- 1MEDFIT Karolina Kłoda, Ul. Narutowicza, Szczecin, Poland
- 2Department of Family Medicine, Wroclaw Medical University, Wroclaw, Poland
- 3Polish Society of Family Medicine, Ul. Syrokomli, Wroclaw, Poland
- 4Institute of Healthcare Management, Lazarski University, Warsaw, Poland
- 5Faculty of Health Science, Institute of Public Health, Jagiellonian University Medical College, Cracow, Poland
Introduction: In Poland, the area of self-medication requires scientific and organizational evaluation. So far, no solutions sanctioning self-medication have been introduced. Therefore, the aim of this study was to recognize and analyze the practical experience of outpatient physicians regarding self-medication of their patients, as well as self-medication of children by their caregivers.
Methods: This study enrolled 386 participants and used a Computer-Assisted Web Interview that was disseminated online from 4th of July 2023 to 23rd of August 2023. The survey was addressed to outpatient healthcare physicians working in Poland.
Results: In doctors’ perspective the main three reasons for choosing self-medication in Poland were: taking advice from other people - family members or friends (59.1%), finding information regarding treatment online (52.9%) and ability to self-medicate in this kind of symptoms/disease (51.6%). Among adult patients, in 72.1% of cases, an independent decision to start antibiotic therapy was made. Such a decision occurred in 39.8% of pediatric patients. Children caregivers were more likely to visit the physician immediately with symptoms than in the case of adult patients (42.2% vs. 22.1%, p < 0.001).
Conclusions: Self-medication in Poland requires educational and organizational support at various levels - both social (information campaigns, school education), the healthcare system (increasing the role of medical professionals, including pharmacists), and finally in the area of legislation. Two areas seem to be particularly alarming - the use of antibiotics by adults and children and the mental health of both populations.
Introduction
According to the WHO definition, self-medication includes the use of medical products by a patient to treat a disease or symptoms, or the self-administration of chronic medications prescribed by a doctor. It also includes self-recognition of the disease or symptoms, which the patient plans to treat. Responsible self-medication involves the use of over-the-counter (OTC) medications according to the label or the use of medications prescribed by a doctor. Irresponsible self-medication means incorrect use of the OTC medications, using expired or prescribed for other purposes medications, or sharing medications with others (WHO, 2000; Shehnaz et al., 2014; Ghodkhande et al., 2023).
Due to the healthcare systems overload during the COVID-19 pandemic, recommendations of social distancing and fear of infection, self-medication has become more common in many countries. According to the research conducted during the pandemic, the frequency of self-medication worldwide was nearly 45% and factors conducive to this behavior were recognized. The incidence was gender-related and increased with age. The most commonly purchased OTC medications were painkillers, vitamins and dietary supplements, anti-allergy drugs and cold and cough medicines (Shrestha et al., 2022). In the case of Poland, the frequency of de novo self-medication has increased (Makowska et al., 2020). The readiness to act on your own, was also high, long before the pandemic. A study from 2009 including data from 50 countries, found that 95% of respondents were open to the possibility of self-medication in minor diseases (The Nielsen Company, 2009; Stosic et al., 2011). Research conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA) in the United States has shown that approximately three million people aged 12 and older have misused OTC medications at least once in their lives (Gonzales et al., 2011; Marathe et al., 2020).
Self-medication carries high risks, such as non intentional misuse or abuse of medications resulting from lack of knowledge. Moreover, the use of some drugs before medical consultation may mask the symptoms allowing obtaining the diagnosis. Especially that patients tend to not inform the physician about the medications they have taken, presenting sometimes new symptoms that can be linked with inappropriate self-medication. Another threat is that patients who take medications long-term because of chronic diseases are at risk of interactions with substances used in self-medication. And finally, drugs that have already been prescribed to a patient may not be properly stored until they are used again, which may result in a decrease or lack of their effect (Ruiz, 2010). These risks drive new research questions and scientific solutions. Recent studies focus on responsible self-medication with medical professional counseling in order to improve clinical effects and unburden healthcare systems. The role of the advising person can be performed by a physician, but by other healthcare workers (Rutter, 2015). The involvement of pharmacists could allow them to conduct consults and solve minor health problems of the patient in the pharmacy. Such an approach would be possible through following an appropriate algorithm, and then proposing treatment using OTC medications or explaining the administration of prescription drugs. However, such a solution needs educational and financial reinforcement (Alexa and Bertsche, 2023).
In Poland, the area of self-medication requires scientific and organizational evaluation. Until now there has been no reliable data on the prevalence of self-medication. So far, no solutions sanctioning self-medication have been introduced, especially supported by the advice of a medical professional. Thus, there are no specific sites, like community pharmacies where an individual can receive an appropriate self-medication consult. We hypothesized that outpatient care (in particular primary healthcare - PHC) physicians are asked to support self-medication or to treat its negative effects and are able to indicate the patterns of their patients’ behavior. Family doctors and other PHC physicians in Poland are the first line medical proffesionnals accessible even on the same day of submitting a request for a consultation. Therefore, the aim of this study was to recognize and analyze the practical experience of outpatient physicians regarding self-medication of their patients, as well as self-medication of children by their caregivers.
Materials and methods
The study was conducted by the Scientific Section of the Polish Society of Family Medicine together with the Institute of Healthcare Management at the Lazarski University. The research tasks discussed in this paper are part of the Self-medication Report, which is currently being developed. This study used a Computer-Assisted Web Interview (CAWI) that was disseminated online from 4th of July 2023 to 23rd of August 2023. The survey was addressed to doctors working in Poland. The survey was distributed via the social networking site Facebook.com within closed groups to which only doctors have access after verification of their professional medical license number. In addition, the mailing database of the Polish Society of Family Medicine was used. Before completing the form, participants were given the information regarding research objectives and methodology and were required to provide informed consent to access the questionnaire. Respondents could discontinue their participation at any time, without explanation. No personal information such as email addresses were collected to ensure anonymity.
