- 1Department of Nephrology, Jieyang People’s Hospital, Jieyang, China
- 2Department of Nephrology, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 3NHC Key Laboratory of Clinical Nephrology (Sun Yat-sen University) and Guangdong Provincial Key Laboratory of Nephrology, Guangzhou, China
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) has been traditionally treated using glucocorticoids and immunosuppressants. However, these treatment modes are associated with high recurrence AAV rates and adverse reactions. Therefore, treatment strategies for AAV need to be urgently optimized. The efficacy and safety of biological agents in the treatment of vasculitis have been clinically validated. This review comprehensively summarizes the evidence-based support for the clinical use of existing biological agents in AAV. The findings reveal that multiple biological agents not only effectively reduce the adverse reactions associated with glucocorticoids and immunosuppressants but also demonstrate significant therapeutic efficacy. Notably, rituximab, an anti-CD20 antibody, has emerged as a first-line treatment option for AAV. Mepolizumab has shown promising results in relapsed and refractory eosinophilic granulomatosis with polyangiitis. Other biological agents targeting cytokines, complement, and other pathways have also demonstrated clinical benefits in recent studies. The widespread application of biological agents provides new insights into the treatment of AAV and is expected to drive further clinical research. These advancements not only improve patient outcomes but also offer more possibilities and hope in the field of AAV treatment.
1 Introduction
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a group of systemic diseases, which are characterized by the ANCA-mediated inflammation and necrosis of small blood vessel walls. The clinical types of AAV include microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), and eosinophilic granulomatosis with polyangiitis (EGPA). Proteinase 3 (PR3)-ANCA and myeloperoxidase (MPO)-ANCA are the two main ANCA antigens, which are found in the cytoplasm of neutrophils. PR3-ANCA is usually associated with GPA, whereas MPO-ANCA is primarily found in the context of MPA (Bossuyt et al., 2017). AAV can occur in all age groups, with a peak incidence in individuals aged 50–60 years. The annual incidence of AAV is reported to be 1.2–2.0 cases per 100,000 people, while its prevalence is 4.6–18.4 cases per 100,000 people (Watts et al., 2015). AVV is traditionally treated with immunosuppressive agents such as glucocorticoids and cyclophosphamide (CYC). However, long-term use of these agents can lead to various treatment-related complications. For instance, glucocorticoid use may cause infections (Cutolo et al., 2008), osteoporosis (Chotiyarnwong and McCloskey, 2020), impaired glucose tolerance (Hwang and Weiss, 2014), and other side effects. Meanwhile, the metabolites of CYC induce bladder and reproductive organ toxicity, which may lead to complications such as the formation of malignant tumors (Rahmattulla et al., 2015) and infertility (Feng et al., 1972) in the long term. Although immunotherapy has somewhat improved the outcomes of patients with AAV, disease recurrence is still very common. Indeed, 30%–50% of AAV patients relapse within 5 years of disease onset, usually within 12–18 months after stopping immunosuppressant therapy (Geetha and Jefferson, 2020). Therefore, treatment strategies for AAV need to be urgently optimized. Biological agents (biologics) target pathogenic mechanisms with a high degree of specificity to rapidly relieve symptoms, lower relapse rates, permit a reduction of corticosteroid dosage, and improve AAV patient quality of life. To date, numerous biologics have shown promise in the treatment of AAV; this review summarizes their clinical applications.
2 Biologics
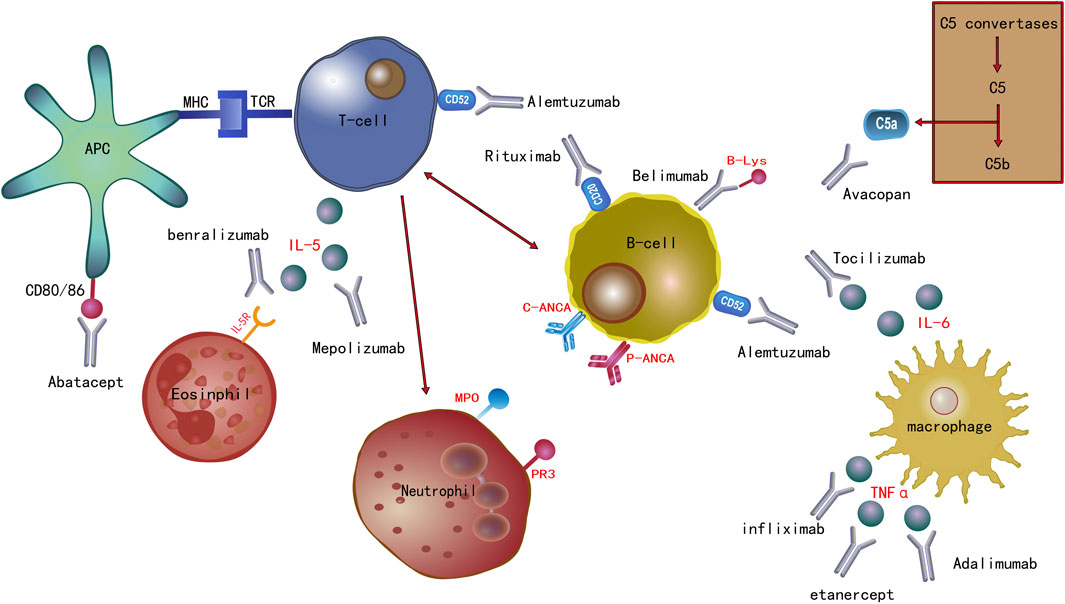
In this section of the review, we have visually presented the target sites of the current biological agents used in the treatment of AAV through illustrative images. Furthermore, we have also delved into the progress of the clinical application of these medications. (Figure 1).
Biological agents currently used in the treatment of anti-neutrophil cytoplasmic antibody-associated vasculitis and their associated molecular targets. Rituximab is an anti-CD20 antibody. Alemtuzumab is an anti-CD52 antibody. Abatacept targets CD80/86. Infliximab, etanercept, and adalimumab target the cytokine tumor necrosis factor (TNF)-α. Interleukin (IL)-6 and IL-5 are the targets of tocilizumab and mepolizumab, respectively. Benralizumab targets IL-5R. Avacopan targets complement factor C5a. The B lymphocyte stimulator (B-Lys) is the target of belimumab.
2.1 Anti-CD20 monoclonal antibody
A strong correlation between the presence of ANCA in serum and AAV pathophysiology suggests a pathogenic role for humoral immunity in AAV (Wilde et al., 2011). CD20 is a protein present on the surface of mature B cells, which supports the strategy of using anti-CD20 antibodies to treat AAV patients.
Rituximab (RTX) is an anti-CD20 IgG1 chimeric mouse/human monoclonal antibody, which was approved by the US Food and Drug Administration (FDA) in 2011 for the treatment of AAV. Its efficacy has been fully affirmed. A UK-based 2020 expert consensus (Tieu et al., 2020) recommended the prolonged use of RTX (i.e., 500 mg or 1,000 mg every 6 months for 2 years) to maintain AAV remission. If the risk of recurrence remained high after 2 years of maintenance therapy, it is recommended that the treatment period is extended to 5 years. Discontinuation of disease-modifying anti-rheumatic drugs is recommended after RTX initiation, whereas hormonal reduction should be completely discontinued within 6–12 months. The 2021 Kidney Disease Improving Global Outcomes (KDIGO) guidelines (Kidney Disease: Improving Global Outcomes KDIGO Glomerular Diseases Work Group, 2021) recommend administering glucocorticoids in combination with CYC or RTX as an initial treatment regimen in de novo AAV. For patients with serum creatinine levels > 354 μmol/L, the combination of CYC and glucocorticoids is the first choice induction therapy, although the combination of RTX and CYC can also be considered. For maintenance therapy after induced remission, azathioprine (AZA) or RTX combined with low-dose corticosteroids or RTX alone is recommended. RTX re-induction therapy is preferred for relapsed patients. For patients with refractory diseases, the amount of glucocorticoid can be increased, and RTX or CYC should be included in the regimen. These viewpoints are mainly derived from randomized clinical trials (RCTs) such as RITUXVAS (Jones et al., 2015; 2010a), RAVE (Stone et al., 2010), MAINRITSAN (Guillevin et al., 2014; Charles et al., 2020, 2018; Terrier et al., 2018), RITAZAREM (Gopaluni et al., 2017; Smith et al., 2020, 2023), and will not be discussed further here. The 2022 European League Against Rheumatism (EULAR) guidelines (Hellmich et al., 2024) and the 2023 Pan American League of Associations for Rheumatology (PANLAR) guidelines (Magri et al., 2023) similarly recommend glucocorticoid use in combination with RTX for the induction of remission in patients with new-onset or relapsing GPA or MPA. Moreover, RTX should be indicated for patients with disease recurrence. Over the past 2 years, new insights into AAV treatment have been revealed. In severely ill patients, for instance, there does not appear to be a clear difference between the efficacies of RTX and CYC. A multicenter retrospective study (Morel et al., 2022) involving 153 patients with AAV, who had serum creatinine levels ≥ 350 μmol, assessed the induction of remission with either RTX or CYC combined hormone therapy; however, no significant difference was observed between the efficacies of the two regimens. Studies (Roccatello et al., 2022) by Roccatello et al. have drawn similar conclusions. The most recent real-world study (Ishikawa et al., 2023), which included 687 patients with life-threatening AAV, who presented with rapidly progressive glomerulonephritis and/or alveolar hemorrhage, also suggested that RTX and CYC had similar short-term effects on mortality. Another study (Morel et al., 2022) suggested that compared with RTX, CYC-assisted plasmapheresis had a higher dialysis-free rate at 12 months. Meanwhile, RTX use may be associated with a lower risk of fungal infection and pneumocystis pneumonia, but a higher risk of short-term renal function deterioration, which may require hemodialysis maintenance (Ishikawa et al., 2023). In a retrospective study (Sorin et al., 2022) involving 17 patients with refractory GPA treated with the RTX/methotrexate (MTX) combination, 94% achieved overall remission, indicating that this combination can be used as a salvage therapy with an acceptable safety profile. The MAINRITSAN trial (Delestre et al., 2023) compared the outcomes of 277 AAV patients who were treated with AZA or an 18-month regimen of tailored RTX. During treatment, 500 mg RTX was reinfused based on testing every 3 months if peripheral CD19+ B cells or ANCA reappeared or ANCA titers increased. The results showed that the 84-month response rate was higher in the group receiving the 18-month fixed RTX regimen (500 mg of RTX at days 0 and 14 and at months 6, 12, and 18) than in the one undergoing AZA treatment. In addition, extending RTX treatment to 36 months did not reduce the long-term AAV recurrence rate compared with that of the group receiving the 18-month fixed RTX regimen. A multicenter retrospective study (Machet et al., 2023), which included 116 patients with AAV, showed that 12% of patients receiving RTX induction therapy were RTX-resistant at 3 months. These patients often have localized disease and rarely receive the initial methylprednisolone pulse and prophylactic trimethoprim-sulfamethoxazole therapy. The LoVAS study (Furuta et al., 2021; Furuta et al., 2023), which included 134 patients with non-severe AAV, compared the performance of RTX combined with low-dose or high-dose glucocorticoid induction regimens. The results showed that a reduced-dose glucocorticoid plus rituximab regimen was noninferior to a high-dose glucocorticoid plus rituximab regimen. At 24 months of follow-up, the incidence of recurrence, death, and end-stage renal disease were not significantly different between the low-dose and the high-dose glucocorticoid groups. Given that glucocorticoids were discontinued at 5 months in the low-dose glucocorticoid group, these results may imply that the continued administration of low-dose glucocorticoid therapy during remission maintenance with RTX is not necessary to prevent relapse in patients with AAV.
