
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pharmacol. , 05 October 2022
Sec. Ethnopharmacology
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.928106
This article is part of the Research Topic Ethnopharmacological Responses to the Coronavirus Disease 2019 (COVID-19) Pandemic: Volume II View all 4 articles
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that causes COVID-19 (coronavirus disease 2019), the respiratory illness responsible for the ongoing COVID-19 pandemic. As at June 2022, increasing numbers of newly diagnosed COVID-19-associated pneumonia cases worldwide have attracted close attention from the international community. The present review analyzes and summarizes the treatment of COVID-19 with traditional Chinese medicine (TCM). A systematic analysis of the efficacies and benefits of TCM for the treatment of COVID-19 was performed, and the mechanisms underlying such treatment are summarized. This analysis of the literature highlights the potential of TCM to prevent and treat COVID-19 via antiviral, anti-inflammatory and immunomodulatory activities, with evidence showing that many TCM components act upon multiple targets and pathways. Famous TCM formulas include Qing-Fei-Pai-Du-Tang (QFPDT), Lianhuaqingwen Capsule (LHC), Taiwan Chingguan Yihau (NRICM101), and Jing Si herbal drink (JSHD). In particular, the botanical preparation NRICM101 was developed in 2020 for use in viral respiratory tract infections and is recommended for treating non-severe and mild COVID-19 infections. NRICM101 has been adopted for use in Taiwan for the clinical treatment of COVID-19. The common components and active ingredients of 10 TCM preparations have been analyzed for the most promising substances. This review aims to provide reliable evidence demonstrating the therapeutic efficacy of TCM substances in support of their further development against novel coronavirus infectious diseases in Taiwan.
Since its emergence in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, COVID-19) has had devastating effects worldwide, with more than 362 million confirmed cases and 5.62 million deaths globally by early February 2022 (Wu et al., 2020a). As at 14 June 2022, epidemic real-time data had recorded 300,501 COVID-19 diagnoses and 4,403 deaths in Taiwan, involving 28,192 immigrants and 2,975,309 native cases (MOHW, 2022). The process of COVID-19 infection involves angiotensin-converting enzyme 2 (ACE2), transmembrane protease serine-2 (TMPRSS2) and 3CL protease (3CLpro) (Hoffmann et al., 2020; Hsu et al., 2020). By binding to the ACE2 receptor, the SARS-CoV-2 spike protein (S protein) drives viral reproduction (Ni et al., 2020), entering host cells via the major host protease, TMPRSS2 (Shang et al., 2020), while 3CLpro is the main protease of SARS-CoV-2 and responsible for viral replication, so is considered to be an important drug target (Mody et al., 2021; Niesor et al., 2021; Wang and Yang, 2021a; Wang et al., 2021).
The clinical symptoms of COVID-19 are most commonly fever, cough, fatigue, myalgia, diarrhea and complications arising from multiple organ damage (Zaim et al., 2020). None of these symptoms are as yet treatable by small-molecule antivirals. Effective prevention and treatment measures are critical for the control of COVID-19 (Jiang et al., 2020).
Traditional Chinese medicine (TCM) philosophy categorizes COVID-19 as an “epidemic disease” caused by an epidemic evil with dampness and heat, termed Li-Qi in Chinese. After invading the human body, Li-Qi enters the lung and induces stagnation of Lung-Qi (vital essence of the lung, governing breathing and qi of the body), then to breathing difficulties, phlegm-heat accumulation and blockage, and finally bring out the dead Yin and the dead Yang. According to TCM treatment philosophy, dampness should be eliminated first, then heat should be cleared away, to restore normal bodily function (Wang et al., 2020a; Wu et al., 2021a). Its pathogenesis is characterized as “wet, heat, poison, stasis, deficiency,” accompanied by lesions manifesting mostly in the lung, spleen and stomach. TCM has accumulated much experience in dealing with this sort of disease over the centuries. In 2020, guidance issued by Taiwan’s Ministry of Health and Welfare Department of Disease Control, “New Coronavirus Disease (New Coronary Pneumonia; NCP) TCM Consultation and Staged Treatment Guidelines,” was intended to slow the development of COVID-19, block its progression to severe disease, and accelerate recovery, while simultaneously reducing disease recurrence, as well as the sequelae of severe pulmonary fibrosis and other complications (George et al., 2020). The existing literature has reviewed COVID-19 etiology, pathogenesis and syndrome characteristics as according to TCM theory, with documented evidence of therapeutic applications (Yang et al., 2020a; Qiu et al., 2020; Wang and Yang, 2021b). In contrast, our review focuses mainly on the use of TCM prescriptions and active ingredients of NRICM101, employing a literature-mining approach to analyze experimental research and clinical applications.
TCM has accumulated a wealth of experience regarding infectious disease. According to TCM theory, this epidemic belongs to the category of “pestilence,” with the pathological characteristics of “dampness, heat, toxin, deficiency, and stasis.” Two thousand years ago, TCM writings first documented the “Yi Bing” concept; an infective disease that differed from the common cold, with the capacity of easily becoming an epidemic. Much later, the Han Dynasty elaborated upon the dialectical relationship and treatment theory of exopathogenic wind-heat diseases (Du et al., 2020). Chinese medicine refers to wind-cold and wind-heat. Wind, cold, and heat are three common pathogens that can enter the human body from the outside. Chills, stiffness (especially in the neck), headache, and white or clear phlegm are signs of wind-chill; a sore throat, feeling warm and/or agitated (with or without fever), yellow or green phlegm, and aversion to heat are some of the signs of wind-heat (Qi and Tang, 2021). Many Chinese herbal formulas have emerged from these theoretical foundations. TCM theories relating to infectious diseases were further developed during the Tang, Song and Yuan dynasties. By the 17th century, China had published the world’s first systematic study of acute epidemic disease in the Treatise on Exogenous Febrile Disease, detailing the etiology, pathogenesis, syndrome and treatment of plague (Xu et al., 2019; Luo et al., 2020). A critical feature of TCM is that this system of medicine is able to apply the same method of treatment for patients afflicted with different diseases, who share the same syndrome. Arguably, the theoretical foundations of TCM mean that this way of treatment is an effective treatment for NCP.
Most TCM prescriptions for COVID-19 are based on heat-clearing and detoxification (Yan et al., 2020). Based on TCM theory, COVID-19 is a “warm-damp epidemic,” with a pathogenesis that is characterized by the external invasion of epidemic toxins and evil affecting the lungs and stomach. Patients with symptoms such as fever due to warm-damp epidemic poisoning should be treated with substances that clear heat, detoxify and dredge the collaterals, dispel cold and dehumidify, so the appropriate TCM formulas are those that clear heat, detoxify dampness and relieve asthma as the core treatment method. The pathogenesis of warm-damp epidemic poisoning is mostly caused by sitting and lying on the ground when the climate is humid. The spleen can transport water and dampness, which means that the spleen likes warm and dry. If the spleen is healthy, the function of transporting water and dampness is normal, and dampness does not easily cause disease. It may be necessary to take into account changes in syndromes, treat the symptoms, and increase or decrease treatment prescriptions over time.
Importantly, TCM has proven effective against coronavirus pneumonia caused by severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome Coronavirus [MERS-CoV] (Zhang et al., 2020). An early TCM intervention reduces the risk of morbidity and thus mortality (Qiu et al., 2020). With regard to the outbreak of COVID-19, an integrated treatment regimen of Chinese and Western medicine has been associated with significant improvements in symptoms and a shorter disease course, superior control of fever, faster clearance of chest infections and other symptoms, and a significant factor in the promotion of recovery (Yang et al., 2020c; Xing and Liu, 2021). Most TCM prescriptions used in the clinic are based on clearing heat and detoxifying, with remarkable therapeutic effects (Yang et al., 2020c). Heat-clearing and detoxifying Chinese medicines mainly include forsythia, honeysuckle, dandelion, Houttuynia cordata Thumb., purslane, Isatis tinctoria subsp. tinctoria, Oldenlandia herbacea (L.) Roxb., Andrographis paniculata (Burm.f.) Nees and lobelia (Yan et al., 2020). Heat-clearing and detoxifying drugs are used in cases of plague, sore throat, diarrhea due to heat poisoning, cancer, scalding, and epidemic fever (Yan et al., 2020). Our review of recent literature concerning Chinese medicine treatment and clinical research in infectious diseases revealed several prescriptions that are detailed below, all of which exhibit good preventive and control measures, as well as high cure rates. Among several antivirals that have demonstrated the ability to improve and eliminate symptoms of COVID-19 (Ren et al., 2020). Although remdesivir has shown potent antiviral activities, more efficacy assessments are urgently warranted in clinical trials (Beigel, et al., 2020; WHO solidarity trial consortium, 2022). Effective broad-spectrum antiviral drugs are rare because viruses are more diverse than bacteria. Antiviral drugs must enter infected cells and work, often resulting in a number of side effects (Wang and Yang, 2020; Wang and Yang, 2021b; Wang and Yang, 2022). TCM formulas are compound prescriptions that are associated with multi-target effects such as antiviral activities, regulation of immunity, and reduction of the inflammatory response, thereby improving clinical efficacy. TCM formulas that have been adopted in the treatment of mild to moderate COVID-19 cases include Qing-Fei-Pai-Du-Tang, Jinhua Qinggan Capsule, Jing Si Herbal Drink (JSHD) and Taiwan Qingguan Yihau (NRICM101) (Table 1).
