- 1Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy
- 2Integrative Medicine Research Group, IMRG, Noceto, Italy
- 3IRCCS SDN, SYNLAB Napoli, Naples, Italy
- 4Gruppo Oncologico Ricercatori Italiani, GORI-Onlus, Pordenone, Italy
- 5Radiotherapy Unit, Policlinico Di Sant'Orsola, University of Bologna, Bologna, Italy
- 6Division of Cardiology, Istituto Nazionale Tumori, Naples, Italy
- 7Department of Advanced Technologies, Nuclear Medicine and PET, “Cannizzaro” Hospital, Catania, Italy
- 8Tirelli Medical Center, Pordenone, Italy
- 9Department of Radiation Oncology and Nuclear Medicine, Verona, Italy
- 10ASL NA2 NORD, Oncology Operative Unit, “Santa Maria Delle Grazie” Hospital, Naples, Italy
- 11Department of Pharmaceutical and Pharmacological Sciences, University of Padova, Padova, Italy
Objectives: According to the National Cancer Institute, the integrative medicine (IM) approach to medical care combines standard medicine with complementary and alternative medicine practices that have proved safe and effective.
Methods: We describe the clinical cases of four patients with malignant pleural mesothelioma (MPM), diffuse malignant peritoneal mesothelioma (DMPM), intrahepatic cholangiocarcinoma, and breast cancer (BC) who received supportive treatment (ST) according to an IM approach after the failure of standard cancer treatments or the appearance of serious adverse events caused by antiblastic chemotherapy. The critical role of complementary drugs in reducing the side effects of cancer treatments and normalizing the white cell count is especially apparent in the case of the patient with metastatic BC, who experienced prolonged neutropenia.
Results: The IM approach was well-tolerated and had no adverse side effects. It improved the quality of life (QoL) of all patients and in two cases extended overall survival.
Conclusion: The extended clinical and instrumental response to IM of the patients with malignant mesothelioma and the improved health-related QoL and good tolerance of the ST demonstrated in all cases support the value of this approach in patients whose cancer therapies have failed but who show a good performance status. Our data require confirmation in a well-designed prospective clinical trial.
Introduction
Health-related quality of life (HR-QoL) is a critical outcome measure in cancer management. It is a dual notion since in terminally patients it involves control of disease-related symptoms, such as pain and cancer-related fatigue (CRF), and of nutritional intake, whereas in patients receiving active cancer treatment [e.g., antiblastic chemotherapy (AC), immunotherapy (IMT), and radiotherapy (RT)] it means control of treatment-related side effects. Satisfactory results have widely been reported (İnci and İnci, 2020) and are best achieved by multidisciplinary teams. In this scenario, integrative medicine (IM) is a new care opportunity (Halil Güneş et al., 2020; Khazaei et al., 2020; Olçar and Karadağ, 2020; İnci and İnci, 2020). According to the US National Cancer Institute (NCI), the IM approach combines standard medicine with complementary and alternative medicine (CAM) practices that have proved safe and effective (PDQ Integrative et al., 2002; Berretta et al., 2017; Berretta et al., 2020c; Berretta et al., 2020a). IM tries to stress patient preferences and to address their mental, physical, and spiritual health.
The biochemical basis for the clinical use of CAM in patients with cancer is its ability to improve the systemic biomarkers of inflammation and prognosis and to delay recurrence. Moreover, some CAM practices reduce the risk factors for cardiometabolic conditions such as diabetes, insulin resistance, metabolic syndrome, and visceral obesity, which involve a higher risk of cancer recurrence, heart failure, atherosclerosis, and overall mortality. Some of the anti-inflammatory effects of CAM are exerted through attenuation of the cytokine storm triggered by the NLRP3 and MYD88 pathways. As summarized in Figure 1, the “micro-cardio-immuno-oncology” axis, a deep network encompassing the microbiome, the cardiovascular and immune systems, and cancer pathways, is susceptible to several types of CAM, which has the ability to improve HR-QoL, CRF, immune function, and survival.
