
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pharmacol. , 11 August 2022
Sec. Ethnopharmacology
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.883148
Background: The incidence of ischemic stroke (IS) is much higher among patients with chronic kidney disease (CKD) compared to the general population. Few studies have evaluated the association between the risk of IS and the use of Chinese herbal medicine (CHM) in patients with CKD. We aimed to investigate the risk of IS among patients with CKD using CHM as add-on therapy.
Methods: We conducted a retrospective cohort study based on Taiwan’s National Health Insurance Research Database to assess 21,641 patients with newly diagnosed CKD between 2003 and 2012. Patients were classified as either the CHM (n = 3,149) or the non-CHM group (n = 3,149) based on whether they used CHM after first diagnosis of CKD. We used the proportional subdistribution hazards model of Fine and Gray to examine the hazard ratio (HR) of IS in propensity-score matched samples at a ratio of 1:1 for two groups.
Results: The risk of IS was significantly reduced in the CHM group (adjusted HR [aHR]: 0.58, 95% confidence interval [CI]: 0.48–0.70) compared with the non-CHM group. Those who used CHM for >180 days had an even lower risk of IS than those in the non-CHM group (aHR: 0.51, 95% CI: 0.41–0.63). Additionally, frequently prescribed formulae, such as Ji-Sheng-Shen-Qi-Wan, Liu-Wei-Di-Huang-Wan, and Zhen-Wu-Tang were associated with a 30%–50% reduced risk of IS.
Conclusion: Our results suggest that patients with CKD who used CHM as add-on therapy had a lower hazard of IS than those in the non-CHM group, especially for patients taking CHM for >180 days. Further experimental studies are required to clarify the causal relationship.
Chronic kidney disease (CKD) has recently been reported as an independent risk factor for stroke. The incidence of ischemic stroke (IS) was much higher among patients with CKD compared to the general population (Tsagalis et al., 2009). A stroke in patients with CKD was associated with a worse functional outcome, a 138% higher risk of in-hospital mortality, a 49% higher risk of neurological deterioration during their hospitalization and greater medical complications including neurological deterioration, urinary tract infections, respiratory infections, and pressure sores than general population (Grams et al., 2017; Kelly and Rothwell, 2020; Kelly et al., 2021). Additionally, the IS in the advanced CKD (stage 4 or 5) patients is associated with an even higher mortality rate and higher risk of kidney failure (Wetmore et al., 2020). Abramson et al. conducted a prospective study (Atherosclerosis Risk in Communities study) which revealed that the risk of stroke was almost doubled in patients with CKD after controlling for conventional cardiovascular risk factors (Abramson et al., 2003). Furthermore, according to a systematic review study, the relative risk of IS was 1.63 (confidence interval [CI]:1.34–1.99) after adjusting the traditional risk factors of ischemic stroke (Kelly and Rothwell, 2019). The mechanism of stroke might be associated with endothelial dysfunction and accelerated arteriosclerosis (Chelluboina and Vemuganti, 2019). The accumulation of uremic toxins due to the gradual decline of kidney function aggravated the endothelial dysfunction (Jing et al., 2018). Indoxyl sulfate, one of the uremic toxins, induced the production of reactive oxygen species, promoting the pathways of activating protein 1 and nuclear factor Kappa B (NF-κB). These pathways are known to be associated with inflammation (Lano et al., 2020). In addition, renin-angiotensin system-induced angiotensin-2 activated the inflammatory reaction and induced vascular fibrosis (Benigni et al., 2010). This kind of oxidative stress response exacerbated arteriosclerosis and arterial stiffness and consequently contributed to IS among patients with CKD (Deanfield et al., 2007; Ma et al., 2015). Since the complications of CKD such as stroke increased mortality and reduced health related quality of life, it was important to slow its progression and reduce the potential complications.
The primary medications for preventing stroke among patients with CKD included antiplatelets, anticoagulants, statins, and antihypertensive agents (Kelly and Rothwell, 2020). These conventional medications have been shown to have a protective effect against stroke in the general population. However, certain kinds of antiplatelets and anticoagulants, such as aspirin, clopidogrel, and warfarin, might contribute to an increased risk of bleeding among patients with CKD (Olesen et al., 2012; Palmer et al., 2013). Antihypertensive agents, such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, could slow the progression of kidney disease, but robust evidence regarding stroke prevention was still lacking (Kelly and Rothwell, 2020). There have been limited evidence for strategies to prevent stroke in patients with CKD and more studies on novel therapeutic interventions are needed (Levin et al., 2017).
In addition to conventional medicine, 25%–50% of CKD patients used complementary and alternative medicine (CAM). The main reason for CAM usage was based on the potential benefits of CAM (Lin et al., 2015; Osman et al., 2015). The potential benefits of CAM for patients with CKD include prolonging time of progression to kidney failure as well as alleviating association problems, including arthritis, pruritus, cardiovascular risk factors, anxiety, depression, and fatigue (Markell, 2005). Among CAM, herbal products were the most commonly used type (Akyol et al., 2011). Based on previous studies, using Chinese herbal medicine (CHM) as add-on therapy with conventional therapy provided better renal protective effects in CKD patients than receiving conventional therapy alone. Patients treated with Abelmoschus manihot (L.) Medik [Malvaceae; Abelmoschi Corolla (Huang-Shu-Kui)] plus lorsatan for 24 weeks had less proteinuria than those treated with lorsatan alone (Zhang et al., 2014). In addition, patients with CKD using Dang-Gui-Bu-Xue-Tang or Fang-Ji-Huang- Qi-Tang and Benazepril in combination had higher estimated glomerular filtration rates (eGFR) and lower proteinuria than those using Benazepril alone (Wang Y. J. et al., 2012). Moreover, a meta-analysis of clinical trials also demonstrated that adding Liu-Wei-Di-Huang-Wan to western medicine might improve renal function including lowering the level of blood urea nitrogen (BUN), improving 24-hour urine total protein, and decreasing the level of serum creatinine (Lin et al., 2016). Furthermore, the underlying mechanism of CHM exerting beneficial effects in patients with CKD have been investigated through animal models. Liu-Wei-Di-Huang-Wan was found to reduce the ameliorate oxidative stress response in diabetic nephropathy rats (Xu et al., 2017). Additionally, Liu-Wei-Di-Huang-Wan was shown to have anti-inflammatory effects through preventing the activation of NF-κB signaling pathways (Xu et al., 2017). Given that some CHM have been suggested to have renal protective and anti-inflammatory effects, we hypothesized that CHM as add-on therapy with conventional therapy may be associated with a decreased risk of IS among patients with CKD. Accordingly, we conducted a retrospective cohort study to evaluate the risk of IS among patients with CKD using a combination of CHM and conventional medicine.
Taiwan launched a single-payer National Health Insurance (NHI) Program in 1995 that coveres almost the entire population. The annual coverage rate has ranged from 96.1% to 99.6% of the population, with more than 20 million Taiwan residents enrolled since 1997. The National Health Insurance Research Database (NHIRD) derived from the NHI program has been used for research purposes. The data we used in this study was from a longitudinal health insurance database from 2002 to 2013 comprised of medical claim data of one million beneficiaries randomly selected from the NHIRD, representing about 4.2% of all enrollees. Data in 2002 were used to identified patients’ medication history and comorbidities. Data during 2003–2012 were used to identify cases with newly diagnosed CKD. Data in 2013 were used for the subsequent follow-up. We extracted data regarding demographic characteristics, including encrypted identification numbers, gender, date of birth and death, and diagnostic information. The diagnostic data contained International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) as well as diagnostic and procedure codes. This study complied with the Declaration of Helsinki and was approved by the Institutional Review Board of the China Medical University (CMUH104-REC2–115 [CR-6]).
