
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Pharmacol. , 28 August 2023
Sec. Ethnopharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1176980
This article is part of the Research Topic Real-World Evidence of Natural Products, Herbal Medicines, and Traditional Chinese Medicine Treatments View all 15 articles
 Qian-Yun Ye1,2†
Qian-Yun Ye1,2† Qing Lin1†
Qing Lin1† Xue-Ling Hu3
Xue-Ling Hu3 Yu-Mei Yang3
Yu-Mei Yang3 Bao-Lin Zheng4
Bao-Lin Zheng4 Ting Li4
Ting Li4 Wen-Qiang Zhong3
Wen-Qiang Zhong3 Hao-Yu Wang1
Hao-Yu Wang1 Zhi-Fen Zhang3
Zhi-Fen Zhang3 Bing-Jie Luo3
Bing-Jie Luo3 Ya-Wen Xiao1
Ya-Wen Xiao1 Ai-Ling Wu1
Ai-Ling Wu1 Yan Li1
Yan Li1 Zhuo-Ling Zou1
Zhuo-Ling Zou1 Ling-Yu Li3,5,6
Ling-Yu Li3,5,6 Xiao-Yun Li3
Xiao-Yun Li3 Pan-Pan Wang2,5,6
Pan-Pan Wang2,5,6 Li Yang3
Li Yang3 Xiao-Feng Zhu1,5*
Xiao-Feng Zhu1,5* Li Han2*
Li Han2* Rong-Hua Zhang3,5,6*
Rong-Hua Zhang3,5,6*Purpose: To conduct a real-world evaluation of the efficacy and safety of combined Chinese and Western medicine in treating knee osteoarthritis (KOA).
Methods: A multicenter, prospective cohort study design was employed, enrolling 450 KOA patients (Kellgren-Lawrence score of 3 or less). The patients were divided into a Western medicine treatment group (WM group) and a combined Western and traditional Chinese medicine treatment group (WM-CM group). A 6-week treatment plan was administered, and follow-up visits occurred at 2 weeks, 4 weeks, and 6 weeks after initiating treatment. The primary outcome indicator was the total Western Ontario and McMaster Universities Arthritis Index (WOMAC) score after 6 weeks of treatment. Secondary outcome indicators included WOMAC subscales for pain, stiffness, and joint function, visual analogue scale (VAS) score, physical component summary (PCS), mental component summary (MCS), and clinical effectiveness. The incidence of drug-related adverse events was used as a safety evaluation indicator.
Results: A total of 419 patients were included in the final analysis: 98 in the WM group and 321 in the WM-CM group. The baseline characteristics of the two groups were comparable, except for the incidence of stiffness symptoms and stiffness scores. After 6 weeks of treatment, the WM-CM group exhibited superior results to the WM group in improving the total WOMAC score (24.71 ± 1.38 vs. 16.36 ± 0.62, p < 0.001). The WM-CM group also outperformed the WM group in WOMAC pain and joint function scores, VAS score, PCS score, MCS score, and clinical effectiveness (p < 0.05), which was consistent with the findings of the main evaluation index. Subgroup analysis indicated that the combined Chinese and Western medicine treatment showed more pronounced benefits in patients under 65 years of age and in those with a Kellgren-Lawrence (K-L) classification of 0-I. Throughout the study, no adverse effects were observed in either group.
Conclusion: The combination of Chinese and Western medicine demonstrated superiority over Western medicine alone in relieving knee pain symptoms, improving knee function, and enhancing the quality of life for KOA patients with a K-L score of 3 or less. Moreover, the treatment exhibited a good safety profile.
Clinical Trial Registration: (https://www.chictr.org.cn/), identifier (ChiCTR1900027175).
Knee osteoarthritis (KOA) is one of the most common musculoskeletal disorders and a major cause of disability in elderly individuals (Collaborators, 2018; Jang S., 2021; Lundberg M., 2022). With the accelerated aging process, the growth of the obese population and the increasing life expectancy, the prevention and treatment of KOA are facing a serious challenge (Mahmoudian A., 2021). According to statistics, KOA has affected more than 250 million people worldwide (Vos T., 2012), and in China, the prevalence of symptomatic KOA in people over 65 years of age is 60%, and the detection rate of radiological KOA is as high as 80% (Huang D., 2018). Moreover, the number of patients with KOA will continue to increase in the future, and it is estimated that it will be close to 400 million by 2030 (Pereira D., 2011; Zhang Z., 2020).
KOA is characterized by a long, irreversible and incurable course, causing pain, reduced mobility and even disability, which places a great burden on patients’ physical and mental health and seriously interferes with their quality of life (Wang X., 2016; Feng X.Q., 2022). In addition, the high medical costs and corresponding indirect costs of KOA not only increase the economic burden of individuals and families but also have a negative impact on the national healthcare system and increase socioeconomic costs (Tang X., 2016).
Conservative therapy is now becoming increasingly important in the long-term management of KOA as the first line of treatment to slow disease progression and avoid or delay knee replacement surgery (Lim W.B., 2022). Western conservative treatment is mainly based on pain control and cartilage nutrition protocols, with the point of action localized to the joint. In fact, KOA involves multiple lesions and complex pathological changes, which are the result of multiple pathogenic factors intertwined and acting over a long period of time, and the efficacy of localized, single western medicine treatment is limited (Li R., 2013).
Traditional Chinese medicine (TCM) has a history of thousands of years in treating KOA, with a wide variety of therapeutic approaches that can play a role in holistic conditioning, and it is widely used in China and other Asian countries. Although there is preliminary evidence that TCM has the advantage of significant efficacy and low adverse effects and can improve the clinical efficacy of KOA in conjunction with Western medicine, overall, the evidence from high-quality clinical studies is still very limited (Chen B., 2016; Zhang J.H., 2019; Deng Y.L., 2021). Therefore, based on the concept of addressing the characteristics of individualized complex interventions and holistic efficacy evaluation of TCM, we conducted a prospective, multicenter cohort study following the requirements of modern clinical epidemiology and evidence-based medicine to further evaluate the clinical efficacy and safety of combined Chinese and Western medicine in the treatment of KOA from a macroscopic perspective to support its early intervention in KOA.
This study was conducted as a prospective, multicenter cohort study from January 2021 to October 2022 in three medical institutions: the First Affiliated Hospital of Jinan University, the Third Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, and Foshan Hospital of Traditional Chinese Medicine. It was approved by the Ethics Committee of the First Hospital of Jinan University (KY-2019-036), and registration was completed at the China Clinical Trials Registry (ChiCTR1900027175). All subjects provided written informed consent.
The inclusion criteria for the study population were as follows: 1) meeting the diagnostic criteria for KOA and having a Kellgren-Lawrence (K-L) radiological diagnosis grade of III or less, based on the Guidelines for the Treatment of Knee Osteoarthritis with Integrative Medicine (Committee, 2018); 2) being aged 30 years or older; 3) not having plans for surgery in the near future and requiring conservative treatment; and 4) demonstrating good compliance and the ability to cooperate with the completion of clinical visits.
