- 1Department of Oncology, Beijing You An Hospital, Capital Medical University, Beijing, China
- 2Department of Hepatology, Beijing You An Hospital, Capital Medical University, Beijing, China
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) is an effective way to improve portal hypertension, however, the role of anticoagulation or antiplatelet therapy following TIPS remains controversial. We conducted this study to evaluate the efficacy and safety of anticoagulation or antiplatelet therapy following TIPS.
Methods: A literature search was conducted on anticoagulation or antiplatelet therapy after TIPS using Pubmed, Web of Science, EMBASE, and Cochrane. The retrieval period was from the earliest accessible date in the database to 31 October 2022. We collected information on the incidence of stent dysfunction, bleeding, hepatic encephalopathy, the new occurrence of portal vein thrombosis, and the survival rate. Stata was analyzed in RevMan.
Results: 1. Four studies received anticoagulation or antiplatelet therapy after TIPS without control groups. According to the single-group rate meta-analysis, stent dysfunction occurred at 27% [95% CI (0.19, 0.38)], bleeding occurred at 21% [95% CI (0.14, 0.29)], new portal vein thrombosis occurred at 17% [(95%CI(0.04.0.71)], hepatic encephalopathy occurred at 47% [95%CI (0.34, 0.63)], and death occurred at 31% [95% CI (0.22, 0.42)]. 2. Eight studies, including 1025 patients, compared anticoagulation and antiplatelet therapy after TIPS to TIPS alone. In terms of stent dysfunction, bleeding, and hepatic encephalopathy, there were no significant differences between the two groups. The use of anticoagulation or antiplatelet therapy may result in a significant decrease in the incidence of new portal vein thrombosis and mortality over 1 year.
Discussion: Anticoagulant or antiplatelet therapy may not improve the patency rate of TIPS, but may effectively prevent new portal vein thrombosis after TIPS. Following TIPS, the use of anticoagulants or antiplatelet drugs does not lead to an increase in bleeding or death.
Introduction
Portal hypertension is a clinical syndrome characterized by gastrointestinal hemorrhage and refractory ascites resulting from an increase in pressure within the portal vein system. Liver cirrhosis is one of the most common causes of portal hypertension. Transjugular intrahepatic portosystemic shunt (TIPS) can be performed (Sankar and Moore, 2017) to mitigate portal hypertension and reduce the occurrence of the above adverse events. As the operation will damage blood vessels and liver tissues, and the stent is implanted as a foreign body, there is a risk of stent stenosis, blockage, and thrombosis in the stent (Cura et al., 2008). After stent implantation, patients with coronary heart disease require anticoagulation and antiplatelet treatment to prevent thrombosis in the stent (Shang et al., 2019). However, it remains controversial whether anticoagulation or antiplatelet treatment after TIPS may also reduce postoperative complications. Due to the fragile balance between the coagulation and anticoagulation systems of liver cirrhosis patients (Lisman et al., 2021), as well as the risk of bleeding, there have been few studies on anticoagulation or antiplatelet treatment after TIPS. At present, there is no clear consensus regarding whether anticoagulation or antiplatelet treatment is needed after TIPS (Boyer et al., 2010), and only limited studies have been conducted in this area. Therefore, we aimed to conduct a meta-analysis of existing studies to evaluate the efficacy and safety of anticoagulation or antiplatelet therapy after TIPS and provide a reference for clinical treatment.
Materials and methods
Search strategy: With free words and subject words, we searched Pubmed, Web of Science, EMBASE, and Cochrane. Medical Subject Headings included “liver cirrhosis”, “hypertension, portal”, “portasystemic shunt, transjugular intrahepatic”, “anticoagulants” and “platelet aggregation inhibitors”. In the entry terms, “hepatic cirrhosis”, “portal hypertension”, “TIPS”, “anticoagulation agents”, “antiplatelet agents”, and so on were included. Except for “anticoagulants” and “platelet aggregation inhibitors” which were combined with Boolean logic symbols “OR”, all other search terms were combined with Boolean logic symbols “AND”. Data were retrieved from the earliest accessible date in the database until 31 October 2022. References were also screened. A manual search was conducted in addition to the electronic search to identify additional studies that were not found through the electronic search.
Inclusion criteria: A cohort of patients with liver cirrhosis and portal hypertension was included in the study. Study findings included at least one aspect of the following information regarding the use of anticoagulant or antiplatelet drugs after TIPS: stent dysfunction (stenosis, occlusion), new portal vein thrombosis, bleeding, hepatic encephalopathy, and death.
Exclusion criteria: Repetitive literatures, case reports, letters, reviews, and meta-analyses were excluded.
