- 1School of Management, Hubei University of Chinese Medicine, Wuhan, Hubei, China
- 2Research Center for the Development of Traditional Chinese Medicine, Key Research Institute of Humanities and Social Sciences of Hubei Province, Wuhan, China
- 3School of Medicine and Health Management, Tongji Medical School, Huazhong University of Science and Technology, Wuhan, Hubei, China
- 4School of Psychology and Public Health, La Trobe University, Melbourne, VIC, Australia
- 5School of Health Policy and Management, Nanjing Medical University, Nanjing, China
Background: Public reporting on health providers’ performance (PRHPP) is increasingly used for empowering patients. This study aimed to test the effect of PRHPP using the theory of the consumer choice model.
Methods: The study was conducted in 10 primary care institutions in Hubei province, China. Information related to the percentage of prescriptions requiring antibiotics, the percentage of prescriptions requiring injections, and average costs per prescription for each prescriber was calculated, ranked and displayed in a public place on a monthly basis. A questionnaire survey was undertaken on 302 patients 10 months after the initiation of the PRHPP, tapping into patient awareness, understanding, perceived value and use of the information in line with the theory of the consumer choice model. The fitness of data with the model was tested using structural equation modelling. The patients who were aware of the PRHPP were compared with those who were unaware of the PRHPP. The propensity score method (considering differences between the two groups of patients in age, gender, education, health and income) was used for estimating the effects of the PRHPP.
Results: About 22% of respondents were aware of the PRHPP. Overall, the patients showed limited understanding, perceived value and use of the disclosed information. The data fit well into the consumer choice model. Awareness of the PRHPP was found to be associated with increased understanding of the antibiotic (p = 0.028) and injection prescribing indictors (p = 0.030). However, no significant differences in perceived value and use of the information (p > 0.097) were found between those who were aware and those who were unaware of the PRHPP.
Conclusion: Although PRHPP may improve patient understanding of the prescribing performance indicators, its impacts on patient choices are limited due to low levels of perceived value and use of information from patients. Additional support is needed to enable patients to make informed choices using the PRHPP.
1 Introduction
Over the past few decades, public reporting of health providers’ performance (PRHPP) has been increasingly used for the purpose of improving the quality of patient care (Marshall et al., 2000). It started in the United States in the 1980s (Hannan et al., 1994) and has since been adopted by many other developed countries (Hibbard et al., 2003; Marshall et al., 2003). PRHPP is considered as an instrument that can improve the quality of care through enhancing transparency and accountability (Lansky, 2002; Hibbard et al., 2003; Fung et al., 2008). It is expected that patients use the information to choose healthcare providers, which would force healthcare providers to improve their underperforming areas in order to maintain their market share (Berwick et al., 2003; Asch et al., 2006; Fung et al., 2008).
Empirical studies showed that patients are interested in information related to quality of care (Longo and Everet, 2003; Boscarino and Adams, 2004; Cheng and Song, 2004; Sofaer et al., 2005), and nearly 50% consider quality as the most important aspect when choosing a healthcare provider (Robinson and Brodie, 1997; Schneider and Epstein, 1998). However, evidence about the association between PRHPP and patient choices has been inconclusive (Faber et al., 2009; Totten et al., 2012).
It is not clear how patients value and use PRHPP (Marshall et al., 2000; Werner and Asch, 2005; Faber et al., 2009). Hibbard and others proposed a theory of the consumer choice model (CCM), which assumes that the impacts of PRHPP take place through four stages in a sequential order (Hibbard et al., 2002). At the first stage, patients become aware of the PRHPP. Gradually, they develop an appropriate understanding of the information involved in the PRHPP (stage two). But before they use PRHPP as an instrument for choosing healthcare providers (stage four), they have to develop an appreciation of the value of PRHPP (stage three). The perceived value of PRHPP is critical and subject to the influences of both personal and environmental factors, such as the characteristics of patients, the interactive dynamic between patients and healthcare providers, and the healthcare system arrangements.
Faber and others, in a systematic review, identified the lack of understanding of the staged effects of PRHPP on patients as a gap in the literature that deserves attention (Faber et al., 2009). Several studies attempted to understand how patients might use PRHPP in simulated environments (Hibbard et al., 1996; Hibbard et al., 2000; Hibbard et al., 2001a; Uhrig et al., 2006; Peters et al., 2007). A few researchers observed how healthy consumers chose a new health plan using reported performance information on various plans (Knutson et al., 1998; Farley et al., 2002a; Farley et al., 2002b; Hibbard et al., 2002). But there is a paucity in the literature documenting how patients choose a provider when they are ill. In addition, all of the existing studies have been conducted in the USA (Faber et al., 2009). Little is known about the effects of PRHPP in other countries, especially in developing countries.
In this study, we applied the propensity score method (PSM) to estimate the effects of PRHPP on patient changes in line with the CCM theory in Hubei province, China. PSM has been increasingly used in health services research (Austin, 2008), which allows us to estimate causal effects based on cross-sectional data (Caliendo and Kopeinig, 2008).
2 Materials and methods
This study was undertaken in 10 primary care institutions in Qianjiang city in China’s Hubei province. A cross-sectional questionnaire survey was conducted on patients who visited the participating institutions, 10 months after PRHPP interventions were introduced.
2.1 Study setting
Qianjiang is situated in central Hubei of China, with a population of 0.95 million. Its economic development ranks in the middle range of all cities in Hubei. On average, about 500,000 outpatient visits were recorded per year in Qianjiang. At the time of the study, there was no restriction imposed by the social health insurance programs on patient choices of providers, either at the institutional level or at the individual physician level.