In terms of safety assessment, both the KDIGO guidelines (, 2024) and multiple authoritative studies (Jones et al., 2010a; Stone et al., 2010; Gérard et al., 2023) have indicated that the incidence of infections is roughly comparable between RTX and CYC when used as first-line induction remission therapies. However, there are differing views within the academic community regarding the safety comparison between these two treatment options. A study Jones et al. (2015) by compared the safety of two treatment combinations: RTX induction therapy followed by AZA maintenance therapy (RTX/AZA) and CYC induction therapy followed by AZA maintenance therapy (CYC/AZA). The primary outcomes observed were death, end-stage renal disease, and recurrence at 24 months. The results showed that the incidence rate in the RTX/AZA group was 42%, while that in the CYC/AZA group was 36%, with no significant difference found between the two. Nevertheless, another multicenter real-world study (Thomas et al., 2021) suggested that CYC induction therapy may lead to a higher incidence of severe infections compared to RTX. Additionally, a comprehensive meta-analysis (Vassilopoulos et al., 2023) found that the cumulative incidence of severe infections was significantly higher in the CYC/AZA group compared to the RTX/AZA group during the total follow-up period. It is worth mentioning that the 2023 RAVE study (Odler et al., 2023) provided new evidence. The study included data from 197 patients and showed that the RTX/AZA group had a similar incidence of severe infections compared to the CYC/AZA group. However, it is noteworthy that the onset of infections occurred earlier in the CYC/AZA group, with 82% of severe infections occurring within the first 6 months after the start of the trial. The study also found that a higher baseline CD19+ B-cell count and the use of trimethoprim-sulfamethoxazole for prevention could reduce the risk of severe infections such as Pneumocystis jirovecii. A study (Liu et al., 2023) focusing on Chinese patients with AAV found that low-dose RTX therapy (total dose of 400 mg within 4 weeks) was comparable in efficacy to CYC therapy but significantly reduced the incidence of serious adverse events (SAEs). Similarly, a real-world study (Ishikawa et al., 2024) in Japan suggested that RTX may have a lower risk of fungal infections and Pneumocystis pneumonia compared to CYC in critically ill patients with AAV. It is important to note that hypogammaglobulinemia is commonly observed in AAV patients receiving RTX therapy, which may be related to patient age and cumulative doses of glucocorticoids. This condition may increase the risk of infections, but immunoglobulin replacement therapy can mitigate this risk (Shah et al., 2017; Tieu et al., 2021; Podestà et al., 2023; Smith et al., 2023). During the maintenance therapy phase, the RITAZAREM study (Jones et al., 2010b) found no significant difference in infection rates between the RTX and AZA groups, despite a lower incidence of SAEs in the RTX group. However, a comprehensive meta-analysis (Lee and Song, 2022) comparing the efficacy and safety of various maintenance therapies showed that RTX performed best in reducing recurrence rates, while MMF had the lowest rate of severe infections. Another study (Thomas et al., 2021) indicated that during maintenance therapy, the incidence of severe infections was similar among RTX and other drugs. Additionally, the LoVAS study (Furuta et al., 2023) explored the safety of RTX combined with different doses of glucocorticoids. The results showed that during the 24-month follow-up period, the incidence of SAEs and infections was significantly lower in the low-dose group compared to the high-dose group. Furthermore, the long-term follow-up results of up to 4 years from the RaVeR study (Merkel et al., 2021) confirmed that the safety of long-term RTX treatment for AAV patients is consistent with short-term treatment and comparable to its safety profile in other autoimmune diseases. In conclusion, while RTX and CYC have similar infection rates during the induction phase of remission, RTX may demonstrate a lower risk of infections in certain specific situations. In the maintenance phase, RTX has shown significant efficacy in reducing recurrence rates, and the safety of long-term RTX use has been supported by research. However, clinicians should closely monitor and appropriately manage low gammaglobulinemia and its associated infection risk in patients receiving RTX therapy.
For specific patient populations, the KDIGO guidelines (, 2024) suggest that the use of RTX is superior to CYC for induction therapy in frail elderly patients, although the specific evidence remains unclear. Meta-analyses (Morris et al., 2020) have shown that in patients with AAV aged 75 and older, the use of CYC or RTX for induction therapy is significantly associated with a lower risk of 2-year mortality. Another multicenter retrospective survival analysis (Aqeel et al., 2023) indicates that CYC, CYC + RTX, and RTX alone are equally effective in inducing remission in AAV patients over the age of 60. Compared to treatment regimens containing CYC, the use of RTX alone may reduce the risk of bone marrow suppression. Research by Weiner et al. (2020) has demonstrated that both CYC and RTX therapies can reduce permanent organ damage in elderly patients with AAV. However, the use of higher doses of glucocorticoids within the first 3 months is associated with treatment-related injuries and fatal infections. A multicenter cohort study (Thietart et al., 2022) examined the outcomes and adverse events of RTX therapy in AAV patients aged 75 and older and found that most patients achieved sustained remission without recurrence. When RTX is used as induction therapy in combination with high-dose glucocorticoid regimens, the incidence of severe infections and death is higher; however, when used as maintenance therapy, these rates are not as high. Nevertheless, a retrospective study Timlin et al. (2015) by in AAV patients aged 60 and older found that while RTX is effective in inducing remission, the incidence of infections is higher. Prospective survival analysis (McGovern et al., 2020) suggests that age, frailty score, and CRP levels at the time of presentation are independently associated with mortality in elderly AAV patients. Although the CYC induction therapy group showed higher survival rates compared to the RTX group, this may be due to the younger age of patients in the CYC group, and further studies are needed to validate this observation. In conclusion, there is still a lack of high-quality research in this field, such as RCTs. Based on the limited evidence available, RTX therapy can be considered a priority choice for elderly patients. However, when RTX is contraindicated or the patient’s economic situation is poor, the CYC regimen is also a reasonable option. When using these treatment regimens, attention should be paid to preventing the occurrence of infections.
2.2 B cell activating factor inhibitors
The lymphocyte stimulating factor (BLyS) is a new member of the tumor necrosis factor (TNF) family, which has a unique role in B cell development/differentiation and autoimmune disease (Do and Chen-Kiang, 2002). BLyS is expressed by neutrophils, which are key cells in the pathogenesis of AAV, as elevated concentrations of circulating BLyS are reported in patients with AAV (Holden et al., 2011; Carter et al., 2013).
Belimumab, a human IgG1λ monoclonal antibody against BLyS, has been approved for the treatment of active, autoantibody-associated systemic lupus erythematosus in adults receiving standard therapy. In an RCT (Jayne et al., 2019), patients with AAV were randomized in a 1:1 ratio to receive AZA (2 mg/kg/day), low-dose oral glucocorticoids (≤10 mg/day), and intravenous belimumab (10 mg/kg) after induction of remission with RTX or CYC plus glucocorticoids. The control group received the placebo. The results suggested that the risk of AAV recurrence was not reduced in the experimental group versus the placebo group; however, no recurrence (0/14) was seen in patients who received RTX induction therapy followed by belimumab maintenance therapy. By contrast, three (23.1%) of the 13 patients who achieved disease remission with RTX in the placebo group relapsed. These findings suggest that dual, B-cell-targeted immunotherapy (i.e., B cell depletion + BLyS blockade) may be more effective than either treatment alone. Notably, however, the study in question had a small sample size and contained some errors. The most recent COMBIVAS study (McClure et al., 2023) included a randomized, double-blind, placebo-controlled trial investigating the mechanisms of sequential treatment of GPA with RTX and belimumab. The primary end point of the trial was the time taken for conversion of PR3-ANCA to a negative status. The results of this study, which was launched in 2023 and expected to run for 2 years, are eagerly awaited by the research community.
