- 1Institute for Medical Information Processing, Biometry, and Epidemiology, Faculty of Medicine, Ludwig Maximilian University of Munich, Munich, Germany
- 2Pettenkofer School of Public Health, Munich, Germany
- 3Munich Center of Health Sciences, Ludwig Maximilian University of Munich, Munich, Germany
- 4German Center for Vertigo and Balance Disorders, University Hospital Munich, Munich, Germany
- 5Institute of General Practice and Family Medicine, University Hospital Munich, Munich, Germany
- 6Department of General Practice/Medical Clinic III, Faculty of Medicine, University Hospital Carl Gustav Carus, Dresden, Germany
Introduction: Anticholinergic and sedative medication is prescribed for various conditions in older patients. While the general association between anticholinergic and sedative medication and impaired functioning is well established, its specific role in older individuals with vertigo, dizziness, and balance disorders (VDB) is still incompletely understood. The objective of this study was to investigate, whether an exposure to anticholinergic and sedative medication is associated with lower generic and lower vertigo-specific functioning in older patients with VDB.
Methods: Data originates from the longitudinal multicenter study MobilE-TRA with two follow-ups, conducted from 2017 to 2019 in two German federal states. Exposure to anticholinergic and sedative medication was quantified using the drug burden index (DBI). Generic functioning was assessed by the Health Assessment Questionnaire Disability Index, appraising the amount of difficulties in performing activities of daily living (ADL). Vertigo-specific functioning was measured using the Vestibular Activities and Participation (VAP) questionnaire, assessing patient-reported functioning regarding activities of daily living that are difficult to perform because of their propensity to provoke VDB (Scale 1) as well as immediate consequences of VDB on activities and participation related to mobility (Scale 2). Longitudinal linear mixed models were applied to assess the association of exposure to anticholinergic and sedative medication at baseline and the level of generic and vertigo-specific functioning status over time.
Results: An overall of 19 (7 from Bavaria) primary care physicians (mean age = 54 years, 29% female) recruited 158 (59% from Bavaria) patients with VDB (median age = 78 years, 70% female). Anticholinergic and sedative medication at baseline was present in 56 (35%) patients. An exposure to anticholinergic and sedative medication at baseline was significantly associated with lower generic functioning [Beta = 0.40, 95%-CI (0.18; 0.61)] and lower vertigo-specific functioning [VAP Scale 1: Beta = 2.47, 95%-CI (0.92; 4.02)], and VAP Scale 2: Beta = 3.74, 95%-CI [2.23; 5.24]).
Conclusion: Our results highlight the importance of a close monitoring of anticholinergic and sedative medication use in older patients with VDB. When feasible, anticholinergic and sedative medication should be replaced by equivalent alternative therapies in order to potentially reduce the burden of VDB.
1 Introduction
Vertigo, dizziness, and balance disorders (VDB) affect approximately 30% of the population beyond 60 years of age (Jönsson et al., 2004; Barin and Dodson, 2011), and up to 50% of those over 85 (Jönsson et al., 2004). A considerable percentage of older adults beyond 65 years with VDB experience severe impairment in their everyday life (van Vugt et al., 2020).
The reasons for VDB are often multifactorial. Distinct treatable vestibular disease entities, cardiovascular diseases or metabolic disorders may align with symptoms of the ageing of vestibular, proprioceptive or somatosensory systems.
In addition, VDB may be an unintended side effect of standard medication (Holt et al., 2010; Hedna et al., 2015; Muncie Jr et al., 2017). This is one of the reasons why a continuous medication review is recommended for older adults (Beuscart et al., 2021; Leitliniengruppe Hessen Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin, 2021). Medication that is causing VDB should be replaced by equivalent but better tolerated alternatives, whenever this is possible.
Of particular interest in this context is medication with anticholinergic and sedative (AS) effects. AS medication is prescribed for a multitude of indications, including urinary incontinence, sleep disturbances, mental illness, pain, cardiovascular diseases, and gastrointestinal disorders (Kouladjian et al., 2014). Certain anticholinergic medication (e.g., Scopolamine or Dimenhydrinate) and selected sedatives (e.g., Diazepam or Lorazepam) might also be prescribed as vestibular suppressants, i.e., drugs that reduce the subjective symptoms and intensity of vertigo as well as the nystagmus evoked by vestibular imbalance, in symptomatic therapy of VDB (Casani et al., 2021).
Previous research has shown that use of AS medication was higher in people with VDB than in the general population, especially in the old aged (Phillips et al., 2018; Phillips et al., 2019). This is of particular concern, since AS medication can lead to adverse effects such as confusion, blurred vision, delirium, and dizziness (Bell et al., 2012; Swain, 2020). Due to these adverse effects, a number of medication with AS properties such as selected antihistamines, urological spasmolytic agents, and benzodiazepines have been assessed as being potentially inappropriate for the general older population in Germany (Holt et al., 2010). The drug burden index (Hilmer et al., 2007) quantifies the combination of AS active substances with their respective dosage in a specific individual. Specifically in older adults, cognitive and physical impairment may be the consequence of a high AS drug burden (Landi et al., 2007; Cao et al., 2008; Hilmer et al., 2009; Koyama et al., 2014; Wouters et al., 2017; Byrne et al., 2019).
While the general association of AS medication and impaired functioning is well established, its specific role in individuals who are already affected by chronic or acute VDB is still incompletely understood.
It seems reasonable to hypothesize that use of AS medication considerably contributes to impaired functioning in two ways: First, it causes difficulties in performing activities of daily living (generic-functioning), such as hygiene, eating, grip, walking, and common daily activities. Furthermore, the use of AS medication could intensify the disease and therewith its direct impairment on the everyday life, especially on daily activities and social participation (vertigo-specific functioning).
The objective of this study thus was to investigate the impact of AS medication on both generic and vertigo-specific functioning in older adults with VDB.
2 Materials and methods
2.1 Study design, study population, and data collection procedures
Data for this research project was collected in the longitudinal multicenter study MobilE-TRA conducted in two German federal states (Bavaria and Saxony) from September 2017 until October 2019. A more detailed description of the study is given elsewhere (Kisch et al., 2018).
