
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol. , 12 March 2025
Sec. Ethnopharmacology
Volume 16 - 2025 | https://doi.org/10.3389/fphar.2025.1550759
 Qiuhan Chen1
Qiuhan Chen1 He Wang2
He Wang2 Lin Zhu1
Lin Zhu1 Ziyi Guo2
Ziyi Guo2 Yingying Cui3
Yingying Cui3 Jifang Ban1
Jifang Ban1 Kuo Chi1
Kuo Chi1 Na Shi1
Na Shi1 Boyu Wang1
Boyu Wang1 Changxing Liu1
Changxing Liu1 Yabin Zhou2*
Yabin Zhou2*Objectives: Several studies have explored the efficacy and safety of various traditional Chinese medicine (TCM) injections for unstable angina pectoris. However, comprehensive systematic evidence confirming the advantages of these injections is still lacking. This Bayesian network meta-analysis was carried out to evaluate and compare the efficacy of different TCM injections in treating unstable angina pectoris.
Methods: A systematic search was implemented across PubMed, Cochrane Library, Embase, and Web of Science, with the date of search cutoff being February 2024. The Cochrane risk of bias tool was utilized to evaluate the bias risk in the included studies.
Results: A total of 44 studies, encompassing 4,362 patients with unstable angina pectoris and 21 types of injections, were included. Compared with the standard treatment group, Danhong injection (SMD = −1.1, 95% CrI: -2.0, −0.15), Danshen Chuanxiongqin injection (SMD = −1.9, 95% CrI: -3.7, −0.12), Ginkgo Damole injection (SMD = −2.5, 95% CrI: -4.8, −0.29), Puerarin injection (SMD = −1.8, 95% CrI: -3.2, −0.37), and Shuxuetong injection (SMD = −7.8, 95% CrI: -13, −2.3) were found to significantly reduce the frequency of angina attacks. However, no significant improvement was observed in the duration of angina episodes with any of the included TCM injections compared with the standard treatment group. There was no significant difference in the incidence of adverse events from TCM injections.
Conclusion: Adjunctive treatment with TCM injections, in addition to conventional therapy, can remarkably reduce the frequency of angina attacks and demonstrates a favorable safety profile. However, it does not appear to significantly reduce the duration of angina episodes. Future studies should include more multicenter populations to validate our conclusions, as the population included in this study was predominantly Chinese.
Systematic Review Registration: identifier [CRD42024501984].
Unstable angina pectoris (UAP), which lies between acute myocardial infarction and stable angina, is a clinical state resulting from acute myocardial ischemia and is categorized under acute coronary syndrome (ACS). One-third of deaths worldwide are due to cardiovascular disease (Roth et al., 2020). The risk factors include age, dyslipidemia, diabetes mellitus, and hypertension. UAP is a complex condition that significantly affects patients’ quality of life. Studies have indicated that approximately 30% of UAP patients progress to myocardial infarction within 3–4 months after onset (Braunwald et al., 2002), with a high mortality.
Currently, treatment regimens for UAP vary widely, focusing on invasive procedures and drug therapy (AuthorAnonymous, 2024). Common invasive procedures for UAP include percutaneous coronary intervention and coronary artery bypass grafting (Bhatt et al., 2022). Drug therapy for UAP includes several classes of medications (Roth et al., 2020): anti-ischemic agents, such as nitrates (for example, nitroglycerin) and β-blockers (for example, metoprolol) (Braunwald et al., 2002); antiplatelet agents, including COX inhibitors (for example, aspirin) and glycoprotein IIb/IIIa receptor antagonists (for example, tirofiban) (AuthorAnonymous, 2024); anticoagulants, such as heparin and low-molecular-weight heparin (Bhatt et al., 2022); lipid-lowering agents, such as statins, which reduce lipids and prevent thrombosis; and (Huang et al., 2024) antihypertensives, including angiotensin-converting enzyme inhibitors and β-blockers. Remote ischemic conditioning has been shown to reduce peak troponin levels and the risk of T4aMI and MACE (Huang et al., 2024). However, despite the effectiveness of biomedical treatments, they are often associated with adverse reactions. For instance, aspirin can cause hypersensitivity reactions (Laidlaw and Cahill, 2017), and in older patients, it increases the overall risk of gastrointestinal hemorrhage by 60% (Mahady et al., 2021). Also, heparin and its derivatives may induce hyperkalemia as a drug-related adverse effect (Ben Salem et al., 2014).
TCM has attracted global attention and has been widely used in clinical practice in recent years. It has demonstrated multi-target, multi-level, and multi-pathway effects in treating coronary artery disease by regulating lipid metabolism, inhibiting inflammatory responses, and protecting myocardial cells. Among oral TCM formulations, Shengshao capsules, Naoxintong capsules, Yinxing Tongzhi dropping pills, and compound Danshen dropping pills have been shown to be effective in treating UAP (Zhang et al., 2021). TCM injections, such as Danhong injection and Danshen injection, are gradually being used for this disease. Moreover, some original studies have indicated that TCM injections offer advantages over standard biomedicine alone. In addition, the therapeutic efficacy of diversified TCM injection treatment regimens remains a subject of debate. Although multiple TCM injections have been revealed to be effective in the treatment of UAP, many questions remain to be studied. For instance, are these injections effective in reducing the frequency of attacks or duration of attacks? Do they effectively reduce both the frequency and duration of attacks, or are they only effective for one of these outcomes? Are they more effective than conventional treatments? Do they carry an increased risk of adverse events? Some systematic reviews (Zhang D. et al., 2016; Ma et al., 2015) have assessed the efficacy and safety of TCM injections in the treatment of UAP. However, given the wide variety of TCM injections used in UAP management, the differences in efficacy among different TCM injections remain to be fully explored. Thus, in order to provide evidence-based recommendations for the clinical usage of TCM injections in the treatment of unstable angina, we carried out this systematic review and Bayesian network meta-analysis to compile the clinical efficacy of these TCM injections.
This study was implemented per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses (PRISMA-NMA) guidelines and was registered with PROSPERO prospectively (ID: CRD42024501984).
P (Population): The target population for this systematic review consisted of patients diagnosed with UAP.
I (Intervention): The intervention for this systematic review included various TCM injections. The information on the components of the traditional Chinese medicine injections discussed in this study can be found in Supplementary Table S1.
C (Comparison): The comparison group consisted of traditional biomedical treatments.
O (Outcome): Frequency and duration of angina attacks.
S (Study design): Randomized controlled trials (RCTs).
Conference abstracts published without peer review;
Studies that only compared different doses or frequencies of the same injection within the original research, as these cannot be linked with other interventions in a Bayesian network meta-analysis.
Studies with very small sample sizes (<10 cases) in the original research, as these are prone to operational errors. Studies with limited subjects are more susceptible to measurement errors. Therefore, these studies with limited subjects should be excluded. In addition, studies with a total of less than 10 subjects in 2 groups had difficulty in meeting statistical efficiency, requiring the exclusion of these studies.
PubMed, Cochrane Library, Embase, Web of Science, CNKI, Wanfang, VIP, and the Chinese Biomedical Database were all thoroughly searched. The initial search was conducted on 1 November 2023, followed by a supplementary search in February 2024 to minimize the risk of omitting relevant studies. The search strategy utilized a combination of MeSH and free text terms, with no restrictions on region or publication date.
