- 1Institute for Brain Disorders, Beijing University of Chinese Medicine, Beijing, China
- 2Department of Neurology, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
- 3Beijing University of Chinese Medicine, Beijing, China
- 4Chinese Medicine Key Research Room of Brain Disorders Syndrome and Treatment of the National Administration of Traditional Chinese Medicine, Beijing, China
Background: Deciphering the biological basis of traditional Chinese medicine (TCM) syndromes in complex diseases is challenging. Rapid advances in multi-omics approaches provide new opportunities to unveil the biological basis of TCM syndromes. We intend to summarize the latest significant progress and highlight the crucial value of applying multi-omics approaches to reveal TCM syndromes of stroke in a new horizon.
Methods: We systematically searched PubMed, EMBASE, Web of Science Core Collection (WOSCC), Cochrane Library, China National Knowledge Infrastructure (CNKI), Chinese Science and Technology Periodical Database (VIP), Wanfang database and China Biology Medicine Database (SinoMed) for relevant studies from their inception to 31 March 2022, and conducted a comprehensive systematic review (PROSPERO registration number: CRD42021285922).
Results: A total of 43 relevant studies were included in the final systematic review, genomics, transcriptomics, proteomics, and metabolomics were all involved. Some gene polymorphisms, differential lncRNAs, mRNAs, miRNAs, proteins, and metabolites may be associated with TCM syndromes of stroke. In addition, some studies conducted a preliminary exploration on the different diseases with the same TCM syndrome. The results showed that thioredoxin-dependent peroxidase reductase may be the specific marker protein of Liver-yang transforming into wind syndrome, and the network formed by mir-146b-5p, -199a-5p, and 23 targeted mRNAs may be the biomarker of Blood-stasis syndrome.
Conclusion: Multi-omics technologies have served as powerful tools to investigate the complexity of TCM syndromes and may hold the promise of promoting the modernization of TCM as well as personalized medicine of TCM in stroke.
1 Introduction
Traditional Chinese medicine (TCM) has accumulated valuable medical experience over thousands of years, which has played an important role in maintaining people’s health (Cheung, 2011). TCM syndrome, as one of the key concepts in TCM, is a generalization of the cause, location, nature, and developmental tendency of a disease at a specific stage and is identified through a comprehensive analysis of the clinical symptoms and signs gathered by a practitioner using inspection, auscultation, olfaction, interrogation, and palpation of the pulses (Wang and Xu, 2014; Wang and Dong, 2017). Usually, the same disease has variable TCM syndromes. Correctly identifying the TCM syndrome is the cornerstone for TCM practitioners to understand diseases and guide individualized clinical medication (Wang and Xu, 2014). However, TCM syndrome differentiation has a certain degree of complexity, ambiguity, and subjectivity (Jiang et al., 2012; Gu and Chen, 2014). Deciphering the biological basis of TCM syndromes will be conducive to objectively diagnosing syndromes, discovering the potential targets of Chinese herbal medicine, and ultimately leading to the discovery of new therapeutic drugs and promoting precision medicine in TCM.
In recent years, a series of studies have been conducted to elucidate the biological basis of TCM syndromes using low-throughput sequencing methods; however, this is insufficient due to the complexity of TCM syndromes (Hou et al., 2014; Liu et al., 2014; Han et al., 2015). With the advent of systems biology era, high-throughput, high-content genomics, transcriptomics, proteomics, and metabolomics methods, combined with robust bioinformatics and computational tools have been widely and effectively applied in the biological basis research of TCM syndromes, which have provided unparalleled information about quantities and interactions of different biomolecules at the system and whole organism levels (Gu and Chen, 2014; Guo et al., 2020). Simultaneously, considerable achievements have been made, such as the biological basis of two TCM syndromes (Cold-congealing and qi-stagnation, Qi-stagnation and blood-stasis) in coronary heart disease, transcriptomic research on two TCM syndromes (Spleen-qi deficiency, Spleen-stomach damp-heat) in chronic atrophic gastritis, and the dynamic biological network of TCM syndromes in chronic hepatitis B (Lu et al., 2019; Wu et al., 2021; You et al., 2021).
It is worth noting that stroke, as the second leading cause of death in the world and ranks first in China, has made great advances in understanding the pathophysiology with omics technology, generating a large amount of data and information at the multi-omics level (Collaborators, 2021). It is encouraging that potential biomarkers associated with etiological classification and prognosis, as well as new therapeutic targets, have been identified (Montaner et al., 2020). Notably, the application of multi-omics technology has also provided new opportunities for the elucidation of TCM syndromes for stroke, including metabolomics research on Phlegm-heat syndrome and Blood-stasis syndrome, as well as transcriptomics research on Yin syndrome and Yang syndrome (Cha et al., 2013; Cha et al., 2015; Zhao et al., 2019).
Considering that there is no comprehensive review on the current status of applying multi-omics approaches to reveal the biological basis of TCM syndromes in stroke, we conducted this systematic review to summarize the related progress, analyze the challenges that need to be addressed, and provide important insights into the biological complexity of TCM syndromes for future research.
2 Methods
This systematic review was registered in PROSPERO (CRD42021285922).
2.1 Search strategy and selection criteria
Eight electronic databases were searched without language limitation (from their inception to 31 March 2022): PubMed, EMBASE, Web of Science Core Collection (WOSCC), Cochrane Library, China National Knowledge Infrastructure (CNKI), Chinese Science and Technology Periodical Database (VIP), Wanfang database, and China Biology Medicine Database (SinoMed). All searches were conducted by combining free-text and MESH terms, including stroke, omics, genomics, transcriptomics, proteomics, metabolomics, multi-omics, syndrome, ZHENG, and traditional Chinese medicine (Supplementary Table S1).
Two reviewers (MQ and XX) independently screened titles and abstracts and selected potential full texts for further analysis. Studies that fulfilled our pre-defined eligibility criteria were included in the review. Any disagreements were resolved through consensus or consultation with a third reviewer (XL). The detailed inclusion criteria were as follows: 1) stroke patients with specific TCM syndromes, 2) application of omics approaches to study TCM syndromes of stroke, and 3) experimental or observational studies. The exclusion criteria were as follows: 1) abstracts, editorials, letters, comments, case reports, and review papers; 2) articles on subarachnoid hemorrhage; and 3) intracerebral hemorrhage (ICH) caused by traumatic injury.
2.2 Data extraction
Data were independently extracted by two reviewers (MQ and XX) using a preformulated data collection form. A narrative summary of the results was produced according to specific data subjects: 1) the article’s author and publication year; 2) study characteristics, including the study site, disease, TCM syndromes, sample size, stroke onset time, omics type, omics technology, and specimen; and 3) the main findings. For each study, all relevant data were extracted from the tables, figures, text, and supplemental materials.
2.3 Quality assessment
The quality of included studies was assessed using an 11-item checklist recommended by the Agency for Healthcare Research and Quality. If an item was answered with “No” or “Unclear,” the item was scored as “0;” if the answer was “Yes,” the item was scored as “1.” Based on the total score (ranging from 0 to 11 points), the quality of the study was divided into high (8–11 points), fair (4–7 points), or low (< 4 points) (Hu et al., 2015; Zeng et al., 2015).
3 Results
Our systematic search yielded 2973 studies through eight electronic databases, 516 of which were excluded after duplication and 2268 were excluded after abstract review. A total of 43 relevant studies were included in the final data set after a full-text review (Figure 1) (Xiong et al., 2007; Huang et al., 2008; Jia et al., 2008; Xiao et al., 2008; Zeng et al., 2008; Zhao et al., 2008; Hu et al., 2009; Xiong et al., 2011; Shang et al., 2012; Wang et al., 2012; Cha et al., 2013; Chen et al., 2013; Xie et al., 2013; Li et al., 2014; Yang et al., 2014; Cha et al., 2015; Shen et al., 2015; Gu et al., 2016a; Gu et al., 2016b; Gu et al., 2016c; Gu et al., 2016d; Huo and Tan, 2016; Liao et al., 2016; Wang et al., 2016; Gu et al., 2017; Zhao et al., 2018; Gu et al., 2019a; Gu et al., 2019b; Gu et al., 2019c; Gu et al., 2019d; Li et al., 2019; Liu et al., 2019; Wei et al., 2019; Yang et al., 2019; Zhang et al., 2019; Zhao et al., 2019; Zhu et al., 2019; Gu et al., 2020a; Gu et al., 2020b; Rong and Li, 2020; Zhang et al., 2020; Gu et al., 2021; Li et al., 2022).
