- 1Department of Hand Surgery/Foot and Ankle Surgery, Shengli Oilfield Central Hospital, Dongying, Shandong, China
- 2Dongying Vocational Institute, Dongying, Shandong, China
- 3Department of Bone/Joint Surgery and Sports Medicine Center, The First Affiliated Hospital of Jinan University, Guangzhou, Guangdong, China
Objective: The present systematic review and meta-analysis aimed to estimate the prophylactic effect of alpha blockers against postoperative urinary retention (POUR) in orthopaedic patients.
Methods: PubMed, Embase, Web of Science and Cochrane Library databases were searched between 1 January 1990 and 1 March 2023. The studies reporting the preventive efficacy of alpha blockers on POUR after orthopaedic procedures were identified. The pooled rates of POUR in the Intervention group (patients receiving alpha blockers) and the Control group (patients not receiving alpha blockers) were estimated and compared. The risk ratios (RRs) were calculated using the random-effects model. Subgroup analysis was performed based on surgical type. Trial sequential analysis (TSA) was conducted to confirm the robustness of pooled results.
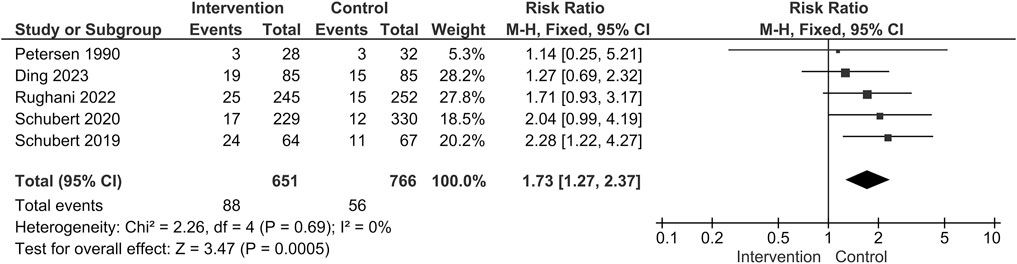
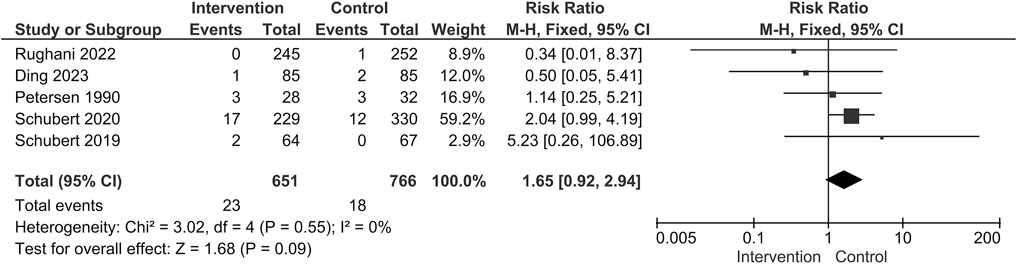
Results: Seven studies containing 1,607 patients were identified. The rates of POUR were similar between the two groups (Intervention group: 126/748 [16.8%] VS. Control group: 168/859 [19.6%]; RR = 0.75; 95% confidence interval [CI] 0.51 to 1.09; p = 0.130; Heterogeneity: I2 = 67.1%; p = 0.006). No significant difference in the incidence of POUR was observed in either the Arthroplasty subgroup or Spine surgery subgroup. The result of TSA suggested that the total sample size of the existing evidence might be insufficient to draw conclusive results. Administrating alpha blockers was associated with a higher risk of complications (88/651 [13.5%] VS. 56/766 [7.3%]; RR = 1.73; 95% CI 1.27 to 2.37; p = 0.0005; Heterogeneity: I2 = 0%; p = 0.69).
Conclusion: Prophylactic alpha blockers do not reduce the risk of POUR in orthopaedic procedures, and administrating these drugs was associated with a higher risk of complications.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=409388.
1 Introduction
Postoperative urinary retention (POUR) is generally defined as the difficulty in completing micturition in the presence of a full bladder after surgery (Darrah et al., 2009). The incidence of POUR ranges from 3% to 70% depending on the type of surgery (Baldini et al., 2009). This variability is also evident in the field of orthopaedic surgery. Törn et al. documented a POUR prevalence of 75% among patients undergoing total joint arthroplasty (Törn et al., 1994). Boulis et al. reviewed the records of 503 patients following spine surgery and observed a POUR incidence of up to 38% (Boulis et al., 2001). POUR is distressing and painful for patients and can affect postoperative outcomes and patient satisfaction. Although catheterization is often deemed an effective solution for POUR, the intervention itself is usually uncomfortable and can introduce the risk of increased hospital expenses and delayed discharge (Foxman, 2003; Parker et al., 2017).
POUR and the use of urinary catheterization may increase the predisposition to urinary tract infections (UTIs), which is a risk factor for the development of implant-related infection, a catastrophic complication in orthopaedic procedures (Yoon and King, 2020; Pertsch et al., 2021; Wang et al., 2021). Hence, there has been a growing endorsement of pharmacologic interventions aimed at reducing POUR occurrence in orthopaedic procedures.
Alpha blockers have been approved for the treatment of hypertension, benign prostatic hyperplasia and neurogenic bladder (Khoury and Kaplan, 1991; Kakizaki et al., 2003). Among these, alpha-1 antagonists, including prazosin, demonstrate the ability to induce vasodilation and promote urinary smooth muscle relaxation. Tamsulosin is a kind of super-selective alpha-1A antagonist with greater affinity for the urinary system, which mainly inhibits urinary smooth muscle contraction and facilitates voiding. The off-label uses of alpha blockers in POUR have also been explored in diverse surgical populations. Chapman et al. reported that tamsulosin was effective in preventing POUR following female pelvic reconstructive surgery (Lose and Lindholm, 1985; Chapman et al., 2021). Similarly, Gönüllü et al. found that prophylactic administration of prazosin could reduce the incidence of POUR and catheterization following herniorrhaphy (Gönüllü et al., 1999).
Nevertheless, the assessment of alpha blockers’ effects on POUR in orthopaedic procedures remains limited and has yielded conflicting results. Choi et al. conducted a randomized controlled trial (RCT) investigating prophylactic tamsulosin in 95 patients undergoing total joint arthroplasty and found that the use of tamsulosin could curtailthe risk of POUR by two-thirds (p = 0.044) (Choi et al., 2021). In contrast, a controversial outcome was observed in the RCT by Schubert et al., wherein the patients receiving tamsulosin exhibited a comparable incidence of POUR with those not receiving the drug after arthroplasty (Tamsulosin: 28.1% VS. Control: 35.8%, p = 0.345) (Schubert et al., 2019). Basheer et al. also detected limited effectiveness of perioperative tamsulosin in mitigating the rate of POUR in spine surgery (Basheer et al., 2017). Given these uncertain findings, determining the prophylactic efficacy of alpha blockers against POUR in orthopaedic procedures remains a subject of interest and debate.