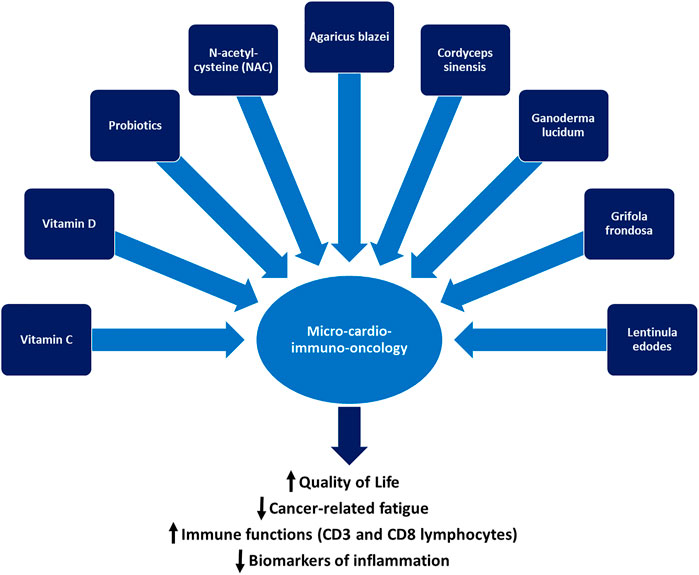
FIGURE 1. The micro-cardio-immuno-oncology axis and the mainstays of complementary and alternative medicine: vitamin C, vitamin D, probiotics, N-acetyl-cysteine, and selected medicinal mushrooms can improve the quality of life and immune function of patients with cancer and reduce cancer-related fatigue and the systemic concentration of pro-inflammatory biomarkers.
Crucially, in patients receiving active cancer treatment, HR-QoL preservation allows for completing AC, IMT, and RT cycles.
The four cases described below clearly demonstrate the safety and efficacy of an IM approach that was devised by a multidisciplinary team as an oncological approach and supportive treatment (ST) and shared with the patients.
Malignant mesothelioma (MM) is a rare, aggressive cancer arising from the mesothelium, the thin tissue that lines the lungs, chest wall, and abdomen. The major risk factors for MM are asbestos exposure and viral infection (e.g., Simian Virus 40, SV40). The most common histological subtypes are the epithelioid (60–80%), the sarcomatoid (20%), and the biphasic (Vita et al., 2021). The outcome of MM is closely cell type-dependent—for instance, epithelioid MM is less aggressive, even though long-term outcomes are still poor. The standard MM treatment is currently based on a multimodal approach, including induction AC (platin and pemetrexed), surgical resection, and sometimes RT, which is generally offered to patients with pleural MM, to young patients with a good Eastern Cooperative Oncology Group (ECOG) (Martin, 2021) performance status (PS), to patients with localized disease and to those with the epithelioid subtype (Vita et al., 2021). The clinical role of second-line AC for progressive or relapsed disease is still undefined, as no post-progression validated treatment has emerged. Recent advances in immunotherapy may provide a breakthrough in the future. In the meantime, poor clinical condition and PS and relapsed and resistant disease after treatment failure hamper therapeutic decision-making, since it is difficult to decide whether to offer second-line treatment or best supportive care (BSC).
iCCA is a rare, aggressive primary liver tumor characterized by a variety of clinical manifestations and by high incidence and mortality rates even after curative treatment with radical resection (Berretta et al., 2015; Xiaopei et al., 2019). Different types of treatments are available for these patients in relation to disease stage, PS, comorbidities, and age. Some are standard (surgery, AC, LRT, and RT), whereas others are being tested in clinical trials. The prognosis is usually poor.
Breast cancer (BC) is still the most commonly diagnosed cancer in women all over the world (Caputo et al., 2020). The majority of patients with metastatic BC experience recurrent metastatic disease after the primary treatment for earlier-stage BC, whereas only a small fraction present with de novo metastatic disease (Mallet et al., 2022). Metastatic BC is currently considered incurable. For this reason, the primary therapeutic goals in these patients are an extension of survival, maintenance of the HR-QoL, and palliation of symptoms.