In short, patients aged 65 years and older were included if they had consulted their primary care physician (PCP) for an episode of VDB in the last quarter. The identification of suitable individuals was accomplished by approaching PCPs who were willing to participate and asking them to search their patient databases for the following ICD-10 codes associated with VDB: R42, A88.1, E53.8, F45.8, G11.8, G43.1, G45.0, G62, G63, H55, H83.0-2, I95.1, and N95.1. A detailed description of the diagnoses related to the ICD-10 codes is provided in the Supplementary Table S1. Additional inclusion criteria were a statutory health insurance, covering approximately 90% of the German population (The Federal Ministry of Health, 2020), as well as sufficient command of the German language.
Data collection consisted of three waves. The baseline assessment in between September 2017 and August 2018 comprised paper-based self-administered health questionnaires for both the patients and the PCPs. For the two follow-ups 6 months and 12 months after individual baseline dates, a cover letter with instructions and the paper-based self-administered health questionnaire were sent via postal mail to the patients’ home addresses. If no questionnaire was sent back within a month after the original follow-up invitation, a reminder was sent. In case of questions about the questionnaire, participants were able to contact the study team via e-mail or phone. There was no loss to follow-up between the study waves.
Ethics approval for MobiLE-TRA was obtained from the Ethics Committee of the Ludwig Maximilian University of Munich in Bavaria (#17-443) and the Ethics Committee of the Technical University Dresden in Saxony (#E365092017). Written informed consent was obtained from all participants. The study was performed in accordance with the Declaration of Helsinki principles.
2.2 Exposure to anticholinergic and sedative medication
Information on medication intake was obtained by the participants self-report during baseline assessment. Active pharmaceutical ingredients, the associated national identification number, and the prescribed daily dose for each medication taken within the last 7 days were recorded. The respective codes of the Anatomical Therapeutic Chemical Classification System (ATC-Codes) were matched to the national identification number.
AS medication was identified based on previous studies (Phillips et al., 2018; Phillips et al., 2019) using applicable published AS medication lists (Hilmer et al., 2007; Durán et al., 2013; Ailabouni et al., 2017; Wouters et al., 2017; Byrne et al., 2018; O'Connell et al., 2018) and potentially inappropriate AS medication from the German PRISCUS List (Holt et al., 2010), a collection of potentially inappropriate medication for older people. A detailed list of all AS medication and the related ATC-Codes present in this study sample is shown in Supplementary Table S2.
Since some AS medication might also be prescribed as vestibular suppressants in symptomatic therapy of VDB, we checked the information on prescribed drugs specifically for treatment of VDB, which was provided by the PCPs for each patient, in order to mitigate confounding by indication. No prescribed AS medication for treatment of VDB was detected.
To quantify the extent of the drug burden by AS medication at baseline, we calculated the drug burden index (DBI) (Hilmer et al., 2007). A DBI greater than zero represents a present AS drug burden with a higher index indicating higher AS burden.
The DBI of each participant was calculated using the following formula, where D denotes the prescribed daily dose of any AS medication for this participant, whereas δ is the defined daily dose (DDD) for this AS medication according to the Federal Institute for Drugs and Medical Devices (GKV-Arzneimittelindex im Wissenschaftlichen Institut der AOK, 2022):
In order to ensure an adequate calculation of the DBI, we excluded all pro re nata medication as well as medication that was applied topically, ophthalmologically or by inhalation, since these dosing forms of medication have not been clearly defined (Kouladjian et al., 2014). Medication that was classified as having both anticholinergic and sedative effects was included only once in the calculation of the DBI (Hilmer et al., 2007; Best et al., 2013).
To handle the observed zero-inflation in the DBI of the study sample, exposure to AS medication at baseline was categorized following published cut-off points (Hilmer et al., 2007) into: No exposure (DBI = 0), low exposure (0 < DBI <1), and high exposure (DBI ≥1). Due to low observation numbers in the high exposure group, the DBI further was dichotomized into present (DBI greater than zero) and absent (DBI equals zero).
2.3 Generic and vertigo-specific functioning
Generic patient-reported functioning was assessed at baseline and both follow-ups by the German version of the Health Assessment Questionnaire Disability Index (HAQ-DI) (Fries et al., 1982; Brühlmann et al., 1994) in which patients reported the amount of difficulty they have in performing activities of daily living and instrumental activities of daily living (ADL and IADL). The overall HAQ-DI index was obtained by using the highest score within each of the eight domains (dressing and grooming, hygiene, arising, reach, eating, grip, walking, and common daily activities) and averaging these values into an overall HAQ-DI value (range = 0–3). Higher values in this overall index indicated stronger difficulties.
Vertigo-specific functioning was assessed at baseline and both follow-ups by the Vestibular Activities and Participation questionnaire (VAP) (Mueller et al., 2015). The VAP measures functioning in two dimensions by using two separate scales consisting of six items each. VAP Scale one measures patient-reported functioning regarding activities that are difficult to perform because of their propensity to provoke VDB (activity VAP). VAP Scale two indicates immediate consequences of VDB on activities and participation related to mobility (mobility VAP). Interval scaled overall scores (range scale 1 = 0–23; range scale 2 = 0–20) were used with higher scores indicating lower functioning.
2.4 Additional covariates
VDB diagnosis for each patient was reported by the respective PCP during baseline assessment as part of the self-administered health questionnaires given to the PCPs. Previous research has shown that unspecific diagnoses of VDB are remarkably over-diagnosed in primary care, resulting in a lack of adequate treatment for the actual underlying cause of VDB in the patients affected (Geser and Straumann, 2012). This lack of adequate treatment might manifest itself in reduced functioning. To account for this possibility and to facilitate analysis, we categorized the diagnoses with a specific cause (e.g., vestibular vertigo, central vertigo, cardiovascular problems, and psychogenic dizziness) as ‘specific’ VDB, whereas all other cases where no diagnostic decision was stated in the questionnaire were summarized as ‘unspecific’ VDB. The diagnosis was labeled as ‘not specified’ if the PCP did not specify any diagnosis in the questionnaire but enrolled the patient in the VDB survey.