The study cohort was composed of the patients with a diagnosis of CKD (ICD-9-CM codes 585 and 586) and having at least three outpatient visits or one inpatient visit within 1 year from 2003 to 2012. The cohort was divided into two groups: those using CHM because of CKD diagnosis (prescribed CHM accompanied with CKD diagnosis code, ICD-9-CM codes 585 and 586) during the study period were allocated to the CHM group; those who did not receive any CHM treatment during the study period were allocated to the non-CHM group. The index date for the CHM group was the first date of taking CHM because of the CKD diagnosis, and the index date of the non-CHM group was randomly assigned a date between CKD diagnosis date and 31 December 2013. We excluded patients who were under 18 years of age, experienced a stroke (ischemic stroke or hemorrhage stroke) before the index date, had dialysis history before the index date (possible history of CKD), and had IS occurring during the first 6 months after CKD diagnosis date. Additionally, we conducted propensity score matching at a ratio of 1:1 cohort sample by age (per 5 years-groups), gender, index year, comorbidities and medication to balance the basic characteristics of two groups.
The main outcome of the study was IS (ICD-9-CM codes 433–437). We followed patients until IS occurred, death, loss to follow-up or 31 December 2013. Death was considered as the competing event; loss to follow-up and the end of this study were considered as censored events.
Baseline comorbidity was defined as comorbid disease with at least three outpatient visits or at least 1 inpatient visit before the index date within 1 year. According to the recommendation of the previous study, hypertension (ICD-9-CM codes 401–405), diabetes mellitus (ICD-9-CM code 250), hyperlipidemia (ICD-9-CM code 272), and atrial fibrillation (ICD-9-CM code 427.31) are thought to be the traditional risk factors for patients with CKD (Kelly and Rothwell, 2020). In addition, chronic obstruction pulmonary disease (COPD, ICD-9-CM codes 491, 492, and 496), chronic liver disease and cirrhosis (ICD-9-CM code 571), coronary artery disease (ICD-9-CM codes 410–414), and cancer (ICD-9-CM codes 140–280) were also included as the covariates. We considered the possible effect of medications for risk of IS as follows: diabetic medications, antihypertensive medications, anti-lipid medications, non-steroidal anti-inflammatory drugs (NSAIDs), steroid, and antiplatelet or anticoagulation agents. Furthermore, a sensitivity analysis was conducted to assess the robustness of the findings. Originally, we excluded patients who had IS occurring during the first 6 months after CKD diagnosis date. For the sensitivity analysis, we extended this period of case exclusion to 12 months and evaluated the impact of longer induction time on the incidence rate of IS between two groups.
Continuous variables are reported as mean and standard deviation, whereas categorical variables are reported as frequencies and percentage. We used standardized mean difference to compare balance of basic characteristics and potential confounders between the two groups, and a value of <0.1 indicates a negligible difference between the two groups. Considering the presence of competing risk, we used the proportional subdistribution hazards model of Fine and Gray to examine the effect of CHM on the risk of IS, reporting as hazard ratio (HR) and 95% confidence interval (CI). A multivariable model was performed by controlling for potential confounding variables, such as gender, age, comorbidities of hypertension, diabetes mellitus, hyperlipidemia, atrial fibrillation, COPD, chronic liver disease and cirrhosis, chronic artery disease, cancer, and the use of diabetes medications, antihypertensive medications, anti-lipid medications, steroid, NSAIDs, and antiplatelet or anticoagulation agents. We applied cumulative incidence function to assess the cumulative incidence rate of IS between the two groups. The Gray’s test (Williamson et al., 2007) was used to compare the differences between the two groups. In addition, subsequent subgroup analysis was performed to examine the effect of cumulative CHM usage days. We stratifised the patients in the CHM group into three subgroups: cumulative CHM usage days ≤90 days, 91–180 days, and >180 days. All statistics significances were set at a p < 0.05 and the SAS 9.4 (SAS Institute Inc. Cary, NC) was used for the statistical analysis.
We identified 21,641 patients diagnosed with CKD during the years 2003–2012. According to the exclusion criteria, 11,816 patients were excluded. A total of 6,299 patients received CHM because of CKD diagnosis, and 3,529 patients received conventional treatment only. After matching with propensity score at a ratio of 1:1 cohort sample by age (per 5 years-groups), gender, index year, comorbidities and medication, there were 3,149 patients in either the CHM group or the non-CHM group. The sampling procedure is presented in Figure 1.
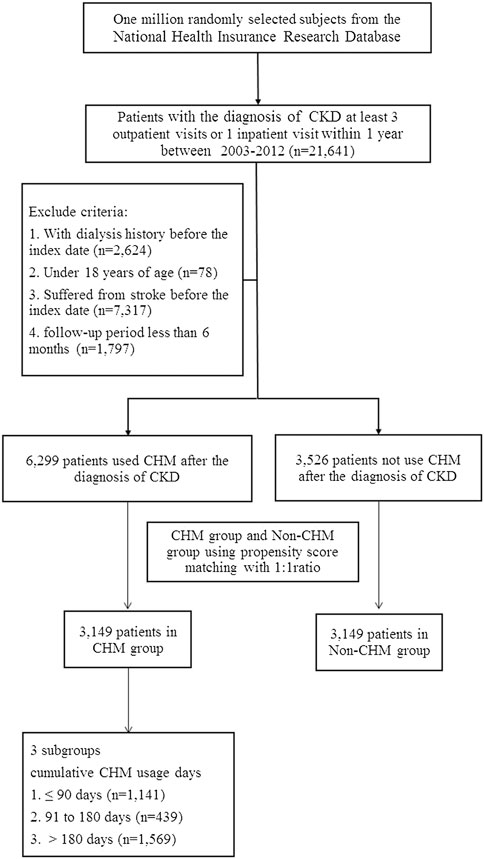
FIGURE 1. Study flowchart of patients with chronic kidney disease. After excluding patients not fitting inclusion criteria, CHM and non-CHM groups comprised 3,732 patients at a ratio of 1:1 cohort sample for propensity score matching.
Table 1 shows the demographic characteristics, comorbidities, and confounding medications of the study patients. There was no difference between the two groups with regard to gender, age comorbidities, and medications (standardized mean difference <0.1). The mean follow-up period of the CHM group was longer than that of the non-CHM group [3.96 (2.78) years vs. 2.90 (2.35) years; standardized mean difference = 0.412]. The period from index date to IS date was also longer in CHM group than that in non-CHM group [3.13 (2.37) years vs. 2.28 (1.73) years; standardized mean difference = 0.407].
