- 1Division of Cardiology, Department of Internal Medicine, Shuang Ho Hospital, Taipei Medical University, Taipei, Taiwan
- 2Taipei Heart Institute, Taipei Medical University, Taipei, Taiwan
- 3Division of Cardiology, Department of Internal Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 4Graduate Institute of Medical Sciences, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 5Department of General Medicine, Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan
- 6Division of Cardiovascular Surgery, Department of Surgery, Shuang Ho Hospital, Taipei Medical University, Taipei, Taiwan
- 7Division of Cardiovascular Surgery, Department of Surgery, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
- 8Department of Emergency, University Hospitals Cleveland Medical Center, Cleveland, OH, United States
- 9Cardiovascular Center, Lo-Hsu Medical Foundation Luodong Poh-Ai Hospital, Yilan, Taiwan
- 10Department of Surgery, Lotung Poh-Ai Hospital, Yilan, Taiwan
- 11Graduate Institute of Data Science, College of Management, Taipei Medical University, Taipei, Taiwan
- 12Department of Neurosurgery, Wan-Fang Hospital, Taipei Medical University, Taipei, Taiwan
Objective: Although influenza vaccination reduces the risk of atrial fibrillation (AF), its protective effect in patients with gout remains unclear. The present study aimed to evaluate the protective effect of influenza vaccination in patients with gout.
Methods: A total of 26,243 patients with gout, aged 55 and older, were enrolled from the National Health Insurance Research Database (NHIRD) between 1 January 2001, and 31 December 2012. The patients were divided into vaccinated (n = 13,201) and unvaccinated groups (n = 13,042). After adjusting comorbidities, medications, sociodemographic characteristics, the risk of AF during follow-up period was analyzed.
Results: In influenza, non-influenza seasons and all seasons, the risk of AF was significantly lower in vaccinated than in unvaccinated patients (Adjust hazard ratio [aHR]: 0.59, 95% confidence interval [CI]: 0.50–0.68; aHR: 0.50, 95% CI: 0.42–0.63; aHR: 0.55, 95% CI: 0.49–0.62, respectively). In addition, the risk of AF significantly decreased with increased influenza vaccination (aHR: 0.85, 95% CI: 0.69–1.04; aHR: 0.72, 95% CI: 0.60–0.87; aHR: 0.40, 95% CI: 0.33–0.49, after first, 2–3 times, and ≥4 times of vaccination, respectively). Furthermore, sensitivity analysis indicated that the risk of AF significantly decreased after influenza vaccination for patients with different sexes, medication histories, and comorbidities.
Conclusions: Influenza vaccination is associated with a lower risk of AF in patients with gout. This potentially protective effect seems to depend on the dose administered.
Introduction
Gout is a common form of inflammatory arthritis that is associated with a certain degree of disease burden (Smith et al., 2014; Dehlin et al., 2020). Nearly one in 16 individuals in Taiwan have gout (Kuo et al., 2015). The prevalence of gout in Taiwan is higher than in other countries such as the United Kingdom (2.49%) and the United States (3.9%) (Kuo et al., 2015). Gout results from uric acid deposition; the uric acid links not only to acute or chronic arthritis but also cardiovascular disease (Kim et al., 2016; Singh and Cleveland, 2018; Dehlin et al., 2020; Khan et al., 2021). Past studies demonstrated that the prevalence of atrial fibrillation (AF) and cardiovascular mortality is higher in patients with gout than in those without (Kim et al., 2016; Singh and Cleveland, 2018; Khan et al., 2021).
AF is a common form of cardiac arrhythmia (Chugh et al., 2014). With the growing population of older adults, the prevalence and severity of AF have increased (Savickas et al., 2020). Various factors are related to the incidence of AF, such as hypertension, diabetes, valvular heart disease, and cardiomyopathy (Staerk et al., 2018). Several studies have reported a strong association between AF and gout (Kuo et al., 2016a; Singh and Cleveland, 2018; Khan et al., 2021). In patients with gout, the risk of AF is considerably higher than in those without (Singh and Cleveland, 2018; Khan et al., 2021). Although both AF and gout have some common risk factors, their exact mechanisms remain unclear. This may be due to the role of chronic inflammation, oxidative stress, and uric acid in atrial remodeling processes (Dalbeth and Haskard, 2005; Kuo et al., 2016a).
Influenza is a highly contagious infection and a critical cause of death among senior citizens. Every year, influenza infections result in the death of over 20,000 individuals worldwide, leading to an economic burden (Fang et al., 2016; Smetana et al., 2018). In particular, among patients with chronic diseases, the morbidity and mortality rates associated with influenza infection are high. Besides, previous reports pointed out that influenza may play an important role to trigger or exacerbate the cardiovascular events, including the increased risk of AF (Chang et al., 2016; Pérez-Rubio et al., 2021).
Previous studies have highlighted that influenza vaccination reduces the risks of flu infection, hospitalization, and severe illness (Rondy et al., 2017). Influenza vaccination may also reduce the risks of major adverse cardiovascular events (risk ratio = 0.64, 95% confidence interval [CI] = 0.48–0.86) and even the development of AF among the general population (odds ratio = 0.88, p < 0.01) (Phrommintikul et al., 2011; Udell et al., 2013; Chang et al., 2016). Some direct or indirect mechanisms had been proposed to explain the possible protective effect of flu-vaccination on decreasing cardiovascular events (Pérez-Rubio et al., 2021). However, the protective effect of influenza vaccination to decrease risk of AF among patients with gout remained unclear. Thus, in this nationwide population based observational study, the association between the risk of AF and influenza vaccination among patients with gout was investigated.
Methods
In 1995, Taiwan’s National Health Insurance (NHI) program was established to provide the residents of Taiwan with comprehensive health insurance. This program currently covers more than 98% of the population in Taiwan (Luo et al., 2020; Chen et al., 2021; Zheng et al., 2021). In this study, the statistical characteristics of the sample group were similar to those of the general population. All researchers using the National Health Insurance Research Database (NHIRD) or its data subsets are required to sign a written agreement stating that they do not intend to obtain information that may violate the privacy of the patients or care providers. All personal information was delinked and deidentified to protect the privacy of the parties involved. This study was approved by the Joint Institutional Review Board of Taipei Medical University (approval no. N201804043).