QFPDT formula is used in the treatment of NCP. This formula combines the four classics of Xiao Chai Hu Tang, Shegan Ma Huang Tang, Maxing Shigan Tang and Wuling San (Liu et al., 2021c). As this prescription dispels cold, clears heat and reduces dryness, it can effectively relieve several major symptoms associated with NCP, and has a clear curative effect in mild and severe infections. The main target organ of QFPDT is the lung; the second is the spleen. QFPDT helps to balance the immune system and eliminate inflammation by regulating ACE2 and protein co-expression, as well as signaling pathways implicated in disease development (Mehrbod et al., 2020). It is speculated that this formula can behave as an antiviral agent because of its ability to target ribosomal proteins found in viral replication and inhibit interactions with viral mRNA translation and other proteins (Zhong et al., 2020; Liu et al., 2021b). Thus, the antiviral effects of QFPDT are achieved mainly through different mechanisms: 1) Through direct action upon viral replication and autophagy; 2) Regulation of host pathways such as Toll-like receptors (TLRs), RIG-1-like helicases (RLH), AMP-activated protein kinase (AMPK), phosphatidyl inositol-3-kinase/protein kinase B (PI3K/AKT), and extracellular regulated kinase 1/2/mitogen-activated protein kinase (ERK/MAPK) signaling; 3) Promotion of the human defense system through T-cell and B cell functions; and 4) By enhancing the free radical scavenging activity of superoxide dismutase, catalase and glutathione peroxidase (Zhong et al., 2020). According to the literature, Ephedrae Herba and Glycyrrhizae Radix are considered to be very important in the treatment of COVID-19. Glycyrrhizae Radix is the most commonly prescribed treatment for respiratory diseases and the prescription for dyspnea is usually a combination of Ephedrae Herba and Glycyrrhizae Radix (Fu et al., 2013). Interestingly, the Ma Xing Shi Gan decoction, which is widely used in the clinical treatment of COVID-19, consists of ephedra and licorice. QFPDT requires further in vivo studies on the synergy and metabolism of active compounds in order to more comprehensively explain the mechanism of action and provide new ideas and evidence for further research on the use of QFPDT in the treatment of COVID-19.
LHC contains 13 herbs within two TCM prescriptions: Maxing Shigan Tang and Yinqiao San. Maxing Shigan Tang was first referenced by Shanghan Lun, a book dating back to the Han Dynasty, as a treatment for febrile diseases. Bronchitis, pneumonia and early-stage measles infections have all been treated with Maxing Shigan Tang (Ding et al., 2017). Yinqiao San is described in the Qing Dynasty TCM monograph Wenbing Tiaobian as a treatment for “Warm disease” with symptoms of fever, thirst and headache. LHC has proven effective in the treatment of seasonal influenza. Randomized clinical trial evidence has demonstrated significant superiority with LHC over oseltamivir in patients with mild H1N1 infection, with LHC more effectively alleviating fever, cough, sore throat and fatigue, accompanied by shorter durations of illness and viral shedding (Dong et al., 2014). In another clinical trial involving patients with mild H1N1 infection found that LHC provided better symptom relief than oseltamivir, but similar viral clearance rates (Hu et al., 2022). LHC has been widely used in China over the last decade, providing curative evidence in various infections, for example, acute bronchitis, asthma, and chronic obstructive pulmonary disease (COPD) (Ding et al., 2017). LHC has broad-spectrum antiviral, antibacterial and anti-inflammatory functions. The main functions of LHC include the inhibition of virus binding to host cells, inhibiting virus replication and release, reducing the expression levels of chemokines/cytokines (tumor necrosis factor alpha [TNF-α], interleukin [IL]-6, monocyte chemoattractant protein-1 [MCP-1] and C-X-C motif chemokine ligand 10 [CXCL10]), enhancing the immune system and improving symptoms caused by different diseases (Shen and Yin, 2021). In a clinical trial, patients with COVID-19 infection were randomly assigned to receive usual care alone (controls) or in combination with LHC for 14 days (Hu et al., 2022). The recovery rate of the LHC treatment group was significantly higher than that of the control group and no serious adverse events were reported. LHC can be considered to improve clinical symptoms of COVID-19 (Hu et al., 2022). Most LHC adverse reactions occur after the first dose and include gastrointestinal discomfort (73.9%) and skin discomfort (9.6%), experienced largely as nausea, vomiting, diarrhea and rash (Shen and Yin, 2021). Adverse reactions are mostly mild, and monitoring should be strengthened to standardize drug instructions to ensure patient safety. LHC exhibits a broad spectrum of effects on a series of influenza viruses by interfering with both viral and host reactions (Li et al., 2020). For now, although LHC significantly relieves the clinical symptoms of COVID-19 infection, the underlying mechanism of antiviral effects in coronavirus infection, especially SARS-CoV-2, remains elusive.
JSHD, an eight-herb formula developed in Taiwan by Tzu Chi University and Tzu Chi Hospital, has received Ministry of Health and Welfare approval for use as an adjuvant therapeutic for COVID-19 infection. Therapeutic justification for this formula draws upon experience from its treatment of SARS cases in 2003. JSHD contains Yu Jen Cao (Anisomeles indica (L.) Kuntze), Ai Ye (Artemisia argyi H. Lév. and Vaniot), Ju Hua (Chrysanthemum × morifolium (Ramat.) Hemsl.), Gan Cao (Glycyrrhiza uralensis Fisch. ex DC.), Yu Xing Cao (Cynoglossum austroafricanum Hilliard and B.L. Burtt), Mai Men Dong (Ophiopogon japonicus (Thunb.) Ker Gawl.), Zi Su Ye (Perilla frutescens (L.) Britton) and Jie Geng (Platycodon grandiflorus (Jacq.) A.DC.). Clinical evidence continues to grow in support of JSHD as an adjuvant treatment in COVID-19 infection (Shibu et al., 2022). The therapeutic efficacy of JSHD in COVID-19 infection is supported by antiviral activity (blocks ACE2, TMPRSS2 and 3CLpro activities), antioxidative (increases SOD activity) and anti-inflammatory activities (decreases iNOS expression and NF-κB phosphorylation; inhibits the production of NO, TNF-α and IL-6), the ability to suppress immune system overactivation (by reducing macrophages, neutrophils, and white blood cells), and attenuate organ injuries (Lu et al., 2021). JSHD is a potential multi-target drug candidate for the inhibition and treatment of COVID-19, but the current study does not evaluate the interactions of JSHD Chinese herbal components in different pathways or drugs, and no relevant preclinical or clinical literature exists on JSHD. This formula can be considered as an adjunctive therapy for patients with COVID-19. Further rigorously designed studies are needed to prove the efficacy and safety of JSHD against COVID-19 infection.
NRICM101 was developed in 2020 in the Republic of China by the National Institute of Traditional Chinese Medicine to relieve mild and severe cases of infectious pneumonia. NRICM101 is derived from increases or decreases to the dosage of “Mild Symptoms Decoction Pieces” detailed in the National Institute of Traditional Chinese Medicine Guidelines for Clinical Staged Treatment of Novel Coronavirus Diseases. NRICM101 has undergone clinical testing.
NRICM101 is based on “Jing Fangbaidu Powder” described in the Ming Dynasty’s Prescriptions for Taking Lives. The original recipe consists of Nepeta, Fangfeng, Bupleurum, Poria, Platycodon, Chuanxiong, Qianghuo, Duhuo, Citrus aurantium, Licorice, Ginger, and other medicinal materials. Wu Youke’s Plague Theory and Dai Tianzhang’s Guang Plague Theory proposed that “Jing Fangbaidu San” is a useful formula for those who want to sweat and cool down. It is important to relieve the evil heat of the epidemic, and the evil heat must come to an end. When the formulas are placed on the surface of the muscle, if there is no sweat, there will be no way out for evil, so the sweat method is an appropriate method for treating epidemics. Because “disease enters the lung and turns heat” is the main clinical manifestation of COVID-19, the prescription is adjusted: the patient’s condition becomes more like diffuse pneumonia, exhibiting a syndrome of lung heat and phlegm. Peppermint and mulberry leaves are the main constituents; Scutellaria baicalensis Georgi, I. tinctoria subsp, tinctoria and H. cordata Thunb. are used as minister medicines for clearing heat, dispelling lung and detoxification, while Quangualou widens the chest and loosens phlegm, and magnolia reduces qi and relieves asthma. Licorice is used to temper the entire formula (Tsai et al., 2021). NRICM101 was able to obtain sales licenses in Europe and the United States, thanks to the deletion of medicinal materials prohibited by foreign laws and regulations, such as Ephedra sinica Stapf, Asarum sieboldii Miq. (asarum) and Gypsum Fibrosum (gypsum), which allowed NRICM101 to enter the global anti-epidemic drug market; on the other hand, QFPDT contains ephedra, so it cannot be sold in the United States. In addition, gypsum is very effective in treating inflammation, because it is a mineral, it affects quality control, and finally decided to delete it. During the spread of the international new crown pneumonia epidemic, NRICM101 have been sold in the United States, Singapore, Australia, Canada, the United Kingdom, France, Belgium, Luxembourg, South Africa, Thailand and the Philippines and other countries for clinicians and the public to use correctly.