Inclusion criteria for the study were: giving informed consent to participate in the study and being a outpatient physician. Failure to meet both criteria meant that no further participation in the study was possible.
A self-administered questionnaire was developed for the project, which consisted of closed-ended single- and multiple-answer questions. The first part of the questionnaire, which was a demographic interview, consisted of questions assessing socio-economic status, including age and gender. This was followed by questions assessing professional status, including career stage, length of service, main place of work (primary care, specialist clinic and hospital) and location of workplace. The main part of the survey consisted of interview regarding their personal experience with patients’ self-medication in both the children and the adults. The last part questioned for doctors’ opinions on self-medication and it is side effects management.
Assessment of physicians’ personal experience included indication from among the examples listed, in which situations their patients used self-medication. Possible answers included: headache, sore throat and pharyngitis, muscular-articular pain, cough, rhinitis, migraine, abdominal pain, back pain, digestive disorders (indigestion, diarrhea, constipation), menstrual pain, urinary tract infection, allergy, mental health disorders and other than those listed. Doctors were then asked to indicate how long, in their experience, patients use self-medication before they decide to consult a doctor, taking into account the time period: less than 3 days, 3–7 days, 7–14 days, 14 days to a month and more than a month. Then, for headache, respiratory tract infections (cough, rhinitis, pharyngitis), mental health problems, abdominal pain and urinary tract infections, doctors were asked to indicate the self-medication methods used by their patients from among the possible answers: home remedies, use of OTC medications, use of drugs previously prescribed by a doctor for similar complaints, staying at home and resting, waiting for symptoms to resolve on their own, implementing antibiotic therapy on their own, seeing a doctor immediately, other than those listed (multiple-answer question). Separate questions were developed for adult and pediatric patients.
In the final stage of the survey, respondents were asked to indicate potential reasons for self-medication of patients and to state whether they had encountered adverse effects following this behavior of their patients.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Bioethics Committee at Lazarski University (approval number: 04/06/23). The study, guided by the principle in scientific research to do no harm, gave the participants control over disclosure. Informed consent for research participation was obtained from all participants.
Statistical analysis
The modified formula of Daniel and Cochran was used to calculate the minimum number of participants, for the total number of subjects, that is, 43130 primary care physicians, maintaining a 95% confidence interval (α = 0.95), a fraction size of 0.5 (unknown a priori response rate) (p = 0.5) and a maximum error of 5% (d = 0.05), the number of subjects could not be less than 381 (Windak et al., 2019).
The variables taken into the analysis had qualitative and quantitative character. The Shapiro-Wilk Test was used to assess the normality of the distribution. For qualitative variables, results were presented as %. For quantitative variables, basic descriptive statistics were presented. The Chi square test was used to assess statistical significance between quantitative variables. A p-value <0.05 was assumed to be statistically significant. The analysis was carried out using Statistica 13.0 by StatSoft.
Results
Characteristics of the study group
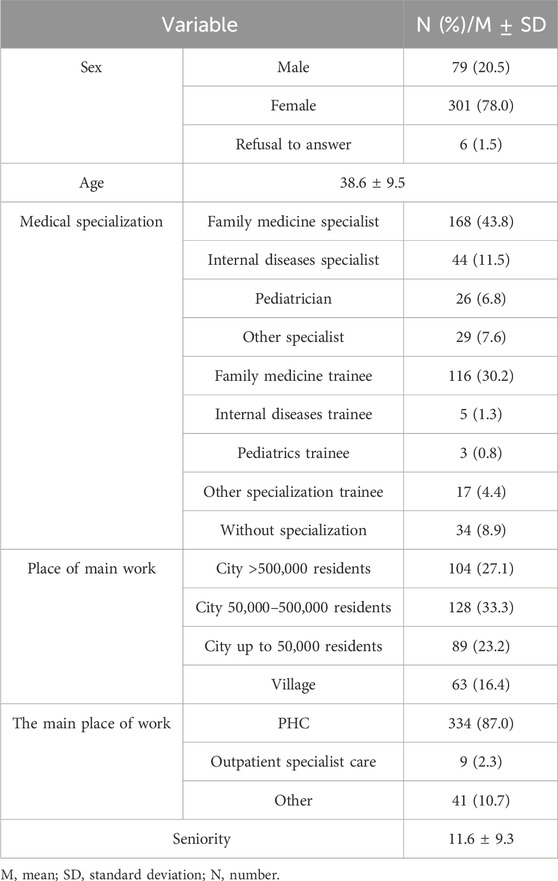
The study enrolled 386 physicians working in Poland, with an average age of 38.6 ± 9.5 years. Among the surveyed doctors, 87% work in PHC, 43.8% of the respondents hold the title of specialist in family medicine, and 30.2% are in the course of this specialization. The average seniority was 11.6 ± 9.3 years. A detailed description of the study group is presented in Table 1.
Reasons for medical consultations after self-treatment
Among the analyzed answers, physicians most often indicate that their patients consult them because of the ineffectiveness of self-medication - 38.5%. For 33.3% of the cases, the reason was a greater severity of symptoms and 14.3% of patients did intend to self-medicate but did not know what treatment they should have started. Physicians observed that their patients most often base their knowledge of the treatment on previous medical recommendations - 62.5% and recommendations of family/friends - 59.6%. In 43.2% of cases, doctors declare that their patients gained knowledge from pharmacists. The list of answers is presented in Table 2.
