
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Physiol., 17 January 2019
Sec. Computational Physiology and Medicine
Volume 9 - 2018 | https://doi.org/10.3389/fphys.2018.01861
This article is part of the Research TopicRecent Advances in Understanding the Basic Mechanisms of Atrial Fibrillation Using Novel Computational ApproachesView all 28 articles
 Cheng Chen1†
Cheng Chen1† Daobo Li1†
Daobo Li1† Jeffery Ho2
Jeffery Ho2 Tong Liu3
Tong Liu3 Xintao Li1
Xintao Li1 Zhao Wang1
Zhao Wang1 Yajuan Lin1
Yajuan Lin1 Fuquan Zou1
Fuquan Zou1 Gary Tse2,4*
Gary Tse2,4* Yunlong Xia1*
Yunlong Xia1*Purpose: Circumferential pulmonary vein isolation (CPVI) is a routine ablation strategy of atrial fibrillation (AF). The adenosine test can be used to unmask dormant conduction (DC) of pulmonary veins after CPVI, thereby demonstrating possible pulmonary vein re-connection and the need for further ablation. However, whether adenosine test could help improve the long term successful rate of CPVI is still controversial. This systemic review and meta-analysis was to determine the clinical utility of the adenosine test.
Methods: PubMed, EMBASE, Web of Science and Cochrane Library database were searched through July 2016 to identify relevant studies using the keywords “dormant pulmonary vein conduction,” “adenosine test,” “circumferential pulmonary vein isolation,” and “atrial fibrillation.” A random-effects model was used to compare pooled outcomes and tested for heterogeneity.
Results: A total of 17 studies including 5,169 participants were included in the final meta-analysis. Two groups of comparisons were classified: (1) Long-term successful rate in those AF patients underwent CPVI with and without adenosine test [Group A (+) and Group A (−)]; (2) Long-term successful rate in those patients who had adenosine test with and without dormant conduction [Group DC (+) and Group DC (−)]. The overall meta-analysis showed that no significant difference can be observed between Group A (+) and Group A (−) (RR 1.08; 95% CI 0.97–1.19; P = 0.16; I2 = 66%) and between Group DC (+) and Group DC (−) (RR 1.01; 95% CI 0.91–1.12; P = 0.88; I2 = 60%).
Conclusion: Pooled meta-analysis suggested adenosine test may not improve long-term successful rate in AF patients underwent CPVI. Furthermore, AF recurrence may not be decreased by eliminating DC provoked by adenosine, even though adenosine test was applied after CPVI.
Atrial fibrillation (AF) is a common cardiac arrhythmia, placing a significant burden on healthcare systems worldwide. It has been estimated that 33.5 million people suffering from AF with an increasing prevalence partly attributable to an aging population (Thacker et al., 2013; Chugh et al., 2014). Because pulmonary veins (PVs) are often the triggering sites for initiating and maintaining AF, circumferential PV isolation (CPVI) has been cornerstone of catheter ablation strategy to restore sinus rhythm for AF (Haïssaguerre et al., 2000; Jaïs et al., 2008; Kirchhof et al., 2017). Although feasibility and visibility of the three-dimensional electroanatomic mapping system have been improved, AF recurrence remains a problem due to PV reconnection after CPVI ablation (Ouyang et al., 2005). A study suggested that 20% of AF patients required repeat procedures after a median follow-up of 13 months (Hocini et al., 2005). Previous studies have suggested that PV re-connection can be identified by unmasking dormant conductions (DCs) induced by adenosine (Arentz et al., 2004; Theis et al., 2015; Ghanbari et al., 2016). The adenosine test has been used extensively to identify DCs (Arentz et al., 2004). The mechanism is thought to involve hyperpolarization of the membrane potential of dormant PVs by activating the IKAdo inward rectifier current, which would transiently establish PV reconnection (Datino et al., 2010).
A recent systematic review and meta-analysis has demonstrated a positive outcome on assessment and ablation of dormant conduction (McLellan et al., 2013). However, some of the enrolled studies were based on segmental ablation strategy. Moreover, many studies suggested that whether DCs are associated with high rate of AF recurrence or adenosine test can improve clinical outcome of PVI remains controversial (Elayi et al., 2013; Kobori et al., 2015; Theis et al., 2015; Ghanbari et al., 2016; Kim et al., 2016). Several investigators have attempted to use the appearance of DCs as indication of further ablation using adenosine test after PVI for AF ablation, while results were restricted by low number of participants (McLellan et al., 2013). Therefore, if adenosine test will help to improve ablation success rates after CPVI remains controversial. We conducted this systematic review and meta-analysis to determine the clinical significance of unmasking DCs after CPVI based on long-term follow up using adenosine test as the guidance of extra ablation for AF patients.