Therefore, the objective of this systematic review and meta-analysis is (Darrah et al., 2009): to identify whether prophylactic alpha blockers can diminish the risk of POUR, and (Baldini et al., 2009) to ascertain the presence of any potential complications associated with the administration of alpha blockers.
2 Methods
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement protocol (CRD42023409388) (Shamseer et al., 2015; Cumpston et al., 2019).
2.1 Search strategy and eligibility
PubMed, Embase, Web of Science and Cochrane Library databases were searched between 1st January 1990 and 1st March 2023. We developed search strategies for each database according to the principle of PICOS (Population, Intervention, Comparison, Outcome, Study design), and the references of the identified studies were checked for potential eligibility (Supplementary Table S1). Specifically, the search strategy for PubMed was: (alpha blocker OR alpha blockade OR alpha antagonist OR prazosin OR phenoxybenzamine OR doxazosin OR terazosin OR alfuzosin OR silodosin OR tamsulosin) AND (urinary retention OR voiding difficulty). The keywords regarding orthopaedic procedures were deliberately omitted during the initial search to avoid the exclusion of potentially relevant studies, given the diversity of orthopaedic procedures.
Eligible studies were identified using the following inclusion criteria: 1) patients following orthopaedic surgery as the interested population; 2) alpha blocker as the intervention; 3) placebo or no treatment as the comparison; 4) incidence of POUR as the primary outcome; 5) with comparative study design.
We excluded non-English language reports, in vitro studies, case reports, brief reports, conference abstracts/posters or reviews. After removing duplicates, titles and abstracts were reviewed to identify eligible papers. Full texts were assessed to determine the final list of publications eligible for inclusion in the study.
2.2 Data extraction
After the final list of included studies was set, we extracted the following information: year of publication, patient age, definition of POUR, operative information, administration of drugs and study design. The primary outcome of interest was the incidence of POUR. Complications were extracted as secondary outcomes.
2.3 Assessment of quality and bias
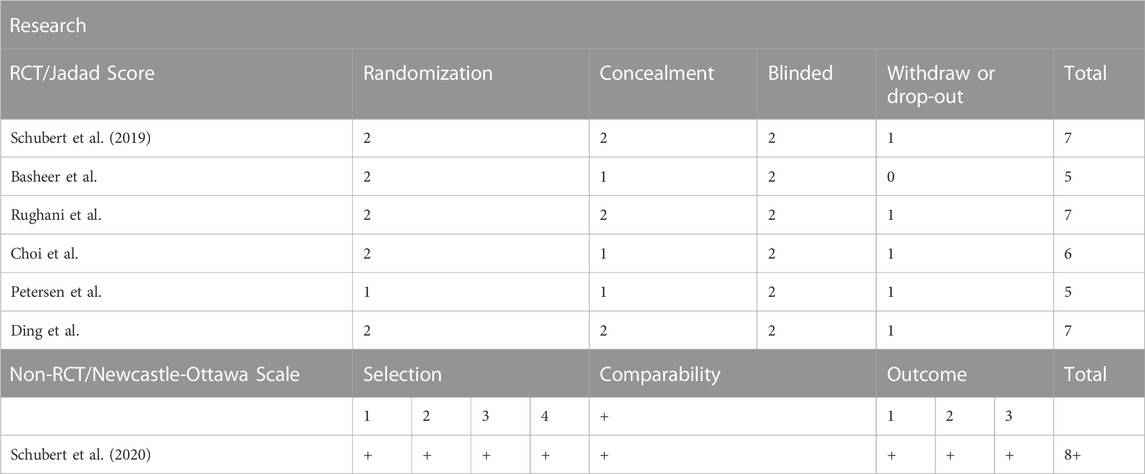
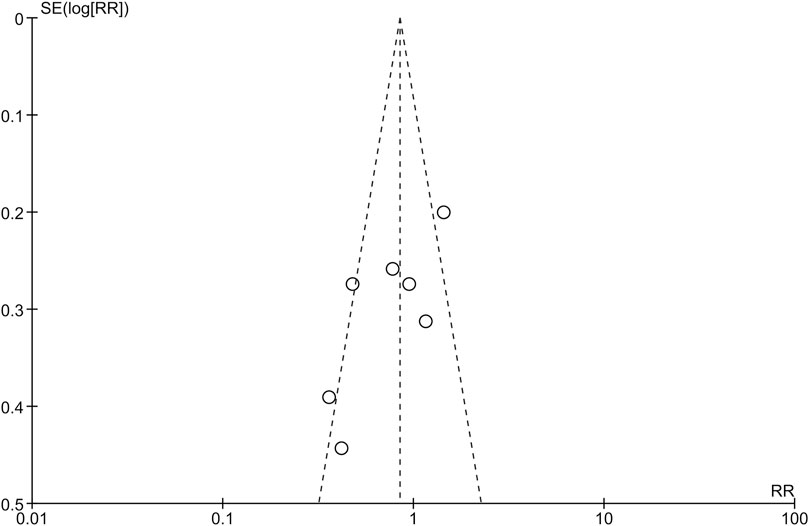
The quality of the included studies was assessed independently by two authors. The modified Jadad Scale was employed for RCTs (Moher et al., 1996), and the Newcastle-Ottawa Scale for cohort studies (Stang, 2010). The publication bias was estimated using the funnel plot and Harbord’s test (Harbord et al., 2006). In case of disagreement, a third senior doctor was consulted.
2.4 Statistical analysis
Statistical analysis was performed using RevMan software (version 5.3, Cochrane Collaboration, Oxford, the United Kingdom), R software (version 4.1.3, R Foundation for Statistical Computing, Vienna, Austria) and Trial Sequential Analysis (TSA) software (version 0.9.5.10 beta, Copenhagen Trial Unit, Copenhagen, Denmark), with p < 0.05 as the threshold for statistical significance. Heterogeneity among the studies was evaluated through the I2 statistic and Q test. Generally, a fixed-effects model is employed to calculate pooled results if I2 is less than 50% and the p-value for the Q test exceeds 0.05. Conversely, a random-effects is employed if I2 exceeds 50% or the p-value for the Q test is below 0.05. In this meta-analysis, we preferred the random-effects model to the fixed-effects model due to the inclusion of various alpha blockers and diverse dosing regimens. We postulated that the effectiveness of these interventions might exhibit variability across studies. Thus, a random-effects model was prespecified (Borenstein et al., 2010; Nikolakopoulou et al., 2014). The pooled rate of POUR or complications was calculated using the Mantel-Haenszel (M-H) method with a 95% confidence interval (CI). To ensure the robustness of the primary outcome of POUR, we evaluated the risk of false positives or false negatives using a post hoc TSA. Sequential boundaries were set according to a type I error of 5% and a power of 80%. The required information size (RIS) was calculated to determine whether the sample size was adequate to reach a reliable conclusion. The cumulative curve of the Z score was plotted. Sensitivity analysis was conducted using the leave-one-out analysis. Subgroup analysis was performed stratified by the type of operation.
