- 1The Graduate School, Beijing Sport University, Beijing, China
- 2The School of Sports Science, Beijing Sport University, Beijing, China
Purpose: Using meta-analysis to evaluate the effect of various long-term exercises (more than 4 weeks) on liver lipid metabolism of Chinese patients with non-alcoholic fatty liver disease (NAFLD) and provides more targeted exercise recommendations.
Methods: Four databases consisting of PubMed, Web of Science, China Science and Technology Journal Database (VIP), China Knowledge Resource Integrated Database (CNKI) were searched up to May 2021. Randomized controlled trials (RCTs) were eligible, and the outcomes of body composition, lipid metabolism [including triglyceride (TG), total cholesterol (TC), low-density lipoprotein-cholesterol (LDL-C), and high-density lipoprotein-cholesterol (HDL-C)], and liver function [including alanine aminotransferase (ALT) and aspartate aminotransferase (AST)] were used to assess the effectiveness of long-term exercise on Chinese patients with NAFLD.
Results: Eleven articles with a total of 13 data points (involving 1,006 participants) satisfied the inclusion criteria and were pooled in the meta-analysis. The findings demonstrated that long-term exercise decreased the level of TG [−0.50, 95%CI (−0.64, −0.36)], TC [−0.55, 95%CI (−0.92, −0.18)], LDL-C [−0.29, 95%CI (−0.43, −0.15)], ALT [−3.45, 95%CI (−6.78, −0.12)], AST [−6.91, 95%CI (−10.00, −3.81)], and body mass index (BMI) of patients who did exercise last more than 6 months [−1.55, 95%CI (−2.32, −0.79)] significantly. The effect on HDL-C was not obvious.
Conclusion: Long-term exercise can improve the levels of TG, TC, LDL-C, ALT, and AST in Chinese patients with NAFLD significantly, and exercise last more than 6 months can decrease the BMI of Chinese patients with NAFLD.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a metabolic-stress liver injury. Epidemiological studies showed that the worldwide prevalence of NAFLD is about 6.3%–45% (Younossi et al., 2016). With the escalating rates of obesity in China, the incidence of NAFLD is in the middle to the upper level (Younossi et al., 2016). Currently, NAFLD has become the principal cause of abnormal liver biochemical indicators in health checkups in China.
Metabolic disturbance of lipids is a hallmark of NAFLD, usually manifested as triglyceride (TG) accumulation in hepatocytes (Day and James, 1998, 2010), an increase of plasma TG, total cholesterol (TC), low-density lipoprotein-cholesterol (LDL-C), and decrease of high-density of lipoprotein-cholesterol (HDL-C) (DeFilippis et al., 2013; Peng et al., 2017), which may cause worse consequences, such as atherosclerosis or type 2 diabetes (Byrne and Targher, 2015). Therefore, improving the lipid metabolism of patients with NAFLD is essential for delaying their condition.
Until now, NAFLD lacks surgical options and pharmacological treatments with significant results. Thus, intervention for NAFLD using non-pharmacological means is becoming a hot topic. Exercise intervention as a considerable means of non-pharmacological intervention has shown to have a positive effect on NAFLD (Romero-Gomez et al., 2017; Farzanegi et al., 2019; Nath et al., 2020). Long-term exercise, defined as cumulative, structured, and planned, repetitive bouts of physical activity lasting ≥4 weeks (Caspersen et al., 1985; Wilmore et al., 2008), are more effective on lipid metabolism in patients with NAFLD than short-term exercise (Bilet et al., 2015), and although studies were chosen to analyze the effects of long-term exercise interventions on lipid metabolism in patients with NAFLD, the literature included in the existing meta-analysis is mainly in English, and its ethnic composition is significantly different from that in China, which makes the analysis of long-term exercise interventions in Chinese NAFLD patients not comprehensive. A comprehensive quantitative evaluation of the effectiveness of long-term exercise interventions on lipid metabolism in Chinese patients with NAFLD is lacking. Therefore, this study intends to select randomized controlled trials (RCTs) on long-term exercise in Chinese patients with NAFLD, to evaluate the consistency between the results of different studies using meta-analysis, and to evaluate the lipid metabolism intervention of various exercise programs in Chinese patients with NAFLD at different age levels, to provide more targeted exercise recommendations for Chinese patients with NAFLD.
Methods
Search Strategy
Relevant research articles from the construction of the database to May 2021 were collected with keywords such as “exercise,” “training,” “liver,” from the following databases: PubMed, Web of Science, China Science and Technology Journal Database (VIP), China Knowledge Resource Integrated Database (CNKI). The complete search used for PubMed was: (exercise [MeSH Terms] OR training [MeSH terms]) AND liver [MeSH terms]. The search was imposed with the limitation of RCTs and without language or status limitations. Supplementary Material details all of the search strategies used in this study.
Inclusion Criteria
The inclusion criteria followed the PICOS principle (i.e., population, intervention, comparison, outcome, and study design): (1) All NAFLD patients included in this study were definitively diagnosed by pathological examination. (2) Interventions need to include exercise interventions for at least 4 weeks. (3) The control group remained in the same condition as the study group, except for no exercise intervention. (4) Outcomes need to include: body mass index (BMI), TG, TC, LDL-C, HDL-C, alanine aminotransferase (ALT), and aspartate aminotransferase (AST). Mean and standard deviation (SD) were reported in the trials. (5) Only the trials designed as RCTs were covered.
Exclusion Criteria
Trials were excluded when they met the exclusion criteria as the following: (1) Conference abstracts, case reports, comments, review, and experimental animal studies. (2) Outcomes did not meet inclusion criteria. (3) Mean and SD could not be obtained from the articles or authors.
Studies Selection
Two reviewers (YG and XL) independently reviewed the titles or abstracts of all studies. The full contents of the relevant studies were checked carefully to evaluate whether the study could be included. Any disagreements were resolved by discussion or consultation with a third independent reviewer (QM) if necessary.
Quality Assessment
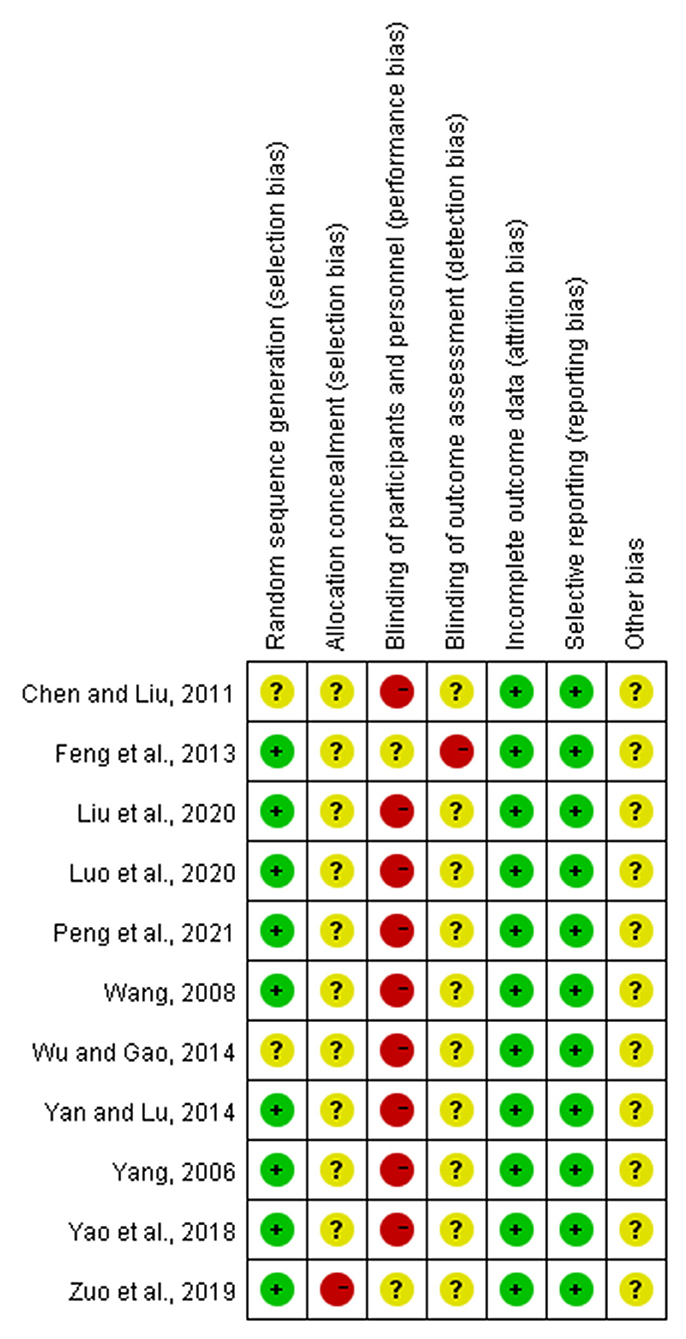
The Cochrane Collaboration tool was used to evaluate the risk of bias of the included trials (Higgins et al., 2011). Two reviewers (YG and XL) independently evaluate seven domain biases as follows: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). Three grades of high, low, or unclear bias were labeled for every study included. Disagreements were resolved by discussion or consulting with a third independent reviewer (QM) if necessary.
