- 1National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
- 2Institute of Traditional Chinese Medicine, Tianjin University of Traditional Chinese Medicine, Tianjin, China
Coronary microvascular disease (CMVD) is common in patients with cardiovascular risk factors and is associated with an increased risk of adverse cardiovascular events. Although the study of CMVD in modern medicine is ongoing, there is still no effective treatment for it. Traditional Chinese medicine (TCM) has some clinical advantages based on syndrome differentiation and individualized treatment. In this review, we review the clinical significance, pathogenesis, and current treatments of CMVD and systematically summarize the clinical efficacy and potential action mechanisms of TCM for CMVD. In addition, the scientific problems that need to be solved urgently and the research strategy of TCM for CMVD are described. CMVD has great clinical significance, but there are still many gaps in the related research. This review aims to attract the attention of clinicians to CMVD and promote research on CMVD in TCM.
1 Introduction
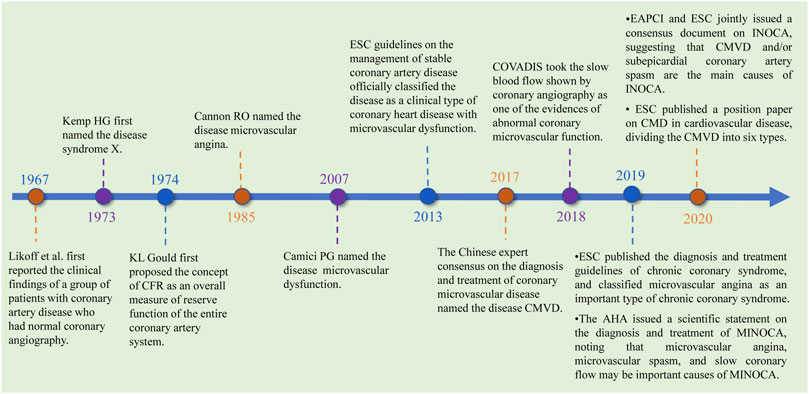
Coronary microvascular disease (CMVD) is a clinical syndrome that exhibits objective evidence of exertional angina pectoris or myocardial ischemia caused by structural and/or functional abnormalities of the coronary artery microvasculature under the action of many pathogenic factors (Zhang et al., 2017). The disease tends to occur in women (Crea et al., 2014; Murthy et al., 2014; Sara et al., 2015; Mileva et al., 2022) and is also prevalent in certain populations, such as those with obesity, hypertension, insulin resistance, diabetes, metabolic syndrome, smoking, myocardial injury, cardiomyopathy, ejection fraction-preserved heart failure, and obstructive and nonobstructive coronary heart disease (Crea et al., 2014; Labazi and Trask, 2017; Taqueti and Di Carli, 2018). In addition, the incidences of major adverse cardiovascular events (MACEs) and all-cause mortality associated with the disease are high (Murthy et al., 2014). In 1973, Kemp HG first referred to CMVD as syndrome X (Kemp et al., 1973). In 1985, Cannon RO referred to the disease as microvascular angina (Cannon et al., 1985). In 2007, Camici PG referred to the disease as microvascular dysfunction. In 2013, the European Society of Cardiology (ESC) issued guidelines that formally named the disease coronary microvascular dysfunction and defined it as one of the types of stable coronary heart disease (Task Force et al., 2013). In 2017, the Chinese Expert Consensus on Diagnosis and Treatment of Coronary Microvascular Disease called the disease “coronary microvascular disease” (Zhang et al., 2017), and CMVD was divided into three types: 1) coronary artery disease without obstruction; 2) coronary artery disease with obstruction; and 3) other types of CMVD, including hypertrophic cardiomyopathy, dilated cardiomyopathy, myocarditis, aortic stenosis, and myocardial amyloidosis. In 2020, the ESC Working Group on Coronary Pathophysiology and Microcirculation published a paper on “coronary microvascular dysfunction in cardiovascular disease,” in which CMVD was divided into 1) CMVD in nonobstructive chronic coronary syndromes, 2) CMVD in obstructive chronic coronary syndromes, 3) CMVD in nonobstructive acute coronary syndromes (ACS), 4) CMVD in obstructive ACS, and 5) CMVD and coronary no-reflow CMVD in reperfused acute myocardial infarction (AMI). The last of these has recently been recognized as the major cause of angina or heart failure following successful reperfusion therapy in AMIs (Padro et al., 2020). In recent years, the study of CMVD has been expanded, and its development and progress are shown in Figure 1.
ESC, European Society of Cardiology; COVADIS, Coronary Vasomotion Disorders International Study Group; MINOCA, Myocardial Infarction with No-Obstructive Coronary Arteries; EAPCI, European Association of Percutaneous Cardiovascular Interventions; INOCA, Ischemia and No Obstructive Coronary Artery Disease.
Coronary artery disease is the leading cause of death worldwide (Khan et al., 2020). Recently, the development of thrombolysis and percutaneous coronary interventions (PCI) has solved the problem of coronary artery stenosis or occlusion to a great extent. It was found that even when adequate and timely reperfusion therapy restored epicardial coronary blood flow, CMVD still occurred in many patients (Niccoli et al., 2016). At present, the main therapeutic drugs used for CMVD are mainly anti-myocardial ischemia drugs, which include beta-blockers, short-acting nitrates, angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), calcium channel blockers (CCB), ivabradine, trimetazidine, and ranolazine (Task Force et al., 2013; Villano et al., 2013; Mumma and Flacke, 2015; Bairey Merz et al., 2016; Shah et al., 2017). Although these drugs have certain clinical efficacy, many patients still require repeated hospitalization and coronary angiography because of chest pain, which seriously affects patients’ quality of life (Zhuang et al., 2020). Therefore, more effective therapies for CMVD are still needed (Marinescu et al., 2015; Vink et al., 2021). Clinical studies have shown that TCM has good clinical efficacy in treating CMVD and can significantly improve the symptoms of angina pectoris, TCM syndrome, ECG ischemia, quality of life, exercise tolerance, and other related physical and chemical indicators (Zhong et al., 2020; Wang M. X. et al., 2021). In this study, the clinical significance, pathogenesis, and current treatments of CMVD, as well as the clinical efficacy and mechanism of TCM for CMVD, are systematically summarized and discussed to attract the attention of clinicians to CMVD and promote basic and clinical research on CMVD in TCM.
2 Clinical significance of CMVD
At present, there are no large-scale epidemiological data for CMVD, and its incidence and prognostic significance have not been clear. A study of predictive models of coronary artery disease in patients with chest pain showed that up to 70% of angina patients had no obstructive coronary stenosis, as observed by coronary angiography. In most of these patients, the coronary angiography results were normal or nearly normal (Reeh et al., 2019). Recent studies have shown that CMVD is an independent predictor of adverse cardiovascular events, and there are significant associations with the incidence of cardiovascular events such as ejection fraction (EF) reserved heart failure, myocardial ischemia, acute coronary syndrome, myocardial infarction, stroke, and cardiogenic death (Gulati et al., 2009; Lind et al., 2011; Jespersen et al., 2012; Crea et al., 2014; Maddox et al., 2014; Petersen et al., 2014; Brainin et al., 2018; Herscovici et al., 2018). In people with chest pain and normal coronary angiography results, the incidence of CMVD was as high as 45%–60%, and the incidence and mortality due to myocardial ischemia, angina, myocardial infarction, and other cardiovascular events were significantly increased (Crea et al., 2014). A 7.5-year follow-up study of 11,223 patients with stable angina showed that nearly one-third of the men and two-thirds of the women admitted to the hospital had no coronary artery disease, and both men and women had significantly higher rates of major cardiovascular events and all-cause mortality in patients with normal and nonobstructive coronary artery disease than in the controls. Researchers speculate that CMVD may be an important cause of poor prognoses in these patients (Jespersen et al., 2012).
Coronary flow reserve (CFR), first proposed by Gould in 1974, is an important physiological measure of coronary microcirculation and can be used to evaluate the reserve function of both subepicardial coronary arteries and microcirculation (Gould et al., 1974). In CMVD without obstructive coronary artery disease, a decrease in CFR is a marker of coronary microcirculatory disturbance (Gould, 2009). At present, there is no consensus on the optimal CFR cut-off value for diagnosing CMVD. CFR values <2.0 are generally recommended as the critical value for diagnosing coronary microvascular dysfunction (Murthy et al., 2014), whereas CFR values <2.5 indicate coronary microvascular disease (Driessen et al., 2017). Decreases in CFR were associated with adverse cardiovascular events (Murthy et al., 2012; Murthy et al., 2014). Decreased CFRs (<1.6) in women were found to predict higher incidences of adverse cardiovascular events (Taqueti et al., 2017). Taqueti et al. (2018) found that patients with nonocclusive coronary artery stenosis who had chest pain and normal left ventricular EFs appeared to be at low risk of heart failure, and a decrease in CFR could lead to an increase in the number of adverse cardiac events. The poor prognosis and pathogenesis of heart failure with preserved EF (HFpEF) are closely related to CMVD. Gdowski et al. published a meta-analysis of 6,631 patients with suspected myocardial ischemia but without coronary artery occlusion, which showed that compared to patients with normal CFRs, CFR decreased the mortality of patients by 3.93 times, whereas the incidence of adverse cardiovascular events increased by 5.16 times (Gdowski et al., 2020). Because CMVD is common in patients with cardiovascular risk factors, CFR measurements should be performed early to determine the presence of CMVD even in people without coronary artery disease to help with early diagnosis and intervention to prevent further progression of CMVD and adverse cardiac events (Del Buono et al., 2021; Tjoe et al., 2021; Lopez et al., 2022). CMVD has a complex etiology, involves a wide range of people, and lacks standardized and effective means of detection, which causes the systematic prevention and management of coronary heart disease to be difficult and seriously affects the prognosis of patients. Therefore, the early diagnosis and treatment of CMVD have important clinical significance (Taqueti et al., 2018; Bairey Merz et al., 2020).
3 Pathogenesis of CMVD
At present, the pathogenesis of CMVD is not completely clear and is mainly divided into structural and functional abnormalities of coronary microvessels.
3.1 Coronary microvascular structural abnormalities
Abnormal structures of the coronary artery microvasculature are closely related to increases in left ventricular mass (Huo and Kassab, 2012), which is common in hypertrophic cardiomyopathy and hypertension (Camici et al., 2020); it is often accompanied by intimal thickening, which results in a mild reduction in the lumen area of the arterioles (Taqueti et al., 2018; Camici et al., 2020). Arteriosclerosis can exacerbate this change and lead to microvascular occlusion, narrowing of intramural arterioles and capillary lumen, and capillary thinning (Labazi and Trask, 2017).
3.2 Coronary microvascular dysfunction
Coronary microvascular dysfunction (CMD) includes endothelial cell-dependent vascular abnormalities, which are commonly seen in people with diabetes, obesity, smoking, and other cardiovascular risk factors, and dependent vasodilation abnormalities, microvascular spasms, microvascular embolisms, and extravascular mechanisms (Zhang et al., 2017; Ford et al., 2018). These physiological and pathological changes in the development of CMD play roles to varying degrees.
During CMVD development, injury to coronary microvascular endothelial cells (CMECs) is the key link (Yin et al., 2021). Current studies suggest that angina in patients with CMVD is associated with myocardial ischemia, and a CMD-induced decrease in CFR is thought to be the main cause of CMVD (Sucato et al., 2017; Padro et al., 2020). CMEC accounts for approximately 1/3 of the total number of cardiac cells and plays an important role in maintaining the normal function of coronary microvessels (Li et al., 2001). CMEC dysfunction often precedes myocardial injury (Scarabelli et al., 2001). Related studies show that the normal proliferation, adhesion, migration, apoptosis, and secretion of CMECs are impaired by risk factors such as old age (Moreau et al., 1998), hypertension (Rizzoni et al., 2003), hyperlipidemia (Kaufmann et al., 2000b), smoking (Kaufmann et al., 2000a), obesity (Chen et al., 2017), insulin resistance (Dagres et al., 2004), and diabetes mellitus (Pitkanen et al., 1998), which leads to CMD, decreased CFRs, insufficiency of myocardial blood supply, and finally occurrence of CMVD (Baumgart et al., 1999; Camici and Crea, 2007).
Microvascular spasms are one of the important mechanisms of CMVD. In some patients with atypical angina but with normal coronary angiography results, abnormal activation of the myocardial α2 adrenergic receptor at rest due to sympathetic nervous system dysfunction leads to coronary microvascular contraction and reduced myocardial perfusion, which cause myocardial ischemia (Baumgart et al., 1999). Microvascular embolization is also an important mechanism of CMVD. Due to interventional therapy or plaque rupture, microthrombi, atheromatous plaque fragments, and thromboemboli block the blood flow in microvessels, which leads to distal microvascular occlusion and causes CMVD (Crea et al., 2014). The extravascular mechanism can be seen in diseases with significantly elevated left ventricular diastolic pressures, such as left ventricular hypertrophy and left ventricular fibrosis, and diseases that can directly decrease coronary diastolic pressures, such as aortic stenosis, severe coronary stenosis, anterior arteriole stenosis, and hypotension (Giacco and Brownlee, 2010). In addition, the formation and development of CMVD is a cumulative process in which metabolic disorders, oxidative stress, and inflammatory reactions play important roles (Labazi and Trask, 2017; Long et al., 2017; Zhang et al., 2017; Oikonomou et al., 2018; Du et al., 2019).
4 Modern drug therapy of CMVD
4.1 Classic anti-myocardial ischemia drugs
Beta-blockers and short-acting nitrates are first-line drugs used to control the symptoms of CMVD (Task Force et al., 2013). Patients who cannot tolerate beta-blockers can be treated with ivabradine instead (Mumma and Flacke, 2015). In the absence of adequate symptom control, the use of calcium antagonists and/or long-acting nitrates in addition to beta-blockers may contribute to improved control of patient symptoms (Task Force et al., 2013). RAAS inhibitors (including ACEIs and ARBs) can also improve coronary artery microvascular function by blocking vasoconstriction due to angiotensinogen II (Task Force et al., 2013). Coronary revascularization is a reasonable approach for CMVD patients with epicardial coronary artery occlusion and may improve the clinical symptoms and prognosis of CMVD patients (Task Force et al., 2013; Taqueti et al., 2015). For patients with cardiogenic chest pain who show signs of ischemia in perfusion tests, beta-blockers reduce myocardial oxygen consumption and improve symptoms. However, in patients with variant angina, beta-blockers should be avoided, and calcium channel blockers should be used as first-line drugs (Padro et al., 2020).
4.2 Non-classic anti-myocardial ischemia drugs
A variety of nonclassical antianginal agents have been used in CMVD patients, including nicorandil, ivabradine, trimetazidine, and ranolazine (Villano et al., 2013; Cattaneo et al., 2015; Bairey Merz et al., 2016; Shah et al., 2017). Nicorandil is one of the most studied drugs, and some studies have shown that nicorandil can effectively improve exercise-induced myocardial ischemia without altering cardiac autonomic nerve activity. It is suggested that nicorandil may have a direct vasodilative effect on coronary microvessels in patients with CMVD (Lanza et al., 2014). In addition, studies have shown that nicorandil can improve the symptoms of CMVD patients by inhibiting inflammatory factors and improving vascular endothelial function (He et al., 2017).
