
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Physiol., 17 December 2020
Sec. Clinical and Translational Physiology
Volume 11 - 2020 | https://doi.org/10.3389/fphys.2020.617845
 Hongyang Xie1,2†
Hongyang Xie1,2† Yaqiong Wang3†
Yaqiong Wang3† Tianqi Zhu1†
Tianqi Zhu1† Shuo Feng1†
Shuo Feng1† Zijun Yan1†
Zijun Yan1† Zhengbin Zhu1
Zhengbin Zhu1 Jingwei Ni1
Jingwei Ni1 Jun Ni1
Jun Ni1 Run Du1
Run Du1 Jinzhou Zhu1
Jinzhou Zhu1 Fenghua Ding1
Fenghua Ding1 Shengjun Liu1
Shengjun Liu1 Hui Han1
Hui Han1 Hang Zhang1
Hang Zhang1 Jiaxin Zhao1
Jiaxin Zhao1 Ruiyan Zhang1*
Ruiyan Zhang1* Weiwei Quan1*
Weiwei Quan1* Xiaoxiang Yan1,2*
Xiaoxiang Yan1,2*Background: Mitsugumin 53 or Tripartite motif 72 (MG53/TRIM72), a myokine/cardiokine belonging to the tripartite motif family, can protect the heart from ischemic injury and regulate lipid metabolism in rodents. However, its biological function in humans remains unclear. This study sought to investigate the relationship between circulating MG53 levels and coronary artery disease (CAD).
Methods: The concentration of MG53 was measured by enzyme-linked immunosorbent assay (ELISA) in serum samples from 639 patients who underwent angiography, including 205 controls, 222 patients with stable CAD, and 212 patients with acute myocardial infarction (AMI). Logistic and linear regression analyses were used to analyze the relationship between MG53 and CAD.
Results: MG53 levels were increased in patients with stable CAD and were highest in patients with AMI. Additionally, patients with comorbidities, such as chronic kidney disease (CKD) and diabetes also had a higher concentration of MG53. We found that MG53 is a significant diagnostic marker of CAD and AMI, as analyzed by logistic regression models. Multivariate linear regression models revealed that serum MG53 was significantly corelated positively with SYNTAX scores. Global Registry of Acute Coronary Events (GRACE) scores also correlated with serum MG53 levels, indicating that MG53 levels were associated with the severity of CAD and AMI after adjusting for multiple risk factors and clinical biomarkers.
Conclusion: MG53 is a valuable diagnostic marker whose serum levels correlate with the presence and severity of stable CAD and AMI, and may represent a novel biomarker for diagnosing CAD and indicating the severity of CAD.
Cardiovascular disease (CVD) is one of the most common causes of mortality and morbidity worldwide (Lu et al., 2012). It has been estimated that more than 23.3 million people will die every year from cardiovascular diseases by the year 2030 (Mathers and Loncar, 2006). Coronary artery disease (CAD), and one of its most severe complications, acute myocardial infarction (AMI), are major subsets of CVD. Stable CAD (sCAD) and AMI have the same pathological background, although there are conspicuous differences in their pathogenesis and symptoms (Agewall, 2008; Libby, 2013). Atherosclerosis is a potential cause of CAD. Stable CAD refers to patients with progressive atherosclerotic plaques in coronary vessels whose clinical symptoms are stable on treatment. The diagnosis of stable CAD is generally based on symptoms or invasively angiography findings. However, these examinations are affected by the influence and bias of the performer, and are associated with some complications (Newby et al., 2012). Assay of cardiac biomarkers using conventional diagnostic methods to predict CAD events does not meet the requirements of sensitivity and specificity (Morse, 2015).
Stable plaques can evolve into unstable vulnerable plaques, which are prone to rupture and thrombosis, and may finally lead to acute myocardial infarction in conditions, such as ischemic cardiomyopathy. AMI can cause cardiac rupture, lethal arrhythmia, and heart failure (Negre-Salvayre et al., 2017). Although AMI can be successfully diagnosed using biomarkers, such as cardiac troponin and creatine kinase (CK), the usefulness of some of these conventional biomarkers in the acute stage of AMI are limited as they could have low concentrations at this stage (Suzuki et al., 2018). Hence, there is a persistent demand for biomarkers that can identify patients with AMI in the acute phase. Furthermore, the lack of protein-based biomarkers that can be used for risk stratification, is also an unmet need that could have increased the ability of biomarkers to identify patients with higher risk of adverse outcomes.
