Corrigendum: Association Between D-dimer and Early Adverse Events in Patients With Acute Type A Aortic Dissection Undergoing Arch Replacement and the Frozen Elephant Trunk Implantation: A Retrospective Cohort Study
- 1Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
- 2Department of Cardiac Surgery, Beijing Aortic Disease Center, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
Objective: In the present study, we investigated the associations between D-dimer levels at admission and early adverse events in patients with acute type A aortic dissection undergoing arch replacement and the frozen elephant trunk (FET).
Methods: We retrospectively analyzed data of patients with acute type A aortic dissection undergoing aortic arch surgery and FET from July 2017 to December 2018 at Beijing Anzhen Hospital. D-dimer levels were evaluated within 24 h of admission. Multivariate Cox regression analysis was used to determine independent predictors of early postoperative adverse events.
Results: A total of 347 patients were included in the study. The average age of the patients was 48.07 ± 10.56 years, with male predominance (79.25%). The incidence of 90-day postoperative adverse events was 18.7%, consisting of 14.7% mortality and 4.0% permanent neurological dysfunction (PND). The median D-dimer level was 1.95 ug/ml (interquartile range, 0.77–3.16 ug/ml). Multivariable Cox regression analysis revealed that D-dimer level was independently associated with 90-day postoperative adverse events after adjustment for confounding factors (hazard ratio = 1.19 per 10 ug/ml increase in D-dimer, 95% confidence interval: 1.01–1.41; P = 0.039). Kaplan–Meier analysis revealed that the highest tertile (median 6.27 ug/ml) had more 90-day postoperative adverse events compared with the median and lowest tertiles (P = 0.0014). Sub-analysis found that the association remained unchanged.
Conclusion: Increased D-dimer levels at admission were associated with 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch replacement and FET. These results may help clinicians optimize the risk evaluation and perioperative clinical management to reduce early adverse events.
Key Question: Explore the relationship between D-dimer and early outcomes in patients with aortic dissection with arch replacement.
Key Findings: Increased D-dimer at admission was associated with adverse events in patients with aortic dissection with arch surgery.
Take-Home Message: The high-risk patients deserve close medical monitoring.
Introduction
The incidence of aortic dissection markedly increases with atherosclerosis and hypertension. Although surgical treatment significantly reduces the mortality of patients with aortic dissection compared with medical management, short-term mortality (30-day or in-hospital mortality) remains high (13–17%) (Mussa et al., 2016).
D-dimer, a specific degradation product of cross-linked fibrin, represents the coagulation and fibrinolytic system activation (Suzuki et al., 2009). It is now commonly used in the diagnosis of pulmonary embolism (van der Hulle et al., 2013), deep vein thrombosis (Faller et al., 2017), acute coronary syndrome (Bayes-Genis et al., 2000), and acute aortic dissection (Akutsu et al., 2005; Suzuki et al., 2009; Shao et al., 2014). For acute aortic dissection, the mechanisms of coagulation and fibrinolytic system activation might be (1) coagulant material from the aortic wall released into the circulation and (2) an accumulation of clotting factors at the site of the lesion, secondary to the local exposition of tissue factors from the torn arterial wall (Ten Cate et al., 1975). Thus, the D-dimer level is elevated in patients with acute aortic dissection. Weber et al. (2003) first observed that D-dimer levels tended to be higher in patients with acute aortic dissection, but no relation was observed between D-dimer levels and in-hospital outcome. On the other hand, Wen et al. (2013) and Huang et al. (2015) found that an elevated D-dimer level was associated with increased in-hospital mortality (Wen et al., 2013; Huang et al., 2015). Nevertheless, the sample size in these two previous studies was relatively small, and the largest sample size was 212 patients. Further, these study populations with aortic dissection not only underwent surgical treatment, but also medical treatment. In addition, few studies have evaluated the association between D-dimer levels and 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch replacement and FET.
For these reasons, we conducted a retrospective cohort study to investigate the association between D-dimer levels and 90-day postoperative adverse events in patients undergoing arch replacement and FET using a multivariate Cox regression model containing all known associated major perioperative predictors. Our hypothesis was that the risk of 90-day postoperative adverse events would increase as D-dimer levels increased.
Materials and Methods
Study Design and Study Population
From July 1, 2017, to December 31, 2018, consecutive patients with aortic disease undergoing aortic arch surgery were retrospectively identified at the aortic center in the Beijing Anzhen Hospital (Capital Medical University of Beijing, China). Patients with acute type A aortic dissection who underwent total arch replacement and the frozen elephant trunk (FET) technique were recruited into this observational retrospective cohort study. Patients who (1) underwent hemi-arch replacement (n = 31), (2) suffered from chronic aortic disease (n = 69), (3) had redo sternotomy (n = 19), (4) did not undergo the FET technique (n = 40), or (5) did not have D-dimer values (n = 4) were excluded.
Study Endpoint
The endpoint of this observational retrospective study was defined as early all-cause mortality or permanent neurological dysfunction (PND) during the hospital stay or within 90 days after surgery. PND was defined as the presence of permanent neurologic deficits, including abnormal movement of limbs, coma, and sensory loss affecting one side of the body, within postoperative 90-day. Confirmation of the diagnosis was made by a neurologist or by means of computed tomographic scanning or magnetic resonance imaging of the brain.