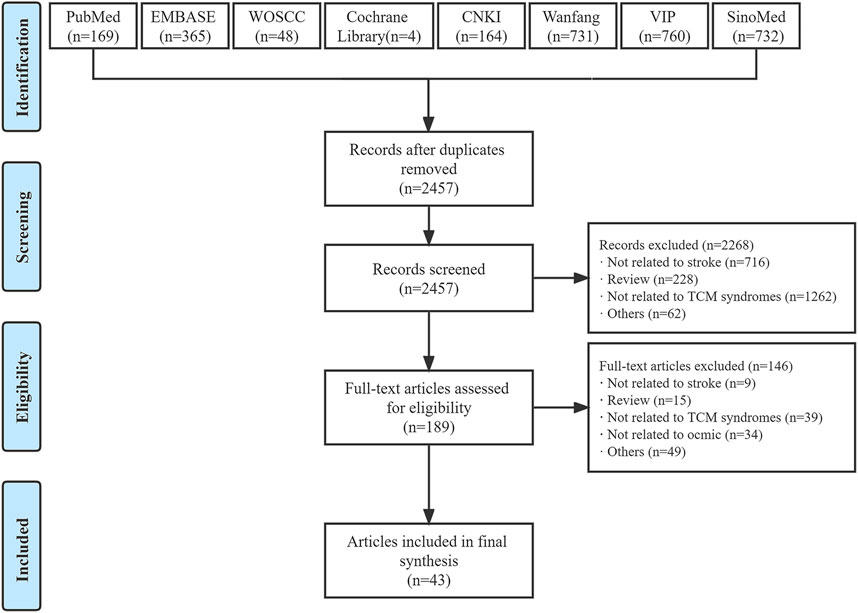
FIGURE 1. Flow diagram of study selection. CNKI, China National Knowledge Infrastructure; TCM, traditional Chinese medicine; VIP, Chinese Science and Technology Periodical Database; WOSCC, Web of Science Core Collection.
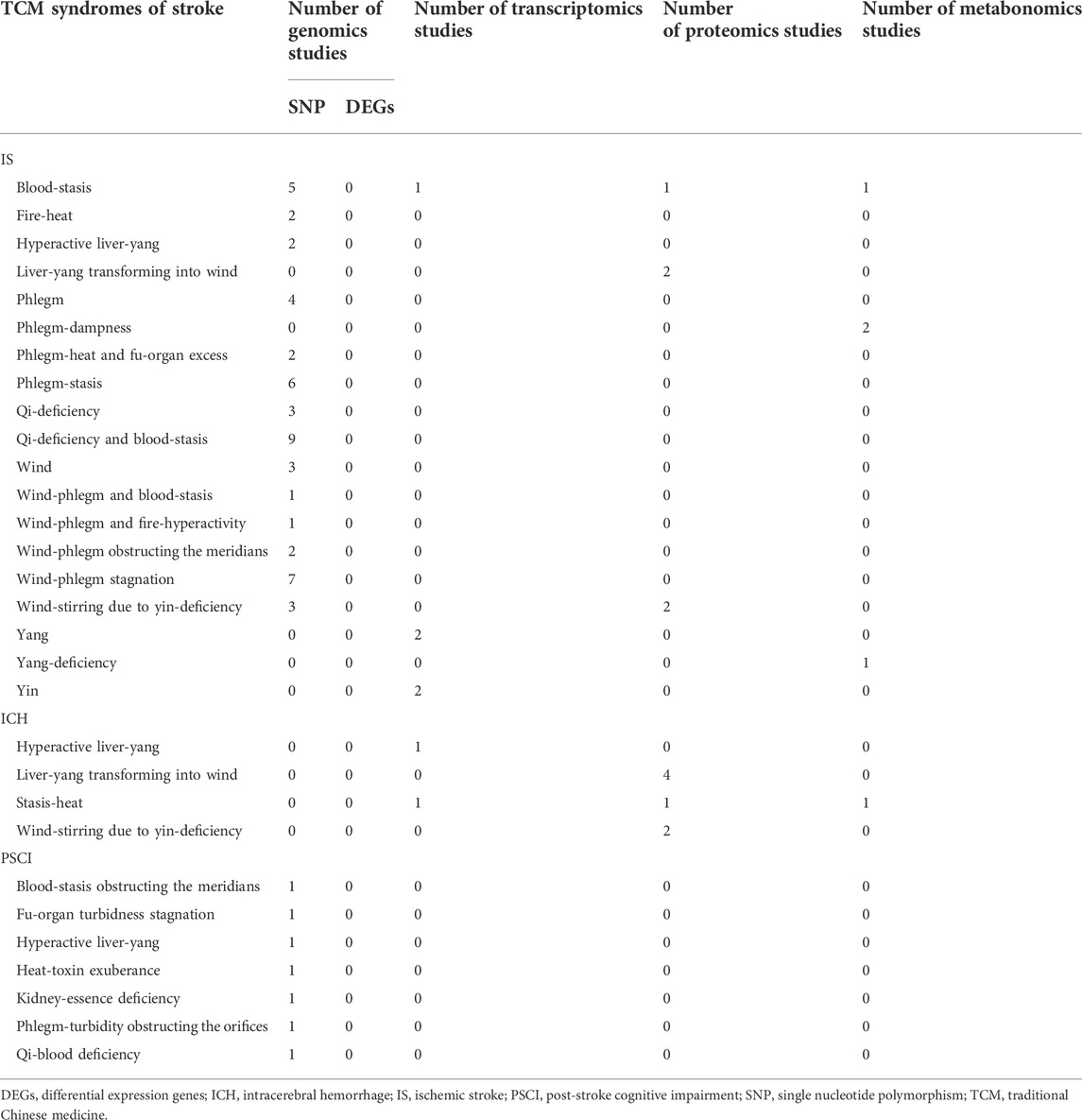
Overall, 43 studies ranged in size from eight to 1802 participants, of which 41 studies were conducted in China (Xiong et al., 2007; Huang et al., 2008; Jia et al., 2008; Xiao et al., 2008; Zeng et al., 2008; Zhao et al., 2008; Hu et al., 2009; Xiong et al., 2011; Shang et al., 2012; Wang et al., 2012; Chen et al., 2013; Xie et al., 2013; Li et al., 2014; Yang et al., 2014; Shen et al., 2015; Gu et al., 2016a; Gu et al., 2016b; Gu et al., 2016c; Gu et al., 2016d; Huo and Tan, 2016; Liao et al., 2016; Wang et al., 2016; Gu et al., 2017; Zhao et al., 2018; Gu et al., 2019a; Gu et al., 2019b; Gu et al., 2019c; Gu et al., 2019d; Li et al., 2019; Liu et al., 2019; Wei et al., 2019; Yang et al., 2019; Zhang et al., 2019; Zhao et al., 2019; Zhu et al., 2019; Gu et al., 2020a; Gu et al., 2020b; Rong and Li, 2020; Zhang et al., 2020; Gu et al., 2021; Li et al., 2022), and two in South Korea (Cha et al., 2013; Cha et al., 2015). Of these, 32 studies enrolled patients with ischemic stroke (IS) (Huang et al., 2008; Jia et al., 2008; Zeng et al., 2008; Hu et al., 2009; Shang et al., 2012; Wang et al., 2012; Cha et al., 2013; Xie et al., 2013; Li et al., 2014; Cha et al., 2015; Shen et al., 2015; Gu et al., 2016a; Gu et al., 2016b; Gu et al., 2016c; Gu et al., 2016d; Huo and Tan, 2016; Liao et al., 2016; Wang et al., 2016; Gu et al., 2017; Gu et al., 2019a; Gu et al., 2019b; Gu et al., 2019c; Gu et al., 2019d; Liu et al., 2019; Zhao et al., 2019; Zhu et al., 2019; Gu et al., 2020a; Gu et al., 2020b; Rong and Li, 2020; Zhang et al., 2020; Gu et al., 2021; Li et al., 2022), nine with ICH (Xiong et al., 2007; Xiao et al., 2008; Zhao et al., 2008; Chen et al., 2013; Yang et al., 2014; Zhao et al., 2018; Li et al., 2019; Yang et al., 2019; Zhang et al., 2019), one with stroke complications (Wei et al., 2019), and one with both IS and ICH (Tables 1–T4) (Xiong et al., 2011). Genomics, transcriptomics, proteomics, and metabolomics were involved in the omics approaches (Table 5). The quality of all the studies was fair (Supplementary Table S2).
