
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol., 13 June 2023
Sec. Translational Pharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1162370
This article is part of the Research TopicEthnopharmacology Research Based on Artificial Intelligence and Symptom PhenotypeView all 5 articles
Background: Frequently, the community pharmacies are the only points of consultation for upper-gastrointestinal symptomology. However, the heterogeneity of symptoms often limits the correct management of the patient. The study aim is to describe the epidemiological and clinical characteristics of patients with upper-gastrointestinal symptoms who ask for advice in community pharmacies.
Methods: A cross-sectional study was performed in 134 Spanish pharmacies (June-October 2022) and we included 1,360 patients. We collected sociodemographic, clinical variables and current medication data. The pharmacist evaluated the gastrointestinal symptoms through the application of the GERD Impact Scale (GIS questionnaire). Patients were classified into three groups according to their symptoms: epigastric, retrosternal and overlapping symptoms.
Results: Median age was 49 years (interquartile range 36–62 years) and 59.3% were women. Most patients reported overlapping symptoms (738%, 54.3%), 433 (31.8%) retrosternal and 189 (13.9%) epigastric symptoms. Patients with overlapping symptoms were more likely to associated consumption of foods and/or drinks and symptoms and showed lower scores on the GIS scale (median 26, IQR 20-30) than those with epigastric (median 32, IQR 29-33) and retrosternal (median 32, IQR 28-34) symptoms (p < 0.001). Patients in treatment with a combination of alginates and antiacids were more likely to think that it better alleviated their symptoms in all the patients included (p = 0.012).
Conclusion: More than half of the patients showed overlapping symptoms and were more likely to associate their symptoms with dietary habits and having poorer scores in the GIS scale. Clinical awareness of such overlapping condition would help optimize the management of patients with upper gastrointestinal symptoms in practice.
Functional Dyspepsia (FD) and Gastroesophageal Reflux (GER) are the two most prevalent upper gastrointestinal disorders (Ford et al., 2015; Eusebi et al., 2018b). FD is defined by the Rome IV criteria (Drossman and Hasler, 2016) as the presence of symptoms thought to originate in the gastroduodenal region. FD includes patients with postprandial distress syndrome (PDS), characterized by meal-induced dyspeptic symptoms, and patients with epi gastric pain syndrome (EPS), which refers to epigastric pain or burning that does not occur exclusively postprandially, may occur during fasting, and may even improve with meal intake; however, both syndromes can coexist (de Bortoli et al., 2018). It is reported to affect approximately 20% of the general population (Tack et al., 2006). GER, defined by the presence of frequent heartburn or acid regurgitation, also affects 20% of the population (Locke et al., 1997). Both diseases are frequently chronic, often need treatment and affect patients’ quality of life (Ronkainen et al., 2006). In addition, GER can lead to Gastroesophageal Reflux Disease (GERD), a more severe and long-lasting condition.
Previous studies demonstrated an overlap between GER and FD, mainly in those patients with EPS. A previous population study in 3,831 subjects found that FD and GER occurred together more commonly than expected by chance (Guillemot et al., 2005; Tack et al., 2005; Ghoshal et al., 2011; Choung et al., 2012). Other studies have also shown this overlap in a considerable proportion of patients. A recent systematic review of studies including general population found that FD and GER overlap in more than 25% of individuals (Eusebi et al., 2018a). The possible causes could include the presence of confounding factors as the infection by Helicobacter pylori or shared pathophysiological mechanisms. In general, chronic gastritis, a known consequence of a chronic H. pylori infection, is known to lead to a reduction in gastric acid secretion and a reduced prevalence of GERD. Lower rates of gastritis were also observed in patients with FD (Quigley and Lacy, 2013). Previous evidence found that a common pathophysiological mechanism might underlie both conditions (Choung et al., 2012); nevertheless, few studies have examined pathogenetic mechanisms among patients in whom these disorders coexist or overlap. A previous systematic review summarized pathophysiological mechanisms that could contribute to this overlap, including esophageal acid exposure, gastric dysmotility and visceral hypersensitivity (Geeraerts et al., 2020). Another study supporting the hypothesis of an underlying pathophysiological mechanism in FD and GERD demonstrated that impaired gastric accommodation, a well-accepted pathophysiological mechanism in FD, was related to the presence of transient lower esophageal sphincter relaxations, which are the main mechanism underlying reflux episodes in both healthy subjects and patients with GERD (Pauwels et al., 2014). In addition, another important feature of FD is the presence of duodenal eosinophilia, which has recently been shown to be associated with an increased risk of new-onset GERD in FD (Ronkainen et al., 2019). The diagnosis of this condition is therefore unclear and the development of uniform definitions for the diagnosis of overlapping GERD and FD would help clinicians in the establishment of treatment approaches rather than symptom-based treatment.
For many patients the community pharmacies are the first points of consultation for gastrointestinal symptomologies, due to their accessibility (Tytgat et al., 2008). Moreover, mild symptoms are often treated with over-the-counter(OTC) medication and patients do not usually visit their general practitioner unless their symptoms worsen, partly due to the burden on primary care. The literature shows that pharmacists play an important role in the management of mild gastrointestinal symptoms, recognizing alarm symptoms, confirming the diagnosis, referring to a specialist when necessary, and guiding patients with OTC treatment (Boardman and Heeley, 2015). Although dispensing OTC are not the best option for clinical care, it is a common strategy in community pharmacies. OTC and proton pump inhibitors (PPi) treatments without prescription are also included in some clinical guidelines, due to their use in daily practice, as patients’ symptoms are sometimes intermittent and mild (Haag et al., 2009). A previous consensus-based guideline on the OTC management of gastroesophageal reflux disease with PPIs, reflected that apart from the physician referral, when necessary, the pharmacist could specify an OTC treatment to control symptoms (Holtmann et al., 2011). Furthermore, a previous Delphi consensus reached by an international group of experts, showed that the use of OTC and PPi was not associated with a significant risk in the treatment of symptoms under the supervision of healthcare professionals (Johnson et al., 2017).
