
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 18 July 2022
Sec. Drugs Outcomes Research and Policies
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.935764
This article is part of the Research Topic Evidence for Assessing Drug Safety and Drug Use in Older People - Volume II View all 11 articles
Objectives: Polypharmacy and potentially inappropriate medication (PIM) use are frequent in older lung cancer patients. This study aimed to examine the trends of polypharmacy and PIM use and explore risk factors for PIM use based on the 2019 Beers criteria in older Chinese lung cancer outpatients with multimorbidity.
Methods: A repeated cross-sectional study was conducted using electronic medical data consisting of the prescriptions of older lung cancer outpatients in China from January 2016 to December 2018. Polypharmacy was defined as the use of five or more medications. The 2019 Beers criteria were used to evaluate the PIM use of older cancer outpatients (age ≥65 years), and multivariate logistic regression was used to identify the risk factors for PIM use.
Results: A total of 3,286 older lung cancer outpatients and their prescriptions were included in the study. The prevalence of polypharmacy was 14.27% in 2016, 16.55% in 2017, and 18.04% in 2018. The prevalence of PIM use, according to the 2019 Beers criteria, was 31.94% in 2016, 35.78% in 2017, and 42.67% in 2018. The two most frequently used PIMs in older lung cancer outpatients were estazolam and tramadol. The logistic regression demonstrated that age 75 to 79, polypharmacy, irrational use of drugs, and lung cancer accompanied by sleep disorders, anxiety or depression, or pain were positively associated with PIM use in older lung cancer outpatients.
Conclusion: The prevalence of polypharmacy and PIM use in older lung cancer outpatients with multimorbidity was high in China, and polypharmacy and PIM use increased over time. Further research on interventions rationing PIM use in the older lung cancer patient population is needed.
Lung cancer is the leading cause of cancer death worldwide, accounting for nearly 1.80 million deaths and causing 18% of total cancer deaths in 2020 (Global Cancer Observatory, 2020; WHO, 2022). Older age is associated with cancer development due to biological factors that include DNA damage over time and shortened telomeres. As the population continues to age, the incidence of lung cancer in older patients is expected to further increase in the coming years (Decoster and Schallier, 2019). Approximately 37% of lung cancer cases occur in individuals over 75 years old. Accordingly, the median age at lung cancer diagnosis is 70 years old for both men and women (Torre et al., 2016). The majority of older lung cancer patients have comorbid chronic diseases and must take multiple medications (Grose et al., 2014; Nilsson et al., 2017; Ding et al., 2020). However, increased number of drug-related problems was associated with age-induced alternations in pharmacokinetics (PK) and pharmacodynamics (PD). Lung cancer also effects pharmacokinetics and pharmacodynamics and occurs more frequently in the elderly. Therefore, lung cancer patients who are elderly are more prone to experience adverse drug events. In addition, previous published studies have confirmed that cancer patients are easily exposed to a higher risk of polypharmacy and inappropriate medication use (Wildiers et al., 2014; Koczwara et al., 2022).
Polypharmacy (defined as the use of more than five medicines) is associated with the prescription of inappropriate medications, and extensive studies have demonstrated the link between polypharmacy and negative outcomes (Maddison et al., 2011; Weng et al., 2013; LeBlanc et al., 2015). Potentially inappropriate medication (PIM) use was firstly proposed in 1991 because PIM use brought a series of drug-related problems, such as adverse drug events, hospitalization, and disability, defined as the use of medications that should be avoided, especially when evidence is insufficient or alternative medicines are available (Hyttinen et al., 2016; Muhlack et al., 2017; Wallace et al., 2017).
Some previous reports have examined the trends of polypharmacy and PIM use in older patients (Davidoff et al., 2015; Moriarty et al., 2015; Muhlack et al., 2018). Approximately half of all cancer care is delivered in an outpatient treatment setting (Maleki et al., 2022). It is necessary to investigate the polypharmacy and PIM use in older lung cancer outpatients. However, no study has specifically reported on the trends of polypharmacy and PIM use in older lung cancer outpatients, and the risk factors for PIM use according to the 2019 Beers criteria in older Chinese lung cancer patients are unclear. Therefore, in this study, we extracted data on the prescriptions of older lung cancer outpatients treated at tertiary hospitals in Chengdu, China over 3 years. The trends of the prevalence of polypharmacy and PIM use were calculated, and PIMs were screened based on the 2019 Beers criteria. The risk factors for PIM use were explored. Ideally, this study will provide useful data for follow-up research.