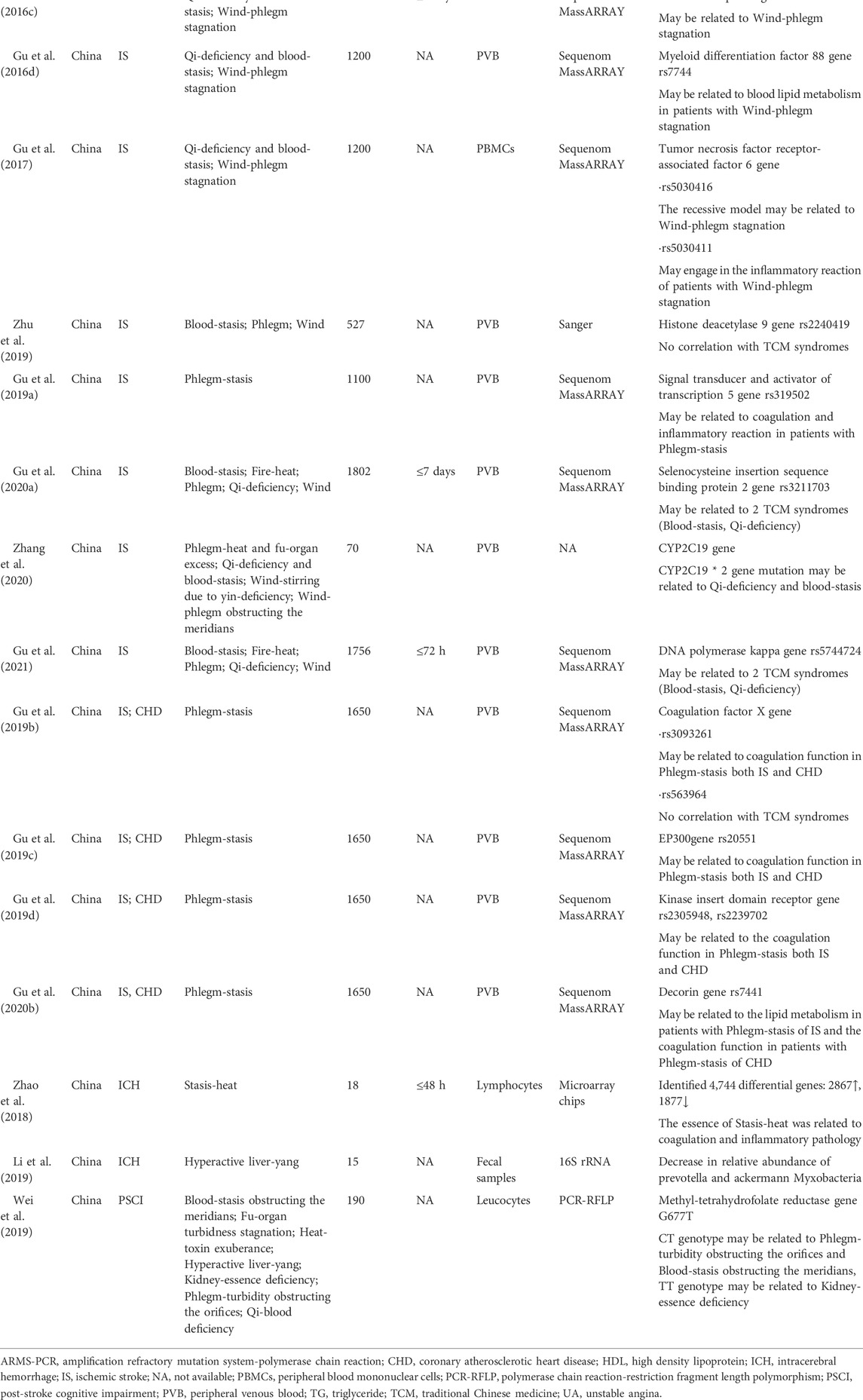
3.1 Genomic studies on traditional Chinese medicine syndromes of stroke
Human genomics, the study of the structure, function, and interactions of all genes in the human genome, are widely used to elucidate the scientific basis of TCM syndrome differentiation (Lazaridis and Petersen, 2005). In this section, 25 studies (Huang et al., 2008; Jia et al., 2008; Hu et al., 2009; Shang et al., 2012; Xie et al., 2013; Shen et al., 2015; Gu et al., 2016a; Gu et al., 2016b; Gu et al., 2016c; Gu et al., 2016d; Huo and Tan, 2016; Wang et al., 2016; Gu et al., 2017; Zhao et al., 2018; Gu et al., 2019a; Gu et al., 2019b; Gu et al., 2019c; Gu et al., 2019d; Li et al., 2019; Wei et al., 2019; Zhu et al., 2019; Gu et al., 2020a; Gu et al., 2020b; Zhang et al., 2020; Gu et al., 2021), containing IS, ICH and post-stroke cognitive impairment, mainly covered research on single nucleotide polymorphisms (SNP) and differentially expressed genes (DEGs) (Table 1).
3.1.1 Ischemic stroke
Genomics studies on TCM syndromes of IS have focused on SNP, which are the most common cause of DNA sequence polymorphism (Griffin and Smith, 2000). To some extent, SNP has few similarities with the “Innate Endowmentt” of TCM, which may affect an individual’s susceptibility to a specific TCM syndrome (Yang et al., 2021). All included studies collected peripheral venous blood at baseline to extract DNA, and then carried out primer design, synthesis, and polymerase chain reaction (PCR) amplification. Finally, specific technology was used for SNP genotyping.
Most studies found that some gene polymorphisms may be pivotal in the occurrence of Wind-phlegm stagnation syndrome of IS, including the platelet glycoprotein Iba (GP Iba) gene VNTR, toll-like receptor 5 gene rs5744174, toll-like receptor 7 gene rs2897827, and tumor necrosis factor receptor-associated factor 6 (TRAF6) gene rs5030416 (Shang et al., 2012; 2016; Gu et al., 2016c; Wang et al., 2016; Gu et al., 2017). Likewise, some gene polymorphisms, such as the GP Iba gene VNTR and CYP2C19 gene may be associated with Qi-deficiency and blood-stasis syndrome in IS (Shang et al., 2012; Zhang et al., 2020). Additionally, methylenetetrahydrofolate reductase C677T and selenocysteine insertion sequence binding protein 2 gene rs3211703 may be related to the pathogenesis of Blood-stasis syndrome of IS (Hu et al., 2009).
In addition to elucidating the scientific basis of TCM syndromes, researchers also revealed the relationships between gene polymorphisms and bodily functions in IS patients with specific TCM syndromes, including coagulation function, immunity, and blood lipid metabolism. The findings included the linkage between fibrinogen β-148C/T and coagulation function in patients with Wind-phlegm obstructing the meridians syndrome (Huo and Tan, 2016), between TRAF6 gene rs5030411 and inflammatory reaction in patients with Wind-phlegm stasis syndrome (Gu et al., 2017), and between myeloid differentiation factor 88 gene rs7744, histone deacetylase 9 gene rs2107595 and coagulation function in patients with Wind-phlegm stagnation syndrome (Gu et al., 2016a; Zhu et al., 2019).
In particular, three studies focused on different diseases with the same TCM syndrome, including Phlegm-stasis syndrome in patients with IS or coronary atherosclerotic heart disease (CHD). The results showed that coagulation factor X gene rs3093261, EP300 gene rs20551, and kinase insert domain receptor genes rs2305948 and rs2239702 may be related to the coagulation function in patients with Phlegm-stasis syndrome of IS and CHD, which indicated that different diseases with the same TCM syndrome may have the same biological basis (Gu et al., 2019b; Gu et al., 2019c; Gu et al., 2019d).
3.1.2 Intracerebral hemorrhage
Stasis-heat syndrome and Hyperactive liver-yang syndrome were the main syndromes of ICH in the two included studies, wherein the biological basis of TCM syndromes was investigated using DEGs. On the one hand, a total of 4,744 DEGs were identified in patients with Stasis-heat syndrome by using microarray chips to analyze lymphocytes (Zhao et al., 2018). Among these DEGs, few were further verified by real-time quantitative PCR, indicating that the Stasis-heat syndrome was intrinsically associated with coagulation and inflammatory pathology. On the other hand, fecal samples from patients were tested using the Illumina MiSeq platform, indicating that the Hyperactive liver-yang syndrome was related to the structural disorder of intestinal flora, with a reduced relative abundance of Prevotella and Ackermann myxobacteria (Li et al., 2019).
3.1.3 Post-stroke cognitive impairment
One study investigated the relationship between gene polymorphisms and TCM syndromes of post-stroke cognitive impairment using PCR-restriction fragment length polymorphism technology (Wei et al., 2019). Kidney-essence deficiency syndrome, Phlegm-turbidity obstructing the orifice syndrome, and Blood-stasis obstructing the meridians syndrome, all had a significant correlation with MTHFR gene C677T locus polymorphisms. Further correlation analysis showed that the former TCM syndrome was associated with the TT genotype, and the two latter TCM syndromes were associated with the CT genotype.