The databases Pubmed, EMBASE, Web of Science and Cochrane library were searched using searching terms and related items including keywords “dormant pulmonary vein conduction,” “adenosine test,” “circumferential pulmonary vein isolation,” and “atrial fibrillation.”
The inclusion criteria were limited to articles published in English, involving human subjects of adult age, and published between 2010 and 2016. The exclusion criteria were: (1) ablation for non-AF patients; (2) no adenosine test used; (3) studies including fewer than 90 participants; (4) follow-up period <12 months; (5) CPVI was not used for AF ablation; (6) articles that were case reports, reviews and meta-analyses.
Data from the different studies were entered in pre-specified spreadsheet in Microsoft Excel. All potentially relevant reports were retrieved as complete manuscripts and assessed for compliance with the inclusion criteria. Two reviewers (C.C. and D.L.) independently reviewed each included study and disagreements were resolved by adjudication with input from a third reviewer (Y.X.). Records matching searching goal were enrolled.
The meta-analysis was performed using Review Manager (RevMan 5. 3, Cochrane Collaboration, Oxford, UK). Relative risk (RR) values with 95% confidence intervals (CI) were calculated. Categorical variables were pooled using the Mantel-Hanseal method. The I2 statistic from the standard chi-square test (χ2), which describes the percentage of the variability in effect estimates resulting from heterogeneity. A fixed effect model was used if I2 ≤ 0.25, otherwise the random effect model was used (Higgins and Green, 2011). P-value < 0. 05 (two-tailed) was considered statistical significant.
We used the modified Newcastle-Ottawa scale for quality assessment of non-randomized trials and the methodological quality of RCTs was assessed by the components recommended by the Cochrane Collaboration (Higgins and Green, 2011). The quality of each trial except RCTs was quantified by a score of 0–9.
A flow diagram detailing the above search terms with inclusion and exclusion criteria is shown in Figure 1. A total of 4,669 records were identified from Pubmed, EMBASE, Web of Science and Cochrane Library databases. Of these, 17 studies met the inclusion criteria and were included in the final meta-analysis (Kumagai et al., 2010; Matsuo et al., 2010; Miyazaki et al., 2012; Van Belle et al., 2012; Cheung et al., 2013; Elayi et al., 2013; Kaitani et al., 2014; Zhang et al., 2014; Compier et al., 2015; Kobori et al., 2015; Kumar et al., 2015; Lin et al., 2015; Macle et al., 2015; Ghanbari et al., 2016; Kim et al., 2016; Tebbenjohanns et al., 2016). Twelve were prospective studies (Matsuo et al., 2010; Van Belle et al., 2012; Elayi et al., 2013; Kaitani et al., 2014; Compier et al., 2015; Kobori et al., 2015; Kumar et al., 2015; Lin et al., 2015; Macle et al., 2015; Theis et al., 2015; Ghanbari et al., 2016; Kim et al., 2016), four were retrospective studies (Kumagai et al., 2010; Matsuo et al., 2010; Miyazaki et al., 2012; Zhang et al., 2014) and four were randomized controlled trials (RCTs) (Kobori et al., 2015; Macle et al., 2015; Theis et al., 2015; Ghanbari et al., 2016). One study used prospective participants as a study group and retrospective cohort as control group (Tebbenjohanns et al., 2016). A total of 5,169 participants were included.
These studies used selective venography or 3-dimensional Electroanatomical Mapping System (including CARTO, Ensite NavX) to identify the PV antrum and subsequently performed CPVI. In four studies, PVI was guided by cryoballoon (second generation cryoballoon, CB-2G) (Van Belle et al., 2012; Compier et al., 2015; Kumar et al., 2015; Tebbenjohanns et al., 2016). The endpoint of electrophysiological study was the presence of entrance block defined by the circular mapping catheter (Lasso, Biosense Webster) or the elimination of all PV potentials or establishment of a bidirectional conduction block between left atrium (LA) and PVs. All participants underwent further ablation if DCs was induced. Two studies described the additional use of superior vena cava isolation (Compier et al., 2015; Kumar et al., 2015).