More than 50% of prescriptions prescribed in primary care institutions in Hubei contained antibiotics or injections (Liu et al., 2015; Liu et al., 2016), much higher than the levels recommended by the World Health Organisation (≤30% for antibiotics; ≤24% for injections) (Li, 2014). In November 2013, the Qianjiang health authority introduced a PRHPP program in 10 primary care institutions (the participating institutions of this study), with an aim to curb over-prescriptions. The information released to the public was selected based on the WHO indicators in relation to the rational use of medicines: percentage of prescriptions requiring antibiotics; percentage of prescriptions requiring injections; and average expenditure of medicines per prescription (Laing et al., 1993). The three indicators were calculated and ranked at the individual physician and institutional levels.
They were printed out and displayed in the entrance hall of each participating primary care institution, along with an explanation about the purpose of the PRHPP. Except the information of the three indicators (percentage of prescriptions requiring antibiotics, percentage of prescriptions requiring injection, and average expenditure of patients), the rankings of the three indictors for each physician were also provided for patients. In addition, adverse effects of irrational use of antibiotics (such as prolonged hospital stay and increased medical expenditure) was also provided for helping consumers understand the information at the footnote of the displayed poster. An example of the displayed poster is provided in the supplementary file. The displayed information was updated on a monthly basis: 49%–71% prescriptions contained antibiotics; 50%–64% prescriptions contained injections; average expenditure per prescription ranged from ¥38 to ¥55 (roughly $5.5–8.0). Details about the design of the PRHPP interventions were published (Du et al., 2015).
2.2 Study instrument
The questionnaire was adapted from Hibbard’s survey instrument (Hibbard et al., 2002). It contained 10 items measuring four domains in line with the CCM theory: awareness, understanding, perceived value and use of information. Patient awareness of PRHPP was captured by one item, asking the respondents whether they had read the PRHHP poster (yes or no). Each of the domains measuring patient understanding, perceived value and use of information contained three items, focusing on antibiotics, injections and costs of prescriptions, respectively. The respondents were asked to rate each item on a five-point Likert scale, with a higher score indicating a more positive response.
The validity of the instrument was tested using exploratory factor analysis (EFA) with varimax rotation, and structural equation modelling (SEM). The EFA produced three factors (excluding the item measuring patient awareness) as expected, with items loading highly and exclusively on their corresponding factors. By testing a model consisting the three latent factors (awareness, understanding, perceived value and use of information) using item parcels as indicators per latent variable, SEM was applied for testing construct validity of the instrument (Keller et al., 1998). The SEM indicated that the CCM had a good fitness with data: RMSEA = 0.051 (<0.08), SRMR = 0.057 (<0.08) and CFI = 0.991 (>0.95) (Hooper et al., 2008).
Data collected for PSM included age, gender, educational attainment, self-rating on health, and income. These variables were selected based on a systematic review (Faber et al., 2009). Self-rating on health was measured using a five-point Likert scale. Annual household average income was estimated with 11 equal intervals ranging from less than 10,000 Yuan (US$1,500) to over 100,000 Yuan (US$15,000). We did not collect diagnostic information because more than half of the respondents completed the questionnaires prior to medical consultations. A translated version of instrument is provided in the supplementary file.
2.3 Sample size
We estimated sample size based on the following formula:
A previous study showed that PRHPP could lead to 0.76 changes in CCM scores (Hibbard et al., 2002). A sample size of 63 (for each group) would enable us to detect a difference (d) of 0.5 in CCM scores (standard deviation σ = 1.0) between those who were aware and those who were unaware of the PRHPP, with a probability of type one error α = 0.05 and statistical power β = 0.8. If 25% of patients became aware of the PRHPP, a minimal of 252 participants would be needed. We increased the sample size to 300.
2.4 Sampling and data collection
Data were collected from the 5th to 8th August 2014, 10 months after the introduction of the PRHPP. Patients who visited the outpatient clinics of the participating primary care institutions were eligible to participate in the survey. About ten or more physicians were made available for patients in the participating primary care institutions at any time of patient visits. For patients younger than 18 years, their parents were surveyed. Adult patients who were unable to read or communicate were excluded from this study.
A systematic sampling strategy was adopted. About 30 questionnaires were collected in each participating primary care institution. It was estimated that about 100 patients visited each outpatient clinic per day. Thus, one in every three patients was invited to participate in the survey. If less than 30 questionnaires were returned in a participating clinic, additional questionnaires were collected the next day.
The questionnaires were administered through face-to-face interviews in the patient waiting areas. Each clinic was attended by two interviewers. Four pairs of postgraduate students were trained to conduct the survey. The returned questionnaires were checked for completeness by XP on the day of the survey.
We planned to distribute 350 questionnaires, and ended up with a final sample size of 302 (86.29%) for data analyses.
2.5 Statistical analysis
The items measuring patient understanding, perceived value and use of information were given a score, ranging from 1 to 5 (with a higher score indicating a more positive response). Shapiro-Francia W′ tests were performed to determine the normality of data distributions. Two-sample independent t tests (for data with normal distributions) or Kruskal–Wallis tests (for data with non-normal distributions) were performed to compare the differences in the scores between the respondents who were aware and those who were unaware of the PRHPP.
We also transformed the scores into dichotomous measurements using a cut-off value: >3 indicating a positive response. Chi-square tests were applied to test the differences between those who were aware and those who were unaware of the PRHPP.
2.5.1 SEM
We established SEM to test the following hypothesis based on the CCM (Hibbard et al., 2002):
• Hypothesis 1: patient awareness of the PRHPP improved their understanding of the prescribing performance information.
• Hypothesis 2: better patient understanding about the prescribing performance information improved their perceived value of the information.
• Hypothesis 3: higher perceived value of the prescribing performance information increased patient use of the information.
In the SEM, patient awareness was treated as an observable variable, while patient understanding, perceived value and use of information were treated as latent variables, each being measured by three observable variables. The standardized structural coefficients were calculated to test the links between those variables.