Exclusion criteria were as follows: 1) having a history of knee trauma or surgery in the last 6 months, along with knee fracture, dislocation, or septic knee arthritis; 2) receiving arthroscopic treatment or intra-articular injection in the last 3 months; 3) receiving hormone therapy in the last 1 month; 4) having undergone knee replacement; 5) having comorbidities such as tumor, tuberculosis, hemophilic arthritis, rheumatoid arthritis, systemic lupus erythematosus, or ankylosing spondylitis; 6) having serious gastrointestinal diseases, severe psychiatric disorders, significant infectious diseases, or severe pathologies affecting vital organs such as the heart, liver, kidneys, or others; 7) having a history of severe allergy to TCM; 8) having local skin ulcers or eczema; and 9) being deemed unsuitable for inclusion in the study by the investigator.
The patients were divided into a Western medicine treatment group (WM group) and a combined Western and traditional Chinese medicine treatment group (WM-CM group) according to the actual treatment protocol used in the clinic. All subjects received basic treatment, including health education and exercise instruction. In the WM group, NSAIDs, sodium glutamate and glucosamine were used as the main treatment drugs according to the relevant guidelines (Bannuru R.R., 2019; Association, 2021; Zhang Z., 2021), while the WM-CM group used a combination of Western and traditional Chinese medicine according to the comprehensive treatment plan we developed in the early stage. All patients included in the study received a 6-week treatment, and the medication was administered following the recommended conventional dosage as per the instructions. The types of medications used during treatment were shown in Table 1. TCM therapy mainly includes commercially available Chinese patent medicines and hospital preparations that have been used for many years. We provided detailed information on the most frequently used oral and topical traditional Chinese medicines in Table 2, including their composition, proportions, dosage, usage, manufacturing processes, and quality control aspects. The detailed information for the other traditional Chinese medicines can be found in Supplementary Tables S1, S2 of the supplementary materials.
Patients were evaluated before treatment and at 2, 4, and 6 weeks of treatment.
The primary outcome measure was the total Western Ontario and McMaster Universities Arthritis Index (WOMAC) score (ranging from 0 to 96, with higher scores indicating more severe symptoms). The primary end point is the WOMAC total score after 6 weeks of treatment.
Secondary efficacy indicators included the following:
1) WOMAC subscale scores, including WOMAC pain score (ranging from 0 to 20, with higher scores indicating more severe pain), WOMAC stiffness score (ranging from 0 to 8, with higher scores indicating more severe knee stiffness), and WOMAC joint function score (ranging from 0 to 68, with higher scores indicating poorer knee function);
2) The visual analogue scale (VAS) score (ranging from 0 to 10, with higher scores indicating more severe pain);
3) 36-item short form (SF-36) scores, divided into physical component summary (PCS) and mental component summary (MCS); the former includes four dimensions of physical functioning (PF), role-physical (RP), bodily pain (BP), and general health (GH), and the latter includes four dimensions of vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH), ranging from 0 to 100, with higher scores indicating better status on that dimension; and
4) Clinical effectiveness. As described in the literature (Angst F., 2001; Nishida Y., 2021), an improvement in the WOMAC total score by more than 12% from the baseline value was defined as effective, and an improvement in the WOMAC total score by more than 50% from the baseline value was defined as significant.
An adverse event was defined as any undesirable medical occurrence associated with the treatment protocol, leading to a persistence or worsening of the patient’s symptoms that required additional interventions (Deyle G.D., 2016). For this study, patients were asked to report at each follow-up visit any adverse outcomes, including complications, signs or symptoms, that they perceived to be related to their treatment. The incidence of adverse events was considered an indicator for safety evaluation.
G*Power 3.1.2 software was used to calculate the sample size for this study. Based on the relevant literature (Cao Y., 2005; Deyle G.D., 2020) and the previous study of our group, assuming that the mean WOMAC values of the WM group and the WM-CM group were equal at baseline and that a 12% difference between the two groups was maintained after each treatment, setting a standard deviation of 7 and a mean correlation of 0.681 between repeated measures, and considering a 10% missed visit rate, then with a sample size of 92 cases per group, there is a 90% test efficacy to find the difference between groups. Therefore, we set the minimum sample size at 92 cases and adjusted the sample size appropriately according to the actual situation.
SPSS 27.0 software was used for statistical analysis. Data analysis is based on all populations completing the study unless otherwise noted. Hypothesis testing was uniformly performed using a two-sided test, with p < 0.05 indicating a statistically significant result. Baseline information was described as the mean ± standard deviation or frequency and composition ratio. Two groups were compared using independent samples t tests or Mann‒Whitney U rank sum tests for measurement data and chi-square tests or Fisher’s exact tests for count data. Repeated measures data were compared between groups using generalized linear mixed models (GLMM). The model included treatment, time, and the interaction of treatment with time as fixed effects and patient-specific random intercepts.
A total of 450 patients were enrolled in this study, and 419 subjects completed the entire study process, eventually forming the analysis cohort, consisting of 98 patients in the WM group and 321 patients in the WM-CM group. Among them, there were 100 patients from Foshan Hospital of Traditional Chinese Medicine, including 14 in the WM group and 86 in the WM-CM group; 106 patients from the First Affiliated Hospital of Jinan University, including 70 in the WM group and 36 in the WM-CM group; and 213 patients from the Third Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine, including 14 in the WM group and 199 in the WM-CM group.
The patient follow-up process and lost visits are presented in Figure 1. Detailed baseline characteristics of the patients are summarized in Table 3. The prevalence of knee stiffness symptoms was higher in the WM-CM group (p = 0.003), while the WOMAC stiffness score was higher in the WM group (p = 0.019); otherwise, the rest of the baseline characteristics were comparable.
The mean total WOMAC values at baseline were 37.62 ± 1.702 in the WM group and 36.23 ± 0.923 in the WM-CM group, and the differences were not statistically significant. After 6 weeks of treatment, the mean WOMAC total score decreased to 24.71 ± 1.38 in the WM group and 16.36 ± 0.62 in the WM-CM group. The mean total WOMAC value was significantly lower in the WM-CM group than in the WM group (p < 0.001) (Table 4). Indeed, from the second week of treatment, there was a significant difference in the total WOMAC values of the two groups, and this trend persisted until the sixth week (Figure 2; Supplementary Table S3).
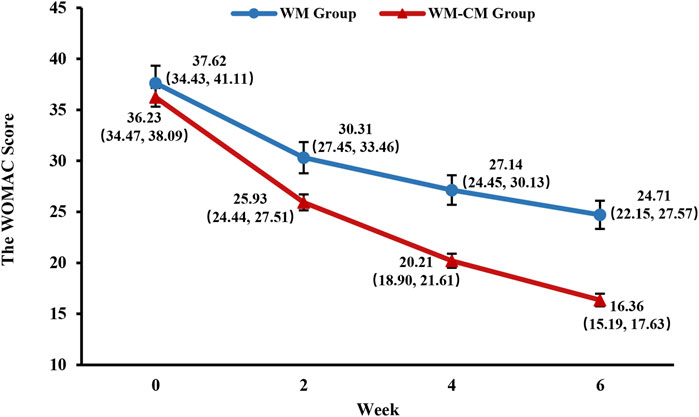
FIGURE 2. Overall trend of the WOMAC total scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
Figure 3 demonstrates the overall change in the WOMAC pain scores of both groups during the treatment period. With consistent baseline scores, the mean WOMAC pain score was significantly lower in the WM-CM group than in the WM group after 6 weeks of treatment (4.1 ± 0.165 vs. 5.39 ± 0.342, p = 0.001) (Table 4).
