- 1Department of Pharmacy, The Second Xiangya Hospital, Central South University, Changsha, China
- 2Institute of Clinical Pharmacy, The Second Xiangya Hospital, Central South University, Changsha, China
Background: Physician-pharmacist collaboration is a well-established care mode for the management of type 2 diabetes mellitus (T2DM) in developed countries, but no study has been conducted in primary healthcare in China. This study aims to evaluate the effects of physician-pharmacist collaborative clinics to manage T2DM in primary healthcare in China, and to better understand the factors influencing the implementation of physician-pharmacist collaborative clinics.
Methods: Two hundred and sixty-seven patients involved in a 12-month randomized controlled trial were assigned to physician-pharmacist collaborative clinics and usual clinics, completing surveys regarding medication compliance, quality of life (QoL) and care-seeking behavior at the baseline, 3rd, 6th, 9th and 12th month respectively, and diabetes knowledge at baseline and 12th month. A sample of twenty-two Patients, nine physicians and twelve pharmacists participated in semi-structured face-to-face interviews. The quantitative and qualitative data was integrated by triangulation.
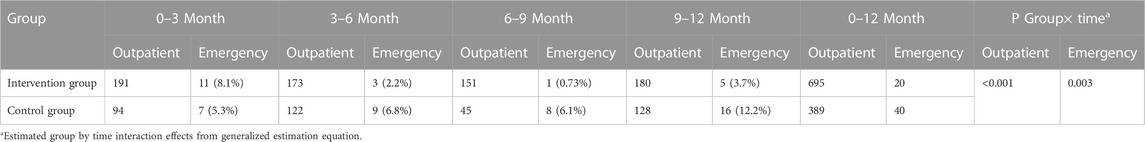
Results: Patients in physician-pharmacist collaborative clinics had significant improvements in medication compliance (p = 0.009), QoL (p = 0.036) and emergency visits (p = 0.003) over the 12-month. Pairwise comparison showed the medication compliance score in the intervention group had been significantly improved at 3rd month (p = 0.001), which is more rapidly than that in the control group at 9th month (p = 0.030). Factors influencing the implementation of physician-pharmacist collaborative clinics were driven by five themes: pharmaceutical service, team-base care, psychological support, acceptability of care and barriers to implementation.
Conclusion: Integration of quantitative and qualitative findings showed the effectiveness of physician-pharmacist collaborative clinics in patient medication compliance and QoL in primary healthcare. The qualitative study uncovered barriers in insufficient clinical experience and understaffing of pharmacist. Therefore, the professional training of the primary pharmacist team should be improved in the future.
Clinical Trial Registration: clinicaltrials.gov, identifier ChiCTR2000031839.
1 Introduction
Diabetes has become a serious global health problem due to its high prevalence and associated disability and mortality (GBD, 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017). Rapid economic development in the last 2 decades has led to changes in the lifestyles of the Chinese population, developing sedentary behaviors, physical inactivity and energy-dense eating habits, which have resulted in a rapidly increasing diabetes population (Pan et al., 2021; Pang et al., 2021). According to the International Diabetes Federation (IDF), the prevalence of diabetes in China is growing rapidly, ranking first in the world, at about 11.9% of the adult population (Saeedi et al., 2019). Estimates show that 116.4 million adults in China have diabetes, more than 90% of which are type 2 diabetes (T2DM), accounting for 24% of the global diabetic population (International Diabetes Federation, 2021).
Diabetes is a long-term chronic disease, and the patient’s daily behavior and self-management ability are key factors affecting the control of diabetes (Yoon et al., 2022). The management of T2DM is complex, requiring multiple interventions to optimize glucose control, reduce risk factors, and prevent complications, which is physician-dominated in China (Conlin et al., 2017; Professional Practice Committee, 2018). So far, diabetes management in China is not yet well implemented, especially in rural areas. The two main reasons for poor management are the lower density of physicians and the lower socioeconomic status and education background of patients, which are particularly common in primary healthcare (Anand et al., 2008; Wang et al., 2014; Liu et al., 2016; Jin et al., 2017). According to a national cross-sectional study in 2018, the rates of awareness, treatment and glucose control of diabetes in urban areas in China were only 40.0%, 36.2%, and 54.1%, respectively. The situation is more serious in rural areas, where rates were 32.6%, 28.8%, and 44.1% respectively (Wang et al., 2021a). There are rigorous challenges in terms of diabetes management, especially in primary medical care.
The physician-pharmacist collaborative clinics were first introduced in the United States, aiming to optimize medical treatment and reduce medical expenses (Hammad et al., 2011; Wei et al., 2022). The mode of physician-pharmacist collaboration was based on Medication Therapy Management (MTM), a service provided by pharmacists to ensure optimum therapeutic outcomes for individualization by reducing the risk of adverse events, improving patient medication compliance and quality of care (Oladapo and Rascati, 2012; Miller et al., 2016; Brandt and Cooke, 2017; Song et al., 2022). Based on comprehensive research evidence, the involvement of pharmacists in diabetes management significantly improve treatment cost-effectiveness and lower clinical parameters of glycosylated hemoglobin (HbA1c) and low-density lipoprotein (LDL) (Kiel and McCord, 2005; Farland et al., 2013).
In tertiary hospitals in China, physician-pharmacist collaborative mode has been well-established. Pharmacists conduct investigations to collect patient information, including laboratory parameters, medical and family history (Zhang et al., 2022). Pharmacists also assess medical risks and monitor adverse drug reactions to help physicians determine the therapeutic scheme. Finally, pharmacists provide medication counseling and disease education to patients (Wang et al., 2021b). However, traditional mode still dominates in primary healthcare, where physicians often make diagnoses, determine treatment plans and provide medication guidance independently, leading to several problems. As reported in previous studies, physicians were overwhelmed by the large number of patient visits, resulting in the limited time for disease education and medication instruction, and low patient satisfaction (Wen et al., 2016; Manzoor et al., 2019; Li et al., 2021).
Despite the physician-pharmacist collaborative clinics have attracted widespread attention in Chinese tertiary hospitals, no study has been carried out in Chinese primary healthcare. Therefore, we conducted a mixed-methods study to evaluate the effects and influencing factors of implementing physician-pharmacist collaborative clinics to manage T2DM in primary healthcare.
2 Materials and methods
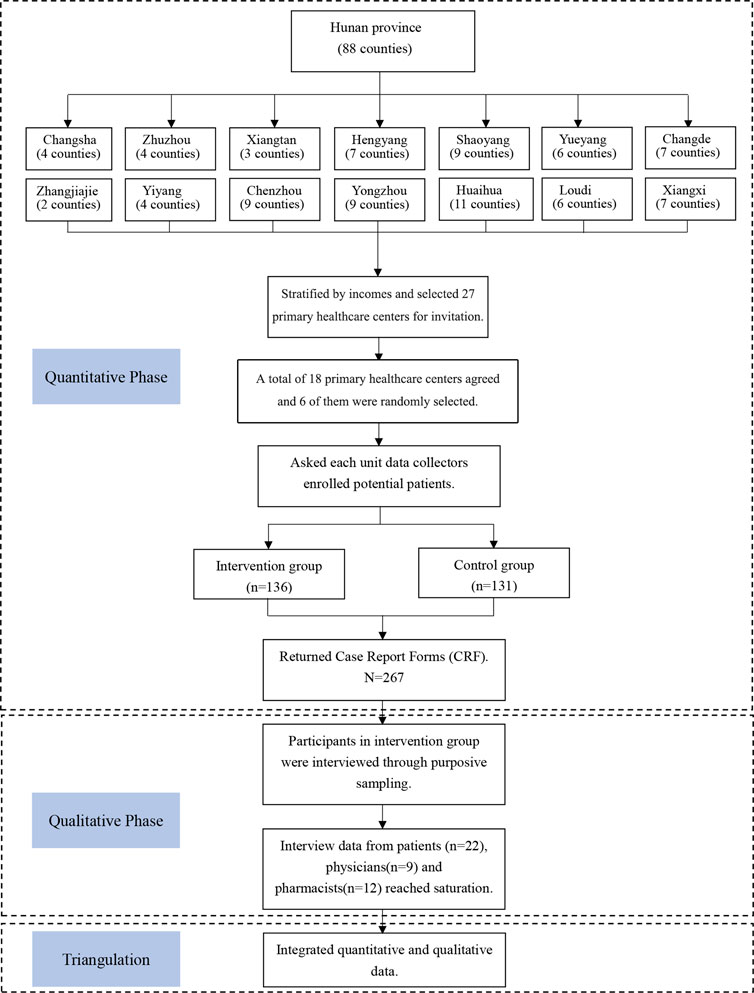
The mixed-methods study using an explanatory design, consists of three key components: a multi-center randomized controlled trial (RCT); and qualitative interviews with participants; and integration of quantitative and qualitative data (Figure 1). This study was reported following the Good Reporting of a Mixed Methods Study (GRAMMS) checklist and Consolidated Standards of Reporting Trials (CONSORT).