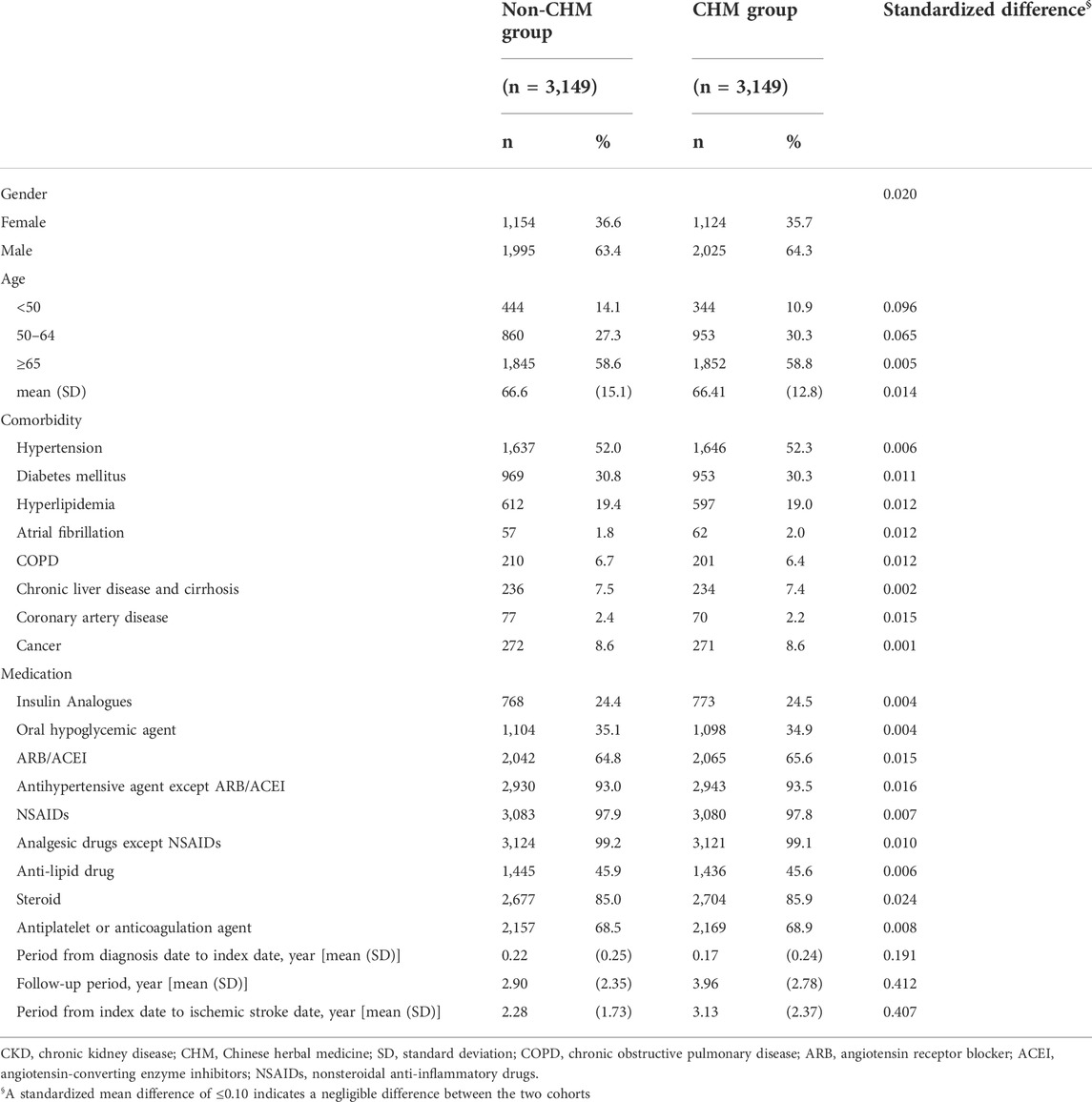
TABLE 1. Characteristics of patients with chronic kidney disease classified according to the use of Chinese herbal medicine after matching with propensity score.
Overall, a total of 434 patients developed IS during the follow-up period; the incidence rates of IS in the CHM and non-CHM group was 16.05 per 1000 person-years and 25.65 per 1000 person-years, respectively (Table 2). As shown in Figure 2, the cumulative incidence function demonstrated that the cumulative incidence of IS in the CHM group was significantly lower than that in the non-CHM group (Gray’s test, p = 0.02). Additionally, the risk of IS was significantly lower in the CHM group than that in the non-CHM group (crude HR: 0.62, 95% CI: 0.51–0.75). After multivariate adjustment, the adjusted HR (aHR) for the risk of IS among patients with CKD taking CHM as add-on therapy remained significantly lower (aHR: 0.58, 95% CI: 0.48–0.70). After stratification by gender, both male and female patients with CKD treated with CHM were significantly associated with a reduced risk of IS, and the risk of IS was much lower in female patients (aHR: 0.49, 95% CI: 0.35–0.69) than that in male patients (aHR: 0.63, 95% CI: 0.50–0.80). Furthermore, patients with CKD aged ≥65 years who received CHM had significantly lower IS risk compared with patients of the same age not receiving CHM (aHR: 0.55, 95% CI: 0.44–0.69). Regarding comorbidities, CKD patients with the traditional IS risk factors, such as hypertension, diabetes mellitus, and hyperlipidemia receiving CHM treatment were associated with a 45%–52% reduced risk of IS compared to those not treated with CHM (aHR: 0.48, 0.53, 0.55, respectively). Moreover, in the stratification analysis of the medication, CKD patients receiving the CHM in combination with conventional medications showed a trend of reduced risk of IS compared with those receiving conventional medications only (Table 2).

TABLE 2. Incidence rates, hazard ratio and confidence intervals of ischemic stroke among chronic kidney disease patients with and without Chinese herbal medicine usage in the stratification of gender, age, comorbidities and medication.
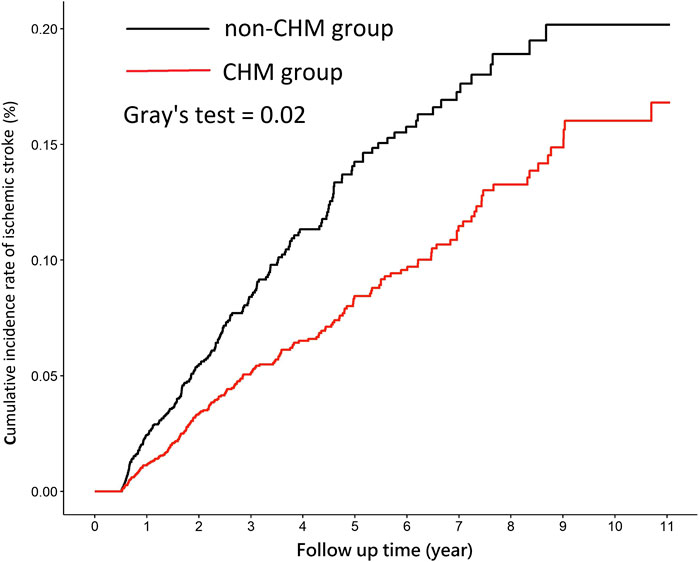
FIGURE 2. Cumulative incidence rate of ischemic stroke among patients with CKD in the CHM and non-CHM group. Abbreviate: CKD, chronic kidney disease; CHM, Chinese herbal medicine.
Table 3 shows the results of the subgroup analysis according to the cumulative usage days of CHM among patients with CKD. Compared to the non-CHM group, there was a significant association between the reduced risk of IS and receiving CHM for more than 180 days (aHR = 0.51, 95% CI = 0.41–0.63).
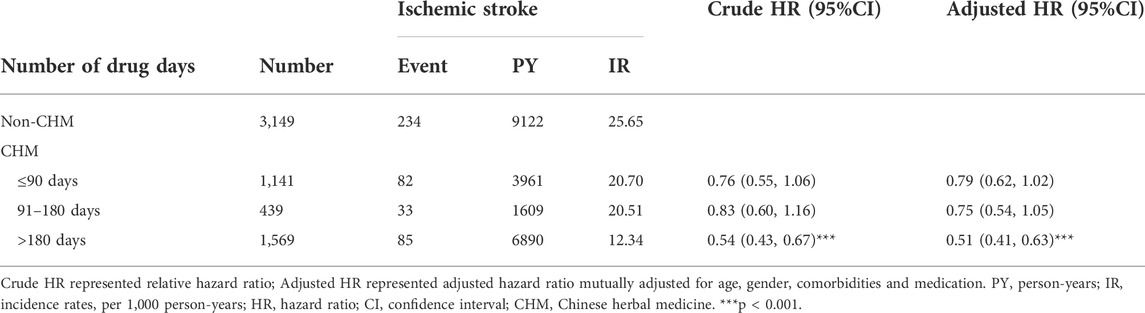
TABLE 3. Hazard Ratios and 95% confidence intervals of ischemic stroke risk associated with the cumulative usage days of CHM during the follow-up period among patients with chronic kidney disease.
The top three single herbs prescribed for CKD patients were Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan- Shen)], Rheum palmatum L [Polygonaceae; Rhei Radix et Rhizoma (Da-Huang)] and Astragalus membranaceus Bunge [Fabaceae; Astragali Radix (Huang-Qi)] and the three most commonly prescribed formulae were Ji-Sheng-Shen-Qi-Wan, Liu-Wei-Di-Huang-Wan, and Zhen-Wu-Tang (The information about composition and processing were shown in Supplementary Table S1). Further analysis using the proportional subdistribution hazards model of Fine and Gray revealed that Ji-Sheng-Shen-Qi-Wan, Liu-Wei-Di-Huang-Wan, and Zhen-Wu-Tang were significantly associated with a reduced risk of IS (Table 4).