Multimorbidity was included into the analysis since it increases the probability for medication and thereby the risk of unwanted effects in older people (Vrdoljak and Borovac, 2015) and is associated with reduced functioning (Loza et al., 2009). Multimorbidity was present, if a patient suffered from at least two chronic conditions additionally to VDB during baseline assessment. The assessment of chronic conditions in Mobile-TRA was accomplished by asking the PCP for existing comorbidities during baseline assessment and was based on the self-report-generated Charlson Comorbidity Index (Chaudhry et al., 2005), excluding HIV. Following (Kirchberger et al., 2012), further comorbidities that had shown to be of high relevance when examining multimorbidity with increasing age (Hunger et al., 2011) were added. Our approach results in an overall of 12 chronic conditions (Supplementary Material S1).
Information on gender (male/female) and age was based on patients’ self-report. Federal states were included as a binary variable (Bavaria/Saxony).
2.5 Statistical analysis
Unadjusted summary statistics were calculated for the overall sample and separately for patients with and patients without exposure to AS medication to compare differences at baseline regarding diagnoses and characteristics of the patients as well as generic and vertigo-specific functioning. Median values and the interquartile range (IQR) between the 25% and 75% - quartiles were reported for continuous variables, relative and absolute frequencies were reported for categorical variables. Group comparison between patients with and patients without exposure to AS medication was based on Kruskal-Wallis-Test for continuous variables and Fisher’s exact test for categorical variables.
We applied longitudinal linear mixed models with random intercepts and fixed slopes to assess the association of exposure to AS medication at baseline, represented by the dichotomized DBI, and the level of generic (HAQ-DI) and vertigo-specific (VAP) functioning status over time. To analyze the effect of baseline exposure on the change in functioning over time, we introduced an interaction term between AS exposure status at baseline and time. Multicollinearity among predictor variables was tested by calculating the variance inflation factor (VIF) for each model, with a highest tolerated VIF lower than five points.
In order to investigate the effect of the level of the AS drug burden, we additionally performed sensitivity analyses, computing the same longitudinal linear mixed models based on the categorized DBI values.
Random effects for the intercepts were reported. Intraclass correlation coefficients (ICC) were introduced for each model to examine the proportion of the overall variation in the respective functioning scale which is explained by the AS medication exposure status at baseline. To facilitate the interpretation of intercept estimates, we subtracted the minimum age of 65 as set by the inclusion criteria from the age in years for every patient in all mixed models.
All computational analyses were carried out with R version 4.1.0 (RStudio Team, 2020) using the nlme and misty libraries (Pinheiro et al., 2007; Yanagida and Yanagida, 2022). Significance level was set to 5% for all tests conducted.
3 Results
3.1 Study population
An overall of 19 PCPs (7 from Bavaria, 12 from Saxony; mean age = 54 years; 29% female) recruited 158 patients with VDB (59% from Bavaria; mean age = 77 years; 70% female). Exposure to AS medication at baseline was present in 56 (35%) patients. Of these, 49 (31%) patients had a low AS exposure status (0 < DBI<1), whereas 7 (4%) patients had a high AS exposure status (DBI ≥1). A total of 42% of the patients had a specific VDB diagnosis, 40% of the patients had an unspecific VDB diagnosis, and the VDB diagnosis was not specified in 18% of the patients. Median HAQ-DI at baseline was 0.38, median activities VAP was 7.36, and mean mobility VAP was 6.42. Patients exposed to AS medication reported significantly higher values for the HAQ-DI and both scales of the VAP scales during baseline assessment. Further details are presented in Table 1.
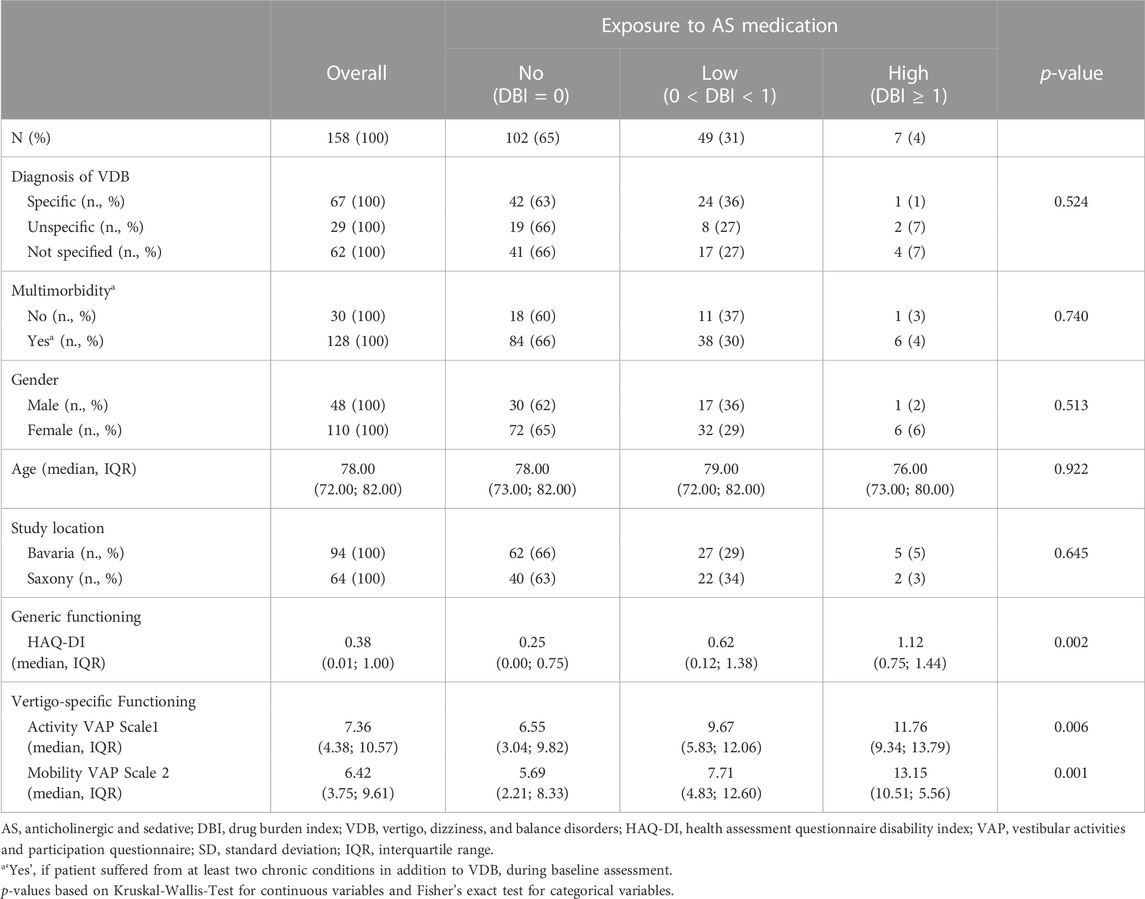
TABLE 1. Unadjusted summary statistics by exposure to AS medication at baseline assessment (n = 158). Median values and interquartile range for continuous variables and absolute and relative frequencies for categorical variables are reported.
