
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 06 April 2023
Sec. Obstetric and Pediatric Pharmacology
Volume 14 - 2023 | https://doi.org/10.3389/fphar.2023.1135736
This article is part of the Research Topic Safety of Drugs and CAM Products in Pregnancy and Breastfeeding: Evidence From Clinical Toxicology View all 9 articles
Objectives: This study aimed to assess the prevalence of trimester-specific dietary supplements (DS)s use and their possible correlates during pregnancy.
Method: Pregnant women were convenience sampled and recruited from a comprehensive obstetric care center in Shanghai, China. Data relating to the use of DS during pregnancy, social support and other social-demographic and obstetric data were collected. Trimester-specific DS use and factors related DS were explored.
Results: Of the 2803 women participating in this study, 94.8%, 96.2%, 93.8%, and 94.4% reported the use of at least one DS during pregnancy (all trimesters) and in the first, second, and third trimesters of pregnancy, respectively. Significant differences were noted in the use of DS containing folic acid, calcium, iron, vitamins, and docosahexaenoic acid (DHA), during the three trimesters of pregnancy. A higher proportion of DS use was negatively associated with certain categories of pregnant woman, including unemployed/housewife, low education level, obese, and low social support. A positive association was identified with gestational age.
Conclusion for practice: Considering the high prevalence of DS use during pregnancy, future studies are needed to evaluate the accuracy and suitability of DS usage during pregnancy.
Maternal nutritional status during pregnancy is essential for both maternal and fetal health. Of particular importance are micronutrients such as folate acid, iron, calcium, and zinc, all of which are considered to be positively related to fetal brain development (Wu et al., 2012; Parisi et al., 2019). However, it has been suggested that diet alone may not fully meet the heightened nutritional requirements during pregnancy (Wu et al., 2012; Mousa et al., 2019). Furthermore, micronutrient deficiencies are common during pregnancy, especially in resource-poor environments and in low- and middle-income countries (Keats et al., 2019; Lander et al., 2019; Parisi et al., 2019). Dietary supplements (DS)s, as defined by the Food and Drug Administration (FDA), are non-drug products that contain dietary ingredients such as vitamins, minerals, and amino acids, that can be used to supplement the diet. The use of DS is a common practice in pregnant women worldwide and aims to address nutritional gaps in their diets of pregnant women so that they may achieve beneficial outcomes in both fetal and maternal health. Among these, the use of folic acid supplements during pregnancy has been recommended by the World Health Organization (WHO), China, and many other countries to prevent neural tube defects (NTDs) (Ren, 2015; Chitayat et al., 2016). Calcium supplements are also used to prevent pregnancy-related hypertensive disorders (Omotayo et al., 2016; Mousa et al., 2019).
Variations on the prevalence of DS use during pregnancy are evident across different countries. The reported prevalence of at least one DS use during pregnancy was 75.3% in Japan (the majority of participants were in mid-to-late pregnancy) (Sato et al., 2013), 77.6% in the United States (Branum et al., 2013; Jun et al., 2020), 78.0% in Sweden (the first trimester) (Bärebring et al., 2018), 81.4% in Norway (the first 4–5 months of pregnancy) (Haugen et al., 2008), 85% in Finland (Arkkola et al., 2006), and 91.0% in Brazil (Miranda et al., 2019). Epidemiological data on the use of DS by Chinese pregnant women is sparse. One study in the Sichuan Province of China reported the use of DS in 81.8% of pregnancies although this data was collected retrospectively (after delivery and before the women had been discharged from the hospital) (Tang et al., 2017). Another study, carried out in Taiwan, investigated the use of DS during pregnancy among 366 women who underwent assisted reproductive technology (Lin et al., 2019).
Furthermore, the use of DS has been reported to relate to a variety of factors at both the individual and national levels. Studies have shown that socioeconomic status, such as age, gender, educational level, employment status, income, marital status, residence, and medical insurance status, are all factors that could affect the use of DS in a general population (Kofoed et al., 2015; Mohd Ashri et al., 2021; Mohsen et al., 2021; Rontogianni et al., 2021). However, how sociodemographic and obstetric-specific factors contribute to the use of DS during pregnancy largely remains unclear. Some previous studies investigated factors related to the use of DS during pregnancy (Bärebring et al., 2018; Jun et al., 2020). One study in Sweden showed that gestational age, parity, birthplace, income, education, and employment, were all factors related to the use of DS in the first trimester (Bärebring et al., 2018). Young age, low family support, and early pregnancy were reported to relate to lower levels of DS use in pregnant women in the United States (Jun et al., 2020). Evidence is emerging in the literature to indicate there are socioeconomic disparities in the use of DS in the general population (Mohd Ashri et al., 2021; Mohsen et al., 2021; Rontogianni et al., 2021). Disparities in the use of DS during pregnancy may have a negative impact on the health of mothers and their offspring; these factors need to be investigated urgently.
It is vital that we understand the specific use of DS during pregnancy, consider important implications for the formulation of appropriate and effective interventions for the appropriate use of DS, and produce public health policies relating to maternal nutrition in pregnancy. Under this perspective, the objectives of the present study were to: (a) measure the prevalence of the trimester-specific use of DS, and (b) investigate the factors related to the use of DS by women. We hypothesized that the prevalence of DS use will vary across the different periods of pregnancy and that the use of DS might be related to sociodemographic and obstetric characteristics in pregnant women.
This was a cross-sectional survey that was conducted to investigate the trimester-specific use of DS by pregnant women in Shanghai, China. We also investigated the factors associated with the use of DS. The paper was written in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
A convenience sampling method was used to recruit pregnant women who registered their pregnancy in the study hospital and attended their routine antenatal visits. Given the utilization of multivariate analysis in the present study, a sample size of 150–300 participants is recommended to ensure a stable test, with 10–20 participants per independent variable being deemed appropriate, and given the estimated number of independent variables that potentially relate to the use of DS in this study, which is 15. And from epidemiological point of view, considering that 300,000 deliveries are reported in the study setting each year, we selected a 10% (n = 3000) sample for our survey. The inclusion criteria were (1) ≥ 18 years of age, (2) pregnancy confirmed by B ultrasound, (3) competent in Mandarin, (4) able to use a mobile phone, and (5) agreed to participate in the study. The exclusion criteria were as follows: (1) cognitive or mental disorders and (2) severe pregnancy complications. Of the 3000 women approached, 124 refused to participate, while 2803 completed the questionnaires (a response rate of 93.4%). This study was reviewed and approved by the Ethics Committee of the Shanghai First Maternity and Infant Hospital (Reference: KS19101).