2.5.2 Effect estimation using PSM
PSM allows researchers to identify matched control groups for estimating the effect size of a certain treatment (such as patient awareness of the PRHPP in this study). It reduces the bias resulting from a lack of distribution overlap between two compared groups, a bias that cannot be detected by regression analyses (Li, 2013). PSM involves three steps: 1) calculating propensity scores based on observational variables that have a significant impact on the estimated results; 2) matching participants in the treatment and control groups based on propensity scores; 3) estimating the effect of treatment based on matched samples.
In this study, propensity scores were calculated using a logistic regression model, considering the distributions of age (elderly/none-elderly), gender (male/female), education (primary school, secondary school, high school, college), self-rated health (good, medium, poor), and family income (<50,000 Yuan or ≥50,000 Yuan) for those who were aware and unware of the PRHPP. These covariates were identified based on a systematic review (Faber et al., 2009). No-replacement one-to-one nearest-neighbor matching was applied to form a matched sample based on the propensity scores. The caliper of matching was set as 0.03 (Austin, 2009). The differences between the paired participants served as the basis for estimating the effects of the PRHPP: average treatment effect (ATE) and average treatment effect on the treated group (ATT) (Li, 2013):
In these formula, E(.) indicates the expectation in the population.
A p-value of <0.05 was considered as significant and all analyses were performed using STATA 12.0.
3 Results
3.1 Demographic characteristics of participants
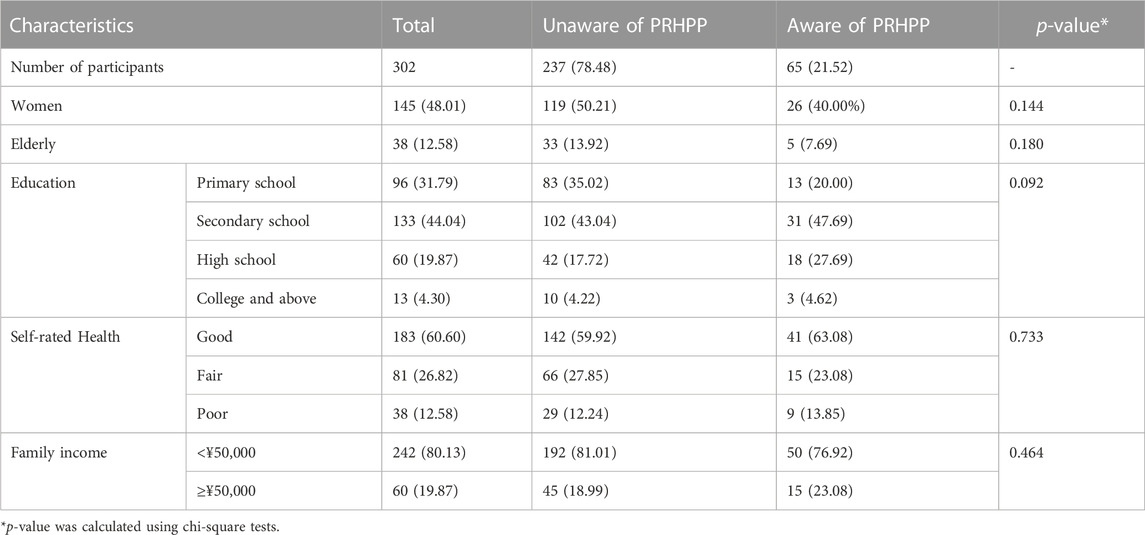
About half (48%) of the respondents were women; less than 13% were 65 years of age or older; over three-quarters completed no more than primary or secondary school; and the majority (80%) had an annual household income under ¥50,000 (US $7264).
Only 21.5% of respondent were aware of the PRHPP. Non-significant differences between those who were aware and those who were unaware of the PRHPP existed in the demographic characteristics (Table 1).
3.2 Findings of SEM
The three hypotheses were supported by the SEM results (Table 2): patient awareness of PRHPP led to better understanding (coefficient = 0.291, p < 0.001) of prescribing performance indicators; better understanding increased perceived value (Coefficient = 0.342, p < 0.001) of the information; higher perceived value increased use of the information (Coefficient = 0.692, p < 0.001).
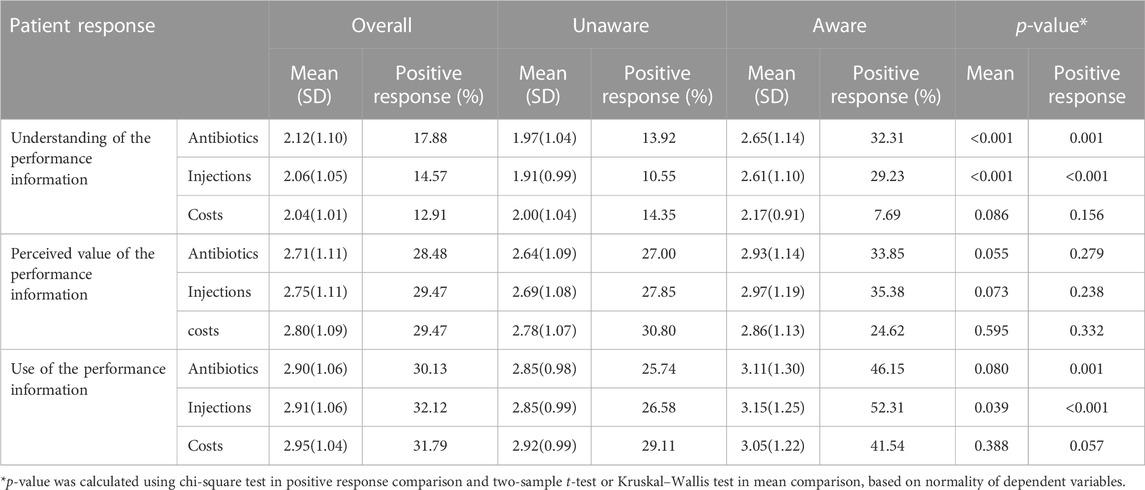
3.3 Effects of PRHPP
The respondents reported limited understanding, perceived value and use of the prescribing performance information, with a mean score ranging from 2.04 to 2.95 out of a possible 5 (Table 3). Those who were aware of the PRHPP had higher scores and a higher percentage of positive responses compared with those who were unaware of the PRHPP in the following aspects: understanding of prescribing indicators associated with antibiotics (p < 0.001) and injections (p < 0.001) and use of the injection indicator (p < 0.05). The patients who were aware of the PRHPP were also more likely to have a positive response to the use of the antibiotic indicator (p = 0.001), despite a lack of significant difference in the mean scores (p = 0.08).