Definition and Procedure
The type of aortic dissection was classified according to Stanford classification (Daily et al., 1970). Acute dissection was defined as clinical symptoms lasting less than 14 days (Hagan et al., 2000). Hypertension was defined by a clinical record of systolic or diastolic blood pressure greater than 140 or 90 mmHg on admission, or the use of anti-hypertension drugs. Diabetes mellitus was defined as treatment with oral hypoglycemic agents or insulin, or as having a fasting blood glucose level ≥7.0 mmol/L (126 mg/dl). Smoking status was defined as smoking within the preceding 1 year based on information in medical records. Renal insufficiency was defined as estimated glomerular filtration rate (eGFR) <60 mL/min per 1.73 m2, calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (Levey et al., 2009). A diagnosis of cardiac artery disease was considered if patients had a history of myocardial infarction or previous PCI or coronary artery bypass grafting (CABG) before admission. Cerebrovascular disease was defined based on relevant neurologic dysfunction before admission or previous stroke. Pericardial tamponade was diagnosed by echocardiography. The details of total arch replacement and FET implantation have been described elsewhere by our team (Sun et al., 2011; Ma et al., 2013). In brief, the arch was opened under moderate hypothermia arrest (21∼28°C). An open stent-graft was deployed into the descending aorta. The arch was replaced with a four-branched vascular graft.
D-dimer Measurement
Within 24 h after admission, whole-blood samples were drawn into blood collection tubes containing sodium citrate (3.2%, 109 mmol/L) as the anticoagulant (9:1 ratio of blood:anticoagulant) to measure prothrombin time (PT), activated partial thromboplastin time (APTT), fibrin degradation products (FDP), and D-dimer. Venous blood was immediately sent to the clinical laboratory center of the Anzhen hospital. Plasma PT, APTT, FDP, and D-dimer were measured using the commercially available automated latex immunoturbidimetric assay (Werfen ACL TOP 700, United States) (Di Nisio et al., 2007; Wang et al., 2018). Routine blood tests and some biochemical indicators were determined by standard quantitative assay techniques, according to the manufacturers’ instructions. All assays were run in duplicate.
Data Collected for Analysis
Clinical, operative, perfusion, and postoperative data have been retrospectively collected in a department database, and further data were extracted from operation reports, perfusion reports, intraoperative computerized records, and review of medical records. Data were compiled via the Empower Dataweb data collection management system (X&Y Solutions, Inc., Boston, MA, United States). The current study was approved by the Human Subjects Review Committee at Anzhen Hospital (Approval No. 2017058X). Follow-up data were obtained from medical records and telephone calls.
Statistical Analysis
Categorical variables were presented as frequencies or percentages, whereas continuous variables were expressed as means ± standard deviations (normal distribution) or medians and interquartile ranges (skewed distribution). First, we grouped D-dimer levels in tertiles. The significant differences between the means and proportions of the tertiles in baseline characteristics were analyzed using a Student’s t-test or Mann–Whitney U test for continuous variables, as appropriate, and a chi-square test for categorical variables (Table 1). Second, univariate Cox regression analyses were used to evaluate the association between each significant variable and 90-day postoperative adverse events (Supplementary Table). Third, multivariate Cox regression models (Table 2) were used to examine whether D-dimer levels had an independent effect on 90-day postoperative adverse events. We simultaneously showed the results from unadjusted, minorly adjusted, and fully adjusted analyses. The covariates, when added to this model, changed the matched odds ratio by at least 10% (Kernan et al., 2000) and covariates of known clinical importance were adjusted. We expanded D-dimer levels 10 times and labeled them per 10 ug/mL change. Trend tests were based on D-dimer level tertiles as continuous variables. Fourth, survival estimates and cumulative event rates were compared using the Kaplan–Meier method by using the time-to-first event for each endpoint among D-dimer level tertiles. The log-rank test was used to compare the Kaplan–Meier hazard ratios (HR) for 90-day postoperative adverse events, and their corresponding 95% confidence intervals (CIs). Finally, subgroup analysis was done to find whether potential risk factors were influencing the results. The interactions of subgroups were inspected by multivariate adjusted Cox regression models (Table 3). All analyses were performed using Empower (R) (1 X&Y Solutions, Inc.) and R2.