Mitsugumin 53 (MG53, also known as TRIM72) is a tripartite motif protein that was first identified in an immuno-proteomic library aimed at discovering proteins that correlated with myogenesis, ion channel, and muscle integrity (Rudnicki et al., 2008; Weisleder et al., 2008). It belongs to the TRIM family, which plays a key role in a large range of biochemical activities such as cell proliferation, differentiation, and immune response (Ozato et al., 2008; Doyle et al., 2010; Hatakeyama, 2011). The biological function of MG53 was first reported by Cai et al. (2009). It was identified as a crucial component of the plasma membrane repair process (Cai et al., 2009). Previous studies have demonstrated that MG53 can increase lipid accumulation in the cardiovascular system by affecting glucose uptake (Liu et al., 2015a). Furthermore, MG53 can also protect the heart against ischemia-reperfusion injury (Liu et al., 2015b). Increasing extracellular MG53 levels also plays an important role in facilitating cardiac oxidative injury (Cao et al., 2010). Other recent studies also show that serum MG53 levels are increased in patients with type 2 diabetes mellitus (Wu et al., 2019).
However, most studies on the pathophysiologic function of MG53 in cardiovascular disease have been performed in animal models. The roles and clinical significance of MG53 in humans with CAD or AMI are not well established. Therefore, in this study, we aimed to determine the clinical value of MG53 in patients with stable CAD and AMI.
A total of 639 consecutive patients with suspected CAD who underwent coronary artery angiography in our facility, were included in this study. The patients comprised 222 patients with chronic stable coronary disease (CAD group), 212 patients with acute myocardial infarction (AMI group), and 205 patients without coronary artery stenosis who were included in the control group (Con group).
The CAD was defined as coronary stenosis of ≥50% in the left main coronary artery or ≥75% in at least one of the major epicardial arteries (Scanlon et al., 1999), while AMI were defined as ST segment elevation or non-ST segment elevation myocardial infarction in accordance with International guidelines (Thygesen et al., 2012). Patients with a history of events suggestive of acute myocardial infarction within 4 weeks were excluded from this study. Other exclusion criteria included severe diseases such as tumors, serious infections, autoimmune diseases, and other physical disabilities. All enrolled patients were ≥18 years old. The study was approved by the Institutional Review Board of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. Each subject provided written informed consent before enrollment. The study protocol of this study conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Blood samples were taken from the radial artery before angiography, and then whole blood was centrifuged at 2000 rpm for 15–20 min to acquire serum. After centrifugation, serum samples were immediately frozen at −80°C for further analysis. The concentration of MG53 was measured using Human-MG53 ELISA kits (Cat# CSB-EL024511HU) from Flarebio Biotech. All samples were tested by scientists that were blinded to the patients’ information.
The patients information including medical history and physical examination data were collected via face-to-face interviews. Echocardiography was performed by the same investigator during hospital admission, and the left ventricular end systolic diameter (LVESD), left ventricular end diastolic diameter (LVEDD), and left atrial diameter (LAD) were measured. The left ventricular ejection fraction (LVEF) was calculated using the Simpson method.
SYNTAX scores were calculated using the SYNTAX score calculator (available at www.syntaxscore.com) before the first PCI. The GRACE score was calculated using the GRACE score calculator website1 during hospital admission.
Continuous variables with normal distribution were reported as mean ± standard deviation (SD), whereas skewed distributed variables were expressed as medians ± quartiles. Categorical data were summarized as proportions with frequencies. Continuous variables were compared using one-way ANOVA test or Kruskal–Wallis tests where appropriate, while the chi-square test or Fisher’s exact test was used to analyze the differences in categorical variables. MG53 levels were log transformed or divided into tertiles for further analysis. Logistic regression analyses were used to ascertain the predictive value of MG53 level for the presence of sCAD in patients in the CAD group and those in the Con group, as well as the predictive value of MG53 level for the presence of AMI in patients with CAD and AMI. Linear regression models was used to evaluate the association between MG53 and SYNTAX scores. Statistical analyses were conducted using SPSS software (version 23.0; SPSS, Inc., Chicago, IL, United States). Statistical significance was considered as 2-tailed, with a p-value of <0.05.
