- 1Department of Developmental and Behavioral Pediatrics, Fujian Children’s Hospital(Fujian Branch of Shanghai Children’s Medical Center), College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, China
- 2The First Clinical Medical College of Nanjing University of Chinese Medicine, Nanjing, China
- 3Department of Developmental and Behavioral Pediatrics, Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Background: Desmopressin acetate (DDAVP) and behavioral interventions (BI) are cornerstone treatments for nocturnal enuresis (NE), a common pediatric urinary disorder. Despite the growing body of clinical studies on massage therapy for NE, comprehensive evaluations comparing the effectiveness of Tuina with DDAVP or BI are scarce. This study aims to explore the efficacy of Tuina in the management of NE.
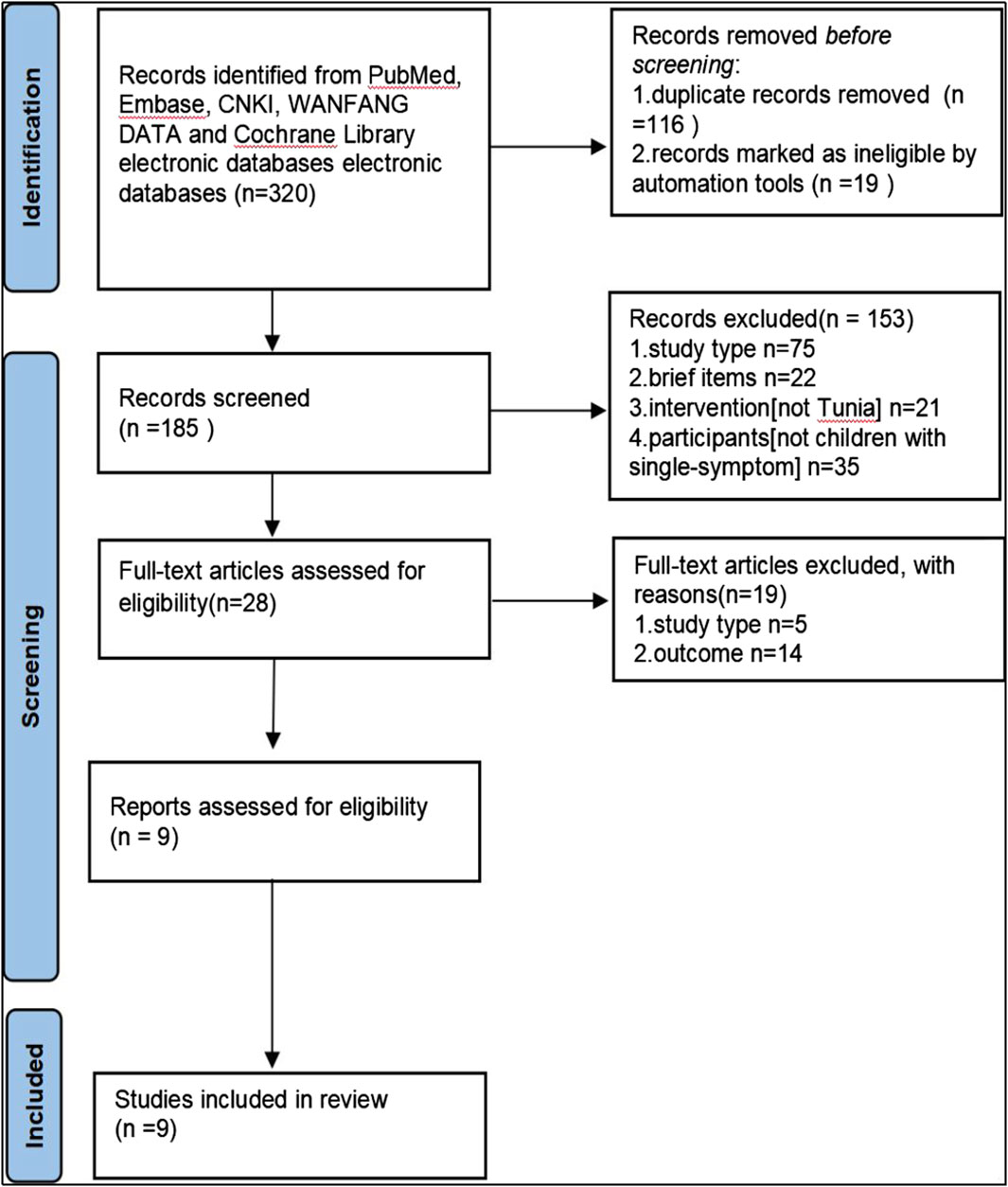
Methods: A systematic search of international databases was conducted using keywords pertinent to Tuina and NE. The inclusion criteria were limited to randomized controlled trials (RCTs) that evaluated NE treatments utilizing Tuina against DDAVP or BI. This meta-analysis included nine RCTs, comprising a total of 685 children, to assess both complete and partial response rates.
Results: Tuina, used as a combination therapy, showed enhanced clinical efficacy and improved long-term outcomes relative to the control group. The therapeutic efficacy of Tuina was not directly associated with the number of acupoints used. Instead, employing between 11 and 20 acupoints appeared to have the most significant effect.
Conclusion: The findings of this meta-analysis support the potential of Tuina as an adjunct therapy to enhance the sustained clinical efficacy of traditional treatments for NE. However, Tuina cannot completely replace DDAVP or BI in the management of NE. While this study illuminates some aspects of the effective acupoint combinations, further research is crucial to fully understand how Tuina acupoints contribute to the treatment of NE in children.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=442644, identifier CRD42023442644.
1 Introduction
Nocturnal enuresis (NE) is characterized by recurrent involuntary urination during sleep in children aged 5 years and older, persisting for over 3 months with at least two episodes per week. This condition, resulting from the child’s inability to awaken from sleep (Austin et al., 2016), exhibits a prevalence rate ranging from 4.8% to 15.2%, which notably declines with advancing age (Ferrara et al., 2020). Moreover, NE significantly impacts the psychological wellbeing and overall quality of life of affected individuals (Kuoch et al., 2019).
The primary treatments for NE include desmopressin acetate (DDAVP) and behavioral interventions (BI) (Alqannad et al., 2021). While these modalities offer therapeutic benefits, their implementation is often protracted and fraught with challenges, including adverse drug reactions and a high rate of symptom recurrence post-treatment discontinuation. These factors complicate adherence for both patients and their families (Kuwertz-Bröking and von Gontard, 2018). Consequently, there is a pressing need for alternative therapeutic strategies to address the multifaceted challenges of managing NE in children.
Tuina, a recognized form of complementary and alternative medicine (CAM), has been integral to human health for centuries. In recent decades, the US Food and Drug Administration (FDA) has established regulatory guidelines for CAM practices (Food and Drug Administration, 2006). Tuina, characterized by its non-invasive, needle-free, cost-effective, and non-pharmacological approach, employs manual manipulation to enhance patient wellbeing (Wan et al., 2018). Gaining substantial popularity in Western nations (Su and Li, 2011), Tuina operates on the principle of activating meridian acupoints (Mehta et al., 2017), which are critical pressure points located superficially on the skin. The activation of these acupoints stimulates myelinated nerve fibers within the hypothalamus and pituitary gland, triggering the release of β-endorphins into the cerebrospinal fluid and bloodstream (Kwan et al., 2014). This biochemical process is instrumental in modulating physiological responses, such as inhibiting bladder contractions by elevating spinal and reflexive β-endorphin levels (Mehta et al., 2017). Previous meta-analyses have highlighted Tuina’s efficacy as a therapeutic option for pediatric NE; however, these studies often excluded trials that compared Tuina with established treatments like DDAVP or BI, which are considered standard care approaches (Tong et al., 2022). The long-term effectiveness of Tuina in treating NE remains to be fully assessed. Given the variety of techniques and the frequency of acupoint utilization, this meta-analysis seeks to delineate the specific roles of different Tuina applications through extensive subgroup analyses. The goal is to provide a comprehensive framework that supports informed decision-making in clinical settings.
