
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pharmacol. , 01 November 2024
Sec. Experimental Pharmacology and Drug Discovery
Volume 15 - 2024 | https://doi.org/10.3389/fphar.2024.1486458
Objective: Currently, traditional Chinese medicine (TCM) and its combinations are widely used in the treatment and rehabilitation of patients with ischemic stroke. However, current studies should mainly focus on the therapeutic effects of traditional Chinese medicines alone. This paper will employ a network meta-analysis to compare the efficacy of different TCM decoctions in the treatment of patients with ischemic stroke.
Methods: Chinese and English databases including PubMed, Embase, Cochrane Library, and Web of Science were searched to collect randomized controlled trials of TCM decoctions in the treatment of patients with ischemic stroke (IS), with a search time frame until April 2024. A library of references was created using EndNote 21. Quality assessment was performed using the Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2). A Bayesian network meta-analysis of data was performed using R4.3.1 and STATA 15.0.
Results: A network meta-analysis was conducted on 119 randomized controlled trials including 12,137 IS patients. The following TCM decoctions were involved: Xinglou Chengqi Decoction (XLCQT), Shenqi Tongluo Decoction (SQTLF), Zhongfeng Jiuxian Decoction (ZFJXT), Yiqi Tongluo Decoction (YQTLT), Tongqiao Huoxue Tang (TQHXT), Tongluo Xifeng Decoction (TLXFT), Tongluo Fuzheng Decoction (TLFZT), Xuefu Zhuyu Decoction (XFZYT), Xiaoxuming Decoction (XXMT), Qufeng Xingxue Tongluo Formula (QFXXTLF), Banxia Baizhu Tianma Decoction (BXBZTMT), Buyang Huanwu Tang (BYHWT),Huatan Tongluo Decoction (HTTLT), Yiqi Huoxue Tongluo Decoction (YQHXTLT), Yiqi Huoxue Decoction (YQHXT), and Yiqi Huoxue Kaiqiao Prescription (YQHXKQP). Of them, XFZYT was most effective in reducing the NIHSS score; SQTLF was most effective in increasing the Barthel Index (BI) score; and HTTLT was most effective in improving activities of daily living (ADL).
Conclusion: This network meta-analysis provided data on the relative efficacy of different TCM decoctions. Of them, XFZYT was most effective in reducing the NIHSS score; SQTLF was most effective in increasing the BI score; and HTTLT was most effective in improving the ADL score. At the same time, overall, XFZYT ranked first with its best efficacy regarding all the three outcome measures above, and SQTLF came second with its impact on two of the outcome measures.
Stroke is divided into ischemic strokes (IS) and hemorrhagic stroke (HS), of which IS the most common type of stroke. IS a clinical syndrome caused by insufficient cerebral blood and oxygen supply due to cerebrovascular lesions, which results in ischemic and hypoxic necrosis of local brain tissues, followed by neurological impairment. Main clinical symptoms include hemiplegia, aphasia, coma, and movement disorders, with high rates of morbidity, disability, recurrence, and fatality (Xie et al., 2022; García-Pérez et al., 2021). According to epidemiological surveys, stroke is the second leading cause of death and the leading cause of acquired long-term disability worldwide (Herpich and Rincon, 2020). About 15 million people are diagnosed with stroke each year globally (Iadecola et al., 2020), and about 80% of them are IS patients (Herpich and Rincon, 2020). A combination of genetic and environmental factors contribute to the occurrence of IS, with well-defined risk factors including coronary heart disease, hypertension, diabetes mellitus, and hyperhomocysteinemia. The aim of current clinical treatment is to restore blood flow in the ischemic penumbra, restore blood circulation, reduce the extent of core infarcts, and ultimately restore neurological function. The drugs and treatments in modern medicine have limited effects (Xu et al., 2023). IS in the hyperacute phase is mainly treated with pharmacological thrombolysis or vascular intervention,but the therapeutic time window for thrombolysis after IS onset is very short. The National Institute of Neurological Disorders and Stroke (NINDS) demonstrated that intravenous thrombolysis (IVT) with recombinant tissue plasminogen activator (rt-PA) was effective in patients with acute IS (AIS) up to 3 h after onset, and the Golden Hour’period was usually within only 3–4.5 h. If post-stroke patients miss the Golden Hour of IVT or fail to seek proper drug therapy (Rønning et al., 2019), followed by pharmacological intervention and rehabilitation, there will be a significantly high incidence of post-stroke sequelae, such as hemiplegia, cognitive impairment, dysphagia, speech disorders, and a variety of psychological and physiological problems.
Modern research has found that TCM has good efficacy in treating IS (Wei et al., 2024). TCM can reduce inflammatory response, oxidative stress, and apoptosis, improve energy metabolism, protect cerebral nerves, improve brain injury after IS, and reduce sequelae. In addition, a combination of TCM with modern medicine can achieve the effect of “1 + 1 > 2”. For example, exogenous stem cell transplantation combined with TCM can better repair damaged nerves and promote the reconstruction of the cerebral neural structure and the generation of different neuronal cell lineages required for functional regeneration after cerebral ischemic injury (Gao et al., 2020; Zhou et al., 2018). Currently there is controversy about TCM regimens in the treatment of IS. There is a lack of direct comparison among different TCM decoctions, and there are a wide variety of TCM regimens. Therefore, this network meta-analysis was conducted to compare the efficacy of different TCM decoctions in the treatment of IS patients. Hopefully, this meta-analysis will provide a rationale for the selection of traditional Chinese medicines for IS treatment.
This study was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009). The study protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO): https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=571089, with a number of CRD42024571089.
The databases, including Cochrane Library, PubMed, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), Wanfang Data, and VIP, were searched using a computer to collect randomized controlled trials (RCTs) of TCM decoctions in the treatment of IS patients, with a search time frame until April 2024. Search was conducted using the following subject headings and free-text words: a combination of ischemic stroke, Tang (decoction) + San (powder) + Fang (formula) + Ji (dosage form), randomized controlled, random grouping or randomized, and NIHSS + BI + ADL. The search strategy is detailed in Supplementary Material 1. To find more eligible studies, we looked for relevant references from the included papers. There were no restrictions on language, year of publication or type of publication.