4.3 Other drugs
Statins are commonly used in the treatment of CMVD. In addition to lowering cholesterol levels, statins inhibit vascular inflammation, increase eNOS levels, and increase NO availability in blood vessels (Padro et al., 2020). Data analysis for eight thrombolytics in myocardial infarction (TIMI) trials found lower 30-day mortalities or reinfarction rates in patients with non-ST-segment elevation acute coronary syndromes (NSTE-ACS) and nonobstructive CAD who received statins (De Ferrari et al., 2014). In addition, long-term follow-up data from the Swedish Web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapy study confirmed that statins can decrease the number of major cardiovascular events (e.g., all-cause mortality, myocardial infarction, ischemic stroke, and heart failure) in patients with CMVD (Lindahl et al., 2017). Statins and ACE inhibitors are recommended for patients with cardiovascular risk factors associated with arteriosclerosis or endothelial dysfunction (Padro et al., 2020). Long-term l-arginine supplementation can improve vascular endothelial function, coronary flow, and symptoms in patients with CMVD (Lerman et al., 1998).
The treatment goals for CMVD include minimizing angina attacks and their associated symptoms, maximizing improvements in patients’ physical functions and quality of life, and extending their lifespans. The treatment options available to patients are very limited due to a lack of standardized diagnoses, nonstandard clinical designs, small sample sizes, and insufficient evidence for clinical improvement of CMVD. At present, most of the drug therapies used for CMVD are empirically based. Although they have certain clinical effects, many patients are still repeatedly hospitalized for chest pain and coronary angiography studies, which seriously affect the quality of life of patients (Zhuang et al., 2020). Modern medicine lacks a definitive treatment for CMVD (Taqueti and Di Carli, 2018).
A clinical study indicated that CMVD treatments by integrating traditional Chinese and Western medicine (WM) were superior to those using Western medicine alone (Ji and Ren, 2009; Li and Yu, 2010; Sun and Wu, 2012; Wu et al., 2013; Chen and Ma, 2014; Lv et al., 2014; Wang et al., 2014; Luo et al., 2017; Qin et al., 2017; Wei, 2018; Yan et al., 2018; Zhang, 2019; Qiu et al., 2021; Sun, 2021; Zhang, 2021; Cao et al., 2022; Chen et al., 2022). A systematic review and meta-analysis of randomized controlled trials (RCTs) involving 1,903 patients with CMVD revealed that integrated Chinese and Western medicine therapies were more effective than Western medicine treatments alone regarding the indicators of frequency of angina pectoris attacks, electrocardiography (ECG), nitroglycerin amounts needed, treadmill exercise tests, TCM syndrome scores, and levels of C-reactive protein (CRP), endothelin-1 (ET-1), and nitric oxide (NO) (Zhong et al., 2020). Another systematic review and meta-analysis of RCTs that included 1,075 CMVD patients showed consistent results that compared to Western medicine treatments alone, TCM with WM treatment could further increase CFRs, decrease the index of microvascular resistance (IMR), increase NO levels, and decrease levels of high-sensitivity C-reactive protein (hs-CRP) (Wang M. X. et al., 2021).
5 TCM in the treatment of CMVD
5.1 Understanding CMVD in TCM theory
There is no specific record of CMVD in ancient Chinese literature. In view of the typical symptoms of angina pectoris, in traditional Chinese medicine, most doctors classify it as “Xiong Bi” and “Xin Tong.” However, considering the microvascular anatomy of coronary arteries, some doctors think that CMVD should belong to the “Luo Bing” described in TCM (Chang et al., 2016). The etiology and pathogenesis of CMVD in TCM have not been universally recognized, but most doctors believe that CMVD is mainly caused by emotional discomfort, stagnation of liver-qi, and the interaction of phlegm and blood stasis in the chest (Bi et al., 2013).
5.2 Clinical evidence of TCM for CMVD
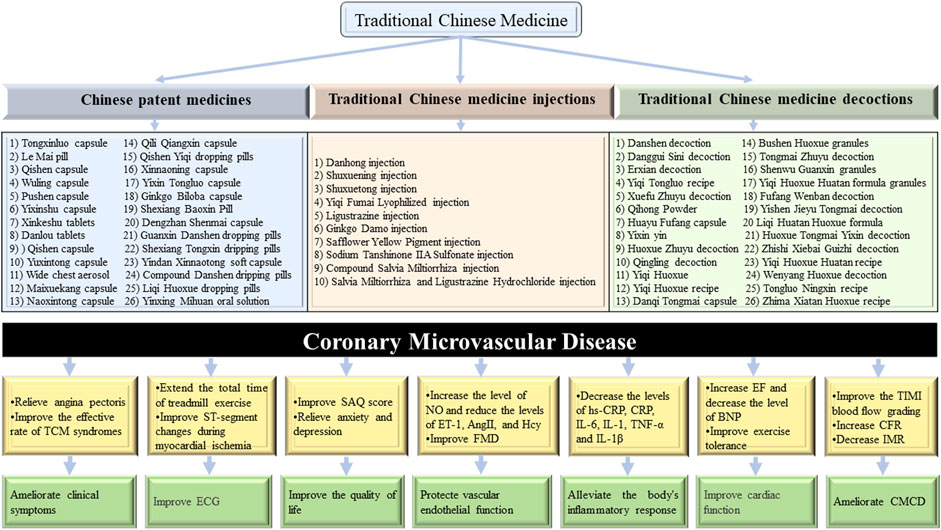
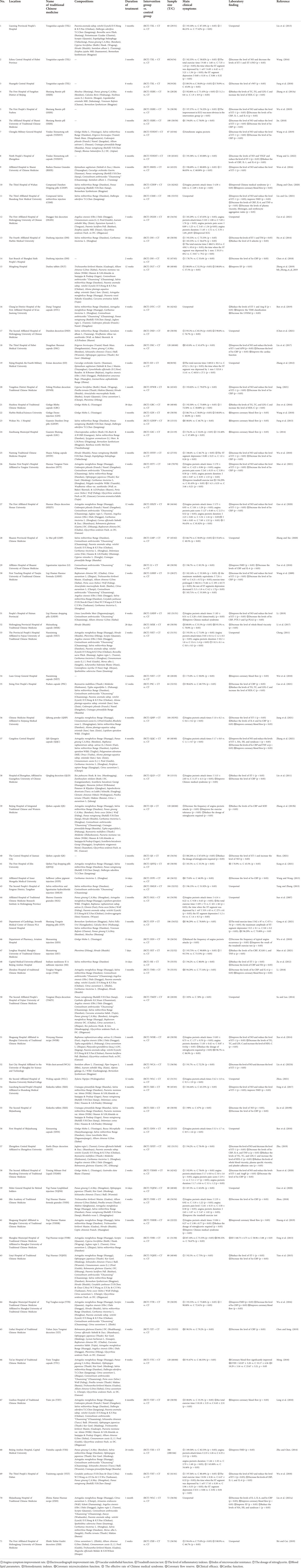
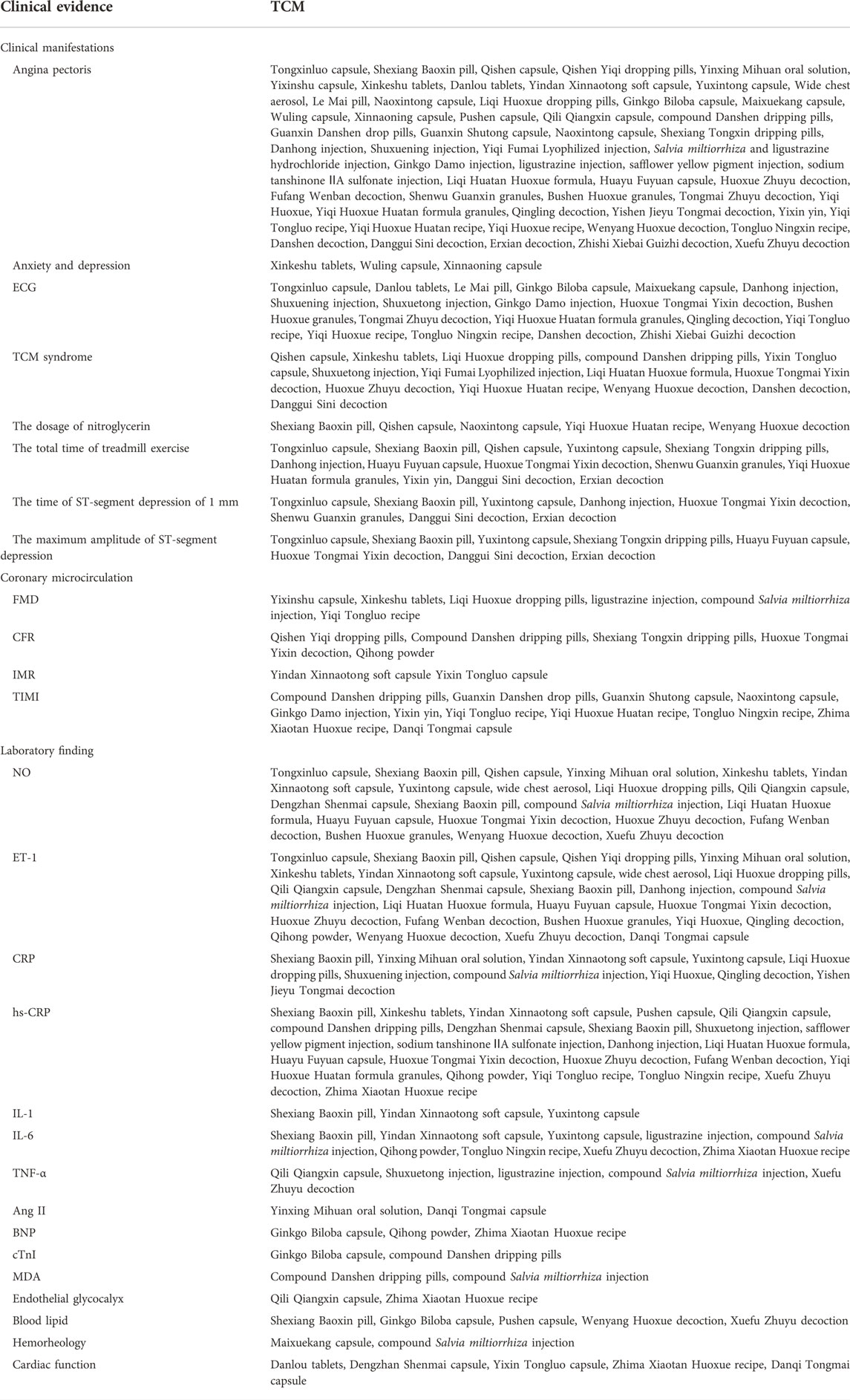
A total of 71 representative RCTs, including 34 Chinese patent medicines (CPMs), 11 TCM injections, and 26 TCM decoctions, were compiled and summarized. According to the available clinical data, there have been many clinical trials on the clinical advantages of TCM in the prevention and treatment of CMVD, as shown in Figure 2. The clinical evidence of TCM for CMVD, including the outcomes of 1) clinical manifestations, 2) coronary microcirculation, and 3) laboratory results, are analyzed and summarized in Table 1. Based on Table 1, the clinical evidence of TCM for the typical manifestations of CMVD is summarized in Table 2.
5.2.1 CPMs for CMVD treatment
Several clinical studies have shown that CPMs injections can play an important role in improving clinical symptoms, improving exercise tolerance, enhancing coronary microcirculation function, and regulating abnormal biomarkers and other aspects in CMVD patients.
1) Tongxinluo capsules (Liu et al., 2013; Wang, 2016; Fang et al., 2018), Shexiang Baoxin pills (Zhang W. N. et al., 2013; Wu et al., 2019), Qishen capsules (Zhang Y. L. et al., 2013; Shen, 2021), Qishen Yiqi dropping pills (Kang et al., 2021), Yinxing Mihuan oral solutions (Xuan et al., 2020), Yixinshu capsules (Zhu and Chen, 2014), Xinkeshu tablets (Feng et al., 2017; Jia W. M. et al., 2019), Danlou tablets (Zheng et al., 2019), Yindan Xinnaotong soft capsules (Wang et al., 2019; Wang and Li, 2022), Yuxintong capsules (Wu et al., 2018), Wide chest aerosols (Liu T. H. et al., 2021), Le Mai pills (Zhang and Xie, 2020), Naoxintong capsules (Cheng, 2011), Liqi Huoxue dropping pills (Li, 2019), Ginkgo Biloba capsules (Zou et al., 2016), Maixuekang capsules (Li et al., 2017), Wuling capsules (Zhou, 2021), Xinnaoning capsules (Ren et al., 2018), Pushen capsules (Cao et al., 2021), Qili Qiangxin capsules (Zhang et al., 2021), compound Danshen dripping pills (Zhang and Chen, 2020), Guanxin Danshen dropping pills (Fang et al., 2013), Guanxin Shutong capsules (Li, 2014), Dengzhan Shenmai capsules (Liu et al., 2017), Naoxintong capsules (Wei et al., 2010), and Shexiang Tongxin dropping pills (Gong et al., 2021) relieved angina symptoms and improved ECG results; Shexiang Baoxin pills (Zhang W. N. et al., 2013; Wu et al., 2019), Qishen capsules (Zhang Y. L. et al., 2013; Shen, 2021), and Naoxintong capsules (Cheng, 2011) decreased the nitroglycerin dosage needed; and Tongxinluo capsules (Fang et al., 2018), Shexiang Tongxin dropping pills (Gong et al., 2021), Qishen capsules (Zhang Y. L. et al., 2013), and Yuxintong capsules (Wu et al., 2018) improved exercise tolerance. 2) Shexiang Baoxin pills (Zhang, 2019), Qishen Yiqi dropping pills (Kang et al., 2021), compound Danshen dropping pills (Zhang and Chen, 2020), Guanxin Danshen dropping pills (Fang et al., 2013), Guanxin Shutong capsules (Li, 2014), and Shexiang Tongxin dropping pills (Gong et al., 2021) effectively improved CFRs; Yindan Xinnaotong soft capsules (Wang and Li, 2022) and Yixin Tongluo capsules (Meng, 2018) improved IMR values; and Guanxin Danshen dropping pills (Fang et al., 2013), Guanxin Shutong capsules (Li, 2014), compound Danshen dropping pills (Zhang and Chen, 2020), and Naoxintong capsules (Wei et al., 2010) improved TIMI blood flow grading. 3) Tongxinluo capsules (Wang, 2016), Shexiang Baoxin pills (Jin, 2018), Qishen capsules (Shen, 2021), Xinkeshu tablets (Feng et al., 2017; Jia W. M. et al., 2019), Yuxintong capsules (Wu et al., 2018), wide chest aerosols (Liu T. H. et al., 2021), Yindan Xinnaotong soft capsules (Wang and Li, 2022), Liqi Huoxue dropping pills (Li, 2019), and Qili Qiangxin capsules (Zhang et al., 2021) increased NO levels and decreased ET-1 levels; Yixinshu capsules (Zhu and Chen, 2014), Xinkeshu tablets (Feng et al., 2017), and Liqi Huoxue dropping pills (Li, 2019) effectively improved flow-mediated dilation (FMD); Yinxing Mihuan oral solutions (Xuan et al., 2020), Yindan Xinnaotong soft capsules (Wang et al., 2019; Wang and Li, 2022), and Yuxintong capsules (Wu et al., 2018) decreased the levels of hs-CRP, IL-6, IL-1, and tumor necrosis factor-α (TNF-α); Liqi Huoxue dropping pills (Li, 2019) decreased the levels of hs-CRP, Pentraxins 3 (PTX-3), and lipoprotein-associated phospholipase A2 (Lp-PLA2); Ginkgo Biloba capsules (Zou et al., 2016) decreased cardiac troponin I (cTnI) and BNP levels; Qili Qiangxin capsules (Zhang et al., 2021) decreased the levels of TNF-α, hs-CRP, hyaluronic acid, heparan sulphate, and syndecan 1; compound Danshen dropping pills (Zhang and Chen, 2020) decreased the levels of cTnI creatine kinase-MB (CK-MB) and malondialdehyde (MDA); and Shexiang Baoxin Pills (Zhang W. N. et al., 2013; Wu et al., 2019), Qishen capsules (Shen, 2021), Ginkgo Biloba capsules (Zou et al., 2016), and Pushen capsules (Cao et al., 2021) increased high-density lipoprotein cholesterol (HDL-C) levels and decreased the levels of triglyceride (TG), total cholesterol (TC), and low-density lipoprotein cholesterol (LDL-C).