Duplicate articles were removed after the retrieved articles were imported into Endnote. After that, titles and abstracts of the remaining research were examined in order to determine which ones were preliminary eligible investigations. Full texts of the remaining were obtained and examined to determine which studies were suitable for inclusion in this systematic review. Two researchers (CQH, WH) carried out the study selection process independently, followed by cross-checking. A third researcher (ZL) was consulted to settle any disagreements.
A standardized data extraction form was created before any data was extracted. The extracted data included: title, first author, publication year, patient source, country of origin, sample size, total population, age, gender, intervention type, detailed intervention protocol, frequency per day, course of treatment, and outcome measures. Data extraction was independently carried out by two researchers (CQH, WH), followed by cross-checking. Discrepancies were resolved by a third researcher (ZL).
The Cochrane Collaboration’s tool for evaluating the risk of bias in RCTs was used to determine the bias risk. This tool includes the following seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. Regarding the generation of the random sequence, some studies failed to provide the complete randomization and methods of random sequence. As a result, the assessment risks for these studies are unclear. Some studies employed pseudo-randomization methods, such as using the parity of admission IDs or grouping based on admission order. These studies were therefore assessed as having a high risk of bias. Regarding allocation concealment, some studies did not employ allocation concealment, leading to a high bias. Other studies employed allocation concealment but did not provide clear descriptions, resulting in an unclear risk of bias. However, some studies utilized opaque envelopes or computer-generated concealment, which were considered to have a low bias. For blinding, some studies implemented single-blind or double-blind procedures, leading to a low bias. Some studies did not employ blinding, resulting in a high risk of bias. In addition, some studies experienced breaches in blinding during implementation, further resulting in a high risk of bias. For the assessment of outcome measures, some studies did not blind assessors, which placed them at a high risk of bias. In contrast, other studies effectively corrected for potential biases in later stages of assessment, resulting in a low risk of bias. Some studies did not provide adequate descriptions of their blinding procedures, leaving the risk of bias unclear. For data integrity, some randomized controlled trials or follow-ups experienced certain data loss. When the data loss is less than 20%, it is generally considered that there is no significant publication bias. The reason for this is that when conducting randomized controlled trials, many studies establish a threshold for follow-up loss of 10%–20% when estimating the number of cases. During selective reporting, some studies set outcomes to be assessed at the onset of the study. If selective reporting of outcomes occurred during the assessment of outcome measures, these studies were considered to have a high risk of bias. Every domain was assessed to have a low, high, or unclear risk of bias. Two researchers (CQH, WH) carried out the risk of bias assessment independently, followed by cross-checking. A third researcher (ZL) was consulted to settle any disagreements.
This study aims to compare the advantages of multiple (>2) types of TCM injections in treating UAP. Traditional meta-analysis can only compare the differences between two interventions, and using a subgroup approach to compare multiple interventions can increase the risk of type I errors. Therefore, a network meta-analysis is necessary. Network meta-analysis includes meta-analysis based on frequency and Bayesian theories. In this study, Bayesian network meta-analysis was chosen over the frequentist meta-analysis due to its unique advantages. On the one hand, Bayesian analysis allows for the incorporation of prior knowledge and new data to update the level of confidence for a hypothesis. This provides a more flexible framework for addressing uncertainty in clinical research. In particular, when dealing with studies with small sample sizes or rare diseases, Bayesian methods can utilize results from previous studies as prior distributions, thereby enhancing the capability of statistical inference. Furthermore, Bayesian analysis directly provides a posterior probability distribution, which allows for the direct quantification of parameter estimates and their degree of uncertainty. Therefore, this approach can provide more comprehensive information compared to traditional P-values.
The network meta-analysis used a Bayesian random-effects model to compare the efficacy of different interventions. The modeling process was conducted via the Markov Chain Monte Carlo (MCMC) method, with four Markov chains running concurrently. The burn-in process was set to 20,000 iterations, followed by an additional 50,000 iterations to complete the model simulation. The deviance information criterion (DIC) was adopted to assess model fit and global consistency. In cases where the network included closed loops, the node-splitting method was applied to evaluate local consistency. In addition, a league table was created to assess the variations in effect between the different interventions. Treatments were then ordered according to the surface under the cumulative ranking curve (SUCRA). To evaluate study heterogeneity graphically, a funnel plot was used.
Model convergence means that the Markov Chain Monte Carlo (MCMC) algorithm has thoroughly explored the posterior distribution and has reached a steady state. This guarantees the authenticity and representativeness of the sampling results. Convergence is typically assessed by examining Gelman-Rubin diagnostic indicators, observing trace plots, calculating effective sample sizes, and other approaches. If multiple independent chains show similar trends and the R-hat value approaches 1, it indicates successful model convergence. Additionally, to evaluate model performance, its predictive performance and generalizability should be tested. These evaluations can be conducted through cross-validation or by using an independent test set for assessment. Stata v15.0 (Stata Corporation, College Station, TX) and R v4.4.1 (R Development Core Team, Vienna) were employed for the analysis.
A total of 14,750 articles were retrieved from the databases. After excluding 8,429 duplicates, 65 articles were reviewed by reading their titles and abstracts. The full texts were then downloaded and thoroughly assessed. We excluded 1 study that was a duplicate publication of the same RCT under different outcomes or populations, 10 studies that did not have relevant outcome measures, 8 studies with non-matching interventions, and 2 non-RCT studies. Ultimately, 44 original studies were included in our analysis (Zhang et al., 2022; Miao and Hu, 2013; Gao et al., 2009; Zhang et al., 2019; Ning et al., 2011; Liu et al., 2008; Wang et al., 2002; Chen, 2004; Liu and Zhang, 2022; Wang, 2021; Wang et al., 2012; Yong and Liu, 2010; Gong, 2014; Li and Zhou, 2015; Zhang and Lu, 2016; Wang, 2009; Zhang et al., 2014; Kudereti, 2016; Li and Zhang, 2018; Quan, 2011; Luo, 2014; Li, 2015; Pan et al., 2013; Zhang, 2007; Shi, 2007; Yao and Jin, 2022; Zeng et al., 2015; Yang et al., 2014; Li et al., 2016; Liu et al., 2021; Ren et al., 2018; Qiu et al., 2008; Han and Wen, 2010; Zhou and Liu, 2007; Song and Bannu, 2009; Peng, 2014; Fang, 2006; Chen and Y, 2009; Zheng and Wang, 2006; Zhang, 2006; Pu et al., 2015; Meng, 2004; Zhou, 2008), and the PRISMA flow diagram for searching was displayed in Figure 1.