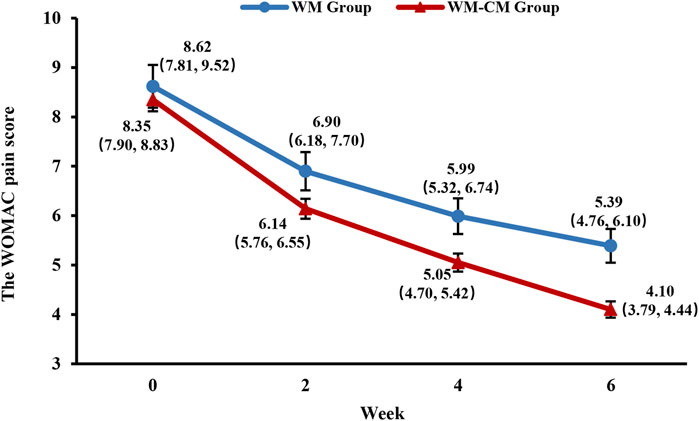
FIGURE 3. Overall trend of the WOMAC pain scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
Figure 4 demonstrates the overall change in WOMAC stiffness scores over the treatment period for both groups. The large difference in baseline WOMAC stiffness scores between the two groups did not allow direct comparison of scores at 2, 4, and 6 weeks of treatment. Therefore, a comparison of the difference from baseline scores at 2, 4, and 6 weeks of treatment between the two groups was performed instead, and test scores were adjusted using the Bonferroni method. The results showed that the difference between the stiffness values at baseline and after treatment was slightly larger in the WM-CM group than in the WM group, but the difference was not statistically significant (p > 0.017) (Table 5).

FIGURE 4. Overall trend of the WOMAC stiffness scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
Figure 5 demonstrates the overall changes in the WOMAC joint function scores of the two groups during the treatment period. With consistent baseline scores, the mean WOMAC joint function score was significantly lower in the WM-CM group than in the WM group after 6 weeks of treatment (11.45 ± 0.438 vs. 17.7 ± 0.986, p < 0.001) (Table 4).
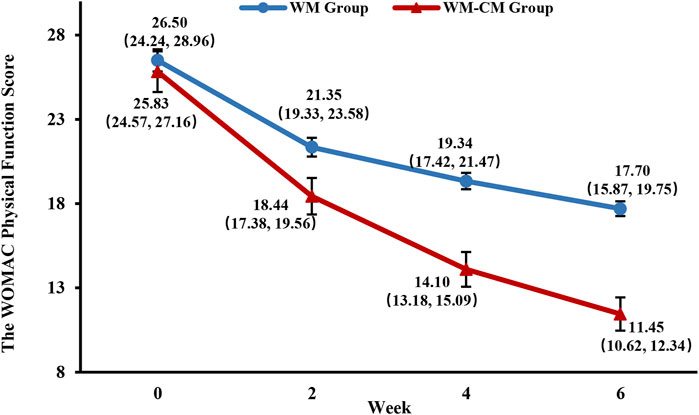
FIGURE 5. Overall trend of the WOMAC physical function scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
The VAS scores of both groups showed a significant decrease with the prolongation of treatment time, but the rate of decrease was faster in the WM-CM group (Figure 6). The intragroup and intergroup multiple comparisons of VAS scores between the two groups at each timepoint are detailed in Supplementary Table S3. After 6 weeks of treatment, the mean VAS score of the WM-CM group decreased to 2.24 ± 0.072, which was much lower than that of the WM group, which was 2.97 ± 0.149 (p < 0.001) (Table 4).
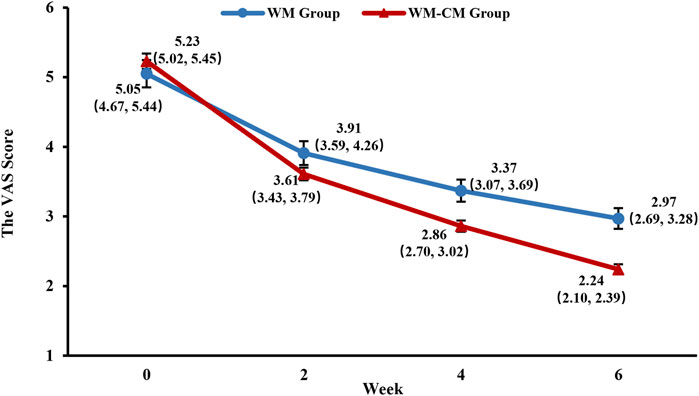
FIGURE 6. Overall trend of the VAS scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
As shown in Figure 7, with consistent scores at baseline, the PCS scores of patients in the WM-CM group began to be gradually higher than those in the WM group after 2 weeks of treatment, but the difference was not statistically significant (p = 0.135). After 4 weeks of treatment, the PCS scores of patients in the WM-CM group were significantly higher than those in the WM group (p = 0.008), and after 6 weeks of treatment, the difference between the two groups was even more significant (p < 0.001) (Table 4; Supplementary Table S3). Details of the results of the 4 dimensions PF, RP, BP, and GH at each follow-up timepoint, as well as multiple comparisons within and between groups, are provided in the supplemental file.
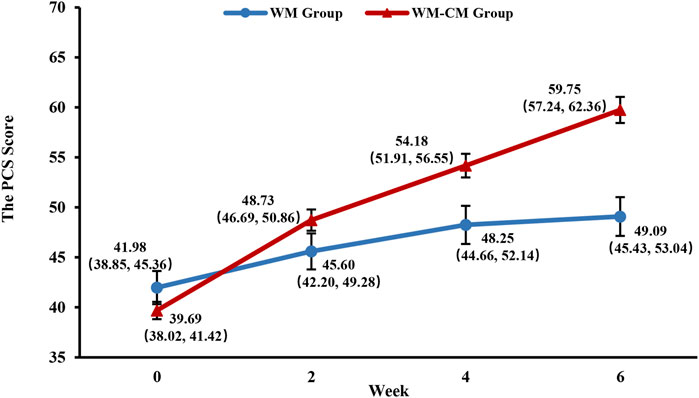
FIGURE 7. Overall trend of the PCS scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
As shown in Figure 8, the MCS scores in the WM-CM group showed a steady upward trend with the prolongation of treatment time, and after 6 weeks of treatment, the mean MCS scores of the two groups began to show significant differences (p = 0.009) (Table 4). Details of the results of the 4 dimensions VT, SF, RE, and MH at each follow-up timepoint, as well as multiple comparisons within and between groups, are provided in the supplemental file.
