
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 16 December 2024
Sec. Obstetric and Pediatric Pharmacology
Volume 15 - 2024 | https://doi.org/10.3389/fphar.2024.1503536
Objectives: To assess the effectiveness of various atropine concentrations in managing myopia among children in East, South, and Southeast Asia, and to determine the most effective concentration.
Methods: A systematic literature review was conducted using PubMed, Web of Science, Cochrane Library, and EMBASE. The search was limited to articles published up to 1 June 2024, and included studies in Chinese or English. Two researchers independently screened the literature, extracted relevant data, and assessed the data quality using the Revised Cochrane risk-of-bias 2 (RoB2) tool. A network meta-analysis was performed using Stata 14.2 software to compare the efficacy of different atropine concentrations in delaying myopia progression, measured by changes in refraction and axial length.
Results: The analysis included 39 studies with 7,712 participants, examining 10 atropine concentrations ranging from 0.005% to 1%. Forest plots indicated that five concentrations (0.01%, 0.02%, 0.025%, 0.05%, and 1%) were more effective than a placebo in controlling myopia progression. The cumulative ordination plot indicated that 0.05% atropine most effectively delayed refraction change, which the mean change per year was 0.62D, while 1% was superior in slowing axial length progression, which the mean change per year was −0.43 mm. Considering both measures, 1% atropine showed the highest efficacy which the mean changes per year were 0.56D in spherical equivalent refraction and −0.43 mm in axial length, followed by 0.05% and 0.125% atropine.
Conclusion: While 1% atropine demonstrated the highest efficacy in myopia control among East, South and Southeast Asian children, its use is not recommended due to increased adverse effects and a rapid rebound in myopia after cessation. Considering both efficacy and safety, 0.05% atropine is suggested as the optimal concentration for myopia management in this population.
Refractive errors are a leading cause of vision impairment globally, affecting an estimated 12.8 million children aged 5-15, with the highest prevalence in Asia (Resnikoff et al., 2008). Myopia, in particular, is a predominant visual health issue among adolescents. Projections indicate that by 2050, nearly half the world’s population—4.8 billion individuals—will be myopic (Holden et al., 2016). The prevalence of myopia in East, South and Southeast Asia is nearly 90%, with a higher proportion of high myopia cases compared to the 50% prevalence rate among European youth (Morgan et al., 2018). This disparity may be due to genetic factors, as well as increased educational pressures and lifestyle changes impacting students’ eye health (Ig et al., 2012). The rising prevalence of myopia annually is linked to serious complications such as glaucoma, scleral staphyloma, retinal tears, and retinal detachment, posing significant threats to the visual health of Asian adolescents (Haarman et al., 2020). Therefore, controlling the onset of myopia in school-aged children and managing its progression is vital for reducing the risk of high myopia and its associated complications later in life (Saw et al., 2019).
Current treatments for myopia encompass spectacles, orthokeratology lenses, pharmaceutical eye drops (including atropine, pirenzepine, and timolol), and repeated low-level red-light (LLRL) therapy (Tapasztó et al., 2023). However, traditional optical interventions have shown limitations in controlling myopia progression, with diminishing effects over time (Jones et al., 2022; Lam et al., 2022; Sankaridurg et al., 2023). For example, a study by Sarkar et al. (2023) found that the maximum control effect of spectacles, soft contact lenses, and orthokeratology lenses occurred within the first 12 months of treatment. Emerging treatments like LLRL, while promising, lack robust clinical evidence due to their brief implementation period and have been associated with adverse events such as choroidal thickening, as reported in a multicenter randomized controlled trial by Jiang et al. (2022).
Atropine eye drops have emerged as a prominent method in myopia control. Clinical studies have shown that various concentrations of atropine are more effective in preventing and slowing the progression of myopia in adolescents than other single treatments (Chia et al., 2016; Yam et al., 2019; Li et al., 2021; Repka et al., 2023). A 2023 study, which analyzed results from 64 trials, concluded that high-dose topical atropine (≥0.5%) is the most effective intervention for reducing the axial elongation rate (Lawrenson et al., 2023). Research by Li et al. (2014) further supports the significant slowing effect of atropine on the progression of myopia in children, particularly in Asian children. As atropine’s use expands in myopia prevention and control among adolescents across different Asian economies, the selection of individualized concentrations and consideration of potential side effects are crucial for clinical decisions. While previous meta-analyses have evaluated the efficacy of different atropine concentrations (Gong et al., 2017; Fu et al., 2020; Wang et al., 2024), a systematic review or meta-analysis comprehensively summarizing its effects on the East, South and Southeast Asian population has been lacking. Thus, leveraging the latest randomized controlled trials (RCTs), we conducted a network meta-analysis to assess the impact of different concentrations of atropine eye drops on key ocular anatomical parameters such as spherical equivalent refraction (SER) and axial length (AL) in Asian children.
This study strictly adhered to the guidelines of the Preferred Reporting Items for Systematic Reviews incorporating Network Meta-Analyses (PRISMA-NMA) and was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the identifier CRD42024551014 (Hutton et al., 2015).
The study included randomized clinical trials (RCTs) and observational studies that met the following criteria:
(ⅰ). Participants were East, South and Southeast Asian individuals under 18 years old with myopia (spherical equivalent ≤ −0.5 diopters).
(ⅱ). Studies utilized at least one concentration of atropine eye drops, with controls including other treatments for myopia, placebos, monovision lenses, or no treatment.
(ⅲ). They reported outcomes related to myopia progression (e.g., changes in refraction and axial length) and/or side effects of atropine therapy.
(ⅳ). Ethical review board approval was documented.
Exclusions applied to studies not available in full text, non-original articles like case reports, reviews, conference abstracts, editorials, letters, non-human studies, and those with duplicate or non-applicable data.
A systematic search was conducted across four databases—PubMed, Web of Science, Cochrane Library, and EMBASE—focusing on RCTs and observational studies concerning atropine concentrations for myopia control in children. The search spanned from database inception to 1 June 2024, and was limited to Chinese or English language publications. Search terms encompassed “atropine,” “atropine sulfate,” “cholinergic antagonists,” “atropinol,” “myopia,” “nearsightedness,” and “shortsightedness.” Adjustments were made for database-specific requirements, and relevant review and meta-analysis literature was traced for additional literature. Detailed search strategies are provided in the Supplementary Tables S1–S4.
Zotero software facilitated the management of retrieved literature. Two researchers independently screened articles based on the inclusion and exclusion criteria, initially reviewing titles and abstracts, followed by full-text assessments. Any discrepancies were resolved through discussion or by a third party, who also evaluated the risk of bias and study quality. Extracted data encompassed first author, publication year, study location, participant demographics, follow-up duration, intervention details, sample size, baseline characteristics, mean change data, and adverse reactions.
The Revised Cochrane risk-of-bias 2 (RoB2) tool was used to assess five bias aspects: the randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported results. Each aspect was rated as ‘high risk’, ‘low risk’, or ‘some concerns' (Jp et al., 2011). Two researchers independently evaluated the studies, with final consensus reached through discussion.