Patient selection process and the definition of the primary endpoint
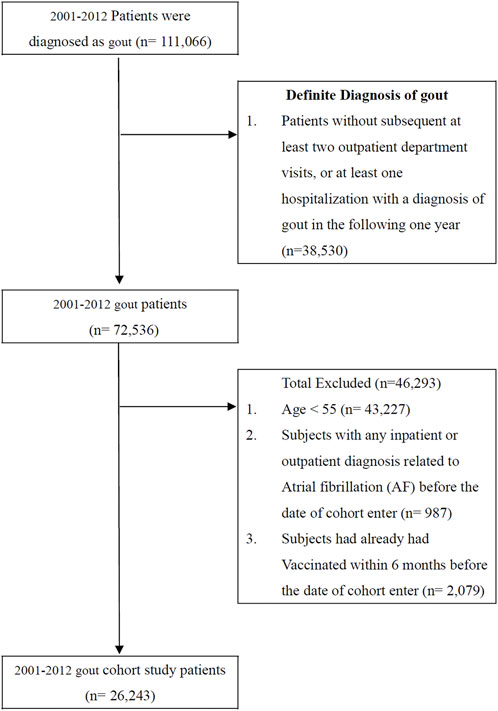
Patients who were diagnosed with gout (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 274. X) over a 12-year period (n = 111,066) from 1 January 2001, to 31 December 2012, were selected. However, patients without at least two subsequent outpatient department visits or at least one instance of hospitalization with a diagnosis of gout in the following year (n = 38,530) were excluded because of the uncertainty of gout diagnosis. The accuracy of the ICD diagnosis of gout has been validated in a previous study (Cheng et al., 2011). Another 46,293 patients meeting the following criteria were excluded from the study: patients aged 55 and younger (n = 43,227), patients with any inpatient or outpatient diagnosis related to AF before the date of enrollment in the cohort (n = 987), and patients who received influenza vaccination within 6 months before the enrollment date (n = 2,097). As a result, 26,243 patients were included in our final study cohort (Figure 1). In line with its public health policy, the government of Taiwan has been offering influenza vaccination free of charge since 1998 for citizens over 50 years of age with systemic diseases, such as chronic pulmonary disease, cardiovascular disease, chronic liver infection with cirrhosis, or type 2 diabetes mellitus, and since 2001 for all individuals over 65 years of age (Taiwan Centers for Disease Control, 2021). Here, we identified the history of vaccination with the ICD-9-CM code V048 and/or with the vaccine drug codes. The primary endpoint of our study was the occurrence of AF (ICD-9-CM code 427.31) in patients with gout during the influenza season (October to March), noninfluenza season (April to September), and all seasons over the follow-up years. All patients were followed up until they received a diagnosis of AF, dropped out from the NHI program, were lost to follow-up, died, or until 31 December 2012.
Potential confounders
We selected the potential confounders of our cohort on the basis of sociodemographic characteristics (age, sex, urbanization level, and monthly income), history of inpatient and outpatient visits before study entry, comorbidities (Charlson Comorbidity Index [CCI], diabetes mellitus, hypertension, dyslipidemia, chronic obstructive pulmonary disease [COPD], cirrhosis, acute myocardial infarction [AMI], Ischemic heart disease, peripheral vascular disease), and medication use (allopurinol, benzbromarone, colchicine, aspirin, statins, renin–angiotensin–aldosterone system inhibitors [RAASIs], and metformin).
Statistical analysis
First, we used a propensity score (PS) method to reduce the selection bias in the comparison between the vaccinated and unvaccinated groups by accounting for the covariates with a logistic regression model (Rosenbaum and Rubin, 1983; D'Agostino, 1998). We employed the chi-square test and t-test for categorical and continuous variables, respectively. We then analyzed the correlation between influenza vaccination and AF in patients with gout by using Cox proportional hazards regression analysis. We also examined the association between the seasonal effect of vaccination and the risk of AF. Subsequently, we determined the dose–response effect of influenza vaccination on the risk of AF. We divided patients with gout into four groups according to their vaccination status: unvaccinated patients, patients who received one vaccine dose, patients who received two or three vaccine doses, and patients who received four or more vaccine doses. These data were stratified by the age, sex, comorbidities, and medication use of the patients. Next, we used sensitivity analysis to evaluate the differences and similarities between influenza vaccination and the risk of AF in patients with gout. All statistical analyses were performed using IBM SPSS Statistics version 22.0 (IBM, Armonk, NY, United States) and SAS version 9.4 (SAS Institute, Cary, NC, United States). A p-value less than 0.05 was considered statistically significant.
Results
Baseline characteristics
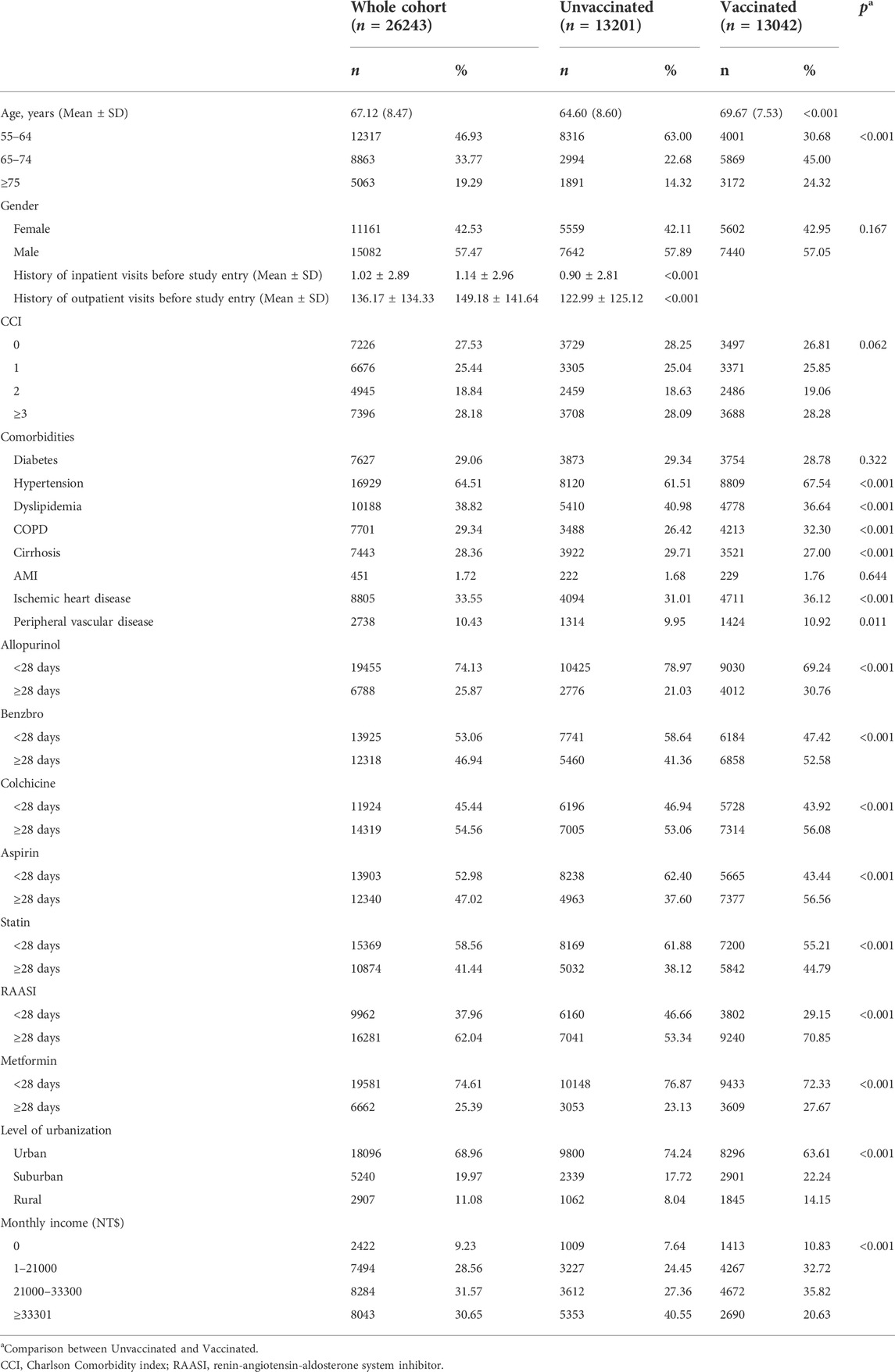
A total of 26,243 eligible patients with gout were included in our cohort. Among these patients, 50.30% (13,201) were vaccinated against influenza, and the remaining 49.69% (13,042) were not. We observed a considerable difference in the age distribution, urbanization level, and monthly income between the two groups (Table 1). Compared with vaccinated patients, unvaccinated patients had higher times of inpatient and outpatient visits. In addition, compared with the vaccinated group, significantly higher prevalence of dyslipidemia and cirrhosis in the unvaccinated group was observed. The prevalence of hypertension, COPD and ischemic heart disease were significantly higher in vaccinated group. Compared with unvaccinated patients, those who were vaccinated demonstrated increased long-term use (≥28 days) of gout medications, such as allopurinol, benzbromarone, and colchicine. Moreover, those who were vaccinated demonstrated increased long-term use of aspirin, statins, RAASIs, and metformin. However, we observed no significant difference in the CCI between the vaccinated and unvaccinated groups.