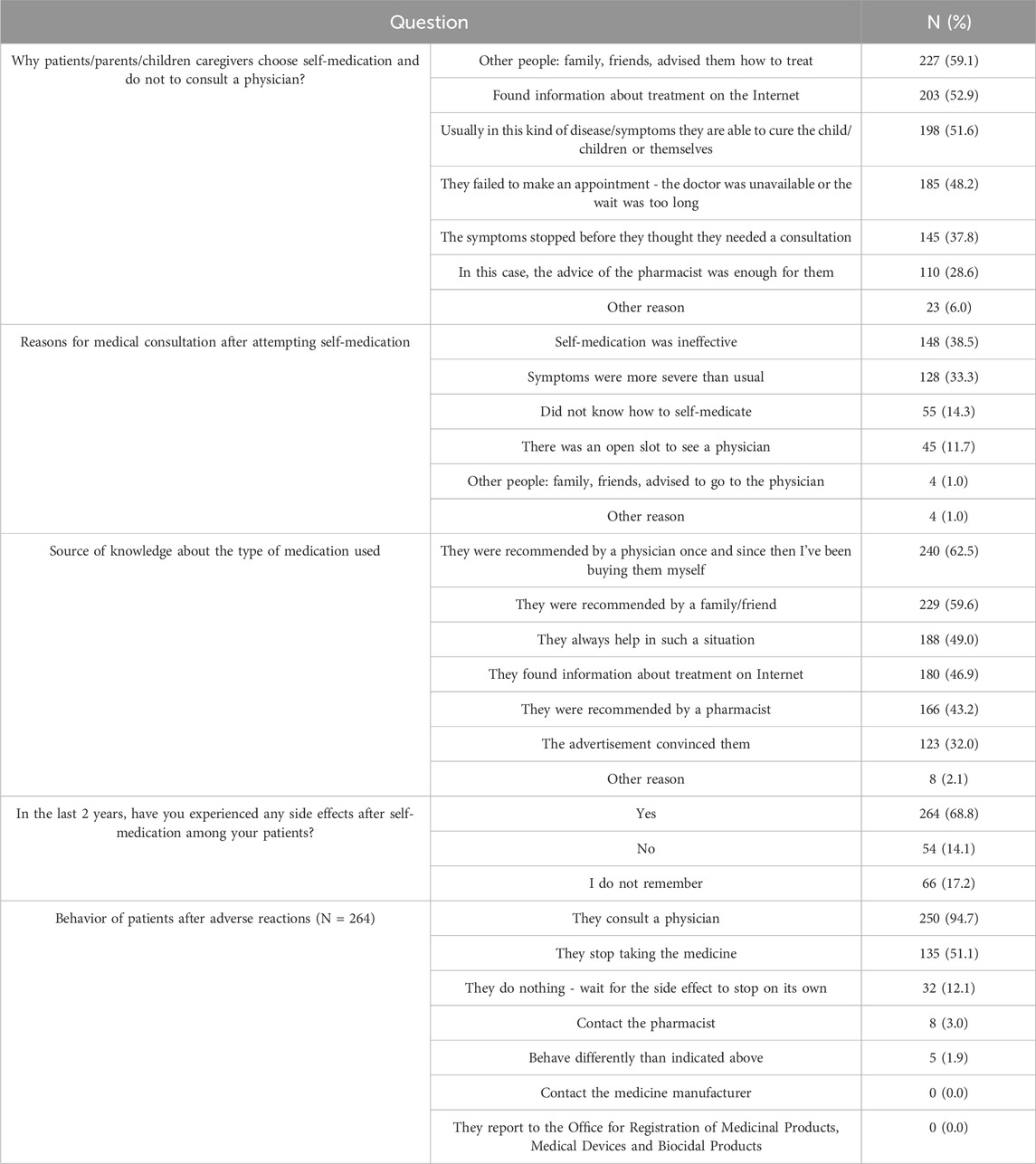
Table 2. List of reasons for medical consultations and sources of knowledge about the recommended treatment among patients.
In addition, 264 (68.8%) physicians report that they have encountered adverse reactions among their patients after self-medication implemented by them. Most often, these patients chose a medical consultation as a solution to their health problem - 94.7%. More than half (51.1%) decided to discontinue the drug, and in 12.1% of cases patients did nothing and waited for spontaneous resolution of symptoms. The results are summarized in Table 2.
Self-medication among adult and pediatric patients
The analysis of questions regarding the reasons for self-medication by the patients showed that they were mostly significantly different in comparison of children and adults. In both groups, the most common cause of self-medication was cough (73.4% vs 88.5%, p < 0.001). Among adults, further causes included sore throat and pharyngitis, back pain, rhinitis and fever. In the case of children, apart from cough, their caregivers significantly more often attempted to self-medicate fever (82.8%), rhinitis (80.7%), abdominal pain (65.9%), and allergies (55.7%). On the other hand, adults more often attempt to self-medicate less specific symptoms, such as headache (54.4% vs. 19.0%, p < 0.001), muscle and joint pain (48.2% vs. 15.1%, p < 0.001) or low mood (15.4% vs. 5.1%, p < 0.001). A detailed list and comparison of the reasons for self-medication are presented in Table 3.