A repeated cross-sectional study was performed to examine the trends of polypharmacy and PIM use among older lung cancer (histology: non-small-cell lung cancer, small cell lung cancer, unspecified lung cancer; stage: American Joint Commission on Cancer 8th Edition (AJCC) stage I-III) outpatients with multimorbidity that might receive chemotherapy and chronic disease treatment in tertiary hospitals in Chengdu, a capital city in southwest China. The prescriptions of older (aged ≥65) lung cancer outpatients with multimorbidity (cancer with other diseases) were cluster sampled from a cooperative hospital prescription analysis project led by the Chinese Pharmaceutical Association. In this study, cluster sampling was used to randomly select nine hospitals from all tertiary hospitals in Chengdu between 1 January 2016 and 31 December 2018, and then the older lung cancer outpatient prescriptions were selected from all departments of the selected hospitals as the survey samples. Multimorbidity of patients was determined by the numbers of diagnosis in medical record. All data were retrospectively collected without any possibility of individual identification.
In this repeated cross-sectional study, we included older adults with lung cancer attending outpatient department at tertiary care hospitals in Chengdu from 1 January 2016 to 31 December 2018; thus, the prescriptions of 1,002, 1,009, and 1,275 older lung cancer outpatients were included from 2016, 2017, and 2018, respectively. The data were collected by diagnosis type as follows: 1) basic information (region, prescription code, and department source); 2) patient characteristics (age, sex, and diagnosis); and 3) medication characteristics (generic name, trade name, drug specifications, dosage form, administration route, number of prescriptions, prescription expenditure, and frequency of administration). The criteria in the count of prescribed medications are as follows: 1) duration of prescription (≤1 month); 2) route of administration (oral medications, injection medications, topical medications, inhaler, etc.); 3) medications directly related to treatment for lung cancer were counted as concomitant medications (such as oral tyrosine kinase inhibitor or antiemetic for chemo); 4) Chinese traditional herbal medications were not included.
The 2019 Beers criteria (By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, 2019) were used to evaluate PIM use in older lung cancer outpatients who were not receiving palliative care or hospice service. The comments about the rationality of prescription were made according to the Chinese Prescription Administrative Policy. The Chinese Prescription Administrative Policy need pharmacists to evaluate the standardization of prescription and the suitability of clinical use of drugs (medication indications, drug selection, route of administration, usage and dosage, drug interaction, incompatibility, etc.) according to relevant regulations, finding existing or potential problems, formulating and implementing intervention and improvement measures to promote the rational application of clinical drugs. Irrational prescriptions were classified as nonstandard prescriptions, inappropriate prescriptions, and supernormal prescriptions referring to medication without indications. Any inconsistencies between the two researchers were reviewed by a third professional and then resolved through collective discussion.
Categorical data are presented according to frequency, and the χ2 test was used to compare categorical variables between groups. Continuous data that were normally distributed are expressed as the mean ± standard deviation (SD), and continuous data that were not normally distributed are expressed as the median (M) and the interquartile range (IQR). Participant sex was categorized as male or female. Age was categorized into four groups: 65–69, 70–74, 75–79, and ≥80 years old, and the number of diseases was divided into three groups: two, three to four, and five or more chronic conditions. For the descriptive analysis, medication use was divided into two strata: the use of one to four medications and the use of five or more medications. Prescriptions were further categorized as rational or irrational. The prescription expenditure was divided into three groups: <500 Chinese yuan, 500–1,000 Chinese yuan, and >1,000 Chinese yuan. Five chronic diseases (sleep disorders, anxiety or depression, pain, pulmonary infection, and chronic obstructive pulmonary disease) were also analyzed. The associations between the risk factors and PIM use (non-PIM use = 0, PIM use = 1) were assessed with a multivariate logistic regression analysis. Statistical analyses were conducted using SPSS version 26.0 (IBM Corp., Armonk, NY). We constructed three models: Model 1 (logistic regression with no adjustment), Model 2 (adjusted for year), and Model 3 (adjusted for year, sex and age). The results are presented as odds ratios (ORs) and 95% confidence intervals (CIs), and p < 0.05 was considered to be statistically significant.
This study protocol was approved by the Sichuan University West China Hospital Research Ethics Board (2020/651).
A total of 3,286 older lung cancer outpatients were included in this study, 55.90% (n = 1,837) of which were male. The median age was 72 (IQR: 68, 76) years old, and age ranged from 65 to 94 years old; the oldest (≥80 years of age) cancer patients accounted for 11.63% (n = 1,153) of the sample. The median number of medical diagnoses was 3 (IQR: 2, 4). The median number of prescriptions was 2 (IQR: 1, 4), and 16.43% (n = 540) of older lung cancer outpatients had polypharmacy. The prevalence of rational prescriptions was 92.64% (n = 3,044), 7.36% (n = 242) had irrational prescription. The characteristics of 242 participants were 60.74% (n = 147) of which were male, the median age was 72 years older and 42.98% (n = 104) of patients had polypharmacy. The median prescription expenditure was 517.90 (IQR: 189.50, 1309.47) Chinese yuan (CNY). In this study, 19.32% (n = 635) of the lung cancer patients had sleep disorders, 3.13% (n = 103) had anxiety or depression, 24.01% (n = 789) had pain, 11.56% (n = 380) had pulmonary infections, and 5.11% (n = 168) had chronic obstructive pulmonary disease (COPD). The basic patient characteristics are provided in Table 1.