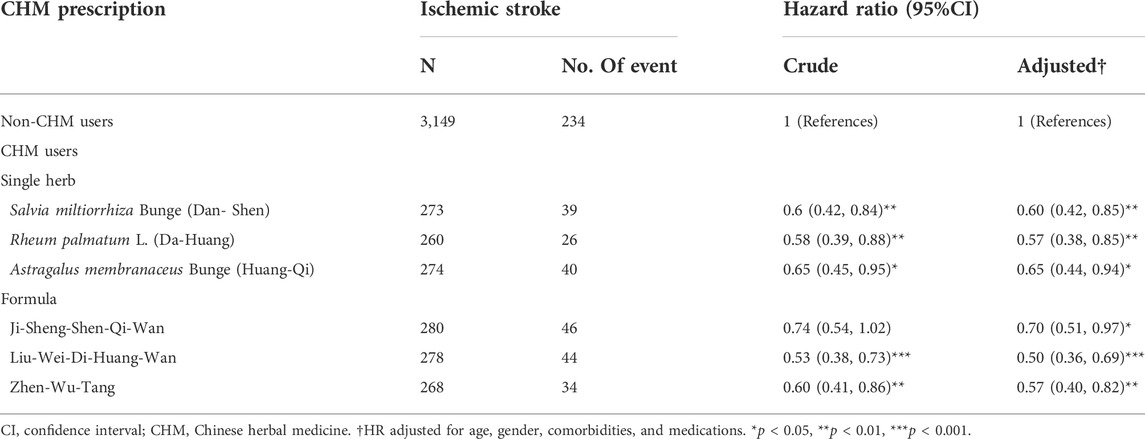
TABLE 4. Hazard Ratios and 95% confidence intervals of ischemic stroke risk associated with the top three most commonly prescribed single herbs and formulas among patients with chronic kidney disease.
In the sensitivity analysis of extending the period of case exclusion from 6 to 12 months, there were 2,808 patients in both the CHM group and non-CHM group after matching with propensity score at a ratio of 1:1 cohort sample by age (per 5 years-groups), gender, index year, comorbidities and medication. The basic characteristics in each group were similar with all standardized mean difference values < 0.1 (Table 5). The incidence rates of IS in the CHM and non-CHM group was 14.09 per 1000 person-years and 18.88 per 1000 person-years, respectively, and we found a 38% lower risk of IS in CHM group than in non-CHM group (aHR = 0.62, 95% CI: 0.50–0.77) (Table 6). In addition, both male and female patients with CKD receiving CHM as add-on therapy were significantly associated with a lower risk of IS [aHR (95% CI): 0.71 (0.54–0.94), 0.60 (0.41–0.87), respectively]. Moreover, Patients with CKD aged ≥65 years who received CHM had a significantly reduced IS risk compared with patients of the same age not receiving CHM (aHR: 0.66, 95% CI: 0.51–0.86). Figure 3 (extending the period of case exclusion from 6 to 12 months) displayed that the cumulative incidence rate of IS in the CHM group was significantly lower than that in the non-CHM group (Gray’s test, p = 0.02).
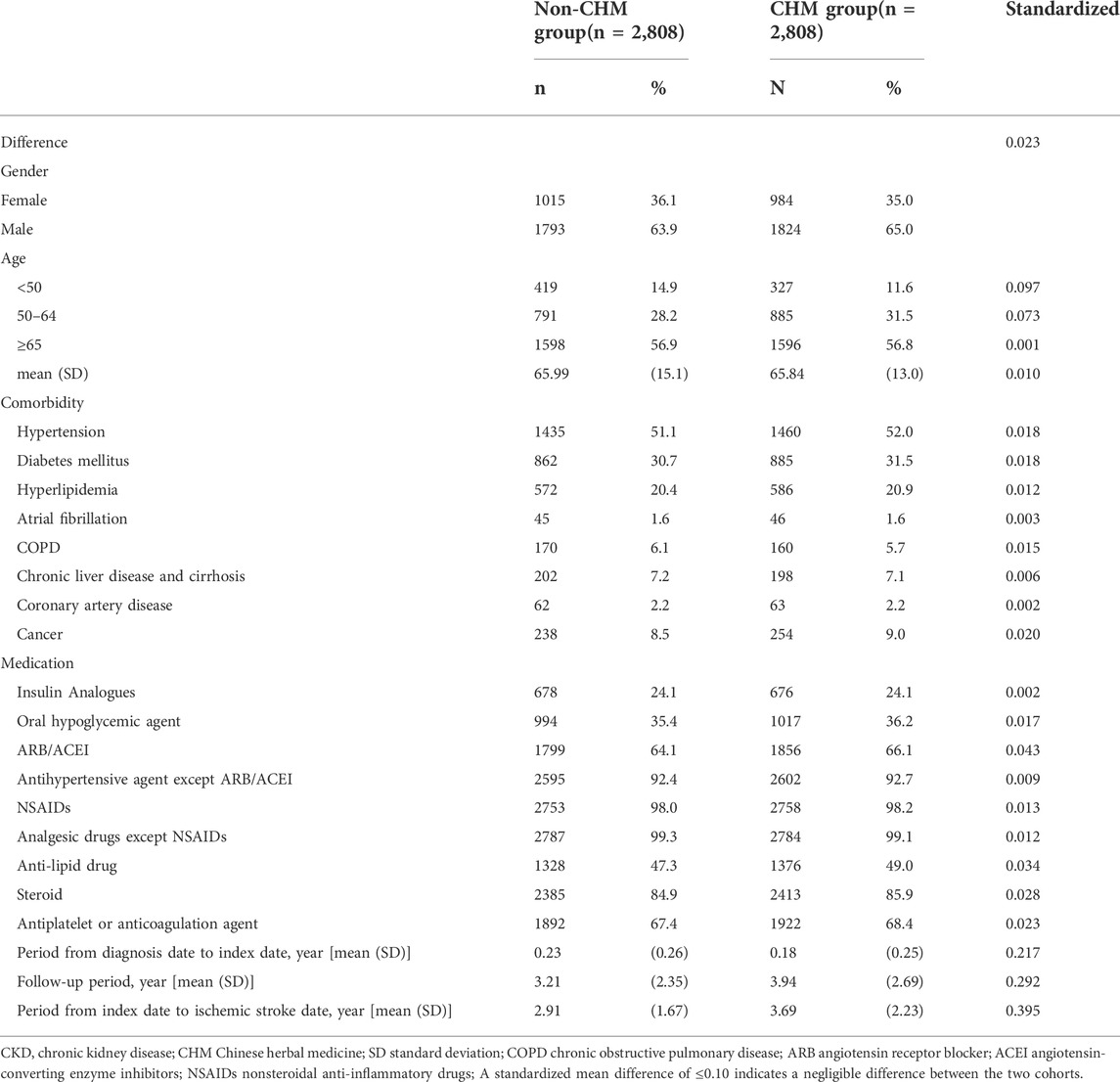
TABLE 5. Characteristics of patients with chronic kidney disease classified according to the use of Chinese herbal medicine after matching (extending the period of case exclusion from 6 months to 12 months).