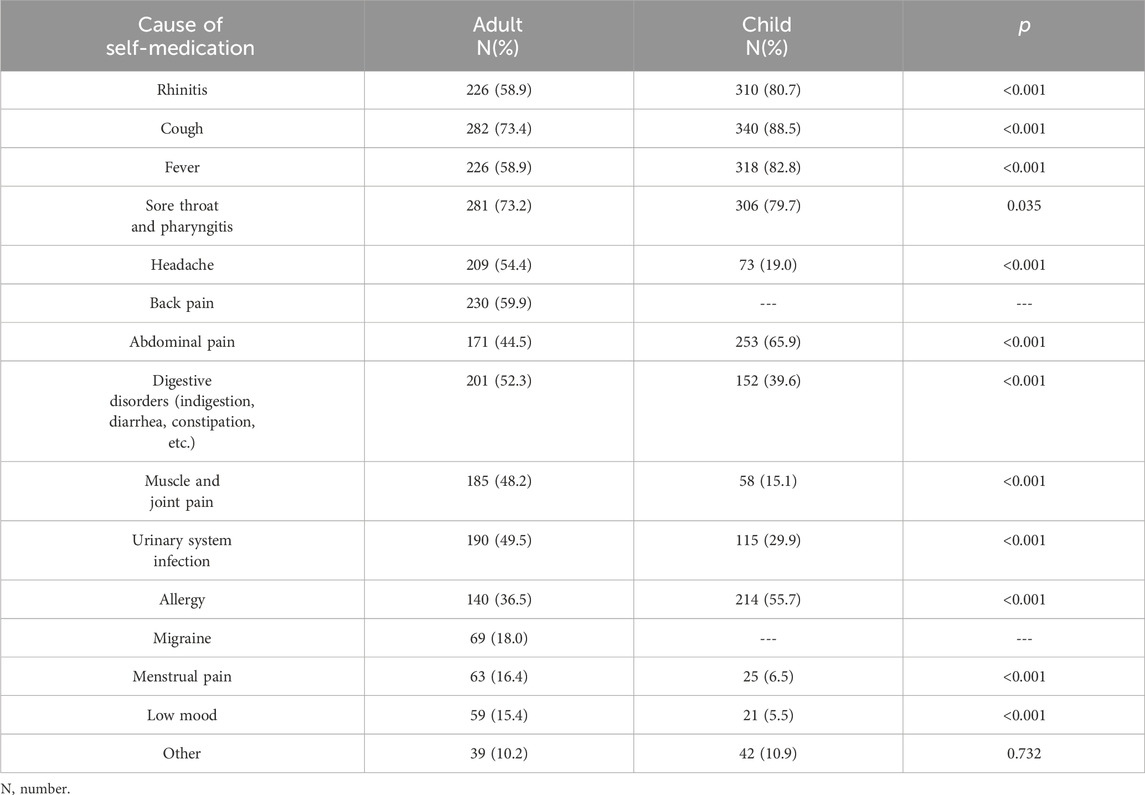
Table 3. Declared reasons for self-medication among patients of physicians in Poland, distinguishing between adult and pediatric patients.
Self-medication methods
When assessing the methods of self-medication, it was shown that in the case of headache, adults and children caregivers alike - most often reached for self-purchased OTC drugs. Moreover, adult patients were more likely to do nothing while waiting for the pain to subside on its own (46.1% vs. 18.5%, p < 0.001). In both cases home remedies were often used. Similarly, for sore throat, cough and rhinitis, self-purchased OTC medications were the most common treatment option for both groups of patients. Among adult patients, in 72.1% of cases, an independent decision to start antibiotic therapy was made. Such a decision occurred in 39.8% of pediatric patients. The surveyed physicians also observed that children caregivers were more likely to visit the physician immediately with symptoms than in the case of adult patients (42.2% vs. 22.1%, p < 0.001). Interestingly mental health disorders occurrence was left without any reaction by 73.2% adults vs. 64.8% of children caregivers (p < 0.0001). Nevertheless, in the case of children, 21.9% of physicians indicate that the caregivers went to