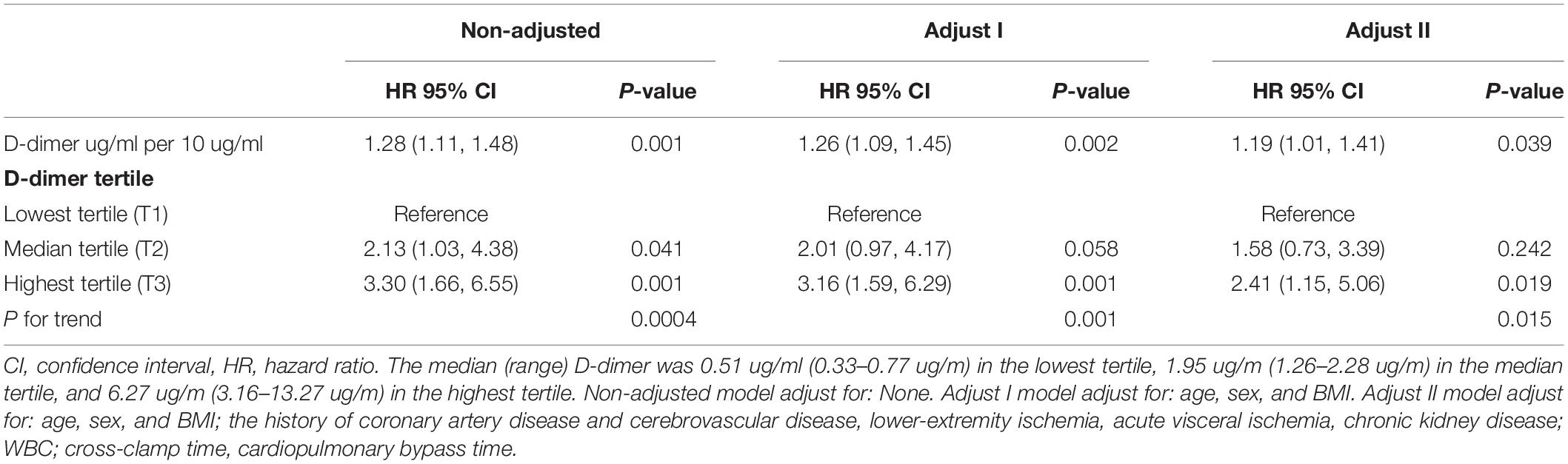
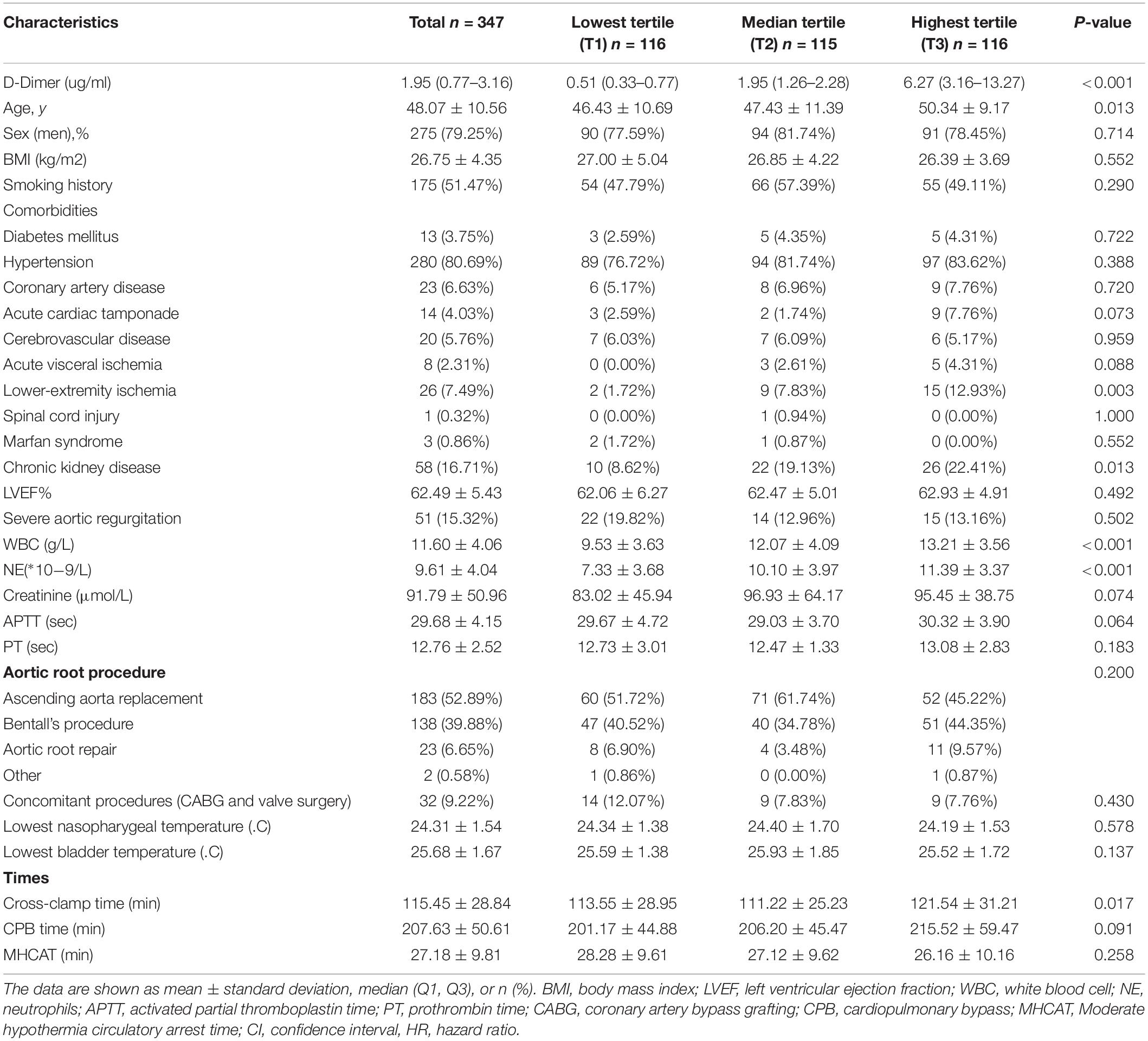
Table 2. Multivariable cox regression analyses of 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch replacement and FET.
