
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 30 July 2024
Sec. Drugs Outcomes Research and Policies
Volume 15 - 2024 | https://doi.org/10.3389/fphar.2024.1422703
This article is part of the Research Topic Clinical Pharmacist Service Promotes the Improvement of Medical Quality Volume II View all 51 articles
 Samuel Berihun Dagnew1*
Samuel Berihun Dagnew1* Samuel Agegnew Wondm2
Samuel Agegnew Wondm2 Fisseha Nigussie Dagnew1
Fisseha Nigussie Dagnew1 Yohannes Shumet Yimer3
Yohannes Shumet Yimer3 Yehualashet Teshome Wondmkun4
Yehualashet Teshome Wondmkun4 Tilaye Arega Moges1
Tilaye Arega Moges1Background: Non-adherence to medication in patients with cardiovascular disease continues to be a main cause of suboptimal management, increased morbidity and mortality, and increased healthcare expenses. The present study assessed the level of medication adherence and its determinants of cardiovascular disease patients.
Methods: An institutional-based multicenter cross-sectional study was conducted with patients with cardiovascular disease in Northwest Ethiopian teaching hospitals. The level of medication adherence was evaluated using a standardized questionnaire of the Adherence in Chronic Disease Scale (ACDS). To find determinants of the level of medication adherence, an ordinal logistic regression model was employed. Statistics were significant when P ≤ 0.05 at a 95% confidence interval (CI).
Results: In the end, 336 participants were included in the research. According to this study, one-third of patients had low medication adherence, half had medium adherence, and one-fifth had high medication adherence. Elderly patients [adjusted odds ratio (AOR) = 2.691; 95% confidence interval (CI), 1.704–4.251; P < 0.000], marital status (AOR = 1.921; 95% CI, 1.214–3.039; P = 0.005), alcoholic patients (AOR = 2.782; 95% CI, 1.745–4.435; P < 0.000), Patients without physical activity (AOR = 1.987; 95% CI 1.251–3.156; P = 0.004), non health insurances (AOR = 1.593; 95% CI 1.003–2.529; P = 0.049), sever Charles comorbidity index (AOR = 2.486; 95% CI 1.103–5.604; P = 0.028), patients with polypharmacy (AOR = 2.998 (1.817–4.947) P < 0.000) and, manypolypharmacy (AOR = 3.031 (1.331–6.898) P = 0.008) were more likely to have low medication adherence.
Conclusion: The current study concluded that one-third of study participants had low medication adherence. Older age, marital status, drinker, physical inactivity, drug source, comorbidity, and polypharmacy all contributed to the low level of medication adherence. To improve patients with cardiovascular disease’s adherence to their medications, intervention is necessary.
Patients with multiple morbidities and chronic non-communicable diseases have increased consistently globally in particular, Cardiovascular disease (Bennett et al., 2018; Burnier, 2023). Cardiovascular diseases (CVDs) are the primary cause of death. Over 75% of CVD-related deaths occur in nations with lower and moderate incomes (Korkmaz and CARDIOVASCULAR DISEASES AND PREVENTION, 2021; Rehman et al., 2021). One of the main factors influencing good treatment outcomes is patient medication nonadherence. The majority of cardiovascular patients have been found they couldn’t recall their medications (Kravitz et al., 1993). Nonadhernace with prescribed treatment is a severe issue that impacts the patient as well as the healthcare system (Jimmy and Jose, 2011; McKenzie et al., 2015). Medication adherence refers to how often a person follows health practitioners’ recommendations whether it comes to drug use or altering their lifestyle (Sabaté, 2003). Numerous chronic drugs are frequently administered to people with cardiovascular disease. Furthermore, regimens have become increasingly complex (Shalansky and Levy, 2002). Medication complexity, which includes the number of prescription drugs supplied, their dosage forms, frequency of dosing, and instruction for using is the major factor for non-adherence.
Nonadherence to medication is a worldwide issue that jeopardizes people’s health and economic results for society (Stewart et al., 2023). Thus, patients are linked to worse treatment results, illness progression, and estimated billions of dollars worth of preventable direct medical expenses annually (DiMatteo, 2004a; DiMatteo, 2004b; Fuchs, 2022). Numerous studies have shown that poorer drug adherence worsened health consequences that extend beyond insufficient treatment of clinical parameters (Sokol et al., 2005; Perreault et al., 2012; Kim et al., 2018). Nevertheless, a lack of adherence has a detrimental impact on many other areas of managing diseases, such as disease exacerbations that occasionally result in acute hospitalizations, higher health costs, and, of course, a decline in the quality of life for patients (Kim et al., 2018; Peacock et al., 2021). An increased average length of hospital stay, functional impairments, poor quality of life, frequent hospital and pharmacy visits, and the occurrence of some more recent health problems or diseases can all be caused by inadequate adherence to the medication (K et al., 2023).
Analyzing the factors that influence adherence could result in improved treatment and results. Because adherence is a multi-factor phenomenon that depends on several factors rather than just one, factors impacting treatment adherence are frequently complex (Kolandaivelu et al., 2014). However, marital status, monthly income, level of education, drug regimen, and co-morbidities are the elements that influence the development of medication non-adherence. It becomes more expensive for the government and people to provide adequate healthcare in a developing nation (Saeed et al., 2023).
Understanding what obstacles patients face to taking their medications as prescribed is essential to improving medication adherence. Developing successful adherence-enhancing therapies requires a deeper knowledge of the factors that lead to poor drug adherence (Van der Laan et al., 2019; Nakajima et al., 2021). This study assessed the level of medication adherence and its determinants of cardiovascular disease patients attending Amhara Regional Teaching Hospitals.
The research was carried out in the Amhara region of Ethiopia from July 1 to 30 September 2023, at three teaching hospitals: Tibebe Ghion, University of Gondar, and Debre Birhan (Hakim Gizaw). The northern and northwest regions of Ethiopia are home to the Amhara region. There are 181 woredas, or districts, 78 urban centers, and 10 administrative zones. The University of Gondar, Tibebe Ghion, and Debre Birhan (Hakim Gizaw) are the three teaching hospitals in the region. More than 15 million patients have received care annually from the studied hospitals.
A multicenter cross-sectional study was conducted in teaching hospitals in the Amahara region to assess the level of adherence among patients with cardiovascular disease and the factors associated with non-adherence between July 1 and 30 September 2023, gregorian calendar.
Patients who visited the University of Gonder, Debre Birhan (Hakim Gizaw) hospitals, and Tibebe Gion Teaching Hospital for medication follow-ups at chronic disease clinics encompassed the source population. The study population comprises all cardiovascular patients who attended treatment during the data collection period. Using a single population proportion formula
All patients who were 18 years of age or older, who visited the chronic disease clinic for follow-up, whose charts plainly showed a diagnosis of cardiovascular diseases, and who were receiving treatment during follow-up were included in the study. Patients from the settings’ data over the preceding 3 months follow-up were eligible for this study. Cardiovascular diseases are collectively referred to as heart and blood vessel illnesses which include coronary heart disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, and pulmonary embolism disorders (Nangia et al., 2016). Conversely, patients who did not voluntarily communicate were excluded from the research.