Given that these disorders frequently coexist, the ability of the pharmacist to distinguish between FD, GER and FD-GER overlap, which affect patients’ health in different ways and imply different treatment approaches (Eusebi et al., 2018a), is essential for patient management. Although lifestyle interventions are required in patients with upper-gastrointestinal symptoms are treated with a proton-pump inhibitor (PPI) because many healthcare professionals assume that all upper gastrointestinal symptoms are due to acid reflux. However, patients with FD show a low response rate to this treatment and thus, their symptoms persist (Pinto-Sanchez et al., 2017). To establish an accurate diagnosis in the community pharmacy, the evaluation of relevant clinical and sociodemographic variables that distinguish patients with overlap symptoms from those who have either FD or GER could support these health professionals to better optimize treatment approaches in these patients.
Considering this scenario, a protocol to manage patients with upper-gastrointestinal symptoms has been developed by community pharmacists, general practitioners and gastroenterologists with the support of the Spanish Society of Community Pharmacy (SEFAC) and the Spanish Society of General Practitioners (SEMERGEN) (Semergen, 2019). The objectives of this protocol are a) to describe the epidemiological characteristics of patients with upper gastrointestinal symptoms who attend a community pharmacy, and b) to provide a precise protocol for the pharmacist in the management of patients with upper-gastrointestinal symptoms.
In this study we aimed to describe the different epidemiological and clinical characteristics of patients with upper gastrointestinal symptoms, who attend community pharmacies for advice or to obtain an OTC medication.
A cross-sectional study was conducted to describe the sociodemographic and clinical characteristics of patients with upper gastrointestinal symptoms who attended community pharmacies between June and October 2022. This study is a part of a pre-post interventional study, whose protocol has already been published, which was carried out to evaluate the impact of a Professional Pharmaceutical Service on both patients’ symptoms and quality of life (López-Pintor et al., 2022).
We invited community pharmacists throughout the national territory to participate. In Spain, pharmacies are private healthcare establishments which work in concordance with the public health system and are subject to the health planning established by the Autonomous Communities. Although there is only one pharmacist owner per pharmacy, other pharmacists can work under the title of assistant pharmacist. Both pharmacists have the qualification requirements established by law, and are registered in the Official College of Pharmacists, according to Law 29/2006, the 26th July (BOE-A-2006-13554, 2006). In Spain, the Royal Decree 1/2015, the 24th July, regulates the sale of non-prescription medicines in pharmacies: non-prescription medicines can only be sold if they have been approved by the Spanish Agency for Medicines and Health Products.The pharmacist is obliged to inform patients about the correct use of medicines, precautions and side effects (BOE-A-2006-13554, 2006; BOE-A-2015-8343, 2015). At the end of 2021, there were 78,128 registered pharmacists and 22,198 community pharmacies in Spain. (Number of pharmacies in Spain 2007-2021, 2022).
We included patients ≥18 years who attended a community pharmacy due to the presence of upper gastrointestinal symptoms or who asked for treatment without prescription (over the counter -OTC- medication) for the treatment of these symptoms. We excluded those who asked for treatment for another person, or women with high-risk pregnancies. The study participants were only included if they had previously signed the informed consent form.
The sample size was estimated to fulfil the second of the objectives of the established protocol, which was to evaluate the impact of a Professional Pharmaceutical Service on both patients’ symptoms and quality of life. We estimated the number of people to assess 0.1 units of change over the GERD Impact Scale questionnaire (GIS), a 4-point Likert scale between 2 visits (from 2.2 to 1.1) with an SD of 0.6 through the estimation of the mean in repeated measures (López-Pintor et al., 2022). Taking into account an alpha risk of 0.05, two-sided test and a beta risk of 0.20 with a dropout of 20% we initially included 707 patients. However, we then increased the sample size to 1,200 patients (15 patients per variable) because we wanted to analyse different factors associated with relevant sociodemographic and clinical variables. This sample size allowed us to adequately describe the sociodemographic and clinical characteristics in patients with upper gastrointestinal symptoms who visited community pharmacies, which was the aim of the present study.
The Spanish Society for Community Pharmacy (SEFAC), RECKITT and the Universidad Miguel Hernandez (UMH) asked a random sample of community pharmacists to voluntarily participate in our study, and we adjusted the sample size to the population of each autonomous community, until the required sample size was reached. We invited 411 community pharmacies to participate, but finally 134 (32.6%) community pharmacies from 23 Spanish provinces were included in the study. We estimated that each community pharmacy would have to include a minimum of 5 patients to achieve sample size. All registered pharmacists received prior training by the research team on the objective, methodology and procedures of the study. This training was accredited by the Miguel Hernandez University of Elche, where the research team is located.
Patients who met the criteria were identified by a community pharmacist and then invited to participate in the study. First, the community pharmacist explained the study and gave them an information sheet (regarding privacy and details of the study) and if they agreed to participate, they signed the informed consent form. Patients were classified with an identification code: CA-III-PN (CA: autonomous community code; III: researchers initials; PN, and N represents participant’s number).