Inclusion criteria: Participants: patients with a clinical diagnosis of IS or stroke; intervention: decoctions based on modified TCM formulas, at least once a day; comparison: Standards of Care (SOC) for IS or SOC developed by hospitals based on expert consensuses or clinical guidelines; outcomes: the NIHSS score as the primary outcome measure, and the BI score and ADL score as secondary outcome measures; study design: all the included studies were randomized controlled trials (RCTs). Exclusion criteria: Duplicates, animal studies, case reports, conference abstracts, reviews, unavailable full texts, studies including participants with other organic diseases as comorbidities.
EndNote 21 was used to create a library of the articles obtained. Literature screening was completed independently by two investigators. Firstly, duplicate articles were excluded. Then, articles were initially screened by regarding their titles and abstracts thoroughly according to the inclusion and exclusion criteria. Next, the articles passing the initial screening were rescreened by reading their full texts according to the inclusion and exclusion criteria. If the results were disputed at any stage, a third investigator was also involved in the discussion to reach a consensus. Information extracted from the included studies included first author, year of publication, sample size, gender, mean age, interventions, and outcome measures.
The latest recommendations in the Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) (Higgins et al., 2019) were used to assess the risk of bias, including the following five main domains: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, and bias in selection of the reported result. In addition, the studies were rated as “low risk”, “unclear risk “or “high risk “of bias. Two assessors independently conducted the quality assessment, and cross-checked the results. Any discrepancies were resolved through discussion or consultation with a third investigator. Then, a schematic diagram of the results of risk of bias assessment was drawn by ReviewManager 5.3.
Bayesian network meta-analysis of data was performed using R4.3.1 (R Foundation for Statistical Computing) and STATA 15.0 (Stata Corp., College Station, TX, United States) to compare different interventions. A Markov Chain Monte Carlo (MCMC) method (Jansen et al., 2008) was used to obtain the best pooled estimates and probabilities for various treatment regimens, thereby assessing the relative efficacy and rank order of different treatment regimens. Continuous outcomes were expressed as the posterior mean difference (MD) along with its corresponding 95% confidence interval (CI). The probability of being the best intervention corresponding to an outcome measure for IS was predicted by calculating the surface under the cumulative ranking curve (SUCRA) value.
Network and funnel plots were drawn using STATA 15.0 to visualize direct and indirect comparative relationships among different treatment regimens, and to detect publication bias and other small-study effects. A metan command was installed to adjust the corresponding TCM decoctions. In a plot, each circle corresponds to a drug, and the edges represent existing comparisons. The size of each circle is proportional to the study size (number of patients included). A cumulative probability plot was drawn using the ggplot2 package.
A preliminary search in the databases yielded 1,621 articles. After the removal of 587 duplicates, 50 studies, including reviews, systematic reviews, and animal experiments, were excluded by reading their titles and abstracts. 622 articles were excluded by reading their full texts. 243 articles containing less than three relevant references were removed. In the end, 119 articles were included in the analysis (Figure 1).
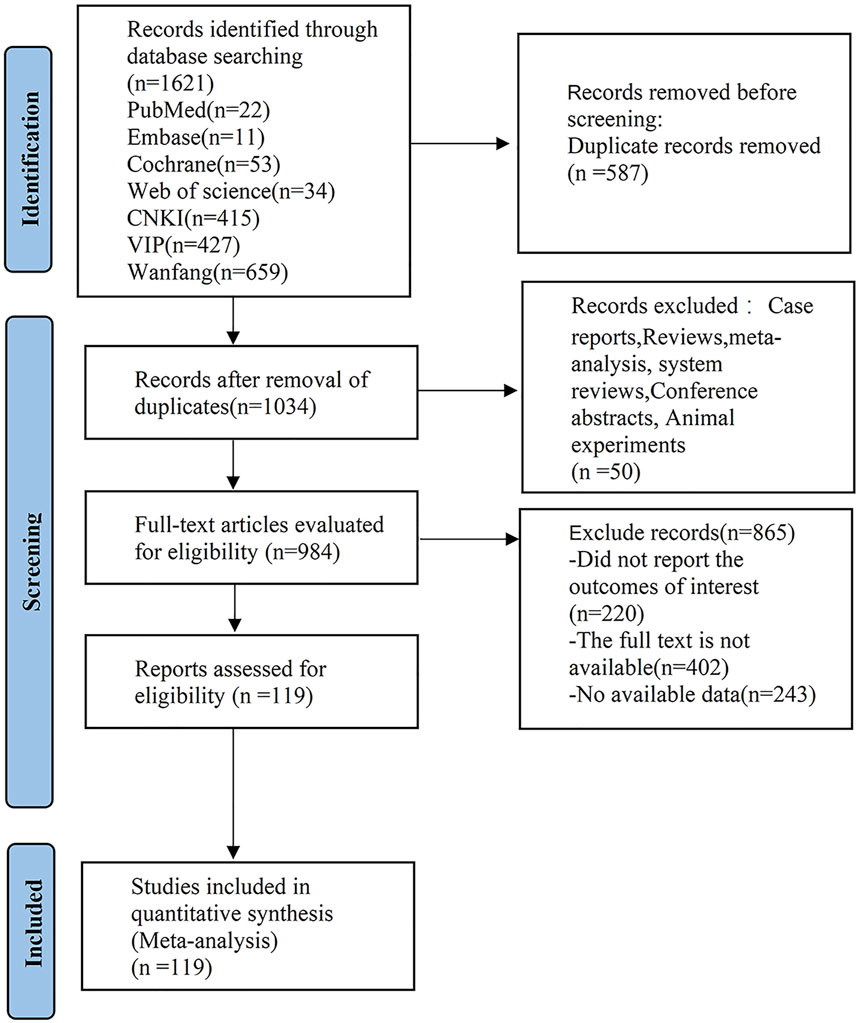
Figure 1. PRISlMA flow diagram of the study process. PRISMA, Preferred Reporting Items for Systematic review and Meta analysis.
The 119 articles included in the analysis involved 12,137 IS patients, and a total of 19 TCM decoctions including XLCQT, BXBZTMT, BYHWT, HTTLT, and XFZYT. The characteristics of the articles are detailed in Table 1. Of the included studies, some did not clearly state blinding methods, and two used non-randomized methods in the random sequence generation process and thus gave rise to a high risk of bias. Another high risk of bias arises mainly from incomplete data on outcome measures due to data loss. The risk of bias assessment of the included studies is shown in Table 2.