Our four patients suffered from malignant pleural mesothelioma (MPM), diffuse malignant peritoneal mesothelioma (DMPM), intrahepatic cholangiocarcinoma (iCCA), and breast cancer (BC) which had been managed with first-line systemic AC (MPM, DMPM, and BC) or loco-regional treatment (LRT; iCCA). After treatment failure, they received a similar ST.
We report the results of ST administration to patients with limited chances of standard cancer treatment due to disease progression or the appearance of serious adverse events.
Patients and Methods
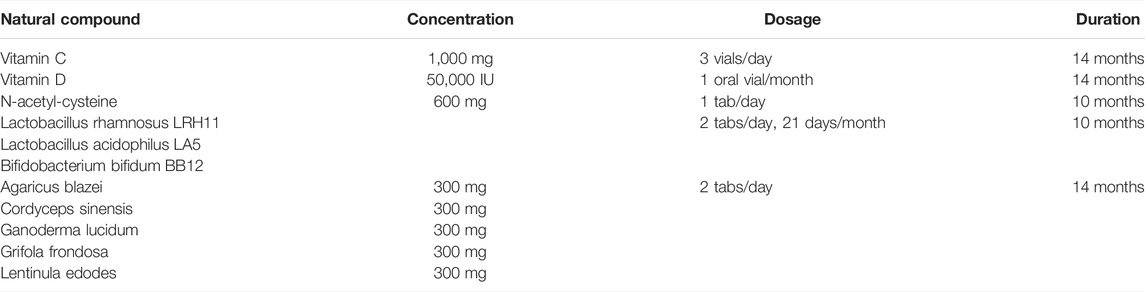
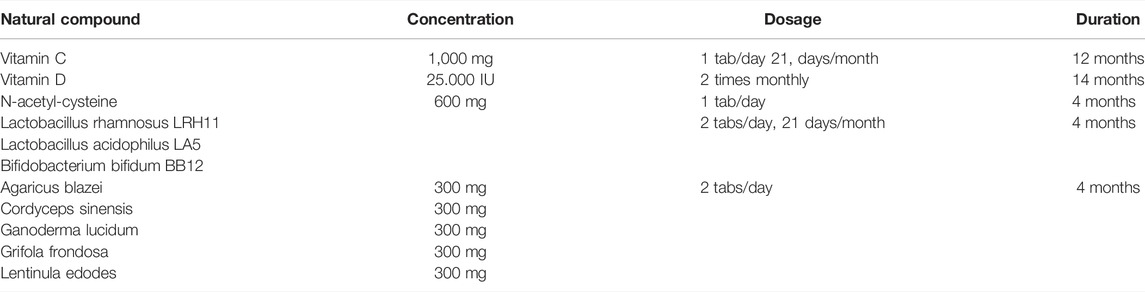
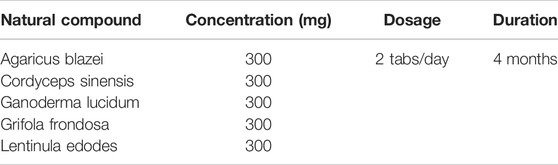
The three patients received standard oncological treatment before beginning the ST, which had been devised by a multidisciplinary team according to international clinical guidelines. The SP consisted mainly of vitamins C (Berretta et al., 2020b) and D, probiotics, and a blend of medicinal mushrooms (Micotherapy U-care, ADV Reform srl, Noceto, Italy) (Roda et al., 2020). Medicinal mushroom extract mixture micotherapy has been registered by the Italian Ministry of Health as a dietary supplement (registration number 627 I.5.i.h.2/2020/627). It is produced from a hot water extract which is precipitated with ethanol and subsequently freeze-dried. This tablet preparation contains a mixture of Ganoderma lucidum, Grifola frondosa, Agaricus blazei, Cordyceps sinensis, and Lentinula edodes, in equal amounts i.e. 300 mg each per tablet. One tablet, therefore, contains total polysaccharides >30% and 1.3–1.6 beta-glucans > 15%.