Refraction and axial length, being continuous variables, were analyzed using mean difference (MD) as the effect size, with each study’s effect size presented as a 95% confidence interval (CI). The significance level was set at 0.05. Network Meta-analysis was conducted using the network package of Stata 14.2 software. We used heterogeneity variance parameter (τ2) and generalized Cochran’s Q to assess heterogeneity between studies. If there is heterogeneity, we use a random-effects model based on a frequentist approach, and conversely, we will use a fixed-effects model. Inconsistency was assessed using the inconsistency model and node-splitting method. Node splitting is an effective method used to test for local inconsistency in network meta-analysis. The method determined the presence of local inconsistencies by splitting nodes (i.e., different atropine concentrations) in a network into multiple parts, thereby assessing the impact of these different parts on the results separately. Compared with the inconsistency model, it can reveal local sources of inconsistency in a finer way, which helped to understand and explain the discrepancies in the results of the study, and ensured the reliability and stability of the results of the network meta-analysis. A p-value > 0.05 indicated no significant inconsistency. If inconsistency was minimal, the consistency model was applied. Loop inconsistency was also tested; a small inconsistency factor (IF) with a 95% CI including 0 indicated no significant loop inconsistency, ensuring stability and reliability of direct and indirect comparisons. Network plots were constructed, with line thickness indicating the number of direct comparisons and node size reflecting sample size. The Surface Under the Cumulative Ranking (SUCRA) was calculated to rank treatments, with values closer to one indicating higher efficacy. Funnel plots and egger’s test were used to assess publication bias, with asymmetry showing potential bias. Forest plots and league tables were also generated.
Our systematic search across PubMed, Web of Science, Cochrane Library, and EMBASE yielded 2,808 documents related to the study topic. After excluding 1,409 duplicates, a full-text evaluation of the remaining 1,399 documents led to the exclusion of 1,360 studies due to incompatibility with the study criteria or other reasons. This rigorous process resulted in the inclusion of 39 eligible studies, the details of which are depicted in the PRISMA flowchart (Figure 1).
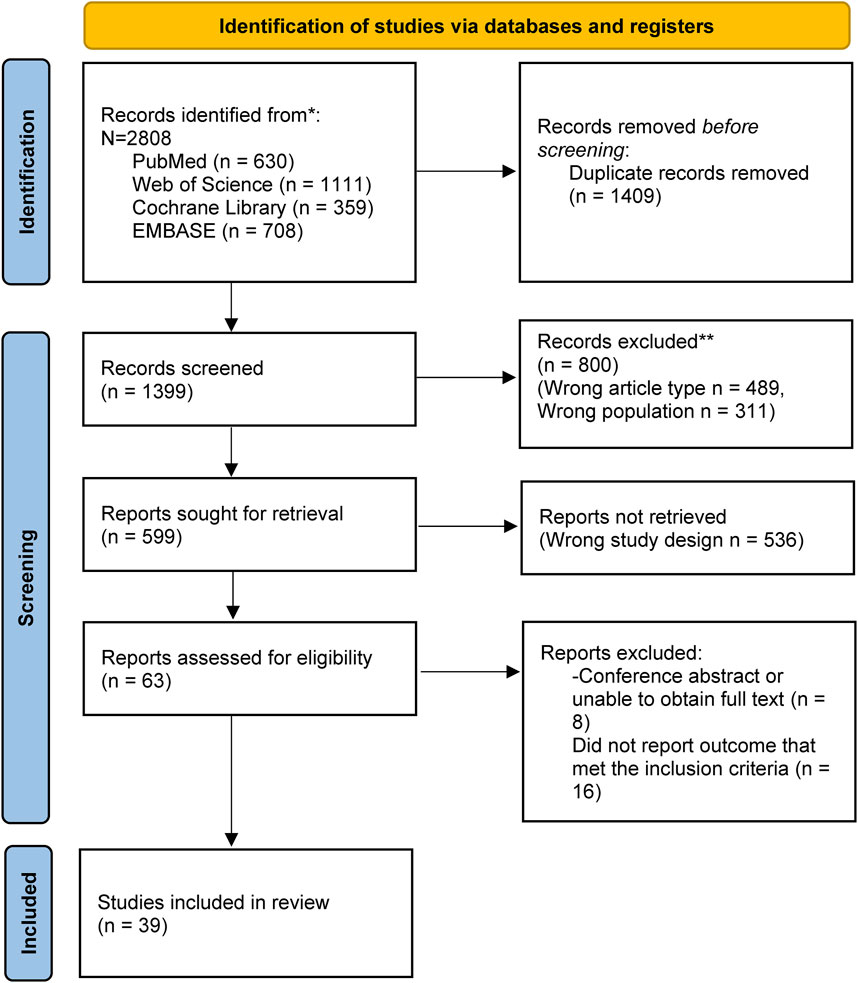
Figure 1. PRISMA flow diagram shows the study process. PRISMA: Preferred reporting items for systematic review and Meta-analysis.
These 39 studies encompassed a total of 7,712 participants, with 2,146 in the non-atropine treatment group and 5,566 in the atropine treatment group. The studies spanned a publication period from 2006 to 2024 and were conducted among East, South and Southeast Asian populations. The follow-up duration varied from 3 to 54 months, encompassing children aged 4–15 years with varying severities of myopia. Treatments involved 10 different atropine concentrations: 0.005%, 0.0025%, 0.01%, 0.02%, 0.025%, 0.05%, 0.1%, 0.125%, 0.5%, and 1%. Most studies provided data on baseline refraction and axial length (AL), as well as mean changes in these parameters. However, only one study reported adverse effects, and there were gaps in the data: two studies lacked mean change in refraction, and three studies did not report both mean change in refraction and AL. A comprehensive list of the included data are presented in Table 1.
In the comprehensive assessment of the included studies, 6 out of the 39 studies were identified to have a high risk of bias, primarily due to issues in the randomization process and deviations from the intended interventions. The most common source of bias observed was the deviation from the intended interventions during subject allocation. This may produce selection bias and performance bias. Selection bias may lead to an inaccurate response to the efficacy of atropine, affecting the representativeness of the sample, and performance bias may result in erroneous data being collected, affecting the veracity and reliability of the study results. However, outcome measurement and result selection were relatively standardized across the studies. Only 2 studies managed to achieve a low risk of bias, indicating that the majority of the trials exhibited varying degrees of concern regarding bias. The visual representation of these risk assessments is provided in Figures 2, 3.
We excluded missing data directly from the analysis when we conducted our analyses.
In our network analysis, 37 studies reported data on changes in refraction following the intervention. Among these, 27 were two-armed studies, and 10 were multi-armed studies. The studies evaluated 10 different concentrations of atropine concentrations: 0.05%, 0.01%, 0.02%, 1%, 0.5%, 0.1%, 0.005%, 0.0025%, 0.025%, and 0.125%. The network plot for refraction change revealed that the 0.01% atropine concentration had a larger node area compared to placebo, indicating a larger total sample size for this concentration. Additionally, the thicker connecting line between 0.01% atropine and placebo in the network plot revealed a greater number of direct comparisons between these two treatments, as illustrated in Figure 4.