the doctor immediately, while such a response was given only for 5.7% of adults. Table 4 presents a detailed list of self-medication methods with the distinction of headache, abdominal pain, symptoms of respiratory tract infection, urinary tract infection and mental health disorders.
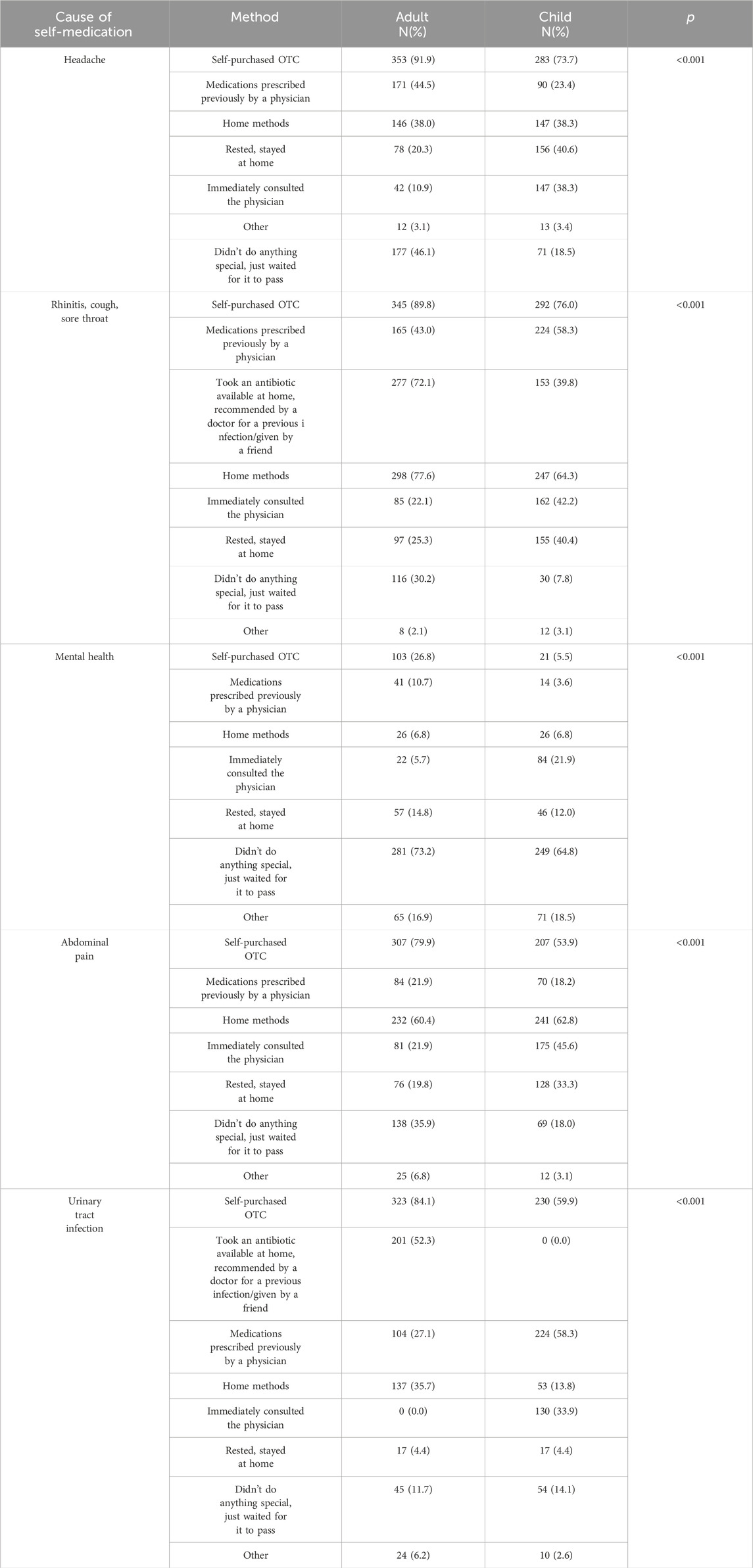
Table 4. Self-medication methods for abdominal pain, symptoms of respiratory tract infections, urinary tract infections and mental health disorders, divided into adult and pediatric patients.
Time between self-medication and medical consultation
In the analysis of the average time that passes from the implementation of self-medication to the visit to the doctor, it was shown that in the case of abdominal pain, headache, urinary tract infection and rhinitis/cough/fever, both for children and adults, visits usually take place within 3 days. In the case of mental health disorders, adult patients most often reported themselves after more than a month, while caregivers with children earlier (p < 0.001). The exact summary and comparison of the visit time from the implementation of self-medication is presented in Table 5.
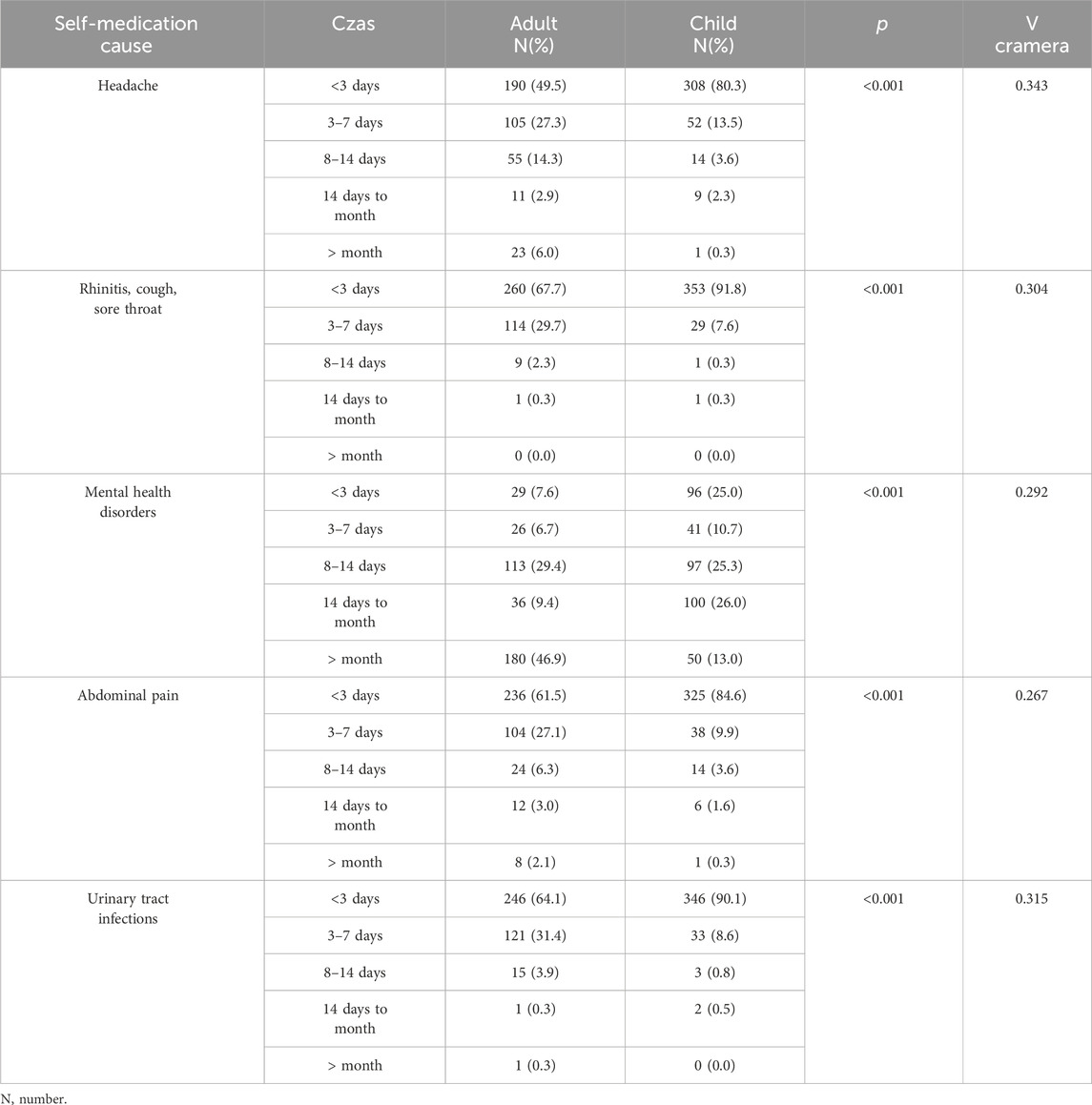
Table 5. Comparison of the time when patients report to the doctor from the self-medication implementation.