2 Methods
This systematic review and meta-analysis were conducted in alignment with the Cochrane Collaboration guidelines and the PRISMA statement. Ethical approval was not required for this study. The protocol was submitted for registration with the International Prospective Register of Systematic Reviews (PROSPERO) on 23 July 2023 (ID: CRD42023442644); the registration was pending at the time of this manuscript’s submission.
2.1 Eligibility criteria
Only randomized controlled trials (RCTs) were considered for inclusion. Cohort studies, case series, and review articles were excluded. Abstracts that met the inclusion criteria were considered; however, if insufficient data were presented, the corresponding authors were contacted for additional information. Abstracts were excluded if no response was obtained. To mitigate selection bias and ensure comprehensive data analysis, all patients diagnosed with NE were included, irrespective of gender, age, educational background, or ethnicity. In the experimental arm, Tuina was administered either alone, in combination with DDAVP, or alongside BI. The control group received standard treatments, which did not include Tuina but may have included DDAVP or BI. The treatments administered to the control and experimental groups, apart from Tuina therapy, were identical. The primary endpoint was the total effective rate (TER), and the secondary endpoint assessed long-term effectiveness.
2.2 Search strategy
From inception through May 2023, comprehensive searches were conducted in several electronic databases including PubMed, Embase, CNKI, WANFANG DATA, and the Cochrane Library. The search terms were derived from the National Medical Library’s medical topic title synonym dictionary. A concurrent search was executed using the terms “Tuina,” “Nocturnal enuresis,” “Desmopressin acetate,” and “Behavioral intervention.” Additionally, reference lists from initially retrieved articles were reviewed to identify further studies eligible for inclusion. The inclusion criteria targeted all RCTs published in English and Chinese that assessed the efficacy of Tuina, DDAVP, and BI in the management of NE.
2.3 Selection and data extraction
Data extraction was conducted by two independent reviewers using a standardized form to capture information on baseline characteristics, eligibility criteria, intervention dosages, and details of experimental and control treatments, including study settings. Upon acquiring potentially relevant studies in full-text format, two authors independently assessed these for inclusion. Any disagreements were resolved through discussion among the authors. The data extraction process focused on participant numbers, demographic characteristics, treatment duration, post-treatment follow-up periods, and specific details of the massage treatment such as types of acupoints and evaluation methods employed. This data was subsequently verified by additional reviewers to ensure robust literature search, data extraction, and quality assessment processes.
2.4 Analyzing the risk of bias in studies included
The risk of bias in the included studies was evaluated using the Cochrane Collaboration’s risk of bias tool (Higgins et al., 2019). This comprehensive assessment addressed randomization type, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, and potential conflicts of interest such as industry support. The evaluations were independently conducted by three reviewers. In instances of differing opinions, a fourth reviewer was consulted to achieve consensus.
2.5 Assessing heterogeneity and recognizing reporting biases
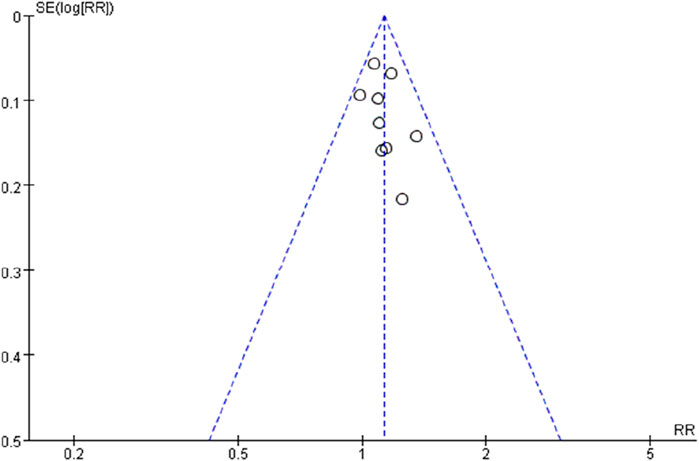
Heterogeneity among the studies was quantified using the I2 statistic. A p-value of less than 0.05 was deemed statistically significant for heterogeneity analyses. I2 values of 0 indicated no observed heterogeneity, while values of 50% or higher suggested substantial heterogeneity. In cases where I2 exceeded 50%, subgroup analyses were conducted to explore potential sources of heterogeneity, such as variations in control types and outcome scoring systems, to maintain the accuracy of the data synthesis. Additionally, funnel plots were utilized to detect potential publication biases.
2.6 Data extraction
Data were collected using standardized forms and analyzed according to traditional Chinese medicine criteria for diagnosing and treating illnesses and syndromes (Su and Li, 2011). The effectiveness of the treatment was categorized into four levels: complete remission (CR), where no recurrence of enuresis was noted within a month; significantly effective (SE), characterized by a reduction in symptoms with recurrence not exceeding once per week within a month; partial remission (PR), defined by a decrease in symptom frequency but occurring more than once a week; and ineffective, where no change in symptom frequency was observed compared to baseline. The calculation of the percentages of individuals achieving CR, SE, or PR facilitated the determination of the TER.
2.7 Data synthesis
Data analysis was performed using Review Manager (RevMan) version 5.4 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) (Cochrane Training, 2020). Subgroup analyses were conducted to assess the efficacy of Tuina in treating NE, both in terms of short-term and long-term effectiveness, and in comparison with other therapies. One subgroup analysis focused on the efficacy of different treatment modalities within Tuina and non-Tuina populations. Another subgroup explored the relationship between the number of Tuina acupoints utilized and treatment outcomes. The commonly used Tuina acupoints, their classifications, and the combinations employed were also summarized.
3 Results
3.1 Study selection
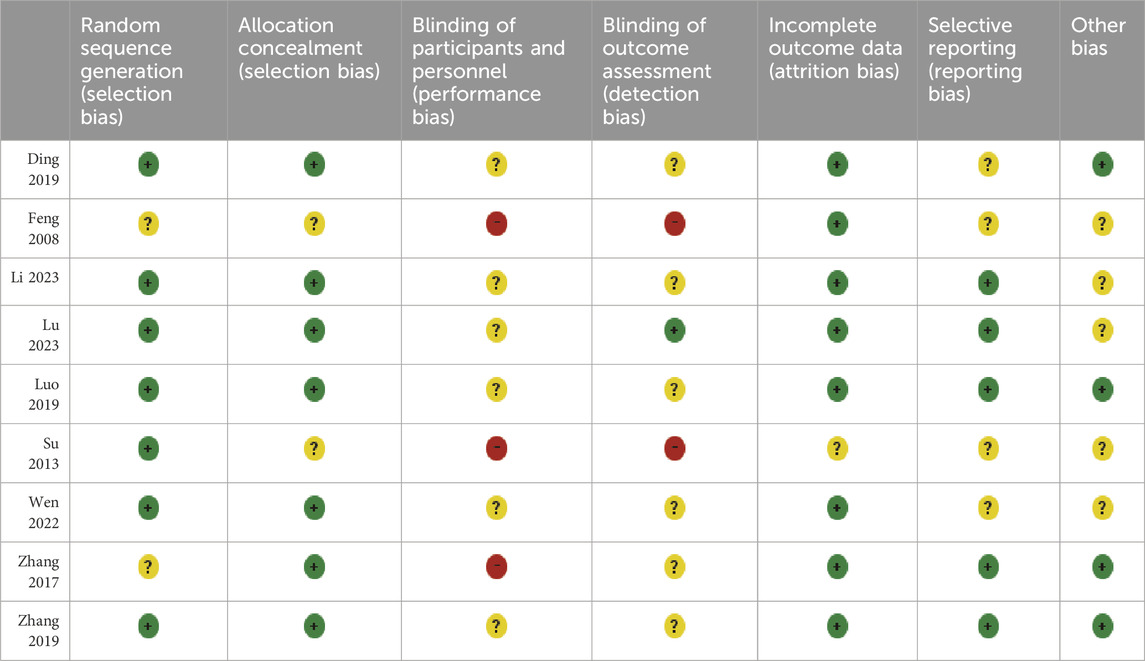
Eligible trials are illustrated in Figure 1, while Table 1 provides a comprehensive overview of the trials incorporated into this analysis. Nine RCTs involving 685 participants, aged between 5 and 18 years, were included. These trials featured varying sample sizes, ranging from 45 to 162 participants, and were conducted in China.