2.3 C5a receptor inhibitors
C5a is a protein fragment released from cleavage of complement component C5 by protease C5-convertase. C5a has been shown to upregulate the cell surface expression of PR3 and MPO, prompting neutrophils to respond to ANCA stimulation and cause tissue damage (Prendecki and McAdoo, 2021a). Neutrophils stimulated by ANCA can also activate the alternative complement pathway, further initiating, recruiting, and activating neutrophils in an inflammatory feedback loop. In addition to being expressed by neutrophils, the C5a receptor (C5aR) is expressed by other myeloid cells, including dendritic cells (DCs), eosinophils, and monocytes. The C5aR may also play a role in the pathogenesis of EGPA (Prendecki and McAdoo, 2021a).
Avacopan was the first oral C5aR inhibitor to be approved by the FDA. To date, avacopan has been approved in several countries, including the United States and Japan, for the treatment of AAV. The ADVOCATE study (Jayne et al., 2021) compared the efficacy, safety, and risk of infection associated with avacopan or a steroid tapering regimen in a cohort of 331 patients with AAV. The results showed that at 26 weeks post-treatment initiation, the clinical response of the avacopan group was no different from that of the prednisone reduction group; however, avacopan was superior to prednisone reduction in terms of sustained remission at 52 weeks. Moreover, avacopan performed better than prednisone reduction in terms of safety. Another study (Cortazar et al., 2023a) analyzing data from the ADVOCATE trial, suggested that after 52 weeks of treatment, the improvement in the estimated glomerular filtration rate (eGFR) was higher in the avacopan group than in the prednisone group among patients with severe renal impairment (eGFR ≤ 20 mL/min/1.73 m2). Cortazar et al. (2023b) reported three cases of rapidly progressive AAV requiring renal replacement therapy. These patients were treated with avacopan in combination with RTX and/or CYC, along with rapid steroid tapering. All patients showed significant improvement in renal function and successfully discontinued hemodialysis. Another RCT (Jayne et al., 2017) compared the control group treated with prednisone (60 mg/day, tapered to 0 mg within 20 weeks), against those treated with avacopan (30 mg/day) or low-dose prednisone (20 mg/day) plus avacopan (30 mg/day), using the main efficacy endpoint of a ≥ 50% reduction in Birmingham Vasculitis Activity Score at week 12. The results showed no inferiority in terms of safety and efficacy among the treatment groups. The study by Merkel et al. (2020) suggested that the addition of avacopan to the standard regimen of glucocorticoids combined with RTX or CYC was not only well tolerated, but also shortened the duration of remission at higher doses. Abe et al. (2023) reported four cases in which an interesting finding was observed; avacopan did not decrease ANCA titers while reducing AAV activity. van Leeuwen et al. (2022) reported that an 84-year-old patient with refractory AAV, who was successful treated avacopan, exhibited a progressive decrease in C3 levels. Thus, avacopan may improve the outcomes of refractory AAV patients with concomitant complement system activation. Based on current clinical evidence, the 2024 KIDGO guidelines (Kidney Disease: Improving Global Outcomes KDIGO ANCA Vasculitis Work Group, 2024) clearly recommend avacopan as an effective alternative therapy for patients who face increased toxicity risks from glucocorticoid treatment. These patients are likely to derive the greatest therapeutic benefit from avacopan therapy. Furthermore, the guidelines emphasize that avacopan treatment may be particularly helpful in promoting significant recovery of glomerular filtration rate (GFR) among patients with low GFR. Thus, avacopan provides clinicians with a new treatment strategy, facilitating the development of optimized therapeutic plans for patients and potentially improving their prognosis.
2.4 Anti-CD52 monoclonal antibody
Cellular immunity also plays a crucial role in the pathogenesis of AAV. CD4+ T-cells facilitate the production of ANCA, and both CD4+ and CD8+ T-cells recognize ANCA antigens deposited in peripheral tissues through activated neutrophils. Animal model studies have provided us with considerable insights into this process. The presence of T-cells has also been observed in the glomeruli and tubulointerstitium of AAV patients (Kitching et al., 2020; Prendecki and McAdoo, 2021b), further emphasizing the importance of cellular immunity in such diseases.
Alemtuzumab is a humanized anti-CD52 monoclonal antibody that depletes all lymphocytes and has a particularly long-lasting effect on T cells, resulting in a CD4+ T cell count that takes approximately 60 months to recover (Coles et al., 2006). The ALEVIATE study (Gopaluni et al., 2022) included 23 patients with refractory AAV or Behçet’s disease (BD). These patients were randomly assigned to receive either 60 mg or 30 mg of alemtuzumab. The study results showed that alemtuzumab provided relief to approximately 2/3 of the patients at 6 months. However, this relief was sustained in only 1/3 of the patients at 12 months. Additionally, there were no significant differences in clinical endpoints between the different dosage groups. Alemtuzumab, as an immunotherapy targeting T-cells, demonstrates some potential in the treatment of AAV. However, its long-term efficacy and optimal dosing strategy still require further research and optimization.
2.5 T cell costimulation modulators
T cells become activated when their T cell receptor interacts with a cognate antigenic peptide presented on a major histocompatibility complex molecule expressed on the surface of antigen-presenting cells. The role of T cell costimulatory molecules is to strengthen the extent of T cell activation. Given that T cells drive granuloma formation, T cell activation could be implicated in the pathogenesis of AAV (Wilde et al., 2011).
Abatacept is a CTLA-4-Ig fusion protein, which binds to the costimulatory ligands CD80 and CD86 and blocks their interaction with the costimulatory receptors CD28 and CTLA-4 expressed by T cells, thereby inhibiting T cell activation (Glatigny et al., 2019; Ortiz-Fernández et al., 2023). A real-world study (Mettler et al., 2022) showed that abatacept was effective in < 50% of patients with refractory and/or relapsing GPA; however, only six patients were included in the study. In another study (Langford et al., 2014) which included 20 patients with non-severe, relapsing GPA, 18 (90%) patients improved while 16 (80%) patients achieved remission following abatacept treatment. Moreover, prednisone could be discontinued in 11 of the 15 (73%) patients as a result of abatacept treatment. These findings indicate that abatacept is well tolerated in patients with non-severe relapsing GPA and achieves a high rate of disease remission, while permitting glucocorticoid discontinuation.
2.6 TNF⁃α inhibitor
Evidence (Kamesh et al., 2002) suggests that TNF-α plays a central role in the pathogenesis of AAV by activating neutrophils, which leads to vascular endothelial injury. Indeed, anti-TNF-α antibody treatment significantly reduced proteinuria, crescent formation, and the incidence of pulmonary hemorrhage in vasculitic mice (Little et al., 2006). These findings suggest that anti-TNF-α antibodies may be effective in treating diagnosed vasculitis.
Infliximab, etanercept, and adalimumab are anti-TNF-α monoclonal antibodies currently being considered as biologic therapies for AAV. A meta-analysis (Bala et al., 2020) of data from four RCTs suggested that etanercept did not show significant efficacy in achieving disease remission or preventing relapse in GPA patients (as well as a small subset of MPA patients). Although etanercept may have exerted a minimal or no impact on severe adverse effects, it could potentially increase the likelihood of adverse reactions, leading to treatment discontinuation. A 33-patient cohort study (Morgan et al., 2011) with a 12-month follow-up period concluded that infliximab in addition to standard treatment did not provide clinical benefits for patients with active AAV. Another multi-center, prospective study with a small sample (Booth A. et al., 2004) showed that induction therapy with infliximab resulted in remission in 88% of AAV patients and a reduction in their glucocorticoid dosage. A prospective study (Laurino et al., 2010), which included 14 patients with active AAV, found that using adalimumab in combination with CYC achieved remission in 11 (78.5%) patients within 14 weeks (mean 12 weeks); however, one patient died and three patients developed infections. Although the efficacy and safety of this regimen were similar to those of the standard treatment, it did permit a reduction in the level of glucocorticoid exposure. Lamprecht et al. (2002) used infliximab for induction therapy in six patients with refractory GPA. The results showed that five patients achieved remission, with a gradual reduction in glucocorticoid dosage; furthermore, these patients remained in remission during the 6–24 months of follow-up. Kleinert et al. (2004) have reported a case of a patient with severe orbital Wegener granuloma who experienced acute renal failure despite receiving aggressive conventional immunosuppressive therapy. However, following the initial infusion of infliximab, there was an improvement in the patient’s renal function, which persisted throughout the course of treatment. The results of a multicenter cohort study (Silva et al., 2011), which included 153 patients with GPA accompanied by vasculitis, revealed that all 13 cases of newly diagnosed solid malignancies were associated with CYC exposure. Specifically, eight cases occurred in the group receiving etanercept, while five cases arose in the placebo group. Moreover, the etanercept group had a significant increased risk of solid malignancy compared with that of the general population. Thus, etanercept treatment appears to increase the risk of malignancy in patients receiving cytotoxic drugs.
2.7 Anti-IL-6-receptor (IL-6R) antibody
IL-6 is a notorious B lineage differentiation factor, which promotes the in situ activation of macrophages, the differentiation of T lymphocytes, and the synthesis of other proinflammatory cytokines (Naka et al., 2002). Inflammatory cytokines and chemokines may play a role in the pathogenesis of AAV (Chen and Kallenberg, 2010). Indeed, some studies have reported raised serum IL-6 levels in AAV patients versus healthy controls (Booth AD. et al., 2004; Krajewska Wojciechowska et al., 2019).
Tocilizumab, an anti-IL-6R antibody, has shown good clinical benefits in the biological treatment of patients with giant cell arteritis (Antonio et al., 2022). Tang et al. (2023) reported findings from a patient with refractory GPA and elevated IL-6 expression. After treatment with tocilizumab, the patient’s symptoms improved and the levels of inflammatory markers, including IL-6, normalized. The study by Berti et al. (2015) found that serum IL-6 levels were significantly increased in AAV patients; moreover, the IL-6 was predominantly expressed at sites of active vasculitis. Crucially, tocilizumab treatment induced complete and sustained disease remission in patients with severe multisystem MPA. In a prospective, single-center cohort study (Sakai et al., 2016) of tocilizumab monotherapy in MPA, two of six patients (33.3%) achieved complete remission at 6 months and three patients (50.0%) achieved complete remission at 12 months. Four patients (66.7%) discontinued treatment after 1 year and were relapse-free for 6–15 months at the time of their last follow-up visit. In view of this, it was concluded that tocilizumab monotherapy is a feasible treatment strategy for some MPA patients.