The pharmacist collected the sociodemographic and clinical information orally by means of a questionnaire. The sociodemographic characteristics included: a) age, b) sex (male or female), c) educational level: no studies, primary education, secondary education and university education. The clinical data included: a) body mass index (BMI) (kg/m2); b) reason for attending the pharmacy: seeking treatment advice or requesting OTC medication; c) requested treatments: antiacid monotherapy, a combination of alginates and antiacids, PPI; d) frequency of physical activity: every day, once or twice a week, 3-5 times a month and never; e) smoking habit: smokers, ex-smoker, never-smoker; f) frequency (daily/3-4 times a week, 1-4 times month, once a year or never) of consumption of foods and drinks associated with studied symptoms in the literature: alcoholic beverages, coffee, chocolate, tea, tomato, carbonated beverages, citrus food, spicy food, heavy or high-fat meals, and if the patients associate symptoms with their consumption of these items; g) onset of symptomatology (1–2 days ago, 3–4 days ago, 5–6 days ago, 7 days ago or more); h) presence of alarm criteria: symptoms (asthenia, dysphagia, recurrent vomiting, unexplained weight loss, gastrointestinal bleeding, severe pain, dyspnea, shortness of breath, nocturnal cough); intake of medicines often associated with symptoms (anti-inflammatory analgesics, bisphosphonates alendronates, calcium antagonists and/or nitrates, progesterone/oral contraceptives, tricyclic antidepressants/amitriptyline, theophylline, iron supplements, benzodiazepines, alpha-adrenergic antagonists/doxazosin and systemic corticosteroids), and diagnosis of gastrointestinal disorders or diseases (GERD, gastric ulcer, hiatus hernia, infection with H. pylori, food intolerances, colon disorders, gastritis); j) previous use of medicines to relieve symptoms, prescribed and/or OTC; k) GERD Impact Scale questionnaire (GIS) consisting in 5 questions: 1) location of symptoms, 2) effect of symptoms on eating and drinking habits, 3) effect of symptoms on sleep quality, 4) effect of symptoms on productivity at work and/or daily activities, 5) frequency of intake of unprescribed treatments. This questionnaire is validated in Spain (Nuevo et al., 2009).
We designed a database structured in accordance with the study variables. After the pharmacist had uploaded the information to the database, it was checked and validated by an external monitor. Only the principal researcher and the monitor had access to the database. The evaluation was carried out using IBM SPSS Statistics for Windows, version 27.0. Armonk, NY, USA: IBM Corp.
Patients were classified in 3 groups: a) patients with epigastric symptoms b) patients with retrosternal symptoms, and c) patients with overlapping epigastric and retrosternal symptoms. This classification was based on the one to five questions of GIS questionnaire related to localization of symptoms. Patients with epigastric symptoms were those who had a punctuation from 1 to 3 (frequency of symptoms: daily, often, or sometimes) in the question which refers to symptoms in the upper part of the stomach associated to the epigastric area and a 4 (never) in questions which refer to symptoms associated with the retrosternal area. Patients with retrosternal symptoms were those who had a punctuation from 1 to 3 (frequency of symptoms: daily, often, or sometimes) in questions which refer to symptoms associated with the retrosternal area and a punctuation of 4 (never) in the question which refers to symptoms associated to the epigastric area. Patients with overlapping symptoms were those who fulfilled both definitions.
Data were analysed and presented in descriptive form using absolute and relative frequencies with the 95% confidence interval, the GIS questionnaire responses were measured using a four-point Likert scale, and then a score is calculated, giving a number between 1 and 4. p-value <0.05 is considered significant.
A multivariate analysis was performed to measure the association between covariates (requested treatments, associations between alcoholic/carbonated drinks, spicy food and symptoms, frequency of avoiding eating or drinking foods because of the symptoms, use of prescribed/non prescribed treatment before to relief symptoms, previous treatment used) and retrosternal and both retrosternal and epigastric symptoms using a logistic regression model. We reported raw and multivariable adjusted odds ratios (ORs) with 95% CI and 0.05 < p-value was considered significant.
Of the 1,498 patients who attended a community pharmacy due to the presence of upper gastrointestinal symptoms or who asked for an OTC- medication, we included 1,360 (90.8%) patients (Figure 1). The included patients were divided into 3 groups according to their symptoms: 738 (54.3%) reported overlapping symptoms, 433 (31.8%) retrosternal symptoms, and 189 (13.9%) epigastric symptoms. Participants were predominantly female (807%, 59.3%), median (IQR) age was 49 years (36-62) and median (IQR) BMI was 25.8 kg/m2 (23.2–28.9). There were no differences between the different 3 groups according to age or sex. Most of the participants who went to the pharmacy were asking for an OTC medication to relieve their symptoms (773%, 57%). Most participants had university (474%, 34.9%) and secondary education (470%, 34.6%). According to lifestyle habits, 310 (22.8%) patients never practised physical activity and 699 (51.4%) were non-smokers (Table 1).
There were statistical differences according to the treatment requested. Antacid monotherapy was the most requested treatment in all groups (70.1%) and mainly in patients with epigastric symptoms (89.1%) in comparison with patients with retrosternal symptoms (70.5%) and overlapping symptoms (65.1%). A combination of alginate and antiacid (16.5%) and PPI (11%) were more frequently requested in patients with overlapping symptoms (11%) than in patients with epigastric (5.5%) and retrosternal symptoms (10.3%) (p = 0.001).
Table 2 shows the patients’ dietary habits according to consumption frequency. Coffee (957%, 70.4%), tomato (1,018%, 74.9%) and citrus fruits (700%, 51.5%) were more frequently consumed (daily/3-4 times per week). In contrast, alcohol beverages (551%, 40.5%), tea (883%, 64.9%), carbonated beverages (647%, 47.6%) and spicy food (868%, 63.8%) were less frequently consumed (once a year/never). There were no significant differences between the frequency of consumption and the different patients’ gastrointestinal symptoms.
There were differences between patients’ gastrointestinal symptoms and the food that patients associated with the symptoms. Patients who associated symptoms with consumption of alcohol beverages (p < 0.001), chocolate (p < 0.001), tomato (p < 0.001), carbonated beverages (p < 0.001), citrus fruits (p < 0.001), coffee (p = 0.017), tea (p = 0.014) and spicy food (p = 0.001) were more likely to present overlapping symptoms (Table 3).