In this meta-analysis, we supposed to determine: (1) if adenosine test would help to increase the success rate of PVI; and (2) furthermore, if DCs induced by adenosine play an important role in AF recurrence after CPVI. Hence, in the first part, Group A (+) and Group A (−) were divided according to whether adenosine was administrated or not. And in the second part, Group DC (+) and Group DC (−) were divided according to whether the DCs appeared or not after adenosine administration. All of DCs induced by adenosine test in Group A (+) and Group DC (+) patients were eliminated after CPVI. The baseline characteristics of these studies are listed in Table 1, and those of procedure parameter are shown in Table 2. Quality assessment of the included studies was made using the Newcastle–Ottawa Scale for non-randomized case–control studies and the Cochrane Collaboration's tool for randomized trials (Table 3).
The pooled meta-analysis demonstrated that there was no significant difference in freedom from recurrent AF between Group A (+) and Group A (−) (RR = 1.08, 95% CI: 0.97–1.19, P = 0.16, I2 = 66%; Figure 2). A funnel plot plotting standard errors against the logarithms of the RR are shown in Figure 3, demonstrating no significant publication bias.
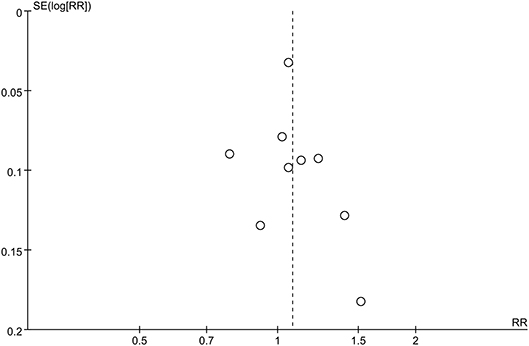
Figure 3. Funnel plot of standard errors against logarithms of odds ratios for studies comparing long-term success rates of PVI between Group A (+) and Group A (−).
No significant difference was observed between Group DC (+) and Group DC (−) with a pooled RR of 1.01 (95% CI: 0. 91–1.12; P = 0. 88; I2 = 60%; Figure 4). A funnel plot plotting standard errors against the logarithms of the RR are shown in Figure 5, demonstrating no significant publication bias.
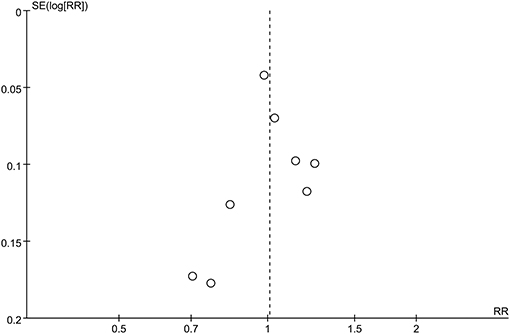
Figure 5. Funnel plot of standard errors against logarithms of odds ratios of studies comparing long-term PVI success rate between Group DC (+) and Group DC (−).
Additional subgroup analyses were performed for radiofrequency catheter ablation (RFCA) and CB-2G catheter ablation for PVI in Group A (+) and Group A (−). For RFCA, no difference in success rate was observed in Group A (+) and Group A (−) for patients with a RR of 1.02 (95% CI: 0.89–1.17; P = 0.80; Figure 6), which was accompanied by significant heterogeneity (I2 = 73%). Similarly, for CB-2G, success rates for those who underwent adenosine testing (n = 134) were not significantly different from those who did not have such a test (n = 212), with a pooled RR of 1.18 (95% CI = 0. 99–1.42; P = 0.07; Figure 7) with significant heterogeneity (I2 = 62%).
Sensitivity analysis included study design and adenosine test, and none of them showed significant interference with study outcomes. Results are shown in Table 4.
