- 1Department of Family and Community Medicine, University of Cincinnati, Cincinnati, OH, United States
- 2Center for Clinical and Translational Science and Training, University of Cincinnati, Cincinnati, OH, United States
- 3Cancer Center, University of Cincinnati, Cincinnati, OH, United States
- 4Department of Pediatrics, Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center/University of Cincinnati, Cincinnati, OH, United States
Introduction: Academic research centers often struggle to recruit and retain a well-trained and diverse clinical and translational science (CTS) workforce. In particular, the clinical research professional (CRP) career pathway is not well known to undergraduate students and other individuals outside of academic medicine despite being a potential career route. To address these workforce challenges, the CRP Task Force at the University of Cincinnati (UC) aims to train a competent and diverse CRP workforce through targeted educational programming in the UC undergraduate population.
Methods: Using a six-step curriculum development process that included: 1) performing a needs assessment, 2) determining content, 3) writing goals and objectives, 4) selecting the educational strategies, 5) implementing the curriculum, and 6) evaluating the curriculum, we designed an undergraduate certificate program in CTS.
Results: The needs assessment included both internal and external data gathering to inform curriculum development and program decisions. Content was determined using the Core Competency Framework for the Clinical Research Professional Version 3.1., and program learning outcomes were written with both the competency framework and local workforce needs in mind. Educational strategies were selected based on optimization of available resources and local expertise with an emphasis on interactive didactics complemented by experiential learning. Implementation is underway and evaluation will follow once students begin enrolling.
Discussion: By educating an undergraduate student population about CTS methods and career opportunities, we anticipate increased numbers of well-qualified, diverse applicants who pursue CRP careers locally and regionally.
1 Introduction
Academic research centers frequently face challenges in the recruitment and retention of well-trained, diverse clinical research professionals (CRPs) for multiple reasons, including a lack of professional identity characterized by insufficient training programs, ill-defined pathways for career advancement, and feelings of low value and burnout (Knapke and Jenkerson, 2022; Knapke and Snyder, 2022; Freel et al., 2023). Freel, et al. (2023) provides a compelling summary of the alarming scale of the problem nationally, and the risk the problem poses to the integrity, quality, and innovation of clinical and translational science (CTS) in the United States. Although CRP retention has not been well-studied in academic medical centers, the turnover rate in healthcare averaged 22.7% in 2022 (‘2023 NSI National Health Care Retention & RN Staffing Report’, 2023). In clinical research organizations (CROs), the average turnover rate from 2017 to 21 was 26.2% (‘2022/23 Clinical Research Organization Insights Report: Managing Talent and Pay in a Competitive Market and Volatile Economy’, 2023). However, it is difficult to compare staffing trends in healthcare and industry to academic research environments. Duke University reported a reduction in CRP turnover from 23% to 16% following implementing a competency-based workforce initiative (Stroo et al., 2020). The COVID-19 pandemic exacerbated CRP workforce problems; one study found that 37% of academic research centers reported decreased staffing and increased turnover as a result of the pandemic (Samuels et al., 2023). Managers and principal investigators (PIs) at the Cincinnati Academic Health Center (AHC) face similar problems to those seen at the national level. The Cincinnati AHC is comprised of three hospitals and one academic institution: the University of Cincinnati Medical Center (UCMC), Cincinnati Children’s Hospital Medical Center (CCHMC), the Cincinnati VA, and the University of Cincinnati (UC), which includes the Colleges of Medicine, Nursing, Allied Health, and Pharmacy on its health sciences campus. Combined, UC and CCHMC employ approximately 1,200 CRPs, but both organizations struggle to recruit and retain a CTS workforce locally, mirroring similar challenges at the national level. During the 2022 fiscal year, turnover rates at both institutions ranged from 18.7% to 37.5%, with the highest turnover rates occurring in the early-to mid-level titles. Turnover rates at these levels introduce a critical roadblock to sustaining high-quality clinical and translational research (CTR) implementation and management.
To overcome these workforce challenges, leaders at the Cincinnati AHC organized a CRP Task Force comprised of key stakeholders from the Center for Clinical and Translational Science and Training (CCTST), the UC Cancer Center, the UC Office of Clinical Research, the Department of Environmental and Public Health Sciences, the UC College of Education, Criminal Justice and Human Services, UC Human Resources, and the Department of Pediatrics/CCHMC. The goal of the Task Force is to develop and implement strategies to recruit, train, and retain CRPs to support the clinical research enterprise at the Cincinnati AHC. Three workgroups within the task force were formed to focus on recruitment, education, and retention. The work described in this paper was completed by the education workgroup, whose goals are to support and promote for-credit training opportunities and non-credit professional development for new and existing CRPs.
Despite the critical role CRPs play in the generation of evidence to support better health outcomes for both individuals and populations, this career pathway is not well known to undergraduate students and other individuals outside of academic medicine despite being a potential career route. Summer research programs for undergraduates and medical students are the most common method for introducing students to research (Black et al., 2013; Kolber et al., 2016; Howell et al., 2019; Avila et al., 2022). Summer programs can also be an effective way to introduce underrepresented minority students to research and prepare them for CTS career pathways (Ghee et al., 2016; Smalley and Warren, 2020; Prince et al., 2023). In Arkansas, an undergraduate curriculum rooted in a real-world CTS study was developed, offered, and evaluated, demonstrating high satisfaction among learners (James et al., 2023). Temple University School of Medicine requires medical students to complete 2 week training in CTS and one CTS scholarly activity during their 4 years of medical school (Feldman, 2015). Evidence suggests that virtual programming is an effective training method when in-person is not feasible (Corson et al., 2021; Lemacks et al., 2022; James et al., 2023). Evidence also suggests that research experience during undergraduate study increases students’ awareness of career options, improves their preparation for graduate training, and ultimately impacts their decisions to pursue advanced degrees and careers related to research (Seymour et al., 2004; Hunter et al., 2007; Adedokun et al., 2012; Yaffe et al., 2014).