3.2 Impact of AS medication on generic and vertigo-specific functioning
Table 2 shows the adjusted estimates for the association of exposure to AS medication at baseline and generic and vertigo-specific functioning. Adjusted for covariates, generic functioning was significantly lower for patients that were exposed to AS medication at baseline [Beta = 0.40, 95%-CI (0.18; 0.61)]. Exposure to AS medication at baseline accounted for nine percent of the total variance observed in the generic functioning (ICC_HAQ-DI = 0.09). Exposure to AS medication at baseline also was significantly associated with higher values on the activity VAP Scale 1 [Beta = 2.47, 95%-CI (0.92; 4.02)] and mobility VAP Scale 2 [Beta = 3.74, 95%-CI (2.23; 5.24)], indicating lower vertigo-specific functioning. Exposure to AS medication at baseline accounted for twelve percent of the total variance observed in the activity VAP Scale 1 (ICC_VAP1 = 0.12) and 17 percent of the total variance observed in the mobility VAP Scale 2 (ICC_VAP2 = 0.17). Impairment in vertigo-specific activity-related functioning (activity VAP Scale 1) declined over time for the overall sample [Beta = −0.47, 95%-CI (-0.91; −0.03)]. No significant differences in the development of functioning over time between patients that were exposed to AS medication at baseline and patients that were not exposed were detected.
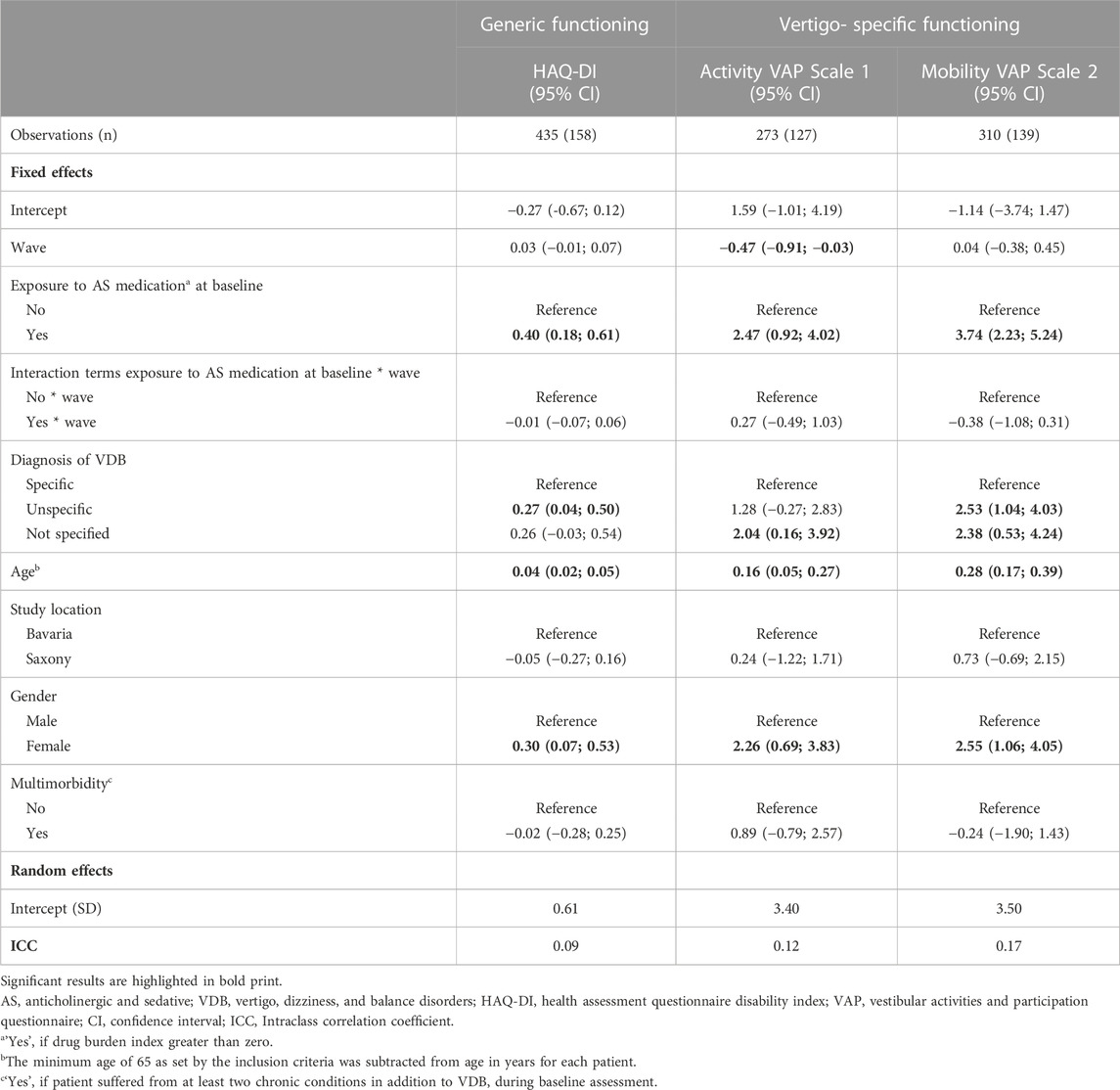
TABLE 2. Longitudinal linear mixed models to assess the influence of exposure to AS medication on generic functioning (HAQ-DI) and vertigo-specific functioning (Activity VAP Scale one and Mobility VAP Scale 2).