Adenosine testing after AF ablation procedures has been widely adopted for demonstrating DCs, which are further ablated to reduce AF recurrence rates (Hocini et al., 2005). However, in our study, the result of pooled meta-analysis suggested that adenosine test may not help to reduce the long-term AF recurrence after CPVI, and further subgroup analysis also confirmed the result. Some recent studies also suggested negative result of adenosine test based on CPVI (Theis et al., 2015; Ghanbari et al., 2016). The reason might be explained by the mechanism of PVI re-connection after CPVI ablation dose not totally attributed by DCs (Linz et al., 2018). Potential mechanisms of AF recurrence after CPVI may due to failure of trans-mural injury of PVAs (Rostock et al., 2006), heterogeneity of myocardial sleeves extending into the pulmonary veins (Ho et al., 2001) or so on. As a consequence, the necessity and applicability of adenosine test diminished in the context of CPVI adoption ablation strategy and Whether other techniques, such as pacing along the PVI line by the distal tip of the ablation catheter to identify viable myocardium or potential gaps (Schaeffer et al., 2015) improves PVI outcome should be investigated in the future.
However, a recent meta-analysis has shown that long-term success rates of PVI were improved by further eliminating DCs that have been identified by adenosine test for patients underwent segmental ablation for AF (McLellan et al., 2017). The discrepancy results with the results of the previous meta-analysis (McLellan et al., 2017) may due to improved ablation strategies (Ouyang et al., 2004). The 3-dimensional Electroanatomical Mapping System for RFA provides better visualization and reduce the need for excessive ablation (Ouyang et al., 2004). Ablation strategies based on CPVI ablation, instead of segmental ablation, were comprehensively adopted for AF patients either paroxysmal AF or persistent AF, leading to better AF control in the long-term (Gepstein et al., 1997). Previous studies had shown that segmental ablation was inferior to long term treatment compared with CPVI, and leads to more complications, such as pulmonary stenosis (Oral et al., 2003). Additionally, cryo-application offers spherical contact with the PV autrum (PVA), guided by annular Achieve catheter and vasography, provided CPVI by the single-shot technique (Nakagawa et al., 2007). Consequently, modifying skills and appliances, meaningful of adenosine administration may have diminished the need for AF re-ablation.
Complications arising from ablating DCs could further contribute to the lack of efficacy. For example, excessive ablation creates scarring of the atrial myocardium, which can serve as substrates for re-entry (Pappone et al., 2004; Tse et al., 2016). Indeed, a previous study compared anatomically guided CPVI with wide atrial ablation, demonstrating that the latter approach significantly increased the likelihood of micro-reentry ablation by producing areas of conduction slowing and block (Hocini et al., 2005). Moreover, we found that fluoroscopic time and procedure time were prolonged due to adenosine administration.
This systematic review and meta-analysis has several potential limitations. There was moderate heterogeneity across the included studies, which may be due to the following factors. Firstly, differences in study participants between each study especially the types of AF, and in detection criteria were observed. Secondly, several studies have used additional methods during adenosine testing for provoking DCs, such as isoproterenol administration during adenosine test. Thirdly, the dose of adenosine, administration method and procedure (such as waiting period after adenosine) used to unmask dormant conduction was not uniform, this may affect the clinical outcomes. Fourthly, the successful rate of PVI may vary across medical centers due to variation in technical competencies, skills, and outcome measures. As such, the readers are advised to interpret the findings carefully. Nevertheless, funnel plot analysis revealed no significant publication bias. RCTs on CB-2G did not include a high number of participants and additional clinical trials are needed to confirm these findings.
In conclusion, regular adoption of adenosine test could not further improve PVI success rate basing on long-term observation and elimination of DCs provoked by adenosine after CPVI did not significantly reduce AF recurrence after catheter ablation.
YX conceived and designed the study. YX and GT guided the study. CC and DL searched and screened studies independently and disagreements were resolved by adjudication with input from YX. XL, ZW, YL, and FZ helped finished the figures and tables. CC, DL, and GT finished the manuscript writing. JH and TL helped to refine the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor is currently editing co-organizing a Research Topic with one of the authors GT, and confirms the absence of any other collaboration.