Research into NRICM101 has confirmed multiple target mechanisms, including blocking the COVID-19 spike protein receptor-binding domain from binding with the ACE2 receptor of the host cell and inhibiting virus infections, inhibiting 3CLpro activity and blocking viral replication by the host cell, inhibiting alveolar macrophage secretion of proinflammatory cytokines (TNF-α and IL-6), regulating the generated inflammatory storm, reducing lung damage and reducing the development of pulmonary fibrosis (Tsai et al., 2021). More investigation is needed to explore possible effects and underlying mechanisms of NRICM101, and to determine the optimal composition of herbal ingredients to maximize the effectiveness of this formula. While the ability of NRICM101 to prevent disease progression requires further validation, our experience in Taiwan suggests a multi-targeting and potentially safe, efficacious new drug candidate.
NRICM101 consists of 10 herbs (Table 2). This review discusses the detailed mechanisms of NRICM101 as an adjuvant COVID-19 treatment for future clinical use and experimental reference. The relevant research and mechanisms of all NRICM101 compounds or their active ingredients are described in detail below and summarized in Table 3.
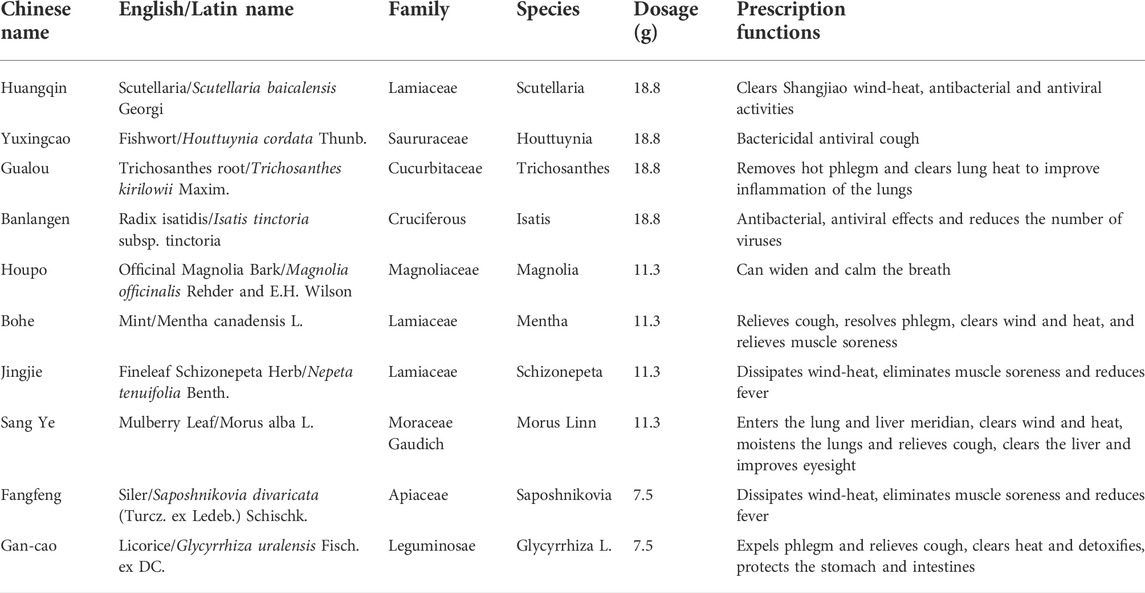
TABLE 2. Overview of TNRICM101 ingredients and the therapeutic efficacies of each ingredient Lin et al. (2007).
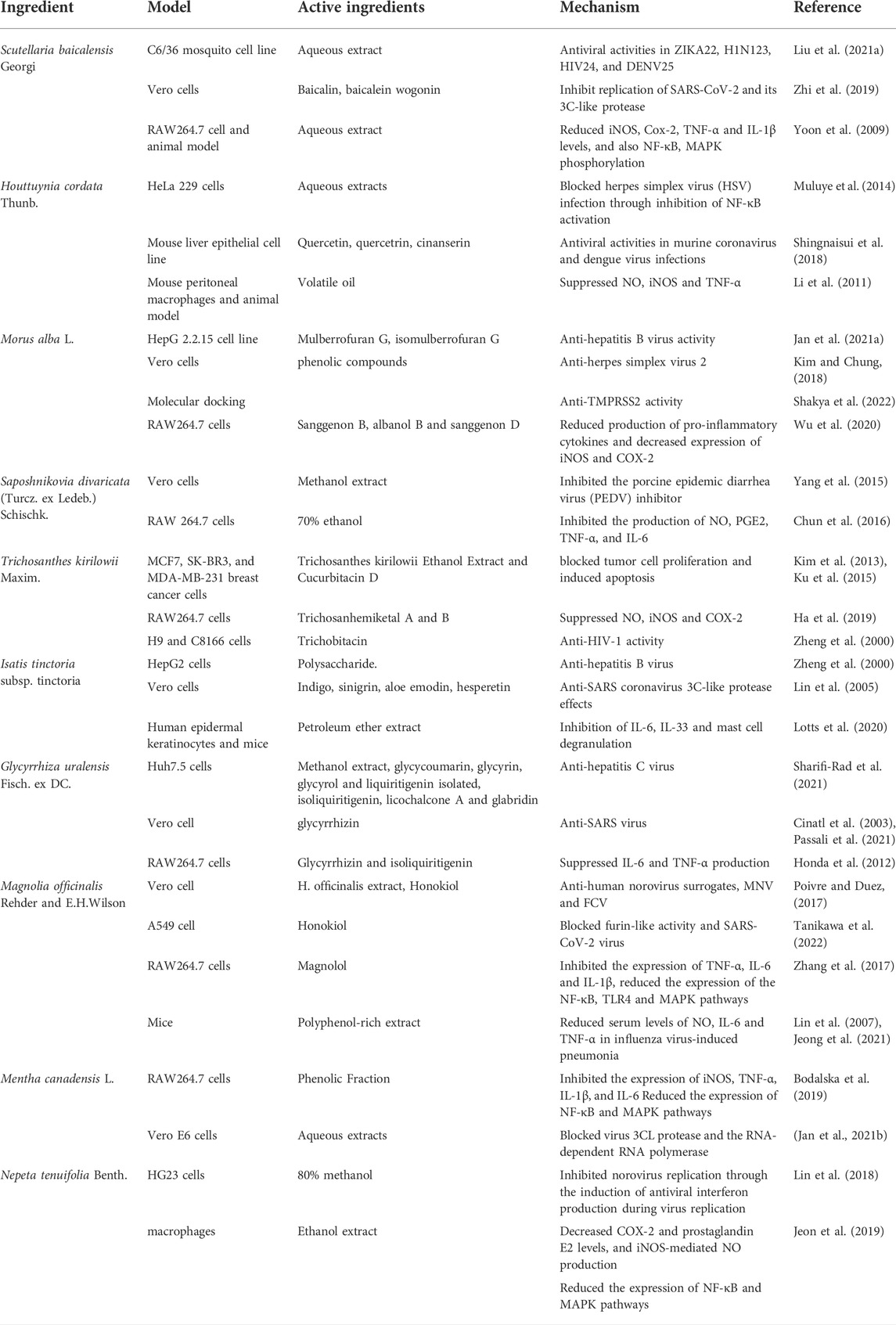
TABLE 3. The potential efficacy of the herbs of Taiwan Chingguan Yihau (NRICM101) used as adjunctive therapies in COVID-19 infection.