3.2 Risk of bias assessment
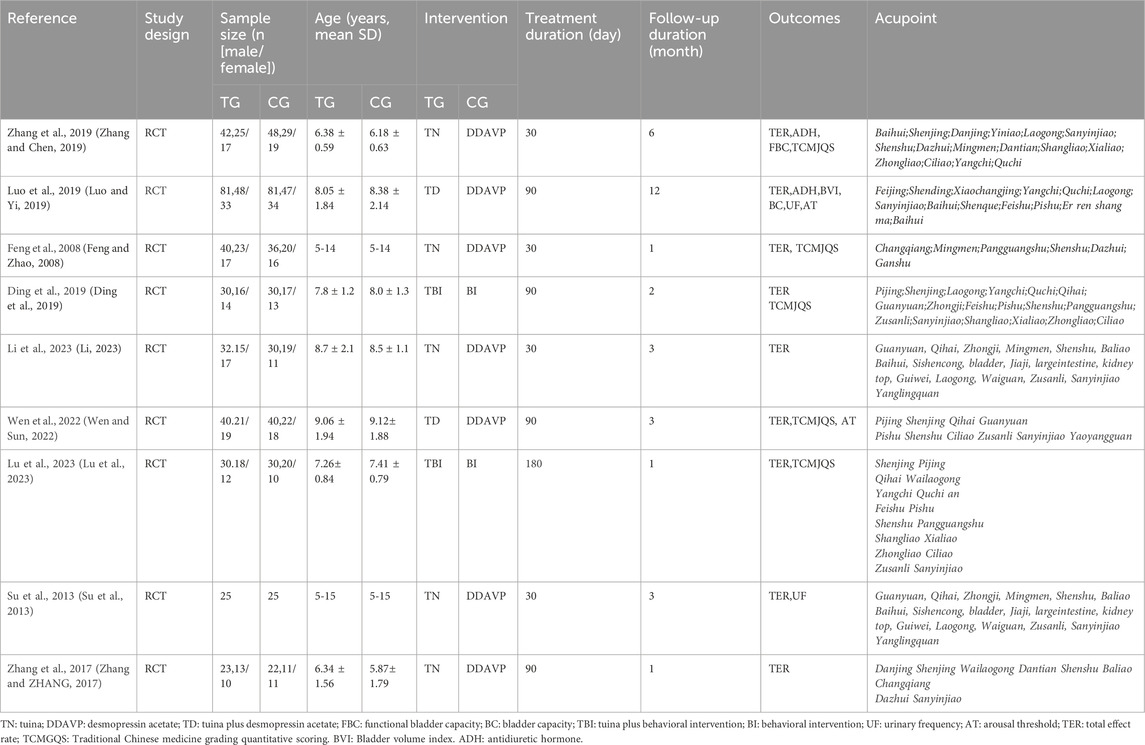
The methodologies employed across studies demonstrated considerable variability in quality (Figure 2; Table 2). The methodological shortcomings identified include unclear sequence generation in two studies, unclear risks associated with allocation concealment in two studies, unclear (six studies) or high risks (three studies) of bias in blinding of participants and personnel, and unclear (six studies) or high risks (two studies) in blinding of outcome assessments. Additionally, one study presented unclear risks regarding incomplete outcome data, and five RCTs had unclear risks related to selective reporting. Risks of other biases were unclear in five studies.
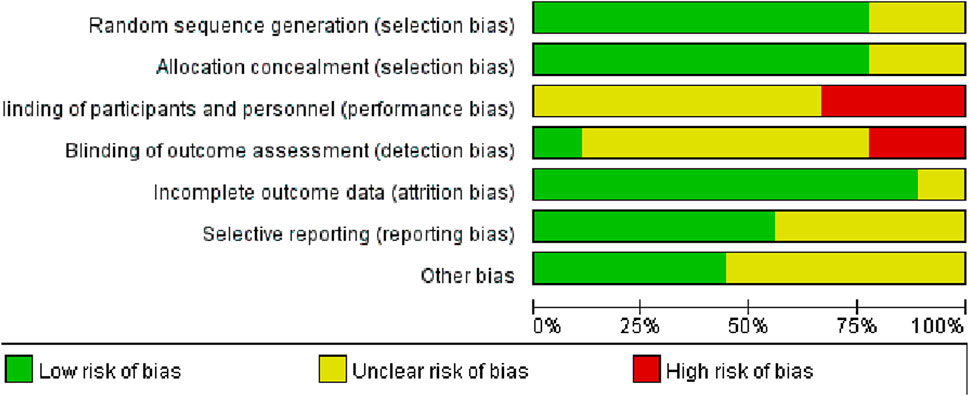
Figure 2. Assessment of methodological quality of randomised trials.  Low risk of bias;
Low risk of bias;  unclear risk of bias;
unclear risk of bias;  high risk of bias.
high risk of bias.
3.3 Total effective rate
The efficacy of Tuina compared with DDAVP and BI for treating NE was assessed across nine studies involving 685 participants (Feng and Zhao, 2008; Su et al., 2013; Zhang and ZHANG, 2017; Ding et al., 2019; Luo and Yi, 2019; Zhang and Chen, 2019; Wen and Sun, 2022; Li, 2023; Lu et al., 2023). No significant heterogeneity was observed among the studies (I2 = 0), prompting the use of a fixed-effects model for the meta-analysis. The results indicated a significantly higher TER in the Tuina treatment group compared to the control group, with a relative risk (RR) of 1.13 (95% confidence interval [CI)], 1.05 to 1.22; p < 0.0009) (Figure 3). Additionally, funnel plots used to assess publication bias showed no evidence of bias (Figure 4).
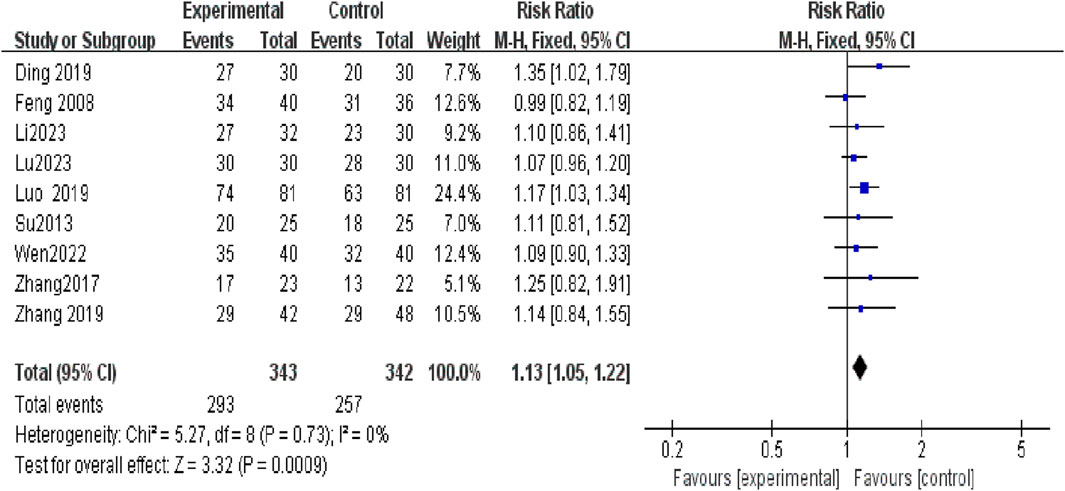
Figure 3. Compared to the control group, the experimental group demonstrated a substantial improvement in the total effective rate.