All enrolled patients were categorized into three groups. Demographic and laboratory features of the patients are reported in Table 1. Compared with the patients in the control group, subjects from the CAD and AMI groups were males, older, and had a history of alcohol use. In addition, medical history including diabetes, dyslipidemia, and chronic kidney disease (CKD) were more frequent in the CAD and AMI groups than in the control group. The values of BMI, platelet, and hemoglobin were comparable among the three groups. Indicators reflecting renal function such as creatinine, cystatin C, and eGFR were higher in the AMI groups than in the other groups. Furthermore, levels of CRP, glucose, troponin I (cTnI), and left ventricular ejection fraction (LVEF) were also worse in the AMI group, indicating a poor general condition.
The serum concentration of MG53 was measured in all patients. MG53 levels were highest in patients in the AMI group. The MG53 levels in patients with stable CAD were compared to those of patients in the control group and the results are presented in Table 1 and Figure 1A. The differences of serum MG53 levels among three groups were similar to traditional markers such as CK-MB and cTnI to some extent (Supplementary Figures 1A,B). When stratified by age and gender in all subjects, the levels of MG53 were higher in patients over 65 years of age than in younger patients. However, there was no statistical significance in the serum concentration of MG53 between female and male patients (Figures 1B,C). However, MG53 levels in patients with comorbidities, such as CKD and diabetes, were significantly increased compared with those without previous such comorbidities (Figures 1D,E and Supplementary Figure 2). Furthermore, when these patients were grouped according to the New York Heart Association (NYHA) cardiac functional class, those in the fourth class showed significantly higher levels of MG53 (Figure 1F).
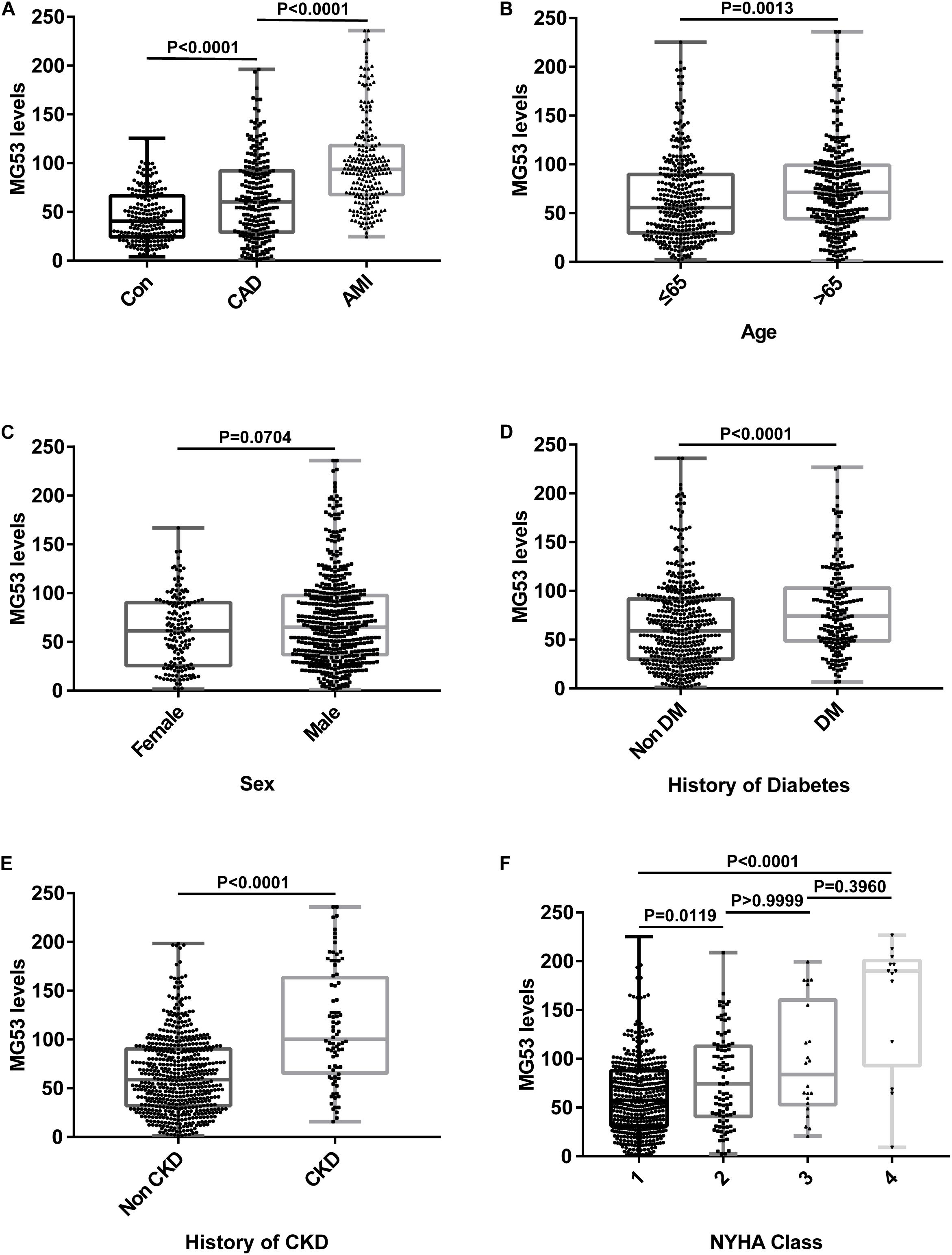