2.8 Anti-IL-5/IL-5-receptor (IL-5R) antibody
IL-5, a cytokine mainly involved in the chemotaxis and activation of eosinophils, is also involved in the pathogenesis of EGPA; thus, targeting IL-5 or its receptor represent promising EGPA treatment strategies (Furuta et al., 2019; Vega Villanueva and Espinoza, 2020).
Mepolizumab is currently the representative drug of anti-IL-5 antibodies, while the representative drugs of IL-5R antibodies are benralizumab and reslizumab. In 2023, Europe published the first evidence-based guidelines for the diagnosis and treatment of EGPA (Emmi et al., 2023). The report summarized a number of important clinical studies (Kahn et al., 2010; Kim et al., 2010; Moosig et al., 2011; Wechsler et al., 2017; Steinfeld et al., 2019; Bettiol et al., 2022; Hadjadj et al., 2022) and recommended that the combination of mepolizumab and glucocorticoids is used to induce remission in patients with relapsed and refractory EGPA without organ damage or other life-threatening complications. Meanwhile, RTX, mepolizumab, or conventional disease-modifying anti-rheumatic drugs combined with glucocorticoids are recommended for maintaining remission in patients with severe EGPA. For patients with non-severe EGPA, glucocorticoids alone or in combination with mepolizumab are currently recommended. Meanwhile, patients with non-severe EGPA and recurrent respiratory symptoms are advised to increase their glucocorticoid dose and/or take mepolizumab. The latest single-center study in Japan (Yamane and Hashiramoto, 2023) also confirmed the efficacy of mepolizumab, as evidenced by its ability to induce remission in EGPA patients treated with glucocorticoids. After 3 years of mepolizumab treatment, glucocorticoids could be discontinued in approximately 50% of EGPA patients, even in those with severe or ANCA-positive EGPA. The 2023 European guidelines (Emmi et al., 2023) suggest that other IL-5 or IL-5R inhibitors, such as benralizumab and relizumab, may be considered in patients refractory to mepolizumab, as their efficacy has been reported in case reports and case series (Koga et al., 2022; Koike et al., 2023). However, the latest retrospective study (Cottu et al., 2023) suggests that benralizumab is an effective treatment for EGPA with refractory asthma or respiratory symptoms in its own right, and can help reduce the dosage of glucocorticoids. By contrast, the efficacy of mepolizumab was lower in patients who had previously failed benralizumab therapy. Another retrospective study (Nanzer et al., 2024) suggests that among 70 EGPA patients treated with benralizumab, 47 patients (67.1%) achieved clinical remission at 1 year, with a similar remission rate maintained at 2 years. 87.1% of patients were relapse-free at 1 year, and among the 53 patients who completed 2 years of treatment, there was an 84.9% relapse-free rate. A total of 67.9% of patients no longer required any glucocorticoids to control their disease. The latest Italian real-world study (Nolasco et al., 2023) discussed the efficacy and safety of mepolizumab and benralizumab in patients with refractory EGPA treated for 24 months. The results suggest that mepolizumab and benralizumab are effective and safe as long-term add-on therapies for patients with EGPA. In 2024, a multicenter, double-blind, phase 3, randomized trial (Wechsler et al., 2024) was conducted involving 140 patients with relapsing or refractory EGPA. The study compared the efficacy and safety of benralizumab versus mepolizumab. The results indicated that benralizumab was non-inferior to mepolizumab in inducing remission among patients with relapsing or refractory EGPA and demonstrated a better safety profile.
3 Conclusion
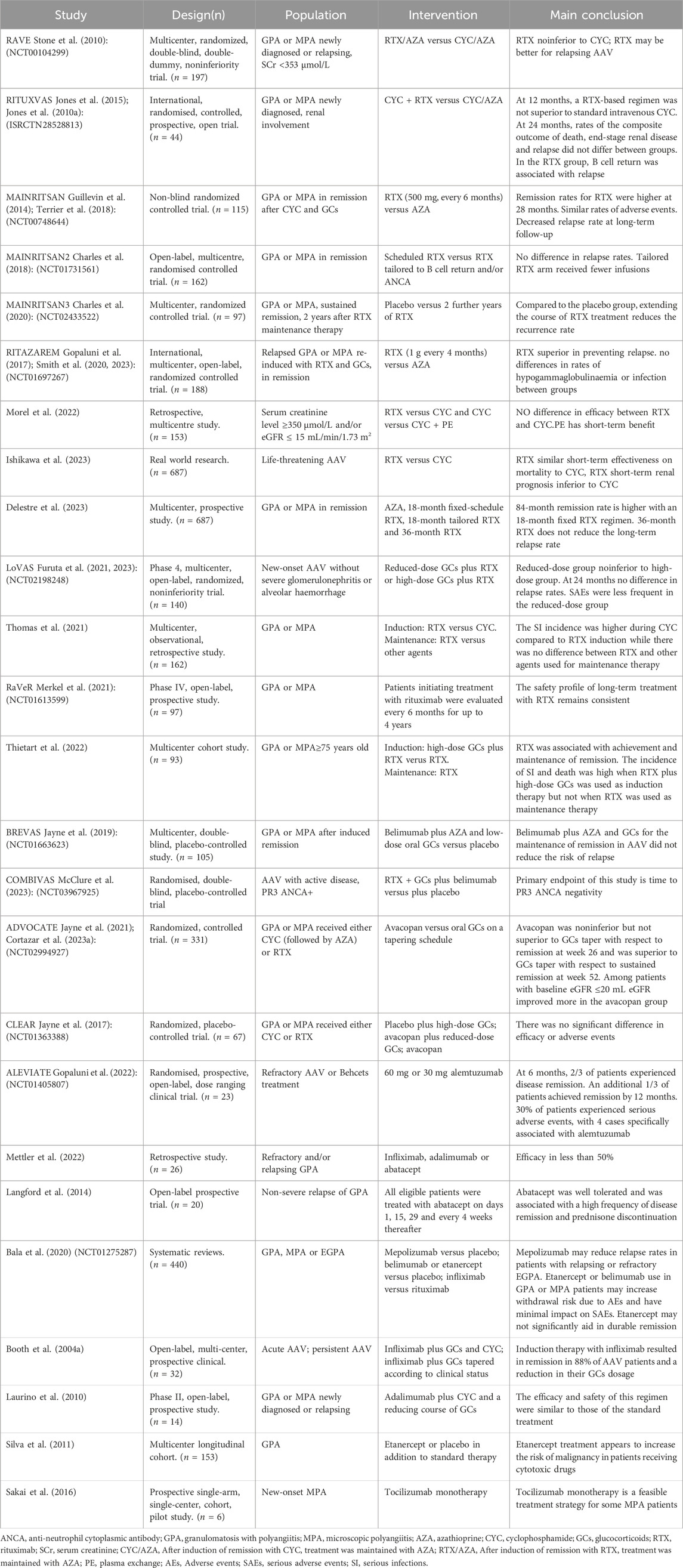
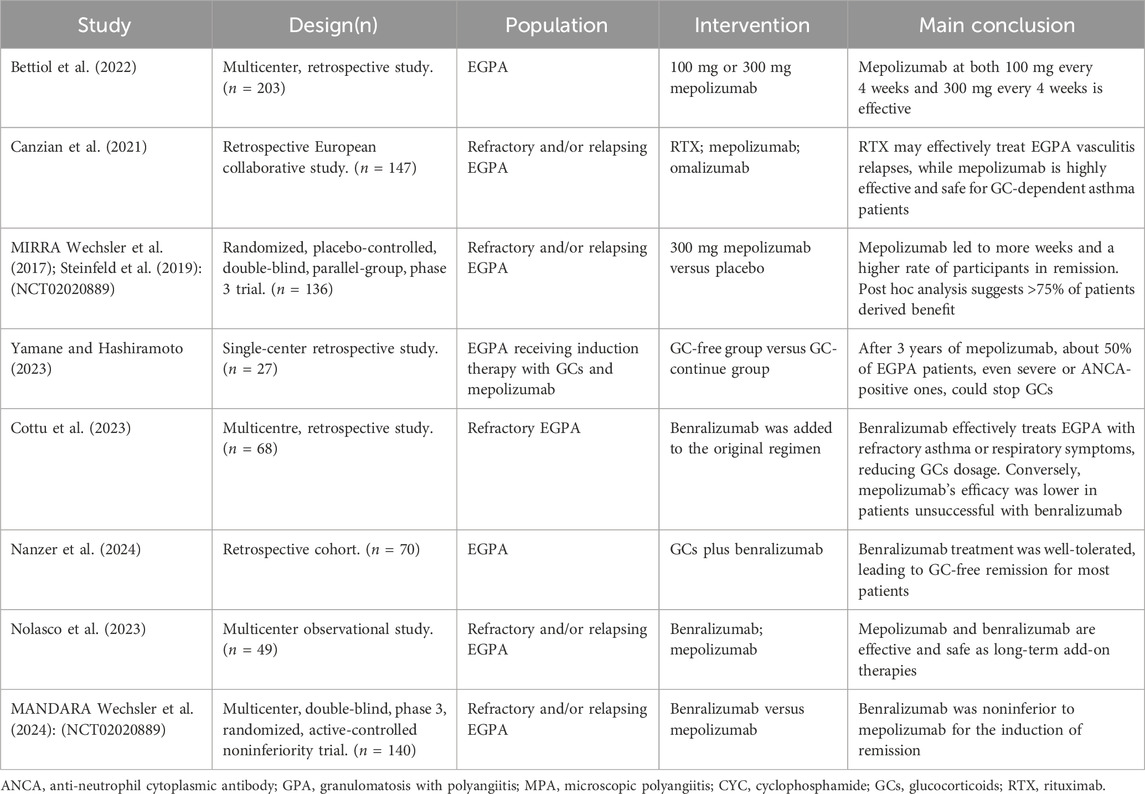
Finally, this article summarizes the key and latest clinical studies in the form of tables for readers’ convenience (Tables 1, 2). The rapid development of biotherapy has played an important role in both AAV-induced remission and maintenance. Biologic research provides new avenues for improving the prognosis of AAV patients and reducing adverse reactions associated with many other forms of immunotherapy. Experts recommend RTX as a first-line treatment option for AAV, for the induction of remission, maintenance therapy, or the treatment of relapsed patients. Avacopan has also received considerable attention in the treatment of AAV by significantly reducing glucocorticoid dosage and adverse reactions without affecting therapeutic efficacy. The sequential use of belimumab and RTX has demonstrated promise in controlling the recurrence of AAV and is likely to become a research hotspot in the future. Phase II studies suggest that alemtuzumab demonstrates some efficacy in the treatment of refractory AAV, but the recurrence rate is high. Abatacept has proved effective in patients with non-severe, recurrent GPA, while facilitating glucocorticoid discontinuation; however, these conclusion are currently based on low-quality data. To date, inhibiting TNF⁃α has not proved effective as a treatment for AAV, and the safety of this method also remains a concern. On the basis of reports that serum IL-6 levels are increased in AAV patients, small studies and case reports have shown that tocilizumab significantly increases complete and sustained remission rates. Meanwhile, mepolizumab has demonstrated efficacy in the treatment of EGPA and is especially recommended for patients with recurrent and refractory EGPA. Belimumab can be used as a second-line regimen for patients with mepolizumab resistance. The second-generation anti-CD20 antibody ofatumumab has demonstrated good efficacy in a series of reports (McAdoo et al., 2016). The third-generation anti-CD20 antibody obinutuzumab has shown stronger effects in B-cell reduction and NK cell activation (Urlaub et al., 2019). Eculizumab is a molecule that blocks the cleavage of C5 complement components into C5a and C5b, and there are currently only successful case reports available (Ribes et al., 2019). As there is not enough clinical evidence for these drugs at present, this article does not provide further discussion. We should look forward to the clinical results of these new biologics. In conclusion, biologics offer new hope to AAV patients, by improving therapeutic efficacy and alleviating adverse reactions typically associated with immunotherapy. However, the development of biologics for AAV is still in its early stages, and more basic research and clinical data are needed to verify their safety and efficacy, especially in the long-term. Thus, the optimization of biologics will be a major focus of future AAV research.