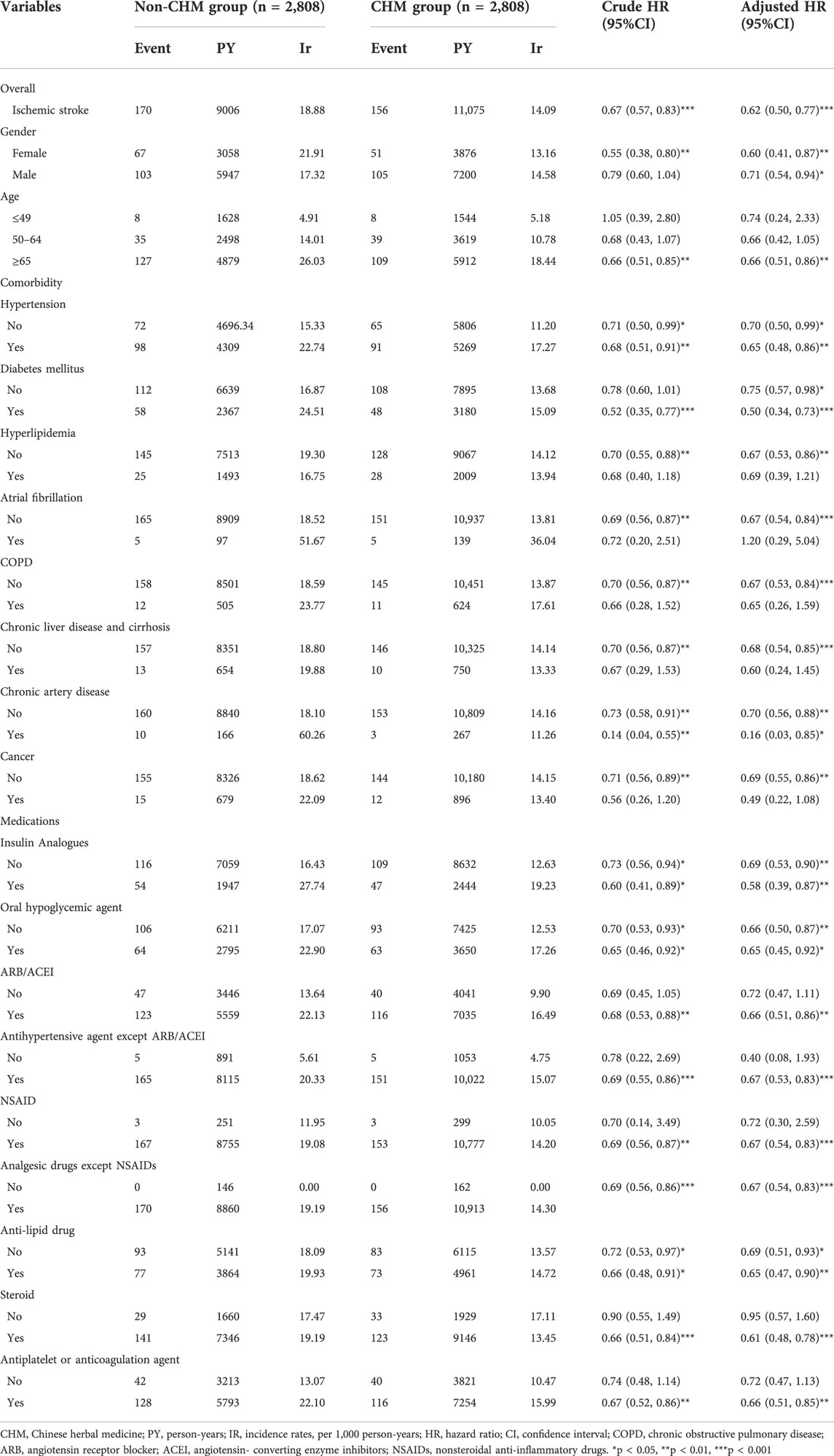
TABLE 6. Incidence rates, hazard ratio and confidence intervals of ischemic stroke among chronic kidney disease patients with and without Chinese herbal medicine usage in the stratification of gender, age, comorbidities and medication (extending the period of case exclusion from 6 to 12 months).
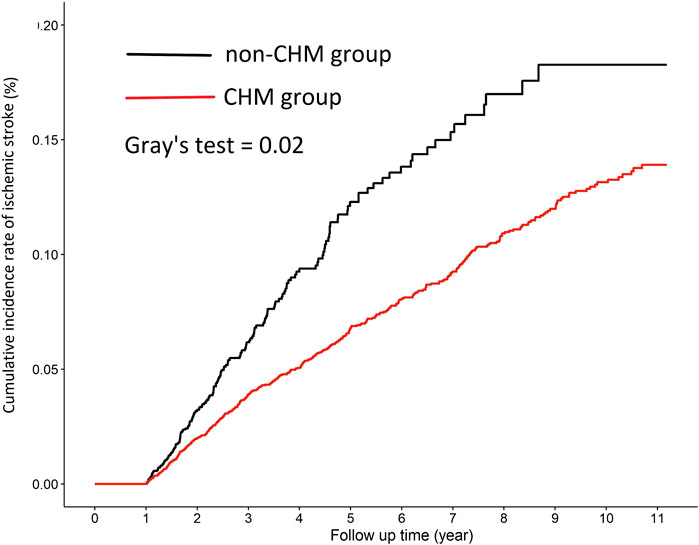
FIGURE 3. Cumulative incidence rate of ischemic stroke among patients with CKD in the CHM and non-CHM group (extending the period of case exclusion from 6 to 12 months).
This nationwide cohort study using real-world data revealed that the use of CHM as add-on therapy was associated with a lower risk of IS among patients with CKD. In the subgroup analysis of different cumulative CHM usage days, we identified an association between longer CHM usage (>180 days) and a reduced risk of IS. To date, few studies have examined conventional medicine along with CHM as adjunctive therapy in relation to the risk of IS among patients with CKD. This study used a large-scale nationwide cohort to address this knowledge gap.
Although the precise mechanism was not clear, multiple factors may contribute to the development of IS among CKD patients. The possible explanation might be that the commonly prescribed CHM attenuates inflammation response and oxidative stress to block the arteriosclerosis progression. Liu-Wei-Di-Huang-Wan was shown to prevent the progression of renal fibrosis by inhibiting the NF-κB pathway in rats with diabetic nephropathy (Xu et al., 2017). Moreover, Zhen-Wu-Tang was demonstrated to have a protective effect against renal fibrosis by alleviating oxidative stress. After treatment with Zhen-Wu-Tang, reactive oxygen species decreased in the kidney and peroxisome proliferator-activated receptor gamma (PPARγ) was up-regulated. PPARγ had anti-inflammatory and anti-fibrosis effects by inhibiting the expression of transforming growth factor beta 1 (TGF-β1) and NF-κB, an important factor in the atherosclerotic process (Li et al., 2018). Astragalus membranaceus Bunge [Fabaceae; Astragali Radix (Huang-Qi)] and Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan-Shen)], the most commonly prescribed single herbs, have also been reported to attenuate kidney injury via anti-inflammatory effects by suppressing the activation of NF-κB signaling pathways in the animal model (Cai et al., 2018; Du et al., 2018). Rheum palmatum L [Polygonaceae; Rhei Radix et Rhizoma (Da-Huang)] has been shown to have effects of attenuating renal inflammatory injury through decreasing the level of certain proinflammatory cytokines, including prostaglandin E, tumor necrosis factor-α, and TGF-β1 (Meng et al., 2015; Hu et al., 2020). The commonly used CHM, via mitigating inflammation response and oxidative stress, was associated with a decreased risk of IS among patients with CKD.
Besides suppressing inflammation and oxidative stress leading to vascular fibrosis or arteriosclerosis, some commonly prescribe CHM has been demonstrated to prevent indoxyl sulfate (a uremic toxin)-induced endothelial dysfunction. For examples, previous investigators (Yamabe et al., 2005) have demonstrated that Ji-Sheng-Shen-Qi-Wan could decrease the level of uremic toxins and hydroxyl radicals to ameliorate renal damage and failure in a subtotal nephrectomy rat model. Ji-Sheng-Shen-Qi-Wan also could reduce interstitial fibrosis and inflammation significantly (Yamabe et al., 2005). Moreover, Astragaloside IV, one of the major compounds of Astragalus membranaceus Bunge [Fabaceae; Astragali Radix (Huang-Qi)], was shown to alleviate indoxyl sulfate-induced kidney injury through suppressing oxidative stress response (Ji et al., 2018). Salvianolic acids, the most effective and abundant compounds extracted from Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan-Shen)] could significantly enhance the dialysis removal of protein-bound indoxyl sulfate (Li et al., 2019). In addition, Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan-Shen)] has also been found to inhibit the elevation of indoxyl sulfate, which is thought to accelerate atherogenesis in patients with CKD (Li et al., 2019; Nakano et al., 2019). Furthermore, over 50% of patients with CKD are known to have multiple comorbidities including hypertension, diabetes mellitus, and hyperlipidemia that may negatively impact IS (Kelly et al., 2021). Certain commonly prescribed CHM, such as Liu-Wei-Di-Huang-Wan, Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan-Shen)] and Astragalus membranaceus Bunge [Fabaceae; Astragali Radix (Huang-Qi)] have been shown to confer benefits in ameliorating these comorbidities (Wang J. et al., 2012; Agyemang et al., 2013; Wang et al., 2017; Gao et al., 2018) thus contributing to the reduction in IS risk. Accordingly, this might be the possible reason that CKD patients comorbid with traditional risk factors of IS taking CHM have a greatly reduced risk of IS than those not taking CHM. Collectively, certain formulae and single herbs taken by patients with CKD might exert anti-inflammatory effects, inhibit oxidative stress response, reduce damages by uremic toxins, and alleviate comorbidity to mitigate the risk of IS. The proposed mechanisms for the benefit of commonly used CHM are described in Figure 4.