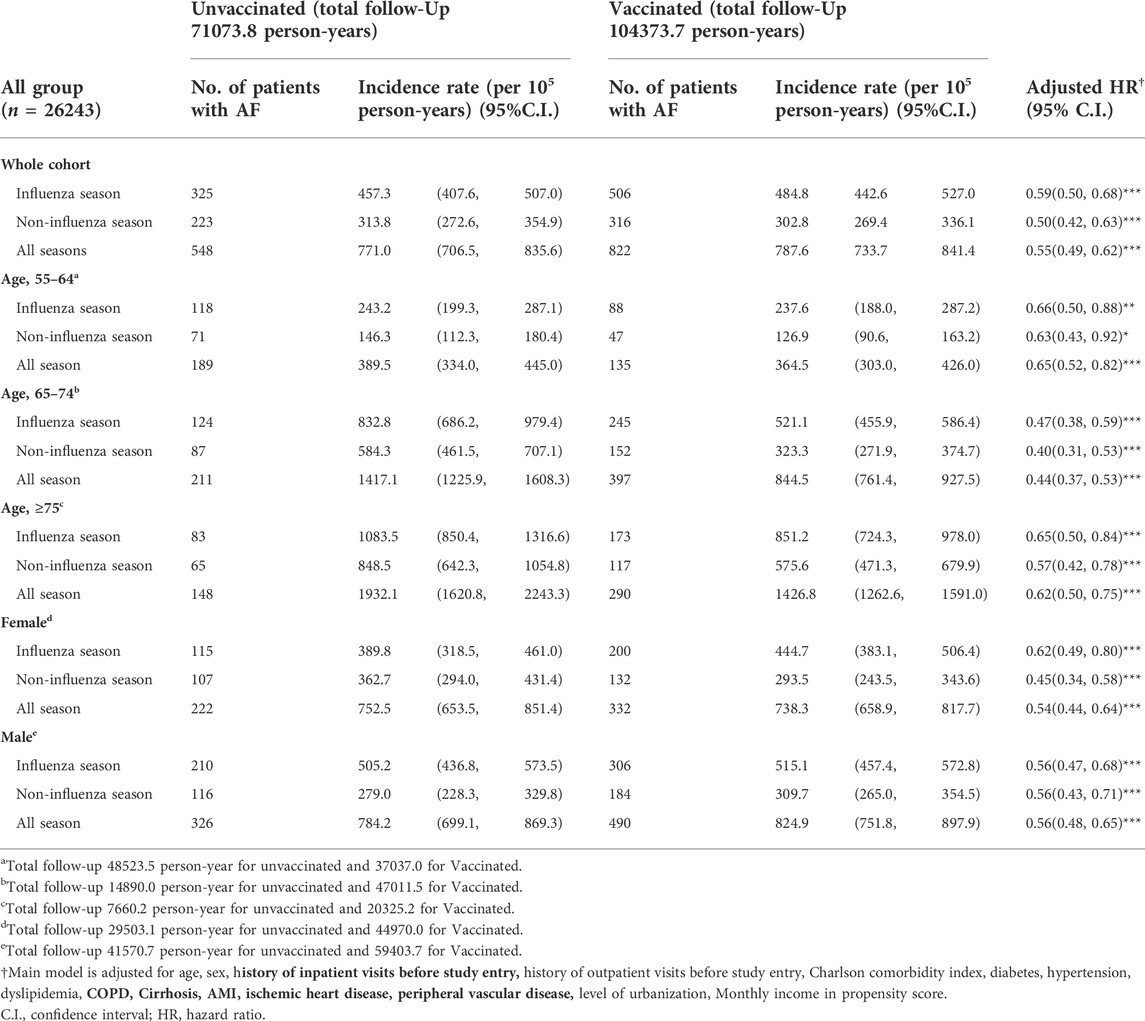
The risk of AF in the vaccinated and unvaccinated groups
The hazard ratio of AF among all patients with gout (vaccinated and unvaccinated) is presented in Table 2. With the aforementioned potential confounders adjusted for, the risk of AF in the vaccinated group was significantly lower than in the unvaccinated group during all seasons (adjusted hazards ratio [aHR] = 0.55, 95% CI = 0.49–0.62, p < 0.001). Compared with the unvaccinated group, a decreased risk of AF was observed during the influenza and noninfluenza seasons among the vaccinated group (aHR = 0.59, 95% CI = 0.50–0.68, and aHR = 0.50, 95% CI = 0.42–0.63 during the influenza and noninfluenza seasons, respectively). Both male and female patients had a significantly decreased risk of AF after vaccination during all seasons. We also observed a significantly decreased risk of AF among patients aged 55–64, 65–74, and ≥75 during all seasons (Table 2).
