- 1School of Pharmacy, Dr. Vishwanath Karad MIT World Peace University, Pune, India
- 2Drug Testing Laboratory, Drug Control Department, Bangalore, India
- 3Koringa College of Pharmacy, East Godavari, India
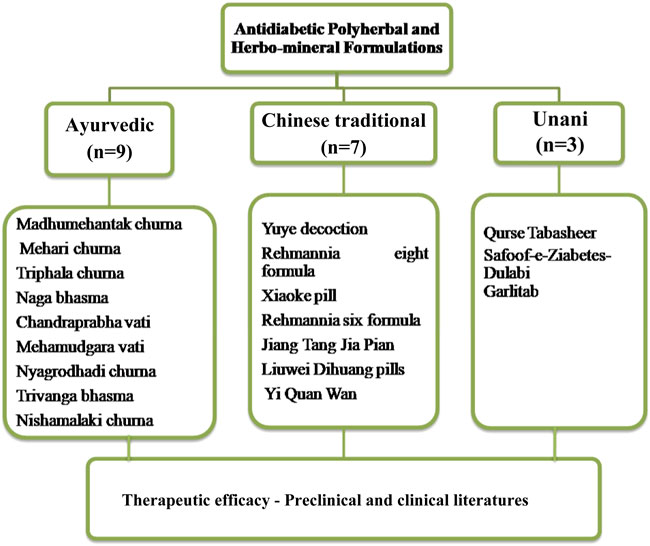
Diabetes mellitus is the most widely recognized endocrine disorder which is influencing a bigger populace on the planet. There are various causes of diabetes, such as physical inactivity, obesity, family history, race, and age. Diabetes mellitus is associated with some life-threatening complications, such as neuropathy, nephropathy, various eye diseases or retinopathy, and cardiovascular disorders. Many synthetic antihyperglycemic agents are available in the market for the treatment of diabetes and its complications. But, due to some serious side effects of these synthetic agents, people are opting for herbal remedies and, therefore, they are now becoming popular. Herbal remedies have lesser side effects and higher affordability and therefore can be preferably used over synthetic agents for a long-term disorder like diabetes mellitus. In the present study, scientific research and review studies on the topic were collected from Science Direct, Scopus, PubMed, Google Scholar, and other relevant sources. The references of all the articles were screened manually for any additional information on popular polyherbal formulations in traditional Ayurvedic, Chinese, and Unani medicinal systems. It is found that these polyherbal formulations are studied for anti-diabetic potential. Furthermore, some are also investigated for mechanism of action of anti-diabetic effects. This review highlights various Ayurvedic, Chinese, and Unani polyherbal formulations commonly utilized in the management of diabetes mellitus along with their pre-clinical and clinical investigations, which will enhance the existing knowledge of the researchers.
Introduction
Diabetes mellitus is a disorder characterized by chronic hyperglycemia in which insulin secretion, insulin action, or both are defective (Kharroubi 2015). It causes life-threatening complications such as neuropathy, nephropathy, various eye diseases or retinopathy, cardiovascular disorders, etc., if left untreated. As per the World Health Organization, about 422 million of the global population, particularly in low- and middle-income countries, is suffering from diabetes mellitus. This high prevalence of diabetes is leading to an excessive burden on public medical service budgets. Diabetes is projected to be one of the principal life-threatening disorders of the globe within the next 25 years. There are various drugs, such as insulin preparations and oral hypoglycemic agents, available for treatment of diabetes mellitus. Despite these, numerous traditional and alternative therapies are popular among people for management of the diabetic condition (https://www.who.int/news-room/fact-sheets/detail/diabetes).
In traditional systems of medicine, various medicinal herbs and herbal-based formulations have been recognized and found to be effective for diabetes mellitus. These traditional herbal medicines have been commonly used due to their cost-effectiveness and lesser side effects (Nagappa et al., 2003). Countries with ancient civilizations, such as China, India, and Egypt, are still utilizing several herbal-based formulations for different health conditions, including diabetes mellitus (Sharma et al., 2008). These polyherbal formulations are safe and effective as compared to the single-herb formulation (Petchi et al., 2014). There is a curiosity among common people and researchers to obtain information about various herbal-based formulations used in traditional systems of medicines for the management of diabetes mellitus. With this background, the present review highlights pre-clinical and clinical aspects of various polyherbal formulations commonly used in Ayurveda, Chinese traditional and Unani systems of medicines for diabetes mellitus.
Methods
Scientific research and reviews on the topic were collected from Science Direct, Scopus, PubMed, Google Scholar, and other sources. Articles from the journals indexed in Scopus, Web of Science, and UGC care list were selected for further study. Also, the references of all the articles were screened manually for any additional information on popular polyherbal and herbo-mineral formulations in traditional Ayurvedic, Chinese, and Unani medicine.
Ayurvedic antidiabetic polyherbal formulations
In Ayurveda, single or multiple herbs (polyherbal) are utilized for treatment of health problems. The idea of polyherbalism was attributed to the Ayurvedic writing Sarangdhar Samhita. Individual plants and their phytoconstituents are insufficient to achieve desired beneficial effects. When multiple herbs are combined or polyherbal formulations are prepared or formulated in a particular ratio, they provide a better therapeutic effect and reduce the toxicity of herbs (Parasuraman et al., 2014).
In herbal preparations, a variety of therapeutic plants, known as Rasayana, have been used for over 1,000 years. Many Ayurveda practitioners formulate their own Ayurvedic formulations and dispense them to the patients for clinical benefits (Modak et al., 2007). Some of the commonly used Ayurvedic antidiabetic formulations are Madhumehantak churna, Mehari churna, Triphala churna, Naga bhasma, Chandraprabha vati, Mehamudgara vati, Nyagrodhadi churna, Trivanga bhasma, and Nishamalaki churna (Table 1).