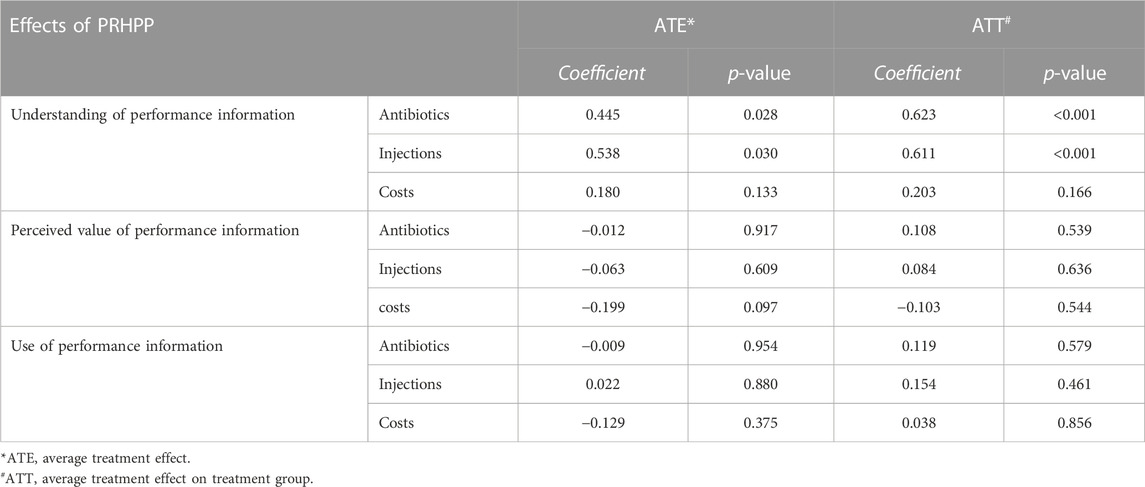
The effects estimated using PSM showed that the PRHPP led to a 0.5 increase in ATE (p < 0.05) and a 0.6 increase in ATT (p < 0.001) with regard to patient understanding of the prescribing performance information associated with antibiotics and injections (Table 4). However, no significant effects were found on the other aspects of the CCM (p > 0.1).
4 Discussion
This study revealed that PRHPP can improve patient understanding about the prescribing performance information, but it failed to translate into a useful tool to help patients make choices. Previous studies also showed no or weak evidence to support the link between PRHPP and patient choices in real world contexts (Faber et al., 2009; Totten et al., 2012), despite strong evidence supporting such a link in an experimental environment.
PRHPP serves as one way to inform consumer healthcare choices by comparing physicians’ performance of various dimensions of quality and cost. PRHPP practice in this study covered the core prescribing indicators of percentage of prescriptions requiring antibiotics, percentage of prescriptions requiring injection and cost indictor of average expenditure of patients. WHO in collaboration with the International Network of Rational Medicine Use (INRDU) recommended the set of core prescribing indictors, which have been widely applied for evaluating antibiotic prescribing quality among primary healthcare facilities in developing countries (Aravamuthan et al., 2017; Amaha et al., 2019; Kilipamwambu et al., 2021).
Based on the results from a recent review, public reporting of physicians’ and hospitals’ performance can help stimulate quality improvement, inform consumer choices and ultimately improve clinical results moderately. For consumers, with transparent and easily available performance information, PRHPP could help facilitate consumers to select a physician or medical institutions that appeared to have better results (Prang et al., 2021). However, whether PRHPP works or how the amount of practical effects depended on a list of various factors, such as the appropriateness of disseminated channel of PRHPP, relevance and meaningfulness of the chosen indictors, and consumer characteristics, which are discussed below for the limited effects of PRHRR in this study (Hibbard and Sofaer, 2010).
The CCM theory postulates a staged process for behavioral changes. It is essential to make sure that the reported information is valuable from the perspective of consumers before they are willing to use the information for decision making. Although in this study, participants enjoyed the freedom to choose providers, they might not necessarily appreciate the value of the PRHPP information for several reasons.
Firstly, the overuse of antibiotic and injection prescriptions is common and consistently high in primary care institutions and prescription costs have already been lowered due to the recent health system reform in China. Empirical studies show that PRHPP is more useful for patients when obvious differences in provider behaviors are observable (Harris, 2002). Otherwise, little value would be perceived by patients in relation to changing providers. Indeed, the percentage of prescriptions requiring antibiotics or injections are overwhelmingly high in China (Liu et al., 2015). Despite strong government interventions to tackle this problem, there has been no sign of decline in antibiotic and injection prescriptions (Li, 2014; Liu et al., 2015; Liu et al., 2016). In the participating institutions of this study, no prescriber was able to meet the WHO recommendations in relation to of the rational use of medicines (Laing et al., 1993).