To the best of our knowledge, there are no widely recognized tools available to investigate the use of DS by women during pregnancy. Referring to a series of related studies (Tang et al., 2017; Lin et al., 2019; Miranda et al., 2019), we developed a self-reported checklist to assess the current use of DS by women over the previous 4 weeks of pregnancy. The checklist included seven common DS items: folic acid, calcium, iron, iodine, zinc, vitamins, and DHA. Vitamins included both multi-vitamins and single vitamins such as vitamins A, C, D, E, etc., but ruled out folic acid supplementation alone. Although folic acid is also a vitamin, we have listed this agent separately because it plays a vital role during pregnancy. We also provide an “other” response for women to record the brand name of the DS they used if they did not know the ingredients. The “other” response was categorized into seven items by the researcher based on ingredients. A panel of experts (three experts in maternal nutrition and three researchers) examined the DS use checklist for validity. A pilot survey of 40 pregnant women showed that the test-retest reliability over 2 weeks of all DS items was 0.75–0.86.
Social-demographic characteristics included age, ethnicity (Han Chinese or ethnic minority), educational level (primary, secondary, college, Bachelor or Master and above), occupation (employed or unemployed/housewife), marital status (married or single/divorced), local residence (Shanghai or non-Shanghai), medical insurance (with medical insurance or no medical insurance), and social support. Except for social support, all social-demographic characteristics were extracted from electronic medical records. Social support was evaluated by the social supported rating scale. This scale was designed by Xiao in 1986 and was revised in 1994 (Xiao, 1994). This is a comprehensive scale that evaluated the level of objective support, subjective support, and use of support received by participants. The sum of scores ranged from 12 to 66; a higher score indicated a higher level of social support. This scale is widely used in the Chinese population with good reliability and validity; previous research showed that Cronbach’s α coefficient was 0.89 and test-retest reliability was 0.92 (Xiao, 1994). In the current study, Cronbach’s α coefficient was 0.87.
We considered a range of obstetric characteristics, including parity (primipara or multipara), mode of conception (natural conception or artificial conception), gestational age, pregnancy risk grading (green, yellow, or orange), pre-pregnancy body mass index (PPBMI), and history of adverse pregnancy. The pregnancy risk grading was routinely evaluated for all Chinese pregnant women who registered their pregnancy in a hospital l. The severity of pregnancy risk was classified into five colors: green (low risk), yellow (general risk), orange (high risk), red (very high risk) and purple (infectious disease). PPBMI was categorized into four groups according to the WHO recommendation on adult body mass index (BMI) classification for the Asian population: underweight (BMI <18.5 kg/m2); normal weight (18.5 kg/m2 ≤ BMI <24.0 kg/m2); overweight (24.0 kg/m2 ≤ BMI <28.0 kg/m2); and obese (BMI ≥28.0 kg/m2) (Consultation, 2004). Histories of abnormal pregnancy included miscarriage (≥3 times), a history of preterm birth, perinatal death, birth defects, a history of ectopic pregnancy, a history of trophoblastic disease, a history of previous pregnancy complications, and comorbidities.
This study was conducted over 1 year (May 2020–May 2021). The study involved a paper-free survey; this was due to the forced restriction of unnecessary contact during the COVID-19 pandemic. The research staff approached pregnant women who were waiting for their routine antenatal visits and explained the basic details of the study to eligible participants. After informed consent was obtained, a quick response code (QR code) for the electronic questionnaire was presented. This allowed the study participants to scan the QR code using their smartphones to complete the survey online. To ensure the uniqueness of each participant, each pregnant woman’s medical card number would only be allowed to participate once in this study. The questionnaire was completed in approximately 3–5 min during pilot testing. The research staff were nearby to provide assistance with the questionnaire if necessary; these staff allowed an adequate time for the patients to rest and ask questions.
Data were analyzed using the Statistical Package for Social Sciences version 20.0 for Windows (IBM Company, Chicago, United States). Social-demographic characteristics, obstetric characteristics, and the use of DS during pregnancy, were reported using descriptive statistics. Trimester-specific DS use was tested by the Chi-squared test and advanced pairwise comparisons were adjusted by the Bonferroni correction. Group differences in the overall use of DS were tested by t-tests or by one-way analysis of variance. And chi-square tests were used to analyze group differences in each DS based on sociodemographic and obstetric data. Multiple linear regression analysis was also performed to explore factors related to the use of DS. Social-demographic and obstetric characteristics that were related to DS use in univariate analysis (p < 0.05) were then re-evaluated by multiple regression analysis with a stepwise procedure (entry 0.05, removal 0.10). For all analyses, the alpha level of significance was set to 0.05.
Tables 1, 2 show the social-demographic and obstetric characteristics of the participants along with the various aspects of DS use in each group. The age of the participating women ranged from 18 to 45 (mean: 30.28 ± 3.81 years), and the mean gestational age was 22.35 ± 4.49 weeks. Most of the participants were Han Chinese (98.0%), employed (83.8%), held a bachelor’s degree or above (62.6%), and had medical insurance (87.5%).