Onset of symptoms was 1–2 days for most of patients (607%, 44.6%), and 7 days or more (556%, 40.9%). Patients whose symptoms had started 1–2 days ago were more likely to have only retrosternal symptoms (236%, 54.5%) than only epigastric (96%, 50.8%) or overlapping symptoms (275%, 35.3%) (p < 0.001). Patients whose symptoms had started 7 days or more ago were more likely to have overlapping symptoms (311%, 42.1%) than either only retrosternal (143, 33%) or only epigastric symptoms (60%, 31.7%) (p < 0.001) (data not shown).
Median GIS score was 21 (IQR 26-34) (Table 4). The group of patients with overlapping symptoms (median 26, IQR 20-30) had worst punctuation in the GIS score than patients with only epigastric (median 32, IQR 29-33) or retrosternal symptoms (median 32, IQR 28-34) (p < 0.001). Patients with overlapping symptoms (51%, 6.9%) reported daily difficult to sleep because of the symptoms more frequently than those with epigastric (9%, 4.8%) and retrosternal symptoms (14%, 3.2%). Moreover, patients with overlapping symptoms (68%, 9.2%) reported daily difficult to eating or drinking because of the symptoms more frequently than those with epigastric (24%, 5.5%) and retrosternal symptoms (3%, 1.6%). Daily difficult to being fully productive in their job and daily activities because of the symptoms was more frequently reported in patients with overlapping symptoms (28%, 3.8%) than those with epigastric (2%, 1.1%) and retrosternal symptoms (5%, 1.2%).
Women were more likely to report daily burning sensation in her chest or behind the breastbone than men (83%, 10.3% vs. 32%, 5.8%, p = 0.007). Women (88%, 10.9%) also reported more frequently presence of regurgitation or acid taste in her mouth daily than men (88%, 10.9% vs. 24%, 4.3%, p < 0.001), and more frequently sore throat or hoarseness that is related to her heartburn or acid reflux daily than men (41%, 5.1% vs. 11%, 2%, p = 0.030). In addition, women reported daily difficulty to sleep more frequently than men (78%, 9.7% vs. 17%, 3.1%, p < 0.001) and difficulties in daily activities (29%, 3.6% vs. 6%, 1.1%, p < 0.001). However, there were no differences in the median GIS score between women and men.
Of the 1,390 patients included in the study, 190 (14%) had asthenia and 118 (8.7%) severe pain, 258 (19%) patients had taken anti-inflammatory analgesics and 140 (10.3%) benzodiazepines, 171 (12.6%) patients had a diagnosis of hiatus hernia and 83 (6.1%) a diagnosis of GERD.
There were differences between the different alarm criteria detected between patients with overlapping symptoms and those with epigastric and retrosternal symptoms: Asthenia (136%, 18.4%%; 13, 6.9%, and 41%, 9.5%, respectively, p < 0.001), dysphagia (53%, 7.2%; 2%, 1.1% and 24%, 5.5%, respectively, p = 0.006), recurrent vomiting (58%, 7.9%; 1%, 0.5%% and 13%, 3%, respectively, p < 0.001), dyspnoea (73%, 9.9%; 1%, 0.5% and 20%, 4.6%, respectively, <p< .001) severe pain (85%, 11.5%; 10%, 5.3% and 23%, 5.3%, respectively, p < 0.001), intake of tricyclic antidepressants/amitriptyline (20%, 2.7%; 0 and 3%, 0.7%, respectively, p = 0.005), diagnosis of GERD (55, 7.5%; 3, 1.6% and 25, 5.8%, respectively, p = 0,001) and gastric ulcer (31%, 4.2%; 7, 3.7%, and 6%, 1.4%, respectively, p = 0.029) were more likely to be detected in patients with overlapping symptoms than in patients with epigastric or retrosternal symptoms.
Most patients (883%, 64.9%) had taken treatment to relief their symptoms previously to the inclusion in the study. Patients with epigastric symptoms were more likely to have an O-T-C medication (91%, 79.8%) than patients with retrosternal symptoms (158%, 60.3%) and those with overlapping symptoms (299%, 59%) (p = 0.006) (Table 5). Treatment with PPI (268%, 36.3%) were more frequently used in patients with overlapping symptoms than in patients with epigastric (42%, 22.2%) and retrosternal symptoms (128%, 29.6%). Patients with epigastric and retrosternal symptoms in treatment with a combination of alginate and antiacid were more likely to think that it better alleviated their symptoms (17%, 100% and 57%, 98.3% respectively) than patients with overlapping symptoms (100%, 86.2%), p = 0.012.
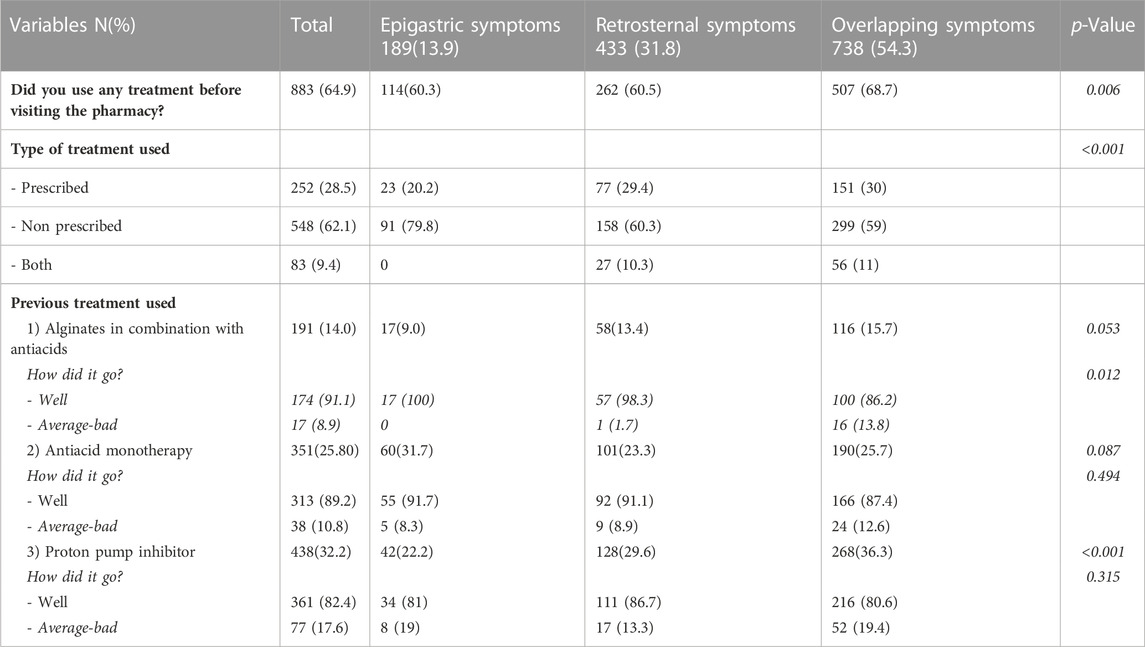
TABLE 5. Description of type of treatment used previously attending the pharmacy and treatment outcome in relieving symptoms.
