
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 26 March 2025
Sec. Pharmacoepidemiology
Volume 16 - 2025 | https://doi.org/10.3389/fphar.2025.1531500
 Mohammed S. Salahudeen1*
Mohammed S. Salahudeen1* Ahmed Samy Saadeldean1
Ahmed Samy Saadeldean1 Gregory M. Peterson1
Gregory M. Peterson1 Behailu Terefe Tesfaye2
Behailu Terefe Tesfaye2 Colin M. Curtain1
Colin M. Curtain1Objective: There is limited information regarding community pharmacists’ perspectives on implementing a self-administered screening tool for identifying patients at risk of medication-related problems. This study assessed Australian pharmacists’ views on introducing such a tool within the community pharmacy setting.
Methods: An online cross-sectional survey was conducted among Australian community pharmacists from March to May 2023. The survey collected relevant demographic data and responses on perceived barriers and facilitators to implementing the screening tool. Reliability statistics were computed for the responses on barriers and facilitators, and chi-square or Fisher’s Exact tests were performed to assess their association with demographic variables.
Results: Two hundred thirty-one community pharmacists across Australia were surveyed. Most (78%) reported that medication-related problems are common and expressed support for a patient self-administered screening tool to identify patients at high risk of medication-related problems (88%). Over two-thirds (69%) were willing to allocate time for reviewing patient medications if flagged for medication-related problems. The most frequently anticipated barriers to implementing screening tools were time constraints for pharmacists (63%), staff shortage and limited patient interest (each accounting for 57%). In contrast, effective communication with patients (69%) and patients’ appreciation of pharmacists’ expertise and efforts (67%) were predominantly stated facilitators.
Conclusion: Most community pharmacists were supportive of implementing a patient self-administered screening tool to identify patients at risk of medication-related problems. The study’s findings provide valuable insights for developing medication-related problems screening tools tailored to the Australian community pharmacy setting.
A medication-related problem (MRP) is defined as any event or situation involving medication therapy that either actually or potentially interferes with desired health outcomes (Cipolle et al., 2012). According to the Pharmaceutical Care Network Europe (PCNE), MRP encompasses unnecessary drug therapy, insufficient drug therapy, ineffective drug therapy, adverse drug events, incorrect dosages, and suboptimal adherence (Pharmaceutical Care Network Europe, 2020). These problems are associated with considerable adverse impact on the healthcare system. For instance, in Australia, around 250,000 hospital admissions annually are estimated to be due to MRPs, costing AUD$1.4 billion (Lim et al., 2022). Of these, over two-thirds are potentially preventable (Lim et al., 2022), highlighting the opportunity to reduce this burden. With the ageing population (Australian Institute of Health and Welfare, 2023) and increasing rates of multimorbidity and medicine use, MRPs are likely to become more common in Australia (Nicosia et al., 2019).
Various tools have been developed to identify and reduce the risk of MRPs. For instance, in the United States, Beer’s Criteria was published in 1991 (American Geriatrics Society Beers Criteria® Update Expert Panel, 2023) followed by McLeod’s Criteria from Canada (McLeod et al., 1997). These tools were developed to guide clinicians in reducing the prescribing of inappropriate medications for older adults and patients with specific conditions (McLeod et al., 1997; American Geriatrics Society Beers Criteria® Update Expert Panel, 2023). Some tools and questionnaires are focused on adverse effects or adherence (Butler et al., 2004; Wetzels et al., 2006), while others screen for a wide range of MRPs (Barenholtz Levy, 2003; Paulino et al., 2004; Blalock and Patel, 2005; Gordon et al., 2005; Pammett et al., 2015). One study by Levy et al. developed a tool to be completed solely by the patient independent of healthcare professional involvement (Barenholtz Levy, 2003). The screening tools have been trialled in small-large groups of patients. Furthermore, a systematic review of eleven MRP risk assessment (screening) tools has revealed significant variations in content among these tools (Puumalainen et al., 2019).
Community pharmacists have the potential to play a vital role in recognising patients at risk of MRPs due to their frequent patient interactions, ready accessibility, and expertise in medicines (Pharmacy Guild of Australia, 2021). In Australia, as part of measures to mitigate MRPs, the government funds programs, such as the MedsCheck and Diabetes MedsCheck (DMC), so community pharmacists can assist patients in improving their health and optimising medicine use (Pharmacy Programs Administrators, 2021; Gargya et al., 2022). However, these services do not benefit everyone taking medication, indicating the need for comprehensive tools. There is limited understanding of pharmacists’ perceptions and insights regarding the implementation of patient self-administered tools for identifying MRPs in community pharmacy setting. It is well-documented that community pharmacists often work under significant time constraints, particularly in busy environments (Pharmacy Guild of Australia, 2021). These pressures may discourage pharmacists from adopting additional tools for addressing MRPs.
Given their unique role, community pharmacists can provide valuable insights into the essential features and content required for a screening tool specifically tailored to the Australian setting. Furthermore, they can offer perspectives on potential barriers and facilitators to implementing such a tool within the pharmacy workflow. Hence, our study aimed to evaluate community pharmacists’ views on implementing a patient self-administered screening tool to identify at-risk patients, contributing to a practical approach for improving MRP identification in the community.
This online cross-sectional national survey was conducted in Australia between March and May 2023 and was hosted on the Qualtrics platform (Qualtrics.XM, 2023). The study targeted Australian Health Practitioner Regulation Agency (AHPRA)-registered community pharmacists across Australia.
According to the Pharmacy Guild of Australia, there were approximately 20,000 pharmacists employed in community pharmacy settings (Pharmacy Guild of Australia, 2021). Based on a 95% confidence interval and a 5% margin of error, an estimated sample size of 377 participants was determined for this survey, based on a sample size calculator provided by Qualtrics (https://www.qualtrics.com/blog/calculating-sample-size/).
To recruit participants, an advertisement with a survey link was shared on Australian pharmacy-focused groups and social media platforms, including Facebook, Twitter, and LinkedIn. An invitation letter, containing both a survey link and a QR code, was also sent to pharmacy organisations, such as the Pharmaceutical Society of Australia (PSA) Tasmanian Branch, PSA Early Career Pharmacist, Consultant Pharmacists Australia (CoPA), Professional Pharmacists Australia, and Pharmacy Daily. Additionally, Raven’s Recruitment (a pharmacist recruitment agency) and Australian Locum Pharmacists Facebook group were contacted to further promote participation in the survey.