Author contributions
WL: Writing–original draft, Writing–review and editing. GT: Writing–original draft, Writing–review and editing. CC: Writing–original draft, Writing–review and editing. MZ: Writing–review and editing. ZC: Writing–review and editing. TC: Writing–review and editing. ZL: Writing–review and editing. WW: Writing–review and editing. YW: Writing–review and editing. KW: Writing–review and editing. QL: Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Natural Science Foundation of Guangdong Province (2023A1515012477).
Acknowledgments
We thank Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abe, Y., Minowa, K., Kogami, M., Ando, T., Makiyama, A., Yamaji, K., et al. (2023). Avacopan is possibly associated with the improvement of ANCA-associated vasculitis activity without decreasing ANCA titres: a four-case series. Rheumatol. Oxf. 62, e317–e318. doi:10.1093/rheumatology/kead191
Antonio, A. A., Santos, R. N., and Abariga, S. A. (2022). Tocilizumab for giant cell arteritis. Cochrane database Syst. Rev. 5 (5), CD013484. doi:10.1002/14651858.CD013484.pub3
Aqeel, F., Xu, L., Salas, A., Wen, Y., Eid, S. M., and Geetha, D. (2023). Outcomes of remission induction therapy for ANCA-associated vasculitis in the elderly. Clin. Rheumatol. 42 (9), 2427–2435. doi:10.1007/s10067-023-06644-2
Bala, M. M., Malecka-Massalska, T. J., Koperny, M., Zajac, J. F., Jarczewski, J. D., and Szczeklik, W. (2020). Anti-cytokine targeted therapies for ANCA-associated vasculitis. Cochrane database Syst. Rev. 9 (9), CD008333. doi:10.1002/14651858.CD008333.pub2
Berti, A., Cavalli, G., Campochiaro, C., Guglielmi, B., Baldissera, E., Cappio, S., et al. (2015). Interleukin-6 in ANCA-associated vasculitis: rationale for successful treatment with tocilizumab. Seminars arthritis rheumatism 45 (1), 48–54. doi:10.1016/j.semarthrit.2015.02.002
Bettiol, A., Urban, M. L., Dagna, L., Cottin, V., Franceschini, F., Del Giacco, S., et al. (2022). Mepolizumab for eosinophilic granulomatosis with polyangiitis: a European multicenter observational study. Arthritis and rheumatology (Hoboken, N.J.) 74 (2), 295–306. doi:10.1002/art.41943
Booth, A., Harper, L., Hammad, T., Bacon, P., Griffith, M., Levy, J., et al. (2004a). Prospective study of TNFalpha blockade with infliximab in anti-neutrophil cytoplasmic antibody-associated systemic vasculitis. J. Am. Soc. Nephrol. JASN 15 (3), 717–721. doi:10.1097/01.asn.0000114554.67106.28
Booth, A. D., Wallace, S., McEniery, C. M., Yasmin, , Brown, J., Jayne, D. R. W., et al. (2004b). Inflammation and arterial stiffness in systemic vasculitis: a model of vascular inflammation. Arthritis rheumatism 50 (2), 581–588. doi:10.1002/art.20002
Bossuyt, X., Cohen Tervaert, J. W., Arimura, Y., Blockmans, D., Flores-Suárez, L. F., Guillevin, L., et al. (2017). Position paper: revised 2017 international consensus on testing of ANCAs in granulomatosis with polyangiitis and microscopic polyangiitis. Nat. Rev. Rheumatol. 13 (11), 683–692. doi:10.1038/nrrheum.2017.140
Canzian, A., Venhoff, N., Urban, M. L., Sartorelli, S., Ruppert, A. M., Groh, M., et al. (2021). Use of biologics to treat relapsing and/or refractory eosinophilic granulomatosis with polyangiitis: data from a European collaborative study. Arthritis and rheumatology (Hoboken, N.J.) 73 (3), 498–503. doi:10.1002/art.41534
Carter, L. M., Isenberg, D. A., and Ehrenstein, M. R. (2013). Elevated serum BAFF levels are associated with rising anti-double-stranded DNA antibody levels and disease flare following B cell depletion therapy in systemic lupus erythematosus. Arthritis rheumatism 65 (10), 2672–2679. doi:10.1002/art.38074
Charles, P., Perrodeau, É., Samson, M., Bonnotte, B., Néel, A., Agard, C., et al. (2020). Long-term rituximab use to maintain remission of antineutrophil cytoplasmic antibody-associated vasculitis: a randomized trial. Ann. Intern. Med. 173 (3), 179–187. doi:10.7326/M19-3827
Charles, P., Terrier, B., Perrodeau, É., Cohen, P., Faguer, S., Huart, A., et al. (2018). Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann. rheumatic Dis. 77 (8), 1143–1149. doi:10.1136/annrheumdis-2017-212878
Chen, M., and Kallenberg, C. G. (2010). ANCA-associated vasculitides--advances in pathogenesis and treatment. Nat. Rev. Rheumatol. 6 (11), 653–664. doi:10.1038/nrrheum.2010.158
Chotiyarnwong, P., and McCloskey, E. V. (2020). Pathogenesis of glucocorticoid-induced osteoporosis and options for treatment. Nat. Rev. Endocrinol. 16 (8), 437–447. doi:10.1038/s41574-020-0341-0
Coles, A. J., Cox, A., Le Page, E., Jones, J., Trip, S. A., Deans, J., et al. (2006). The window of therapeutic opportunity in multiple sclerosis: evidence from monoclonal antibody therapy. J. neurology 253 (1), 98–108. doi:10.1007/s00415-005-0934-5
Cortazar, F. B., Cerda, J., Dhanani, R., Roglieri, J., and Santoriello, D. (2023b). Avacopan in patients with rapidly progressive glomerulonephritis requiring dialysis. Kidney Int. Rep. 8 (8), 1687–1691. doi:10.1016/j.ekir.2023.05.017
Cortazar, F. B., Niles, J. L., Jayne, D., Merkel, P. A., Bruchfeld, A., Yue, H., et al. (2023a). Renal recovery for patients with ANCA-associated vasculitis and low eGFR in the ADVOCATE trial of avacopan. Kidney Int. Rep. 8 (4), 860–870. doi:10.1016/j.ekir.2023.01.039
Cottu, A., Groh, M., Desaintjean, C., Marchand-Adam, S., Guillevin, L., Puechal, X., et al. (2023). Benralizumab for eosinophilic granulomatosis with polyangiitis. Ann. rheumatic Dis. 82 (12), 1580–1586. doi:10.1136/ard-2023-224624
Cutolo, M., Seriolo, B., Pizzorni, C., Secchi, M. E., Soldano, S., Paolino, S., et al. (2008). Use of glucocorticoids and risk of infections. Autoimmun. Rev. 8 (2), 153–155. doi:10.1016/j.autrev.2008.07.010
Delestre, F., Charles, P., Karras, A., Pagnoux, C., Néel, A., Cohen, P., et al. (2023). Rituximab as maintenance therapy for ANCA-associated vasculitides: pooled analysis and long-term outcome of 277 patients included in the MAINRITSAN trials. Ann. Rheum. Dis. 83 (2), 233–241. doi:10.1136/ard-2023-224623
Do, R. K., and Chen-Kiang, S. (2002). Mechanism of BLyS action in B cell immunity. Cytokine and growth factor Rev. 13 (1), 19–25. doi:10.1016/s1359-6101(01)00025-9
Emmi, G., Bettiol, A., Gelain, E., Bajema, I. M., Berti, A., Burns, S., et al. (2023). Evidence-Based Guideline for the diagnosis and management of eosinophilic granulomatosis with polyangiitis. Nat. Rev. Rheumatol. 19 (6), 378–393. doi:10.1038/s41584-023-00958-w
Feng, P. H., George, C. R., Evans, R. A., Murkin, G. E., Spicer, E., Thomas, B. S., et al. (1972). Cyclophosphamide and infertility. Lancet 1 (7755), 840–842. doi:10.1016/s0140-6736(72)90819-7
Furuta, S., Iwamoto, T., and Nakajima, H. (2019). Update on eosinophilic granulomatosis with polyangiitis. Allergology Int. official J. Jpn. Soc. Allergology 68 (4), 430–436. doi:10.1016/j.alit.2019.06.004
Furuta, S., Nakagomi, D., Kobayashi, Y., Hiraguri, M., Sugiyama, T., Amano, K., et al. (2021). Effect of reduced-dose vs high-dose glucocorticoids added to rituximab on remission induction in ANCA-associated vasculitis: a randomized clinical trial. JAMA 325 (21), 2178–2187. doi:10.1001/jama.2021.6615
Furuta, S., Nakagomi, D., Kobayashi, Y., Hiraguri, M., Sugiyama, T., Amano, K., et al. (2023). Reduced-dose versus high-dose glucocorticoids added to rituximab on remission induction in ANCA-associated vasculitis: predefined 2-year follow-up study. Ann. rheumatic Dis. 83, 96–102. doi:10.1136/ard-2023-224343
Geetha, D., and Jefferson, J. A. (2020). ANCA-associated vasculitis: core curriculum 2020. Am. J. kidney Dis. official J. Natl. Kidney Found. 75 (1), 124–137. doi:10.1053/j.ajkd.2019.04.031