In multivariate analysis comparing patients with overlapping symptoms with either retrosternal or epigastric symptoms, patients who associated alcoholic beverages with symptoms were more likely to have overlapping symptoms (aOR 1.41, 95% CI 1.01–1.85) than patients with either epigastric or retrosternal (p = 0.016). Patients who associated citrus with symptoms were more likely to have overlapping symptoms (aOR 1.40, 95% CI 1.05–1.86) than patients with either epigastric or retrosternal (p = 0.020). Patients with overlapping symptoms were less likely to never have difficulty to sleep than those with either epigastric or retrosternal symptoms (aOR 0.53, 95% CI 0,30-0.95 (p = 0.032). Patients with overlapping symptoms were less likely to never have difficulty to being fully productive in their job or daily activities than those with either epigastric or retrosternal symptoms (aOR 0.34, 95% CI 0,14-0.87 (p = 0.024).
In this study, 54.3% of patients presented overlapping symptoms, 31.8% of patients presented retrosternal symptoms and 13.9% of patients, epigastric symptoms. There were no differences in the clinical and sociodemographic variables associated with patients with different symptoms. However, patients with overlapping symptoms were more likely to relate their symptoms to their dietary habits and showed alarm criteria more frequently than those with epigastric and retrosternal symptoms. In addition, patients with overlapping symptoms had poorer scores in the GIS scale and were more likely to have taken a previous treatment with PPI. Antacid monotherapy was the most frequently requested treatment by all patient groups and most of the patients had previously used an OTC medication to relieve their symptoms. Patients with a previous treatment based on a combination of antacid and alginate were more likely to acknowledge an improvement in their symptoms.
The prevalence of overlapping symptoms in patients with upper-gastrointestinal symptoms in patients attending a community pharmacy was higher than previous frequencies shown in general population. A previous systematic review examined the overlapping symptomatology of GER and FD in the general population, and they found that both conditions overlap in more than 25% of individuals (Eusebi et al., 2018a). However, the included studies showed a high heterogeneity (ranging from 3% to 51%) due to the different population characteristics and the various instruments used to evaluate the symptoms.
Our results support previous evidence that FD-GER overlap is a separate clinical entity since patients with this condition were more likely to have more severe symptoms and other differential characteristics than those with either only epigastric or only retrosternal symptoms. A community study in Belgium undertook a survey of FD-GER symptoms in a random sample of 2,025 subjects (Piessevaux et al., 2009). As in our study, they found that patients with overlapping symptoms were more likely to have more severe and higher frequency of dyspeptic symptoms compared to dyspeptic subjects without heartburn.
Our results showed no significant association between lifestyle variables such as dietary habits or smoking habit and the three clinical conditions. Nevertheless, there were significant results when the patients themselves associated their symptomatology with specific dietary habits. Patients with overlapping symptoms more frequently associated their symptoms with the consumption of alcoholic beverages and citrus fruits than patients with either only epigastric or only retrosternal symptoms. In a previous systematic review, citrus fruits, carbonate beverages, spicy and fried foods were found to increase the risk of developing GER (Heidarzadeh-Esfahani et al., 2021). However, the authors concluded that more studies are needed to clarify the specific effect of diet on the disease. Although other systematic reviews stated that weight loss, smoking habit and intake of alcohol, chocolate, fatty food, spicy food and citrus showed a relationship with developing GER, they also concluded that additional clinical studies were required (Kaltenbach et al., 2006; Festi et al., 2009).Changing dietary habits are the first-line recommendation in gastrointestinal disorders, so carrying out further studies to evaluate specific food groups that can produce these symptoms could be important to improve or avoid symptomatology.
As in previous studies, we assessed impairment of quality of life using the GIS scale. We found similar scores in patients with either only retrosternal or only epigastric symptoms, but patients with overlapping symptoms showed the lowest scores. Some studies that used SF-36 found a greater impairment of quality of life in patients with overlapping symptoms which was consistent with our results (Kaji et al., 2010; Lee et al., 2014). In addition, patients with overlapping symptoms were more likely to show worse scores in the items related with insomnia, and impact of the symptoms on their eating/drinking intakes and on their daily activities than patients with either only epigastric or only retrosternal symptoms. Self-reported insomnia has been found to be a risk factor for FD-GER overlap compared to either only FD or only GER in several studies (Schey et al., 2007; Gerson and Fass, 2009), which showed that this association might be directional.