5.2.2 TCM injections for CMVD treatment
Many clinical studies have shown that TCM injections can play an important role in improving clinical symptoms, enhancing coronary microcirculation function, and regulating abnormal biomarkers and other aspects in CMVD patients.
1) Danhong injection (Hu et al., 2014), Shuxuening injection (Wu et al., 2010), Shuxuetong injection (Mao et al., 2021), Yiqi Fumai Lyophilized injection (Guo et al., 2020), Salvia miltiorrhiza and ligustrazine hydrochloride injection (Yang and Zhang, 2013), Ginkgo Damo injection (Wang et al., 2010), ligustrazine injection (Yue et al., 2018), safflower yellow pigment (SYPI) injection (Wang and Wang, 2013), and sodium tanshinone ⅡA sulfonate injection (Zu et al., 2012) improved angina symptoms and/or ECGs. 2) Ginkgo Damo injection (Wang et al., 2010) improved TIMI blood flow grading. 3) Danhong injection (Hu et al., 2014) and compound Salvia miltiorrhiza injection (Liu and Gu, 2021) increased NO levels and decreased ET-1 levels; ligustrazine injection (Yue et al., 2018) and compound Salvia miltiorrhiza injection (Liu and Gu, 2021) improved FMD; Shuxuetong injection (Mao et al., 2021), ligustrazine injection (Yue et al., 2018), and compound Salvia miltiorrhiza injection (Liu and Gu, 2021) decreased the levels of hs-CRP, TNF-α, and IL-6; Danhong injection (Chen et al., 2018), Safflower Yellow Pigment injection (Wang and Wang, 2013), and sodium tanshinone IIA sulfonate injection (Zu et al., 2012) decreased hs-CRP levels; and Danhong injection (Hu et al., 2014; Chen et al., 2018) increased E-selectin levels and decreased thrombomodulin levels.
5.2.3 TCM decoctions for CMVD treatment
Many clinical studies have shown that TCM decoctions can play an important role in improving clinical symptoms, improving exercise tolerance and quality of life, enhancing coronary microcirculation function, and regulating abnormal biomarkers and other aspects in CMVD patients.
1) Liqi Huatan Huoxue formula (Wang et al., 2009), Huayu Fuyuan capsule (Peng and Yao, 2019), Huoxue Tongmai Yixin decoction (Li et al., 2020), Huoxue Zhuyu decoction (He et al., 2020), Fufang Wenban decoction (Jiang, 2021), Shenwu Guanxin granule (Sun et al., 2007), Bushen Huoxue granule (Wen et al., 2016), Tongmai Zhuyu decoction (Su and Luo, 2014), Yiqi Huoxue (Tian et al., 2015), Yiqi Huoxue Huatan formula granule (Zhou, 2018), Qingling decoction (Lin et al., 2011), Yishen Jieyu Tongmai decoction (Chen and Song, 2019), Qihong powder (Jiang et al., 2021), Yixin yin (Long et al., 2010), Yiqi Tongluo recipe (Wu et al., 2016), Yiqi Huoxue Huatan recipe (Huang et al., 2019), Yiqi Huoxue recipe (Feng et al., 2013), Wenyang Huoxue decoction (Xue et al., 2014), Tongluo Ningxin recipe (Li, 2018), Danshen decoction (Chen et al., 2021), Danggui Sini decoction (Cui et al., 2021), Erxian decoction (Zhang et al., 2012), Zhishi Xiebai Guizhi decoction (Shi and Cui, 2019), and Xuefu Zhuyu decoction (Zhu, 2019) improved angina symptoms and/or ECG results; Wenyang Huoxue decoction (Xue et al., 2014) reduced the nitroglycerin dosage needed; Huoxue Tongmai Yixin decoction (Li et al., 2020), Yixin yin (Long et al., 2010), Danggui Sini decoction (Cui et al., 2021), and Erxian decoction (Zhang et al., 2012) improved exercise tolerance; Qihong powder (Jiang et al., 2021), Yixin yin (Long et al., 2010), and Yiqi Tongluo recipe (Wu et al., 2016) improved quality of life. 2) Huoxue Tongmai Yixin decoction (Li et al., 2020) and Qihong powder (Jiang et al., 2021) improved CFRs; Zhima Xiaotan Huoxue recipe (Liu Q. et al., 2021), Yixin yin (Long et al., 2010), Yiqi Tongluo recipe (Wu et al., 2016), Yiqi Huoxue Huatan recipe (Huang et al., 2019), and Tongluo Ningxin recipe (Li, 2018) improved TIMI blood flow grading. 3) Liqi Huatan Huoxue formula (Wang et al., 2009), Huayu Fuyuan capsule (Peng and Yao, 2019), Huoxue Tongmai Yixin decoction (Li et al., 2020), Huoxue Zhuyu decoction (He et al., 2020), Fufang Wenban decoction (Jiang, 2021), Bushen Huoxue granule (Wen et al., 2016), Yiqi Huoxue (Tian et al., 2015), Qingling decoction (Lin et al., 2011), Qihong powder (Jiang et al., 2021), Yiqi Huoxue Huatan recipe (Huang et al., 2019), Wenyang Huoxue decoction (Xue et al., 2014), and Xuefu Zhuyu decoction (Zhu, 2019) increased NO levels and decreased ET-1 levels; Yiqi Tongluo recipe (Wu et al., 2016) improved FMD; Danqi Tongmai capsule (Ren et al., 2019) significantly decreased the levels of plasma ET-1, AngⅡ, and IL-6; Zhima Xiaotan Huoxue recipe (Liu Q. et al., 2021), Qihong powder (Jiang et al., 2021), Tongluo Ningxin recipe (Li, 2018), and Xuefu Zhuyu decoction (Jiang, 2021) significantly decreased the levels of IL-6 and hs-CRP; and Wenyang Huoxue decoction (Xue et al., 2014) and Xuefu Zhuyu decoction (Zhu, 2019) significantly decreased the TG, TC, and LDL-C levels and increased HDL-C levels.
In summary, clinical evidence indicates that TCM is beneficial for treating CMVD in 1) relieving the main clinical symptoms of angina pectoris, including decreasing the frequency of angina pectoris attacks, shortening the duration of angina pectoris, and alleviating the pain due to angina pectoris; improving the total effective rates of TCM syndromes; improving the quality of life of patients, including improving Seattle Angina Questionnaire scores and improving anxiety and depression; improving ECG results, including extending the total treadmill exercise times, enhancing the time of ST-segment depression of 1 mm, decreasing the maximum amplitude of ST-segment depression, and reducing the descending degree of the ST-T segment; and reducing the nitroglycerin dosage needed; 2) enhancing coronary microcirculation functions, including decreasing TIMI blood flow grading, increasing CFRs, and reducing IMRs; improving cardiac function, including decreasing cTnI and CK-MB levels and increasing EF levels; and 3) protecting vascular endothelial functions, including decreasing ET-1 levels, increasing NO levels, and improving FMDs; inhibiting inflammatory responses; decreasing the levels of hs-CRP, CRP, TNF-α, IL-1, IL-2, and IL-6; and improving blood lipids, which include decreasing the TG, TC, and LDL-C levels and increasing HDL-C levels.
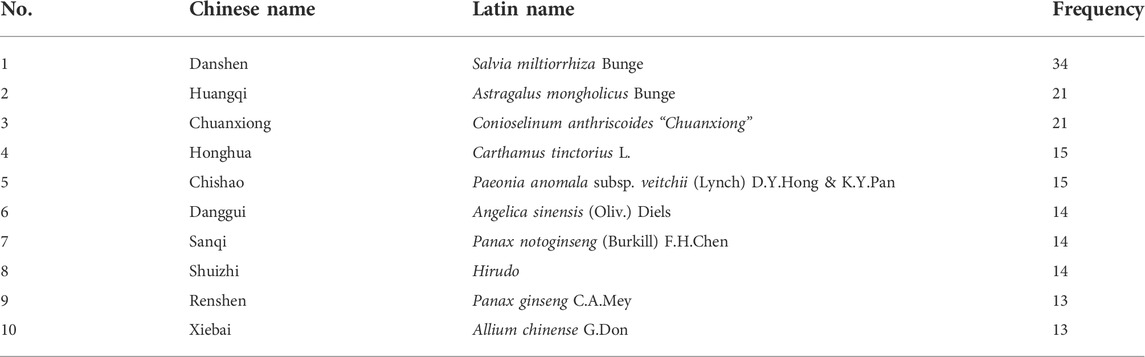
6 Frequency of commonly used chinese herbs from TCM compounds
According to the statistics provided in Table 1, the most frequently used herb among the 107 Chinese herbs studied was Danshen (Salvia miltiorrhiza Bunge). The top 10 Chinese herbs that are ranked by their relatively high usage frequencies are shown in Table 3. Table 3 shows that the top ten Chinese herbs are mainly blood-activating and stasis-removing drugs.
7 Potential action mechanisms of TCM for CMVD
7.1 Exploring the potential action mechanisms of TCM for CMVD based on clinical research
Coronary microcirculation disturbance (CMCD) is the main cause of myocardial ischemia in patients with CMVD (Padro et al., 2020). Vascular endothelial dysfunction is the main pathological mechanism of CMVD, and improving vascular endothelial dysfunction is one of the most important strategies in the treatment of CMVD (Ford et al., 2018; Kaski et al., 2018; Mangiacapra et al., 2020). CFRs, IMRs, and TIMI blood flow grading are commonly used methods to evaluate coronary microvascular function (Gibson et al., 2000; Gould, 2009; Cuculi et al., 2014). CFR is one of the sensitive indices that reflect changes in coronary hemodynamics, and it is also an index to evaluate the reserve functions of the coronary arteries and microcirculation. In CMVD without occlusive epicardial coronary artery disease, a decrease in CFR is a marker of CMCD (Gould, 2009). A decrease in CFR was associated with adverse cardiovascular events (Gibson et al., 2000; Cuculi et al., 2014). IMR can accurately reflect the pathological changes in microcirculation, and it is a specific method used for assessing CMCD (Murthy et al., 2014). IMR can specifically evaluate the microvascular functions of the distal ends of stenotic lesions and can accurately predict myocardial perfusion levels, ventricular remodeling, and cardiac function recovery after reperfusion therapy in AMI (Murthy et al., 2012; Choi et al., 2021). The normal value of IMR has not been universally determined, and IMRs >25 indicate the presence of CMD (Fearon et al., 2008). Clinical studies show that TCM can increase CFRs, decrease IMRs, and improve TIMI blood flow grading and correct TIMI frames in patients with CMVD, which suggests that the mechanism of TCM treatment of CMVD may be related to the improvement of CMCD.
The endothelium is key to maintaining intravascular homeostasis, and endothelial function impairment is the main etiological basis for the occurrence and development of arteriosclerosis. Therefore, determinations of vascular endothelial function are of great clinical significance in the prevention and treatment of cardiovascular diseases (Godo and Shimokawa, 2017). ET-1 and NO, a pair of antagonistic vasoactive substances synthesized by the endothelium, are commonly used markers of endothelial cell function. The dynamic equilibrium between them is important for maintaining vascular tension and stability of the cardiovascular system. The brachial artery FMD technique was first developed by Celermajer et al. (1992). It is a noninvasive, high-frequency ultrasound method used to evaluate vascular endothelial function. FMD can reflect the overall functional changes of the vascular endothelium, and early detection can reveal the early progression of arteriosclerosis. Clinical studies have shown that TCM can significantly increase NO and NO/ET levels, decrease ET-1 levels, and improve FMD and vascular endothelial function. It is suggested that the protection of vascular endothelial function may be one of the mechanisms of TCM treatment of CMVD.
Inflammatory reactions play an important role in the development of CMD. Inflammatory factors not only cause endothelial injury and intimal thickening but also decrease NO and prostacyclin synthesis in endothelial cells and activate immune cells to release human ET and ET-like immune complexes, ultimately leading to endothelial dysfunction (Marroquin et al., 2005; Arroyo-Espliguero and Kaski, 2006). Clinical studies have shown that the levels of IL-6, hs-CRP, WBC, and neutrophil-lymphocyte in the peripheral blood of patients with CMVD are significantly higher than those of healthy subjects, which suggests that endothelial dysfunction induced by inflammatory reactions may be one of the pathogenic mechanisms of CMVD (Demirkol et al., 2014; Jia J. Z. et al., 2019). TCM can significantly reduce the levels of CRP, hs-CRP, IL-1, IL-6, TNF-α, and other inflammatory factors, suggesting that the inhibition of inflammatory reactions and protection of vascular endothelial function may be one of the mechanisms of TCM treatments of CMVD.
7.2 Exploring the potential action mechanisms of TCM for CMVD based on basic experimental research
Table 3 shows that the top ten Chinese herbs used to treat CMVD consist mainly of blood-activating, stasis-removing, and qi-reinforcing drugs. Next, we discuss the potential mechanisms of Chinese herbs such as Danshen (Salvia miltiorrhiza Bunge), Honghua (Carthamus tinctorius L.), Huangqi (Astragalus mongholicus Bunge), and Danghui (Angelica sinensis (Oliv.) Diels) in the treatment of CMVD.