Thirty-six studies reported changes in axial length following the intervention, with 27 being two-armed and 9 being multi-armed studies. Nine different atropine concentrations were considered in these analyses, but the 0.0025% concentration was not included in the axial length studies. The network plot for the change showed larger node areas for the 0.01% atropine concentration, placebo, 0.05% atropine concentration, and 0.025% atropine concentration, indicating a larger total sample size for these concentrations. The thicker connecting line between 0.01% atropine and placebo in this plot also indicated a greater number of direct comparisons, mirroring the pattern observed in the network plot, as shown in Figure 5.
The results of heterogeneity showed τ2 of 0.0579 and Cochran’s Q of 534.84 (p < 0.05) for change in refraction and τ2 of 0.0121 and Cochran’s Q of 475.76 (p < 0.05) for change in axial length, suggesting that there was heterogeneity among the studies. Therefore, we will choose a random effects model based on the frequentist approach for our analysis.
The global inconsistency of the network meta-analysis was assessed using Stata 14.2’s inconsistency model. The resulting p-value of 0.7882, which is greater than 0.05, indicated that the global inconsistency is not significant. Further analysis of local inconsistency using the node splitting method also revealed p-values greater than 0.05 for each study, reporting that local inconsistencies are negligible. This implied that the discrepancies between direct and indirect comparison results were minimal. Consequently, the consistency model was appropriate for this study’s analysis. Additionally, the loop inconsistency test results showed small inconsistency factors (IFs) close to zero for each closed loop, with confidence intervals that include zero. This indicated that loop inconsistency was not significant, further supporting the stability and reliability of both direct and indirect comparison outcomes, as detailed in the Supplementary Figure S1 and Figure 2.
The forest plot, which included 55 pairs of two-by-two comparisons with refraction change as the outcome metric, was depicted in Figures 6, 8. In comparisons against placebo, the mean changes per year and their 95% confidence intervals (CIs) for atropine concentrations at 0.025%, 1%, 0.02%, 0.01%, and 0.05% were 0.43D/year (0.24, 0.63), 0.56D/year (0.35, 0.77), 0.29D/year (0.08, 0.49), 0.31D/year (0.21, 0.41), and 0.62D/year (0.46, 0.79), respectively. All p-values were less than 0.05, indicating that these atropine concentrations were more effective in delaying refraction progression than placebo. When compared to 0.05% atropine, the mean changes per year and their 95% confidence intervals for 0.01%, 0.02%, and 0.0025% atropine were −0.32D/year (−0.48, −0.15), −0.34D/year (−0.59, −0.09), and −0.55D/year (−1.02, −0.08), respectively, with p-values less than 0.05, reflecting these concentrations were less effective than 0.05% atropine. The comparison of 1% atropine against 0.01% showed a mean change of 0.25D/year (0.03, 0.48) with a p-value less than 0.05, indicating that 1% atropine was more effective in delaying refraction progression.
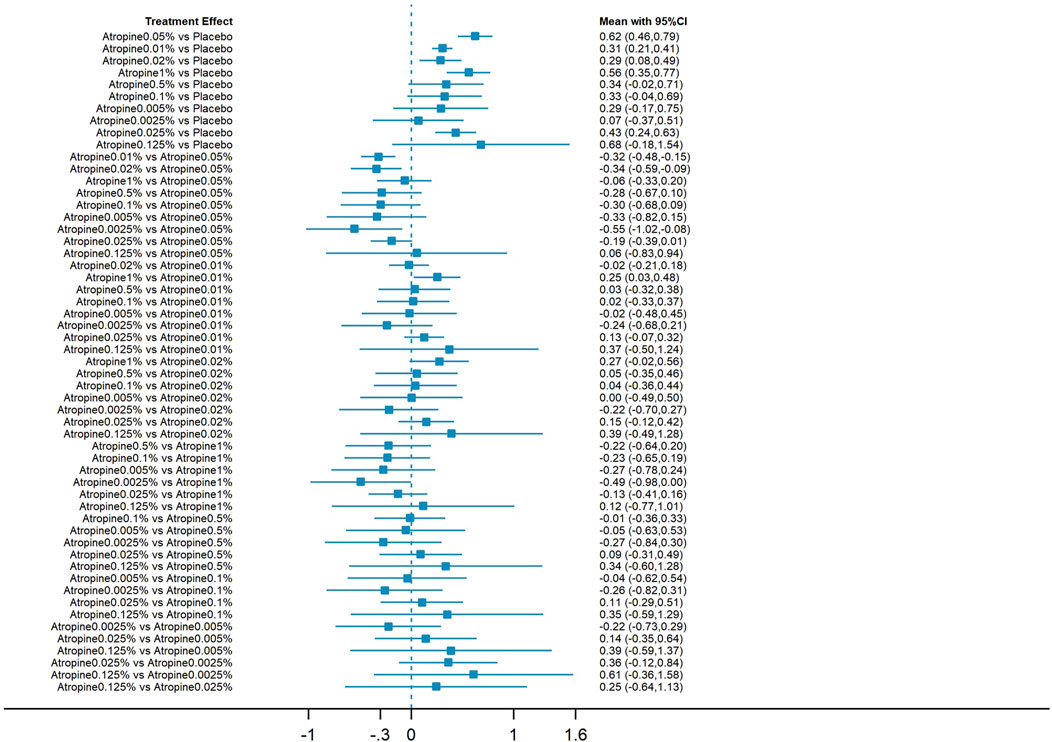
Figure 6. Forest plot contrasting various atropine doses for refraction change. CI: Confidence interval.
The forest plot with 45 pairs of two-by-two comparisons using axial length change as the outcome metric is shown in Figures 7, 8. In placebo comparisons, the mean changes per year and their 95% confidence intervals for atropine concentrations at 0.05%, 0.01%, 0.02%, 1%, and 0.025% were −0.27 mm/year (−0.39, −0.15), −0.13 mm/year (−0.20, −0.07), −0.17 mm/year (−0.29, −0.04), −0.43 mm/year (−0.56, −0.31), and −0.20 mm/year (−0.33, −0.06), respectively, with p-values less than 0.05, indicating these atropine concentrations were more effective in slowing axial length progression than placebo. The comparison of 0.01% atropine against 0.05% showed a mean change of 0.13 mm/year (0.02, 0.25) with a p-value less than 0.05, suggesting 0.01% atropine was less effective. The comparison of 1% atropine against 0.01% showed a mean change of −0.30 mm/year (−0.43, −0.17) with a p-value less than 0.05, indicating 1% atropine was more effective. When comparing 1% atropine with 0.02%, the mean change was −0.27 mm/year (−0.44, −0.09) with a p-value less than 0.05, showing 1% atropine was more effective. In comparisons with 1% atropine, the means and 95% confidence intervals for 0.1%, 0.005%, and 0.025% atropine were 0.29 mm (0.03, 0.54), 0.34 mm (0.04, 0.63), and 0.24 mm/year (0.05, 0.42), respectively, with p-values less than 0.05, indicating these concentrations were less effective than 1% atropine in slowing axial length progression.