Most of the patients included in the study requested a specific treatment to relieve their symptoms than to seek pharmaceutical advice. In a Spanish study, 13% of patients had taken medication to control gastroesophageal reflux symptoms and antacid monotherapy was the most used medication (Ponce et al., 2006). In the present study, similarly, antiacid monotherapy was the most requested treatment followed by PPi therapy. PPi treatment is the first line of treatment included in the clinical guidelines of GER symptoms, and in a previously mentioned study, PPi treatment was more frequently used in patients with overlapping upper gastrointestinal symptoms in comparison to those with either only esophagic or only retrosternal symptoms (Choung et al., 2012). The presence of epigastric symptoms, however, has been showed as a risk factor for poorer response to PPi in GER patients (Matsuhashi et al., 2015). Therefore, overlapping FD and GER might have important effects on therapeutic responses. The combination of alginate and antiacid was the treatment with the highest level of patient satisfaction regarding symptom relief, especially in patients with either only epigastric or only retrosternal symptoms, but also showed positive results among those with overlapping symptoms. In the literature, some studies showed that alginates were more effective than placebo or antiacid monotherapy and had a similar effect to PPIs in the management of GER symptoms (Leiman et al., 2017; Zhao et al., 2020). In a German study, patients on chronic PPi treatment with additional alginates treatment showed an improvement in their GERD-Q score (Müller et al., 2019).
As many patients in our study went to a pharmacy requesting treatment, it is essential to review patients’ previous treatment considering their symptomatology to offer optimum symptom management and to optimize treatment approaches.
This study has several limitations. First, categorizing patients might be a limitation due to the heterogeneity of symptoms, but we included a pre-training of the research pharmacists and a monitor to validate the data collected to reduce potential bias. Another limitation is the fact that given that we performed a cross-sectional study, we were unable to establish a temporal relationship between the symptoms and clinical and sociodemographic variables.
One of the strengths is that it is the first study describing clinical and sociodemographic characteristics of patients with upper gastrointestinal symptoms attending a community pharmacy. Given the sample size and the distribution of the pharmacies along the national territory, we think our results could be generalised to other settings. In addition, we categorized patients into three groups of symptoms (epigastric, retrosternal and overlapping symptoms) to identify the different symptoms and variables associated with more precision, thus reflecting clinical practice. In addition, the present study was carried out following the outline of a protocol developed by gastroenterologists, primary care providers and community pharmacists (López-Pintor et al., 2022).
In conclusion, patients with overlapping symptoms were the most frequent clinical condition detected in the patients included in our study. In addition, these patients were more likely to associate their symptoms with dietary habits, had poorer scores in the GIS scale and used more PPi therapy before visiting the pharmacy than those with either only epigastric or only retrosternal symptoms. These findings suggest that overlap patients may represent a different condition and thus need different management strategies in the community pharmacy.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethic Committee of Hospital Sant Joan d’Alacant (code: 19/335 Tut). The patients/participants provided their written informed consent to participate in this study.
BL and EL-P conceived of and designed the study, and EL-P obtained funding. EL-P coordinated the data management, and BL wrote the study protocol. EL-P and MP-M acquired the data. MP-M and BL prepared the data. MP-M and BL did the statistical analyses and drafted the data Table. BL, EL-P, and MP-M interpreted statistical analyses. All the authors co-wrote the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by Reckitt Benckiser and supported by the Spanish Society of Family and Community Pharmacy (SEFAC). (Grant number: SEFAC 1.19). The funders were not involved in any aspect of the design of this study, management, analysis, and interpretation of data; writing of the report or decision to submit it for publication.
We would like to thank Reckitt Benckisser (RB) and the Spanish Society of Family and Community Pharmacy (SEFAC) for funding and supporting this study and for the trust placed in our research team to design and carry it out. To Havas Medea Madrid for facilitating this research. To Professor Roger Jones, author of the GIS questionnaire, for his kindness and facilities in using the GIS questionnaire in this study. To Jessica Gorlin for language editing.
EL-P is a member of the SEFAC Scientific Committee and has previously worked as an external consultant for RB. However, this has not influenced any aspect of this research or the work presented.
All the authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organizations that might have had an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
FD, functional dyspepsia; GERD, gastroesophageal reflux disease; GER, gastroesophageal reflux; GERD impact scale questionnaire (GIS questionnaire); OTC, over the counter medication.
Boardman, H. F., and Heeley, G. (2015). The role of the pharmacist in the selection and use of over-the-counter proton-pump inhibitors. Int. J. Clin. Pharm. 37 (5), 709–716. doi:10.1007/s11096-015-0150-z
BOE-A-2006-13554 (2006). BOE-A-2006-13554 Ley 29/2006, de 26 de julio, de garantías y uso racional de los medicamentos y productos sanitarios.
BOE-A-2015-8343 (2015). BOE-A-2015-8343 Real Decreto Legislativo 1/2015, de 24 de julio, por el que se aprueba el texto refundido de la Ley de garantías y uso racional de los medicamentos y productos sanitarios.