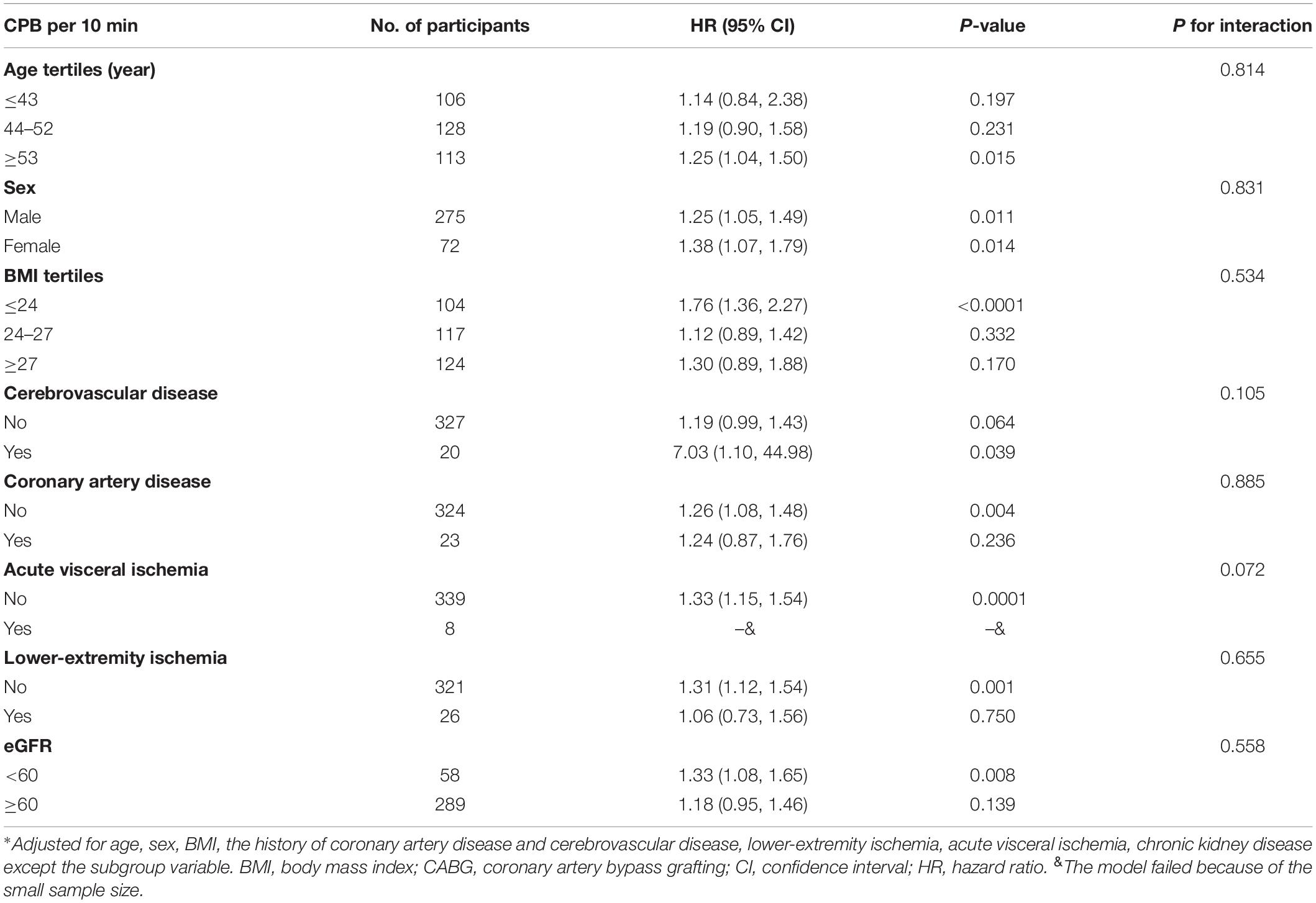
Table 3. Effects of D-dimer on 90-day postoperative adverse events in each subgroup by multivariable Cox model.
Results
From July 1, 2017, to December 31, 2018, 510 consecutive patients received aortic arch surgery at the cardiac surgery center in the Beijing Anzhen Hospital. We excluded patients who underwent hemi-arch replacement (n = 31), had chronic aortic disease (n = 69), underwent redo-sternotomy (n = 19), or did not have FET implantation (n = 40) (Figure 1).
Demographic Characteristics
The final analysis included 347 patients with acute type A aortic dissection who underwent total arch replacement and FET implantation (Figure 1). The median D-dimer value was 1.95 ug/mL, with an interquartile range of 0.77–3.16 ug/mL. The baseline demographic, clinical, operative, and perfusion characteristics are presented in Table 1. At admission, the mean age of the 347 patients was 48 years (48.07 ± 10.56), 275 (79.25%) were men. On echocardiography, the mean LVEF was 62.49 ± 5.43 and severe aortic regurgitation was identified in 51 (15.32%) patients at presentation. Moreover, 280 (80.69%) patients had previous hypertension, 13 (3.75%) had previous diabetes mellitus, 58 (16.71%) had chronic kidney dysfunction (CKD), 23 (6.63%) had coronary artery disease, and 20 (5.76%) had cerebrovascular disease. At admission, 26 (7.49%) patients presented with lower-extremity ischemia, 14 (4.03%) with acute cardiac tamponade, 8 (2.31%) with acute visceral ischemia, and 1 (0.32%) with spinal cord injury.
At the time of presentation, no difference was found in the patients’ sex, BMI, LVEF, and clinical status regarding diabetes mellitus, hypertension, coronary artery disease, cerebrovascular disease, the type of aortic root procedure, and concomitant procedures. However, lower-extremity ischemia and CKD were more common among those with higher D-dimer. Further, higher white blood cell counts and longer cross-clamp times were also associated with higher D-dimer.