Secondly, consumer demand for antibiotics and injections are high. In China, many patients believe that antibiotics and injections are a shortcut to quick recovery from many illnesses, including common colds (Wei et al., 2006). Such a misunderstanding may seriously jeopardize the value of PRHPP (Baker et al., 2014; Spaling et al., 2015; Dodds et al., 2016). The misconception could negatively affect the perception of the raking indictors of PRHPP practice. It was likely that PRHPP may lead more patients to seek services from those doctors prescribed more antibiotics and injections. Numerous studies have demonstrated that a lack of appropriate understanding is a major barrier preventing patients from using PRHPP information (Hibbard and Jewett, 1996; Jewett and Hibbard, 1996; Boscarino and Adams, 2004; Richard et al., 2005; Sofaer et al., 2005; Robinowitz and Dudley, 2006). Although we found significant improvement in patient understanding of the PRHPP information, such improvement is limited. Some researchers recommend simplified presentations such as a star rating to improve understanding and endorsement from patients (Peters et al., 2007; Damman et al., 2012).
Thirdly, the disclosed information may not be considered relevant to the priorities of the patients. Patients are more likely to appreciate the information that fits better with their needs. For example, cancer patients would need quite different information compared to diabetic patients (Edgman-Levitan and Cleary, 1996). Unfortunately, we were not able to collect diagnostic information because more than half of the questionnaires were collected prior to medical consultations.
Finally, the level of patient awareness of the PRHPP is low. Only one-fifth of the respondents reported being aware of the PRHPP. This rate is much lower compared with those (49%–78%) found in studies conducted in the USA (Knutson et al., 1998; Farley et al., 2002a; Hibbard et al., 2002). However, it is important to acknowledge that these studies offered participants a choice of a healthcare plan which is relevant to almost everyone (Knutson et al., 1998; Farley et al., 2002a; Farley et al., 2002b; Hibbard et al., 2002). For information related to patient care interventions, however, it is challenging to attempt to attract attention from all patients. Some researchers argued that patients with different illness conditions may have very different preferences in the choice of medical interventions. The rationale behind their choices could not be understood through observations of choices made by healthy people (Faber et al., 2009). Schneider and Epstein reported that only 12% of hospital patients who underwent coronary artery bypass grafting (CABG) surgery paid attention to reported CABG mortality rates (Schneider and Epstein, 1998). It is not clear why so many CABG patients ignored the reported mortality information.
A lack of understanding and support from patients for the rational use of medicines is a serious issue of concern. The overuse of antibiotics and injections is very common in China and many other developing countries. It has contributed to the rapid spread of antibiotic resistance (Robinowitz and Dudley, 2006), transmission of the human immunodeficiency virus and hepatitis B virus (Damman et al., 2012), and escalation of medical costs.
PRHPP is intended to be an instrument for empowering patients. However, careful design of the PRHPP is essential to obtain endorsement from patients. A number of guidelines are available for developing a readable and understandable PRHPP (Drozda et al., 2008; Hussey et al., 2014).
New approaches should be developed to solve the effectiveness of PRHPP practice, such as engagement of professional societies, increasing disseminating channel of public information, determining the best format for presentation of information to consumers, and eliminating the misconceptions of the information by consumers (Dehmer et al., 2014). The engagement of professional societies has been mentioned as one effective way for developing meaningful performance measures and promoting use of public reporting. Increasing the disseminating channel is also identified as one effective strategy, for example, information can be reported through a range of media, such as individual reminders, educational materials, public forums, clinical audits and feedback (Grimshaw et al., 2004). Research evidence shows that explanatory messages are not effective in correcting misconceptions and in increasing the perceived value of PRHPP (Hibbard et al., 2000). A simple message about risks may be more effective. A study conducted in India suggests that information disseminated from physicians is more effective than public reporting, resulting in lower injection use (Bhunia et al., 2010), possibly because the information targeted those with the highest risk. General education of the public plays an important role in the effectiveness of PRHPP. Low levels of education and socioeconomic status are usually associated with low awareness and poor understanding of PRHPP (Hibbard et al., 2001b). The average level of education and income of the participants of this study was low, which might have contributed to the limited effects of the PRHPP.
The effects of PRHPP should be explained with caution. The effects of the PRHPP, both positive and negative, are context dependent. In this study, three prescription indicators were reported in line with the WHO recommendations (Laing et al., 1993). Similar to the findings of other studies (Robinson and Brodie, 1997; Schneider and Epstein, 1998), these three indicators did not attract equal attention from patients: patients are more concerned about the quality rather than the cost of prescriptions. However, given the prevalent misconception about antibiotic and injection interventions from consumers, there is a risk that PRHPP may encourage more patients to seek services from those doctors who are more likely to prescribe antibiotics and injections. In addition, the doctors who rank low in the league table may choose to increase antibiotic and injection prescriptions in order to increase their market share (Wang et al., 2014). Some researchers worry that the reported poor performance of health workers may exacerbate the existing strained relationship between physicians and patients in China (Tang et al., 2008), stimulating distrust and more defensive practices (Totten et al., 2012). Further studies are needed to tap into these questions.
This study has made a significant contribution to the literature by applying CCM theory to explore the effects of PRHPP in a real-world context. The SEM analysis showed that the CCM theory fits well with the data. The application of PSM reduced potential bias in estimating the effect size of the PRHPP (Li, 2013).
4.1 Limitation
There were several limitations in this study. First, the data were collected 10 months after the introduction of the PRHPP, which may not be long enough to detect the effects of PRHPP, especially for those at a later stage of the CCM. However, the immediate effect of PRHPP on patient understanding of prescription information is still promising. On the other hand, the effects of PRHPP on informing patient choices is limited and further measures targeting on improving effectiveness of PRHPP should be considered in future studies. Third, the participants of this study had relatively low socioeconomic status, which may result in under-estimation of the effects of PRHPP. Finally, the survey was undertaken in primary care institutions in Hubei province. Generalization of the results to other facilities and regions needs to be cautious.