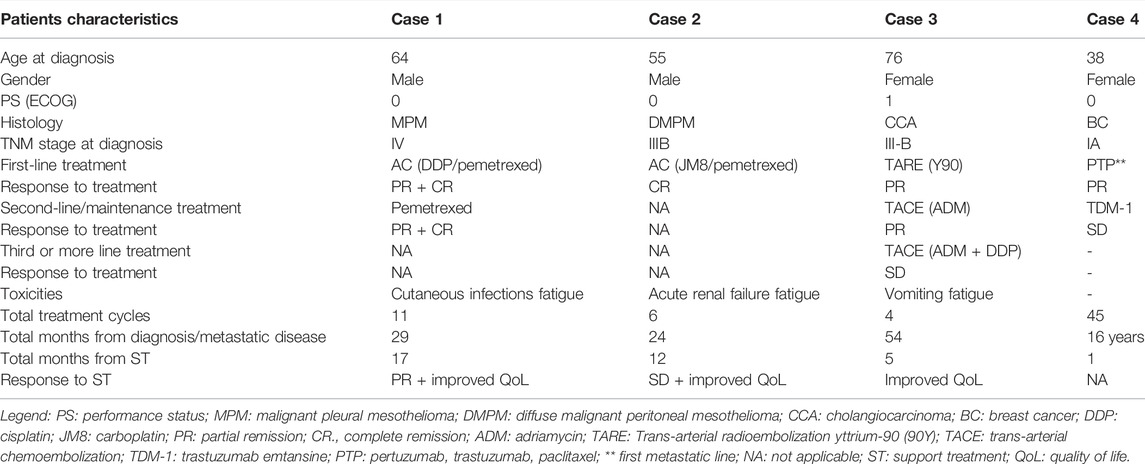
Probiotics (Acticolon) are a freeze-dried probiotic preparation containing 2 × 109 cfu microorganisms/day strains of lactic acid bacteria (Lactobacillus rhamnosus LRH11, Lactobacillus acidophilus LA5, and Bifidobacterium bifidum BB12), microcrystalline cellulose, stearic acid, magnesium stearate, and vegetable capsule (hydroxypropyl methylcellulose), silicon dioxide (registration number 3587 I.5. i.h.2/2018/3587). Patients received ample information about the proposed ST and signed the informed consent. Data collection and analysis of these cases were in line with the principles of the Declaration of Helsinki. Patients’ clinical characteristics are reported in Table 1.
CASE 1. Malignant pleural mesotheliomaThis 64-year-old man suffered from metastatic MPM. He was admitted to the emergency room in May 2019 due to dyspnea and pain in the right chest wall. The chest x-rays and CT scan disclosed right pleural effusion and a suspicious osteolytic lesion on the right 9th rib. The patient underwent partial right parietal pleurectomy and pleurodesis with medical graded talc using a video-assisted thoracoscopy surgery approach. There were no postoperative complications. The histological examination revealed a pleural epithelial mesothelioma, whereas immunohistochemistry (IHC) showed that the tissue was positive for calretinin, CK5/6, and D2-40 and negative for EpCAM and TTF1. Perioperative staging with total body CT and CT/PET fdg scans demonstrated mediastinal lymph node and left adrenal gland metastases. From August to December 2019, the patient received six cycles of pemetrexed/cisplatin AC as a first-line treatment and achieved partial (PR) and complete remission (CR) respectively of his lymph node and adrenal gland metastases. The AC was well-tolerated and there were no serious adverse events. From January to August 2020, the patient was scheduled to receive six cycles of pemetrexed single-agent AC (q28) as the maintenance treatment (Bearz et al., 2008). Eventually, he developed marked CRF, (Giacalone et al., 2013; Giacalone et al., 2012) lack of appetite, and recurrent erysipelas infection of the lower limbs. A new CT/PET fdg scan showed a stable disease (SD). Given the total number of AC cycles already administered, his objective response, the adverse events, and the HR-QoL, we decided together with the patient to suspend the AC and begin follow-up and ST, whose primary goals were to manage the erysipelas infection and to improve HR-QoL. The ST consisted of antibiotics and oral vitamin C, vitamin D (in relation to its serum level), probiotics, and a blend of medicinal mushrooms (Micotherapy U-care care) (see Table 2 for dosage). The use of the mushroom blend was supported by clinical evidence obtained from cancer patients (Roda et al., 2020; Del Buono et al., 2016; Barbieri et al., 2017; Rossi et al., 2018). The ST was well tolerated, there were no new infections and the HR-QoL improved quickly. The patient returned to work. In February 2021, a new CT/PET fdg scan, performed 6 months from AC withdrawal, documented a PR of the disease. The ST was continued until May 2021, when a new CT/PET fdg scan showed a minimal progression of disease (PD) with the involvement of a lumbar aortic lymph node. Considering the single site, in June 2021 the patient underwent RT (7Gy in five fractions). The most recent CT/PET fdg scan shows CR. Notably, the time to progression (TTP) was 22 months, 13 months while receiving AC, and 9 months while receiving ST. Thirty-two months from the diagnosis, the patient is alive. The ST is well-tolerated and has induced no serious adverse events. The patient’s HR-QoL is excellent and his PS (0) is good.