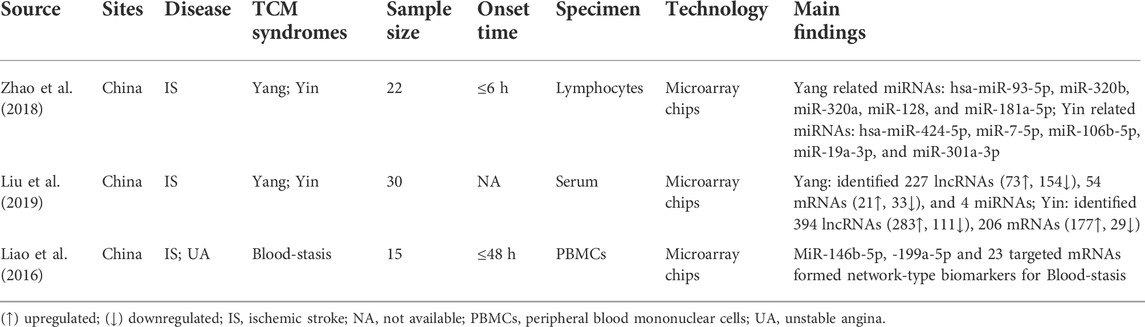
3.2 Transcriptomic studies on traditional Chinese medicine syndromes of stroke
Transcriptomics is the study of all transcripts in cells using microarray or RNA sequencing, including coding and non-coding RNAs, which is beneficial for revealing the intrinsic regulatory mechanisms of TCM syndromes (Manzoni et al., 2018; Montaner et al., 2020). Microarray technology is limited by the amount of RNA, quantification of transcript levels, and sequence information, however, it can still reveal the biological basis of TCM syndromes to a certain extent (Mutz et al., 2013). Microarray chips were used to investigate the transcriptomic characteristics of TCM syndromes of IS in the three included studies (Table 2) (Liao et al., 2016; Liu et al., 2019; Zhao et al., 2019).
Liu et al. (2019) and Zhao et al. (2019) focused on two TCM syndromes (Yin and Yang) of IS. The former found that there were some differences in the expression profiles of lncRNA, mRNA, and miRNA between the Yin syndrome and Yang syndrome. Further enrichment analysis revealed that the phenotypic differences between the Yin syndrome and Yang syndrome may be caused by blood pressure regulation, adrenergic receptor regulation, the renin-angiotensin system, and other pathways. The latter also identified some differentially expressed miRNAs; further enrichment analysis indicated that the key regulatory miRNAs, genes and pathways in Yang syndrome were hsa-miR-93-5p and -320b, enabled homologs, metabolic pathways, and mitogen-activated protein kinase signaling pathways, respectively, while those in Yin syndrome were hsa-miR-424-5p and -106b-5p, CNOT4, hepatitis B and pathways in cancer, respectively. Liao et al. (2016) found that 401 mRNAs and 11 miRNAs were differentially expressed in two conditions (IS and unstable angina) with the same TCM syndrome (Blood-stasis). Further bioinformatics analysis with validation by real-time quantitative PCR in an independent cohort demonstrated that miR-146b-5p, -199a-5p and 23 targeted mRNAs formed network-type biomarkers for the Blood-stasis syndrome.
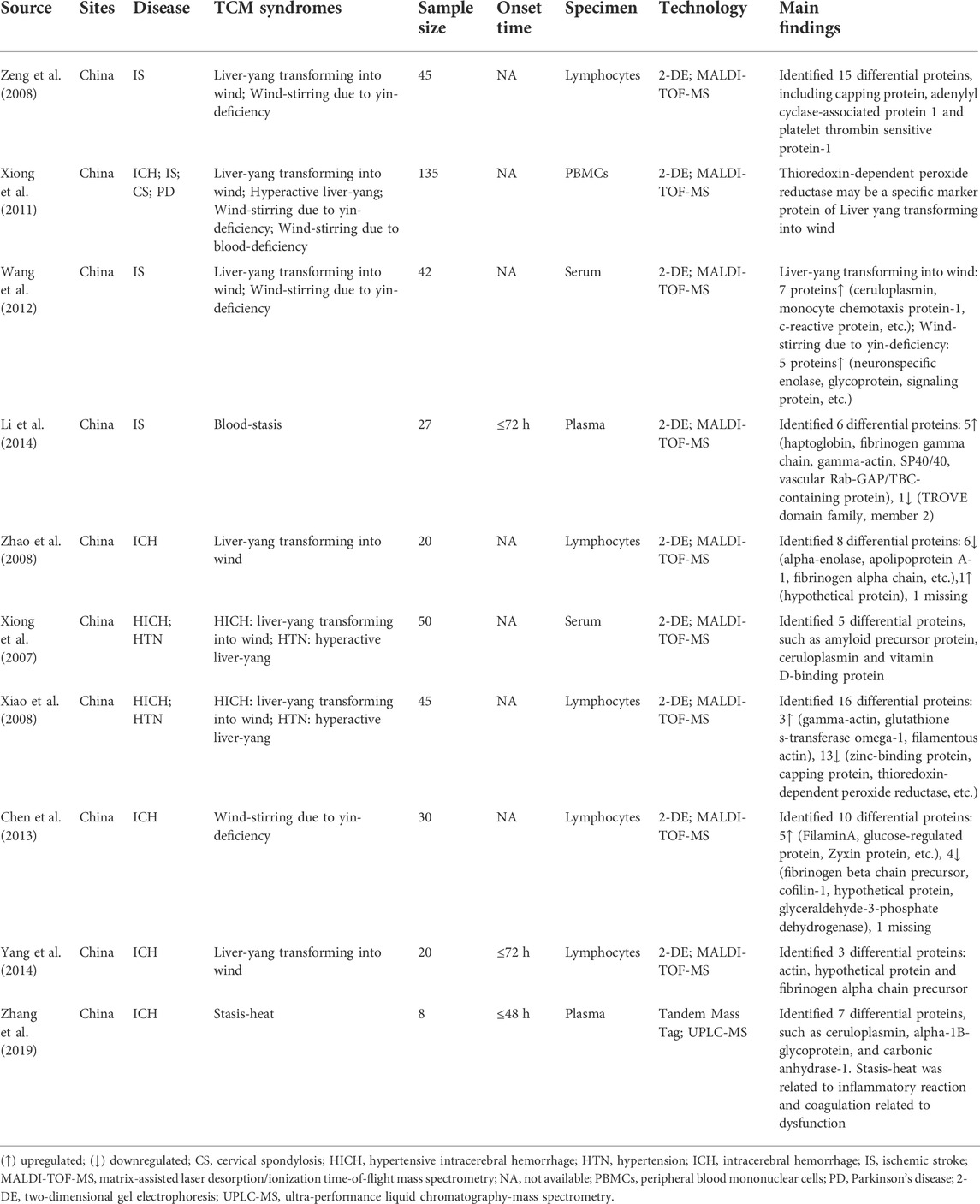
3.3 Proteomic studies on traditional Chinese medicine syndromes of stroke
The aim of proteomics in modern biology is to understand the expression, function, and regulation of the entire set of proteins encoded by an organism, the information of which will be invaluable for understanding how complex biological processes occur at a molecular level (Zhu et al., 2003). Proteomics research is conducive to exploring the microscopic material basis of TCM syndromes at the surface level (Zhou et al., 2012; Yang et al., 2021). At present, proteomic studies on TCM syndromes of stroke have mainly focused on exploring differential proteins (Table 3) (Xiong et al., 2007; Xiao et al., 2008; Zeng et al., 2008; Zhao et al., 2008; Xiong et al., 2011; Wang et al., 2012; Chen et al., 2013; Li et al., 2014; Yang et al., 2014; Zhang et al., 2019).
3.3.1 Ischemic stroke
A total of three studies were conducted by using two-dimensional gel electrophoresis (2DE) combined with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF-MS) analyses, in which Blood-stasis syndrome and Liver-yang transforming into wind syndrome of IS were investigated (Zeng et al., 2008; Wang et al., 2012; Li et al., 2014). Six differentially expressed proteins were identified in Blood-stasis syndrome of IS, of which one protein (TROVE domain family, member 2) was downregulated, while the others, such as haptoglobin, fibrinogen gamma chain, and gamma-actin, were upregulated (Li et al., 2014). Interestingly, Zeng et al. (2008) and Wang et al. (2012) compared the Liver-yang transforming into wind syndrome with Wind-stirring due to yin-deficiency syndrome of IS, but their results were different. The former identified 15 differentially expressed proteins, including capping protein, adenylyl cyclase-associated protein 1, and platelet thrombin sensitive protein-1. The latter identified seven upregulated proteins in the Liver-yang transforming into wind syndrome, including ceruloplasmin, monocyte chemotaxis protein-1, and c-reactive protein, and five upregulated proteins in Wind-stirring due to yin-deficiency syndrome, including neuron-specific enolase, glycoprotein, and signaling proteins.