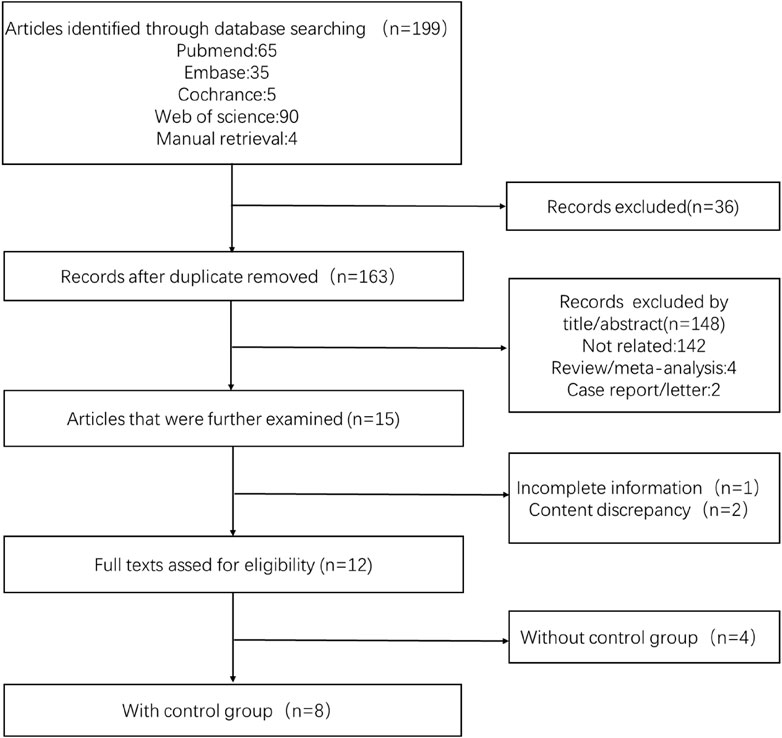
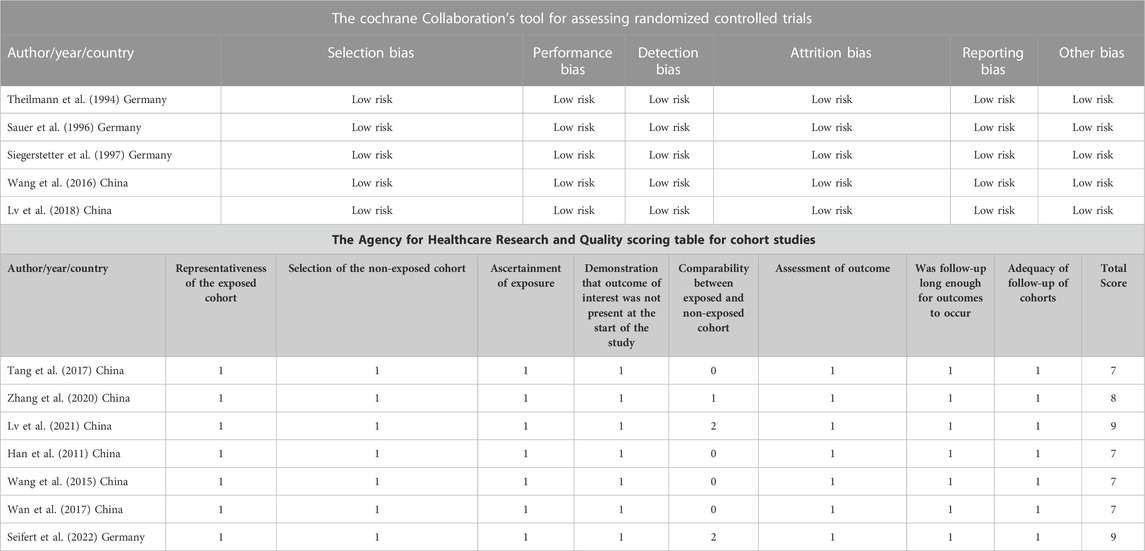
Literature screening and quality evaluation: We selected the literature that met the standards based on screening the titles and abstracts by two independent evaluators (Xiaotong Xu and Yunlai Fu). A quality evaluation table was used to evaluate the quality of the literature. In the randomized controlled study, the Cochrane risk bias evaluation tool was used, while in the observational study, the Agency for Healthcare Research and Quality (AHRQ) scoring table was utilized. For the ambiguous part, we would resolve it through discussion with a third evaluator. The process of filtering was illustrated in Figure 1. The information regarding the article’s quality evaluation was presented in Table 1.