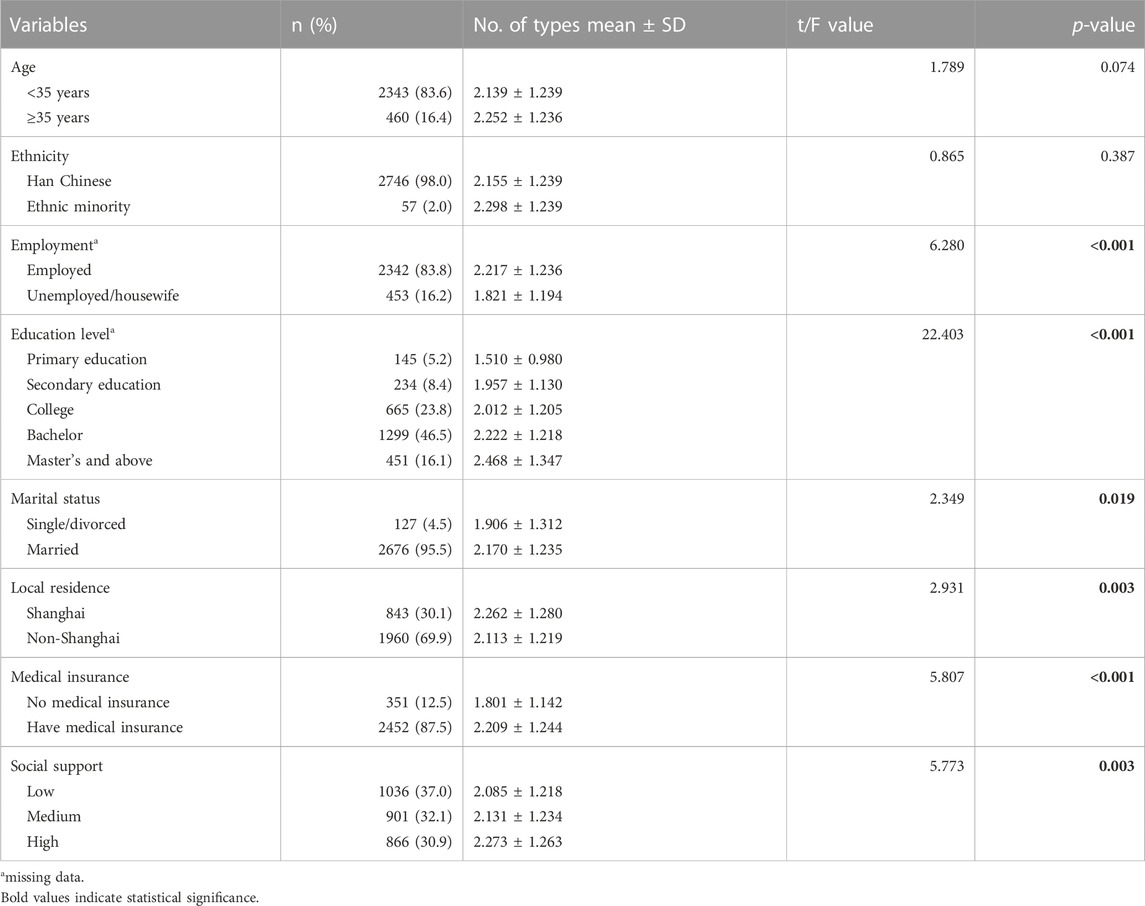
TABLE 1. Relationships in the use of different types of dietary supplements with social-demographic characteristics in pregnant women (N = 2803).
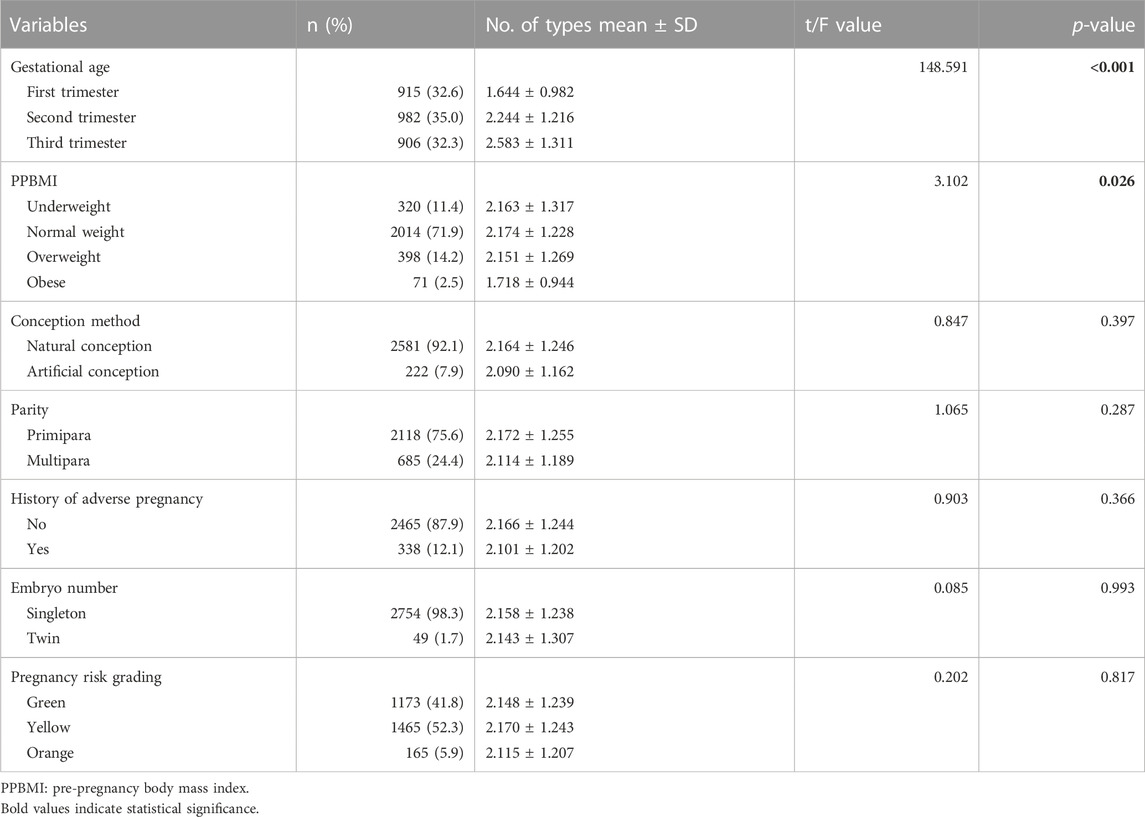
TABLE 2. Relationships in the use of different types of dietary supplements with women’s obstetric characteristics (N = 2803).
The prevalence of DS use during pregnancy (all trimesters) and in the first, second, and third trimester of pregnancy was 94.8%, 96.2%, 93.8%, and 94.4%, respectively. 278 (9.9%) of the women chose an “other” option. The “other” responses mainly include some brand names of DS which could be categorized into folic acid, multi-vitamins, and DHA. But also include some traditional Chinese medicine, such as bird’s-nest, donkey-hide gelatin, etc. Our data showed that the mean number of different types of DS used was 2.16 ± 1.24.