Sensitivity analysis of the association between different times of vaccination and the risk of atrial fibrillation
Main model analysis revealed a significantly lower risk of AF after the administration of more than two vaccine doses during the influenza season (aHR = 0.85, 95% CI = 0.69–1.04; aHR = 0.72, 95% CI = 0.60–0.87; and aHR = 0.40, 95% CI = 0.33–0.49 for the first dose, second and third doses, and ≥fourth dose, respectively). With the covariates of medication use adjusted for (allopurinol, benzbromarone, colchicine, aspirin, statins, RAASIs, and metformin), the risk of AF significantly decreased after the administration of more than two vaccine doses. Among patients aged above 65, a significantly decreased risk of AF was observed after the administration of more than two vaccine doses (aHR = 0.79, 95% CI = 0.62–1.01; aHR = 0.70, 95% CI = 0.56–0.87; and aHR = 0.38, 95% CI = 0.31–0.47 for the first dose, second and third doses, and ≥fourth dose, respectively). After the administration of more than four vaccine doses, both male and female patients demonstrated a significantly decreased risk of AF. Moreover, among patients with or without diabetes, dyslipidemia, hypertension, COPD, cirrhosis, ischemic heart disease, and peripheral vascular disease, significantly lower risk of AF was observed after receiving more than four times of vaccination. In patients on allopurinol, benzbromarone, colchicine, aspirin, statins, RAASIs, or metformin (either short- or long-term use), the risk of AF significantly decreased with the administration of more vaccine doses (Table 3).
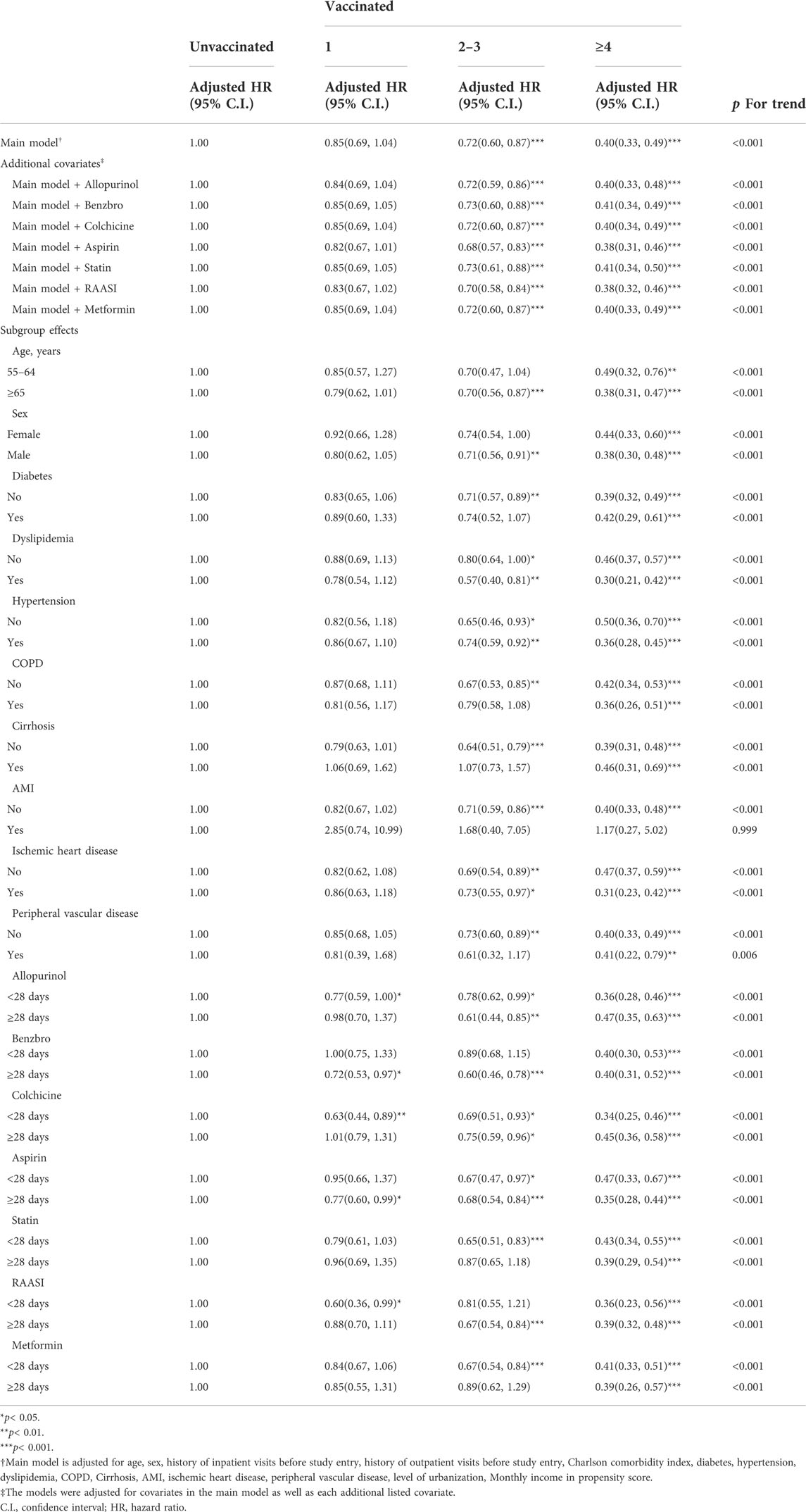
TABLE 3. Sensitivity analysis of adjusted HRs of vaccination in risk reduction of atrial fibrillation in influenza season.
During both the noninfluenza season and all seasons, main model analysis indicated a significantly decreased risk of AF with the administration of more vaccine doses (aHR = 0.86, 95% CI = 0.68–1.10; aHR = 0.62, 95% CI = 0.49–0.79; and aHR = 0.30, 95% CI = 0.24–0.38 for the first dose, second and third doses, and ≥fourth dose, respectively, during the noninfluenza season, and aHR = 0.86, 95% CI = 0.73–1.00; aHR = 0.68, 95% CI = 0.59–0.79; and aHR = 0.36, 95% CI = 0.31–0.42 for the first dose, second and third doses, and ≥fourth dose, respectively, during all seasons). Subgroup analysis indicated that both male and female patients, patients above or below 65 years of age, patients with or without comorbidities, and patients on medications exhibited a significantly decreased risk of AF after the administration of more vaccine doses during both the noninfluenza season and all seasons (Tables 4, 5).