A structured questionnaire was used as a data-gathering tool using journals that were previewed (Nangia et al., 2016; Kubica et al., 2017; Van der Laan et al., 2019; Peacock et al., 2021; Fuchs, 2022). The data collection instrument was created in English after a review of other related studies on related subjects, with minor adjustments made on account of the local clinical surroundings. The sociodemographic information about the participants, including gender, age, place of residence, religion, ethnicity, income, marital status, level of education, BMI, residency, educational status, employment status, physical activity, and health insurance status were included.
Following instructions regarding the study’s objectives, data collection tools and producers, and ethical considerations, three hospital-based pharmacists gathered the data. The participants in the data collection were willing. Primary data came from in-person patient interviews, and medical records from the patients were used to document laboratory results, medical conditions, and prescription dosages.
Based on several relevant investigations, a systematic questionnaire was created. Monitoring and verifying that all surveys were completed ensured the quality of the data. Three professionals reviewed the questionnaire’s face validity to ensure that the questions were clear. After that, 10% of research participants not included in the final analysis had the survey pretested for content, design, readability, and comprehension. Next, a suitable modification was implemented. Following a 2-day training session, three pharmacists collected the data. The study’s goal as well as the methods and instruments used for gathering data were made very clear by the supervisor. Using the WHO’s recommendations, socio-cultural adaptation was carried out, and adjustments were made in response to feedback. As a result, the survey yielded accurate results and was simple to comprehend and complete.
The Adherence for Chronic Disease (ACDs) which was validated by Kubica, A., et al., in 2017 was used for assessing adherence. This scale consists of seven items, each of which has five possible alternatives. The questions address both the situations and viewpoints that may have an indirect impact on adherence (Questions 6 and 7) as well as the behaviors that directly determine adherence (Questions 1–5). Every question has five possible answers, A through E. A stands for four, B for three, C for two, D for one, and E for zero points. The results fall between 0 and 28 points: a total score of less than 21 indicates low adherence, a total score of 21–26 indicates medium adherence and a total score of more than 26 indicates high adherence (Kubica et al., 2017).
Every piece of information gathered was personally examined for consistency and completeness of response. Data were cleaned, coded, and then imported into EpiData version 4.6 before being exported to STATA for additional analysis. To investigate the data’s normal distribution, Shapiro-Wilk tests, Q-Q plots, and histograms were employed. Using descriptive statistics, means (±SD), proportions, tables, and figures, the characteristics of the study participants were outlined, and the study findings were presented. The relationship between the level of medication adherence and other predictor variables was examined using an ordinal logistic regression model. The statistical techniques of taste of parallel line and the proportional odds assumption were applied to all variables and those that met the assumptions of ordinal logistic regression. To discover predictor variables with the level of medication adherence, variables with p < 0.25 in the bivariate analysis were taken into consideration for additional analyses in the multivariable analysis. The significance level was p ≤ 0.05 at 95% CI.
The Debre Tabor University Ethical Review Committee gave its ethical approval to the proposal with a reference number of CHS/265/2023. The research subjects were required to give their informed consent after being fully informed about the goals of the investigation. Written informed consent was acquired from every person in the study who was included. The study followed Helsinki legislation in terms of doing it in a properly anonymous and confidential manner.
The research had 336 study participants in total. The participants’ average age (±SD) was 63.06 ± 13.45 years, with 57.34% of them being females. A BMI of less than 25 was found in 79.76% of the patients. About half of patients (53.27%) get their medication for free. Of the subjects, one-fifth (20.24%) acquired adverse drug reactions (Table 1).
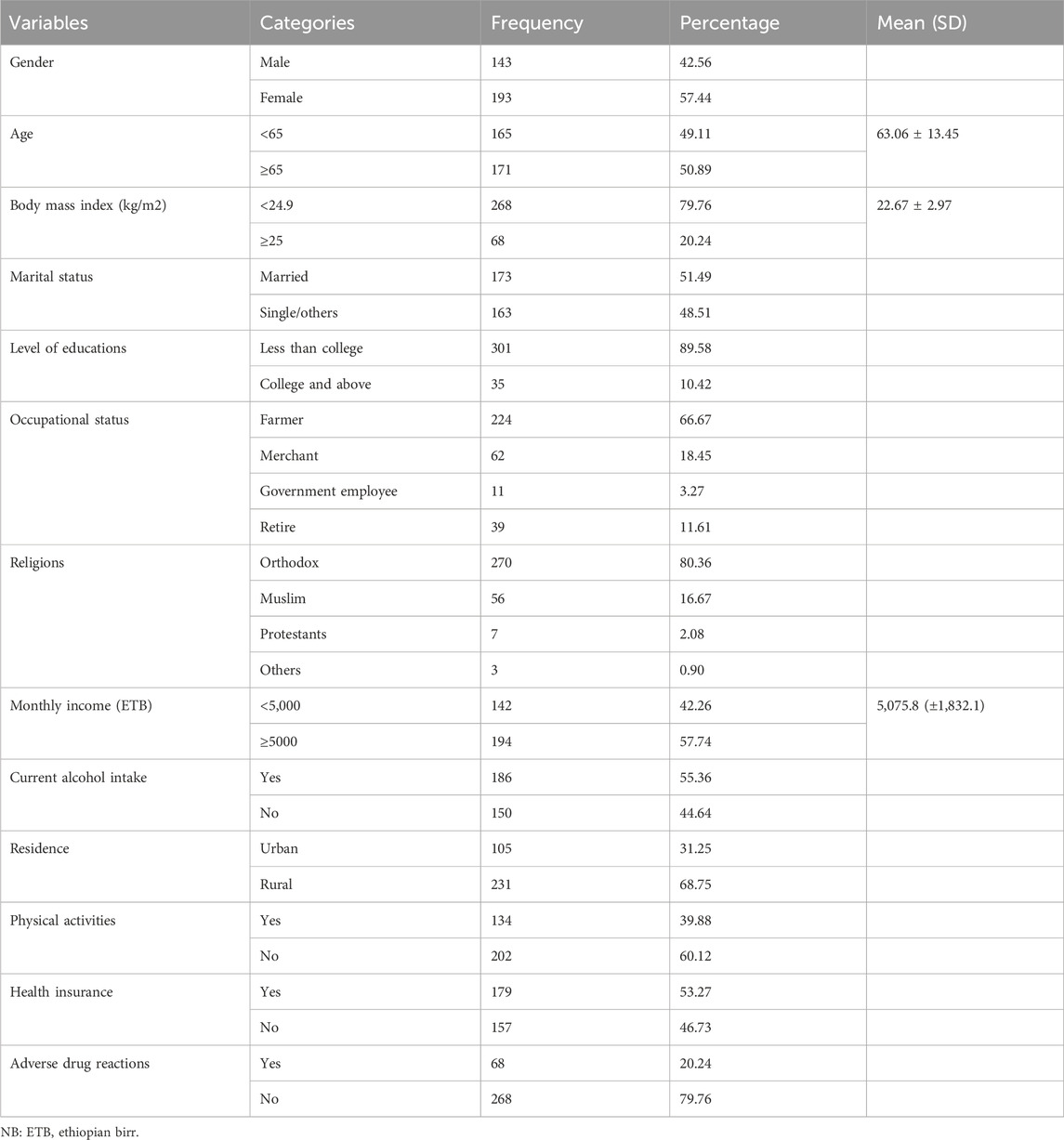
Table 1. Sociodemographic characteristics of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (N = 336).