Table 3 shows the seven types of DS use during pregnancy (all trimesters) and in the first (n = 915), second (n = 982) and third trimester (n = 906) of pregnancy. Significant differences were noted in the use of folic acid, calcium, iron, vitamins, and DHA supplements (all p < 0.001) during the three trimesters, as determined by the Chi-squired test. Pairwise comparisons further showed that the use of folic acid supplements decreased as the pregnancy progressed. Peak use (93.1%) was noted in the first trimester; this rate decreased dramatically (by 49.4%) in the second trimester and reduced even further during the third trimester. In contrast, the use of iron supplements increased as the pregnancy progressed; the use of these supplements was. relatively low (7.9%) in the first trimester but then increased during the second trimester and reached a peak (61.7%) during the third trimester. The use of calcium, vitamins, and DHA supplements, all increased during the second trimester and remained stable in the third trimester. The use of iodine and zinc supplements was extremely low throughout pregnancy (all rates <5.0%).
Univariate analysis showed that employment, educational level, marital status, local residence, medical insurance, social support, gestational age, and PPBMI, were all factors that were significantly related to the number of DS types used by pregnant women (Table 1; Table 2).
Multiple linear regression analysis showed that the use of a higher number of DS types was negatively associated with several factors: unemployed/housewife (B = −0.180, p = 0.010), low educational level (primary education: B = −0.459, p < 0.001; college: B = −0.158, p = 0.001), obese (B = −0.372, p = 0.008) and low social support (B = −0.168, p = 0.002), but was positively associated with gestational age (second trimester: B = 0.611, p < 0.001; third trimester: B = 0.907, p < 0.001) (Table 4). Factors related to folic acid, calcium, iron, iodine, zinc, vitamins, and DHA use separately were presented in the Supplementary File.
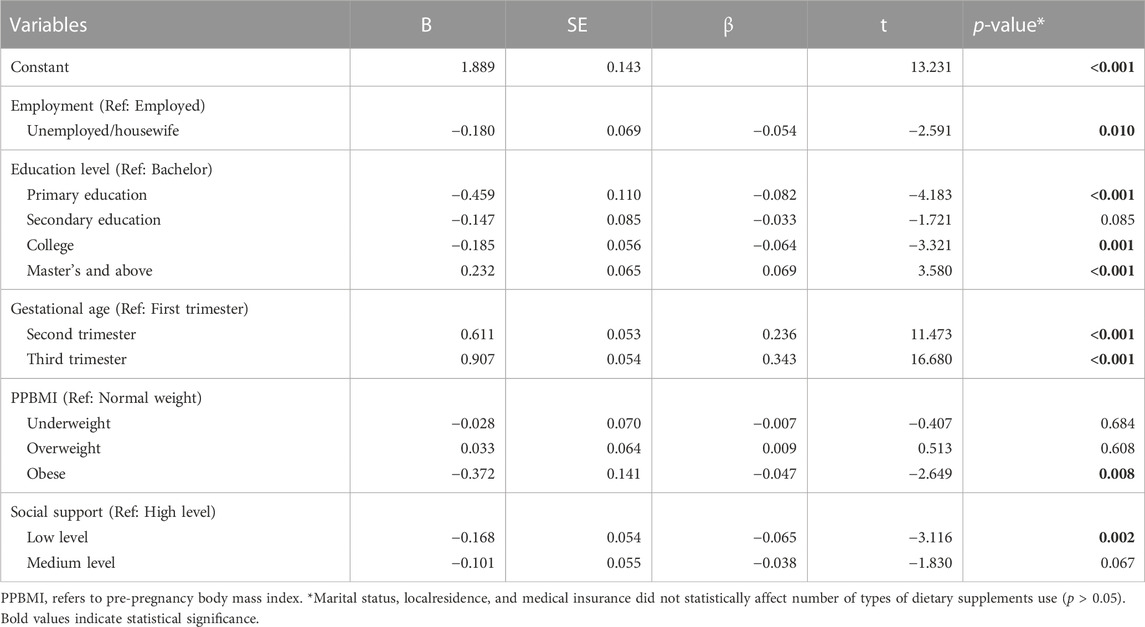
TABLE 4. Multivariable analysis of factors related to the number of different dietary supplements used by pregnant women.
In the present study, we investigated the use of DS by women during pregnancy as well as the social-demographic and obstetric factors related to the use of DS. This is the first contemporary study to describe the trimester-specific prevalence of DS use in a population of Chinese pregnant women. In this study, the utilization rate of DS among pregnant women in Shanghai, China, was much higher than that reported in other counties (Arkkola et al., 2006; Haugen et al., 2008; Branum et al., 2013; Sato et al., 2013; Miranda et al., 2019), thus suggesting a crucial need for healthcare providers to discuss DS use and guide the use of DS during pregnancy.
We also identified a relatively higher proportion of women taking folic acid supplements during pregnancy (93.1%, 43.7%, and 34.8%, during the first second, and third trimesters, respectively) when compared to the study of a Swedish cohort (74.4% used folic acid in the first trimester compared to 43.2% in the third trimester). However, our results were similar to those reported by a previous study conducted in four cities in China, which found that 95.1% of pregnant women took folic acid supplements during pregnancy or 3 months prior to pregnancy (Cui et al., 2021). The reported high use of folic acid supplements reflects the fact that folic acid supplementation is common in China. The typical Chinese main staple (rice) is not fortified with folate acid, thus resulting in a high prevalence of NTDs in China. To reduce the high prevalence of NTDs, the Chinese government started a nation-wide program in 2009 that provides all women with rural household registration who plan to become pregnant with free folic acid supplements (Ren, 2015).
But it is indicated that socioeconomic disparities in the utilization of folic acid during pregnancy still exist (Liu et al., 2017). Furthermore, routine empirical folic acid supplementation of 0.4 mg/day is recommended by the Chinese Nutrition Society from 3 months prior to conception to the first trimester of pregnancy, in addition to the consumption of folate-rich foods (Wang et al., 2016; Yang et al., 2018). The overall prevalence of folic acid supplement use was 75.62% when reported by a National Free Preconception Health Examination Project of 907,720 rural Chinese women (Liu et al., 2017). The periconceptional folic acid supplementation program has successfully reduced the prevalence of NTDs in China (Cui et al., 2021).