A total of 109 articles reported the NIHSS score, as shown in Table 1 and Supplementary Material 2. The network plot (Figures 2A) showed that a closed loop was not formed, and no interconnections were formed among different TCM decoctions. The included studies mostly investigated BYHWT, followed by XFZYT and HTTLT. As shown in Figures 2B, compared with SOC, BXBZTMT [MD = −4.6, 95% CI (−6.5, −2.6)], BYHWT [MD = −4., 95% CI (-5.0, −2.9)], HTTLT [MD = −3.4, 95% CI (−6.1, −0.65)], SQTLF [MD = −4.9, 95% CI (−8.7, −1.1)], TLFZT [MD = −4.3, 95% CI (−8.1, −0.56)], XFZYT [MD = −5.5, 95% CI (−7.2, −3.8)], XXMT [MD = −4.2, 95% CI (−7.5, −0.85)], YQHXTLT [MD = −3.8, 95% CI (−7.0, −0.48)], and ZFJXT [MD = −4.9, 95% CI (−8.7, −1.1)], were able to improve neurological deficits and reduce NIHSS scores in IS patients. SOC was mostly less effective than TCM decoctions. Of them, XFZYT was the most effective (−4.1 (−7.5, −0.7)). The results are shown in Supplementary Table S1 in Supplementary Material 3. The ranking of SUCRA values was as follows: XFZYT (84.3%) > ZFJXT (71.1%) > SQTLF (70.9%) > SOC(5%) (Figures 2C; Table 3).
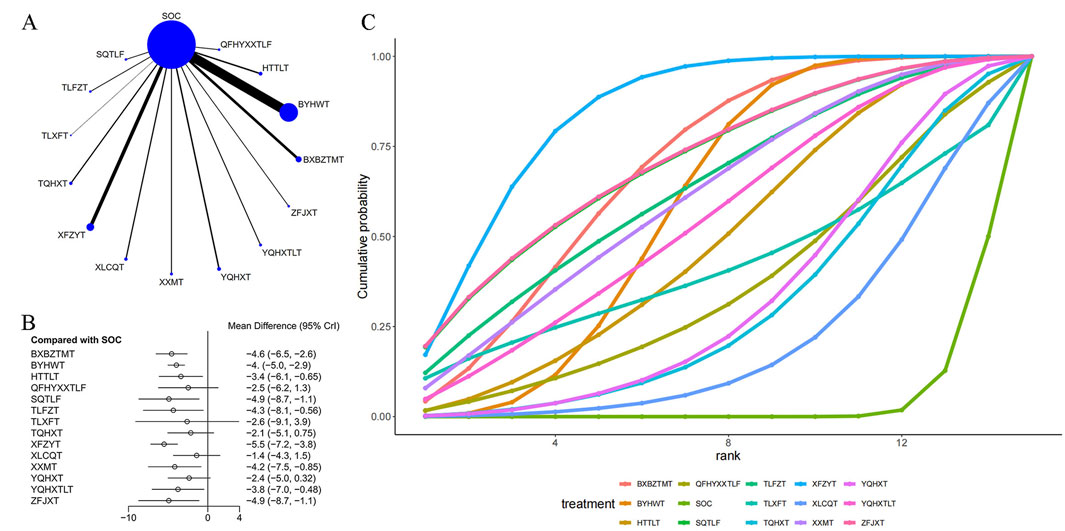
Figure 2. Effect of traditional Chinese medicine decoctions on NIHSS effect. (A) Network plot of comparisons for efficacy Nihss effects; (B) Forest plot of Nihss effect: Chinese medicine decoction vs. Standard of care; (C) Surface under the cumulative ranking curve plots for different Chinese medicine decoctions effects. The vertical axis represents cumulative probabilities and the horizontal axis represents rank. BXBZTMT, Banxia Baizhu Tianma decoction; BYHWT, Buyang Huanwu Tang or Buyang Huanwu decoction; HTTLT, Huatan Tongluo decoction; QFHYXXTLF, dispelling pathogenic wind and expelling blood stasis for promoting blood circulation and dredging collateral prescription or Qufeng Xingxue Tongluo Formula; SOC, Standard of care; SQTLF, Shenqi Tongluo decoction; TLFZT, Tongluo Fuzheng decoction; TLXFT, Tongluo Xifeng decoction; TQHXT, Tongqiao Huoxue Tang or Tongqiao Huoxue decoction; XFZYT, Xuefu Zhuyu decoction; XLCQT, Xinglou Chengqi decoction; XXMT, Xiaoxuming decoction; YQHXT, Yiqi Huoxue decoction; YQHXTLT, Yiqi Huoxue Tongluo decoction; ZFJXT, Zhongfeng Jiuxian decoction.
40 articles mentioned the BI score, as shown in Table 1. The network plot (Figures 3A) showed that no closed loop was formed, and no interconnections were formed among different TCM decoctions. The included studies mostly investigated BYHWT and HTTLT, and rarely investigated XXMT and SQTLF. As shown in Figures 3B, compared with SOC, BXBZTMT [MD = 17., 95% CI (9.1, 25.)], BYHWT [MD = 11., 95% CI (8., 15.)], HTTLT [MD = 12., 95% CI (7.8, 17.)], SQTLF [MD = 21., 95% CI (11., 30.)], TLFZT [MD = 9.8, 95% CI (2.8, 17.)], XFZYT [MD = 19., 95% CI (14., 24.)], YQHXT [MD = 10., 95% CI (5.1, 15.)], and YQHXTLT [MD = 19., 95% CI (14., 24.)] were able to enhance independence in patients. There was a significant difference between SOC and most TCM decoctions. Of TCM decoctions, SQTLF was most effective (−20.71 (−30.33, −11.13)). YQHXTLT and XFZYT were more effective than most other TCM decoctions, but their difference was not significant. The results are shown in Supplementary Table S2 in Supplementary Material 3. The ranking of SUCRA values was as follows: SQTLF (89.5%) > YQHXTLT (85.9%) > XFZYT (85.3%) > SOC (2.2%) (Figures 3C; Table 3).