TCM use of S. baicalensis includes purposes of heat clearing, fire purging, detoxification, and hemostasis. Evidence supports anti-tumour, antiviral, antimicrobial, and anti-inflammatory activities associated with S. baicalensis (Zhao et al., 2016). S. baicalensis extracts have shown broad-spectrum antiviral activities against ZIKA, H1N1, HIV, and DENV viruses (Liu et al., 2021a). Most S. baicalensis ingredients are flavonoids (baicalin, baicalein, and wogonin) that reportedly inhibit in vitro replication of SARS-CoV-2 and 3Cpro (Wang and Yang, 2021c). Flavonoid-enriched S. baicalensis extract significantly lowers nitric oxide (NO) production and levels of TNF-α, IL-6, and MCP-1 expression (Zhi et al., 2019). In lipopolysaccharide (LPS)-stimulated RAW 264.7 macrophages, S. baicalensis water extract significantly inhibits NO production, interleukins 3, 6, 10, 12p40 and 17, interferon-inducible protein-10, vascular endothelial growth factor (VEGF) and keratinocyte-derived chemokines (Yoon et al., 2009).
The perennial medicinal herb H. cordata, often called Yu-Xing-Cao in Chinese, is widely distributed throughout East and South Asia. Traditional uses of H. cordata include the treatment of pneumonia, bronchitis, and chronic obstructive respiratory disease. Modern pharmacology has revealed that H. cordata has antiviral, anti-inflammatory, and antioxidative activities (Muluye et al., 2014). H. cordata has shown promising in vitro activity against envelope viruses, including herpes simplex virus 1 (HSV-1), influenza virus, and human immunodeficiency virus type 1 (HIV-1) (Muluye et al., 2014).
H. cordata essential oil inhibits activities of cyclooxygenase-2, an important inflammatory regulator (Shingnaisui et al., 2018), while H. cordata aqueous extracts reduce influenza symptoms and LPS-induced lung injury. Quercitrin is an important flavonoid glycoside in H. cordata (Li et al., 2011), capable of inhibiting the cellular content of murine Broncho alveolar fluid in mice with LPS-induced lung injury (Wu et al., 2009). Quercitrin also decreases weight loss, viral titers and mortality in mice with influenza A/WS/33 virus infection (Huang et al., 2015; Wu et al., 2021b).
M. alba L. leaves can treat headache, dizziness, cough, bronchitis, asthma, and eye infection (DeFilipps and Krupnick, 2018). Traditional Korean medicine applies M. alba root bark for upper respiratory diseases. European countries consider M. alba a “superfood,” because of the high proportion of bioactive constituents supporting health and longevity (DeFilipps and Krupnick, 2018). M. alba juice and seeds reportedly possess activity against influenza viruses (Jan et al., 2021a). M. alba aqueous extract has exhibited activity against various stages of the dengue virus replication cycle (Kim and Chung, 2018). Phenolic compounds from M. alba root bark, including α-acetyl-amyrin, cyclomorusin, eudraflavone B hydroperoxide, kuwanon S, leachianone G, moralbanone, mulberroside C and oxydihydromorusin, have shown anti-infective activities, particularly against HSV-1 and HSV-2 replication, which could be associated with its inhibition of HSV-1 DNA polymerase and HSV-2 protease (Maryam et al., 2020). Notably, M. alba extract may prevent SARS-CoV-2 cell entry by inhibiting the biological process necessary for TMPRSS2 (Shakya et al., 2022). Sanggenon B, albanol B and sanggenon D from M. alba showed inhibitory effects on NO production in LPS-stimulated RAW264.7 cells (Wu et al., 2020b).
S. divaricata, a member of the Umbelliferae family, is a perennial herb native to northern Asia. S. divaricata is listed as a high-grade drug in the Chinese Materia Medica that is indicated for the treatment of vertigo, headaches, generalized aching and arthralgia associated with “wind, cold, and dampness.” S. divaricata root extract has inhibitory effects on the central nervous system and peptic ulcer, reduces fever, and has analgesic, anticonvulsant, antioxidant and anti-inflammatory activities (Yang et al., 2020b). Chemical research into this herb has isolated several different components including chromones, coumarins, lignans, polyacetylenes and sterols (Yang et al., 2020b). Some evidence suggests that coumarins from S. divaricata inhibit the activity of porcine epidemic diarrhea virus (Yang et al., 2015). Ethanol extracts of S. divaricata showed anti-inflammatory activity by inhibiting the production of NO, prostaglandin E2 (PGE2), TNF-α, and IL-6 in LPS-induced RAW 264.7 cells (Chun et al., 2016).
T. kirilowii is a perennial liana plant of the Cucurbitaceae family that is mainly found throughout East Asia. It is an important medicinal plant that is commonly used in Chinese herbalism. T. kirilowii tuber extract has long been used in Eastern Asian medicine to alleviate diabetes symptoms. Several types of cucurbitacins demonstrate anti-inflammatory and anticancer activities, including cucurbitacin D, which has been isolated from T. kirilowii. This substance induces apoptosis and suppresses tumor cell proliferation by inhibiting signal transducer and activator of transcription 3 (STAT3) and phosphorylating nuclear factor kappa B (NF-kB) (Kim et al., 2013; Ku et al., 2015). Trichosanhemiketal A and B from T. kirilowii inhibited inducible nitric oxide synthase (iNOS) and cyclooxygenase (COX)-2 expression (Ha et al., 2019). In addition, trichosanthin extract from T. kirilowii potently inhibits HIV-1 replication and exhibits antitumor activities (Zheng et al., 2000).
I. indigotica root (Radix isatidis) is a member of the Cruciferae family and a native Chinese herb. I. indigotica root and other phenolic Chinese herbs were popular amongst TCM practitioners for controlling SARS outbreaks in 2002–2004 throughout China, Hong Kong and Taiwan. I. indigotica root has antiviral activity against influenza, hepatitis A and Japanese encephalitis (Chen et al., 2012). Substances found in I. indigotica root include indican (indoxyl-β-d-glucoside), indigo, indirubin, β-sitosterol, γ-sitosterol and sinigrin. Indigo, sinigrin, aloe emodin and hesperetin have all demonstrated anti-influenza virus effects by blocking 3CLpro cleavage (Lin et al., 2005). Petroleum ether extract of I. indigotica reportedly inhibits the levels of IL-6 and IL-33 expression and mast cell degranulation (Lotts et al., 2020).
G. glabra L. (Fabaceae family), commonly known as licorice, is a small perennial herb indigenous to West Asia. The Glycyrrhiza genus is found worldwide and contains over 30 species. Rhizomes and roots are the most important medicinal parts of licorice and are used alone or in combination with other herbs in the treatment of diverse digestive system disorders (e.g., stomach ulcers, hyperdipsia, flatulence, colic), respiratory tract disorders (e.g., asthma, coughs, sore throat, and tonsillitis), jaundice, hemorrhagic diseases, malaria, fever, epilepsy, sexual debility, paralysis, rheumatism, leucorrhea, psoriasis, and prostate cancer. This substance is also used to flavor foods and beverages (El-Saber Batiha et al., 2020).
Several active compounds are found in G. glabra roots, including the flavonoids glucoliquiritin, licoarylcoumarin, licopyranocoumarin, liquirtin, liquiritigenin, rhamnoliquirilin, and glycyrrhizin. The main active constituent of G. glabra is glycyrrhizin, capable of inhibiting virus-cell binding and beneficial in the treatment of HIV-1 and chronic hepatitis C virus (HCV) infections (Sharifi-Rad et al., 2021). Glycyrrhizin markedly inhibits SARS viral reproduction (Cinatl et al., 2003; Passali et al., 2021). In addition, glycyrrhizin and isoliquiritigenin suppress LPS-induced activation of signaling cascades and cytokine production (Honda et al., 2012).
M. officinalis is an important TCM herb for the treatment of a wide variety of conditions, including gastrointestinal disorders, typhoid fever, thrombotic stroke, allergies, anxiety, and nervous disturbances. Biologically active compounds found in M. officinalis include 4-O-methylhonokiol, honokiol, magnolol, obovatol, and other neolignan compounds. The two major metabolites, honokiol and magnolol, have wide-ranging pharmacological effects, including antitumorigenic, anti-inflammatory, antithrombotic, antioxidative, and neuroprotective activities (Honda et al., 2012). M. officinalis extract and Honokiol reportedly suppresses against human norovirus surrogates, murine norovirus (MNV) and feline calicivirus (FCV) in vitro, and in model food system (Kim et al., 2021). Honokiol inhibited the furin-like activity and SARS-CoV-2 infection (Tanikawa et al., 2022). Interestingly, high levels of NO, IL-6 and TNF-α expression in a mouse model of pneumonia were effectively lowered after treatment with polyphenol-rich extract from M. officinalis bark, which also provided long-term protection against reinfection (Lin et al., 2007; Zhang et al., 2017; Jeong et al., 2021).