3.4 Short-term and long-term treatment durations analysis
Subgroup analyses revealed a significantly higher TER in the Tuina treatment group compared to the non-Tuina control group. For short-term treatments (less than 45 days), the RR was 1.13 (95% CI, 1.01 to 1.26; p = 0.03); and for long-term treatments (3 months), the RR was 1.13 (95% CI, 1.03 to 1.25; p = 0.01) (Figure 5).
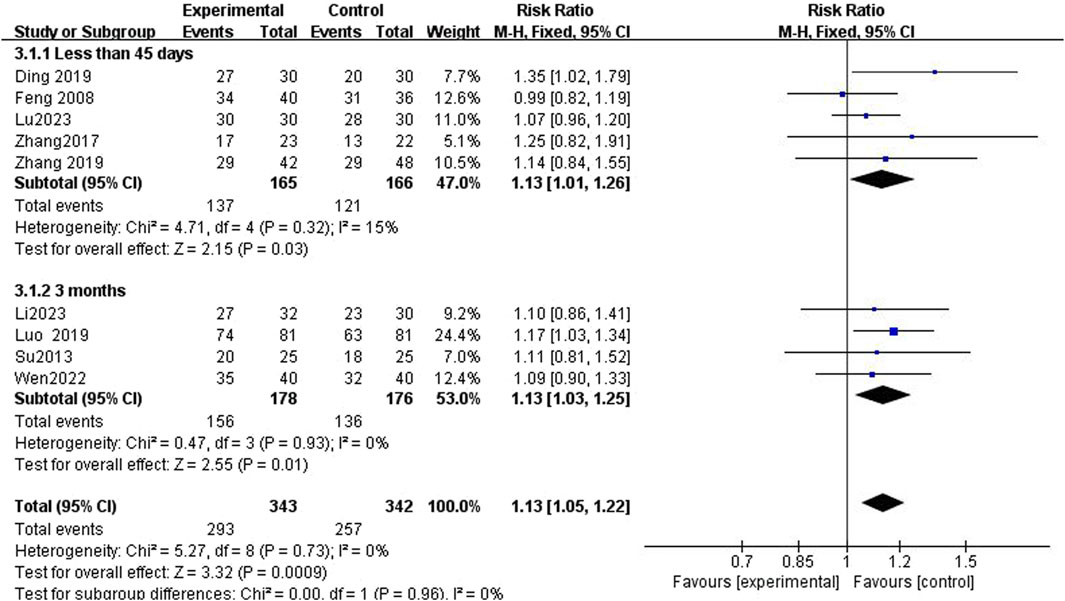
Figure 5. In subgroup analysis, the experimental group demonstrated a significantly improved total effective rate compared to the control group.
3.5 Tuina versus non-Tuina treatment analysis
Five studies (Feng and Zhao, 2008; Su et al., 2013; Zhang and ZHANG, 2017; Zhang and Chen, 2019; Li, 2023) investigated the efficacy of Tuina for treating NE in children compared to DDAVP alone. The analysis showed no statistically significant difference in TER between Tuina alone and the DDAVP group, with an RR of 1.10 (95% CI, 0.97 to 1.24; p = 0.15). However, in two studies (Luo and Yi, 2019; Wen and Sun, 2022), the combination of Tuina with DDAVP exhibited a higher TER compared to DDAVP alone, reaching statistical significance (RR = 1.15; 95% CI, 1.03 to 1.28; p = 0.01). Additionally, two studies (Ding et al., 2019; Lu et al., 2023) compared the TER of Tuina combined with BI against BI alone, showing an RR of 1.19 (95% CI, 1.03 to 1.36; p = 0.05) (Figure 6).
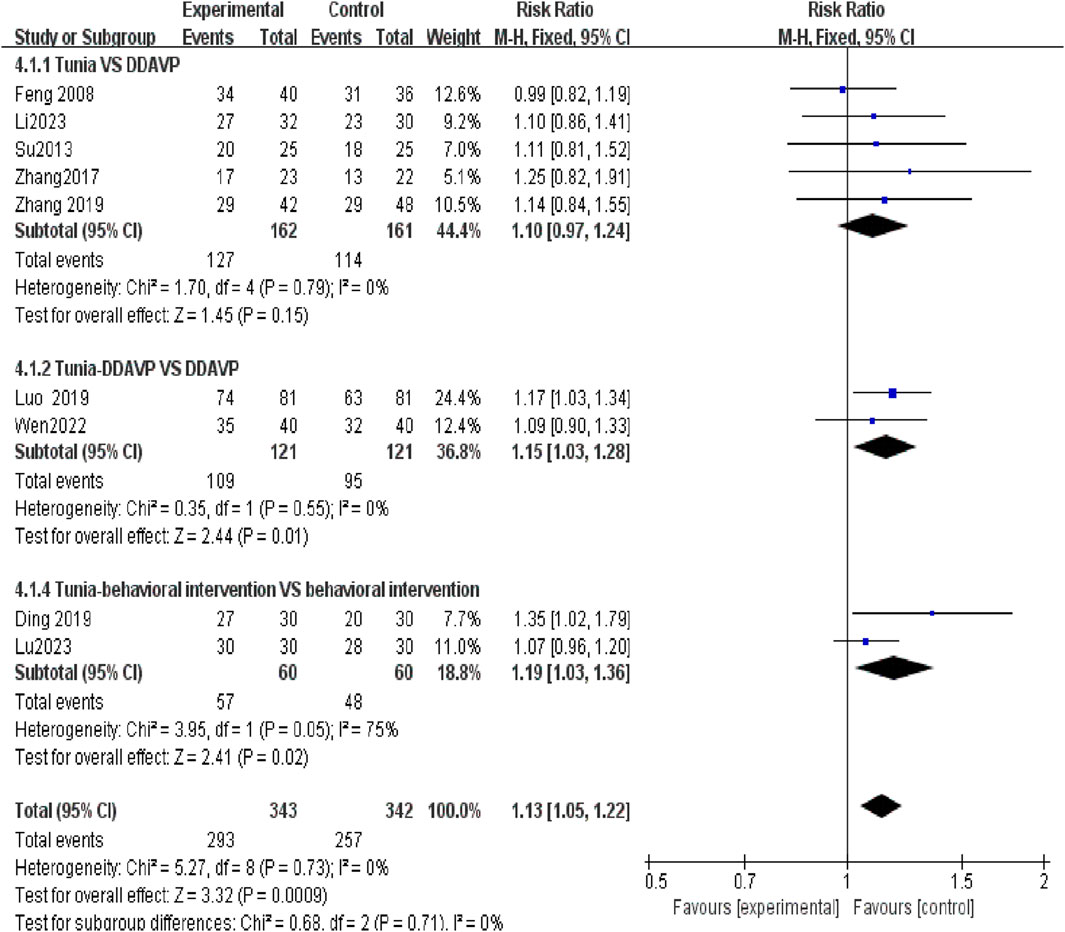
Figure 6. In subgroup analysis, the efficacy of Tuina as a monotherapy is inferior to that of an adjuvant treatment.