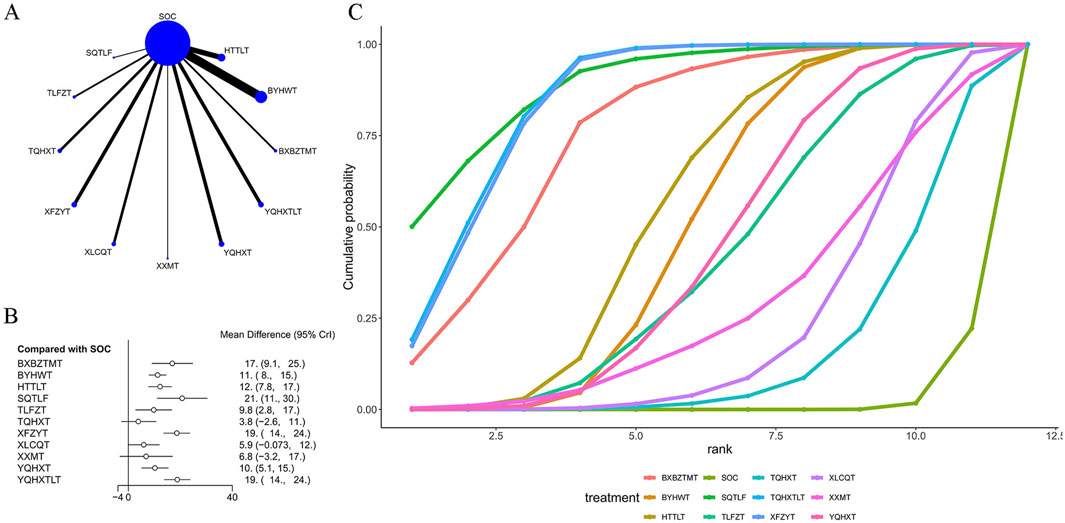
Figure 3. Effect of traditional Chinese medicine decoctions on BI effect. (A) Network plot of comparisons for efficacy BI effects; (B) Forest plot of BI effect: Chinese medicine decoction vs. Standard of care; (C) Surface under the cumulative ranking curve plots for different Chinese medicine decoctions effects. The vertical axis represents cumulative probabilities and the horizontal axis represents rank. BXBZTMT, Banxia Baizhu Tianma decoction; BYHWT, Buyang Huanwu Tang or Buyang Huanwu decoction; HTTLT, Huatan Tongluo decoction; SOC, Standard of care; SQTLF, Shenqi Tongluo decoction; TLFZT, Tongluo Fuzheng decoction; TQHXT, Tongqiao Huoxue Tang or Tongqiao Huoxue decoction; XFZYT, Xuefu Zhuyu decoction; XLCQT, Xinglou Chengqi decoction; XXMT, Xiaoxuming decoction; YQHXT, Yiqi Huoxue decoction; YQHXTLT, Yiqi Huoxue Tongluo decoction.
26 articles used the ADL score as an outcome measure, as shown in Table 1. The network plot (Figures 4A) showed that no closed loop was formed, and no interconnections were formed among different TCM decoctions. The included studies mostly investigated BYHWT, TLXFT, and BXBZTMT, and rarely investigated other TCM decoctions. As shown in Figures 4B, compared with SOC, BYHWT [MD = 10., 95% CI (5.7, 15.)], HTTLT [MD = 28., 95% CI (12., 43.)], TLXFT [MD = 15., 95% CI (5.3, 24.)], and XFZYT [MD = 17., 95% CI (5.1, 28.)] were able to regulate functional status in individual patients to enable them to better perform various activities independently in daily life. SOC was found to be less effective than TCM decoctions. Of them, BXBZTMT (−18.38 (−36.83, −0.15)), BYHWT (−17.22 (−33.58, −0.59)), and XXMT (19.51 (0.06, 38.86)) were significantly different from HTTLT, but none of them was as effective as HTTLT, and HTTLT (27.5 (11.72, 43.36)) itself was most effective in improving the outcome measure. The results are shown in Supplementary Table S3 in Supplementary Material 3. The ranking of SUCRA values was as follows: HTTLT (94.8%) > XFZYT (72.4%) > TLXFT (66.4%) > SOC (5.3%) (Figures 4C; Table 3).
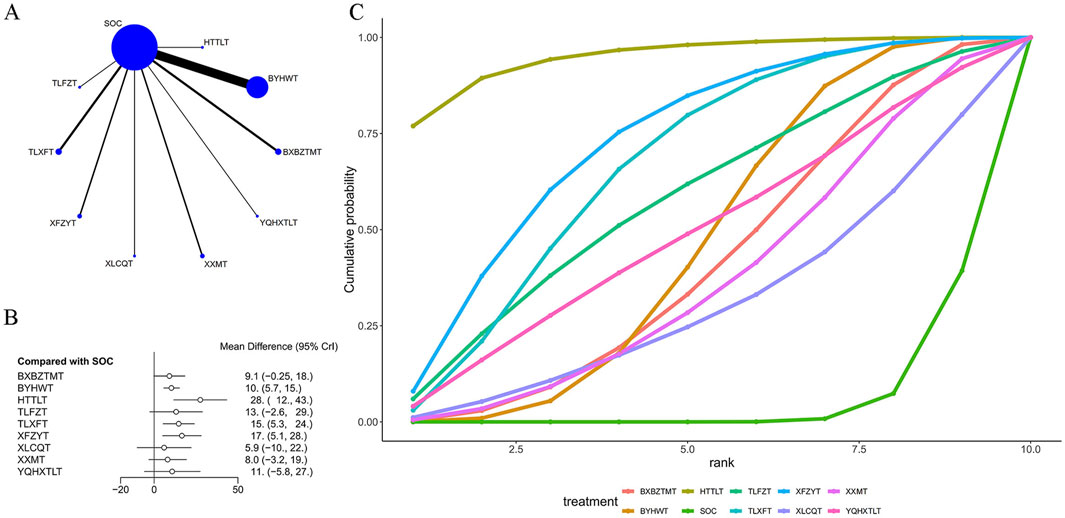
Figure 4. Effect of traditional Chinese medicine decoctions on ADL effect. (A) Network plot of comparisons for efficacy Nihss effects; (B) Forest plot of Nihss effect: Chinese medicine decoction vs. Standard of care; (C) Surface under the cumulative ranking curve plots for different Chinese medicine decoctions effects. The vertical axis represents cumulative probabilities and the horizontal axis represents rank. BXBZTMT, Banxia Baizhu Tianma decoction; BYHWT, Buyang Huanwu Tang or Buyang Huanwu decoction; HTTLT, Huatan Tongluo decoction; SOC, Standard of care; TLFZT, Tongluo Fuzheng decoction; TLXFT, Tongluo Xifeng decoction; XFZYT, Xuefu Zhuyu decoction; XLCQT, Xinglou Chengqi decoction; XXMT, Xiaoxuming decoction; YQHXTLT, Yiqi Huoxue Tongluo decoction.