Based on the Charles comorbidity index level, nearly half (48.21%) of the patients’ diseases were mild, according to the study. The most common diagnoses for the patients were heart failure (38.39%), hypertension (36.31%), and stroke (33.93%) (Table 2).
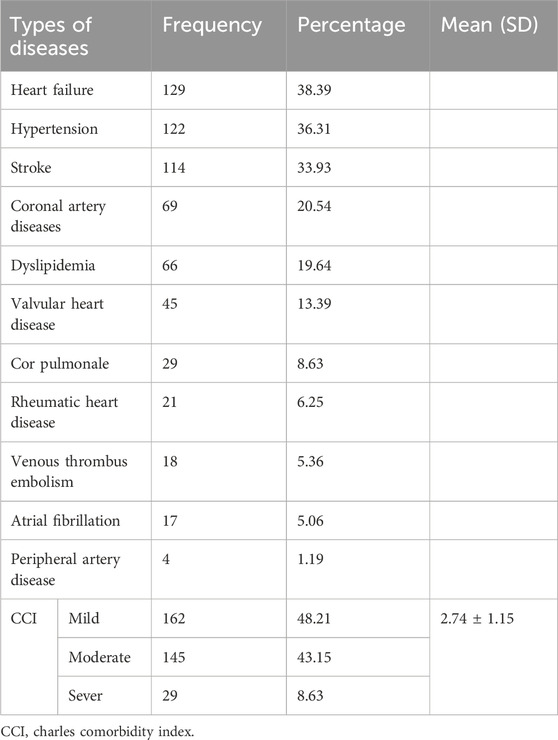
Table 2. Diseases pattern of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023.
In this investigation, the majority of patients (45.83%) were treated with diuretics, followed by ACEIs/ARBs (36.01%), and dyslipidemia (31.25%), and mean (SD) of the drugs 5.69 ± 2.43 Table 3
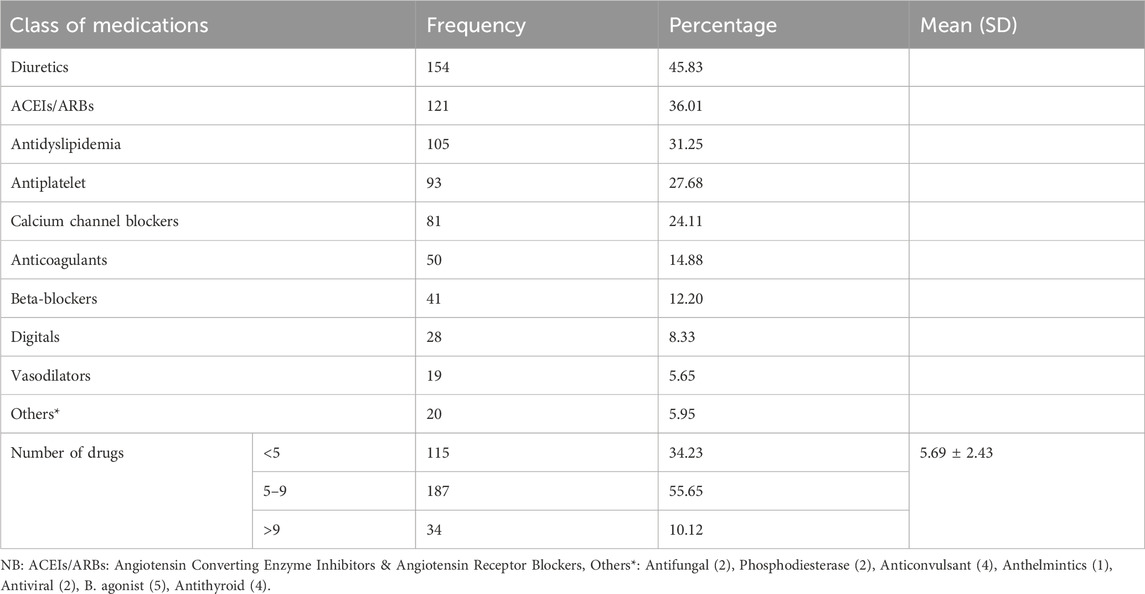
Table 3. Medication profiles of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023.
According to the Adherence in Chronic Disease Scale (ACDS), the mean and standard deviation of the adherences was 22.73 ± 4.49. Nearly one-third (29.17%) of patients had low adherence, and approximately half (50.89%) of research participants had medium adherence (Figure 1).
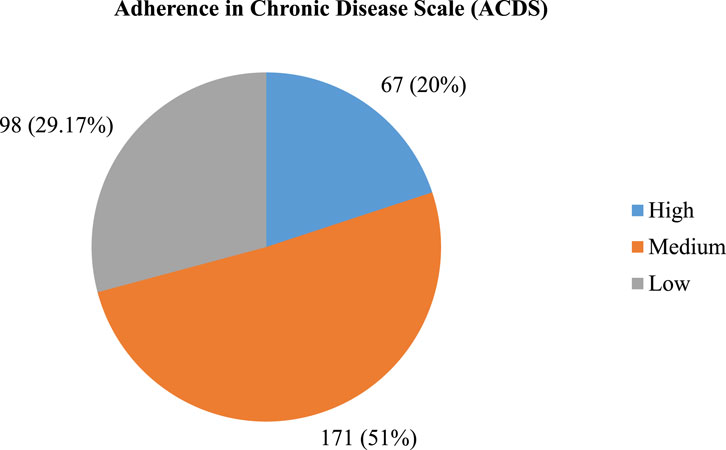
Figure 1. Level of adherence among cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (N = 336).
Based on the analysis of all low adherence cases, 92.86% of them had intervations; this means that 62.25% of patient counseling, 13.27% of spoken information to family members or caregivers, and 9.18% of written information was given (Table 4)
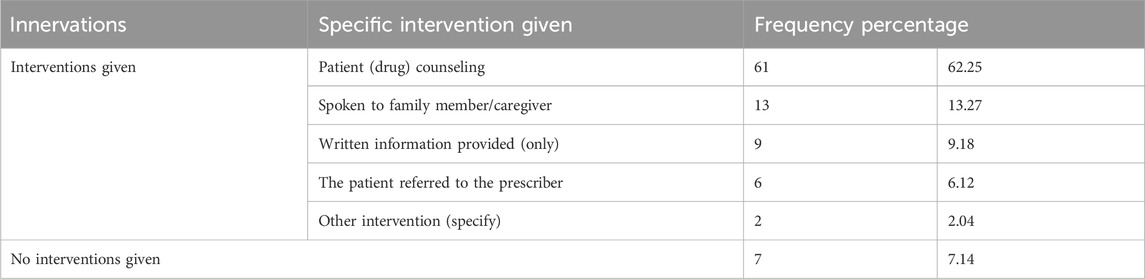
Table 4. Interventions given for low adherence among cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (98).
Ordinal logistic regression analysis was used to identify predictor variables of the level of medication adherence. According to the results of the multivariable ordinal logistic regression analysis, the level of medication adherence was substantially correlated with older age, marital status, alcoholism, lack of physical activity, and drug source. Comparing elderly people to adults, the lower level of adherence has increased by 2.7 times (AOR = 2.691; 95% CI, 1.704–4.251; p < 0.000). (AOR = 1.921; 95% CI, 1.214–3.039; p = 0.005) shows that the likelihood of singles and other nonmarried individuals had 1.9 times lower levels of adherence than married individuals. Compared to non-drinkers, patients who had consumed alcohol had 2.8 times higher odds of having poor adherence (AOR = 2.782; 95% CI, 1.745–4.435; p < 0.000). Patients without physical activity were twice more likely to have low levels of adherence than those with regular physical activity (AOR = 1.987; 95% CI 1.251–3.156; p = 0.004). When compared to patients who receive their medication for free, medication by payment adherence is significantly worse by the odds of 1.6 times (AOR = 1.593; 95% CI 1.003–2.529; p = 0.049) (Table 5).