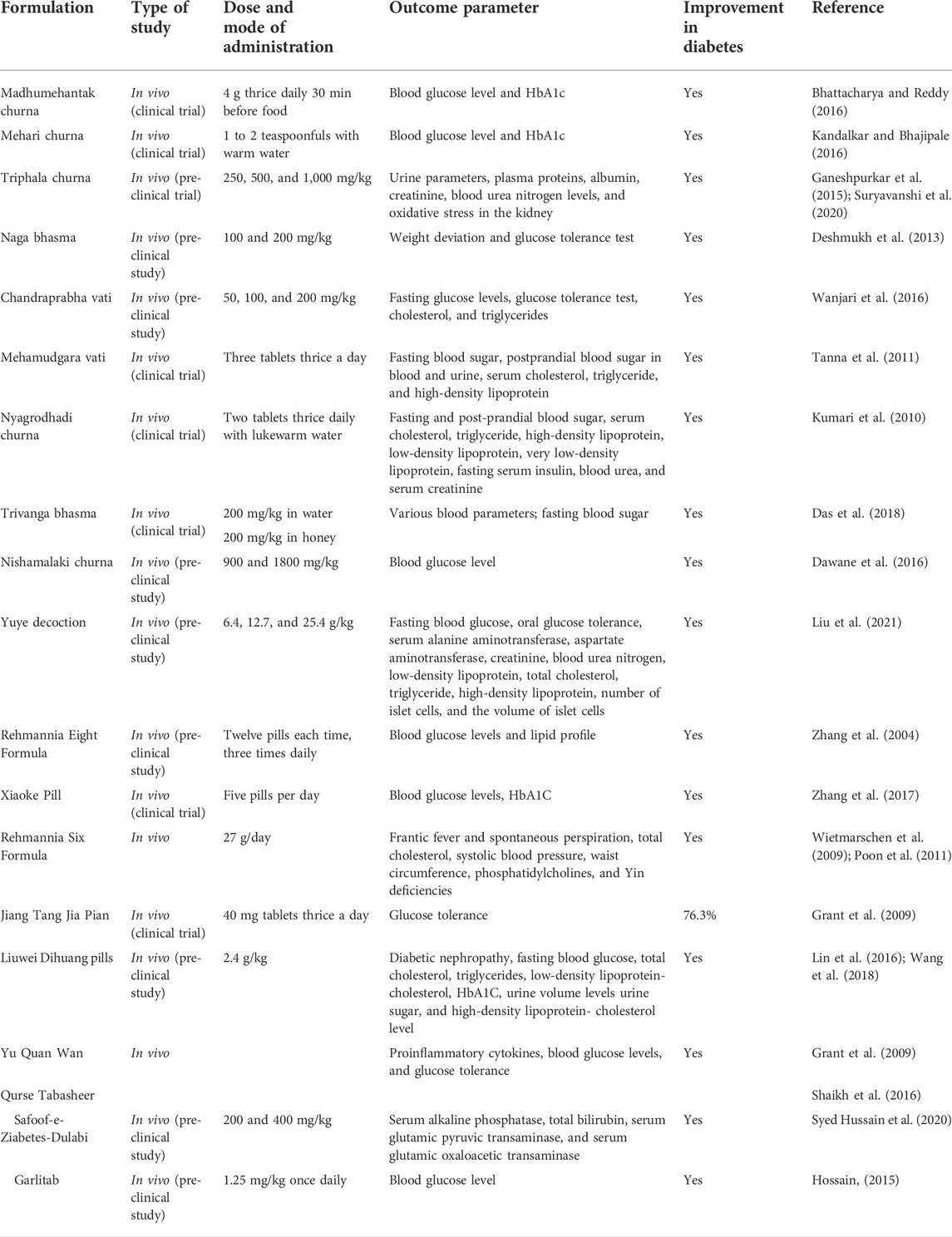
TABLE 1. Summary of the various formulations of Ayurveda, Chinese, and Unani medicine systems used for the management of diabetes.
Madhumehantak churna
The Madhumehantak churna (MMC) is one of Ayurvedic polyherbal formulations. This formulation is a combination of eleven herbs individually having reported antidiabetic activity, namely, amra-beej-majja (Mangifera indica Linn. seed) (Ganogpichayagrai et al., 2017), karavella phalli (Momordica charantia Linn. fruits) (Welihinda et al., 1986), jambubeej (Syzygium cumini Linn. fruits) (Kumar et al., 2008), nimbabeej (Azadirachta indica Linn. seeds) (Patil et al., 2013), palandubeej (Allium sepa Linn. seeds) (Mathew and Augusti 1975), babbula phalli (Acacia nilotica Linn. fruits) (Ahmad et al., 2008), balabeej (Sida cordifolia Linn. seeds) (Kaur et al., 2011), Methikabeej (Trigonella foenum-graecum Linn. fruits) (Ghosh et al., 2009), meshashrungi (Gymnema sylvestre R. Br.) (Baskaran et al., 1990), haridra (Curcuma longa Linn.) (Lekshmi et al., 2014), and haritaki-phala-majja (Terminalia chebula R. fruits) (Borgohain et al., 2012; Bhattacharya and Reddy 2016).
An experimental preclinical study was performed on laboratory animals. Diabetic rats were treated with MMC for 28 days to prove that MMC is safe and effective. The effect of MMC on blood glucose showed a lowering of blood glucose effectively at two doses, 216 and 648 mg/kg, when compared with diabetic control group. The dose of 216 mg daily to rats is equivalent to 1 karsa ∼12 g dose, recommended by Ayurveda as an optimal human dose (Bhattacharya and Reddy 2016).
A clinical study was also performed with a total of 101 out-patients placed into three groups. They were treated with MMC for three continuous months, preceded and followed by an assessment of long-term glucose control using glycated hemoglobin (HbA1c) testing. The MMC was found effective in lowering blood glucose and HbA1c in diabetic patients (Bhattacharya and Reddy 2016).
Mehari churna
Mehari churna is a commonly used antidiabetic polyherbal formulation in Ayurveda. This formulation is a powder of various herbs helpful in treating pre-diabetes conditions and diabetes mellitus. It consists of various Ayurvedic ingredients possessing antidiabetic potentials like turmeric (Curcuma longa Linn.) (Kuroda et al., 2005), amla (Emblica officinalis Gaertn.) (Akhtar et al., 2011), jamun (Syzygium cumini Linn.) (Kandalkar and Bhajipale 2016), guduchi (Tinospora cordifolia Thunb. Miers) (Patel and Mishra 2011), manjishtha (Rubia cordifolia Linn.) (Rani et al., 2013), methi (Trigonella foenum-gracecum Linn.) (Al-Juraisy 2014), and hirda (Terminalia chebula R.) (Borgohain et al., 2012).
Mehari churna helps to reduce symptoms of diabetes. It normalizes the blood glucose level by enhancing insulin release from the beta cells of the pancreas and thereby prevents diabetes and diabetic complications. Mehari churna stimulates pancreatic action and improves the release of insulin. This churna also improves the overall lipid profile by lowering low-density lipoprotein or low-density cholesterol. It also reduces excessive urination and glycosuria (Kandalkar and Bhajipale 2016).
Triphala churna
Triphala churna is a well-recognized and highly efficacious Ayurvedic polyherbal formulation. It consists of fruits of the antidiabetic plants, namely, amla (Emblica officinalis Gaertn.) (Akhtar et al., 2011), beheda (Terminalia bellerica gaertn. Roxb) (Gupta et al., 2020), and hirda (Terminalia chebula R.) (Borgohain et al., 2012). Triphala churna is an antioxidant-rich polyherbal formulation having diverse beneficial properties. As per the Ayurvedic Formulary of India (AFI), Triphala churna is prepared by mixing amla, behda, and hirda in a ratio of 1:1:1. Triphala churna has immune-modulatory properties and, therefore, it helps in improving the body’s defense system (Prativadibhayankaram et al., 2008).
Triphala churna has antidiabetic activity and also treats some of its complications. It is evaluated for diabetic nephropathy in streptozotocin-induced diabetic rats. The diabetic rats were treated with Triphala churna at doses of 250, 500, and 1,000 mg/kg for 4 weeks. Results showed that treatment with Triphala churna significantly improves urine parameters. It also caused improvement in various biochemical parameters, such as plasma proteins, albumin, creatinine, and blood urea nitrogen levels. After treatment with Triphala churna, oxidative stress was reduced in the kidney. Histopathology showed that Triphala churna decreases renal or kidney damage in experimental rats and helps in treating diabetic nephropathy (Ganeshpurkar et al., 2015; Suryavanshi et al., 2020).
Naga bhasma
Naga bhasma is an ancient Ayurvedic herbo-mineral formulation. It contains Naga which is also known as calcinated lead. The complex found in Naga bhasma is known as lead sulfide. This lead sulfide is mixed with plant materials and may contain a variety of mineral deposits of plants. Antidiabetic properties of Naga bhasma were found around the 12th century CE. Naga bhasma mainly contains antidiabetic constituents, namely, haridra (Curcuma longa L.) (Kuroda et al., 2005), amalaki (Emblica officinalis Gaertn.) (Akhtar et al., 2011), guduchi (Tinospora cordifolia (Thunb.) Miers) (Patel and Mishra 2011), and madhu (honey) (Hemmati et al., 2015). Naga bhasma, therefore, shows antidiabetic activity and is also capable of treating diabetic complications (Tate et al., 2009).