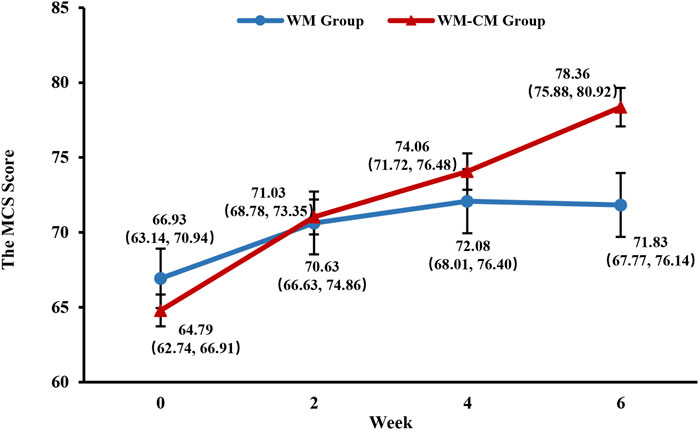
FIGURE 8. Overall trend of the MCS scores. Note: The values shown are least-squares mean calculated based on generalized linear mixed model, with 95% confidence intervals (indicated by error bars) in parentheses.
As shown in Table 6, the effective rate of the WM-CM group was as high as 95%, which exceeded that of the WM group (80.6%), and the difference was statistically significant (p < 0.001); the significant response rate of the WM-CM group was 63.6%, which exceeded that of the WM group (32%), and the difference was statistically significant (p < 0.001).
To examine the robustness of the results, we stratified patients by age, sex, and K-L grade and then compared the differences in changes in WOMAC total score between the two groups compared with baseline after 6 weeks of treatment in different subgroups using GLMM. As shown in Figure 9, in both the under-65 and over-65 age groups, the difference in WOMAC total score at baseline and after 6 weeks of treatment was larger in the WM-CM group than in the WM group, and the difference was significant (p < 0.001). The difference was more pronounced in the under-65 patient group. For both male and female patients, the improvement in WOMAC total score after 6 weeks of treatment was significantly better in the WM-CM group than in the WM group (p < 0.05). For patients with K-L classification 0-I, the WM-CM group performed better (p < 0.001), and for patients with grades II-III, the difference in WOMAC total score at baseline and after 6 weeks of treatment was slightly greater in the WM-CM group than in the WM group, but the difference was not significant (p = 0.091).
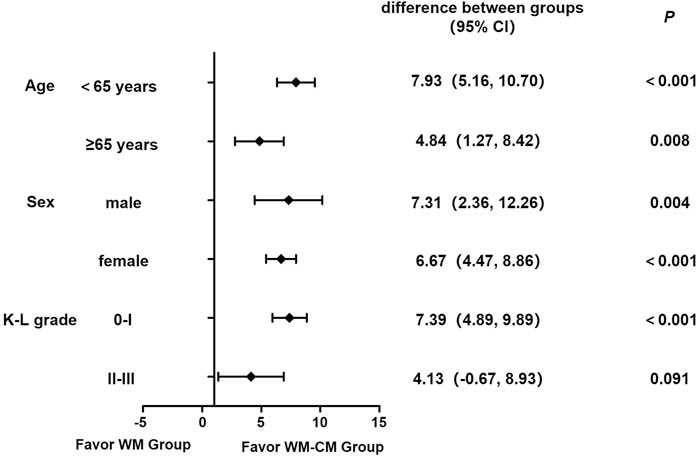
FIGURE 9. Forest plot for subgroup analysis. Note: The forest plot shows the differences in the changes in WOMAC total score between the two groups compared with baseline after 6 weeks of treatment stratifying by different subgroups. The difference between groups is calculated based on the least squares mean using GLMM, with a 95% confidence interval in parentheses. p values were Bonferroni corrected at a significance level of 0.05.
We focused on monitoring potential drug-related adverse events such as local pain and swelling from injections, gastrointestinal discomfort, cardiovascular events, and skin sensitization. No drug-related adverse events occurred in either group throughout the treatment cycle, and no patient discontinued the study due to adverse events.
KOA has become a medical problem plaguing the world due to its high morbidity, high disability, high health hazard and high economic burden. Currently, Western drug treatment of KOA is based on Nonsteroidal Anti-inflammatory Drugs (NSAIDs), glucosamine, and sodium citrate injections. Among them, NSAIDs are recognized as first-line agents, but gastrointestinal and cardiovascular safety risks exist (Blumenthal K.G., 2017; Lim W.B., 2022), while the use of glucosamine and sodium citrate injections is controversial in clinical practice due to varying efficacy reported in different studies (Clegg D.O., 2006; Fransen M., 2015; Jevsevar D., 2015; Reginster J.Y., 2017; Honvo G., 2019; Peng B., 2019; Cai Z., 2022). Recently, there has been increasing evidence that TCM therapy is effective in preventing and treating KOA, improving clinical efficiency and reducing adverse effects (Zhu G.Q., 2014; Wu H.Y., 2015; Yu T. M, 2018), especially with Chinese patent medicines such as Xianling Gubao capsules, Zhuangguguanjie capsules, Jintiange capsules, Xiaotong patch and compound Nanxing analgesic ointment, which are recommended in many clinical guidelines in China (project group, 2021; Chen W.H., 2020; Association, 2021).
Most of the TCM preparations observed in this study have been proven to be effective in treating KOA in previous clinical researches (project group, 2021; Zhao J., 2022; Zhang W., 2016; Wu K.Y., 2015; Li X.L., 2019; Tan W.X., 2014; Guo X.X., 2017; Kang X.Z., 2011). However, it is important to note that these findings were obtained in the context of clinical trials and require verification in real-life clinical practice. The treatment process of TCM is highly individualized and complex, and the real medical environment is significantly more intricate than the controlled setting of a clinical trial. Therefore, real-world studies are essential to truly and comprehensively evaluate the effectiveness of complex TCM intervention programs. As far as we know, there have been very few large-scale real-world studies evaluating the overall efficacy of TCM combined with chemotherapy in the KOA field. Our early initiation of this research has the potential to garner attention from medical professionals, patients, and administrative personnel alike towards the benefits of TCM. We hope that the results of this research will receive the attention they deserve, enabling more KOA patients to benefit from the integration of TCM into their treatment plans.
In this study, we investigated the efficacy and safety of combined Chinese and Western medicine protocols for KOA patients with K-L score of 3 or less based on real clinical treatment scenarios. It was found that the combination of Chinese and Western medicine had significant advantages over Western medicine alone in relieving pain, improving knee function, and improving quality of life, and there was no significant difference between the two groups in relieving stiffness symptoms, but the interference caused by the insufficient reliability of the stiffness dimension of the WOMAC scale could not be excluded (Van de Graaf V.A., 2014), which needs to be further determined by combining other scales in future studies. In addition, subgroup analysis found that the benefit of the combination therapy group was more pronounced in younger patients under 65 years of age and in patients with milder disease with a K-L grade of 0-I. To some extent, this suggests an early intervention of TCM therapy.