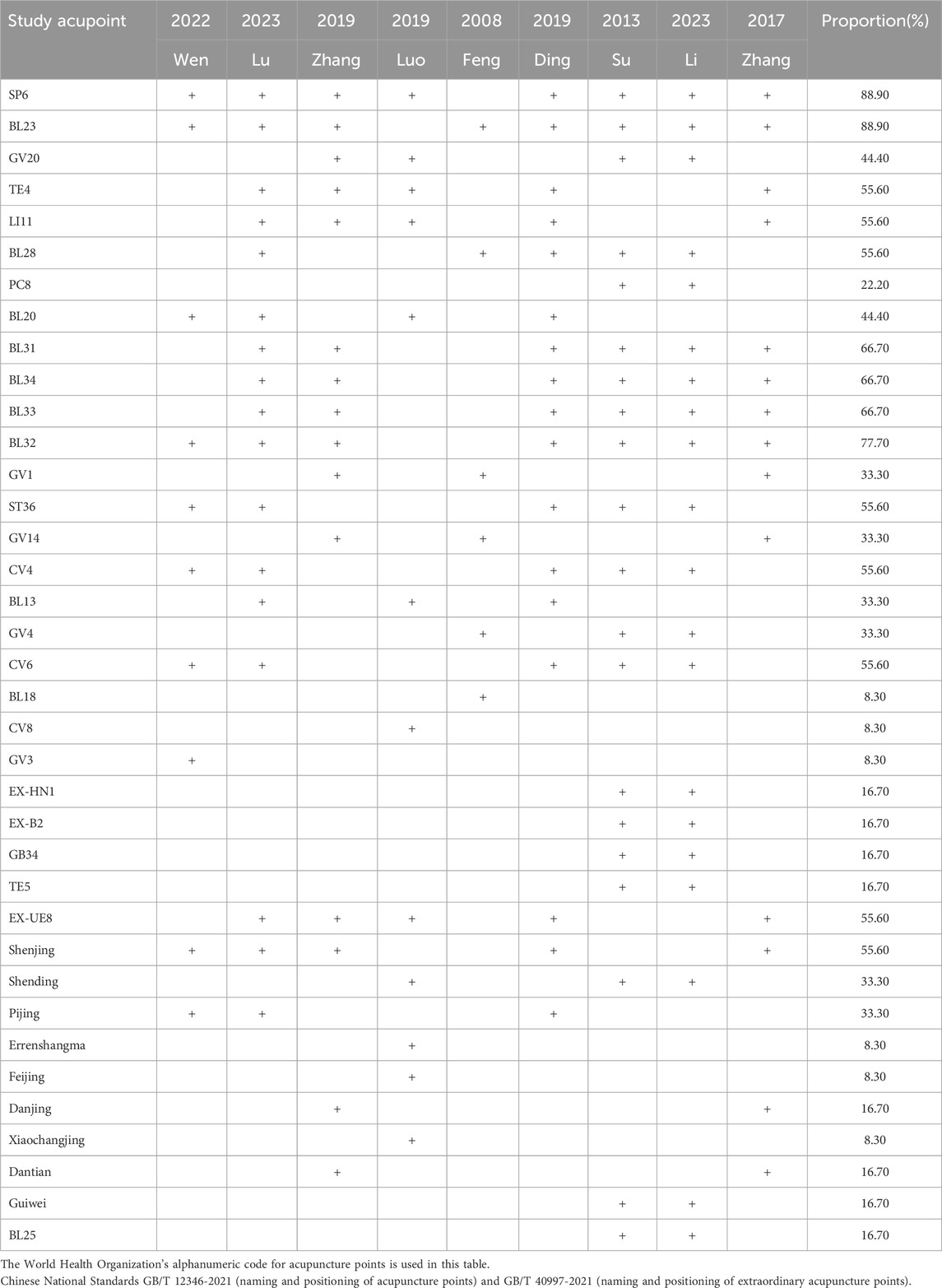
3.6 Acupoint in the selected studies
In Tuina therapy, the conventional wisdom that “more acupuncture points yield better results” is not supported by our findings. Subgroup analyses suggest that employing 11–20 acupoints tends to produce the most pronounced effects (Figure 7). The most frequently used acupoints were San Yin Jiao (SP6) and Shen Shu (BL23) (Table 3). Other commonly applied acupoints included Bai Hui (GV20), Yang Chi (TE4), Qu Chi (LI11), Pang Guang Shu (BL28), Lao Gong (PC8), Pi Shu (BL20), Shang Liao (BL31), Xia Liao (BL34), Zhong Liao (BL33), Ci Liao (BL32), Chang Qiang (GV1), Zu San Li (ST36), Da Zhui (GV14), Guan Yuan (CV4), Fei Shu (BL13), Ming Men (GV4), Qi Hai (CV6), Gan Shu (BL18), Shen Que (CV8), Si Shen Cong (EX-HN1), Jia Ji (EX-B2), Yan Ling Quan (GB34), Yao Yang Guan (GV3), Wai Guan (TE5), Tian Shu (ST25), Wai Lao Gong (EX-UE8).
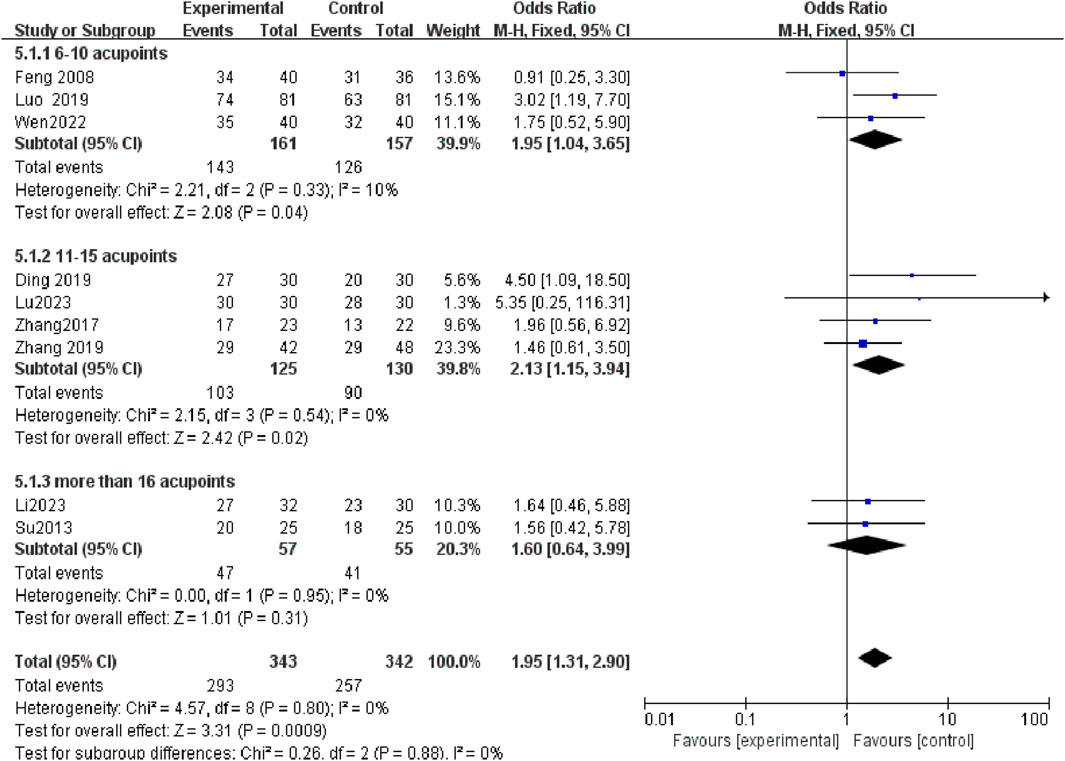
Figure 7. In subgroup analysis, the most notable therapeutic benefit is evident in Tuina when utilizing 11–20 acupoints.