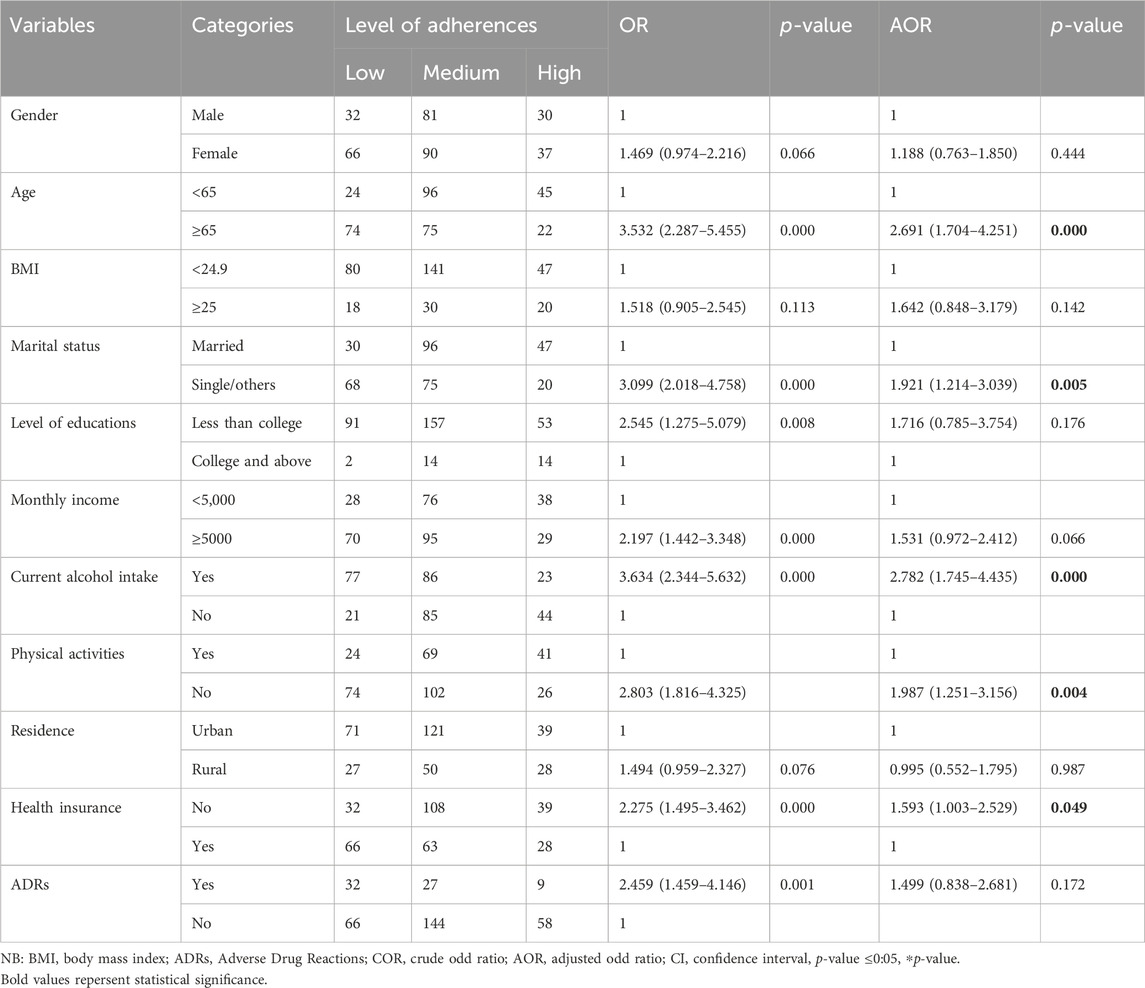
Table 5. Independent factors for the low level of medication adherence of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (N = 336).
Regarding the disease patterns that determine the adherence level, the Charles Comorbidities Index and stroke have a substantial correlation with the adherence level. Accordingly, the likelihood of a patient experiencing a stroke increases low adherence levels by a factor of 2.7 (AOR = 2.729; 95% CI 1.732–4.3011; p < 000). When compared to patients with mild CCI, those with severe CCI exhibited chances of a 2.5 higher probability of low-level adherences (AOR = 2.486; 95% CI 1.103–5.604; p = 0.028) (Table 6).
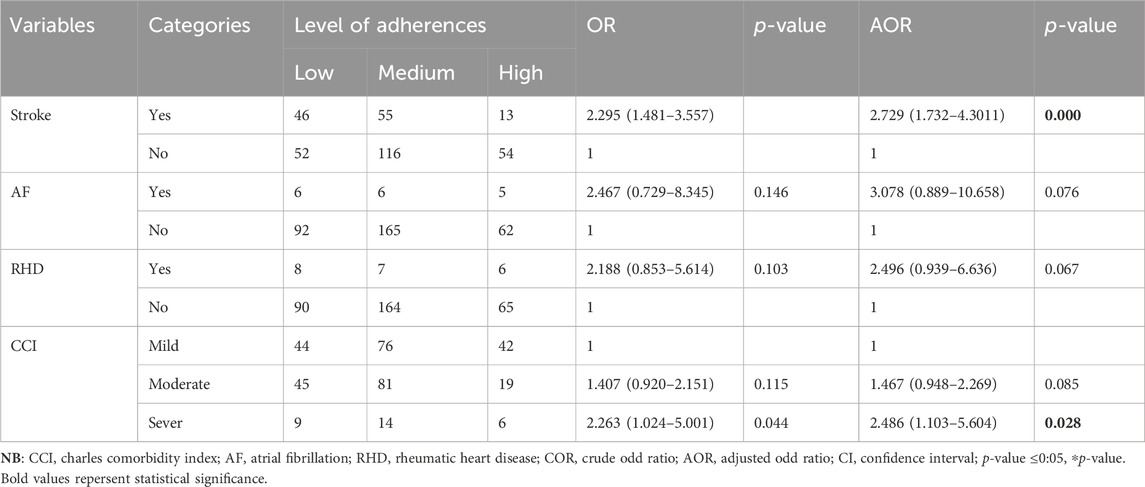
Table 6. Diseases factors for the low level of medication adherence of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (N = 336).
Medication patterns that were found to have an impact on medication adherence include the number of medications used, diuretics, CCBs, and anticoagulants. Compared to individuals who did not take diuretics, diuretic users had lower levels of adherence [AOR = 1.730, 95% CI (1.094–2.736); p = 0.019]. Patients taking CCBs were more likely to have low levels of adherence than those not taking the medicine by odds of 2.2 [AOR = 2. 153, 95% CI (1.116–3.129); p = 0.017]. AOR = 1.642, 95% CI (1.025–2.629); p = 0.039] shows that patients on anticoagulants had a 1.6-fold higher risk of low adherence than those not on these medicines. Similarly, patients who had more than five medications (AOR = 2.998 (1.817–4.947) p < 0.000) and patients who had more than nine medications (AOR = 3.031 (1.331–6.898) p = 0.008) were also more likely to have low medication adherence (Table 7).