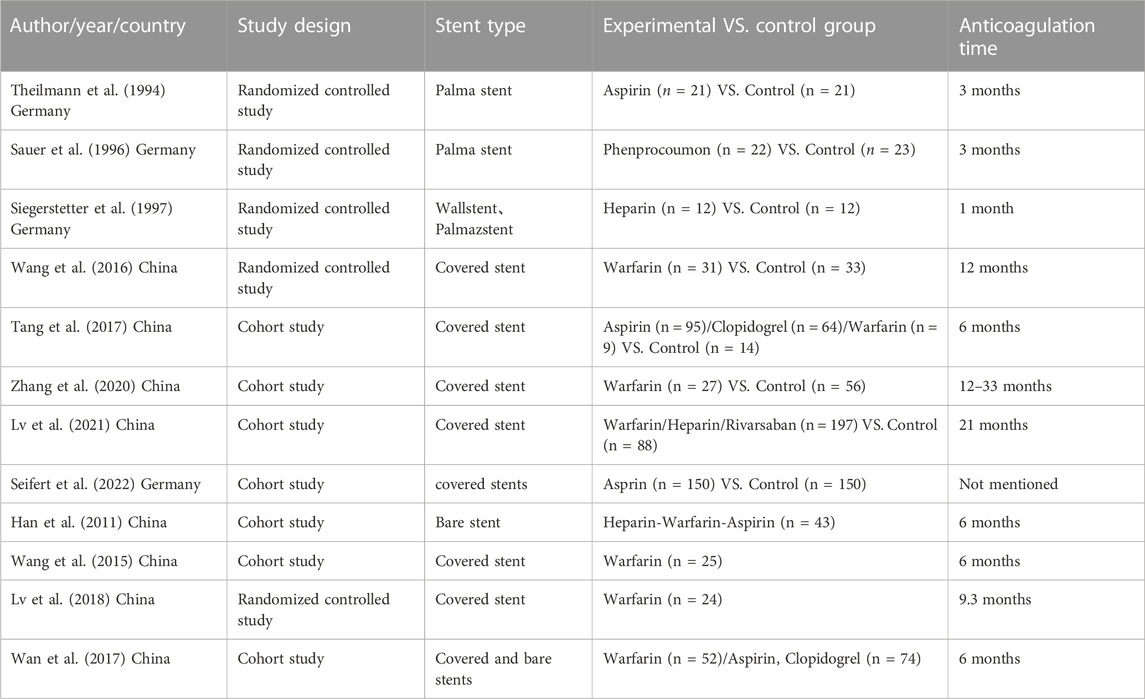
Data extraction and statistical analysis: The following data was collected from the literature that met the inclusion and exclusion criteria: author, country, year, research type, the incidence of stent dysfunction, new portal vein thrombosis (PVT), hemorrhage, and hepatic encephalopathy (HE). After TIPS, the experimental group received anticoagulation or antiplatelet therapy, whereas the control group was not given anticoagulation or antiplatelet therapy. Considering the limited literature retrieved, we performed a single-group rate meta-analysis of the literature that does not include a control group. The collected data were analyzed in RevMan software, and the random effect model was selected.
Results
Initially, 199 articles were searched in the database. A total of 12 articles were evaluated after screening. Finally, eight articles including 1025 patients were analyzed, of which 628 patients received anticoagulation or antiplatelet therapy after TIPS, while 397 patients received TIPS only. In addition, four of the studies included only the anticoagulation or antiplatelet treatment group following TIPS without a control group. Since there was a limited amount of related research, a single-group rate meta-analysis was conducted. Therefore, the results mainly included two aspects. The basic characteristics of the included articles were shown in Table 2. This analysis focused on stent function, bleeding, new occurrence of PVT, HE, and survival after TIPS.
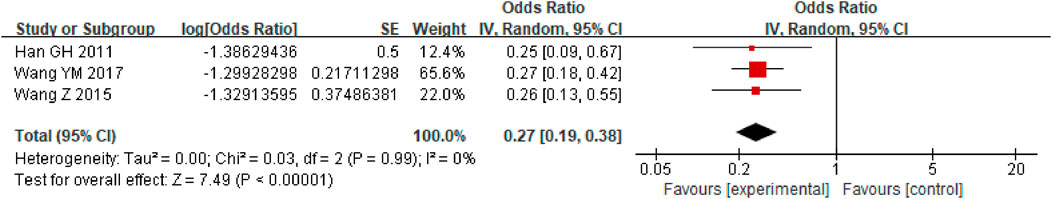
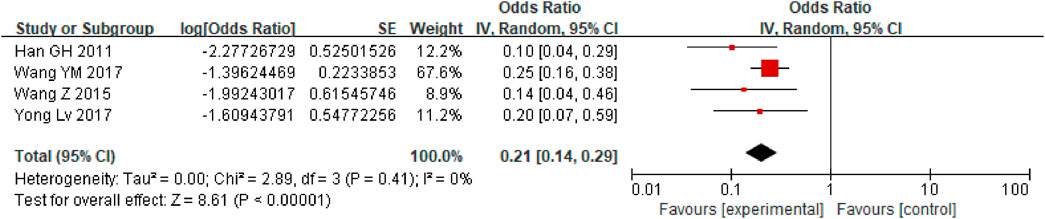
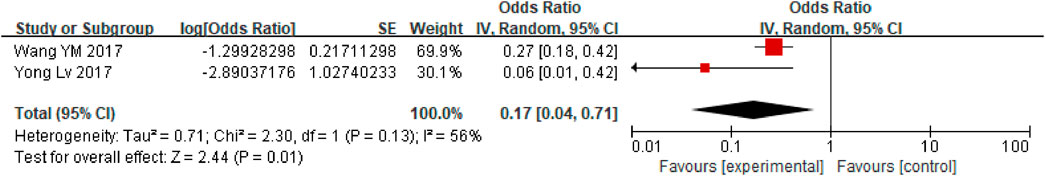
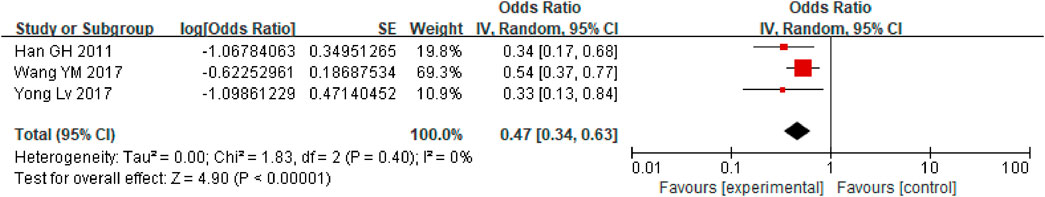
First, a single-group rate meta-analysis of four studies was conducted in which only patients receiving anticoagulation or antiplatelet therapy after TIPS were included. The analysis was conducted based on the incidence of stent dysfunction, new occurrence of PVT, hemorrhage, HE, and death. Specifically, as shown in Figure 2, the results showed a 27% incidence of stent dysfunction [95% CI (0.19, 0.38)] in patients receiving anticoagulation or antiplatelet therapy following TIPS. The incidence of bleeding, new occurrence of PVT, HE, and death was 21% [95% CI(0.14, 0.29)], 17% [95% CI (0.04, 0.71)], 47% [95% CI (0.34, 0.63)], 31% [95% CI (0.22, 0.42)] respectively, as shown in Figures 3–6.