The included studies were published between 2002 and 2022 and involved 4,362 patients with UAP. These studies examined 21 different TCM injections. Danhong injection was the most frequently studied, appearing in 12 studies (Miao and Hu, 2013; Gao et al., 2009; Ning et al., 2011; Liu et al., 2008; Gong, 2014; Wang, 2009; Zhang et al., 2014; Li and Zhang, 2018; Pan et al., 2013; Yao and Jin, 2022; Zeng et al., 2015; Zhou, 2008). Other injections included Puerarin (5 studies) (Chen, 2004; Fang, 2006; Chen and Y, 2009; Zheng and Wang, 2006; Meng, 2004), Danshen Chuanxiongqin injection (Li and Zhang, 2018; Yang et al., 2014; Ren et al., 2018), and Xueshuantong injection (Kudereti, 2016; Luo, 2014; Qiu et al., 2008), each appearing in 3 studies. Additional injections studied included Compound Danshen injection (Wang et al., 2002; Song and Bannu, 2009), Danshen injection (Liu et al., 2008; Yong and Liu, 2010), Dengzhanxixin injection (Wang et al., 2012; Yong and Liu, 2010), Ginkgo Damole injection (Quan, 2011; Pu et al., 2015), Shuxuening (Ginkgo Leaf) injection (Wang, 2021; Zhou and Liu, 2007), Gualoupi injection (Zhang, 2007; Song and Bannu, 2009), Ligustrazine hydrochloride injection (Han and Wen, 2010; Peng, 2014), Xingxiong sodium chloride injection (Yao and Jin, 2022; Liu et al., 2021), each appearing in 2 studies, and Guanxinning injection (Zhang, 2006), Hongjingtian injection (Zhang and Lu, 2016), Kudiezi injection (Liu and Zhang, 2022), Safflower yellow pigment injection (Li et al., 2016), Salvianolate injection (Zhai and Jiaol, 2013), Shenmai injection (Li, 2015), Shenxiong glucose injection (Li and Zhou, 2015), Shuxuetong injection (Wang et al., 2002), and Tanshinone injection (Zhang, 2007), each appearing in 1 study. The course of treatment ranged from 2 weeks to 24 weeks (Supplementary Table S2).
All the studies included were RCTs. However, 27 studies described randomization without specifying the exact method used, leading to a classification of low risk of bias. Allocation concealment and blinding were generally not well described, resulting in unclear risk of bias in these domains. There were no significant concerns regarding attrition bias, reporting bias, or other biases, hence these were classified as low risk of bias (Figures 2, 3).
A total of 44 studies (Zhang et al., 2022; Miao and Hu, 2013; Gao et al., 2009; Zhang et al., 2019; Ning et al., 2011; Liu et al., 2008; Wang et al., 2002; Chen, 2004; Liu and Zhang, 2022; Wang, 2021; Wang et al., 2012; Yong and Liu, 2010; Gong, 2014; Li and Zhou, 2015; Zhang and Lu, 2016; Wang, 2009; Zhang et al., 2014; Kudereti, 2016; Li and Zhang, 2018; Quan, 2011; Luo, 2014; Li, 2015; Pan et al., 2013; Zhang, 2007; Shi, 2007; Yao and Jin, 2022; Zeng et al., 2015; Yang et al., 2014; Li et al., 2016; Liu et al., 2021; Ren et al., 2018; Qiu et al., 2008; Han and Wen, 2010; Zhou and Liu, 2007; Song and Bannu, 2009; Peng, 2014; Fang, 2006; Chen and Y, 2009; Zheng and Wang, 2006; Zhang, 2006; Pu et al., 2015; Meng, 2004; Zhou, 2008) reported on the frequency of angina attacks treated with TCM injections for UAP. Due to differences in the statistical units used, we employed the standardized mean difference (SMD) as the measure for the outcome. The analysis included 21 different TCM injections. The overall heterogeneity of these studies was 4%, and the DIC values for the consistency and inconsistency models were 88.17 and 88.15, respectively, with Danhong injection (Danhong, n = 12), Puerarin injection (Puerarin, n = 5), Danshen Chuanxiongqin injection (DanshenCXQ, n = 3), Xueshuantong injection (Xueshuantong, n = 3), Compound Danshen injection (CompoundDS, n = 2), Danshen injection (Danshen, n = 2), Dengzhanxixin injection (Dengzhanxixin, n = 2), Ginkgo Damole injection (GinkgoDamole, n = 2), Ginkgo Leaf injection (GinkgoLeaf, n = 2), Gualoupi injection (Gualoupi, n = 2), Ligustrazine hydrochloride injection (LigustrazineH, n = 2), Xingxiong sodium chloride injection (Xingxiong, n = 2), Guanxinning injection (Guanxinning, n = 1), Hongjingtian injection (Hongjingtian, n = 1), Kudiezi injection (Kudiezi, n = 1), Safflower yellow pigment injection (Saffloweryellow, n = 1), Salvianolate injection (Salvianolate, n = 1), Shenmai injection (Shenmai, n = 1), Shenxiong glucose injection (Shenxiong, n = 1), Shuxuetong injection (Shuxuetong, n = 1), and Tanshinone injection (Tanshinone, n = 1) included in the network diagram (Figure 4).
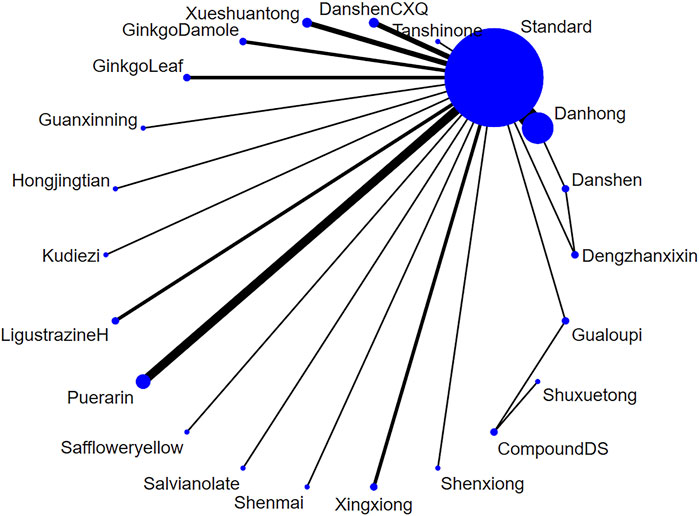
Figure 4. The network relationship of various injections for the frequency of unstable angina pectoris (Note: Each blue circle represents an intervention. A larger diameter indicates that more studies were included for that intervention. A line connecting two blue circles represents a direct comparison between two interventions. A thicker line indicates a higher number of studies comparing the two interventions.).
The network meta-analysis results indicated that Shuxuetong, Danshen Chuanxiongqin, and Puerarin were the top three interventions in terms of effectiveness for reducing the frequency of angina attacks. Compared with the standard treatment group, Danhong injection (SMD = −1.1, 95% CrI: −2.0, −0.15), Danshen Chuanxiongqin injection (SMD = −1.9, 95% CrI: −3.7, −0.12), Ginkgo Damole injection (SMD = −2.5, 95% CrI: −4.8, −0.29), Puerarin injection (SMD = −1.8, 95% CrI: −3.2, −0.37), and Shuxuetong injection (SMD = −7.8, 95% CrI: −13, −2.3) significantly reduced the frequency of angina attacks (Figure 5; Supplementary Table S3).