Locally, we coordinate several efforts to introduce students to research principles and careers. Every semester, the workforce development core of our Center for Clinical and Translational Science and Training visits undergraduate courses across several programs to introduce students to CTS careers and training opportunities. Research 101 is an asynchronous research primer available to medical students and summer research students (Blackard et al., 2022; 2023). Every summer, the Summer Undergraduate Research Fellowship (SURF) program awards research fellowships to 150 undergraduate students from UC and other institutions. The Office of Undergraduate Research on UC’s main campus also provides programs and resources to help students access research experiences across an array of disciplines. However, currently, there is no formal training pathway specific to CTS that results in a major, minor, or certificate for undergraduates at UC. In order to introduce and better prepare undergraduate students for careers in CTS, the education workgroup of the CRP Task Force at the Cincinnati AHC sought to develop a competency-based, for-credit undergraduate certificate program by undertaking a six-step curriculum development process.
2 Pedagogical frameworks
Two pedagogical frameworks informed our task: existing CRP competencies and an established six-step curriculum development method. We began with CRP competencies that were developed by a national consortium of medical association leaders and industry collaborators called the Joint Task Force (JTF) for Clinical Trial Competency, organized by the Multi-Regional Clinical Trials (MRCT) Center of Brigham and Women’s Hospital and Harvard. This framework has undergone multiple iterations between 2014-20; we utilized the most recent “Core Competency Framework for the Clinical Research Professional Version 3.1.” (Sonstein et al., 2014; 2020; JTF Task Force, 2017). The Core Competency Framework for the CRP Version 3.1 defines 49 competency statements that address CRP knowledge, skills, and attitudes under 8 scientific domains: 1) Scientific Concepts and Research Design, 2) Ethical and Participant Safety Considerations, 3) Investigational Products Development and Regulation, 4) Clinical Study Operations (Good Clinical Practice), 5) Study and Site Management, 6) Data Management and Informatics, 7) Leadership and Professionalism, and 8) Communications and Teamwork. Additionally, we utilized a six-step curriculum development process described by Schneiderhan, Guetterman and Dobson (2019) that included: 1) performing a needs assessment, 2) determining content, 3) writing goals and objectives, 4) selecting the educational strategies, 5) implementing the curriculum, and 6) evaluating the curriculum.
3 Learning environment
UC is designated a “very high research activity” university by the Carnegie Commission, holding ∼$206.6 million in grants in 2019 with $89.4 million coming from the NIH. The College of Medicine received $105.3 million in sponsored awards in 2019 and was ranked in the top 38% of medical schools for research in the 2020 U.S. News and World Report rankings. The College of Medicine is composed of 23 departments, 5 basic science and 18 clinical, which retain in excess of 2,000 faculty. CCHMC is a 700-bed non-profit organization serving as the AHC’s major teaching facility for pediatrics and as the only children’s hospital in the Cincinnati metropolitan area (population 2.3 million). Of 184 pediatric institutions surveyed nationally, CCHMC is consistently ranked top 3 in the Honor Roll of America’s Best Children’s Hospitals compiled by U.S. News & World Report. CCHMC has a major emphasis on research and held over $240 million in grants with over $161 million coming from the NIH in 2019. The two institutions are located on the same campus and have a long record of close collaboration. There are constant interactions between researchers and clinicians, and CCHMC faculty hold dual appointments in the UC College of Medicine. The institutions are administratively linked in many endeavors ranging from clinical to research and education. This emphasis on research impacts the learning environment in a multitude of ways (e.g., collaborations across faculty research, training grants, core facilities, and CRP training). UC’s undergraduate population includes approximately 40,000 students, with a quarter identifying as a racial or ethnic minority. Reaching a small fraction of those students and introducing them to CTS principles and career opportunities could have a major impact on local workforce development.
4 Methods
The education subgroup of the CRP Task Force followed the six-step curriculum development process outlined by Schneiderhan, Guetterman and Dobson (2019) to design an undergraduate certificate program in CTS.
4.1 Needs assessment
An educational needs assessment is a data-gathering exercise to understand what the needs for a particular discipline or group of learners are and why a curriculum should be developed and implemented. It can include a wide range of data sources: consultations with those familiar with the field and/or potential learners, data-driven descriptions of an educational gap in a particular discipline, or accreditation or regulatory specifications (e.g., Accreditation Council for Graduate Medical Education requirements) that must be achieved.
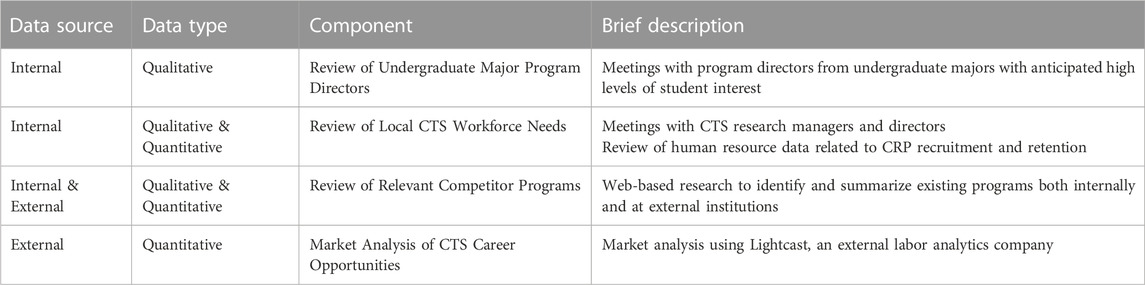
Our needs assessment included four components. We gathered information from local CTS leaders about the undergraduate majors where most of their employees come from, and then we conducted an internal review with program directors from these programs, seeking to better understand the major curricula and their students’ educational needs and career interests. We also provided the directors with an overview of CTS careers and noted their perceptions of how well an undergraduate certificate would fit the needs and interests of their student populations. We worked with local CTS leaders and Human Resources to conduct an internal review of employment needs within the local CTS research workforce. We reviewed and summarized relevant competitor programs (both internal and external). When reviewing external programs, we focused on direct competitors: undergraduate certificate programs offered by 4-year universities. Finally, we completed an external market analysis to better understand career opportunities for potential graduates. These components occurred simultaneously over approximately 6 months and are described in Table 1.