There were 1,002, 1,009, and 1,275 older lung cancer outpatients with prescriptions included in 2016, 2017, and 2018, respectively. The prevalence of polypharmacy increased from 14.27% (n = 143) in 2016 to 18.04% (n = 230) in 2018. The prevalence of PIM use increased from 31.94% (n = 320) to 42.67% (n = 544) over the 3 years. The number of medications and diseases showed an increasing trend from 2016 to 2018. The prevalence of rational prescriptions increased from 91.22% (n = 914) in 2016 to 93.65% (n = 1194) in 2018, but the average prescription expenditure showed a decreasing trend from 1,260.77 CNY per prescription in 2016 to 1,170.45 CNY per prescription in 2018 (Figure 1).
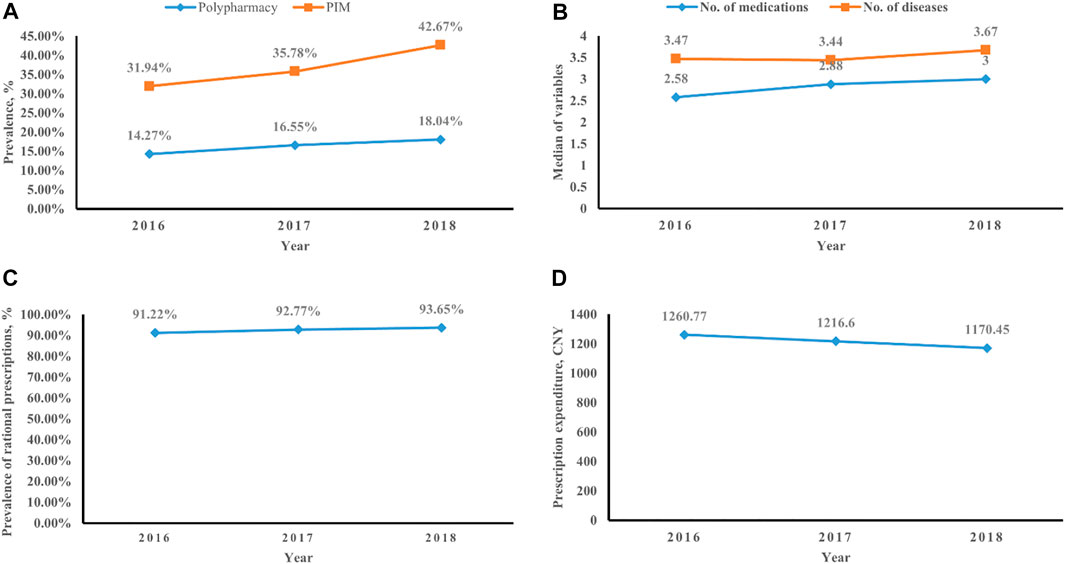
FIGURE 1. Trends in older lung cancer outpatients with multimorbidity. (A) Prevalence of polypharmacy and PIM use. (B) Number of medications and diseases. (C) Rate of rational prescriptions. (D) Prescription expenditure.
Among the 1,002 older lung cancer outpatients with prescriptions in 2016, 320 (31.94%) outpatients were identified to have at least one PIM, and a total of 428 PIMs were detected according to the 2019 Beers criteria. Of the patients with PIM prescriptions, 80.00% received one PIM, 15.31% received two PIMs, and 4.69% received at least three PIMs according to the criteria (Table 2). Overall, estazolam, tramadol, and megestrol were the most used PIMs according to the 2019 Beers criteria, at 18.60%, 13.44, and 12.92%, respectively (Table 3).
Among the 1,009 older lung cancer outpatients with prescriptions in 2017, 361 (35.78%) outpatients were identified to have at least one PIM, and a total of 480 PIMs were detected by the 2019 Beers criteria. Of the patients with PIM prescriptions, 82.27% received one PIM, 11.36% received two PIMs, and 6.37% received at least three PIMs according to the criteria (Table 2). Overall, estazolam, tramadol, and megestrol were the most used PIMs according to the 2019 Beers criteria, at 21.25%, 15.70, and 10.62%, respectively (Table 3).