Regarding the NIHSS score, SOC was significantly different from BXBZTMT, BYHWT, HTTLT, SQTLF, TLFZT, TQHXT, XFZYT, XLCQT, XXMT, YQHXT, YQHXTLT, and ZFJXT. Regarding the BI score, SOC was significantly different from BXBZTMT, BYHWT, HTTLT, SQTLF, TLFZT, XFZYT, YQHXT, and YQHXTLT. Regarding the ADL score, SOC was significantly different from BYHWT, HTTLT, TLXFT, and XFZYT. The results corresponding to the three outcome measures are shown in Supplementary Material 4.
Regarding the outcome measures, their publication bias was assessed using funnel plots. The results are shown in Supplementary Figures S1–S3 in Supplementary Material 3. TCM decoctions were distinguished by different colors. As shown in the funnel plot of the NIHSS score (Supplementary Figure S1), the left and right sides were not completely symmetrical, with most of the data concentrated in the upper part, indicating that there was some publication bias. The funnel plot of the BI score (Supplementary Figure S2) was basically symmetrical, indicating less publication bias. The funnel plot of ADL (Supplementary Figure S3) was not completely symmetrical, indicating that there was some publication bias.
An innovative aspect of this study is that we are the first to use a network meta-analysis to evaluate the efficacy of different TCM decoctions in IS patients.
This study found that regarding the therapeutic impact on the NIHSS score, XFZYT did the best, ZFJXT came second, while SQTLF came third and got close to ZFJXT. NIHSS score was used to systematically review the severity of neurological deficits in stroke patients. This study showed that XFZYT had a significant effect on all outcome measures, especially the NIHSS score. We therefore believed that overall, XFZYT had the best efficacy against IS. XFZYT originates from Yilin Gaicuo (Correction on Errors in Medical Works) written by Wang Qingren in Qing Dynasty. It is composed of 11 medicinal materials that promote blood circulation to remove blood stasis and relieve pain: Carthamus tinctorius, Semen persicae (peach kernels), Rehmannia glutinosa, Achyranthes root, Fructus aurantii, Bupleurum chinense, Paeonia veitchii, Platycodon grandiflorus, Glycyrrhizae Radix et Rhizoma (licorice), and Chuan Xiong (Chuanxiong rhizome) (Fu et al., 2020). XFZYT significantly improved the NIHSS score. This effect may be associated with its ingredients such as Amygdalin, Paeoniflorin, and Ligustrazine. These ingredients have been shown to have significant anti-inflammatory effects in relevant studies (Feng F. et al., 2024; Xu et al., 2024). In a study in a mouse model of IS (Yanfang Guo et al., 2020), it was found that luteolin in XFZYT inhibited not only microglia and astrocyte activation but also the HIF-1α/NLRP3 signaling pathway, thereby attenuating apoptosis of apoptosis of nerve cells, inflammation, and the degree of oxidative stress, so as to relieve cognitive impairmen (Zhang et al., 2022; Feng et al., 2021). On the other hand, found that kaempferol in the decoction not only modulated the classical pro-inflammatory NF-kB signaling pathway to promote the expression of anti-apoptotic proteins, inhibited neuronal death induced by cerebral ischemia and glial cell activation, reduced the activation and number of neutrophils in peripheral blood and brains of the rats, and significantly suppressed the levels of oxidative stress, inflammation, and apoptosis, which in turn alleviated IS . In addition, the components in the formula, such as Huang Qi and Dang Gui, enhance the body’s immunity and promote the repair of nerve cells. They help improve the recovery of neurological function after stroke by repairing neurological impairment and improving the NIHSS score (Wang et al., 2020).
XFZYT has also been shown to improve hemorheology and reduce blood viscosity, thereby promoting blood circulation and oxygen supply to the damaged brain tissues (Chen and Sui, 2020). Gao et al., (2024) showed that related serum biomarker levels were significantly reduced in patients after treatment with XFZYT, suggesting that it has a positive effect on inflammatory response and neural repair after stroke. Lee et al. (2011) also revealed that XFZYT might play a neuroprotective role by inhibiting HIF-1 and TNF-α to enhance the neuroprotective effect of rt-PA, and inhibit inflammation and apoptosis, thus improving neurological impairment. XFZYT has also shown efficacy in the treatment of hyperlipidemia to reduce the risk of IS by regulating blood lipids (Lee et al., 2021; Wenkai Yu et al., 2024; Xiangjun Zhong et al., 2018). Several studies have demonstrated that it exhibits significant efficacy in regulating cholesterol, improving inflammation and lipid metabolism, protecting vascular endothelial function and promoting neovascularization, as well as increasing patients’ BI score and ADL score to improve motor function and quality of life (Fu et al., 2024).