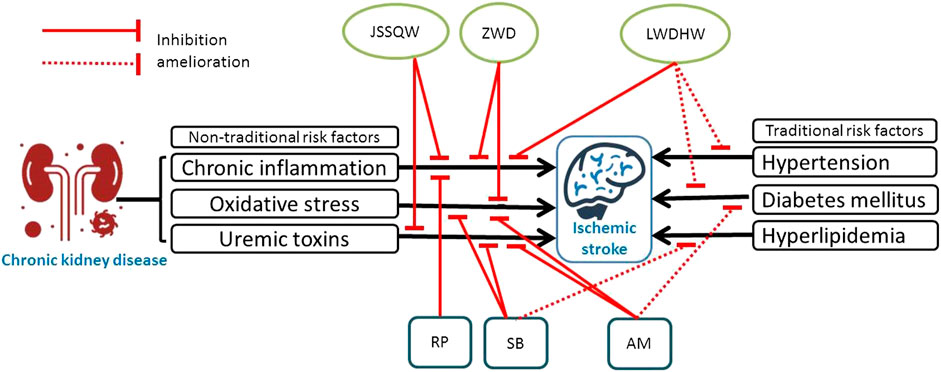
FIGURE 4. Schematic diagram illustrating the proposed mechanisms for the benefit of commonly prescribed CHM in reducing the risk of ischemic stroke.
Another major finding in our study was that the use of CHM for more than 180 days was associated with a lower risk of IS in the CHM group. It seems possible that CHM required at least 180 days to achieve an adequate protective effect in patients with CKD. Although no firm evidence indicated the minimum cumulative usage days for renal protection in CHM, the minimum effective usage days of CHM in our study was similar to the treatment duration of certain randomized controlled trials. Patients with primary glomerular disease, the most common type of CKD, receiving Abelmoschus manihot (L.) Medik [Malvaceae; Abelmoschi Corolla (Huang-Shu-Kui)] combined with losartan for 24 weeks showed a more reduction in 24-hour proteinuria than those taking losartan alone (Zhang et al., 2014). In addition, compared with taking benazepril alone, patients with stage 3 CKD taking CHM combined with benazepril for 24 weeks had lower 24-hour proteinuria levels and higher eGFR values (Wang Y. J. et al., 2012). A previous study confirmed that decreased eGFR was one of the main risk factors of IS (Synhaeve et al., 2016). In brief, CKD is characterized by increased oxidative stress and chronic systemic inflammation, and taking CHM as add-on therapy for >180 days might exert an adequate anti-inflammatory and anti-oxidative effect to reduce the risk of IS among CKD patients. Moreover, our analysis reveals that the CHM-related reduction in IS risk was more apparent in CKD patients aged ≥65 years compared to other age groups. The possible reason for this observation is that CKD patients aged ≥65 years are known to have many traditional risk factors of IS that could substantially elevate the risk of IS. (Peng et al., 2011; Liang et al., 2020; Tsao et al., 2021). CHM may exert a potential effect in ameliorating the impact of comorbidities (Wang J. et al., 2012; Agyemang et al., 2013; Wang et al., 2017; Gao et al., 2018) thus conducing to the decreased risk of IS in this age group.
The Yin-Yang theory of traditional Chinese medicine may explain why clinical doctors choose those herbs as CKD treatments. CKD is characterized by three syndromes based on the theory of Chinese medicine, syndrome of Yang deficincy and water overflowing, syndrome of Qi deficiency and blood stasis, and syndrome of kidney Yin deficincy (Wang et al., 2016). The clinical symptom of Yang deficiency and water overflowing in CKD patients is swelling over lower extremities. The commonly prescribed formulae such as Ji-Sheng-Shen-Qi-Wan and Zhen-Wu-Tang could exert the function of activating Yang and promoting diuresis to alleviate the swelling. In addition, the typical feature of Qi deficiency and blood stasis in CKD patients is fatigue. Certain single herbs including Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae Radix et Rhizoma (Dan-Shen)], Rheum palmatum L [Polygonaceae; Rhei Radix et Rhizoma (Da-Huang)] and Astragalus membranaceus Bunge [Fabaceae; Astragali Radix (Huang-Qi)] have the potential to enrich Qi and remove blood stasis to invigorate these patients. Furthermore, the clinical signs of kidney Yin deficiency in CKD patients are dizziness, tinnitus, and oliguria. The second most commonly prescribed formula, Liu-Wei-Di-Huang-Wan, could nourish kidney Yin to ameliorate the associated signs. Our findings provide evidence suggesting that those herbs may lower the IS risk in CKD patients, a benefit that is beyond the relief of clinical symptoms.
The strength of our study was using large-scale real-world data with longitudinal follow-up. Compared to randomized clinical trials, real world studies had broader generalizability and give evidence of effectiveness in daily practice settings (Blonde et al., 2018). The study also had limitations which may have affected results. First, important clinical characteristics, such as smoking, body mass index, diet, exercise habits, and eGFR were unavailable from our database. However, we applied the proportional subdistribution hazards model of Fine and Gray by controlling for the available potential confounding factors of IS, including age, gender, comorbidities, and medications, to make the two groups comparable. Second, there was a possibility of misclassification bias in the disease coding. To reduce the bias, we identified patients with CKD through at least three outpatient visits or one inpatient visit within 1 year, and patients who were diagnosed with IS through at least three outpatient visits or one inpatient visit. Furthermore, the accuracy of the NHIRD for patients with a diagnosis of IS and CKD is high, and the database we used is a valid resource for this research (Cheng et al., 2011; Lin et al., 2015). Third, medications compliance should be noted. We supposed that all of the CHM prescribed was taken by the patients, but the actual dosage taken might have been overestimated due to poor compliance. The compliance is likely to be decreased over time especially in the case of a long follow-up period. Poor compliance may be associated with a higher risk of IS among patients with CKD, thus supporting the robustness of our findings. Last, the present study investigated patients with CKD in Taiwan; thus, the application of the study findings to populations of other countries or races is inadequate. Forth, we noted that the IS risk in female patients with CKD who used CHM was much lower than that in male patients with CKD who used CHM. The exact reasons for this difference remain unclear, but it is known that many physiologic and pathophysiologic aspects of females and males are different.
In this real-world, nationwide cohort study, the use of CHM as add-on therapy for patients with CKD was associated with a decreased risk of IS compared to using conventional treatment alone. In particular, CKD patients taking CHM for >180 days had a significantly lower risk of IS. Additionally, Ji-Sheng-Shen-Qi-Wan, Liu-Wei-Di-Huang-Wan, and Zhen-Wu-Tang might be associated with a 30%–50% reduced risk of IS. Although adjunctive CHM may have beneficial effects for IS prevention in patients with CKD, further randomized clinical trials are required to clarify the causal relationship of these results. Also, patients with other chronic inflammatory diseases such as rheumatoid arthritis (Tam et al., 2018; Tang et al., 2019) also have a high risk of IS. Whether adjunctive CHM may have beneficial effects for IS prevention in these patients warrant further investigation.
The datasets presented in this article are not readily available because the datasets is limited to research purposes only. The datasets we analyzed from NHIRD was provided by the National Health Insurance Administration and maintained by the National Health Research Institutes of Taiwan. The use of NHIRD is limited to research purposes only. Applicants must follow the Computer-Processed Personal Data Protection Law and related regulations of National Health Insurance Administration and National Health Research Institutes. Requests to access the datasets should be directed to National Health Insurance Administration, Ministry of Health and Welfare, Taiwan, nhird@nhri.edu.tw.