The functions of the drugs used in this study are mainly to dispel wind and dampness, activate blood to relieve pain, and tonify the liver and kidney. “Jin-Gu theory” in TCM can make a reasonable explanation for why these drugs are selected in clinical practice. This theory regards KOA as a kind of “Jin-Gu” disease, and “Jin-Gu” refers to both the location of the disease and the different stages of the disease. When the disease is located in the “Jin”, it mainly affects the soft tissues around the knee. At this time, the disease is still in the early stage, which is an excess syndrome. It is necessary to use medicines for dispelling wind and dampness, and promoting blood circulation to soothe sinews and harmonize collaterals. When the disease is located in the “Gu”, the disease progresses and involves articular cartilage and bone tissue, and some symptoms of deficiency syndrome appear. Therefore, medicines for tonifying the liver and kidney are often chosen to protect cartilage and strengthen the bone.
Although most TCM doctors prescribe prescriptions based on TCM theory, the understanding of the active ingredients and targets of TCM is of great significance for elucidating the drug mechanism and even for the development of TCM. At present, studies have pointed out that Duhuo Jisheng Decoction and Yougui Pill can regulate the Wnt/β-catenin signaling pathway, thereby inhibiting the synovial inflammation and protecting articular cartilage (Lyu S., 2017; Yan C.L., 2018; Shi Q., 2022). Wangbi Tablet inhibits cartilage damage and inflammatory response by down-regulating NF-κB and p38-MAPK signaling pathways (Li H., 2021). The potential mechanism of Zhuifeng Tougu Pill against KOA may be the inhibition of TLR4/MyD88/NF-kB signaling pathway and inflammatory cytokines (Xu X., 2022). External preparations such as Wentong ointment and Daiwenjiu Ointment may promote the apoptosis of inflammatory cells, reduce the inflammatory response and inhibit neovascularization (Peng Y.L., 2014; Zhang L.W., 2022). Some botanical drugs frequently appear in these TCM prescriptions, showing immense potential in the treatment of KOA. Rehmanniae Radix Praeparata (Shu-Di-Huang) and Notopterygii Rhizoma Et Radix (Qiang-Huo) show significant anti-inflammatory effects (Pan T., 2017; Jhun J.Y., 2018). Drynariae Rhizoma (Gu-Sui-Bu) and its active components exhibit properties such as inhibiting inflammatory reactions, improving oxidative stress, suppressing cell apoptosis, regulating autophagy, influencing hormone levels, and enhancing microcirculation (Yang Y.J., 2021). Sodium ferulate, abundant in Angelicae Sinensis Radix (Dang-Gui), demonstrates remarkable anti-inflammatory and anti-apoptotic characteristics, while its polysaccharide component promotes the biosynthesis of proteoglycans in cartilage matrix (Magdalou J., 2015). Safflower yellow from Carthami Flos (Hong-Hua) protects chondrocytes and inhibits inflammation by regulating the NF-κB/SIRT1/AMPK pathway and ER stress (Wang C., 2020).
When selecting evaluation indicators, we refer to previous internationally influential literature and Chinese guidelines (Lu Z., 2018; Chen W.H., 2020; Belk J.W., 2021). In this study, the total score of WOMAC scale was used as the main efficacy index, which can comprehensively reflect the overall state of the knee joint of patients, and has high sensitivity and reliability for elderly patients and patients with mild symptoms (Walker L.C., 2018). The VAS score is mainly to quantify and visualize the pain symptoms of patients (Xu X.M., 2021), which is simpler and easier to understand than the WOMAC scale, and can be mutually corroborated with the WOMAC pain score. In addition, considering that chronic pain is significantly related to psychological depression and seriously affects the quality of life of patients, we also adopted the SF-36 scale, which is often used in combination with the WOMAC scale in the evaluation of the efficacy of KOA (Angst F., 2001).
We chose mature products that have been marketed for many years or in-hospital preparations developed from classical prescriptions or experimental prescriptions, and administered them following the recommended conventional methods stated in the instruction manual. This approach has three major advantages. Firstly, it provides clear side effect profiles, enabling us to better monitor adverse events and determine the correlation between adverse events and the medication. This study focused on monitoring all possible adverse events, and no drug-related adverse events occurred in either group throughout the treatment cycle. This strongly demonstrates the safety of short-term drug application as observed in our study. Secondly, the protocol is easy to replicate as the selected drugs are readily available, making it possible to repeat the study and apply the research plan more easily to a broader context. Thirdly, it reflects the real-world application of the medication, providing direct reference evidence for clinical treatment plan development.
Although this study controlled confounding factors through prospective design and statistical processing, it still has the common limitations of real-world studies. It is difficult to achieve randomization and blinding in real-world studies. Compared with randomized controlled trials, there are more confounding factors and bias. For example, our research center comprises two traditional Chinese medicine hospitals and one comprehensive hospital. Patients seen at the traditional Chinese medicine hospitals tend to lean towards receiving combined Chinese and Western medicine treatment, while patients visiting the comprehensive hospital are more inclined to undergo Western medicine treatment. Patient treatment preferences could introduce some bias into the study. In addition, the subjects of this study mainly come from three medical institutions, limiting the generalizability of the research conclusions to other populations. Therefore, cautious consideration is necessary when extrapolating the research conclusions to other populations. Moreover, due to the complexity of the intervention measures, the sample size currently included is still insufficient for conducting subgroup analysis of treatment regimens to further explore the differences in therapeutic effects among various approaches and their associations with disease phenotypes. Nonetheless, the results of our study do provide preliminary confirmation of the overall advantages of integrated Chinese and Western medicine in treating KOA. In the future, we will include more research centers and continue to increase the sample size to enhance the objectivity and rigor of our conclusions. The accumulation of research data will also facilitate further prescription analysis, helping us identify drugs with greater potential research value, leading to targeted randomized controlled trials and mechanism studies.
In summary, our findings demonstrate that TCM can be an important complementary therapy to conventional Western conservative treatment and should be used early and promptly. This conclusion still needs to be validated by further large cohort studies or randomized controlled trials.
The original contributions presented in the study can be found in the article and in the Supplementary Material. The data underlying this article will be shared on reasonable request to the corresponding author.
The studies involving humans were approved by the Ethics Committee of the First Hospital of Jinan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
R-HZ and X-FZ provided oversight and leadership responsibilities for planning and executing the research activities. LH offered guidance in revising the manuscript and enhancing its quality. Q-YY designed the entire clinical study, analyzed the data, and drafted the paper. X-LH, Y-MY, B-LZ, TL, W-QZ, H-YW, Z-FZ, B-JL, Y-WX, A-LW, YL, QL, and Z-LZ conducted research across various centers and participated in data collation. QL, L-YL, X-YL, P-PW, and LY were involved in manuscript revision. All authors contributed to the article and approved the submitted version.
This work was supported by National Key R&D Program of China (No. 2018YFC2002500), Guangdong Provincial Key Laboratory of Traditional Chinese Medicine Informatization (No. 2021B1212040007), the National Natural Science Foundation of China (No. 82074287 and 82274232), Guangdong Provincial Bureau of Chinese Medicine Research Project (No. 20223009), and Medical Joint Fund of Jinan University (No. YXZY2022026).