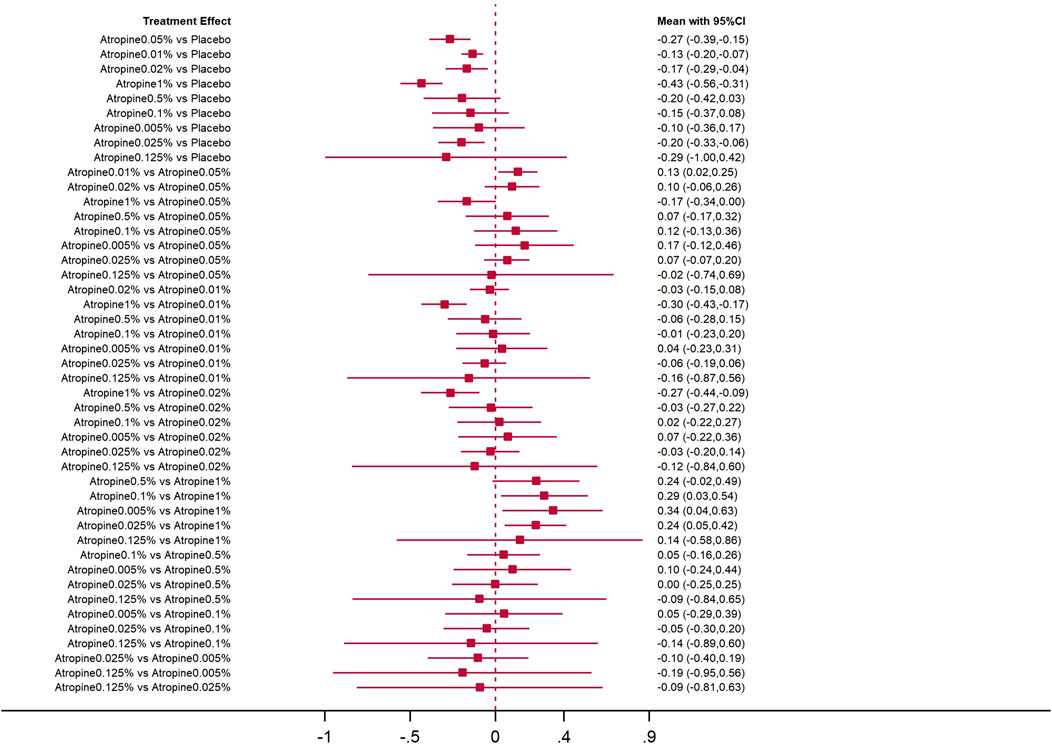
Figure 7. Forest plot contrasting various atropine doses for axial length change. CI: Confidence interval.
The Surface Under the Cumulative Ranking (SUCRA) analysis provided insights into the relative efficacy of different atropine concentrations and placebo in managing myopia. For changes in refraction, 0.05% atropine was the most effective, with a SUCRA value of 88.7%, ranking it first among all treatments. The efficacy ranking, from highest to lowest, was as follows: 0.05% atropine, 1% atropine (80.3%), 0.125% atropine (75.5%), 0.025% atropine (63.1%), 0.5% atropine (48.4%), 0.1% atropine (46.7%), 0.005% atropine (42.8%), 0.01% atropine (41.6%), 0.02% atropine (39%), 0.0025% atropine (17.7%), and placebo with the lowest efficacy at 6.4%.
In contrast, when considering changes in axial length, 1% atropine emerged as the most efficacious with a SUCRA value of 95.3%, ranking it first. The ranking for the change was: 1% atropine, followed by 0.05% atropine (73.7%), 0.125% atropine (60.4%), 0.5% atropine (54.7%) which was equally effective as 0.025% atropine (54.7%), 0.02% atropine (47.3%), 0.1% atropine (41.2%), 0.01% atropine (34.8%), 0.005% atropine (31.2%), and finally placebo at 6.9%. These rankings are visually represented in Figures 9, 10.
To determine the most effective atropine concentration for controlling myopia progression, cluster analysis was conducted on the key outcome measures: refraction and axial length changes. The analysis revealed that the 1% atropine concentration was the most distant from the origin (zero point) in the two-dimensional coordinate system, indicating its superior efficacy in delaying both refraction and axial length increases. Conversely, the placebo was found to be the closest to the origin, indicating the least effective treatment in this context. These findings are visually depicted in Figure 11.
To assess potential publication bias, funnel plots were constructed based on two key outcome measures: changes in refraction and axial length. The distribution of the studies across the funnel plots indicated a generally symmetrical pattern around the midline, suggesting that the majority of the clinical efficacy studies were consistent in their findings. However, the presence of some studies at the lower end of the funnel, falling outside the 95% confidence interval boundaries, raised concerns about possible publication bias and the influence of small sample sizes. Egger’s test showed that the p-value was 0.4763 (>0.05) in refraction change, which indicated that there was no significant publication bias or small-sample effect; and the p-value was <0.05 in axial length change, which indicated that there was publication bias. These observations are illustrated in Figures 12, 13.
In this study, a network meta-analysis was conducted on 39 papers to evaluate the effectiveness of 10 different atropine concentrations in delaying myopia progression in East, South and Southeast Asian children. The analysis revealed that five concentrations—0.05%, 0.01%, 0.02%, 1%, and 0.025% atropine—were more effective in delaying refraction change compared to other concentrations. Similarly, these concentrations also showed comparable efficacy in slowing the progression of the axial length.
When ranking the efficacy of these atropine concentrations, 0.05% atropine emerged as the most effective in slowing refraction change, while 1% atropine was found to be the most effective in slowing the progression of axial length. The combined efficacy in terms of both refraction and axial length indicated that 1% atropine was superior, followed by 0.05% and 0.125% atropine.
Despite its high efficacy, 1% atropine is associated with a higher incidence of post-dose adverse effects and a more rapid rebound of myopia after treatment cessation, as noted in previous studies (Kumaran et al., 2015; Wu et al., 2019; Gan et al., 2022). This indicates that 1% atropine may not be the optimal concentration. An adverse effect is a harmful reaction unrelated to the therapeutic purpose that occurs during the prevention, diagnosis or treatment of a disease when the drug is used according to normal usage and dosage. Common adverse effects are seen in the use of atropine solution to delay myopia: photophobia, poor near visual acuity, allergy, chalazion and systemic effects. Post-medication myopia rebound is a phenomenon in which myopia is effectively controlled or slows down during treatment with atropine solution, but after stopping the medication, myopia increases again to a certain extent due to various factors. Several studies have shown that the higher the concentration of atropine, the more likely it is that adverse effects or myopia rebound will occur (Kumaran et al., 2015; Gong et al., 2017). A meta-analysis showed that the incidence of photophobia during the treatment period was 43.1% for atropine at concentrations of 0.5%–1%, compared with only 17.8% for atropine at concentrations of 0.01%–0.5% (Gong et al., 2017).The ideal atropine concentration should balance efficacy and safety, not merely focusing on the former (Ha et al., 2022). 0.05% atropine, which is the second most effective, offers efficacy comparable to 1% atropine but with a lower incidence of adverse effects and a slower myopia rebound rate after discontinuation (Gong et al., 2017; Zhu Q. et al., 2023). This makes 0.05% atropine a potential optimal concentration for myopia control in children in East, South and Southeast Asia.
