- 1Department of Exercise and Sport, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Department of Health and Human Development, University of Pittsburgh, Pittsburgh, PA, United States
- 3Department of Exercise Physiology, King Saud University, Riyadh, Saudi Arabia
Prolonged sitting increases cardiovascular disease (CVD) risk, however the physiological mechanisms contributing to CVD from acute sitting exposure are not well-understood. Therefore, this study investigated the heart rate (HR) and variability (HRV) responses to prolonged sitting and after interrupting prolonged sitting (e.g., walking). Electronic databases were searched (inception-August 2020) for studies which exposed adults to prolonged (≥1 h) sitting with and/or without interruptions. Twenty-one articles (27 trials, n = 537) met inclusion criteria. Prolonged sitting non-significantly increased HR (weighted mean difference (WMD) = 0 bpm, 95% CI: −2, 3) and HRV (standardized mean difference (SMD) = 0.12, 95% CI: −0.08, 0.33) compared to pre-sitting baseline. Interrupting prolonged sitting yielded a non-significant small increase in HR (WMD = 4 bpm, 95% CI: 0, 7) compared to pre-sitting baseline. Sub-group analyses investigating interrupting prolonged sitting revealed small-to-moderate increases in HR in healthy populations (WMD = 6 bpm, 95% CI: 1, 10) and following walking interruptions (WMD = 7 bpm, 95% CI: 3, 11). In conclusion, prolonged sitting does not significantly affect HR or HRV. However, interrupting prolonged sitting yielded a small non-significant increase in HR, potentially indicative of increased metabolic demand. Further research is needed to investigate poor CVD outcomes via autonomic disruption from prolonged sitting.
Introduction
Regular sedentary behavior exposure, defined as low energy expenditure (≤1.5 metabolic equivalents) in a seated, reclined, or lying posture (Tremblay et al., 2017), is associated with increased cardiovascular disease (CVD) incidence and mortality (Biswas et al., 2015). However, the mechanisms connecting acute prolonged sitting exposure to CVD risk are not well-understood. In order to understand how repeated exposure to prolonged sitting contributes to CVD overtime, we need to first understand the physiological response to a single bout of sitting. A recent meta-analysis (Paterson et al., 2020) reported that exposure to uninterrupted prolonged sitting leads to acute lower-extremity endothelial dysfunction, perhaps indicating a direct hemodynamic effect on the lower extremity vasculature. These effects may result from systemic cardiovascular effects where prolonged sitting causes blood pooling in the lower extremities (Dempsey et al., 2018), leading to reduced venous return, decreased stroke volume, and a subsequent decrease in lower extremity blood flow (Thosar et al., 2012; De Brito et al., 2015; Credeur et al., 2019). The decrease in lower extremity blood flow leads to a decrease in shear stress – the principal stimulus maintaining endothelial cell health (Wheeler et al., 2019). Additionally, the decrease in stroke volume can unload the baroreceptors, triggering the autonomic nervous system to increase heart rate (HR) in an attempt to maintain cardiac output while vasoconstricting resistance vessels to maintain blood pressure (Shaffer et al., 2014). Overtime, this may result in an elevated resting heart rate, which is associated with CVD risk (Altenburg et al., 2019). Furthermore, reduced heart rate variability (HRV) at rest is indicative of autonomic dysfunction, a known risk factor of CVD (Ebara et al., 2008), however research evaluating the effects of prolonged sitting exposure on cardio-autonomic function is limited and inconsistent in both findings and methodology (sitting duration, sitting control, measurement devices, etc.).
Breaking up prolonged sitting bouts with interruption strategies reduces blood pressure (Barone Gibbs et al., 2017a) and preserves lower extremity endothelial function (Paterson et al., 2020). Thus, interruption may help to protect the cardiovascular system potentially reducing the burden of blood pooling (decreasing resting HR) stimulating cardio-autonomic activity (increasing HRV). At present specific guidelines for interrupting sitting behavior, i.e., what to substitute prolonged sitting behavior with, are lacking. Interruption strategies including standing (Wennberg et al., 2016; Barone Gibbs et al., 2017b; Carter et al., 2018; Kruse et al., 2018; Dogra et al., 2019), walking (De Brito et al., 2015; Evans et al., 2019; Kowalsky et al., 2019), cycling (Sperlich et al., 2018; Dogra et al., 2019), calf-raises (Cabak et al., 2017), or strength training (Garten et al., 2018; Headid et al., 2020) have been tested. However, the findings have been inconsistent and the optimal strategy for interrupting prolonged sitting remains unknown. Summarizing the effects of sitting interruptions on the cardio-autonomic system can help to quantify effects, identify strengths and limitations of the existing literature, and indicate further research requirements.
Objective
The purpose of this meta-analysis was to consolidate the literature investigating the effects of acute prolonged sitting on the cardio-autonomic system, specifically the HR and heart rate variability (HRV) responses (Shvartz et al., 1983; Moher et al., 2009; Higgins et al., 2011, 2019; Thosar et al., 2012; De Brito et al., 2015; Restaino et al., 2015; Wennberg et al., 2016; Barone Gibbs et al., 2017b; Cabak et al., 2017; Kerr et al., 2017; Vranish et al., 2017; Carter et al., 2018; Garten et al., 2018; Horiuchi et al., 2018; Kruse et al., 2018; Sperlich et al., 2018; Credeur et al., 2019; Dogra et al., 2019; Evans et al., 2019; Kowalsky et al., 2019; Headid et al., 2020). Additionally, a secondary purpose of this meta-analysis was to increase our understanding with regard to how interrupting sitting may attenuate CVD effects of prolonged sitting such as HR when available.
Methods
This meta-analysis was carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Barendregt and Doi, 2015) and registered with PROSPERO (International Prospective Register of Systematic Reviews: CRD42020196685).
Data Sources and Searches
Electronic databases (PubMed and Google Scholar) were searched by two authors (LB, AA) utilizing the following search terms: (sitting or sedentarism or sedentary or television time or screen time) AND (HRV or heart rate variability or heart rate).
The reference lists of all identified trials and relevant reviews or editorials were also examined. The search was limited titles and abstracts written in English language with human adult (18 years of age and older) populations published between database inception and August 31st, 2020.
Article Selection
Two researchers (LB and AA) completed the study selection independently. For the purpose of this meta-analysis, the term “article” is used synonymously with “study” and “trial” is the unit included in the meta-analysis. A given article may have resulted in more than one eligible “trial” if the article included more than one HR and HRV measure and/or more than one intervention group or condition. Initially, article titles and abstracts were screened for relevance by two reviewers (LB and AA) and a third reviewer was used to settle a potential split-decision (LS). The full-text versions of potentially eligible articles were obtained to evaluate for eligibility, also by two reviewers (LB and AA). The following criteria were used to select trials for inclusion in this review: (i) English language, (ii) human studies, (iii) adults (18 years of age and older), (iv) inclusion of an uninterrupted prolonged (>1 h) sitting bout. The following criteria were used to select trials for the secondary objective of interrupting prolonged sitting (i) prolonged sitting occurred prior to interruption, (ii) subjects returned to sitting following interruption. Repeated publications from the same studies were excluded.
Data Extraction and Quality Assessment
Data extraction, quality assessment, and investigation of the sitting interruption were completed by two reviewers (LB and LS). Data extracted for each eligible trial included bibliographic information (author, publication year), baseline participant characteristics, details of prolonged sitting bout (and interruption condition, if relevant), and reported outcomes.
Study quality was assessed using the RoB2: revised Cochrane risk-of-bias tool for randomized trials (range 1–3), which includes items related to randomization, deviations from intended interventions, missing data, measurement of the outcome, selection of the reported result, and overall bias (Assink and Wibbelink, 2016). Because it is difficult (if not impossible) to blind participants to a bout of prolonged sitting (or interruption to prolonged sitting), we considered blinding of the operator assessing the outcome as the quality criterion for this item. Additionally, pre-assessment guidelines (including abstaining from alcohol, tobacco, caffeine, food, and exercise) as well as quality of prolonged sitting (i.e., were bathroom breaks allowed and/or standardized) were further quality criterion.