CASE 2. Diffuse malignant peritoneal mesotheliomaThe second case involved a 56-year-old man with DMPM. In July 2019, he underwent exploratory laparotomy due to ascites and peritoneal nodules. The histological examination identified peritoneal epithelial mesothelioma that was positive for CK5/7 and calretinin and negative for CK20 and CDX2. There were no postoperative complications. Postoperative staging, documented by total body CT and CT/PET fdg scans, demonstrated a diffuse peritoneal involvement. From August 2019 to January 2020, the patient received first-line pemetrexed/carboplatin AC (6 cycles) and achieved CR, as documented by a CT/PET fdg scan. The AC was well tolerated without serious adverse events and the patient began the follow-up. In April 2020, he experienced PD complicated by acute renal failure (ARF) with an estimated glomerular filtration rate (eGFR) of 13 ml/min, diffused abdominal pain due to frozen pelvis, and loss of appetite and weight. Given his clinical condition and the fact that he could receive no further AC cycles, we decided, together with the patient to begin ST. This consisted of hydration therapy, oral N-acetyl-cysteine (NAC), vitamin D, intravenous (iv) vitamin C, probiotics, and micotherapy U-care (see Table 3 for dosage). The primary treatment goals were to address the ARF and improve symptoms and HR-QoL. The ST was well-tolerated. The HR-QoL improved quickly as did renal function (eGFR, from 13 to 23 ml/min), the abdominal pain disappeared and the patient began eating again. In August 2020, a new CT scan showed SD, which remained unchanged until June 2021, when PD was documented. The patient died in July 2021 due to PD. The most notable outcomes of this case with aggressive cancer are an OS of 24 months and a TTP of 14 months from ST inception.
CASE 3. Intrahepatic cholangiocarcinomaThis patient was a 76-year-old woman with iCCA. Her family history included the death of three brothers from bile duct cancer. In June 2017, she underwent a liver biopsy due to right abdominal pain, weight loss, dyspeptic symptoms, and CT evidence of liver lesions. Histopathological examination demonstrated a poorly differentiated carcinoma that was positive for pancreatin and CK7 and negative for TTF1, hepatocyte, and CK20 and was consistent with upper gastrointestinal tract biliary-pancreatic origin and iCCA. The blood examination evidenced an alpha-fetoprotein (αFP) value of 450 IU/ml (range, 0–15) and a lactate dehydrogenase (LDH) value of 512 (range, 230–460), which suggested a clinical diagnosis of iCCA. In consideration of her age, comorbidities (hypertension), disease stage (IIIB TNM AJCC), and the poor sensitivity of iCCA to AC, in November 2017 the patient received trans-arterial radioembolization (TARE) with yttrium-90 (Y90) resin microspheres, an emerging local treatment option for iCCA (Paprottka et al., 2021). There were no serious adverse events. The patient achieved PR, as demonstrated by a CT scan performed at 3 months. Her αFP value fell significantly (from 450 to 27). The patient began a quarterly follow-up. In August 2019, after 21 months of first-line treatment, a new CT scan showed local PD. After multidisciplinary consultation, we proposed two cycles of trans-arterial chemoembolization (TACE) with adriamycin (ADM), which were administered between August and September. The treatment was well-tolerated, the ECOG PS was 0 and in December 2019 the CT scan showed a PR. PD was documented in June 2020, 6 months into the second-line treatment. A month later the patient received the third cycle of TACE with ADM and cisplatin, which induced moderate and persistent adverse events including nausea, vomiting, weight loss, and CRF. In January 2021, 5 months from the third cycle of TACE, a new CT scan showed local PD. The patient refused palliative single-agent chemotherapy, due to the previous adverse events. We, therefore, decided to wait and see and began follow-up, based on her stable clinical condition and her PS of 1. In August 2021, a further local PD was documented by CT and abdominal ultrasound scans. Her αFP rose to 192 IU/ml; the abdominal pain and loss of appetite and weight returned and CRF was the most evident symptom; the ECOG PS was 2. Considering the relevant factors (PD, clinical condition, previous treatments, refusal to undergo a new