The survey questionnaire was developed through a structured process that included a literature review, expert opinion, and feedback from community pharmacists. The questionnaire covered key areas, including participant demographics, characteristics of MRPs encountered in community pharmacy, pharmacists' perspectives on the benefits and essential features of a suitable MRP screening tool, and their views on the barriers and facilitators to implementing a brief, patient-administered MRP screening tool in the Australian community pharmacy setting.
To provide context for participants, the survey included a reference screening tool, the ‘Medication Risk Questionnaire’ developed by Barenholtz Levy (Barenholtz Levy, 2003), to assess the risk of MRPs in community pharmacy. Participants were invited to offer suggestions for improvements, evaluate the tool’s feasibility, and provide insights into its integration into the pharmacy workflow (e.g., completion time, applicability).
A pilot test was conducted with five registered pharmacists to assess face and content validity. Based on their feedback, revisions were made to improve clarity and ease of completion. The final version, designed for a 10–15-min completion time, included five sections with Likert scales, closed, and open-ended questions. Section A collected demographic information, Section B addressed MRPs, Section C focused on patient-administered screening tools for identifying MRPs, and Section D explored barriers and facilitators to implementation. Data were collected via Qualtrics between March and May 2023. The full survey questionnaire is provided in Supplementary Table S1.
The primary outcome measures included community pharmacists’ views and attitudes towards implementing a patient self-administered screening tool designed to identify patients at potential risk of MRPs in community pharmacy. Additionally, they provided perspectives on potential barriers and facilitators for implementing such a tool effectively within the pharmacy workflow.
Survey data were imported into IBM SPSS version 28 for analysis. All responses were reviewed for completeness, and any incomplete entries were excluded from further analysis. Descriptive statistics, including median with range, frequencies, and percentages, were calculated as appropriate. Inferential statistics were conducted using chi-square tests or Fisher’s Exact tests to examine associations on beliefs, barriers, and facilitators for implementing a screening tool. The chi-square test was employed when expected cell counts were ≥5 in at least 80% of cells, with no cell containing a zero. If these conditions were not met, Fisher’s exact test was used.
Items related to barriers and facilitators were assessed on a 5-point Likert scale (5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree, and 1 = strongly disagree). For the purpose of running chi-square tests or Fisher’s Exact Test and to simplify interpretation, Likert responses were re-categorised as follows: “Agree” (combining “strongly agree” and “agree”) and “Disagree” (combining “neutral,” “disagree,” and “strongly disagree”), assuming the psychological distance between categories was uniform.
The reliability of the barriers and facilitators questions was evaluated using Cronbach’s alpha, with a value above 0.7 considered acceptable. Cronbach’s alpha values for the barriers and facilitators questions were 0.77 and 0.75, respectively, indicating acceptable internal consistency. Additional open-ended responses regarding barriers and facilitators were thematically summarised inductively. All p-values less than 0.05 were considered statistically significant.
We followed the reporting guidelines of the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement for observational studies (Elm et al., 2007).
Among the total survey responses received (n = 256), we included 231 completed responses (90%) in the final analysis. The respondents were predominantly in the age range of 20–39 years (77%). Pharmacists or pharmacists in charge accounted for 78%, and over two-thirds (67%) had practised as a community pharmacist in Australia for less than 10 years (Table 1).
Respondents stated that MRPs were common (78%), and most (46%) were moderately severe. The most common issues encountered were improper drug selection (18%), drug interactions (18%) and adverse drug reactions (17%), as shown in Table 2.
Most pharmacists (62.8%) believed a screening tool could help identify patients at risk of MRPs, and 88% perceived that MRP screening tools could be helpful in their community pharmacy. Over two-thirds (69%) said they had time to review patient medications. However, only 55% thought the questions in the reference screening tool (Barenholtz Levy, 2003) would be understood by patients. Respondents were asked for suggestions on whether a particular medication or medication class should be included in an MRP screening tool. They suggested statins, anticoagulants, amiodarone, non-steroidal anti-inflammatory drugs, and medications increasing the risk of falls. Respondents indicated that the MRP screening tool should be completed within 15 min by patients, with or without assistance from staff, to fit within the community pharmacy workflow. Respondents mostly preferred to review a patient’s medication at quiet times during workday by scheduling an appointment with the patient (42.5%), as illustrated in Table 3.
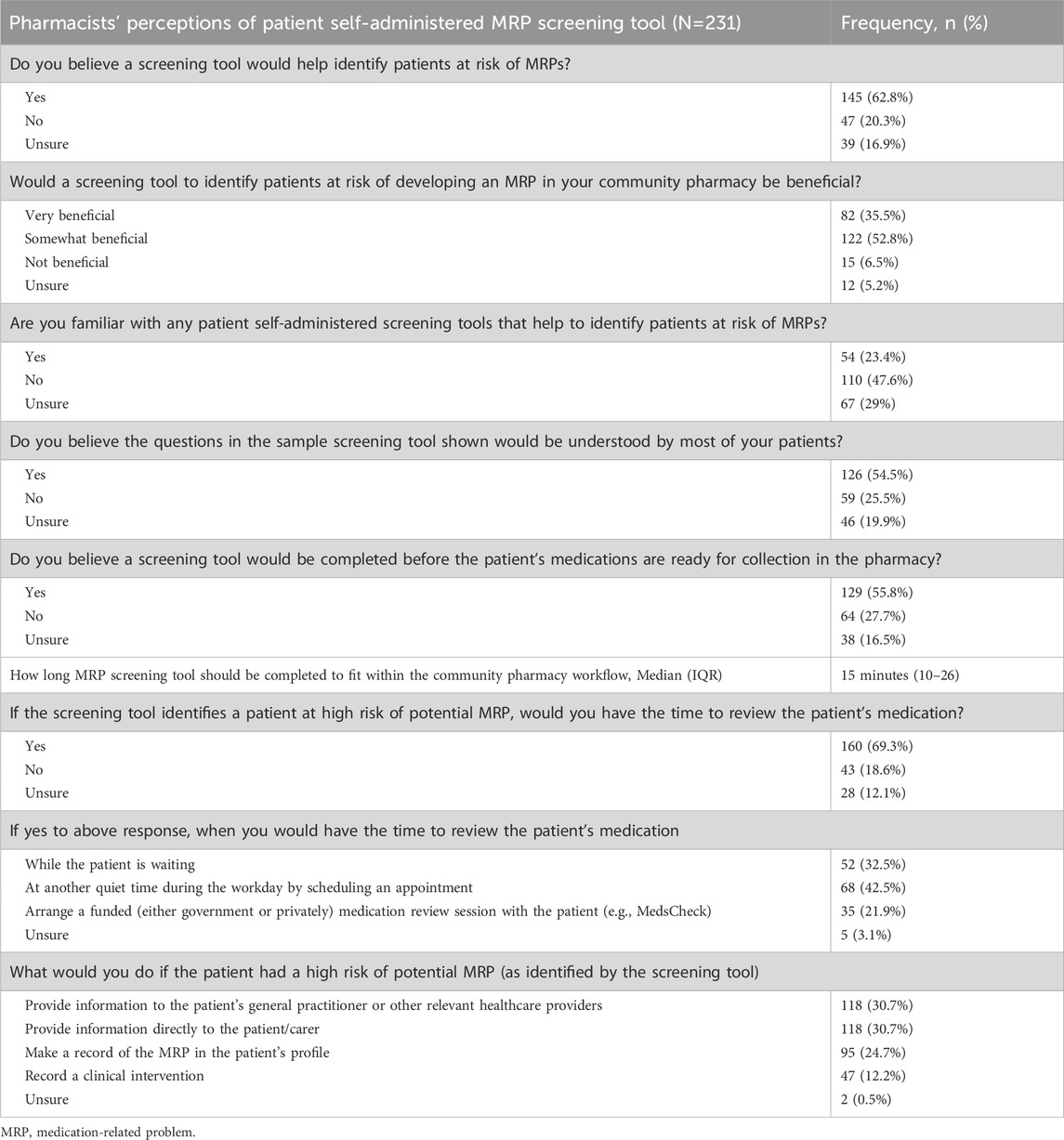
Table 3. Pharmacists’ Perceptions of self-administered screening tool for identifying patients at greatest risk of MRP.