Discussion
In our study, we hypothesized that physicians working in outpatient care, deal with self-medication or its negative effects in everyday practice, and are able to indicate the patterns of their patients’ behavior. Thus, we aimed to recognize and analyze the practical experience of outpatient physicians regarding self-medication of their adult and pediatric patients. We have indeed received abundant feedback showing both the causes and the frequencies for self-medication. The main three reasons for choosing self-medication in Poland according to surveyed doctors were: taking advice from other people - family members or friends (59.1%), finding information regarding treatment online (52.9%) and ability to self-medicate in this kind of symptoms/disease (51.6%). Failing to make an appointment with the physician was the fourth most common cause. When asked about the source of knowledge regarding used medication, the most often answers were: physician former recommendation (62.5%), member of family or friend recommendation (59.6%), own experience (49.0%) and finding suitable information online (46.9%). Data from the European Health Interview Survey (2006–2009) including 14 countries have shown that the mean self-medication prevalence in those years was 26.3%, being the highest in Poland (49.4%) (Brandão et al., 2020). The frequency of self-medication in developing countries varies from 60%–80% and is currently estimated for Europe at approximately 68% (Auta et al., 2012; Samuvel Babu et al., 2023). Interesting observations come from comparing our study with a report from India. Similarly to our observations, its authors found that one of the main sources of knowledge for practicing self-medication were the family members (Samuvel Babu et al., 2023).
Self-medication poses serious challenges for doctors. When a patient is commiting a misdiagnosis on the basis of similar symptoms in their family or loved ones, doctors have found it difficult to convince them of the error. Patients usually are convinced of the need for a specific treatment, often found on the Internet, which the doctor does not usually prescribe. In both of these situations, it is important to explain to the patient why the suspected disease or treatment is not appropriate, because despite the error, they will persist in their opinion and will not want to follow the treatment proposed by the doctor. Another danger of self-medication is sharing the medications with family members, which might be even life-threatening (Zanini et al., 2014). Excessive consumption of drugs, especially psychotropic drugs, is also a threat. As studies have shown, people with psychiatric illnesses tend to abuse prescribed drugs and develop addiction (Jeong et al., 2021; Martínez-León et al., 2023).
One of the forms of self-medication is the inappropriate use of antibiotics, which is associated with the administration of the wrong dose or treatment in the wrong time frame (Bi et al., 2023). Overuse of this group of drugs is associated with the emergence of pathogen resistance, especially in countries where there is a greater use of antibiotics. Research shows that about 57% of patients do not know that antibiotics do not affect viruses, therefore 44% are not aware that they are ineffective against cold or flu. Patients overestimate their knowledge of antibiotics, which can have a big impact on self-medication. In Poland, antibiotics are prescription drugs, but there are websites where they can be purchased without the prescription or where you can get a prescription without consulting a doctor. It is also common to use antibiotics prescribed by a doctor in the past, which the patient did not use or did not take the right dose (leftover antibiotics). Physicians also feel pressure from patients to prescribe antibiotics, despite the lack of indications for their use (Machowska and Stålsby Lundborg, 2018). In our study 72.1% of adults and nearly 40% of children caregivers used an antibiotic available at home recommended by a doctor for a previous infection because of the rhinitis, cough or sore throat, which are caused mainly by viral infections. The emerging problem of antibiotics misuse has been noticed especially among children under 3 years of age due to higher consumption of these drugs than in the general population (Alzahrani et al., 2018). A qualitative study from Spain found that antibiotics were misused both, by the children’s caregivers, as well as the physicians. Pediatricians declared that they felt to be forced to prescribe antibiotics as a rapid cure in unjustified circumstances. Parents’ self-medication was related to belief in the curative potential of antibiotics and the possibility of obtaining these drugs from pharmacies without prescription. At the same time physicians misused the antibiotics due to lack of education and the limited application of clinical guidelines (Arnau-Sánchez et al., 2023).
Numerous scientific studies show that increasing value is attached to the role of self-medication in supporting medical staff, which can improve clinical effects and relieve the burden on medical care systems (Dineen-Griffin et al., 2019). The role of the person educating the patient may be undertaken by a doctor, but also by other members of the medical staff (Ge et al., 2022). The introduction of pharmaceutical care in Poland opens the possibility of pharmaceutical consultations, and thus to solving minor health problems of the patient in the pharmacy. This would be possible thanks to the Minor Ailments Program, in which a pharmacist recognizes the disease, follows an appropriate treatment algorithm, and then offers the patient treatment with OTC or prescription drugs (Report, 2020).