M. canadensis, a perennial herbaceous plant of the Lamiaceae family, is found throughout Taiwan and popularly used in food, cosmetics and medicines. In TCM, M. canadensis is used to treat diseases related to the nervous, respiratory, reproductive and digestive systems (He et al., 2019). Pharmacological studies of M. canadensis have revealed antimicrobial, anti-inflammatory, antiviral, antioxidant, antitumor, gastrointestinal protective and hepatoprotective activities (He et al., 2019). M. canadensis contains many volatile compounds including menthol and menthone, as well as polyphenolic acids, flavonoids, monoterpenoids and glycosides, which are speculated to be responsible for the medicinal benefits (Tafrihi et al., 2021). Amongst M. canadensis -related flavonoids, hesperidin and linarin are abundant active substances. Hesperidin has shown anti-inflammatory, antioxidative and antitumor activities, while linarin has anti-inflammatory and acetylcholinesterase activities (Bodalska et al., 2019). In addition, in a hamster disease model of SARS-CoV-2 infection, M. canadensis prophylaxis effectively prevented the disease from developing (Jan et al., 2021b).
N. tenuifolia belongs to the Lamiaceae family and has a long history of medicinal use in China, Taiwan, Japan and Korea. N. tenuifolia is used to treat symptoms of common influenza (e.g., fever, headache, virus infections and sore throat) and is supported by pharmacological evidence of anti-inflammatory (Kim and Chung, 2018), immunomodulatory, antioxidative and antipruritic activities (Lin et al., 2018; Jeon et al., 2019). The major identified constituents in this substance are (−)-pulegone, (+)-menthone and (+)-limonene. N. tenuifolia has been marketed for the treatment of common cold and fever in Chinese proprietary medicines (Fung and Lau, 2002).
Ten constituent herbs were identified in an HPLC fingerprint analysis of NRICM101 (Tsai et al., 2021). Baicalin is the main compound in NRICM101 (2.38 mg/ml); many other compounds that have been identified include mainly caffeoylquinic acid, quercetin, rutin, chrysin, baicalin, breviscapine, wogonin, and licorice.
A randomized clinical trial of 98 confirmed cases were treated with QFPD, patients were treated for 9 days and the total effective rate was 92.09%, of which the recovery rate was 41.13%, the significant efficiency was 26.92%, and the effective rate was 24.04% (Wang, et al., 2020b). QFPDQ has a good therapeutic effect on the treatment of COVID-19 in clinical practice. In addition, when used as adjuvant therapy with western medicine, QFPD can relieve symptoms and improve pulmonary inflammation regression, showing a trend of reducing the degree of multi-organ damage in patients with COVID-19 (Xin, et al., 2020). It significantly improves the clinical symptoms of patients, reduces the adverse reactions of patients, and improves the therapeutic effect.
A randomized clinical trial on LHQW of 284 (142 each in treatment and control group) COVID-19 patients is useful to confirm the beneficial effect. In the trial, 142 patients were given LHQW for 14 consecutive days, the results manifested that the recovery rate (91.5% vs. 82.4%), the improvement rate (83.8% vs. 64.1%) and the clinical cure rate (78.9% vs. 66.2%) of the treatment group were higher than the control group (Wang et al 2020a). Time to recovery of fever (2 vs. 3 days), fatigue (3 vs. 6 days) and coughing (7 vs. 10 days) was also significantly shorter in treatment group. This trial showed that LHQW could be considered to ameliorate clinical symptoms of COVID-19 (Hu, et al., 2022).
In clinical studies, NRICM101 (100 ml) was administered three times a day, 30 min after each meal, until hospital discharge (Tsai et al., 2021). Taiwan study discharge criteria stipulated three consecutive negative test results for SARS-CoV-2 in respiratory tract samples that were collected at ≥24 h intervals (3 N). Any adverse events were recorded on a standard form. In patients given symptomatic care only, 3 N was reached at a median of 22 days after the onset of hospitalization. NRICM101 was administered to those patients who failed to show signs of improvement after a median 21.5 days in hospital; 3 N was observed at a median 9 days after intervention. However, while the evidence suggests that NRICM101 shortens the time to symptom recovery, no between-group differences were observed in the conversion rate to severe cases or viral assay findings (Tsai et al., 2021). An analysis of the literature has found that NRICM101 can reduce virus infections and replication withdrawal syndrome in patients with COVID-19 (Tsai et al., 2021). In light of the safety and effectiveness profiles, NRICM101 can be considered as capable of ameliorating clinical symptoms of COVID-19 (Tsai et al., 2021). The potential feasibility of TCM prescriptions for the treatment of COVID-19 is elucidated. More experimental and clinical research is needed to prove the safety and effectiveness of this formula.
The COVID-19 epidemic remains serious, with no available measures or drug treatments that can effectively control the spread of infection. For those in home isolation, TCM can be used to prevent and avoid severe illness. The ingredients prescribed are mainly polyphenols, which are used to avoid infection and boost autoimmunity (Ali et al., 2013). Prescriptions for COVID-19 prevention based on the “natural factor” theory were used to maintain life qi (Liu et al. 2022). Modern pharmacological studies have shown that TCM ingredients have the functions of clearing away heat and detoxification, removing moisture from the surface and inhibiting viruses. Much evidence shows that TCM can improve the symptoms of COVID-19, delay the clinical deterioration, and reduce all-cause mortality in severe cases. Different combinations of TCM compounds may improve therapeutic efficacy. There are two ways in which TCM acts as an antiviral drug. One is to directly inhibit the entry and replication of the virus, mainly to clear heat and detoxify such as honeysuckle, Radix isatidis and Scutellaria for inhibition. The second is to indirectly exert antiviral effects or inhibit virus-mediated inflammatory responses by regulating the immune function of organisms. Astragalus, licorice and mint are used as antivirals and induce interferon and immunoglobulin. TCM focuses on the overall regulation of the body. Therefore, TCM can play a multi-target role in the regulation of body systems (Zhong, et al., 2019). A single targeted drug may not be suitable for curing complex diseases such as COVID-19. Chinese medicine has good potential to complement the medical treatment of COVID-19, in part perhaps because of the multi-component and multi-target effects of Chinese medicine. Different Chinese medicines may act on the same or similar targets or pathways. However, current understandings of the mechanisms of action of TCM have mostly been generated by molecular analysis and network pharmacology-based approaches. In vitro cellular assays and in vivo animal studies are required to confirm these predicted mechanisms. In addition, many clinical studies and statistical methods still have the safety and efficacy of TCM in the treatment of new coronavirus infection should be carefully evaluated. It remains necessary to elucidate the mechanisms of action of TCM that ameliorate symptoms of COVID-19. Further evaluations are needed to explore the clinical efficacy of TCM against COVID-19, potential molecular mechanisms that improve multiple organ damage, and use various modern scientific techniques to determine the material basis of possible drugs. It is hoped that this review can provide a reference and basis for the development of new drugs for the prevention and treatment of viral infectious diseases such as COVID-19.
NRICM101 is an herbal formula that has been developed according to TCM theory and preclinical experiments. Mechanism of action studies involving NRICM101 have shown that NRICM101 exerts potential therapeutic effects by comprehensively regulating multiple targets via multichannel synergistic mechanisms, providing a theoretical basis for further empirical research and drug development. However, despite the promise of in-depth research into pathogenic targets of COVID-19, the global outbreak continues to worsen. It is therefore hoped that NRICM101 may be used in addition to conventional drug therapy for treating COVID-19 infection. More clinical studies are needed to explore NRICM101-associated efficacy and safety in COVID-19 infection.
G-JH collected and analyzed literature and made charts. Y-CS and J-GL coordinated and jointly wrote and revised the paper. All authors read and approved the manuscript.