Moreover, eight studies were analyzed to compare the differences in stent dysfunction, bleeding, new occurrence of PVT, HE, and death between patients who received anticoagulation or antiplatelet therapy after TIPS, and those who received only TIPS.
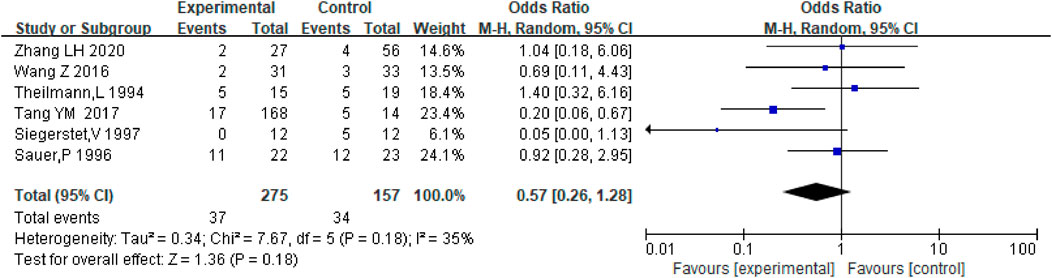
Stent dysfunction
Stent dysfunction includes stent stenosis and occlusion. Six studies including the data on stent dysfunction in patients receiving anticoagulation or antiplatelet therapy after TIPS and TIPS only were analyzed, and there was no significant difference between the two groups with respect to the incidence of stent dysfunction [OR = 0.57.95% CI (0.26–1.28), p = 0.18] as shown in Figure 7. And we analyzed the data of anticoagulation only after TIPS, with the similar results [OR = 0.56.95% CI (0.22–1.46), p = 0.24], as shown in Supplementary Figure S1. Considering the different types of stents and PVT, we further conducted subgroup analysis, as shown in Supplementary Figure S2–S4.
Hemorrhage
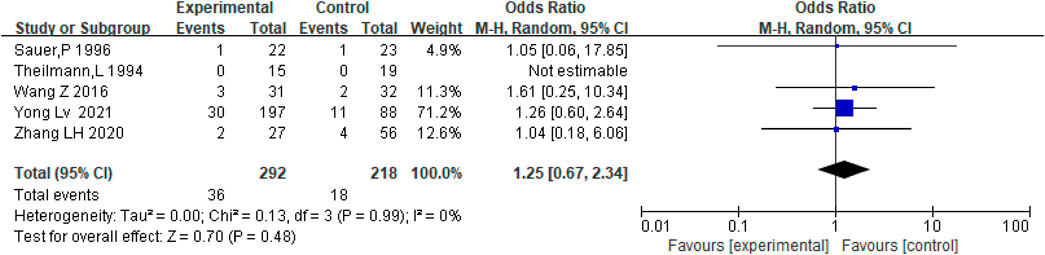
Hemorrhage mainly refers to major bleeding events, including gastrointestinal bleeding, intracranial hemorrhage, and hematuria. There were five studies, including the data on bleeding in patients who received anticoagulation or antiplatelet therapy after TIPS and TIPS only. Results show that there was no significant difference between the two groups regarding bleeding rates [OR = 1.25, 95% CI (0.67–2.34), p = 0.48], as shown in Figure 8. Considering the different types of stents, we conducted subgroup analysis, as shown in Supplementary Figure S5–S6.
New occurrence of portal vein thrombosis
Anticoagulation or antiplatelet therapy after TIPS can significantly reduce the incidence of PVT [OR = 0.39.95% CI (0.17–0.91), p = 0.03] compared with patients who only underwent TIPS, as shown in Figure 9. The stents were all covered stents. Then, we further conducted subgroup analysis based on whether the subjects had PVT in the past, as shown in Supplementary Figure S7–S8.