A preclinical study was carried out for assessment of the antidiabetic effect of Naga bhasma in alloxan-induced diabetic rats. Naga bhasma was given at a dose of 100 and 200 mg/kg for 14 days in the form of suspension with milk by oral gavage to the normal and alloxan-induced diabetic rats. Glucose tolerance test was conducted in experimental rats. In this study, glibenclamide was used as a standard drug. It was observed that treatment with Naga bhasma regularized the impaired glucose tolerance on long-term treatment. It was, therefore, concluded that Naga bhasma has an antidiabetic effect and also treats diabetic complications (Tate et al., 2009; Deshmukh et al., 2013).
Chandraprabha vati
Chandraprabha vati is an ancient Ayurvedic polyherbal formulation. This formulation is notably utilized for improvement of Prameha i.e., diabetes (Baskaran et al., 1990). This formulation is known to have potent anti-inflammatory properties and is also used to treat diseases of the urinary tract, thyroid gland, kidney, pancreas, bones, and joints. It contains thirty-seven herbo-mineral ingredients. Many of these ingredients such as Acorus calamus Linn. (Prisilla et al., 2012), Cyperus rotundus Linn. (Singh et al., 2015), Phyllanthus niruri Linn. (Okoli et al., 2010), Tinospora cordifolia Thunb. Miers (Patel and Mishra 2011), Curcuma longa Linn. (Lekshmi et al., 2014), Berberis aristata DC. (Upwar et al., 2011), Piper longum Linn. (Nabi et al., 2013), Coriandrum sativum Linn. (Naquvi et al., 2004), Terminalia chebula Retz. (Borgohain et al., 2012), Terminalia belerica Gaertn. Roxb. (Gupta et al., 2020), Embelica officinalis Gaertn. (Akhtar et al., 2011), Embelia ribes Burm. f. (Bhandari et al., 2013), Zingiber officinale Roscoe. (Al-Amin et al., 2006), Piper nigrum Linn. (Kaleem et al., 2005), Hordeum vulgare Linn. (Deng et al., 2020), Ipomoea turpethum Linn. (Pulipaka et al., 2012), and Cinnamomum zeylanicum Linn. (Verspohl et al., 2005) showed remarkable antidiabetic effects in several studies.
The antihyperglycemic effect of Chandraprabha vati was studied in Wistar rats. This formulation was administered at the doses of 50, 100 and 200 mg/kg orally for 7 days to alloxan-induced diabetic rats. An oral glucose tolerance test was also performed. Fasting glucose levels were determined at different time intervals. Cholesterol and triglyceride levels were also measured. Metformin (500 mg/kg orally) was used as a standard drug (Tate et al., 2009). It was concluded that Chandraprabha vati has an antihyperglycemic and antihyperlipidemic effects. The findings support the use of Chandraprabha vati in clinical practice for diabetes mallitus (Wanjari et al., 2016).
Mehamudgara vati
The Mehamudgara vati is an Ayurvedic herbo-mineral formulation containing Lauha bhasma, guggulu (Commiphora wightii (Arnott) Wightii), haritaki (Terminalia chebula R.), bibhitaki (Terminalia bellerica Gaertn. Roxb), amalaki (Embelica officinalis Gaertn.), shunthi (Zingiber officinalis Roscoe.), marich (Piper nigrum Linn.), pippali (Piper longum Linn.), trivrita (Operculina terpethum L.), pippalimula (Piper longum Linn.), Bidalavana, bilva (Aegle marmelos Linn.), gokshura (Tribulus terrestris Linn.), dadima (Punica granatum Linn.), devadaru (Cedrus deodara Roxb. G.Don), rasanjana (Berberis aristata DC.), Kiratatikta (Swertia chirayita Linn.), and Triphala kwatha. Mehamudgara vati is well known for its hypolipidemic, hypocholesterolemic, antihyperglycemic, and antioxidant activities, which make this medicine beneficial for diabetic patients.
The clinical efficacy of Mehamudgara vati (MMV) was studied in type 2 diabetic patients (Tanna et al., 2011). In this study, one group of patients with mild-to-moderate type 2 diabetes was given three tablets of MMV, thrice a day for 3 months. In another group, the type 2 diabetic patients who took modern antidiabetic treatment but with uncontrolled diabetes were additionally given MMV in the same manner. The MMV was found to be highly effective in decreasing both fasting as well as postprandial blood sugar levels. Furthermore, it is established that MMV has synergistic action when combined with modern antidiabetic drugs (Tanna et al., 2011).
Nyagrodhadi churna
Chakradatta, an Ayurvedic text, mentions Nyagrodhadi churna, which is converted into ghanvati for improving patient compliance. This formulation contains antidiabetic plants namely vata (Ficus benghalensis Linn.), udumber (Ficus racemosa Linn.), aswatha (Ficus religiosa Linn.), bijaka (Pterocarpus marsupium f.), Amra (Magnifera indica Linn.), jambu (Syzygium samarangense Blume.), arjuna (Terminalia arjuna Roxb.), dhava (Anogeissus latifolia Roxb.), paribhadra (Erythrina orientalis Murr.), meshashringi (Gymnema sylvestre R. Br.), chitrak (Plumbago zeylanica Linn.), karanja (Millettia pinnata Linn.), triphala, kutaja (Holarrhena pubescens Wall.), and bhallataka (Semecarpus anacardium Linn.). Amalaki (Emblica officinalis Gaertn.), a constituent of Nyagrodhadi churna, is an immunomodulator along with an antihyperglycemic effect and thus may be used in autoimmune diabetes mellitus (Kumari et al., 2010). Similar effects are found in bhallataka (Semecarpus anacardium Linn.), haritaki (Terminalia chebula Retz.), mulethi (Glycyrrhiza glabra Linn.), madhuka (Madhuca longifolia J. Konig.), dhava (Anogeissus latifolia Roxb.), etc. The herbs like bijaka (Pterocarpus marsupium f.), arjuna (Terminalia arjuna Roxb.), chitraka (Plumbago zeylanica Linn.), patola (Cucumis acutangulus Linn.), meshashringi (Gymnemasylvestre R. Br.), amalaki (Emblica officinalis Gaertn.), haritaki (Terminalia chebula Retz.), etc. have a hypolipidemic action (Simha and Laxminarayana, 2007; Kumari et al., 2010).
Trivanga bhasma
Trivanga bhasma (TB) is a metallic preparation containing bhasmas of Naga, Vanga, and Yashada, i.e., lead, tin, and zinc, respectively (Jamadagni et al., 2017). Sprague Dawley rats were injected with streptozotocin (STZ) to induce diabetes followed by dosing of drugs (TB with herbal ingredients (bhawna) and without herbal ingredients) in a human equivalent therapeutic dose i.e., 200 mg/kg for 30 days. Various blood parameters and histopathology of organs were analyzed to evaluate the antidiabetic effect and reveal the side effects of the drugs. TB with herbal ingredients showed better antidiabetic effects in STZ-induced diabetic rats. In the prophylactic study, Trivanga bhasma-treated animals had lower blood sugar levels than non-treated rats even after injecting them with STZ. After treatment with TB for 30 days, the fasting blood sugar level of diabetic animals was significantly lower than that of diabetic control animals in a curative study (Das et al., 2018).
Nishamalaki churna
This herbal preparation contains two ingredients amla (Emblica officinalis Gaertn.) and turmeric (Curcuma longa L.). Amla and turmeric are mixed in equal parts to prepare Nishamalaki churna. In Ayurveda, Nishamalaki churna was recommended to treat the initial phase of diabetes mellitus. This formulation also possesses antioxidant and neuroprotective properties (Das et al., 2018).