2.1 Research design
The study was conducted in Hunan province, which is a medium-level province in China and could represent the average medical condition in China. We randomly selected six primary healthcare centers in Hunan province (three in each group) to conduct multi-center randomized control trial. Potential patients were invited and randomly assigned to the intervention group (physician-pharmacist collaborative clinics) or the control group (usual care clinics). Patients in the intervention group underwent physician-pharmacist collaboration diabetes clinics, while patients in control group received routine clinics without pharmacist involving. A study protocol was reported in previous study (Tan et al., 2022). We collected patients’ characteristics and survey responses on medication compliance scale, EQ-5D-3L instrument and care-seeking behavior at baseline, 3rd, 6th, 9th, 12th months, and the diabetes knowledge questionnaire responses at baseline and 12th month.
Qualitative study based on descriptive phenomenological design to perceive patients’, physicians’ and pharmacists’ personal experiences, attitudes and perceptions on physician-pharmacist collaborative clinics. After the 12-month follow-ups, patients, physicians and pharmacists in the intervention group were invited to face-to-face interviews.
2.2 Randomization and masking
Six primary healthcare centers were selected in Hunan Province by using a standard randomization protocol (http://stattrek.com/statistics/random-number-generator.aspx). After recruitment, the six selected primary healthcare centers were randomly divided into the intervention group (physician-pharmacist collaborative clinics) or the control group (usual clinics), with three in each group. Due to the nature of pharmacist intervention, it was impossible to mask participants in the study.
2.3 Interventions
Local pharmacists who received standardized intervention training for 3 months at the Second Xiangya Hospital were finally assessed and qualified to participate in the collaborative clinic. Patients in the physician-pharmacist collaborative clinics received pharmaceutical care at each follow up visit, including diabetes education, medication guidance, lifestyle intervention, treatment of adverse drug reactions and identification of complications. Patients were enrolled in WeChat groups, where pharmacist conducted daily management, disease education, and send messages of diabetes knowledge, dietary advice and exercise programs. In addition, patients received peer support and encouragement from others through the WeChat group.
Both groups received routine outpatient services from physicians, including diagnosis, treatment due to limited time. There is no intervention provided by pharmacists in usual clinics.
2.4 Participants
Sample size is calculated using a formula for clinical trial (Billings et al., 2017). We indicated that to detect an absolute difference score of 1.14 in medication compliance in favor of the intervention group with α = 0.05, β = 0.1, and standard deviation of 1.5. Thus, a sample size of 36 patients per center was required (Tan et al., 2022). An additional 10% was added to allow for patients dropping out of the study, making a target sample size of at least 40 patients in each primary healthcare center. Participants were randomized to either intervention group or control group and performed on a 1:1 ratio. Patients were recruited in multi-center randomized control trial if: (1) have been diagnosed with T2DM; (2) 18 years or older; (3) the HbA1c level of the past 2 months was>7.5% prior to the study; (4) an informed consent signed by the patient or a legal guardian. Patients were excluded if: (1) currently pregnant; (2) have end-stage renal failure; (3) have dementia or severe psychiatric disorders; (4) receive treatment for cancer; (5) have congestive heart failure; (6) have a history of pancreatitis. The inclusion criteria for pharmacists were: (1) have received a standardized training as a clinical pharmacist; (2) have worked as a clinical pharmacist in endocrinology specialty for over 2 years; (3) be able to get comprehensive training for 3 months. Quantitative data were collected from a total of 267 patients.
Qualitative study utilized purposive sampling technique. According to maximum difference sampling, voluntarily patients, physicians and collaborating pharmacists were selected to form matching feedback models. Participants were stratified according to gender, age, educational background, course of disease and complications (for patients), working experience and professional titles (for physicians and pharmacists). Participants were recruited if: (1) took part in physician-pharmacist collaborative diabetes clinics; (2) have completed 12-month follow-ups. Recruitment continued until the researchers reached data saturation, and no participants contribute additional input in the interviews (Saunders et al., 2018). A total of 22 patients, 9 physicians, 12 pharmacists from three primary healthcare centers participated in the interviews.
2.5 Data collection
The primary outcomes of RCT were assessed by medication compliance scale with chronic patients, EQ-5D-3L instrument, while the second outcomes were diabetes knowledge score and care-seeking behaviour. Before the main study, we conducted a pilot study in two primary healthcare centers to evaluate the reliability of the instruments. The medication compliance scale with chronic diseases was widely used in China, with a high reliability and validity, and the Cronbach’s alpha index was 0.717 (Xu et al., 2008). The EQ-5D-3L instrument, including the visual analogue scale (VAS) and time trade-off (TTO), is widely used to assess the quality of life in China, and the Cronbach’s alpha index was 0.815 (Zhuo et al., 2018). The diabetes knowledge scale and Treatment Behaviour Survey were developed by the diabetes centre of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, which has been proved suitable for the disease control requirements of Chinese patients. The Cronbach’s alpha index of diabetes knowledge scale was 0.802 (Zhao et al., 2004).
Semi-structured face-to-face interviews were carried out by researchers from September to December 2021. To collect data in a comprehensive and detailed manner, participants were asked to provide real examples and stories of their first-hand experience in physician-pharmacist collaborative clinics. The participants were also encouraged to discuss their experiences with diabetes care. The interview outline was designed to cover the feelings of participants and their willingness to promote the implementation of physician-pharmacist collaborative clinics (Supplementary Appendix S1). The mean interview time lasted 30 min with patients, and 40 min with physicians and pharmacists, based on participants’ availability. Each interview continued until data was saturated when no more new information. All interviews were recorded with the participant’s prior permission. Audio files were transcribed by two researchers respectively to ensure data quality.
2.6 Data analysis
Quantitative data were analyzed using the Statistical Product and Service Solutions (SPSS). We summarized baseline characteristics using descriptive statistics and compare groups through Mann-Whitney u tests or chi-square test as appropriate. Differences in the intervention for the patient survey responses were examined with generalized estimating equations (GEE) analysis. GEE provides reliable estimate of main and interaction effects for time-dependent repeated measures data. Orthogonal polynomial contrasts were used to test for the fixed trend of mean change curve. Pairwise comparison with Dunnett’s t-test or Dunnett’s T3 test was also conducted to evaluate time points within each group. Missing data were not included in the analysis, as GEE approach flexibly accommodates various missing patterns and proportions (Koivusalo et al., 2016). Two-side p-values <0.05 were considered statistically significant.
Qualitative data were analyzed by the researchers in accordance with the Colaizzi method. The researchers read the interview transcript carefully multiple times, highlighting significant statements and assigning interpretations to them in the form of beginning codes respectively. Then the researchers identified similar viewpoints and coded them accordingly. According to the consistency of concepts, the various classes were merged, and finally, the ultimate theme concept was sublimed. Trustworthiness was achieved by credibility, transferability, dependability and confirmability (Amin et al., 2020). To ensure the credibility, purposeful sampling technique was used to select the samples with the greatest variation in participant characteristics, and participant verification was performed for the analysis and coding. Since the researchers have experience of qualitative research and interviews, they could easily communicate with the participants and extract relevant information. Researchers documented the memos and coding process in detail, and all authors from different disciplines were involved in discussions at all stages of the study to obtain the dependability criterion. Participants with different roles in collaborative clinics were interviewed to enrich perspectives, and two researchers coded separately to ensure confirmability. The perspectives of qualitative research experts and pharmacists with expertise experience were included in coding and data processing to establish confirmability. The transferability criterion was met through the depth and multi-perspective of descriptions for each category. All texts were coded by two researchers, respectively, and the contexts with inconsistent coding were discussed by all authors to reach consensus. Qualitative data were managed by NVivo 12.
2.7 Integration
A triangulation protocol enhances the validity and reliability of the mixed methods by exploring the convergence, complementary and dissonance (O'Cathain et al., 2010). We employed three types of triangulation techniques to integrate quantitative data and qualitative data, including investigator triangulation, methodological triangulation and data triangulation. Two researchers reviewed each data set and coded respectively, focusing on the following question: What were the factors that influenced the physician-pharmacist collaborative clinics for patient management? Researchers compared the results and data source of the two methods, and to determine whether the themes were agreement, partial agreement, silent or dissonant (Farmer et al., 2006).
2.8 Ethics approval
The study was approved by the Clinical Research Ethics Committee of the Second Xiangya Hospital of Central South University (No. 2019–213), and all of six primary healthcare centers accepted the ethic approval. All participants signed informed consent in the quantitative study and qualitative interview.