The frequently anticipated barriers to implementing the screening tools were pharmacist time constraints (63%), staff shortage (57%), and lack of patient interest (57%). On the other hand, good communication with the patients (69%), patient appreciation of the pharmacist’s expertise (67%), and support from the employer (65%) were anticipated facilitators for implementing the screening tool, as seen in Table 4. Respondents reported several additional potential barriers and facilitators to implement a self-administered MRP screening tool. These open-ended responses were thematically summarised in Table 5.
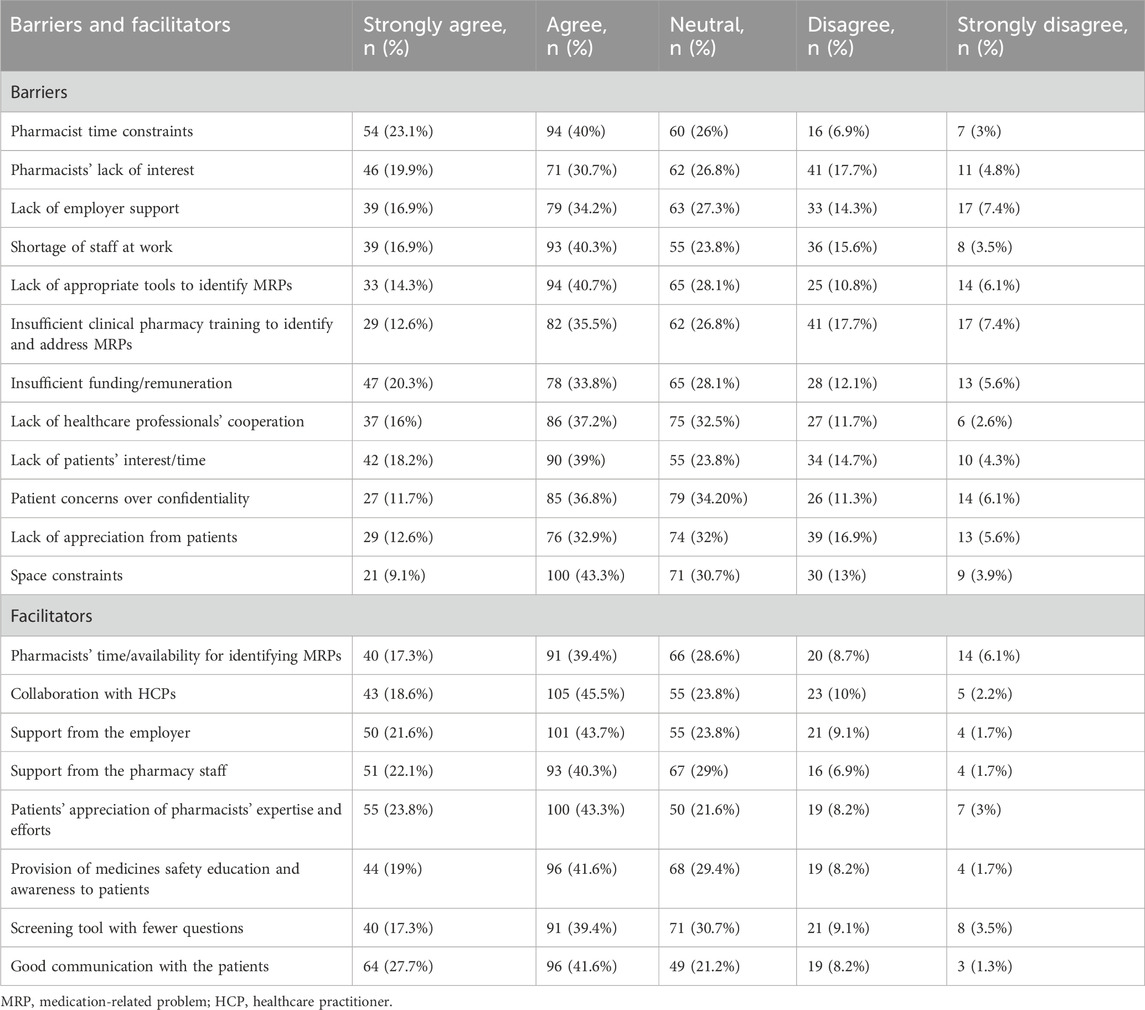
Table 4. Barriers and facilitators to implementing patient self-administered screening tools to identify patients at high risk of MRPs.