Summary
To sum up, the aim of this study was to recognize and analyze the practical experience of outpatient physicians regarding self-medication of their patients, as well as self-medication of children by their caregivers. This experience of outpatient physicians indicates that patients undertake self-treatment as a result of advice from family members or friends, relying on information regarding online treatment, and the patient’s own experience, which draws attention to the need for educational and organizational support for patients. According to doctors, the main sources of knowledge for patients when choosing drugs used in self-medication are physicians first, then family members or friends, their own experiences and information available online, which indicates the important role of a professional with medical education when deciding on the use of a drug. Further research is needed to assess whether the differences in antibiotics uptake may result from the awareness of the need to assess the indications for antibiotic therapy and the potential risks arising from the use of antibiotics, or from adults relying on their experience with the use of these drugs. The professional experience of doctors shows that patients are insufficiently involved in the area of mental health. Most often, the lack of independent reaction on the part of patients and children’s caregivers to the deterioration of their mental condition was observed. Although in the case of children, almost 22% of doctors indicate that caregivers immediately consulted a doctor, for adults this percentage was only 5.7%. Side effects after self-medication are a common phenomenon observed in medical practice, and medical consultation is the most common form of seeking a solution to the problem by patients. Pharmacists were indicated as an important source of knowledge about the medicine used - according to doctors’ declarations, 43.2% of patients took advantage of such advice, which is an argument for increasing the role of pharmaceutical care within the Polish healthcare system.
The authors are aware of the limitations of this study, which undoubtedly include the methodology of collecting data using an online questionnaire. Nevertheless, CAWI-type tests are currently widely used in science. Firstly, they provide the opportunity to reach a wide group of recipients, increasing the scope of the research. Secondly, numerous studies have shown that people participating in anonymous Internet research have a greater predisposition to tell the truth and show lower levels of stress (Milton et al., 2017). Another limitation of the study is the lack of representativeness of the study group among all doctors in Poland, therefore it is necessary to conduct further research on a representative sample of doctors.
Conclusions
Self-medication in Poland requires educational and organizational support at various levels - both social (information campaigns, school education), the healthcare system (increasing the role of medical professionals, including pharmacists), and finally in the area of legislation. Two areas seem to be particularly alarming - the use of antibiotics by adults and children and the mental health of both populations. We recommend cooperation between scientific societies like Polish Society of Family Medicine and government entities to develop educational programs which will be an integral part of national and European health strategy. Allocation of financial resources for research on the effectiveness of various forms of self-treatment is strongly needed. As well as establishing cross-sectoral cooperation to promote self-medication as an element of public health.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
KK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing–original draft, Writing–review and editing. MB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Writing–original draft. AB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing–original draft. MG-S: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Validation, Writing–review and editing. IK-B: Conceptualization, Methodology, Supervision, Writing–review and editing. AM-M: Supervision, Validation, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1413811/full#supplementary-material
References
Alexa, J. M., and Bertsche, T. (2023). An online cross-sectional survey of community pharmacists to assess information needs for evidence-based self-medication counselling. Int. J. Clin. Pharm. 2, 1452–1463. Epub ahead of print. PMID: 37532842. doi:10.1007/s11096-023-01624-7
Alzahrani, M. S., Maneno, M. K., Daftary, M. N., Wingate, L., and Ettienne, E. B. (2018). Factors associated with prescribing broad-spectrum antibiotics for children with upper respiratory tract infections in ambulatory care settings. Clin. Med. Insights Pediatr. 12, 1179556518784300. doi:10.1177/1179556518784300
Arnau-Sánchez, J., Jiménez-Guillén, C., Alcaraz-Quiñonero, M., Vigueras-Abellán, J. J., Garnica-Martínez, B., Soriano-Ibarra, J. F., et al. (2023). Factors influencing inappropriate use of antibiotics in infants under 3 Years of age in primary care: a qualitative study of the paediatricians' perceptions. Antibiot. (Basel) 12 (4), 727. PMID: 37107089; PMCID: PMC10135072. doi:10.3390/antibiotics12040727
Auta, A., Omale, S., Folorunsho, T. J., David, S., and Banwat, S. B. (2012). Medicine vendors: self-medication practices and medicine knowledge. N. Am. J. Med. Sci. 4, 24–28. doi:10.4103/1947-2714.92899
Bi, B., Qin, J., Zhang, L., Lin, C., Li, S., and Zhang, Y. (2023). Systematic review and meta-analysis of factors influencing self-medication in children. Inquiry 60, 469580231159744. PMID: 36998210; PMCID: PMC10069002. doi:10.1177/00469580231159744
Brandão, G. R., Teixeira, L., Araújo, L., Paúl, C., and Ribeiro, O. (2020). Self-medication in older European adults: prevalence and predictive factors. Arch. Gerontol. Geriatr. 91, 104189. Epub ahead of print. PMID: 32717589. doi:10.1016/j.archger.2020.104189
Dineen-Griffin, S., Garcia-Cardenas, V., Williams, K., and Benrimoj, S. I. (2019). Helping patients help themselves: a systematic review of self-management support strategies in primary health care practice. PLoS One 14 (8), e0220116. PMID: 31369582; PMCID: PMC6675068. doi:10.1371/journal.pone.0220116
Ge, P., Liu, S. T., Xu, S. X., Zhang, J. Z., Lai, Y. J., Fu, R. C., et al. (2022). The influence of parents on medication adherence of their children in China: a cross-sectional online investigation based on health belief model. Front. Public Health 10, 845032. PMID: 35493366; PMCID: PMC9046660. doi:10.3389/fpubh.2022.845032
Ghodkhande, K. P., Choudhari, S. G., and Gaidhane, A. (2023). Self-medication practices among the geriatric population: a systematic literature review. Cureus 21 (7), e42282. PMID: 37609089; PMCID: PMC10440492. doi:10.7759/cureus.42282
Gonzales, R., Brecht, M. L., Mooney, L., and Rawson, R. A. (2011). Prescription and over-the-counter drug treatment admissions to the California public treatment system. J. Subst. Abuse Treat. 40, 224–229. doi:10.1016/j.jsat.2010.11.003
Jeong, H. J., Suh, H., Lee, Y. M., Kyung Park, H., Kim, H. J., Pak, K., et al. (2021). Association of temporolimbic volumes with treatment response to antipsychotic medication for delusion in patients with alzheimer's disease. Alpha Psychiatry 22 (5), 244–249. PMID: 36447443; PMCID: PMC9685667. doi:10.1530/alphapsychiatry.2021.21157
Machowska, A., and Stålsby Lundborg, C. (2018). Drivers of irrational use of antibiotics in Europe. Int. J. Environ. Res. Public Health 16 (1), 27. PMID: 30583571; PMCID: PMC6338985. doi:10.3390/ijerph16010027
Makowska, M., Boguszewki, R., Nowakowski, M., and Podkowińska, M. (2020). Self-medication-related behaviors and Poland's COVID-19 lockdown. Int. J. Environ. Res. Public Health 17 (22), 8344. PMID: 33187315; PMCID: PMC7696561. doi:10.3390/ijerph17228344
Marathe, P. A., Kamat, S. K., Tripathi, R. K., Raut, S. B., and Khatri, N. P. (2020). Over-the-counter medicines: global perspective and Indian scenario. J. Postgrad. Med. 66 (1), 28–34. PMID: 31898596; PMCID: PMC6970327. doi:10.4103/jpgm.JPGM_381_19
Martínez-León, M. A., Carballo, J. L., and Pérez-Jover, V. (2023). Prevalence and risk factors for misuse of prescription psychotropic drug in patients with severe mental illness: a systematic review. Actas Esp. Psiquiatr. 51 (5), 229–240. Epub 2023 Sep 1. PMID: 38117263; PMCID: PMC10803847.