TACE, and age), we proposed to the patient to begin ST, to reduce her CRF and improve her HR-QoL. The ST consisted of oral administration of NAC, vitamins C and D, probiotics, and micotherapy U-care (see Table 4 for dosage) and was well-tolerated. There were no serious adverse events and the QoL improved quickly; the CRF decreased significantly and a moderate weight gain was observed. In January 2022, an abdominal ultrasound scan showed a liver PD at S8 (52 vs. 70 mm), an SD at S4 (63 vs. 65 mm), and three new liver lesions <1 cm. The αFP value rose to 200 IU/ml with normal serum bilirubin and AST/ALT. The patient’s PS was 1. Her clinical condition deteriorated and she was admitted to the hospital, where she died in January 2022 due to the rapid decline of her clinical conditions.
Case 4. Metastatic breast cancer with prolonged neutropenia after Comirnaty vaccine administrationThe fourth patient was a 62-year-old woman with lymph node and lung metastatic disease from a primary hormone-receptor and HER2 positive BC that had been diagnosed and surgically removed in 1997. Eight years later (May 2005), lung metastases were discovered by CT scan and primarily treated with radical stereotactic radiotherapy. At further PD, in January 2017, she was treated with the standard first-line AC treatment for metastatic disease (pertuzumab and trastuzumab) for about 2 years. In February 2018, the patient began the second-line treatment with trastuzumab emtansine, which is ongoing and still ensures disease control. In January 2021, the worldwide Covid-19 pandemic involved the launch of a massive vaccination campaign to protect the population, especially fragile and oncological patients, from the adverse outcomes of Covid-19 virus infection. The most widely used vaccines were based on messenger ribonucleic acid (mRNA) molecules, which stimulate host cells to synthesize the Spike surface protein of Coronavirus. A large body of data has demonstrated the safety of such vaccines (Faermann et al., 2021; Seban et al., 2021). Our patient received the two doses of Pfizer-BioNTech (COMIRNATY) BNT162b2 mRNA between March and April 2021, at the correct 3-weeks interval. Following the second dose, the patient—who had never needed treatment postponement or dose reduction—experienced prolonged grade-2 neutropenia (see Figure 2) from which she recovered only in May 2021 after administration of micotherapy U-care for 15 days (see Table 5). The ST was administered for a month. From then on she has tolerated AC without further episodes of neutropenia.This case is not comparable to those of the first three patients, either in terms of prognosis or of available therapeutic options, which in this patient are very limited in number and effectiveness. BC is largely a curable tumor that can be managed with a powerful armamentarium of several and ever-increasing lines of treatment even in patients with advanced/metastatic disease. However, other issues can be found in the management of these prolonged histories of succeeding therapies. In particular, clinicians may deal with phases of psychological refusal and adverse events related to psycho-organic factors like asthenia that are not easily relieved by available supportive care. The control of adverse events is essential to achieve and maintain a good HR-QoL and optimize patient compliance. In this case, AC combined with the mRNA Covid-19 vaccine induced a prolonged phase of neutropenia that was probably due to the immune reaction to lymphocyte populations concentrating at peripheral drainage sites. This phenomenon may reflect the relative reduction in peripheral blood and the atypical figures found especially in BC patients following Covid-19 vaccination (Faermann et al., 2021; Seban et al., 2021).Micotherapy has recognized properties in attenuating the side effects of anticancer treatments, specifically AC-induced neutropenia (Liu et al., 2008; Ito et al., 2009; Jiang et al., 2017; Lei et al., 2020). The mushroom blend is rich in polysaccharides and B-glucans, which have well-documented immunomodulatory properties. Although their heterogeneous composition and the lack of funds hamper basic as well as clinical research on these types of ST, work in this area would provide valuable insight into the role and properties of micotherapy and help its wider use as an ST.