Patients with an unspecific diagnosis had lower generic functioning [Beta = 0.27, 95%-CI (0.04; 0.50)] and lower vertigo-specific mobility [Beta = 2.53, 95%-CI (1.04; 4.03)]. Patients in which the VDB diagnosis remained unspecified reported significantly worse vertigo-specific functioning on both VAP scales. Older participants and women were significantly more disabled.
The performed sensitivity analyses based on the categorized DBI showed, that patients with a low exposure to AS medication (0 < DBI<1) showed lower generic functioning and lower vertigo-specific functioning, when compared to patients without any AS exposure (DBI = 0). Patients with a high exposure to AS medication (DBI ≥1) had even lower vertigo-specific functioning on the VAP Scale 1 [Beta = 3.45, 95%-CI (0.15; 6.75)] and mobility VAP Scale 2 [Beta = 5.63, 95%-CI (1.93; 9.32)]. Further details are presented in Supplementary Table S3.
4 Discussion
Using data from a German primary care-based longitudinal multicenter study, we have shown that an exposure to AS medication was associated with lower values in both generic and vertigo-specific functioning in older patients with VDB. Patients in which the underlying mechanism of VDB remained unspecified were particularly at risk of impaired functioning.
In our study, patients that were exposed to AS medication at baseline had lower generic functioning than patients who were not exposed to AS medication. This is in line with previous findings stating that use of AS medication is associated with functional impairments (Landi et al., 2007; Cao et al., 2008; Hilmer et al., 2009; Koyama et al., 2014; Wouters et al., 2017; Byrne et al., 2019), due to its adverse effects (Holt et al., 2010; Bell et al., 2012) that are increasing the amount of difficulty that patients have in performing activities of their daily living.
The most striking observation of our study is that lower vertigo-specific functioning also was associated with exposure to AS medication. Apart from increasing difficulties in performing general tasks of daily living, the use of AS medication also intensifies the direct major impairment on the everyday life, especially on daily activities, social participation, and mobility. To our knowledge, no study has yet explicitly investigated this before. These results are highly alerting since it has been noted that use of AS medication was higher in people with VDB than in the general population, especially in the old aged (Phillips et al., 2018; Phillips et al., 2019).
Regardless of their exposure to AS medication, patients diagnosed with unspecific VDB, i.e., cases in which the cause of VDB remained unspecified by the respective PCP, and patients in which the entire diagnosis of VDB remained unspecified by their PCP, had lower functioning than patients with a specific diagnosis. It has been mentioned that VDB, especially in older patients, can have multiple causes (Maarsingh et al., 2010; Fernández et al., 2015) and that the symptoms often are ambiguous. It therefore is of little surprise that unspecific VDB is frequently over-diagnosed in primary care by as much as up to 60%, when compare to diagnostic procedures at specialized care centers, possibly resulting in inadequate treatment (Geser and Straumann, 2012). This inadequate treatment might ultimately manifest itself in worse functioning.
Our findings demonstrate that women are at risk of lower generic and vertigo-specific functioning. This is in line with recent findings that women at the age of 65 and above in Germany expect to spend less of their remaining life years in good health than men, due to their higher morbidity and despite their higher life expectancy (Stephan et al., 2021). It further has been shown that the overall potentially inappropriate medication use was higher in older women (Nothelle et al., 2017; Nothelle et al., 2019), possibly contributing to the lower functioning found in this study.
Several limitations of our study have to be considered. Information on medication intake was based on self-report. Chances are that patients did not indicate a comprehensive list or that the indicated doses taken was inaccurate. The true extent of the exposure to AS medication thus might have been underestimated. Likewise, the assessment of generic functioning via the HAQ-DI and vertigo-specific functioning via the VAP was based on the participants’ self-report and thus might have potentially exposed to a variety of information bias. Though we cannot fully exclude the chance that such bias might be present in our data, self-reported measure is commonly seen as a valid outcome, assessing the patients’ perspective. Both the HAQ-DI and the VAP are standardized and validated instruments which have frequently used in the past. Patients further were offered contact information of the study team in case of any uncertainty regarding their study participation or the questionnaire in order to reduce the risk of bias. The DBI within this study was calculated using the DDD instead of the minimum effective dose as specified in the original calculation of the DBI (Hilmer et al., 2007) since the German ATC classification system was closely linked to the DDD. Using the DDD as a replacement of the minimum effective dose has been introduced in the past (Faure et al., 2013). This however might have resulted in an underestimation of the actual DBI, since the DBI is higher for some drugs, but not for others (Hilmer, 2018). Suitable subjects for this study were identified by searching for ICD-10 codes associated with VDB in the databases of the participating PCPs. The reliability of ICD-10 codes as a reliable classification system in primary care has been discussed in the past (Wockenfuss et al., 2009), especially since they became one of the corner stones of reimbursement in the German healthcare system and thus might be divergent from the actual diagnosis. While the diagnosis of VDB use in this analysis was given directly by the PCP as part of the questionnaire and therefore decoupled from the ICD codes, some potential participants might have been left out due to inaccurate ICD-10 codes that were not listed in our inclusion criteria. The VDB diagnoses used in this analysis were solely based on the assessments of the participating PCPs at baseline. This is of relevance, since previous research has shown that PCPs tend to frequently over-diagnose unspecific VDB in patients who later were diagnosed with a specific cause of VDB (Geser and Straumann, 2012) due to reported difficulties in establishing an accurate VDB diagnosis in the past (Stephan et al., 2018). Also, we do not know if (and when) the PCP or specialist made a specific diagnosis during the follow-up time. While the list of assessed comorbidities within this study was comprehensive, it did not include all comorbidities that are associated with the use of AS medication, such as sleep and pain disorders, urinary incontinence, mental disorders, and dementia (Kouladjian et al., 2014). Single comorbidities might also differ with regard to their relation with VDB, the prescription frequency of AS medication, and their direct impact on generic and vertigo-specific functioning. Using multimorbidity as a substitute, the estimation of the impact of AS medication on functioning might be distorted due to unaccounted confounders. We therefore strongly suggest to further review our findings, including a more detailed assessment of the present medication intake and existing comorbidities.