Data Synthesis
Aggregation (LB) and calculation of final results was conducted by one author (LS). For each outcome of interest, the pre- and post-prolonged sitting bout values (mean and standard deviation) were extracted. When mean differences and associated standard deviations were not published, they were estimated from the pre- and post-intervention values based on methods (calculated from standard errors or from confidence intervals) from the Cochrane Handbook for Systematic Reviews of Interventions (Doi et al., 2015a) or provided by the authors following contact. For studies reporting multiple time points, only the final time point was used in analyses. Primary study outcomes were HR (bpm) and HRV (Root mean square of the successive differences [RMSSD], standard deviation of all NN intervals [SDNN], high frequency [HF], low frequency [LF], high frequency/low frequency ratio [HF/LF], and/or total variance [TV]).
Data Analysis
A single author (LS) conducted all statistical analysis using the MetaXL software (Doi et al., 2015b), and ancillary analysis using the metafor-package (Cohen, 1988) for the R statistical environment (RKWard version 0.7.1). HR parameter estimates are expressed as both the weighted mean difference (WMD) and standardized mean difference (SMD, Cohen's). Considering HRV measures are expressed using different units and scales, HRV parameter estimates are only reported as SMD. Data were pooled using the inverse variance heterogeneity (IVhet) model of meta-analysis to account for potential heterogeneity within and between studies (Sterne et al., 2011). This method has been shown to be a preferred alternative to the more traditional random-effects model which has been suggested to underestimate statistical error and produce overconfident estimates when using heterogenous data. Additionally, the IVhet models were adjusted according to the adjudicated quality (RoB2 score) of each included study (Duval and Tweedie, 2000). The SMD was used to assess the magnitude of effect, where <0.2, 0.2, 0.5, and 0.8 was defined as trivial, small, moderate, and large, respectively (Furuya-Kanamori et al., 2018).
Subsequent to running the IVhet and Quality Effects models, we examined the robustness of the pooled results and the potential for publication bias. Sensitivity analyses were conducted by removing one trial at a time. Measures of publication bias included visual inspection of Begg's funnel plots (Higgins et al., 2003), recalculation of the pooled estimate using Duval and Tweedie's trim and fill method (Cheung, 2019), and inspection of Doi plots in tandem with The Luis Furuya Kanamori (LFK) index (Sakowski et al., 2011). Doi plots are reported to be more objective than the qualitative Begg's funnel plot, and the LFK index has been reported to be a more sensitive quantitative measure of asymmetry and potential bias than the Egger's regression intercept test (Moher et al., 2009). Using the LFK method, <1 indicates no asymmetry, 1–2 suggests minor asymmetry, and >2 indicates major asymmetry (Moher et al., 2009). Last, statistical heterogeneity was assessed using the I2 statistic, where <25, 25–75, and >75% represent low, moderate, and considerable heterogeneity, respectively (Peddie et al., 2013). Heterogeneity >25% was assumed to indicate that effect sizes could not be treated as estimates of one common effect size, justifying a priori determined sub-group analysis.
The metafor-package for R statistical software was used to conduct ancillary analyses (Crespo et al., 2016). Meta-analysis statistical models typically assume independent effect sizes (Crespo et al., 2016). For the current meta-analysis, most included studies reported more than one estimate of HRV (e.g., RMSSD and HF). To more robustly account for effect size dependency, a 3-level model was conducted with restricted maximum likelihood estimation (Cohen, 1988; Crespo et al., 2016). The 3 sources of variance taken into account included: variance at the level of the subject (Level 1), variance between effect sizes extracted from the same study (Level 2), and variance between studies (Level 3). To determine the significance of the level 2 and level 3 variance, the full model was compared to a model excluding one of these variance parameters in two separate log-likelihood ratio tests. In the event of significant level- 2 and/or level-3 variance, the distribution of effect sizes was considered heterogeneous.
Results
Literature Search and Trial Selection
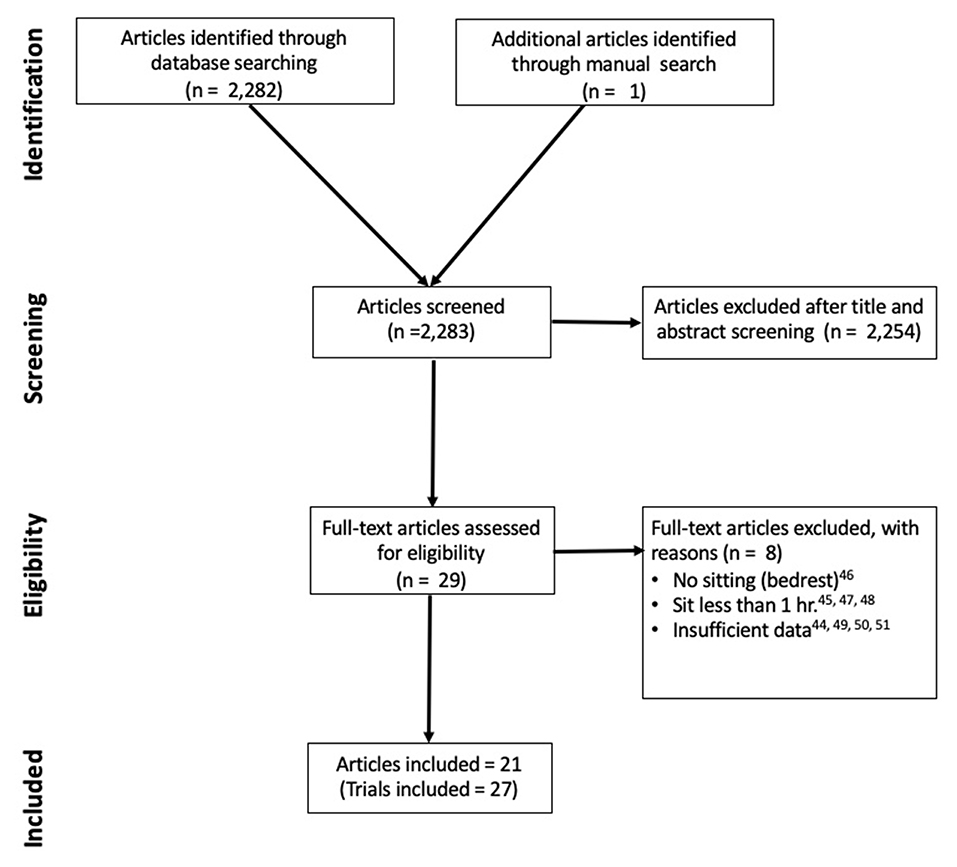
Figure 1 outlines the literature search strategy. A total of 2,283 potentially eligible articles were identified. Following screening of titles and abstracts, 2,254 articles were excluded because they did not meet selection criteria. Of these, 29 randomized cross-over trials underwent full text screening and 8 were excluded (Chaput and Tremblay, 2007; Bourdin et al., 2010; Jean-François et al., 2010; Larsen et al., 2014; Restaino et al., 2015; Botter et al., 2016; Garten et al., 2018; Snarr et al., 2019). The final analysis included 22 studies (27 trials) with 21 studies reporting HR data (Shvartz et al., 1983; Chowienczyk et al., 1994; Higgins et al., 2011, 2019; Thosar et al., 2012; De Brito et al., 2015; Restaino et al., 2015; Wennberg et al., 2016; Barone Gibbs et al., 2017b; Cabak et al., 2017; Vranish et al., 2017; Carter et al., 2018; Garten et al., 2018; Horiuchi et al., 2018; Sperlich et al., 2018; Credeur et al., 2019; Dogra et al., 2019; Evans et al., 2019; Kowalsky et al., 2019; Cheng-Hsuan et al., 2020; Headid et al., 2020) and seven studies reporting HRV data (Shvartz et al., 1983; Chowienczyk et al., 1994; Thosar et al., 2012; Restaino et al., 2015; Cabak et al., 2017; Kruse et al., 2018; Credeur et al., 2019). Additionally, 13 of the HR studies reported interruption conditions to the bout of prolonged sitting (De Brito et al., 2015; Wennberg et al., 2016; Barone Gibbs et al., 2017b; Cabak et al., 2017; Vranish et al., 2017; Carter et al., 2018; Garten et al., 2018; Kruse et al., 2018; Sperlich et al., 2018; Dogra et al., 2019; Evans et al., 2019; Kowalsky et al., 2019; Headid et al., 2020), however there were not enough HRV studies reporting interruption conditions (Cabak et al., 2017; Kruse et al., 2018) to summarize with meta-analysis.