Figure 1. Concentration of serum MG53 in different groups. (A) Comparison of serum MG53 levels in patients with CAD, AMI, or negative coronary angiography. (B) Stratified analyses were performed by age (≤65 years/ > 65 years). (C) Stratified analyses were performed by gender (men/women). (D) Comparison of serum MG53 levels in patients with or without diabetes. (E) Comparison of serum MG53 levels in patients with or without CKD. (F) Serum mg53 levels were highest in patients with the 4th New York Heart Association (NYHA) functional class.
In order to clarify the diagnostic value of MG53 as a possible biomarker for stable CAD and AMI, we performed univariate and multivariate logistic regression analyses. As shown in Table 2, there was an independent correlation between log-transformed MG53 levels and increased risk for stable CAD in the CAD and control groups, when unadjusted and adjusted for age, sex, smoking, and medical history. To further demonstrate this relationship, we separated MG53 levels into three groups by tertiles. The tertiles of MG53 were also significantly related to the presence of CAD, even when adjusted for full models.
Univariate and multivariate logistic regression models also revealed an association between serum MG53 and the prevalence of AMI in patients in the CAD and AMI groups (Table 3). These values persisted after full adjustment, both in logarithmic form or divided into tertiles.
Linear regression analysis demonstrated that log MG53 levels significantly correlated positively with SYNTAX scores in the CAD group. This result indicated that MG53 correlated with the severity of CAD. The results of multivariate linear regression further proved this relationship after full adjustment. Similar values were also observed in patients with CAD and AMI (Table 4).
To verify the association between MG53 and the severity of AMI, The patients in the AMI group were divided into a high-risk group (>140), middle-risk group (109–140), and low-risk group (≤108) according to their GRACE scores. As shown in Figure 2, the serum levels of patients in the high-risk group were highest in the three groups, and the result was statistically comparable.