A preclinical study was carried out to determine the antidiabetic effect of Nishamalaki churna. In this study, diabetes was induced by intraperitoneal administration of streptozotocin at a dose of 35 mg/kg to the rats. A high-fat, high-fructose diet was also given along with streptozotocin injection. The diabetic animals were treated with Nishamalaki churna at a dose of 900 and 1800 mg/kg for 12 weeks and blood glucose levels were determined after 15 days. Rats were also examined for their lipid profile. For determination of thermal hyperalgesia and cold allodynia, methods like Eddy’s hot plate and tail immersion method were used. Results of the study showed that diabetic rats treated with Nishamalaki churna have an improvement in thermal hyperalgesia and cold allodynia. Nishamalaki churna was found to lower blood sugar levels and thus possesses anti-diabetic activity (Dawane et al., 2016).
Chinese antidiabetic polyherbal formulations
Traditional Chinese Medicine (TCM) is a holistic system of medicines that focuses on increasing the body’s resilience to illness. TCM uses herbal therapeutic strategies to improve health (Lu et al., 2004). Commonly used Chinese antidiabetic formulations are Yuye decoction, Rehmannia eight formula, Xiaoke pill, Rehmannia six formula, Jiang Tang Jia Pian, Liuwei Dihuang pills, and Yi Quan Wan (Table 1).
Yuye decoction
Yuye decoction (YYD) is a traditional Chinese polyherbal formulation. This formulation was first mentioned in the customary Chinese medication volume called “yixuezhongzhongcanxilu”. This formulation is utilized in traditional Chinese medication to treat diabetes mellitus, essentially type 2 diabetes mellitus (Liu et al., 2021). There are seven medicinal herbs that compose Yuye decoction, namely, Dioscorea L, Astragalus membranaceus Fisch, Trichosanthes kirilowii Maxim., Anemarrhena asphodgfoides Bunge, Schisandra chinensis Turcz, Gallus gallusdomesticus Brisson, and Pueraria lobata Maesen.
For preclinical evaluation, rats with type 2 diabetes mellitus were used in the study (Liu et al., 2021). Diabetic condition was induced in rats by administration of high-fat, high-glucose diet for 6 weeks. Later, the diabetic rats were randomly divided into the diabetic group, the metformin (90 mg/kg) control group, and the modified Yuye decoction (6.4 g/kg, 12.7 g/kg, 25.4 g/kg) groups. The drug was administered for 4 weeks, and fasting blood glucose was monitored. After 4 weeks of treatment, oral glucose tolerance test was carried out. Results from fasting blood glucose and oral glucose tolerance test showed that modified Yuye decoction significantly improves the blood glucose levels and insulin resistance. In addition, modified Yuye decoction significantly reduced the serum levels of alanine aminotransferase, aspartate aminotransferase, creatinine, blood urea nitrogen, low-density lipoprotein, total cholesterol and triglycerides, whereas it increased the level of high-density lipoprotein. At the same time, hematoxylin–eosin staining of pancreas, liver and kidney tissues showed that modified Yuye decoction increases the number of islet cells, reduces the volume of islet cells, improves liver edema and inflammation, and improves renal glomerular hypertrophy (Liu et al., 2021).
Rehmannia eight formula
Rehmannia Eight Formula is well known, Chinese traditional formulation. It consists of Chinese foxglove root (Rehmannia glutinosa Gaertn.) (Zhang et al., 2004), Japanese cornel fruit (Cornus officinalis Torr.) (Kim 2005), Chinese yam (Dioscorea polystachya Turcz.) (Maithili et al., 2011), poria mushroom (Poriacocos sclerotium Peck.) (Lee et al., 2014), horny goat weed (Epimedium grandiflorum C. Morren.), water plantain (Alisma plantago Linn.), astragalus (Astragalus membranaceus Fisch.) or moutan root bark (Paeonia suffruticosa Andrews.) (He et al., 2011) and Chinese cinnamon bark (Cinnamomum cassia L.).
Rehmannia Eight Formula has an antidiabetic effect due to various herbal constituents. It is also known for blood glucose and lipid-lowering properties. Cornus officinalis Torr. and Alisma plantago Linn. are ingredients in the formula, which help to maintain blood glucose levels and improve the lipid profile. Cinnamon in Rehmannia Eight Formula prevents diabetes by lowering fasting blood glucose levels (Zhang et al., 2004).
Xiaoke pill
Xiaoke Pill is a polyherbal formulation utilized for management of type 2 diabetes mellitus (Zhang et al., 2017). Xiaoke Pill consists of Radix Puerariae, Radix Rehmanniae, Radix Astragali, Fructus Schisandrae Sphenantherae, Rhizoma Dioscoreae, Radix Trichosanthis, and Stylus Zeae Maydis. The clinical outcome of Xiaoke Pill showed that it has greater glucose-lowering property (Zhang et al., 2017).
Rehmannia six formula
This Chinese formula is used for the treatment of diabetes mellitus. There are a total of six Chinese herbs in this formulation, i.e., Rehmannia glutinosa Gaertn. (Zhang et al., 2004), Fructus corni (Cornus officinalis Sieb.) (Kim 2005), Dioscorea opposita Linn. (Maithili et al., 2011), Poriacocos (Wolfiporia extensa Peck.) (Lee et al., 2014), Alisma orientalis Sam, and Paeoniasuf fruticosa Andrews.
For the assessment of Rehmannia Six Formula, a clinical study was conducted in which various clinical parameters were measured. Symptoms like hectic fever and spontaneous perspiration were observed to be alleviated during this treatment time (Wietmarschen et al., 2009). There are evidences that plasma glucose levels of rats was reduced by treatment of this formulation but in humans, it did not show any effects on plasma glucose levels (Poon et al., 2011). Total cholesterol, systolic blood pressure, and waist circumference were also lowered (Wietmarschen et al., 2009).
Jiang Tang Jia Pian
Jiang Tang Jia Pian is used in Chinese traditional medicine to treat diabetes mellitus. This formulation contains various Chinese herbs, namely, astragalus (Astragalus membranaceus Fisch.) (Yin et al., 2009), polygonatum (Polygonatum kingianum Mill.) (Lu et al., 2016), trichosanthes root (Zhang et al., 2004), pseudostellaria (Pseudostellaria heterophylla R.) (Hu et al., 2013), and rehmannia (Rehmannia glutinosa Gaertn.) (Yin et al., 2009). This formula is mainly suggested for patients who are capable of producing low insulin (Zhang et al., 2004). Clinical studies were performed to check the efficacy of Jiang Tang Jia Pian. The results showed that Jiang Tang Jia Pian can be considered for people with impaired glucose tolerance and it also reduces the incidence of diabetes (Grant et al., 2009).
Liuwei Dihuang pills
Liuwei Dihuang pill formula in is a Chinese traditional medicine for treatment of diabetic nephropathy and also used as a dietary supplement (Lin et al., 2016). It contains Rehmannia glutinosa (Gaertn.) Steud, Cornus officinalis Torr, Paeonia suffruticosa Andrews, Dioscorea opposite Thunb, Poriacocos Fr., and Alisma orientalis Sam.
Clinical study was performed in order to check the effect of Liuwei Dihuang pills. The result showed that Liuwei Dihuang pills when given daily to the patients with diabetic nephropathy causes improvement in kidney function (Lin et al., 2016; Wang et al., 2018).
Yu Quan Wan
This traditional Chinese formula is used to treat diabetes patients at a dose of 50 gm daily. This formulation is also known as Jade Spring Pills. It consist of various herbal Chinese ingredients, such as licorice (Glycerrhiza glabra Linn.) (Takii et al., 2001), pueraria (Wu et al., 2013), schizandra (Schizandra repanda Linn.) (Wu et al., 2013), and trichosanthes roots (Trichosanthes cucumerinia Linn.) (Arawwawala et al., 2009). It is helpful in the proper functioning of islets of Langerhans and are therefore used to treat early-phase diabetes. Preclinical studies showed that Yu Quan Wan improves liver glycogen levels. In clinical studies, Yu Quan Wan improved proinflammatory cytokines in patients with type 2 diabetes mellitus. It has significant glucose-lowering property and is thus recommended for treatment of diabetes mellitus (Grant et al., 2009).