We thank Iona J. MacDonald from China Medical University for her editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ali, M. R., Seo, J., Lee, D., and Kim, Y. (2013). Teratocyte-secreting proteins of an endoparasitoid wasp, Cotesia plutellae, prevent host metamorphosis by altering endocrine signals. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 166 (2), 251–262. doi:10.1016/j.cbpa.2013.06.028
Beigel, J. H., Tomashek, K. M., Dodd, L. E., Mehta, A. K., Zingman, B. S., Kalil, A. C., et al. (2020). Remdesivir for the treatment of covid-19 - final report. N. Engl. J. Med. 383 (19), 1813–1826. doi:10.1056/NEJMoa2007764
Bodalska, A., Kowalczyk, A., Włodarczyk, M., and Fecka, I. (2019). Analysis of polyphenolic composition of a herbal medicinal product-peppermint tincture. Molecules 25 (1), 69. doi:10.3390/molecules25010069
Chen, M., Gan, L., Lin, S., Wang, X., Li, L., Li, Y., et al. (2012). Alkaloids from the root of Isatis indigotica. J. Nat. Prod. 75 (6), 1167–1176. doi:10.1021/np3002833
Chun, J. M., Kim, H. S., Lee, A. Y., Kim, S.-H., and Kim, H. K. (2016). Anti-inflammatory and antiosteoarthritis effects of saposhnikovia divaricata ethanol extract: In vitro and in vivo studies. Evid. Based. Complement. Alternat. Med. 2016, 1984238. doi:10.1155/2016/1984238
Cinatl, J., Morgenstern, B., Bauer, G., Chandra, P., Rabenau, H., and Doerr, H. W. (2003). Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet 361 (9374), 2045–2046. doi:10.1016/s0140-6736(03)13615-x
DeFilipps, R. A., and Krupnick, G. A. (2018). The medicinal plants of Myanmar. PhytoKeys 102, 1–341. doi:10.3897/phytokeys.102.24380
Ding, Y., Zeng, L., Li, R., Chen, Q., Zhou, B., Chen, Q., et al. (2017). The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Complement. Altern. Med. 17 (1), 130. doi:10.1186/s12906-017-1585-7
Dong, L., Xia, J. W., Gong, Y., Chen, Z., Yang, H. H., Zhang, J., et al. (2014). Effect of lianhuaqingwen capsules on airway inflammation in patients with acute exacerbation of chronic obstructive pulmonary disease. Evid. Based. Complement. Alternat. Med. 2014, 637969. doi:10.1155/2014/637969
Du, H. Z., Hou, X. Y., Miao, Y. H., Huang, B. S., and Liu, D. H. (2020). Traditional Chinese medicine: An effective treatment for 2019 novel coronavirus pneumonia (NCP). Chin. J. Nat. Med. 18 (3), 206–210. doi:10.1016/s1875-5364(20)30022-4
El-Saber Batiha, G., Magdy Beshbishy, A., El-Mleeh, A., Abdel-Daim, M. M., and Prasad Devkota, H. (2020). Traditional uses, bioactive chemical constituents, and pharmacological and toxicological activities of Glycyrrhiza glabra L. (Fabaceae). Biomolecules 10 (3), E352. doi:10.3390/biom10030352
Fu, X. J., Song, X. X., Wei, L. B., and Wang, Z. G. (2013). Study of the distribution patterns of the constituent herbs in classical Chinese medicine prescriptions treating respiratory disease by data mining methods. Chin. J. Integr. Med. 19 (8), 621–628. doi:10.1007/s11655-012-1090-2
Fung, D., and Lau, C. B. (2002). Schizonepeta tenuifolia: Chemistry, pharmacology, and clinical applications. J. Clin. Pharmacol. 42 (1), 30–36. doi:10.1177/0091270002042001003
George, P. M., Wells, A. U., and Jenkins, R. G. (2020). Pulmonary fibrosis and COVID-19: The potential role for antifibrotic therapy. Lancet. Respir. Med. 8 (8), 807–815. doi:10.1016/s2213-2600(20)30225-3
Ha, M. T., Phan, T. N., Kim, J. A., Oh, W. K., Lee, J. H., Woo, M. H., et al. (2019). Trichosanhemiketal A and B: Two 13, 14-seco-13, 14-epoxyporiferastanes from the root of Trichosanthes kirilowii maxim. Bioorg. Chem. 83, 105–110. doi:10.1016/j.bioorg.2018.10.019
He, X. F., Geng, C. A., Huang, X. Y., Ma, Y. B., Zhang, X. M., and Chen, J. J. (2019). Chemical constituents from Mentha haplocalyx Briq. (Mentha canadensis L.) and Their α-glucosidase inhibitory activities. Nat. Prod. Bioprospect. 9 (3), 223–229. doi:10.1007/s13659-019-0207-0
Hoffmann, M., Kleine-Weber, H., Schroeder, S., Krüger, N., Herrler, T., Erichsen, S., et al. (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181 (2), 271–280. e278. doi:10.1016/j.cell.2020.02.052
Honda, H., Nagai, Y., Matsunaga, T., Saitoh, S. i., Akashi‐Takamura, S., Hayashi, H., et al. (2012). Glycyrrhizin and isoliquiritigenin suppress the LPS sensor Toll like receptor 4/MD‐2 complex signaling in a different manner. J. Leukoc. Biol. 91 (6), 967–976. doi:10.1189/jlb.0112038
Hsu, C. H., Lin, H. H., Wang, C. C., and Jhang, S. (2020). How to defend COVID-19 in taiwan? Talk about people's disease awareness, attitudes, behaviors and the impact of physical and mental health. Int. J. Environ. Res. Public Health 17 (13), E4694. doi:10.3390/ijerph17134694
Hu, K., Guan, W. J., Bi, Y., Zhang, W., Li, L., Zhang, B., et al. (2022). Efficacy and safety of lianhuaqingwen capsules, a repurposed Chinese herb, in patients with coronavirus disease 2019: A multicenter, prospective, randomized controlled trial. Phytomedicine. 85, 153242. doi:10.1016/j.phymed.2020.153242
Huang, R., Zhong, T., and Wu, H. (2015). Quercetin protects against lipopolysaccharide-induced acute lung injury in rats through suppression of inflammation and oxidative stress. Arch. Med. Sci. 11 (2), 427–432. doi:10.5114/aoms.2015.50975
Jan, B., Parveen, R., Zahiruddin, S., Khan, M. U., Mohapatra, S., and Ahmad, S. (2021a). Nutritional constituents of mulberry and their potential applications in food and pharmaceuticals: A review. Saudi J. Biol. Sci. 28 (7), 3909–3921. doi:10.1016/j.sjbs.2021.03.056
Jan, J. T., Cheng, T. R., Juang, Y. P., Ma, H. H., Wu, Y. T., Yang, W. B., et al. (2021b). Identification of existing pharmaceuticals and herbal medicines as inhibitors of SARS-CoV-2 infection. Proc. Natl. Acad. Sci. U. S. A. 118 (5), e2021579118. doi:10.1073/pnas.2021579118
Jeon, B.-R., Irfan, M., Kim, M., Lee, S. E., Lee, J. H., and Rhee, M. H. (2019). Schizonepeta tenuifolia inhibits collagen stimulated platelet function via suppressing MAPK and Akt signaling. J. Biomed. Res. 33 (4), 250. doi:10.7555/JBR.32.20180031
Jeong, S., Lee, Y. S., Kim, K., Yoon, J. S., Kim, S., Ha, J., et al. (2021). 2-O-Methylhonokiol suppresses HCV replication via TRAF6-mediated NF-kB activation. Int. J. Mol. Sci. 22 (12), 6499. doi:10.3390/ijms22126499
Jiang, F., Deng, L., Zhang, L., Cai, Y., Cheung, C. W., and Xia, Z. (2020). Review of the clinical characteristics of coronavirus disease 2019 (COVID-19). J. Gen. Intern. Med. 35 (5), 1545–1549. doi:10.1007/s11606-020-05762-w
Kim, H., and Chung, M. S. (2018). Antiviral activities of mulberry (morus alba) juice and seed against influenza viruses. Evid. Based. Complement. Alternat. Med. 2018, 2606583. doi:10.1155/2018/2606583
Kim, H., Lim, C. Y., and Chung, M. S. (2021). Magnolia officinalis and its honokiol and magnolol constituents inhibit human norovirus surrogates. Foodborne Pathog. Dis. 18 (1), 24–30. doi:10.1089/fpd.2020.2805
Kim, S. R., Seo, H. S., Choi, H.-S., Cho, S.-G., Kim, Y. K., Hong, E. H., et al. (2013). Trichosanthes kirilowii ethanol extract and cucurbitacin D inhibit cell growth and induce apoptosis through inhibition of STAT3 activity in breast cancer cells. Evid. Based. Complement. Alternat. Med. 2013, 975350. doi:10.1155/2013/975350
Ku, J. M., Kim, S. R., Hong, S. H., Choi, H. S., Seo, H. S., Shin, Y. C., et al. (2015). Cucurbitacin D induces cell cycle arrest and apoptosis by inhibiting STAT3 and NF-κB signaling in doxorubicin-resistant human breast carcinoma (MCF7/ADR) cells. Mol. Cell. Biochem. 409 (1-2), 33–43. doi:10.1007/s11010-015-2509-9
Li, R., Hou, Y., Huang, J., Pan, W., Ma, Q., Shi, Y., et al. (2020). Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2). Pharmacol. Res. 156, 104761. doi:10.1016/j.phrs.2020.104761
Li, W., Zhou, P., Zhang, Y., and He, L. (2011). Houttuynia cordata, a novel and selective COX-2 inhibitor with anti-inflammatory activity. J. Ethnopharmacol. 133 (2), 922–927. doi:10.1016/j.jep.2010.10.048