Data Extraction
The two reviewers independently extracted the data from every included eligible trial as the following: study characteristics (i.e., author and year), participant characteristics (i.e., age and number of participants), description of interventions, and outcomes. Any disagreements were settled by discussion to reach unanimity, and the authors of the trials were contacted directly to acquire original studies and data if necessary.
Statistical Analysis
All statistical analyses were performed using R (RStudio V1.4.1106, Boston, Massachusetts, USA), with the meta package. The percentage of variation across studies indicative of heterogeneity was reported using the I2 statistic and the Chi2 test. Interpretation of the I2 statistic was in accordance with Cochrane guidelines as following: <40% might not be important; 30–60% may represent moderate heterogeneity; 50–90% may represent substantial heterogeneity; and >75% considerable heterogeneity (Higgins et al., 2021). A statistically significant effect based on the Chi2 test suggested evidence of heterogeneity. If p < 0.05, it was considered to be a significant difference. The presence of moderate and substantial heterogeneity may provoke further investigation through a subgroup analysis of moderator variables (duration of intervention, age groups, and frequencies). Sensitivity analysis was used to study the source of heterogeneity and evaluate the stability of the results by removing each trial one by one. All experimental data were continuous variables. The value of quantitative data was shown by the mean difference (MD) with 95% confidence interval (CI). The possible publication bias was evaluated by Funnel plot asymmetry and Begg's test if more than nine trials were included.
Results
Search Results
From our initial search, 243 records were obtained. After reviewing the information on the articles' titles and abstracts, 69 potentially eligible articles were identified. After reviewing the full content of the studies, 11 articles with 13 data points (1,006 participants) satisfied the inclusion criteria and were pooled in this meta-analysis (Yang, 2006; Wang, 2008; Chen and Liu, 2011; Feng et al., 2013; Wu and Gao, 2014; Yan and Lu, 2014; Yao et al., 2018; Zuo et al., 2019; Liu et al., 2020; Luo et al., 2020; Peng et al., 2021). The details of the process of identifying articles from initially searching to inclusion are shown in Figure 1.
Description of Included Studies
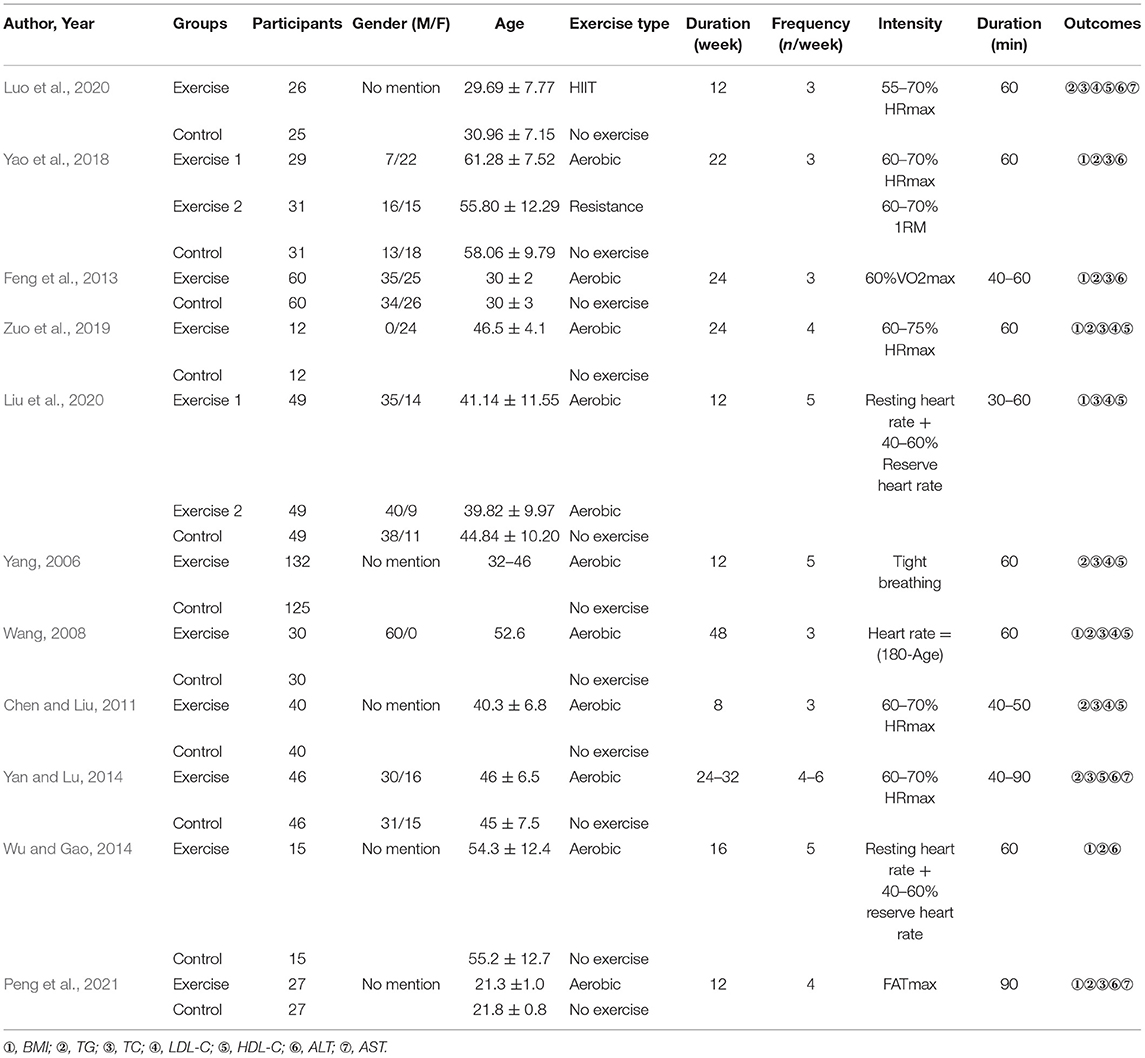
The characteristics of the included articles were summarized in Table 1, including the name of the first author, publication year, groups, participants, gender, age, intervention methods. One article was published in English, and ten in Chinese.