7.2.1 Danshen (salvia miltiorrhiza bunge)
Salvia miltiorrhiza Bunge is the most commonly used traditional Chinese medicine for the clinical treatment of CMVD. Modern pharmacological studies have shown that Salvia miltiorrhiza Bunge has anti-inflammatory, antioxidant, anti-atherosclerotic, anti-coagulant, and anti-thrombotic effects, which regulate blood lipids, increase coronary blood flow, improve microcirculation, and protect vascular endothelial function. Liu et al. (2008) reported that Salvia miltiorrhiza Bunge could inhibit platelet aggregation and activation, prevent microthrombosis, promote nitric oxide production, dilate blood vessels, increase blood flow, and improve blood hypercoagulability, thus playing an anticoagulant role. Tanshinone IIA, one of the most abundant components of tanshinone, can alleviate pathological injury of cardiac tissue, attenuate myocardial damage, reduce myocardial infarct sizes, and promote the recovery of cardiac function (Zhang et al., 2010). In addition, tanshinone IIA sodium sulfonate could increase coronary flow, improve myocardial hypoxia tolerance, improve myocardial metabolic disorders, and effectively inhibit platelet aggregation and antithrombosis in patients with coronary heart failure (Wang and Liu, 2013; Qu et al., 2016). Salvianolic acid is a water-soluble phenolic acid extracted from Salvia miltiorrhiza Bunge that significantly reduced cardiomyocyte injury, reduced myocardial inflammatory cell infiltration, and protected the myocardium in a rat model of myocardial ischemia–reperfusion injury (Qiu et al., 2017). Meng et al. (2014) found that salvianolic acid salt plus vitamin D3 injections could alleviate atherosclerosis induced by high-fat diets by inhibiting the inflammatory process. Its protective mechanism in atherosclerosis is closely related to the inhibition of oxidative stress and inflammatory responses and the improvement of endothelial dysfunction (Song et al., 2019). In addition, it was found (Wang et al., 2018) that the polysaccharides of Salvia miltiorrhiza Bunge also exhibited good antioxidant activities. Compared with vitamin C, Salvia miltiorrhiza polysaccharides could scavenge more than 90% of free radicals and could be used to prevent cell damage caused by free radicals and intracellular reactive oxygen species (ROS). Cong and Yu (2015) reported that Danshensu could reduce MDA contents, increase SOD activities, enhance cellular oxygen radical scavenging abilities, and improve vascular endothelial cell viabilities in vascular endothelial cells with H2O2-induced injuries and play a protective role against H2O2-induced oxidative damage in vascular endothelial cells. Salvianolic acid B, as one of the main water-soluble components of Salvia miltiorrhiza Bunge, has significant anti-inflammatory and cardiovascular protective effects. Hu et al. (2020) established a myocardial ischemia model and H9C2 cell inflammation model in rats and treated them with different concentrations of salvianolic acid B. Results showed that salvianolic acid B could significantly decrease acute myocardial ischemic injury in rats, significantly inhibit the production of ROS in H9C2 cells, increase the mitochondrial membrane potential, inhibit activation of the NLRP3 inflammasome, and inhibit apoptosis. Animal experiments revealed that salvianolic acid A could exert antiapoptotic effects during myocardial ischemia–reperfusion by activating extracellular signal-regulated kinase 1/2 (ERK1/2) and inhibiting Jun kinase (JNK) (Xu et al., 2014). In addition, Salvia miltiorrhiza Bunge also has hypolipidemic effects. Lim et al. (2017) established a hyperlipidemic mouse model with a high-fat diet and investigated the lipid-regulating mechanisms of methanol extracts of Salvia miltiorrhiza Bunge. It was found that the methanol extracts of Salvia miltiorrhiza Bunge ameliorated hyperlipidemia in mice fed a high-fat diet mainly by inhibiting the increase in serum triacylglycerol levels.
7.2.2 Honghua (carthamus tinctorius L.)
Salvia miltiorrhiza Bunge and Carthamus tinctorius L. were used as a herb pair to treat cardiovascular diseases. Bai et al. (2021) reported that they could reduce the sizes of myocardial infarcts, alleviate ischemic injuries, and inhibit cardiomyocyte apoptosis in a myocardial ischemia/reperfusion injury (MIRI) model in vitro. Danhong injections are composed of Salvia miltiorrhiza Bunge and Carthamus tinctorius L. Modern research has found that Danhong injections can protect against cardiomyocyte injury, inhibit cardiomyocyte apoptosis, and improve the cell survival rates of myocardial cells (Duan et al., 2015). In addition, Yuan (2019) reported that Danhong injections protected against myocardial ischemia–reperfusion injuries in rabbits via antioxidation and the inhibition of cardiomyocyte apoptosis. Hydroxysafflor yellow A, one of the main active ingredients of Carthamus tinctorius L., alleviates MI/RI damage to both heart structures and functions (Ye et al., 2021). In addition, safranal, an active ingredient extracted from saffron, exerts a protective effect on the cardiovascular system. Wang H. et al. (2021) reported that safranal could increase the viability of H9c2 cardiac myoblasts and alleviate H/R-induced H9c2 cardiac myoblast injuries via the PI3K/AKT/GSK3β signaling pathway.
7.2.3 Huangqi (astragalus mongholicus bunge) and danghui (angelica sinensis (Oliv.) diels)
Astragalus mongholicus Bunge and Angelica sinensis (Oliv.) Diels are commonly used as couplet medicine in the clinical treatment of CMVD. Modern pharmacological studies have shown that Astragalus mongholicus Bunge–Angelica sinensis (Oliv.) Diels improved blood circulation, had anti-inflammation and antioxidation effects, and protected the vascular endothelium. By promoting the expression of endothelial nitric oxide synthase (eNOS) and phosphorylation of protein kinase B (PKB/Akt), Astragalus mongholicus Bunge–Angelica sinensis (Oliv.) Diels can promote nitric oxide (NO) release and diastolic blood vessels, which protect the endothelium. It can also inhibit the apoptosis of vascular endothelial cells by inhibiting inducible NOS (iNOS) expressions, improving the expressions of local inflammatory response factors in blood vessels, and inhibiting intimal hyperplasia due to endothelial injury (Xiang et al., 2022). Astragaloside IV is one of the major active components of Astragalus membranaceus, which can reduce cardiomyocyte injuries and attenuate cardiomyocyte apoptosis induced by hypoxia/reoxygenation (H/R) via the inhibition of the calcium-sensing receptor (CaSR)/extracellular signal-regulated kinase 1/2 (ERK1/2), and related apoptotic signaling pathways (Yin et al., 2019). Astragalus polysaccharide can significantly increase human cardiac microvascular endothelial cell viabilities and reduce apoptosis levels due to H/R injury (Xie et al., 2016).
7.2.4 Other chinese herbs
Conioselinum anthriscoides “Chuanxiong,” Paeonia lactiflora Pall, Panax notoginseng (Burkill) F.H. Chen, and Hirudo are all blood-activating and stasis-resolving medicines. Modern pharmacological studies have shown that they all exhibit anti-myocardial ischemia–reperfusion injury, blood flow alteration, anti-atherosclerosis, platelet aggregation inhibition effects, and scavenge oxygen free radicals and also have anti-inflammation, vasodilation, protection of vascular endothelium, and promotion of angiogenesis effects (Liu Y. C. et al., 2021; Wu et al., 2021; Zhang and Ma, 2021; Jiang et al., 2022). Tetramethylpyrazine is one of the main active components of Conioselinum anthriscoides “Chuanxiong.” Tetramethylpyrazine can significantly reduce myocardial infarction sizes, improve myocardial function, reduce cardiomyocyte apoptosis, and provide significant protective effects on cardiomyocytes after ischemia–reperfusion. Its mechanism may be through the regulation of Janus kinase signal transducers 2/signal transducers, activators of the transcription 3 signaling pathway, and mitochondrial autophagy (Cheng et al., 2021). Total paeony glycoside improved the survival rate of cardiomyocytes, inhibited cardiomyocyte apoptosis, and protected H9c2 cardiomyocytes from H/R injury (Shen et al., 2018). Ginsenoside Rb1, ginsenoside Rg1, ginsenoside Re, and notoginsenoside R1 are the major, active components of Panax notoginseng (Burkill) F.H. Chen. Studies have reported (Cui et al., 2017; Li et al., 2018) that ginsenoside Rb1 and ginsenoside Rg1 can decrease I/R-induced myocardial infarct sizes, ameliorate cardiomyocyte injuries, restore myocardial blood flow, and improve heart function. Ginsenoside Re and notoginsenoside R1 can increase NO release in vascular endothelial cells and stimulate vasodilation (Huang et al., 2005; Wang et al., 2016). As a representative TCM for breaking blood and expelling blood stasis, Hirudo has a significant antithrombotic effect. Li et al. (2021) found that Hirudo extracts could inhibit venous thrombosis through antioxidant effects, thus achieving antithrombotic effects. Atherosclerosis is the pathological basis of many cardiovascular diseases. Hirudo and its extracts can exert anti-atherosclerotic effects by regulating lipid metabolism, protecting endothelial cells, and inhibiting smooth muscle proliferation. Chen et al. (2013) found that hirudin could exert an anti-atherosclerotic effect by decreasing the levels of inflammatory factor TNF-α and inhibiting the proliferation of smooth vascular muscle cells.
In conclusion, TCM may achieve the purpose of CMVD treatment through anti-inflammatory and antioxidant effects, improve vascular endothelial function, protect cardiomyocytes, and improve coronary microcirculation.
8 Scientific problems and research directions of CMVD
Although significant progress has been made in the basic and clinical research of CMVD, many scientific issues in this field remain to be solved. 1) Nonuniform clinical classifications: in the early literature, patients exhibiting chest pain without significant coronary angiography abnormalities were classified as having syndrome X. With the improvements in clinical research and diagnostic techniques, the clinical classification of CMVD has become increasingly detailed. Reasonable clinical classifications are helpful to elucidate the pathogenesis, establish diagnostic criteria and treatment choices, and determine prognoses. Establishing a more reasonable clinical classification of CMVD needs further study. 2) Unknown pathogeneses: because the clinical phenotype of CMVD is very complex, many CMVD mechanisms have been proposed, including endothelial cell-dependent and non-dependent vasodilation abnormalities, microvascular spasms, microvascular embolization, extravascular compression, and other mechanisms (Ford et al., 2018). What are the pathogenic differences among the clinical phenotypes of CMVD? What are the key factors that influence these mechanisms? Do interventions involving these mechanisms improve clinical symptoms and patient prognoses? These questions remain unanswered. In order to explore the mechanisms of CMVD, it is necessary to establish an animal model similar to pathological CMVD changes in humans. However, there is still a lack of animal models that can simulate human CMVD. 3) Inadequate clinical diagnoses: because the diameters of coronary microvessels are smaller than the resolution of existing imaging techniques, the morphology of these vessels cannot be observed by clinicians. Therefore, laboratory diagnoses of CMVD are mainly based on measurements of coronary microvascular function. Although the value of invasive examinations in the diagnosis of coronary artery function is well known, there are a few clinical applications for various reasons, which lead to a lack of CMVD diagnoses. (4) Unclear drug efficacies: currently, although there are small randomized clinical studies or nonrandomized observational studies in the literature that focus on CMVD and end-point coronary microvascular function, there is still a lack of results from large randomized clinical trials with CMVD as the subject and cardiovascular events as the endpoint of the observations (Crea et al., 2014). CMVD treatments are still limited to controlling the traditional risk factors for arteriosclerosis, improving lifestyles, and relieving angina symptoms. Therefore, the treatments that can decrease the incidence of cardiovascular events in CMVD have not been determined.
In view of the above scientific challenges, we suggest that future research should focus on the following areas: 1) studying animal models that can simulate human CMVD; 2) exploring the key molecules and targets of CMVD development and studying CMVD pathogenesis by using genomics, transcriptomics, and proteomics techniques to search for molecular markers and intervention targets; 3) developing highly sensitive and specific serological markers that can predict and detect CMVD and developing molecular imaging techniques that can reveal the extent of CMVD; and 4) conducting large-sample, multicenter, randomized clinical trials with cardiovascular event endpoints to validate the potential for new CMVD-specific drugs and therapies to improve clinical endpoints and establish evidence-based medical treatments. Objective and accurate evaluations of CMVD are of great value for both CMVD diagnosis and searching for new intervention measures. In the future, more in-depth research on the diagnosis, treatment, and pathological mechanism of CMVD is expected to be conducted to establish a better and more accurate diagnosis and treatment strategies.
9 Conclusion and perspectives
Cardiovascular disease is one of the main causes of human death. Previous studies have shown that myocardial ischemia is mainly caused by epicardial coronary artery occlusion. However, in some patients with angina pectoris, coronary angiography (CAG) did not reveal occlusive disease, which suggested that myocardial ischemia may be the cause of coronary microcirculation dysfunction (Padro et al., 2020). Although the CAG technique has resulted in great progress in recent decades and the diagnostic accuracy of subepicardial coronary artery stenosis has been improved, the diagnostic sensitivity of CAG for myocardial ischemia is still limited. Studies have shown that half of the patients with known or suspected angina who receive CAG have nonobstructive coronary stenosis, which may be related to CMVD (Ford et al., 2020). CMVD is associated with an increased risk of MACEs (Jespersen et al., 2012; Maddox et al., 2014). The coronary angiography results were associated with significantly higher rates of cardiovascular events and all-cause mortality in patients with angina and with nonobstructive coronary artery disease than in the controls. The main cause of the poor prognoses in these angina patients may be related to CMVD, as researchers have determined (Taqueti et al., 2017; Taqueti and Di Carli, 2018). Therefore, the detection and treatment of CMVD have important clinical significance. There are no consensus on CMVD treatments, clinical practices for patients to improve symptoms, and intervention strategies for cardiovascular risk factors. Although CMVD has received increasing attention in the cardiovascular field, the etiological screening of myocardial ischemia is still limited to assessments of the epicardial coronary arteries, and assessments of coronary microcirculation have not received enough attention. At present, there is no large-scale clinical study of CMVD with cardiovascular outcomes. In summary, CMVD is an important problem in the cardiovascular field. Although the study of CMVD has been deepened in modern medicine, the diagnosis, evaluation, and treatment of CMVD still face great challenges.
In recent years, the understanding of CMVD with respect to traditional Chinese medicine has been greatly improved, and many clinical studies have been conducted. Treatments based on syndrome differentiation using CPMs, TCM injections, and TCM decoctions can effectively relieve the clinical symptoms of patients, improve their quality of life and exercise tolerance, improve their long-term prognoses, and decrease their readmission rates, which provide new ideas and directions for the study of CMVD. However, due to the flexibility of treatment based on syndrome differentiation, the standards for syndrome differentiation and reasonable diagnosis and treatment schemes have not been unified, making it difficult to introduce TCM in clinics. At present, most clinical studies of traditional Chinese medicine for CMVD are characterized by inconstant designs, small sample sizes, short observation times, and a lack of large-scale multicenter prospective randomized control studies; therefore, the results of such studies cannot be extended to a wide range of clinical applications.
In addition, TCM compounds have multicomponent, multitarget, and multi-pathway synergistic actions. At present, research on CMVD mainly focuses on the action of one extract or one part of a single drug, which lays a foundation for research on the material basis of TCM compound prescriptions. Studying single ingredients ignores the relationships among drug taste, drug properties, and symptoms, and studies of compound prescriptions have mostly remained at the pharmacodynamic stage. Pharmacodynamic evaluations mostly use the evaluation system of a single target of chemical drugs for reference and neglect the characteristics of synergistic effects and multipoint fine-tuning. However, it should be noted that compound TCM prescriptions are the main form of clinical TCM use, and the clinical applications of TCM should be based on syndrome differentiation. At present, little attention has been paid to the compatibility of effective components, interactions among components, and the differences among different components. As a result, the current approach fails to emphasize the concept of compatibility of TCM to increase efficacy and decrease toxicity.