In conclusion, we found that an exposure to AS medication was associated with lower values in both generic and vertigo-specific functioning in older patients with VDB. When feasible, AS medication thus should be replaced by equivalent alternative therapies that are adapted to the situation and needs of each patient individually. Valid approaches have already been examined and include change of medication as well as non-pharmacological treatment, such as physical exercises or behavioral therapy (Holt et al., 2010). The use of AS medication in symptomatic therapy of VDB remains debated (Hunter et al., 2022). Our results support recent recommendations that their use as vestibular suppressants should be limited only to the acute phase of the disease and must be used with special caution in the older population (Casani et al., 2021).
A close monitoring of AS medication use in older patients with VDB symptoms is crucial and should be considered as an integral component in medication monitoring guidelines in a primary care setting, as, for example, happened in the German DEGAM-Guideline (S3) for polypharmacy (Leitliniengruppe Hessen Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM), 2021). Using the drug burden index could be a valid approach to do so and should be accompanied by implementation studies in order to ensure feasibility. In doing so, exposure to AS medication could be reduced and thus help to potentially reduce the burden of VDB.
Previous research aimed at evaluating the utility of the DBI in practice showed that, while using the DBI as an assessment tool in older adults can have the potential to reduce AS burden in some studies (Nishtala et al., 2009; Castelino et al., 2010), the effect could not always be shown (van der Meer et al., 2018) or was lower than anticipated (Gnjidic et al., 2010). Agreement is that future research needs to be implemented targeting multidisciplinary and multifactorial approaches, including the DBI, to evaluate drug prescription and to evaluate functional outcomes in older adults (Kouladjian et al., 2014).
Data availability statement
The datasets presented in this article are not readily available because of data privacy regulations that apply in the country of data collection. Requests to access the datasets should be directed to the corresponding author BK (YmVuZWRpY3Qua2F0emVuYmVyZ2VyQG1lZC51bmktbXVlbmNoZW4uZGU=).
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Ludwig Maximilian University of Munich in Bavaria (#17-443) and the Ethics Committee of the Technical University Dresden in Saxony (#E365092017). The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed to the study conception and execution. Material preparation and data collection were performed by RK, LS, and KV, DK, BK, RK, and EG are responsible for the study’s quality assessment. The data analysis was performed by BK, DK, and RS. The first draft of the manuscript was written by BK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study is part of the project “Munich Network Healthcare Research—MobilE-Net” and was funded by the German Federal Ministry of Education and Research (grant number 01GY1603A).
Acknowledgments
The MobilE-TRA cohort study was conducted under the consortium leadership of the Institute for Medical Information Processing, Biometry and Epidemiology at the Ludwig Maximilian University of Munich. The authors acknowledge the patients’ and general practitioners’ willingness to participate in the study and their valuable feedback in the pilot testing of the questionnaires. The authors thank Dr. Anna-Janina Stephan and Amanda Phillips for their valuable contribution during the data collection of MobilE-TRA.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1136757/full#supplementary-material
References
Ailabouni, N., Mangin, D., and Nishtala, P. S. (2017). Deprescribing anticholinergic and sedative medicines: Protocol for a feasibility trial (DEFEAT-polypharmacy) in residential aged care facilities. BMJ Open 7 (4), e013800. doi:10.1136/bmjopen-2016-013800
Barin, K., and Dodson, E. E. (2011). Dizziness in the elderly. Otolaryngol. Clin. North Am. 44 (2), 437. doi:10.1016/j.otc.2011.01.013
Bell, J., Mezrani, C., Blacker, N., LeBlanc, T., Frank, O., Alderman, C. P., et al. (2012). Anticholinergic and sedative medicines: Prescribing considerations for people with dementia. Aust. Fam. Physician 41 (1/2), 45–49.
Best, O., Gnjidic, D., Hilmer, S. N., Naganathan, V., and McLachlan, A. J. (2013). Investigating polypharmacy and drug burden index in hospitalised older people. Intern Med. J. 43 (8), 912–918. doi:10.1111/imj.12203
Beuscart, J.-B., Pelayo, S., Robert, L., Thevelin, S., Marien, S., and Dalleur, O. (2021). Medication review and reconciliation in older adults. Eur. Geriatr. Med. 12 (3), 499–507. doi:10.1007/s41999-021-00449-9
Brühlmann, P., Stucki, G., and Michel, B. A. (1994). Evaluation of a German version of the physical dimensions of the Health Assessment Questionnaire in patients with rheumatoid arthritis. J. Rheumatol. 21, 1245–1249.
Byrne, C. J., Walsh, C., Cahir, C., and Bennett, K. (2019). Impact of drug burden index on adverse health outcomes in Irish community-dwelling older people: A cohort study. BMC Geriatr. 19 (1), 121–210. doi:10.1186/s12877-019-1138-7
Byrne, C. J., Walsh, C., Cahir, C., Ryan, C., Williams, D. J., and Bennett, K. (2018). Anticholinergic and sedative drug burden in community-dwelling older people: A national database study. BMJ Open 8 (7), e022500. doi:10.1136/bmjopen-2018-022500
Cao, Y. J., Mager, D., Simonsick, E., Hilmer, S., Ling, S., Windham, B., et al. (2008). Physical and cognitive performance and burden of anticholinergics, sedatives, and ACE inhibitors in older women. Clin. Pharmacol. Ther. 83 (3), 422–429. doi:10.1038/sj.clpt.6100303
Casani, A. P., Gufoni, M., and Capobianco, S. (2021). Current insights into treating vertigo in older adults. Drugs Aging 38 (8), 655–670. doi:10.1007/s40266-021-00877-z
Castelino, R. L., Hilmer, S. N., Bajorek, B. V., Nishtala, P., and Chen, T. F. (2010). Drug burden index and potentially inappropriate medications in community-dwelling older people: The impact of home medicines review. Drug Aging 27, 135–148. doi:10.2165/11531560-000000000-00000
Chaudhry, S., Jin, L., and Meltzer, D. (2005). Use of a self-report-generated Charlson comorbidity index for predicting mortality. Med. Care 43, 607–615. doi:10.1097/01.mlr.0000163658.65008.ec
Durán, C. E., Azermai, M., and Vander Stichele, R. H. (2013). Systematic review of anticholinergic risk scales in older adults. Eur. J. Clin. Pharmacol. 69 (7), 1485–1496. doi:10.1007/s00228-013-1499-3
Faure, R., Dauphinot, V., Krolak-Salmon, P., and Mouchoux, C. (2013). A standard international version of the drug burden index for cross-national comparison of the functional burden of medications in older people. J. Am. Geogr. Soc. N. Y. 61 (7), 1227–1228. doi:10.1111/jgs.12343
Fernández, L., Breinbauer, H. A., and Delano, P. H. (2015). Vertigo and dizziness in the elderly. Front. Neurol. 6, 144. doi:10.3389/fneur.2015.00144
Fries, J. F., Spitz, P. W., and Young, D. (1982). The dimensions of health outcomes: The health assessment questionnaire, disability and pain scales. J. Rheumatol. 9 (5), 789–793.