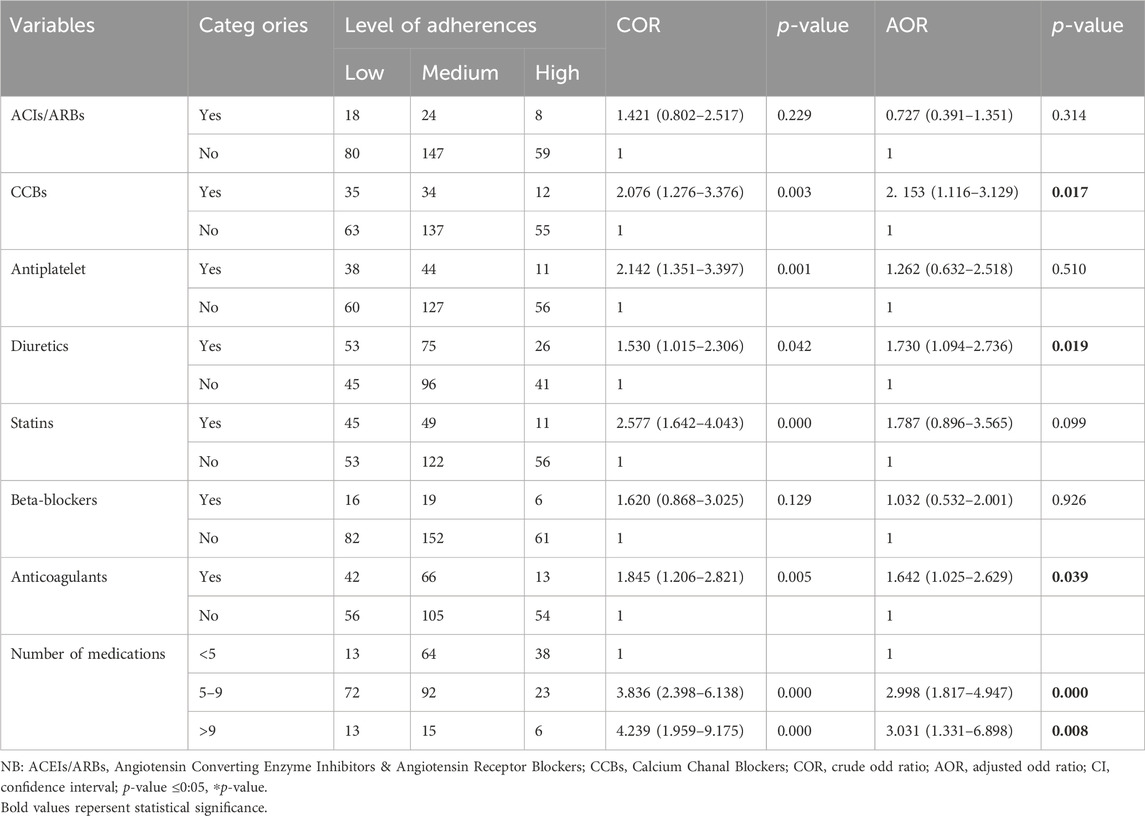
Table 7. Medication factors for the low level of medication adherence of cardiovascular disease patients at teaching hospitals in Amahara region, Ethiopia, 2023 (N = 336).
This study revealed the level of medication adherence among patients with cardiovascular diseases attending teaching hospitals in the Amahara region by using an ordinal logistic regression model. Globally, cardiovascular disease is the primary cause of death. The most difficult task in healthcare practice continues to be ensuring medication adherence in patients with chronic diseases, particularly in multimorbid patients, due to the complexity and many burdens of medications.
The current study found that half of the patients had medium adherence and one-third had poor adherence. Compared to studies from India, this study found relatively lower levels of adherence, with 44.4% of elderly patients with both diabetes and hypertension non-adherence (Jeyalakshmi et al., 2023). However, a study carried out in Jordan reveals that low (27.7%), medium (22.9%), and high (49.4%) (Al-Tarawneh et al., 2023). Another study in Taiwan found that low and high medication adherences were (34%) and medium adherences (32%) (Tsai et al., 2012). The variations in findings amongst studies may be due to various approaches, populations, economic conditions, and medication adherence instruments.
The results of this study indicated that non-adherence was more common in people over 65 years. This study’s findings were corroborated by some research including people with chronic disease (Mazzaglia et al., 2009; Jimmy and Jose, 2011; Kim et al., 2019; Li et al., 2021; Al-Tarawneh et al., 2023). There are numerous explanations for non-adherence in the specific group of older individuals. Among these include a higher likelihood of drug-related side effects as a result of pharmacodynamic and pharmacokinetic alterations, as well as a high frequency of comorbidity leading to polypharmacy.
In our study, patients who were single or otherwise unmarried had twice the chance of having poor adherence than patients who were married. This is consistent with a North Carolina study that found that single people had poor adherence rates twice (Trivedi et al., 2008; Wu et al., 2012; Doggrell and Kairuz, 2014). The reason behind married patients’ higher adherence rate compared to single patients remains unknown. Researchers have hypothesized that one explanation would be that spouses encourage adherence by offering helpful assistance (Kulkarni et al., 2006).
Alcohol use is a reliable indicator of poor treatment outcomes due to a decline in their cognitive abilities and unhealthy consequences may result from medication non-adherence. According to the current study, patients who were alcoholics had 2.8 times the likelihood of having low probability adherence. This result is in line with a study conducted in China (Li et al., 2021) that outlined the increased risk of medication nonadherence in patients who drank alcoholic drinks. Our finding is also partly consistent with those of Ahmed and colleagues, who discovered a link between alcohol use and a lack of adherence to diabetic self-care practice (Ahmed et al., 2006), non-adherence was associated with alcohol consumption (Aminde et al., 2019), Medication adherence was found to be negatively impacted by alcohol use, according to a systematic study (Grodensky et al., 2012). In another study conducted in Korea compared to people who never drank, moderate and heavy drinkers were less likely to exhibit good medication adherence (Han et al., 2017). However, the frequency of hospital visits by patients is negatively correlated with alcohol usage, according to prior research (Armstrong et al., 1998).
Patients in this trial who did not engage in physical activity had a two times higher likelihood of nonadherence than those who did. From a public health standpoint, physical activity can enhance wellbeing, medication adherence, and quality of life while lowering the burden of disease on both patients and the medical system (Kallings, 2008). Regular physical exercise has a good impact on medication adherence, according to a study done on hypertension patients at a cardiology unit in Italy (Sampogna et al., 2023). Another study conducted in Southwest Missouri State proves that exercise has a positive impact on improving medication adherence (Dishman, 1982).
Our findings show that patients who have no health insurance receiving their medication had nonadherence 1.6 times more frequently than those receiving it for free. This study’s supporting literature suggests that a rise in medicine nonadherence related to cost may be caused by growing consumer goods prices and drug costs (Dusetzina et al., 2023). One of the biggest obstacles to medication adherence is the financial strain and expense of prescription drugs (Chen et al., 2014). Another study also showed that sources of medications have a greater impact on medication adherence (Gast and Mathes, 2019). Medical costs associated with non-adherence may increase, as well as the frequency of doctor visits and hospital stays. The annual cost of healthcare could be decreased by addressing drug adherence.