Lin, C. W., Tsai, F. J., Tsai, C. H., Lai, C. C., Wan, L., Ho, T. Y., et al. (2005). Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antivir. Res. 68 (1), 36–42. doi:10.1016/j.antiviral.2005.07.002
Lin, Y. H., Chen, H. Y., Chiu, J. C., Chen, K. J., Ho, H. Y., and Yang, S. H. (2018). Immunomodulation effects of schizonepeta tenuifolia briq. On the IgE-induced allergic model of RBL-2H3 cells. Evid. Based. Complement. Alternat. Med. 2018, 6514705. doi:10.1155/2018/6514705
Lin, Y. R., Chen, H. H., Ko, C. H., and Chan, M. H. (2007). Effects of honokiol and magnolol on acute and inflammatory pain models in mice. Life Sci. 81 (13), 1071–1078. doi:10.1016/j.lfs.2007.08.014
Liu, H., Ye, F., Sun, Q., Liang, H., Li, C., Li, S., et al. (2021a). Scutellaria baicalensis extract and baicalein inhibit replication of SARS-CoV-2 and its 3C-like protease in vitro. J. Enzyme Inhib. Med. Chem. 36 (1), 497–503. doi:10.1080/14756366.2021.1873977
Liu, W., Huang, J., Zhang, F., Zhang, C. C., Li, R. S., Wang, Y. L., et al. (2021b). Comprehensive profiling and characterization of the absorbed components and metabolites in mice serum and tissues following oral administration of Qing-Fei-Pai-Du decoction by UHPLC-Q-Exactive-Orbitrap HRMS. Chin. J. Nat. Med. 19 (4), 305–320. doi:10.1016/s1875-5364(21)60031-6
Liu, Z., Du, S., Shao, F., Li, H., Xu, S., Ma, X., et al. (2021c). Efficacy of qingfei paidu decoction on patients with COVID-19 pneumonia in wuhan, China: A propensity score matching study. Evid. Based. Complement. Alternat. Med. 2021, 4303380. doi:10.1155/2021/4303380
Liu, Y. X., Zhou, Y. H., Jiang, C. H., Liu, J., and Chen, D. Q. (2022). Prevention, treatment and potential mechanism of herbal medicine for corona viruses: A review. Bioengineered 13 (3), 5480–5508. doi:10.1080/21655979.2022.2036521
Lotts, T., Kabrodt, K., Hummel, J., Binder, D., Schellenberg, I., Staender, S., et al. (2020). Isatis tinctoria L.-derived petroleum ether extract mediates anti-inflammatory effects via inhibition of interleukin-6, interleukin-33 and mast cell degranulation. Acta Derm. Venereol. 100 (10), adv00131. doi:10.2340/00015555-3476
Lu, P. H., Tseng, C. W., Lee, J. L., Lee, E. Y., Lin, Y. P., Lin, I.-H., et al. (2021). Jing Si herbal drink as a prospective adjunctive therapy for COVID-19 treatment: Molecular evidence and mechanisms. Pharmacol. Res. - Mod. Chin. Med. 2, 100024. doi:10.1016/j.prmcm.2021.100024
Luo, H., Gao, Y., Zou, J., Zhang, S., Chen, H., Liu, Q., et al. (2020). Reflections on treatment of COVID-19 with traditional Chinese medicine. Chin. Med. 15, 94. doi:10.1186/s13020-020-00375-1
Maryam, M., Te, K. K., Wong, F. C., Chai, T. T., Gary, K., Gan, S. C., et al. (2020). Antiviral activity of traditional Chinese medicinal plants Dryopteris crassirhizoma and Morus alba against dengue virus. J. Integr. Agric. 19 (4), 1085–1096. doi:10.1016/S2095-3119(19)62820-0
Mehrbod, P., Hudy, D., Shyntum, D., Markowski, J., Łos, M. J., and Ghavami, S. (2020). Quercetin as a natural therapeutic candidate for the treatment of influenza virus. Biomolecules 11 (1), 10. doi:10.3390/biom11010010
Mody, V., Ho, J., Wills, S., Mawri, A., Lawson, L., Ebert, M., et al. (2021). Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents. Commun. Biol. 4 (1), 93. doi:10.1038/s42003-020-01577-x
MOHW (The Ministry of Health and Welfare) (2022). Total number of notifications of Novel coronavirus in Taiwan [Online] [Accessed]. Available: https://sites.google.com/cdc.gov.tw/2019ncov/taiwan.
Muluye, R. A., Bian, Y., and Alemu, P. N. (2014). Anti-inflammatory and antimicrobial effects of heat-clearing Chinese herbs: A current review. J. Tradit. Complement. Med. 4 (2), 93–98. doi:10.4103/2225-4110.126635
Ni, W., Yang, X., Yang, D., Bao, J., Li, R., Xiao, Y., et al. (2020). Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care 24 (1), 422. doi:10.1186/s13054-020-03120-0
Niesor, E. J., Boivin, G., Rhéaume, E., Shi, R., Lavoie, V., Goyette, N., et al. (2021). Inhibition of the 3CL protease and SARS-CoV-2 replication by Dalcetrapib. ACS Omega 6 (25), 16584–16591. doi:10.1021/acsomega.1c01797
Passali, D., Ciprandi, G., Damiani, V., De Marco, A., Cianfrone, F., and Passali, F. (2021). Glycyrrhizin for topical use and prophylaxis of COVID-19: An interesting pharmacological perspective. J. Biol. Regul. Homeost. Agents 35 (1), 15–19. doi:10.23812/21-1supp2-4
Qi, F., and Tang, W. (2021). Traditional Chinese medicine for treatment of novel infectious diseases: Current status and dilemma. Biosci. Trends 15 (4), 201–204. doi:10.5582/bst.2021.01263
Qiu, Q., Huang, Y., Liu, X., Huang, F., Li, X., Cui, L., et al. (2020). Potential therapeutic effect of traditional Chinese medicine on coronavirus disease 2019: A review. Front. Pharmacol. 11, 570893. doi:10.3389/fphar.2020.570893
Ren, W., Ma, Y., Wang, R., Liang, P., Sun, Q., Pu, Q., et al. (2020). Research advance on Qingfei Paidu decoction in prescription principle, mechanism analysis and clinical application. Front. Pharmacol. 11, 589714. doi:10.3389/fphar.2020.589714
Shakya, A., Chikhale, R. V., Bhat, H. R., Alasmary, F. A., Almutairi, T. M., Ghosh, S. K., et al. (2022). Pharmacoinformatics-based identification of transmembrane protease serine-2 inhibitors from Morus Alba as SARS-CoV-2 cell entry inhibitors. Mol. Divers. 26 (1), 265–278. doi:10.1007/s11030-021-10209-3
Shang, J., Wan, Y., Luo, C., Ye, G., Geng, Q., Auerbach, A., et al. (2020). Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. U. S. A. 117 (21), 11727–11734. doi:10.1073/pnas.2003138117
Sharifi-Rad, J., Quispe, C., Herrera-Bravo, J., Belén, L. H., Kaur, R., Kregiel, D., et al. (2021). Glycyrrhiza genus: Enlightening phytochemical components for pharmacological and health-promoting abilities. Oxid. Med. Cell. Longev. 2021, 7571132. doi:10.1155/2021/7571132
Shen, X., and Yin, F. (2021). The mechanisms and clinical application of traditional Chinese medicine Lianhua-Qingwen capsule. Biomed. Pharmacother. 142, 111998. doi:10.1016/j.biopha.2021.111998
Shibu, M. A., Lin, Y. J., Chiang, C. Y., Lu, C. Y., Goswami, D., Sundhar, N., et al. (2022). Novel anti-aging herbal formulation Jing Si displays pleiotropic effects against aging associated disorders. Biomed. Pharmacother. 146, 112427. doi:10.1016/j.biopha.2021.112427
Shingnaisui, K., Dey, T., Manna, P., and Kalita, J. (2018). Therapeutic potentials of Houttuynia cordata Thunb. Against inflammation and oxidative stress: A review. J. Ethnopharmacol. 220, 35–43. doi:10.1016/j.jep.2018.03.038
Tafrihi, M., Imran, M., Tufail, T., Gondal, T. A., Caruso, G., Sharma, S., et al. (2021). The wonderful activities of the genus mentha: Not only antioxidant properties. Molecules 26 (4), 1118. doi:10.3390/molecules26041118
Tanikawa, T., Hayashi, T., Suzuki, R., Kitamura, M., and Inoue, Y. (2022). Inhibitory effect of honokiol on furin-like activity and SARS-CoV-2 infection. J. Tradit. Complement. Med. 12 (1), 69–72. doi:10.1016/j.jtcme.2021.09.005
Tsai, K. C., Huang, Y. C., Liaw, C. C., Tsai, C. I., Chiou, C. T., Lin, C. J., et al. (2021). A traditional Chinese medicine formula NRICM101 to target COVID-19 through multiple pathways: A bedside-to-bench study. Biomed. Pharmacother. 133, 111037. doi:10.1016/j.biopha.2020.111037
Wang, S. X., Wang, Y., Lu, Y. B., Li, J. Y., Song, Y. J., Nyamgerelt, M., et al. (2020a). Diagnosis and treatment of novel coronavirus pneumonia based on the theory of traditional Chinese medicine. J. Integr. Med. 18 (4), 275–283. doi:10.1016/j.joim.2020.04.001
Wang, R. Q., Yang, S. J., Xie, C. G., Shen, Q., Li, M., Lei, X., et al. (2020b). Clinical observation of qingfeipaidu decoction in the treatment of COVID-19. Pharmacol. Clin. Chin. Mat. Med. 36 (1), 13–18.