Among the 1,275 older lung cancer outpatients with prescriptions in 2018, 544 (42.67%) outpatients were identified to have at least one PIM, and a total of 723 PIMs were detected according to the 2019 Beers criteria. Of the patients with PIM prescriptions, 80.70% received one PIM, 12.13% received two PIMs, and 7.17% received at least three PIMs according to the criteria (Table 2). Overall, estazolam, tramadol, and ibuprofen were the most used PIMs according to the 2019 Beers criteria, at 22.44%, 17.47, and 9.34%, respectively (Table 3).
PIM use, based on the 2019 Beers criteria, was the dependent variable in the logistic regression analysis (non-PIM use = 0, PIM use = 1). The logistic regression analysis indicated that age 75–79 (OR: 1.276 in Model 1, OR: 1.273 in Model 2), polypharmacy (OR: 2.587 in Model 1, OR: 2.672 in Model 2, OR: 2.678 in Model 3), and the irrational use of drugs (OR: 2.146 in Model 1, OR: 2.082 in Model 2, OR: 2.078 in Model 3) were positively associated with PIM use in older lung cancer outpatients. Older lung cancer patients with sleep disorders (OR: 11.408 in Model 1, OR: 11.433 in Model 2, OR: 11.158 in Model 3), anxiety or depression (OR: 5.079 in Model 1, OR: 5.135 in Model 2, OR: 4.834 in Model 3), and pain (OR: 7.021 in Model 1, OR: 7.047 in Model 2, OR: 6.884 in Model 3) were more likely to have PIM prescriptions (Table 4).
To the best of our knowledge, this is the first study to assess the trends of polypharmacy and PIM use in older Chinese lung cancer outpatients with multimorbidity. Previous studies based on national representative surveys have shown an alarming increase in the polypharmacy trends in the United States (from 8.2% in 1999 to 15% in 2012; Kantor et al., 2015), Sweden (from 16.9% in 2006 to 19.0% in 2014; Zhang et al., 2020), and France (from 44.9% in 2011 to 47.8% in 2019; Drusch et al., 2021), which are consistent with regional register-based studies on this period in the United Kingdom (a polypharmacy increase from 11.2% in 1995 to 22.8% in 2010; Guthrie et al., 2015) and those using the University Groningen IADB.nl prescription database in the Netherlands (showing an increase from 56.5% in 2012 to 58.2% in 2016; Oktora et al., 2021). Subjective measures, such as sleep diaries and anxiety and depression screening scales, also assist the diagnosis. As the diagnosis is determined, the use of drugs may be further increased (Hita-Yañez et al., 2013). In our study, the number of medications and diseases showed an increasing trend from 2016 to 2018. Therefore, the prevalence of polypharmacy increased in our study. Some studies in Europe and the United States have reported a decrease in the prevalence of PIMs (Ble et al., 2012; Hovstadius et al., 2014; Davidoff et al., 2015; Muhlack et al., 2018). With the popularization of Beers criteria, clinicians pay more attention to PIMs use in older patients; however, due to the increase of chronic diseases, the number of medications increased. This may be the reason that studies in the US indicate increased polypharmacy yet decrease in prevalence of PIMs use. However, one study in Ireland showed that the prevalence of PIM use rose from 32.6% in 1997 to 37.3% in 2012 (Moriarty et al., 2015). Our previous study showed an increasing trend of PIM use in older inpatients, from 71.17% in 2016 to 73.39% in 2018 (Tian et al., 2021). These results were similar to those of our present study, in which an increased prevalence of PIM use was observed in an older lung cancer patient population. Because polypharmacy is associated with an increased risk of inappropriate prescriptions, the prevalence of polypharmacy and PIM use in our studies were related, showing an increasing trend.
Our study was the first repeated cross-sectional study on the prevalence and risk factors for PIM use in older Chinese lung cancer outpatients. A United States study reported that the monthly prevalence of any PIM prior to cancer diagnosis was similar across all three cancer cohorts (breast cancer, colon cancer, and lung cancer), hovering between 37 and 40%, whereas PIM prevalence sharply increased in the first few months following the lung cancer (stage I–II) diagnosis. This may be when the lung cancer is diagnosed, the anti-emetics, antispasmodic drugs, and hydrochlorothiazide were usually used (Lund et al., 2018). The prevalence of PIM use in older lung cancer patients was higher than that in patients with the other two cancers according to the 2012 Beers criteria. The prevalence of PIM use, according to the 2019 Beers criteria, in our study was 37.28% over 3 years, which was higher than that reported in another study on the prevalence of PIM use among older Chinese cancer outpatients which were outside of palliative care and hospice service (32.65%; Tian et al., 2022a). Our previous study found that lung cancer was positively associated with PIM use in older cancer outpatients, which explains the higher prevalence of PIM use in this study. It is of great significance to study the high-risk population of PIMs use and provide targeted drug intervention for the follow-up. The prevalence of PIM use in our study was slightly higher than that the older advanced NSCLC patients who underwent epidermal growth factor receptor tyrosine kinase inhibitor in Japan, with a prevalence of 31.9% (Hakozaki et al., 2021), and lower than that in older NSCLC and SCLC patients at the end of life in the Netherlands, at 45% (Ham et al., 2021). The high prevalence of PIM use in these end-of-life patients is explained by the fact that these patients are usually in serious condition, both physically and mentally, and are thus highly willing to take more medications. Another potential reason for this difference is that the adverse outcomes in older lung cancer patients at the end of life are highly associated with PIM use; the poor clinical outcome of these patients further aggravates the prevalence of PIM use (Mohamed et al., 2020; Chen et al., 2021).