Regarding the disease factors, patients with stroke would experience a 2.7-fold increase in low adherence. Because of polypharmacy and multimorbidity, stroke patients are more likely to have lower levels of medication adherence and self-care behaviors. Given the correlation between stroke and a roughly two-fold increased risk of cognitive decline, a stroke would be a significant contributing factor to nonadherence (Rohde et al., 2017). Consistent with what we discovered Numerous research suggest that stroke is the main reason for nonadherence (Crayton et al., 2018; Liu et al., 2021; Basheti et al., 2022; Cao et al., 2022).
The majority of research indicated that medication adherence was significantly associated with comorbidities. Patients with cardiovascular disease with comorbidities are especially difficult to adhere to their medication regimens. Patients in our study who had severe comorbidities exhibited 2.5 times lower levels of adherence than those with less severe comorbidities. Medication adherence for co-occurring disorders can be extremely challenging for individuals with cardiovascular illness, and non-adherence could hurt overall health. This has been documented in several studies that have demonstrated the influence of comorbidities on medication nonadherence (Loeppke et al., 2011; Curkendall et al., 2013; Smaje et al., 2018; Doya et al., 2024).
Identifying nonadherence in every patient who is not responding to treatment is the most crucial step toward increasing adherence because medication non-adherence and cardiovascular illness are expected to rise in frequency (Nelson et al., 2024). Thus, low adherence was more common in our study when patients were using calcium channel blockers, diuretics, and anticoagulants. Consistent with our findings, different studies discovered that the pharmacological class most strongly linked to nonadherence was CCBs, diuretics, and BBs (Kronish et al., 2011; Lemstra and Alsabbagh, 2014). However, some earlier research indicates that patients with diuretics had low adherence (Suol Thanh et al., 2022). This is due to Patients may skip dosages or restrict their medicine due to high expenses or difficulties getting refills of some medications; Patients who have uncomfortable or irritating side effects from their medications may purposefully miss doses or stop taking them completely; Complicated dosage regimens, multiple daily dosages, and the requirement to take the medication with food or on an empty stomach might make it difficult for patients to remember and follow the prescribed course of action.
Patients with cardiovascular illness are more likely to be polypharmacy, which means that it is associated with non-adherence. The occurrence of low adherence rates was significantly linked in our study to patients with polypharmacy and multiple polypharmacy, as these patients are less likely to take their medications as prescribed. On top of this, due to the increased number of prescriptions that can be overlooked daily, polypharmacy can result in medication nonadherence. Comparably, several drugs have been linked to medication adherence in the literature (Smaje et al., 2018; Wakai et al., 2021; Cao et al., 2022). Several studies also confirm that drug adherence has been published, with polypharmacy being one of the most often researched risk factors for nonadherence (Cooney and Pascuzzi, 2009; Nakajima et al., 2021; Basheti et al., 2022).
Clinical pharmacists can improve treatment outcomes for patients by improving patient adherence and managing cardiovascular diseases. In our study, 92.86% of nonadherence had interventions. For cardiovascular disease patients to have optimal treatment outcomes, it is imperative to identify and resolve adherence hurdles such as drug cost, transportation concerns, and healthcare availability. Medication non-adherence has a negative impact on psychosocial variables, expenses, and results that are shared by patients, caregivers, healthcare systems, payers, and society at large (Bosworth et al., 2017).
The study was strong in several areas. Because it was a multicenter study, its generalizability was enhanced. The study site had enough resources because it was a teaching Hospital. The study also establishes a correlation between subjective and objective findings. Furthermore, a consecutive sampling approach was employed. This might have lessened the study’s source of bias. The present research has certain shortcomings. Patients’ self-reported adherence measuring scale, which is based on respondents’ honesty and faith in them, is used to estimate the adherence level. Responses may be influenced, leading to an overestimation or underestimation of the medication adherence level. Notwithstanding these drawbacks, the power of our investigation was sufficient, and the results aligned favorably with those of other global studies of a comparable nature.
Cardiovascular drug adherence lowers morbidity and death significantly while also saving money on medical expenses. Medication nonadherence persists despite these benefits because of several obstacles at the patient, provider, and systemic levels. The current study concluded that one-third of study participants had low medication adherence, roughly half had medium adherence, and one-fifth had good adherence. Older age, marital status, drinker, physical inactivity, drug source, comorbidity, and polypharmacy all contributed to the low level of medication adherence. Therefore, to slow the course of the disease and achieve better treatment outcomes, healthcare professionals should endeavor to increase patient knowledge of the importance of taking their medication adherence.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The Debre Tabor University Ethical Review Committee gave its ethical approval to the proposal with a reference number of CHS/265/2023. The studies were conducted in Accordance with the local legislation and institutional requirements. The participants provided their written informed consent to Participate in this study. The study followed Helsinki legislation in terms of doing it in a properly anonymous and confidential manner.
SD: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing–original draft, Writing–review and editing. SW: Data curation, Formal Analysis, Visualization, Writing–review and editing. FD: Data curation, Project administration, Supervision, Writing–review and editing. YY: Data curation, Resources, Supervision, Writing–review and editing. YW: Data curation, Resources, Writing–review and editing. TM: Data curation, Resources, Visualization, Writing–review and editing, Project administration.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
For their cooperation during the study, the hospital administration and study participants are much appreciated by the authors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1422703/full#supplementary-material
Ahmed, A., Karter, A., and Liu, J. (2006). Alcohol consumption is inversely associated with adherence to diabetes self-care behaviours. Diabet. Med. 23 (7), 795–802. doi:10.1111/j.1464-5491.2006.01878.x
Al-Tarawneh, F., Ali, T., Al-Tarawneh, A., Altwalbeh, D., Gogazeh, E., Bdair, O., et al. (2023). Study of adherence level and the relationship between treatment adherence, and superstitious thinking related to health issues among chronic disease patients in southern Jordan: cross-sectional study. Patient Prefer. adherence 17, 605–614. doi:10.2147/PPA.S390997
Aminde, L. N., Tindong, M., Ngwasiri, C. A., Aminde, J. A., Njim, T., Fondong, A. A., et al. (2019). Adherence to antidiabetic medication and factors associated with non-adherence among patients with type-2 diabetes mellitus in two regional hospitals in Cameroon. BMC Endocr. Disord. 19, 35–39. doi:10.1186/s12902-019-0360-9
Armstrong, M. A., Midanik, L. T., and Klatsky, A. L. (1998). Alcohol consumption and utilization of health services in a health maintenance organization. Med. care 36 (11), 1599–1605. doi:10.1097/00005650-199811000-00009
Basheti, I. A., Ayasrah, S. M., Ahmad, M. M., Abu-Snieneh, H. M., and Abuadas, F. H. (2022). Medications adherence and associated factors among patients with stroke in the Kingdom of Saudi Arabia. Pharm. Pract. (Granada) 20 (4), 2736. doi:10.18549/PharmPract.2022.4.2736
Bennett, J. E., et al. (2018). NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 392 (10152), 1072–1088. doi:10.1016/S0140-6736(18)31992-5
Bosworth, H. B., Fortmann, S. P., Kuntz, J., Zullig, L. L., Mendys, P., Safford, M., et al. (2017). Recommendations for providers on person-centered approaches to assess and improve medication adherence. J. General Intern. Med. 32, 93–100. doi:10.1007/s11606-016-3851-7
Burnier, M. (2023). The role of adherence in patients with chronic diseases. Eur. J. Intern. Med. 119, 1–5. doi:10.1016/j.ejim.2023.07.008
Cao, W., Kadir, A. A., Wang, J., Hu, L., Wen, L., Yu, M., et al. (2022). Medication non-adherence and associated factors among older adult stroke survivors in China. Front. Pharmacol. 13, 1054603. doi:10.3389/fphar.2022.1054603
Chen, L.-C., Chen, T. C., Huang, Y. B., and Chang, C. S. (2014). Disease acceptance and adherence to imatinib in Taiwanese chronic myeloid leukaemia outpatients. Int. J. Clin. Pharm. 36, 120–127. doi:10.1007/s11096-013-9867-8
Cooney, D., and Pascuzzi, K. (2009). Polypharmacy in the elderly: focus on drug interactions and adherence in hypertension. Clin. geriatric Med. 25 (2), 221–233. doi:10.1016/j.cger.2009.01.005
Crayton, E., Wright, A. J., and Ashworth, M. (2018). Improving medication adherence in stroke survivors: the intervention development process. BMC Health Serv. Res. 18, 772–813. doi:10.1186/s12913-018-3572-1
Curkendall, S. M., Thomas, N., Bell, K. F., Juneau, P. L., and Weiss, A. J. (2013). Predictors of medication adherence in patients with type 2 diabetes mellitus. Curr. Med. Res. Opin. 29 (10), 1275–1286. doi:10.1185/03007995.2013.821056
DiMatteo, M. R. (2004a). Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med. care 42, 200–209. doi:10.1097/01.mlr.0000114908.90348.f9
DiMatteo, M. R. (2004b). Evidence-based strategies to foster adherence and improve patient outcomes: the author's recent meta-analysis indicates that patients do not follow treatment recommendations unless they know what to do, are committed to doing it, and have the resources to be able to adhere. JAAPA-Journal Am. Acad. Physicians Assistants 17 (11), 18–22.