In addition, Xiong et al. (2011) tried to reveal the biological mechanism of Liver-yang transforming into wind syndrome in four different diseases: including ICH, IS, Parkinson’s disease, and cervical spondylosis. Through the application of 2DE combined with MALDI-TOF-MS technology and further comparative analysis, the results demonstrated that thioredoxin-dependent peroxide reductase may be a common marker protein of Liver-yang transforming into wind syndrome in multiple diseases.
3.3.2 Intracerebral hemorrhage
Similar to proteomic studies on TCM syndromes of IS, there were five other studies using 2DE combined with MALDI-TOF-MS technology to carry out related TCM syndromes of ICH, including Wind-stirring due to yin-deficiency syndrome and Live-yang transforming wind syndrome (Xiong et al., 2007; Xiao et al., 2008; Zhao et al., 2008; Chen et al., 2013; Yang et al., 2014). Ten differential proteins were finally identified in Wind-stirring due to yin-deficiency syndrome, five of which were upregulated, including FilaminA, Zyxin protein, and glucose-regulated protein, while four were downregulated, including fibrinogen beta chain precursor, cofilin-1, and hypothetical protein (Chen et al., 2013). Eight differential proteins were identified in the Live-yang transforming wind syndrome, among which the hypothetical protein was upregulated, and six were downregulated, including alpha-enolase, apolipoprotein A-1, and fibrinogen alpha chain (Zhao et al., 2008). Moreover, two studies also focused on Liver-Yang transforming wind syndrome; however, they only concentrated on ICH caused by hypertension (Xiong et al., 2007; Xiao et al., 2008). In comparison with hypertensive patients with Hyperactive liver-yang syndrome and healthy individuals, one study identified five differentially expressed, including amyloid precursor protein, ceruloplasmin, and vitamin D-binding protein (Xiong et al., 2007); the other identified 16 differential proteins, three of which were upregulated, such as gamma-actin, glutathione s-transferase omega-1, and filamentous actin, while 13 were downregulated, such as zinc-binding protein, capping protein, and thioredoxin-dependent peroxide reductase (Xiao et al., 2008).
Of note, one study included 10 patients with Liver-yang transforming into wind syndrome of ICH within 3 days of onset, and thereafter observed patients whose TCM syndrome changed to Wind-stirring due to yin-deficiency syndrome within 3 months (Yang et al., 2014). Through comparative analysis before and after, actin, hypothetical protein, and fibrinogen alpha chain precursor may be closely related to the dynamic evolution of these two TCM syndromes. Furthermore, through Tandem Mass Tag combined with ultra-performance liquid chromatography-mass spectrometry (UPLC-MS), Zhang et al. (2019) finally identified seven differential proteins, such as ceruloplasmin, alpha-1B-glycoprotein, and carbonic anhydrase-1, which proved that the basis of Stasis-heat syndrome may be related to inflammatory reactions and coagulation related to dysfunctions.
3.4 Metabolomic studies on traditional Chinese medicine syndromes of stroke
Metabolomics is defined as the comprehensive analysis in which all the metabolites of a biological system are identified and quantified (Lindon and Nicholson, 2008). Unlike genes and proteins, metabolites serve as direct signatures of biochemical activity and are therefore, easier to correlate with phenotypes (Ussher et al., 2016). Nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry combined with chromatography are the main primary analytical methods. In this section, five studies were included, four of which focused on TCM syndromes of IS (Cha et al., 2013; Cha et al., 2015; Rong and Li, 2020; Li et al., 2022), whereas the rest focused on TCM syndromes of ICH (Table 4) (Yang et al., 2019).
3.4.1 Ischemic stroke
Metabolomic studies on the TCM syndromes of IS carried out by different groups have helped elucidate the biological basis of TCM syndromes. Phlegm-dampness syndrome, Yang-deficiency syndrome, and Blood-stasis syndrome were the main syndromes investigated in the four included studies. There were two studies on Phlegm-dampness syndrome using different metabolomics technologies (Cha et al., 2013; Rong and Li, 2020). The former used NMR and found 30 different metabolites, including 1-methylhistidine, alanine, and acetic acid, which were potential biomarkers for the Phlegm-dampness syndrome of IS (Cha et al., 2013). The latter used UPLC-MS and found that the levels of lysophosphatidylcholine (18:2) and lysophosphatidylcholine (20:3) in the Phlegm dampness syndrome were low, suggesting that the variation in plasma lipid profiles may serve as a potential biomarker for its diagnosis (Rong and Li, 2020). In addition, Seven differential metabolites, including acyl-carnitines, creatinine, and kynureninem, were identified to be associated with Blood-stasis syndrome by using ultra-high performance liquid chromatography-quadrupole-time of flight-mass spectrometry (Yang et al., 2019). In addition, the gas chromatography-time of flight-mass spectrometry method was applied in the study of Yang-deficiency syndrome, with 27 metabolites as potential markers (Li et al., 2022).
3.4.2 Intracerebral hemorrhage
Metabolomics has also been used to gain insights into the biological basis of TCM syndromes in ICH. Yang et al. (2019) investigated the metabolomic characteristics of the Stasis-heat syndrome of ICH by analyzing peripheral blood using UPLC-MS. The results showed that the pathogenesis of Stasis-heat syndrome of ICH was related to excess oxidative stress, inflammatory response, vascular sclerosis, and apoptosis. Moreover, the obtained cortisone 21 acetate, methyl acetate, and triglycerides could be used as potential biomarkers for the Stasis-heat syndrome of ICH.
4 Discussion
This systematic review provided a summary of the application of multi-omics approaches to reveal the biological basis of TCM syndromes in stroke. Omics data have prompted elucidation of the remarkable complexity of TCM syndromes. The current results demonstrated that some gene polymorphisms, differential lncRNAs, mRNAs, miRNAs, proteins, and metabolites may all be associated with TCM syndromes of stroke. Of note, some studies conducted a preliminary exploration of different diseases with the same TCM syndrome. The results showed that thioredoxin-dependent peroxidase reductase may be a common marker protein of Liver-yang transforming into wind syndrome, and the network formed by mir-146b-5p, -199a-5p, and 23 targeted mRNAs may be the biomarker of Blood-stasis syndrome. These results brought us closer to deciphering the biological basis of TCM syndromes in stroke, and even uncovered some potential biomarkers, especially for Liver-yang transforming into wind syndrome and Blood-stasis syndrome. With further validation, these findings may be applied to the objective diagnosis of TCM syndromes in future clinical practice and may also be potential targets of Chinese herbal medicine, which will facilitate the discovery of new therapeutic drugs. However, these results should be interpreted with caution because of the moderate quality of the included studies.
In addition to the omics methods used in the included studies, there are also epigenomics, glycomics, and lipidomics, which generate a large amount of information at the sample level but neglect the characteristics within individual cells concurrently. As new omics technologies continue to emerge, single-cell omics technologies, including single-cell genomes, transcriptomes, epigenomes, proteomes, and metabolomes, may be able to address cellular level heterogeneities and further discover new diagnostic and therapeutic targets (Islam et al., 2020). Currently, it has been used in the exploration of TCM syndromes. For example, Lu et al. (2021) used single-cell RNA sequencing technology to explore the significance of tumor heterogeneity in the classification of TCM syndromes of colorectal cancer and finally found that Excess syndrome and Deficiency syndrome may be related to tumor heterogeneity.
Notably, none of these included studies performed multi-omics integrated analysis. These included studies only stayed at a single omics level, ignoring the crosstalk between different molecular entities at different omics levels, which may have led to the omission of biologically relevant information. We did not perform an integrated analysis in this review due to significant heterogeneity among participants from different studies as well as the limited data from these included original articles. The main goal of omics research is not merely to find identifiable differences at the single-omics level but also to decipher the complexity of TCM syndromes at multiple layers at the molecular-level. Consequently, the integration of multi-omics data is becoming crucial for in-depth understanding of the biological basis of TCM syndromes in stroke, which ultimately leads to the discovery of biomarkers and novel therapeutic drugs, and promotes the modernization of TCM and personalized medicine of TCM in stroke (Gu and Chen, 2014; Guo et al., 2020). Future omics research on TCM syndromes should focus on the multi-omics levels and get the utmost out of high-precision algorithms. The best strategy to conduct integrated multi-omics analysis would rely on proteomics, genomics, transcriptomics, and metabolomics data which are acquired simultaneously from participants with low heterogeneity.