D-dimer Levels and 90-day Postoperative Adverse Events in Patients With Acute Type A Aortic Dissection Undergoing Arch Replacement and FET
Sixty-five (18.7%) patients developed 90-day postoperative mortality and PND, consisting of 51 (14.7%) patient deaths and 14 (4.0%) patients with PND.
The results of univariate analyses of 90-day postoperative adverse events are summarized in the Supplementary Table. Univariate analyses showed that age, history of coronary artery disease, history of cerebrovascular disease, cardiopulmonary bypass time, cross-clamp time, and D-dimer values were associated with a significant increase in the incidence of 90-day postoperative adverse events. We performed a multivariate Cox regression analysis to further explore D-dimer as a prognostic marker. In the multivariable analysis shown in Table 2, D-dimer level was the independent risk factor for 90-day postoperative adverse events in Model I (HRadj 1.26 per 10 ug/ml increase, 95% CI: 1.09–1.45; P = 0.002), after adjusting for age, sex, and BMI. This was also true in Model II (HRadj 1.19 per 10 ug/ml increase, 95% CI: 1.01–1.41; P = 0.039) after adjusting for age, sex, BMI, history of coronary artery disease, history of cerebrovascular disease, lower-extremity ischemia, acute visceral ischemia, chronic kidney disease, WBC, cross-clamp time, and cardiopulmonary bypass time. Kaplan–Meier survival analysis (Figure 2) showed a significant difference among patients stratified by D-dimer level tertiles; specifically, D-dimer values in the highest tertile had more 90-day postoperative adverse events compared with the median and lowest tertiles (P = 0.0014).
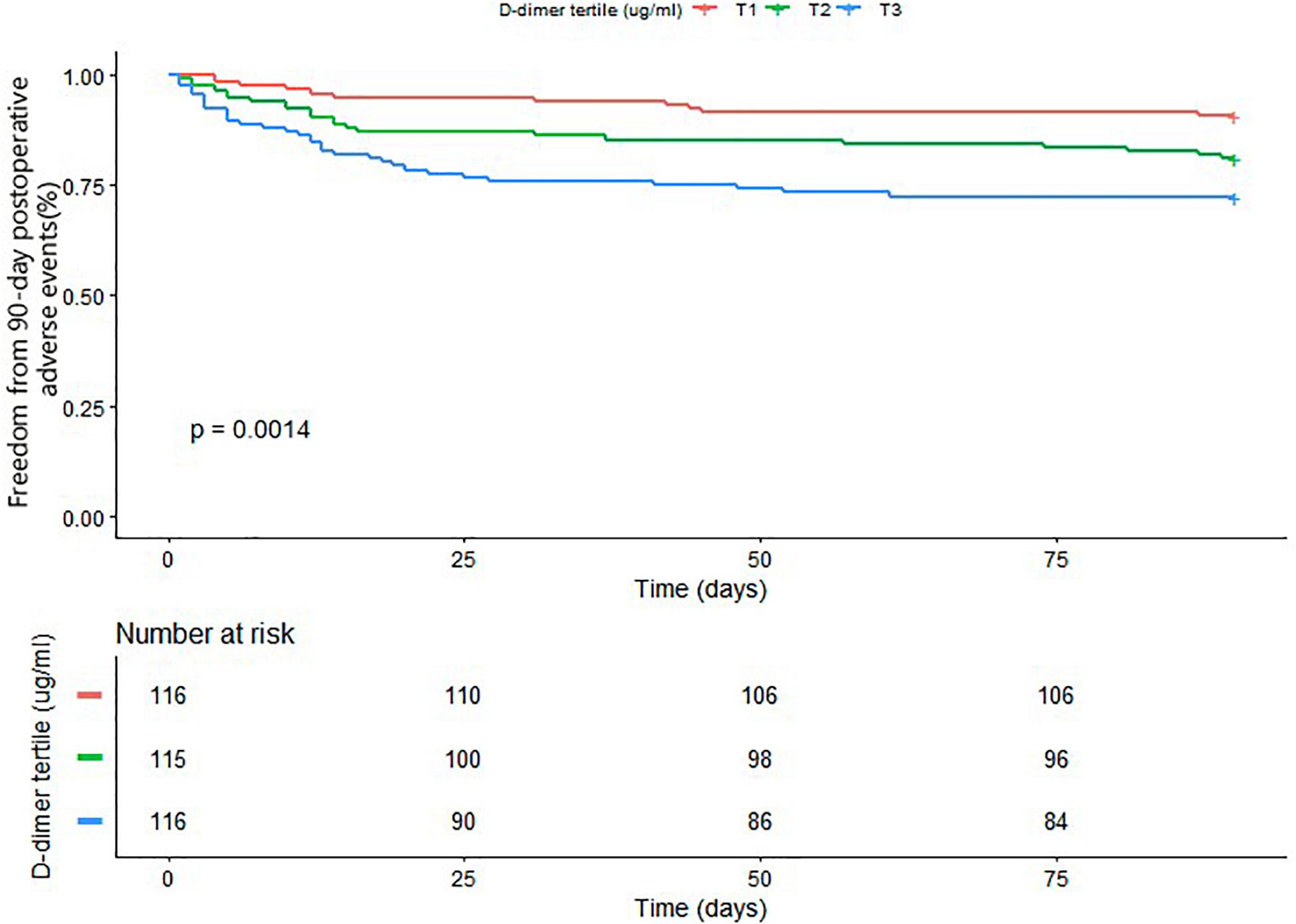
Figure 2. Kaplan–Meier analysis of freedom from 90-day postoperative adverse events based on D-dimer tertile (Log-rank, P = 0.0014).