3 Results
3.1 Overview of search results
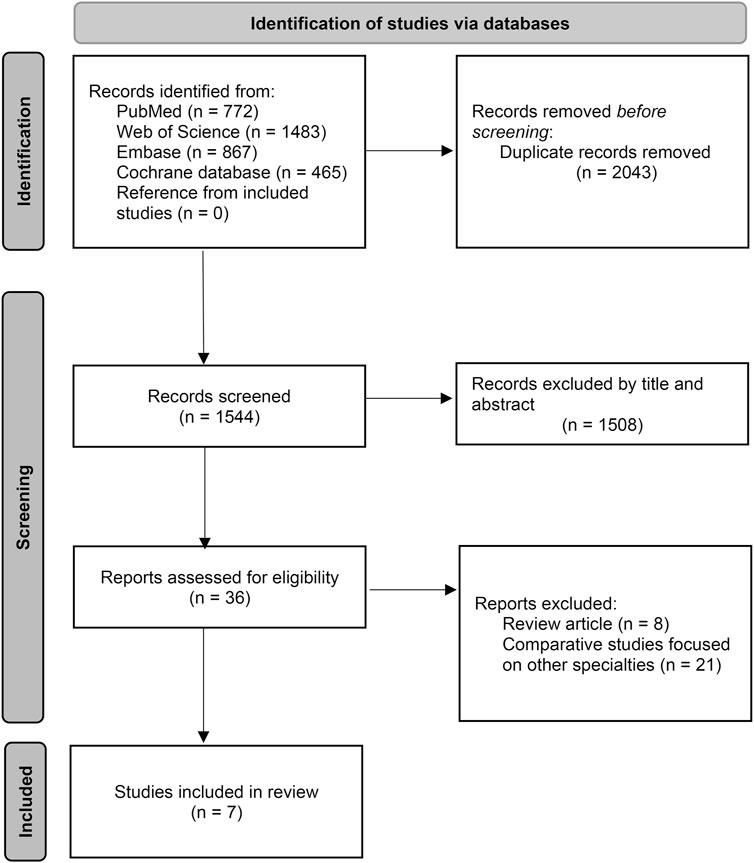
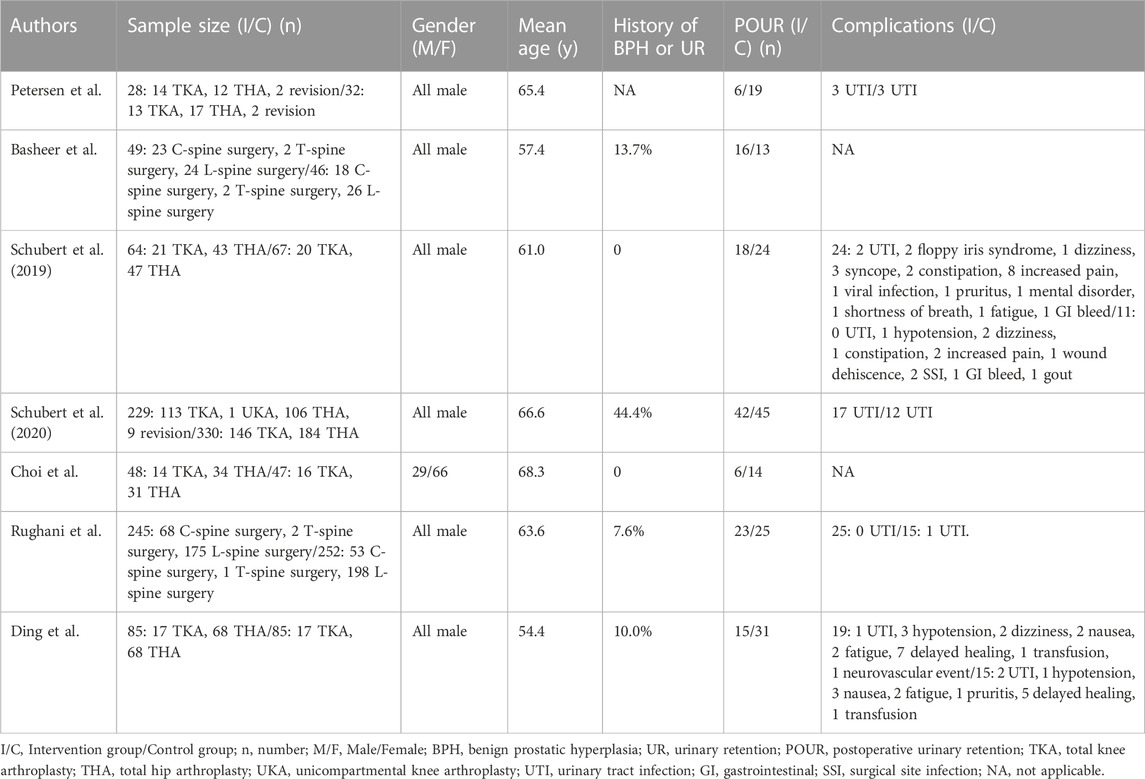
A total of 3,587 studies were identified at the initial search. After removing duplicates, 1,544 records were screened by titles and abstracts. Of these, 36 papers were assessed for eligibility by reading the full texts. Finally, seven studies (six RCTs and one retrospective cohort study) were included in the analysis (Figure 1) (Petersen et al., 1991; Basheer et al., 2017; Schubert et al., 2019; Schubert et al., 2020; Choi et al., 2021; Ding et al., 2022; Rughani et al., 2022). Among these studies, five focused on patients undergoing arthroplasty, while two investigated cases undergoing spine surgery. Six out of the seven studies reported the proportion of patients with a history of benign prostatic hyperplasia or urinary retention, with the cohort study exhibiting the highest proportion in this regard. Tamsulosin was the most commonly used drug. The details of the included studies were summarized in Table 1.
3.2 Assessment of quality and bias
All RCTs had a Jadad score higher than four, indicating that they were of high quality. The Newcastle-Ottawa rank also revealed the high quality of the cohort study. The details of the assessment were summarized in Table 2. The funnel plot did not show the concerns of possible publication bias (Figure 2), which was also consistent with the formal test (Harbord’s test, p = 0.145).