4.2 Determine content
The next step was to consider areas of content that should be included in the curriculum, making decisions about what to focus on and prioritize. Subject matter experts are important to include in this step of the process, as they are familiar with large thematic areas as well as content specifics that could inform the organization of the training program or coursework. Our process for determining content included two components: a review and prioritization of existing competencies and a review of relevant undergraduate courses that already existed at our institution.
Using the Core Competency Framework for the CRP Version 3.1 as a foundation, we carefully reviewed the competencies with subject matter experts (including a CRP, a CRP manager, and a CTS director) to determine areas of prioritization that would best support the types of studies commonly conducted at our AHC. We categorized each competency as essential, important, or not needed in an entry-level CRP position. We also adjusted competency language when necessary to make competency achievement feasible in undergraduate learners, e.g., lowering the level of competency to “understanding” or “summarizing” rather than “analyzing” or “evaluating” (Bloom, 1956). We also noted competencies that should be introduced in the certificate curriculum, but that would be further explicated as part of employee onboarding and/or required training.
The second component of our content determination process was reviewing existing courses at our institution that were relevant to the content areas within the JTF competencies. This entailed searching for several keywords within the course catalog, collating a list of potential course numbers, and then examining the internal course management system and reviewing details such as course descriptions and student learning outcomes for alignment with program competencies. The “determine content” step of the curriculum development process resulted in an early draft of required courses for the certificate program.
4.3 Write goals and objectives
Once content areas were identified and prioritized using the Core Competency Framework for the CRP Version 3.1, we established goals and objectives for the certificate program. Schneiderhan, Guetterman and Dobson (2019) draw an important distinction between goals and objectives: goals are broad and general statements of knowledge or skill that learners should attain, while objectives are specific and measurable outcomes learners should achieve after program completion. Goals were drawn from the content areas outlined in step two, and objectives were more specific summaries of the competencies to be achieved. We chose the verbs for our objectives carefully, focusing on achievement that could be measured (e.g., describe or compare) as opposed to more vague characterizations of achievement (e.g., know or appreciate).
4.4 Select educational methods
Given the plethora of methods available to contemporary educators (e.g., lectures, flipped classrooms, case studies, experiential learning, hands-on skill delivery, web-based synchronous or asynchronous learning, role plays, etc.), selecting strategies to effectively facilitate the curriculum was a critical step in the development process. Strategy selection required us to give holistic consideration to several elements of the program that had been identified and described in the first three steps: the needs of the disciplinary field and the learners (step 1), effective content delivery based on these needs (step 2), and the optimal methods to support and measure achievement of program learning objectives (step 3). As we considered strategies to teach undergraduate students introductory principles of CTS, we consulted with stakeholders who had knowledge regarding two key facets that would impact our training strategies: 1) the real-life challenges and opportunities when engaging with an undergraduate student population, and 2) the on-the-job needs of a new CRP hire. We also consulted with potential instructors of the content areas to talk through benefits and barriers of different methods of content delivery.
4.5 Curriculum implementation
Implementation of the curriculum encompassed several discrete but related tasks such as identifying the necessary resources (e.g., personnel, time, facilities, and budget), obtaining any necessary internal and external stakeholder support, designing an educational management plan that includes logistical details regarding curriculum components, educational methods, barrier mitigation, and other implementation processes such as learner recruitment, retention, and program completion. The final step is actual delivery of the curriculum to learners, sometimes via pilot rollouts or a phased approach over time. In our case, several of these tasks had been discussed in earlier steps of the development process but this step brought them all together in a formal program proposal required by our institution for the new program approval process. During this step, we brainstormed and contacted potential course instructors, discussed admission requirements, considered budgetary or logistical limitations, and identified existing resources at our institution that could be leveraged to implement or improve educational methods.
4.6 Curriculum evaluation and improvement
Evaluation is an essential element to any educational program, not only for continuous program improvement but also for reporting program outcomes to key stakeholders. Evaluation is iterative in nature, often including formative (process) and summative (outcome) evaluation methods. Schneiderhan, Guetterman and Dobson (2019) describe a five-step curriculum evaluation process: 1) determine how evaluation results will be used, 2) identify the best metrics for evaluating objective achievement, 3) collect data, 4) analyze data, and 5) improve the program using results. Our evaluation planning included an exploration of data that would be obtained through the common administrative processes at our institution, identified gaps within those data that we determined were important in order to measure program success, and developed measures and accompanying processes to collect data in order to effectively evaluate the program. We gave careful consideration to whom these data would be important to (e.g., key stakeholders, institutional administrators, and potentially granting agencies who may support our training efforts), and we discussed ways to embed evaluation measures into learner assessments at the course level. We also developed a utilization plan for evaluation results, designed to promote regular review of evaluation data and integration of curriculum changes annually, as needed and informed by evaluation results.