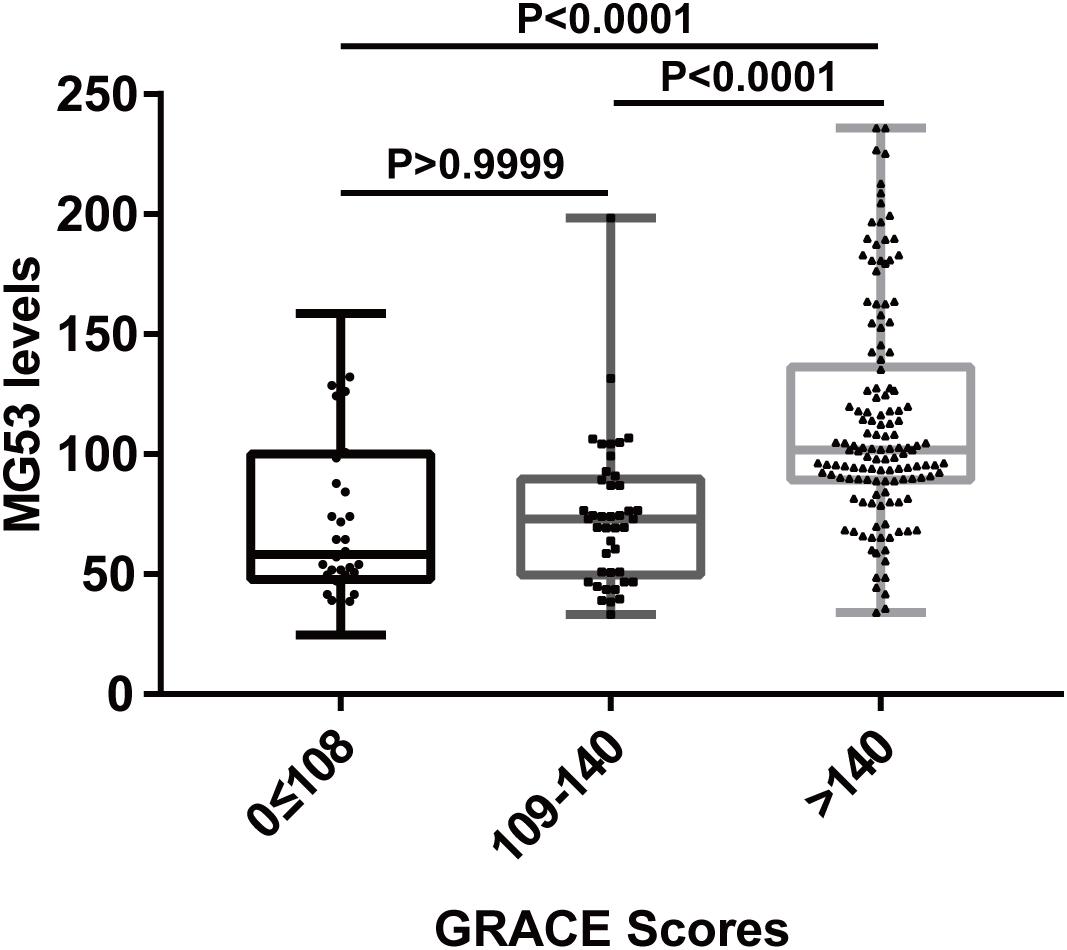
Figure 2. Serum MG53 levels in different groups stratified by GRACE score. The patients with AMI were divided into three groups according to their GRACE scores. Patients in the 3rd groups showed the highest MG53 level.
Our study has demonstrated for the first time that the serum concentration of MG53 does not only correlate with the presence of stable coronary artery disease but is also strongly associated with the prevalence of AMI in patients with CAD. Furthermore, we found that MG53 is an independent biomarker for the severity of stable CAD and AMI. We also observed that MG53 levels may be related to systemic disorders such as CKD and diabetes. To our knowledge, this is the first study on the correlation between MG53 and CAD in humans.
Coronary artery disease and its most serious complication, AMI, are major causes of morbidity and mortality worldwide (Lu et al., 2012), and both share a similar pathologic connection to atherosclerosis. While CAD is associated with lipid deposition and plaque formation, AMI is caused by atherosclerotic plaque rupture or thrombosis (Libby, 2013). The inflammatory response is an important driver of both CAD and AMI, and it is worse in the presence of factors, such as diabetes, dyslipidemia, smoking, and hypertension.