Wang, Z., Yang, L., and Zhao, X. E. (2021). Co-crystallization and structure determination: An effective direction for anti-SARS-CoV-2 drug discovery. Comput. Struct. Biotechnol. J. 19, 4684–4701. doi:10.1016/j.csbj.2021.08.029
Wang, Z., and Yang, L. (2021a). Chinese herbal medicine: Fighting SARS-CoV-2 infection on all fronts. J. Ethnopharmacol. 270, 113869. doi:10.1016/j.jep.2021.113869
Wang, Z., and Yang, L. (2021b). Broad-spectrum prodrugs with anti-SARS-CoV-2 activities: Strategies, benefits, and challenges. J. Med. Virol. 94 (4), 1373–1390. doi:10.1002/jmv.27517
Wang, Z., and Yang, L. (2021c). Natural products, alone or in combination with FDA-approved drugs, to treat COVID-19 and lung cancer. Biomedicines 9, 689. doi:10.3390/biomedicines9060689
Wang, Z., and Yang, L. (2020). GS-5734: A potentially approved drug by FDA against SARS-cov-2. New J. Chem. 44 (29), 12417–12429. doi:10.1039/D0NJ02656E
Wang, Z., and Yang, L. (2022). In the age of Omicron variant: Paxlovid raises new hopes of COVID-19 recovery. J. Med. Virol. 94 (5), 1766–1767. doi:10.1002/jmv.27540
WHO Solidarity Trial Consortium (2022). Remdesivir and three other drugs for hospitalised patients with COVID-19: Final results of the WHO solidarity randomised trial and updated meta-analyses. Lancet 399 (10339), 1941–1953. doi:10.1016/S0140-6736(22)00519-0
Wu, L. S., Si, J. P., Yuan, X. Q., and Shi, X. R. (2009). Quantitive variation of flavonoids in Houttuynia cordata from different geographic origins in China. Chin. J. Nat. Med. 7 (1), 40–46. doi:10.1016/S1875-5364(09)60042-X
Wu, Y. C., Chen, C. S., and Chan, Y. J. (2020a). The outbreak of COVID-19: An overview. J. Chin. Med. Assoc. 83 (3), 217–220. doi:10.1097/JCMA.0000000000000270
Wu, Y. X., Kim, Y. J., Kwon, T. H., Tan, C. P., Son, K. H., and Kim, T. (2020b). Anti-inflammatory effects of mulberry (Morus alba L.) root bark and its active compounds. Nat. Prod. Res. 34 (12), 1786–1790. doi:10.1080/14786419.2018.1527832
Wu, D. Y., Hou, X. T., Xia, Z. S., Hao, E. W., Xie, J. L., Liang, J. Y., et al. (2021a). Analysis on oral medication rules of traditional Chinese medicine prescriptions for prevention of COVID-19. Chin. Herb. Med. 13 (4), 502–517. doi:10.1016/j.chmed.2021.10.007
Wu, Z., Deng, X., Hu, Q., Xiao, X., Jiang, J., Ma, X., et al. (2021b). Houttuynia cordata Thunb: An ethnopharmacological review. Front. Pharmacol. 12, 714694. doi:10.3389/fphar.2021.714694
Xin, S., Cheng, X., Zhu, B., Liao, X., Yang, F., Song, L., et al. (2020). Clinical retrospective study on the efficacy of Qingfei Paidu decoction combined with Western medicine for COVID-19 treatment. Biomed. Pharmacother. 129, 110500. doi:10.1016/j.biopha.2020.110500
Xing, D., and Liu, Z. (2021). Effectiveness and safety of traditional Chinese medicine in treating COVID-19: Clinical evidence from China. Aging Dis. 12 (8), 1850–1856. doi:10.14336/ad.2021.0906
Xu, H. Y., Zhang, Y. Q., Liu, Z. M., Chen, T., Lv, C. Y., Tang, S. H., et al. (2019). Etcm: An encyclopaedia of traditional Chinese medicine. Nucleic Acids Res. 47 (D1), D976–d982. doi:10.1093/nar/gky987
Yan, S., Lu, Y., Zhang, G., Li, X., Wang, Z., Yao, C., et al. (2020). Effect of heat-clearing and detoxifying Chinese medicines combined with conventional therapy on mild hand, foot, and mouth disease with fever: An individual patient data meta-analysis. Med. Baltim. 99 (23), e20473. doi:10.1097/md.0000000000020473
Yang, J. L., Dhodary, B., Quy Ha, T. K., Kim, J., Kim, E., and Oh, W. K. (2015). Three new coumarins from Saposhnikovia divaricata and their porcine epidemic diarrhea virus (PEDV) inhibitory activity. Tetrahedron 71 (28), 4651–4658. doi:10.1016/j.tet.2015.04.092
Yang, K. L., Jin, X. Y., Gao, Y., Xie, J., Liu, M., Zhang, J. H., et al. (2020a). Bibliometric analysis of researches on traditional Chinese medicine for coronavirus disease 2019 (COVID-19). Integr. Med. Res. 9 (3), 100490. doi:10.1016/j.imr.2020.100490
Yang, M., Wang, C.-c., Wang, W.-l., Xu, J.-p., Wang, J., Zhang, C.-h., et al. (2020b). Saposhnikovia divaricata—an ethnopharmacological, phytochemical and pharmacological review. Chin. J. Integr. Med. 26 (11), 873–880. doi:10.1007/s11655-020-3091-x
Yang, Y., Islam, M. S., Wang, J., Li, Y., and Chen, X. (2020c). Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): A review and perspective. Int. J. Biol. Sci. 16 (10), 1708–1717. doi:10.7150/ijbs.45538
Yoon, S. B., Lee, Y. J., Park, S. K., Kim, H. C., Bae, H., Kim, H. M., et al. (2009). Anti-inflammatory effects of Scutellaria baicalensis water extract on LPS-activated RAW 264.7 macrophages. J. Ethnopharmacol. 125 (2), 286–290. doi:10.1016/j.jep.2009.06.027
Zaim, S., Chong, J. H., Sankaranarayanan, V., and Harky, A. (2020). COVID-19 and multiorgan response. Curr. Probl. Cardiol. 45 (8), 100618. doi:10.1016/j.cpcardiol.2020.100618
Zhang, F. H., Ren, H. Y., Shen, J. X., Zhang, X. Y., Ye, H. M., and Shen, D. Y. (2017). Magnolol suppresses the proliferation and invasion of cholangiocarcinoma cells via inhibiting the NF-κB signaling pathway. Biomed. Pharmacother. 94, 474–480. doi:10.1016/j.biopha.2017.07.085
Zhang, W., Huai, Y., Miao, Z., Qian, A., and Wang, Y. (2019). Systems pharmacology for investigation of the mechanisms of action of traditional Chinese medicine in drug discovery. Front. Pharmacol. 10, 743. doi:10.3389/fphar.2019.00743
Zhang, Y., Wang, Z., Zhang, Y., Tong, H., Zhang, Y., and Lu, T. (2020). Potential mechanisms for traditional Chinese medicine in treating airway mucus hypersecretion associated with coronavirus disease 2019. Front. Mol. Biosci. 7, 577285. doi:10.3389/fmolb.2020.577285
Zhao, Q., Chen, X. Y., and Martin, C. (2016). Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Sci. Bull. (Beijing) 61 (18), 1391–1398. doi:10.1007/s11434-016-1136-5
Zheng, Y. T., Ben, K. L., and Jin, S. W. (2000). Anti-HIV-1 activity of trichobitacin, a novel ribosome-inactivating protein. Acta Pharmacol. Sin. 21 (2), 179–182.
Zhi, H. J., Zhu, H. Y., Zhang, Y. Y., Lu, Y., Li, H., and Chen, D. F. (2019). In vivo effect of quantified flavonoids-enriched extract of Scutellaria baicalensis root on acute lung injury induced by influenza A virus. Phytomedicine 57, 105–116. doi:10.1016/j.phymed.2018.12.009
Keywords: SARS-CoV-2, antivirus, anti-inflammation, traditional Chinese medicine, viral infection
Citation: Su Y-C, Huang G-J and Lin J-G (2022) Chinese herbal prescriptions for COVID-19 management: Special reference to Taiwan Chingguan Yihau (NRICM101). Front. Pharmacol. 13:928106. doi: 10.3389/fphar.2022.928106
Received: 25 April 2022; Accepted: 13 September 2022;
Published: 05 October 2022.
Edited by:
Lyndy Joy McGaw, University of Pretoria, South AfricaReviewed by:
Liyan Yang, Qufu Normal University, ChinaCopyright © 2022 Su, Huang and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guan-Jhong Huang, Z2podWFuZ0BtYWlsLmNtdS5lZHUudHc=; Jaung-Geng Lin, amdsaW5AbWFpbC5jbXUuZWR1LnR3
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.