5 Results
5.1 Needs assessment
5.1.1 Review of undergraduate major program directors
Our information-gathering from local CTS leaders identified Biological Sciences, Medical Sciences, Psychology, and Public Health as the most common undergraduate majors held by their employees, allowing us to select these as programs that could potentially yield high numbers of interested students. Meetings with the program directors of these four majors led us to conclude that an undergraduate certificate was the appropriate educational path to pursue due to limited room for additional credits in student major curricula, as well as student preference for a certificate rather than a minor. Program directors were unanimously in favor of development of the program. The majority were unaware of CTS career pathways that might be appropriate for their graduates, but felt there would be high levels of interest from their students and that the skills taught in such a certificate program would be new yet complementary to content offered through existing courses. These programs also offer significant numbers of majors: approximately 900 in Biological Sciences, 375 in Medical Sciences, 1,000 in Psychology, and 125 in Public Health.
5.1.2 Review of local CTS workforce needs
In addition, our meetings with CTS research managers and directors at the Cincinnati AHC led to a better understanding of the workforce challenges they have faced, revealing that although recruitment and retention have long plagued the CTS field, the COVID-19 pandemic exacerbated the problem, and the workforce has not recovered. The CRP workforce at the Cincinnati AHC includes approximately 1,200 positions, encompassing titles from clinical research assistant (high school diploma required) to clinical research director (master’s required, some staff have doctorates). UC employs approximately 400 CRPs and CCHMC employs approximately 800 CRPs. Additionally, several corporate Clinical Research Organizations (CROs) operate large offices in the Cincinnati area, primarily specializing in clinical trials. In 2022, turnover rates at the Cincinnati AHC varied from 20% to 37.5% at CCHMC and 19%–32% at UC, with the highest rates occurring in the entry- and median-level position titles. A search of job postings in July 2023 using “clinical research” as a keyword results in 389 results at UC and 247 at CCHMC.
5.1.3 Review of relevant competitor programs
We reviewed potential competitor programs both at UC and at external institutions. We found no similar programs locally, but web-based research allowed us to summarize primary components of external competitor programs as shown in Table 2. An important discovery within this review was that all of the existing programs in our geographic region were only open to students enrolled at those universities (i.e., UC students could not enroll in them).
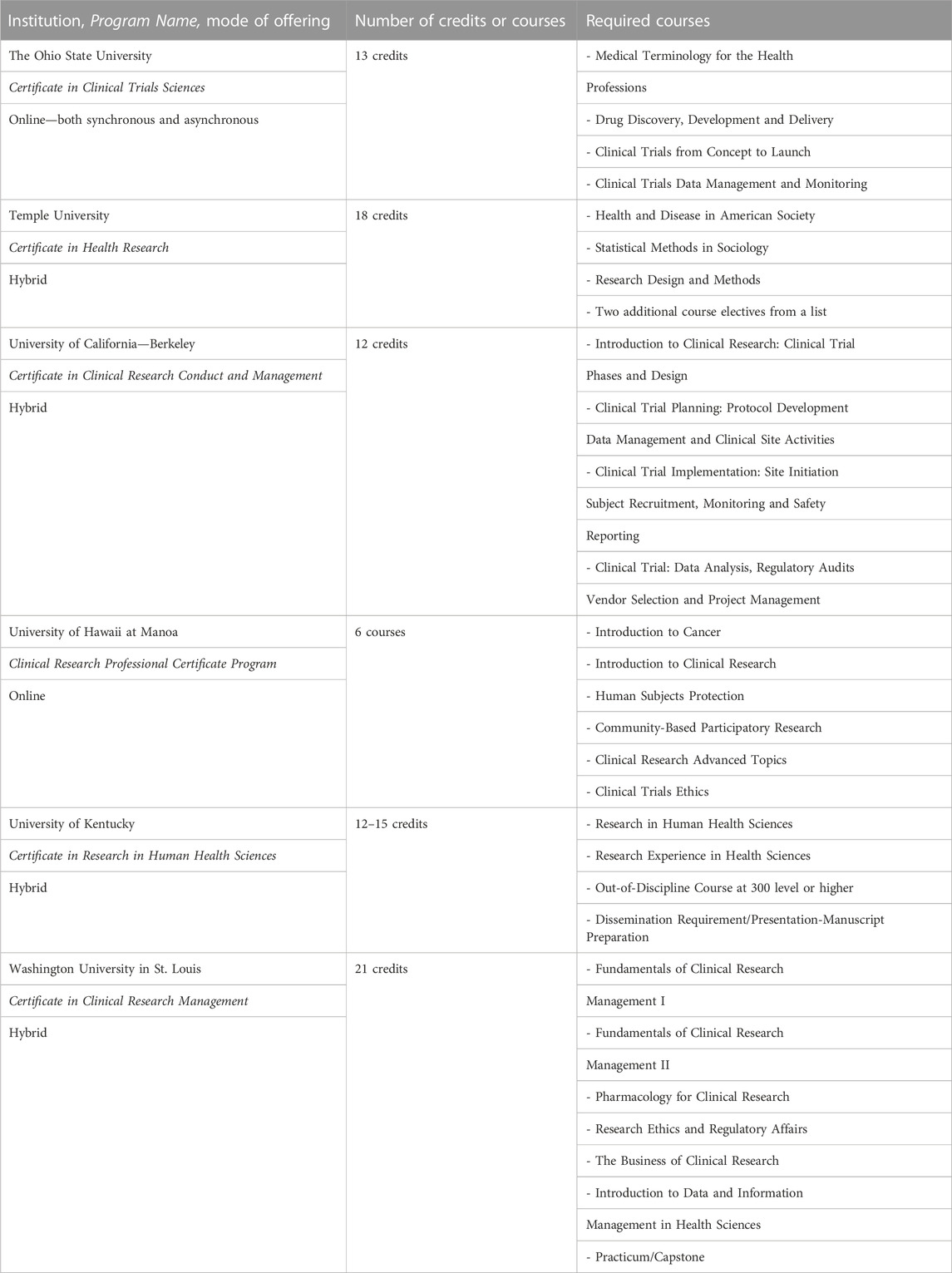
TABLE 2. External undergraduate certificate programs with institution, program name, mode of offering, number of credits, and required courses.