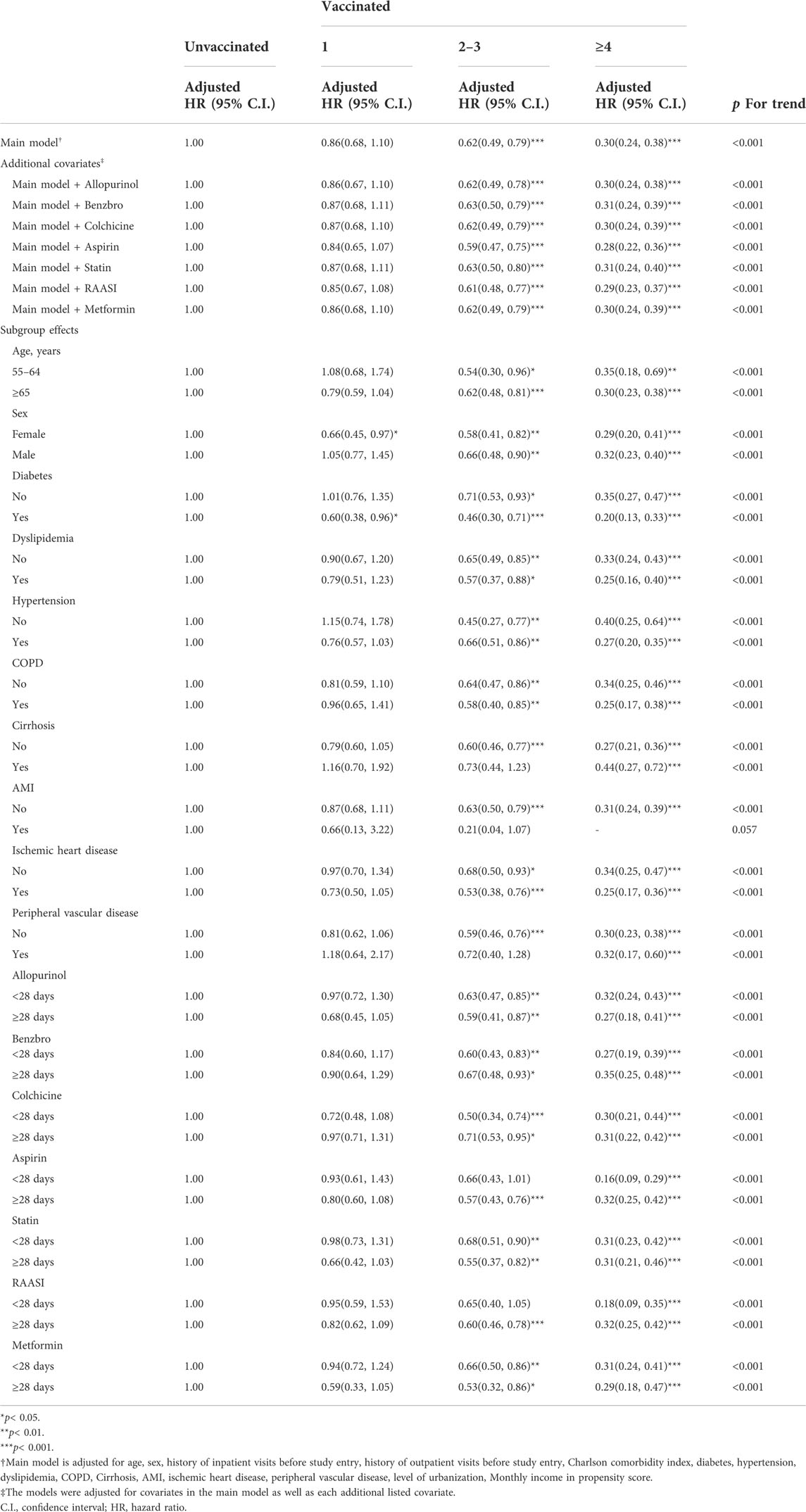
TABLE 4. Sensitivity analysis of adjusted HRs of vaccination in risk reduction of atrial fibrillation in non-influenza season.
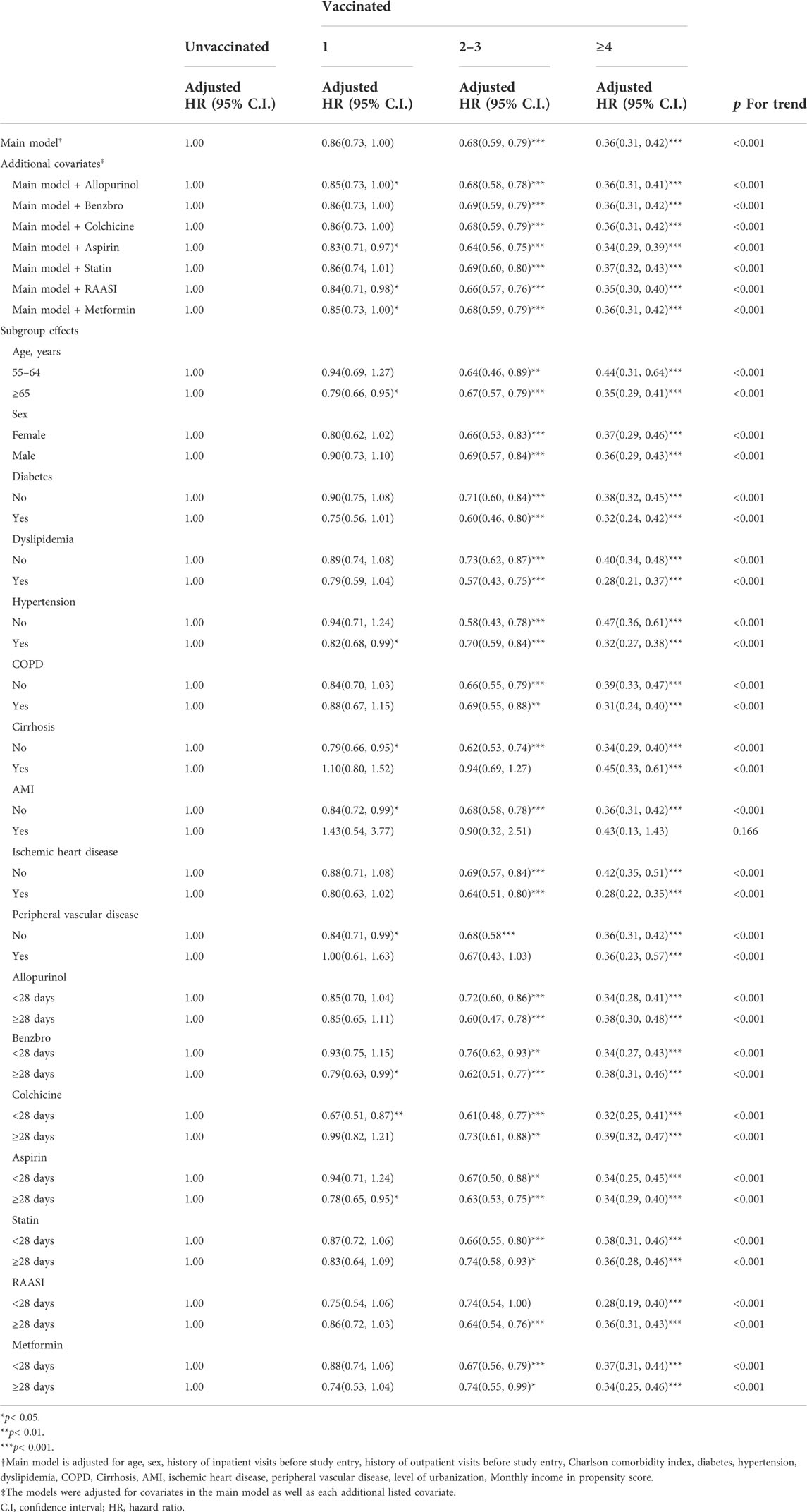
TABLE 5. Sensitivity analysis of adjusted HRs of vaccination in risk reduction of atrial fibrillation in all Sseasons.