3 Results
3.1 Phase Ⅰ—Quantitative study
3.1.1 Baseline characteristics
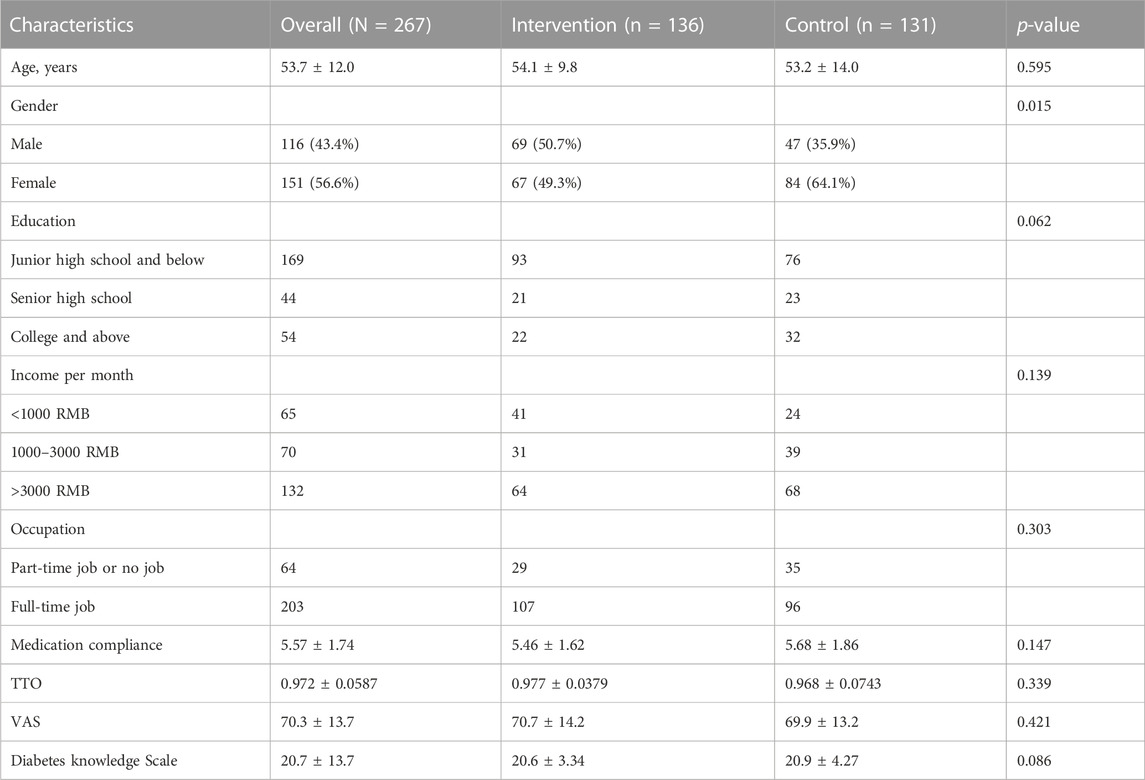
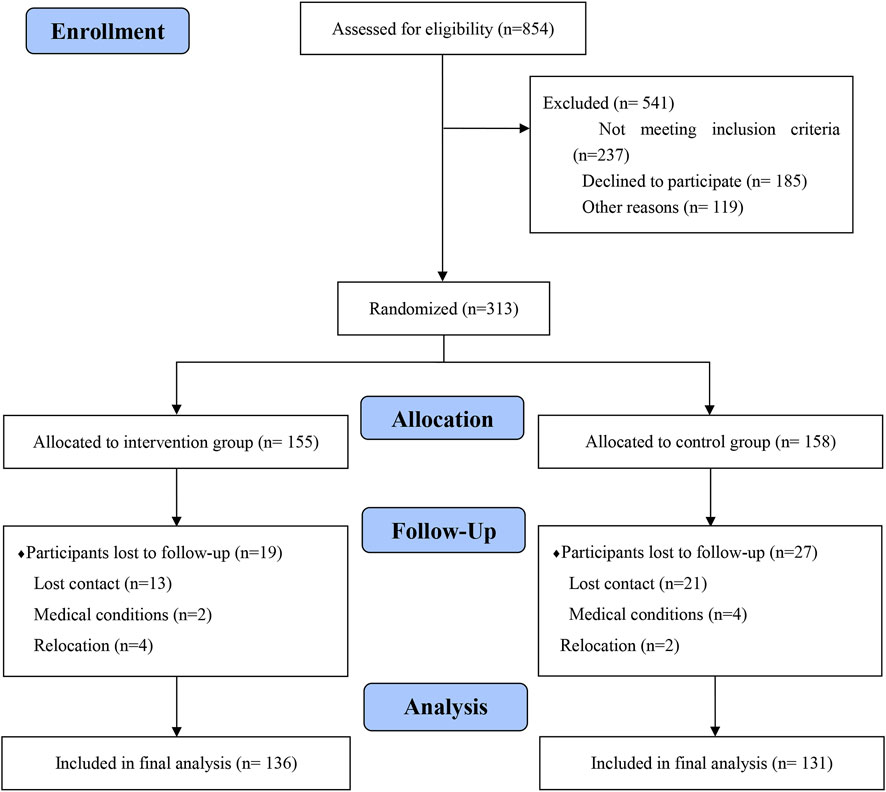
From the total enrolled patients (n = 267), 50.9% (n = 136) participated in physician-pharmacist collaborative clinics for 12 months. The mean age of the enrolled patients was 53.7 ± 12.0 years (n = 267) and 56.6% (n = 151) are female. Overall, the mean medication compliance score was 5.57 ± 1.74. The mean TTO value was 0.972 ± 0.0587. The mean VAS index score was 70.3 ± 13.7. The diabetes knowledge score was 20.7 ± 13.7. Baseline characteristics of the two groups were generally comparable (Table 1). Figure 2 summarizes participants recruitment and allocation.
3.1.2 Medication compliance
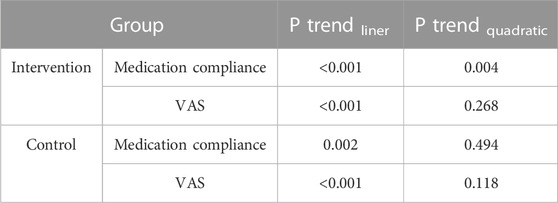
The mean improvement in medication compliance was significant between the intervention and control groups by time interaction effects over the 12 months (Collaborative clinics: 1.06 vs. Usual clinics: 0.52, p = 0.009). The medication compliance score in the intervention group significantly improved from 5.46 ± 1.62 at baseline to 6.15 ± 1.55 at 3 months [(CI: 0.244 to 1.13), p = 0.001], and improved higher to 6.53 ± 1.46 at 12 months [CI (0.620 to 1.51), p < 0.001] (Table 2, 3). The temporal trend curve of medication compliance in the intervention group showed a quadratic relationship (p = 0.004), which means the collaborative clinics significantly improved patients medication compliance in a very short period of time (Figure 3; Table 4). The medication compliance in the control group significantly improved from 5.68 ± 1.86 at baseline to 6.21 ± 1.55 at 9 months [CI [0.391 to 1.026), p = 0.030] and to 6.20 ± 1.56 at 12 months [CI (0.277 to 1.014), p = 0.035], which was 6 months later than the patients in the intervention group. The temporal trend curve showed liner trend (p = 0.002), indicating a gradual improvement in patients with usual care, but this process and outcomes were slower and worse than the intervention group.
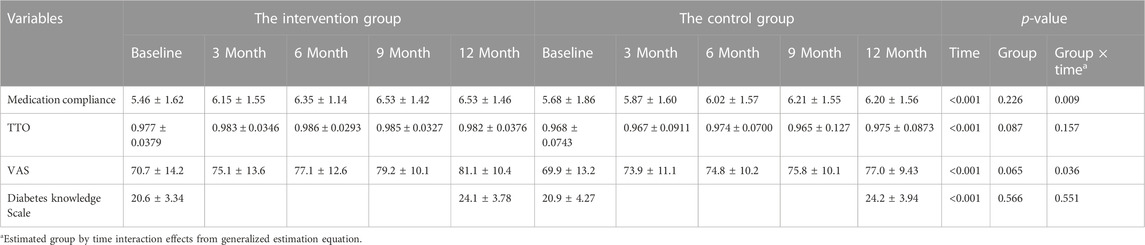
TABLE 2. The 12-month efficacy of the physician-pharmacist collaborative clinics on medication compliance, QoL and diabetes knowledge.
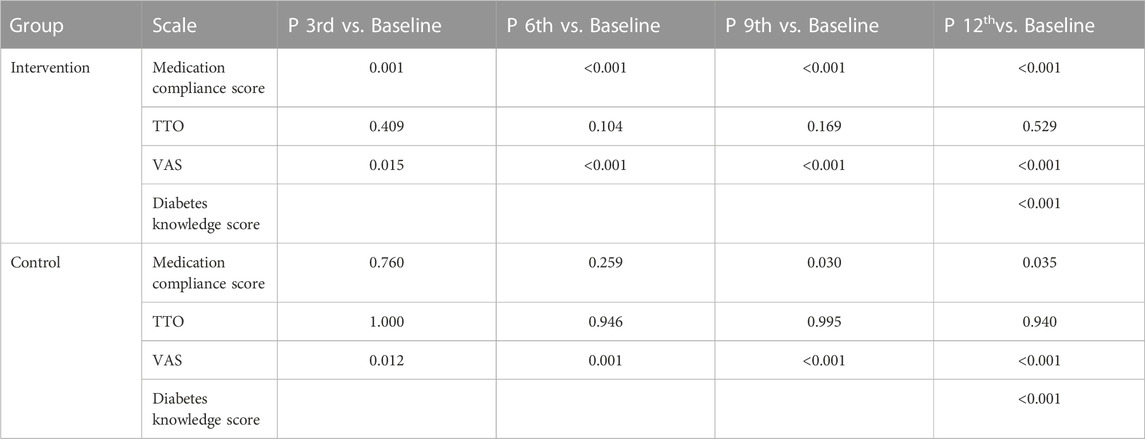
TABLE 3. The 12-month efficacy within each group on medication compliance, QoL and diabetes knowledge.