Therefore, future studies of TCM treatment of CMVD should begin from the following three perspectives. 1) For the theoretical research aspect, it is necessary to systematize and summarize the relevant ancient books and existing research to further improve the understanding of CMVD in TCM. 2) With regard to clinical research, we need to strengthen scientific and normative research and conduct large-sample, multicenter randomized clinical trials with the endpoints of cardiovascular events, evaluate the potential for CMVD-specific new drugs and therapies to improve clinical endpoints, and conduct efficacy and safety evaluations to provide stronger evidence-based medical evidence. 3) In basic research, we should use network pharmacology, metabolomics, molecular biology, proteomics, and other new research methods to explain the mechanisms of TCM in treating CMVD at the metabolite, gene, and protein levels to provide a new strategy for controlling CMVD.
In summary, CMVD still presents a thorny clinical problem. TCM has great therapeutic potential with respect to CMVD, but more large-scale and in-depth clinical and animal studies are needed to promote the clinical applications of TCM in CMVD.
Author contributions
ZY, SL, YL, QR, ZG, CW, and YB performed the literature search, selected relevant articles, interpreted data, and wrote the report; ZY and SL contributed equally to this work and shared the first authorship; ZY and SL were responsible for the entire manuscript; XW and JM designed and supervised this work. All authors have read and approved the final submission.
Funding
This work was supported by the National Natural Science Foundation of China (no. 82174326), the Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (No: ZYYCXTD-C-202203), the “Innovation Team Development Plan” of the Ministry of Education-Research on the prevention and treatment of cardiovascular diseases in traditional Chinese medicine (no. IRT_16R54), the Tianjin Research Innovation Project for Postgraduate Students (no. 2021YJSB294), and the Graduate Research Innovation Project of Tianjin University of Traditional Chinese Medicine (no. YJSKC-20211012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Arroyo-Espliguero, R., and Kaski, J. C. (2006). Microvascular dysfunction in cardiac syndrome X: The role of inflammation. CMAJ 174, 1833–1834. doi:10.1503/cmaj.051331
Bai, J., Wang, X., Du, S., Wang, P., Wang, Y., Quan, L., et al. (2021). Study on the protective effects of danshen-honghua herb pair (DHHP) on myocardial ischaemia/reperfusion injury (MIRI) and potential mechanisms based on apoptosis and mitochondria. Pharm. Biol. 59, 335–346. doi:10.1080/13880209.2021.1893346
Bairey Merz, C. N., Handberg, E. M., Shufelt, C. L., Mehta, P. K., Minissian, M. B., Wei, J., et al. (2016). A randomized, placebo-controlled trial of late Na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): Impact on angina and myocardial perfusion reserve. Eur. Heart J. 37, 1504–1513. doi:10.1093/eurheartj/ehv647
Bairey Merz, C. N., Pepine, C. J., Shimokawa, H., and Berry, C. (2020). Treatment of coronary microvascular dysfunction. Cardiovasc Res. 116, 856–870. doi:10.1093/cvr/cvaa006
Baumgart, D., Haude, M., Görge, G., Liu, F., Ge, J., Grosse-Eggebrecht, C., et al. (1999). Augmented alpha-adrenergic constriction of atherosclerotic human coronary arteries. Circulation 99, 2090–2097. doi:10.1161/01.cir.99.16.2090
Bi, Y. F., Mao, J. Y., Zhang, Z. P., Wang, X. L., Wang, H. H., Ge, Y. B., et al. (2013). Research progress of traditional Chinese medicine treatment for cardiac syndrome X. Shanghai J. Traditional Chin. Med. 47, 77–80.
Brainin, P., Frestad, D., and Prescott, E. (2018). The prognostic value of coronary endothelial and microvascular dysfunction in subjects with normal or non-obstructive coronary artery disease: A systematic review and meta-analysis. Int. J. Cardiol. 254, 1–9. doi:10.1016/j.ijcard.2017.10.052
Camici, P. G., and Crea, F. (2007). Coronary microvascular dysfunction. N. Engl. J. Med. 356, 830–840. doi:10.1056/NEJMra061889
Camici, P. G., Tschöpe, C., Di Carli, M. F., Rimoldi, O., and Van Linthout, S. (2020). Coronary microvascular dysfunction in hypertrophy and heart failure. Cardiovasc Res. 116, 806–816. doi:10.1093/cvr/cvaa023
Cannon, R. O., Leon, M. B., Watson, R. M., Rosing, D. R., and Epstein, S. E. (1985). Chest pain and "normal" coronary arteries--role of small coronary arteries. Am. J. Cardiol. 55, 50b–60b. doi:10.1016/0002-9149(85)90613-7
Cao, X. C., Zhao, H. Z., Kong, D. Y., Yi, S. W., Wu, Z. Y., and Sun, W. (2021). Observation of curative effect of Pushen capsule combined with rosuvastatin calcium in the treatment of coronary slow blood flow dyslipidemia. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 19, 1861–1863.
Cao, Y., Wang, H. F., Yuan, R. H., Wang, Y., He, R., Cheng, Y., et al. (2022). Systematic review and meta analysis of treating both Qi and Blood Method in adjuvant treatment of microvascular angina pectoris. J. Shandong Univ. Traditional Chin. Med. 46, 54–63.
Cattaneo, M., Porretta, A. P., and Gallino, A. (2015). Ranolazine: Drug overview and possible role in primary microvascular angina management. Int. J. Cardiol. 181, 376–381. doi:10.1016/j.ijcard.2014.12.055
Celermajer, D. S., Sorensen, K. E., Gooch, V. M., Spiegelhalter, D. J., Miller, O. I., Sullivan, I. D., et al. (1992). Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340, 1111–1115. doi:10.1016/0140-6736(92)93147-f
Chang, C. C., Wei, C., and Wu, Y. L. (2016). “Minute Collaterals and Microvessels” concept and its clinical guiding significance in meridian and collateral theory. J. Traditional Chin. Med. 57, 7–11. doi:10.13288/j.11-2166/r.2016.01.002
Chen, B., Liu, H., Zhang, Y. J., Ma, Z. H., Tao, J. P., Hu, Y., et al. (2018). Effect of Danhong Injection on the levels of plasma hs-CRP and Hcy and clinical efficacy in patients with microvascular angina pectoris. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 16, 2116–2118. doi:10.12102/j.issn.1672-1349.2018.15.002
Chen, B. Z., Feng, M. J., Chang, F. Y., Sun, Z. G., Zhang, Y., Feng, Z. R., et al. (2022). Effect of Shexiang Baoxin Pill on vascular endothelial function in patients with coronary artery microcirculation disorder. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 20, 182–184. doi:10.12102/j.issn.1672-1349.2022.01.041
Chen, C., Wei, J., Albadri, A., Zarrini, P., and Bairey Merz, C. N. (2017). Coronary microvascular Dysfunction - epidemiology, pathogenesis, prognosis, diagnosis, risk factors and therapy. Circ. J. 81, 3–11. doi:10.1253/circj.CJ-16-1002
Chen, G. W., Pan, Y., Shang, L., and Yu, H. (2013). Effects of leech on atherosclerotic lesion in apolipoprotein E deficient mice. Med. J. Wuhan Univ. 34, 344–347+367. doi:10.14188/j.1671-8852.2013.03.002
Chen, H. J., Zhang, Y. J., and Ke, R. (2021). Clinical observation on modified Danshen decoction for the treatment of microvascular angina pectoris with syndrome of heart blood stagnation. J. Guangzhou Univ. Traditional Chin. Med. 38, 455–459. doi:10.13359/j.cnki.gzxbtcm.2021.03.004
Chen, H., and Ma, Q. (2014). Observation of Yixinshu capsule on clinical symptoms and anxiety state of cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 12, 561–562. doi:10.1016/s2095-4964(14)60027-3
Chen, L. Y., and Song, Y. J. (2019). Treatment of 106 cases of climacteric female microvascular angina pectoris with Yishen Jieyu Tongmai decoction. Chin. J. Traditional Med. Sci. Technol. 26, 244–245.
Cheng, C. B., Chen, T. B., and Xu, Y. B. (2021). Mechanism of ligustrazine on mitochondrial autophagy reducing myocardial ischemia reperfusion injury through JAK2/STAT3 signaling pathway. Chin. J. Immunol. 37, 819–823. doi:10.3969/j.issn.1000-484X.2021.07.009
Cheng, F. (2011). Combined Naoxintong Capsule treatment of 62 cases of cardiac syndrome X. Chin. Tradit. Pat. Med. 33, 2041–2043.
Choi, K. H., Dai, N., Li, Y., Kim, J., Shin, D., Lee, S. H., et al. (2021). Functional coronary angiography-derived index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 14, 1670–1684. doi:10.1016/j.jcin.2021.05.027
Cong, L. Y., and Yu, H. (2015). Protective effect of Danshensu on H2O2-induced oxidative damage of vascular endothelial cells. World Latest Med. Inf. 15, 136–137.
Crea, F., Camici, P. G., and Bairey Merz, C. N. (2014). Coronary microvascular dysfunction: an update. Eur. Heart J. 35, 1101–1111. doi:10.1093/eurheartj/eht513
Cuculi, F., De Maria, G. L., Meier, P., Dall'armellina, E., De Caterina, A. R., Channon, K. M., et al. (2014). Impact of microvascular obstruction on the assessment of coronary flow reserve, index of microcirculatory resistance, and fractional flow reserve after ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 64, 1894–1904. doi:10.1016/j.jacc.2014.07.987
Cui, J. K., Wang, C. Y., and Leng, Y. L. (2021). Clinical observation of modified Danggui Sini decoction in the treatment of cold coagulated heart vessel type of microvascular angina pectoris. J. Emerg. Traditional Chin. Med. 30, 1987–1990. doi:10.3969/j.issn.1004-745X.2021.11.02
Cui, Y. C., Pan, C. S., Yan, L., Li, L., Hu, B. H., Chang, X., et al. (2017). Ginsenoside Rb1 protects against ischemia/reperfusion-induced myocardial injury via energy metabolism regulation mediated by RhoA signaling pathway. Sci. Rep. 7, 44579. doi:10.1038/srep44579
Dagres, N., Saller, B., Haude, M., Hüsing, J., Von Birgelen, C., Schmermund, A., et al. (2004). Insulin sensitivity and coronary vasoreactivity: Insulin sensitivity relates to adenosine-stimulated coronary flow response in human subjects. Clin. Endocrinol. (Oxf) 61, 724–731. doi:10.1111/j.1365-2265.2004.02156.x
De Ferrari, G. M., Fox, K. A., White, J. A., Giugliano, R. P., Tricoci, P., Reynolds, H. R., et al. (2014). Outcomes among non-ST-segment elevation acute coronary syndromes patients with no angiographically obstructive coronary artery disease: Observations from 37,101 patients. Eur. Heart J. Acute Cardiovasc Care 3, 37–45. doi:10.1177/2048872613489315
Del Buono, M. G., Montone, R. A., Camilli, M., Carbone, S., Narula, J., Lavie, C. J., et al. (2021). Coronary microvascular dysfunction across the spectrum of cardiovascular diseases: JACC state-of-the-art review. J. Am. Coll. Cardiol. 78, 1352–1371. doi:10.1016/j.jacc.2021.07.042
Demirkol, S., Balta, S., Unlu, M., Arslan, Z., Cakar, M., Kucuk, U., et al. (2014). Neutrophils/lymphocytes ratio in patients with cardiac syndrome X and its association with carotid intima-media thickness. Clin. Appl. Thromb. Hemost. 20, 250–255. doi:10.1177/1076029612467227
Driessen, R. S., Raijmakers, P. G., Stuijfzand, W. J., and Knaapen, P. (2017). Myocardial perfusion imaging with PET. Int. J. Cardiovasc Imaging 33, 1021–1031. doi:10.1007/s10554-017-1084-4
Du, J., Hou, J., Feng, J., Zhou, H., Zhao, H., Yang, D., et al. (2019). Plin5/p-Plin5 guards diabetic CMECs by regulating FFAs metabolism bidirectionally. Oxid. Med. Cell Longev. 2019, 8690746. doi:10.1155/2019/8690746
Duan, Z. Z., Li, Y. H., Li, Y. Y., Fan, G. W., Chang, Y. X., Yu, B., et al. (2015). Danhong injection protects cardiomyocytes against hypoxia/reoxygenation- and H2O2-induced injury by inhibiting mitochondrial permeability transition pore opening. J. Ethnopharmacol. 175, 617–625. doi:10.1016/j.jep.2015.08.033
Fang, L., Sun, J. P., Wang, Y., and Wei, X. (2018). Cardiac hydatid disease. Chin. J. Difficult Complicat. Cases 17, 325–328. doi:10.1002/9781119453192.ch58
Fang, Y., Zhang, F., Leng, Q., Wen, F., and He, L. Q. (2013). Clinical observation on Guanxin Danshen drop pills for coronary slow flow phenomenon. Inn. Mong. J. Traditional Chin. Med. 32, 30–31. doi:10.16040/j.cnki.cn15-1101.2013.13.113
Fearon, W. F., Shah, M., Ng, M., Brinton, T., Wilson, A., Tremmel, J. A., et al. (2008). Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 51, 560–565. doi:10.1016/j.jacc.2007.08.062
Feng, Q. M., Dong, Y. R., Zhao, Y., Wang, S. L., Wang, J. L., and Ma, Z. Y. (2013). Treatment of sixty-one patients with coronary slow flow phenomenon by yiqi huoxue recipe combined western drugs: a clinical research. Zhongguo Zhong Xi Yi Jie He Za Zhi 33, 747–750.