Risk of Bias of Included Studies
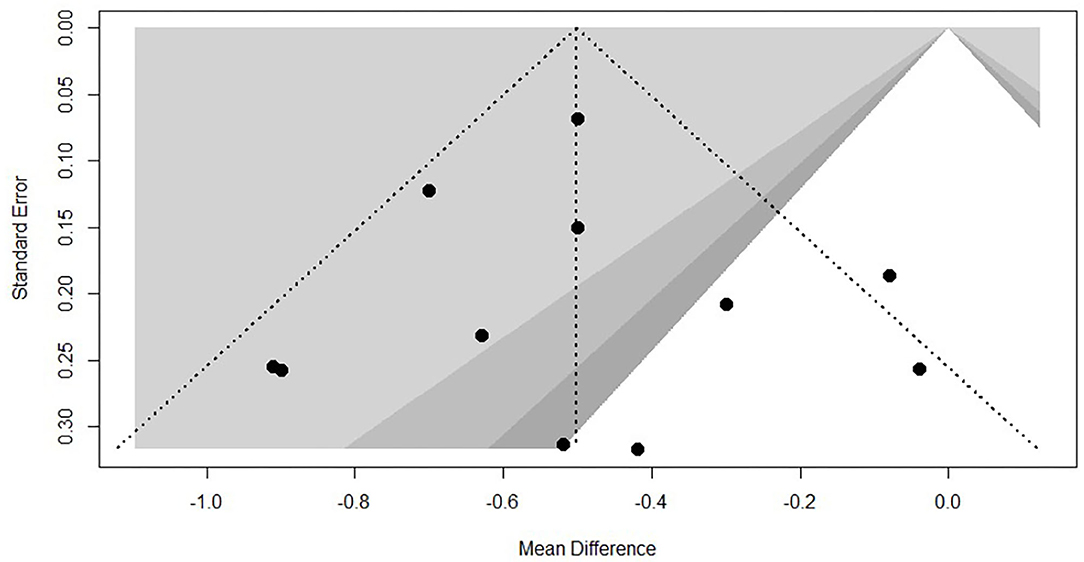
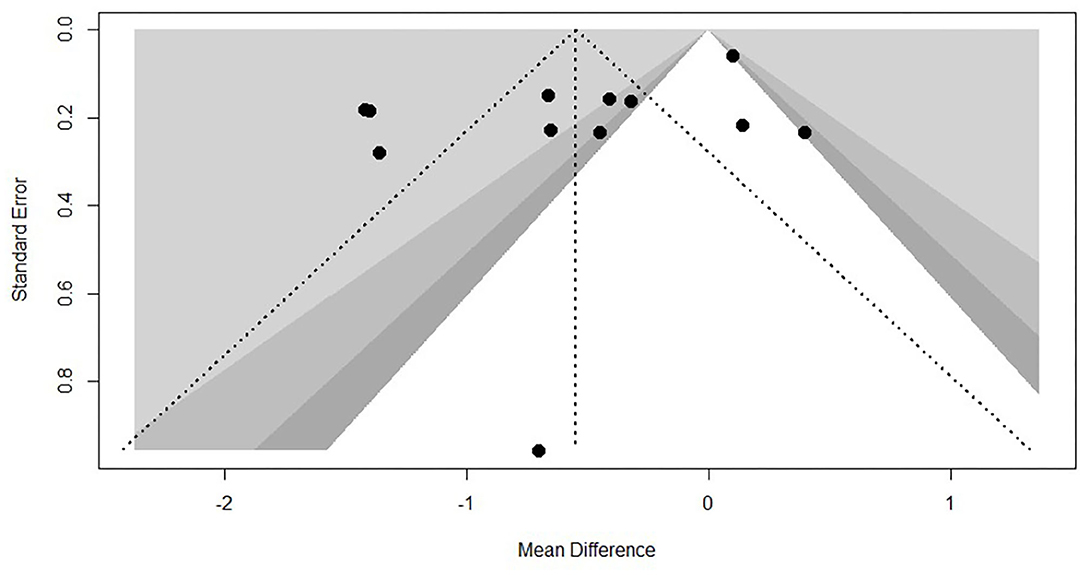
Every included study was assessed for the risk of bias according to instructions by Higgins and Green (2011). As shown in Figure 2. Most (nine articles) of the studies used a randomization method, but none of these reported any information about allocation concealment. None of the trials met the requirements for the blinding of participants. However, it seems unfeasible to use the blinding method in view of the exercise intervention. No studies masked their long-term exercise intervention, which increased the risk of detection bias. All studies showed a low risk of incomplete outcome bias and selective reporting bias. It was unclear if the studies have additional bias. Funnel plot of TC and TG, showed in Figures 3, 4, presents the MD of each individual study against its own precision (standard error). Visual inspection of the funnel plot did not reveal significant asymmetry. The statistical testing of publication bias using Begg's regression did not reach statistical significance (Begg's test for TG, p = 0.88; Begg's test for TC, p = 1).
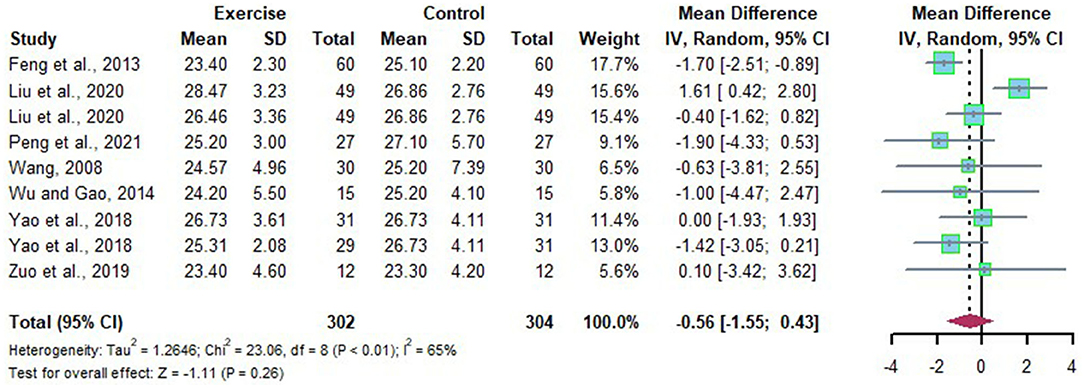
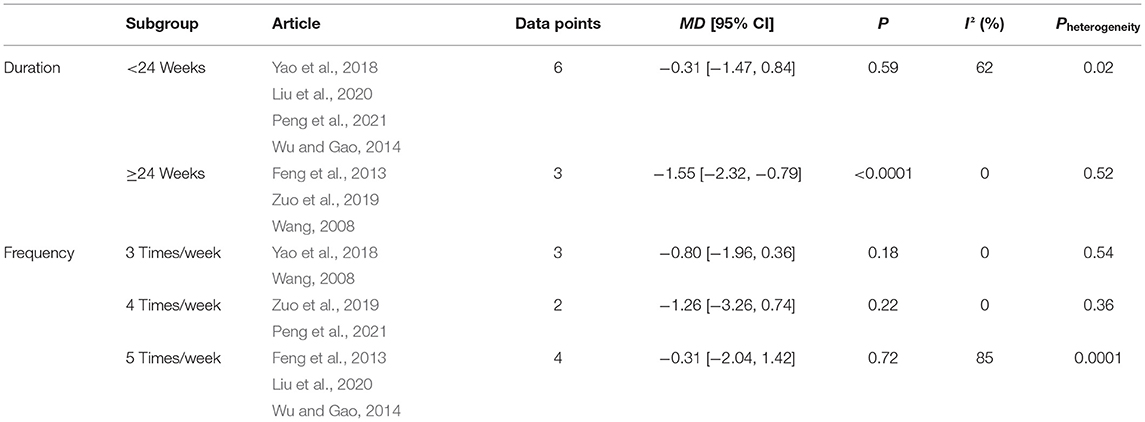
Effects of Long-Term Exercise on BMI of Chinese Patient With NAFLD
Nine data points reported the change of BMI in Chinese patients with NAFLD. Substantial heterogeneity was detected among the studies (I2 = 65%, p < 0.01). The random effects model revealed that the BMI in Chinese patients with NAFLD was not significantly reduced after long-term exercise intervention compared to that of the control group (MD = −0.56, 95%CI: −1.55 to 0.43, P = 0.26) (Figure 5). Subgroup analysis showed that long-term exercise lasts more than 6 months could significantly reduce BMI in Chinese Patients with NAFLD (MD = −1.55, 95%CI: −2.32 to −0.79, p < 0.0001), and no heterogeneity was detected in long-term exercise lasts more than 6 months subgroups (I2 = 0, p = 0.52) (Table 2).