Unani antidiabetic polyherbal formulations
The Unani System of medicine is Greco–Arabic medicine, which is based on the knowledge of Greek and Roman physicians. It is not only the original science of medicine but also a rich storehouse of principles and philosophies of medicine that can be of immense value to medicine in general and science in particular (Ansari et al., 2017). Some of the Unani antidiabetic formulations are Qurse Tabasheer, , Safoof-e-Ziabetes-Dulabi, and Garlitab (Table 1).
Qurse Tabasheer
Qurse Tabasheer contains six ingredients, namely, Tabasheer (Siliceous concretions) (Bambosa arundinaceae Retz.) (Jayarambabu et al., 2021), GuleSurkh (Rosa damascena Mill. flower) (Gholamhoseinian and Fallah 2009), Gulnar (Punica granatum Linn. flower) (Li et al., 2009), Tukhmekahu (Lactucasatisva Linn. seeds) (Bagri et al., 2009), Tukhmekhurfa (Portulaca oleraceae Linn. seeds) (Li et al., 2009), and Gile Armani (Armenian bole) (Ahmed et al., 2013). This particular formulation is mentioned in Unani texts, Bayaaze Kabeer and Kitabul Murakkabat Al Maroof Makhzanul Murakkabat. It is used in the treatment of Dhayabitus (diabetes), Hummae Hadda (acute fever), and Is’hal (diarrhea). Moreover, this formulation has been reported to possess hypoglycemic activity (Shaikh et al., 2016).
Safoof-e-Ziabetes Dulabi
Safoof-e-Ziabetes-Dulabi is an Unani polyherbal preparation widely given for Ziabetussadiq and Zof-e-kulya. Ziabetussadiq is known as diabetes mellitus, and Zof-e-kulya is known as kidney disease. This formulation consists of six herbal ingredients, namely, Gular (Ficus racemosa Linn.) (Veerapur et al., 2012), Gulnarfarsi (Punica granatum Linn) (Bagri et al., 2009), Dana anarshireen (Punica granatum Linn.), Maghz-eTukhm-e-Anba (Aderibigbe et al., 2001), Kishneez Khushk (Naquvi et al., 2006), and Gil-e-Armani alongwith Qand Safaid (sugar). This preparation has antidiabetic, anticancer, and immunomodulatory activities.
An acute oral toxicity study of Safoof-e-Ziabetes-Dulabi (SZD) was conducted on Swiss albino mice and, the result of the toxicity study showed no toxicity at a dose of 2,000 mg/kg (Syed Hussain et al., 2020). The antidiabetic activity of SZD was evaluated in streptozotocin-induced diabetic rats. Various biochemical parameters were evaluated in the study. It was observed that when diabetic rats were given SZD at doses of 200 mg/kg and 400 mg/kg for 8 weeks, their body weight increased significantly as compared to that of the diabetic control group. It was also observed that the blood glucose levels and glycated hemoglobin were reduced in SZD-treated groups when compared with diabetic control. A liver function test was also performed to evaluate the safety profile of SZD. Treatment with SZD at 200 and 400 mg/kg for 8 weeks caused significant decrease in serum levels of alkaline phosphatase, total bilirubin, serum glutamic pyruvic transaminase (SGPT), and serum glutamic oxaloacetic transaminase (SGOT) when compared with the diabetic control group. Thus, the results suggested that SZD possesses antidiabetic activity (Syed Hussain et al., 2020).
Garlitab
Garlic is the most recommended Unani medicine for health benefits. This formulation consists of garlic (Allium sativum L.) (Eidi et al., 2006), onion (Allium sepa L.) (Mathew and Augusti 1975), and clove (Syzygium aromaticum L.) (Kuroda et al., 2015). It also contains other constituents such as allicin, volatile oil, minerals, and vitamins, which are essential for good health (Hossain 2015).
In a preclinical study, the efficacy of Garlitab was evaluated. A formulation of garlic, onion, and clove was evaluated in streptozotocin-induced diabetic rats. The blood glucose level and body weight were measured. In this study, diabetic rats were treated with Garlitab at the dose of 1.25 mg/kg once daily for 28 days. The outcome of the study showed that Garlitab reduces blood glucose levels and therefore supports the traditional use of Garlitab as a hypoglycemic formulation (Hossain 2015).
Conclusion
Diabetes has become a common health problem around the world in recent years, affecting people of all ages, genders, and races. Furthermore, its incidences have been increasing at an alarming rate day by day. The available synthetic antidiabetic medications cause substantial side effects. Many of the drugs cause damage or failure of vital organs like kidneys and the liver over a period of time. The use of multiple drugs for long duration results in the patient's non-compliance. As a result, a diverse range of traditionally claimed herbs have been used either exclusively or in the form of polyherbal formulations to manage diabetes and associated complications. These polyherbal formulations have potential antidiabetic effects, and scientists have performed several preclinical and clinical studies to establish their safety and efficacy profile. One additional advantage of these formulations is that many of them have efficacy on diabetes and its complications as well. This makes them patient-friendly. The side effects from these formulations are much lesser than that of synthetic drugs, although an overdose can have certain side effects. The ever-increasing safe use of such formulations with proper guidance from physicians can lead to a decreased burden of diabetes, worldwide. However, there is a need to examine active components and their molecular interactions to comply regulatory standards of modern medicines.
Author contributions
PM, MT, CB, BB, and AP contributed to conception and design of the review article. All the authors contributed to manuscript revision and read and approved the submitted version.
Acknowledgments
The authors are thankful to the Management, Dean, and Head of the School of Pharmacy, Dr. Vishwanath Karad MIT World Peace University, Pune for their guidance and necessary support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aderibigbe, A, O., Emudianughe, T. S., and Lawal, B. A. (2001). Evaluation of the antidiabetic action of Mangifera indica in mice. Phytother. Res. 15, 456–458. doi:10.1002/ptr.859
Ahmad, M., Zaman, F., Sharif, T., and Ch, M. Z. (2008). Antidiabetic and hypolipidemic effects of aqueous methanolic extract of Acacia nilotica pods in alloxan-induced diabetic rabbits. Scand. J. Lab. Anim. Sci. 35, 29–34. doi:10.23675/sjlas.v35i1.135
Ahmed, D., Sharma, M., Mukerjee, A., Ramteke, P. W., and Kumar, V. (2013). Improved glycemic control, pancreas protective and hepatoprotective effect by traditional poly-herbal formulation "Qurs Tabasheer" in streptozotocin induced diabetic rats. BMC Complement. Altern. Med. 13, 10. doi:10.1186/1472-6882-13-10
Akhtar, M. S., Ramzan, A., Ali, A., and Ahmad, M. (2011). Effect of amla fruit (Emblica officinalis Gaertn.) on blood glucose and lipid profile of normal subjects and type 2 diabetic patients. Int. J. Food Sci. Nutr. 62, 609–616. doi:10.3109/09637486.2011.560565
Al-Amin, Z. M., Thomson, M., Al-Qattan, K. K., Peltonen-Shalaby, R., and Ali, M. (2006). Anti-diabetic and hypolipidaemic properties of ginger (Zingiber officinale) in streptozotocin-induced diabetic rats. Br. J. Nutr. 96, 660–666. doi:10.1079/BJN20061849
Al-Juraisy, Y. H. (2014). The hypoglycemic effect of Fenugreek (Trigonella foenum-gracecum) seed extract in experimentally diabetic rats. Al-Mustansiriyah J. Sci. 25, 1–8.