Description of the Included Trials
Trial Setting and Participants
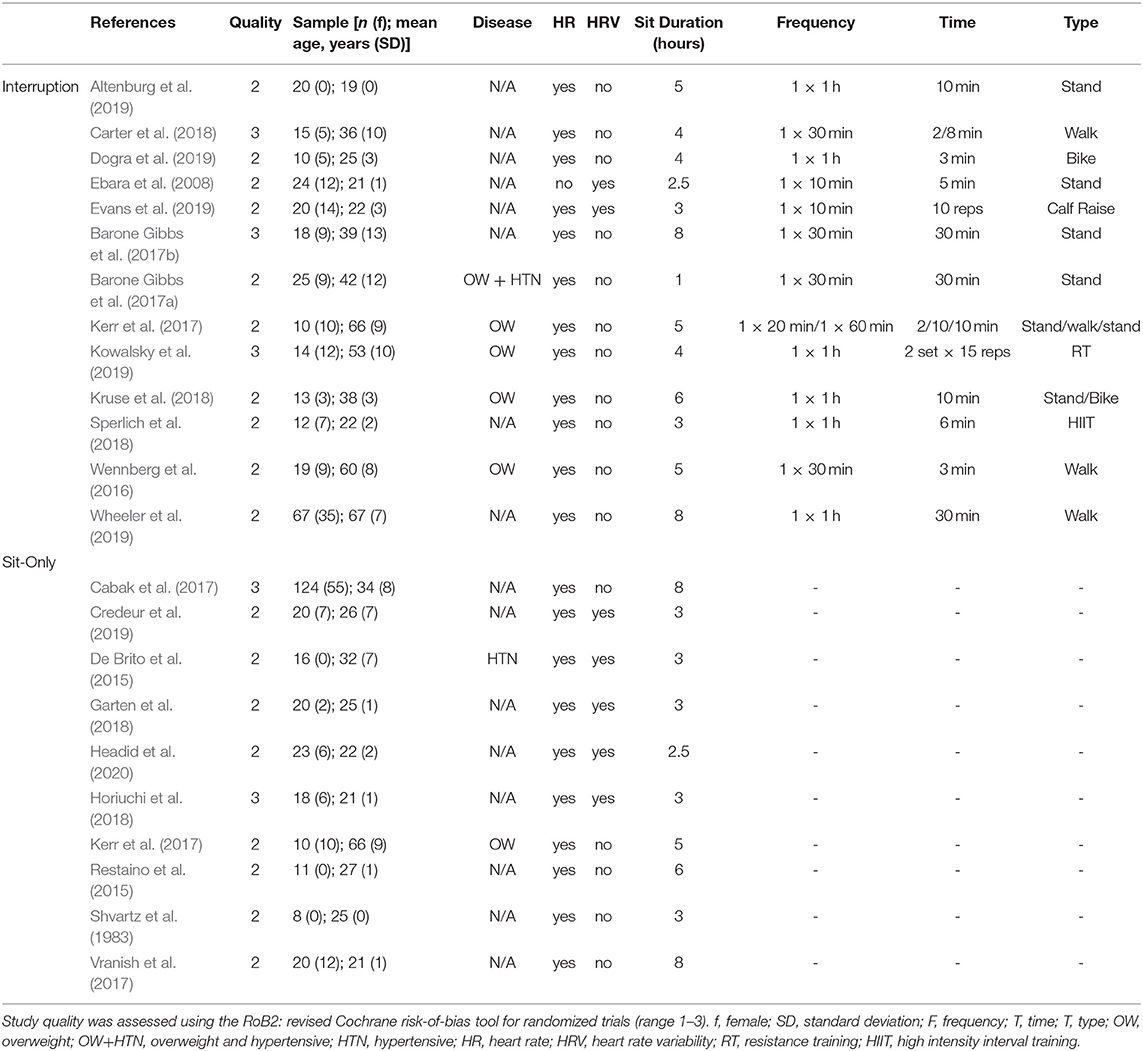
Characteristics of included trials are summarized in Table 1. The number of participants in each trial ranged from 8 (Higgins et al., 2011) to 124 (Horiuchi et al., 2018). One HR trial included only females (Vranish et al., 2017) and 4 HR trials (Higgins et al., 2011; Barone Gibbs et al., 2017b; Credeur et al., 2019; Cheng-Hsuan et al., 2020) and 1 HRV (Credeur et al., 2019) trial included only males. The mean age of the participants ranged from 19 ± 0 (Cheng-Hsuan et al., 2020) to 67 ± 7 years (Garten et al., 2018). Seven trials included clinical populations with cardiometabolic diseases including one trial with hypertensive participants (Credeur et al., 2019), four trials with overweight/obese participants (Vranish et al., 2017; Garten et al., 2018; Dogra et al., 2019; Kowalsky et al., 2019), and two trials with both hypertension and overweight/obese participants (Wennberg et al., 2016; Carter et al., 2018). Bouts of prolonged sitting ranged from 1 (Headid et al., 2020) to 9 (Dogra et al., 2019) h with an average duration of 5 h. It should also be noted that all HRV studies (Shvartz et al., 1983; De Brito et al., 2015; Vranish et al., 2017; Carter et al., 2018; Garten et al., 2018; Wheeler et al., 2019) l for <3 h, which was characterized as a short bout of sitting. Of the 22 trials, 13 included interruptions to sitting (De Brito et al., 2015; Wennberg et al., 2016; Barone Gibbs et al., 2017b; Cabak et al., 2017; Vranish et al., 2017; Carter et al., 2018; Garten et al., 2018; Kruse et al., 2018; Sperlich et al., 2018; Dogra et al., 2019; Evans et al., 2019; Kowalsky et al., 2019; Headid et al., 2020). The duration and frequency of interruption varied in length from 10 calf raises every 10 min (Cabak et al., 2017) to 30 min of walking once (De Brito et al., 2015). The trials included varying modalities of interruption strategies as well including standing, walking, biking and/or pedaling, calf-raises, or strength training interruptions.
Methodological Quality Assessment
As reported in Table 1, the quality of the included studies ranged from 1 to 3 out of 3. Overall, included studies had a median quality score of 2 indicating fair quality.