Gérard, M., de Boysson, H., Morello, R., Martin-Silva, N., Leroux, A. C., Dumont, A., et al. (2023). Early infectious risk in patients with anti-neutrophil cytoplasmic antibody-associated vasculitis according to remission-induction therapy. Scand. J. rheumatology 52 (2), 161–173. doi:10.1080/03009742.2021.2001929
Glatigny, S., Höllbacher, B., Motley, S. J., Tan, C., Hundhausen, C., Buckner, J. H., et al. (2019). Abatacept targets T follicular helper and regulatory T cells, disrupting molecular pathways that regulate their proliferation and maintenance. J. Immunol. Baltim. Md 1950 202 (5), 1373–1382. doi:10.4049/jimmunol.1801425
Gopaluni, S., Smith, R., Goymer, D., Cahill, H., Broadhurst, E., Wallin, E., et al. (2022). Alemtuzumab for refractory primary systemic vasculitis-a randomised controlled dose ranging clinical trial of efficacy and safety (ALEVIATE). Arthritis Res. Ther. 24 (1), 81. doi:10.1186/s13075-022-02761-6
Gopaluni, S., Smith, R. M., Lewin, M., McAlear, C. A., Mynard, K., Jones, R. B., et al. (2017). Rituximab versus azathioprine as therapy for maintenance of remission for anti-neutrophil cytoplasm antibody-associated vasculitis (RITAZAREM): study protocol for a randomized controlled trial. Trials 18 (1), 112. doi:10.1186/s13063-017-1857-z
Guillevin, L., Pagnoux, C., Karras, A., Khouatra, C., Aumaître, O., Cohen, P., et al. (2014). Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N. Engl. J. Med. 371 (19), 1771–1780. doi:10.1056/NEJMoa1404231
Hadjadj, J., Canzian, A., Karadag, O., Contis, A., Maurier, F., Sanges, S., et al. (2022). Use of biologics to treat relapsing and/or refractory polyarteritis nodosa: data from a European collaborative study. Rheumatol. Oxf. Engl. 62 (1), 341–346. doi:10.1093/rheumatology/keac332
Hellmich, B., Sanchez-Alamo, B., Schirmer, J. H., Berti, A., Blockmans, D., Cid, M. C., et al. (2024). EULAR recommendations for the management of ANCA-associated vasculitis: 2022 update. Ann. rheumatic Dis. 83 (1), 30–47. doi:10.1136/ard-2022-223764
Holden, N. J., Williams, J. M., Morgan, M. D., Challa, A., Gordon, J., Pepper, R. J., et al. (2011). ANCA-stimulated neutrophils release BLyS and promote B cell survival: a clinically relevant cellular process. Ann. rheumatic Dis. 70 (12), 2229–2233. doi:10.1136/ard.2011.153890
Hwang, J. L., and Weiss, R. E. (2014). Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment. Diabetes/metabolism Res. Rev. 30 (2), 96–102. doi:10.1002/dmrr.2486
Ishikawa, Y., Tokutsu, K., Nakayamada, S., Kuchiba, A., Fushimi, K., Matsuda, S., et al. (2023). Short-term effectiveness and safety of rituximab versus cyclophosphamide for life-threatening ANCA-associated vasculitis: a propensity score analysis of the real-world nationwide database. Ann. rheumatic Dis. 83, 103–111. doi:10.1136/ard-2023-224472
Ishikawa, Y., Tokutsu, K., Nakayamada, S., Kuchiba, A., Fushimi, K., Matsuda, S., et al. (2024). Short-term effectiveness and safety of rituximab versus cyclophosphamide for life-threatening ANCA-associated vasculitis: a propensity score analysis of the real-world nationwide database. Ann. rheumatic Dis. 83 (1), 103–111. doi:10.1136/ard-2023-224472
Jayne, D., Blockmans, D., Luqmani, R., Moiseev, S., Ji, B., Green, Y., et al. (2019). Efficacy and safety of belimumab and azathioprine for maintenance of remission in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled study. Arthritis and rheumatology (Hoboken, N.J.) 71 (6), 952–963. doi:10.1002/art.40802
Jayne, D., Bruchfeld, A. N., Harper, L., Schaier, M., Venning, M. C., Hamilton, P., et al. (2017). Randomized trial of C5a receptor inhibitor avacopan in ANCA-associated vasculitis. J. Am. Soc. Nephrol. JASN 28 (9), 2756–2767. doi:10.1681/ASN.2016111179
Jayne, D., Merkel, P. A., Schall, T. J., and Bekker, P.ADVOCATE Study Group (2021). Avacopan for the treatment of ANCA-associated vasculitis. N. Engl. J. Med. 384 (7), 599–609. doi:10.1056/NEJMoa2023386
Jones, R. B., Furuta, S., Tervaert, J. W., Hauser, T., Luqmani, R., Morgan, M. D., et al. (2015). Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis: 2-year results of a randomised trial. Ann. rheumatic Dis. 74 (6), 1178–1182. doi:10.1136/annrheumdis-2014-206404
Jones, R. B., Tervaert, J. W., Hauser, T., Luqmani, R., Morgan, M. D., Peh, C. A., et al. (2010a). Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N. Engl. J. Med. 363 (3), 211–220. doi:10.1056/NEJMoa0909169
Jones, R. B., Tervaert, J. W., Hauser, T., Luqmani, R., Morgan, M. D., Peh, C. A., et al. (2010b). Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N. Engl. J. Med. 363 (3), 211–220. doi:10.1056/NEJMoa0909169
Kahn, J. E., Grandpeix-Guyodo, C., Marroun, I., Catherinot, E., Mellot, F., Roufosse, F., et al. (2010). Sustained response to mepolizumab in refractory Churg-Strauss syndrome. J. allergy Clin. Immunol. 125 (1), 267–270. doi:10.1016/j.jaci.2009.10.014
Kamesh, L., Harper, L., and Savage, C. O. (2002). ANCA-positive vasculitis. J. Am. Soc. Nephrol. JASN 13 (7), 1953–1960. doi:10.1097/01.asn.0000016442.33680.3e
Kidney Disease: Improving Global Outcomes (KDIGO) ANCA Vasculitis Work Group (2024). KDIGO 2024 clinical practice guideline for the management of antineutrophil cytoplasmic antibody (ANCA)-Associated vasculitis. Kidney Int. 105 (3S), S71–S116. doi:10.1016/j.kint.2023.10.008
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021). KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 100 (4S), S1–S276. doi:10.1016/j.kint.2021.05.021
Kim, S., Marigowda, G., Oren, E., Israel, E., and Wechsler, M. E. (2010). Mepolizumab as a steroid-sparing treatment option in patients with Churg-Strauss syndrome. J. allergy Clin. Immunol. 125 (6), 1336–1343. doi:10.1016/j.jaci.2010.03.028
Kitching, A. R., Anders, H. J., Basu, N., Brouwer, E., Gordon, J., Jayne, D. R., et al. (2020). ANCA-associated vasculitis. Nat. Rev. Dis. Prim. 6 (1), 71. doi:10.1038/s41572-020-0204-y
Kleinert, J., Lorenz, M., Köstler, W., Hörl, W., Sunder-Plassmann, G., and Soleiman, A. (2004). Refractory Wegener's granulomatosis responds to tumor necrosis factor blockade. Wien. Klin. Wochenschr. 116 (9-10), 334–338. doi:10.1007/BF03040906
Koga, Y., Aoki-Saito, H., Kamide, Y., Sato, M., Tsurumaki, H., Yatomi, M., et al. (2022). Perspectives on the efficacy of benralizumab for treatment of eosinophilic granulomatosis with polyangiitis. Front. Pharmacol. 13, 865318. doi:10.3389/fphar.2022.865318
Koike, H., Nishi, R., Yagi, S., Furukawa, S., Fukami, Y., Iijima, M., et al. (2023). A review of anti-IL-5 therapies for eosinophilic granulomatosis with polyangiitis. Adv. Ther. 40 (1), 25–40. doi:10.1007/s12325-022-02307-x
Krajewska Wojciechowska, J., Kościelska-Kasprzak, K., Krajewski, W., and Morawski, K. (2019). Serum levels of interleukin-32 and interleukin-6 in granulomatosis with polyangiitis and microscopic polyangiitis: association with clinical and biochemical findings. Eur. cytokine Netw. 30 (4), 151–159. doi:10.1684/ecn.2019.0439
Lamprecht, P., Voswinkel, J., Lilienthal, T., Nolle, B., Heller, M., Gross, W. L., et al. (2002). Effectiveness of TNF-alpha blockade with infliximab in refractory Wegener's granulomatosis. Rheumatol. Oxf. Engl. 41 (11), 1303–1307. doi:10.1093/rheumatology/41.11.1303
Langford, C. A., Monach, P. A., Specks, U., Seo, P., Cuthbertson, D., McAlear, C. A., et al. (2014). An open-label trial of abatacept (CTLA4-IG) in non-severe relapsing granulomatosis with polyangiitis (Wegener's). Ann. rheumatic Dis. 73 (7), 1376–1379. doi:10.1136/annrheumdis-2013-204164