We found that serum levels of MG53 correlated with the presence of diabetes in control and CAD group. This observation is consistent with those of previous studies showing that MG53 levels could be increased in patients with obesity and type 2 diabetes (Wu et al., 2019). Wu et al. (2019), reported that in response to high serum glucose concentration, MG53 is secreted from skeletal and cardiac muscles as a secretory cytokine to regulate tissue insulin sensitivity and homeostasis. Secretory MG53 could bind to the insulin receptor and inhibit insulin signaling, while injection of exogenous MG53 can restore the insulin response. Moreover, circulating MG53 levels were also elevated in patients with CKD. Duann et al. (2015), found that MG53 is mainly expressed in the renal cortex, and downregulation of MG53 can significantly exaggerate kidney ischemic-reperfusion injury, highlighting the protective effect of MG53 in the kidneys.
The results of logistic and linear regression models demonstrated that MG53 is positively correlated with the presence and severity of stable CAD. Subjects with higher MG53 levels were more likely to have stable CAD and higher SYNTAX scores than those with low MG53 levels. In a previous study, it was reported that MG53 could aggravate lipid accumulation in the cardiovascular system (Liu et al., 2015a). Mechanistically, MG53 may impair lipid metabolism via the upregulated peroxisome proliferation-activated receptor-α (PPAR-α) signaling pathway and its downstream receptors (Liu et al., 2015a). Furthermore, genes associated with lipid metabolism are elevated in response to the overexpression of MG53 (Wang et al., 2010). These relationships could be observed in multiple animal models, suggesting that MG53 plays an important role in lipid uptake.
We also found that circulating MG53 levels were highest in patients with AMI. In addition, when the GRACE scores of AMI patients were divided into three groups, patients with higher GRACE scores had significantly elevated MG53 levels. These findings indicate that MG53 may also be related to the presence of AMI and its severity. These results are in line with those reported by Cao et al. (2010). In their study, found that MG53 was an important cardioprotective factor in cardiac ischemia-reperfusion injury. The protective effects of MG53 were attributed to the interaction with caveolin-3 (CaV3) and activation of pro-survival factors, which could facilitates ischemic preconditioning (IPC). Intracellular MG53 levels were decreased after ischemia reperfusion (I/R) injury. Injection of recombinant human-MG53 can protect hypoxic tissues against oxidative injury. More importantly, Liu et al. (2015b), reported that intravenous delivery of the recombinant MG53 could repair membrane damage to the ischemia-induced injury in porcine models. They also found that damaged myocardium could release abundant endogenous MG53 into circulation in rodent I/R models (Liu et al., 2015b). In addition, the circulating MG53 levels in mice with I/R injury correlated with the concentration of creatine kinase. More importantly, Dan et al. showed that IPC and oxidative stress could promoted MG53 secretion from perfused hearts in rodent (Shan et al., 2020). This effect was mediated by H2O2-induced PKC-δ phosphorylation at Y311. These studies may be involved in the association between elevated serum MG53 levels and AMI in humans.
Although Lemckert et al. (2016) study had reported there is very to no low level of MG53 expressed in human heart detected by western-blot. The studies of Dan et al. had proved that MG53 is present in human left ventricle tissue by using mass spectrometry analysis, and its abundance is about 1/10 of that of human skeletal muscle. They also demonstrated that MG53 could secreted from human ES cell-derived cardiomyocytes in response to low-dose H2O2 stimulation. Regardless of its low expression levels in cardiomyocytes, knockdown of MG53 with siRNA would aggravate oxidative stress injury of cardiomyocytes differentiated from human ES cells. These discrepancy between previous studies and present research might be attributed to different experimental method or differences in the antibodies used. In addition, the ages of human heart donors were various in their research. The biological functions of MG53 in human heart tissue need further fundamental research.
This study reveals that serum MG53 levels were significantly associated with the presence and severity of stable CAD and AMI. Thus, MG53 could be useful, novel biomarker for diagnosing CAD and AMI, and for identifying patients at higher risk of CAD.
First, the sample size was small, and this was a single-center study. The findings of this study need to be verified in multi-center studies with a large sample size. Second, we could not evaluate the causal relationship between MG53 levels and the presence of CAD and AMI because this was a cross-sectional study. Further studies involving following-up of patients with CAD in order to assess if they develop AMI in the future are required. Third, the ages of the different groups were comparable. Hence, age-matched groups need to be used in future studies. Finally, basic research tools such as immunohistochemistry and flow cytometry need to be performed to verify the role of MG53 in the cardiovascular system in humans. Furthermore, the identifying the underlying mechanism of action of MG53 in CVD is also necessary.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Review Board of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (2018-183). The patients/participants provided their written informed consent to participate in this study.