Synthesis of the Results
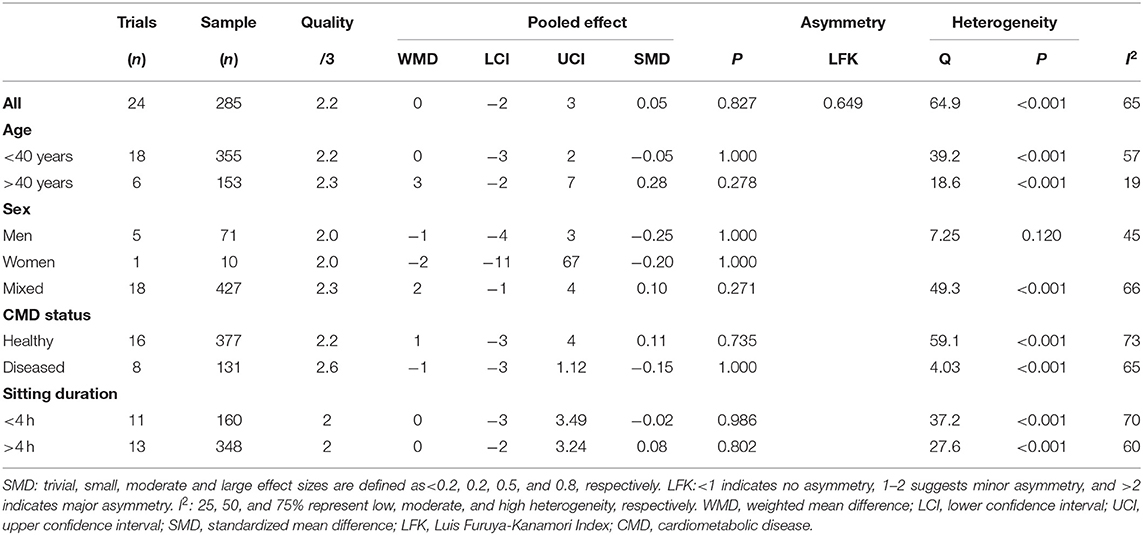
Prolonged Sitting: Heart Rate
Prolonged sitting resulted in a trivial, non-significant increase in HR (Table 2). Sensitivity analysis indicated that none of the trials unduly influenced the pooled estimate. Visual inspection of the funnel plot did not reveal asymmetry (Supplementary Figure 2) and the estimate does not change despite almost reaching significance. Additionally, the LFK index was 0.649 and indicated no asymmetry. The heterogeneity was moderate (I2 = 65%, p < 0.001), which may be explained partially by sample population differences. However, sub-group analysis did not reveal any effects of age, sex, cardiometabolic status (CMD), or sitting duration on the pooled estimate (Figure 2).
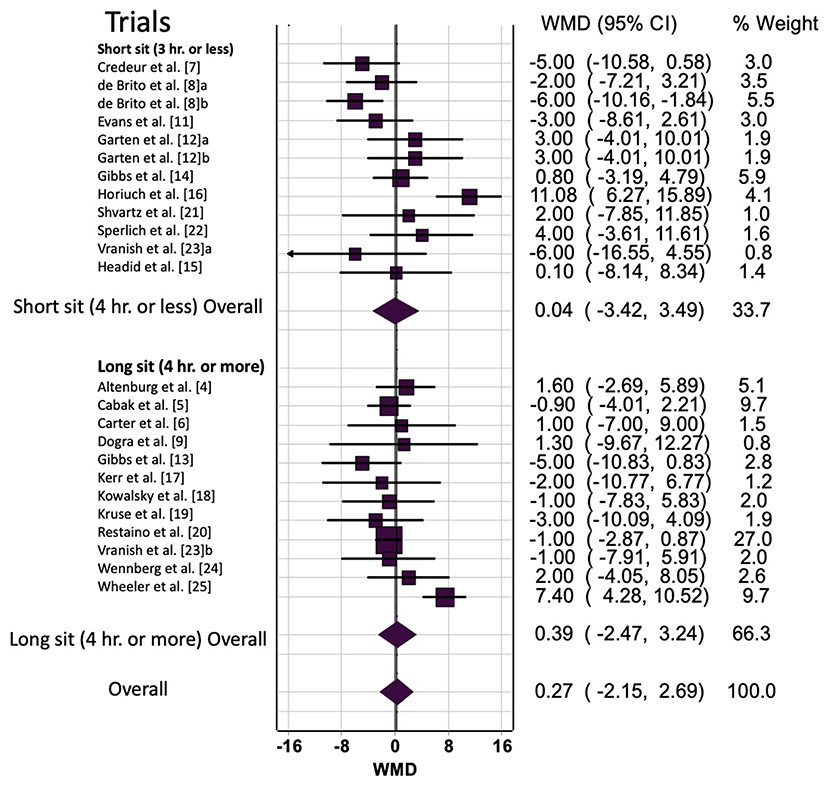
Figure 2. Prolonged sitting bout duration (short vs. long) effect on heart rate. a/b, multiple trials within the same study; hr, hours; WMD, weighted mean difference; BPM, beats per minute; CI, confidence interval.
Prolonged Sitting With Interruption: Heart Rate
Overall and sub-group analyses are reported in Table 3 and Figure 2 displays the forest plot for trials grouped by <4 or >4 h. Across all trials prolonged sitting with interruption resulted in a small non-significant increase in HR (WMD = 4 bpm, 95% CI: 0, 7, p = 0.02). Sensitivity analysis indicated that none of the trials unduly influenced the pooled estimate. Visual inspection of the funnel plot revealed asymmetry (Supplementary Figure 2), which was supported by the LFK index −2.78 of (major asymmetry). The trim and fill analysis decreased the WMD to 2 bpm (95% CI: 0, 5) (Supplementary Figure 2). Additionally, the heterogeneity was considerable (I2 = 73%, p < 0.001), which may be explained by variation in the strategy for interrupting prolonged sitting, age or biological sex differences, or prolonged sitting duration variation between studies.
When the populations were grouped by age, there was a non-significant moderate increase in HR for those aged >40 years (WMD = 5 bpm, SMD = 0.56, p = 0.060) and a negligible change for those aged under <40 years (WMD = 1 bpm, SMD = 0.03, p = 0.717). For women, there was a moderate increase in HR (WMD =7 bpm, SMD = 0.69, p = 0.007) but non-significant change for men (p = 0.585) and mixed sex (p = 0.088). For populations without CMDs, there was a moderate increase in HR (WMD = 6 bpm, SMD = 0.60, p = 0.008), and, for populations with CMDs, there was a non-significant change (p = 1.000). When the sitting bout length was >4 h, there was a moderate increase in HR (WMD = 5 bpm, SMD = 0.48, p = 0.007), and when the bout was <4 h there was a small, non-significant (p = 1.000) change. Last, there was a moderate increase in HR for walking-based interruptions (WMD = 7 bpm, SMD = 0.70, p = 0.001), but non-significant changes for standing (p = 1.000) or other (p = 0.339) interruptions.