Subgroup Analysis Between D-Dimer Level and 90-day Postoperative Adverse Events in Patients With Acute Type A Aortic Dissection Undergoing Arch Replacement and FET
To evaluate the potential influence of other factors, a sub-analysis was conducted stratifying patients by age tertiles, sex, BMI tertiles, history of cerebrovascular disease, history of coronary artery disease, acute visceral ischemia, lower-extremity ischemia, and chronic kidney disease, as presented in Table 3. Notably, all subgroups demonstrated a similar overall relationship between D-dimer level and 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch replacement and FET.
Discussion
The results of this study show that serum D-dimer level upon admission is independently associated with 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch surgery with FET. For every 10 ug/mL increase in plasma D-dimer concentration, the risk of 90-day postoperative adverse events increased by 19%, after adjusting for multiple factors. To the best of our knowledge, this is the first study to show an association between D-dimer level and 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch surgery with FET.
D-dimer is a degradation product of cross-linked fibrin. Elevated D-dimer levels are generally thought to be the result of intravascular activation of the coagulation system and secondary fibrinolysis. Several studies have shown that D-dimer is a good diagnostic test for diverse thrombotic conditions, such as ischemic stroke (Nezu et al., 2018), venous thromboembolism (Faller et al., 2017), pulmonary embolism (van der Hulle et al., 2013), and aortic dissection (Mussa et al., 2016). In addition to its high diagnostic value for thrombotic disease, recent studies have also reported its relationship with short-term and long-term prognosis of these diseases (Kim et al., 2015; Vele et al., 2016; Faller et al., 2017). Additionally, several studies have shown an association in the general population (Di Castelnuovo et al., 2013). For type A aortic dissection, high levels of tissue factors are released from the aortic wall injury, after which marked coagulation activation and subsequent marked enhancement of fibrinolysis occur (Weber et al., 2003). This pathophysiological process elevates serum D-dimer levels in patients with type A aortic dissection. The role of D-dimer in predicting short-term and long-term outcomes in patients with type A aortic dissection has been reported in previous cohort studies (Weber, 2005; Ohlmann et al., 2006; Wen et al., 2013; Huang et al., 2015). Nevertheless, these studies were made in only a limited number of patients. Further, there was significant heterogeneity in the study population, including dissection of different pathological types, as well as dissection patients treated with drugs and surgery. Additionally, for dissection patients undergoing surgery treatment, no surgical-related variables were collected. Thus, there are very few studies that focus on the relationship between D-dimer and 90-day postoperative adverse events in patients with acute type A aortic dissection undergoing arch replacement and FET.
The present study confirmed that D-dimer remains an independent predictor of 90-day postoperative adverse events in patients with type A aortic dissection despite surgical treatment. Although the mechanism of this relationship is not yet clear, some possible explanations may clarify its existence. Firstly, D-dimer concentrations may reflect the anatomical extent of the dissection, which represents the extent of the aortic injury (Weber et al., 2003; Ohlmann et al., 2006). Secondly, plasma D-dimer concentration reflects the volume of intraluminal thrombus, which is the biologically active material that takes part in the evolution of the dissection. It contains neutrophils, released pro-inflammatory cytokines, and proteolytic enzymes, which are associated with the destruction of the aortic wall and the progression of the dissection (Vele et al., 2016). Another study indicated that D-dimer values in mild to moderate traumatic brain injury predict hematoma expansion (Sugimoto et al., 2017). Finally, D-dimer also activates inflammatory cytokines and causes advanced blood coagulation or progression of dissection status. These factors might contribute to the association of high D-dimer concentrations with 90-day postoperative adverse events in patients with type A aortic disease undergoing arch replacement and FET.
In our center, over the past 10 years, although arch replacement with FET under moderate hypothermic circulatory arrest (MHAC) plus ante-grade cerebral perfusion has already become a standard procedure for aortic dissection (Sun et al., 2011; Ma et al., 2013), arch replacement is still a challenging procedure (Leontyev et al., 2016; Mussa et al., 2016). Some previous studies analyzed pre- and intraoperative predictors of early death and PND after arch replacement (Khaladj et al., 2008; Martens et al., 2016; Liu et al., 2017). Liu et al. (2017) found that the history of cerebrovascular diseases was a strong predictor of adverse outcome following arch replacement in 626 consecutive patients in China. Khaladj et al. (2008) found that advanced age and multiple comorbidities (renal insufficiency, coronary heart disease, and reoperation) were risk factors for adverse outcomes in 501 patients undergoing aortic arch surgery. However, these studies did not collect variables of preoperative coagulation status and there was high heterogeneity of selected patients. Considering that preoperative clinical status is a strong risk factor for surgical prognosis in previous studies (Khaladj et al., 2008; Liu et al., 2017), we not only adjusted based on these potential confounding factors in multiple regression models, but we also performed subgroup analysis according to the preoperative clinical status in the current study. Our results also indicate that the relationship between D-dimer and 90-day postoperative adverse events remained unchanged (Table 3).