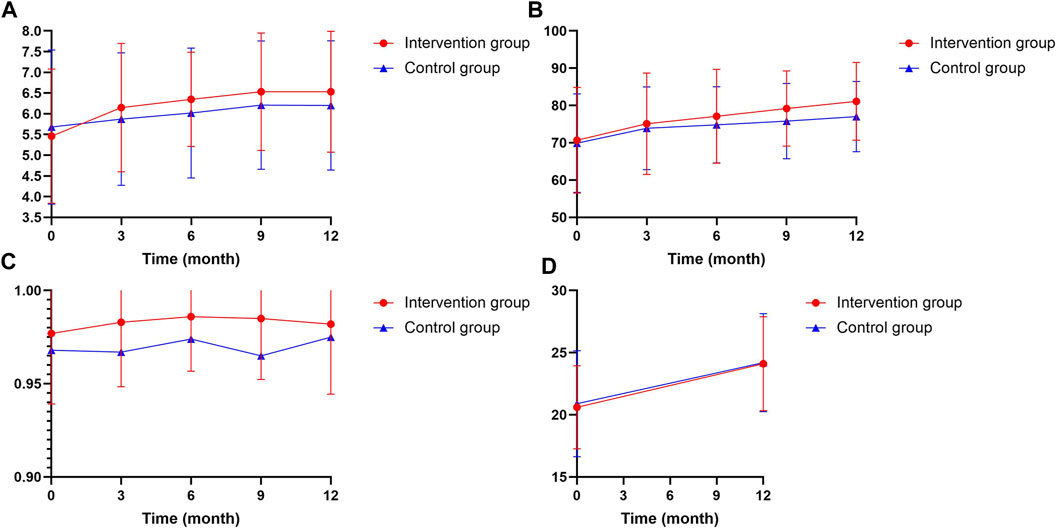
FIGURE 3. Indicated the change in medication compliance (A), VAS (B), TTO (C) and diabetes knowledge score (D).
3.1.3 Quality of life
Participants in the intervention group showed great improvement in their VAS score by time interaction effects over the 12 months compared to the usual clinics (Collaborative clinics: 10.40 vs. Usual clinics: 7.08, p = 0.036). But there were no significant differences by time interaction effects between groups in the TTO score (Collaborative clinics:0.00525 vs. Usual clinics: 0.00668, p = 0.157), although time effects were significant (p < 0.001).
The mean VAS score significantly improved from 70.7 ± 14.2 at baseline to 81.1 ± 10.4 at 12 months in the intervention group [(CI: 0.638 to 8.16, p < 0.001)], and also improved from 69.9 ± 13.2 at baseline to 77.0 ± 9.43 at 12 months in the control group [(CI: 0.680 to 7.26, p < 0.001)]. The temporal trend curve showed liner trend both in the intervention group (p < 0.001) and control group (p < 0.001), representing a similar VAS score growth trend, although the increments are significantly different. However, there were no significance in TTO score both in intervention group [(CI: −0.00425 to 0.0163), p = 0.529] and control group [(CI: −0.0288 to 0.0270, p = 0.940)] over the 12 months.
3.1.4 Diabetes knowledge
There was no significant difference in diabetes knowledge score by time effects between the intervention group and control group over the 12 months (Collaborative clinics: 3.52 vs. Usual clinics:3.28, p = 0.551). The mean diabetes knowledge score for patients in the intervention group significantly improved from 20.6 ± 3.34 at baseline to 24.1 ± 3.78 at 12 months (p < 0.001). Similarly, the diabetes knowledge score for patients in control group also improved from 20.9 ± 4.27 at baseline to 24.2 ± 3.94 at the 12 months (p < 0.001).
3.1.5 Care-seeking behavior
The number of care-seeking behavior showed great significance between the groups by time effects over the 12 months, including the number of outpatient visits (p < 0.001) and emergency visits (p = 0.003). Compared to control group, the number of outpatient clinic visits in the intervention group increased 1.78 times (collaborative clinics: 695 vs. usual clinics: 389), and emergency visits decreased to half (collaborative clinics: 20 vs. usual clinics: 40) in the last 12 months (Table 5).
3.2 Phase Ⅱ—Qualitative study
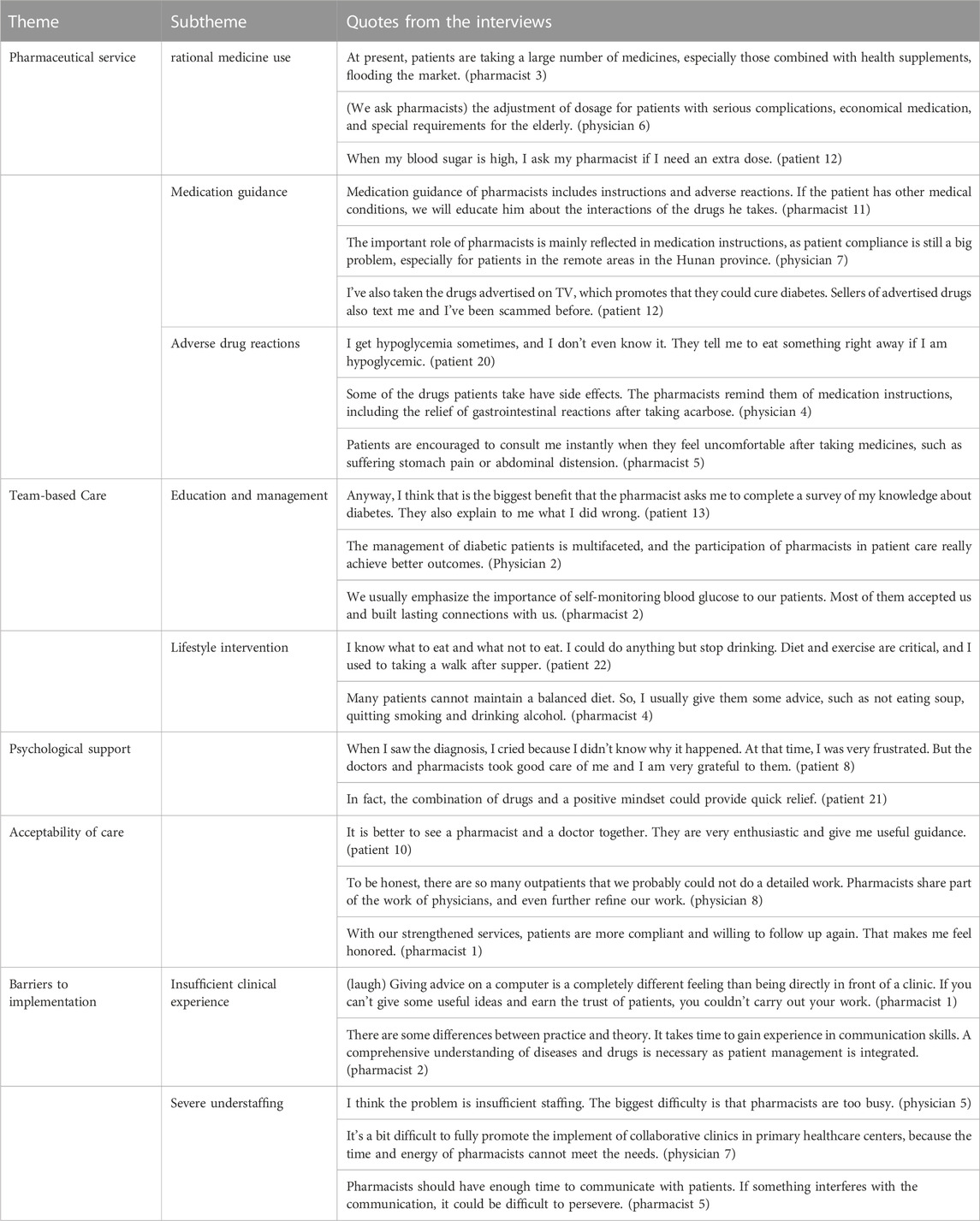
Five themes and seven subthemes were defined after analysis (Table 6).
3.3 Participant characteristics
We analyzed data from 22 patients, 9 physicians, and 12 pharmacists involved in physician-pharmacist collaborative clinics (Supplementary Appendix S2).