Discussion
Major findings
In this section, we highlight the main findings of this population-based cohort study. 1) In patients with gout, influenza vaccination was associated with a decreased risk of AF. 2) In patients with or without chronic comorbidities, the risk of AF significantly decreased after influenza vaccination, and the potentially protective effect appeared to be dose-dependent. 3) In patients above or below 65 years of age, the risk of AF significantly decreased after influenza vaccination. 4) The potentially protective effect was observed during influenza season, noninfluenza season and all seasons.
Mechanism of atrial fibrillation development in patients with gout
Both AF and gout have similar risk factors. According to the literature, the prevalence of AF in patients with gout is higher than in those without, although the mechanisms of both conditions remain unclear (Kim et al., 2016; Singh and Cleveland, 2018; Khan et al., 2021). Although the pathogenesis of AF remains only partially understood, the current evidence links AF to inflammation and autonomic nervous system complications. Several studies have demonstrated increased levels of inflammatory biomarkers (e.g., interleukin-2 [IL-2], IL-6, and IL-8, tumor necrosis factor-α, and C-reactive protein) in patients with AF (Engelmann and Svendsen, 2005; Liu et al., 2007; Guo et al., 2012). Other studies have also reported elevated levels of systemic inflammation markers (e.g., cytokines) in patients with gout, which may trigger oxidative stress, heart inflammation, and structural and electrical remodeling of the heart (Lee et al., 2007; Musa et al., 2013; Kuo et al., 2016b). Similar studies on African American patients have highlighted that an increase in the levels of serum uric acid is associated with an increased risk of AF, suggesting that uric acid is involved in atrial remodeling (Tamariz et al., 2011; KORANTZOPOULOS et al., 2012; Kuo et al., 2016a). All of these findings highlight the potential association between AF and gout.
Mechanism of risk reduction of atrial fibrillation after influenza vaccination
According to the literature, influenza vaccination can reduce the risks of AF. In patients with influenza, inflammatory cytokines are produced and the sympathetic nervous system is activated (Chang et al., 2016). Infection with influenza may also cause myocarditis, which leads to AF by affecting the electrical system of the heart (Karjalainen et al., 1980; Rothberg et al., 2008). Therefore, influenza vaccination can prevent AF by reducing the aforementioned risks during an infection with influenza. In this study, we observed a robust protective effect for influenza vaccination. This may be because patients with gout are already in a state of inflammation (with elevated levels of inflammatory factors) and are susceptible to infection (Spaetgens et al., 2017). We also observed that this protective effect was further enhanced after influenza vaccination in patients with comorbidities. Furthermore, we observed that patients aged 65 and above with gout benefited more from influenza vaccination than patients aged 55–64 regardless of the season. This may be because the immune systems of older individuals are less capable of fighting off infections.
Mechanism between the vaccination dose and atrial fibrillation risk
A dose effect was found in our study; patients with more vaccinations were associated with lower hazard ratio of AF. In previous study, significantly lower risk of AF was observed among heart failure patients who received greater numbers of influenza vaccination (Modin et al., 2019). The function of the memory immune cells in patients with chronic diseases are more likely to diminish over time than in normal people (Sester et al., 2013). Therefore, with more vaccinations, the protective effect might became greater. However, the present study also demonstrated that the potential dose effect was also observed during noninfluenza season. In the study from (Zhu et al 2009), significantly lower risk of venous thromboembolism event was observed across the 12 months evenly after influenza vaccination. A recent study from Pang et al. showed that the risk of in-hospital death was significantly lower in patients received influenza vaccination during both influenza and summer months (Pang et al., 2022). Therefore, the possible mechanism other than influenza infection prevention might exist. Anti-inflammatory and plaque stabilization after influenza vaccination are the potential mechanisms of decreasing risk of AF after vaccination among patients with gout(Bermúdez-Fajardo and Oviedo-Orta, 2011; Pothineni et al., 2017; Atoui et al., 2021). However, future study is warranted to validate the result of present study.
Limitations
This study has several limitations. First, some parameters (e.g., body mass index), personal information (e.g., smoking status and alcohol consumption), and biochemical data (e.g., level of uric acid) were not available from the NHIRD. Therefore, we used a PS method to minimize bias. Second, because of the influenza vaccination policy of Taiwan, we excluded patients younger than 55 years. Therefore, future studies should include younger patients with gout. Third, this study had a retrospective and observational design. Therefore, prospective studies are required to validate our findings. Fourth, although previous study demonstrated the anti-inflammatory effect and plaque stabilization from influenza vaccination beyond the infection prevention effect (Bermúdez-Fajardo and Oviedo-Orta, 2011; Pothineni et al., 2017; Atoui et al., 2021), these findings still could not fully explain the finding of potential protective effect from vaccination across influenza season, noninfluenza season and all seasons in the present study. Potential unknown confounding factor could exist in the present study and future research is warranted to validate this finding. Fifth, healthy user bias potentially exist in this observational study (Shrank et al., 2011). In Taiwan, the influenza vaccine was provided free of charge to the patients with chronic disease. In addition, to minimize the bias, we further performed PS and adjusted age, sex, urbanization level, monthly incomes, comorbidities, inpatient and outpatient visits among vaccinated and unvaccinated patients in calculation of hazard ratio of AF risk. (Rosenbaum and Rubin, 1983; D'Agostino, 1998). Sixth, the selected cohort in the present study was during 2001–2012. Future study analysis from more recent data to validate the findings of present study is warranted.
Conclusion
Influenza vaccination is associated with a decreased the risk of AF in patients with gout. This potentially protective effect seems to be dose-dependent.
Data availability statement
The data supporting the findings of this research were sourced from NHIRD in Taiwan. Owing to the legal restrictions imposed by the Government of Taiwan related to the Personal Information Protection Act, the database cannot be made publicly available.
Author contributions
W-RH and J-CL are the guarantors of the content of the manuscript, including the data and analysis. C-CC conceived and designed the study. Y-AF was responsible for data collection. Y-AF, C-HL, W-RH, C-CC, T-YY, M-HH, WJ, M-HL, and H-TY analyzed and interpreted the data and manuscript revisions. C-CC and N-HC drafted the manuscript. All authors have reviewed the manuscript and approve its submission.