Removing each trial one by one to evaluate the stability of the result, Liu's study was found to significantly affect the heterogeneity of included studies. The heterogeneity was reduced when this study was excluded (MD = −1.38, 95%CI: −2.00 to −0.76, p < 0.0001). Therefore, Liu's article was the key factor affecting the heterogeneity of studies.
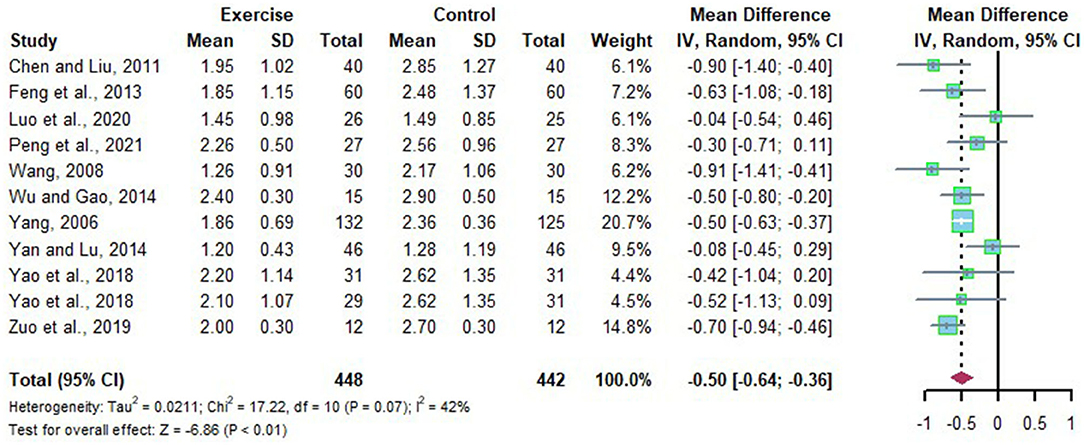
Effects of Long-Term Exercise on TG of Chinese Patient With NAFLD
Eleven studies revealed the change of TG in Chinese patients with NAFLD who received the long-term intervention. There were moderate heterogeneities detected among the studies (I2 = 42%, p = 0.07). The random effects model was applied for meta-analysis, and it revealed that the level of TG in Chinese patients with NAFLD was significantly decreased after long-term exercise intervention compared to that of the control group (MD = −0.50, 95%CI: −0.64 to −0.36, p < 0.01) (Figure 6).
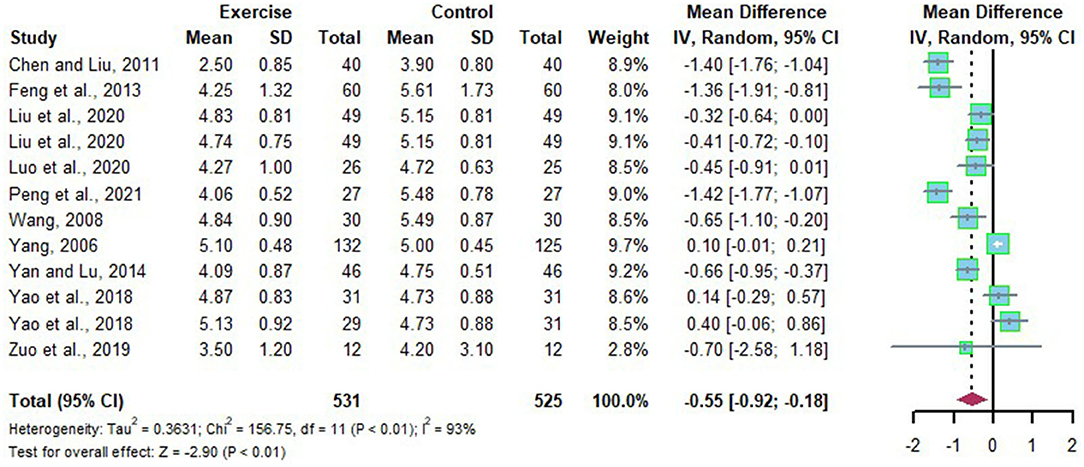
Effects of Long-Term Exercise on TC of Chinese Patient With NAFLD
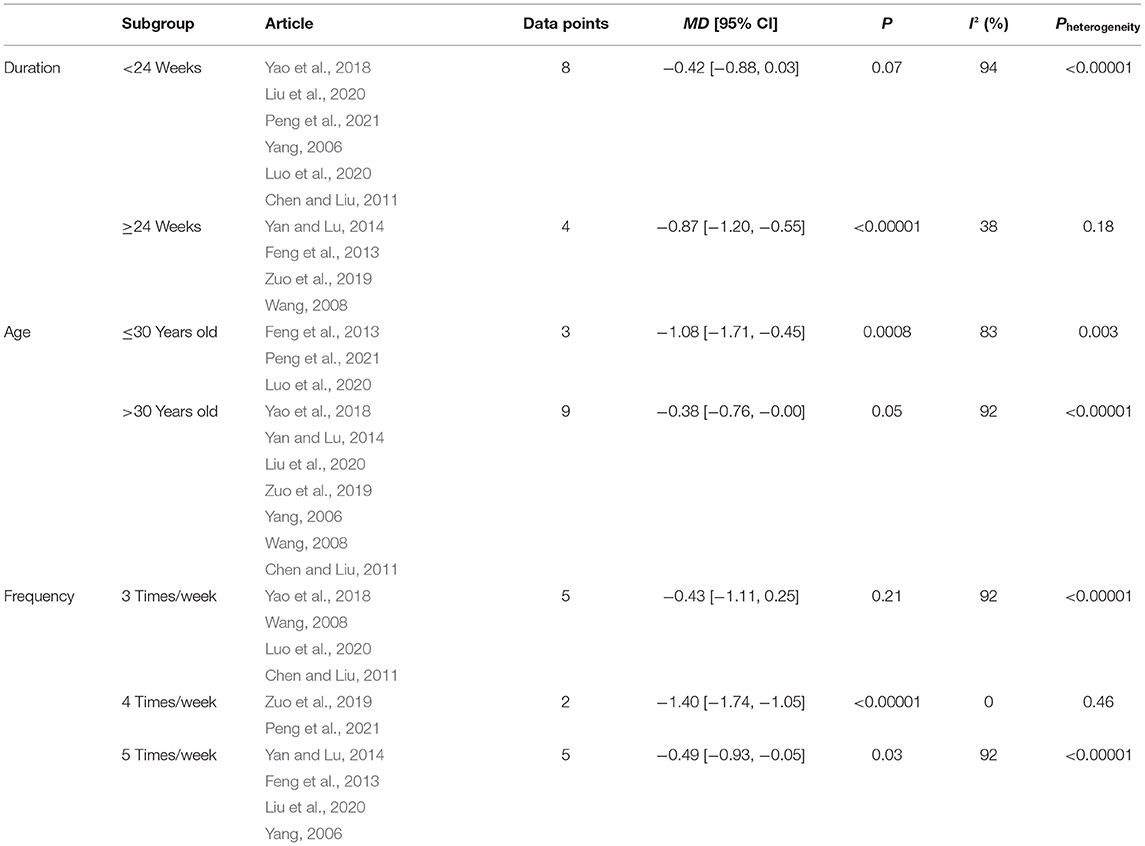
A total of 12 data points explored the efficacy of long-term exercise intervention by evaluating the change of TC in Chinese patients with NAFLD with substantial heterogeneities (I2 = 93%, p < 0.01). Meta-analysis was performed with the application of the random effects model, and the source of heterogeneity was analyzed by subgroup analysis and sensitivity analysis. Compared to the control group, TC was significantly reduced after long-term exercise intervention in Chinese patients with NAFLD (MD = −0.55, 95%CI: −0.92 to −0.18, p < 0.01) (Figure 7). Subgroup analysis showed that long-term exercise intervention lasts more than 6 months or exercising four times a week could significantly reduce TC in Chinese patients with NAFLD (MD = −0.87, 95%CI: −1.20 to −0.55, p < 0.00001) (MD = −1.40, 95%CI: −1.74 to −1.05, p < 0.00001) (Table 3).