5.1.4 Market analysis of CTS career opportunities
In addition to the local market needs described above, we worked with UC Online to conduct a market analysis using Lightcast. (Lightcast—Labor Market Analytics, 2023). The Lightcast report, run in June 2023, found over 13,000 unique job postings for CRP positions with a median advertised salary of $78,600. The median income for CRPs from June 2022 to May 2023 showed a steep increase of 16% because the number of open jobs currently exceeds the supply of qualified applicants. The minimum education levels for employment were: 11% required a high school diploma or GED, 11% required an associate’s degree, and 78% required a bachelor’s degree. Given that large majority of entry level jobs require a bachelor’s degree, we determined that students graduating with a baccalaureate degree would benefit from targeted training in CTS in the form of a certificate that would complement their major curricula. Colleges and universities were the top employers of CRPs.
5.2 Determining content
The competency review process generated a final list of prioritized competencies that are essential and/or important to an undergraduate learner who might begin an entry-level position after graduation. The final list acknowledged that while all of the competencies are essential or important to a CRP over the lifetime of their career, many of them will be acquired with onboarding, professional development training, and career experience; thus, some competencies need only to be introduced to undergraduate trainees so that they are aware of common processes, terms, or aspects of CTS. Table 3 provides details on how competencies were prioritized for undergraduate education. Changes to competency language in order to bring them to an undergraduate/introductory level are provided in red. Competencies that may be supported by completion of the Collaborative Institutional Training Initiative Program (CITI) training as part of employment onboarding are noted with an asterisk. Alignment with competencies was the major driving force of the content determination process, but careful review of the external programs summarized in Table 2 was also informative as we considered different ways to organize the topics into required courses.

TABLE 3. Core competency framework for the CRP version 3.1, prioritized for undergraduate education.
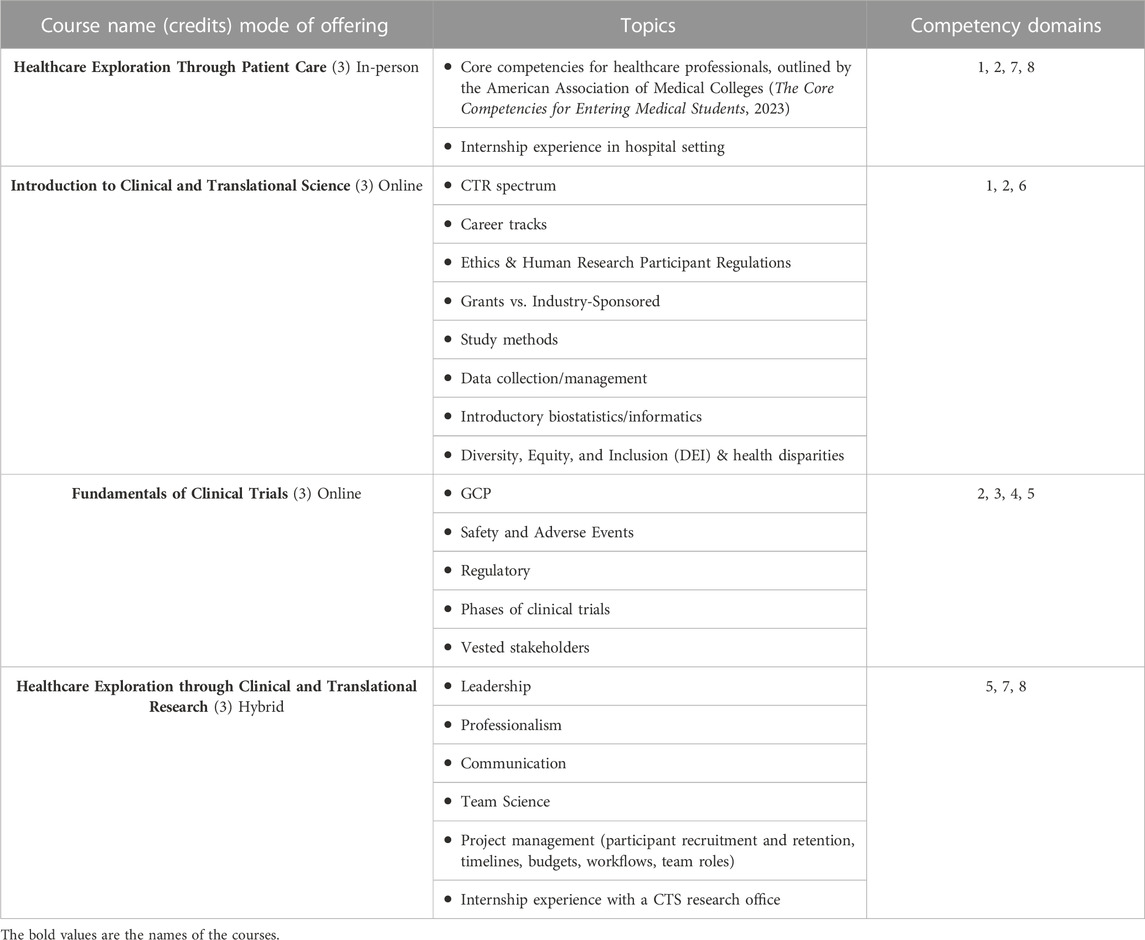
The second piece of the determination and prioritization of content entailed a thorough review of existing courses at UC that might be incorporated into a certificate curriculum. No courses were identified that were specific enough in scope to be a good fit for the certificate. Completion of this step of the curriculum development process led to development of a 12-credit curriculum detailed in Table 4, including general topics for each course as well as competency domains.