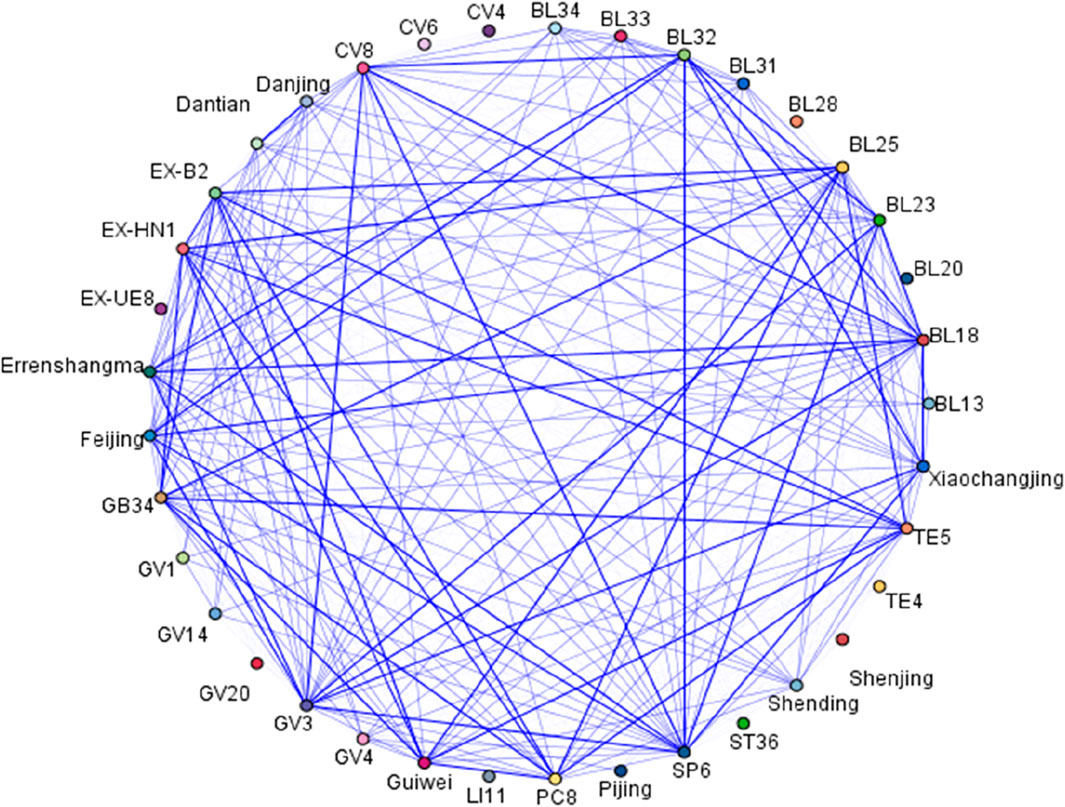
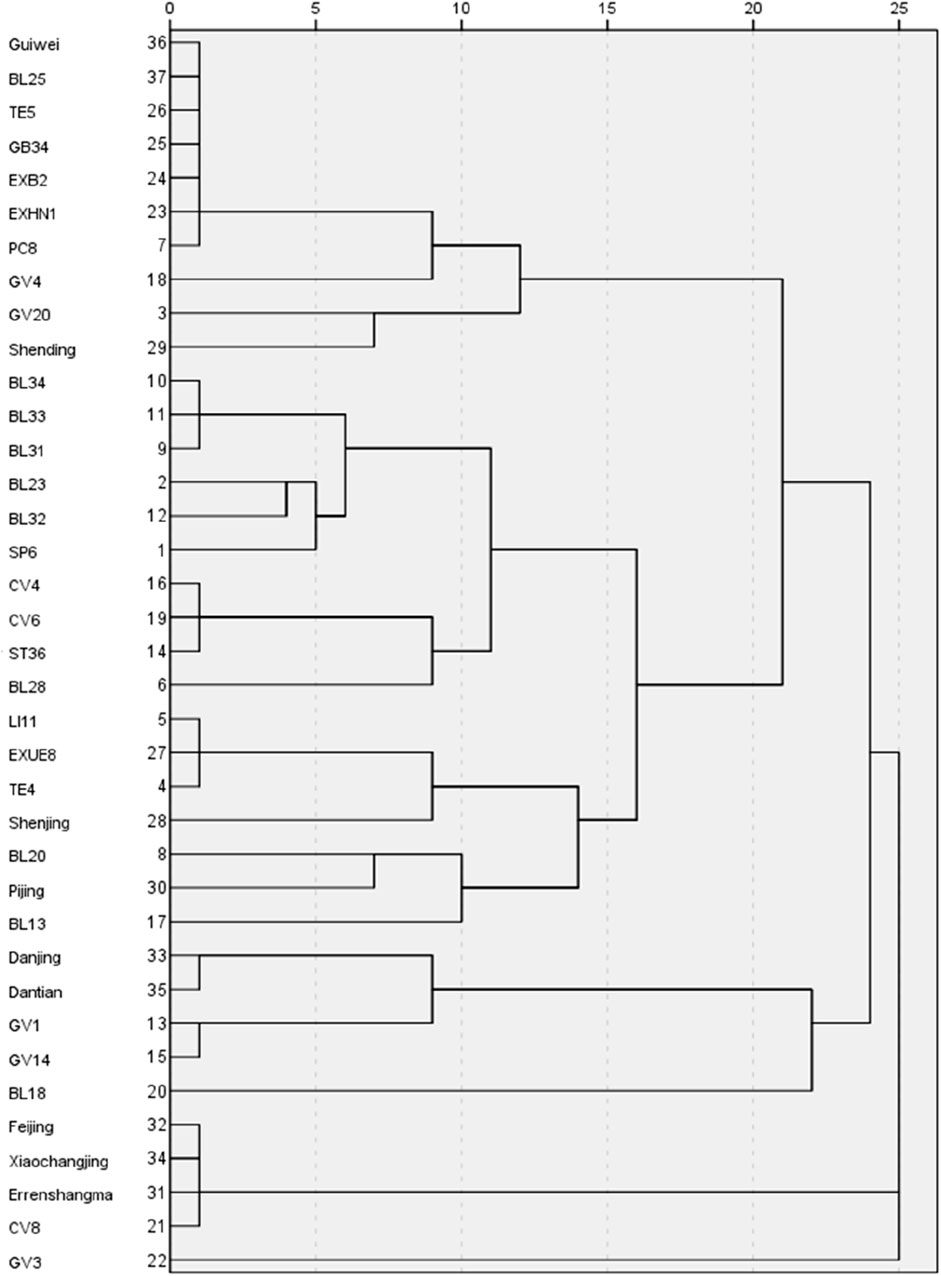
Figure 8 illustrates the relationships between these acupoints in this study, with thicker lines indicating stronger associations. In the association analysis, the confidence percentage for the association of (Sanyinjiao, Shenshu, Baliao) BL23, SP6, and Baliao was the highest at 85.71%. The acupoints used in Tuina treatment for NE are broadly classified into six categories, with the combination of first and second groups reflecting traditional acupoint in prior research (Yuksek et al., 2003). These groupings are: 1) Guiwei/BL25/TE5/GB34/EXB2/EXHN1/PC8/GV4/GV20/Shengding; 2) BL34/BL33/BL31/BL23/BL32/SP6/CV4/CV6/ST36/BL28/LI11/EXUE8/TE4/Shenjing/BL20/Pijing/BL13; 3)Danjing/Dantian/GV1/GV14; 4)BL28; 5)Feijing/Xiaochangjing/Errenshangma/CV8; 6) GV3 (Figure 9).
3.7 Adverse events
Treatment-related adverse events were recorded in two of the studies reviewed (Feng and Zhao, 2008; Li, 2023), and the remaining seven studies (Su et al., 2013; Zhang and ZHANG, 2017; Ding et al., 2019; Luo and Yi, 2019; Zhang and Chen, 2019; Lu et al., 2023) observed no adverse reactions.
4 Discussion
This systematic review represents a first study to evaluate the efficacy of Tuina in RCTs for pediatric NE, using DDAVP and BI as control. The review encompassed data from nine RCTs involving 658 participants. It was noted that all studies in the experimental group used Tuina, either as a standalone treatment or in combination with DDAVP or BI. The findings suggest that Tuina, particularly when combined with other treatments, offers substantial benefits in enhancing clinical efficacy and improving the long-term prognosis for children experiencing NE. Given its safety, non-invasive nature, painlessness, and ease of application, Tuina emerges as an attractive treatment modality for parents.