Limitations
There are several limitations in this study. First, this study is a retrospective design from a single center, and our results may not be extendable to patients in other centers. Second, we measured D-dimer only on admission, and a series of measurements after arch replacement might be more valuable for evaluation of the association between D-dimer level and 90-day postoperative adverse events. Third, for the treatment of acute type A aortic dissection, aortic arch replacement combined with FET is a preferred choice at our center, while other centers may select more conventional procedures. This might lead to differences in study results. Fourth, this study lacks data on aortic computed tomography angiography (CTA). Because our center is the largest referral center for aortic disease in China, we only referred to the images from the local hospitals, as we can’t repeat the imaging examination for patients with type A aortic dissection given a limited time. Post-operative CTA was also not collected in every patient. The relationship between the level of D-dimer and CTA was not analyzed. Finally, other coagulation factors and tissue factors, such as factor II, V, VII, VIII, IX et al., were not collected because it was not the routine items of the clinical practice in the Beijing Anzhen Hospital (Capital Medical University of Beijing, China).
Conclusion
D-dimer is easily available in routine medical practice. Our results show that increased D-dimer levels at admission were associated with 90-day postoperative adverse events in patients with type A aortic dissection undergoing arch surgery with FET. This indicates that such high-risk patients deserve close medical monitoring.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Beijing Anzhen Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Chen Chang-zhong MD, Ph.D. and Chen Xinlin MD, Ph.D. (Department of Epidemiology and Biostatistics, X&Y Solutions Inc., Boston, MA, United States) and for their helpful review and comments about the manuscript. We also thank the Dr. Jie Liu from the Chinese PLA General Hospital for his advice and support.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2019.01627/full#supplementary-material
Footnotes
References
Akutsu, K., Sato, N., Yamamoto, T., Morita, N., Takagi, H., Fujita, N., et al. (2005). A rapid bedside D-dimer assay (cardiac D-dimer) for screening of clinically suspected acute aortic dissection. Circ. J. 69, 397–403. doi: 10.1253/circj.69.397
Bayes-Genis, A., Mateo, J., Santaló, M., Oliver, A., Guindo, J., Badimon, L., et al. (2000). D -Dimer is an early diagnostic marker of coronary ischemia in patients with chest pain. Am. Heart. J. 140, 379–384. doi: 10.1067/mhj.2000.108823
Daily, P. O., Trueblood, H. W., Stinson, E. B., Wuerflein, R. D., and Shumway, N. E. (1970). Management of acute aortic dissections. Ann. Thorac. Surg. 3, 237–247.
Di Castelnuovo, A., de Curtis, A., Costanzo, S., Persichillo, M., Olivieri, M., Zito, F., et al. (2013). Association of D-dimer levels with all-cause mortality in a healthy adult population: findings from the MOLI-SANI study. Haematologica 98, 1476–1480. doi: 10.3324/haematol.2012.083410
Di Nisio, M., Squizzato, A., Rutjes, A. W., Buller, H. R., Zwinderman, A. H., and Bossuyt, P. M. (2007). Diagnostic accuracy of D-dimer test for exclusion of venous thromboembolism: a systematic review. J. Thromb. Haemost. 5, 296–304. doi: 10.1111/j.1538-7836.2007.02328.x
Faller, N., Limacher, A., Méan, M., Righini, M., Aschwanden, M., Beer, J. H., et al. (2017). Predictors and causes of long-term mortality in elderly patients with acute venous thromboembolism: a prospective cohort study. Am. J. Med. 130, 198–206. doi: 10.1016/j.amjmed.2016.09.008
Hagan, P. G., Nienaber, C. A., Isselbacher, E. M., Bruckman, D., Karavite, D. J., Russman, P. L., et al. (2000). The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 283, 897–903.
Huang, B., Yang, Y., Lu, H., Zhao, Z., Zhang, S., Hui, R., et al. (2015). Impact of d-Dimer levels on admission on inhospital and long-term outcome in patients with type A acute Aortic dissection. Am. J. Cardiol. 115, 1595–1600. doi: 10.1016/j.amjcard.2015.02.067
Kernan, W. N. I, Viscoli, C. M., Brass, L. M., Broderick, J. P., Brott, T., Feldmann, E., et al. (2000). Phenylpropanolamine and the risk of hemorrhagic stroke. N. Engl. J. Med. 343, 1826–1832.
Khaladj, N., Shrestha, M., Meck, S., Peterss, S., Kamiya, H., Kallenbach, K., et al. (2008). Hypothermic circulatory arrest with selective antegrade cerebral perfusion in ascending aortic and aortic arch surgery: a risk factor analysis for adverse outcome in 501 patients. J. Thorac. Cardiovasc. Surg. 135, 908–914. doi: 10.1016/j.jtcvs.2007.07.067
Kim, Y. D., Song, D., Nam, H. S., Lee, K., Yoo, J., Hong, G. R., et al. (2015). D-dimer for prediction of long-term outcome in cryptogenic stroke patients with patent foramen ovale. Thromb. Haemost. 114, 614–622. doi: 10.1160/TH14-12-1040
Leontyev, S., Tsagakis, K., Pacini, D., Di Bartolomeo, R., Mohr, F. W., Weiss, G., et al. (2016). Impact of clinical factors and surgical techniques on early outcome of patients treated with frozen elephant trunk technique by using EVITA open stent-graft: results of a multicentre study. Eur. J. Cardio-Thorac. 49, 660–666. doi: 10.1093/ejcts/ezv150
Levey, A. S., Stevens, L. A., Schmid, C. H., Zhang, Y. L., Castro, A. F., Feldman, H. I., et al. (2009). A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 9, 604–612.