5 Conclusion
Patient awareness of the PRHPP is low. The effects of the PRHPP are limited, with some improvement of patient understanding about the antibiotic and injection prescription indicators. The PRHPP failed to show significant impacts on patient perceived value and use of information. The healthcare system contexts and low socio-economic status of the participants may be associated with the limited effects of the PRHPP. Appropriate patient education and provider training are prerequisites for the introduction of PRHPP programs.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (NO: IORG 0003571). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CL and XZ designed the project and participated in the collection and interpretation of data. MC contributed to the acquisition, analysis and interpretation of data and drafted the manuscript. CL and DW participated in data analysis, interpretation of results, and writing of the manuscript. DW and HC participated in the acquisition, cleaning and interpretation of data. DW takes responsibility for the accuracy of the data analysis and contents of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Natural Science Foundation of China (Grant No. 71373092 & 72004066). The funding body played no part in the study design, collection, analysis and interpretation of data, writing of the manuscript or the decision to submit the manuscript for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1110653/full#supplementary-material
Abbreviations
PRHPP, Public reporting of health providers’ performance; ATE, Average treatment effect; ATT, Average treatment effect on the treated group; CCM, Consumer choice model; PSM, Propensity-score method; SD, Standard deviation; SEM, Structural equation modelling; CABG, Coronary artery bypass grafting.
References
Amaha, N. D., Weldemariam, D. G., Abdu, N., and Tesfamariam, E. H. (2019). Prescribing practices using WHO prescribing indicators and factors associated with antibiotic prescribing in six community pharmacies in asmara, Eritrea: A cross-sectional study. Antimicrob. Resist Infect. Control 8, 163. doi:10.1186/s13756-019-0620-5
Aravamuthan, A., Subramaniam, K., and Udaya Chander J, S. J. (2017). Assessment of current prescribing practices using World Health Organization core drug use and complementary indicators in selected rural community pharmacies in southern India. J. Pharm. Policy Pract. 10 (1), 1. doi:10.1186/s40545-016-0074-6
Asch, S. M., Kerr, E. A., Keesey, J., Adams, J. L., Setodji, C. M., Malik, S., et al. (2006). Who is at greatest risk for receiving poor-quality health care? New Engl. J. Med. 354 (11), 1147–1156. doi:10.1056/NEJMsa044464
Austin, P. C. (2008). A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Statistics Med. 27 (12), 2037–2049. doi:10.1002/sim.3150
Austin, P. C. (2009). Some methods of propensity-score matching had superior performance to others: Results of an empirical investigation and Monte Carlo simulations. Biometrical J. 51 (1), 171–184. doi:10.1002/bimj.200810488
Baker, T. A., O'connor, M. L., and Krok, J. L. (2014). Experience and knowledge of pain management in patients receiving outpatient cancer treatment: What do older adults really know about their cancer pain? Pain Med. 15 (1), 52–60. doi:10.1111/pme.12244
Berwick, D. M., James, B., and Coye, M. J. (2003). Connections between quality measurement and improvement. Med. Care 41 (1), I30–I38. doi:10.1097/00005650-200301001-00004
Bhunia, R., Hutin, Y., Ramkrishnan, R., Ghosh, P. K., Dey, S., and Murhekar, M. (2010). Reducing use of injections through interactional group discussions: A randomized controlled trial. Indian Pediatr. 47 (5), 409–414. doi:10.1007/s13312-010-0076-4
Boscarino, J. A., and Adams, R. E. (2004). Public perceptions of quality care and provider profiling in New York: implications for improving quality care and public health. J. Public Health Manag. Pract. 10 (3), 241–250. doi:10.1097/00124784-200405000-00008
Caliendo, M., and Kopeinig, S. (2008). Some practical guidance for the implementation of propensity score matching. J. Econ. Surv. 22 (1), 31–72. doi:10.1111/j.1467-6419.2007.00527.x
Cheng, S. H., and Song, H. Y. (2004). Physician performance information and consumer choice: A survey of subjects with the freedom to choose between doctors. Qual. Saf. health care 13 (2), 98–101. doi:10.1136/qshc.2003.006981
Damman, O. C., Hendriks, M., Rademakers, J., Spreeuwenberg, P., Delnoij, D. M., and Groenewegen, P. P. (2012). Consumers’ interpretation and use of comparative information on the quality of health care: The effect of presentation approaches. Health Expect. 15 (2), 197–211. doi:10.1111/j.1369-7625.2011.00671.x
Dehmer, G. J., Drozda, J. P., Brindis, R. G., Masoudi, F. A., Rumsfeld, J. S., Slattery, L. E., et al. (2014). Public reporting of clinical quality data: An update for cardiovascular specialists. J. Am. Coll. Cardiol. 63 (13), 1239–1245. doi:10.1016/j.jacc.2013.11.050
Dodds, C. M., Britto, M. T., Denson, L. A., Lovell, D. J., Saeed, S., and Lipstein, E. A. (2016). Physicians' perceptions of shared decision making in chronic disease and its barriers and facilitators. J. Pediatr. 171, 307–309. doi:10.1016/j.jpeds.2015.12.071
Drozda, J. P., Hagan, E. P., Mirro, M. J., Peterson, E. D., and Wright, J. S.American College of Cardiology Foundation Writing Committee (2008). ACCF 2008 health policy statement on principles for public reporting of physician performance data: A report of the American college of cardiology foundation writing committee to develop principles for public reporting of physician performance data. J. Am. Coll. Cardiol. 51 (20), 1993–2001. doi:10.1016/j.jacc.2008.03.004
Du, X., Wang, D., Wang, X., Yang, S., and Zhang, X. (2015). Exploring the transparency mechanism and evaluating the effect of public reporting on prescription: A protocol for a cluster randomized controlled trial. BMC public health 15, 277. doi:10.1186/s12889-015-1454-6
Edgman-Levitan, S., and Cleary, P. D. (1996). What information do consumers want and need? Health Aff. 15 (4), 42–56. doi:10.1377/hlthaff.15.4.42
Faber, M., Bosch, M., Wollersheim, H., Leatherman, S., and Grol, R. (2009). Public reporting in health care: How do consumers use quality-of-care information? A systematic review. Med. care 47 (1), 1–8. doi:10.1097/MLR.0b013e3181808bb5
Farley, D. O., Elliott, M. N., Short, P. F., Damiano, P., Kanouse, D. E., and Hays, R. D. (2002b). Effect of CAHPS performance information on health plan choices by Iowa Medicaid beneficiaries. Med. care Res. Rev. MCRR 59 (3), 319–336. doi:10.1177/107755870205900305
Farley, D. O., Short, P. F., Elliott, M. N., Kanouse, D. E., Brown, J. A., and Hays, R. D. (2002a). Effects of CAHPS health plan performance information on plan choices by New Jersey Medicaid beneficiaries. Health Serv. Res. 37 (4), 985–1007. doi:10.1034/j.1600-0560.2002.62.x
Fung, C. H., Lim, Y. W., Mattke, S., Damberg, C., and Shekelle, P. G. (2008). Systematic review: The evidence that publishing patient care performance data improves quality of care. Ann. Intern Med. 148 (2), 111–123. doi:10.7326/0003-4819-148-2-200801150-00006
Grimshaw, J., Thomas, R., MacLennan, G., Fraser, C., Ramsay, C., Vale, L., et al. (2004). Effectiveness and efficiency of guideline dissemination and implementation strategies.