Sensitivity analysis showed that outcomes of the effects of long-term exercise on TC of Chinese patients with NAFLD were stable when trials were removed one by one.
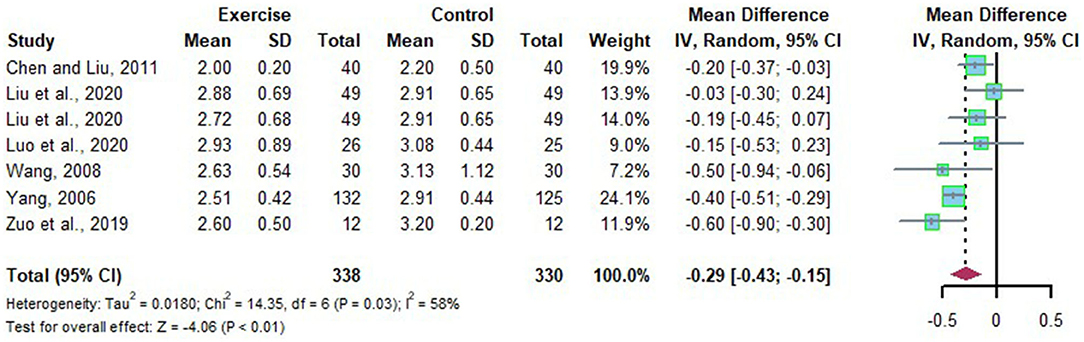
Effects of Long-Term Exercise on LDL-C of Chinese Patient With NAFLD
Seven studies evaluated the alteration of LDL-C in Chinese patients with NAFLD who received long-term exercise intervention. Moderate heterogeneities were detected among the included studies (I2 = 58%, p = 0.03). Subgroup analysis, sensitivity analysis was adopted to explore the source of heterogeneity. The random effects model was applied for meta-analysis, which suggests LDL-C was significantly declined after long-term exercise intervention compared to that of the control group in Chinese patients with NAFLD (MD = −0.29, 95%CI: −0.43 to −0.15, p < 0.01) (Figure 8). Subgroup analysis showed that long-term exercise lasts more than 6 months could significantly reduce LDL-C in Chinese patients with NAFLD (MD = −0.57, 95%CI: −0.82 to −0.32, p < 0.00001) with low heterogeneity (I2 = 0%, p = 0.72) (Table 4).
The sensitivity analysis suggested that Yang's study had an impact on the heterogeneity. We found the heterogeneity was decreased when this study was removed (MD = −0.25, 95%CI: −0.41 to −0.09, p < 0.0001). Therefore, Yang's study was the key factor affecting the heterogeneity of studies.
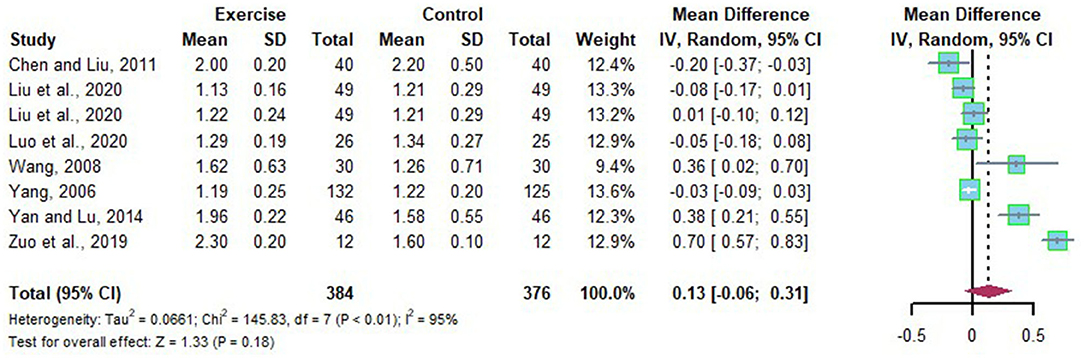
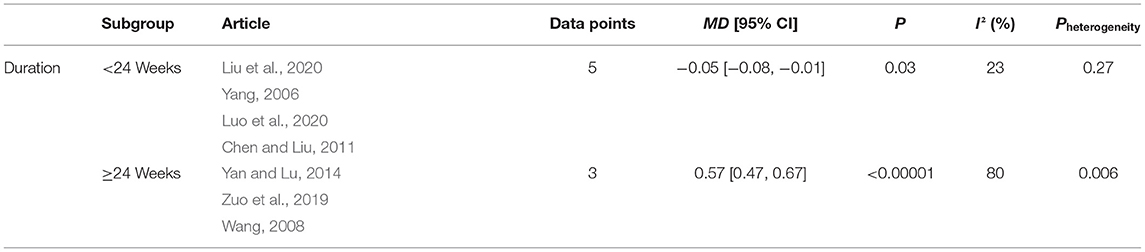
Effects of Long-Term Exercise on HDL-C of Chinese Patient With NAFLD
Eight studies reported the alteration of HDL-C in Chinese patients with NAFLD before and after long-term exercise intervention. Substantial heterogeneities were detected among the included studies (I2=95%, p < 0.01). The random effects model was applied for meta-analysis, and the source of heterogeneity was analyzed by subgroup analysis, sensitivity analysis. The random effects model revealed that HDL-C was not significantly increased after long-term exercise intervention compared to that of the control group in Chinese patients with NAFLD (MD = 0.13, 95%CI: −0.06 to 0.31, p = 0.18) (Figure 9). Subgroup analysis showed that long-term exercise more minor than half a year is not adequate for HDL-C (MD = −0.05, 95%CI: −0.08 to −0.01, p = 0.03), with low heterogeneity detected in long-term exercise less than half a year subgroups (I2 = 23%, p = 0.27) (Table 5).
The source of heterogeneity was further explored by sensitivity analysis, which found that outcomes of the effects of long-term exercise on HDL-C of Chinese patients with NAFLD were stable when trials were removed one by one.