3.3 Primary outcome
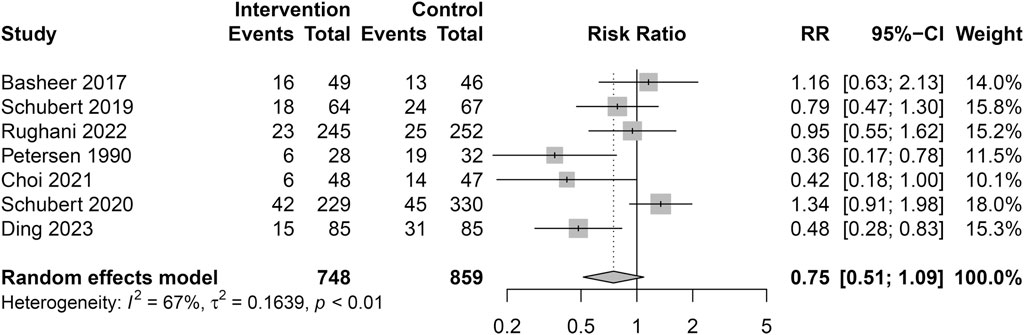
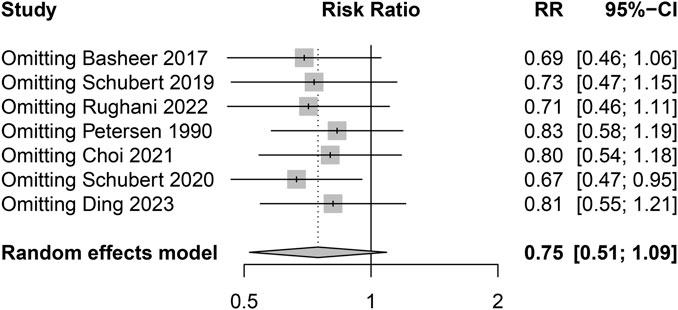
A total of 748 patients (Male: 95.6% VS. Female: 4.4%) received alpha blockers (Intervention group), while 859 patients (Male: 96.2% VS. Female: 3.8%) received a placebo or no intervention (Control group). Overall, there were 294 episodes of POUR in 1,607 patients (18.3%). The pooled analysis showed no significant difference in the incidence of POUR between the two groups with moderate heterogeneity (Intervention group: 126/748 [16.8%] VS. Control group: 168/859 [19.6%]; RR = 0.75; 95% CI 0.51 to 1.09; p = 0.130; Heterogeneity: I2 = 67.1%; p = 0.006) (Table 3; Figure 3). The sensitivity analysis using the leave-one-out analysis revealed that the exclusion of the study by Schubert et al. (2020) (Schubert et al., 2020), representing the only retrospective cohort study in this meta-analysis, demonstrated a statistically significant impact on the pooled results (Figure 4).
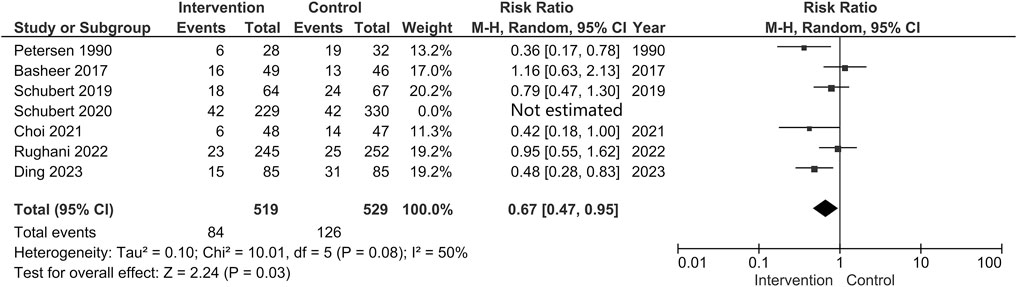
Considering the level of evidence of each study, we subsequently analyzed the data only from RCTs. This analysis reflected that the pooled incidence of POUR was lower in the Intervention group than that in the Control group (Intervention group: 84/519 [16.2%] VS. Control group: 126/529 [23.8%]; RR = 0.67; 95% CI 0.47 to 0.95; p = 0.03; Heterogeneity: I2 = 50%; p = 0.08) (Figure 5). However, the post hoc TSA showed that the cumulative curve of the Z score did not cross the sequential boundary nor the RIS, suggesting that the total sample size of the existing evidence may be insufficient to draw conclusive results (Figure 6).
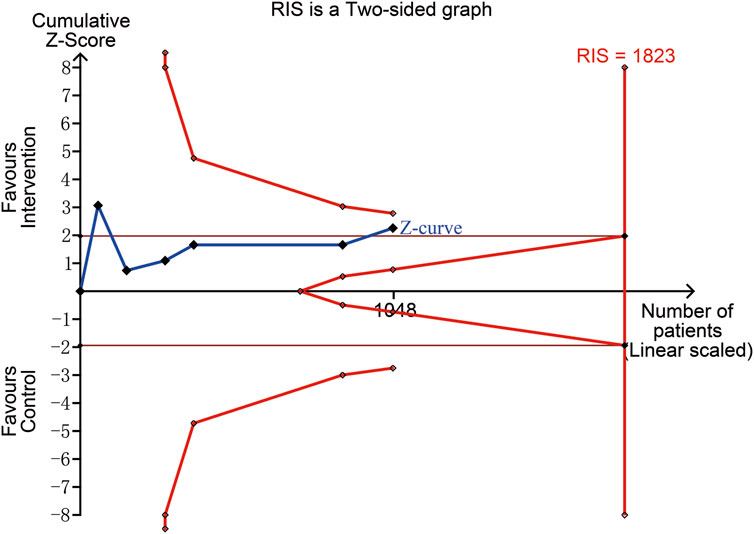
FIGURE 6. Trial sequential analysis for the incidence of POUR. The cumulative curve of the Z score (blue line) crossed naïve boundary (parallel brown line), which reflected that the difference of the incidence of POUR between the two groups were statistically significant. However, the curve did not cross the upper sequential boundary (red curved line) nor reach the required information size (RIS) (red longitudinal line), which indicated that the pooled results failed to support the benefit of alpha blockers due to the limited sample size.