The pathogenesis of NE is complex, influenced by multiple factors including the disruption of the circadian rhythm of hormone release and the resultant nocturnal polyuria. These factors play significant roles in the pathophysiology of NE (Yousefichaijan et al., 2016; Keten et al., 2020; Alqannad et al., 2021).
A key pathophysiological contributor to NE is the diminished bladder functional capacity coupled with increased detrusor muscle activity during the night (Kawauchi et al., 2003). Treatments with DDAVP and BI are specifically designed to address these underlying issues (Glazener and Evans, 2000; Keten et al., 2020). Concurrently, Tuina therapy stimulates myelinated nerve fibers in the hypothalamus and pituitary gland, which are essential components in the neural regulation of urinary function (Keten et al., 2020). The selection of acupoints that impact both the spinal cord urination center and the parasympathetic nerve innervation of the urinary tract is critical (Radmayr et al., 2001; Glazener et al., 2005). By increasing β-endorphin levels in the cerebrospinal fluid, Tuina may help to inhibit bladder contractions (Su and Li, 2011; Kwan et al., 2014).
Further evidence supporting the long-term efficacy of Tuina comes from four studies (Su et al., 2013; Luo and Yi, 2019; Wen and Sun, 2022; Li, 2023), which demonstrate that its therapeutic benefits persist for at least 3 months post-treatment. This data underscores Tuina’s potential to enhance the management of NE symptoms over extended periods.
In the RCTs investigating the efficacy of treating NE with Tuina and DDAVP as standalone treatments, no statistically significant outcomes were observed (Feng and Zhao, 2008; Su et al., 2013; Zhang and ZHANG, 2017; Zhang and Chen, 2019; Li, 2023). This underscores the necessity for caution in recommending Tuina as an adjunct therapy in combination with other established treatments. Tuina, with its origins in ancient Chinese medicine, is designed to correct bodily imbalances by stimulating specific acupoints along the body’s meridian system. According to traditional Chinese medicine theory, the body is viewed as a holistic network of channels and organs, and it is believed that activating these acupoints can restore balance and harmony within the organ system (Radmayr et al., 2001). Acupoints are used to influence health conditions, including NE, potentially affecting the spinal urination center and the parasympathetic innervation of the urinary tract (Chapple, 2013). The most frequently used Tuina acupoints in the treatment of NE are San Yin Jiao (SP6) and Shen Shu (BL23), with our evidence suggesting that the use of 11-20acupoints provides the most significant therapeutic effect. These acupoints are categorized into six distinct groups. Notably, two studies included in this analysis (Luo and Yi, 2019; Zhang and Chen, 2019) demonstrate an improvement in bladder function following treatment.
The study has several limitations that should be considered when interpreting the findings. First, the inclusion of studies was predominantly restricted to Chinese research, resulting in a lack of diversity in regional characteristics. Second, due to traditional practices, achieving complete double-blindness in RCTs through randomized allocation was not possible. Third, the primary outcome of overall effectiveness limited the scope of the meta-analysis. Although some studies reported on various outcome measures, including antidiuretic hormone, bladder volume index, functional bladder capacity, bladder capacity, urinary frequency, and arousal threshold (Luo and Yi, 2019; Zhang and Chen, 2019), there is a recommendation for future research to standardize data units to enhance the accuracy of Tuina’s performance evaluation in NE.
Despite facing numerous challenges, Tuina has emerged as a burgeoning CAM gaining global recognition. This study marks the first to present substantial evidence regarding the adjunctive impact of Tuina in treating NE, detailing its therapeutic methodologies and acupoint categorization. It highlights a potentially valuable complementary approach for managing NE.
5 Conclusion
Within the scope of adjuvant therapies for pediatric NE, Tuina demonstrates promising long-term efficacy. The acupoints most commonly employed include San Yin Jiao (SP6) and Shen Shu (BL23), with the application of 11–20 acupoints typically yielding the most significant effects. To further enhance the treatment of NE in children, extensive research is required to substantiate and standardize these methods. Although only a few reports of adverse reactions have been documented, the inherent limitations concerning study inclusion underscore the need for more comprehensive, high-quality, long-term follow-up RCTs to validate these findings.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XC: Data curation, Formal Analysis, Funding acquisition, Writing–original draft, Writing–review and editing. W-jS: Data curation, Writing–original draft. J-rW: Data curation, Formal Analysis, Methodology, Writing–review and editing. Y-yC: Data curation, Formal Analysis, Methodology, Writing–review and editing. X-dY: Writing–review and editing, Data curation, Formal Analysis, Funding acquisition, Methodology.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the first batch of high-level medical and health personnel teams with flexible introduction in Fujian Province in 2021 (no. RT 2022-002), Fujian Provincial Health Technology Project (no. 2023QNA067) and the Clinical Research Center for Pediatric Neurodevelopmental Disease of Fujian Province.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alqannad, E. M., Alharbi, A. S., Almansour, R. A., and Alghamdi, M. S. (2021). Alarm therapy in the treatment of enuresis in children: types and efficacy review. Cureus 13, e17358. doi:10.7759/cureus.17358
Austin, P. F., Bauer, S. B., Bower, W., Chase, J., Franco, I., Hoebeke, P., et al. (2016). The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization committee of the International Children’s Continence Society. Neurourol. Urodyn. 35, 471–481. doi:10.1002/nau.22751
Chapple, W. (2013). Proposed catalog of the neuroanatomy and the stratified anatomy for the 361 acupuncture points of 14 channels. J. Acupunct. Meridian Stud. 6, 270–274. doi:10.1016/j.jams.2013.01.001
Cochrane Training (2020). Collaboration C. Review Manager (RevMan). Version 5.4. 4 ed. The Cochrane Collaboration, 5. Available at: https://training.cochrane.org/system/files/uploads/protected_file/RevMan5.4_user_guide.pdf
Ding, L. F., Ma, J., and Jin, Y. Y. (2019). Clinical observation of combination of massage and behavioral intervention in treating primary nocturnal enuresis in children. Acad. J. Shanghai Univ. Traditional Chin. Med. 33, 46–49. doi:10.16306/j.1008-861x
Feng, J. K., and Zhao, F. (2008). Clinical study of pinching massage on pediatric enuresis. J. Hunan Univ. Chin. Med. 28, 68–69. doi:10.3969/j.issn.1674-070X.2008.03.026
Ferrara, P., Franceschini, G., Bianchi Di Castelbianco, F., Bombace, R., Villani, A., and Corsello, G. (2020). Epidemiology of enuresis: a large number of children at risk of low regard. Ital. J. Pediatr. 46, 128. doi:10.1186/s13052-020-00896-3
Food and Drug Administration (2006). GUIDANCE D. Complementary and alternative medicine products and their regulation by the food and drug administration. US FDA.
Glazener, C. M., and Evans, J. H. (2000). Desmopressin for nocturnal enuresis in children. Cochrane Database Syst. Rev. 2010, Cd002112. doi:10.1002/14651858.CD002112
Glazener, C. M., Evans, J. H., and Cheuk, D. K. (2005). Complementary and miscellaneous interventions for nocturnal enuresis in children. Cochrane Database Syst. Rev., Cd005230. doi:10.1002/14651858.CD005230
Higgins J., Thomas J., Chandler J., Cumpston M., Li T., and Page M. J. (2019). Cochrane handbook for systematic reviews of interventions. Version 6.0.
Kawauchi, A., Tanaka, Y., Naito, Y., Yamao, Y., Ukimura, O., Yoneda, K., et al. (2003). Bladder capacity at the time of enuresis. Urology 61, 1016–1018. doi:10.1016/s0090-4295(02)02515-3
Keten, T., Aslan, Y., Balci, M., Erkan, A., Senel, C., Oguz, U., et al. (2020). Comparison of the efficacy of desmopressin fast-melting formulation and enuretic alarm in the treatment of monosymptomatic nocturnal enuresis. J. Pediatr. Urol. 16, e1–e645. doi:10.1016/j.jpurol.2020.07.018
Kuoch, K. L., Hebbard, G. S., O’Connell, H. E., Austin, D. W., and Knowles, S. R. (2019). Urinary and faecal incontinence: psychological factors and management recommendations. N. Z. Med. J. 132, 25–33.