Furthermore, this study finds that there may be no significant difference between 0.5%, 0.1%, 0.005%, 0.0025% atropine, 0.125% atropine, and placebo in terms of delaying refractive error and axial length progression. This finding contrasts with other studies (Wu et al., 2019; Ha et al., 2022). The inconsistency could be attributed to the limited number of studies that included these atropine concentrations and the potential influence of small sample sizes. Small sample effects and publication bias may lead to overestimate the true effect of a treatment and increase the uncertainty of the results, thereby interfering with the overall findings. Thus, the results from this study should be viewed with caution. Future research should prioritize higher-quality studies to ascertain the true efficacy of these atropine concentrations.
Low-concentration atropine, which includes 0.05% atropine, slows myopic progression primarily by reducing axial length growth, and it does not cause significant changes in other ocular biometric parameters, which reduces the incidence of ocular complications (Li et al., 2020; Yam et al., 2022). Although 0.05% atropine is the optimal concentration for balancing effectiveness and safety, 0.05% atropine can also produce adverse effects such as photophobia. To reduce the incidence and magnitude of adverse effects, UV photochromic lenses can be worn along with the medication (Qin et al., 2023). Regarding when to stop using atropine, some studies suggest that it is better to stop using atropine at an older age, when myopia progression is minimized. Before discontinuing atropine, atropine concentrations should be gradually reduced until the time of discontinuation (Yam et al., 2022).
The exploration of 0.01% atropine as a treatment for controlling myopia in children has gained significant interest. It maintains effectiveness while minimizing side effects and the rebound of myopia after treatment cessation, as well as facilitating a quicker recovery of pupil diameters affected by the medication (Chia et al., 2014; 2023). However, the suitability of 0.01% atropine is not universal among myopic children (Wang et al., 2020). Research indicates that Asian myopic children and those of Asian descent tend to respond better to 0.01% atropine than Caucasian children, possibly due to differences in iris melanin content (Jeon et al., 2022). Additionally, the age of onset of myopia influences the effectiveness of atropine, with earlier onset associated with reduced efficacy. Furthermore, children with high myopia or a family history of high myopia, as well as those with rapid myopia progression, may not respond as well to low concentrations of atropine (Clark and Clark, 2015; Jeon et al., 2022). Interestingly, some studies propose that 0.01% atropine may have a preventive effect on myopia development in non-myopic children who are at high risk. In summary, 0.01% atropine is deemed appropriate for older children of Asian or Asian descent with low initial myopia and for myopia prevention in at-risk children. However, the optimal duration of treatment, continuation, and cessation remain unclear and warrant further investigation.
The progression of myopia in adolescents is influenced by a multitude of factors, including genetic, environmental, gender, and ocular parameters (Yu et al., 2023). Genetic predisposition plays a role, with children from families with a history of myopia being more susceptible to developing myopia (Xiao et al., 2022). In addition to this, genetic differences are also reflected in the efficacy of atropine in the treatment of myopia. Atropine is more effective in controlling the progression of myopia in Asian children compared to white children. The exact mechanism by which atropine slows the progression of myopia is yet unknown, but some research indicates that it primarily affects the retina’s melanocytes, which among other things release new molecules that prevent scleral expansion and slow the progression of myopia (Zhao and Hao, 2021). The effectiveness of atropine may be impacted by the quantity of melanin in the iris, which can differ between races (Fu et al., 2020). Moreover, it may also be related to the fact that Asian children themselves have a high degree of myopia, which progresses more rapidly. Environmental factors, particularly in East, South and Southeast Asia, contribute to a higher prevalence of myopia among children, potentially linked to the economic and educational standards of the region (Chen et al., 2024). Children from low-income countries and those from highly educated environments are more likely to be affected by myopia. This may be related to time spent outdoors and time spent using electronic screens. Prolonged close work and increased screen time, are positively correlated with myopia development, while outdoor activities have a negative correlation (Liu et al., 2024; Zhang X.B. et al., 2024). In addition, female children appear to have a higher incidence of myopia than males (Ying et al., 2024). Ocular characteristics, including smaller refractive error, longer axial length, lower accommodation, thinner lens, greater anterior chamber depth, and larger pupil diameter, are also associated with myopia development. Identifying these risk factors is crucial for targeting high-risk individuals for prevention and early intervention strategies to reduce the prevalence of myopia (Zhu S. et al., 2023).
This study represents one of the first network meta-analyses assessing the efficacy of atropine concentrations for myopia control in this specific demographic. Despite its contributions, the study has several limitations. Firstly, it focused solely on the efficacy of atropine concentrations in managing myopia, neglecting to conduct a network meta-analysis on their safety. This omission was due to the scarcity of studies reporting adverse events and the rebound of myopia following treatment cessation. There may be 2 reasons for this: first, before, most researchers focused mainly on the efficacy of atropine in delaying myopia, and few researchers focused on adverse effects and myopia rebound; moreover, the study period of atropine in delaying myopia is long, usually more than 6 months, and some studies lasted for up to 4 years, and the determination of adverse effects relies on the chief complaints of patients or patients’ families, which may generate recall bias, which increases the difficulty of collecting information. Going forward, there is a need for researchers to focus on the adverse effects and myopic rebound phenomenon produced by atropine, which will help in the comprehensive evaluation of atropine. Researchers can reduce recall bias by increasing the number of observations and shortening the duration of observations to make the data collected more accurate and reliable. Secondly, the analysis of publication bias demonstrated the potential influence of small sample sizes, necessitating a cautious interpretation of some findings. Additionally, the results indicate heterogeneity across studies, it is important to acknowledge that both known and unknown confounding factors, such as the age of initial myopia onset and family history of high myopia, could impact the efficacy of atropine. These factors could ideally be explored through subgroup analysis, but this was not feasible due to inadequate reporting in the existing literature. As different atropine concentrations become more widely available, it is anticipated that future research will provide more comprehensive insights, ultimately leading to a more definitive consensus on the optimal concentration for atropine use.
This study presents a network meta-analysis of 39 research papers focusing on the role of atropine concentrations in controlling myopia among children in East, South and Southeast Asia. It assessed 10 different concentrations of atropine, ranking their efficacy in terms of refraction and axial length. The analysis indicated that the 1% atropine concentration demonstrated the highest combined efficacy. However, when weighing efficacy against safety, 0.05% atropine emerges as a preferable option for myopia management in this demographic. It is important to recognize that 0.01% atropine, while popular, is not universally suitable for all myopic children. Customized treatment protocols tailored to individual characteristics are essential for optimal outcomes.