Feng, Z. R., Wang, F., Chang, F. Y., Ma, L., Xu, Y. C., Chen, B. Z., et al. (2017). Effect of combined Xinkeshu tablets and nicorandil on vascular endothelial function in X syndrome patients. Chin. J. Geriatric Heart Brain Vessel Dis. 19, 381–383. doi:10.3969/j.issn.1009-0126.2017.04.012
Ford, T. J., Ong, P., Sechtem, U., Beltrame, J., Camici, P. G., Crea, F., et al. (2020). Assessment of vascular dysfunction in patients without obstructive coronary artery disease: Why, how, and when. JACC Cardiovasc Interv. 13, 1847–1864. doi:10.1016/j.jcin.2020.05.052
Ford, T. J., Rocchiccioli, P., Good, R., Mcentegart, M., Eteiba, H., Watkins, S., et al. (2018). Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur. Heart J. 39, 4086–4097. doi:10.1093/eurheartj/ehy529
Gdowski, M. A., Murthy, V. L., Doering, M., Monroy-Gonzalez, A. G., Slart, R., and Brown, D. L. (2020). Association of isolated coronary microvascular dysfunction with mortality and major adverse cardiac events: A systematic review and meta-analysis of aggregate data. J. Am. Heart Assoc. 9, e014954. doi:10.1161/JAHA.119.014954
Giacco, F., and Brownlee, M. (2010). Oxidative stress and diabetic complications. Circ. Res. 107, 1058–1070. doi:10.1161/CIRCRESAHA.110.223545
Gibson, C. M., Cannon, C. P., Murphy, S. A., Ryan, K. A., Mesley, R., Marble, S. J., et al. (2000). Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 101, 125–130. doi:10.1161/01.cir.101.2.125
Godo, S., and Shimokawa, H. (2017). Endothelial functions. Arterioscler. Thromb. Vasc. Biol. 37, e108–e114. doi:10.1161/ATVBAHA.117.309813
Gong, Y. M., Si, L., Guo, X. J., Zhang, M., Song, W., Zhao, B., et al. (2021). Curative effect and clinical safety of Shexiang Tongxin dropping Pills for microvascular angina. Chin. J. Evidence-Based Cardiovasc. Med. 13, 577–579+583. doi:10.3969/j.issn.1674-4055.2021.05.16
Gould, K. L. (2009). Does coronary flow trump coronary anatomy? JACC Cardiovasc Imaging 2, 1009–1023. doi:10.1016/j.jcmg.2009.06.004
Gould, K. L., Lipscomb, K., and Hamilton, G. W. (1974). Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am. J. Cardiol. 33, 87–94. doi:10.1016/0002-9149(74)90743-7
Gulati, M., Cooper-Dehoff, R. M., Mcclure, C., Johnson, B. D., Shaw, L. J., Handberg, E. M., et al. (2009). Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the women's ischemia syndrome evaluation study and the st james women take heart project. Arch. Intern Med. 169, 843–850. doi:10.1001/archinternmed.2009.50
Guo, X. B., Hu, M. Q., Gao, R. T., and Li, S. (2020). Clinical evaluation of Yiqi Fumai Lyophilized Injection combined with nicorandil in treatment of microvascular angina with Qi and Yin deficiency. Drug Eval. Res. 43, 1597–1601. doi:10.7501/j.issn.1674-6376.2020.08.022
He, X. K., Dong, J., Zhao, Y., Ma, S. H., and Zhao, Y. J. (2017). Efficacy of Nicorandil for treating the patients with cardiac syndrome X and its impact on vascular endothelial function. Chin. Circulation J. 32, 676–679. doi:10.3969/j.issn.1000-3614.2017.07.013
He, Z. H., Wang, Z. Q., Wang, G. L., Ma, G., Xue, Y. L., Teng, W., et al. (2020). Clinical study on Huoxue Zhuyu decoction combined with Nicorandil for microvascular angina. New Chin. Med. 52, 60–63. doi:10.13457/j.cnki.jncm.2020.18.017
Herscovici, R., Sedlak, T., Wei, J., Pepine, C. J., Handberg, E., and Bairey Merz, C. N. (2018). Ischemia and No obstructive coronary artery disease ( INOCA ): What is the risk? J. Am. Heart Assoc. 7, e008868. doi:10.1161/JAHA.118.008868
Hu, G. L., Bai, X. P., and Hou, X. L. (2014). Clinical efficacy of Danhong Injection on cardiac syndrome X. Chin. J. Evidence-Based Cardiovasc. Med. 6, 558–561. doi:10.3969/j.1674-4055.2014.05.14
Hu, Y., Wang, X., Li, Q., Pan, Y., and Xu, L. (2020). Salvianolic acid B alleviates myocardial ischemic injury by promoting mitophagy and inhibiting activation of the NLRP3 inflammasome. Mol. Med. Rep. 22, 5199–5208. doi:10.3892/mmr.2020.11589
Huang, Y. C., Chen, C. T., Chen, S. C., Lai, P. H., Liang, H. C., Chang, Y., et al. (2005). A natural compound (ginsenoside Re) isolated from Panax ginseng as a novel angiogenic agent for tissue regeneration. Pharm. Res. 22, 636–646. doi:10.1007/s11095-005-2500-3
Huang, Y., Wang, X. L., Guo, W., Guan, J. S., Xue, J. G., Chen, T. J., et al. (2019). Intervention effect of Yiqi Huoxue Huatan decoction on patients with slow blood flow after percutaneous coronary intervention. J. Nanjing Univ. Traditional Chin. Med. 35, 387–390. doi:10.14148/j.issn.1672-0482.2019.0387
Huo, Y., and Kassab, G. S. (2012). Compensatory remodeling of coronary microvasculature maintains shear stress in porcine left-ventricular hypertrophy. J. Hypertens. 30, 608–616. doi:10.1097/HJH.0b013e32834f44dd
Jespersen, L., Hvelplund, A., Abildstrøm, S. Z., Pedersen, F., Galatius, S., Madsen, J. K., et al. (2012). Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 33, 734–744. doi:10.1093/eurheartj/ehr331
Ji, Y. M., and Ren, B. J. (2009). Observation on the curative effect of Shuxuetong injection in the treatment of cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 7, 1147–1148.
Jia, J. Z., Wang, A. X., and Xu, K. (2019a). The diagnostic value of serum IL-6 expression to coronary microvascular dysfunction in patients with acute coronary syndrom. J. Cardiovasc. Pulm. Dis. 38, 1106–1109+1142. doi:10.3969/j.issn.1007-5062.2019.11.004
Jia, W. M., Niu, S. Z., Zhang, L. Z., Li, Z., Chen, J. B., and Niu, L. (2019b). Clinical efficacy of Xinkeshu tablets combined with nicorandil in the treatment of microvascular angina pectoris and its effect on inflammatory factors. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 17, 1044–1046. doi:10.12102/j.issn.1672-1349.2019.07.024
Jiang, H. B., Zhai, X. Q., Chen, Z. X., and Wang, X. F. (2021). Effectiveness of Qihong powder combined with nicorandil on coronary slow flow: a randomized controlled trial. Chin. J. Integr. Traditional West. Med. 41, 1174–1178. doi:10.7661/j.cjim.20210812.056
Jiang, Q., Wang, L. N., Liu, Q., Yang, C. M., and Zhang, Y. Q. (2022). Research progress on processing history evolution, chemical constituents and pharmacological action of Hirudo. China J. Chin. Materia Medica, 1–14. doi:10.19540/j.cnki.cjcmm.20220411.201
Jiang, Z. L. (2021). The effect of Fufang Wenban decoction adjuvant therapy on patients with coronary slow blood flow microvascular angina pectoris. Prev. Treat. Cardiovasc. Dis. 11, 31–33.
Jin, H. L. (2018). Clinical observation on Shexiang Baoxin Pill combined with Nicorandil in treating microvascular angina pectoris. Guangming J. Chin. Med. 33, 2265–2267. doi:10.3969/j.issn.1003-8914.2018.15.053
Kang, L. R., Yuan, J. J., A, N. R., Liu, Y., Song, L. Y., and Wang, Y. L. (2021). Effect of Qishen Yiqi dropping pills on coronary microcirculation dysfunction in patients with ischemic non-obstructive coronary arteries. Cent. South Pharm. 19, 1014–1018. doi:10.7539/j.issn.1672-2981.2021.05.042
Kaski, J. C., Crea, F., Gersh, B. J., and Camici, P. G. (2018). Reappraisal of ischemic heart disease. Circulation 138, 1463–1480. doi:10.1161/CIRCULATIONAHA.118.031373
Kaufmann, P. A., Gnecchi-Ruscone, T., Di Terlizzi, M., Schäfers, K. P., Lüscher, T. F., and Camici, P. G. (2000a). Coronary heart disease in smokers: Vitamin C restores coronary microcirculatory function. Circulation 102, 1233–1238. doi:10.1161/01.cir.102.11.1233
Kaufmann, P. A., Gnecchi-Ruscone, T., Schäfers, K. P., Lüscher, T. F., and Camici, P. G. (2000b). Low density lipoprotein cholesterol and coronary microvascular dysfunction in hypercholesterolemia. J. Am. Coll. Cardiol. 36, 103–109. doi:10.1016/s0735-1097(00)00697-5
Kemp, H. G., Vokonas, P. S., Cohn, P. F., and Gorlin, R. (1973). The anginal syndrome associated with normal coronary arteriograms. Report of a six year experience. Am. J. Med. 54, 735–742. doi:10.1016/0002-9343(73)90060-0
Khan, M. A., Hashim, M. J., Mustafa, H., Baniyas, M. Y., Al Suwaidi, S. K. B. M., Alkatheeri, R., et al. (2020). Global epidemiology of ischemic heart disease: Results from the global burden of disease study. Cureus 12, e9349. doi:10.7759/cureus.9349
Labazi, H., and Trask, A. J. (2017). Coronary microvascular disease as an early culprit in the pathophysiology of diabetes and metabolic syndrome. Pharmacol. Res. 123, 114–121. doi:10.1016/j.phrs.2017.07.004
Lanza, G. A., Parrinello, R., and Figliozzi, S. (2014). Management of microvascular angina pectoris. Am. J. Cardiovasc Drugs 14, 31–40. doi:10.1007/s40256-013-0052-1
Lerman, A., Burnett, J. C., Higano, S. T., Mckinley, L. J., and Holmes, D. R. (1998). Long-term L-arginine supplementation improves small-vessel coronary endothelial function in humans. Circulation 97, 2123–2128. doi:10.1161/01.cir.97.21.2123
Li, B. (2018). Effect of Tongluo Ningxin recipe on coronary blood flow velocity and inflammatory factors in patients with coronary slow blood flow. Chin. J. Ethnomedicine Ethnopharmacy 27, 82–84.
Li, H. Y. (2019). Effects of Liqi Huoxue dropping pills combined with nicorandil on exercise treadmill test, inflammatory response and vascular endothelial function of cardiac microvascular angina pectoris. Mod. J. Integr. Traditional Chin. West. Med. 28, 1096–1099. doi:10.3969/j.issn.1008-8849.2019.10.017
Li, J. (2014). Effect of Guanxinshutong capsule on coronary slow flow phenomenon. Pract. J. Cardiac Cereb. Pneumal Vasc. Dis. 22, 4–6. doi:10.3696/j.issn.1008-5971.2014.10.002
Li, J. M., Mullen, A. M., and Shah, A. M. (2001). Phenotypic properties and characteristics of superoxide production by mouse coronary microvascular endothelial cells. J. Mol. Cell Cardiol. 33, 1119–1131. doi:10.1006/jmcc.2001.1372
Li, L., Pan, C. S., Yan, L., Cui, Y. C., Liu, Y. Y., Mu, H. N., et al. (2018). Ginsenoside Rg1 ameliorates rat myocardial ischemia-reperfusion injury by modulating energy metabolism pathways. Front. Physiol. 9, 78. doi:10.3389/fphys.2018.00078
Li, L., Yu, X., Li, Y., Zhang, L. L., Qi, Y. J., and Xu, Y. F. (2017). A clinical study on treating microvascular angina with the Maixuekang capsule. Clin. J. Chin. Med. 9, 23–24. doi:10.3969/j.issn.1674-7860.2017.24.011
Li, L., and Yu, X. (2010). Observation of curative effect of Shuxuetong in the treatment of cardiac syndrome X. J. Liaoning Univ. Traditional Chin. Med. 12, 171–172. doi:10.13194/j.jlunivtcm.2010.11.173.lil.047
Li, P., Lin, B., Tang, P., Ye, Y., Wu, Z., Gui, S., et al. (2021). Aqueous extract of Whitmania pigra Whitman ameliorates ferric chloride-induced venous thrombosis in rats via antioxidation. J. Thromb. Thrombolysis 52, 59–68. doi:10.1007/s11239-020-02337-8
Li, Y. H., Yang, Y. L., Li, J., Wan, X., and Gong, F. (2020). Influences of Huoxue Tongmai Yixin decoction on vascular endothelial function, coronary blood flow reserve and cardiac microcirculation in patients with microvascular angina pectoris of Qi stagnation and blood stasis type. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 18, 2963–2967. doi:10.12102/j.issn.1672-1349.2020.18.005
Lim, C., Lim, S., Lee, B., Kim, B., and Cho, S. (2017). Effect of methanol extract of Salviae miltiorrhizae Radix in high-fat diet-induced hyperlipidemic mice. Chin. Med. 12, 29. doi:10.1186/s13020-017-0150-0
Lin, K. X., Han, Y. J., Xie, C. L., Huang, G. Q., Li, J. G., and Chen, X. (2011). Clinical observation of Qingling decoction for microvascular angina pectoris. Asia-Pacific Tradit. Med. 7, 46–47.
Lind, L., Berglund, L., Larsson, A., and Sundström, J. (2011). Endothelial function in resistance and conduit arteries and 5-year risk of cardiovascular disease. Circulation 123, 1545–1551. doi:10.1161/CIRCULATIONAHA.110.984047
Lindahl, B., Baron, T., Erlinge, D., Hadziosmanovic, N., Nordenskjöld, A., Gard, A., et al. (2017). Response by Lindahl et al to Letter Regarding Article, "Medical Therapy for Secondary Prevention and Long-Term Outcome in Patients With Myocardial Infarction With Nonobstructive Coronary Artery Disease". Circulation 136, 1082–1083. doi:10.1161/CIRCULATIONAHA.117.029938
Liu, D., Gao, M. T., Wu, Y. J., and Zhang, B. L. (2008). Protective effects of Salvia miltiorrhiza granule on experimental myocardial ischemia and coagulation system. Pharmacol. Clin. Chin. Materia Medica 01, 43–47. doi:10.13412/j.cnki.zyyl.2008.01.025
Liu, P., and Gu, W. P. (2021). Effects of Compound Salvia Miltiorrhiza injection on hemorheology, inflammatory factor, oxidative stress and vascular endothelial cell function in angina pectoris patients after PCI. J. Hunan Normal Univ. Sci. 18, 135–137.
Liu, Q., Jia, Y. S., Song, W. T., and Li, W. W. (2021a). Effects of Zhima Xiaotan Huoxue recipe on no-reflow and prognosis after percutaneous coronary intervention in low-risk non-ST-elevation acute coronary syndrome patients. J. Clin. Med. Pract. 25, 69–73. doi:10.7619/jcmp.20212580
Liu, T. H., Yang, Y. Y., and Mei, X. (2021b). Clinical observation of wide chest aerosol in the treatment of coronary microvascular angina pectoris. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 19, 1593–1594. doi:10.12102/j.issn.1672-1349.2021.09.039
Liu, Y. C., Zhang, T. J., Guo, H. B., Xu, J., Lin, J., Zhang, H. B., et al. (2021c). Research progress on Notoginseng Radix et Rhizoma and predictive analysis on its Q-Marker. Chin. Traditional Herb. Drugs 52, 2733–2745. doi:10.7501/j.issn.0253-2670.2021.09.023
Liu, Y., Li, Y., Xiao, W. L., Zhang, J., Xu, T. S., Wei, L. G., et al. (2017). Clinical effect of Dengzhan Shengmai on patients with coronary slow blood flow. Guangdong Med. J. 38, 626–629. doi:10.13820/j.cnki.gdyx.2017.04.023
Liu, Z. Y., Yin, X. G., Li, Z. L., Jin, D. Q., and Chen, Z. Q. (2013). Clinical observation of Tongxinluo Capsule in treating cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 11, 1390–1391. doi:10.3969/j.issn.1672-1349.2013.11.063
Long, M., Huang, Z., Zhuang, X., Huang, Z., Guo, Y., Liao, X., et al. (2017). Association of inflammation and endothelial dysfunction with coronary microvascular resistance in patients with cardiac syndrome X. Arq. Bras. Cardiol. 109, 397–403. doi:10.5935/abc.20170149
Long, W. P., Chen, J., He, H. K., and Yang, J. Y. (2010). Clinical study of Yixinyin for coronary slow blood flow. Glob. Tradit. Chin. Med. 3, 286–287. doi:10.3969/j.issn1674-1749.2010.04.017
Lopez, D. M., Divakaran, S., Gupta, A., Bajaj, N. S., Osborne, M. T., Zhou, W., et al. (2022). Role of exercise treadmill testing in the assessment of coronary microvascular disease. JACC Cardiovasc Imaging 15, 312–321. doi:10.1016/j.jcmg.2021.07.013
Luo, W. P., Wen, Y. N., Shi, F. F., Wang, Y. G., and Ma, J. (2017). Effects of Bushen Huoxue granule on vascular endothelial function and inflammatory factors in postmenopausal patients with microvascular angina pectoris. J. Pract. Traditional Chin. Med. 33, 227–228.