In addition, the demand for additional calcium during pregnancy has been well-established (Hacker et al., 2012). An adequate intake of calcium is especially critical during pregnancy because of its potential effect on maternal and fetal bone health (Hacker et al., 2012). Furthermore, calcium may also reduce the risk of gestational diabetes mellitus and pregnancy-related hypertensive disorders (Khaing et al., 2017; Osorio-Yáñez et al., 2017; Hofmeyr et al., 2018). A previous study in China showed that calcium supplementation was significantly associated with a lower preterm birth risk (Liu D. et al., 2021). Routine calcium supplementation is strong recommended by the WHO to prevent preeclampsia (Omotayo et al., 2016). Furthermore, it has been frequently reported that women do not consume the recommended quantity of calcium from their routine diets, even in developed countries (Hacker et al., 2012). It has been reported that annual milk consumption in China is the lowest in the world and that 90% of the Chinese population is at risk of an inadequate calcium intake (He et al., 2016). The dietary reference intake for calcium among pregnant women in China is 800–1,000 mg/day (Liu X. H. et al., 2021). The typical Chinese diet does not usually meet the increased calcium requirements during pregnancy (Wang et al., 2010; Liu D. et al., 2021). A high prevalence of calcium deficiency was previously reported in pregnant women in Chengdu, China (Wang et al., 2010). These facts may explain the high rate (>75% in the second and third trimesters of pregnancy) of calcium supplement use in the current study.
Along with folate acid and calcium, iron is one of the nutrients for which dietary intake alone cannot realistically meet the increased demands of pregnancy. In addition, due to the low bioavailability of dietary iron, iron supplementation is usually recommended for women during pregnancy to prevent and treat maternal iron deficiency anemia (IDA), but must be used with caution (Hacker et al., 2012; Siu, 2015). In fact, iron requirements fluctuate across pregnancy. In the first trimester, iron requirements decrease; this is due to the cessation of menses and the improved absorption capacity of iron from the diet during pregnancy (EFSA Panel on Dietetic Products and Allergies, 2015). In the second trimester, due to expansion of plasma volume and red cell mass, iron requirements increase; they also continue to increase during the third trimester as iron accumulates in the placenta (Hacker et al., 2012). A prospective multi-racial study reported that elevated iron stores in the first trimester were positively associated with the development of gestational diabetes (Rawal et al., 2017). Actually, routine iron supplementation for all women is not recommended (Pavord et al., 2012). And given that iron requirements vary during pregnancy and the adverse effects of both iron deficiency and overload (Fu et al., 2016; Rawal et al., 2017), precise recommendations exist for iron intake within the context of body iron status, pregnancy stage, and dietary iron intake. In China, the estimated prevalence of anemia is 23.5% (entire pregnancy), and 2.7%, 14.7%, and 16.6% in the first, second, and third trimesters, respectively, as defined by a hemoglobin concentration of 110 g/L at any stage of pregnancy (Lin et al., 2018). To achieve the goal set in The National Nutrition Plan (2017–2030), which was issued by the General Office of the State Council, P.R. China, to reduce the prevalence of anemia in pregnant women to <10% by 2030 (Council, 2017), there are still many measures that require attention. In the hospital where the study was conducted, 100–200 mg/day of elemental iron is usually recommended for women with IDA (Association, 2014). Of the pregnant women in the current study, 7.9%, 23.6%, and 61.7%, took iron supplements in the first, second, and third trimesters, respectively. This result is consistent with the increased iron requirement during mid-late pregnancy (Hacker et al., 2012). Similarly, an Australian cohort study reported the use of triple iron supplementation from the first-to-third trimesters (Livock et al., 2017).
In this study, vitamin supplements were used by 30.9%, 40.6%, and 43.7% of women in the first, second, and third trimesters; these figures are relatively lower than those reported by Savard et al. (86.1%, 84.8%, and 78.5%, respectively) (Savard et al., 2018). This finding can be explained by the fact that prenatal multivitamins are the most favored supplement taken by the Western population (Savard et al., 2018). Vitamin D, an essential fat-soluble vitamin, is very important during pregnancy. It is reported that a considerable proportion (40.7%) of Chinese pregnant women suffer from vitamin D deficiency (Yang et al., 2021). In this study, we did not investigate the intake vitamin D separately. However, it is worth mentioning that calcium supplements are almost always supplemented with vitamin D. In this study, calcium supplements were used by 17.4%, 76.3%, and 80.4% of women in the first, second, and third trimesters. In addition, DHA, a key and essential n-3 long-chain polyunsaturated fatty acid, is essential for the fetal central nervous system along with retina function development and immunomodulation (Massari et al., 2020). Dietary DHA can be readily found in seafood, particularly deep-sea fish, such as salmon, herring, and anchovies. In China, women are encouraged to eat deep-sea fish 2–3 times a week during pregnancy (Wang et al., 2016; Yang et al., 2018). Compared to other ethnic groups, the intake of DHA from dietary sources is very low in China (Li et al., 2015; Deng et al., 2017). This finding may explain the higher use of DHA supplements reported in the current study (11.9%–34.9%) than other areas (4.5% in the first trimester and 4.6% in the third trimester in Sweden) (Bärebring et al., 2018). The high proportion of DHA supplement use in Chinese pregnant women may also reflect an increased awareness in the role of DHA in fetal brain development (Li et al., 2015).
This study considered the use of dietary supplements (DS) during pregnancy under both medical guidance and self-administration by pregnant women. Folic acid supplementation during the first trimester is generally a self-initiated practice among expectant mothers for prenatal care. In cases where early prenatal consultations reveal a lack of folic acid intake, physicians may prescribe the supplement accordingly. Clinical assessments are typically used to detect calcium and iron deficiencies, and if such deficiencies are diagnosed, supplementation or prescription may be recommended. However, some pregnant women may choose to take these supplements for preventive purposes. Vitamins and DHA, on the other hand, are typically self-administered by pregnant women.