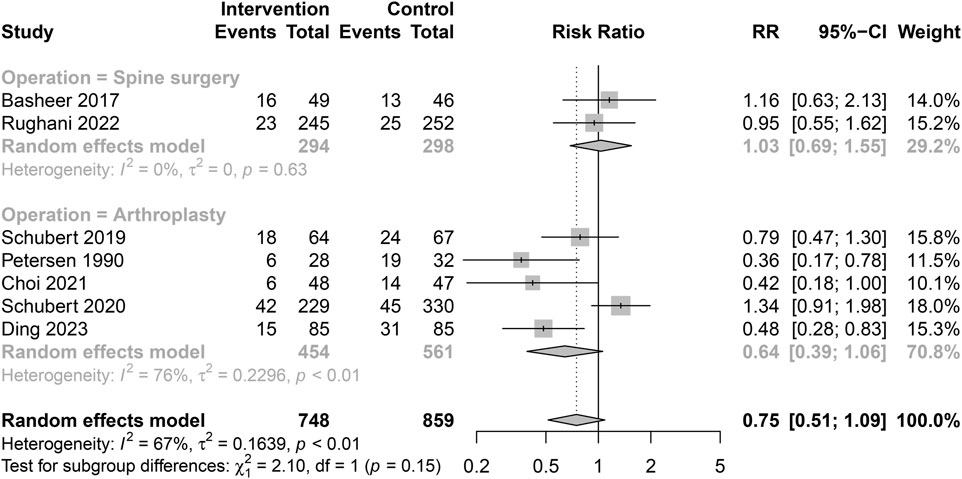
3.4 Subgroup analysis of primary outcome
The included studies were stratified into two subgroups: the Arthroplasty subgroup and the Spine surgery subgroup. In the Arthroplasty subgroup, the incidence of POUR was 19.2% in the Intervention group and 23.2% in the Control group, respectively. Two studies conducted a comparative assessment of knee and hip arthroplasty. In the study by Petersen et al., the incidence of POUR was comparable (Knee arthroplasty: 41% VS. Hip arthroplasty: 48%) (Petersen et al., 1991). Choi et al. reported that hip arthroplasty was not a risk factor for POUR as compared with knee arthroplasty (OR = 0.821, p = 0.711) (Choi et al., 2021).
In the Spine surgery subgroup, POUR was documented at a rate of 13.3% in the Intervention group and 12.8% in the Control group, respectively. The main surgical level was the lumbar region. The relationship between the incidence of POUR and the surgical levels remained unexplored in the two studies (Basheer et al., 2017; Rughani et al., 2022).
Prophylactic administration of alpha blockers did not show a significant protective effect in either subgroup (Arthroplasty subgroup: RR = 0.64, 95% CI 0.39 to 1.06; Spine surgery subgroup: RR = 1.03, 95% CI 0.69–1.55). Little heterogeneity was observed between the two subgroups (p = 0.15) (Figure 7).
3.5 Secondary outcomes
Five studies reported the data of complications and the pooled analysis showed that the administration of alpha blockers would introduce a higher risk of complications (88/651 [13.5%] VS. 56/766 [7.3%]; RR = 1.73; 95% CI 1.27 to 2.37; p = 0.0005; Heterogeneity: I2 = 0%; p = 0.69) (Figure 8) (Petersen et al., 1991; Schubert et al., 2019; Schubert et al., 2020; Ding et al., 2022; Rughani et al., 2022). UTI was the most commonly described and concerned complication. The rate of UTI was similar between the two groups (23/651 [3.5%] VS. 18/766 [2.3%]; RR = 1.65; 95% CI 0.92 to 2.94; p = 0.09; Heterogeneity: I2 = 0; p = 0.55) (Figure 9).
4 Discussion
Based on available evidence, we failed to identify a significant efficacy of prophylactic alpha blockers in reducing the risk of POUR after orthopaedic procedures. The pooled analysis of seven studies demonstrated that the incidence of POUR was comparable between the Intervention group and Control group (16.8% VS. 19.6%, respectively). Although the pooled results of six RCTs represented the highest level of evidence, suggesting a statistically significant 33% reduction in the risk of POUR (RR = 0.67; 95% CI 0.47–0.95) associated with alpha blockers, this finding must be approached with caution due to the relatively limited sample size. In addition, we found that the prophylactic alpha blockers might potentially increase the risk of complications.
4.1 Incidence of POUR
Our research holds clinical importance as it seeks to investigate the efficacy of pharmacologic interventions against POUR in orthopaedic patients. However, our findings showed a lack of statistically significant difference in the incidence of POUR when comparing cases with or without the administration of alpha blockers. These results differed from previous studies and meta-analyses in other clinical disciplines. Ghuman et al. conducted a meta-analysis of 15 RCTs in general surgery and urologic surgery and found that the prophylactic use of alpha blockers could yield a 17.1% absolute reduction in POUR risk (Ghuman et al., 2018). Another meta-analysis encompassing five RCTs revealed a reduction of 20.6% in the risk of POUR among patients after hernia repair following the administration of alpha blockers (Clancy et al., 2018). The discrepancy between our results and prior findings may be attributed to multiple factors. First, orthopaedic patients have an elevated inherent susceptibility to POUR owing to multiple factors, such as advanced age demographics, frequent use of neuraxial anaesthesia, and routine employment of indwelling urinary catheters (Schubert et al., 2019; Leitner et al., 2021). As a result, the perceived effectiveness of alpha blockers might not manifest to the same extent as witnessed in other disciplines. Second, orthopaedic procedures are typically major surgeries (Hoogeboom et al., 2014; Dietz et al., 2019), which pose a challenge for cautious perioperative fluid management (Heming et al., 2020). Arthroplasty and spine surgery often entails substantial intraoperative fluid administration (exceeding 1,000 mL), which is also linked to a potential risk of POUR (Lee et al., 2017; Aiyer et al., 2018; Halawi et al., 2019; Ongaigui et al., 2020). Third, our post hoc TSA to evaluate the robustness of our findings provided a more conservative estimation. It could be inferred that our aggregated results of RCTs might be false positive due to a relatively small sample size. Thus, more high-level evidence is required to determine the true efficacy of alpha blockers against POUR in orthopaedic patients.
4.2 Risk factors of POUR for orthopaedic procedures
Only two kinds of orthopaedic procedures, arthroplasty and spine surgery, were included in our review despite a thorough investigation across four main databases. In terms of lower-limb arthroplasty, our subgroup data indicated that the efficacy of alpha blockers seemed to be consistent between knee and hip procedures. However, it should be noted that the incidence of POUR might not be close between these two procedures. Abdul-Muhsin et al. reported that knee arthroplasty had a higher prevalence of POUR than hip arthroplasty (Abdul-Muhsin et al., 2020). As for the spine surgery, the majority of cases in our review pertained to lumbar-level interventions, which was reported to be associated with an elevated susceptibility to POUR as compared with surgeries targeting the cervical or thoracic regions (Altschul et al., 2017). Due to the limited available data, our review was unable to explore potential correlations between surgical levels and drug efficacy.