The studies involving human participants were reviewed and approved by Institutional Review Board of the China Medical University (CMUH104-REC2–115) [CR-6]. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
H-SS was responsible for the study’s conception and design, reviewing and interpreting the data, and drafting the manuscript. C-YH and I-HL was responsible for modifying the study design, interpreting the data, and the critical revision. H-TY contributed to the collection and analysis of the data. I-HL supervised the project, contributed to conception and design of the study and finalized the manuscript. H-SS, C-YH, H-TY and I-HL were responsible for the final approval of the revised manuscript. All authors read and approved the final manuscript.
The authors are grateful to YK for his valuable suggestions for the preparation of this manuscript. This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212–114004), MOST Clinical Trial Consortium for Stroke (MOST 109–2321-B-039–002), China Medical University Hospital (DMR-110–222), Tseng-Lien Lin Foundation, Taichung, Taiwan.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor JW and reviewer RC declared a past co-authorship with the authors H-TY, C-YH.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.883148/full#supplementary-material
Abramson, J. L., Jurkovitz, C. T., Vaccarino, V., Weintraub, W. S., and McClellan, W. (2003). Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: The ARIC study. Kidney Int. 64 (2), 610–615. doi:10.1046/j.1523-1755.2003.00109.x
Agyemang, K., Han, L., Liu, E., Zhang, Y., Wang, T., Gao, X., et al. (2013). Recent advances in Astragalus membranaceus anti-diabetic research: Pharmacological effects of its phytochemical constituents. Evid. Based. Complement. Altern. Med. 2013, 654643. doi:10.1155/2013/654643
Akyol, A. D., Yildirim, Y., Toker, E., and Yavuz, B. (2011). The use of complementary and alternative medicine among chronic renal failure patients. J. Clin. Nurs. 20 (7-8), 1035–1043. doi:10.1111/j.1365-2702.2010.03498.x
Benigni, A., Cassis, P., and Remuzzi, G. (2010). Angiotensin II revisited: New roles in inflammation, immunology and aging. EMBO Mol. Med. 2 (7), 247–257. doi:10.1002/emmm.201000080
Blonde, L., Khunti, K., Harris, S. B., Meizinger, C., and Skolnik, N. S. (2018). Interpretation and impact of real-world clinical data for the practicing clinician. Adv. Ther. 35 (11), 1763–1774. doi:10.1007/s12325-018-0805-y
Cai, H., Su, S., Li, Y., Zeng, H., Zhu, Z., Guo, J., et al. (2018). Protective effects of Salvia miltiorrhiza on adenine-induced chronic renal failure by regulating the metabolic profiling and modulating the NADPH oxidase/ROS/ERK and TGF-β/Smad signaling pathways. J. Ethnopharmacol. 212, 153–165. doi:10.1016/j.jep.2017.09.021
Chelluboina, B., and Vemuganti, R. (2019). Chronic kidney disease in the pathogenesis of acute ischemic stroke. J. Cereb. Blood Flow. Metab. 39 (10), 1893–1905. doi:10.1177/0271678x19866733
Cheng, C. L., Kao, Y. H., Lin, S. J., Lee, C. H., and Lai, M. L. (2011). Validation of the national health insurance research database with ischemic stroke cases in taiwan. Pharmacoepidemiol. Drug Saf. 20 (3), 236–242. doi:10.1002/pds.2087
Deanfield, J. E., Halcox, J. P., and Rabelink, T. J. (2007). Endothelial function and dysfunction: Testing and clinical relevance. Circulation 115 (10), 1285–1295. doi:10.1161/circulationaha.106.652859
Du, N., Xu, Z., Gao, M., Liu, P., Sun, B., Cao, X., et al. (2018). Combination of Ginsenoside Rg1 and Astragaloside IV reduces oxidative stress and inhibits TGF-β1/Smads signaling cascade on renal fibrosis in rats with diabetic nephropathy. Drug Des. devel. Ther. 12, 3517–3524. doi:10.2147/dddt.s171286
Gao, X., Shang, J., Liu, H., and Yu, B. (2018). A meta-analysis of the clinical efficacy of TCM decoctions made from formulas in the liuwei dihuang wan categorized formulas in treating diabetic nephropathy proteinuria. Evid. Based. Complement. Altern. Med., 2427301. doi:10.1155/2018/2427301
Grams, M. E., Yang, W., Rebholz, C. M., Wang, X., Porter, A. C., Inker, L. A., et al. (2017). Risks of adverse events in advanced CKD: The chronic renal insufficiency cohort (CRIC) study. Am. J. Kidney Dis. 70 (3), 337–346. doi:10.1053/j.ajkd.2017.01.050
Hu, J., Yang, Z., Wu, H., and Wang, D. (2020). Rhein attenuates renal inflammatory injury of uric acid nephropathy via lincRNA-Cox2/miR-150-5p/STAT1 axis. Int. Immunopharmacol. 85, 106620. doi:10.1016/j.intimp.2020.106620
Ji, C., Luo, Y., Zou, C., Huang, L., Tian, R., Lu, Z., et al. (2018). Effect of astragaloside IV on indoxyl sulfate-induced kidney injury in mice via attenuation of oxidative stress. BMC Pharmacol. Toxicol. 19 (1), 53. doi:10.1186/s40360-018-0241-2
Jing, W., Jabbari, B., and Vaziri, N. D. (2018). Uremia induces upregulation of cerebral tissue oxidative/inflammatory cascade, down-regulation of Nrf2 pathway and disruption of blood brain barrier. Am. J. Transl. Res. 10 (7), 2137–2147.
Kelly, D. M., Ademi, Z., Doehner, W., Lip, G. Y. H., Mark, P., Toyoda, K., et al. (2021). Chronic kidney disease and cerebrovascular disease: Consensus and guidance from a KDIGO controversies conference. Stroke 52 (7), e328–e346. doi:10.1161/strokeaha.120.029680
Kelly, D. M., and Rothwell, P. M. (2019). Does chronic kidney disease predict stroke risk independent of blood pressure? A systematic review and meta-regression. Stroke 50 (11), 3085–3092. doi:10.1161/strokeaha.119.025442
Kelly, D. M., and Rothwell, P. M. (2020). Prevention and treatment of stroke in patients with chronic kidney disease: An overview of evidence and current guidelines. Kidney Int. 97 (2), 266–278. doi:10.1016/j.kint.2019.09.024
Lano, G., Burtey, S., and Sallée, M. (2020). Indoxyl sulfate, a uremic endotheliotoxin. Toxins (Basel) 12 (4), E229. doi:10.3390/toxins12040229
Levin, A., Tonelli, M., Bonventre, J., Coresh, J., Donner, J. A., Fogo, A. B., et al. (2017). Global kidney health 2017 and beyond: A roadmap for closing gaps in care, research, and policy. Lancet 390 (10105), 1888–1917. doi:10.1016/s0140-6736(17)30788-2
Li, J., Wang, Y., Xu, X., Cao, W., Shen, Z., Wang, N., et al. (2019). Improved dialysis removal of protein-bound uremic toxins by salvianolic acids. Phytomedicine 57, 166–173. doi:10.1016/j.phymed.2018.12.018
Li, S., Xiao, X., Han, L., Wang, Y., and Luo, G. (2018). Renoprotective effect of Zhenwu decoction against renal fibrosis by regulation of oxidative damage and energy metabolism disorder. Sci. Rep. 8 (1), 14627. doi:10.1038/s41598-018-32115-9
Liang, C. C., Hsu, W. C., Tsai, Y. T., Weng, S. J., Liu, S. C., Lin, C. H., et al. (2020). Factors related to diabetes mellitus in the middle-aged and over in taiwan. Healthc. (Basel) 8 (3), E242. doi:10.3390/healthcare8030242