We also investigated the sociodemographic and obstetric factors related to the use of DS among pregnant women. We found that being unemployed, being a housewife, having a low educational level, low levels of social support, and being obese, were all negatively associated with the number of DS types used by pregnant women. These results are supported by a previous study carried out in Sweden which showed that education level and employment were associated with the use of DS during early pregnancy (Bärebring et al., 2018). A previous study reported that high socioeconomic status was associated with a healthier diet during pregnancy (Poulain et al., 2021). It is possible that socioeconomic status is related to a woman’s ability to purchase DS. The relationship between educational level and DS in the present study was consistent with previous studies conducted in the Sichuan Province of China (Tang et al., 2017) and the United States (Branum et al., 2013). These findings suggest a tendency for women with a higher level of education to make greater efforts to achieve a better nutritional status during pregnancy. This might be explained by the fact that a higher level of education was related to a higher level of health awareness and better health literacy. Social support has been shown to be related to improved adherence to the use of folic acid supplements during pregnancy (Wiradnyani et al., 2016). Our present data suggested that low social support may affect the number of different types of DS used by women during pregnancy. Constant and comprehensive maternal social support is important for healthy dietary habits during pregnancy (Hopkins et al., 2018). Clear and open communication between women and healthcare providers, along with the involvement of family members, may help to improve the use of DS during pregnancy, particularly with regards to the benefits of DS, concerns related to adverse effects, as well as financial barriers (Wiradnyani et al., 2016; Jun et al., 2020). BMI has been reported to be inversely associated with the use of DS in the general population (Rontogianni et al., 2021). Importantly, our data also revealed that obese women are associated with a lower use of DS during pregnancy. As excessive body weight and obesity are known to represent global public health problems in both developed and developing countries, obesity itself has been proven to be associated with adverse health outcomes during pregnancy and over the longer term (Simon et al., 2020). Our research has enhanced our understanding of this field by suggesting that obese women should be supported/educated with regards to their nutritional health during the critical period of pregnancy.
In addition, we observed an increase in the use of DS in married women, those living in Shanghai, and those that had medical insurance. However, these associations did not retain significance in the multivariable model. Although parity was also reported as a factor related to the use of DS during pregnancy in Sweden (Bärebring et al., 2018) and Norway (Haugen et al., 2008), our present data did not concur with these earlier results. This inconsistency may be explained by the different characteristics of the participants in our study. In China, the proportion of primiparous women is much higher within the maternal population (75.6%) than that reported in previous studies carried out in Sweden (42.3%) (Bärebring et al., 2018) or Norway (47.3%) (Haugen et al., 2008).
There are some limitations associated with the present study that we need to consider. First, this study was conducted in one hospital in Shanghai; most participants were highly educated. Second, the use of DS in this study was only evaluated by yes or no questions, the advantage of this instrument is that it provides a time-effective means of providing dietary surveys in a busy clinical setting. A disadvantage, however, is the limited accuracy of the dietary data. Furthermore, we were unable to calculate the actual intake of supplements and food sources. Therefore, it was impossible to compare the actual intake with dietary recommendations in the current study. Future studies should involve a larger and more representative sample and include more detailed dietary investigations. In addition, the use of DS prior to conceptional was not investigated in this study. Finally, the cross-sectional study design precludes the investigation of any specific causal relationships.
In summary, we demonstrated a high prevalence of DS use in women during pregnancy and the use of DS was associated with employment status, educational level, perceived social support, PPBMI, and gestational age. The findings of the current study emphasized the crucial need for future studies to evaluate the accuracy and suitability of DS usage during pregnancy. Due to the high prevalence of DS use during pregnancy, synergistic efforts between policymakers, maternal and child nutrition experts, and obstetric health workers, are highly recommended to guide the appropriate use of DS during pregnancy, such as education, monitoring, and taking necessary actions.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethical Community of the Shanghai First Maternity and Infant Hospital. The patients/participants provided their written informed consent to participate in this study.
Conceptualization: HJ, NG, and YL; Data collection: YL and HF; Data analysis: YL and NG; Writing the original draft preparation: YL and HF; Writing the review and editing: YL, NG, and HJ; Funding acquisition: HJ. All authors have read and agreed to the published version of the manuscript.
The research was supported and funded by the Medical Innovation Project of Shanghai Science and Technology Commission (grant No. 20Y11907100 &No. 22DZ2203800). The funders had no role in the design of the study, in the collection, analyses, or interpretation of data in writing the manuscript, or in the decision to publish the results.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1135736/full#supplementary-material
Arkkola, T., Uusitalo, U., Pietikäinen, M., Metsälä, J., Kronberg-Kippilä, C., Erkkola, M., et al. (2006). Dietary intake and use of dietary supplements in relation to demographic variables among pregnant Finnish women. Br. J. Nutr. 96 (5), 913–920. doi:10.1017/bjn20061929
Association, P. M. B. o. C. M. (2014). Guidelines for the diagnosis and treatment of iron deficiency and iron deficiency anemia in pregnancy. Chin. J. Perinat. Med. (7), 451–454. (In Chinese).
Bärebring, L., Mullally, D., Glantz, A., Elllis, J., Hulthén, L., Jagner, Å., et al. (2018). Sociodemographic factors associated with dietary supplement use in early pregnancy in a Swedish cohort. Br. J. Nutr. 119 (1), 90–95. doi:10.1017/S0007114517003270
Branum, A. M., Bailey, R., and Singer, B. J. (2013). Dietary supplement use and folate status during pregnancy in the United States. J. Nutr. 143 (4), 486–492. doi:10.3945/jn.112.169987
Chitayat, D., Matsui, D., Amitai, Y., Kennedy, D., Vohra, S., Rieder, M., et al. (2016). Folic acid supplementation for pregnant women and those planning pregnancy: 2015 update. J. Clin. Pharmacol. 56 (2), 170–175. doi:10.1002/jcph.616
Consultation, W. E. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363 (9403), 157–163. doi:10.1016/S0140-6736(03)15268-3
Council, G. O. o. t. S. (2017). National nutrition plan (2017-2030). J. Nutr. 39 (04), 315–320. (In Chinese).