Fortunately, it was encouraging to see some promising findings recently, in which Li et al. (2007) established a network research paradigm integrating high-precision computational prediction, multi-omics data and experimental validation. Using this network strategy, we successfully discovered the molecular network characteristics of Spleen-deficiency syndrome at multiple molecular levels, and revealed that this TCM syndrome was closely related to insufficient immune response, including decreased macrophage activity and decreased lymphocyte proliferation (Wang et al., 2020).
Despite promising findings and advances in this field, multi-omics research related to TCM syndromes of stroke still needs to be improved in future studies. First, a recognized and consistent standard for TCM syndrome diagnosis or identification is fundamental for further uncovering the biological mechanism of TCM syndromes. Second, the control group should be set reasonably and strictly matched with the group of interest TCM syndrome to eliminate confounding factors. Third, to ensure data quality, strict standard operating procedures (SOP) should be set for sample collection, storage, processing and acquisition, such as SOP for the collection, storage, and transportation of fecal samples that conform to the unique features of TCM for fecal samples (Su et al., 2022). Fourth, external validation of biomarkers for potential TCM syndromes should be performed before incorporating them into clinical practice.
5 Conclusion
In facing the great challenge of research on TCM syndromes, multi-omics technologies combined with high-precision computational algorithms have served as powerful tools to investigate the complexity of TCM syndromes and may hold the promise of promoting the modernization of TCM as well as personalized medicine of TCM in stroke.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
YG and XL contributed to the concept and design. TL contributed to the systematic search of studies. MQ and XX contributed to study screening and data extraction. TL and XL drafted the manuscript. YG and XL contributed to the critical revision of the manuscript.
Funding
This work was supported by the the National Key Research and Development Project (2018YFC1705000), the National Science Foundation of China (82104823), Beijing Nova Program of Science and Technology (Z211100002121061) and the Young Elite Scientist Sponsorship Program by the China Association for Science and Technology (2021-QNRC1-04).
Acknowledgments
The authors acknowledge contributions from all the included studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.980650/full#supplementary-material
Abbreviations
CHD, coronary atherosclerotic heart disease; CNKI, China National Knowledge Infrastructure; DE, dimensional gel electrophoresis; DEGs, differentially expressed genes; GP, glycoprotein; ICH, intracerebral hemorrhage; IS, ischemic stroke; MALDI-TOF-MS, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry; NMR, nuclear magnetic resonance; PCR, polymerase chain reaction; SinoMed, China Biology Medicine Database; SNP, single nucleotide polymorphism; SOP, strict standard operating procedure; TCM, traditional Chinese medicine; TRAF6, tumor necrosis factor receptor-associated factor 6; UPLC-MS, ultra-performance liquid chromatography-mass spectrometry; VIP, Chinese Science and Technology Periodical Database; WOSCC, Web of Science Core Collection.
References
Cha, M. H., Jones, A. D., Ko, M. M., Zhang, C., and Lee, M. S. (2013). Metabolic profiles distinguish non-dampness-phlegm and dampness-phlegm patterns among Korean patients with acute cerebral infarction. Evid. Based. Complement. Altern. Med. 2013, 517018. doi:10.1155/2013/517018
Cha, M. H., Kim, M. J., Jung, J., Kim, J. H., Lee, M. S., and Kim, M. S. (2015). Metabolomic analysis of clinical plasma from cerebral infarction patients presenting with blood stasis. Evid. Based. Complement. Altern. Med. 2015, 453423. doi:10.1155/2015/453423
Chen, J., Zhang, Y., Xiong, X., Liang, Q., and Zhao, Y. (2013). Proteomics study on the syndrome-effect relationship of Dading Fengzhu decoction for intracerebral hemorrhage patients with Wind-stirring due to yin-deficiency syndrome in recovery stage. J. Hunan Univ. traditional Chin. Med. 33 (11), 57–62.
Collaborators, G. S., Stark, B. A., Johnson, C. O., Roth, G. A., Bisignano, C., Abady, G. G., et al. (2021). Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol. 20 (10), 795–820. doi:10.1016/S1474-4422(21)00252-0
Griffin, T. J., and Smith, L. M. (2000). Single-nucleotide polymorphism analysis by MALDI-TOF mass spectrometry. Trends Biotechnol. 18 (2), 77–84. doi:10.1016/s0167-7799(99)01401-8
Gu, L., Chen, Z., Li, M., Yan, Y., Liang, B., Yang, J., et al. (2019d). Correlation between KDR gene rs2305948, rs2239702 polymorphism and coagulation function of ischemic stroke, coronary heart disease with Phlegm-stasis syndrome. J. Beijing Univ. Traditional Chin. Med. 32 (4), 345–352.
Gu, L., Chen, Z., Long, J., Zhu, L., and Su, L. (2021). Correlation between rs5744724 polymorphism of DNA polymerase kappa (Polk) gene and ischemic stroke with Qi-deficiency syndrome and Blood-stasis syndrome. Chin. Archives Traditional Chin. Med. 39 (6), 8–13.
Gu, L., Chen, Z., Su, L., Yan, Y., Wu, G., Liang, B., et al. (2017). Association between TRAF6 gene polymorphisms and risk and inflammatory reactions of stroke with Wind-phlegm stagnation syndrome. J. Beijing Univ. Traditional Chin. Med. 40 (12), 1030–1036.
Gu, L., Chen, Z., Yan, Y., Long, J., Zhu, L., and Su, L. (2020a). Selenocysteine insertion sequence binding protein 2 gene rs3211703 polymorphism is significantly associated with Blood-stasis syndrome and Qi-deficiency syndrome in ischemic stroke. Chin. Archives Traditional Chin. Med. 38 (6), 34–38+65.
Gu, L., Gong, L., Huang, S., Li, J., Li, M., Li, T., et al. (2019a). Correlation analysis of STAT5A gene polymorphism rs319502 between coagulation function and inflammatory reaction in ischemic stroke of Phlegm-stasis syndrome. Liaoning J. Traditional Chin. Med. 46 (11), 2241–2245.
Gu, L., Huang, S., Li, M., Li, J., Li, T., Gong, L., et al. (2020b). Association analyses between decorin gene rs7441 polymorphism and Phlegm-Stasis syndrome of ischemic stroke and coronary atherosclerotic heart disease. Chin. Archives Traditional Chin. Med. 38 (2), 130–134.
Gu, L., Li, M., Li, J., Liang, B., Huang, S., and Su, L. (2019b). Correlation between genetic polymorphisms of F10 gene and coagulation markers of Phlegm-stasis syndrome in ischemic stroke and Phlegm-stasis syndrome in coronary heart disease. Chin. J. Gerontology 39 (16), 3878–3884.
Gu, L., Li, T., Li, M., Huang, S., Gong, L., Li, J., et al. (2019c). Relationship of EP300 gene rs20551 polymorphism with Phlegm-stasis syndrome and blood coagulation function in patients with ischemic stroke and coronary atherosclerotic heart disease. Chin. J. Geriatric Heart Brain Vessel Dis. 21 (7), 720–724.
Gu, L., Shen, T., Liang, B., Tan, J., Yan, Y., and Tang, N. (2016a). GWAS-supported variant rs2107595 polymorphism influence the serum lipid metabolism of ischemic stroke patients with Wind-phlegm stagnation syndrome. China J. Traditional Chin. Med. Pharm. 31 (11), 4484–4487.
Gu, L., Wu, Y., Liang, B., Tan, J., Chen, Q., Wei, Q., et al. (2016b). Association analysis of gene polymorphism of MAP2K4and MAPK1 and different traditional Chinese medicine syndromes and serum lipid levels in patients with ischemic stroke. J. Tradit. Chin. Med. 57 (10), 864–869.
Gu, L., Wei, Q., Xie, J., Chen, Q., Liang, B., and Tang, N. (2016d). Myeloid differentiation factor gene ( MYD88) polymorphism affects blood lipid metabolism in stroke with Phlegm-Stasis syndrome. Lishizhen Med. Materia Medica Res. 27 (5), 1266–1288.
Gu, L., Zhou, J., Chen, Q., Xie, J., Yan, Y., Liang, B., et al. (2016c). TOLL-like receptor-7 gene rs2897827 polymorphism increase the risk on stroke with Wind-phlegm stagnation syndrome in Han nationality females. China J. Traditional Chin. Med. Pharm. 31 (10), 4219–4222.