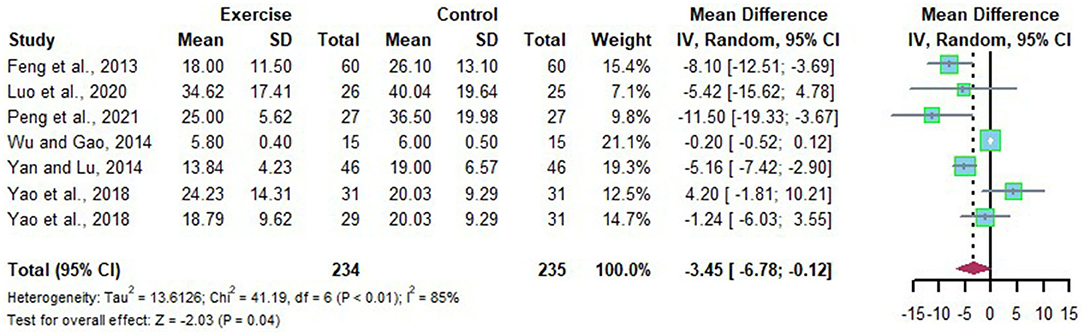
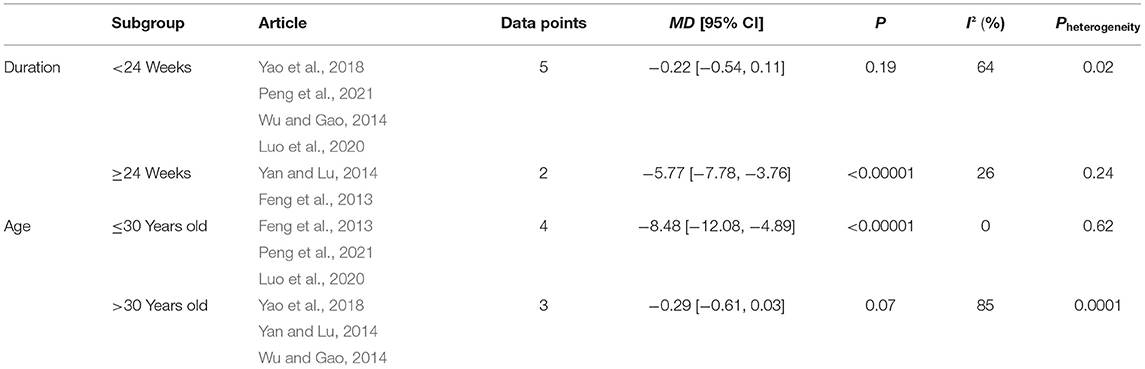
Effects of Long-Term Exercise on ALT of Chinese Patient With NAFLD
A total of seven studies assessed the efficacy of long-term exercise intervention in the treatment of NAFLD by analyzing the change of ALT with substantial heterogeneities (I2 = 85%, p < 0.01). Meta-analysis was conducted using the random effects model, and the source of heterogeneity was analyzed by subgroup and sensitivity analysis. The random effects model suggest that long-term exercise intervention tended to decrease ALT in Chinese patient with NAFLD significantly compared to that of the control group (MD = −3.45, 95%CI: −6.78 to −0.12, p = 0.04) (Figure 10). Subgroup analysis revealed that Chinese patients with NAFLD who exercised for more than or equal to 6 months at the time of the intervention or who were ≤ 30 years old were able to effectively reduce ALT levels after long-term exercise (MD = −5.77, 95%CI: −7.78 to −3.76, p < 0.00001), (MD = −8.48, 95%CI: −12.08 to −4.89, p < 0.00001) (Table 6).
The source of heterogeneity was searched for using an article-by-article exclusion, it was found that the exclusion of any article did not lead to a decrease in heterogeneity, indicating that the results of this part of the Meta-analysis were more robust.
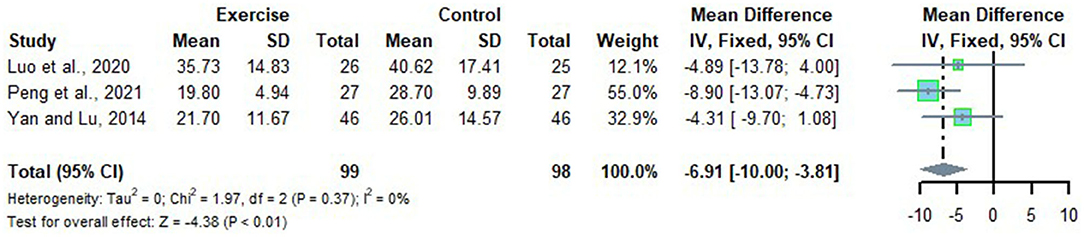
Effects of Long-Term Exercise on AST of Chinese Patient With NAFLD
Three studies looked at the alteration of AST in Chinese patients with NAFLD who received long-term exercise intervention with no heterogeneity detected (I2 = 0%, p = 0.37). Therefore, a fixed effects model was adopted for meta-analysis, and the results showed that the level of AST in Chinese patients with NAFLD was significantly reduced after long-term exercise intervention compared to that of the control group (MD = −6.91, 95%CI: −10.00 to −3.81, p < 0.01) (Figure 11).
Discussion
In recent years, the risk of NAFLD in China has been increasing. Studies have confirmed the benefits of exercise for improving NAFLD, but there is no research focusing on the effect of long-term exercise on lipid metabolism in Chinese NAFLD patients. This study aims to explore the effect of long-term exercise on the lipid metabolism of Chinese NAFLD patients.
Effects on BMI
Obesity is one of the important risk factors for NAFLD (Vernon et al., 2011). Therefore, obesity reduction can improve the status of NAFLD patients. Body mass index is widely used to identify individual obesity, and the BMI criteria for determining obesity in Chinese adults developed by the Chinese Obesity Working Group states that the reasonable range of BMI is 18.5–23.9 kg/m2 (Zhou, 2002). In the articles included in this study, the baseline of BMI in Chinese patients were all higher above this level. It shows that most Chinese patients with NAFLD are in obesity.
Our finding demonstrated that Chinese patients with NAFLD need to exercise longer than a 6 month to improve BMI significantly. But other studies held a different conclusion. For example, Zou et al. showed that exercise in any duration all had a beneficial effect on BMI in patients with NAFLD (Zou et al., 2018). Similar experimental results were also presented in Xiong's study (Xiong et al., 2021). The different results could be explained by the fact that the exercise intensity was not consistent across the literature included in the different studies. Higher intensity exercise can cause better fat loss in a short period, thus reducing BMI (Zhu et al., 2020). Most articles in our study used aerobic exercise as an intervention, and intensity was about 50–70% maximum heart rate, which did not fall within the intensity range of strenuous exercise. In contrast, in the studies by Zou et al. and Xiong et al., the character intensity of the long-term exercise intervention was less described. Therefore, lower exercise intensity may be why Chinese NAFLD patients need to exercise for longer periods to achieve improved BMI, and further studies are required in order to adjust the settings of long-term exercise intensity so that Chinese NAFLD patients can improve their BMI more efficiently.
Effects on TC, LDL-C, and HDL-C
This systematic review and meta-analysis showed that long-term exercise could significantly improve TC of Chinese patients with NAFLD. It can be related to the high baseline level of TC in participants included in this study. According to guidelines for the prevention and treatment of dyslipidemia in Chinese adults (Zhu et al., 2016), a reasonable range for TC should not exceed 5.2 mmol/L. However, there are more than half of the participants higher than this level. In this condition, they are usually diagnosed as hyperlipidemia (Zhu et al., 2016). Other studies have been conducted to demonstrate the significant improvement effect of long-term exercise on TC in hyperlipidemia populations. In addition, the results of subgroup analysis showed that long-term exercise was more effective in improving TC in younger Chinese patients with NAFLD. The same results were also shown in another study (Costa et al., 2020). It may be related to differences in basal metabolic levels in humans at different ages.
The decrease in TC may also be associated with a reduction in LDL-C. Our study showed that long-term exercise significantly decreases LDL-C in Chinese patients with NAFLD, and LDL-C accounts for 20–30% of TC in the blood, so a decline in LDL-C is an important cause of TC decline.