3.4 Pharmaceutical service
3.4.1 Rational medicine use
During clinical treatment, pharmacists were considered experts in pharmacotherapy from patients’ and physicians’ perspectives. Many patients in primary healthcare centers tend to take more medicines when their blood glucose was high, and even take health supplements with safety risks. Additionally, polypharmacy and medication for special populations are also big challenges for physicians, in which pharmacists act as important assistants. Although the conventional medications for diabetes treatment are already familiar to physicians and the majority of patients, pharmacists also play an important role in medication safety, efficacy, economy and property in physician-pharmacist collaborative clinics.
3.4.2 Medication guidance
Patients received individualized medication guidance in physician-pharmacist collaborative clinics, including administration time, drug-drug interaction, drug storage, oral and injection medication, and adverse drug reactions. Individualized medication guidance has effectively improved patients’ medication compliance, especially those combined with other diseases.
Many patients in primary healthcare centers are less educated, especially the elderly, and they are more likely to be misled by TV advertisements and false information. Due to poor knowledge of diabetes, they are easily inclined to taking fake medicines which claim to cure diabetes radically. Another pressing request from patients is to be educated to identify counterfeit medicines.
3.4.3 Adverse drug reactions
Few patients experienced hypoglycemia and gastrointestinal reaction while taking hypoglycemic drugs, which reduces their medication compliance and even damages their health due to improper handling. Pharmacists teach patients to identify and handle adverse reactions in a timely manner, which really reduces emergencies. In fact, significantly fewer patients had adverse drug reactions (ADRs) in physician-pharmacist collaborative clinics due to improved medication compliance.
3.5 Team-based care
3.5.1 Education and management
The majority of patients considered collaborative clinics have changed their misconceptions about diabetes, supporting more forms of education, such as popular medical articles, health lectures and diabetes counseling. Seven of nine physicians extremely expect more health professionals, especially pharmacists, involved in diabetes treatment and management in primary healthcare centers to make up for their lack in educating and managing patients. The participation of pharmacists in patient education and management will gradually change the status quo of the diabetic population. Diabetes education included disease introduction, control target and self-monitoring of blood glucose.
3.5.2 Lifestyle intervention
Comprehensive management of patients with diabetes requires a balanced diet and moderate exercise. Actually, through repeated education and reminders, most of the patients controlled their diet well and engaged in physical activity, especially those overweight patients. However, despite being educated by physicians and pharmacists, 6 of 10 male patients reported smoking or drinking after illness. Supervising patients to quit smoking and alcohol will be the focus in the future physician-pharmacist collaborative clinics.
3.6 Psychological support
The psychological effects of suffering from diabetes were wide reaching. Nine of 22 patients reported the feeling of distress, anxiety, embarrassment and depression were continuous, resulting in psychological avoidance from treatment. Unmarried female patients described severe anxiety about getting married and having children, seeking support from physicians and pharmacists. Psychological support by medical team helps relieve the pressure of patients with diabetes, improving psychological resilience and enabling patients to have the ability to properly cope with the disease.
3.7 Acceptability of care
Patients who undergone treatment in diabetes described physician-pharmacist collaborative clinics as an excellent policy that was accountable for patients’ health, and they were willing to visit them in the future. Physicians explained patients in primary healthcare centers need repeated education to understand the disease and treatment properly, which required a more detailed work, and pharmacists acted as assistances of physicians in collaborative clinics. Additionally, pharmacists showed great passion for clinical practice, which allows them to leverage their expertise and motivates them to improve their professional competency.
3.8 Barriers to implementation
3.8.1 Insufficient clinical experience
Many pharmacists described lack of clinical experience was the main obstacle in clinical procedures, of which insufficient knowledge of clinical medicine, deficient understanding of clinical need and inadequate communication skills were most frequently mentioned. Pharmacists noted that patient management is integrative and requires them to be proficient in clinical medicine, clinical pharmacy and clinical psychology, which made them spend more time on self-learning. Pharmacists who had less in-depth communications with patients reported that their professional advice lacked comprehensive consideration of patient’s clinical needs. As a result, the communication gap between pharmacist and patients appeared. Pharmacists in primary healthcare centers are aware of these problems and expect taking training courses in tertiary hospitals to enhance their professional capabilities.
3.8.2 Severe understaffing
Almost all pharmacists and physicians reported the biggest barrier is the shortage of experienced pharmacists in primary healthcare centers. The limited number of trained pharmacists undertook many tasks including review of prescriptions, management of antibiotics, monitoring of adverse drug reactions and medication education for inpatients. The scarcity of pharmacists and their busy daily work hindered their participation in patient education and management and the accumulation of clinical experience, finally impeding the implementation of physician-pharmacist collaborative clinics in primary healthcare centers.
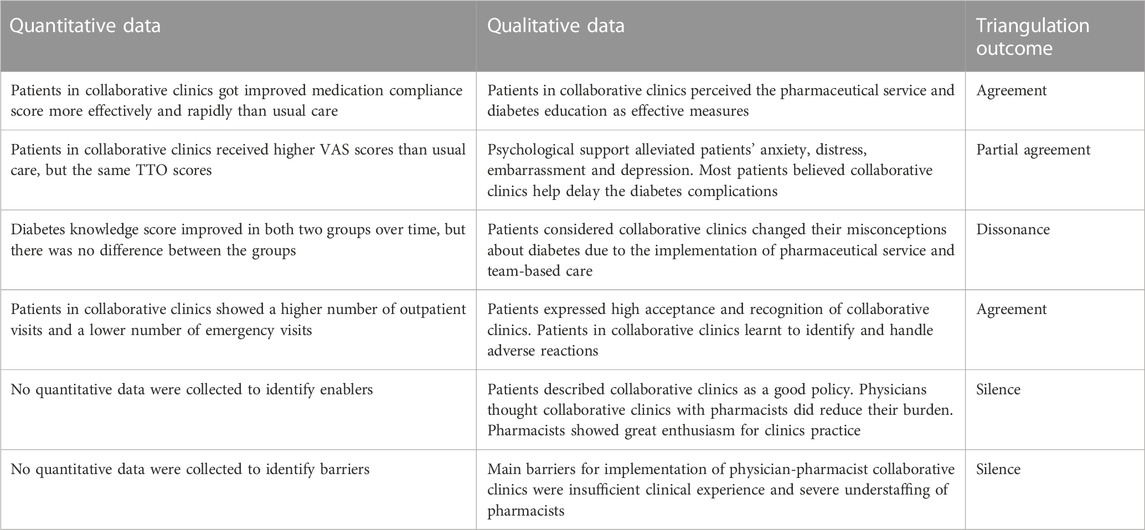
3.9 Phase Ⅲ—Integration
The triangulation found that pharmaceutical service and diabetes education provided by physicians and pharmacists effectively eliminated misconceptions about diabetes and hypoglycemic drugs, and improved patients’ self-management ability, resulting in a significant difference in medication compliance score between the two groups. Additionally, psychological support from physicians and pharmacists alleviated patients’ anxiety, distress and other negative emotions, manifested as a significant improvement in VAS score. In contrast, TTO score showed no improvement between the two groups, even patients in collaboratives believed it was beneficial for delaying diabetes complications.
An interesting result showed patients considered collaboratives clinics changed their misconceptions and provided them with more knowledge, but there was no significant improvement between the two groups over the 12 months. Patients high acceptance of care had led to an increase of outpatient visits. Furthermore, the high acceptance of diabetes education, including identification and management of adverse reactions, significantly reduced emergency visits.
From the qualitative data, high acceptance of participants mainly due to high-quality care, lighter burden and the enthusiasm of pharmacists, which greatly promoted the implementation of physician-pharmacist collaborative clinics. However, main barriers of insufficient clinical experience and severe understaffing of pharmacists impeded the implementation of physician-pharmacist collaborative clinics. Table 7 shows the triangulation of key qualitative and quantitative findings.
4 Discussion
This study integrated findings from the quantitative and qualitative data, providing a conducive perspective through which to evaluate the effects of physician-pharmacist collaborative clinics. In the 12-month RCT among patients with diabetes, we found that patients in collaborative clinics improved medication compliance and QoL more effectively and rapidly than usual care. As a result, the number of outpatient visits for patients in collaborative clinics increased while the emergency visits significantly decreased. The four thematic domains from qualitative study showed that pharmaceutical service, team-base care, psychological support and acceptability of care were the core of physician-pharmacist collaborative clinics, providing better healthcare for diabetic patients in primary healthcare. These findings demonstrate that the physician-pharmacist collaborative clinics effectively achieve better patient outcomes by improving medication compliance and QoL.
The integration of quantitative data and qualitative data showed partial agreement in the difference of QoL and dissonance in diabetes knowledge score between groups. It is worth noting that the TTO score at baseline both in the intervention group (0.977 ± 0.0380) and the control group (0.968 ± 0.0743) are better than the average of 2017 Chinese Heilongjiang population TTO score (0.959) (Huang et al., 2017). A mainly reason for this may be that most of patients included the trail had no complications that affect daily life. Due to the long process of the emergence of diabetic complications, the main impact of diabetes on early stage patients was reflected in the VAS score.