A total of 38 studies (Zhang et al., 2022; Miao and Hu, 2013; Gao et al., 2009; Zhang et al., 2019; Ning et al., 2011; Liu et al., 2008; Wang et al., 2002; Chen, 2004; Liu and Zhang, 2022; Wang, 2021; Wang et al., 2012; Yong and Liu, 2010; Gong, 2014; Li and Zhou, 2015; Zhang and Lu, 2016; Wang, 2009; Zhang et al., 2014; Kudereti, 2016; Li and Zhang, 2018; Quan, 2011; Luo, 2014; Li, 2015; Pan et al., 2013; Zhang, 2007; Shi, 2007; Yao and Jin, 2022; Zeng et al., 2015; Yang et al., 2014; Li et al., 2016; Liu et al., 2021; Ren et al., 2018; Qiu et al., 2008; Han and Wen, 2010; Zhou and Liu, 2007; Song and Bannu, 2009; Peng, 2014; Fang, 2006; Zhai and Jiaol, 2013) reported on the duration of angina attacks treated with TCM injections for UAP. Due to heterogeneity in the measurement units across studies, SMD was adopted as the measure for the outcome. The analysis included 20 different TCM injections. The overall heterogeneity of these studies was 4%, and the DIC values for the consistency and inconsistency models were 76.21 and 76.14, respectively, with Danhong injection (Danhong, n = 11), Danshen Chuanxiongqin injection (DanshenCXQ, n = 3), Xueshuantong injection (Xueshuantong, n = 3), Compound Danshen injection (CompoundDS, n = 2), Danshen injection (Danshen, n = 2), Puerarin injection (Puerarin, n = 2), Dengzhanxixin injection (Dengzhanxixin, n = 2), Ginkgo Leaf injection (GinkgoLeaf, n = 2), Gualoupi injection (Gualoupi, n = 2), Ligustrazine hydrochloride injection (LigustrazineH, n = 2), Xingxiong sodium chloride injection (Xingxiong, n = 2), Hongjingtian injection (Hongjingtian, n = 1), Kudiezi injection (Kudiezi, n = 1), Ginkgo Damole injection (GinkgoDamole, n = 1), Safflower yellow pigment injection (Saffloweryellow, n = 1), Salvianolate injection (Salvianolate, n = 1), Shenmai injection (Shenmai, n = 1), Shenxiong glucose injection (Shenxiong, n = 1), Shuxuetong injection (Shuxuetong, n = 1), and Tanshinone injection (Tanshinone, n = 1) included in the network diagram (Figure 6).
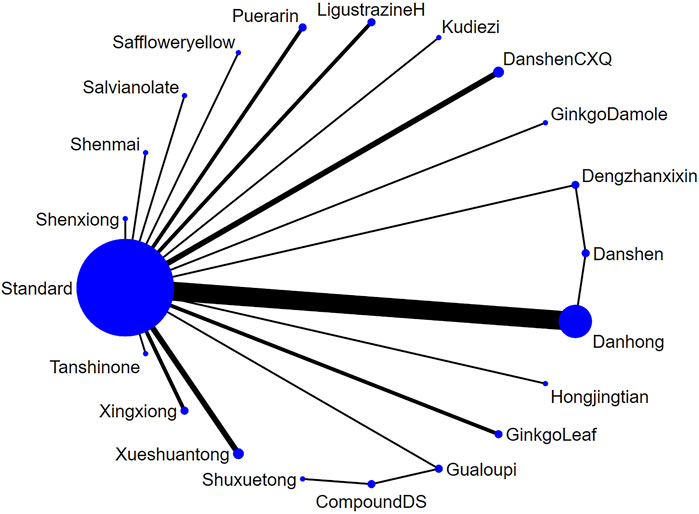
Figure 6. The network relationship of various injections for the duration of unstable angina pectoris. (Note: Each blue circle represents an intervention. A larger diameter indicates that more studies were included for that intervention. A line connecting two blue circles represents a direct comparison between two interventions. A thicker line indicates a higher number of studies comparing the two interventions.)
The network meta-analysis results indicated that Shuxuetong, Puerarin, and Xingxiong were the top three interventions in terms of effectiveness for reducing the duration of angina attacks. However, when comparing the experimental groups receiving TCM injections with the standard treatment group, no notable differences were observed in improving the duration of angina attacks (Figure 7; Supplementary Table S4).
A total of 22 studies reported adverse events of TCM injections in treating UAP. Adverse events occurred in 14 of 314 subjects treated with Danhong injection, 4 of 126 patients treated with Danshen Chuanxiongqin injection, 3 of 60 patients treated with Dengzhanxin injection, 6 of 145 patients treated with Ginkgo Leaf injection, 2 of 30 patients treated with Guanxinning injection, 6 of 43 patients treated with Kudiezi injection, 1 of 43 patients treated with Ligustrazine hydrochloride injection, 1 of 92 patients treated with Puerarin injection, 7 of 98 patients treated with Xingxiong sodium chloride injection, and 14 of 153 patients treated with Xueshantong injection. Ten injections and standard treatment regimens were included. The overall heterogeneity across these studies was 0%, and the DIC values for the consistency and inconsistency models were 63.53 and 61.84, respectively. Specifically, these include Danhong injection (Danhong, n = 6), Danshen Chuanxiongqin injection (DanshenCXQ, n = 2), Dengzhanxixin injection (Dengzhanxixin, n = 1), Ginkgo Leaf injection (GinkgoLeaf, n = 2), Guanxinning injection (Guanxinning, n = 1), Kudiezi injection (Kudiezi, n = 1), Ligustrazine hydrochloride injection (LigustrazineH, n = 1), Puerarin injection (Puerarin, n = 3), Xingxiong injection (Xingxiong, n = 2), Xueshuantong injection (Xueshuantong, n = 3) and standard treatment regimen (Standard, n = 22) (Figure 8).
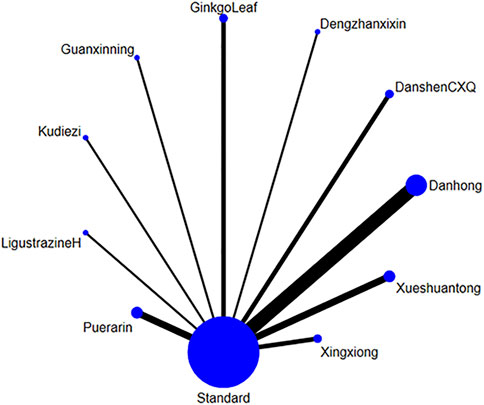
Figure 8. The network relationship of various injections for AEs of unstable angina pectoris. (Note: Each blue circle represents an intervention. A larger diameter indicates that more studies were included for that intervention. A line connecting two blue circles represents a direct comparison between two interventions. A thicker line indicates a higher number of studies comparing the two interventions.)
The results of the network meta-analysis revealed that there were no significant differences in the risk of adverse events across various TCM injections (Figure 9; Supplementary Table S5).
Currently, there are diverse treatment regimens involving TCM injections for UAP. Our study found that TCM injections demonstrated efficacy in reducing both the frequency and duration of angina attacks. Specifically, Shuxuetong injection, Danshen Chuanxiongqin injection, and Puerarin injection were effective in reducing the frequency of angina attacks, while Shuxuetong injection, Puerarin injection, and Xingxiong sodium chloride injection were effective in reducing the duration of angina attacks.