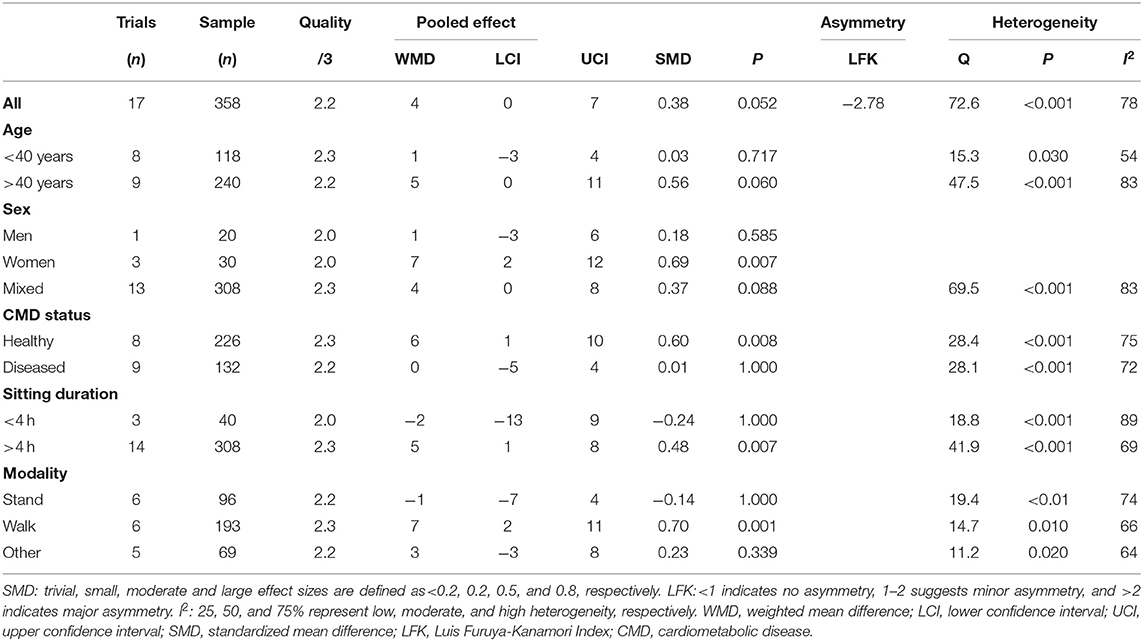
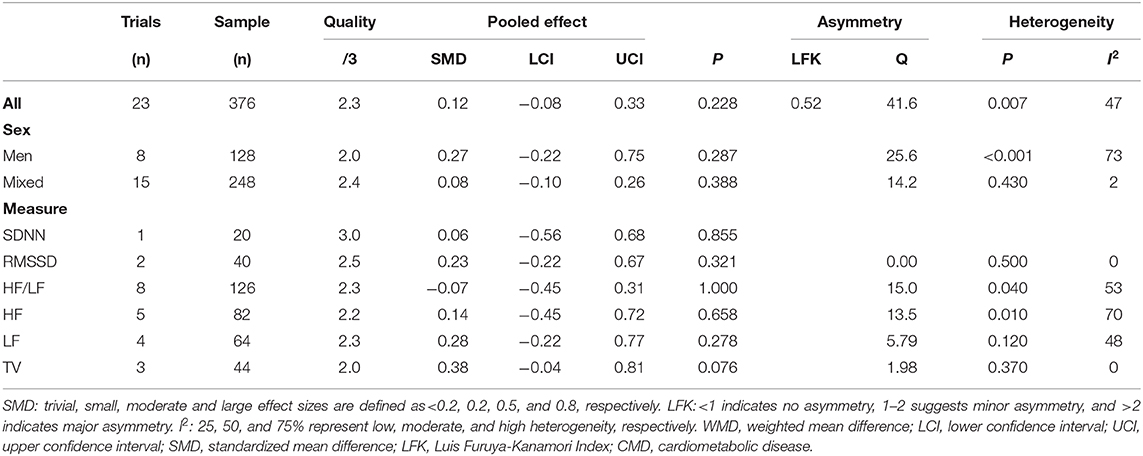
Prolonged Sitting: Heart Rate Variability
Overall and sub-group analyses are reported in Table 4 and Figure 3 displays the forest plot for trails grouped by HRV outcome type. Prolonged sitting resulted in a trivial, non-significant change in HRV of SMD = 0.12 with p = 0.228. Sensitivity analysis indicated that none of the trials unduly influenced the pooled estimate. Visual inspection of the funnel plot did not reveal asymmetry, which was confirmed by the LFK index of 0.52. The was moderate heterogeneity (I2 = 50%, p < 0.001), which was potentially explained by the differences in biological sex differences or the use of different HRV outcomes. When the populations were grouped by sex for sub-group analysis, there were negligible-small, non-significant changes in HRV for men (SMD = 0.27, p = 0.287) and mixed-sex (SMD = 0.06, p = 0.388). When the trials were grouped by HRV outcome type, there were negligible-small and non-significant changes for out outcomes (SMD = 0.06–0.38, p = 0.076–1.000).
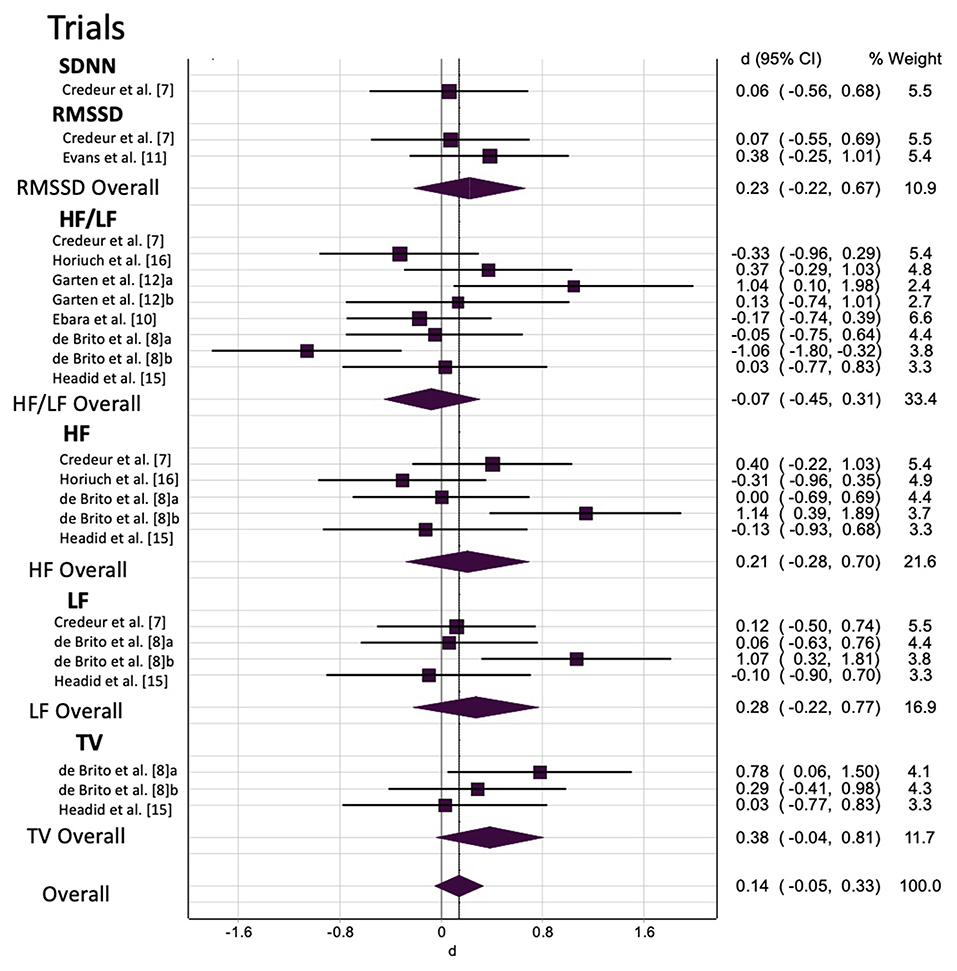
Figure 3. The effect of prolonged sitting on heart rate variability by outcome measure. a/b, multiple trials within the same study; SDNN, standard deviation of NN intervals; RMSSD, root mean of successive difference; HF, high frequency; LF, low frequency; HF/LF, high frequency/low frequency ratio; TV, total variance; WMD, weighted mean difference; CI, confidence interval.
We attempted to account multiple HRV estimates (RMSSD, SDNN, HF, LF, HF/LF, TV) within a single trial by using two approaches: (i) sub-group analysis by HRV estimate (e.g., a given study may include both RMSSD and HF) as reported in the previous paragraph; and (ii) a multi-level meta-analysis model. The findings were consistent when we examined the data with the multi-level model, which revelated that all the heterogeneity was at level 1, suggesting our first approach was robust.
Discussion
The aim of this meta-analysis was to synthesize the existing literature investigating the effects of acute exposure to prolonged sitting, with and without sitting interruptions, on HR and HRV. The main findings were that prolonged sitting without interruption does not significantly affect HR or HRV. Interrupting prolonged sitting with walking increased HR while standing or other (strength training, calf-raises, or biking) interruption modalities had trivial-small, non-significant effects, respectively. There were not enough HRV studies with an interruption condition to examine HRV response to interrupting prolonged sitting.