Information regarding the use of alpha blockers to prevent POUR in other orthopaedic surgeries is lacking. Several studies have identified the risk factors and preventive regimens for patients following different orthopaedic surgeries. Tobu et al. found that patients with femoral neck fractures who had dementia and/or delirium had a tenfold higher risk of developing POUR (Tobu et al., 2014). Higashikawa et al. also found that cognitive impairment in female patients with proximal hip fractures was associated with a higher likelihood of POUR (Higashikawa et al., 2019). The authors recommended necessary nursing care in activities of daily living and neurofunctional assistance to mitigate the risk. A history of benign prostatic hyperplasia or neurogenic bladder is also a well-established risk factor. A meta-analysis showed that patients with such a condition were associated with a 3.8-fold risk of developing POUR after spine surgery (Chang et al., 2021). In our meta-analysis, a strategic exclusion of patients with a history of benign prostatic hyperplasia was instituted across most RCTs to mitigate potential bias. However, this discerning protocol also attenuated the generalizability of the pooled results. Further studies are appealed to explore the strategy against POUR in patients at higher risk, such as those with benign prostatic hyperplasia or neurogenic bladder. Other risk factors including spinal/epidural anaesthesia, advanced age and excessive fluid administration should also be considered in orthopaedic surgeries (Cha et al., 2020). Santini et al. adopted the International Prostate Symptom Score to assess the risk of POUR and found that a score above 18 was strongly related to a predisposition to POUR (Santini et al., 2019). However, to our knowledge, few scoring systems for POUR in orthopaedic surgeries have been widely used with a well-validated prediction (Bracey et al., 2022).
4.3 Concerns about complications
Our research found that the administration of alpha blockers was related to a higher risk of complications while the incidence of UTI was similar between the two groups. Other reported complications included dizziness and vomiting, which might result from vasodilation caused by the drugs. Previous studies have also raised concerns about alpha blockers, such as the carcinogenicity of phenoxybenzamine and the cardiovascular effects of prazosin (Hasford et al., 1991; Suarez-Torres et al., 2021). In our included studies, Schubert et al. reported two cases of tamsulosin-induced floppy iris syndrome (Schubert et al., 2019). Bell et al. found that the risk of floppy iris syndrome in patients after cataract surgery was 2.3 times higher when tamsulosin was administered (Bell et al., 2009), and the authors attributed this complication to the mechanism that the alpha-1A adrenergic receptors were also present in the dilator smooth muscle of the iris, and thus tamsulosin might compromise mydriasis. Surgeons should pay attention to our assembled data and inform patients of the associated complications.
4.4 Limitations
We noted several limitations in our meta-analysis. First, the possibility of missing relevant studies cannot be completely avoided, which may introduce bias into our methodology. Second, one of the included studies utilized a cohort study design, which may affect the level of evidence of our pooled data. However, we performed a leave-one-out analysis and calculated the pooled results after excluding the cohort study. We used the TSA to estimate the robustness of our conclusion, which suggested that our results of RCTs might not possess full sufficiency and conclusiveness. Third, we included all the studies with multiple alpha blockers as an intervention and assumed that the efficacy of alpha blockers was similar. We used the random-effects model to synthesize the data more conservatively. However, we still noticed that the pooled results reflected a moderate degree of heterogeneity, despite performing a subgroup analysis. Fourth, the data on POUR that were pooled were extracted directly from the articles and we found that the definitions of POUR in each study were similar but not identical, which might bring quantitative bias into the data. Fifth, only two types of orthopaedic surgeries were included, which might jeopardize the generalizability of the conclusion. The distribution of surgical subtypes between the intervention and control groups might also introduce bias.
5 Conclusion
The current meta-analysis of existing evidence found that prophylactic alpha blockers might not reduce the risk of POUR after orthopaedic procedures, and the TSA suggested that more trials were required. Administrating these drugs could be associated with a possibly higher risk of complications.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributions
SW, HL, and LS designed the protocol of this review. LS and PS completed the papers searches and screening. LS, PS, HL, and WZ extracted data and performed meta-analysis through software. LS and PS were the two major contributors in drafting the paper. SW, HL, and WZ were the major contributors in the revision of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1214349/full#supplementary-material
References
Abdul-Muhsin, H. M., Jakob, N., Cha, S., Zhang, N., Schwartz, A., Navaratnam, A., et al. (2020). Incidence, outcomes, and prediction of postoperative urinary retention after a nonurologic procedure. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 4 (5), e1900149. Epub 2021/05/11. doi:10.5435/JAAOSGlobal-D-19-00149
Aiyer, S. N., Kumar, A., Shetty, A. P., Kanna, R. M., and Rajasekaran, S. (2018). Factors influencing postoperative urinary retention following elective posterior lumbar spine surgery: A prospective study. Asian Spine J. 12 (6), 1100–1105. Epub 2018/10/17. doi:10.31616/asj.2018.12.6.1100
Altschul, D., Kobets, A., Nakhla, J., Jada, A., Nasser, R., Kinon, M. D., et al. (2017). Postoperative urinary retention in patients undergoing elective spinal surgery. J. Neurosurg. Spine 26 (2), 229–234. Epub 2016/10/22. doi:10.3171/2016.8.Spine151371
Baldini, G., Bagry, H., Aprikian, A., and Carli, F. (2009). Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology 110 (5), 1139–1157. Epub 2009/04/09. doi:10.1097/ALN.0b013e31819f7aea