Pharmacological research indicated that Danhong injection can reduce blood viscosity and increase blood flow velocity, thereby correcting myocardial ischemia by establishing collateral circulation and enhancing coronary blood flow. This mechanism can greatly improve clinical outcomes by reducing the frequency of angina attacks (Qin et al., 2020). A systematic evaluation of Danhong injection for treating ACS demonstrated that, in combination with standard biomedical treatment, Danhong injection more effectively increased the overall efficacy rate, reduced inflammatory cytokines such as high-sensitivity C-reactive protein (hs-CRP) and interleukin-6 (IL-6), lowered plasma viscosity, and reduced levels of plasma endothelin-1 (ET-1) and brain natriuretic peptide (BNP). Additionally, it decreased the production of myeloperoxidase (MPO) and the number of inverted T waves (Wu et al., 2015).
Danshen Chuanxiongqin injection, which contains the active ingredients of Danshensu and ligustrazine hydrochloride, promotes vasodilation to improve myocardial hypoxia and ischemia, inhibit phosphodiesterase activity, and prevents lipid deposition, thereby stabilizing atherosclerotic plaques (Guo, 2018; Bai et al., 2020; Liu and Xu, 2023). A systematic review of Danshen Chuanxiongqin injection showed that its combined use with standard biomedicine was more effective in increasing the total effective rate, especially in improving electrocardiogram (ECG) outcomes, indicating that Danshen Chuanxiongqin injection combined with biomedicine is effective in treating UAP (Zhang X. et al., 2016).
Ginkgo Damole injection, which contains Ginkgo biloba extract and dipyridamole, enhances coronary blood supply and dilation, reduces the rate of apoptosis in damaged cells, and thereby improves myocardial ischemia while maintaining the structural and functional integrity of cells (Yang, 2020; Li, 2019). Additionally, by inhibiting platelets, phosphodiesterase, and thromboxane A2, it also increases endogenous prostacyclin levels, thereby alleviating coronary artery disease symptoms (Fan and Yang, 2021; Feng and Liang, 2019). Xingxiong sodium chloride injection, composed of Ginkgo biloba extract and ligustrazine, has anticoagulant and antithrombotic effects. It can improve microcirculation, act against oxidative free radicals, promote the opening of collateral circulation, and protect ischemic cells. In addition, it can further modulate SDF-1 and CXCR7 expression levels, reduce oxidative stress, alleviate angina symptoms, and improve cardiac function (Zhang et al., 2022; Wu, 2019). Systematic reviews have shown that Ginkgo leaf extract injections (Sun et al., 2015; Liu et al., 2024) are beneficial for patients with angina. These injections have demonstrated efficacy in alleviating symptoms and myocardial ischemia while maintaining a good safety profile.
Puerarin injection (Jiang et al., 2022), primarily composed of an isoflavonoid metabolite derived from Pueraria lobata extract, has a marked effect on dilating coronary arteries. It effectively increases coronary blood flow and reduces vascular resistance (Tan and Li, 2020; Jiang et al., 2020). Puerarin also has antihypertensive properties and can inhibit serotonin (5-HT) release from thrombin-induced platelets, thereby mitigating risk factors that promote the progression of angina (Wang, 2020; He, 2020). Systematic reviews have shown that Puerarin injection (Gao et al., 2015; Shao et al., 2022) is superior to standard biomedicine alone in reducing angina symptoms and improving ECG findings. It also reduces the frequency and duration of angina attacks, nitroglycerin consumption, and plasma endothelin levels. These analyses revealed that the use of Puerarin injection is superior to conventional biomedicine alone in treating UAP.
As another effective TCM preparation, Shuxuetong is composed of Hirudo (leech) and Pheretima (earthworm), both of which have potent blood-activating and stasis-resolving effects. Modern pharmacological research has shown that hirudin, derived from leech, is the most potent specific thrombin inhibitor currently known (Moher et al., 1998). The extract from earthworms has been found to prolong thrombus formation time in the body and significantly reduce the dry weight and length of thrombi (Guo, 2017).
Safety analysis of the included studies demonstrated that TCM injections exhibited no significant differences in adverse events. Adverse events, such as headaches, dizziness, gastrointestinal reactions, and allergic reactions, were generally well tolerated by patients. In addition, the results of the network meta-analysis demonstrated that the risk of adverse events did not increase with the use of TCM injections compared to standard treatment. There was no significant difference in the incidence of adverse events across different TCM injections. Overall, reasonable use of TCM injections demonstrates favorable safety profiles when properly administered.
Multiple TCM injections are widely applied in the treatment of UAP. This study has demonstrated that the combination of TCM injections with conventional treatment contributes to decreasing the frequency and duration of UAP attacks, with a significant effect on reducing the frequency of angina attacks. The evidence suggests that a reasonable increase in TCM injection use can further improve the symptoms of UAP on the basis of conventional treatment. For patients with more frequent UAP attacks, Danhong injection, Danshen Chuanxiongqin injection, Ginkgo Damole injection, Puerarin injection, and Shuxuetong injection may be considered for adjuvant treatment. Compared to conventional treatment, TCM injections do not increase the incidence of adverse events. Therefore, TCM injections can continue to be used as an adjunct to conventional therapy.
Our research offered a thorough analysis of the effectiveness of different TCM injections for the treatment of UAP. However, several limitations should be noted. First, because TCM is rooted in Chinese culture, the studies included in our analysis were conducted exclusively on Chinese populations. It is hoped that further trials will be carried out with participants from diverse international backgrounds. Second, the studies we included were single-center clinical trials, which may introduce a certain level of bias during the research process. Third, in the studies we included, a substantial number did not report whether allocation concealment or blinding was implemented. As a result, this may pose certain limitations to the interpretation of the results, and further multicenter blinded studies are needed for validation in the future. Fourth, the included studies primarily reported on the frequency and duration of angina attacks, with fewer studies reporting other outcome measures. We hope that future research will explore a broader range of indicators to better assess the efficacy of TCM injections.
Study results demonstrated that TCM injections showed significant therapeutic effects in the treatment of UAP. When used as an adjunct to conventional treatment, TCM injections reduced the frequency of angina attacks, though they did not significantly decrease the duration of angina episodes. In addition, their use does not lead to a significant increase in the incidence of adverse events.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
QC: Conceptualization, Formal Analysis, Investigation, Methodology, Resources, Writing–original draft. HW: Formal Analysis, Investigation, Writing–review and editing. LZ: Formal Analysis, Investigation, Writing–review and editing. ZG: Formal Analysis, Investigation, Writing–review and editing. YC: Formal Analysis, Investigation, Writing–review and editing. JB: Writing–review and editing. KC: Formal Analysis, Investigation, Writing–review and editing. NS: Writing–review and editing. BW: Writing–review and editing. CL: Writing–review and editing. YZ: Funding acquisition, Writing–review and editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Administration of Traditional Chinese Medicine national famous old Chinese medicine experts inheritance studio construction project (grant number [Chinese Medicine Human Education and Development [2022] No. 75]).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1550759/full#supplementary-material
Bai, X. X., Liu, N. N., and Zhi, L. Q. (2020). Clinical effect of hyperbaric oxygen combined with salvia miltiorrhiza ligustrazine injection in the treatment of patients with coronary heart disease and angina pectoris. Clin Res Pract 5 (30), 31–33. doi:10.19347/j.cnki.2096-1413.202030012
Ben Salem, C., Badreddine, A., Fathallah, N., Slim, R., and Hmouda, H. (2014). Drug-induced hyperkalemia. Drug Saf. 37 (9), 677–692. doi:10.1007/s40264-014-0196-1
Bhatt, D. L., Lopes, R. D., and Harrington, R. A. (2022). Diagnosis and treatment of acute coronary syndromes: a review. Jama 327 (7), 662–675. doi:10.1001/jama.2022.0358
Braunwald, E., Autman, E. M., Beasley, J. W., Califf, R. M., and Cheitlin, M. D. (2002). ACC/AHA guideline update for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction. Circulation 106 (14), 1893–1900. doi:10.1161/01.CIR.0000037106.76139.53
Chen, Q., and Y, L. M. (2009). Curative effects of puerarin injection on unstable angina pectoris. Chin Arch Trad Chin Med. 27 (2), 447–448.