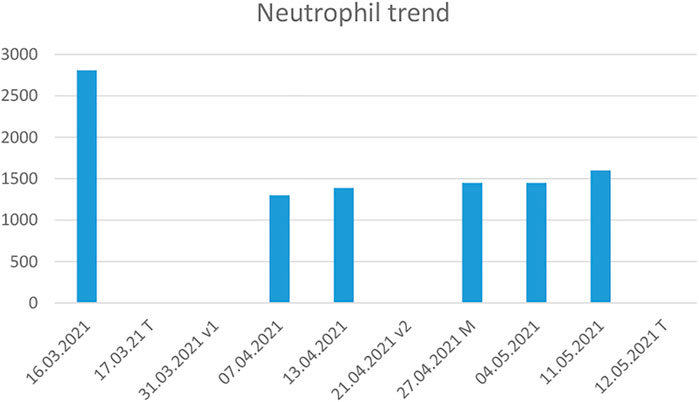
FIGURE 2. Graphical representation of the neutrophil trend, which declined after the first vaccine dose and whose persistently a low level required extending the interval between antiblastic treatments to nearly 2 months. T: treatment administration, v1: first vaccine dose, v2: second vaccine dose, M: mushrooms integration.
Discussion
Integrative medicine is a novel approach to medical care that combines standard medicine with CAM practices that have been shown to be safe and effective.
The four clinical cases described herein provide typical examples of an IM approach that was devised by a multidisciplinary team and shared with the patient. All four patients, who suffered from metastatic MPM and DMPM, locally advanced iCCA, and metastatic BC, had a poor prognosis and their median OS was, respectively, 15.3 months (Bearz et al., 2008), 11.5 months (Serio et al., 2017), 12.5 months (Mavros et al., 2014), and 55 months (Mallet et al., 2022). After the failure of oncological treatment, these patients experienced a progressive deterioration of the clinical condition and PS, and the only available therapy is often palliative treatment. The rationale for administering an ST consisting of vitamins C and D, probiotics, and medicinal mushrooms was based on clinical evidence reported in the literature and on the guidelines of the NCI and the National Center for Complementary and Integrative Health (NCCIH) (PDQ Integrative et al., 2002), which consider IM as a valid ST strategy after the failure of standard cancer treatments and/or the occurrence of serious adverse events. IM-based ST is closely patient-tailored since it depends on a variety of parameters such as age, PS, comorbidities, cancer-related symptoms, treatment failure, AC cycles received, adverse events, and terminal illness. The ST drugs/supplements proposed to our patients were based on their clinical features and disease characteristics. Vitamin C improves HR-QoL and attenuates cancer-related side effects (Berretta et al., 2020b). The most important clinical benefits are provided by iv administration but in the patients with MPM and iCCA oral vitamin C did enhance HR-QoL (Berretta et al., 2020b). Our STs were safe and effective, they did not induce adverse events and significantly improved HR-QoL; moreover, they extended OS in the two patients with MM.
The use of vitamin D is supported by observational studies which have demonstrated that it is associated with longer survival in cancer patients (Imran Ali Shah, 2020; İnci et al., 2020; Gnagnarella et al., 2021). Moreover, there are reasonable mechanisms for its effect in reducing tumor invasiveness and propensity to metastasize and in influencing immunomodulatory properties (Jiang et al., 2017; Imran Ali Shah, 2020; İnci et al., 2020; Gnagnarella et al., 2021) that may contribute to reducing metastatic disease and fatal cancer.