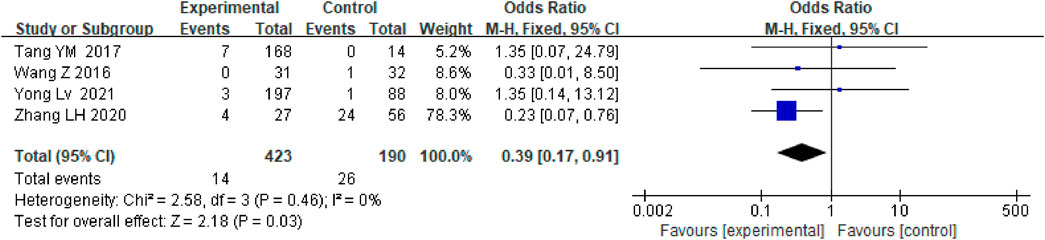
FIGURE 9. Effect of anticoagulation or antiplatelet treatment on new portal vein thrombosis after TIPS.
Hepatic encephalopathy
The incidence of HE did not differ significantly between patients who received anticoagulation and antiplatelet therapy after TIPS and those who only received TIPS [OR = 1.10.95% CI (0.71–1.71), p = 0.68], as shown in Figure 10.
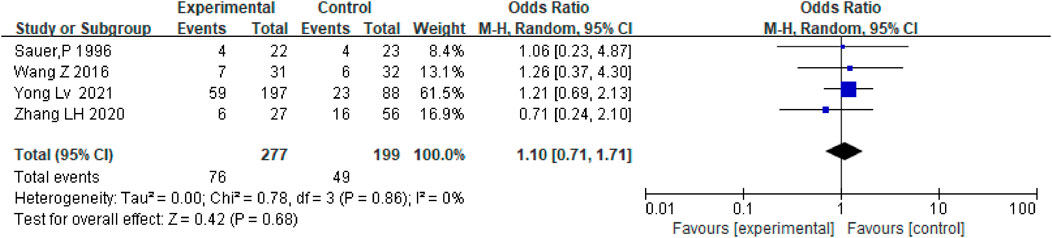
FIGURE 10. Effect of anticoagulation or antiplatelet treatment on hepatic encephalopathy after TIPS.
Occurrence of death
Depending on the follow-up time, the data were analyzed for 3 months, 1 year, and 3 years. There was no difference in mortality between the two groups at 3 months (OR = 0.70.95%CI (0.07–6.59), p = 0.75) and 3 years [OR = 0.79.95%CI (0.45.1.39), p = 0.42], but anticoagulation or antiplatelet therapy after TIPS reduced mortality at 1 year [OR = 0.55.95%CI (0.34.0.89), p = 0.02], as shown in Figures 11–13.
Discussion
In order to understand the incidence of stent dysfunction, bleeding and other events during anticoagulation or antiplatelet therapy after TIPS, we first conducted a single-group rate meta-analysis of four articles without control. In previous studies (Luca et al., 2011), dysfunction of bare stents in 1 year after TIPS was approximately 38% and that of covered stents was approximately 21%. In our study, anticoagulation or antiplatelet therapy after TIPS, there were approximately 27% of patients with stent dysfunction, 21% with bleeding,17% with new PVT,47% with HE and 31% death. It was concluded that the preventive use of anticoagulant or antiplatelet drugs after TIPS has limited effect on the reduction of stent dysfunction in patients undergoing TIPS.
Although TIPS is an effective treatment for portal hypertension, some complications may occur such as stent dysfunction (de Franchis and Baveno, 2015; Boike et al., 2022). The prognosis and survival may be affected by these adverse events (Dissegna et al., 2019). Based on the time of occurrence, stenosis after TIPS can be divided into early, middle, and late stages. An early stent stenosis occlusion is primarily caused by thrombotic stenosis. In the middle and long term, stent stenosis is mainly caused by excessive hyperplasia of pseudointima (Liu et al., 2021). Theoretically, postoperative anticoagulation or antiplatelet therapy can inhibit platelet aggregation and change the coagulation state, which is related not only to patients with PVT before TIPS (Dong et al., 2021), but also to the occurrence of possible stent stenosis or blockage after TIPS.
The evaluation of safety and effectiveness mainly included five aspects: bleeding, the new occurrence of PVT, HE, stent dysfunction, and survival. In our study, anticoagulation or antiplatelet therapy after TIPS did not reduce the incidence of stent dysfunction. In previous studies, bare stents were mostly used, and in current studies, covered stents are mostly recommended (de Franchis et al., 2022). Then we conducted subgroup analysis according to different stents. The result of our study was that whether using bare stents or covered stents, postoperative anticoagulation or antiplatelet therapy did not significantly reduce the incidence of stent dysfunction. The anticoagulant or antiplatelet drugs used in the study were inconsistent, but no further subgroup analysis was totally carried out due to the limited number of studies. We analyzed two articles of covered stents that only used warfarin, and the results were similar. There was no significant difference between the experiment group and the control group.