Regarding the therapeutic impact on the BI score, SQTLF did the best, YQHXTLT came second, and XFZYT came third. However, there were no significant difference among these TCM formulas, as shown in a league table. BI is often used to measure the ability to perform activities of daily living in patients with stroke or physical dysfunction, and is also often used for rehabilitation assessments, clinical research, and other scenarios (Shah et al., 1989). A higher BI score means that the patient is less dependent and is able to perform most of the activities of daily living.SQTLF replenishes qi, warms meridians to remove stagnation/stasis, promotes blood circulation, and unblocks collaterals. It is composed of Huang Qi (milkvetch root), Danshen (red sage), Pinellia Rhizome, Fructus aurantii, Poria cocos, Chuan Xiong, San Qi (Panax notoginseng), Dang Gui (Angelica sinensis), leeches, stir-fried Glycyrrhizae Radix et Rhizoma, Di Long (earthworm), and Radix Aucklandiae. In the past, SQTLF was frequently used to treat conditions mainly characterized by blood stasis (Jian et al., 2020). We believed that was why it performed best in improving the BI score. Huang Qi is the principal component (sovereign ingredient) in the formula. It replenishes qi and elevates yang to help strengthen healthy qi and improve qi flow and blood circulation. Danshen and Chuan Xiong boost blood flow to remove blood stasis, and unblock collaterals to remove stagnation. They are able to promote blood circulation and reduce blood viscosity, thereby improving microcirculation and cerebral blood flow supply. In addition, San Qi in the formula fights platelet aggregation to help prevent thrombosis and further promote the recovery of neurological function (Gao et al., 2014; Cong, 2021). A study by Zhang Yingfeng, et al. demonstrated that a lyophilisate of Danshen and Chuan Xiong significantly improved the cerebral lipidomic profile in a rat model of middle cerebral artery occlusion by regulating lipid metabolism to improve IS (Zhang et al., 2019). Fu Xueqin, et al. demonstrated that Danshen plus Chuanxiong was able to exert an anti-apoptotic effect through the PI3K/AKT signaling pathway to ameliorate cerebral ischemia/reperfusion injury in rats (Fu et al., 2022). These mechanisms of action were further evidenced by the findings of Wen Yijun, et al. Their research found that after treatment in the observational group, activated partial thromboplastin time (APTT), prothrombin time (PT), and clotting time (TT) were all prolonged, and the level of fibrinogen (FIB) was reduced (Wen, 2024). We therefore concluded that SQTLF promoted improved coagulation function through antiplatelet agglutination to regulate blood circulation and hemorheology and then promoted the recovery of neurological function, while protecting nerve cells through regulation of lipid metabolism and antiapoptotic function, thus significantly improving the BI score in post-stroke hemiplegic patients. SQTLF is able to improve patients’ ability to walk and take care of themselves in daily life.
It also had a significant effect in on the NIHSS score. Modern pharmacological research has demonstrated that this may be due to ingredients such as Ginsenoside 4 and Astragalus polysaccharide (Liu et al., 2023; Shi and Ma, 2024), which have a stronger affinity for the corresponding receptors to regulate the release of neurotransmitters and fight against oxidative stress, thus protecting nerve cells and promoting the recovery of nerve function. Therefore, we believed that SQTLF protected nerve cells and promoted the recovery of nerve function mainly by enhancing neurotransmitter release and fighting against oxidative stress. At the same time, it attenuated apoptosis, improved blood flow and inhibited inflammatory response to improve the NIHSS score in IS patients.
In this study, we investigated the impact of different TCM decoctions on the ADL score in IS patients. We found that HTTLT, XFZYT, and TLXFT all showed positive efficacy in improving the ADL score. HTTLT exhibited the best effect on this outcome measure. It is mainly composed of Danshen, Rhizoma Gastrodiae, Pinellia Rhizome, Poria cocos, unprepared Atractylodes rhizome, Xiang Fu (Rhizoma Cyperi), Rhei Radix et Rhizoma prepared with alcohol, Arisaema cum Bile (Dan Nanxing in Chinese, DNX), Bambusae Concretio Silicea, and San Qi. HTTLT plays a main role in breaking up phlegm, activating meridians, and boosting blood flow to remove blood stasis. HTTLT increased the BI score possibly due to its function to improve the internal environment so as to reduce pathological factors, thereby improving nerve function and motor function (Zhao et al., 2022). Tang San, et al. (Tang et al., 2023) found that HTTLT significantly reduced the NIHSS score after cerebral ischemia/reperfusion, increased the expression of brain-derived neurotrophic factor (BDNF), and reduced the levels of neuron-specific enolase (NSE), high-sensitivity C-reactive protein (hs-CRP), and homocysteine (Hcy) levels in rats. In addition, Luo Fanghe, et al. found that HTTLT significantly improve the limb motor function of post-stroke hemiplegic patients who was recovering (Luo, 2024).
Pharmacological studies have demonstrated that Danshen in the formula is able to reduce the incidence of brain infarction and attenuate nerve injury caused by ischemia/reperfusion (Chen et al., 2024). Di Long is often used to treat joint inflammation. In this prescription, Di Long was shown to ameliorate inflammation by inhibiting the activation of the NF-κB signaling pathway and modulating the Th1/Th2 balance (Bao et al., 2022). Atractylodes rhizome has immunomodulatory and anti-inflammatory effects (Feng J. M. et al., 2024). We believed that Atractylodes rhizome as an important ingredient of HTTLT might reduce inflammatory response in brain tissue to protect neurons. HTTLT improved limb motor function to increase the ADL score through its role in reducing neurological impairment, modulating immune response and reducing inflammation. Its value for long-term rehabilitation can be further explored in future studies.
This study explored the differences in efficacy among different TCM decoctions, but found no significant differences between these top-ranked interventions in the league table, possibly due to the impact of dose selection and frequency of oral medication. Our conclusion needs to be justified by more studies to provide IS patients with a choice of treatment. However, our study has some limitations. Firstly, there is a wide range of traditional Chinese medicines. This study reviewed the data on TCM decoctions only, and did not include many other types of traditional Chinese medicines, such as “creams”, “pills”, “granules”, and “Chinese patent medicines”. Secondly, the included studies were different in quality. Some of them did not clearly state methods for random assignment, contained small sample sizes, and failed to implement blinding strictly, thus possibly affecting the reliability of the results. Thirdly, there was large heterogeneity among the included studies regarding the treatment modality for patient populations. Fourthly, the inability to establish criteria involving dosage and strength in a unified manner for interventions may limit direct and indirect comparisons of outcomes. Fifthly, regarding the selection of outcome measures, cognitive indicators such as MOCCA and MSSE may be added in the future for comprehensive evaluation. Finally, we cannot completely rule out the effect of unmeasured confounders.