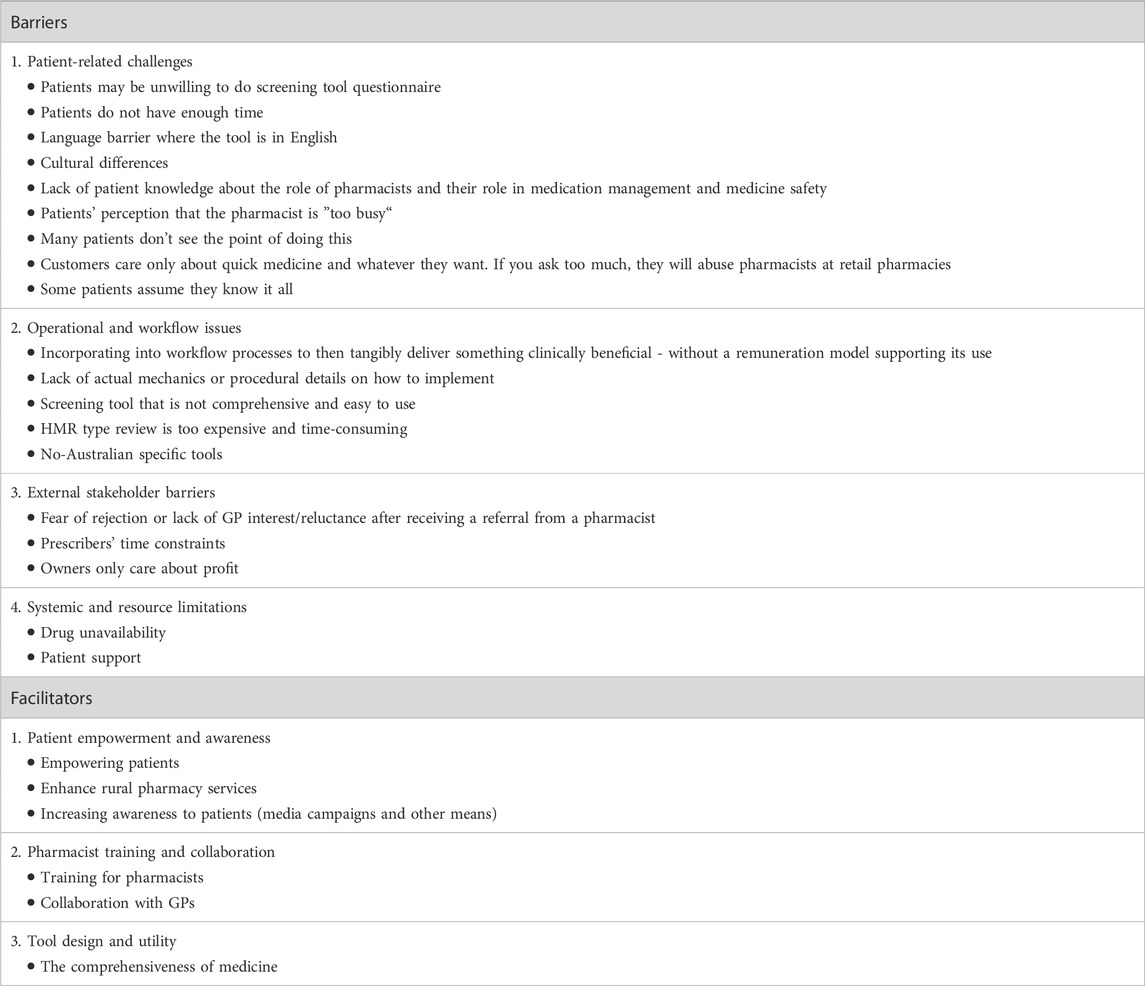
Table 5. Additional barriers and facilitators reported by pharmacists for implementing self-administered screening tools to identify patients at high risk for MRPs.
Several demographic factors were significantly associated with the barriers to implementing a self-administered MRP screening tool (Table 6). Eight out of the 12 barriers to the implementation of the MRP screening tool showed a statistically significant association with various demographics of the participants. For instance, pharmacist time constraints were linked to years of practice (p = 0.023), working in forward-dispensing pharmacies (p = 0.009), and accreditation to conduct Home Medicine Reviews (HMR) and/or Residential Medication Management Reviews (RMMR) (p = 0.042). Similarly, a lack of pharmacist interest was associated with the principal place of employment (p = 0.039). Other notable findings included patient confidentiality concerns being associated with years of practice (p = 0.035) and pharmacist’s role (p = 0.002), while funding and remuneration challenges were tied to age group (p = 0.019), years of practice (p = 0.033), and place of employment (p = 0.060). Conversely, no significant associations were observed for barriers such as lack of employer support, patient interest or time, staff shortages, or healthcare professionals’ cooperation. The details are presented in Table 6.
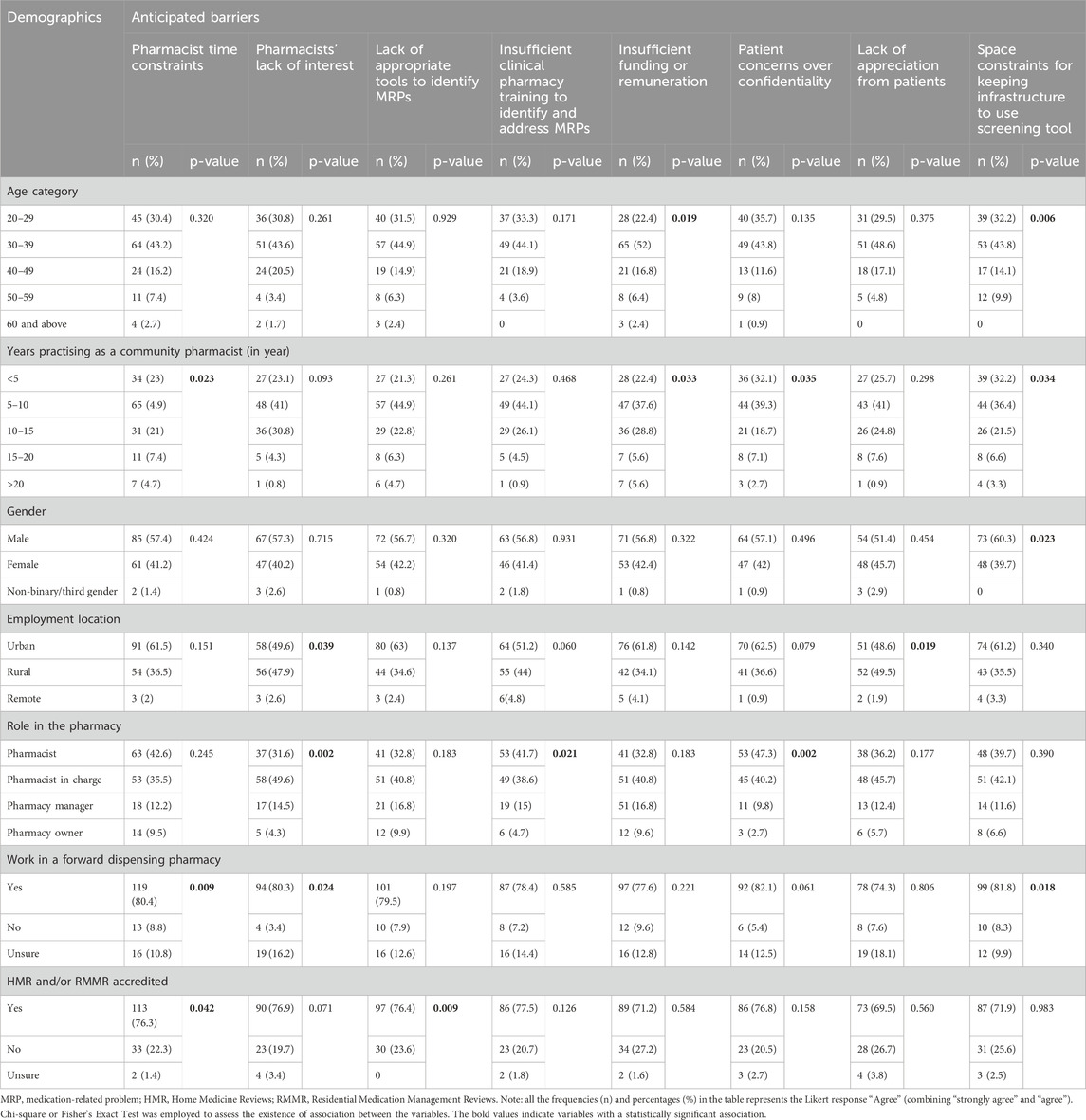
Table 6. The association of pharmacists’ perception of the anticipated barriers to implementing self-administered screening tools to identify patients at high risk of MRPs with demographics.