Looking ahead, there is a clear need for more extensive, multi-center, large-sample randomized controlled trials. These studies should aim to thoroughly investigate the adverse effects of atropine concentrations and the potential rebound effect following drug cessation. Researchers can reduce recall bias by increasing the number of observations and shortening the duration of observations to make the data collected more accurate and reliable. It is also not known whether there are potential long-term effects of atropine on children’s eye health. Long-term follow-up studies are needed to explore this question. Such research will enable a more comprehensive and nuanced evaluation of atropine concentrations for myopia control.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
XW: Methodology, Software, Validation, Writing–original draft. LZ: Methodology, Writing–original draft. JG: Project administration, Writing–review and editing. YW: Supervision, Writing–review and editing. WY: Project administration, Supervision, Writing–review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Supported by the Science and Technology Innovation Committee of Shenzhen (JCYJ20210324125614039).
We extend our sincerest gratitude to all the professionals who participated in this research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1503536/full#supplementary-material
Aicun, F., Junbo, R., Weiqun, W., Li, W., Junjie, Z., Bingxin, Z., et al. (2022). A randomized controlled clinical study of 0.01% and 0.02% atropine eye drops on myopia development in adolescents. Chin. J. Exp. Ophthalmol. 40, 253–259.
Chan, H. H. L., Choi, K. Y., Ng, A. L. K., Choy, B. N. K., Chan, J. C. H., Chan, S. S. H., et al. (2022). Efficacy of 0.01% atropine for myopia control in a randomized, placebo-controlled trial depends on baseline electroretinal response. Sci. Rep. 12, 11588. doi:10.1038/s41598-022-15686-6
Chaurasia, S., Negi, S., Kumar, A., Raj, S., Kaushik, S., Optom, R. K. M., et al. (2022). Efficacy of 0.01% low dose atropine and its correlation with various factors in myopia control in the Indian population. Sci. Rep. 12, 7113. doi:10.1038/s41598-022-10079-1
Chen, N., Sheng, Y., Wang, G., and Liu, J. (2024). Association between physical indicators and myopia in American adolescents: national health and nutrition examination survey 1999-2008. Am. J. Ophthalmol. 260, 132–139. doi:10.1016/j.ajo.2023.12.014
Chia, A., Chua, W. H., Cheung, Y. B., Wong, W. L., Lingham, A., Fong, A., et al. (2012). Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 119, 347–354. doi:10.1016/j.ophtha.2011.07.031
Chia, A., Chua, W. H., Wen, L., Fong, A., Goon, Y. Y., and Tan, D. (2014). Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5%. Am. J. Ophthalmol. 157, 451–457.e1. doi:10.1016/j.ajo.2013.09.020
Chia, A., Lu, Q.-S., and Tan, D. (2016). Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology 123, 391–399. doi:10.1016/j.ophtha.2015.07.004
Chia, A., Ngo, C., Choudry, N., Yamakawa, Y., and Tan, D. (2023). Atropine ophthalmic solution to reduce myopia progression in pediatric subjects: the randomized, double-blind multicenter phase ii apple study. Asia-Pacific J. Ophthalmol. 12, 370–376. doi:10.1097/APO.0000000000000609
Chua, W.-H., Balakrishnan, V., Chan, Y. H., Tong, L., Ling, Y., Quah, B. L., et al. (2006). Atropine for the treatment of childhood myopia. Ophthalmology 113, 2285–2291. doi:10.1016/j.ophtha.2006.05.062
Clark, T. Y., and Clark, R. A. (2015). Atropine 0.01% eyedrops significantly reduce the progression of childhood myopia. J. Ocular Pharmacol. Ther. 31, 541–545. doi:10.1089/jop.2015.0043
Cui, C. (2023). Effects of 0.01% atropine on ocular biometrics in myopic adolescents. Chin. J. Exp. Ophthalmol. 41, 330–337.
Cui, C., Li, X., Lyu, Y., Wei, L., Zhao, B., Yu, S., et al. (2021). Safety and efficacy of 0.02% and 0.01% atropine on controlling myopia progression: a 2-year clinical trial. Sci. Rep. 11, 22267. doi:10.1038/s41598-021-01708-2
Fang, P.-C., Chung, M.-Y., Yu, H.-J., and Wu, P.-C. (2010). Prevention of myopia onset with 0.025% atropine in premyopic children. J. Ocul. Pharmacol. Ther. 26, 341–345. doi:10.1089/jop.2009.0135
Fu, A., Stapleton, F., Wei, L., Wang, W., Zhao, B., Watt, K., et al. (2020). Effect of low-dose atropine on myopia progression, pupil diameter and accommodative amplitude: low-dose atropine and myopia progression. Br. J. Ophthalmol. 104, 1535–1541. bjophthalmol-2019-315440. doi:10.1136/bjophthalmol-2019-315440
Fu, A., Stapleton, F., Wei, L., Wang, W., Zhao, B., Watt, K., et al. (2021). Risk factors for rapid axial length elongation with low concentration atropine for myopia control. Sci. Rep. 11, 11729. doi:10.1038/s41598-021-88719-1
Gan, J., Li, S. M., Wu, S., Cao, K., Ma, D., He, X., et al. (2022). Varying dose of atropine in slowing myopia progression in children over different follow-up periods by meta-analysis. Front. Med. 8, 756398. doi:10.3389/fmed.2021.756398
Gong, Q., Janowski, M., Luo, M., Wei, H., Chen, B., Yang, G., et al. (2017). Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. 135, 624–630. doi:10.1001/jamaophthalmol.2017.1091
Ha, A., Kim, S. J., Shim, S. R., Kim, Y. K., and Jung, J. H. (2022). Efficacy and safety of 8 atropine concentrations for myopia control in children: a network meta-analysis. Ophthalmology 129, 322–333. doi:10.1016/j.ophtha.2021.10.016
Haarman, A. E. G., Enthoven, C. A., Tideman, J. W. L., Tedja, M. S., Verhoeven, V. J. M., and Klaver, C. C. W. (2020). The complications of myopia: a review and meta-analysis. Invest Ophthalmol. Vis. Sci. 61, 49. doi:10.1167/iovs.61.4.49
Han, W. T., Rong, A., and Xu, W. (2019). Combination with different anticholinergic eyedrops for the treatment of children myopia. Zhonghua Yi Xue Za Zhi 99, 1859–1863. doi:10.3760/cma.j.issn.0376-2491.2019.24.005
Hieda, O., Hiraoka, T., Fujikado, T., Ishiko, S., Hasebe, S., Torii, H., et al. (2021). Efficacy and safety of 0.01% atropine for prevention of childhood myopia in a 2-year randomized placebo-controlled study. Jpn. J. Ophthalmol. 65, 315–325. doi:10.1007/s10384-021-00822-y
Holden, B. A., Fricke, T. R., Wilson, D. A., Jong, M., Naidoo, K. S., Sankaridurg, P., et al. (2016). Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042. doi:10.1016/j.ophtha.2016.01.006
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 162, 777–784. doi:10.7326/M14-2385
Ig, M., K, O.-M., and Sm, S. (2012). Myopia. Lancet London, Engl. 379, 1739–1748. doi:10.1016/S0140-6736(12)60272-4