The authors thank Lei Wan, Sheng-Ting Chai, and Guo-Qiang Ye of the Third Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine and Associate Huan-Tian Zhang of the First Affiliated Hospital of Jinan University for their help in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1176980/full#supplementary-material
KOA, knee osteoarthritis; WM group, Western medicine treatment group; WM-CM group, Combined Western and traditional Chinese medicine treatment group; PCS, Physical Component Summary; MCS, Mental Component Summary; WOMAC, Western Ontario and McMaster Universities Arthritis Index; VAS, the visual analogue scale; SF-36, 36-item short form; physical functioning; RP, physical functioning; BP, physical pain; CH, general health; VT, vitality; SF, social functioning; RE, emotional functioning; MH, mental health; GLMM, generalized linear mixed models; K-L, Kellgren-Lawrence; TCM, traditional Chinese medicine; NSAIDs, Nonsteroidal Antiinflammatory Drugs.
Angst, F., Aeschlimann, A., and Stucki, G. (2001). Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 45 (4), 384–391. doi:10.1002/1529-0131(200108)45:4<384:AID-ART352>3.0.CO;2-0
Bannuru, R. R., Osani, M. C., Vaysbrot, E. E., Arden, N. K., Bennell, K., Bierma-Zeinstra, S. M. A., et al. (2019). OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 27 (11), 1578–1589. doi:10.1016/j.joca.2019.06.011
Belk, J. W., Kraeutler, M. J., Houck, D. A., Goodrich, J. A., Dragoo, J. L., and McCarty, E. C. (2021). Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Am. J. Sports Med. 49 (1), 249–260. doi:10.1177/0363546520909397
Blumenthal, K. G., Lai, K. H., Huang, M., Wallace, Z. S., Wickner, P. G., and Zhou, L. (2017). Adverse and hypersensitivity reactions to prescription nonsteroidal anti-inflammatory agents in a large health care system. J. Allergy Clin. Immunol. Pract. 5 (3), 737–743. doi:10.1016/j.jaip.2016.12.006
Cai, Z., Cui, Y., Wang, J., Qi, X., He, P., Bu, P., et al. (2022). A narrative review of the progress in the treatment of knee osteoarthritis. Ann. Transl. Med. 10 (6), 373. doi:10.21037/atm-22-818
Cao, Y., Shi, Y., Zheng, Y., Shi, M., and Lo, S. K. (2005). Blood-nourishing and hard-softening capsule costs less in the management of osteoarthritic knee pain: A randomized controlled trial. Evid. Based Complement. Altern. Med. 2 (3), 363–368. doi:10.1093/ecam/neh104
Chen, B., Zhan, H., Marszalek, J., Chung, M., Lin, X., Zhang, M., et al. (2016). Traditional Chinese medications for knee osteoarthritis pain: A meta-analysis of randomized controlled trials. Am. J. Chin. Med. 44 (4), 677–703. doi:10.1142/S0192415X16500373
Chen, W. H., Han, Y. F., Liang, J. D., Tian, W. Y., and Liang, Z. Q. (2020). Morphological and phylogenetic characterisations reveal three new species of Samsoniella (Cordycipitaceae, Hypocreales) from Guizhou, China. J. Traditional Chin. Orthop. Traumatology 32, 1–15. doi:10.3897/mycokeys.74.56655
Clegg, D. O., Reda, D. J., Harris, C. L., Klein, M. A., O'Dell, J. R., Hooper, M. M., et al. (2006). Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N. Engl. J. Med. 354 (8), 795–808. doi:10.1056/NEJMoa052771
Committee of Orthopedics and Traumatology of the Chinese Society of Integrated Traditional and Western Medicine, (2018). Guidelines for diagnosis and treatment of knee osteoarthritis with integrated traditional and Western medicine. Natl. Med. J. China 98, 3653–3658. doi:10.3760/cma.j.issn.0376-2491.2018.45.005
Deng, Y. L. (2021). A Meta-analysis of treating knee osteoarthritis in the integrative medicine. Clin. J. Chin. Med. 13 (13), 134–138. doi:10.3969/j.issn.1674-7860.2021.13.043
Deyle, G. D., Allen, C. S., Allison, S. C., Gill, N. W., Hando, B. R., Petersen, E. J., et al. (2020). Physical therapy versus glucocorticoid injection for osteoarthritis of the knee. N. Engl. J. Med. 382 (15), 1420–1429. doi:10.1056/NEJMoa1905877
Deyle, G. D., Gill, N. W., Rhon, D. I., Allen, C. S., Allison, S. C., Hando, B. R., et al. (2016). A multicenter randomised, 1-year comparative effectiveness, parallel-group trial protocol of a physical therapy approach compared to corticosteroid injection on pain and function related to knee osteoarthritis (PTA Trial). BMJ Open 6 (3), e010528. doi:10.1136/bmjopen-2015-010528
Feng, X. Q., Cai, D. Z., Yu, X. L., Zhou, S. J., and Jiang, W. (2022). Analysis of current status and trends of disease burden of knee osteoarthritis in China based on GBD big data. Mod. Prev. Med. 49 (10), 1753–1760. doi:10.3969/j.issn.1003-8507.2022.10.xdyfyx202210005
Fransen, M., Agaliotis, M., Nairn, L., Votrubec, M., Bridgett, L., Su, S., et al. LEGS study collaborative group (2015). Glucosamine and chondroitin for knee osteoarthritis: A double-blind randomised placebo-controlled clinical trial evaluating single and combination regimens. Ann. Rheum. Dis. 74 (5), 851–858. doi:10.1136/annrheumdis-2013-203954
Gbd 2017 Disease and Injury Incidence and Prevalence Collaborators, (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet 392 (10159), 1789–1858. doi:10.1016/S0140-6736(18)32279-7
Guo, X. X., Wu, X. R., Huang, X. B., and Xie, H. M. (2017). Clinical observation on Wentong paste in treating knee osteoarthritis of wind-cold-damp syndrome. J. Chin. Med. Mater. 40 (10), 2466–2468. doi:10.13863/j.issn1001-4454.2017.10.052
Honvo, G., Reginster, J. Y., Rannou, F., Rygaert, X., Geerinck, A., Rabenda, V., et al. (2019). Safety of intra-articular hyaluronic acid injections in osteoarthritis: outcomes of a systematic review and meta-analysis. Drugs Aging 36 (Suppl. 1), 101–127. doi:10.1007/s40266-019-00657-w
Huang, D., Liu, Y. Q., Liang, L. S., Lin, X. W., Song, T., Zhuang, Z. G., et al. (2018). The diagnosis and therapy of degenerative knee joint disease: expert consensus from the Chinese pain medicine panel. Pain Res. Manag. 13, 2010129. doi:10.1155/2018/2010129
Jang, S., Lee, K., and Ju, J. H. (2021). Recent updates of diagnosis, pathophysiology, and treatment on osteoarthritis of the knee. Int. J. Mol. Sci. 22 (5), 2619. doi:10.3390/ijms22052619
Jevsevar, D., Donnelly, P., Brown, G. A., and Cummins, D. S. (2015). Viscosupplementation for osteoarthritis of the knee: A systematic review of the evidence. J. Bone Jt. Surg. Am. 97 (24), 2047–2060. doi:10.2106/JBJS.N.00743
Jhun, J. Y., Na, H. S., Shin, J. W., Jung, K. A., Seo, H. B., Ryu, J. Y., et al. (2018). Notoginseng radix and rehmanniae radix preparata extract combination (YH23537) reduces pain and cartilage degeneration in rats with monosodium iodoacetate-induced osteoarthritis. J. Med. Food. 21 (8), 745–754. doi:10.1089/jmf.2017.4041
Joint Surgery Group of Chinese Medical Association, , and Osteoarthritis Group of Chinese Medical Association, National Clinical Medical Research Center for Geriatrics (Xiangya Hospital), (2021). Chinese guidelines for the diagnosis and treatment of osteoarthritis (version 2021). Chin. J. Orthop. 41, 1291–1314. doi:10.3760/cma.j.cn121113-20210624-00424
Kang, X. Z., Wu, Q. F., and Jie, H. Y. (2011). Clinical study on the treatment of knee osteoarthritis by wangbi tablet. Zhongguo Zhong Xi Yi Jie He Za Zhi 31 (9), 1205–1208.