Hannan, E. L., Kilburn, H., Racz, M., Shields, E., and Chassin, M. R. (1994). Improving the outcomes of coronary artery bypass surgery in New York State. Jama 271 (10), 761–766. doi:10.1001/jama.1994.03510340051033
Harris, K. M. (2002). Can high quality overcome consumer resistance to restricted provider access? Evidence from a health plan choice experiment. Health Serv. Res. 37 (3), 551–571. doi:10.1111/1475-6773.00037
Hibbard, J., and Sofaer, S. (2010). Best practices in public reporting no. 1: How to effectively present health care performance data to consumers.
Hibbard, J. H., Berkman, N., McCormack, L. A., and Jael, E. (2002). The impact of a CAHPS report on employee knowledge, beliefs, and decisions. Med. care Res. Rev. MCRR 59 (1), 104–116. doi:10.1177/107755870205900106
Hibbard, J. H., Harris-Kojetin, L., Mullin, P., Lubalin, J., and Garfinkel, S. (2000). Increasing the impact of health plan report cards by addressing consumers' concerns. Health Aff. 19 (5), 138–143. doi:10.1377/hlthaff.19.5.138
Hibbard, J. H., and Jewett, J. J. (1996). What type of quality information do consumers want in a health care report card? Med. care Res. Rev. 53 (1), 28–47. doi:10.1177/107755879605300102
Hibbard, J. H., Peters, E., Slovic, P., Finucane, M. L., and Tusler, M. (2001a). Making health care quality reports easier to use. Jt. Comm. J. Qual. Improv. 27 (11), 591–604. doi:10.1016/s1070-3241(01)27051-5
Hibbard, J. H., Slovic, P., Peters, E., Finucane, M. L., and Tusler, M. (2001b). Is the informed-choice policy approach appropriate for Medicare beneficiaries? Health Aff. 20 (3), 199–203. doi:10.1377/hlthaff.20.3.199
Hibbard, J. H., Sofaer, S., and Jewett, J. J. (1996). Condition-specific performance information: Assessing salience, comprehension, and approaches for communicating quality. Health care financ. Rev. 18 (1), 95–109.
Hibbard, J. H., Stockard, J., and Tusler, M. (2003). Does publicizing hospital performance stimulate quality improvement efforts? Health Aff. 22 (2), 84–94. doi:10.1377/hlthaff.22.2.84
Hooper, D., Coughlan, J., and Mullen, M. (2008). Structural equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 6 (1), 53–60.
Hussey, P. S., Luft, H. S., and McNamara, P. (2014). Public reporting of provider performance at a crossroads in the United States: Summary of current barriers and recommendations on how to move forward. Med. Care Res. Rev. 71 (5), 5S–16S. doi:10.1177/1077558714535980
Jewett, J. J., and Hibbard, J. H. (1996). Comprehension of quality care indicators: Differences among privately insured, publicly insured, and uninsured. Health care financ. Rev. 18 (1), 75–94.
Keller, S. D., Ware, J. E., Bentler, P. M., Aaronson, N. K., Alonso, J., Apolone, G., et al. (1998). Use of structural equation modeling to test the construct validity of the SF-36 health survey in ten countries: Results from the IQOLA project. International quality of life assessment. J. Clin. Epidemiol. 51 (11), 1179–1188. doi:10.1016/s0895-4356(98)00110-3
Kilipamwambu, A., Bwire, G. M., Myemba, D. T., Njiro, B. J., and Majigo, M. V. (2021). WHO/INRUD core prescribing indicators and antibiotic utilization patterns among primary health care facilities in Ilala district, Tanzania. JAC Antimicrob. Resist 3 (2), dlab049. doi:10.1093/jacamr/dlab049
Knutson, D. J., Kind, E. A., Fowles, J. B., and Adlis, S. (1998). Impact of report cards on employees: A natural experiment. Health care financ. Rev. 20 (1), 5–27.
Laing, R. O., Bimo, , Chowdhury, A., Das, A., Diwan, V., Kafle, K. K., et al. (1993). How to investigate drug use in health facilities: Selected drug use indicators. Geneva: World Health Organization, 92.
