz-Snyder, R., et al. (2018). Exercise training mitigates multisystem deconditioning during bed rest. Med. Sci. Sports Exerc. 50, 1920–1928. doi: 10.1249/MSS.0000000000001618
Poole, D. C., Burnley, M., Vanhatalo, A., Rossiter, H. B., and Jones, A. M. (2016). Critical power: an important fatigue threshold in exercise physiology. Med. Sci. Sports Exerc. 48, 2320–2334. doi: 10.1249/MSS.0000000000000939
Poole, D. C., Rossiter, H. B., Brooks, G. A., and Gladden, L. B. (2021). The anaerobic threshold: 50+ years of controversy. J. Physiol. 599, 737–767. doi: 10.1113/JP279963
Powers, S. K., Dodd, S., and Garner, R. (1984). Precision of ventilatory and gas exchange alterations as a predictor of the anaerobic threshold. Eur. J. Appl. Physiol. Occup. Physiol. 52, 173–177. doi: 10.1007/BF00433388
Reinhard, U., Müller, P., and Schmülling, R.-M. (1979). Determination of anaerobic threshold by the ventilation equivalent in normal individuals. Respiration 38, 36–42.
Riedel, K. S. (1994). Detection of Abrupt Changes: Theory and Application. United Kingdom: Taylor&Francis.
Schuirmann, D. J. (1987). A comparison of the two one-sided tests procedure and the power approach for assessing the equivalence of average bioavailability. J. Pharmacokinet. Biopharm. 15, 657–680. doi: 10.1007/BF01068419
Shimizu, M., Myers, J., Buchanan, N., Walsh, D., Kraemer, M., Mcauley, P., et al. (1991). The ventilatory threshold: method, protocol, and evaluator agreement. Am. Heart J. 122, 509–516. doi: 10.1016/0002-8703(91)91009-C
Volkov, N. I., Shirkovets, E. A., and Borilkevich, V. E. (1975). Assessment of aerobic and anaerobic capacity of athletes in treadmill running tests. Eur. J. Appl. Physiol. Occup. Physiol. 34, 121–130. doi: 10.1007/BF00999924
Whipp, B. J., Davis, J. A., and Wasserman, K. (1989). Ventilatory control of the isocapnic buffering region in rapidly-incremental exercise. Respir. Physiol. 76, 357–367. doi: 10.1016/0034-5687(89)90076-5
Keywords: incremental exercise, noninvasive measurement, ventilatory threshold, respiratory compensation point, automated determination
Citation: Kim KJ, Rivas E, Prejean B, Frisco D, Young M and Downs M (2021) Novel Computerized Method for Automated Determination of Ventilatory Threshold and Respiratory Compensation Point. Front. Physiol. 12:782167. doi: 10.3389/fphys.2021.782167
Received: 23 September 2021; Accepted: 18 November 2021;
Published: 17 December 2021.
Edited by:
Gary W. Mack, Brigham Young University, United StatesReviewed by:
Stephen Seiler, University of Agder, NorwayCopyright © 2021 Kim, Rivas, Prejean, Frisco, Young and Downs. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kyoung Jae Kim, a3lvdW5namFlLmtpbUBuYXNhLmdvdg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.