Limitations
Several limitations should be borne in mind when considering these findings. First, the sample size of included trials was small, with a limited number of trials reporting HRV (n = 7). The trials that reported HRV utilized different HRV assessment methodology and reported a variety of outcomes, resulting in different units of frequency and time components. This was addressed by standardizing the unit of measure and by performing sub-group analysis by HRV assessment type (i.e., SDNN, RMSSD, HF/LF, HF, LF, or TV) and conducting a multi-level analysis. Second, the small number of HRV trials limits the conclusions drawn from the sub-group analysis. We were unable to investigate the effect of interrupting prolonged sitting on HRV as only two HRV trials reported interruption conditions. It should be noted that we attempted to perform an additional sub-group analysis of age using study population recruitment criteria (for example: 25–65 years old) instead of average age because mean age includes a large age range. However, this was not possible as only a few studies reported recruitment criteria. Lastly, the majority of the HRV trials were mixed sex, and it remains unclear whether both sexes respond similarly.
Uninterrupted Prolonged Sitting: HR and HRV
Overall, there was a non-significant effect of acute exposure to prolonged sitting on HR and HRV. We speculated that HR would increase in response to prolonged sitting, and that greater increases would be observed in older aged or CMD populations compared to young and/or healthy populations. Additionally, we believed that HRV would decrease following acute prolonged sitting, again with more pronounced adverse effects in older and CMD participants (compared to younger and healthy participants). Our hypothesized mechanism proposed that blood pooling in the lower extremities as a consequence of prolonged sitting (Dempsey et al., 2018) would then lead to a reduction in venous return (decrease in stroke volume and cardiac output) (Thosar et al., 2012; De Brito et al., 2015; Credeur et al., 2019). Baroreceptors would then signal on afferent pathways to cardiovascular centers in the medulla, triggering a decrease in parasympathetic activation along with an increase in sympathetic activation to the heart and vessels (Shaffer et al., 2014). Thus, following, we would expect an increase in HR and a decrease in HRV. By way of explanation for the lack of support for this effect in this meta-analysis, it is possible that the balance between parasympathetic and sympathetic activity is unchanged with acute prolonged sitting (Restaino et al., 2015) or that sympathetic stimulation may change independently to parasympathetic stimulation. Further studies are warranted which combined HRV with measures of SNS activity, perhaps including muscle sympathetic nerve activity, galvanic skin sensors, or pupil dilation, to explore these potentially complex cardio-autonomic responses.
Interrupting Prolonged Sitting: HR
Prolonged sitting with interruption approached statistical significance and resulted in a small increase in HR (WMD = 4 bpm). An increase in HR with interruption was expected and represents an increased metabolic demand following muscle contractions. Sub-group analyses revealed moderate effects (increase) of sitting interruption on HR in healthy populations (p = 0.008), for females (p = 0.007), and when interrupting longer bouts of sitting (p = 0.007). Additionally, walking as the interruption strategy resulted in the greatest and only significant increase in HR (p = 0.001), as compared to standing or other strategies. Since this meta-analysis measured the change in HR from before and after the sitting bout with interruption conditions (and not immediately after the interruption), we can speculate that an increase in HR is a result of the cardio-autonomic system acclimating to the lack of increase in blood pooling, therefore preserving stroke volume in order to maintain venous return. The aforementioned mechanism may also explain the lack of effect of sitting interruptions on HR in populations with CMDs. That is, in populations with CMD, sitting interruptions may be ineffective at preventing blood pooling in the lower extremities – at least with the strategies that have been trialed thus far. Additionally, the increase in HR for female populations is potentially indictive of the protective effect of estrogen receptors in the endothelium. The 17 β-estradiol (E2) receptor increases the production of nitric oxide (vasodilator) in endothelium and preserve healthy endothelial function (Wheeler et al., 2019). The presence of E2 in women may be responsible for our ability to detect the increase in HR following interruption at the post-prolonged sitting bout measure because the physiologic effect (increase in HR) of the interruption may last longer in women due to superior endothelial function compared to men (Chowienczyk et al., 1994).
It should be acknowledged that HR and HRV do not provide a comprehensive insight into the influence of interrupting prolonged sitting on the cardio-autonomic system. Studies examining both parasympathetic and sympathetic nervous system activity are needed to better understand the role the autonomic nervous system plays in the mechanisms involved in uninterrupted prolonged sitting which contribute to CVD risk. Future studies should consider measuring muscle sympathetic nervous activity or use of galvanic skin sensors, as well as the use of rate pressure product to determine myocardial load, which would provide us with additional knowledge about whether the HR response is protective or not. Additionally, consideration should be given to heart rate rhythm complexity, which measures the complexity of the total cardiovascular system rather than a sub-component univariate variable (i.e., HRV) alone (Cheng-Hsuan et al., 2020). Finally, investigators should keep in mind that there was variation in frequency, duration, and type of interruption strategy as well as when HR was measured (i.e., before, after, or during interruption) in the current literature. Standardizing guidelines or direct, within-study comparisons of prolonged sitting interruption strategies may yield more meaningful results.
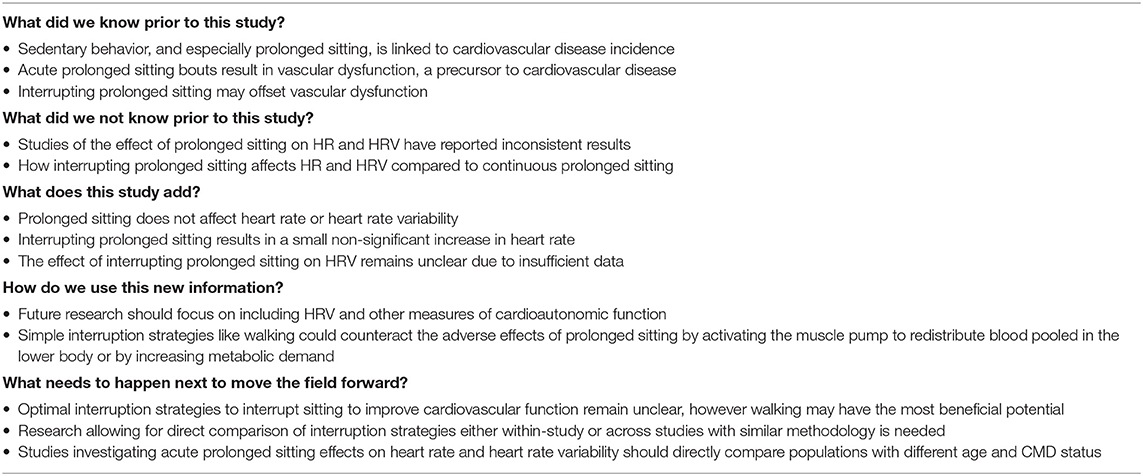
Implications
This meta-analysis is the first to our knowledge to consolidate the existing literature in this area in hope to investigate potentially deleterious effects of prolonged sitting. Such investigations on this and other outcomes are crucial for informing sedentary behavior intervention strategies, including optimization of interruption (i.e., frequency, intensity, and timing). Our findings are summarized in Table 5. The data indicates that a prolonged sitting bout (>1 h) resulted in trivial and non-significant increases in HR and HRV. However, interrupting sitting resulted in a small increase in HR especially apparent in healthy female populations. Current data suggests walking may be the optimum sitting interruption strategy. In the future, prolonged sitting studies should include additional measures of the cardio-autonomic system in order to better understand autonomic balance.
There are important gaps in the current literature which were identified. For example, due to the low number of included trails which investigated the effect of interrupting sitting on HRV, the current meta-analysis was unable to draw any firm conclusions. Additionally, the wide variety in sitting interruption strategies make it difficult to determine the optimal prescription for sedentary behavior guidelines. Thus, direct within-study comparisons of interruption strategies as well as standardized frequency, intensity, and duration guidelines for prolonged sitting interruptions across studies that facilitate comparisons may result in a better understanding of the cardio-autonomic mechanisms contributing to the CVD risk associated with sedentary behavior. It is also worth noting that, like exercise guidelines, sedentary behavior guidelines should consider whether specific guidelines are required for special populations, including those with CMDs or disabilities.