However, some studies have shown (Tang et al., 2017)that anticoagulation or antiplatelet therapy after TIPS can reduce the occurrence of stent dysfunction. According to Xia YF (Yifu et al., 2022), continuous anticoagulation after TIPS can effectively prevent stent stenosis or blockage within 30 days for patients with partial PVT before TIPS, but between 180 days and 90 days there was no significant difference. In patients with patency, spongiform change, or complete occlusion of the PVT, anticoagulation after TIPS had no significant impact on stenosis or occlusion of the stent. It should be noted that the study object was cirrhosis with PVT, so patients may be relatively hypercoagulable, and the use of anticoagulants reduced stent stenosis or obstruction. We tried to conduct a subgroup analysis based on whether there was PVT in the past and found that anticoagulation or antiplatelet therapy was ineffective in preventing the occurrence of stent dysfunction after TIPS.
In the past, TIPS was contraindicated for patients with PVT, but it is now being increasingly applied to cirrhosis patients with PVT. Researchers found that TIPS was as safe as anticoagulation and could reduce the load of PVT (Zhan et al., 2021). According to our research findings, the use of anticoagulation and antiplatelet therapy can prevent the occurrence of new PVT after TIPS. Following this, we conducted a subgroup analysis based on whether PVT had occurred in the past. Results showed that it could reduce the incidence of new PVT in patients without previous PVT. Therefore, it was effective for the de novo PVT, but not for the recurrence of PVT in patients with previous PVT. And Yong Lv (Lv et al., 2021) found that administration with Heparin or Rivalsaban after TIPS were associated with higher the probability of PVT recanalization, reduced thrombosis risk, improved survival rates. Angelo Luca (Wang et al., 2016) maintained that TIPS itself assisted in the recanalization of the PVT in patients with PVT by improving the flow of blood following the procedure, even in patients who are not prescribed anticoagulants or antiplatelet medications.
Anticoagulation or antiplatelet therapy after TIPS did not increase the risk of bleeding and HE, and the results were similar in subgroup analysis based on the different stents. Because almost all the included studies used warfarin, no further subgroup analysis was conducted.
In terms of survival, we found that anticoagulation or antiplatelet therapy after TIPS can reduce the 1-year mortality, but it did not significantly reduce the mortality of 3 months and 3 years after TIPS. The long-term effect of anticoagulation on the survival of TIPS still needs further study with large samples and randomized trial designs to draw firm conclusions.
According to a Germany survey on anticoagulant treatment following TIPS (Steib et al., 2020), 43 hospitals were included, four of which had not used an anticoagulant and eight of which had used both Aspirin and Clopidogrel. It is common for hospitals to use low-molecular-weight heparin for several days to 1 month. Due to the lack of clear guidelines, there are great differences in anticoagulation, antiplatelet therapy, and drug selection after TIPS (Fagiuoli et al., 2017; Rajesh et al., 2020). As there are few large-scale studies in this area and a limited amount of literature has been retrieved, further research is needed to evaluate the effectiveness of anticoagulation and antiplatelet therapy after TIPS.
Several systematic reviews or meta-analysis focusing on anticoagulation treatment after TIPS have been published recently. In the Guo et al. (2022) article, they only analyzed the incidence of bleeding based on the different anticoagulation percentages. But in our study, instead of analyzing the incidence of bleeding, we also compared the new occurrence of PVT, stent dysfunction, HE, and survival. Our research results were consistent with Jiao et al. (2022). Anticoagulation after TIPS can prevent the incidence of new occurrence of PVT. And we updated the included articles.
Some potential limitations of this study should be acknowledged. First, the number of relevant literatures retrieved was limited, and although the subjects included in the study were all patients with liver cirrhosis, some of them were accompanied by PVT, and the timing of thrombosis and the specific degree of blockage were not clear. Furthermore, the therapy option of anticoagulant and antiplatelet drugs were not consistent between different studies, which might also have a potential effect on final results. And current recommendations discourage (European Association for the Study of the Liver, 2022) the use of Vitamin-K-antagonists in patients with cirrhosis due to the unreliable results of coagulation monitoring. However, due to limited data, we cannot conduct subgroup analysis based on different anticoagulant drugs. Therefore, studies with more patients and longer follow-up time based on different anticoagulant or antiplatelet drugs should be carried out.