Jeon, G. S., Hong, I. H., Lee, J. H., Song, T. G., Lee, T. Y., and Han, J. R. (2022). Analysis of treatment response about low-dose (0.01%) atropine eye-drops in myopic children. Eur. J. Ophthalmol. 32, 2011–2017. doi:10.1177/11206721211038817
Jiang, Y., Zhu, Z., Tan, X., Kong, X., Zhong, H., Zhang, J., et al. (2022). Effect of repeated low-level red-light therapy for myopia control in children A multicenter randomized controlled trial. OPHTHALMOLOGY 129, 509–519. doi:10.1016/j.ophtha.2021.11.023
Jones, J. H., Mutti, D. O., Jones-Jordan, L. A., and Walline, J. J. (2022). Effect of combining 0.01% atropine with soft multifocal contact lenses on myopia progression in children. Optom. Vis. Sci. 99, 434–442. doi:10.1097/OPX.0000000000001884
Jp, H., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ Clin. Res. ed. 343, d5928. doi:10.1136/bmj.d5928
Kao, P.-H., Chuang, L. H., Lai, C. C., Chen, S. Y., Lin, K. K., Lee, J. S., et al. (2021). Evaluation of axial length to identify the effects of monocular 0.125% atropine treatment for pediatric anisometropia. Sci. Rep. 11, 21511. doi:10.1038/s41598-021-96414-4
Kumaran, A., Htoon, H. M., Tan, D., and Chia, A. (2015). Analysis of changes in refraction and biometry of atropine- and placebo-treated eyes. Investigative Ophthalmol. & Vis. Sci. 56, 5650–5655. doi:10.1167/iovs.14-14716
Lam, C. S. Y., Tang, W. C., Lee, P. H., Zhang, H. Y., Qi, H., Hasegawa, K., et al. (2022). Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. Br. J. Ophthalmol. 106, 1110–1114. doi:10.1136/bjophthalmol-2020-317664
Lawrenson, J. G., Shah, R., Huntjens, B., Downie, L. E., Virgili, G., Dhakal, R., et al. (2023). Interventions for myopia control in children: a living systematic review and network meta-analysis. Cochrane Database Syst. Rev. 2023. doi:10.1002/14651858.CD014758.pub2
Lee, J.-J., Fang, P. C., Yang, I. H., Chen, C. H., Lin, P. W., Lin, S. A., et al. (2006). Prevention of myopia progression with 0.05% atropine solution. J. Ocul. Pharmacol. Ther. 22, 41–46. doi:10.1089/jop.2006.22.41
Li, F. F., Kam, K. W., Zhang, Y., Tang, S. M., Young, A. L., Chen, L. J., et al. (2020). Differential effects on ocular biometrics by 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology 127, 1603–1611. doi:10.1016/j.ophtha.2020.06.004
Li, F. F., Zhang, Y., Zhang, X., Yip, B. H. K., Tang, S. M., Kam, K. W., et al. (2021). Age effect on treatment responses to 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology 128, 1180–1187. doi:10.1016/j.ophtha.2020.12.036
Li, S.-M., Wu, S. S., Kang, M. T., Liu, Y., Jia, S. M., Li, S. Y., et al. (2014). Atropine slows myopia progression more in Asian than white children by meta-analysis. Optom. Vis. Sci. 91, 342–350. doi:10.1097/OPX.0000000000000178
Liang, X., Wei, S., Li, S. M., An, W., Du, J., Sun, Y., et al. (2023). Effect of atropine 0.01% eye drops on the difference in refraction and axial length between right and left eyes. Ophthalmic Res. 66, 496–505. doi:10.1159/000528878
Liu, X., Zhao, F., Yuan, W., and Xu, J. (2024). Causal relationships between height, screen time, physical activity, sleep and myopia: univariable and multivariable Mendelian randomization. Front. Public Health 12, 1383449. doi:10.3389/fpubh.2024.1383449
Moon, J.-S., and Shin, S. Y. (2018). The diluted atropine for inhibition of myopia progression in Korean children. Int. J. Ophthalmol. 11, 1657–1662. doi:10.18240/ijo.2018.10.13
Morgan, I. G., French, A. N., Ashby, R. S., Guo, X., Ding, X., He, M., et al. (2018). The epidemics of myopia: aetiology and prevention. Prog. Retin Eye Res. 62, 134–149. doi:10.1016/j.preteyeres.2017.09.004
Pan, S.-Y., Wang, Y. Z., Li, J., Zhang, X. H., Wang, J., Zhu, X. P., et al. (2022). Short-term effect of 0.01% atropine sulphate eye gel on myopia progression in children. Int. J. Ophthalmol. 15, 1122–1127. doi:10.18240/ijo.2022.07.12
Qin, J., Lyu, Y., Wei, L., Zhang, J., Zhao, B., and Fu, A. (2021). Comparison of myopia progression between different concentrations and application frequencies of atropine eye drops in children. Chin. J. Exp. Ophthalmol. 39, 423–429.
Repka, M. X., Weise, K. K., Chandler, D. L., Wu, R., Melia, B. M., Manny, R. E., et al. (2023). Low-dose 0.01% atropine eye drops vs placebo for myopia control: a randomized clinical trial. JAMA Ophthalmol. 141, 756–765. doi:10.1001/jamaophthalmol.2023.2855
Resnikoff, S., Pascolini, D., Mariotti, S. P., and Pokharel, G. P. (2008). Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull. World Health Organ 86, 63–70. doi:10.2471/blt.07.041210
Rong, J. (2020). Clinical effect of 0.01% atropine eye drops on myopia progression in school-age children. Chin. J. Exp. Ophthalmol. 38, 494–498.
Sankaridurg, P., Berntsen, D. A., Bullimore, M. A., Cho, P., Flitcroft, I., Gawne, T. J., et al. (2023). IMI 2023 digest. Invest Ophthalmol. Vis. Sci. 64, 7. doi:10.1167/iovs.64.6.7
Sarkar, S., Khuu, S., and Kang, P. (2023). A systematic review and meta-analysis of the efficacy of different optical interventions on the control of myopia in children. Acta Ophthalmol. 102, e229–e244. doi:10.1111/aos.15746
Saw, S.-M., Matsumura, S., and Hoang, Q. V. (2019). Prevention and management of myopia and myopic pathology. Invest Ophthalmol. Vis. Sci. 60, 488–499. doi:10.1167/iovs.18-25221
Sen, S., Yadav, H., Jain, A., Verma, S., and Gupta, P. (2022). Effect of atropine 0.01% on progression of myopia. Indian J. Ophthalmol. 70, 3373–3376. doi:10.4103/ijo.IJO_256_22
Tapasztó, B., Flitcroft, D. I., Aclimandos, W. A., Jonas, J. B., De Faber, J. T. H. N., Nagy, Z. Z., et al. (2023). Myopia management algorithm. Annexe to the article titled Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol. 34, 952–966. doi:10.1177/11206721231219532
Wang, M., Cui, C., Yu, S. A., Liang, L. L., Ma, J. X., and Fu, A. C. (2023a). Effect of 0.02% and 0.01% atropine on ocular biometrics: a two-year clinical trial. Front. Pediatr. 11, 1095495. doi:10.3389/fped.2023.1095495
Wang, W., Zhang, F., Yu, S., Ma, N., Huang, C., Wang, M., et al. (2023b). Prevention of myopia shift and myopia onset using 0.01% atropine in premyopic children - a prospective, randomized, double-masked, and crossover trial. Eur. J. Pediatr. 182, 2597–2606. doi:10.1007/s00431-023-04921-5
Wang, X.-Y., Deng, H. W., Yang, J., Zhu, X. M., Xiang, F. L., Tu, J., et al. (2024). The optimal atropine concentration for myopia control in Chinese children: a systematic review and network Meta-analysis. Int. J. Ophthalmol. 17, 1128–1137. doi:10.18240/ijo.2024.06.19
Wang, Y. (2022). Short-term effects of atropine 0.01% on the structure and vasculature of the choroid and retina in myopic Chinese children. Ophthalmol. Ther. 11, 833–856.