5.3 Writing goals and objectives
Steps two to three were completed concurrently: as the curriculum was being discussed, so were the goals and objectives (or student learning outcomes, in the language of our specific institution) being developed. The overarching goal for the certificate program is broad and general, following the guidelines of Schneiderhan, Guetterman and Dobson (2019): to introduce undergraduate students to the principles of CTS in order to prepare them for CTS research careers upon graduation. The objectives for the certificate program are much more specific, measurable, and grounded in the Core Competency Framework for the CRP Version 3.1:
• Explain Good Clinical Practice according to the NIH.
• Summarize the fundamental processes of clinical and translational science, including participant recruitment, addressing diversity, equity, inclusion, and accessibility, data collection and management, study site management, and financial management to support clinical research activities.
• Describe the stages of clinical trials and their relevant regulatory components.
• Demonstrate project management and communication skills in a team-based research setting.
• Connect the goals and outcomes of clinical and translational research to the goals and outcomes of patient care and population health.
5.4 Selecting educational methods
Training undergraduate students was a new concept to the majority of CRP Task Force members, so we relied heavily on the expertise of our undergraduate program directors to understand student needs when considering how best to deliver the curriculum. Two key points guided decision-making of certificate educational methods: undergraduate students are often limited in time and the number of credits they can devote to non-major curriculum requirements, and although the AHC is less than 1 mile from UC’s main campus, most undergraduates are not physically present on the AHC campus. Requiring students to attend numerous in-person courses on the AHC campus would likely prohibit their participation in the program.
Balancing student needs with the desired level of competency upon program completion, we determined a hybrid program was optimal. Two experiential learning courses were incorporated into the curriculum: a paid work experience course where students attend a weekly, 2.5 h evening seminar and work as a patient care team member at the UCMC approximately 12 h per week over one semester, and a second research experience where students work in a clinical and translational research unit at UC or CCHMC over the course of a semester while also participating in an online weekly seminar. To balance these in-person requirements with more flexibly scheduled courses, the remaining two required courses will be offered online.
Two national professional societies offer CRP credentialing: the Society of Clinical Research Associates (SOCRA) and the Association of Clinical Research Professionals (ACRP). Although the certificate will not be credentialed through SOCRA or ACRP, we plan to explore that possibility post-implementation. Both SOCRA and ACRP accept some form of CRP-related coursework as part of their credentialing process (ACRP, 2023; SOCRA, 2023). Students will be provided with certification information as part of the program as well, and they may choose to pursue CRP certification after graduation. The undergraduate certificate curriculum should help students move toward certification if desired and allow them to choose the credentialing society that best meets their needs.
5.5 Curriculum implementation and curriculum evaluation/improvement
We are currently in steps five to six of the curriculum development process, with most of the work framed around the formal approval and implementation process required by our institution. New certificate program proposals undergo a multi-step internal review process using a proposal template that includes many of the components addressed above, in addition to a financial plan to support the program. We determined minimum admission criteria: must be an undergraduate enrolled at UC, minimum 2.5 grade point average, must include a personal statement describing educational interests and career goals, and must include one letter of support from a faculty member or professional manager. We identified a program director and a program coordinator to manage administrative tasks and advise students, as well as core faculty for the new courses, supporting their development of syllabi. We collaborated with the Office of Undergraduate Education within the College of Medicine to determine what baseline administrative support they offer, such as course ordering and course evaluation. We also developed an evaluation plan to supplement basic course evaluations; it includes an annual student focus group and alumni survey to evaluate learner satisfaction and career outcomes, identifying areas of strength and improvement.
6 Discussion, acknowledgement of limitations, and lessons learned
The six-step curriculum development process achieved several critical goals as we sought to establish an undergraduate training program in CTS. The results of our needs assessment not only supported anecdotal evidence we had from informal exchanges with principal investigators and clinical research directors, but also uncovered important new information we had not previously considered, particularly related to the national landscape (e.g., typical minimum educational requirements for an entry-level job and income trends). Steps one to five allowed us to engage with key stakeholders in meaningful ways, guiding information-gathering and decision-making in order to design the best possible program using national competencies while also leveraging institutional strengths and addressing the unique needs of our local student population.
This project had several limitations. We have not completed the final two steps of the process: implementation and evaluation. The major work of developing the curriculum is accomplished, however, and we anticipate our program proposal will be approved in 2024, with a soft launch of the new program shortly after. A second limitation is the informal way in which we collected qualitative data from stakeholders in needs assessment. We kept meeting notes in this early phase, not recording or transcribing what was said in order to allow for more careful review. We mitigated this limitation by continuing to engage stakeholders throughout, sharing results and obtaining their feedback as the curriculum came together. Future work following the process outlined above would benefit from formalized data collection and analysis procedures so that they may be reported more fully and replicated when desired.
Our CRP Task Force learned several lessons during the development process, which we wish to present here for others working in CTS education. The first is the importance of identifying key stakeholders and working to build bridges and relationships early in the process. Continuous engagement with a diverse group of stakeholders—spanning content experts working in the CTS field, educators knowledgeable about institutional policies and undergraduate student needs, and curriculum development and evaluation experts familiar with CTS workforce development—benefited us throughout the process, helping to identify the right individuals with whom to confer so that we avoided potential missteps. A second lesson learned is to leverage existing resources wherever possible, particularly at large academic institutions where infrastructure to support new training and programming is already in place. Our capacity may have been limited by the grant funding we rely upon to do our work but combining our grant-funded efforts with the vast resources available at our institution expanded our capability far beyond the grant-specific portion. A final suggestion to others pursuing this type of project is not to become too attached to particular plans or ideas early in the process. In our experience, plans shifted regularly throughout each step and an unwillingness to change course or adapt to new information would have hindered progress.