Geser, R., and Straumann, D. (2012). Referral and final diagnoses of patients assessed in an academic vertigo center. Front. Neurol. 3, 169. doi:10.3389/fneur.2012.00169
GKV-Arzneimittelindex im Wissenschaftlichen Institut der AOK (WIdO) (2022). Amtliche Fassung des ATC-Index mit DDD-Angaben für Deutschland im Jahre 2022. Berlin/ Bonn: Bundesinstitut für Arzneimittel und Medizinprodukte BfArM.
Gnjidic, D., Couteur, D. G. L., Abernethy, D. R., and Hilmer, S. N. (2010). A pilot randomized clinical trial utilizing the drug burden index to reduce exposure to anticholinergic and sedative medications in older people. Ann. Pharamacother 44 (11), 1725–1732. doi:10.1345/aph.1P310
Hedna, K., Hakkarainen, K. M., Gyllensten, H., Jönsson, A. K., Petzold, M., and Hägg, S. (2015). Potentially inappropriate prescribing and adverse drug reactions in the elderly: A population-based study. Eur. J. Clin. Pharmacol. 71 (12), 1525–1533. doi:10.1007/s00228-015-1950-8
Hilmer, S. N. (2018). Calculating and using the drug burden index score in research and practice. Expert Rev. Clin. Phar 11 (11), 1053–1055. doi:10.1080/17512433.2018.1528145
Hilmer, S. N., Mager, D. E., Simonsick, E. M., Cao, Y., Ling, S. M., Windham, B. G., et al. (2007). A drug burden index to define the functional burden of medications in older people. Arch. Intern Med. 167 (8), 781–787. doi:10.1001/archinte.167.8.781
Hilmer, S. N., Mager, D. E., Simonsick, E. M., Ling, S. M., Windham, B. G., Harris, T. B., et al. (2009). Drug burden index score and functional decline in older people. Am. J. Med. 122 (12), 1142–1149.e1-2. doi:10.1016/j.amjmed.2009.02.021
Holt, S., Schmiedl, S., and Thürmann, P. A. (2010). Potentially inappropriate medications in the elderly: The PRISCUS list. Dtsch. Arztebl Int. 107 (31-32), 543–551. doi:10.3238/arztebl.2010.0543
Hunger, M., Thorand, B., Schunk, M., Döring, A., Menn, P., Peters, A., et al. (2011). Multimorbidity and health-related quality of life in the older population: Results from the German KORA-age study. Health Qual. Life Out. 9 (1), 53. doi:10.1186/1477-7525-9-53
Hunter, B. R., Wang, A. Z., Bucca, A. W., Musey, P. I., Strachan, C. C., Roumpf, S. K., et al. (2022). Efficacy of benzodiazepines or antihistamines for patients with acute vertigo: A systematic review and meta-analysis. JAMA Neurol. 79, 846–855. doi:10.1001/jamaneurol.2022.1858
Jönsson, R., Sixt, E., Landahl, S., and Rosenhall, U. (2004). Prevalence of dizziness and vertigo in an urban elderly population. J. Vestib. Res. 14 (1), 47–52. doi:10.3233/ves-2004-14105
Kirchberger, I., Meisinger, C., Heier, M., Zimmermann, A.-K., Thorand, B., Autenrieth, C. S., et al. (2012). Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PloS One 7 (1), e30556. doi:10.1371/journal.pone.0030556
Kisch, R., Bergmann, A., Koller, D., Leidl, R., Mansmann, U., Mueller, M., et al. (2018). Patient trajectories and their impact on mobility, social participation and quality of life in patients with vertigo/dizziness/balance disorders and osteoarthritis (MobilE-TRA): Study protocol of an observational, practice-based cohort study. BMJ Open 8 (4), e022970. doi:10.1136/bmjopen-2018-022970
Kouladjian, L., Gnjidic, D., Chen, T. F., Mangoni, A. A., and Hilmer, S. N. (2014). Drug burden index in older adults: Theoretical and practical issues. Clin. Interv. Aging 9, 1503–1515. doi:10.2147/CIA.S66660
Koyama, A., Steinman, M., Ensrud, K., Hillier, T. A., and Yaffe, K. (2014). Long-term cognitive and functional effects of potentially inappropriate medications in older women. J. Gerontol. A Biol. Sci. Med. Sci. 69 (4), 423–429. doi:10.1093/gerona/glt192
Landi, F., Russo, A., Liperoti, R., Cesari, M., Barillaro, C., Pahor, M., et al. (2007). Anticholinergic drugs and physical function among frail elderly population. Clin. Pharmacol. Ther. 81 (2), 235–241. doi:10.1038/sj.clpt.6100035
Leitliniengruppe Hessen Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM) (2021). S3-Leitlinie hausärztliche leitlinie: Multimedikation. Berlin: AWMF.
Loza, E., Jover, J. A., Rodriguez, L., Carmona, L., and Group, E. S. (2009). Multimorbidity: Prevalence, effect on quality of life and daily functioning, and variation of this effect when one condition is a rheumatic disease. Semin. Arthritis Rheum. Elsevier 58, 312–319. doi:10.1016/j.semarthrit.2008.01.004
Maarsingh, O. R., Dros, J., Schellevis, F. G., van Weert, H. C., Bindels, P. J., and van der Horst, H. E. (2010). Dizziness reported by elderly patients in family practice: Prevalence, incidence, and clinical characteristics. BMC Fam. Pract. 11 (1), 2–9. doi:10.1186/1471-2296-11-2
Mueller, M., Whitney, S. L., Alghwiri, A., Alshebber, K., Strobl, R., Alghadir, A., et al. (2015). Subscales of the vestibular activities and participation questionnaire could be applied across cultures. J. Clin. Epidemiol. 68 (2), 211–219. doi:10.1016/j.jclinepi.2014.10.004
Muncie, H. L., Sirmans, S. M., and James, E. (2017). Dizziness: Approach to evaluation and management. Am. Fam. Physician 95 (3), 154–162.