However, we noticed that both groups showed improvements in the medication compliance and VAS scores, despite the collaborative clinics being more effective and rapid. It means that the routine treatment in primary healthcare also has a positive effect on patients, but takes longer and carries a greater risk of complications. We also found that diabetes knowledge score showed great improvement in both two groups over the 12 months, indicating no additional benefit from the collaborative clinics. In fact, a survey on the awareness rate of diabetes knowledge in Chinese counties reported that diabetes-related knowledge of patients with T2DM was mainly acquired through media such as television or the Internet, accounting for 85.58%, followed by books or newspapers, accounting for 32.84% (Shao et al., 2022). This suggests that the traditional education mode seems to be ineffective in primary healthcare, and that the education mode in collaborative clinics needs to be combined with common and fast-spreading media.
We compared the sociodemographic characteristics of the patients to illustrate comparability between the two groups. There was a difference in gender between the two groups at baseline. As a matter of fact, the dramatic increase in T2DM and related complications is accompanied by evidence of clinical gender differences, in which both biological and psychosocial factors contribute to gender differences in diabetes risk and outcome (Kautzky-Willer et al., 2016). Overall, psychosocial stress appears to affect women more than men. However, previous studies have showed that gender differences have no influence on medication compliance and diabetes knowledge score, but educational background had a greater influence (Zhao et al., 2004). Therefore, gender differences between the two groups at baseline did not affect the results of this study.
Effectiveness of physician-pharmacist collaborative clinics for T2DM management has been proved by many clinical studies. By providing comprehensive medication education and patient management, pharmacists helped patients reduce HbA1c, LDL cholesterol, total cholesterol and blood pressure, further reducing emergency events compared to usual care (Shane-McWhorter and Oderda, 2005; Aguiar et al., 2018; Matzke et al., 2018). Moreover, pharmacists’ qualifications and service contribute to better healthcare and a favorable return on investment of $1.1–2.8 million dollars for patients (Lehn et al., 2019). Pharmaceutical care, pharmacist counselling and diabetes management provided by pharmacists have been proved to improve patient outcomes (Shao et al., 2017; Lum et al., 2019; Besemah et al., 2021).
A burning question over diabetes healthcare in primary healthcare of China is to maintain stable glucose control, delay diabetic complications and reduce emergency events, which require an effective and feasible healthcare mode. The diabetes population in primary healthcare, especially in rural China, has been increasing dramatically due to multiple reasons, including the growth of the economy, the aged tendency of the population, and the changed lifestyle (Huang et al., 2022). Diabetes management, as the most important part of treatment, includes physician’s management and patient self-management. However, both two aspects are insufficient in primary healthcare. Firstly, the number of physicians in China ranks forefront in the world with 2.27 per 1000, slightly less than the United State with 2.61 per 1000 in 2019 (World Health Organization, 2022). However, there is a serious maldistribution of physician density, which in urban areas was more than twice that in rural areas (Anand et al., 2008). Moreover, each physician per 1,000 population added to primary healthcare centers was associated with 67% more outpatient visits (Anand et al., 2008). However, certified physicians tend to serve in provincial urban centers rather than in rural areas due to multiple reasons, including low income, limitations in their qualification and career development (Hu et al., 2017; Wang et al., 2021c). Therefore, it’s necessary to ensure and improve the quality and quantity of health professionals in primary healthcare, especially in rural areas. Secondly, the lower socioeconomic status and educational background of rural patients limit their diabetes self-management (Wallace et al., 2010; Le et al., 2016). Studies show that patients with a higher level of education had a greater probability of regularly self-monitoring blood glucose, medication compliance, and taking measures to control diabetes (Hill et al., 2013).
Actually, with the development of clinical pharmacy, pharmacists have gradually completed the transition from pharmacy to clinical practice. They made a lot of attempts in the process, including pharmacotherapy clinics (Shahrami et al., 2022), MTM service (Johnson et al., 2018), and patient centered pharmacist care (Paneerselvam et al., 2022). Those pharmacists with rich pharmacotherapy knowledge reserves, as irreplaceable partners of physicians, ensure rational drug use, improve patient medication compliance, and ultimately ameliorate patient outcomes (Marr et al., 2018). Under the brunt of Corona Virus Disease 2019 (COVID-19), pharmacists motivated by medical professionalism were reassigned to new tasks, such as disseminating educational materials, intensive care and remote clinical service (Hao et al., 2021). Undoubtedly, pharmacists play a more important role in healthcare during the special time.
Due to the COVID-19 pandemic, medical resources have been reallocated, resulting in reduced outpatient clinics, which inevitably affected chronic disease management. Recently, research focused on diabetes management has shifted from outpatient clinics to online remote management. However, trials with larger populations tend to be negative, especially among patients broadly recruited from primary healthcare (Jia et al., 2021). One obvious reason is that eHealth platforms seem not user-friendly for patients, particularly for elderly users who are the major group of diabetics (Gao et al., 2017). Moreover, remote training may spend longer time for patients, resulting in poor patient adherence (Heselmans et al., 2020). Conversely, pharmacists in collaborative clinics play an important role in diabetes education, management, follow-up visits and remote introduction if necessary during the COVID-19 pandemic.
However, the main barriers to implement physician-pharmacist collaborative clinics are the lack of clinical experience and understaffing of pharmacists. In fact, the education background and knowledge structure of pharmacists in primary healthcare are far from the current clinical needs, resulting in their poor capability in guiding clinical practice, especially for the highly educated population (Hu et al., 2014). Overall, it’s more important to carry out professional training for pharmacists in primary healthcare, including knowledge in disease, communication skills and comprehensive management capabilities (Huang et al., 2021). Due to the long payback period, many primary healthcare centers do not attach importance to the development of pharmacy departments. Fortunately, pharmacists participate in clinical practices gradually, which is conducive to the development of pharmacy and the transformation of pharmacists in primary healthcare. In our enrolled intervention healthcare centers, Taoyuan People’s Hospital was the first to officially launch physician-pharmacist collaborative clinics for T2DM management.
This study has several limitations. First, unobserved confounding bias cannot be ruled out in this study. Second, the sample size was calculated based on primary outcomes, that may restrict the representative of this study. All primary healthcare centers are from Hunan Province, which may not reflect the situation in other regions of China. Third, this study could not be blinded, and Hawthorne effect could appear.
This study is the first mixed study to explore the effects and influencing factors of implementation of physician-pharmacist collaborative clinics in primary healthcare in China. Implementation of physician-pharmacist collaborative clinics had effectively strengthened patient management, especially the management of patient medication compliance and QoL. Through the pharmaceutical service, team-based care, psychological support and acceptability of care, physician-pharmacist collaborative clinics improved patient medication compliance and QoL more effectively and rapidly than usual care, which had been highly commended by patients. Our findings suggest that the insufficient clinical knowledge and severe understaffing of pharmacists should be considered in primary healthcare. In the future, professional training of primary pharmacist should become the focus of pharmacy practice to enhance patient-centered care in primary healthcare. Our findings provide evidence of the effectiveness of physician-pharmacist collaborative clinics and lay a solid foundation for further development and implementation of collaborative clinics in primary healthcare.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Clinical Research Ethics Committee of the Second Xiangya Hospital of Central South University (No. 2019-213). The patients/participants provided their written informed consent to participate in this study.
Author contributions
PX conceived and designed the study. Material preparation, data collection and analysis were performed by JX, QW, BT, SH, and YZ. The first draft of the manuscript was written by JX, ST, and LC. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research is funded by the China Medical Board (CMB) grant with $80,000 scholarship (Grant No.18-292) and Hunan Provincial Health Commission (Grant No.2019158). The current research has been independently peer-reviewed by funding agencies. The sponsors provided funding and reviewed the research but had no role in study design, data collection or writing of this manuscript.