Lansky, D. (2002). Improving quality through public disclosure of performance information. Health Aff. 21 (4), 52–62. doi:10.1377/hlthaff.21.4.52
Li, M. (2013). Using the propensity score method to estimate causal effects: A review and practical guide. Organ. Res. Methods 16 (2), 188–226. doi:10.1177/1094428112447816
Li, Y. (2014). China’s misuse of antibiotics should be curbed. BMJ Br. Med. J. 348, g1083. doi:10.1136/bmj.g1083
Liu, C., Zhang, X., and Wan, J. (2015). Public reporting influences antibiotic and injection prescription in primary care: A segmented regression analysis. J. Eval. Clin. Pract. 21 (4), 597–603. doi:10.1111/jep.12343
Liu, C., Zhang, X., Wang, X., Zhang, X., Wan, J., and Zhong, F. (2016). Does public reporting influence antibiotic and injection prescribing to all patients? A cluster-randomized matched-pair trial in China. Medicine 95 (26), e3965. doi:10.1097/MD.0000000000003965
Longo, D. R., and Everet, K. D. (2003). Health care consumer reports: An evaluation of consumer perspectives. J. health care finance 30 (1), 65–71.
Marshall, M. N., Shekelle, P. G., Davies, H. T., and Smith, P. C. (2003). Public reporting on quality in the United States and the United Kingdom. Health Aff. 22 (3), 134–148. doi:10.1377/hlthaff.22.3.134
Marshall, M. N., Shekelle, P. G., Leatherman, S., and Brook, R. H. (2000). The public release of performance data: What do we expect to gain? A review of the evidence. Jama 283 (14), 1866–1874. doi:10.1001/jama.283.14.1866
Peters, E., Dieckmann, N., Dixon, A., Hibbard, J. H., and Mertz, C. K. (2007). Less is more in presenting quality information to consumers. Med. Care Res. Rev. 64 (2), 169–190. doi:10.1177/10775587070640020301
Prang, K. H., Maritz, R., Sabanovic, H., Dunt, D., and Kelaher, M. (2021). Mechanisms and impact of public reporting on physicians and hospitals' performance: A systematic review (2000-2020). PLoS One 16 (2), e0247297. doi:10.1371/journal.pone.0247297
Richard, S. A., Rawal, S., and Martin, D. K. (2005). Patients' views about cardiac report cards: A qualitative study. Can. J. Cardiol. 21 (11), 943–947.
Robinowitz, D. L., and Dudley, R. A. (2006). Public reporting of provider performance: Can its impact be made greater? Annu. Rev. Public Health 27, 517–536. doi:10.1146/annurev.publhealth.27.021405.102210
Robinson, S., and Brodie, M. (1997). Understanding the quality challenge for health consumers: The kaiser/AHCPR survey. Jt. Comm. J. Qual. Improv. 23 (5), 239–244. doi:10.1016/s1070-3241(16)30313-3
Schneider, E. C., and Epstein, A. M. (1998). Use of public performance reports - a survey of patients undergoing cardiac surgery. Jama-J Am. Med. Assoc. 279 (20), 1638–1642. doi:10.1001/jama.279.20.1638
Sofaer, S., Crofton, C., Goldstein, E., Hoy, E., and Crabb, J. (2005). What do consumers want to know about the quality of care in hospitals? Health Serv. Res. 40, 2018–2036. doi:10.1111/j.1475-6773.2005.00473.x
Spaling, M. A., Currie, K., Strachan, P. H., Harkness, K., and Clark, A. M. (2015). Improving support for heart failure patients: A systematic review to understand patients' perspectives on self-care. J. Adv. Nurs. 71 (11), 2478–2489. doi:10.1111/jan.12712
Tang, S., Meng, Q., Chen, L., Bekedam, H., Evans, T., and Whitehead, M. (2008). Tackling the challenges to health equity in China. Lancet 372 (9648), 1493–1501. doi:10.1016/S0140-6736(08)61364-1
Totten, A. M., Wagner, J., Tiwari, A., O'Haire, C., Griffin, J., and Walker, M. (2012). Closing the quality gap: Revisiting the state of the science (vol. 5: Public reporting as a quality improvement strategy). Evid. report/technology Assess. 208 (5), 1–645.
Uhrig, J. D., Harris-Kojetin, L., Bann, C., and Kuo, T. M. (2006). Do content and format affect older consumers' use of comparative information in a medicare health plan choice? Results from a controlled experiment. Med. Care Res. Rev. 63 (6), 701–718. doi:10.1177/1077558706293636
Wang, X., Tang, Y., Zhang, X., Yin, X., Du, X., and Zhang, X. (2014). Effect of publicly reporting performance data of medicine use on injection use: A quasi-experimental study. PloS one 9 (10), e109594. doi:10.1371/journal.pone.0109594
Wei, W., Xinneng, B., Zhengyan, L., and Li, J. (2006). Investigation on knowledge about rational drug use in 2 419 inpatients. China Pharm. 6, 033.
Keywords: public reporting, health providers’ performance, physicians, the propensity score method, primary care, antibiotics prescription
Citation: Chen M, Zhang X, Liu C, Chen H, Wang D and Liu C (2023) Effects of public reporting of prescription indicators on patient choices: evidence from propensity scores matching. Front. Pharmacol. 14:1110653. doi: 10.3389/fphar.2023.1110653
Received: 29 November 2022; Accepted: 25 September 2023;
Published: 09 October 2023.
Edited by:
Jean-Marie Boeynaems, Université libre de Bruxelles, BelgiumReviewed by:
Douglas Slain, West Virginia University, United StatesStephen Henry Gillespie, University of St Andrews, United Kingdom
Copyright © 2023 Chen, Zhang, Liu, Chen, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Wang, ODE1MzEwMDE2QHFxLmNvbQ==
 Manli Chen
Manli Chen Xinping Zhang
Xinping Zhang Chaojie Liu
Chaojie Liu Haihong Chen
Haihong Chen Dan Wang
Dan Wang Chenxi Liu
Chenxi Liu