Based on this study, we concluded that TCM decoctions were able to improve outcome measures in the patients. Of them, XFZYT was most effective in reducing the NIHSS score, SQTLF was most effective in increasing the BI score, and HTTLT was most effective in improving the ADL score. At the same time, overall assessment showed that XFZYT ranked first with its best efficacy regarding all the three outcome measures above, and SQTLF came second with its impact on two of the outcome measures.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
BN: Conceptualization, Formal Analysis, Investigation, Methodology, Resources, Writing–original draft, Writing–review and editing. XZ: Conceptualization, Formal Analysis, Investigation, Methodology, Writing–original draft. XW: Methodology, Writing–original draft. WZ: Writing–original draft. RW: Writing–original draft. CQ: Formal Analysis, Investigation, Writing–original draft. ML: Resources, Supervision, Writing–review and editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1486458/full#supplementary-material
Bao, Y., Peng, J., Yang, K.-L., Wang, C.-H., Guo, Y.-F., Guo, Z.-S., et al. (2022). Therapeutic effects of Chinese medicine Di-Long (Pheretima vulgaris) on rheumatoid arthritis through inhibiting NF-κB activation and regulating Th1/Th2 balance. Biomed. and Pharmacother. 147, 112643. doi:10.1016/j.biopha.2022.112643
Chen, G., Jin, Z., Wang, X., Yu, Q.-H., and Hu, G.-B. (2024). Danshen injection mitigated the cerebral ischemia/reperfusion injury by suppressing neuroinflammation via the HIF-1α/CXCR4/NF-κB signaling pathway. NeuroReport 35, 601–611. doi:10.1097/WNR.0000000000002043
Chen, Y., and Sui, D. (2020). Progress in the study of the mechanism of action of Hematopoeia and Blood Stasis Tang in different systemic diseases. Jilin Chin. Med. doi:10.13463/j.cnki.jlzyy.2020.05.036
Cong, X. (2021). Efficacy of Senqi Tongluo Tang in the treatment of hemiplegia in recovering ischemic stroke. J. Pract. Chin. Med. doi:10.13729/j.issn.1671-7813.Z20201226
Feng, F., Xu, D.-Q., Yue, S.-J., Chen, Y.-Y., and Tang, Y.-P. (2024a). Neuroprotection by tetramethylpyrazine and its synthesized analogues for central nervous system diseases: a review. Mol. Biol. Rep. 51, 159. doi:10.1007/s11033-023-09068-y
Feng, J. M., Zhan, Z., Gu, F., Li, L., and Zhang, T. (2024b). Bibliometric analysis of research progress and development trend of Rhizoma Atractylodis Macrocephalae. China: Chinese Traditional and Herbal Drugs.
Feng, Z., Wang, C., Jin, Y., Meng, Q., Wu, J., and Sun, H. (2021). Kaempferol-induced GPER upregulation attenuates atherosclerosis via the PI3K/AKT/Nrf2 pathway. Pharm. Biol. 59, 1104–1114. doi:10.1080/13880209.2021.1961823
Fu, C., Liu, Y., Zeng, L., and Peng, L. (2024). Progress of chemical composition, pharmacological effect and clinical application of blood palace chasing blood stasis soup. Asia-Pacific Tradit. Med.
Fu, C.-Y., Wang, H.-Y., Liu, Y.-H., and Wang, Y., Simultaneous determination of eight components in Xuefu Zhuyu Decoction based on UPLC-ESI-IT-TOF-MS method. (2020).
Fu, X., Lan, R., Zou, X., Wang, W., and Wang, M. M. (2022). Network pharmacology-based study on the mechanism of anti-ischemia/reperfusion injury of Salvia miltiorrhiza and Rhizoma Ligustici Chuanxiong and its experimental validation. China Animal Husb. Veterinary Med. 49, 3643–3654. doi:10.16431/j.cnki.1671-7236.2022.09.038
Gao, H., Huo, Y., Wang, W., Yue, S., Cao, S., Chen, X., et al. (2024). Effectiveness of hemiparesis in ischemic stroke treated with the aid of blood-fu and blood-stasis-expelling soup. Liaoning J. Chin. Med.
Gao, J., Bai, P., Li, Y., Li, J., Jia, C., Wang, T., et al. (2020). Metabolomic profiling of the synergistic effects of ginsenoside Rg1 in combination with neural stem cell transplantation in ischemic stroke rats. J. proteome Res. 19, 2676–2688. doi:10.1021/acs.jproteome.9b00639
Gao, L., Yang, F., Li, F., Jiao, J., Chen, L., Zuo, J., et al. (2014). Study on the cerebral protective mechanism of self-proposed Astragalus Ginseng and Tongluo Tang on ischemic stroke patients. Chin. Med. Emerg. 23, 1602–1604.
García-Pérez, D., Parra-Serrano, J., Panero, I., Moreno, L. M., Campollo, J., and Alén, J. F. (2021). Transient cortical blindness secondary to contrast-induced encephalopathy following diagnostic cerebral angiography: report of 2 cases. Acta Neurol. Belg. 121, 585–589. doi:10.1007/s13760-020-01532-x
Herpich, F., and Rincon, F. (2020). Management of acute ischemic stroke. Crit. care Med. 48, 1654–1663. doi:10.1097/CCM.0000000000004597
Higgins, J. P., Savović, J., Page, M. J., and Sterne, J. A. (2019). Revised Cochrane risk-of-bias tool for randomized trials (RoB 2). Cochrane Handb. Syst. Rev. interventions.
Iadecola, C., Buckwalter, M. S., and Anrather, J. (2020). Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J. Clin. investigation 130, 2777–2788. doi:10.1172/JCI135530
Jansen, J. P., Crawford, B., Bergman, G., and Stam, W. (2008). Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health 11, 956–964. doi:10.1111/j.1524-4733.2008.00347.x
Jian, S., Zhang, J., and Zhan, K. (2020). Clinical study on the treatment of hemiplegia in recovering ischemic stroke with Senqi Tongluo Tang. J. Cardiovasc. Cerebrovasc. Dis. Central West. Med.