Conclusion
Although anticoagulation or antiplatelet therapy after TIPS may not improve the short-term shunt patency rate, it may effectively prevent the formation of new portal vein thrombosis and decreased 1-year mortality. In terms of safety, the use of anticoagulants and antiplatelet drugs after surgery will not increase the incidence of bleeding and death.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
XX, YF, MJ, and MW contributed to the literature database search, data collection, data extraction. XX contributed to the data analysis, and writing of the manuscript. The topic was conceptualized by QM and XX. Language proofread by JW.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1116177/full#supplementary-material
References
Boike, J. R., Thornburg, B. G., Asrani, S. K., Fallon, M. B., Fortune, B. E., Izzy, M. J., et al. (2022). North American practice-based recommendations for transjugular intrahepatic portosystemic shunts in portal hypertension. Clin. Gastroenterol. Hepatol. 20 (8), 1636–1662.e36. doi:10.1016/j.cgh.2021.07.018
Boyer, T. D., and Haskal, Z. J.American Association for the Study of Liver Diseases (2010). The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: Update 2009. Hepatology 51 (1), 306. doi:10.1002/hep.23383
Cura, M., Cura, A., Suri, R., El-Merhi, F., Lopera, J., and Kroma, G. (2008). Causes of TIPS dysfunction. AJR Am. J. Roentgenol. 191 (6), 1751–1757. doi:10.2214/ajr.07.3534
de Franchis, R., Bosch, J., Garcia-Tsao, G., Reiberger, T., and Ripoll, C.Baveno VII Faculty (2022). Baveno VII—renewing consensus in portal hypertension. J. Hepatol. 76 (4), 959–974. doi:10.1016/j.jhep.2021.12.022
de Franchis, R., and Baveno, F. (2015). Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J. Hepatol. 63 (3), 743–752. doi:10.1016/j.jhep.2015.05.022
Dissegna, D., Sponza, M., Falleti, E., Fabris, C., Vit, A., Angeli, P., et al. (2019). Morbidity and mortality after transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis. Eur. J. Gastroenterol. Hepatol. 31 (5), 626–632. doi:10.1097/meg.0000000000001342
Dong, S., Qi, H., Li, Y., Men, P., Alifu, M., Zhang, Y., et al. (2021). A systematic review and meta-analysis of anticoagulation therapy for portal vein thrombosis in patients with cirrhosis: To treat or not to treat? Hepatol. Int. 15 (6), 1356–1375. doi:10.1007/s12072-021-10233-3
European Association for the Study of the Liver (2022). EASL Clinical Practice Guidelines on prevention and management of bleeding and thrombosis in patients with cirrhosis. J. Hepatol. 76 (5), 1151–1184. doi:10.1016/j.jhep.202109.003
Fagiuoli, S., Bruno, R., Debernardi Venon, W., Schepis, F., Vizzutti, F., Toniutto, P., et al. (2017). Consensus conference on TIPS management: Techniques, indications, contraindications. Dig. Liver Dis. 49 (2), 121–137. doi:10.1016/j.dld.2016.10.011
Guo, D. F., Fan, L. W., Le, Q., and Huang, C. B. (2022). Transjugular intrahepatic portosystemic shunt for the prevention of rebleeding in patients with cirrhosis and portal vein thrombosis: Systematic review and meta-analysis. Front. Pharmacol. 13, 968988. doi:10.3389/fphar.2022.968988
Han, G., Qi, X., He, C., Yin, Z., Wang, J., Xia, J., et al. (2011). Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J. Hepatol. 54 (1), 78–88. doi:10.1016/j.jhep.2010.06.029
Jiao, P., Chen, X-Y., Zheng, H-Y., Qin, J., Li, C., and Zhang, X. L. (2022). Anticoagulation after transjugular intrahepatic portosystemic shunt for portal hypertension: A systematic review and meta analysis. Med. Baltim. 101 (26), e29742. doi:10.1097/md.0000000000029742
Lisman, T., Hernandez-Gea, V., Magnusson, M., Roberts, L., Stanworth, S., Thachil, J., et al. (2021). The concept of rebalanced hemostasis in patients with liver disease: Communication from the ISTH SSC working group on hemostatic management of patients with liver disease. J. Thromb. Haemost. 19 (4), 1116–1122. doi:10.1111/jth.15239
Liu, J., Meng, J., Zhou, C., Shi, Q., Yang, C., Ma, J., et al. (2021). A new choice of stent for transjugular intrahepatic portosystemic shunt creation: Viabahn ePTFE covered stent/bare metal stent combination. J. Interv. Med. 4 (1), 32–38. doi:10.1016/j.jimed.2020.10.003
Luca, A., Miraglia, R., Caruso, S., Milazzo, M., Sapere, C., Maruzzelli, L., et al. (2011). Short- and long-term effects of the transjugular intrahepatic portosystemic shunt on portal vein thrombosis in patients with cirrhosis. Gut 60 (6), 846–852. doi:10.1136/gut.2010.228023
Lv, Y., Bai, W., Li, K., Wang, Z., Guo, W., Luo, B., et al. (2021). Anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis: A prospective observational study. Am. J. Gastroenterol. 116 (7), 1447–1464. doi:10.14309/ajg.0000000000001194
Lv, Y., Qi, X., He, C., Wang, Z., Yin, Z., Niu, J., et al. (2018). Covered TIPS versus endoscopic band ligation plus propranolol for the prevention of variceal rebleeding in cirrhotic patients with portal vein thrombosis: A randomised controlled trial. Gut 67 (12), 2156–2168. doi:10.1136/gutjnl-2017-314634