Lv, X. L., Zhao, Z. Q., Feng, Z., Q., Feng, J. Y., and Gu, H. M. (2014). Effects of Tongxinluo capsule on endothelial function and inflammatory factors in patients with cardiac syndrome X. J. Clin. Med. Pract. 18, 135–136. doi:10.7619/jcmp.201421046
Maddox, T. M., Stanislawski, M. A., Grunwald, G. K., Bradley, S. M., Ho, P. M., Tsai, T. T., et al. (2014). Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312, 1754–1763. doi:10.1001/jama.2014.14681
Mangiacapra, F., Del Buono, M. G., Abbate, A., Gori, T., Barbato, E., Montone, R. A., et al. (2020). Role of endothelial dysfunction in determining angina after percutaneous coronary intervention: Learning from pathophysiology to optimize treatment. Prog. Cardiovasc Dis. 63, 233–242. doi:10.1016/j.pcad.2020.02.009
Mao, M. J., Zhao, Y. L., Deng, B., Deng, B. W., Zheng, W., Liu, Y., et al. (2021). Effects of Shuxuetong injection on coronary microcirculation and serum ICAM-1,TNF-α and hs-CRP levels in patients with acute ST-segment elevation myocardial infarction after PCI. Acad. J. Shanghai Univ. Traditional Chin. Med. 35, 7–13. doi:10.16306/j.1008-861x.2021.05.002
Marinescu, M. A., Löffler, A. I., Ouellette, M., Smith, L., Kramer, C. M., and Bourque, J. M. (2015). Coronary microvascular dysfunction, microvascular angina, and treatment strategies. JACC Cardiovasc Imaging 8, 210–220. doi:10.1016/j.jcmg.2014.12.008
Marroquin, O. C., Kip, K. E., Mulukutla, S. R., Ridker, P. M., Pepine, C. J., Tjandrawan, T., et al. (2005). Inflammation, endothelial cell activation, and coronary microvascular dysfunction in women with chest pain and no obstructive coronary artery disease. Am. Heart J. 150, 109–115. doi:10.1016/j.ahj.2004.08.003
Meng, C., Zhuo, X. Q., Xu, G. H., and Liu, J. L. (2014). Protection of salvianolate against atherosclerosis via regulating the inflammation in rats. J. Huazhong Univ. Sci. Technol. Med. Sci. 34, 646–651. doi:10.1007/s11596-014-1331-z
Meng, X. L. (2018). Clinical study of Yixin Tongluo capsule in the treatment of 60 cases of coronary microcirculation. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 16, 2069–2071. doi:10.12102/j.issn.1672-1349.2018.14.037
Mileva, N., Nagumo, S., Mizukami, T., Sonck, J., Berry, C., Gallinoro, E., et al. (2022). Prevalence of coronary microvascular disease and coronary vasospasm in patients with nonobstructive coronary artery disease: Systematic review and meta-analysise023207. J. Am. Heart Assoc. 11. doi:10.1161/JAHA.121.023207
Moreau, P., D'uscio, L. V., and Lüscher, T. F. (1998). Structure and reactivity of small arteries in aging. Cardiovasc Res. 37, 247–253. doi:10.1016/s0008-6363(97)00225-3
Mumma, B., and Flacke, N. (2015). Current diagnostic and therapeutic strategies in microvascular angina. Curr. Emerg. Hosp. Med. Rep. 3, 30–37. doi:10.1007/s40138-014-0059-1
Murthy, V. L., Naya, M., Foster, C. R., Gaber, M., Hainer, J., Klein, J., et al. (2012). Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 126, 1858–1868. doi:10.1161/CIRCULATIONAHA.112.120402
Murthy, V. L., Naya, M., Taqueti, V. R., Foster, C. R., Gaber, M., Hainer, J., et al. (2014). Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 129, 2518–2527. doi:10.1161/CIRCULATIONAHA.113.008507
Niccoli, G., Scalone, G., Lerman, A., and Crea, F. (2016). Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 37, 1024–1033. doi:10.1093/eurheartj/ehv484
Oikonomou, E., Mourouzis, K., Vogiatzi, G., Siasos, G., Deftereos, S., Papaioannou, S., et al. (2018). Coronary microcirculation and the No-reflow phenomenon. Curr. Pharm. Des. 24, 2934–2942. doi:10.2174/1381612824666180911122230
Padro, T., Manfrini, O., Bugiardini, R., Canty, J., Cenko, E., De Luca, G., et al. (2020). ESC Working Group on Coronary Pathophysiology and Microcirculation position paper on 'coronary microvascular dysfunction in cardiovascular disease'. Cardiovasc Res. 116, 741–755. doi:10.1093/cvr/cvaa003
Peng, J. X., and Yao, Z. P. (2019). Clinical observation of Huayu Fuyuan capsule for coronary microvascular disease angina pectoris. Yunnan J. Traditional Chin. Med. Materia Medica 40, 32–34. doi:10.16254/j.cnki.53-1120/r.2019.10.012
Petersen, J. W., Johnson, B. D., Kip, K. E., Anderson, R. D., Handberg, E. M., Sharaf, B., et al. (2014). TIMI frame count and adverse events in women with No obstructive coronary disease: A pilot study from the NHLBI-sponsored women's ischemia syndrome evaluation (WISE). Plos One 9, e96630. doi:10.1371/journal.pone.0096630
Pitkänen, O. P., Nuutila, P., Raitakari, O. T., Rönnemaa, T., Koskinen, P. J., Iida, H., et al. (1998). Coronary flow reserve is reduced in young men with IDDM. Diabetes 47, 248–254. doi:10.2337/diab.47.2.248
Qin, H. F., Liu, X. C., Xing, D. M., and Zhang, L. T. (2017). Clinical observation of Shexiang Baoxin Pill in the treatment of microvascular angina pectoris. J. Med. Forum 38, 147–148.
Qiu, C. P., Xu, M. X., Hao, R. R., Zhang, M. X., Zhuang, P. W., Cui, G. Z., et al. (2017). Protective effects of Salvianolic acid on myocardial ischemic injury of rats from the aspect of inhibiting inflammatory reaction. Chin. J. Clin. Pharmacol. 33, 794–797. doi:10.13699/j.cnki.1001-6821.2017.09.007
Qiu, Z. C., Deng, Y., Chen, Y. T., Zhang, J. Y., Liu, G. B., and Yuan, Y. Q. (2021). Observation on the curative effect of Yinxing Mihuan oral solution in the treatment of microvascular angina pectoris. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 19, 3956–3958. doi:10.12102/j.issn.1672-1349.2021.22.026
Qu, Z. Q., Lin, X. Q., He, X. R., Zhou, D. H., Zhao, Y. F., and Tang, Y. (2016). Effect analysis of tanshinone IIA sulfonate sodium on the coronary artery hemodynamics of patients with chronic heart failure. Clin. J. Chin. Med. 8, 16–17+19. doi:10.3969/j.issn.1674-7860.2016.06.008
Reeh, J., Therming, C. B., Heitmann, M., Højberg, S., Sørum, C., Bech, J., et al. (2019). Prediction of obstructive coronary artery disease and prognosis in patients with suspected stable angina. Eur. Heart J. 40, 1426–1435. doi:10.1093/eurheartj/ehy806
Ren, J., Li, T. T., and Guo, W. J. (2019). Relieving effect of Danqi Tongmai capsule on impairment of coronary microcirculation in patients with STEMI after PCI. Chin. J. Evidence-Based Cardiovasc. Med. 11, 1233–1235. doi:10.3969/j.issn.1674-4055.2019.10.20
Ren, Y. C., Zhao, Y. F., Zhang, X. L., Wang, S., Dong, J. J., and Yang, Y. (2018). Clinical observation of Xinnaoning capsule in the treatment of cardiac syndrome X patients with anxiety state. J. China Prescr. Drug 16, 12–13.
Rizzoni, D., Palombo, C., Porteri, E., Muiesan, M. L., Kozàkovà, M., La Canna, G., et al. (2003). Relationships between coronary flow vasodilator capacity and small artery remodelling in hypertensive patients. J. Hypertens. 21, 625–631. doi:10.1097/00004872-200303000-00030
Sara, J. D., Widmer, R. J., Matsuzawa, Y., Lennon, R. J., Lerman, L. O., and Lerman, A. (2015). Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv. 8, 1445–1453. doi:10.1016/j.jcin.2015.06.017
Scarabelli, T., Stephanou, A., Rayment, N., Pasini, E., Comini, L., Curello, S., et al. (2001). Apoptosis of endothelial cells precedes myocyte cell apoptosis in ischemia/reperfusion injury. Circulation 104, 253–256. doi:10.1161/01.cir.104.3.253
Shah, N. R., Cheezum, M. K., Veeranna, V., Horgan, S. J., Taqueti, V. R., Murthy, V. L., et al. (2017). Ranolazine in symptomatic diabetic patients without obstructive coronary artery disease: Impact on microvascular and diastolic function. J. Am. Heart Assoc. 6, e005027. doi:10.1161/JAHA.116.005027
Shen, P., Chen, J., and Pan, M. (2018). The protective effects of total paeony glycoside on ischemia/reperfusion injury in H9C2 cells via inhibition of the PI3K/Akt signaling pathway. Mol. Med. Rep. 18, 3332–3340. doi:10.3892/mmr.2018.9335
Shen, X. (2021). Effect of Qishen capsule combined with Nicorandil on elderly patients with qi deficiency and blood stasis syndrome of microvascular angina pectoris. Med. J. Chin. People's Health 33, 62–64. doi:10.3969/j.issn.1672-0369.2021.08.025
Shi, L. C., and Cui, J. K. (2019). Clinical observation on Zhishi Xiebai Guizhi decoction for microvascular angina pectoris. Chin. J. Traditional Med. Sci. Technol. 26, 560–562.
Song, Q., Zhang, Y., Han, X., Zhang, Y., Zhang, X., Gao, Y., et al. (2019). Potential mechanisms underlying the protective effects of salvianic acid A against atherosclerosis in vivo and vitro. Biomed. Pharmacother. 109, 945–956. doi:10.1016/j.biopha.2018.10.147
Su, T. S., and Luo, J. H. (2014). Clinical observation of Tongmai Zhuyu decoction for cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 12, 263–264. doi:10.3969/j.issn.1672-1349.2014.03.00
Sucato, V., Evola, S., Novo, G., Bellante, N., Andolina, G., and Novo, S. (2017). [Coronary microvascular dysfunction: Past, present, and future of an evolving disease]. G. Ital. Cardiol. (Rome) 18, 837–844. doi:10.1714/2815.28467
Sun, M. Q., and Wu, L. H. (2012). Clinical Study on Ginkgo Damo injection in treating cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 10, 32–33. doi:10.3736/jcim20120406
Sun, Q. L. (2021). Clinical effect of Shexiang Baoxin pill on patients with hyperlipidemia and cardiac syndrome X. Guide China Med. 19, 134–135. doi:10.3969/j.issn.1672-1349.2014.03.00
Sun, Y. Y., Guo, M. S., Zhao, X. G., and Guo, W. Q. (2007). Shenwu Guanxin granule in the treatment of 34 cases of cardiac syndrome X. Jiangxi J. Traditional Chin. Med. 11, 21–22.
Taqueti, V. R., and Di Carli, M. F. (2018). Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2625–2641. doi:10.1016/j.jacc.2018.09.042
Taqueti, V. R., Hachamovitch, R., Murthy, V. L., Naya, M., Foster, C. R., Hainer, J., et al. (2015). Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 131, 19–27. doi:10.1161/CIRCULATIONAHA.114.011939
Taqueti, V. R., Shaw, L. J., Cook, N. R., Murthy, V. L., Shah, N. R., Foster, C. R., et al. (2017). Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve, not obstructive disease. Circulation 135, 566–577. doi:10.1161/CIRCULATIONAHA.116.023266
Taqueti, V. R., Solomon, S. D., Shah, A. M., Desai, A. S., Groarke, J. D., Osborne, M. T., et al. (2018). Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur. Heart J. 39, 840–849. doi:10.1093/eurheartj/ehx721
Task Force, M., Montalescot, G., Sechtem, U., Achenbach, S., Andreotti, F., Arden, C., et al. (2013). 2013 ESC guidelines on the management of stable coronary artery disease: The task Force on the management of stable coronary artery disease of the European society of Cardiology. Eur. Heart J. 34, 2949–3003. doi:10.1093/eurheartj/eht296
Tian, X. T., Liu, N., and Li, C. (2015). Clinical observation on yiqi huoxue for cardiac syndrome X. J. Shandong Med. Coll. 37, 1–3. doi:10.3969/j.issn.1674-0947.2015.01.001
Tjoe, B., Barsky, L., Wei, J., Samuels, B., Azarbal, B., Merz, C. N. B., et al. (2021). Coronary microvascular dysfunction: Considerations for diagnosis and treatment. Cleve Clin. J. Med. 88, 561–571. doi:10.3949/ccjm.88a.20140
Villano, A., Di Franco, A., Nerla, R., Sestito, A., Tarzia, P., Lamendola, P., et al. (2013). Effects of ivabradine and ranolazine in patients with microvascular angina pectoris. Am. J. Cardiol. 112, 8–13. doi:10.1016/j.amjcard.2013.02.045
Vink, C. E. M., Van De Hoef, T. P., Götte, M. J. W., Eringa, E. C., and Appelman, Y. (2021). Reduced microvascular blood volume as a driver of coronary microvascular disease in patients with non-obstructive coronary artery disease: Rationale and design of the MICORDIS study. Front. Cardiovasc Med. 8, 730810. doi:10.3389/fcvm.2021.730810
Wang, C. G., and Li, Q. (2022). Clinical observation of Yindan Xinnaotong soft capsule combined with nicorandil in the treatment of microvascular angina pectoris. J. Pract. Traditional Chin. Med. 38, 50–52.