Basheer, A., Alsaidi, M., Schultz, L., Chedid, M., Abdulhak, M., and Seyfried, D. (2017). Preventive effect of tamsulosin on postoperative urinary retention in neurosurgical patients. Surg. Neurol. Int. 8, 75. Epub 2017/06/07. doi:10.4103/sni.sni_5_17
Bell, C. M., Hatch, W. V., Fischer, H. D., Cernat, G., Paterson, J. M., Gruneir, A., et al. (2009). Association between tamsulosin and serious ophthalmic adverse events in older men following cataract surgery. Jama 301 (19), 1991–1996. Epub 2009/05/21. doi:10.1001/jama.2009.683
Borenstein, M., Hedges, L. V., Higgins, J. P., and Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 1 (2), 97–111. Epub 2010/04/01. doi:10.1002/jrsm.12
Boulis, N. M., Mian, F. S., Rodriguez, D., Cho, E., and Hoff, J. T. (2001). Urinary retention following routine neurosurgical spine procedures. Surg. Neurol. 55 (1), 23–27. discussion 27-8. Epub 2001/03/15. doi:10.1016/s0090-3019(01)00331-7
Bracey, D. N., Barry, K., Khanuja, H. S., and Hegde, V. (2022). Postoperative urinary retention in modern rapid recovery total joint arthroplasty. J. Am. Acad. Orthop. Surg. 30 (10), 443–447. Epub 2022/02/26. doi:10.5435/jaaos-d-21-00963
Cha, Y. H., Lee, Y. K., Won, S. H., Park, J. W., Ha, Y. C., and Koo, K. H. (2020). Urinary retention after total joint arthroplasty of hip and knee: systematic review. J. Orthop. Surg. Hong. Kong) 28 (1), 2309499020905134. Epub 2020/03/03. doi:10.1177/2309499020905134
Chang, Y., Chi, K. Y., Tai, T. W., Cheng, Y. S., Lee, P. H., Huang, C. C., et al. (2021). Risk factors for postoperative urinary retention following elective spine surgery: A meta-analysis. Spine J. 21 (11), 1802–1811. Epub 2021/05/21. doi:10.1016/j.spinee.2021.05.009
Chapman, G. C., Sheyn, D., Slopnick, E. A., Roberts, K., El-Nashar, S. A., Henderson, J. W., et al. (2021). Tamsulosin vs placebo to prevent postoperative urinary retention following female pelvic reconstructive surgery: A multicenter randomized controlled trial. Am. J. Obstet. Gynecol. 225 (3), 274.e1–274274.e11. e11. Epub 2021/04/25. doi:10.1016/j.ajog.2021.04.236
Choi, C. I., Kim, J. K., Choo, M. S., Lee, S. H., Chang, J. D., and Han, J. H. (2021). Preventive effects of tamsulosin for postoperative urinary retention after lower limb arthroplasty: A randomized controlled study. Investig. Clin. Urol. 62 (5), 569–576. Epub 2021/08/14. doi:10.4111/icu.20200523
Clancy, C., Coffey, J. C., O'Riordain, M. G., and Burke, J. P. (2018). A meta-analysis of the efficacy of prophylactic alpha-blockade for the prevention of urinary retention following primary unilateral inguinal hernia repair. Am. J. Surg. 216 (2), 337–341. Epub 2017/03/28. doi:10.1016/j.amjsurg.2017.02.017
Cumpston, M., Li, T., Page, M. J., Chandler, J., Welch, V. A., Higgins, J. P., et al. (2019). Updated guidance for trusted systematic reviews: A new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst. Rev. 10, Ed000142. Epub 2019/10/24. doi:10.1002/14651858.Ed000142
Darrah, D. M., Griebling, T. L., and Silverstein, J. H. (2009). Postoperative urinary retention. Anesthesiol. Clin. 27 (3), 465–484. table of contents. Epub 2009/10/15. doi:10.1016/j.anclin.2009.07.010
Dietz, N., Sharma, M., Adams, S., Alhourani, A., Ugiliweneza, B., Wang, D., et al. (2019). Enhanced recovery after surgery (eras) for spine surgery: A systematic review. World Neurosurg. 130, 415–426. Epub 2019/07/06. doi:10.1016/j.wneu.2019.06.181
Ding, Z., Cao, J., Huang, C., Zhou, K., Wang, H., and Zhou, Z. (2022). Prophylactic doxazosin reduces urinary retention and promotes recovery after total joint arthroplasty: A randomized controlled trial. Front. Pharmacol. 13, 1016203. Epub 2023/01/27. doi:10.3389/fphar.2022.1016203
Foxman, B. (2003). Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Dis. Mon. 49 (2), 53–70. Epub 2003/02/26. doi:10.1067/mda.2003.7
Ghuman, A., de Jonge, S. W., Dryden, S. D., Feeney, T., Buitrago, D. H., and Phang, P. T. (2018). Prophylactic use of alpha-1 adrenergic blocking agents for prevention of postoperative urinary retention: A review and meta-analysis of randomized clinical trials. Am. J. Surg. 215 (5), 973–979. Epub 2018/02/06. doi:10.1016/j.amjsurg.2018.01.015
Gönüllü, N. N., Dülger, M., Utkan, N. Z., Cantürk, N. Z., and Alponat, A. (1999). Prevention of postherniorrhaphy urinary retention with prazosin. Am. Surg. 65 (1), 55–58. Epub 1999/01/23. doi:10.1177/000313489906500113
Halawi, M. J., Caminiti, N., Cote, M. P., Lindsay, A. D., and Williams, V. J. (2019). The most significant risk factors for urinary retention in fast-track total joint arthroplasty are iatrogenic. J. Arthroplasty 34 (1), 136–139. Epub 2018/10/01. doi:10.1016/j.arth.2018.08.042
Harbord, R. M., Egger, M., and Sterne, J. A. (2006). A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat. Med. 25 (20), 3443–3457. Epub 2005/12/14. doi:10.1002/sim.2380
Hasford, J., Bussmann, W. D., Delius, W., Koepcke, W., Lehmann, K., and Weber, E. (1991). First dose hypotension with enalapril and prazosin in congestive heart failure. Int. J. Cardiol. 31 (3), 287–293. Epub 1991/06/01. doi:10.1016/0167-5273(91)90379-4
Heming, N., Moine, P., Coscas, R., and Annane, D. (2020). Perioperative fluid management for major elective surgery. Br. J. Surg. 107 (2), e56–e62. Epub 2020/01/07. doi:10.1002/bjs.11457
Higashikawa, T., Shigemoto, K., Goshima, K., Usuda, D., Okuro, M., Moriyama, M., et al. (2019). Urinary retention as a postoperative complication associated with functional decline in elderly female patients with femoral neck and trochanteric fractures: A retrospective study of a patient cohort. Med. Baltim. 98 (24), e16023. Epub 2019/06/14. doi:10.1097/md.0000000000016023
Hoogeboom, T. J., Dronkers, J. J., Hulzebos, E. H., and van Meeteren, N. L. (2014). Merits of exercise therapy before and after major surgery. Curr. Opin. Anaesthesiol. 27 (2), 161–166. Epub 2014/02/07. doi:10.1097/aco.0000000000000062
Kakizaki, H., Ameda, K., Kobayashi, S., Tanaka, H., Shibata, T., and Koyanagi, T. (2003). Urodynamic effects of alpha1-blocker tamsulosin on voiding dysfunction in patients with neurogenic bladder. Int. J. Urol. 10 (11), 576–581. Epub 2003/11/25. doi:10.1046/j.1442-2042.2003.00710.x
Khoury, A. F., and Kaplan, N. M. (1991). Alpha-blocker therapy of hypertension. An unfulfilled promise. Jama 266 (3), 394–398. Epub 1991/07/17. doi:10.1001/jama.266.3.394