Nishtala, P. S., Hilmer, S. N., McLachlan, A. J., Hannan, P. J., and Chen, T. F. (2009). Impact of residential medication management reviews on drug burden index in aged-care homes: A retrospective analysis. Drug Aging 26, 677–686. doi:10.2165/11316440-000000000-00000
Nothelle, S. K., Sharma, R., Oakes, A. H., Jackson, M., and Segal, J. B. (2017). Determinants of potentially inappropriate medication use in long-term and acute care settings: A systematic review. J. Am. Med. Dir. Assoc. 18 (9), 806.e1–806806.e17. doi:10.1016/j.jamda.2017.06.005
Nothelle, S. K., Sharma, R., Oakes, A., Jackson, M., and Segal, J. B. (2019). Factors associated with potentially inappropriate medication use in community-dwelling older adults in the United States: A systematic review. IJPP 27 (5), 408–423. doi:10.1111/ijpp.12541
O'Connell, J., Burke, É., Mulryan, N., O'Dwyer, C., Donegan, C., McCallion, P., et al. (2018). Drug burden index to define the burden of medicines in older adults with intellectual disabilities: An observational cross-sectional study. Br. J. Clin. Pharmacol. 84 (3), 553–567. doi:10.1111/bcp.13479
Phillips, A., Heier, M., Strobl, R., Linkohr, B., Holle, R., Peters, A., et al. (2019). Exposure to anticholinergic and sedative medications using the Drug Burden Index and its association with vertigo, dizziness and balance problems in older people–Results from the KORA-FF4 Study. Exp. Gerontol. 124, 110644. doi:10.1016/j.exger.2019.110644
Phillips, A., Strobl, R., Grill, E., and Laux, G. (2018). Anticholinergic and sedative medications and the risk of vertigo or dizziness in the German primary care setting—a matched case-control study from the CONTENT registry. Pharmacoepidemiol. Drug Saf. 27 (8), 912–920. doi:10.1002/pds.4575
Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D., and Team, R. C. (2007). Linear and nonlinear mixed effects models. R. package version 3 (57), 1–89.
Stephan, A.-J., Kovacs, E., Phillips, A., Schelling, J., Ulrich, S. M., and Grill, E. (2018). Barriers and facilitators for the management of vertigo: A qualitative study with primary care providers. Implement Sci. 13 (1), 25–10. doi:10.1186/s13012-018-0716-y
Stephan, A.-J., Schwettmann, L., Meisinger, C., Ladwig, K.-H., Linkohr, B., Thorand, B., et al. (2021). Living longer but less healthy: The female disadvantage in health expectancy. Results from the KORA-Age study. Exp. Gerontol. 145, 111196. doi:10.1016/j.exger.2020.111196
Swain, S. K. (2020). Pharmacotherapy for vertigo: A current perspective. Int. J. Otorhinolaryngol. Head. Neck Surg. 6 (7), 1400–1406. doi:10.18203/issn.2454-5929.ijohns20202806
The Federal Ministry of Health (2020). Daten des Gesundheitswesens. Berlin: The Federal Ministry of Health.
van der Meer, H. G., Wouters, H., Pont, L. G., and Taxis, K. (2018). Reducing the anticholinergic and sedative load in older patients on polypharmacy by pharmacist-led medication review: A randomised controlled trial. BMJ Open 8 (7), e019042. doi:10.1136/bmjopen-2017-019042
van Vugt, V. A., Bas, G., van der Wouden, J. C., Dros, J., van Weert, H. C., Yardley, L., et al. (2020). Prognosis and survival of older patients with dizziness in primary care: A 10-year prospective cohort study. Ann. Fam. Med. 18 (2), 100–109. doi:10.1370/afm.2478
Vrdoljak, D., and Borovac, J. A. (2015). Medication in the elderly-considerations and therapy prescription guidelines. Acta Med. Acad. 44 (2), 159–168. doi:10.5644/ama2006-124.142
Wockenfuss, R., Frese, T., Herrmann, K., Claussnitzer, M., and Sandholzer, H. (2009). Three-and four-digit ICD-10 is not a reliable classification system in primary care. Scand. J. Prim. Healt 27 (3), 131–136. doi:10.1080/02813430903072215
Wouters, H., van der Meer, H., and Taxis, K. (2017). Quantification of anticholinergic and sedative drug load with the drug burden index: A review of outcomes and methodological quality of studies. Eur. J. Clin. Pharmacol. 73 (3), 257–266. doi:10.1007/s00228-016-2162-6
Keywords: vertigo, dizziness, balance disorders, anticholinergic and sedative medications, drug burden index, functioning
Citation: Katzenberger B, Koller D, Strobl R, Kisch R, Sanftenberg L, Voigt K and Grill E (2023) Exposure to anticholinergic and sedative medication is associated with impaired functioning in older people with vertigo, dizziness and balance disorders—Results from the longitudinal multicenter study MobilE-TRA. Front. Pharmacol. 14:1136757. doi: 10.3389/fphar.2023.1136757
Received: 03 January 2023; Accepted: 20 February 2023;
Published: 03 March 2023.
Edited by:
Carlos Alves, University of Coimbra, PortugalReviewed by:
Petra Thürmann, University of Witten/Herdecke, GermanyPrasad Nishtala, University of Bath, United Kingdom
Mohammed S. Salahudeen, University of Tasmania, Australia
Copyright © 2023 Katzenberger, Koller, Strobl, Kisch, Sanftenberg, Voigt and Grill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benedict Katzenberger, QmVuZWRpY3QuS2F0emVuYmVyZ2VyQG1lZC51bmktbXVlbmNoZW4uZGU=
 Benedict Katzenberger
Benedict Katzenberger Daniela Koller1,3
Daniela Koller1,3 Ralf Strobl
Ralf Strobl Rebecca Kisch
Rebecca Kisch Linda Sanftenberg
Linda Sanftenberg Eva Grill
Eva Grill