Wang, C. Y., and Wang, Y. X. (2013). Efficacy of safflower yellow injection in the treatment of cardiac X syndrome and its effect on hs-CRP. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 12, 1459–1460. doi:10.3969/j.issn.1672-1349.2013.12.025
Wang, H., Zheng, B., Che, K., Han, X., Li, L., Wang, H., et al. (2021a). Protective effects of safranal on hypoxia/reoxygenation-induced injury in H9c2 cardiac myoblasts via the PI3K/AKT/GSK3β signaling pathway. Exp. Ther. Med. 22, 1400. doi:10.3892/etm.2021.10836
Wang, H. H., and Liu, X. C. (2013). Influence of Tanshinone IIA sulfonate injection on inflammatory factors for coronary heart disease heart failure and BNP. Clin. J. Chin. Med. 5, 89–90. doi:10.3969/j.issn.1674-7860.2013.24.047
Wang, M. X., Shan, Y. W., Sun, W. X., Han, J., Tong, H. Q., Fan, M. L., et al. (2021b). Effects of Shexiang Baoxin pill for coronary microvascular function: A systematic review and meta-analysis. Front. Pharmacol. 12, 751050. doi:10.3389/fphar.2021.751050
Wang, X., Gao, A., Jiao, Y., Zhao, Y., and Yang, X. (2018). Antitumor effect and molecular mechanism of antioxidant polysaccharides from Salvia miltiorrhiza Bunge in human colorectal carcinoma LoVo cells. Int. J. Biol. Macromol. 108, 625–634. doi:10.1016/j.ijbiomac.2017.12.006
Wang, X. L., Mao, J. Y., Wang, H. H., Yu, D. L., Wang, Q., Zhang, Y., et al. (2009). Clinical study on Liqi Huatan Huoxue formula for cardiac syndrome X. Shanghai J. Traditional Chin. Med. 43, 33–35. doi:10.1134/s0026893309040049
Wang, Y., Ren, Y., Xing, L., Dai, X., Liu, S., Yu, B., et al. (2016). Endothelium-dependent vasodilation effects of Panax notoginseng and its main components are mediated by nitric oxide and cyclooxygenase pathways. Exp. Ther. Med. 12, 3998–4006. doi:10.3892/etm.2016.3890
Wang, Y. L., Li, X. Q., Wang, X. F., and Luo, M. (2010). Clinical study on ginkgo damole for coronary slow blood flow. J. Pract. Med. 26, 3028–3030. doi:10.7661/CJIM.2013.08.1138
Wang, Y. X. (2016). Clincial observation of Tongxinluo capsule on the treatment of female microvascular angina. J. Liaoning Univ. Traditional Chin. Med. 18, 175–176. doi:10.13194/j.issn.1673-842x.2016.03.061
Wang, Z. Q., Li, Y., and Xiao, W. L. (2014). Effect of Tongxinluo capsule on the vascular endothelial function in patients with coronary slow flow. China J. Traditional Chin. Med. Pharm. 29, 2034–2036.
Wang, Z., Xin, D., Peng, K., Wang, Q., and Li, D. (2019). Effect of Yindan Xinnaotong soft capsule on coronary microcirculation function in microvascular angina patients with slow-flow coronary artery. Chin. J. Integr. Traditional West. Med. 39, 418–422. doi:10.7661/j.cjim.20180907.177
Wei, H. S., Gao, H. W., Wang, L. L., Wang, C. P., Niu, Z. S., Wang, Q. M., et al. (2010). Study on the treatment of slow coronary blood flow with Buchang Naoxintong capsule. Pract. J. Cardiac Cereb. Pneumal Vasc. Dis. 18, 1445–1446.
Wei, Y. (2018). Clinical study of compound Danshen dripping pills in adjuvant treatment of patients with cardiac syndrome X. Contemp. Med. 24, 100–102. doi:10.3969/j.issn.1009-4393.2018.13.044
Wen, Y. N., Ma, J., Shi, F. F., Luo, W. P., Li, R., and Wang, Y. G. (2016). Therapeutic effect of Bushen Huoxue Granules for postmenopausal microvascular angina pectoris and its effect on serum NO and ET-1. Shaanxi J. Traditional Chin. Med. 37, 987–988. doi:10.3969/j.issn.1000-7369.2016.08.022
Wu, C. Y., Wang, G. M., and Sun, Z. J. G. (2019). Effect of Shexiang Baoxin pill combined with nicorandil in the treatment of patients with coronary slow flow angina. Shanghai Med. Pharm. J. 40, 26–28+43.
Wu, L. F., Wang, Z. M., Hao, K. Q., Li, W. Y., Jia, B. T., Jia, F., et al. (2021). Chemical constituents and pharmacological effects of paeoniae radix rubra:A review. Chin. J. Exp. Traditional Med. Formulae 27, 198–206. doi:10.13422/j.cnki.syfjx.20211770
Wu, L. H., Sun, J. L., Wang, C. Y., Liu, Y. X., Shi, S. F., and Liu, F. (2010). Clinical study on Shuxuening injection in treating cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 8, 652–653. doi:10.3736/jcim20101001
Wu, Q. F., Wang, D. Y., Yan, G. L., Wang, H. H., and Liu, Z. J. (2016). Clinical observation of Yiqi Tongluo recipe combined with routine Western medicines in the treatment of coronary slow flow phenomenon. Shanghai J. Traditional Chin. Med. 50, 38–41. doi:10.16305/j.1007-1334.2016.11.012
Wu, Y. H., Li, N., and Xu, B. H. (2018). Clinical study on Yuxintong Capsules combined with nicorandil in treatment of microvascular angina. Drugs & Clin. 33, 2787–2790. doi:10.7501/j.issn.1674-5515.2018.11.005
Wu, Y. H., Wu, L. H., and Shi, Z. (2013). Clinical observation on cardiac syndrome X treated with Sulfotanshinone Sodium injection. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 11, 909–910. doi:10.3969/j.issn.1672-1349.2013.08.006
Xiang, L., Zhang, Q. Y., Zhao, Q. M., Qin, L. P., and Gong, W. (2022). Research progress on chemical constituents, pharmacological effects and clinical applications of Astragali Radix-Angelicae Sinensis Radix. Chin. Traditional Herb. Drugs 53, 2196–2213. doi:10.7501/j.issn.0253-2670.2022.07.030
Xie, L., Wu, Y., Fan, Z., Liu, Y., and Zeng, J. (2016). Astragalus polysaccharide protects human cardiac microvascular endothelial cells from hypoxia/reoxygenation injury: The role of PI3K/AKT, Bax/Bcl-2 and caspase-3. Mol. Med. Rep. 14, 904–910. doi:10.3892/mmr.2016.5296
Xu, T., Wu, X., Chen, Q., Zhu, S., Liu, Y., Pan, D., et al. (2014). The anti-apoptotic and cardioprotective effects of salvianolic acid a on rat cardiomyocytes following ischemia/reperfusion by DUSP-mediated regulation of the ERK1/2/JNK pathway. PLoS One 9, e102292. doi:10.1371/journal.pone.0102292
Xuan, J., Zhang, J., Li, Z. Y., and Bian, Y. (2020). Effect of Yinxing Mihuan oral solution combined with Nicorandil on coronary microcirculation disorder after angina pectoris and changes of NO,Ang Ⅱ,ET-1 and CRP. J. Liaoning Univ. Traditional Chin. Med. 22, 141–144. doi:10.13194/j.issn.1673-842x.2020.09.034
Xue, J. G., Lan, D. H., Zhao, F. R., Wang, Y. Q., Wang, X. L., and Zhou, H. (2014). Clinical observation of Wenyang Huoxue decoction for coronary slow flow. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 12, 1289–1291. doi:10.3969/j.issn.1672-1349.2014.11.001
Yan, W. L., Gao, P., and Lu, H. (2018). Clinical effect of Nicorandil combined with Qishen capsule on patients with microangiopathy anginapectoris. Clin. J. Med. Officers 46, 1153–1155+1159. doi:10.16680/j.1671-3826.2018.10.12
Yang, L. Y., and Zhang, H. L. (2013). Therapeutic effect of Salvia miltiorrhiza ligustrazine Hydrochloride injection on cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 11, 616–617.
Ye, J. X., Wang, R. Y., Wang, M., Fu, J. H., Zhang, Q., Sun, G. B., et al. (2021). Hydroxysafflor yellow A ameliorates myocardial ischemia/reperfusion injury by suppressing calcium overload and apoptosis. Oxidative Med. Cell. Longev. 2021, 6643615. doi:10.1155/2021/6643615
Yin, A. W., Shen, L. H., and He, B. (2021). [Research progress on the mechanisms of coronary microvascular endothelial cell dysfunction]. Zhonghua Xin Xue Guan Bing Za Zhi 49, 90–95. doi:10.3760/cma.j.cn112148-20200310-00183
Yin, B., Hou, X. W., and Lu, M. L. (2019). Astragaloside IV attenuates myocardial ischemia/reperfusion injury in rats via inhibition of calcium-sensing receptor-mediated apoptotic signaling pathways. Acta Pharmacol. Sin. 40, 599–607. doi:10.1038/s41401-018-0082-y
Yuan, W. (2019). Protective effects of pretreatment and posttreatment with Danhong Injection on myocardial ischemia reperfusion injury of rabbits. Mod. J. Integr. Traditional Chin. West. Med. 28, 1834–1837+1842. doi:10.3969/j.issn.1008-8849.2019.17.003
Yue, L. M., Chang, H., and Yang, Z. C. (2018). Influence of ligustrazine on vascular endothelial function in patients with coronary slow flow. Chin. J. Evidence-Based Cardiovasc. Med. 10, 193–195. doi:10.3969/j.issn.1674-4055.2018.02.18
Zhang, G. P., and Xie, H. N. (2020). Clinical observation of Lemai Pill in treating cardiac syndrome X. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 18, 301–302. doi:10.12102/j.issn.1672-1349.2020.02.027
Zhang, H. B., Liu, F., Ma, J. H., Zhao, J. H., and Zhang, J. (2021). Clinical efficacy of Qiliqiangxin capsule combined with Nicorandil in the treatment of coronary slow flow. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 19, 1353–1355. doi:10.12102/j.issn.1672-1349.2021.08.026
Zhang, L. M., and Ma, P. F. (2021). A study on the pharmacology and clinical application of Conioselinum anthriscoides 'Chuanxiong' in treating cardiovascular diseases. Clin. J. Chin. Med. 13, 18–20. doi:10.3969/j.issn.1674-7860.2021.01.006
Zhang, L. W. (2019). Study on effect of Shexiang Baoxin pill on microcirculation disorder after coronary intervention. China Pract. Med. 14, 70–72. doi:10.14163/j.cnki.11-5547/r.2019.22.036
Zhang, P. K. (2021). Effect of Xuefu Zhuyu decoction on cardiac syndrome X and its influence on endothelial function. Guangming J. Chin. Med. 36, 1201–1203. doi:10.3969/j.issn.1003-8914.2021.08.004
Zhang, W. N., Hu, Z. T., Gao, X. D., Peng, X. M., and Zhang, X. G. (2013a). Curative effect of Shexiang Baoxin pill in patients with cardiac syndrome X complicating hyperlipidemia. Chin. J. Evidence-Based Cardiovasc. Med. 5, 285–287. doi:10.3969/j.1674-4055.2013.03.025
Zhang, Y., Wei, L., Sun, D., Cao, F., Gao, H., Zhao, L., et al. (2010). Tanshinone IIA pretreatment protects myocardium against ischaemia/reperfusion injury through the phosphatidylinositol 3-kinase/Akt-dependent pathway in diabetic rats. Diabetes Obes. Metab. 12, 316–322. doi:10.1111/j.1463-1326.2009.01166.x
Zhang, Y., Chen, Y. D., Fu, X. H., Chen, W. Q., Li, D. D., Gu, X. S., et al. (2017). Chinese expert consensus on the diagnosis and treatment of coronary microvascular disease. Chin. Circulation J. 32, 421–430. doi:10.3969/j.issn.1000-3614.2017.05.003
Zhang, Y. F., Chen, Y. Q., Chen, J., Liu, M. L., and Ma, J. (2012). Modified Erxian decoction treatment of post-menopause patients with microvascular angina. J. Liaoning Univ. Traditional Chin. Med. 14, 96–98. doi:10.13194/j.jlunivtcm.2012.10.98.zhangyf.080
Zhang, Y. H., and Chen, X. J. (2020). Effect of compound danshen dripping pills combined with tirofiban in improving coronary slow flow and microcirculation after elective PCI for coronary heart disease. Anhui Med. Pharm. J. 24, 1639–1642.
Zhang, Y. L., Zhu, X. M., and Yuan, X. Q. (2013b). Clinical observation of Qishen capsule in treating microvascular angina pectoris. Chin. J. Integr. Traditional West. Med. 33, 1138–1139. doi:10.7661/CJIM.2013.08.1138
Zheng, R. G., Guo, Z. P., and Wu, C. T. (2019). Clinical effect of Danlou tablets on coronary microcirculation disturbance in patients with acute myocardial infarction after percutaneous coronary intervention. Chin. J. Clin. Ration. Drug Use 12, 3–4+7. doi:10.15887/j.cnki.13-1389/r.2019.15.002
Zhong, L., Zhuang, J., Jin, Z., Chen, Y., and Chen, B. (2020). Effect of Chinese medicine for promoting blood circulation on microvascular angina: A systematic review and meta-analysis. Am. J. Emerg. Med. 38, 2681–2692. doi:10.1016/j.ajem.2020.07.072
Zhou, L. (2021). Observation on the effect of Wuling capsule in treating cardiac syndrome X with anxiety and depression. J. Shantou Univ. Med. Coll. 34, 150–152. doi:10.13401/j.cnki.jsumc.2021.03.006
Zhou, S. P. (2018). Therapeutic effect of Yiqi Huoxue Huatan formula granule on microvascular angina pectoris. Med. Innovation China 15, 65–69. doi:10.3969/j.issn.1674-4985.2018.26.016
Zhu, H. G., and Chen, H. (2014). Therapeutic effect of Yixinshu capsule on cardiac syndrome X and its effect on vascular endothelial function. Chin. J. Integr. Med. Cardio-Cerebrovascular Dis. 12, 680–682. doi:10.3696/j.issn.1672-1349.2014.06.018
Zhu, W. (2019). Efficacy of Xuefu Zhuyu decoction for microvascular angina pectoris and its effect on vascular endothelial function. Shaanxi J. Traditional Chin. Med. 40, 46–48. doi:10.3969/j.issn.1000-7369.2019.01.014
Zhuang, J. Q., Liu, S. L., Cai, H. R., Dai, X. Z., Chen, Y. H., Jin, Z. L., et al. (2020). Efficacy and safety of guhong injection for treating coronary microvascular disease: study protocol for a randomized controlled trial. Trials 21, 75. doi:10.1186/s13063-019-3990-3
Zou, Z. Y., Zhou, Q. Q., Wu, L. E., Rao, L. L., Chen, S. S., and Luo, Q. L. (2016). Effects of Ginkgo Biloba capsule combined with isosorbide dinitrate tablets on serum cTnI, BNP and blood lipid levels in patients with cardiac syndrome X. J. Hubei Univ. Chin. Med. 18, 21–23. doi:10.3969/j.issn.1008-987x.2016.03.07
Keywords: traditional Chinese medicine, clinical evidence, coronary microvascular disease, coronary microvascular dysfunction, coronary flow reserve, potential mechanism
Citation: Yang Z, Lin S, Liu Y, Ren Q, Ge Z, Wang C, Bi Y, Wang X and Mao J (2022) Traditional chinese medicine in coronary microvascular disease. Front. Pharmacol. 13:929159. doi: 10.3389/fphar.2022.929159
Received: 26 April 2022; Accepted: 27 June 2022;
Published: 08 August 2022.
Edited by:
Jaw-Wen Chen, Taipei Veterans General Hospital, TaiwanReviewed by:
Feng-Yen Lin, Taipei Medical University, TaiwanNathan Andrew Holland, Texas Tech University Health Sciences Center El Paso, United States
Copyright © 2022 Yang, Lin, Liu, Ren, Ge, Wang, Bi, Wang and Mao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianliang Wang, eGx3YW5nMTk4MUAxMjYuY29t; Jingyuan Mao, anltYW9AMTI2LmNvbQ==
†These authors have contributed equally to this work
 Zhihua Yang
Zhihua Yang Shanshan Lin
Shanshan Lin Yangxi Liu1
Yangxi Liu1 Xianliang Wang
Xianliang Wang