Conclusion
Sedentary behaviors, like prolonged sitting, are associated with CVD incidence and mortality. This meta-analysis consolidated the existing literature on the effects of prolonged sitting, with and without interruption, on HR and HRV. Furthermore, gaps in the existing literature were identified in order to better inform investigators in establishing the optimum guidelines to mitigate prolonged sitting. The results of this analysis suggest that there are not meaningful changes in HR or HRV during uninterrupted sitting bouts (>1 h). Interrupting sitting resulted in a non-significant increase in HR, which may be indicative of the increase in metabolic demand. Future research is needed in order to optimize interruption strategies including frequency, duration, and intensity and more sitting interruption studies investigating HRV are needed to better inform sedentary behavior guidelines.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
LB, AA, BG, and LS: conceptualization, methodology, and formal analysis and investigation. LB and LS: writing - original draft preparation. All authors: writing - review and editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2021.664628/full#supplementary-material
References
Altenburg, T. M., Rotteveel, J., Serné, E. H., and Chinapaw, M. J. M. (2019). Standing is not enough: a randomized crossover study on the acute cardiometabolic effects of variations in sitting in healthy young men. J. Sci. Med. Sport 22, 790–796. doi: 10.1016/j.jsams.2018.12.016
Assink, M., and Wibbelink, C. J. M. (2016). Fitting three-level meta-analytic models in R: a step-by-step tutorial. Quan. Methods Psychol. 12, 154–174. doi: 10.20982/tqmp.12.3.p154
Barendregt, J. J., and Doi, S. (2015). MetaXL User Guide, Queensland: EpiGear International Pty Ltd, 1–52.
Barone Gibbs, B., Kowalsky, R. J., Perdomo, S. J., Grier, M., and Jakicic, J. M. (2017a). Energy expenditure of deskwork when sitting, standing or alternating positions. Occupat. Med. 67, 121–127. doi: 10.1093/occmed/kqw115
Barone Gibbs, B., Kowalsky, R. J., Perdomo, S. J., Taormina, J. M., Balzer, J. R., and Jakicic, J. M. (2017b). Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J. Hypertens. 35, 2411–2418. doi: 10.1097/HJH.0000000000001463
Biswas, A., Oh, P. I., Faulkner, G. E., Bajaj, R. R., Silver, M. A., Mitchell, M. S., et al. (2015). Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults. Ann. Intern. Med. 162, 123–132. doi: 10.7326/M14-1651
Botter, J., Ellegast, R. P., Burford, E.-M., Weber, B., Könemann, R., and Commissaris, D. A. C. M. (2016). Comparison of the postural and physiological effects of two dynamic workstations to conventional sitting and standing workstations. Ergonomics 59, 449–463. doi: 10.1080/00140139.2015.1080861
Bourdin, G., Barbier, J., Burlem, J.-F., Durante, G., Passant, S., Vincent, B., et al. (2010). The feasibility of early physical activity in intensive care unit patients: a prospective observational one-center study. Res. Care 55, 400–407.
Cabak, A., Mikicin, M., Łyp, M., Stanisławska, I., Kaczor, R., and Tomaszewski, W. (2017). “Preventive chair massage with algometry to maintain psychosomatic balance in white-collar workers,” in Clinical Management of Pulmonary Disorders and Diseases, ed M. Pokorski (Cham: Springer), 77–84. doi: 10.1007/5584_2017_45
Carter, S. E., Draijer, R., Holder, S. M., Brown, L., Thijssen, D. H. J., and Hopkins, N. D. (2018). Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J. Appl. Physiol. 125, 790–798. doi: 10.1152/japplphysiol.00310.2018
Chaput, J.-P., and Tremblay, A. (2007). Acute effects of knowledge-based work on feeding behavior and energy intake. Physiol. Behav. 90, 66–72. doi: 10.1016/j.physbeh.2006.08.030
Cheng-Hsuan, T., Jenq-Wen, H., Chen, L., Hsi-Pin, M., Men-Tzung, L., Daisy, L. L., et al. (2020). Heart rhythm complexity predicts long-term cardiovascular outcomes in peritoneal dialysis patients: a prospective cohort study. J. Am. Heart Assoc. 9:e013036. doi: 10.1161/JAHA.119.013036
Cheung, M. W. L. (2019). A guide to conducting a meta-analysis with non-independent effect sizes. Neuropsychol. Rev. 29, 387–396. doi: 10.1007/s11065-019-09415-6
Chowienczyk, P. J., Cockcroft, J. R., Brett, S. E., Ritter, J. M., and Watts, G. F. (1994). Sex differences in endothelial function in normal and hypercholesterolaemic subjects. Lancet 344, 305–306. doi: 10.1016/S0140-6736(94)91342-0
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences. 2nd Edn. Hillsdale, NJ: Erlbaum.
Credeur, D. P., Miller, S. M., Jones, R., Stoner, L., Dolbow, D. R., Fryer, S. M., et al. (2019). Impact of prolonged sitting on peripheral and central vascular health. Am. J. Cardiol. 123, 260–266. doi: 10.1016/j.amjcard.2018.10.014
Crespo, N. C., Mullane, S. L., Zeigler, Z. S., Buman, M. P., and Gaesser, G. A. (2016). Effects of standing and light-intensity walking and cycling on 24-h glucose. Med. Sci. Sports Exerc. 48, 2503–2511. doi: 10.1249/MSS.0000000000001062
De Brito, L. C., Rezende, R. A., Da Silva, N. D., Tinucci, T., Casarini, D. E., Cipolla-Neto, J., et al. (2015). Post-exercise hypotension and its mechanisms differ after morning and evening exercise: a randomized crossover study. PLoS ONE 10:e0132458. doi: 10.1371/journal.pone.0132458
Dempsey, P. C., Larsen, R. N., Dunstan, D. W., Owen, N., and Kingwell, B. A. (2018). Sitting less and moving more: implications for hypertension. Hypertension 72, 1037–1046. doi: 10.1161/HYPERTENSIONAHA.118.11190
Dogra, S., Wolf, M., Jeffrey, M. P., Foley, R. C. A., Logan-Sprenger, H., Jones-Taggart, H., et al. (2019). Disrupting prolonged sitting reduces IL-8 and lower leg swell in active young adults. BMC Sports Sci. Med. Rehabil. 11, 1–7. doi: 10.1186/s13102-019-0138-4
Doi, S. A. R., Barendregt, J. J., Khan, S., Thalib, L., and Williams, G. M. (2015a). Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemp. Clin. Trials 45, 130–138. doi: 10.1016/j.cct.2015.05.009
Doi, S. A. R., Barendregt, J. J., Khan, S., Thalib, L., and Williams, G. M. (2015b). Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp. Clin. Trials 45, 123–129. doi: 10.1016/j.cct.2015.05.010
Duval, S., and Tweedie, R. (2000). Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463. doi: 10.1111/j.0006-341X.2000.00455.x
Ebara, T., Kubo, T., Inoue, T., Murasaki, G. I., Takeyama, H., Sato, T., et al. (2008). Effects of adjustable sit-stand VDT workstations on workers' musculoskeletal discomfort, alertness and performance. Ind. Health 46, 497–505. doi: 10.2486/indhealth.46.497
Evans, W. S., Stoner, L., Willey, Q., Kelsch, E., Credeur, D. P., and Hanson, E. D. (2019). Local exercise does not prevent the aortic stiffening response to acute prolonged sitting: a randomized crossover trial. J. Appl. Physiol. 127, 781–787. doi: 10.1152/japplphysiol.00318.2019