Kuwertz-Bröking, E., and von Gontard, A. (2018). Clinical management of nocturnal enuresis. Pediatr. Nephrol. 33, 1145–1154. doi:10.1007/s00467-017-3778-1
Kwan, R. Y., Leung, M. C., and Lai, C. K. (2014). Acupressure for agitation in nursing home residents with dementia: study protocol for a randomized controlled trial. Trials 15, 410. doi:10.1186/1745-6215-15-410
Li, P. J. (2023). Clinical observation on the efficacy of Tongdu Tuina manipulation in the treatment of primary enuresis in children. Open Med. (Wars) 18, 20230712. doi:10.1515/med-2023-0712
Lu, D. Y., Gu, T. T., and Wen, J. H. (2023). The clinical impact of combining tuina with behavioral intervention for treating primary nocturnal enuresis in children. Shenzhen J. Integr. Traditional Chin. West. Med. 33, 54–57. doi:10.16458/j.cnki.1007-0893.2023.18.016
Luo, M., and Yi, X. (2019). Effect of massage combined with desmopressin acetate in treating pediatric primary enuresis and its effect on serum vasopressin levels. Mod. J. Integr. Traditional Chin. West. Med. 28, 1547–1550. doi:10.3969/j.issn.1008-8849.2019.14.017
Mehta, P., Dhapte, V., Kadam, S., and Dhapte, V. (2017). Contemporary acupressure therapy: adroit cure for painless recovery of therapeutic ailments. J. Tradit. Complement. Med. 7, 251–263. doi:10.1016/j.jtcme.2016.06.004
Radmayr, C., Schlager, A., Studen, M., and Bartsch, G. (2001). Prospective randomized trial using laser acupuncture versus desmopressin in the treatment of nocturnal enuresis. Eur. Urol. 40, 201–205. doi:10.1159/000049773
Su, D., and Li, L. (2011). Trends in the use of complementary and alternative medicine in the United States: 2002-2007. J. Health Care Poor Underserved 22, 296–310. doi:10.1353/hpu.2011.0002
Su, K., Wang, Y., Zhou, X., and Huang, R. (2013). Clinical observation of the short-term and long-term efficacy of Tuina in the treatment of primary enuresis in children. Inn. Mong. Tradit. Chin. Med. 32, 86–87. doi:10.3969/j.issn.1006-0979.2013.09.088
Tong, C., He, Q., Ho, M., Zhong, Z., Wu, Q., and Chen, M. (2022). Tuina for enuresis in children: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health 10, 821781. doi:10.3389/fpubh.2022.821781
Wan, Z. Y., Du, K., and Li, C., (2018). Guideline for TCM pediatrics clinical diagnosis and treatment·infantile enuresis (amendment). J. Pediatr. Traditional Chin. Med. 14 (1), 4–8. doi:10.16840/j.issn1673-4297.2018.01.02
Wen, D. M., and Sun, Y. N. (2022). A clinical study on treating monosymptomatic enuresis in children by massage for warming kidney and strengthening spleen instead of structural withdrawal of desmopressin. Clin. J. Chin. Med. 14, 87–89. doi:10.3969/j.issn.1674-7860.2022.27.022
Yousefichaijan, P., Sharafkhah, M., Salehi, B., and Rafiei, M. (2016). Attention deficit hyperactivity disorder in children with primary monosymptomatic nocturnal enuresis: a case-control study. Saudi J. Kidney Dis. Transpl. 27, 73–80. doi:10.4103/1319-2442.174077
Yuksek, M. S., Erdem, A. F., Atalay, C., and Demirel, A. (2003). Acupressure versus oxybutinin in the treatment of enuresis. J. Int. Med. Res. 31, 552–556. doi:10.1177/147323000303100611
Zhang, C., and Zhang, J. (2017). Evaluation of the efficacy of brain and kidney tonifying massage in the treatment of enuresis in children with kidney qi insufficiency. Clin. Res. Traditional Chin. Med. 9, 73–74. doi:10.3969/j.issn.1674-7860.2017.08.037
Zhang, H., and Chen, F. H. (2019). Effective evaluation on treating infantile enuresis of the Shenqi Buzu type by the Yi’nao Bushen Tuina therapy. J. Sichuan Traditional Chin. Med. 37, 184–187.
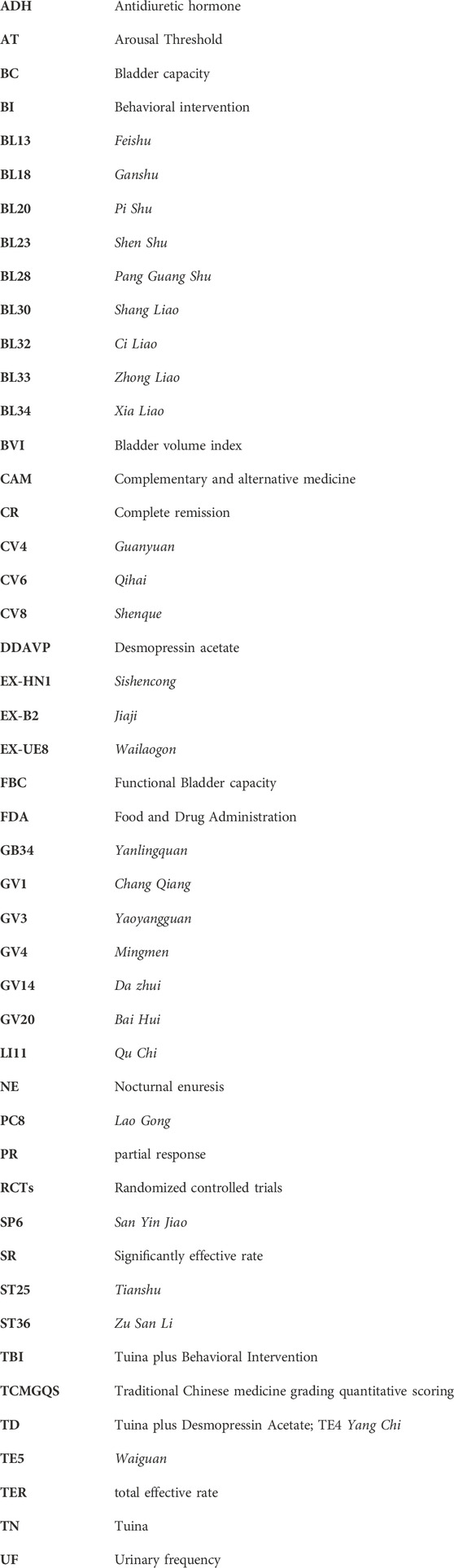
Glossary
Keywords: Tuina, systematic review, desmopressin acetate, behavioral interventions, single-symptom nocturnal enuresis
Citation: Chen X, Sun W-j, Wang J-r, Cai Y-y and Yu X-d (2024) A systematic review and meta-analysis assessing the efficacy of Tuina for nocturnal enuresis in children. Front. Pharmacol. 15:1421130. doi: 10.3389/fphar.2024.1421130
Received: 21 April 2024; Accepted: 27 May 2024;
Published: 19 June 2024.
Edited by:
Nannan Shi, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Juanjuan Zheng, Shanghai University of Traditional Chinese Medicine, ChinaYanchun Shan, Qingdao University, China
Copyright © 2024 Chen, Sun, Wang, Cai and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-dan Yu, eGRfeXUyMDAzQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Xin Chen
Xin Chen Wei-jie Sun2†
Wei-jie Sun2† Xiao-dan Yu
Xiao-dan Yu