The perception of pharmacists regarding facilitators for implementing patient self-administered screening tools showed notable associations with specific demographic variables. Collaboration with healthcare professionals was significantly associated with pharmacists’ age category (p = 0.012), gender (p = 0.008), and accreditation to conduct HMR and/or RMMR (p = 0.042). Furthermore, the provision of education and awareness to patients about medicine safety was linked to working in a forward dispensing pharmacy (p = 0.026). The perception of screening tools with fewer questions was associated with pharmacists’ gender (p = 0.019). Lastly, good communication with patients was strongly associated with working in a forward dispensing pharmacy (p = 0.001). These key associations are detailed in Table 7.
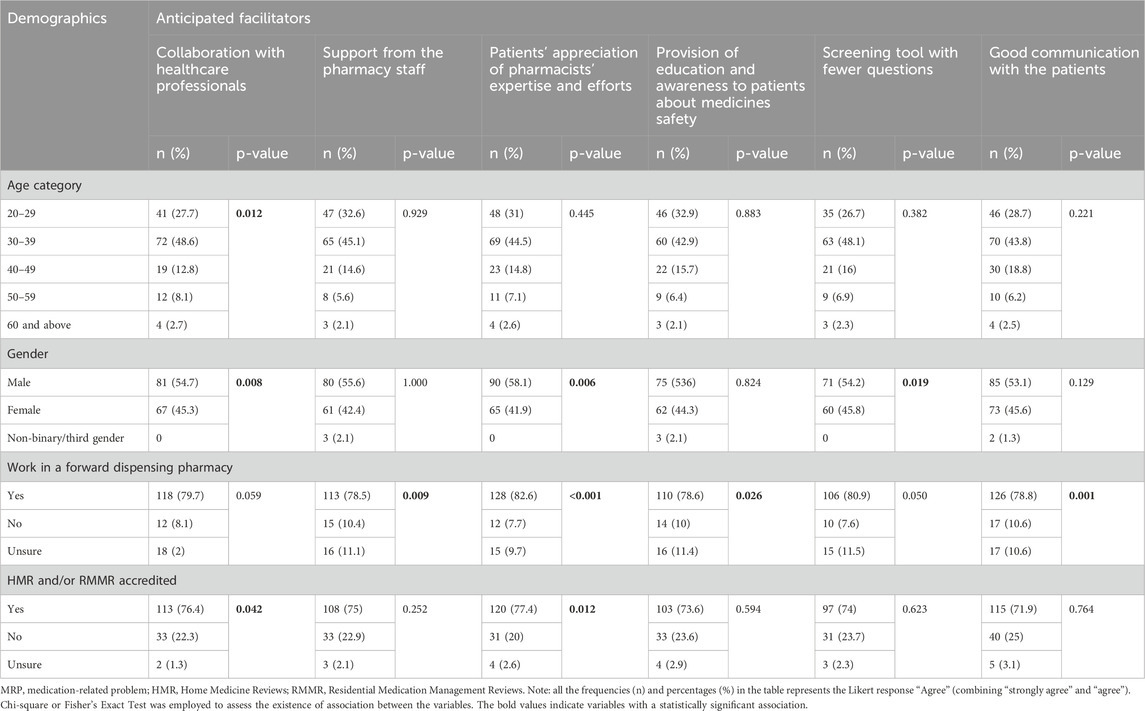
Table 7. The association of pharmacists’ perception of the facilitators to implementing patient self-administered screening tools to identify patients at high risk of MRPs with demographics.
This survey assessed community pharmacists’ views on implementing a self-administered screening tool for identifying patients at high risk of MRPs within community pharmacy setting. In Australia, although there have been attempts to develop MRP screening tools in various non-community pharmacy setting environments (Taylor et al., 2022; Wembridge et al., 2023) and to integrate electronic documentation of MRPs in community pharmacy setting (Williams et al., 2011), evidence regarding community pharmacists’ views on a patient self-administered, community pharmacist-based MRP screening tool is limited. Our study found that most pharmacists believe MRPs are common and they were open to implementing a self-administered screening tool to identify patients at high risk for MRPs. The majority of pharmacists identified time constraints as the primary barrier to implementing the screening tool, followed by staff shortages. Conversely, about two-thirds of the pharmacists felt that effective communication with patients and recognition of the pharmacist’s expertise could facilitate the implementation of the tool. Several anticipated barriers (e.g., pharmacist time constraints, insufficient funding or remuneration, and inadequate clinical pharmacy training to identify and address MRPs) and facilitators (e.g., support from pharmacy staff and effective communication with patients) were found to have significant associations with participants’ demographics, such as their principal place of employment. These findings align with existing literature, which highlights that pharmacists often dedicate substantial time to dispensing, supply, and management activities, leaving limited capacity to provide additional professional services (Lounsbery et al., 2009; Karia et al., 2022; Ali et al., 2023).