Ansari, S., Khan, Q., Anjum, R., Siddiqui, A., and Sultana, K. (2017). Fundamentals of Unani system of medicine-a review. Eur. J. Biomed. Pharm. 4, 219–223.
Arawwawala, M., Thabrew, I., and Arambewela, L. (2009). Antidiabetic activity of Trichosanthes cucumerina in normal and streptozotocin–induced diabetic rats. Int. J. Biol. Chem. Sci. 3, 287–296. doi:10.4314/ijbcs.v3i2.44504
Bagri, P., Ali, M., Aeri, V., Bhowmik, M., and Sultana, S. (2009). Antidiabetic effect of Punica granatum flowers: Effect on hyperlipidemia, pancreatic cells lipid peroxidation and antioxidant enzymes in experimental diabetes. Food Chem. Toxicol. 47, 50–54. doi:10.1016/j.fct.2008.09.058
Baskaran, K., Ahamath, B. K., Shanmugasundaram, K. R., and Shanmugasundaram, E. R. (1990). Antidiabetic effect of a leaf extracts from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J. Ethnopharmacol. 30, 295–300. doi:10.1016/0378-8741(90)90108-6
Bhandari, U., Chaudhari, H. S., Khanna, G., and Najmi, A. K. (2013). Antidiabetic effects of Embelia ribes extract in high fat diet and low dose streptozotocin-induced type 2 diabetic rats. Front. Life Sci. 7, 186–196. doi:10.1080/21553769.2014.881304
Bhattacharya, B., and Reddy, K. (2016). Pharmaceutico therapeutic study of Madhumehantak Churna (Ayurveda powder) for diabetes. [Ph. D. thesis]. Banaras (India): Department of Rasa Shastra. Faculty of Ayurveda-IMS.
Borgohain, R. A., Lahon, K. I., Das, S. W., and Gohain, K. A. (2012). Evaluation of mechanism of anti-diabetic activity of Terminalia chebula on alloxan and adrenaline-induced diabetic albino rats. Int. J. PharmaBioSci. 3, 256–266.
Das, N., Saha, S., Kumar, L., Nathani, S., Samantaray, S., Sircar, D., et al. (2018). “Anti-diabetic effect of Trivanga Bhasma- an ancient Indian nanomedicine,” in International conference on BioMaterials, BioEngineering, and BioTheranostics [BIOMET2018]. Vellore, India: ResearchGate.
Dawane, J. S., Pandit, A. V., Bhosale, M. S., and Khatavkar, P. S. (2016). Evaluation of Effect of Nishamalaki on STZ and HFHF diet induced diabetic neuropathy in Wistar rats. J. Clin. Diagn. Res. 10, FF01–FF05. doi:10.7860/JCDR/2016/21011.8752
Deng, N., Zheng, B., Li, T., and Liu, R. H. (2020). Assessment of the phenolic profiles, hypoglycemic activity, and molecular mechanism of different highland barley (Hordeum vulgare L.) varieties. Int. J. Mol. Sci. 21, 1175. doi:10.3390/ijms21041175
Deshmukh, S. M., Kshirsagar, S. J., and Bhingare, C. L. (2013). Screening of antidiabetic effect of naga bhasma in alloxan induced hyperglycemic rats. Int. J. Res. Ayurveda Pharm. 4, 240–243. doi:10.7897/2277-4343.04231
Eidi, A., Eidi, M., and Esmaeili, E. (2006). Antidiabetic effect of garlic (Allium sativum L.) in normal and streptozotocin-induced diabetic rats. Phytomedicine 13, 624–629. doi:10.1016/j.phymed.2005.09.010
Ganeshpurkar, A., Jain, S., and Agarwal, S. (2015). Experimental studies on glycolytic enzyme inhibitory and antiglycation potential of Triphala. Ayu 36, 96–100. doi:10.4103/0974-8520.169000
Ganogpichayagrai, A., Palanuvej, C., and Ruangrungsi, N. (2017). Antidiabetic and anticancer activities of Mangifera indica cv. okrong leaves. J. Adv. Pharm. Technol. Res. 8, 19–24. doi:10.4103/2231-4040.197371
Gholamhoseinian, A., and Fallah, H. (2009). Inhibitory effect of methanol extract of Rosa damascena Mill. flowers on α-glucosidase activity and postprandial hyperglycemia in normal and diabetic rats. Phytomedicine 16, 935–941. doi:10.1016/j.phymed.2009.02.020
Ghosh, D. E., Bera, T. K., Chatterjee, K., Ali, K. M., and De, D. (2009). Antidiabetic and antioxidative effects of aqueous extract of seed of Psoralea corylifolia (somraji) and seed of Trigonella foenum-graecum L.(methi) in separate and composite manner in streptozotocin-induced diabetic male Albino rat. Trop. J. Pharm. Res. 1, 1–10.
Grant, S. J., Bensoussan, A., Chang, D., Kiat, H., Klupp, N. L., Liu, J. P., et al. (2009). Chinese herbal medicines for people with impaired glucose tolerance or impaired fasting blood glucose. Cochrane Database Syst. Rev. 6. doi:10.1002/14651858.CD006690.pub2
Gupta, A., Kumar, R., and Pandey, A. K. (2020). Antioxidant and antidiabetic activities of Terminalia bellirica fruit in alloxan induced diabetic rats. S. Afr. J. Bot. 130, 308–315. doi:10.1016/j.sajb.2019.12.010
He, K., Li, X., Chen, X., Ye, X., Huang, J., Jin, Y., et al. (2011). Evaluation of antidiabetic potential of selected traditional Chinese medicines in STZ-induced diabetic mice. J. Ethnopharmacol. 137, 1135–1142. doi:10.1016/j.jep.2011.07.033
Hemmati, M., Karamian, M., and Malekaneh, M. (2015). Anti-atherogenic potential of natural honey: Anti-diabetic and antioxidant approaches. J. Pharm. Pharmacol. 3, 278–284. doi:10.17265/2328-2150/2015.06.004
Hossain, R. (2015).Evaluation of the efficacy of Alisa Garlitab, an anti-diabetic herbal preparation in streptozotocin induced diabetic rats. Bangladesh: Daffodil International University. [B. Pharm. Thesis].
Hu, J., Pang, W., Bai, S., Zheng, Z., and Wu, X. (2013). Hypoglycemic effect of polysaccharides with different molecular weight of Pseudostellaria heterophylla. BMC Complement. Altern. Med. 13, 267–269. doi:10.1186/1472-6882-13-267
Jamadagni, P., Jamadagni, S., Singh, R., Upadhyay, S., Gaidhani, S., and Hazra, J. (2017). Repeated dose oral toxicity of Trivanga Bhasma in Swiss albino mice. Ayu 34, 118–123. doi:10.4103/0974-8520.115449
Jayarambabu, N., Rao, T. V., Kumar, R. R., Akshaykranth, A., Shanker, K., and Suresh, V. (2021). Anti-hyperglycemic, pathogenic and anticancer activities of Bambusa arundinacea mediated zinc oxide nanoparticles. Mat. Today Commun. 26, 101688. doi:10.1016/j.mtcomm.2020.101688
Kaleem, M., Sheema, S. H., and Bano, B. (2005). Protective effects of Piper nigrum and Vinca rosea in alloxan induced diabetic rats. Indian J. Physiol. Pharmacol. 49, 65–71.
Kandalkar, A. M., and Bhajipale, N. S. (2016). Quality evaluation and standardization of an Ayurvedic anti-diabetic formulation: Mehari Choorna. Int. J. Pharmacogn. 3, 156–160.