There are two possible reasons for lower LDL-C. One is that long-term exercise may improve LDL receptor activity on hepatocyte membranes, enhance the liver's ability to transport LDL-C, thus reducing the level of LDL-C in the blood (Chen et al., 2005). Another possibility is that increased insulin sensitivity enhances the expression of LDL-R mRNAs, thereby accelerating the rate of LDL-C metabolism (Young and Stout, 1987). How exercise affects LDL-C is still unknown, but another study has demonstrated the effect of long-term exercise in improving LDL-C in patients with NAFLD (Fu et al., 2018). This study also reported the effect of long-term exercise on the improvement of HDL-C. Our study did not get the same conclusion. Through further analysis of the literature, we found that exercise intensity may be an important reason why there was no significant difference in HDL-C between exercise and control groups. In the article that get significant results, the intensity of the exercise selected was greater (Wang et al., 2020). Stein et al. concluded that the minimum intensity of improvement in HDL-C was 75% maximum heart rate, while in our included articles, exercise intensity was mostly maintained at 50–70% maximum heart rate. Therefore, it can be assumed that the reason for the failure of long-term exercise to increase HDL-C in Chinese patients with NAFLD is related to the selection of exercise intensity.
Effects on TG
Our study shows that long-term exercise significantly reduces TG level in Chinese patients with NAFLD, which can be explained that long-term exercise increased lipolytic enzyme activity and accelerates the decomposition of TG into mitochondrial for energy supply (Boesch et al., 2010; Yu et al., 2017). In addition, the mechanism by which long-term exercise improves TG in Chinese patients with NAFLD may be related to adipocytokines such as leptin, adiponectin, and interleukin-6 (IL-6). Some studies have shown that adipocytokines are one of the causes of TG elevation (Izadi et al., 2013). The way in which long-term exercise actually improves adipokine levels still needs further research to confirm.
Effects on ALT and AST
Alanine aminotransferase and aspartate aminotransferase are the most important transaminases. Elevated blood levels of ALT and AST are a sign that the liver is damaged. This systematic review and meta-analysis showed that long-term exercise significantly improves ALT and AST in Chinese patients with NAFLD. Similar results to ours have been reported in other studies (Smart et al., 2018; Ye et al., 2019). This could be considered the ability of long-term exercise to improve the inflammatory state of the liver by increasing SIRT activity and enhancing the deacetylation of key transcription factors of inflammation and metabolism, such as NF-κB and PGC-1α (Bianchi et al., 2021), which in turn improves the state of the liver. Thus, the changes may have benefited from the improvement in inflammatory state of liver.
Strength and Limitations
This study is the first meta-analysis that focus on effect of long-term exercise on liver lipid metabolism in Chinese patients with NAFLD. Current evidence suggest that long-term exercise can improve almost all indicators related to lipid metabolism. This review searched a wide variety of databases including two Chinese electronic databases for relevant articles and two authors independently searched and selected the included studies, extracted the data, and assessed the risk of bias of every trial using recommended protocols and methodological schemes. Therefore, the results of this metaanalysis are considered a significant contribution.
However, this meta-analysis has several limitations. First, the quality of all the included trials in this meta-analysis was low. None of the studies detailed allocation concealment although all the trials used a randomization method. None of the studies met the blinding of participants though it seems unfeasible to use the blinding method in view of the exercise intervention. Second, the trials varied in methodological design (i.e., intervention methods) and conditions (i.e., duration). Thus, the outcomes have high heterogeneity although the total effects of outcomes were stable. Third, there may be some publication bias as unpublished articles could not be searched in this review although the funnel plot asymmetry did not show the bias.
Conclusion
This systematic review and meta-analysis demonstrated that long-term exercise can significantly improve the levels of TG, TC, LDL-C, ALT, and AST in Chinese patients with NAFLD and exercise last more than 6 months can decrease BMI of Chinese patients with NAFLD.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material.
Author Contributions
YG and JL designed the systematic review and supervised the entire program. YG and XL reviewed all the studies and extracted the information from the eligible trials. QM and JL analyzed the data and prepared the figures and table. YG, QM, and YS wrote the paper. YG, JL, and HS revised the manuscript. All authors reviewed and approved the manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (No. 2018YFC2000600) and Fok Ying Tung Education Foundation (No. 161094). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2021.748517/full#supplementary-material
References
Bianchi, A., Marchetti, L., Hall, Z., Lemos, H., Vacca, M., Paish, H., et al. (2021). Moderate exercise inhibits age-related inflammation, liver steatosis, senescence, and tumorigenesis. J. Immunol. 206, 904–916. doi: 10.4049/jimmunol.2001022
Bilet, L., Brouwers, B., van Ewijk, P. A., Hesselink, M. K. C., Kooi, M. E., Schrauwen, P., et al. (2015). Acute exercise does not decrease liver fat in men with overweight or NAFLD. Sci. Rep. 5, 9709. doi: 10.1038/srep09709
Boesch, C., Slotboom, J., Hoppeler, H., and Kreis, R. (2010). In vivo determination of intra-myocellular lipids in human muscle by means of localized 1H-MR-spectroscopy. Magn. Reson. Med. 37, 484–493. doi: 10.1002/mrm.1910370403
Byrne, C. D., and Targher, G. (2015). NAFLD: a multisystem disease. J. Hepatol. 62, S47–S64. doi: 10.1016/j.jhep.2014.12.012
Caspersen, C. J., Powell, K. E., and Christenson, G. M. (1985). Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 100, 126–131.
Chen, C., and Liu, J. (2011). The study of the relevance of nonalcoholic fatty liver disease with exercise and cholinesterase. J. Taishan Med. Coll. 32, 731–734.
Chen, W., Penumetcha, M., Santanam, N., Liu, Y. G., and Parthasarathy, S. (2005). Exercise might favor reverse cholesterol transport and lipoprotein clearance: potential mechanism for its anti-atherosclerotic effects. Biochim. Biophys. Acta. 1723, 124–127. doi: 10.1016/j.bbagen.2005.03.005
Costa, R. R., Barroso, B. M., Reichert, T., Vieira, A. F., and Kruel, L. F. M. (2020). Effects of supervised exercise training on lipid profile of children and adolescents: systematic review, meta-analysis and meta-regression. Sci. Sports 35, 321–329. doi: 10.1016/j.scispo.2020.02.007
Day, C. P., and James, O. (1998). Steatohepatitis: a tale of two 'Hits'? Gastroenterology 114, 842–845. doi: 10.1016/S0016-5085(98)70599-2
Day, C. P., and James, O. F. (2010). Hepatic steatosis: innocent bystander or guilty party? Hepatology 27, 1463–1466. doi: 10.1002/hep.510270601
DeFilippis, A. P., Blaha, M. J., Martin, S. S., Reed, R. M., Jones, S. R., Nasir, K., et al. (2013). Nonalcoholic fatty liver disease and serum lipoproteins: the multi-ethnic study of atherosclerosis. Atherosclerosis 227, 429–436. doi: 10.1016/j.atherosclerosis.2013.01.022
Farzanegi, P., Dana, A., Ebrahimpoor, Z., Asadi, M., and Azarbayjani, M. A. (2019). Mechanisms of beneficial effects of exercise training on non-alcoholic fatty liver disease (NAFLD): roles of oxidative stress and inflammation. Eur. J. Sport Sci. 19, 994–1003. doi: 10.1080/17461391.2019.1571114
Feng, R., Ma, R., Zhang, X., Wang, S., and Li, Y. (2013). Clinical efficacy of diet, exercise and combined early intervention in young people with non-alcoholic fatty liver disease. J. Hebei Med. Univ. 34, 1432–1435. doi: 10.3969/j.issn.1007-3205.2013.11.027
Fu, Y., Meng, M., Rong, N., Liu, l., Zhang, J., and Chen, S. (2018). Study on the effect of aerobic exercise and resistance exercise on patients with nonalcoholic fatty liver disease. J. Nanjing Med. Univ. Nat. Sci. 38, 528–531. doi: 10.7655/NYDXBNS20180422
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi: 10.1136/bmj.d5928
Higgins, J. P., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al (2021). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2. Available online at: https://training.cochrane.org/handbook/current (accessed September 16, 2021).