Cui, M., Lu, X. L., Lyu, Y. Y., Wang, F., Xie, X. L., Cheng, X. Y., et al. (2021). Knowledge and intake of folic acid to prevent neural tube defects among pregnant women in urban China: A cross-sectional study. BMC Pregnancy Childbirth 21 (1), 432. doi:10.1186/s12884-021-03893-4
Deng, J., Li, X., Ding, Z., Wu, Y., Chen, X., and Xie, L. (2017). Effect of DHA supplements during pregnancy on the concentration of PUFA in breast milk of Chinese lactating mothers. J. Perinat. Med. 45 (4), 437–441. doi:10.1515/jpm-2015-0438
EFSA Panel on Dietetic Products and Allergies (2015). Scientific opinion on dietary reference values for iron. EFSA J. 13 (10), 4254. doi:10.2903/j.efsa.2015.4254
Fu, S., Li, F., Zhou, J., and Liu, Z. (2016). The relationship between body iron status, iron intake and gestational diabetes: A systematic review and meta-analysis. Med. Baltim. 95 (2), e2383. doi:10.1097/MD.0000000000002383
Hacker, A. N., Fung, E. B., and King, J. C. (2012). Role of calcium during pregnancy: Maternal and fetal needs. Nutr. Rev. 70 (7), 397–409. doi:10.1111/j.1753-4887.2012.00491.x
Haugen, M., Brantsaeter, A. L., Alexander, J., and Meltzer, H. M. (2008). Dietary supplements contribute substantially to the total nutrient intake in pregnant Norwegian women. Ann. Nutr. Metab. 52 (4), 272–280. doi:10.1159/000146274
He, Y., Yang, X., Xia, J., Zhao, L., and Yang, Y. (2016). Consumption of meat and dairy products in China: A review. Proc. Nutr. Soc. 75 (3), 385–391. doi:10.1017/S0029665116000641
Hofmeyr, G. J., Lawrie, T. A., Atallah Á, N., and Torloni, M. R. (2018). Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst. Rev. 10 (10), Cd001059. doi:10.1002/14651858.CD001059.pub5
Hopkins, A. L., Yeoman, M., and Ritenbaugh, C. (2018). Healthy foods prepared at home: Diet and support as protective strategies during pregnancy for Hispanic women. Ecol. Food Nutr. 57 (2), 140–161. doi:10.1080/03670244.2018.1423971
Jun, S., Gahche, J. J., Potischman, N., Dwyer, J. T., Guenther, P. M., Sauder, K. A., et al. (2020). Dietary supplement use and its micronutrient contribution during pregnancy and lactation in the United States. Obstet. Gynecol. 135 (3), 623–633. doi:10.1097/AOG.0000000000003657
Keats, E. C., Haider, B. A., Tam, E., and Bhutta, Z. A. (2019). Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst. Rev. 3 (3), Cd004905. doi:10.1002/14651858.CD004905.pub6
Khaing, W., Vallibhakara, S. A., Tantrakul, V., Vallibhakara, O., Rattanasiri, S., McEvoy, M., et al. (2017). Calcium and vitamin D supplementation for prevention of preeclampsia: A systematic review and network meta-analysis. Nutrients 9 (10), 1141. doi:10.3390/nu9101141
Kofoed, C. L., Christensen, J., Dragsted, L. O., Tjønneland, A., and Roswall, N. (2015). Determinants of dietary supplement use-healthy individuals use dietary supplements. Br. J. Nutr. 113 (12), 1993–2000. doi:10.1017/S0007114515001440
Lander, R. L., Hambidge, K. M., Westcott, J. E., Tejeda, G., Diba, T. S., Mastiholi, S. C., et al. (2019). Pregnant women in four low-middle income countries have a high prevalence of inadequate dietary intakes that are improved by dietary diversity. Nutrients 11 (7), 1560. doi:10.3390/nu11071560
Li, Y., Li, H. T., Trasande, L., Ge, H., Yu, L. X., Xu, G. S., et al. (2015). DHA in pregnant and lactating women from coastland, lakeland, and inland areas of China: Results of a DHA evaluation in women (DEW) study. Nutrients 7 (10), 8723–8732. doi:10.3390/nu7105428
Lin, C. Y., Chen, Y. J., Lee, S. H., Kuo, C. P., Lee, M. S., and Lee, M. C. (2019). Uses of dietary supplements and herbal medicines during pregnancy in women undergoing assisted reproductive technologies- A study of taiwan birth cohort. Taiwan J. Obstet. Gynecol. 58 (1), 77–81. doi:10.1016/j.tjog.2018.11.015
Lin, L., Wei, Y., Zhu, W., Wang, C., Su, R., Feng, H., et al. (2018). Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: A multicentre retrospective study. BMC Pregnancy Childbirth 18 (1), 111. doi:10.1186/s12884-018-1739-8
Liu, D., Li, S., Lei, F., Zhao, Y., Cheng, Y., Dang, S., et al. (2021a). Associations between maternal calcium intake from diet and supplements during pregnancy and the risk of preterm birth in a Chinese population. Eur. J. Clin. Nutr. 75 (1), 141–150. doi:10.1038/s41430-020-00701-8
Liu, M., Chen, J., Liu, J., Zhang, S., Wang, Q., Shen, H., et al. (2017). Socioeconomic inequality in periconceptional folic acid supplementation in China: A census of 0.9 million women in their first trimester of pregnancy. BMC Pregnancy Childbirth 17 (1), 422. doi:10.1186/s12884-017-1618-8
Liu, X. H., Su, Y. X., Wang, Z. X., Qi, H. B., and Li, T. (2021b). Expert consensus on calcium supplementation for pregnant women in China (2021). J. Pract. Obstetrics Gynecol. 37 (05), 345–347. (In Chinese).