Acknowledgments
We would like to acknowledge the China Medical Board (CMB) and Hunan Provincial Health Commission for their funding. Additionally, we would like to thank Mr. Lu Hao for his ideas on data analysis. We would like to thank all patients, physicians and pharmacists of physician-pharmacist collaborative clinics for participating in the interview.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1098207/full#supplementary-material
References
Aguiar, P. M., da Silva, C. H. P., Chiann, C., Dórea, E. L., Lyra, D. P., and Storpirtis, S. (2018). Pharmacist-physician collaborative care model for patients with uncontrolled type 2 diabetes in Brazil: Results from a randomized controlled trial. J. Eval. Clin. Pract. 24 (1), 22–30. doi:10.1111/jep.12606
Amin, M. E. K., Nørgaard, L. S., Cavaco, A. M., Witry, M. J., Hillman, L., Cernasev, A., et al. (2020). Establishing trustworthiness and authenticity in qualitative pharmacy research. Res. Soc. Adm. Pharm. 16 (10), 1472–1482. doi:10.1016/j.sapharm.2020.02.005
Anand, S., Fan, V. Y., Zhang, J., Zhang, L., Ke, Y., Dong, Z., et al. (2008). China's human resources for health: Quantity, quality, and distribution. Lancet 372 (9651), 1774–1781. doi:10.1016/S0140-6736(08)61363-X
Besemah, N. A., Sartika, R. A. D., and Sauriasari, R. (2021). Effect of pharmacist intervention on medication adherence and clinical outcomes of type 2 diabetes mellitus outpatients in primary healthcare in Indonesia. J. Res. Pharm. Pract. 9 (4), 186–195. doi:10.4103/jrpp.JRPP_20_59
Billings, M., Lopez Mitnik, G., and Dye, B. A. (2017). Sample size for clinical trials. Oral Dis. 23 (8), 1013–1018. doi:10.1111/odi.12611
Brandt, N. J., and Cooke, C. E. (2017). Centers for medicare and medicaid services support for medication therapy management (enhanced medication therapy management): Testing strategies for improving medication use among beneficiaries enrolled in medicare Part D. Clin. Geriatr. Med. 33 (2), 153–164. doi:10.1016/j.cger.2017.01.001
Conlin, P. R., Colburn, J., Aron, D., Pries, R. M., Tschanz, M. P., and Pogach, L. (2017). Synopsis of the 2017 U.S. Department of veterans affairs/U.S. Department of defense clinical practice guideline: Management of type 2 diabetes mellitus. Ann. Intern Med. 167 (9), 655–663. doi:10.7326/M17-1362
Farland, M. Z., Byrd, D. C., McFarland, M. S., Thomas, J., Franks, A. S., George, C. M., et al. (2013). Pharmacist-physician collaboration for diabetes care: The diabetes initiative program. Ann. Pharmacother. 47 (6), 781–789. doi:10.1345/aph.1S079
Farmer, T., Robinson, K., Elliott, S. J., and Eyles, J. (2006). Developing and implementing a triangulation protocol for qualitative health research. Qual. Health Res. 16 (3), 377–394. doi:10.1177/1049732305285708
Gao, C., Zhou, L., Liu, Z., Wang, H., and Bowers, B. (2017). Mobile application for diabetes self-management in China: Do they fit for older adults? Int. J. Med. Inf. 101, 68–74. doi:10.1016/j.ijmedinf.2017.02.005
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the global burden of disease study 2016. Lancet 390 (10100), 1211–1259. doi:10.1016/S0140-6736(17)32154-2
Hammad, E. A., Yasein, N., Tahaineh, L., and Albsoul-Younes, A. M. (2011). A randomized controlled trial to assess pharmacist-physician collaborative practice in the management of metabolic syndrome in a University medical clinic in Jordan. J. Manag. Care Pharm. 17 (4), 295–303. doi:10.18553/jmcp.2011.17.4.295
Hao, J., Wang, X., Jia, X., Yang, Y., Du, S., and Yin, Z. (2021). Qualitative research on the work experience of pharmacists in fever clinics and isolation wards of designated hospitals for novel coronavirus pneumonia (COVID-19). BMJ Open 11 (11), e048466. doi:10.1136/bmjopen-2020-048466
Heselmans, A., Delvaux, N., Laenen, A., Van de Velde, S., Ramaekers, D., Kunnamo, I., et al. (2020). Computerized clinical decision support system for diabetes in primary care does not improve quality of care: A cluster-randomized controlled trial. Implement Sci. 15 (1), 5. doi:10.1186/s13012-019-0955-6
Hill, J. O., Galloway, J. M., Goley, A., Marrero, D. G., Minners, R., Montgomery, B., et al. (2013). Scientific statement: Socioecological determinants of prediabetes and type 2 diabetes. Diabetes Care 36 (8), 2430–2439. doi:10.2337/dc13-1161
Hu, D., Zhu, W., Fu, Y., Zhang, M., Zhao, Y., Hanson, K., et al. (2017). Development of village doctors in China: Financial compensation and health system support. Int. J. Equity Health 16 (1), 9. doi:10.1186/s12939-016-0505-7
Hu, M., Yee, G., Zhou, N., Yang, N., Jiang, X., and Klepser, D. (2014). Development and current status of clinical pharmacy education in China. Am. J. Pharm. Educ. 78 (8), 157. doi:10.5688/ajpe788157
Huang, W., Yu, H., Liu, C., Liu, G., Wu, Q., Zhou, J., et al. (2017). Assessing health-related quality of life of Chinese adults in Heilongjiang using EQ-5D-3L. Int. J. Environ. Res. Public Health 14 (3), 224. doi:10.3390/ijerph14030224
Huang, Y., Huang, Q., Xu, A., Lu, M., and Xi, X. (2022). Patient preferences for diabetes treatment among People with type 2 diabetes mellitus in China: A discrete choice experiment. Front. Public Health 9, 782964. doi:10.3389/fpubh.2021.782964
Huang, Y., Yao, D., Zhou, H., Xi, X., Wang, Y., and Yao, W. (2021). Association of hospital pharmacy-related knowledge and skills with occupational stress of clinical pharmacists in tertiary hospitals of China. J. Am. Pharm. Assoc. 61 (3), 266–275. doi:10.1016/j.japh.2021.01.011
International Diabetes Federation (2021). IDF diabetes atlas. Available at: https://www.diabetesatlas.org/atlas/tenth-edition (Accessed October 10, 2022).
Jia, W., Zhang, P., Zhu, D., Duolikun, N., Li, H., Bao, Y., et al. (2021). Evaluation of an mHealth-enabled hierarchical diabetes management intervention in primary care in China (roadmap): A cluster randomized trial. PLoS Med. 18 (9), e1003754. doi:10.1371/journal.pmed.1003754
Jin, Y., Zhu, W., Yuan, B., and Meng, Q. (2017). Impact of health workforce availability on health care seeking behavior of patients with diabetes mellitus in China. Int. J. Equity Health 16 (1), 80. doi:10.1186/s12939-017-0576-0
Johnson, M., Jastrzab, R., Tate, J., Johnson, K., Hall-Lipsy, E., Martin, R., et al. (2018). Evaluation of an academic-community partnership to implement MTM services in rural communities to improve pharmaceutical care for patients with diabetes and/or hypertension. J. Manag. Care Spec. Pharm. 24 (2), 132–141. doi:10.18553/jmcp.2018.24.2.132
Kautzky-Willer, A., Harreiter, J., and Pacini, G. (2016). Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr. Rev. 37 (3), 278–316. doi:10.1210/er.2015-1137
Kiel, P. J., and McCord, A. D. (2005). Pharmacist impact on clinical outcomes in a diabetes disease management program via collaborative practice. Ann. Pharmacother. 39 (11), 1828–1832. doi:10.1345/aph.1G356
Koivusalo, S. B., Rönö, K., Klemetti, M. M., Roine, R. P., Lindström, J., Erkkola, M., et al. (2016). Gestational diabetes mellitus can be prevented by lifestyle intervention: The Finnish gestational diabetes prevention study (RADIEL): A randomized controlled trial. Diabetes Care 39 (1), 24–30. doi:10.2337/dc15-0511
Le, C., Rong, S., Dingyun, Y., and Wenlong, C. (2016). Socioeconomic disparities in type 2 diabetes mellitus prevalence and self-management behaviors in rural southwest China. Diabetes Res. Clin. Pract. 121, 9–16. doi:10.1016/j.diabres.2016.07.032
Lehn, J. M., Gerkin, R. D., Kisiel, S. C., O'Neill, L., and Pinderhughes, S. T. (2019). Pharmacists providing palliative care services: Demonstrating a positive return on investment. J. Palliat. Med. 22 (6), 644–648. doi:10.1089/jpm.2018.0082
Li, D., Hu, Y., Chen, H., Zhu, X., Wu, X., Li, J., et al. (2021). Identifying the subtypes and characteristics of mental workload among Chinese physicians in outpatient practice: A latent profile analysis. Front. Public Health 9, 779262. doi:10.3389/fpubh.2021.779262
Liu, X., Li, Y., Li, L., Zhang, L., Ren, Y., Zhou, H., et al. (2016). Prevalence, awareness, treatment, control of type 2 diabetes mellitus and risk factors in Chinese rural population: The RuralDiab study. Sci. Rep. 6, 31426. doi:10.1038/srep31426
Lum, Z. K., Siaw, M. Y. L., Lee, M. J. X., Koh, Z., Zhang, P. Q., Eng, S. K., et al. (2019). Impact of pharmaceutical care on mental well-being and perceived health among community-dwelling individuals with type 2 diabetes. Qual. Life Res. 28 (12), 3273–3279. doi:10.1007/s11136-019-02253-2