Lin, L., Wang, Q., Yi, Y., Wang, S., and Qiu, Z. (2016). Liuwei dihuang pills enhance the effect of western medicine in treating diabetic nephropathy: A meta-analysis of randomized controlled trials. Evid. Based. Complement. Altern. Med. 2016, 1509063. doi:10.1155/2016/1509063
Lin, M. Y., Chiu, Y. W., Chang, J. S., Lin, H. L., Lee, C. T., Chiu, G. F., et al. (2015). Association of prescribed Chinese herbal medicine use with risk of end-stage renal disease in patients with chronic kidney disease. Kidney Int. 88 (6), 1365–1373. doi:10.1038/ki.2015.226
Ma, Y., Zhou, L., Dong, J., Zhang, X., and Yan, S. (2015). Arterial stiffness and increased cardiovascular risk in chronic kidney disease. Int. Urol. Nephrol. 47 (7), 1157–1164. doi:10.1007/s11255-015-1009-x
Markell, M. S. (2005). Potential benefits of complementary medicine modalities in patients with chronic kidney disease. Adv. Chronic Kidney Dis. 12 (3), 292–299. doi:10.1016/j.ackd.2005.03.004
Meng, Z., Yan, Y., Tang, Z., Guo, C., Li, N., Huang, W., et al. (2015). Anti-hyperuricemic and nephroprotective effects of rhein in hyperuricemic mice. Planta Med. 81 (4), 279–285. doi:10.1055/s-0034-1396241
Nakano, T., Katsuki, S., Chen, M., Decano, J. L., Halu, A., Lee, L. H., et al. (2019). Uremic toxin indoxyl sulfate promotes proinflammatory macrophage activation via the interplay of OATP2B1 and dll4-notch signaling. Circulation 139 (1), 78–96. doi:10.1161/circulationaha.118.034588
Olesen, J. B., Lip, G. Y., Kamper, A. L., Hommel, K., Køber, L., Lane, D. A., et al. (2012). Stroke and bleeding in atrial fibrillation with chronic kidney disease. N. Engl. J. Med. 367 (7), 625–635. doi:10.1056/NEJMoa1105594
Osman, N. A., Hassanein, S. M., Leil, M. M., and NasrAllah, M. M. (2015). Complementary and alternative medicine use among patients with chronic kidney disease and kidney transplant recipients. J. Ren. Nutr. 25 (6), 466–471. doi:10.1053/j.jrn.2015.04.009
Palmer, S. C., Di Micco, L., Razavian, M., Craig, J. C., Perkovic, V., Pellegrini, F., et al. (2013). Antiplatelet agents for chronic kidney disease. Cochrane Database Syst. Rev. (2), Cd008834. doi:10.1002/14651858.CD008834.pub2
Peng, L.-N., Liu, C.-L., Lin, M.-H., Hwang, S.-J., and Chen, L.-K. (2011). Nondiabetic older adults with untreated hypertension in Taiwan: Treatment implication in elderly hypertension. J. Clin. Gerontology Geriatrics 2 (2), 58–61. doi:10.1016/j.jcgg.2011.03.003
Synhaeve, N. E., van Alebeek, M. E., Arntz, R. M., Maaijwee, N. A., Rutten-Jacobs, L. C., Schoonderwaldt, H. C., et al. (2016). Kidney dysfunction increases mortality and incident events after young stroke: The FUTURE study. Cerebrovasc. Dis. 42 (3-4), 224–231. doi:10.1159/000444683
Tam, H. W., Chen, C. M., Leong, P. Y., Chen, C. H., Li, Y. C., Wang, Y. H., et al. (2018). Methotrexate might reduce ischemic stroke in patients with rheumatoid arthritis: A population-based retrospective cohort study. Int. J. Rheum. Dis. 21 (8), 1591–1599. doi:10.1111/1756-185x.13267
Tang, C. H., Yu, F., Huang, C. Y., and Chen, D. Y. (2019). Potential benefits of biologics on stroke and mortality in patients with rheumatoid arthritis: A nationwide population-based cohort study in taiwan. Int. J. Rheum. Dis. 22 (8), 1544–1552. doi:10.1111/1756-185x.13611
Tsagalis, G., Akrivos, T., Alevizaki, M., Manios, E., Stamatellopoulos, K., Laggouranis, A., et al. (2009). Renal dysfunction in acute stroke: An independent predictor of long-term all combined vascular events and overall mortality. Nephrol. Dial. Transpl. 24 (1), 194–200. doi:10.1093/ndt/gfn471
Tsao, C. F., Chang, C. M., Weng, S. W., Wang, P. W., Lin, C. Y., Lu, S. N., et al. (2021). Identifying endemic areas and estimating the prevalence of hyperlipidemia in Taiwan's townships. J. Formos. Med. Assoc. 120 (1), 460–465. doi:10.1016/j.jfma.2020.05.031
Wang, J., Yao, K., Yang, X., Liu, W., Feng, B., Ma, J., et al. (2012a). Chinese patent medicine Liu wei di huang wan combined with antihypertensive drugs, a new integrative medicine therapy, for the treatment of essential hypertension: A systematic review of randomized controlled trials. Evid. Based. Complement. Altern. Med. 2012, 714805. doi:10.1155/2012/714805
Wang, L., Ma, R., Liu, C., Liu, H., Zhu, R., Guo, S., et al. (2017). Salvia miltiorrhiza: A potential red light to the development of cardiovascular diseases. Curr. Pharm. Des. 23 (7), 1077–1097. doi:10.2174/1381612822666161010105242
Wang, X. Q., Zou, X. R., and Zhang, Y. C. (2016). From "kidneys govern bones" to chronic kidney disease, diabetes mellitus, and metabolic bone disorder: A crosstalk between traditional Chinese medicine and modern science. Evid. Based. Complement. Altern. Med., 4370263. doi:10.1155/2016/4370263
Wang, Y. J., He, L. Q., Sun, W., Lu, Y., Wang, X. Q., Zhang, P. Q., et al. (2012b). Optimized project of traditional Chinese medicine in treating chronic kidney disease stage 3: A multicenter double-blinded randomized controlled trial. J. Ethnopharmacol. 139 (3), 757–764. doi:10.1016/j.jep.2011.12.009
Wetmore, J. B., Herzog, C. A., Sexter, A., Gilbertson, D. T., Liu, J., Kasner, S. E., et al. (2020). Outcomes following ischemic stroke in older patients with CKD stages 4 and 5: A retrospective cohort study. Am. J. Kidney Dis. 76 (6), 784–793. doi:10.1053/j.ajkd.2020.03.021
Williamson, P. R., Kolamunnage-Dona, R., and Tudur Smith, C. (2007). The influence of competing-risks setting on the choice of hypothesis test for treatment effect. Biostatistics 8 (4), 689–694. doi:10.1093/biostatistics/kxl040
Xu, Z. J., Shu, S., Li, Z. J., Liu, Y. M., Zhang, R. Y., Zhang, Y., et al. (2017). Liuwei Dihuang pill treats diabetic nephropathy in rats by inhibiting of TGF-β/SMADS, MAPK, and NF-kB and upregulating expression of cytoglobin in renal tissues. Med. Baltim. 96 (3), e5879. doi:10.1097/md.0000000000005879
Yamabe, N., Yokozawa, T., Kim, H. Y., and Cho, E. J. (2005). Protective effect of Hachimi-jio-gan against renal failure in a subtotal nephrectomy rat model. J. Pharm. Pharmacol. 57 (12), 1637–1644. doi:10.1211/jpp.57.12.0014
Keywords: chronic kidney disease, ischemic stroke (IS), Chinese herbal medicine, inflammation, traditional Chinese medecine
Citation: Shen H-S, Hsu C-Y, Yip H-T and Lin I-H (2022) Lower risk of ischemic stroke among patients with chronic kidney disease using chinese herbal medicine as add-on therapy: A real-world nationwide cohort study. Front. Pharmacol. 13:883148. doi: 10.3389/fphar.2022.883148
Received: 24 February 2022; Accepted: 11 July 2022;
Published: 11 August 2022.
Edited by:
James Cheng-Chung Wei, Chung Shan Medical University Hospital, TaiwanReviewed by:
Renin Chang, Tajen University, TaiwanCopyright © 2022 Shen, Hsu, Yip and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: I-Hsin Lin, Y2NtcDIyMEBtYWlsLnRjdS5lZHUudHc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.