The curriculum development process described by Schneiderhan, Guetterman and Dobson (2019) and followed in the study presented proved an effective framework to develop a new undergraduate certificate program in CTS. It provided a systematic approach to a potentially daunting task, breaking it down into manageable components. Following the process allowed for regular stakeholder engagement and provided a clear path to completion, generating enthusiasm for the positive impact this undergraduate certificate may have on our local CTS workforce.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JK: Writing–original draft, Writing–review and editing. MM: Writing–review and editing. AM: Writing–review and editing. PR: Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Work for this manuscript was supported by the CCTST at the University of Cincinnati, which is funded by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant UL1TR001425. The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences (NCATS). This information or content and conclusion are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by NIH, NCATS, or the U.S. Government.
Acknowledgments
The authors wish to acknowledge other members of the education workgroup who contributed to the curriculum development process: Nathaniel Harris, John (Jack) Kues, Karen Ramos, Nicky Kurtzweil, Melissa Loyd, Regan Johnson, and Scott Langevin. We also acknowledge Gina Nilsson and Brandi Bittner from UC Online for their support with the Lightcast market analysis. Finally, we acknowledge Dr. Anil Menon, Associate Dean of Undergraduate Education at the UC College of Medicine, for sharing his wisdom and resources throughout the process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2022/23 Clinical Research Organization Insights Report, 2023 2022/23 Clinical Research Organization Insights Report (2023). Managing talent and Pay in a competitive market and volatile Economy. Virginia, United States BDO USA. Available at: https://www.bdo.com/getmedia/a6fb62d9-36f2-46d9-a053-deeffc84ca30/TAX_GES_2022-2023-BDO-CRO-Insights-Report.pdf?ext=.pdf (Accessed: October 20, 2023).
2023 NSI National Health Care Retention & RN Staffing Report, 2023 2023 NSI National Health Care Retention & RN Staffing Report (2023). Nursing solutions, inc. Available at: https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf (Accessed October 20, 2023).
Acrp, (2023). CCRC certification. Available at: https://acrpnet.org/certification/crc-certification/ (Accessed: October 20, 2023).
Adedokun, O., Zhang, D., Parker, L., Bessenbacher, A., Childress, A., and Burgess, W. (2012). Understanding how undergraduate research experiences influence student aspirations for research careers and graduate education. J. Coll. Sci. Teach. 42 (1), 82–90.
Avila, A. H., Weixelbaum, J. H., and Compton, W. M. (2022). The national institute on drug abuse summer research internship program: building a diverse national scientific workforce. Neuropsychopharmacology 47 (13), 2184–2188. doi:10.1038/s41386-022-01377-3
Black, M. L., Curran, M. C., Golshan, S., Daly, R., Depp, C., Kelly, C., et al. (2013). Summer research training for medical students: impact on research self-efficacy. Clin. Transl. Sci. 6 (6), 487–489. doi:10.1111/cts.12062
Blackard, J. T., Knapke, J. M., Ryan, P. H., Schuckman, S., Veevers, J., Hardie, W. D., et al. (2022). Research 101: an online course introducing medical students to research. J. Clin. Transl. Sci. 6 (1), e102. doi:10.1017/cts.2022.435
Blackard, J. T., Knapke, J. M., Schuckman, S., Veevers, J., Hardie, W. D., and Ryan, P. H. (2023). Introducing trainees to research using an online, asynchronous course. J. Clin. Transl. Sci. 7 (1), e155. doi:10.1017/cts.2023.579
Bloom, B. (1956). Taxonomy of educational objectives, handbook I: the cognitive domain. 2nd edn. New York: David McKay Co Inc.
Corson, T. W., Hawkins, S. M., Sanders, E., Byram, J., Cruz, L. A., Olson, J., et al. (2021). Building a virtual summer research experience in cancer for high school and early undergraduate students: lessons from the COVID-19 pandemic. BMC Med. Educ. 21 (1), 422. doi:10.1186/s12909-021-02861-y
Feldman, A. M. (2015). Incorporating clinical and translational science into the undergraduate medical education curriculum. Clin. Transl. Sci. 8 (4), 267. doi:10.1111/cts.12333
Freel, S. A., Snyder, D. C., Bastarache, K., Jones, C. T., Marchant, M. B., Rowley, L. A., et al. (2023). Now is the time to fix the clinical research workforce crisis. Clin. Trials 20, 457–462. doi:10.1177/17407745231177885
Ghee, M., Keels, M., Collins, D., Neal-Spence, C., and Baker, E. (2016). Fine-tuning summer research programs to promote underrepresented students’ persistence in the STEM pathway. CBE—Life Sci. Educ. Marsteller 15 (3), ar28. doi:10.1187/cbe.16-01-0046
Howell, L. P., Wahl, S., Ryan, J., Gandour-Edwards, R., and Green, R. (2019). Educational and career development outcomes among undergraduate summer research interns: a pipeline for pathology, laboratory medicine, and biomedical science. Acad. Pathol. 6, 2374289519893105. doi:10.1177/2374289519893105
Hunter, A.-B., Laursen, S., and Seymour, E. (2007). Becoming a scientist: the role of undergraduate research in students’ cognitive, personal, and professional development. Sci. Educ. 91 (1), 36–74. doi:10.1002/sce.20173
James, L., Venable, T., Caro, A., Moran, J. H., Nesmith, C., Gannon, M. A., et al. (2023). Development of a clinical and translational research curriculum for undergraduate students. J. Clin. Transl. Sci. 7 (1), e118. doi:10.1017/cts.2023.532
JTF Task Force (2017). The Joint task force for clinical trial competency and the harmonized core competency framework for the clinical research professional. Available at: https://mrctcenter.org/clinical-trial-competency/framework/domains/ (Accessed August 15, 2023).