Gu, P., and Chen, H. (2014). Modern bioinformatics meets traditional Chinese medicine. Brief. Bioinform. 15 (6), 984–1003. doi:10.1093/bib/bbt063
Guo, R., Luo, X., Liu, J., Liu, L., Wang, X., and Lu, H. (2020). Omics strategies decipher therapeutic discoveries of traditional Chinese medicine against different diseases at multiple layers molecular-level. Pharmacol. Res. 152, 104627. doi:10.1016/j.phrs.2020.104627
Han, X., Gao, Y., Ma, B., Gao, Y., Sun, Y., Jiang, R., et al. (2015). The clinical relevance of serum NDKA, NMDA, PARK7, and UFDP levels with phlegm-heat syndrome and treatment efficacy evaluation of traditional Chinese medicine in acute ischemic stroke. Evid. Based. Complement. Altern. Med. 2015, 270498. doi:10.1155/2015/270498
Hou, J., Wang, J., Lin, C., Fu, J., Ren, J., Li, L., et al. (2014). Circulating MicroRNA profiles differ between qi-stagnation and qi-deficiency in coronary heart disease patients with blood stasis syndrome. Evid. Based. Complement. Altern. Med. 2014, 926962. doi:10.1155/2014/926962
Hu, J., Dong, Y., Chen, X., Liu, Y., Ma, D., Liu, X., et al. (2015). Prevalence of suicide attempts among Chinese adolescents: A meta-analysis of cross-sectional studies. Compr. Psychiatry 61, 78–89. doi:10.1016/j.comppsych.2015.05.001
Hu, M., Wang, Z., Li, T., Zhang, X., Xing, Z., Zhou, C., et al. (2009). Study on MTHFR C677T polymorphism in ischemic stroke with Blood-stasis syndrome. Chin. J. Inf. Traditional Chin. Med. 16 (3), 16–18.
Huang, B., Shao, W., Dong, M., Tu, J., and Wang, L. (2008). Association between traditional Chinese medicine syndromes in cerebral infarction and angiotensinogen gene M235T polymorphism. Med. J. Wuhan Univ. 29 (4), 482–484+507.
Huo, Q., and Tan, F. (2016). Study on traditional Chinese medicine syndromes of cerebral infarction and fibrinogen related gene polymorphism. Chin. J. Mod. Drug Appl. 10 (12), 80–81.
Islam, M., Chen, B., Spraggins, J. M., Kelly, R. T., and Lau, K. S. (2020). Use of single-cell -omic technologies to study the gastrointestinal tract and diseases, from single cell identities to patient features. Gastroenterology 159 (2), 453–466.e1. e1. doi:10.1053/j.gastro.2020.04.073
Jia, N., You, J., and Huang, P. (2008). Relationship between ACE gene polymorphism and initial traditional Chinese medicine syndrome of acute ischemic stroke. Liaoning J. traditional Chin. Med. 35 (4), 481–483.
Jiang, M., Lu, C., Zhang, C., Yang, J., Tan, Y., Lu, A., et al. (2012). Syndrome differentiation in modern research of traditional Chinese medicine. J. Ethnopharmacol. 140 (3), 634–642. doi:10.1016/j.jep.2012.01.033
Lazaridis, K. N., and Petersen, G. M. (2005). Genomics, genetic epidemiology, and genomic medicine. Clin. Gastroenterol. Hepatol. 3 (4), 320–328. doi:10.1016/s1542-3565(05)00085-6
Li, J., Chen, Z., Ma, Y., Wu, D., Hu, Y., and Li, J. (2022). Analysis of biomarkers of ischemic stroke with Yang-deficiency syndrome based on GC-TOF-MS combined with metabolomics. Hunan J. traditional Chin. Med. 38 (1), 6–10.
Li, S., Wang, F., Li, P., Zhao, H., Zhang, W., and Wang, Y. (2014). Preliminary study on proteomics of Blood-stasis syndrome in ischemic stroke. China J. Traditional Chin. Med. Pharm. 29 (12), 3977–3980.
Li, S., Zhang, Z. Q., Wu, L. J., Zhang, X. G., Li, Y. D., and Wang, Y. Y. (2007). Understanding ZHENG in traditional Chinese medicine in the context of neuro-endocrine-immune network. IET Syst. Biol. 1 (1), 51–60. doi:10.1049/iet-syb:20060032
Li, Y., Xu, H., Wang, J., Zheng, F., Deng, L., Li, J., et al. (2019). Analysis of bacterial flora structure of patients with cerebral hemorrhage due to Hyperactive liver-yang syndrome by 16S rRNA gene sequencing technique. Chin. J. Exp. Traditional Med. Formulae 25 (8), 83–88.
Liao, J., Liu, Y., and Wang, J. (2016). Identification of more objective biomarkers for Blood-Stasis syndrome Diagnosis. BMC Complement. Altern. Med. 16 (1), 371. doi:10.1186/s12906-016-1349-9
Lindon, J. C., and Nicholson, J. K. (2008). Spectroscopic and statistical techniques for information recovery in metabonomics and metabolomics. Annu. Rev. Anal. Chem. 1, 45–69. doi:10.1146/annurev.anchem.1.031207.113026
Liu, L., Gao, Y., and Ma, B. (2014). Exploring molecular mechanism underlying Chinese medicine syndrome: A study on correlation between Chinese medicine syndrome and biomarkers for ischemic stroke. Chin. J. Integr. Med. 20 (1), 11–18. doi:10.1007/s11655-013-1194-8
Liu, W., Li, G., He, C., Qiao, L., Shen, X., Cheng, X., et al. (2019). Analysis of serum transcriptome characteristics of patients with Yin syndrome and Yang syndrome of acute ischemic stroke. Chin. J. Exp. Traditional Med. Formulae 25 (15), 122–130.
Lu, Y., Fang, Z., Zeng, T., Li, M., Chen, Q., Zhang, H., et al. (2019). Chronic hepatitis B: Dynamic change in traditional Chinese medicine syndrome by dynamic network biomarkers. Chin. Med. 14, 52. doi:10.1186/s13020-019-0275-4
Lu, Y., Zhou, C., Zhu, M., Fu, Z., Shi, Y., Li, M., et al. (2021). Traditional Chinese medicine syndromes classification associates with tumor cell and microenvironment heterogeneity in colorectal cancer: A single cell RNA sequencing analysis. Chin. Med. 16 (1), 133. doi:10.1186/s13020-021-00547-7
Manzoni, C., Kia, D. A., Vandrovcova, J., Hardy, J., Wood, N. W., Lewis, P. A., et al. (2018). Genome, transcriptome and proteome: The rise of omics data and their integration in biomedical sciences. Brief. Bioinform. 19 (2), 286–302. doi:10.1093/bib/bbw114
Montaner, J., Ramiro, L., Simats, A., Tiedt, S., Makris, K., Jickling, G. C., et al. (2020). Multilevel omics for the discovery of biomarkers and therapeutic targets for stroke. Nat. Rev. Neurol. 16 (5), 247–264. doi:10.1038/s41582-020-0350-6
Mutz, K. O., Heilkenbrinker, A., Lonne, M., Walter, J. G., and Stahl, F. (2013). Transcriptome analysis using next-generation sequencing. Curr. Opin. Biotechnol. 24 (1), 22–30. doi:10.1016/j.copbio.2012.09.004
Rong, L., and Li, Y. (2020). Study on biomarkers of Phlegm-dampness syndrome in ischemic stroke based on metabonomics. J. Guangzhou Univ. Traditional Chin. Med. 37 (2), 195–200.
Shang, Y., Bai, J., Shi, C., Li, T., Feng, Q., Zheng, H., et al. (2012). Correlation between platelet membrane glycoprotein Iba gene polymorphism and traditional Chinese medicine syndromes of arteriosclerotic cerebral infarction. Lishizhen Med. Materia Medica Res. 23 (8), 1994–1996.
Shen, T., Gu, L., Chen, Q., Liang, B., and Yan, Y. (2015). Association study on rs2107595 polymorphism identified by GWAS and ischemic stroke of Qi-deficiency syndrome and Blood-stasis syndrome. J. Guangxi Univ. Traditional Chin. Med. 18 (4), 5–8.