Wang, Y., Yao, J., and Qu, X. (2020). Atropine 0.01% for the control of myopia in Chinese children: effect on accommodation functions and pupil size. J. Ophthalmol. 2020, 1–8. doi:10.1155/2020/7525180
Wu, P.-C., Chuang, M. N., Choi, J., Chen, H., Wu, G., Ohno-Matsui, K., et al. (2019). Update in myopia and treatment strategy of atropine use in myopia control. Eye 33, 3–13. doi:10.1038/s41433-018-0139-7
Wu, P.-C., Yang, Y.-H., and Fang, P.-C. (2011). The long-term results of using low-concentration atropine eye drops for controlling myopia progression in schoolchildren. J. Ocul. Pharmacol. Ther. 27, 461–466. doi:10.1089/jop.2011.0027
Xiao, J., Liu, M., Huang, Q., Sun, Z., Ning, L., Duan, J., et al. (2022). Analysis and modeling of myopia-related factors based on questionnaire survey. Comput. Biol. Med. 150, 106162. doi:10.1016/j.compbiomed.2022.106162
Yam, J. C., Jiang, Y., Tang, S. M., Law, A. K. P., Chan, J. J., Wong, E., et al. (2019). Low-concentration atropine for myopia progression (lamp) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology 126, 113–124. doi:10.1016/j.ophtha.2018.05.029
Yam, J. C., Li, F. F., Zhang, X., Tang, S. M., Yip, B. H. K., Kam, K. W., et al. (2020). Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: phase 2 report. Ophthalmology 127, 910–919. doi:10.1016/j.ophtha.2019.12.011
Yam, J. C., Zhang, X. J., Zhang, Y., Wang, Y. M., Tang, S. M., Li, F. F., et al. (2022). Three-year clinical trial of low-concentration atropine for myopia progression (LAMP) study: continued versus washout: phase 3 report. Ophthalmology 129, 308–321. doi:10.1016/j.ophtha.2021.10.002
Yam, J. C., Zhang, X. J., Zhang, Y., Yip, B. H. K., Tang, F., Wong, E. S., et al. (2023). Effect of low-concentration atropine eyedrops vs placebo on myopia incidence in children: the LAMP2 randomized clinical trial. JAMA 329, 472–481. doi:10.1001/jama.2022.24162
Ye, L., Xu, H., Shi, Y., Yin, Y., Yu, T., Peng, Y., et al. (2022). Efficacy and safety of consecutive use of 1% and 0.01% atropine for myopia control in Chinese children: the atropine for children and adolescent myopia progression study. Ophthalmol. Ther. 11, 2197–2210. doi:10.1007/s40123-022-00572-1
Yi, S., Huang, Y., Yu, S. Z., Chen, X. J., Yi, H., and Zeng, X. L. (2015). Therapeutic effect of atropine 1% in children with low myopia. J. AAPOS 19, 426–429. doi:10.1016/j.jaapos.2015.04.006
Ying, Z.-Q., Li, D.-L., Zheng, X.-Y., Zhang, X.-F., and Pan, C.-W. (2024). Risk factors for myopia among children and adolescents: an umbrella review of published meta-analyses and systematic reviews. Br. J. Ophthalmol. 108, 167–174. doi:10.1136/bjo-2022-322773
Yu, M., Hu, Y., Han, M., Song, J., Wu, Z., Xu, Z., et al. (2023). Global risk factor analysis of myopia onset in children: a systematic review and meta-analysis. PloS one 18, e0291470. doi:10.1371/journal.pone.0291470
Zhang, X. B., Jiang, H. H., Zhang, L. L., Li, C. J., Chen, C., Xing, M. Z., et al. (2024). Potential causal associations between leisure sedentary behaviors, physical activity, sleep traits, and myopia: a Mendelian randomization study. BMC Ophthalmol. 24, 104. doi:10.1186/s12886-024-03367-z
Zhang, X. J., Zhang, Y., Yip, B. H. K., Kam, K. W., Tang, F., Ling, X., et al. (2024). Five-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: phase 4 report. Ophthalmology S0161-6420 (24), 1011–1020. doi:10.1016/j.ophtha.2024.03.013
Zhao, Q., and Hao, Q. (2021). Clinical efficacy of 0.01% atropine in retarding the progression of myopia in children. Int. Ophthalmol. 41, 1011–1017. doi:10.1007/s10792-020-01658-0
Zhu, Q., Tang, G. Y., Hua, Z. J., Xue, L. P., Zhou, Y., Zhang, J. Y., et al. (2023c). 0.05% atropine on control of myopia progression in Chinese school children: a randomized 3-year clinical trial. Int. J. Ophthalmol. 16, 939–946. doi:10.18240/ijo.2023.06.17
Zhu, Q., Tang, Y., Guo, L., Tighe, S., Zhou, Y., Zhang, X., et al. (2020). Efficacy and safety of 1% atropine on retardation of moderate myopia progression in Chinese school children. Int. J. Med. Sci. 17, 176–181. doi:10.7150/ijms.39365
Zhu, S., Zhan, H., Yan, Z., Wu, M., Zheng, B., Xu, S., et al. (2023a). Prediction of spherical equivalent refraction and axial length in children based on machine learning. Indian J. Ophthalmol. 71, 2115–2131. doi:10.4103/IJO.IJO_2989_22
Zhu, X., Wang, Y., Liu, Y., Ye, C., Zhou, X., and Qu, X. (2023b). Effects of atropine 0.01% on refractive errors in children with myopia. Heliyon 9, e18743. doi:10.1016/j.heliyon.2023.e18743
Keywords: atropine, concentration, effectiveness, myopia, children, AISA
Citation: Wang X, Zhang L, Gan J, Wang Y and Yang W (2024) Effectiveness of various atropine concentrations in myopia control for Asian children: a network meta-analysis. Front. Pharmacol. 15:1503536. doi: 10.3389/fphar.2024.1503536
Received: 29 September 2024; Accepted: 02 December 2024;
Published: 16 December 2024.
Edited by:
Catherine M. T. Sherwin, University of Western Australia, AustraliaReviewed by:
Karel Allegaert, KU Leuven, BelgiumCopyright © 2024 Wang, Zhang, Gan, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weihua Yang, YmVuYmVuMDYwNkAxMzkuY29t; Yun Wang, c195d2FuZ0AxMjYuY29t; Jinhua Gan, MTYwMzcxNzMxMEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.