Laurino, S., Chaudhry, A., Booth, A., Conte, G., and Jayne, D. (2010). Prospective study of TNFalpha blockade with adalimumab in ANCA-associated systemic vasculitis with renal involvement. Nephrol. dialysis, Transplant. official Publ. Eur. Dialysis Transpl. Assoc. - Eur. Ren. Assoc. 25 (10), 3307–3314. doi:10.1093/ndt/gfq187
Lee, Y. H., and Song, G. G. (2022). Comparative efficacy and safety of rituximab, mycophenolate, methotrexate, and cyclophosphamide versus azathioprine as maintenance therapy in antineutrophil cytoplasmic antibody-associated vasculitis: a Bayesian network meta-analysis of randomized controlled trials. Int. J. Clin. Pharmacol. Ther. 60 (2), 97–105. doi:10.5414/CP204053
Little, M. A., Bhangal, G., Smyth, C. L., Nakada, M. T., Cook, H. T., Nourshargh, S., et al. (2006). Therapeutic effect of anti-TNF-alpha antibodies in an experimental model of anti-neutrophil cytoplasm antibody-associated systemic vasculitis. J. Am. Soc. Nephrol. JASN 17 (1), 160–169. doi:10.1681/ASN.2005060616
Liu, L., Lu, H., Zou, G., Wang, H., Li, J., Yang, Y., et al. (2023). Efficacy and safety of low-dose rituximab as induction therapy for antineutrophil cytoplasmic antibody-associated vasculitis with renal involvement: a Chinese case series. BMC Nephrol. 24 (1), 28. doi:10.1186/s12882-023-03075-8
Machet, T., Quémeneur, T., Ledoult, E., Mesbah, R., Lebas, C., Hachulla, E., et al. (2023). Rituximab resistance at 3months of induction therapy in newly diagnosed or relapsing ANCA-associated vasculitis: a French multicentre retrospective study in 116 patients. Jt. bone spine 90 (5), 105591. doi:10.1016/j.jbspin.2023.105591
Magri, S. J., Ugarte-Gil, M. F., Brance, M. L., Flores-Suárez, L. F., Fernández-Ávila, D. G., Scolnik, M., et al. (2023). Pan American League of Associations for Rheumatology guidelines for the treatment of ANCA-associated vasculitis. Lancet Rheumatol. 5, e483–e494. doi:10.1016/S2665-9913(23)00128-5
McAdoo, S. P., Bedi, R., Tarzi, R., Griffith, M., Pusey, C. D., and Cairns, T. D. (2016). Ofatumumab for B cell depletion therapy in ANCA-associated vasculitis: a single-centre case series. Rheumatol. Oxf. Engl. 55 (8), 1437–1442. doi:10.1093/rheumatology/kew199
McClure, M. E., Gopaluni, S., Wason, J., Henderson, R. B., Van Maurik, A., Savage, C. C. O., et al. (2023). A randomised study of rituximab and belimumab sequential therapy in PR3 ANCA-associated vasculitis (COMBIVAS): design of the study protocol. Trials 24 (1), 180. doi:10.1186/s13063-023-07218-y
McGovern, D., Williams, S. P., Parsons, K., Farrah, T. E., Gallacher, P. J., Miller-Hodges, E., et al. (2020). Long-term outcomes in elderly patients with ANCA-associated vasculitis. Rheumatol. Oxf. Engl. 59 (5), 1076–1083. doi:10.1093/rheumatology/kez388
Merkel, P. A., Niles, J., Jimenez, R., Spiera, R. F., Rovin, B. H., Bomback, A., et al. (2020). Adjunctive treatment with avacopan, an oral C5a receptor inhibitor, in patients with antineutrophil cytoplasmic antibody-associated vasculitis. ACR Open Rheumatol. 2 (11), 662–671. doi:10.1002/acr2.11185
Merkel, P. A., Niles, J. L., Mertz, L. E., Lehane, P. B., Pordeli, P., and Erblang, F. (2021). Long-term safety of rituximab in granulomatosis with polyangiitis and in microscopic polyangiitis. Arthritis care and Res. 73 (9), 1372–1378. doi:10.1002/acr.24332
Mettler, C., Durel, C. A., Guilpain, P., Bonnotte, B., Cohen-Aubart, F., Hamidou, M., et al. (2022). Off-label use of biologics for the treatment of refractory and/or relapsing granulomatosis with polyangiitis. Eur. J. Intern. Med. 96, 97–101. doi:10.1016/j.ejim.2021.10.028
Moosig, F., Gross, W. L., Herrmann, K., Bremer, J. P., and Hellmich, B. (2011). Targeting interleukin-5 in refractory and relapsing Churg-Strauss syndrome. Ann. Intern. Med. 155 (5), 341–343. doi:10.7326/0003-4819-155-5-201109060-00026
Morel, P., Karras, A., Porcher, R., Belenfant, X., Audard, V., Rafat, C., et al. (2022). Management of severe renal disease in anti-neutrophil-cytoplasmic-antibody-associated vasculitis: the place of rituximab and plasma exchange. Rheumatol. Oxf. Engl. 61 (10), 4056–4064. doi:10.1093/rheumatology/keac046
Morgan, M. D., Drayson, M. T., Savage, C. O., and Harper, L. (2011). Addition of infliximab to standard therapy for ANCA-associated vasculitis. Nephron. Clin. Pract. 117 (2), c89–c97. doi:10.1159/000319655
Morris, A. D., Elsayed, M. E., Ponnusamy, A., Rowbottom, A., Martin, F., Geetha, D., et al. (2020). Treatment outcomes of anti-neutrophil cytoplasmic autoantibody-associated vasculitis in patients over age 75 Years: a meta-analysis. Am. J. Nephrol. 51 (4), 327–336. doi:10.1159/000506532
Naka, T., Nishimoto, N., and Kishimoto, T. (2002). The paradigm of IL-6: from basic science to medicine. Arthritis Res. 4 (Suppl. 3), S233–S242. doi:10.1186/ar565
Nanzer, A. M., Maynard-Paquette, A. C., Alam, V., Green, L., Thomson, L., Lam, J., et al. (2024). Long-term effectiveness of benralizumab in eosinophilic granulomatosis with polyangiitis. J. allergy Clin. Immunol. 12 (3), 724–732. doi:10.1016/j.jaip.2024.01.006
Nolasco, S., Portacci, A., Campisi, R., Buonamico, E., Pelaia, C., Benfante, A., et al. (2023). Effectiveness and safety of anti-IL-5/Rα biologics in eosinophilic granulomatosis with polyangiitis: a two-year multicenter observational study. Front. Immunol. 14, 1204444. doi:10.3389/fimmu.2023.1204444
Odler, B., Riedl, R., Gauckler, P., Shin, J. I., Leierer, J., Merkel, P. A., et al. (2023). Risk factors for serious infections in ANCA-associated vasculitis. Ann. rheumatic Dis. 82 (5), 681–687. doi:10.1136/ard-2022-223401
Ortiz-Fernández, L., Carmona, E. G., Kerick, M., Lyons, P., Carmona, F. D., López Mejías, R., et al. (2023). Identification of new risk loci shared across systemic vasculitides points towards potential target genes for drug repurposing. Ann. rheumatic Dis. 82 (6), 837–847. doi:10.1136/ard-2022-223697
Podestà, M. A., Mescia, F., Ricchiuto, A., Smith, R., Tedesco, M., Cassia, M. A., et al. (2023). Predictors of hypogammaglobulinemia in ANCA-associated vasculitis after a rituximab-based induction: a multicentre study. Rheumatol. Oxf. Engl. 62 (8), 2850–2854. doi:10.1093/rheumatology/keac716
Prendecki, M., and McAdoo, S. P. (2021a). Targeting complement in ANCA-associated vasculitis: insights from ADVOCATE. Nat. Rev. Nephrol. 17 (7), 439–440. doi:10.1038/s41581-021-00417-3
Prendecki, M., and McAdoo, S. P. (2021b). New therapeutic targets in antineutrophil cytoplasm antibody-associated vasculitis. Arthritis and rheumatology (Hoboken, N.J.) 73 (3), 361–370. doi:10.1002/art.41407
Rahmattulla, C., Berden, A. E., Wakker, S. C., Reinders, M. E. J., Hagen, E. C., Wolterbeek, R., et al. (2015). Incidence of malignancies in patients with antineutrophil cytoplasmic antibody-associated vasculitis diagnosed between 1991 and 2013. Arthritis and rheumatology (Hoboken, N.J.) 67 (12), 3270–3278. doi:10.1002/art.39317
Ribes, D., Belliere, J., Piedrafita, A., and Faguer, S. (2019). Glucocorticoid-free induction regimen in severe ANCA-associated vasculitis using a combination of rituximab and eculizumab. Rheumatol. Oxf. Engl. 58 (12), 2335–2337. doi:10.1093/rheumatology/kez190
Roccatello, D., Sciascia, S., Murgia, S., Quattrocchio, G., Ferro, M., De Simone, E., et al. (2022). Treating patients with ANCA-associated vasculitis and very severe renal injury with an intensified B cell depletion therapy: comparison with a control cohort receiving a conventional therapy. Front. Immunol. 13, 777134. doi:10.3389/fimmu.2022.777134