Knapke, J. M., Jenkerson, M., Tsao, P., Freel, S., Fritter, J., Helm, S. L., et al. (2022). Academic medical center clinical research professional workforce: Part 2 – issues in staff onboarding and professional development. J. Clin. Transl. Sci. 6 (1), e81. doi:10.1017/cts.2022.412
Knapke, J. M., Snyder, D. C., Carter, K., Fitz-Gerald, M. B., Fritter, J., Kolb, H. R., et al. (2022). Issues for recruitment and retention of clinical research professionals at academic medical centers: Part 1 – collaborative conversations Un-Meeting findings. J. Clin. Transl. Sci. 6 (1), e80. doi:10.1017/cts.2022.411
Kolber, B. J., Janjic, J. M., Pollock, J. A., and Tidgewell, K. J. (2016). Summer undergraduate research: a new pipeline for pain clinical practice and research. BMC Med. Educ. 16 (1), 135. doi:10.1186/s12909-016-0648-7
Lemacks, J. L., Greer, T., Aras, S., Iverson, C., Willis, D., Duplantis, T., et al. (2022). Mississippi INBRE Outreach Scholars program: adapting a summer scholars program to the virtual world amidst the COVID-19 pandemic. Adv. Physiology Educ. 46 (3), 472–480. doi:10.1152/advan.00026.2021
Lightcast - Labor Market Analytics (2023). Lightcast. Available at: https://www.lightcast.io (Accessed: August 22, 2023).
Prince, L. Y., Williams, T. B., Allen, A. R., McGehee, R. E., and Thomas, B. R. (2023). Outcomes of the UAMS summer undergraduate research program to increase diversity in research and health professions. Adv Physiology Educ. 47 (1), 20–25. doi:10.1152/advan.00201.2022
Samuels, M. H., Hommeyer, E., Booty, B., Frost, K., and Morris, C. (2023). Impact of the COVID-19 pandemic on CTSA clinical research centers over 2 years. J. Clin. Transl. Sci. 7 (1), e116. doi:10.1017/cts.2023.543
Schneiderhan, J., Guetterman, T. C., and Dobson, M. L. (2019). Curriculum development: a how to primer. Fam. Med. Community Health 7, e000046. doi:10.1136/fmch-2018-000046
Seymour, E., Hunter, A. B., Laursen, S. L., and DeAntoni, T. (2004). Establishing the benefits of research experiences for undergraduates in the sciences: first findings from a three-year study. Sci. Educ. 88 (4), 493–534. doi:10.1002/sce.10131
Smalley, K. B., and Warren, J. C. (2020). Disparities elimination summer research experience (DESRE): an intensive summer research training program to promote diversity in the biomedical research workforce. Ethn. Dis. 30 (1), 47–54. doi:10.18865/ed.30.1.47
SOCRA (2023). Certification: candidate eligibility. Available at: https://www.socra.org/certification/ccrp-certification-exam/candidate-eligibility/ (Accessed: October 20, 2023).
Sonstein, S. A, Seltzer, J., Li, R., Silva, H., Jones, C. T., and Daemen, E. (2014). Moving from compliance to competency: a harmonized core competency framework for the clinical research professional. Clin. Res. 28 (3), 17–23. doi:10.14524/CR-14-00002R1.1
Sonstein, S. A., Namenek Brouwer, R. J., Gluck, W., Robert Kolb, H., Aldinger, C., Bierer, B. E., et al. (2020). Leveling the Joint task force core competencies for clinical research professionals. Ther. Innovation Regul. Sci. 54 (1), 1–20. doi:10.1007/s43441-019-00024-2
Stroo, M., Asfaw, K., Deeter, C., Freel, S. A., Brouwer, R. J. N., Hames, B., et al. (2020). Impact of implementing a competency-based job framework for clinical research professionals on employee turnover. J. Clin. Transl. Sci. 4 (4), 331–335. doi:10.1017/cts.2020.22
The Core Competencies for Entering Medical Students (2023). Association of American medical Colleges. Washington, D.C. Available at: https://students-residents.aamc.org/applying-medical-school/article/core-competencies.
Keywords: workforce development, clinical and translational science, clinical and translational research, curriculum development, undergraduate research training, clinical research professional
Citation: Knapke J, Marcum M, Mendell A and Ryan P (2023) Development of an undergraduate certificate in clinical and translational science: improving competence of the clinical research workforce. Front. Pharmacol. 14:1294534. doi: 10.3389/fphar.2023.1294534
Received: 14 September 2023; Accepted: 13 November 2023;
Published: 06 December 2023.
Edited by:
Stephen Sonstein, Eastern Michigan University, United StatesReviewed by:
Kimberly McCall, University of Alabama at Birmingham, United StatesAudra N. Iness, Baylor College of Medicine, United States
Jared Kerr, University of North Carolina Wilmington, United States
Copyright © 2023 Knapke, Marcum, Mendell and Ryan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jacqueline Knapke, a25hcGtlamVAdWMuZWR1
 Jacqueline Knapke
Jacqueline Knapke Michelle Marcum
Michelle Marcum Angela Mendell
Angela Mendell Patrick Ryan2,4
Patrick Ryan2,4