Milton, A. C., Ellis, L. A., Davenport, T. A., Burns, J. M., and Hickie, I. B. (2017). Comparison of self-reported telephone interviewing and web-based survey responses: findings from the second Australian young and well national survey. JMIR Ment. Health 4 (3), e37. PMID: 28951382; PMCID: PMC5635234. doi:10.2196/mental.8222
Report (2020). Report on the work of the team for pharmaceutical care appointed by the Minister of Health pursuant to the order of July 8, 2020. Off. J. Minist. Health July 9, 2020, Wars. [Raport z prac zespołu ds. opieki farmaceutycznej powołanego przez Ministra Zdrowia na podstawie zarządzenia z dnia 8 lipca 2020 r. (Dziennik Urzędowy Ministra Zdrowia z dnia 9 lipca 2020 r., Warszawa)].
Ruiz, M. E. (2010). Risks of self-medication practices. Curr. Drug Saf. 5 (4), 315–323. PMID: 20615179. doi:10.2174/157488610792245966
Rutter, P. (2015). Role of community pharmacists in patients’ self-care and self-medication. Integr. Pharm. Res. Pract. 4, 57–65. doi:10.2147/IPRP.S70403
Samuvel Babu, P., Balu, V., Uma Maheswari, B., K, M. C., K, E. P., and Dkhar, E. (2023). A comparative study to assess the prevalence, knowledge of impact, and practice of self-medication among adults in urban and rural communities in Bangalore. Cureus 15 (5), e39672. PMID: 37398726; PMCID: PMC10308061. doi:10.7759/cureus.39672
Shehnaz, S. I., Agarwal, A. K., and Khan, N. (2014). A systematic review of self-medication practices among adolescents. J. Adolesc. Health 55 (4), 467–483. PMID: 25245937. doi:10.1016/j.jadohealth.2014.07.001
Shrestha, A. B., Aryal, M., Magar, J. R., Shrestha, S., Hossainy, L., and Rimti, F. H. (2022). The scenario of self-medication practices during the Covid-19 pandemic; a systematic review. Ann. Med. Surg. (Lond). 82, 104482. Epub 2022 Aug 27. PMID: 36059596; PMCID: PMC9419440. doi:10.1016/j.amsu.2022.104482
Stosic, R., Dunagan, F., Palmer, H., Fowler, T., and Adams, I. (2011). Responsible self-medication: perceived risks and benefits of over-the-counter analgesic use. Int. J. Pharm. Pract. 19 (4), 236–245. Epub 2011 Mar 21. PMID: 21733011. doi:10.1111/j.2042-7174.2011.00097.x
The Nielsen Company (2009). The changing landscape: a multi-country study undertaken for AESGP. Available at: https://www.selfcareforum.org/wp-content/uploads/2011/07/AESGPResearchJun09.pdf (access August 27, 2023).
WHO (2000). Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva, Switzerland: WHO.
Windak, A., Niżankowski, R., and Lukas, W. (2019). Raport „Podstawowa opieka zdrowotna w Polsce - diagnoza i projekty zmian.
Keywords: family medicine, GP, OTC, primary care, self-medication
Citation: Kłoda K, Babicki M, Biesiada A, Gałązka-Sobotka M, Kowalska-Bobko I and Mastalerz-Migas A (2024) Self-medication of adults and children in Poland - results from outpatient health care physicians online questionnaire. Front. Pharmacol. 15:1413811. doi: 10.3389/fphar.2024.1413811
Received: 17 April 2024; Accepted: 24 July 2024;
Published: 13 August 2024.
Edited by:
Catherine M. T. Sherwin, University of Western Australia, AustraliaCopyright © 2024 Kłoda, Babicki, Biesiada, Gałązka-Sobotka, Kowalska-Bobko and Mastalerz-Migas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Iwona Kowalska-Bobko, aXcua293YWxza2FAdWouZWR1LnBs
 Karolina Kłoda1
Karolina Kłoda1 Mateusz Babicki
Mateusz Babicki Iwona Kowalska-Bobko
Iwona Kowalska-Bobko