Dishman, R. K. (1982). Compliance/adherence in health-related exercise. Health Psychol. 1 (3), 237–267. doi:10.1037/0278-6133.1.3.237
Doggrell, S. A., and Kairuz, T. (2014). Comparative studies of how living circumstances influence medication adherence in≥ 65-year-olds. Int. J. Clin. Pharm. 36, 30–35. doi:10.1007/s11096-013-9894-5
Doya, I. F., Yahaya, J. J., Ngaiza, A. I., and Bintabara, D. (2024). Low medication adherence and its associated factors among patients with type 2 diabetes mellitus attending Amana Hospital in Dar es Salaam, Tanzania: a cross-sectional study. Int. Health 16 (2), 200–207. doi:10.1093/inthealth/ihad042
Dusetzina, S. B., Besaw, R. J., Whitmore, C. C., Mattingly, T. J., Sinaiko, A. D., Keating, N. L., et al. (2023). Cost-related medication nonadherence and desire for medication cost information among adults aged 65 years and older in the US in 2022. JAMA Netw. Open 6 (5), e2314211. doi:10.1001/jamanetworkopen.2023.14211
Fuchs, R. A. (2022). The association of lower medication adherence and increased medical spending. University of Nebraska Medical Center.
Gast, A., and Mathes, T. (2019). Medication adherence influencing factors—an (updated) overview of systematic reviews. Syst. Rev. 8 (1), 112. doi:10.1186/s13643-019-1014-8
Grodensky, C. A., Golin, C. E., Ochtera, R. D., and Turner, B. J. (2012). Systematic review: effect of alcohol intake on adherence to outpatient medication regimens for chronic diseases. J. Stud. Alcohol Drugs 73 (6), 899–910. doi:10.15288/jsad.2012.73.899
Han, E., Sohn, H. S., Lee, J. Y., and Jang, S. (2017). Health behaviors and medication adherence in elderly patients. Am. J. health Promot. 31 (4), 278–286. doi:10.4278/ajhp.150205-QUAN-709
Jeyalakshmi, K., Rao, M., Yn, S., Thunga, G., Sudhakar, C., et al. (2023). Determinants of medication non-adherence among the elderly with co-existing hypertension and type 2 diabetes mellitus in rural areas of Udupi District in Karnataka, India. Patient Prefer. adherence 17, 1641–1656. doi:10.2147/PPA.S380784
Jimmy, B., and Jose, J. (2011). Patient medication adherence: measures in daily practice. Oman Med. J. 26 (3), 155–159. doi:10.5001/omj.2011.38
Kallings, L. V. (2008). Physical activity on prescription: studies on physical activity level, adherence, and cardiovascular risk factors. Karolinska Institutet Swed.
Kim, S. J., Kwon, O. D., Han, E. B., Lee, C. M., Oh, S. W., Joh, H. K., et al. (2019). Impact of number of medications and age on adherence to antihypertensive medications: a nationwide population-based study. Medicine 98 (49), e17825. doi:10.1097/MD.0000000000017825
Kim, Y.-Y., Lee, J. S., Kang, H. J., and Park, S. M. (2018). Effect of medication adherence on long-term all-cause-mortality and hospitalization for cardiovascular disease in 65,067 newly diagnosed type 2 diabetes patients. Sci. Rep. 8 (1), 12190. doi:10.1038/s41598-018-30740-y
K, J., Rao, M., Yn, S., Thunga, G., Sudhakar, C., et al. (2023). Determinants of medication non-adherence among the elderly with Co-existing hypertension and type 2 diabetes mellitus in rural areas of Udupi district in Karnataka, India. Patient Prefer Adherence 17, 1641–1656. doi:10.2147/PPA.S380784
Kolandaivelu, K., Leiden, B. B., O'Gara, P. T., and Bhatt, D. L. (2014). Non-adherence to cardiovascular medications. Eur. Heart J. 35 (46), 3267–3276. doi:10.1093/eurheartj/ehu364
Korkmaz, U. T. K.CARDIOVASCULAR DISEASES AND PREVENTION (2021). Surgical medical sciences diagnosis and treatment, 31.
Kravitz, R. L., Hays, R. D., Sherbourne, C. D., DiMatteo, M. R., Rogers, W. H., Ordway, L., et al. (1993). Recall of recommendations and adherence to advice among patients with chronic medical conditions. Archives Intern. Med. 153 (16), 1869–1878. doi:10.1001/archinte.1993.00410160029002
Kronish, I. M., Woodward, M., Sergie, Z., Ogedegbe, G., Falzon, L., and Mann, D. M. (2011). Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation 123 (15), 1611–1621. doi:10.1161/CIRCULATIONAHA.110.983874
Kubica, A., et al. (2017). The Adherence in Chronic Diseases Scale—a new tool to monitor implementation of a treatment plan. Folia Cardiol. 12 (1), 19–26.