Lee, J. J. L. J., Hsu WenHsien, H. W., Yen TingLin, Y. T., Chang NenChung, C. N., Luo YueJyun, L. Y., Hsiao, G., et al. (2011). Traditional Chinese medicine, Xue-Fu-Zhu-Yu decoction, potentiates tissue plasminogen activator against thromboembolic stroke in rats. J. Ethnopharmacol. 134, 824–830. doi:10.1016/j.jep.2011.01.033
Lee, J. J. L. J., Hsu WenHsien, H. W., Yen TingLin, Y. T., Chang NenChung, C. N., Luo YueJyun, L. Y., Hsiao, G., et al. (2021). Traditional Chinese medicine, Xue-Fu-Zhu-Yu decoction, potentiates tissue plasminogen activator against thromboembolic stroke in rats. J Ethnopharmacol 134, 824–30. doi:10.1016/j.jep.2011.01.033
Liu, S., Chen, W., Zhao, Y., Zong, Y., Li, J., and He, Z. (2023). Research Progress on effects of Ginsenoside Rg2 and Rh1 on nervous system and related mechanisms. Molecules 28, 7935. doi:10.3390/molecules28237935
Luo, F. (2024). Clinical study on the treatment of patients with ischemic stroke in the recovery period by combining phlegm-reducing and channelizing tonic soup with fu zheng and earth tonic acupuncture therapy. J. Chronic Dis. doi:10.16440/J.CNKI.1674-8166.2024.07.20
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and Group, T. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097. doi:10.1371/journal.pmed.1000097
Rønning, O. M., Logallo, N., Thommessen, B., Tobro, H., Novotny, V., Kvistad, C. E., et al. (2019). Tenecteplase versus alteplase between 3 and 4.5 hours in low national institutes of health stroke scale. Stroke 50, 498–500. doi:10.1161/STROKEAHA.118.024223
Shah, S., Vanclay, F., and Cooper, B. (1989). Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 42, 703–709. doi:10.1016/0895-4356(89)90065-6
Shi, Y., and Ma, P. (2024). Pharmacological effects of Astragalus polysaccharides in treating neurodegenerative diseases. Front. Pharmacol. 15, 1449101. doi:10.3389/fphar.2024.1449101
Tang, S., Yang, X., Zhu, Q., Ding, H., Liu, X., Huang, M., et al. (2023). Protective effect of phlegm-cleansing and channelizing soup on “gut-brain” axis injury after cerebral ischemia/reperfusion in rats. Propr. Chin. Med.
Wang, K., Lei, L., Cao, J., Duan, J., Wen, A., Qiao, Y., et al. (2020). Research progress on the protective effect of Chinese medicinal herbs saffron and astragalus on cerebral ischemic injury. China Med. Her. 17, 22–25.
Wei, L., Chen, S., Deng, X., Liu, Y., Wang, H., Gao, X., et al. (2024). Metabolomic discoveries for early diagnosis and traditional Chinese medicine efficacy in ischemic stroke. Biomark. Res. 12, 63. doi:10.1186/s40364-024-00608-7
Wen, Y. (2024). Effect of Senqi Tongluo Tang on neurological deficits and serological indices in hemiplegic patients after stroke. China Metallurgical Industry Med. J. doi:10.13586/j.cnki.yjyx1984.2024.01.095
Wenkai Yu, K. W., Cao, K., Ni, J., and Chang, J. (2024). Clinical observation on the treatment of hyperlipidemia with phlegm-dampness internal obstruction evidence by combining Blood Palace and Blood Stasis Tang with atorvastatin calcium. West. Tradit. Chin. Med.
Xiangjun Zhong, J. H., Gong, L., and Zhu, J. (2018). Rational application of Chinese patent medicines for hyperlipidemia. People's Military Surgeon.
Xie, H., Gao, M., Lin, Y., Yi, Y., and Liu, Y. (2022). An emergency nursing and monitoring procedure on cognitive impairment and neurological function recovery in patients with acute cerebral infarction. NeuroRehabilitation 51, 161–170. doi:10.3233/NRE-210310
Xu, G., Liu, G., Wang, Z., Li, Y., and Fang, W. (2023). Circular RNAs: promising treatment targets and biomarkers of ischemic stroke. Int. J. Mol. Sci. 25, 178. doi:10.3390/ijms25010178
Xu, S.-y., Cao, H.-y., Yang, R.-h., Xu, R.-x., Zhu, X.-y., Ma, W., et al. (2024). Genus Paeonia monoterpene glycosides: a systematic review on their pharmacological activities and molecular mechanisms. Phytomedicine 127, 155483. doi:10.1016/j.phymed.2024.155483
Yanfang Guo, X. D., Wang, Y., Dong, X., Xu, B., and Cheng, Y. (2020). Effects of lignocaine inhibition of HIF-1α/NLRP3 signaling pathway on cognitive impairment and neuronal apoptosis in stroke rats. Trop. Med. J.
Zhang, S.-S., Liu, M., Liu, D.-N., Shang, Y.-F., Du, G.-H., and Wang, Y.-H. (2022). Network pharmacology analysis and experimental validation of kaempferol in the treatment of ischemic stroke by inhibiting apoptosis and regulating neuroinflammation involving neutrophils. Int. J. Mol. Sci. 23, 12694. doi:10.3390/ijms232012694
Zhang, Y., Wei, Y., Huang, X., and Zhu, L. (2019). UPLC-Q-TOF-MS based brain lipidomics study of Dan Shen Chuan Xiong intervention in ischemic stroke. Chin. J. Traditional Chin. Med. doi:10.19540/j.cnki.cjcmm.20190321.404
Zhao, J., Liu, J., Wu, D., Luo, C., and Pang, R. (2022). Study on the efficacy of hemiplegia treatment after stroke by combining phlegm-intoxicating soup and rehabilitation training. Shaanxi Tradit. Chin. Med.
Zhou, C.-l., Zhao, L., Shi, H.-y., Liu, J.-w., Shi, J.-w., Kan, B.-h., et al. (2018). Combined acupuncture and HuangDiSan treatment affects behavior and synaptophysin levels in the hippocampus of senescence-accelerated mouse prone 8 after neural stem cell transplantation. Neural Regen. Res. 13, 541–548. doi:10.4103/1673-5374.228760
Keywords: traditional Chinese medicine, network meta-analysis, ischemic stroke, Xuefu Zhuyu decoction, Huatan Tongluo Decoction
Citation: Ning B, Zhu X, Wu X, Zhu W, Wang R, Qi C and Li M (2024) Efficacy of different traditional Chinese medicine decoctions in the treatment of ischemic stroke: a network meta-analysis. Front. Pharmacol. 15:1486458. doi: 10.3389/fphar.2024.1486458
Received: 26 August 2024; Accepted: 22 October 2024;
Published: 01 November 2024.
Edited by:
Germain Sotoing Taiwe, University of Buea, CameroonReviewed by:
Yuanqi Zhao, Guangzhou University of Chinese Medicine, ChinaCopyright © 2024 Ning, Zhu, Wu, Zhu, Wang, Qi and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingquan Li, bGltaW5ncXVhbjAwMDFAMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.