Li, H., You, Y., Jiang, B., Li, H., Li, X., Wu, W., et al. (2021). Wang-Bi tablet ameliorates DMM-induced knee osteoarthritis through suppressing the activation of p38-MAPK and NF-κB signaling pathways in mice. Evid. Based Complement. Altern. Med. 2021, 3930826. doi:10.1155/2021/3930826
Li, R., Bai, L., and Li, S. Z. (2013). Research progress on TCM treatment models for knee osteoarthritis. J. Changchun Univ. Chin. Med. 29 (6), 1140–1142. doi:10.3969/j.issn.1008-8849.2014.01.046
Li, X. L., Xu, D. X., and Chen, W. C. (2019). Clinical study on therapy of muscular thermal conductivity of silver needle combined with external application for early knee osteoarthritis. New Chin. Med. 51 (04), 215–217. doi:10.13457/j.cnki.jncm.2019.04.065
Lim, W. B., and Al-Dadah, O. (2022). Conservative treatment of knee osteoarthritis: A review of the literature. World J. Orthop. 13 (3), 212–229. doi:10.5312/wjo.v13.i3.212
Lu, Z., Li, X., Chen, R., and Guo, C. (2018). Kinesio taping improves pain and function in patients with knee osteoarthritis: A meta-analysis of randomized controlled trials. Int. J. Surg. 59, 27–35. doi:10.1016/j.ijsu.2018.09.015
Lundberg, M., Johansson, M. S., Søndergaard, J., and Thorlund, J. B. (2022). Opioid use among Danish patient s with severe knee osteoarthritis: A drug utilization study. Eur. J. Clin. Pharmacol. 78 (9), 1481–1486. doi:10.1007/s00228-022-03350-x
Lyu, S., Ji, B., Gao, W., Chen, X., Xie, X., and Zhou, J. (2017). Effects of Angelicae Pubescentis and Loranthi Decotion on repairing knee joint cartilages in rats. J. Orthop. Surg. Res. 12 (1), 189. doi:10.1186/s13018-017-0679-8
Magdalou, J., Chen, L. B., Wang, H., Qin, J., Wen, Y., Li, X. J., et al. (2015). Angelica sinensis and osteoarthritis: A natural therapeutic link? Biomed. Mater. Eng. 25 (Suppl. l), 179–186. doi:10.3233/BME-141250
Mahmoudian, A., Lohmander, L. S., Mobasheri, A., Englund, M., and Luyten, F. P. (2021). Early-stage symptomatic osteoarthritis of the knee-time for action. Nat. Rev. Rheumatol. 17 (10), 621–632. doi:10.1038/s41584-021-00673-4
Nishida, Y., Kano, K., Nobuoka, Y., and Seo, T. (2021). Efficacy and safety of diclofenac-hyaluronate conjugate (diclofenac etalhyaluronate) for knee osteoarthritis: A randomized phase III trial in Japan. Arthritis Rheumatol. 73 (9), 1646–1655. doi:10.1002/art.41725
Pan, T., Cheng, T. F., Jia, Y. R., Li, P., and Li, F. (2017). Anti-rheumatoid arthritis effects of traditional Chinese herb couple in adjuvant-induced arthritis in rats. J. Ethnopharmacol. 205, 1–7. doi:10.1016/j.jep.2017.04.020
Peng, B., Bogduk, N., DePalma, M. J., and Ma, K. (2019). Chronic spinal pain: pathophysiology, diagnosis, and treatment. Pain Res. Manag. 2019, 1729059. doi:10.1155/2019/1729059
Peng, Y. L., Li, Y. M., and Peng, S. Z. (2014). Study on anti-inflammatory effect of Dai Wenjiu ointment. Hunan J. Traditional Chin. Med. 30 (10), 148–149. doi:10.16808/j.cnki.issn1003-7705.2014.10.078
Pereira, D., Peleteiro, B., Araújo, J., Branco, J., Santos, R. A., and Ramos, E. (2011). The effect of osteoarthritis definition on prevalence and incidence estimates: A systematic review. Osteoarthr. Cartil. 19 (11), 1270–1285. doi:10.1016/j.joca.2011.08.009
Reginster, J. Y., Dudler, J., Blicharski, T., and Pavelka, K. (2017). Pharmaceutical-grade chondroitin sulfate is as effective as celecoxib and superior to placebo in symptomatic knee osteoarthritis: the ChONdroitin versus CElecoxib versus placebo trial (CONCEPT). Ann. Rheum. Dis. 76 (9), 1537–1543. doi:10.1136/annrheumdis-2016-210860
Shi, Q., Huang, L., Duan, J., Kuang, G., Lu, M., and Tan, X. (2022). The effects of Jiawei Duhuo Jisheng mixture on Wnt/β-catenin signaling pathway in the synovium inflamed by knee osteoarthritis: an in vitro and in vivo experiment. J. Ethnopharmacol. 294, 115363. doi:10.1016/j.jep.2022.115363
Standardization project group of Clinical Practice Guidelines for Dominant Diseases Treated with Chinese Patent Medicine, (2021). Guidelines for clinical application of Chinese patent medicine in the treatment of knee osteoarthritis (2020). Chin. J. Integr. Traditional West. Med. 41 (5), 522–533. doi:10.7661/j.cjim.20210225.104
Tan, W. X., and Li, G. S. (2014). Li guanghai wind-dispelling plaster for traumatic injury +Sinew-stretching and fumigation-washing granules on knee osteoarthritis: A clinical observation. Glob. Tradit. Chin. Med. 7 (09), 687–690. doi:10.3969/j.issn.1674-1749.2014.09.007
Tang, X., Wang, S., Zhan, S., Niu, J., Tao, K., Zhang, Y., et al. (2016). The prevalence of symptomatic knee osteoarthritis in China: results from the China health and retirement longitudinal study. Arthritis Rheumatol. 68 (3), 648–653. doi:10.1002/art.39465
Van de Graaf, V. A., Wolterbeek, N., Scholtes, V. A., Mutsaerts, E. L., and Poolman, R. W. (2014). Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am. J. Sports Med. 42 (6), 1408–1416. doi:10.1177/0363546514524698
Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet 380, 2163–2196. doi:10.1016/S0140-6736(12)61729-2