HYX, YQW, and SF collected and analyzed the data. ZJY performed the echocardiography. TQZ, ZBZ, JWN, JN, RD, JZZ, and FHD performed PCI and collected blood samples, HH, HZ, and JXZ performed the statistical analysis. XXY and HYX designed this study and wrote the manuscript. WWQ and RYZ made critical revisions of the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (81670457, 81922007, and 91939103 to XXY), Shanghai Municipal Education Commission–Gaofeng Clinical Medicine Grant Support (20191803 to XXY), Shanghai Science and Technology Supporting Project (19411963400 to XXY), and Natural Science Research Funding from Shanghai Jiao Tong University School of Medicine (19XJ11002 to XXY).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors gratefully acknowledge the collaboration of all the participants.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2020.617845/full#supplementary-material
Agewall, S. (2008). Acute and stable coronary heart disease: different risk factors. Eur. Heart J. 29, 1927–1929. doi: 10.1093/eurheartj/ehn321
Cai, C., Masumiya, H., Weisleder, N., Matsuda, N., Nishi, M., Hwang, M., et al. (2009). MG53 nucleates assembly of cell membrane repair machinery. Nat. Cell Biol. 11, 56–64. doi: 10.1016/j.bpj.2008.12.1824
Cao, C. M., Zhang, Y., Weisleder, N., Ferrante, C., Wang, X., Lv, F., et al. (2010). MG53 constitutes a primary determinant of cardiac ischemic preconditioning. Circulation 121, 2565–2574. doi: 10.1161/CIRCULATIONAHA.110.954628
Doyle, J. M., Gao, J., Wang, J., Yang, M., and Potts, P. R. (2010). MAGE-RING protein complexes comprise a family of E3 ubiquitin ligases. Mol. Cell 39, 963–974. doi: 10.1016/j.molcel.2010.08.029
Duann, P., Li, H., Lin, P., Tan, T., Wang, Z., Chen, K., et al. (2015). MG53-mediated cell membrane repair protects against acute kidney injury. Sci. Transl. Med. 7:279ra236. doi: 10.1126/scitranslmed.3010755
Lemckert, F. A., Bournazos, A., Eckert, D. M., Kenzler, M., Hawkes, J. M., Butler, T. L., et al. (2016). Lack of MG53 in human heart precludes utility as a biomarker of myocardial injury or endogenous cardioprotective factor. Cardiovasc. Res. 110, 178–187. doi: 10.1093/cvr/cvw017
Libby, P. (2013). Mechanisms of acute coronary syndromes and their implications for therapy. N. Engl. J. Med. 368, 2004–2013. doi: 10.1056/NEJMra1216063
Liu, F., Song, R., Feng, Y., Guo, J., Chen, Y., Zhang, Y., et al. (2015a). Upregulation of MG53 induces diabetic cardiomyopathy through transcriptional activation of peroxisome proliferation-activated receptor alpha. Circulation 131, 795–804. doi: 10.1161/CIRCULATIONAHA.114.012285
Liu, J., Zhu, H., Zheng, Y., Xu, Z., Li, L., Tan, T., et al. (2015b). Cardioprotection of recombinant human MG53 protein in a porcine model of ischemia and reperfusion injury. J. Mol. Cell Cardiol. 80, 10–19. doi: 10.1016/j.yjmcc.2014.12.010
Lu, X., Wang, L., Chen, S., He, L., Yang, X., Shi, Y., et al. (2012). Genome-wide association study in Han Chinese identifies four new susceptibility loci for coronary artery disease. Nat. Genet. 44, 890–894. doi: 10.1038/ng.2337
Mathers, C. D., and Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 3:e442. doi: 10.1371/journal.pmed.0030442
Morse, E. A. (2015). Nonobstructive coronary artery disease and risk of myocardial infarction. J. Emerg. Med. 48:401. doi: 10.1016/j.jemermed.2015.01.027