Higgins, J. P. T., and Green, S., (eds.). (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available online at: www.handbook.cochrane.org.
Izadi, V., Farabad, E., and Azadbakht, L. (2013). Epidemiologic evidence on serum adiponectin level and lipid profile. Int. J. Prev. Med. 4, 133–140.
Liu, Y., Liu, Y., Liu, Y., and Sun, P. (2020). Implementation of aerobic exercise intervention in patients with metabolic associated fatty liver disease: a prospective study. J. Clin. Hepatol. 36, 2467–2472. doi: 10.3969/j.issn.1001-5256.2020.11.014
Luo, C., Li, H., Tian, D., Song, L., Yang, Y., Wang, M., et al. (2020). High intensity interval exercise on NAFLD under exercise and medical integration: exercise method and evaluation. J. Beijing Norm. Univ. Nat. Sci. 56, 132–140. doi: 10.16360/j.cnki.jbnuns.2020.01.018
Nath, P., Panigrahi, M. K., Sahu, M. K., Narayan, J., Sahoo, R. K., Patra, A. A., et al. (2020). Effect of exercise on NAFLD and its risk factors: comparison of moderate versus low intensity exercise. J. Clin. Transl. Hepatol. 8, 120–126. doi: 10.14218/JCTH.2019.00012
Peng, K. P., Mo, Z. N., and Tian, G. X. (2017). Serum lipid abnormalities and nonalcoholic fatty liver disease in adult males. Amer. J. Med. Sci. 353, 236–241. doi: 10.1016/j.amjms.2017.01.002
Peng, Y., Zhu, H., Yang, M., Zhou, H., Liu, X., and Wang, C. (2021). The effects of 12-week fatmax intensity exercise on blood glucose, blood lipids and liver function in obese non-alcoholic fatty liver patients. Genom. Appl. Biol. 2021, 1–16.
Romero-Gomez, M., Zelber-Sagi, S., and Trenell, M. (2017). Treatment of NAFLD with diet, physical activity and exercise. J. Hepatol. 67, 829–846. doi: 10.1016/j.jhep.2017.05.016
Smart, N. A., King, N., McFarlane, J. R., Graham, P. L., and Dieberg, G. (2018). Effect of exercise training on liver function in adults who are overweight or exhibit fatty liver disease: a systematic review and meta-analysis. Brit. J. Sports Med. 52, 834–843. doi: 10.1136/bjsports-2016-096197
Vernon, G., Baranova, A., and Younossi, Z. M. (2011). Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharmacol. Therapeut. 34, 274–285. doi: 10.1111/j.1365-2036.2011.04724.x
Wang, S. T., Zheng, J., Peng, H. W., Cai, X. L., Pan, X. T., Li, H. Q., et al. (2020). Physical activity intervention for non-diabetic patients with non-alcoholic fatty liver disease: a meta-analysis of randomized controlled trials. BMC Gastroenterol. 20:66. doi: 10.1186/s12876-020-01204-3
Wang, X. (2008). Intervention of appropriate intensity aerobic exercise on the efficacy of nonalcoholic fatty liver disease. Chin. J. Gerontol. 8, 777–779.
Wilmore, J. H., Costill, D. L., and Kenney, W. L. (2008). Physiology of Sport and Exercise, Vol. 4. Champaign, IL: Human Kinetics.
Wu, S., and Gao, L. (2014). Effect of diet control combined with aerobic exercise on TNF-α, SREBP-1C levels in patients with non-alcoholic fatty liver. China Mod. Doct. 52, 4–8.
Xiong, Y. Z., Peng, Q. W., Cao, C. M., Xu, Z. J., and Zhang, B. (2021). Effect of different exercise methods on non-alcoholic fatty liver disease: a meta-analysis and meta-regression Int. J. Environ. Res. Public Health. 18, 3242. doi: 10.3390/ijerph18063242
Yan, M., and Lu, H. (2014). Clinical observation of fitness running (walking) and Tai Ji Quanin treatment of mild fatty liver. J. Liaon. Univ. Trad. Chin. Med. 16, 96–98. doi: 10.13194/j.issn.1673-842x.2014.02.033
Yang, Y. (2006). The role and experience of exercise therapy in the treatment of fatty liver. Chin. J. Convalesc. Med. 6, 462–463. doi: 10.13517/j.cnki.ccm.2006.06.043
Yao, J., Meng, M., Yang, S., Li, F., Anderson, R. M., Liu, C., et al. (2018). Effect of aerobic and resistance exercise on liver enzyme and blood lipids in Chinese patients with nonalcoholic fatty liver disease: a randomized controlled trial. Int. J. Clin. Exp. Med. 11, 4867–4874.
Ye, Y., Chen, L. L., and Yang, X. P. (2019). The efficacy of resistance training for non-alcoholic fatty-liver disease: a meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 12, 13188–13195.
Young, I. R., and Stout, R. W. (1987). Effects of insulin and glucose on the cells of the arterial wall: interaction of insulin with dibutyryl cyclic AMP and low density lipoprotein in arterial cells. Diabete Metab. 13(3 Pt 2), 301–306.
Younossi, Z. M., Koenig, A. B., Abdelatif, D., Fazel, Y., Henry, L., and Wymer, M. (2016). Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84. doi: 10.1002/hep.28431
Yu, N., Ruan, Y. T., Gao, X. Y., and Sun, J. (2017). Systematic review and meta-analysis of randomized, controlled trials on the effect of exercise on serum leptin and adiponectin in overweight and obese individuals. Horm. Metab. Res. 49, 164–173. doi: 10.1055/s-0042-121605
Zhou, B. (2002). Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Chin. J. Epidemiol. 23, 5–10.
Zhu, J., Gao, R., Zhao, S., Lu, G., Zhao, D., and Li, J. (2016). Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (2016 revised edition). Chin. Circ. J. 31, 937–953. doi: 10.3969/j.issn.1000-3614.2016.10.001
Zhu, L., Liu, J., Yu, Y., and Liu, W. (2020). Effectiveness of high-intensity interval training on fat loss overweight and obese adolescent: a meta-analysis. J. Guang. Sport Univ. 40, 96–101. doi: 10.13830/j.cnki.cn44-1129/g8.2020.01.022
Zou, T. T., Zhang, C., Zhou, Y. F., Han, Y. J., Xiong, J. J., Wu, X. X., et al. (2018). Lifestyle interventions for patients with nonalcoholic fatty liver disease: a network meta-analysis. Eur. J. Gastroenterol. Hepatol. 30, 747–755. doi: 10.1097/MEG.0000000000001135
Keywords: long-term exercise, non-alcoholic fatty liver disease, lipid metabolism, meta-analysis, systematic review
Citation: Gao Y, Lu J, Liu X, Liu J, Ma Q, Shi Y and Su H (2021) Effect of Long-Term Exercise on Liver Lipid Metabolism in Chinese Patients With NAFLD: A Systematic Review and Meta-Analysis. Front. Physiol. 12:748517. doi: 10.3389/fphys.2021.748517
Received: 28 July 2021; Accepted: 05 October 2021;
Published: 22 November 2021.
Edited by:
Shahrad Taheri, Cornell University, United StatesReviewed by:
Zhaowei Kong, University of Macau, Macao SAR, ChinaKhaled Trabelsi, University of Sfax, Tunisia
Copyright © 2021 Gao, Lu, Liu, Liu, Ma, Shi and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Su, c3VoYW8xOTgyQDE2My5jb20=
 Ye Gao
Ye Gao Jiandong Lu
Jiandong Lu Xinhong Liu
Xinhong Liu Jingqi Liu
Jingqi Liu Qirui Ma
Qirui Ma Yajun Shi
Yajun Shi Hao Su
Hao Su