Lee, S., Kim, C. H., Chung, C. K., Park, S. B., Yang, S. H., Kim, S. H., et al. (2017). Risk factor analysis for postoperative urinary retention after surgery for degenerative lumbar spinal stenosis. Spine J. 17 (4), 469–477. Epub 2016/03/26. doi:10.1016/j.spinee.2016.03.017
Leitner, L., Wanivenhaus, F., Bachmann, L. M., Liechti, M. D., Aguirre, J. A., Farshad, M., et al. (2021). Bladder management in patients undergoing spine surgery: an assessment of care delivery. N. Am. Spine Soc. J. 6, 100059. Epub 2022/02/11. doi:10.1016/j.xnsj.2021.100059
Lose, G., and Lindholm, P. (1985). Prophylactic phenoxybenzamine in the prevention of postoperative retention of urine after vaginal repair: A prospective randomized double-blind trial. Int. J. Gynaecol. Obstet. 23 (4), 315–320. Epub 1985/09/01. doi:10.1016/0020-7292(85)90026-8
Moher, D., Jadad, A. R., and Tugwell, P. (1996). Assessing the quality of randomized controlled trials. Current issues and future directions. Int. J. Technol. Assess. Health Care 12 (2), 195–208. Epub 1996/01/01. doi:10.1017/s0266462300009570
Nikolakopoulou, A., Mavridis, D., and Salanti, G. (2014). How to interpret meta-analysis models: fixed effect and random effects meta-analyses. Evid. Based Ment. Health 17 (2), 64. Epub 2014/04/30. doi:10.1136/eb-2014-101794
Ongaigui, C., Fiorda-Diaz, J., Dada, O., Mavarez-Martinez, A., Echeverria-Villalobos, M., and Bergese, S. D. (2020). Intraoperative fluid management in patients undergoing spine surgery: A narrative review. Front. Surg. 7, 45. Epub 2020/08/28. doi:10.3389/fsurg.2020.00045
Parker, V., Giles, M., Graham, L., Suthers, B., Watts, W., O'Brien, T., et al. (2017). Avoiding inappropriate urinary catheter use and catheter-associated urinary tract infection (CAUTI): A pre-post control intervention study. BMC Health Serv. Res. 17 (1), 314. Epub 2017/05/04. doi:10.1186/s12913-017-2268-2
Pertsch, N. J., Darveau, S. C., Tang, O. Y., Toms, S. A., and Weil, R. J. (2021). Urinary tract infection after elective spine surgery: timing, predictive factors, and outcomes. Spine (Phila Pa 1976) 46 (5), 337–346. Epub 2021/02/04. doi:10.1097/brs.0000000000003794
Petersen, M. S., Collins, D. N., Selakovich, W. G., and Finkbeiner, A. E. (1991). Postoperative urinary retention associated with total hip and total knee arthroplasties. Clin. Orthop. Relat. Res. 269 (269), 102–108. Epub 1991/08/01. doi:10.1097/00003086-199108000-00016
Rughani, A., Cushing, D., Lary, C. W., Cox, S., Jumper, B., Johnson, N., et al. (2022). Does tamsulosin decrease postoperative urinary retention in spine surgery? A double-blind, randomized controlled trial. J. Neurosurg. 137, 1172–1179. Epub 2022/02/12. doi:10.3171/2021.10.Jns212393
Santini, A. J., Jakaraddi, C. A., Polydoros, F., and Metikala, S. (2019). Validity of the International Prostate Symptoms Score in predicting urinary retention after joint replacement. J. Orthop. Surg. Hong. Kong) 27 (3), 2309499019868670. Epub 2019/08/28. doi:10.1177/2309499019868670
Schubert, M. F., Thomas, J. R., Gagnier, J. J., McCarthy, C. M., Lee, J. J., Urquhart, A. G., et al. (2019). The aahks clinical research award: prophylactic tamsulosin does not reduce the risk of urinary retention following lower extremity arthroplasty: a double-blinded randomized controlled trial. J. Arthroplasty 34 (7), S17–S23. Epub 2019/04/16. doi:10.1016/j.arth.2019.03.039
Schubert, M. F., Thomas, J. R., Yashar, J., Lee, J. J., Urquhart, A. G., Gagnier, J. J., et al. (2020). Post-operative urinary retention after lower extremity arthroplasty and the peri-operative role of selective alpha-1 adrenergic blocking agents in adult male patients: A propensity-matched retrospective cohort study. Int. Orthop. 44 (1), 39–44. Epub 2019/10/24. doi:10.1007/s00264-019-04420-z
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj 350, g7647. Epub 2015/01/04. doi:10.1136/bmj.g7647
Stang, A. (2010). Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 (9), 603–605. Epub 2010/07/24. doi:10.1007/s10654-010-9491-z
Suarez-Torres, J. D., Orozco, C. A., and Ciangherotti, C. E. (2021). The numerical probability of carcinogenicity to humans of some pharmaceutical drugs: alkylating agents, topoisomerase inhibitors or poisons, and dna intercalators. Fundam. Clin. Pharmacol. 35 (6), 1069–1089. Epub 2021/03/28. doi:10.1111/fcp.12674
Tan, E., Braithwaite, I., McKinlay, C. J. D., and Dalziel, S. R. (2020). Comparison of acetaminophen (paracetamol) with ibuprofen for treatment of fever or pain in children younger than 2 Years: A systematic review and meta-analysis. JAMA Netw. Open 3 (10), e2022398. Epub 2020/10/31. doi:10.1001/jamanetworkopen.2020.22398
Tobu, S., Noguchi, M., Hashikawa, T., and Uozumi, J. (2014). Risk factors of postoperative urinary retention after hip surgery for femoral neck fracture in elderly women. Geriatr. Gerontol. Int. 14 (3), 636–639. Epub 2013/11/13. doi:10.1111/ggi.12150
Törn, K., Tuominen, M., Tarkkila, P., and Lindgren, L. (1994). Effects of sub-hypnotic doses of propofol on the side effects of intrathecal morphine. Br. J. Anaesth. 73 (3), 411–412. Epub 1994/09/01. doi:10.1093/bja/73.3.411
Wang, C., Huang, W., Gu, Y., Xiong, J., Ye, Z., Yin, D., et al. (2021). Effect of urinary tract infection on the risk of prosthetic joint infection: A systematic review and meta-analysis. Surgeon 19 (3), 175–182. Epub 2020/05/27. doi:10.1016/j.surge.2020.04.010
Keywords: orthopaedic procedures, prophylactic alpha blockers, postoperative urinary retention, systematic review and meta-analysis, trial sequential analysis
Citation: Shan L, Sun P, Zhang W, Zheng X, Li H and Wang S (2023) Prophylactic alpha blockers fail to prevent postoperative urinary retention following orthopaedic procedures: evidence from a meta-analysis and trial sequential analysis of comparative studies. Front. Pharmacol. 14:1214349. doi: 10.3389/fphar.2023.1214349
Received: 26 May 2023; Accepted: 14 August 2023;
Published: 25 August 2023.
Edited by:
Elham Ahmadian, Tabriz University of Medical Sciences, IranReviewed by:
Thomas Hsueh, Taipei City Hospital, TaiwanAlbert Botchway, Southern Illinois University Carbondale, United States
Copyright © 2023 Shan, Sun, Zhang, Zheng, Li and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songling Wang, c3p3azAwN0AxNjMuY29t; Hua Li, bGlodWFvcnRob3Bfam51QHllYWgubmV0
 Lianliang Shan1
Lianliang Shan1 Hua Li
Hua Li