AF, atrial fibrillation; CPVI, circumferential pulmonary vein isolation; PVI, pulmonary vein isolation; DC, dormant conduction; PVs, pulmonary veins
Arentz, T., Macle, L., Kalusche, D., Hocini, M., Jais, P., Shah, D., et al. (2004). “Dormant” pulmonary vein conduction revealed by adenosine after ostial radiofrequency catheter ablation. J. Cardiovasc. Electrophysiol. 15, 1041–1047. doi: 10.1046/j.1540-8167.2004.04031.x
Cheung, J. W., Lin, F. S., Ip, J. E., Bender, S. R., Siddiqi, F. K., Liu, C. F., et al. (2013). Adenosine-induced pulmonary vein ectopy as a predictor of recurrent atrial fibrillation after pulmonary vein isolation. Circ. Arrhythm. Electrophysiol. 6, 1066–1073. doi: 10.1161/CIRCEP.113.000796
Chugh, S. S., Havmoeller, R., Narayanan, K., Singh, D., Rienstra, M., Benjamin, E. J., et al. (2014). Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation 129, 837–847. doi: 10.1161/CIRCULATIONAHA.113.005119
Compier, M. G., De Riva, M., Dyrda, K., Zeppenfeld, K., Schalij, M. J., and Trines, S. A. (2015). Incidence and predictors of dormant conduction after cryoballoon ablation incorporating a 30-min waiting period. Europace 17, 1383–1390. doi: 10.1093/europace/euu411
Datino, T., Macle, L., Qi, X. Y., Maguy, A., Comtois, P., Chartier, D., et al. (2010). Mechanisms by which adenosine restores conduction in dormant canine pulmonary veins. Circulation 121, 963–972. doi: 10.1161/CIRCULATIONAHA.109.893107
Elayi, C. S., Di Biase, L., Bai, R., Burkhardt, J. D., Mohanty, P., Santangeli, P., et al. (2013). Administration of isoproterenol and adenosine to guide supplemental ablation after pulmonary vein antrum isolation. J. Cardiovasc. Electrophysiol. 24, 1199–1206. doi: 10.1111/jce.12252
Gepstein, L., Hayam, G., and Ben-Haim, S. A. (1997). A novel method for nonfluoroscopic catheter-based electroanatomical mapping of the heart. In vitro and in vivo accuracy results. Circulation 95, 1611–1622. doi: 10.1161/01.CIR.95.6.1611
Ghanbari, H., Jani, R., Hussain-Amin, A., Al-Assad, W., Huether, E., Ansari, S., et al. (2016). Role of adenosine after antral pulmonary vein isolation of paroxysmal atrial fibrillation: a randomized controlled trial. Heart Rhythm 13, 407–415. doi: 10.1016/j.hrthm.2015.10.016
Haïssaguerre, M., Jaïs, P., Shah, D. C., Garrigue, S., Takahashi, A., Lavergne, T., et al. (2000). Electrophysiological end point for catheter ablation of atrial fibrillation initiated from multiple pulmonary venous foci. Circulation 101, 1409–1417. doi: 10.1161/01.CIR.101.12.1409
Higgins, J., and Green, S. (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Library. Chichester: John Wiley & Sons.
Ho, S. Y., Cabrera, J. A., Tran, V. H., Farré, J., Anderson, R. H., and Sánchez-Quintana, D. (2001). Architecture of the pulmonary veins: relevance to radiofrequency ablation. Heart 86, 265–270. doi: 10.1136/heart.86.3.265
Hocini, M., Sanders, P., Jaïs, P., Hsu, L. F., Weerasoriya, R., Scavée, C., et al. (2005). Prevalence of pulmonary vein disconnection after anatomical ablation for atrial fibrillation: consequences of wide atrial encircling of the pulmonary veins. Eur. Heart J. 26, 696–704. doi: 10.1093/eurheartj/ehi096
Jaïs, P., Cauchemez, B., Macle, L., Daoud, E., Khairy, P., Subbiah, R., et al. (2008). Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation 118, 2498–2505. doi: 10.1161/CIRCULATIONAHA.108.772582
Kaitani, K., Kurotobi, T., Kobori, A., Okajima, K., Yao, T., Nakazawa, Y., et al. (2014). Late re-conduction sites in the second session after pulmonary vein isolation using adenosine provocation for atrial fibrillation. Europace 16, 521–527. doi: 10.1093/europace/eut258
Kim, J. Y., Kim, S. H., Song, I. G., Kim, Y. R., Kim, T. S., Kim, J. H., et al. (2016). Achievement of successful pulmonary vein isolation: methods of adenosine testing and incremental benefit of exit block. J. Interv. Card. Electrophysiol. 46, 315–324. doi: 10.1007/s10840-016-0122-9