Sakai, R., Kondo, T., Kikuchi, J., Shibata, A., Chino, K., Okuyama, A., et al. (2016). Corticosteroid-free treatment of tocilizumab monotherapy for microscopic polyangiitis: a single-arm, single-center, clinical trial. Mod. Rheumatol. 26 (6), 900–907. doi:10.3109/14397595.2016.1160968
Shah, S., Jaggi, K., Greenberg, K., and Geetha, D. (2017). Immunoglobulin levels and infection risk with rituximab induction for anti-neutrophil cytoplasmic antibody-associated vasculitis. Clin. kidney J. 10 (4), 470–474. doi:10.1093/ckj/sfx014
Silva, F., Seo, P., Schroeder, D. R., Stone, J. H., Merkel, P. A., Hoffman, G. S., et al. (2011). Solid malignancies among etanercept-treated patients with granulomatosis with polyangiitis (Wegener's): long-term followup of a multicenter longitudinal cohort. Arthritis rheumatism 63 (8), 2495–2503. doi:10.1002/art.30394
Smith, R. M., Jones, R. B., Specks, U., Bond, S., Nodale, M., Aljayyousi, R., et al. (2020). Rituximab as therapy to induce remission after relapse in ANCA-associated vasculitis. Ann. rheumatic Dis. 79 (9), 1243–1249. doi:10.1136/annrheumdis-2019-216863
Smith, R. M., Jones, R. B., Specks, U., Bond, S., Nodale, M., Al-Jayyousi, R., et al. (2023). Rituximab versus azathioprine for maintenance of remission for patients with ANCA-associated vasculitis and relapsing disease: an international randomised controlled trial. Ann. rheumatic Dis. 82 (7), 937–944. doi:10.1136/ard-2022-223559
Sorin, B., Samson, M., Durel, C. A., Diot, E., Guichard, I., Grados, A., et al. (2022). Rituximab plus methotrexate combination as a salvage therapy in persistently active granulomatosis with polyangiitis. Rheumatol. Oxf. Engl. 61 (6), 2619–2624. doi:10.1093/rheumatology/keab791
Steinfeld, J., Bradford, E. S., Brown, J., Mallett, S., Yancey, S. W., Akuthota, P., et al. (2019). Evaluation of clinical benefit from treatment with mepolizumab for patients with eosinophilic granulomatosis with polyangiitis. J. allergy Clin. Immunol. 143 (6), 2170–2177. doi:10.1016/j.jaci.2018.11.041
Stone, J. H., Merkel, P. A., Spiera, R., Seo, P., Langford, C. A., Hoffman, G. S., et al. (2010). Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N. Engl. J. Med. 363 (3), 221–232. doi:10.1056/NEJMoa0909905
Tang, P. F., Xu, L. C., Hong, W. T., and Shi, H. Y. (2023). Successful treatment of granulomatosis with polyangiitis using tocilizumab combined with glucocorticoids: a case report. World J. Clin. cases 11 (5), 1144–1151. doi:10.12998/wjcc.v11.i5.1144
Terrier, B., Pagnoux, C., Perrodeau, É., Karras, A., Khouatra, C., Aumaître, O., et al. (2018). Long-term efficacy of remission-maintenance regimens for ANCA-associated vasculitides. Ann. rheumatic Dis. 77 (8), 1150–1156. doi:10.1136/annrheumdis-2017-212768
Thietart, S., Karras, A., Augusto, J. F., Philipponnet, C., Carron, P. L., Delbrel, X., et al. (2022). Evaluation of rituximab for induction and maintenance therapy in patients 75 Years and older with antineutrophil cytoplasmic antibody-associated vasculitis. JAMA Netw. open 5 (7), e2220925. doi:10.1001/jamanetworkopen.2022.20925
Thomas, K., Argyriou, E., Kapsala, N., Panagiotopoulos, A., Chalkia, A., Hadziyannis, E., et al. (2021). Serious infections in ANCA-associated vasculitides in the biologic era: real-life data from a multicenter cohort of 162 patients. Arthritis Res. Ther. 23 (1), 90. doi:10.1186/s13075-021-02452-8
Tieu, J., Smith, R., Basu, N., Brogan, P., D'Cruz, D., Dhaun, N., et al. (2020). Rituximab for maintenance of remission in ANCA-associated vasculitis: expert consensus guidelines. Rheumatol. Oxf. Engl. 59 (4), e24–e32. doi:10.1093/rheumatology/kez640
Tieu, J., Smith, R. M., Gopaluni, S., Kumararatne, D. S., McClure, M., Manson, A., et al. (2021). Rituximab associated hypogammaglobulinemia in autoimmune disease. Front. Immunol. 12, 671503. doi:10.3389/fimmu.2021.671503
Timlin, H., Lee, S. M., Manno, R. L., Seo, P., and Geetha, D. (2015). Rituximab for remission induction in elderly patients with ANCA-associated vasculitis. Seminars arthritis rheumatism 45 (1), 67–69. doi:10.1016/j.semarthrit.2015.02.005
Urlaub, D., Zhao, S., Blank, N., Bergner, R., Claus, M., Tretter, T., et al. (2019). Activation of natural killer cells by rituximab in granulomatosis with polyangiitis. Arthritis Res. Ther. 21 (1), 277. doi:10.1186/s13075-019-2054-0
van Leeuwen, J. R., Bredewold, O. W., van Dam, L. S., Werkman, S. L., Jonker, J. T., Geelhoed, M., et al. (2022). Compassionate use of avacopan in difficult-to-treat antineutrophil cytoplasmic antibody-associated vasculitis. Kidney Int. Rep. 7 (3), 624–628. doi:10.1016/j.ekir.2021.11.036
Vassilopoulos, A., Vassilopoulos, S., Kalligeros, M., Shehadeh, F., and Mylonakis, E. (2023). Incidence of serious infections in patients with ANCA-associated vasculitis receiving immunosuppressive therapy: a systematic review and meta-analysis. Front. Med. 10, 1110548. doi:10.3389/fmed.2023.1110548
Vega Villanueva, K. L., and Espinoza, L. R. (2020). Eosinophilic vasculitis. Curr. Rheumatol. Rep. 22 (1), 5. doi:10.1007/s11926-020-0881-2
Watts, R. A., Mahr, A., Mohammad, A. J., Gatenby, P., Basu, N., and Flores-Suárez, L. F. (2015). Classification, epidemiology and clinical subgrouping of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. Nephrol. Dial. Transpl. 30 Suppl 1, i14–i22. doi:10.1093/ndt/gfv022
Wechsler, M. E., Akuthota, P., Jayne, D., Khoury, P., Klion, A., Langford, C. A., et al. (2017). Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N. Engl. J. Med. 376 (20), 1921–1932. doi:10.1056/NEJMoa1702079
Wechsler, M. E., Nair, P., Terrier, B., Walz, B., Bourdin, A., Jayne, D. R. W., et al. (2024). Benralizumab versus mepolizumab for eosinophilic granulomatosis with polyangiitis. N. Engl. J. Med. 390 (10), 911–921. doi:10.1056/NEJMoa2311155
Weiner, M., Goh, S. M., Mohammad, A. J., Hrušková, Z., Tanna, A., Sharp, P., et al. (2020). Effect of treatment on damage and hospitalization in elderly patients with microscopic polyangiitis and granulomatosis with polyangiitis. J. rheumatology 47 (4), 580–588. doi:10.3899/jrheum.190019
Wilde, B., van Paassen, P., Witzke, O., and Tervaert, J. (2011). New pathophysiological insights and treatment of ANCA-associated vasculitis. Kidney Int. 79 (6), 599–612. doi:10.1038/ki.2010.472
Yamane, T., and Hashiramoto, A. (2023). Mepolizumab exerts crucial effects on glucocorticoid discontinuation in patients with eosinophilic granulomatosis with polyangiitis: a retrospective study of 27 cases at a single center in Japan. Arthritis Res. Ther. 25 (1), 110. doi:10.1186/s13075-023-03097-5
Keywords: anti-neutrophil cytoplasmic antibody, biological agents, vasculitis, treatment, microscopic polyangiitis, granulomatosis with polyangiitis, rituximab
Citation: Liu W, Tian G, Chen C, Zhang M, Chen Z, Chen T, Lin Z, Wu W, Wu Y, Wu K and Liu Q (2024) Application of biological agents in the treatment of anti-neutrophil cytoplasmic antibody-associated vasculitis. Front. Pharmacol. 15:1378384. doi: 10.3389/fphar.2024.1378384
Received: 22 February 2024; Accepted: 19 April 2024;
Published: 20 May 2024.
Edited by:
Vincenzo Montinaro, Ospedale Generale Regionale Francesco Miulli, ItalyReviewed by:
Vincenzo Di Leo, Azienda Ospedaliero Universitaria Consorziale Policlinico di Bari, ItalyFrancesca Cianciotta, ASLBari—Azienda Sanitaria Localedella Provincia di Bari (ASL BA), Italy
Copyright © 2024 Liu, Tian, Chen, Zhang, Chen, Chen, Lin, Wu, Wu, Wu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kefei Wu, d3VrZWZlaTIwMTJAMTYzLmNvbQ==; Qinghua Liu, bGl1cWh1YTZAbWFpbC5zeXN1LmVkdS5jbg==
†These authors have contributed equally to this work
 Weijun Liu
Weijun Liu Guanyuan Tian1†
Guanyuan Tian1† Mingying Zhang
Mingying Zhang Qinghua Liu
Qinghua Liu