Choung, R. S., Locke, G. R., Schleck, C. D., Zinsmeister, A. R., and Talley, N. J. (2012). Overlap of dyspepsia and gastroesophageal reflux in the general population: One disease or distinct entities? Neurogastroenterol. Motil. Official J. Eur. Gastrointest. Motil. Soc. 24 (3), 229–234. doi:10.1111/j.1365-2982.2011.01845.x
de Bortoli, N., Tolone, S., Frazzoni, M., Martinucci, I., Sgherri, G., Albano, E., et al. (2018). Gastroesophageal reflux disease, functional dyspepsia and irritable bowel syndrome: Common overlapping gastrointestinal disorders. Ann. Gastroenterology 31 (6), 639–648. doi:10.20524/aog.2018.0314
Drossman, D. A., and Hasler, W. L. (2016). Rome IV—functional GI disorders: Disorders of gut-brain interaction. Gastroenterology 150 (6), 1257–1261. doi:10.1053/j.gastro.2016.03.035
Eusebi, L. H., Ratnakumaran, R., Bazzoli, F., and Ford, A. C. (2018a). Prevalence of dyspepsia in individuals with gastroesophageal reflux-type symptoms in the community: A systematic review and meta-analysis. Clin. Gastroenterology Hepatology Official Clin. Pract. J. Am. Gastroenterological Assoc. 16 (1), 39–48. doi:10.1016/j.cgh.2017.07.041
Eusebi, L. H., Ratnakumaran, R., Yuan, Y., Solaymani-Dodaran, M., Bazzoli, F., and Ford, A. C. (2018b). Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: A meta-analysis. Gut 67 (3), 430–440. doi:10.1136/gutjnl-2016-313589
Festi, D., Scaioli, E., Baldi, F., Vestito, A., Pasqui, F., Biase, A. R. D., et al. (2009). Body weight, lifestyle, dietary habits and gastroesophageal reflux disease. World J. Gastroenterology WJG 15 (14), 1690–1701. doi:10.3748/wjg.15.1690
Ford, A. C., Marwaha, A., Sood, R., and Moayyedi, P. (2015). Global prevalence of, and risk factors for, uninvestigated dyspepsia: A meta-analysis. Gut 64 (7), 1049–1057. doi:10.1136/gutjnl-2014-307843
Geeraerts, A., Van Houtte, B., Clevers, E., Geysen, H., Vanuytsel, T., Tack, J., et al. (2020). Gastroesophageal reflux disease—functional dyspepsia overlap: Do birds of a feather flock together? Official J. Am. Coll. Gastroenterology | ACG 115 (8), 1167–1182. doi:10.14309/ajg.0000000000000619
Gerson, L. B., and Fass, R. (2009). A systematic review of the definitions, prevalence, and response to treatment of nocturnal gastroesophageal reflux disease. Clin. Gastroenterology Hepatology Official Clin. Pract. J. Am. Gastroenterological Assoc. 7 (4), 372–378. quiz 367. doi:10.1016/j.cgh.2008.11.021
Ghoshal, U. C., Singh, R., Chang, F.-Y., Hou, X., Wong, B. C. Y., Kachintorn, U., et al. (2011). Epidemiology of uninvestigated and functional dyspepsia in asia: Facts and fiction. Neurogastroenterol. Motil. 17 (3), 235–244. doi:10.5056/jnm.2011.17.3.235
Guillemot, F., Ducrotté, P., and Bueno, L. (2005). Prevalence of functional gastrointestinal disorders in a population of subjects consulting for gastroesophageal reflux disease in general practice. Gastroenterologie Clinique Biol. 29 (3), 243–246. doi:10.1016/s0399-8320(05)80756-0
Haag, S., Andrews, J. M., Katelaris, P. H., Gapasin, J., Galmiche, J. P., Hunt, R., et al. (2009). Management of reflux symptoms with over-the-counter proton pump inhibitors: Issues and proposed guidelines. Digestion 80 (4), 226–234. doi:10.1159/000235953
Heidarzadeh-Esfahani, N., Soleimani, D., Hajiahmadi, S., Moradi, S., Heidarzadeh, N., and Nachvak, S. M. (2021). Dietary intake in relation to the risk of reflux disease: A systematic review. Prev. Nutr. Food Sci. 26 (4), 367–379. doi:10.3746/pnf.2021.26.4.367
Holtmann, G., Bigard, M.-A., Malfertheiner, P., and Pounder, R. (2011). Guidance on the use of over-the-counter proton pump inhibitors for the treatment of GERD. Int. J. Clin. Pharm. 33 (3), 493–500. doi:10.1007/s11096-011-9489-y
Johnson, D. A., Katz, P. O., Armstrong, D., Cohen, H., Delaney, B. C., Howden, C. W., et al. (2017). The safety of appropriate use of over-the-counter proton pump inhibitors: An evidence-based review and Delphi consensus. Drugs 77 (5), 547–561. doi:10.1007/s40265-017-0712-6
Kaji, M., Fujiwara, Y., Shiba, M., Kohata, Y., Yamagami, H., Tanigawa, T., et al. (2010). Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J. Gastroenterology Hepatology 25 (6), 1151–1156. doi:10.1111/j.1440-1746.2010.06249.x
Kaltenbach, T., Crockett, S., and Gerson, L. B. (2006). Are lifestyle measures effective in patients with gastroesophageal reflux disease?: An evidence-based approach. Archives Intern. Med. 166 (9), 965–971. doi:10.1001/archinte.166.9.965
Lee, S.-W., Lee, T.-Y., Lien, H.-C., Yeh, H.-Z., Chang, C.-S., and Ko, C.-W. (2014). The risk factors and quality of life in patients with overlapping functional dyspepsia or peptic ulcer disease with gastroesophageal reflux disease. Gut Liver 8 (2), 160–164. doi:10.5009/gnl.2014.8.2.160
Leiman, D. A., Riff, B. P., Morgan, S., Metz, D. C., Falk, G. W., French, B., et al. (2017). Alginate therapy is effective treatment for gastroesophageal reflux disease symptoms: A systematic review and meta-analysis. Dis. Esophagus Official J. Int. Soc. Dis. Esophagus 30 (2), 1–8. doi:10.1111/dote.12535
Locke, G. R., Talley, N. J., Fett, S. L., Zinsmeister, A. R., and Melton, L. J. (1997). Prevalence and clinical spectrum of gastroesophageal reflux: A population-based study in olmsted county, Minnesota. Gastroenterology 112 (5), 1448–1456. doi:10.1016/s0016-5085(97)70025-8
López-Pintor, E., Puig-Moltó, M., and Lumbreras, B. (2022). EsReflux protocol: Epidemiological study of heartburn and reflux-like symptoms in Spanish community pharmacies. Int. J. Environ. Res. Public Health 19 (16), 9807. doi:10.3390/ijerph19169807
Matsuhashi, N., Kudo, M., Yoshida, N., Murakami, K., Kato, M., Sanuki, T., et al. (2015). Factors affecting response to proton pump inhibitor therapy in patients with gastroesophageal reflux disease: A multicenter prospective observational study. J. Gastroenterology 50 (12), 1173–1183. doi:10.1007/s00535-015-1073-0
Müller, M., Labenz, G., Borkenstein, D.-P., Labenz, J., and Studiengruppe, L. (2019). Alginate on demand as add-on for patients with gastro-oesophageal reflux disease and insufficient PPI effect. Dtsch. Med. Wochenschr. 144 (4), e30–e35. doi:10.1055/a-0736-5959
Nuevo, J., Tafalla, M., and Zapardiel, J. (2009). Validation of the reflux disease questionnaire (RDQ) and gastrointestinal impact scale (GIS) in patients with gastroesophageal reflux disease in the Spanish population. Gastroenterol. Y Hepatol. 32 (4), 264–273. doi:10.1016/j.gastrohep.2008.12.004
Number of pharmacies in Spain 2007-2021 (2022). Statista. Available at: https://es.statista.com/estadisticas/629239/numero-de-farmacias-en-espana/(Accessed December 13, 2022).