Liu, H., Chang, Q., Zhang, H., and Yu, C. (2017). Predictors of adverse outcome and transient neurological dysfunction following Aortic arch replacement in 626 consecutive patients in China. Heart Lung Circ. 26, 172–178. doi: 10.1016/j.hlc.2016.02.004
Ma, W., Zheng, J., Liu, Y., Zhu, J., and Sun, L. (2013). Dr. Sun’s procedure for type A aortic dissection: total arch replacement using tetrafurcate graft with stented elephant trunk implantation. AORTA 1, 59–64. doi: 10.12945/j.aorta.2013.13.015
Martens, A., Beckmann, E., Kaufeld, T., Umminger, J., Fleissner, F., Koigeldiyev, N., et al. (2016). Total aortic arch repair: risk factor analysis and follow-up in 199 patients. Eur. J. Cardio-Thorac. 50, 940–948. doi: 10.1093/ejcts/ezw158
Mussa, F. F., Horton, J. D., Moridzadeh, R., Nicholson, J., Trimarchi, S., and Eagle, K. A. (2016). Acute aortic dissection and intramural Hematoma. JAMA 316, 754–763. doi: 10.1001/jama.2016.10026
Nezu, T., Kitano, T., Kubo, S., Uemura, J., Yamashita, S., Iwanaga, T., et al. (2018). Impact of D-dimer levels for short-term or long-term outcomes in cryptogenic stroke patients. J. Neurol. 265, 628–636. doi: 10.1007/s00415-018-8742-x
Ohlmann, P., Faure, A., Morel, O., Petit, H., Kabbaj, H., Meyer, N., et al. (2006). Diagnostic and prognostic value of circulating D-Dimers in patients with acute aortic dissection. Crit. Care Med. 34, 1358–1364. doi: 10.1097/01.ccm.0000216686.72457.ec
Shao, N., Xia, S., Wang, J., Zhou, X., Huang, Z., Zhu, W., et al. (2014). The role of D-dimers in the diagnosis of acute aortic dissection. Mol. Biol. Rep. 41, 6397–6403. doi: 10.1007/s11033-014-3520-z
Sugimoto, K., Suehiro, E., Shinoyama, M., Sadahiro, H., Haji, K., Fujiyama, Y., et al. (2017). D-Dimer elevation as a blood biomarker for detection of structural disorder in mild traumatic brain injury. J. Neurotraum. 34, 3245–3248. doi: 10.1089/neu.2017.5240
Sun, L., Qi, R., Zhu, J., Liu, Y., and Zheng, J. (2011). Total arch replacement combined with stented elephant trunk implantation. Circulation 123, 971–978. doi: 10.1161/CIRCULATIONAHA.110.015081
Suzuki, T., Distante, A., Zizza, A., Trimarchi, S., Villani, M., Counselman, F., et al. (2009). Diagnosis of acute aortic dissection by D-Dimer. Circulation 119, 2702–2707. doi: 10.1161/CIRCULATIONAHA.108.833004
Ten Cate, J. W., Timmers, H., and Becker, A. E. (1975). Coagulopathy in ruptured or dissecting aortic aneurysms. Am. J. Med. 59, 171–176. doi: 10.1016/0002-9343(75)90351-4
van der Hulle, T., den Exter, P. L., Erkens, P. G. M., van Es, J., Mos, I. C. M., Ten Cate, H., et al. (2013). Variable D-dimer thresholds for diagnosis of clinically suspected acute pulmonary embolism. J. Thromb. Haemost. 11, 1986–1992. doi: 10.1111/jth.12394
Vele, E., Kurtcehajic, A., Zerem, E., Maskovic, J., Alibegovic, E., and Hujdurovic, A. (2016). Plasma D-dimer as a predictor of the progression of abdominal aortic aneurysm. J. Thromb. Haemost. 11, 2298–2303. doi: 10.1111/jth.13487
Wang, Y., Tan, X., Gao, H., Yuan, H., Hu, R., Jia, L., et al. (2018). Magnitude of soluble ST2 as a novel biomarker for acute aortic dissection. Circulation 137, 259–269. doi: 10.1161/CIRCULATIONAHA.117.030469
Weber, T. (2005). Plasma concentrations of D-dimer predict mortality in acute type A aortic dissection. Heart 92, 836–837. doi: 10.1136/hrt.2005.072959
Weber, T., Gler, S. H., Auer, J., Berent, R., Lassnig, E., Kvas, E., et al. (2003). D-dimer in acute aortic dissection. Chest 123, 1375–1378.
Keywords: D-dimer, predictor, 90-day postoperative adverse events, aortic arch replacement, frozen elephant trunk
Citation: Liu T, Zheng J, Zhang Y-C, Zhu K, Gao H-Q, Zhang K, Jin X-F and Xu S-D (2020) Association Between D-dimer and Early Adverse Events in Patients With Acute Type A Aortic Dissection Undergoing Arch Replacement and the Frozen Elephant Trunk Implantation: A Retrospective Cohort Study. Front. Physiol. 10:1627. doi: 10.3389/fphys.2019.01627
Received: 17 August 2019; Accepted: 24 December 2019;
Published: 21 January 2020.
Edited by:
Gerald A. Meininger, University of Missouri, United StatesReviewed by:
Barbara Ruszkowska-Ciastek, Nicolaus Copernicus University in Toruń, PolandSivareddy Kotla, University of Texas MD Anderson Cancer Center, United States
Copyright © 2020 Liu, Zheng, Zhang, Zhu, Gao, Zhang, Jin and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shang-Dong Xu, xushangdong@126.com
†First author
 Tong Liu1†
Tong Liu1† Kai Zhang
Kai Zhang Shang-Dong Xu
Shang-Dong Xu