Kaur, G., Kamboj, P., and Kalia, A. N. (2011). Antidiabetic and anti-hypercholesterolemic effects of aerial parts of Sida cordifolia Linn. on Streptozotocin-induced diabetic rats. Indian J. Nat. Prod. Resour. 2, 428–434.
Kharroubi, A. T., and Darwish, H. M. (2015). Diabetes mellitus: The epidemic of the century. World J. Diabetes 6, 850–867. doi:10.4239/wjd.v6.i6.850
Kim, O. K. (2005). Antidiabetic and antioxidative effects of Corni fructus in streptozotocin-induced diabetic rats. J. Korean Oil Chemists' Soc. 22, 157–167. doi:10.12925/jkocs.2005.22.2.9
Kumar, A., Ilavarasan, R., Deecaraman, M., Aravindan, P., Padmanabhan, N., and Krishan, M. R. (2008). Anti-diabetic activity of Syzygium cumini and its isolated compound against streptozotocin-induced diabetic rats. J. Med. Plant Res. 2, 246–249.
Kumari, J., Mehta, C. S., Shukla, V. D., Dave, A. R., and Shingala, T. M. (2010). A comparative clinical study of Nyagrodhadi Ghanavati and Virechana Karma in the management of madhumeha. Ayu 31, 300–304. doi:10.4103/0974-8520.77152
Kuroda, M., Mimaki, Y., Nishiyama, T., Mae, T., Kishida, H., Tsukagawa, M., et al. (2005). Hypoglycemic effects of turmeric (Curcuma longa L. rhizomes) on genetically diabetic KK-Ay mice. Biol. Pharm. Bull. 28, 937–939. doi:10.1248/bpb.28.937
Kuroda, M., Mimaki, Y., Ohtomo, T., Yamada, J., Nishiyama, T., Mae, T., et al. (2015). Hypoglycemic effects of clove (Syzygium aromaticum flower buds) on genetically diabetic KK-A y mice and identification of the active ingredients. J. Nat. Med. 66, 394–399. doi:10.1007/s11418-011-0593-z
Lee, H. C., Cheng, W. Y., Huang, B. E., Hsu, Y. H., and Huang, S. Y. (2014). Anti-inflammatory and hypoglycemic efficacy of Poria cocos and Dioscorea opposita in prediabetes mellitus rats. RSC Adv. 4, 55649–55657. doi:10.1039/C4RA10539G
Lekshmi, P. C., Arimboor, R., Nisha, V. M., Menon, A. N., and Raghu, K. G. (2014). In vitro antidiabetic and inhibitory potential of turmeric (Curcuma longa L) rhizome against cellular and LDL oxidation and angiotensin converting enzyme. J. Food Sci. Technol. 51, 3910–3917. doi:10.1007/s13197-013-0953-7
Li, F., Li, Q., Gao, D., Peng, Y., and Feng, C. (2009). Preparation and antidiabetic activity of polysaccharide from Portulaca oleracea L. Afr. J. Biotechnol. 8, 569–573.
Lin, L., Qiuhong, W., Yongxin, Y., Shihan, W., and Zonglin, Q. (2016). Liuwei dihuang pills enhance the effect of Western medicine in treating diabetic nephropathy: A meta-analysis of randomized controlled trials. Evid. Based Complement. Altern. Med. 2016, 1509063. doi:10.1155/2016/1509063
Liu, A. Q., Chen, X., Wang, Y. M., Jin, L., Yang, L., Dong, X., et al. (2021). Protective effect of modified Yu-Ye decoction on type 2 diabetes mellitus rats. TMR Pharmacol. Res. 1, 3. doi:10.53388/tmrpr20210217001
Lu, A. P., Jia, H. W., Xiao, C., and Lu, Q. P. (2004). Theory of traditional Chinese medicine and therapeutic method of diseases. World J. Gastroenterol. 10, 1854–1856. doi:10.3748/wjg.v10.i13.1854
Lu, J. M., Wang, Y. F., Yan, H. L., Lin, P., Gu, W., and Yu, J. (2016). Antidiabetic effect of total saponins from Polygonatum kingianum in streptozotocin-induced diabetic rats. J. Ethnopharmacol. 179, 291–300. doi:10.1016/j.jep.2015.12.057
Maithili, V., Dhanabal, S. P., Mahendran, S., and Vadivelan, R. (2011). Antidiabetic activity of ethanolic extract of tubers of Dioscorea alata in alloxan induced diabetic rats. Indian J. Pharmacol. 43, 455–459. doi:10.4103/0253-7613.83121
Mathew, P. T., and Augusti, K. T. (1975). Hypoglycaemic effects of onion, Allium cepa Linn. on diabetes mellitus-a preliminary report. Indian J. Physiol. Pharmacol. 19, 213–217.
Modak, M., Dixit, P., Londhe, J., Ghaskadbi, S., and Devasagayam, T. P. A. (2007). Indian herbs and herbal drugs used for the treatment of diabetes. J. Clin. Biochem. Nutr. 40, 163–173. doi:10.3164/jcbn.40.163
Nabi, S. A., Kasetti, R. B., Sirasanagandla, S., Tilak, T. K., Kumar, M. V., and Rao, C. A. (2013). Antidiabetic and antihyperlipidemic activity of Piper longum root aqueous extract in STZ induced diabetic rats. BMC Complement. Altern. Med. 13, 37–39. doi:10.1186/1472-6882-13-37
Nagappa, A. N., Thakurdesai, P. A., Rao, N. V., and Singh, J. (2003). Antidiabetic activity of Terminalia catappa Linn fruits. J. Ethnopharmacol. 88, 45–50. doi:10.1016/s0378-8741(03)00208-3
Naquvi, K. J., Ali, M. O., and Ahmad, J. (2004). Antidiabetic activity of aqueous extract of Coriandrum sativum L. fruits in streptozotocin induced rats. Indian J. Exp. Biol. 42 (9), 909–912.
Okoli, C. O., Ibiam, A. F., Ezike, A. C., Akah, P. A., and Okoye, T. C. (2010). Evaluation of antidiabetic potentials of Phyllanthus niruri in alloxan diabetic rats. Afr. J. Biotechnol. 9, 248–259.
Parasuraman, S., Thing, G., and Dhanaraj, S. (2014). Polyherbal formulation: Concept of Ayurveda. Pharmacogn. Rev. 8, 73–80. doi:10.4103/0973-7847.134229
Patel, M. B., and Mishra, S. (2011). Hypoglycemic activity of alkaloidal fraction of Tinospora cordifolia. Phytomedicine 18, 1045–1052. doi:10.1016/j.phymed.2011.05.006
Patil, P., Patil, S., Mane, A., and Verma, S. (2013). Antidiabetic activity of alcoholic extract of neem (Azadirachta indica) root bark. Natl. J. Physiol. Pharm. Pharmacol. 3, 142–146. doi:10.5455/njppp.2013.3.134-138
Petchi, R. R., Vijaya, C., and Parasuraman, S. (2014). Antidiabetic activity of polyherbal formulation in streptozotocin-nicotinamide induced diabetic wistar rats. J. Tradit. Complement. Med. 4, 108–117. doi:10.4103/2225-4110.126174
Poon, T. Y. C., Ong, K. L., and Cheung, B. M. Y. (2011). Review of the effects of the traditional Chinese medicine Rehmannia Six Formula on diabetes mellitus and its complications. J. Diabetes 3 (3), 184–200. doi:10.1111/j.1753-0407.2011.00130.x
Prativadibhayankaram, V. S., Malhotra, S., Pandhi, P., and Singh, A. (2008). Anti-diabetic activity of triphala fruit extracts, individually and in combination, in a rat model of insulin resistance. Nat. Prod. Commun. 3, 1934578X0800300–6. doi:10.1177/1934578x0800300230
Prisilla, D. H., Balamurugan, R., and Shah, H. R. (2012). Antidiabetic activity of methanol extract of Acorus calamus in STZ induced diabetic rats. Asian pac. J. Trop. Biomed. 2, S941–S946. doi:10.1016/S2221-1691(12)60341-4
Pulipaka, S., Challa, S. R., and Pingili, R. B. (2012). Comparative antidiabetic activity of methanolic extract of Operculina turpethum stem and root against healthy and streptozotocin induced diabetic rats. Int. Curr. Pharm. J. 1, 272–278. doi:10.3329/icpj.v1i9.11618
Rani, S., Mandave, P., Khadke, S., Jagtap, S., Patil, S., and Kuvalekar, A. (2013). Antiglycation, antioxidant and antidiabetic activity of traditional medicinal plant: Rubia cordifolia Linn. For management of hyperglycemia. CABI Agric. Biosci. 3, 42–49.