Pauwels, A., Altan, E., and Tack, J. (2014). The gastric accommodation response to meal intake determines the occurrence of transient lower esophageal sphincter relaxations and reflux events in patients with gastro-esophageal reflux disease. Neurogastroenterol. Motil. 26 (4), 581–588. doi:10.1111/nmo.12305
Piessevaux, H., De Winter, B., Louis, E., Muls, V., De Looze, D., Pelckmans, P., et al. (2009). Dyspeptic symptoms in the general population: A factor and cluster analysis of symptom groupings. Neurogastroenterol. Motil. Official J. Eur. Gastrointest. Motil. Soc. 21 (4), 378–388. doi:10.1111/j.1365-2982.2009.01262.x
Pinto-Sanchez, M. I., Yuan, Y., Hassan, A., Bercik, P., and Moayyedi, P. (2017). Proton pump inhibitors for functional dyspepsia. Cochrane Database Syst. Rev. 11, CD011194. doi:10.1002/14651858.CD011194.pub3
Ponce, J., Vegazo, O., Beltrán, B., Jiménez, J., Zapardiel, J., Calle, D., et al. (2006). Prevalence of gastro-oesophageal reflux disease in Spain and associated factors. Alimentary Pharmacol. Ther. 23 (1), 175–184. doi:10.1111/j.1365-2036.2006.02733.x
Quigley, E. M. M., and Lacy, B. E. (2013). Overlap of functional dyspepsia and GERD—Diagnostic and treatment implications. Nat. Rev. Gastroenterology Hepatology 10 (3), 175–186. doi:10.1038/nrgastro.2012.253
Ronkainen, J., Aro, P., Storskrubb, T., Lind, T., Bolling-Sternevald, E., Junghard, O., et al. (2006). Gastro-oesophageal reflux symptoms and health-related quality of life in the adult general population--the Kalixanda study. Alimentary Pharmacol. Ther. 23 (12), 1725–1733. doi:10.1111/j.1365-2036.2006.02952.x
Ronkainen, J., Aro, P., Walker, M. M., Agréus, L., Johansson, S.-E., Jones, M., et al. (2019). Duodenal eosinophilia is associated with functional dyspepsia and new onset gastro-oesophageal reflux disease. Alimentary Pharmacol. Ther. 50 (1), 24–32. doi:10.1111/apt.15308
Schey, R., Dickman, R., Parthasarathy, S., Quan, S. F., Wendel, C., Merchant, J., et al. (2007). Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease. Gastroenterology 133 (6), 1787–1795. doi:10.1053/j.gastro.2007.09.039
Semergen (2019). Update on the management of patients with heartburn and/or reflux in primary care and community pharmacy pharmacy [Spanish]. 1a Edición. Medea, Medical Education Agency S.L. ISBN: 978-84-09-13267-6. Available at: https://semergen.es/files/docs/grupos/digestivo/guia_practica_reflujo.pdf (Accessed April 26, 2023).
Tack, J., Caenepeel, P., Arts, J., Lee, K. J., Sifrim, D., and Janssens, J. (2005). Prevalence of acid reflux in functional dyspepsia and its association with symptom profile. Gut 54 (10), 1370–1376. doi:10.1136/gut.2004.053355
Tack, J., Talley, N. J., Camilleri, M., Holtmann, G., Hu, P., Malagelada, J.-R., et al. (2006). Functional gastroduodenal disorders. Gastroenterology 130 (5), 1466–1479. doi:10.1053/j.gastro.2005.11.059
Tytgat, G. N., McColl, K., Tack, J., Holtmann, G., Hunt, R. H., Malfertheiner, P., et al. (2008). New algorithm for the treatment of gastro-oesophageal reflux disease. Alimentary Pharmacol. Ther. 27 (3), 249–256. doi:10.1111/j.1365-2036.2007.03565.x
Keywords: community pharmacy, gastroesophageal reflux, functional dyspepsia, epigastric symptoms, retrosternal symptoms
Citation: Puig-Moltó M, Lumbreras B and López-Pintor E (2023) Prevalence and risk factors of upper gastrointestinal symptoms in community pharmacies in Spain: a cross-sectional study. Front. Pharmacol. 14:1162370. doi: 10.3389/fphar.2023.1162370
Received: 06 March 2023; Accepted: 02 June 2023;
Published: 13 June 2023.
Edited by:
Li Li, The University of Queensland, AustraliaReviewed by:
Rajan Singh, University of Nevada, United StatesCopyright © 2023 Puig-Moltó, Lumbreras and López-Pintor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Blanca Lumbreras, Ymx1bWJyZXJhc0B1bWguZXM=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.