Chen, X. H. (2004). The clinical observation of puerarin injection on unstable angina pectoris. J. Chin Med Mater 27 (1), 77–78. doi:10.3321/j.issn:1001-4454.2004.01.038
AuthorAnonymous, (2024). Correction to: 2023 esc guidelines for the management of acute coronary syndromes: developed by the task force on the management of acute coronary syndromes of the european society of cardiology (esc). Eur. Heart J. 45(13):1145. doi:10.1093/eurheartj/ehad870
Fan, Y. F., and Yang, G. Y. (2021). Application effect of ginkgo biloba dripping pills combined with metoprolol tartrate in the treatment of patients with coronary heart disease. Inn. Mong. Med. J. 53 (11), 1303–1306. doi:10.16096/J.cnki.nmgyxzz.2021.53.11.008
Fang, G. H. (2006). Efficacy of puerarin injection in the treatment of unstable angina pectoris in the elderly. J. Emerg Trad Chin Med 15 (7), 690–691. doi:10.3969/j.issn.1004-745X.2006.07.004
Feng, C. Z., and Liang, L. L. (2019). Ginkgundamo injection combined with metoprolol tartrate in the treatment of unstable angina in coronary atherosclerotic heart disease. Clin Res Pract 4 (3), 2. doi:10.19347/j.cnki.2096-1413.201903017
Gao, W., Shi, Y. Y., and Suo, D. M. (2009). Clinical efficacy of beitong danhong injection in the treatment of unstable angina pectoris. J Liaoning Trad Chn Med 36 (2), 235–236.
Gao, Z., Wei, B., and Qian, C. (2015). Puerarin injection for treatment of unstable angina pectoris: a meta-analysis and systematic review. Int. J. Clin. Exp. Med. 8 (9), 14577–14594.
PubMed Abstract PubMed Abstract PubMed Abstract | Google Scholar
Gong, F. S. (2014). Clinical study on danhong injection in the treatment of blood stasis type unstable angina. J Navy Med (3), 188–190. doi:10.3969/j.issn.1009-0754.2014.03.008
Guo, C. Q. (2018). Effect of danshen chuanxiongzizine injection combined with nicorandil in the treatment of angina pectoris in coronary heart disease. Henan Med. Res. 27 (24), 4494–4495. doi:10.3969/j.issn.1004-437X.2018.24.037
Guo, Z. B. (2017). Analysis of the pharmacological effects and active ingredients of the Chinese medicine dilong. Contemp. Med. 23 (19), 199–200. doi:10.3969/j.issn.1009-4393.2017.19.108
Han, Y., and Wen, Y. C. (2010). The effect of liqustrazine hydrochloridefor the unstable angina to the senior patients. J Xinjiang Med Univ. 33 (2), 208–209. doi:10.3969/j.issn.1009-5551.2010.02.033
He, P. (2020). Effect of musk heart pills combined with gerberellin injection on cardiac enzymes in patients with acute non-st-segment elevation myocardial infarction. Pract Clin J Integr Trad Chin West Med 20 (15), 10–11. doi:10.13638/j.issn.1671-4040.2020.15.005
Huang, W., Frederich, A., and Putri, A. R. (2024). Effects of remote ischaemic conditioning in stable and unstable angina patients undergoing percutaneous coronary intervention: a systematic review and meta-analysis. Heart Lung Circ. 33 (4), 406–419. doi:10.1016/j.hlc.2024.01.023
Jiang, D. J., Yan, X. B., and Yu, Z. Z. (2020). Study on the efficacy of puerarin injection in the treatment of arrhythmia after myocardial infarction. Clin. Med. 40 (3), 124. doi:10.19528/j.issn.1003-3548.2020.03.053
Jiang, Z., Cui, X., Qu, P., Shang, C., Xiang, M., and Wang, J. (2022). Roles and mechanisms of puerarin on cardiovascular disease:a review. Biomed. Pharmacother. 147, 112655. doi:10.1016/j.biopha.2022.112655
Kudereti, A. (2016). Clinical efficacy analysis of thromboxane injection combined with nicorand il in the treatment of unstable angina pectoris in the elderly. Lab Med Clin. 13 (23), 3407–3409. doi:10.3969/j.issn.1672-9455.2016.23.052
Laidlaw, T. M., and Cahill, K. N. (2017). Current knowledge and management of hypersensitivity to aspirin and nsaids. J. Allergy Clin. Immunol. Pract. 5 (3), 537–545. doi:10.1016/j.jaip.2016.10.021
Li, K. W. (2019). Analysis of the efficacy of metoprolol tartrate combined with ginkgolides injection in patients with angina pectoris of coronary heart disease. Heilongjiang Med. J. 32 (3), 558–560. doi:10.14035/j.cnki.hljyy.2019.03.021
Li, T., and Zhang, P. P. (2018). The effect of aspirin with danhong injection on unstable angina pectoris and vascular endothelial function in elderly patients with coronary heart disease. Shaanxi Med. J. 47 (7), 937–939. doi:10.3969/j.issn.1000-7377.2018.07.038
Li, W. H., and Zhou, J. Y. (2015). Clinical observation of shenxiong glucose injection combined with western medicine routine therapy on unstable angina pectoris. Hebei J Trad Chin Med. 37 (11), 1655–1657. doi:10.3969/j.issn.1002-2619.2015.11.018
Li, W. Q. (2015). Study on the clinical efficacy of shenmai injection in the adjuvant treatment of unstable angina pectoris. Pract J Card Cereb Pneumal Vasc Dis (5), 116–117. doi:10.3969/j.issn.1008-5971.2015.05.038
Li, X. Q., Gao, Y. B., and Zheng, W. W. (2016). Clinical study on safflower yellow combined with atorvastatin in treatment of unstable angina pectoris. Drugs and Clin. 31 (9), 1360–1364. doi:10.7501/j.issn.1674-5515.2016.09.010
Liu, G. W., Zhang, F. S., and Cai, J. (2021). Clinical study on floium ginkgo extract and tertram ethypyrazine sodium chloride combined with ticagrelor in treatment of unstable angina pectoris. Drugs and Clin. 36 (2), 260–264. doi:10.7501/j.issn.1674-5515.2021.02.010
Liu, L. Q., Duan, H. D., and You, X. (2008). Observation on the clinical efficacy of danhong injection in the treatment of unstable angina pectoris. J Liaoning Trad Chn Med 35 (11), 1711–11.