In our present study, the two most frequent PIMs in older Chinese lung cancer outpatients according to the 2019 Beers criteria were estazolam and tramadol over the 3 years. Sleep disorders can be both complex and common in older age, although reported prevalence varies (Hishikawa et al., 2017; Patel et al., 2018). Although research on the causal effect of sleep disorders on lung cancer incidence is still lacking, many lung cancer patients were also diagnosed with sleep disorders or pain in our study. Use of estazolam, a benzodiazepine, increases the risk of falls in older adults and co-prescribing of opioids exponentiates this risk (Niznik et al., 2022). Meanwhile, long-term use of benzodiazepines will increase the risk of respiratory depression and overdose with administration of benzodiazepine in older patients with sleep disorders. Pain is the most common symptom that occurs in 40% of lung cancer patients (Iwase et al., 2015), which can arise as a result of local effects (i.e., hemorrhaging into the tumor, obstruction/perforation of the lungs) or anti-cancer treatments, such as chemotherapy (Tang et al., 2021). The treatment of cancer pain mostly utilizes the three-step “ladder” treatment principle proposed by the World Health Organization; tramadol is commonly used for mild and moderate pain (Tian et al., 2022b). Although the analgesic effect of tramadol is good, its side effects induce syndrome of inappropriate antidiuretic hormone secretion (SIADH) or hyponatremia, and these risks are higher in older adults, which limits the clinical application of this medication (Li et al., 2021). Older patients with lung cancer need help with sleeping especially if in pain, especially in elderly patients with lower pain threshold levels. Therefore, sedative hypnotic drugs are taken more frequently than elderly patients without lung cancer. In order to ensure the risk-benefit balance of drug use in this population, it is of great significance to develop models that meet the PK/PD characteristics of this population to evaluate the appropriate medication use rather than keeping to a specific number of medicines in this fragile population. According to the logistic regression analysis, risk factors for PIM use were the same among the three models: 75–79 years of age, polypharmacy, irrational use of drugs and lung cancer accompanied by sleep disorders, anxiety or depression, or pain. However, some pulmonary diseases, such as pulmonary infection and COPD, were not risk factors for PIM use. Therefore, we suggest reducing the prescription of unnecessary medications and that doctors or pharmacists carefully perform medication reconciliation for older lung cancer outpatients taking multiple medications.
Several limitations of this study should be noted. First, this study only investigated 3 years of data in China, and more years of data are needed to determine long-term trends of polypharmacy and PIM use in older lung cancer outpatients with multimorbidity. Second, outpatients attending tertiary hospitals were the main focus of the study; thus, lung cancer outpatients who were in nursing homes and communities were not evaluated. In addition, the research aimed at only one area population may have limited popularization.
This study investigated the trends of polypharmacy and PIM use in older lung cancer outpatients with multimorbidity in China based on the 2019 Beers criteria. The prevalence of polypharmacy and PIM use showed an increasing trend in older Chinese lung cancer outpatients, and age 75–79, polypharmacy, irrational use of drugs, and lung cancer accompanied by sleep disorders, anxiety or depression, or pain were risk factors for PIM use.
The original contributions presented in the study are included in the article/Supplementary Materials; further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by this study protocol, which was approved by the Sichuan University West China Hospital Research Ethics Board. Written informed consent from participation was not required for this study in accordance with the national legislation and the institutional requirements.
Conception and design: FT. Administrative support: FT. Provision of study materials or patients: FT, MZ. Collection and assembly of data: FT, XC. Data analysis and interpretation: FT and ZC. Manuscript writing: all authors. Final approval of manuscript: all authors.