Shaikh, H., Ali, W., Abdullah, A., and Khanam, S. (2016). Standardization of Unani antidiabetic tablet-qurse tabasheer. Pharmacogn. Res. 8, 147–152. doi:10.4103/0974-8490.175611
Sharma, A., Shanker, C., Tyagi, L. K., Singh, M., and Rao, C. V. (2008). Herbal medicine for market potential in India: An overview. Acad. J. Plant Sci. 1, 26–36.
Simha, K. R., and Laxminarayana, V. (2007). Standardization of Ayurvedic polyherbal formulation, Nyagrodhadi churna. Indian J. Traditional Knowl. 6, 648–652.
Singh, P., Khosa, R. L., Mishra, G., and Jha, K. K. (2015). Antidiabetic activity of ethanolic extract of Cyperus rotundus rhizomes in streptozotocin-induced diabetic mice. J. Pharm. Bioallied Sci. 7, 289–292. doi:10.4103/0975-7406.168028
Suryavanshi, S. V., Garud, M. S., Barve, K., Addepalli, V., Utpat, S. V., and Kulkarni, Y. A. (2020). Triphala Ameliorates nephropathy via Inhibition of TGF-β1 and oxidative stress in diabetic rats. Pharmacology 105, 681–691. doi:10.1159/000508238
Syed Hussain, S. K., Qureshi, A., and Koneru, D. (2020). Evaluation of anti-diabetic activity of safoof-e-ziabetus dulabi against metformin in streptozotocin induced diabetic rats. Indo. Am. J. Pharm. Sci. 7, 219–225.
Takii, H., Kometani, T., Nishimura, T., Nakae, T., Okada, S., and Fushiki, T. (2001). Antidiabetic effect of glycyrrhizin in genetically diabetic KK-Ay mice. Biol. Pharm. Bull. 24, 484–487. doi:10.1248/bpb.24.484
Tanna, I., Joshi, J. R., and Chandola, H. M. (2011). Clinical efficacy of Mehamudgara vati in type 2 diabetes mellitus. Ayu 32, 30–39. doi:10.4103/0974-8520.85722
Tate, P. M., Patgiri, B. J., and Prajapati, P. K. (2009). Pharmaceutical standardization of naga bhasma. Ayu 30, 300–309.
Upwar, N., Patel, R., Waseem, N., and Mahobia, N. K. (2011). Hypoglycemic effect of methanolic extract of Berberis aristata DC stem on normal and streptozotocin induced diabetic rats. Int. J. Pharm. Pharm. Sci. 3, 222–224.
Veerapur, V. P., Prabhakar, K. R., Thippeswamy, B. S., Bansal, P., Srinivasan, K. K., and Unnikrishnan, M. K. (2012). Antidiabetic effect of Ficus racemosa Linn. Stem bark in high-fat diet and low-dose streptozotocin-induced type 2 diabetic rats: A mechanistic study. Food Chem. 132, 186–193. doi:10.1016/j.foodchem.2011.10.052
Verspohl, E. J., Bauer, K., and Neddermann, E. (2005). Antidiabetic effect of Cinnamomum cassia and Cinnamomum zeylanicum in vivo and in vitro. Phytother. Res. 19, 203–206. doi:10.1002/ptr.1643
Wang, H., Gang, H., Zhou, S., Liu, L., Ding, T., Gui, Z., et al. (2018). Liuwei Dihuang exhibits antidiabetic effects through inhibiting α-amylase and α-glucosidase. Med. Sci. 34, 4–7. doi:10.1051/medsci/201834f101
Wanjari, M. M., Mishra, S., Dey, Y. N., Sharma, D., Gaidhani, S. N., and Jadhav, A. D. (2016). Antidiabetic activity of chandraprabha vati – a classical Ayurvedic formulation. J. Ayurveda Integr. Med. 7, 144–150. doi:10.1016/j.jaim.2016.08.010
Welihinda, J., Karunanayake, E. H., Sheriff, M. H., and Jayasinghe, K. S. (1986). Effect of Momordica charantia on the glucose tolerance in maturity onset diabetes. J. Ethnopharmacol. 17, 277–282. doi:10.1016/0378-8741(86)90116-9
Wietmarschen, H. A. V., Greef, J. V. D., Schroën, Y., and Wang, M. (2009). Evaluation of symptom, clinical chemistry and metabolomics profiles during Rehmannia six formula (R6) treatment: An integrated and personalized data analysis approach. J. Ethnopharmacol. 150, 851–859. doi:10.1016/j.jep.2013.09.041
Wu, K., Liang, T., Duan, X., Xu, L., Zhang, K., and Li, R. (2013). Anti-diabetic effects of puerarin, isolated from Pueraria lobata (Willd.), on streptozotocin-diabetogenic mice through promoting insulin expression and ameliorating metabolic function. Food Chem. Toxicol. 60, 341–347. doi:10.1016/j.fct.2013.07.077
Yin, Y., Heo, S. I., Jung, M. J., and Wang, M. H. (2009). Antioxidant and antidiabetic effects of various sections of Astragalus membranaceus. Korean J. Pharmacogn. 40, 1–5.
Zhang, R., Zhou, J., Jia, Z., Zhang, Y., and Gu, G. (2004). Hypoglycemic effect of Rehmannia glutinosa oligosaccharide in hyperglycemic and alloxan-induced diabetic rats and its mechanism. J. Ethnopharmacol. 90, 39–43. doi:10.1016/j.jep.2003.09.018
Keywords: Diabetic complications, diabetes mellitus, hyperglycemia, metabolic disorder, polyherbal formulations
Citation: Murudkar PH, Tambe MS, Chandrasekar SB, Boddeda B and Pawar AT (2022) Common Ayurvedic, Chinese traditional and Unani antidiabetic formulations- a review. Front. Pharmacol. 13:991083. doi: 10.3389/fphar.2022.991083
Received: 11 July 2022; Accepted: 22 August 2022;
Published: 12 October 2022.
Edited by:
Pukar Khanal, KLE College of Pharmacy, IndiaReviewed by:
Kunal Bhattacharya, Pratiksha Institute of Pharmaceutical Sciences (PIPS), IndiaSadia Nikhat, Jamia Hamdard University, India
Copyright © 2022 Murudkar, Tambe, Chandrasekar, Boddeda and Pawar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anil T. Pawar, YW5pbC5wYXdhckBtaXR3cHUuZWR1Lmlu
 Prajakta H. Murudkar
Prajakta H. Murudkar Mukul S. Tambe
Mukul S. Tambe S.B. Chandrasekar2
S.B. Chandrasekar2 Anil T. Pawar
Anil T. Pawar