Liu, M. Y., and Zhang, M. Y. (2022). Effect of kudiezi injection combined with nicorandil in the treatment of unstable angina pectoris of coronary heart disease. J Pract Trad Chin Intern Med 36 (9), 52–54. doi:10.13729/j.issn.1671-7813.Z20211915
Liu, T., and Xu, F. Y. (2023). Clinical effect of salviae miltiorrhizae and ligustrazine hydrochloride injection combined with nicorandil tablets in the treatment of coronary heart disease angina pectoris. Clin Res Pract 8 (19), 68–71. doi:10.19347/j.cnki.2096-1413.202319017
Liu, Y., Niu, P., Yan, J., Ji, H., Wang, Z., Jin, X., et al. (2024). Efficacy and safety of ginkgo biloba extract in the treatment of unstable angina pectoris: a systematic review and network meta-analysis. J. Ethnopharmacol. 331, 118297. doi:10.1016/j.jep.2024.118297
Luo, J. E. (2014). Effectiveness and safety of xueshuantong injection in the treatment of unstable angina. Pract J Card Cereb Pneumal Vasc Dis (9), 11–12. doi:10.3969/j.issn.1008-5971.2014.09.004
Ma, X. C., Li, J. X., Xu, M. D., Deng, X. Q., Yue, G. H., and Zheng, C. H. (2015). Meta-analysis on effectiveness and safety of tanshinoneⅱa sulfonate sodium injection in treatment of unstable angina pectoris. World Sci Tech-Mod Trad Chin Med (9), 1766–1774. doi:10.11842/wst.2015.09.003
Mahady, S. E., Margolis, K. L., Chan, A., Polekhina, G., Woods, R. L., Wolfe, R., et al. (2021). Major gi bleeding in older persons using aspirin: incidence and risk factors in the aspree randomised controlled trial. Gut 70 (4), 717–724. doi:10.1136/gutjnl-2020-321585
Meng, Q. G. (2004). Clinical observation of unstable angina treated by puerarin injection and its effect on oxidized low-density lipoprotein. Hebei J Trad Chin Med. 26 (10), 779–780. doi:10.3969/j.issn.1002-2619.2004.10.051
Miao, L., and Hu, Y. H. (2013). Observation of the curative effect on atorvastatin joint danhong injection in the treatment of unstable angina pectoris. China Med. Her. 10 (1), 78–80. doi:10.3969/j.issn.1673-7210.2013.01.033
Moher, D., Pham, B., Jones, A., Cook, D. J., Jadad, A. R., Moher, M., et al. (1998). Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 352 (9128), 609–613. doi:10.1016/s0140-6736(98)01085-x
Ning, W. Z. J. M., Li, T., and Huang, Q. (2011). Danhong injection in the treatment of unstable angina. China Med. Her. 8 (21), 91–92. doi:10.3969/j.issn.1673-7210.2011.21.040
Pan, J. X., Chen, L. H., Ren, Y. C., and Pu, G. J. (2013). Analysis of clinical efficacy and mechanism of action of danhong injection combined with atorvastatin in the treatment of unstable angina pectoris. J Clin Med Pract. 17 (21), 114–115. doi:10.7619/jcmp.201321033
Peng, L. (2014). Observation on the efficacy of chuanxiongxizine injection in the adjuvant treatment of unstable angina pectoris. Mod J Integr Trad Chin West Med 23 (10), 1108–1110. doi:10.3969/j.issn.1008-8849.2014.10.037
Pu, H. W., Chen, M. S., and Tang, Q. Y. (2015). Clinical observation on the treatment of unstable angina pectoris with ginkgolides injection. Phar Clin. Chin Mater Med 31 (2), 187–188.
Qin, Y., Liu, Y. Q., and Li, F. (2020). Effect of danhong injection on hemorheology and inflammatory factors in patients with coronary heart dis-ease and angina pectoris. Chin J Thromb Hemost 26 (2), 218–219. doi:10.3969/j.issn.1009-6213.2020.02.013
Qiu, Z. W., Xia, C. X., and Sun, R. (2008). Observation on the efficacy of thromboxane injection in the treatment of unstable angina pectoris in the elderly. Shanghai J Trad Chin Med. (03), 34–35. doi:10.16305/j.1007-1334.2008.03.009
Quan, Z. R. (2011). Efficacy of ginkgundamo injection in the treatment of 87 cases of unstable angina pectoris in the elderly Shandong Med J. 51(1):109. doi:10.3969/j.issn.1002-266X.2011.01.070
Ren, L. Q., Wu, Z., Liao, W., Li, B., and Ma, J. L. (2018). Clinical study of salviae miltiorrhizae and ligustrazine hydrochloride injection combined with ticagrelor in treatment of unstable angina pectoris. Drugs and Clin. 33 (8), 1921–1927. doi:10.7501/j.issn.1674-5515.2018.08.014
Roth, G. A., Mensah, G. A., Johnson, C. O., Addolorato, G., Ammirati, E., Baddour, L. M., et al. (2020). Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76 (25), 2982–3021. doi:10.1016/j.jacc.2020.11.010
Shao, H., Huang, Y., Xu, D., Huang, S., and Tong, R. (2022). A systematic review and meta-analysis on the efficacy of puerarin injection as adjunctive therapy for unstable angina pectoris. Front. Cardiovasc Med. 9, 763567. doi:10.3389/fcvm.2022.763567
Shi, Y. T. (2007). Effect of xintong injection in combination with low molecular heparin on unstable angina pectoris and blood-fat. China J Tradi Chin Med Pha 22 (11), 804–805. doi:10.3969/j.issn.1673-1727.2007.11.025
Song, H. Y., and Bannu, K. (2009). Observations on the efficacy of psidium guajava bark injection in the treatmepn`t of unstable angina pectoris. Mod J IntegrTrad Chin West Med 18 (31), 3820–3821. doi:10.3969/j.issn.1008-8849.2009.31.015
Sun, T., Wang, X., and Xu, H. (2015). Ginkgo biloba extract for angina pectoris: a systematic review. Chin. J. Integr. Med. 21 (7), 542–550. doi:10.1007/s11655-015-2070-0
Tan, B. Z., and Li, X. Q. (2020). Efficacy and safety analysis of puerarin injection and compound danshen injection combined with amiodarone in the treatment of acute myocardial infarction complicated with arrhythmia. Chin J Integr Med Cardio/Cerebrovas Dis. 18 (6), 924–928. doi:10.12102/j.issn.1672-1349.2020.06.014
Wang, D., Zhai, C. S., and Sun, X. M. (2012). Observation on the efficacy of 60 cases of unstable angina pectoris treated with lanjian xinxin injection. Guangdong Med. J. 33 (17), 2668–2670. doi:10.3969/j.issn.1001-9448.2012.17.054
Wang, P. N. (2009). Observation on the efficacy of danhong injection in the treatment of unstable angina pectoris. J. Henan Univ (Med Sci). 28 (2), 143–144. doi:10.3969/j.issn.1672-7606.2009.02.021
Wang, R. F. (2021). Evaluation of the efficacy of shu xuning injection combined with isosorbide mononitrate in the treatment of patients with unstable angina pectoris of coronary heart disease. Pract Clin J Integr Trad Chin West Med 21 (8), 8–9. doi:10.13638/j.issn.1671-4040.2021.08.003