Previous studies have shown that MRPs are prevalent in Australian community pharmacy (Williams et al., 2011; Collins et al., 2023). This finding aligns with the responses from pharmacists in our study, which highlights the necessity for implementing measures to prevent or address MRPs within these settings. This is also strengthened by the fact that most pharmacists agreed on the need for screening tools to identify patients at high risk of MRPs in their settings. However, a significant portion of pharmacists reported a lack of familiarity with any MRP screening tools. Among those who were familiar, many mentioned the STOPP/START criteria (O’Mahony et al., 2023) and Beer’s criteria (American Geriatrics Society Beers Criteria® Update Expert Panel, 2023). Nonetheless, these criteria are not comprehensive for all age groups and were not designed to serve as patient screening tools in community pharmacy setting (Milton et al., 2008; Lim et al., 2022).
The willingness of community pharmacists to provide extended services may be influenced by several factors, including time constraints. In a study conducted by Jarab et al., 59% of community pharmacists’ indicated their willingness to provide extended community pharmacy services, such as screening for MRPs (Jarab et al., 2024). This percentage is lower than the proportion of community pharmacists’ willing to provide such services in our study. In our study, a significant portion of the surveyed community pharmacists (71%) were accredited to provide HMR and/or RMMR. Consequently, these respondents are likely to express interest in using MRP screening tools to enhance patient outcomes. Most of the surveyed participants were also pharmacists or pharmacists-in-charge, who are typically responsible for the day-to-day operations of community pharmacies, making them well-positioned to recognise the advantages of the MRP screening tool. In addition to the pressing burden of MRPs in community pharmacy, the willingness to implement a screening tool for identifying patients at high risk for MRPs also indicates the presence of need.
Our findings indicated that pharmacists’ time constraints are a significant anticipated barrier to implementing a patient self-administered MRP screening tool. This issue has also been highlighted in similar studies (Cardwell et al., 2018; Hamadouk et al., 2023; Hogervorst et al., 2024). The pharmacists’ preference to review patients’ medications at quieter times during workday by scheduling an appointment with patients, might also reflect the time limitations they face in their daily activities. To address this, we suggest enhancing the efficiency of the MRP screening tool and minimising the time required for the screening process.
Our study also identified lack of remuneration for performing MRP screening activities as another major anticipated barrier to the implementation of MRP screening tool. Integrating the MRP screening task into government-funded services, such as MedsChecks and DMC (Pharmacy Programs Administrators, 2021), HMR, and RMMR (Pharmacy Programs Administrators, 2022), or facilitating service payment by patients, could help for the implementation of the screening tool in everyday practice and ensure its sustainability.
Previous studies in community pharmacy settings (Cardwell et al., 2018; Hamadouk et al., 2023; Hogervorst et al., 2024), identified barriers not mentioned in our research, such as the prioritisation of other clinical tasks, difficulty accessing patient clinical information, and a perceived disconnect from the primary healthcare team (Cardwell et al., 2018). In contrast, our study found several new patient-related barriers, including concerns about confidentiality, a lack of patient appreciation, cultural differences, language barriers (particularly when the tool is in English), patients’ reluctance to engage in MRP screening, and their preference to quickly collect prescriptions rather than engage further.
Effective communication is widely recognised as crucial for improving pharmacy services (de Oliveira and Shoemaker, 2006). Our findings underscore this importance, suggesting that training pharmacists to use MRP screening tools should also include communication and confidence-building components. While previous research noted different facilitators [e.g., perceived professional roles, clinical outcomes, and peer influence (Cardwell et al., 2018)], our study highlights additional ones, such as strengthening rural pharmacy services and using screening tools with fewer questions.
In forward dispensing pharmacies, where there is no physical barrier between pharmacist and patient, pharmacists can counsel patients immediately as they approach the dispensary (Berbatis et al., 2007). Although this model can enhance patient interaction, it may also increase workload, which could explain the strong association we observed between time constraints and forward dispensing practices (p = 0.009). Furthermore, owners and managers in some community pharmacies may emphasise efficiency over extended patient care, potentially dampening staff motivation to adopt additional interventions (Resnik et al., 2000). This may clarify why pharmacists’ roles were strongly associated with perceptions of patient disinterest (p = 0.002).
Location also appears to influence perceptions. Pharmacists in metropolitan areas often face heavier patient flow, leading to workload pressures that may deter them from adopting additional professional tasks (Kanaani et al., 2023). This aligns with the moderate association noted between pharmacists’ lack of interest and their employment location (p = 0.039). Alternatively, when sufficient staff support is available, particularly in forward dispensing pharmacies, pharmacists can conduct activities like MRP screening more effectively (p = 0.009).
With MRPs posing a significant public health issue, this study addresses an important gap in understanding community pharmacists' roles in early identification of high-risk patients. Our findings offer insights into the attitudes and perspectives of pharmacists who are particularly interested in reducing MRPs within the community setting. The survey may not fully represent all community pharmacists across Australia due to convenience sampling methods or overrepresentation from certain regions, demographic groups, or practice settings (e.g., urban vs. rural areas). Additionally, because the survey was widely advertised across Australia without precise tracking, we were unable to determine an exact response rate. Moving forward, incorporating patient feedback will be essential in determining the feasibility and acceptability of these tools. Exploring artificial intelligence (AI) could further enhance efficiency, as indicated in recent literature (Chalasani et al., 2023; Alsanosi and Padmanabhan, 2024; Graafsma et al., 2024; Maleki Varnosfaderani and Forouzanfar, 2024). Finally, addressing staff shortages by hiring or delegating certain responsibilities to pharmacy technicians may aid in the successful implementation of these screening tools (Michel et al., 2023).
Despite their demanding schedules, Australian community pharmacists are open to incorporating a patient-self-administered MRP screening tool into their daily routines within the community pharmacy environment. They demonstrate a strong awareness of the prevalence of MRPs in the community and value the recognition they receive from patients for their dedication and expertise. Additionally, effective communication with patients, patient appreciation of pharmacists' expertise, and employer support serves as key facilitators in this process. The study's findings provide valuable insights for developing MRP screening tools tailored to the Australian community pharmacy setting, ensuring they are both feasible and effectively integrated into pharmacists' workflows. Future research should explore implementation strategies and assess the impact of such tools on patient outcomes and pharmacy practice.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Tasmanian Human Research Ethics Committee (Reference: H0028348). It was conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because Anonymous survey used implied consent.