This work was supported by the Sichuan Science and Technology Program (Project number 2022JDR0326).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.935764/full#supplementary-material
Ble, A., Masoli, J. A., Barry, H. E., Winder, R. E., Tavakoly, B., Henley, W. E., et al. (2012). Any versus Long-Term Prescribing of High Risk Medications in Older People Using 2012 Beers Criteria: Results from Three Cross-Sectional Samples of Primary Care Records for 2003/4, 2007/8 and 2011/12. BMC Geriatr. 15, 146. doi:10.1186/s12877-015-0143-8
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel (2019). American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 67, 674–694. doi:10.1111/jgs.15767
Chen, L. J., Trares, K., Laetsch, D. C., Nguyen, T. N. M., Brenner, H., and Schöttker, B. (2021). Systematic Review and Meta-Analysis on the Associations of Polypharmacy and Potentially Inappropriate Medication with Adverse Outcomes in Older Cancer Patients. J. Gerontol. A Biol. Sci. Med. Sci. 76 (6), 1044–1052. doi:10.1093/gerona/glaa128
Davidoff, A. J., Miller, G. E., Sarpong, E. M., Yang, E., Brandt, N., and Fick, D. M. (2015). Prevalence of Potentially Inappropriate Medication Use in Older Adults Using the 2012 Beers Criteria. J. Am. Geriatr. Soc. 63, 486–500. doi:10.1111/jgs.13320
Decoster, L., and Schallier, D. (2019). Treatment of Older Patients with Advanced Non-small Cell Lung Cancer: A Challenge. J. Geriatr. Oncol. 10 (4), 528–533. doi:10.1016/j.jgo.2018.09.008
Ding, R., Zhu, D., He, P., Ma, Y., Chen, Z., and Shi, X. (2020). Comorbidity in Lung Cancer Patients and its Association with Medical Service Cost and Treatment Choice in China. BMC Cancer 20 (1), 250. doi:10.1186/s12885-020-06759-8
Drusch, S., Le Tri, T., Ankri, J., Zureik, M., and Herr, M. (2021). Decreasing Trends in Potentially Inappropriate Medications in Older People: a Nationwide Repeated Cross-Sectional Study. BMC Geriatr. 21 (1), 621. doi:10.1186/s12877-021-02568-1
Global Cancer Observatory: Cancer Today (2020). International Agency for Research on Cancer. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf (Accessed March 23, 2022).
Grose, D., Morrison, D. S., Devereux, G., Jones, R., Sharma, D., Selby, C., et al. (2014). Comorbidities in Lung Cancer: Prevalence, Severity and Links with Socioeconomic Status and Treatment. Postgrad. Med. J. 90 (1064), 305–310. doi:10.1136/postgradmedj-2013-132186
Guthrie, B., Makubate, B., Hernandez-Santiago, V., and Dreischulte, T. (2015). The Rising Tide of Polypharmacy and Drug-Drug Interactions: Population Database Analysis 1995-2010. BMC Med. 13, 74. doi:10.1186/s12916-015-0322-7
Hakozaki, T., Matsuo, T., Shimizu, A., Ishihara, Y., and Hosomi, Y. (2021). Polypharmacy Among Older Advanced Lung Cancer Patients Taking EGFR Tyrosine Kinase Inhibitors. J. Geriatr. Oncol. 12 (1), 64–71. doi:10.1016/j.jgo.2020.09.011
Ham, L., Geijteman, E. C. T., Aarts, M. J., Kuiper, J. G., Kunst, P. W. A., Raijmakers, N. J. H., et al. (2022). Use of Potentially Inappropriate Medication in Older Patients with Lung Cancer at the End of Life. J. Geriatr. Oncol. 13 (1), 53–59. doi:10.1016/j.jgo.2021.07.009
Hishikawa, N., Fukui, Y., Sato, K., Ohta, Y., Yamashita, T., and Abe, K. (2017). Cognitive and Affective Functions Associated with Insomnia: a Population-Based Study. Neurol. Res. 39 (4), 331–336. doi:10.1080/01616412.2017.1281200
Hita-Yañez, E., Atienza, M., and Cantero, J. L. (2013). Polysomnographic and Subjective Sleep Markers of Mild Cognitive Impairment. Sleep 36 (9), 1327–1334. doi:10.5665/sleep.2956
Hovstadius, B., Petersson, G., Hellström, L., and Ericson, L. (2014). Trends in Inappropriate Drug Therapy Prescription in the Elderly in Sweden from 2006 to 2013: Assessment Using National Indicators. Drugs Aging 31, 379–386. doi:10.1007/s40266-014-0165-5