Kirchhof, P., Benussi, S., Kotecha, D., Ahlsson, A., Atar, D., Casadei, B., et al. (2017). 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 70:50. doi: 10.1016/j.rec.2016.11.033
Kobori, A., Shizuta, S., Inoue, K., Kaitani, K., Morimoto, T., Nakazawa, Y., et al. (2015). Adenosine triphosphate-guided pulmonary vein isolation for atrial fibrillation: the UNmasking dormant electrical reconduction by adenosine triphosphate (UNDER-ATP) trial. Eur. Heart J. 36, 3276–3287. doi: 10.1093/eurheartj/ehv457
Kumagai, K., Naito, S., Nakamura, K., Hayashi, T., Fukazawa, R., Sato, C., et al. (2010). ATP-induced dormant pulmonary veins originating from the carina region after circumferential pulmonary vein isolation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 21, 494–500. doi: 10.1111/j.1540-8167.2009.01667.x
Kumar, N., Dinh, T., Phan, K., Timmermans, C., Philippens, S., Dassen, W., et al. (2015). Adenosine testing after second-generation cryoballoon ablation (ATSCA) study improves clinical success rate for atrial fibrillation. Europace. 17, 871–876. doi: 10.1093/europace/euu352
Lin, F. S., Ip, J. E., Markowitz, S. M., Liu, C. F., Thomas, G., Lerman, B. B., et al. (2015). Limitations of dormant conduction as a predictor of atrial fibrillation recurrence and pulmonary vein reconnection after catheter ablation. Pacing Clin. Electrophysiol. 38, 598–607. doi: 10.1111/pace.12596
Linz, D., Kadhim, K., Lau, D., and Sanders, P. (2018). Recovery of adenosine-sensitive dormant conduction is but one mechanism of pulmonary vein reconnection. Indian Pacing Electrophysiol. J. 18, 201–202. doi: 10.1016/j.ipej.2018.10.003
Macle, L., Khairy, P., Weerasooriya, R., Novak, P., Verma, A., Willems, S., et al. (2015). Adenosine-guided pulmonary vein isolation for the treatment of paroxysmal atrial fibrillation: an international, multicentre, randomised superiority trial. Lancet 386, 672–679. doi: 10.1016/S0140-6736(15)60026-5
Matsuo, S., Yamane, T., Date, T., Hioki, M., Ito, K., Narui, R., et al. (2010). Comparison of the clinical outcome after pulmonary vein isolation based on the appearance of adenosine-induced dormant pulmonary vein conduction. Am. Heart J. 160, 337–345. doi: 10.1016/j.ahj.2010.05.025
McLellan, A. J., Kumar, S., Smith, C., Morton, J. B., Kalman, J. M., and Kistler, P. M. (2013). The role of adenosine following pulmonary vein isolation in patients undergoing catheter ablation for atrial fibrillation: a systematic review. J. Cardiovasc. Electrophysiol. 24, 742–751. doi: 10.1111/jce.12121
McLellan, A. J. A., Kumar, S., Smith, C., Ling, L. H., Prabhu, S., Kalman, J. M., et al. (2017). The role of adenosine challenge in catheter ablation for atrial fibrillation: a systematic review and meta-analysis. Int J Cardiol. 236, 253–261. doi: 10.1016/j.ijcard.2017.01.070
Miyazaki, S., Kuwahara, T., Kobori, A., Takahashi, Y., Takei, A., Sato, A., et al. (2012). Impact of adenosine-provoked acute dormant pulmonary vein conduction on recurrence of atrial fibrillation. J. Cardiovasc. Electrophysiol. 23, 256–260. doi: 10.1111/j.1540-8167.2011.02195.x
Nakagawa, H., Antz, M., Wong, T., Schmidt, B., Ernst, S., Ouyang, F., et al. (2007). Initial experience using a forward directed, high-intensity focused ultrasound balloon catheter for pulmonary vein antrum isolation in patients with atrial fibrillation. J. Cardiovasc. Electrophysiol. 18, 136–144. doi: 10.1111/j.1540-8167.2006.00715.x
Oral, H., Scharf, C., Chugh, A., Hall, B., Cheung, P., Good, E., et al. (2003). Catheter ablation for paroxysmal atrial fibrillation: segmental pulmonary vein ostial ablation versus left atrial ablation. Circulation 108, 2355–2360. doi: 10.1161/01.CIR.0000095796.45180.88