Negre-Salvayre, A., Auge, N., Camare, C., Bacchetti, T., Ferretti, G., and Salvayre, R. (2017). Dual signaling evoked by oxidized LDLs in vascular cells. Free Radic. Biol. Med. 106, 118–133. doi: 10.1016/j.freeradbiomed.2017.02.006
Newby, L. K., Jesse, R. L., Babb, J. D., Christenson, R. H., De Fer, T. M., Diamond, G. A., et al. (2012). ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on clinical expert consensus documents. J. Am. Coll. Cardiol. 60, 2427–2463. doi: 10.1016/j.jacc.2012.08.969
Ozato, K., Shin, D. M., Chang, T. H., and Morse, H. C. III (2008). TRIM family proteins and their emerging roles in innate immunity. Nat. Rev. Immunol. 8, 849–860. doi: 10.1038/nri2413
Rudnicki, M. A., Le Grand, F., McKinnell, I., and Kuang, S. (2008). The molecular regulation of muscle stem cell function. Cold Spring Harb. Symp. Quant. Biol. 73, 323–331. doi: 10.1101/sqb.2008.73.064
Scanlon, P. J., Faxon, D. P., Audet, A. M., Carabello, B., Dehmer, G. J., Eagle, K. A., et al. (1999). ACC/AHA guidelines for coronary angiography: executive summary and recommendations. a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation 99, 2345–2357. doi: 10.1161/01.cir.99.17.2345
Shan, D., Guo, S., Wu, H. K., Lv, F., Jin, L., Zhang, M., et al. (2020). Cardiac ischemic preconditioning promotes MG53 secretion through H2O2-activated protein kinase C-delta signaling. Circulation 142, 1077–1091. doi: 10.1161/CIRCULATIONAHA.119.044998
Suzuki, K., Komukai, K., Nakata, K., Kang, R., Oi, Y., Muto, E., et al. (2018). The usefulness and limitations of point-of-care cardiac troponin measurement in the emergency department. Intern. Med. 57, 1673–1680. doi: 10.2169/internalmedicine.0098-17
Thygesen, K., Alpert, J. S., Jaffe, A. S., Simoons, M. L., Chaitman, B. R., White, H. D., et al. (2012). Third universal definition of myocardial infarction. Eur. Heart J. 33, 2551–2567. doi: 10.1093/eurheartj/ehs184
Wang, X., Xie, W., Zhang, Y., Lin, P., Han, L., Han, P., et al. (2010). Cardioprotection of ischemia/reperfusion injury by cholesterol-dependent MG53-mediated membrane repair. Circ. Res. 107, 76–83. doi: 10.1161/CIRCRESAHA.109.215822
Weisleder, N., Takeshima, H., and Ma, J. (2008). Immuno-proteomic approach to excitation–contraction coupling in skeletal and cardiac muscle: molecular insights revealed by the mitsugumins. Cell Calcium 43, 1–8. doi: 10.1016/j.ceca.2007.10.006
Keywords: MG53, coronary artery disease, acute myocardial infarction, biomarker, risk stratification
Citation: Xie H, Wang Y, Zhu T, Feng S, Yan Z, Zhu Z, Ni J, Ni J, Du R, Zhu J, Ding F, Liu S, Han H, Zhang H, Zhao J, Zhang R, Quan W and Yan X (2020) Serum MG53/TRIM72 Is Associated With the Presence and Severity of Coronary Artery Disease and Acute Myocardial Infarction. Front. Physiol. 11:617845. doi: 10.3389/fphys.2020.617845
Received: 15 October 2020; Accepted: 25 November 2020;
Published: 17 December 2020.
Edited by:
George Grant, University of Aberdeen, United KingdomReviewed by:
Noah Lucas Weisleder, The Ohio State University, United StatesCopyright © 2020 Xie, Wang, Zhu, Feng, Yan, Zhu, Ni, Ni, Du, Zhu, Ding, Liu, Han, Zhang, Zhao, Zhang, Quan and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruiyan Zhang, emhhbmdydWl5YW5AMjYzLm5ldA==; Weiwei Quan, c3ByaW5ncXd3QDE2My5jb20=; Xiaoxiang Yan, Y2FyZGV4eWFueHhAaG90bWFpbC5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.