Manzoor, F., Wei, L., Hussain, A., Asif, M., and Shah, S. I. A. (2019). Patient satisfaction with health care services; an application of physician's behavior as a moderator. Int. J. Environ. Res. Public Health 16 (18), 3318. doi:10.3390/ijerph16183318
Marr, T. D., Pinelli, N. R., Jarmul, J. A., Waldron, K. M., Eckel, S. F., Cicci, J. D., et al. (2018). Continuous care provided through comprehensive medication management in an acute care practice model. Ann. Pharmacother. 52 (4), 314–324. doi:10.1177/1060028017738071
Matzke, G. R., Moczygemba, L. R., Williams, K. J., Czar, M. J., and Lee, W. T. (2018). Impact of a pharmacist-physician collaborative care model on patient outcomes and health services utilization. Am. J. Health Syst. Pharm. 75 (14), 1039–1047. doi:10.2146/ajhp170789
Miller, D. E., Roane, T. E., Salo, J. A., and Hardin, H. C. (2016). Evaluation of comprehensive medication review completion rates using 3 patient outreach models. J. Manag. Care Spec. Pharm. 22 (7), 796–800. doi:10.18553/jmcp.2016.22.7.796
O'Cathain, A., Murphy, E., and Nicholl, J. (2010). Three techniques for integrating data in mixed methods studies. BMJ 341, c4587. doi:10.1136/bmj.c4587
Oladapo, A. O., and Rascati, K. L. (2012). Review of survey articles regarding medication therapy management (MTM) services/programs in the United States. J. Pharm. Pract. 25 (4), 457–470. doi:10.1177/0897190012442715
Pan, X. F., Wang, L., and Pan, A. (2021). Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9 (6), 373–392. doi:10.1016/S2213-8587(21)00045-0
Paneerselvam, G. S., Aftab, R. A., Sirisinghe, R. G., Lai, P. S. M., and Lim, S. K. (2022). Study protocol: Effectiveness of patient centered pharmacist care in improving medication adherence, clinical parameters and quality of life among hemodialysis patients. PLoS One 17 (2), e0263412. doi:10.1371/journal.pone.0263412
Pang, S., Song, P., Sun, X., Qi, W., Yang, C., Song, G., et al. (2021). Dietary fructose and risk of metabolic syndrome in Chinese residents aged 45 and above: Results from the China national nutrition and health survey. Nutr. J. 20 (1), 83. doi:10.1186/s12937-021-00739-9
Professional Practice Committee (2018). Professional practice committee: Standards of medical care in diabetes-2018. Diabetes Care 41 (1), S3. PMID: 29222370. doi:10.2337/dc18-Sppc01
Saeedi, P., Petersohn, I., Salpea, P., Malanda, B., Karuranga, S., Unwin, N., et al. (2019). Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res. Clin. Pract. 157, 107843. doi:10.1016/j.diabres.2019.107843.157
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., et al. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 52 (4), 1893–1907. doi:10.1007/s11135-017-0574-8
Shahrami, B., Sefidani Forough, A., Najmeddin, F., Hadidi, E., Toomaj, S., Javadi, M. R., et al. (2022). Identification of drug-related problems followed by clinical pharmacist interventions in an outpatient pharmacotherapy clinic. J. Clin. Pharm. Ther. 47, 964–972. doi:10.1111/jcpt.13628
Shane-McWhorter, L., and Oderda, G. M. (2005). Providing diabetes education and care to underserved patients in a collaborative practice at a Utah community health center. Pharmacotherapy 25 (1), 96–109. doi:10.1592/phco.25.1.96.55623
Shao, H., Chen, G., Zhu, C., Chen, Y., Liu, Y., He, Y., et al. (2017). Effect of pharmaceutical care on clinical outcomes of outpatients with type 2 diabetes mellitus. Patient Prefer Adherence 11, 897–903. doi:10.2147/PPA.S92533
Shao, Z. J., Han, N., Qiu, C. Y., Wei, L., and Liu, R. X. (2022). Investigation and analysis of diabetic knowledge awareness among type 2 diabetic patients in county area of Guizhou Province. South China J. Prev. Med. 48 (1), 132–134. doi:10.12183/j.scjpm.2022.0132
Song, Z., Hu, Y., Ren, Z., Wang, G., Liu, S., Zheng, S., et al. (2022). Optimal management of the public and patients by pharmacists in the era of COVID-19: An evidence-based review and practical recommendations. Front. Public Health 9, 758325. doi:10.3389/fpubh.2021.758325
Tan, S. L., Xiao, J., Yuan, H. Y., Chen, L., Wang, Q., Xiang, D. X., et al. (2022). Establishing and evaluating physician-pharmacist collaborative clinics to manage patients with type 2 diabetes in primary hospitals in hunan province: Study protocol of a multi-site randomized controlled trial in the era of COVID-19 pandemic. BMC Health Serv. Res. 22 (1), 299. doi:10.1186/s12913-022-07653-8
Wallace, A. S., Carlson, J. R., Malone, R. M., Joyner, J., and Dewalt, D. A. (2010). The influence of literacy on patient-reported experiences of diabetes self-management support. Nurs. Res. 59 (5), 356–363. doi:10.1097/NNR.0b013e3181ef3025
Wang, C., Yu, Y., Zhang, X., Li, Y., Kou, C., Li, B., et al. (2014). Awareness, treatment, control of diabetes mellitus and the risk factors: Survey results from northeast China. PLoS One 9 (7), e103594. doi:10.1371/journal.pone.0103594
Wang, L., Peng, W., Zhao, Z., Zhang, M., Shi, Z., Song, Z., et al. (2021). Prevalence and treatment of diabetes in China, 2013-2018. JAMA 326 (24), 2498–2506. doi:10.1001/jama.2021.22208
Wang, N., Qiu, S., Yang, Y., Zhang, C., Gu, Z. C., and Qian, Y. (2021). Physician-pharmacist collaborative clinic model to improve anticoagulation quality in atrial fibrillation patients receiving warfarin: An analysis of time in therapeutic range and a nomogram development. Front. Pharmacol. 12, 673302. doi:10.3389/fphar.2021.673302
Wang, Y., Hu, X. J., Wang, H. H. X., Duan, H. Y., Chen, Y., Li, Y. T., et al. (2021). Follow-up care delivery in community-based hypertension and type 2 diabetes management: A multi-centre, survey study among rural primary care physicians in China. BMC Fam. Pract. 22 (1), 224. doi:10.1186/s12875-021-01564-z
Wei, E. T., Gregory, P., Halpern, D. J., Felton, M., Goldstein, B. A., Yeatts, J., et al. (2022). Impact of a clinical pharmacist on provider prescribing patterns in a primary care clinic. J. Am. Pharm. Assoc. 62 (1), 209–213. e1. doi:10.1016/j.japh.2021.10.007
Wen, J., Cheng, Y., Hu, X., Yuan, P., Hao, T., and Shi, Y. (2016). Workload, burnout, and medical mistakes among physicians in China: A cross-sectional study. Biosci. Trends 10 (1), 27–33. doi:10.5582/bst.2015.01175
World Health Organization (2022). Global health workforce statistics database. Available at: https://www.who.int/data/gho/data/themes/topics/health-workforce (Accessed October 10, 2022).
Xu, W. H., Wang, Q., and Liang, W. X. (2008). Development of a medication compliance scale in patients with chronic diseases. Chin. J. Prey Contr Chron. Dis. 16, 558–560.
Yoon, S., Ng, J. H., Kwan, Y. H., and Low, L. L. (2022). Healthcare professionals' views of factors influencing diabetes self-management and the utility of a mHealth application and its features to support self-care. Front. Endocrinol. (Lausanne) 13, 793473. doi:10.3389/fendo.2022.793473
Zhang, Q., Su, H., Li, B., Bai, X., Yan, S., and Li, X. (2022). Physician-pharmacist collaborative management in patients after percutaneous coronary intervention: A retrospective propensity score matching cohort study. Int. J. Clin. Pharm. 44 (1), 90–99. doi:10.1007/s11096-021-01316-0
Zhao, L. B., Chen, Q. D., Zhou, Y. X., Wang, Q. Q., Su, L. Z., Lu, L., et al. (2004). Application of control status scale in type 2 diabetic patients. Chin. J. Endocrinol. Metab. 4, 318–322.
Keywords: medication compliance, quality of life, diabetes milletus, pharmacist, primary healtcare
Citation: Xiao J, Wang Q, Tan S, Chen L, Tang B, Huang S, Zhou Y and Xu P (2023) Analysis of patient medication compliance and quality of life of physician-pharmacist collaborative clinics for T2DM management in primary healthcare in China: A mixed-methods study. Front. Pharmacol. 14:1098207. doi: 10.3389/fphar.2023.1098207
Received: 14 November 2022; Accepted: 16 March 2023;
Published: 24 March 2023.
Edited by:
Hong Cheng, Zhongnan Hospital, Wuhan University, ChinaReviewed by:
Mohamed Hassan Elnaem, University of Science Malaysia (USM), MalaysiaRongsheng Zhao, Peking University Third Hospital, China
Jiaxing Zhang, Guizhou Provincial People’s Hospital, China
Copyright © 2023 Xiao, Wang, Tan, Chen, Tang, Huang, Zhou and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Xu, eHVwaW5nMTEwOUBjc3UuZWR1LmNu
 Jie Xiao1,2
Jie Xiao1,2 Shenglan Tan
Shenglan Tan Bingjie Tang
Bingjie Tang Yangang Zhou
Yangang Zhou Ping Xu
Ping Xu