Livock, M., Anderson, P. J., Lewis, S., Bowden, S., Muggli, E., and Halliday, J. (2017). Maternal micronutrient consumption periconceptionally and during pregnancy: A prospective cohort study. Public Health Nutr. 20 (2), 294–304. doi:10.1017/S1368980016002019
Massari, M., Novielli, C., Mandò, C., Di Francesco, S., Della Porta, M., Cazzola, R., et al. (2020). Multiple micronutrients and docosahexaenoic acid supplementation during pregnancy: A randomized controlled study. Nutrients 12 (8), 2432. doi:10.3390/nu12082432
Miranda, V. I. A., da Silva Dal Pizzol, T., Silveira, M. P. T., Mengue, S. S., da Silveira, M. F., Lutz, B. H., et al. (2019). The use of folic acid, iron salts and other vitamins by pregnant women in the 2015 pelotas birth cohort: Is there socioeconomic inequality? BMC Public Health 19 (1), 889. doi:10.1186/s12889-019-7269-0
Mohd Ashri, M. H., Abu Saad, H., and Adznam, S. (2021). Socio-demographic characteristics, body weight status and energy intake among users and non-users of dietary supplements among government employees in putrajaya, Malaysia. Nutrients 13 (7), 2248. doi:10.3390/nu13072248
Mohsen, H., Yazbeck, N., Al-Jawaldeh, A., Bou Chahine, N., Hamieh, H., Mourad, Y., et al. (2021). Knowledge, attitudes, and practices related to dietary supplementation, before and during the COVID-19 pandemic: Findings from a cross-sectional survey in the Lebanese population. Int. J. Environ. Res. Public Health 18 (16), 8856. doi:10.3390/ijerph18168856
Mousa, A., Naqash, A., and Lim, S. (2019). Macronutrient and micronutrient intake during pregnancy: An overview of recent evidence. Nutrients 11 (2), 443. doi:10.3390/nu11020443
Omotayo, M. O., Dickin, K. L., O'Brien, K. O., Neufeld, L. M., De Regil, L. M., and Stoltzfus, R. J. (2016). Calcium supplementation to prevent preeclampsia: Translating guidelines into practice in low-income countries. Adv. Nutr. 7 (2), 275–278. doi:10.3945/an.115.010736
Osorio-Yáñez, C., Qiu, C., Gelaye, B., Enquobahrie, D. A., and Williams, M. A. (2017). Risk of gestational diabetes mellitus in relation to maternal dietary calcium intake. Public Health Nutr. 20 (6), 1082–1089. doi:10.1017/S1368980016002974
Parisi, F., di Bartolo, I., Savasi, V. M., and Cetin, I. (2019). Micronutrient supplementation in pregnancy: Who, what and how much? Obstet. Med. 12 (1), 5–13. doi:10.1177/1753495X18769213
Pavord, S., Myers, B., Robinson, S., Allard, S., Strong, J., Oppenheimer, C., et al. (2012). UK guidelines on the management of iron deficiency in pregnancy. Br. J. Haematol. 156 (5), 588–600. doi:10.1111/j.1365-2141.2011.09012.x
Poulain, T., Spielau, U., Vogel, M., Dathan-Stumpf, A., Körner, A., and Kiess, W. (2021). Changes in diet from pregnancy to one year after birth: A longitudinal study. BMC Pregnancy Childbirth 21 (1), 600. doi:10.1186/s12884-021-04038-3
Rawal, S., Hinkle, S. N., Bao, W., Zhu, Y., Grewal, J., Albert, P. S., et al. (2017). A longitudinal study of iron status during pregnancy and the risk of gestational diabetes: Findings from a prospective, multiracial cohort. Diabetologia 60 (2), 249–257. doi:10.1007/s00125-016-4149-3
Ren, A. G. (2015). Prevention of neural tube defects with folic acid: The Chinese experience. World J. Clin. Pediatr. 4 (3), 41–44. doi:10.5409/wjcp.v4.i3.41
Rontogianni, M. O., Kanellopoulou, A., Markozannes, G., Bouras, E., Derdemezis, C., Doumas, M. T., et al. (2021). Prevalence and determinants of sex-specific dietary supplement use in a Greek cohort. Nutrients 13 (8), 2857. doi:10.3390/nu13082857
Sato, Y., Nakanishi, T., Chiba, T., Yokotani, K., Ishinaga, K., Takimoto, H., et al. (2013). Prevalence of inappropriate dietary supplement use among pregnant women in Japan. Asia Pac J. Clin. Nutr. 22 (1), 83–89. doi:10.6133/apjcn.2013.22.1.08
Savard, C., Lemieux, S., Weisnagel, S. J., Fontaine-Bisson, B., Gagnon, C., Robitaille, J., et al. (2018). Trimester-specific dietary intakes in a sample of French-Canadian pregnant women in comparison with national nutritional guidelines. Nutrients 10 (6), 768. doi:10.3390/nu10060768
Simon, A., Pratt, M., Hutton, B., Skidmore, B., Fakhraei, R., Rybak, N., et al. (2020). Guidelines for the management of pregnant women with obesity: A systematic review. Obes. Rev. 21 (3), e12972. doi:10.1111/obr.12972
Siu, A. L. (2015). Screening for iron deficiency anemia and iron supplementation in pregnant women to improve maternal health and birth outcomes: U.S. Preventive services task force recommendation statement. Ann. Intern Med. 163 (7), 529–536. doi:10.7326/M15-1707
Tang, L., Lee, A. H., Yau, K. K. W., Hui, Y. V., and Binns, C. W. (2017). Consumption of dietary supplements by Chinese women during pregnancy and postpartum: A prospective cohort study. Matern. Child. Nutr. 13 (4), e12435. doi:10.1111/mcn.12435
Wang, J., Yang, F., Mao, M., Liu, D. H., Yang, H. M., and Yang, S. F. (2010). High prevalence of vitamin D and calcium deficiency among pregnant women and their newborns in Chengdu, China. World J. Pediatr. 6 (3), 265–267. doi:10.1007/s12519-010-0224-x
Wang, S. S., Lay, S., Yu, H. N., and Shen, S. R. (2016). Dietary guidelines for Chinese residents (2016): Comments and comparisons. J. Zhejiang Univ. Sci. B 17 (9), 649–656. doi:10.1631/jzus.B1600341
Wiradnyani, L. A., Khusun, H., Achadi, E. L., Ocviyanti, D., and Shankar, A. H. (2016). Role of family support and women's knowledge on pregnancy-related risks in adherence to maternal iron-folic acid supplementation in Indonesia. Public Health Nutr. 19 (15), 2818–2828. doi:10.1017/S1368980016001002
Wu, G., Imhoff-Kunsch, B., and Girard, A. W. (2012). Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatr. Perinat. Epidemiol. 26 (1), 4–26. doi:10.1111/j.1365-3016.2012.01291.x
Xiao, S. Y. (1994). The theoretical basis and research application of "Social Support Rating Scale. J. Clin. Psychiatry, 98–100. (In Chinese).
Yang, C., Jing, W., Ge, S., and Sun, W. (2021). Vitamin D status and vitamin D deficiency risk factors among pregnancy of Shanghai in China. BMC Pregnancy Childbirth 21 (1), 431. doi:10.1186/s12884-021-03889-0
Keywords: dietary supplements, nutrition, folic acid, iron, calcium, pregnant women
Citation: Liu Y, Guo N, Feng H and Jiang H (2023) The prevalence of trimester-specific dietary supplements and associated factors during pregnancy: An observational study. Front. Pharmacol. 14:1135736. doi: 10.3389/fphar.2023.1135736
Received: 01 January 2023; Accepted: 20 March 2023;
Published: 06 April 2023.
Edited by:
Giada Crescioli, University of Florence, ItalyReviewed by:
Maryam Rangchian, Hamadan University of Medical Sciences, IranCopyright © 2023 Liu, Guo, Feng and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Jiang, amlhbmdodWl0ZXN0QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.