Wang, S. Q., Cao, C. G., and Liu, B. F. (2002). Clinical observation on shuxuetong injection in treatment of unstable angina pectoris. Chin J Integr Trad West Med Intens Crit Care 9 (4), 226–227. doi:10.3321/j.issn:1008-9691.2002.04.015
Wang, Z. L. (2020). Effect of puerarin injection combined with dual antiplatelet therapy for coronary artery disease and its effect on vascular endothelial function. Heilongjiang Med And Pharm 43 (6), 133–134. doi:10.3969/j.issn.1008-0104.2020.06.061
Wu, J. R., Zhang, X. M., and Zhang, B. (2015). Danhong injection in the treatment of acute coronary syndrome: a systematic review and meta-analysis. Am. J. Chin. Med. 43 (2), 199–214. doi:10.1142/s0192415x15500135
Wu, Z. Q. (2019). Clinical effect of apricot and sodium chloride injection in the treatment of ischemic cardiomyopathy with heart failure. China Mod. Med. 26 (31), 42–44. doi:10.3969/j.issn.1674-4721.2019.31.013
Yang, J. Y. (2020). Observation on the effect of lipitor combined with ginkgoloderma injection in the treatment of angina pectoris in coronary heart disease the J of Med Theory and Pract. 33(2):220–221. doi:10.19381/j.issn.1001-7585.2020.02.018
Yang, K., Wei, X. M., Liu, W. J., Gou, C. W., Su, F., Zhou, X. S., et al. (2014). Clinical observation of 137 cases by using salviae miltiorrhizae and ligustrazine hydrochloride injection in the treatment of unstable angina pectoris. Northwest Phar J. (2), 194–196. doi:10.3969/j.issn.1004-2407.2014.02.029
Yao, Y. Y., and Jin, Z. T. (2022). Application value of danhong injection in assisting with basic western medicine treatment for unstable angina pectoris of coronary heart disease. World J Integr Trad West Med 17 (4), 769–773. doi:10.13935/j.cnki.sjzx.220424
Yong, X. F., and Liu, X. W. (2010). Observation on the efficacy of 60 cases of unstable angina pectoris treated with lanjian xinxin injection. Guangdong Med. J. 31 (4), 516–518. doi:10.3969/j.issn.1001-9448.2010.04.049
Zeng, X. J., Luo, Y., and Ma, L. J. (2015). Clinical observation of using danhong injection to treat 150 cases of unstable angina pectoris. J Sichuan Trad Chin Med. 33 (6), 171–172.
Zhai, Y. Y., and Jiaol, L. Q. (2013). Clinical observation on 56 cases of unstable angina pectoris treated with injectable danshen polyphenate. Hebei J Trad Chin Med. (11), 1687–1688. doi:10.3969/j.issn.1002-2619.2013.11.052
Zhang, C. J. (2006). Treatment of 30 cases of unstable angina pectoris in the elderly with coronary heart injection Herald of Med. 25(10):1025–1026. doi:10.3870/j.issn.1004-0781.2006.10.021
Zhang, D., Wu, J., Liu, S., Zhang, X., and Zhang, B. (2016a). Salvianolate injection in the treatment of unstable angina pectoris: a systematic review and meta-analysis. Med. Baltim. 95 (51), e5692. doi:10.1097/md.0000000000005692
Zhang, D. L., Yin, L., Jiang, F., Guo, F., and Hao, W. H. (2019). Effect of danshen ligustrazine injection combined with isosorbide mononitrate on blood lipid level and efficacy in patients with coronary heart disease unstable angina pectoris. Chin Arch Trad Chin Med 37 (6), 1451–1454. doi:10.13193/j.issn.1673-7717.2019.06.043
Zhang, L., and Lu, G. X. (2016). Therapeutic effects of hongjingtian injection combined with clopidogrel on unstable angina pectoris. Hebei Med. J. 38 (14), 2140–2142. doi:10.3969/j.issn.1002-7386.2016.14.016
Zhang, L. M., Du, T. H., Niu, L. L., Wang, L. Y., Li, J. N., Ma, P. F., et al. (2021). Network meta-analysis of Chinese patent medicine in treatment of unstable angina pectoris. Zhongguo Zhong Yao Za Zhi 46 (3), 703–711. doi:10.19540/j.cnki.cjcmm.20201103.502
Zhang, W., Hu, J. T., Yang, S. G., and Hu, X. M. (2022). The effect of apricot rhizome sodium chloride injection combined with arolol hydrochloride tablets in the treatment of unstable angina pectoris. World Clin. Drug 43 (08), 1044–1050. doi:10.13683/j.wph.2022.08.014
Zhang, X., Li, H., Yu, S. J., Qiu, X. M., Zhang, C., Yuan, M., et al. (2014). Curative efficacy of danhong injiction in combination with clopidogrel in treatments of patients with unstable angina pectoris and its effect on hemorheological parameters. J Clin Exp Med (24), 2058–2061. doi:10.3969/j.issn.1671-4695.2014.24.018
Zhang, X., Wu, J., Zhang, B., and Zhou, W. (2016b). Danshenchuanxiongqin injection in the treatment of unstable angina pectoris: a systematic review and meta-analysis. J. Tradit. Chin. Med. 36 (2), 144–150. doi:10.1016/s0254-6272(16)30020-6
Zhang, Y. H. (2007). The efficacy of tanshinone injection in the treatment of unstable angina pectoris. Pract. Geriatr. 21 (3), 212–213. doi:10.3969/j.issn.1003-9198.2007.03.024
Zheng, Y., and Wang, H. H. (2006). Clinical observation on the treatment of unstable angina pectoris by pueraria mirifica. Chin J Integr Trad West Med Intens Crit Care 13 (3), 189–190. doi:10.3321/j.issn:1008-9691.2006.03.022
Zhou, X. Y. (2008). Observation on the efficacy of danhong injection in the treatment of unstable angina pector. Pract J Card Cereb Pneumal Vasc Dis 16 (12), 38–39. doi:10.3969/j.issn.1008-5971.2008.12.023
Keywords: traditional Chinese medicine, injection, unstable angina pectoris, Bayesian network meta-analysis, systematic review
Citation: Chen Q, Wang H, Zhu L, Guo Z, Cui Y, Ban J, Chi K, Shi N, Wang B, Liu C and Zhou Y (2025) Efficacy and safety of different traditional Chinese medicine injections in the treatment of unstable angina pectoris: a systematic review and Bayesian network meta-analysis. Front. Pharmacol. 16:1550759. doi: 10.3389/fphar.2025.1550759
Received: 24 December 2024; Accepted: 26 February 2025;
Published: 12 March 2025.
Edited by:
Javier Echeverria, University of Santiago, ChileReviewed by:
Luca Rastrelli, University of Salerno, ItalyCopyright © 2025 Chen, Wang, Zhu, Guo, Cui, Ban, Chi, Shi, Wang, Liu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yabin Zhou, NTI2NzY1MjYyQHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.