MS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. AS: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Validation, Writing–original draft, Writing–review and editing. GP: Conceptualization, Methodology, Supervision, Visualization, Writing–review and editing. BT: Formal Analysis, Visualization, Writing–review and editing. CC: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing–review and editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to extend immense gratitude to the participants in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author MS declared that they were an editorial board member of Frontiers at the time of submission. This had no impact on the peer review process and the final decision.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1531500/full#supplementary-material
DMC, Diabetes MedsCheck; HMR, Home Medicine Review; MRP, Medication-Related Problem; PCNE, Pharmaceutical Care Network Europe; PIC, Pharmacists In Charge; RMMR, Residential Medication Management Review; STOPP/START, Screening Tool of Older Persons’ Prescriptions/Screening Tool to Alert to Right Treatment.
Ali, S., Curtain, C. M., Peterson, G. M., and Salahudeen, M. S. (2023). Exploring Australian pharmacists’ views toward reducing the risk of medicines-related harm in aged care residents. Pharmacol. Res. Perspect. 11, e01104. doi:10.1002/prp2.1104
Alsanosi, S. M., and Padmanabhan, S. (2024). Potential applications of artificial intelligence (AI) in managing polypharmacy in Saudi Arabia: a narrative review. Healthc. (Basel) 5 (12), 788. doi:10.3390/healthcare12070788
American Geriatrics Society Beers Criteria® Update Expert Panel (2023). American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 71, 2052–2081. doi:10.1111/jgs.18372
Australian Institute of Health and Welfare (2023). Older Australians. Available online at: https://www.aihw.gov.au/reports/older-people/older-australians/contents/demographic-profile (Accessed November 15, 2024).
Barenholtz Levy, H. (2003). Self-administered medication-risk questionnaire in an elderly population. Ann. Pharmacother. 37, 982–987. doi:10.1345/aph.1C305
Berbatis, C. G., Sunderland, V. B., Joyce, A., Bulsara, M., and Mills, C. (2007). Characteristics of Australia’s community pharmacies: national Pharmacy Database project. Int. J. Pharm. Pract. 15, 265–271. doi:10.1211/ijpp.15.4.0003
Blalock, S. J., and Patel, R. A. (2005). Drug therapy concerns questionnaire: initial development and refinement. J. Am. Pharm. Assoc. 45, 160–169. doi:10.1331/1544345053623465
Butler, J. A., Peveler, R. C., Roderick, P., Horne, R., and Mason, J. C. (2004). Measuring compliance with drug regimens after renal transplantation: comparison of self-report and clinician rating with electronic monitoring. Transplantation 77, 786–789. doi:10.1097/01.tp.0000110412.20050.36
Cardwell, K., Hughes, C. M., and Ryan, C. (2018). Community pharmacists’ views of using a screening tool to structure medicines use reviews for older people: findings from qualitative interviews. Int. J. Clin. Pharm. 40, 1086–1095. doi:10.1007/s11096-018-0659-z
Chalasani, S. H., Syed, J., Ramesh, M., Patil, V., and Kumar, T. P. (2023). Artificial intelligence in the field of pharmacy practice: a literature review. Explor Res. Clin. Soc. Pharm. 12, 100346. doi:10.1016/j.rcsop.2023.100346
Cipolle, R. J., Strand, L. M., and Morley, P. C. (2012). Pharmaceutical care practice: the patient-centered approach to medication management 3e. The McGraw-Hill Companies. Available online at: https://accesspharmacy.mhmedical.com/content.aspx?bookid=491§ionid=39674898 (Accessed March 03, 2025).
Collins, J. C., Hu, J., McMillan, S. S., O’Reilly, C. L., El-Den, S., Kelly, F., et al. (2023). Medication-related problems identified by community pharmacists: a descriptive case study of two Australian populations. J. Pharm. Policy Pract. 16, 133. doi:10.1186/s40545-023-00637-x
de Oliveira, D. R., and Shoemaker, S. J. (2006). Achieving patient centeredness in pharmacy practice: openness and the pharmacist’s natural attitude. J. Am. Pharm. Assoc. 46, 56–64. doi:10.1331/154434506775268724
Elm, E. von, Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., and Vandenbroucke, J. P. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335, 806–808. doi:10.1136/bmj.39335.541782.ad
Gargya, D., Mirkazemi, C., and Curtain, C. (2022). Qualitative exploration of the experiences of community pharmacists delivering the Diabetes MedsCheck service. J. Clin. Pharm. Ther. 47, 1194–1200. doi:10.1111/jcpt.13654
Gordon, K. J., Smith, F. J., and Dhillon, S. (2005). The development and validation of a screening tool for the identification of patients experiencing medication-related problems. Int. J. Pharm. Pract. 13, 187–193. doi:10.1211/ijpp.13.3.0004
Graafsma, J., Murphy, R. M., van de Garde, E. M., Karapinar-Çarkit, F., Derijks, H. J., Hoge, R. H., et al. (2024). The use of artificial intelligence to optimize medication alerts generated by clinical decision support systems: a scoping review. J. Am. Med. Inf. Assoc. 31, 1411–1422. doi:10.1093/jamia/ocae076
Hamadouk, R. M., Yousef, B. A., Albashair, E. D., Mohammed, F. M., and Arbab, A. H. (2023). Perceptions of community pharmacists towards patient counseling and continuing pharmacy education programs in Sudan. Integr. Pharm. Res. Pract. 12, 77–85. doi:10.2147/iprp.s406219
Hogervorst, S., Adriaanse, M. C., Vervloet, M., Teichert, M., Beckeringh, J. J., van Dijk, L., et al. (2024). A survey on the implementation of clinical medication reviews in community pharmacies within a multidisciplinary setting. BMC Health Serv. Res. 24, 575. doi:10.1186/s12913-024-11013-z
Jarab, A. S., Al-Qerem, W., Alzoubi, K. H., Almomani, N., Abu Heshmeh, S., Mukattash, T., et al. (2024). Exploring pharmacists’ attitude, willingness and barriers to provide extended community pharmacy services: implications for improved pharmacy services. Plos one 19, e0310141. doi:10.1371/journal.pone.0310141
Kanaani, E., Salahudeen, M. S., and Curtain, C. (2023). Australian community pharmacists’ experiences during the COVID-19 pandemic. Int J Pharm Prac 31, 472–477. doi:10.1093/ijpp/riad038
Karia, A., Norman, R., Robinson, S., Lehnbom, E., Laba, T. L., Durakovic, I., et al. (2022). Pharmacist’s time spent: space for Pharmacy-based Interventions and Consultation TimE (SPICE)-an observational time and motion study. BMJ Open 12, e055597. doi:10.1136/bmjopen-2021-055597
Lim, R., Ellett, L. M. K., Semple, S., and Roughead, E. E. (2022). The extent of medication-related hospital admissions in Australia: a review from 1988 to 2021. Drug Saf. 45, 249–257. doi:10.1007/s40264-021-01144-1
Lounsbery, J. L., Green, C. G., Bennett, M. S., and Pedersen, C. A. (2009). Evaluation of pharmacists’ barriers to the implementation of medication therapy management services. J. Am. Pharm. Assoc. 49, 51–58. doi:10.1331/JAPhA.2009.017158
Maleki Varnosfaderani, S., and Forouzanfar, M. (2024). The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering 11, 337. doi:10.3390/bioengineering11040337
McLeod, P. J., Huang, A. R., Tamblyn, R. M., and Gayton, D. C. (1997). Defining inappropriate practices in prescribing for elderly people: a national consensus panel. CMAJ 156, 385–391.