Kulkarni, S. P., Alexander, K. P., Lytle, B., Heiss, G., and Peterson, E. D. (2006). Long-term adherence with cardiovascular drug regimens. Am. Heart J. 151 (1), 185–191. doi:10.1016/j.ahj.2005.02.038
Lemstra, M., and Alsabbagh, M. W. (2014). Proportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysis. Patient Prefer. adherence 8, 211–218. doi:10.2147/PPA.S55382
Li, J., Zhang, Z., Wang, B., and Xue, F. (2021). Antihypertensive medication adherence and cardiovascular disease risk: a longitudinal cohort study. Atherosclerosis 320, 24–30. doi:10.1016/j.atherosclerosis.2021.01.005
Liu, M., Zheng, G., Cao, X., Chang, X., Zhang, N., Liang, G., et al. (2021). Better medications adherence lowers cardiovascular events, stroke, and all-cause mortality risk: a dose-response meta-analysis. J. Cardiovasc. Dev. Dis. 8 (11), 146. doi:10.3390/jcdd8110146
Loeppke, R., Haufle, V., Jinnett, K., Parry, T., Zhu, J., Hymel, P., et al. (2011). Medication adherence, comorbidities, and health risk impacts on workforce absence and job performance. J. Occup. Environ. Med. 53 (6), 595–604. doi:10.1097/JOM.0b013e318223470b
Mazzaglia, G., Ambrosioni, E., Alacqua, M., Filippi, A., Sessa, E., Immordino, V., et al. (2009). Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 120 (16), 1598–1605. doi:10.1161/CIRCULATIONAHA.108.830299
McKenzie, S. J., McLaughlin, D., Clark, J., and Doi, S. A. R. (2015). The burden of non-adherence to cardiovascular medications among the aging population in Australia: a meta-analysis. Drugs & aging 32, 217–225. doi:10.1007/s40266-015-0245-1
Nakajima, R., Watanabe, F., and Kamei, M. (2021). Factors associated with medication non-adherence among patients with lifestyle-related non-communicable diseases. Pharm. (Basel) 9 (2), 90. doi:10.3390/pharmacy9020090
Nangia, R., Singh, H., and Kaur, K. (2016). Prevalence of cardiovascular disease (CVD) risk factors. Med. J. Armed Forces India 72 (4), 315–319. doi:10.1016/j.mjafi.2014.07.007
Nelson, A. J., Pagidipati, N. J., and Bosworth, H. B. (2024). Improving medication adherence in cardiovascular disease. Nat. Rev. Cardiol. 21, 417–429. doi:10.1038/s41569-023-00972-1
Peacock, E., Joyce, C., Craig, L. S., Lenane, Z., Holt, E. W., Muntner, P., et al. (2021). Low medication adherence is associated with decline in health-related quality of life: results of a longitudinal analysis among older women and men with hypertension. J. Hypertens. 39 (1), 153–161. doi:10.1097/HJH.0000000000002590
Perreault, S., Yu, A. Y. X., Côté, R., Dragomir, A., White-Guay, B., and Dumas, S. (2012). Adherence to antihypertensive agents after ischemic stroke and risk of cardiovascular outcomes. Neurology 79 (20), 2037–2043. doi:10.1212/WNL.0b013e3182749e56
Rehman, S., Rehman, E., Ikram, M., and Jianglin, Z. (2021). Cardiovascular disease (CVD): assessment, prediction and policy implications. BMC Public Health 21 (1), 1299–1314. doi:10.1186/s12889-021-11334-2
Rohde, D., Merriman, N. A., Doyle, F., Bennett, K., Williams, D., and Hickey, A. (2017). Does cognitive impairment impact adherence? A systematic review and meta-analysis of the association between cognitive impairment and medication non-adherence in stroke. PloS one 12 (12), e0189339. doi:10.1371/journal.pone.0189339
Sabaté, E. (2003). Adherence to long-term therapies: evidence for action. Pan American Health Organization, World Health Organization.
Saeed, A., Amin, Q. K., Saeed, R., and Yousafzai, Z. A. (2023). Comparing medication non-adherence in cardiovascular disease patients at public and private hospitals in Peshawar: a cross-sectional study of prevalence and contributing factors. Cureus 15 (3), e36345. doi:10.7759/cureus.36345
Sampogna, G., Luciano, M., Di Vincenzo, M., Toni, C., D'Ambrosio, E., Rampino, A., et al. (2023). Physical activity influences adherence to pharmacological treatments in patients with severe mental disorders: results from the multicentric, randomized controlled LIFESTYLE trial. Front. Pharmacol. 14, 1285383. doi:10.3389/fphar.2023.1285383
Shalansky, S. J., and Levy, A. R. (2002). Effect of number of medications on cardiovascular therapy adherence. Ann. Pharmacother. 36 (10), 1532–1539. doi:10.1345/aph.1C044
Smaje, A., Weston-Clark, M., Raj, R., Orlu, M., Davis, D., and Rawle, M. (2018). Factors associated with medication adherence in older patients: a systematic review. Aging Med. 1 (3), 254–266. doi:10.1002/agm2.12045
Sokol, M. C., McGuigan, K. A., Verbrugge, R. R., and Epstein, R. S. (2005). Impact of medication adherence on hospitalization risk and healthcare cost. Med. care 43, 521–530. doi:10.1097/01.mlr.0000163641.86870.af
Stewart, S.-J. F., Moon, Z., and Horne, R. (2023). Medication nonadherence: health impact, prevalence, correlates, and interventions. Psychol. Health 38 (6), 726–765. doi:10.1080/08870446.2022.2144923
Suol Thanh, P., et al. (2022). “Medication adherence in cardiovascular diseases,” in Novel Pathogenesis and treatments for cardiovascular disease. Editor C. G. David (Rijeka: IntechOpen). Ch. 22.
Trivedi, R. B., Ayotte, B., Edelman, D., and Bosworth, H. B. (2008). The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J. Behav. Med. 31, 489–497. doi:10.1007/s10865-008-9173-4
Tsai, K.-T., Chen, J. H., Wen, C. J., Kuo, H. K., Lu, I. S., Chiu, L. S., et al. (2012). Medication adherence among geriatric outpatients prescribed multiple medications. Am. J. geriatric Pharmacother. 10 (1), 61–68. doi:10.1016/j.amjopharm.2011.11.005
Van der Laan, D. M., Elders, P. J. M., Boons, C. C. L. M., Nijpels, G., and Hugtenburg, J. G. (2019). Factors associated with nonadherence to cardiovascular medications: a cross-sectional study. J. Cardiovasc. Nurs. 34 (4), 344–352. doi:10.1097/JCN.0000000000000582
Wakai, E., Ikemura, K., Kato, C., and Okuda, M. (2021). Effect of number of medications and complexity of regimens on medication adherence and blood pressure management in hospitalized patients with hypertension. PLoS One 16 (6), e0252944. doi:10.1371/journal.pone.0252944
Keywords: adherence, cardiovascular, determinate factors, Ethiopia, ordinal logistic regression
Citation: Dagnew SB, Wondm SA, Dagnew FN, Yimer YS, Wondmkun YT and Moges TA (2024) Level of medication adherence and its determinants of cardiovascular disease patients attending at specialized teaching hospitals of Amhara regional state, Ethiopia: a multicenter cross-sectional study. Front. Pharmacol. 15:1422703. doi: 10.3389/fphar.2024.1422703
Received: 24 April 2024; Accepted: 05 July 2024;
Published: 30 July 2024.
Edited by:
Hao Li, Shanghai Jiao Tong University, ChinaReviewed by:
Yumao Zhang, Sun Yat-sen University, ChinaCopyright © 2024 Dagnew, Wondm, Dagnew, Yimer, Wondmkun and Moges. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuel Berihun Dagnew, c2FtdWVsYmVyaWh1bjEyQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.