Ouyang, F., Antz, M., Ernst, S., Hachiya, H., Mavrakis, H., Deger, F. T., et al. (2005). Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation 111, 127–135. doi: 10.1161/01.CIR.0000151289.73085.36
Ouyang, F., Bänsch, D., Ernst, S., Schaumann, A., Hachiya, H., Chen, M., et al. (2004). Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double-Lasso technique in paroxysmal atrial fibrillation. Circulation 110, 2090–2096. doi: 10.1161/01.CIR.0000144459.37455.EE
Pappone, C., Manguso, F., Vicedomini, G., Gugliotta, F., Santinelli, O., Ferro, A., et al. (2004). Prevention of iatrogenic atrial tachycardia after ablation of atrial fibrillation: a prospective randomized study comparing circumferential pulmonary vein ablation with a modified approach. Circulation 110, 3036–3042. doi: 10.1161/01.CIR.0000147186.83715.95
Rostock, T., O'Neill, M. D., Sanders, P., Rotter, M., Jaïs, P., Hocini, M., et al. (2006). Characterization of conduction recovery across left atrial linear lesions in patients with paroxysmal and persistent atrial fibrillation. J. Cardiovasc. Electrophysiol. 17, 1106–1111. doi: 10.1111/j.1540-8167.2006.00585.x
Schaeffer, B., Willems, S., Sultan, A., Hoffmann, B. A., Lüker, J., Schreiber, D., et al. (2015). Loss of pace capture on the ablation line during pulmonary vein isolation versus “dormant conduction”: is adenosine expendable? J. Cardiovasc. Electrophysiol. 26, 1075–1080. doi: 10.1111/jce.12759
Tebbenjohanns, J., Hofer, C., Bergmann, L., Dedroogh, M., Gaudin, D., von Werder, A., et al. (2016). Shortening of freezing cycles provides equal outcome to standard ablation procedure using second-generation 28 mm cryoballoon after 15-month follow-up. Europace 18, 206–210. doi: 10.1093/europace/euv189
Thacker, E. L., McKnight, B., Psaty, B. M., Longstreth, Jr. W. T, Dublin, S., et al. (2013). Association of body mass index, diabetes, hypertension, and blood pressure levels with risk of permanent atrial fibrillation. J. Gen. Intern. Med. 28, 247–253. doi: 10.1007/s11606-012-2220-4
Theis, C., Konrad, T., Mollnau, H., Sonnenschein, S., Kämpfner, D., Potstawa, M., et al. (2015). Arrhythmia termination versus elimination of dormant pulmonary vein conduction as a procedural end point of catheter ablation for paroxysmal atrial fibrillation: a prospective randomized trial. Circ. Arrhythm. Electrophysiol. 8, 1080–1087. doi: 10.1161/CIRCEP.115.002786
Tse, G., Lai, E. T., Yeo, J. M., Tse, V., and Wong, S. H. (2016). Mechanisms of electrical activation and conduction in the gastrointestinal system: lessons from cardiac electrophysiology. Front. Physiol. 7:182. doi: 10.3389/fphys.2016.00182
Van Belle, Y. L., Janse, P. A., de Groot, N. M., Anné, W., Theuns, D. A., and Jordaens, L. J. (2012). Adenosine testing after cryoballoon pulmonary vein isolation improves long-term clinical outcome. Neth. Heart J. 20, 447–455. doi: 10.1007/s12471-012-0319-1
Keywords: adenosine, dormant conduction, atrial fibrillation, circumferential pulmonary vein isolation, meta-analysis
Citation: Chen C, Li D, Ho J, Liu T, Li X, Wang Z, Lin Y, Zou F, Tse G and Xia Y (2019) Clinical Implications of Unmasking Dormant Conduction After Circumferential Pulmonary Vein Isolation in Atrial Fibrillation Using Adenosine: A Systematic Review and Meta-Analysis. Front. Physiol. 9:1861. doi: 10.3389/fphys.2018.01861
Received: 30 November 2017; Accepted: 11 December 2018;
Published: 17 January 2019.
Edited by:
Jichao Zhao, The University of Auckland, New ZealandReviewed by:
Arun V. Holden, University of Leeds, United KingdomCopyright © 2019 Chen, Li, Ho, Liu, Li, Wang, Lin, Zou, Tse and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gary Tse, dHNlZ0BjdWhrLmVkdS5oaw==
Yunlong Xia, eXVubG9uZ194aWFAMTI2LmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.