Hyttinen, V., Jyrkkä, J., and Valtonen, H. (2016). A Systematic Review of the Impact of Potentially Inappropriate Medication on Health Care Utilization and Costs Among Older Adults. Med. Care 54 (10), 950–964. doi:10.1097/MLR.0000000000000587
Iwase, S., Kawaguchi, T., Tokoro, A., Yamada, K., Kanai, Y., Matsuda, Y., et al. (2015). Assessment of Cancer-Related Fatigue, Pain, and Quality of Life in Cancer Patients at Palliative Care Team Referral: a Multicenter Observational Study (JORTC PAL-09). PLoS One 10, e0134022. doi:10.1371/journal.pone.0134022
Kantor, E. D., Rehm, C. D., Haas, J. S., Chan, A. T., and Giovannucci, E. L. (2015). Trends in Prescription Drug Use Among Adults in the United States from 1999-2012. JAMA 314, 1818–1831. doi:10.1001/jama.2015.13766
Koczwara, B., Deckx, L., Ullah, S., and van den Akker, M. (2022). Impact of Comorbidities on Physical Function and Survival of Middle-Aged, as Compared to Older, Individuals with Cancer. Support Care Cancer 30 (2), 1625–1632. doi:10.1007/s00520-021-06567-1
LeBlanc, T. W., McNeil, M. J., Kamal, A. H., Currow, D. C., and Abernethy, A. P. (2015). Polypharmacy in Patients with Advanced Cancer and the Role of Medication Discontinuation. Lancet Oncol. 16 (7), e333–41. doi:10.1016/S1470-2045(15)00080-7
Li, D. H., Su, Y. F., Fan, H. F., Guo, N., and Sun, C. X. (2021). Acupuncture Combined with Three-step Analgesic Drug Therapy for Treatment of Cancer Pain: A Systematic Review and Meta-Analysis of Randomised Clinical Trials. Evid. Based Complement. Altern. Med. 2021, 5558590. doi:10.1155/2021/5558590
Lund, J. L., Sanoff, H. K., Peacock Hinton, S., Muss, H. B., Pate, V., and Stürmer, T. (2018). Potential Medication-Related Problems in Older Breast, Colon, and Lung Cancer Patients in the United States. Cancer Epidemiol. Biomarkers Prev. 27 (1), 41–49. doi:10.1158/1055-9965.EPI-17-0523
Maddison, A. R., Fisher, J., and Johnston, G. (2011). Preventive Medication Use Among Persons with Limited Life Expectancy. Prog. Palliat. Care 19, 15–21. doi:10.1179/174329111X576698
Maleki, S., Glewis, S., Fua, T., Liu, C., Rischin, D., Alexander, M., et al. (2022). A Randomised Controlled Trial of Clinical Pharmacy Intervention versus Standard Care to Improve Medication Adherence in Outpatients with Head and Neck Cancer Receiving Radiotherapy. Support Care Cancer 30 (5), 4243–4253. doi:10.1007/s00520-021-06779-5
Mohamed, M. R., Ramsdale, E., Loh, K. P., Arastu, A., Xu, H., Obrecht, S., et al. (2020). Associations of Polypharmacy and Inappropriate Medications with Adverse Outcomes in Older Adults with Cancer: A Systematic Review and Meta-Analysis. Oncologist 25 (1), e94–e108. doi:10.1634/theoncologist.2019-0406
Moriarty, F., Hardy, C., Bennett, K., Smith, S. M., and Fahey, T. (20152015). Trends and Interaction of Polypharmacy and Potentially Inappropriate Prescribing in Primary Care over 15 Years in Ireland: a Repeated Cross-Sectional Study. BMJ Open 5, e008656. doi:10.1136/bmjopen-2015-008656
Muhlack, D. C., Hoppe, L. K., Stock, C., Haefeli, W. E., Brenner, H., and Schöttker, B. (2018). The Associations of Geriatric Syndromes and Other Patient Characteristics with the Current and Future Use of Potentially Inappropriate Medications in a Large Cohort Study. Eur. J. Clin. Pharmacol. 74, 1633–1644. doi:10.1007/s00228-018-2534-1
Muhlack, D. C., Hoppe, L. K., Weberpals, J., Brenner, H., and Schöttker, B. (2017). The Association of Potentially Inappropriate Medication at Older Age with Cardiovascular Events and Overall Mortality: A Systematic Review and Meta-Analysis of Cohort Studies. J. Am. Med. Dir. Assoc. 18 (3), 211–220. doi:10.1016/j.jamda.2016.11.025
Nilsson, J., Berglund, A., Bergström, S., Bergqvist, M., and Lambe, M. (2017). The Role of Comorbidity in the Management and Prognosis in Nonsmall Cell Lung Cancer: a Population-Based Study. Acta Oncol. 56 (7), 949–956. doi:10.1080/0284186X.2017.1324213