Furuya-Kanamori, L., Barendregt, J. J., and Doi, S. A. R. (2018). A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthcare 16, 195–203. doi: 10.1097/XEB.0000000000000141
Garten, R. S., Hogwood, A. C., Weggen, J. B., Fralin, R. C., LaRosa, K., Lee, D., et al. (2018). Aerobic training status does not attenuate prolonged sitting-induced lower limb vascular dysfunction. Appl. Physiol. Nutr. Metab. 44, 425–433. doi: 10.1139/apnm-2018-0420
Headid, R. J., Pekas, E. J., Wooden, T. S. K., Son, W. M., Layec, G., Shin, J., et al. (2020). Impacts of prolonged sitting with mild hypercapnia on vascular and autonomic function in healthy recreationally active adults. Am. J. Physiol. Heart Circ. Physiol. 319, H468–H480. doi: 10.1152/ajpheart.00354.2020
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi: 10.1136/bmj.d5928
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al. (2019). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley and Sons. doi: 10.1002/9781119536604
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. Bmj 327, 557–560. doi: 10.1136/bmj.327.7414.557
Horiuchi, M., Takiguchi, C., Kirihara, Y., and Horiuchi, Y. (2018). Impact of wearing graduated compression stockings on psychological and physiological responses during prolonged sitting. Int. J. Environ. Res. Public Health 15:1710. doi: 10.3390/ijerph15081710
Jean-François, A., Coralie, F., Audrey, B.-G., Julie, F., Henrik, L., Françoise, L., et al. (2010). Estrogen receptors and endothelium. Arterioscler. Thromb. Vasc. Biol. 30, 1506–1512. doi: 10.1161/ATVBAHA.109.191221
Kerr, J., Crist, K., Vital, D. G., Dillon, L., Aden, S. A., Trivedi, M., et al. (2017). Acute glucoregulatory and vascular outcomes of three strategies for interrupting prolonged sitting time in postmenopausal women: a pilot, laboratory-based, randomized, controlled, 4-condition, 4-period crossover trial. PLoS ONE 12:0188544. doi: 10.1371/journal.pone.0188544
Kowalsky, R. J., Jakicic, J. M., Hergenroeder, A., Rogers, R. J., and Gibbs, B. B. (2019). Acute cardiometabolic effects of interrupting sitting with resistance exercise breaks. Appl. Physiol. Nutr. Metab. 44, 1025–1032. doi: 10.1139/apnm-2018-0633
Kruse, N. T., Hughes, W. E., Benzo, R. M., Carr, L. J., and Casey, D. P. (2018). Workplace strategies to prevent sitting-induced endothelial dysfunction. Med. Sci. Sports Exerc. 50, 801–808. doi: 10.1249/MSS.0000000000001484
Larsen, R. N., Kingwell, B. A., Sethi, P., Cerin, E., Owen, N., and Dunstan, D. W. (2014). Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr. Metab. Cardiovasc. Dis. 24, 976–982. doi: 10.1016/j.numecd.2014.04.011
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D., Antes, G., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:1000097. doi: 10.1371/journal.pmed.1000097
Paterson, C., Fryer, S., Zieff, G., Stone, K., Credeur, D. P., Barone Gibbs, B., et al. (2020). The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: a meta-analysis. Sports Med 50, 1929–1942. doi: 10.1007/s40279-020-01325-5
Peddie, M. C., Bone, J. L., Rehrer, N. J., Skeaff, C. M., Gray, A. R., and Perry, T. L. (2013). Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am. J. Clin. Nutr. 98, 358–366. doi: 10.3945/ajcn.112.051763
Restaino, R. M., Holwerda, S. W., Credeur, D. P., Fadel, P. J., and Padilla, J. (2015). Impact of prolonged sitting on lower and upper limb micro- and macrovascular dilator function. Exp. Physiol. 100, 829–838. doi: 10.1113/EP085238
Sakowski, C., Starc, V., Smith, S. M., and Schlegel, T. T. (2011). Sedentary long-duration head-down bed rest and ECG repolarization heterogeneity. Aviat. Space. Environ. Med. 82, 416–423. doi: 10.3357/ASEM.2945.2011
Shaffer, F., McCraty, R., and Zerr, C. L. (2014). A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front. Psychology 5:1040. doi: 10.3389/fpsyg.2014.01040
Shvartz, E., Gaume, J. G., White, R. T., and Reibold, R. C. (1983). Hemodynamic responses during prolonged sitting. J. Appl. Physiol. 54, 1673–1680. doi: 10.1152/jappl.1983.54.6.1673
Snarr, R. L., Langford, E. L., Ryan, G. A., and Wilhoite, S. (2019). Cardiovascular and metabolic responses of active sitting while performing work-related tasks. Ergonomics 62, 1227–1233. doi: 10.1080/00140139.2019.1633476
Sperlich, B., De Clerck, I., Zinner, C., Holmberg, H. C., and Wallmann-Sperlich, B. (2018). Prolonged sitting interrupted by 6-min of high-intensity exercise: circulatory, metabolic, hormonal, thermal, cognitive, and perceptual responses. Front. Physiol. 9:1279. doi: 10.3389/fphys.2018.01279
Sterne, J. A. C., Sutton, A. J., Ioannidis, J. P. A., Terrin, N., Jones, D. R., Lau, J., et al. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343, 1–8. doi: 10.1136/bmj.d4002
Thosar, S. S., Johnson, B. D., Johnston, J. D., and Wallace, J. P. (2012). Sitting and endothelial dysfunction: the role of shear stress. Med. Sci. Monitor 18, RA173–RA180. doi: 10.12659/MSM.883589
Tremblay, M. S., Aubert, S., Barnes, J. D., Saunders, T. J., Carson, V., Latimer-Cheung, A. E., et al. (2017). Sedentary behavior research network (sbrn) – terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Activ. 14:75. doi: 10.1186/s12966-017-0525-8
Vranish, J. R., Young, B. E., Kaur, J., Patik, J. C., Padilla, J., and Fadel, P. J. (2017). Influence of sex on microvascular and macrovascular responses to prolonged sitting. Am. J. Physiol. 312, H800–H805. doi: 10.1152/ajpheart.00823.2016
Wennberg, P., Boraxbekk, C. J., Wheeler, M., Howard, B., Dempsey, P. C., Lambert, G., et al. (2016). Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open 6, 1–9. doi: 10.1136/bmjopen-2015-009630
Wheeler, M. J., Dunstan, D. W., Ellis, K. A., Cerin, E., Phillips, S., Lambert, G., et al. (2019). Effect of morning exercise with or without breaks in prolonged sitting on blood pressure in older overweight/obese adults: evidence for sex differences. Hypertension 73, 859–867. doi: 10.1161/HYPERTENSIONAHA.118.12373
Keywords: heart rate, heart rate variability, prolonged sitting, interrupting prolonged sitting, cardioautonomic function
Citation: Bates LC, Alansare A, Gibbs BB, Hanson ED and Stoner L (2021) Effects of Acute Prolonged Sitting and Interrupting Prolonged Sitting on Heart Rate Variability and Heart Rate in Adults: A Meta-Analysis. Front. Physiol. 12:664628. doi: 10.3389/fphys.2021.664628
Received: 05 February 2021; Accepted: 06 April 2021;
Published: 03 May 2021.
Edited by:
Giuseppe De Vito, University of Padua, ItalyReviewed by:
Gavin W. Lambert, Swinburne University of Technology, AustraliaEric Goulet, Université de Sherbrooke, Canada
Copyright © 2021 Bates, Alansare, Gibbs, Hanson and Stoner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lauren C. Bates, bGJhdGVzMTVAbGl2ZS51bmMuZWR1
 Lauren C. Bates
Lauren C. Bates Abdullah Alansare
Abdullah Alansare Bethany Barone Gibbs
Bethany Barone Gibbs Erik D. Hanson
Erik D. Hanson Lee Stoner
Lee Stoner