Rajesh, S., George, T., Philips, C. A., Ahamed, R., Kumbar, S., Mohan, N., et al. (2020). Transjugular intrahepatic portosystemic shunt in cirrhosis: An exhaustive critical update. World J. Gastroenterol. 26 (37), 5561–5596. doi:10.3748/wjg.v26.i37.5561
Sankar, K., and Moore, C. M. (2017). Transjugular intrahepatic portosystemic shunts. Jama 317 (8), 880. doi:10.1001/jama.2016.20899
Sauer, P., Theilmann, L., Herrmann, S., Bruckner, T., Roeren, T., Richter, G., et al. (1996). Phenprocoumon for prevention of shunt occlusion after transjugular intrahepatic portosystemic stent shunt: A randomized trial. Hepatology 24 (6), 1433–1436. doi:10.1002/hep.510240622
Seifert, L. L., Schindler, P., Sturm, L., Gu, W., Seifert, Q. E., Weller, J. F., et al. (2022). Aspirin improves transplant-free survival after TIPS implantation in patients with refractory ascites: A retrospective multicentre cohort study. Hepatol. Int. 16 (3), 658–668. doi:10.1007/s12072-022-10330-x
Shang, P., Liu, G. G., Zheng, X., Ho, P. M., Hu, S., Li, J., et al. (2019). Association between medication adherence and 1-year major cardiovascular adverse events after acute myocardial infarction in China. J. Am. Heart Assoc. 8 (9), e011793. doi:10.1161/jaha.118.011793
Siegerstetter, V., Krause, T., Rössle, M., Haag, K., Ochs, A., Hauenstein, K. H., et al. (1997). Transjugular intrahepatic portosystemic shunt (TIPS). Thrombogenicity in stents and its effect on shunt patency. Acta Radiol. 38 (1), 558–564. doi:10.1080/02841859709174387
Steib, C. J., Li, H., Zhang, J., Mayerle, J., Ricke, J., Gerbes, A. L., et al. (2020). Transjugular intrahepatic portosystemic shunt for patients with liver cirrhosis: Survey evaluating indications, standardization of procedures and anticoagulation in 43 German hospitals. Eur. J. Gastroenterol. Hepatol. 32 (9), 1179–1185. doi:10.1097/meg.0000000000001628
Tang, Y., Zheng, S., Yang, J., Bao, W., Yang, L., Li, Y., et al. (2017). Use of concomitant variceal embolization and prophylactic antiplatelet/anticoagulative in transjugular intrahepatic portosystemic shunting: A retrospective study of 182 cirrhotic portal hypertension patients. Med. Baltim. 96 (49), e8678. doi:10.1097/md.0000000000008678
Theilmann, L., Sauer, P., Roeren, T., Otto, G., Arnold, J. C., Noeldge, G., et al. (1994). Acetylsalicylic-acid in the prevention of early stenosis and occlusion of transjugular intrahepatic portal-systemic stent shunts - a controlled-study. Hepatology 20 (3), 592–597. doi:10.1002/hep.1840200307
Wan, Y-M., Li, Y-H., Wu, H-M., Xu, Z. Y., Xu, Y., Yang, L. H., et al. (2017). Portal vein thrombosis before and after transjugular intrahepatic portosystemic shunt placement: An observational study (STROBE compliant). Med. Baltim. 96 (45), e8498. doi:10.1097/md.0000000000008498
Wang, Z., Jiang, M-S., Zhang, H-L., Weng, N. N., Luo, X. F., Li, X., et al. (2016). Is post-TIPS anticoagulation therapy necessary in patients with cirrhosis and portal vein thrombosis? A randomized controlled trial. Radiology 279 (3), 943–951. doi:10.1148/radiol.2015150369
Wang, Z., Zhao, H., Wang, X., Zhang, H., Jiang, M., Tsauo, J., et al. (2015). Clinical outcome comparison between TIPS and EBL in patients with cirrhosis and portal vein thrombosis. Abdom. Imaging 40 (6), 1813–1820. doi:10.1007/s00261-014-0320-9
Yifu, X., Lijun, S., and Guangchuan, W. (2022). Analysis of the necessity of anticoagulation therapy and influencing factors of stent occlusion after transjugular intrahepatic portosystemic shunt. Chin. J. Hepatology 2022 (07), 728–734. doi:10.3760/cma.j.cn501113-20210106-00010
Zhan, C., Prabhu, V., Kang, S. K., Zhu, Y., Kim, S., et al. (2021). Comparison of non-tumoral portal vein thrombosis management in cirrhotic patients: TIPS versus anticoagulation versus No treatment. J. Clin. Med. 10 (11), 2316. doi:10.3390/jcm10112316
Keywords: liver cirrhosis, hypertension, portal, portasystemic shunt, transjugular intrahepatic anticoagulants, platelet aggregation inhibitors
Citation: Xu X, Fu Y, Jiang M, Wu M, Wu J and Meng Q (2023) The effects and safety of anticoagulation or antiplatelet therapy following TIPS in cirrhotic patients with portal hypertension: A meta-analysis. Front. Pharmacol. 14:1116177. doi: 10.3389/fphar.2023.1116177
Received: 06 December 2022; Accepted: 24 January 2023;
Published: 20 February 2023.
Edited by:
Domenico Criscuolo, Italian Society of Pharmaceutical Medicine, ItalyReviewed by:
Andreas Benesic, Krankenhaus GmbH Weilheim—Schongau, GermanyXin Long, Huazhong University of Science and Technology, China
Copyright © 2023 Xu, Fu, Jiang, Wu, Wu and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qinghua Meng, bWVuZ19xaDA4MDVAY2NtdS5lZHUuY24=
 Xiaotong Xu1
Xiaotong Xu1 Minjie Jiang
Minjie Jiang Qinghua Meng
Qinghua Meng