Funding
This work was financially supported of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, Taipei Medical University-National Taiwan University Hospital Joint Research Program, (111-TMU085), and 111FRP-02 from the Taipei Medical University-Shuang Ho Hospital, Ministry of Health and Welfare.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Atoui, R., Ebrahim, F., Saroka, K., Mireau, J., McElhaney, J. E., and Hare, G. M. T. (2021). Influenza vaccination blunts the inflammatory response in patients undergoing cardiopulmonary bypass. Ann. Thorac. Surg. 111 (6), 1923–1930. doi:10.1016/j.athoracsur.2020.07.052
Bermúdez-Fajardo, A., and Oviedo-Orta, E. (2011). Influenza vaccination promotes stable atherosclerotic plaques in apoE knockout mice. Atherosclerosis 217 (1), 97–105. doi:10.1016/j.atherosclerosis.2011.03.019
Chang, T. Y., Chao, T. F., Liu, C. J., Chen, S. J., Chung, F. P., Liao, J. N., et al. (2016). The association between influenza infection, vaccination, and atrial fibrillation: A nationwide case-control study. Heart rhythm. 13 (6), 1189–1194. doi:10.1016/j.hrthm.2016.01.026
Chen, C.-C., Lin, C. H., Hao, W. R., Yeh, J. S., Chiang, K. H., Fang, Y. A., et al. (2021). Influenza vaccination and the risk of ventricular arrhythmias in patients with chronic obstructive pulmonary disease: A population-based longitudinal study. Front. Cardiovasc. Med. 8, 731844. doi:10.3389/fcvm.2021.731844
Cheng, C. L., Kao, Y. H. Y., Lin, S. J., Lee, C. H., and Lai, M. L. (2011). Validation of the national health insurance research Database with ischemic stroke cases in taiwan. Pharmacoepidemiol. Drug Saf. 20 (3), 236–242. doi:10.1002/pds.2087
Chugh, S. S., Havmoeller, R., Narayanan, K., Singh, D., Rienstra, M., Benjamin, E. J., et al. (2014). Worldwide epidemiology of atrial fibrillation: A global burden of disease 2010 study. Circulation 129 (8), 837–847. doi:10.1161/CIRCULATIONAHA.113.005119
D'Agostino, R. B. (1998). Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 17 (19), 2265–2281. doi:10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b
Dalbeth, N., and Haskard, D. O. (2005). Mechanisms of inflammation in gout. Rheumatol. Oxf. 44 (9), 1090–1096. doi:10.1093/rheumatology/keh640
Dehlin, M., Jacobsson, L., and Roddy, E. (2020). Global epidemiology of gout: Prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 16 (7), 380–390. doi:10.1038/s41584-020-0441-1
Engelmann, M. D. M., and Svendsen, J. H. (2005). Inflammation in the Genesis and perpetuation of atrial fibrillation. Eur. Heart J. 26 (20), 2083–2092. doi:10.1093/eurheartj/ehi350
Fang, Y. A., Chen, C. I., Liu, J. C., and Sung, L. C. (2016). Influenza vaccination reduces hospitalization for heart failure in elderly patients with chronic kidney disease: A population-based cohort study. Acta Cardiol. Sin. 32 (3), 290–298. doi:10.6515/acs20150424l
Guo, Y., Lip, G. Y., and Apostolakis, S. (2012). Inflammation in atrial fibrillation. J. Am. Coll. Cardiol. 60 (22), 2263–2270. doi:10.1016/j.jacc.2012.04.063
Karjalainen, J., Nieminen, M. S., and Heikkilä, J. (1980). Influenza A1 myocarditis in conscripts. Acta Med. Scand. 207 (1-6), 27–30. doi:10.1111/j.0954-6820.1980.tb09670.x
Khan, M. Z., Patel, K., Patel, K. A., Doshi, R., Shah, V., Adalja, D., et al. (2021). Burden of atrial fibrillation in patients with rheumatic diseases. World J. Clin. Cases 9 (14), 3252–3264. doi:10.12998/wjcc.v9.i14.3252
Kim, S. C., Liu, J., and Solomon, D. H. (2016). Risk of incident atrial fibrillation in gout: A cohort study. Ann. Rheum. Dis. 75 (8), 1473–1478. doi:10.1136/annrheumdis-2015-208161
Korantzopoulos, P., Letsas, K., and Liu, T. (2012). Xanthine oxidase and uric acid in atrial fibrillation. Front. Physiol. 3, 150. doi:10.3389/fphys.2012.00150
Kuo, C. F., Grainge, M. J., Mallen, C., Zhang, W., and Doherty, M. (2016). Impact of gout on the risk of atrial fibrillation. Rheumatol. Oxf. 55 (4), 721–728. doi:10.1093/rheumatology/kev418
Kuo, C. F., Grainge, M. J., See, L. C., Yu, K. H., Luo, S. F., Zhang, W., et al. (2015). Epidemiology and management of gout in taiwan: A nationwide population study. Arthritis Res. Ther. 17, 13. doi:10.1186/s13075-015-0522-8
Kuo, Y. J., Tsai, T. H., Chang, H. P., Chua, S., Chung, S. Y., Yang, C. H., et al. (2016). The risk of atrial fibrillation in patients with gout: A nationwide population-based study. Sci. Rep. 6, 32220. doi:10.1038/srep32220
Lee, S. H., Chen, Y. C., Chen, Y. J., Chang, S. L., Tai, C. T., Wongcharoen, W., et al. (2007). Tumor necrosis factor-alpha alters calcium handling and increases arrhythmogenesis of pulmonary vein cardiomyocytes. Life Sci. 80 (19), 1806–1815. doi:10.1016/j.lfs.2007.02.029
Liu, T., Li, G., Li, L., and Korantzopoulos, P. (2007). Association between C-reactive protein and recurrence of atrial fibrillation after successful electrical cardioversion: A meta-analysis. J. Am. Coll. Cardiol. 49 (15), 1642–1648. doi:10.1016/j.jacc.2006.12.042
Luo, C. S., Chi, C. C., Fang, Y. A., Liu, J. C., and Lee, K. Y. (2020). Influenza vaccination reduces dementia in patients with chronic obstructive pulmonary disease: A nationwide cohort study. J. Investig. Med. 68 (4), 838–845. doi:10.1136/jim-2019-001155
Modin, D., Jorgensen, M. E., Gislason, G., Jensen, J. S., Kober, L., Claggett, B., et al. (2019). Influenza vaccine in heart failure. Circulation 139 (5), 575–586. doi:10.1161/CIRCULATIONAHA.118.036788
Musa, H., Kaur, K., O'Connell, R., Klos, M., Guerrero-Serna, G., Avula, U. M. R., et al. (2013). Inhibition of platelet-derived growth factor-AB signaling prevents electromechanical remodeling of adult atrial myocytes that contact myofibroblasts. Heart rhythm. 10 (7), 1044–1051. doi:10.1016/j.hrthm.2013.03.014