Michel, D. E., Tonna, A. P., Dartsch, D. C., and Weidmann, A. E. (2023). Just a ‘romantic idea’? A theory-based interview study on medication review implementation with pharmacy owners. Int J Clin Pharm 45, 451–460. doi:10.1007/s11096-022-01524-2
Milton, J. C., Hill-Smith, I., and Jackson, S. H. D. (2008). Prescribing for older people. BMJ 336, 606–609. doi:10.1136/bmj.39503.424653.80
Nicosia, F. M., Spar, M. J., Stebbins, M., Sudore, R. L., Ritchie, C. S., Lee, K. P., et al. (2019). What is a medication-related problem? A qualitative study of older adults and primary care clinicians. J. Gen. Intern Med. 35, 724–731. doi:10.1007/s11606-019-05463-z
O’Mahony, D., Cherubini, A., Guiteras, A. R., Denkinger, M., Beuscart, J.-B., Onder, G., et al. (2023). STOPP/START criteria for potentially inappropriate prescribing in older people: version 3. Eur. Geria Med. 14, 625–632. doi:10.1007/s41999-023-00777-y
Pammett, R. T., Blackburn, D., Taylor, J., Mansell, K., Kwan, D., Papoushek, C., et al. (2015). Evaluation of a community pharmacy–based screening questionnaire to identify patients at risk for drug therapy problems. Pharmacotherapy 35, 881–886. doi:10.1002/phar.1633
Paulino, E. I., Bouvy, M. L., Gastelurrutia, M. A., Guerreiro, M., and Buurma, H.ESCP-SIR Rejkjavik Community Pharmacy Research Group (2004). Drug related problems identified by European community pharmacists in patients discharged from hospital. Pharm. World Sci. 26, 353–360.
Pharmaceutical Care Network Europe (2020). PCNE Classification for drug-related problems V9, 1. Available online at: https://www.pcne.org/upload/files/417_PCNE_classification_V9-1_final.pdf (Accessed December 21, 2023).
Pharmacy Guild of Australia (2021). Skills shortages as reported by ACCI members. Available online at: https://www.aph.gov.au/DocumentStore.ashx?id=5bf53bc9-99a2-41f3-ac86-d39f8cdbeb15 (Accessed December 22, 2023).
Pharmacy Programs Administrators (2021). MedsCheck and Diabetes Medscheck program Rules. Available online at: https://www.ppaonline.com.au/wp-content/uploads/2019/01/MedsCheck-and-Diabetes-Medscheck-Program-Rules.pdf (Accessed November 15, 2024).
Pharmacy Programs Administrators (2022). Residential medication management review and Quality Use of medicines. Available online at: https://www.ppaonline.com.au/programs/medication-management-programs/residential-medication-management-review-and-quality-use-of-medicines (Accessed November 15, 2024).
Puumalainen, E., Airaksinen, M., Jalava, S. E., Chen, T. F., and Dimitrow, M. (2019). Comparison of drug-related problem risk assessment tools for older adults: a systematic review. Eur. J. Clin. Pharmacol. 76, 337–348. doi:10.1007/s00228-019-02796-w
Qualtrics.XM (2023). Available online at: https://www.qualtrics.com (Accessed November 5, 2023).
Resnik, D. B., Ranelli, P. L., and Resnik, S. P. (2000). The conflict between ethics and business in community pharmacy: what about patient counseling? J. Busi Ethics. 28, 179–186. doi:10.1023/a:1006280300427
Taylor, S. E., Mitri, E. A., Harding, A. M., Taylor, D. M., Weeks, A., Abbott, L., et al. (2022). Development of screening tools to predict medication-related problems across the continuum of emergency department care: a prospective, multicenter study. Front. Pharmacol. 13, 865769. doi:10.3389/fphar.2022.865769
Wembridge, P., Ngo, C., Tran, T. H. T., and Ivar, M. P. (2023). Evaluating pharmacy high-needs criteria: a tool for identifying inpatients at risk of medication-related problems. J. Pharm. Pract. Res. 53, 91–95. doi:10.1002/jppr.1845
Wetzels, G., Nelemans, P., van Wijk, B., Broers, N., Schouten, J., and Prins, M. (2006). Determinants of poor adherence in hypertensive patients: development and validation of the Maastricht Utrecht adherence in Hypertension (MUAH)-questionnaire. Patient Educ. Couns. 64, 151–158. doi:10.1016/j.pec.2005.12.010
Keywords: community pharmacist, medication-related problem, drug-related problem, screening tool, self-administered, medication safety, community pharmacy
Citation: Salahudeen MS, Saadeldean AS, Peterson GM, Tesfaye BT and Curtain CM (2025) Community pharmacists’ views towards implementing a patient self-administered screening tool designed to identify risk of medication-related problems. Front. Pharmacol. 16:1531500. doi: 10.3389/fphar.2025.1531500
Received: 20 November 2024; Accepted: 06 March 2025;
Published: 26 March 2025.
Edited by:
Olga Lourenço, University of Beira Interior, PortugalReviewed by:
Dalia Almaghaslah, King Khalid University, Saudi ArabiaCopyright © 2025 Salahudeen, Saadeldean, Peterson, Tesfaye and Curtain. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed S. Salahudeen, bW9oYW1tZWQuc2FsYWh1ZGVlbkB1dGFzLmVkdS5hdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.