Walker, L. C., Clement, N. D., Bardgett, M., Weir, D., Holland, J., Gerrand, C., et al. (2018). The WOMAC score can be reliably used to classify patient satisfaction after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 26 (11), 3333–3341. doi:10.1007/s00167-018-4879-5
Wang, C., Gao, Y., Zhang, Z., Chi, Q., Liu, Y., Yang, L., et al. (2020). Safflower yellow alleviates osteoarthritis and prevents inflammation by inhibiting PGE2 release and regulating NF-κB/SIRT1/AMPK signaling pathways. Phytomedicine 78, 153305. doi:10.1016/j.phymed.2020.153305
Wang, X., Jin, X., Han, W., Cao, Y., Halliday, A., Blizzard, L., et al. (2016). Cross-sectional and longitudinal associations between knee joint effusion synovitis and knee pain in older adults. J. Rheumatol. 43 (1), 121–130. doi:10.3899/jrheum.150355
Wu, H. Y., and Shu, Y. F. (2015). Observation on curative effect of integrated traditional Chinese and Western medicine combined with nursing intervention on knee osteoarthritis. New Chin. Med. 47 (11), 224–225. doi:10.13457/j.cnki.jncm.2015.11.099
Wu, K. Y., Zhu, Q. D., Huang, W. B., and Zhong, J. M. (2015). Clinical observation on treating arthritis with wenxing jingjintong tie plaster. J. Chin. Med. Mater. 38 (06), 1331–1333. doi:10.13863/j.issn1001-4454.2015.06.056
Xu, X., Li, N., Wu, Y., Yan, K., Mi, Y., Yi, N., et al. (2022). Zhuifeng tougu capsules inhibit the TLR4/MyD88/NF-κB signaling pathway and alleviate knee osteoarthritis:in vitro and in vivo experiments. Front. Pharmacol. 13, 951860. doi:10.3389/fphar.2022.951860
Xu, X. M., Liu, W. G., Xu, S. C., Li, Y. K., Zhang, Q. W., Huang, H. X., et al. (2021). Clinical practice guidelines for knee osteoarthritis in integrated traditional Chinese and Western medicine. J. Pract. Med. 37 (22), 2827–2833. doi:10.3969/j.issn.1006-5725.2021.22.001
Yan, C. L., Li, S. H., An, F. Y., Liu, Y. Q., Xia, P. F., Ma, Z. M., et al. (2018). The therapeutic effects of Yougui pill on knee osteoarthritis and the expression of Wnt signal pathway related factors in rats. Zhongguo Ying Yong Sheng Li Xue Za Zhi 34 (2), 177–181. doi:10.12047/j.cjap.5603.2018.043
Yang, Y. J., Wang, J. F., Fan, C. B., and Guan, X. F. (2021). Exploring the potential mechanism of Gusuibu(Drynariae Rhizoma)in the treatment of osteoarthritis based on network pharmacology and molecular docking. J. Liaoning Univ. Traditional Chin. Med. 23 (12), 159–165. doi:10.13194/j.issn.1673-842x.2021.12.034
Yu, T. M., Miao, H. L., and Gao, F. (2018). Effect of treating knee osteoarthritis with combination of TCM and western medicine. Liaoning J. Traditional Chin. Med. 45 (4), 771–773. doi:10.13192/j.issn.1000-1719.2018.04.035
Zhang, J. H., Sun, X., Li, Y. P., and Zhang, B. L. (2019). Evidence-based traditional Chinese medicine: present and future. Chin. J. Evidence-Based Med. 19 (5), 1722. doi:10.7507/1672-2531.201904053
Zhang, L. W., Weng, J. X., Wu, H., Huang, X. B., Zhong, B. L., and Wu, X. R. (2022). Network pharmacology analysis of Wentong ointment for the treatment of knee osteoarthritis. Traditional Chin. Drug Res. Clin. Pharmacol. 33 (09), 1228–1235. doi:10.19378/j.issn.1003-9783.2022.09.011
Zhang, W., Wang, S., Zhang, R., Zhang, Y., Li, X., Lin, Y., et al. (2016). Evidence of Chinese herbal medicine Duhuo Jisheng decoction for knee osteoarthritis: A systematic review of randomised clinical trials. BMJ Open 6 (1), e008973. doi:10.1136/bmjopen-2015-008973
Zhang, Z., Huang, C., Cao, Y., Mu, R., Zhang, M. C., Xing, D., et al. (2021). 2021 revised algorithm for the management of knee osteoarthritis-the Chinese viewpoint. Aging Clin. Exp. Res. 33 (8), 2141–2147. doi:10.1007/s40520-021-01906-y
Zhang, Z., Huang, C., Jiang, Q., Zheng, Y., Liu, Y., Liu, S., et al. (2020). Guidelines for the diagnosis and treatment of osteoarthritis in China (2019 edition). Ann. Transl. Med. 8 (19), 1213. doi:10.21037/atm-20-4665
Zhao, J., Liang, G., Pan, J., Yang, W., Zeng, L., and Liu, J. (2022). Efficacy of Duhuo Jisheng decoction for treating cold-dampness obstruction syndrome-type knee osteoarthritis: A pooled analysis. Biomed. Res. Int. 2022, 2350404. doi:10.1155/2022/2350404
Keywords: knee osteoarthritis, combined Chinese and Western medicine, prospective cohort, efficacy, real-world study
Citation: Ye Q-Y, Lin Q, Hu X-L, Yang Y-M, Zheng B-L, Li T, Zhong W-Q, Wang H-Y, Zhang Z-F, Luo B-J, Xiao Y-W, Wu A-L, Li Y, Zou Z-L, Li L-Y, Li X-Y, Wang P-P, Yang L, Zhu X-F, Han L and Zhang R-H (2023) Efficacy and safety of combined Chinese and Western medicine in the treatment of knee osteoarthritis: a prospective, multicenter cohort study. Front. Pharmacol. 14:1176980. doi: 10.3389/fphar.2023.1176980
Received: 01 March 2023; Accepted: 15 August 2023;
Published: 28 August 2023.
Edited by:
Yi Guo, Tianjin University of Traditional Chinese Medicine, ChinaReviewed by:
Huanan Li, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, ChinaCopyright © 2023 Ye, Lin, Hu, Yang, Zheng, Li, Zhong, Wang, Zhang, Luo, Xiao, Wu, Li, Zou, Li, Li, Wang, Yang, Zhu, Han and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-Feng Zhu, enhpYW9mQGpudS5lZHUuY24=; Li Han, aGFubGkxNjhAYWxpeXVuLmNvbQ==; Rong-Hua Zhang, dHpyaEBqbnUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.