Pang, Y., Liu, X., Liu, G., Lv, M., Lu, M., Wu, J., et al. (2022). Effectiveness of influenza vaccination on in-hospital death and recurrent hospitalization in older adults with cardiovascular diseases. Int. J. Infect. Dis. 122, 162–168. doi:10.1016/j.ijid.2022.05.059
Pérez-Rubio, A., San Román, J. A., and Eiros Bouza, J. M. (2021). The impact of influenza vaccination on cardiovascular disease. Med. Clin. 157 (1), 22–32. doi:10.1016/j.medcli.2021.01.017
Phrommintikul, A., Kuanprasert, S., Wongcharoen, W., Kanjanavanit, R., Chaiwarith, R., and Sukonthasarn, A. (2011). Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur. Heart J. 32 (14), 1730–1735. doi:10.1093/eurheartj/ehr004
Pothineni, N. V. K., Subramany, S., Kuriakose, K., Shirazi, L. F., Romeo, F., Shah, P. K., et al. (2017). Infections, atherosclerosis, and coronary heart disease. Eur. Heart J. 38 (43), 3195–3201. doi:10.1093/eurheartj/ehx362
Rondy, M., El Omeiri, N., Thompson, M. G., Leveque, A., Moren, A., and Sullivan, S. G. (2017). Effectiveness of influenza vaccines in preventing severe influenza illness among adults: A systematic review and meta-analysis of test-negative design case-control studies. J. Infect. 75 (5), 381–394. doi:10.1016/j.jinf.2017.09.010
Rosenbaum, P. R., and Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika 70 (1), 41–55. doi:10.1093/biomet/70.1.41
Rothberg, M. B., Haessler, S. D., and Brown, R. B. (2008). Complications of viral influenza. Am. J. Med. 121 (4), 258–264. doi:10.1016/j.amjmed.2007.10.040
Savickas, V., Stewart, A. J., Rees-Roberts, M., Short, V., Bhamra, S. K., Corlett, S. A., et al. (2020). Opportunistic screening for atrial fibrillation by clinical pharmacists in UK general practice during the influenza vaccination season: A cross-sectional feasibility study. PLoS Med. 17 (7), e1003197. doi:10.1371/journal.pmed.1003197
Sester, U., Schmidt, T., Kuhlmann, M. K., Gartner, B. C., Uhlmann-Schiffler, H., and Sester, M. (2013). Serial influenza-vaccination reveals impaired maintenance of specific T-cell memory in patients with end-stage renal failure. Vaccine 31 (38), 4111–4120. doi:10.1016/j.vaccine.2013.06.076
Shrank, W. H., Patrick, A. R., and Brookhart, M. A. (2011). Healthy user and related biases in observational studies of preventive interventions: A primer for physicians. J. Gen. Intern. Med. 26 (5), 546–550. doi:10.1007/s11606-010-1609-1
Singh, J. A., and Cleveland, J. D. (2018). Gout and the risk of incident atrial fibrillation in older adults: A study of US medicare data. RMD Open 4 (2), e000712. doi:10.1136/rmdopen-2018-000712
Smetana, J., Chlibek, R., Shaw, J., Splino, M., and Prymula, R. (2018). Influenza vaccination in the elderly. Hum. Vaccin. Immunother. 14 (3), 540–549. doi:10.1080/21645515.2017.1343226
Smith, E., Hoy, D., Cross, M., Merriman, T. R., Vos, T., Buchbinder, R., et al. (2014). The global burden of gout: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73 (8), 1470–1476. doi:10.1136/annrheumdis-2013-204647
Spaetgens, B., de VriesF., , Driessen, J. H. M., Leufkens, H. G., Souverein, P. C., Boonen, A., et al. (2017). Risk of infections in patients with gout: A population-based cohort study. Sci. Rep. 7 (1), 1429. doi:10.1038/s41598-017-01588-5
Staerk, L., Wang, B., Preis, S. R., Larson, M. G., Lubitz, S. A., Ellinor, P. T., et al. (2018). Lifetime risk of atrial fibrillation according to optimal, borderline, or elevated levels of risk factors: Cohort study based on longitudinal data from the framingham heart study. Bmj 361, k1453. doi:10.1136/bmj.k1453
Taiwan Centers for Disease Control (2021). 2021 government-funded influenza vaccination program. Available from: http://at.cdc.tw/GV3J16 (Accessed 01 23, 2022).
Tamariz, L., Agarwal, S., Soliman, E. Z., Chamberlain, A. M., Prineas, R., Folsom, A. R., et al. (2011). Association of serum uric acid with incident atrial fibrillation (from the Atherosclerosis Risk in Communities [ARIC] study). Am. J. Cardiol. 108 (9), 1272–1276. doi:10.1016/j.amjcard.2011.06.043
Udell, J. A., Zawi, R., Bhatt, D. L., Keshtkar-Jahromi, M., Gaughran, F., Phrommintikul, A., et al. (2013). Association between influenza vaccination and cardiovascular outcomes in high-risk patients: A meta-analysis. Jama 310 (16), 1711–1720. doi:10.1001/jama.2013.279206
Zheng, J. Q., Lin, C. H., Chen, C. C., Lin, Y. F., Chiu, C. C., Yang, T. Y., et al. (2021). Role of annual influenza vaccination against lung cancer in type 2 diabetic patients from a population-based cohort study. J. Clin. Med. 10 (15), 3434. doi:10.3390/jcm10153434
Keywords: gout, influenza vaccination, arrhythmia, atrial fibrillation, hyperuricemia
Citation: Chen C-C, Chiu C-C, Chen N-H, Yang T-Y, Lin C-H, Fang Y-A, Jian W, Lei M-H, Yeh H-T, Hsu M-H, Hao W-R and Liu J-C (2022) Influenza vaccination and risk of atrial fibrillation in patients with gout: A nationwide population-based cohort study. Front. Pharmacol. 13:990713. doi: 10.3389/fphar.2022.990713
Received: 10 July 2022; Accepted: 18 August 2022;
Published: 26 September 2022.
Edited by:
James Cheng-Chung Wei, Chung Shan Medical University Hospital, TaiwanReviewed by:
Ming-Li Chen, Harvard University, United StatesTe-Chun Shen, China Medical University (Taiwan), Taiwan
Copyright © 2022 Chen, Chiu, Chen, Yang, Lin, Fang, Jian, Lei, Yeh, Hsu, Hao and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Rui Hao, Yjg1MDEwNDNAdG11LmVkdS50dw==; Ju-Chi Liu, bGl1bWRjdkB0bXUuZWR1LnR3
†These authors have contributed equally to this work
 Chun-Chao Chen
Chun-Chao Chen Chun-Chih Chiu1,2
Chun-Chih Chiu1,2 Nai-Hsuan Chen
Nai-Hsuan Chen Yu-Ann Fang
Yu-Ann Fang Hsien-Tang Yeh
Hsien-Tang Yeh Ju-Chi Liu
Ju-Chi Liu