Su, W., Du, Y., Lian, F., Wu, H., Zhang, X., Yang, W., et al. (2022). Standards for collection, preservation, and transportation of fecal samples in TCM clinical trials. Front. Cell. Infect. Microbiol. 12, 783682. doi:10.3389/fcimb.2022.783682
Ussher, J. R., Elmariah, S., Gerszten, R. E., and Dyck, J. R. (2016). The emerging role of metabolomics in the diagnosis and prognosis of cardiovascular disease. J. Am. Coll. Cardiol. 68 (25), 2850–2870. doi:10.1016/j.jacc.2016.09.972
Wang, H., and Xu, A. (2014). Zheng: A systems biology approach to diagnosis and treatments. Science 346 (6216), S13–S15.
Wang, L., Liang, Q., Chen, X., Yang, L., Tang, K., Liu, Q., et al. (2012). A comparative study on proteomics of cerebral infarction with Liver-yang transforming into wind syndrome and Wind-stirring due to yin-deficiency syndrome. J. Hunan Univ. traditional Chin. Med. 32 (7), 54–57.
Wang, T., and Dong, J. (2017). What is “zheng” in traditional Chinese medicine? J. Traditional Chin. Med. Sci. 4 (1), 14–15. doi:10.1016/j.jtcms.2017.08.005
Wang, W., Huang, J., Tan, J., Chen, Q., Xie, J., Yang, J., et al. (2016). Toll like receptor 5 polymorphism is significantly associated with ischemic stroke with Wind-phlegm stagnation syndrome. Liaoning J. traditional Chin. Med. 43 (12), 2495–2497.
Wang, X., Wu, M., Lai, X., Zheng, J., Hu, M., Li, Y., et al. (2020). Network pharmacology to uncover the biological basis of spleen qi deficiency syndrome and herbal treatment. Oxid. Med. Cell. Longev. 2020, 2974268. doi:10.1155/2020/2974268
Wei, L., Xie, D., Zhang, J., Bao, Y., Huang, X., Jin, S., et al. (2019). Investigation of the correlation between traditional Chinese medicine syndromes and MTHFR C677T polymorphism of methylenetetrahydrofolate reductase in post-stroke cognitive impairment. J. Liaoning Univ. Traditional Chin. Med. (2), 95–98.
Wu, G., Zhao, J., Zhao, J., Song, N., Zheng, N., Zeng, Y., et al. (2021). Exploring biological basis of Syndrome differentiation in coronary heart disease patients with two distinct Syndromes by integrated multi-omics and network pharmacology strategy. Chin. Med. 16 (1), 109. doi:10.1186/s13020-021-00521-3
Xiao, M., Liang, Q., Xiong, X., Zeng, N., Qu, J., Zhang, Y., et al. (2008). Study of peripheral blood mononuclear cells of hypertension intracerebral hemorrhage patients with Liver-yang transforming into wind syndrome by proteomics technology. Pract. Prev. Med. 15 (3), 623–627.
Xie, J., Gu, L., Chen, Q., Wu, G., Yan, Y., and Su, L. (2013). Correlation study on 12p13 single nucleotide polymorphism rs12425791 and Chinese medical syndrome types in ischemic stroke patients of the Han nationality. Chin. J. Integr. Traditional West. Med. 33 (1), 47–50.
Xiong, X., Chen, J., Liang, Q., Fan, R., Zeng, Q., Qu, J., et al. (2011). Proteomics study on the essence of wind syndrome caused by gan-yang hyperactivity in Chinese medicine. Chin. J. Integr. Traditional West. Med. 31 (7), 913–920.
Xiong, X., Liang, Q., Hou, J., Chen, J., Liu, A., Yan, D., et al. (2007). Study on serum proteomics of hypertensive intracerebral hemorrhage patients with Liver-yang transforming into wind syndrome and Hyperactive liver-yang syndrome. Pract. Prev. Med. 14 (6), 1649–1652.
Yang, B., Liang, Q., Xiong, X., Chen, J., and Xiao, M. (2014). A proteomic comparative study of hypertensive cerebral hemorrhage in acute stage of Liver-yang transforming into wind syndrome and in recovery stage of Wind-stirring due to yin-deficiency syndrome. J. Hunan Univ. Traditional Chin. Med. 34 (10), 34–38+65.
Yang, G., He, H., Dong, Y., Duan, L., Chen, H., and Wang, J. (2021). Research progress and reflection on omics studies on coronary heart disease with binding of Phlegm-stasis syndrome. J. Tradit. Chin. Med. 62 (3), 189–194.
Yang, X., Gao, J., Zhang, N., Yang, S., Yang, D., Yu, M., et al. (2019). Biomarkers of the pathogenesis of Stasis-heat syndrome in acute intracerebral hemorrhage based on the plasma differential metabonomics. Mod. Traditional Chin. Med. Materia Materia-World Sci. Technol. 21 (10), 2062–2072.
You, L., Zhang, S., Li, T., Sang, X., Li, K., Wang, W., et al. (2021). Integrated analyses of miRNA and mRNA profiles in leukocytes and serums in traditional Chinese medicine (TCM)-defined Pi-qi-deficiency syndrome and Pi-wei damp-heat syndrome resulting from chronic atrophic gastritis. Chin. Med. 16 (1), 4. doi:10.1186/s13020-020-00416-9
Zeng, N., Liang, Q., Xiong, X., Qu, J., Xiao, M., Zhang, Y., et al. (2008). Proteromics analysis and identification on peripheral blood lymphocyte of Liver-yang transforming into wind syndrome of cerebral infarction. Chin. J. Inf. Traditional Chin. Med. 15 (4), 11–15.
Zeng, X., Zhang, Y., Kwong, J. S., Zhang, C., Li, S., Sun, F., et al. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based. Med. 8 (1), 2–10. doi:10.1111/jebm.12141
Zhao, F., Huang, Y., Wu, M., Li, G., and Wu, M. (2018). Expressions of spectrum of inflammation-related and clotting-related genes in hemorrhagic stroke patients with Stasis-heat syndrome. J. Tradit. Chin. Med. 59 (20), 1753–1757.
Zhang, N., Tian, T., Yu, M., and Li, G. (2019). Differential proteomics analysis of pathogenic unit of Stasis-heat syndrome for acute intracerebral hemorrhage. Chin. J. Integr. Traditional West. Med. 39 (6), 675–680.
Zhang, Y., Wang, Q., Ding, Q., Wang, S., Zhu, K., Wang, J., et al. (2020). Correlation between CYP2C19 gene polymorphism and traditional Chinese medicine syndromes distribution in 70 patients with cerebral infarction. Chin. J. Hosp. Pharm. 40 (9), 1033–1037.
Zhao, H., Liu, P., Xu, C., Li, G., Gao, L., and Luo, Y. (2019). Unique MicroRNAs signature of lymphocyte of yang and yin syndromes in acute ischemic stroke patients. Chin. J. Integr. Med. 25 (8), 590–597. doi:10.1007/s11655-018-2843-3
Zhao, Y., Liang, Q., Xiong, X., Fan, R., Liang, X., Yang, B., et al. (2008). Effect of Zhengan Xifeng decoction on proteomics of peripheral blood mononuclear cell in intracerebral hemorrhage patients with Liver-yang transforming into wind syndrome. China J. Traditional Chin. Med. Pharm. 23 (10), 885–889.
Zhou, H., Chen, H., Zhou, X., Wang, M., and Wu, M. (2012). Proteomics is the important technology platform of Chinese medicine pathogenesis research. Chin. J. Integr. Traditional West. Med. 32 (7), 990–993.
Zhou, M., Wang, H., Zeng, X., Yin, P., Zhu, J., Chen, W., et al. (2019). Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet 394 (10204), 1145–1158. doi:10.1016/S0140-6736(19)30427-1
Zhu, H., Bilgin, M., and Snyder, M. (2003). Proteomics. Annu. Rev. Biochem. 72, 783–812. doi:10.1146/annurev.biochem.72.121801.161511
Keywords: stroke, traditional Chinese medicine, syndromes, multi-omics, systematic review
Citation: Liu T, Qin M, Xiong X, Lai X and Gao Y (2022) Multi-omics approaches for deciphering the complexity of traditional Chinese medicine syndromes in stroke: A systematic review. Front. Pharmacol. 13:980650. doi: 10.3389/fphar.2022.980650
Received: 28 June 2022; Accepted: 08 August 2022;
Published: 06 September 2022.
Edited by:
Xian-Jun Fu, Shandong University of Traditional Chinese Medicine, ChinaReviewed by:
Dong Bai, China Academy of Chinese Medical Science, ChinaYunhui Chen, Chengdu University of Traditional Chinese Medicine, China
Xuezhong Zhou, Beijing Jiaotong University, China
Copyright © 2022 Liu, Qin, Xiong, Lai and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Gao, gaoying973@163.com; Xinxing Lai, new-star@163.com
 Tingting Liu
Tingting Liu