Niznik, J. D., Collins, B. J., Armistead, L. T., Larson, C. K., Kelley, C. J., Hughes, T. D., et al. (2022). Pharmacist Interventions to Deprescribe Opioids and Benzodiazepines in Older Adults: A Rapid Review. Res. Soc. Adm. Pharm. 18 (6), 2913–2921. doi:10.1016/j.sapharm.2021.07.012
Oktora, M. P., Alfian, S. D., Bos, H. J., Schuiling-Veninga, C. C. M., Taxis, K., Hak, E., et al. (2021). Trends in Polypharmacy and Potentially Inappropriate Medication (PIM) in Older and Middle-Aged People Treated for Diabetes. Br. J. Clin. Pharmacol. 87 (7), 2807–2817. doi:10.1111/bcp.14685
Patel, D., Steinberg, J., and Patel, P. (2018). Insomnia in the Elderly: a Review. J. Clin. Sleep. Med. 14 (6), 1017–1024. doi:10.5664/jcsm.7172
Tang, H., Chen, L., Wang, Y., Zhang, Y., Yang, N., and Yang, N. (2021). The Efficacy of Music Therapy to Relieve Pain, Anxiety, and Promote Sleep Quality, in Patients with Small Cell Lung Cancer Receiving Platinum-Based Chemotherapy. Support Care Cancer 29 (12), 7299–7306. doi:10.1007/s00520-021-06152-6
Tian, F., Liao, S., Chen, Z., and Xu, T. (2021). The Prevalence and Risk Factors of Potentially Inappropriate Medication Use in Older Chinese Inpatients with Multimorbidity and Polypharmacy: a Cross-Sectional Study. Ann. Transl. Med. 9 (18), 1483. doi:10.21037/atm-21-4238
Tian, F., Yang, R., Chen, Z., Duan, X., and Yuan, P. (2022b). The Prevalence and Factors Associated with Potentially Inappropriate Medication Use in Chinese Older Outpatients with Cancer with Multimorbidity. J. Geriatr. Oncol. 2022 (22), S187900021–S187940682. doi:10.1016/j.jgo.2022.02.006
Tian, F., Zhao, M., Chen, Z., and Yang, R. (2022a). Prescription of Potentially Inappropriate Medication Use in Older Cancer Outpatients with Multimorbidity: Concordance Among the Chinese, AGS/Beers, and STOPP Criteria. Front. Pharmacol. 13, 857811. doi:10.3389/fphar.2022.857811
Torre, L. A., Siegel, R. L., and Jemal, A. (2016). Lung Cancer Statistics. Adv. Exp. Med. Biol. 893, 1–19. doi:10.1007/978-3-319-24223-1_1
Wallace, E., McDowell, R., Bennett, K., Fahey, T., and Smith, S. M. (2017). Impact of Potentially Inappropriate Prescribing on Adverse Drug Events, Health Related Quality of Life and Emergency Hospital Attendance in Older People Attending General Practice: A Prospective Cohort Study. J. Gerontol. A Biol. Sci. Med. Sci. 72 (2), 271–277. doi:10.1093/gerona/glw140
Weng, M. C., Tsai, C. F., Sheu, K. L., Lee, Y. T., Lee, H. C., Tzeng, S. L., et al. (2013). The Impact of Number of Drugs Prescribed on the Risk of Potentially Inappropriate Medication Among Outpatient Older Adults with Chronic Diseases. QJM 106, 1009–1015. doi:10.1093/qjmed/hct141
WHO (2022). Cancer. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer (Accessed March 23, 2022).
Wildiers, H., Heeren, P., Puts, M., Topinkova, E., Janssen-Heijnen, M. L., Extermann, M., et al. (2014). International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients with Cancer. J. Clin. Oncol. 32, 2595–2603. doi:10.1200/JCO.2013.54.8347
Keywords: polypharmacy, potentially inappropriate medication, lung cancer, older, outpatient
Citation: Tian F, Chen Z, Chen X and Zhao M (2022) Increasing Trends of Polypharmacy and Potentially Inappropriate Medication Use in Older Lung Cancer Patients in China: A Repeated Cross-Sectional Study. Front. Pharmacol. 13:935764. doi: 10.3389/fphar.2022.935764
Received: 04 May 2022; Accepted: 21 June 2022;
Published: 18 July 2022.
Edited by:
Brian Godman, University of Strathclyde, United KingdomReviewed by:
Taiki Hakozaki, Tokyo Metropolitan Komagome Hospital, JapanCopyright © 2022 Tian, Chen, Chen and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fangyuan Tian, dGlhbmZhbmd5dWFuMDYwOEAxNjMuY29t
†Orcid: Fangyuan Tian orcid.org/0000-0002-5187-0386
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.