Probiotics are live microorganisms that are known to attenuate the side effects of AC and in general to restore intestinal eubiosis and nutrient absorption, which are the key mechanisms to improve outcomes and HR-QoL. Administered in adequate doses, they confer benefits such as improved immune function and support for the competitive exclusion of pathogens (Deleemans et al., 2021). In oncological settings, they may help to maintain the balance of the intestinal microbiota, to reduce potential pathogenic bacterial infection, improve bowel regularity, and restore homeostasis to the intestinal microbiota after AC (Barbieri et al., 2017; Rossi et al., 2018; Garau et al., 2021).
The role of medicinal mushroom blends is more intriguing. According to the NCI and the NCCIH, they can improve HR-QoL and immunomodulation. Moreover, they have been approved as adjuncts to standard cancer treatment in Japan and China more than 30 years ago and have an extensive history of safe clinical use alone or combined with RT or AC (Roda et al., 2020; Barbieri et al., 2017; Nowakowski et al., 2021). The different blends produce numerous bioactive compounds that influence several cancer-related pathways, often synergistically, also by modulating the cellular targets involved in cell proliferation, survival, and angiogenesis (Barbieri et al., 2017; Rossi et al., 2018; Garau et al., 2021; Nowakowski et al., 2021).
Medicinal mushrooms exert immune enhancing activities through the stimulation of the growth and differentiation of lymphocytes (Moradali et al., 2007; Vanneman and Dranoff, 2012). For example, Turkey tail extract is able to increase CD8+ T cells and CD19 + B cells in breast cancer patients (Martínez-Montemayor et al., 2011). Reishi increases significantly IFN-γ, IL-2, IL-6, and NK cells (CD56 + cells) levels in lung cancer patients thereby increasing potentially immune therapies (Gao et al., 2003). Other studies indicate that the mushrooms reishi, cordyceps, agaricus, and maitake reduce TH-2 cytokines with anti-inflammatory and immune-enhancing functions (Kar Mahapatra et al., 2011). The clinical outcomes of medicinal mushrooms still to be studied in a deeper manner; however, it has been clarified that protein complexes, polysaccharides, and β-glucans of medicinal mushrooms reduce NF-kB expression in APC cells, increase the synthesis and release of INF-γ from NK cells, and TH-1 pathways which lead to the activation of macrophages and cytotoxic lymphocytes with antitumor properties (Borchers et al., 2004; Guggenheim et al., 2014; Zhao et al., 2020).
Here, every supplement/drug included in IM approaches has a different beneficial role and action that often complements those of the other treatment constituents. We believed that these supplements exert a synergistic activity, for instance on the gut microbiota. There is evidence that gut microbiota dysbiosis can trigger inflammatory signaling pathways that affect the intestinal and extra-intestinal immune function and contribute to carcinogenesis and cancer progression (Toor et al., 2019; Rizzetto et al., 2018). Carcinogenesis is an inflammatory process where the microbiota appears to be involved both directly and through indirect mechanisms, via the immune pathways. The primary goals of the ST administered to our patients were to improve HR-QoL and help the immune system contrast disease progression. The good TTP and OS outcomes of the patients with MPM and DMPM were frankly unexpected.
According to the English literature, about half of cancer patients already combine CAM remedies with oncological treatments without informing their physician (Berretta et al., 2020c). We feel that this decision should be made by the medical staff. Nutraceuticals fully fall into the category of CAM with interesting implications in oncology and cardioncology (Quagliariello et al., 2018). Nutraceuticals are extracts of medicinal plants or complexes of natural bioactive able to reduce the metabolism of cancer cells by inhibiting the synthesis and release of cytokines, chemokines, and growth factors associated with apoptosis escape and cancer cell survival/angiogenesis (de Mejia and Dia, 2010). Nutraceuticals include curcuma longa, artichoke, milk thistle, rhodiola rosea, berberis, boswellia, and others. Several clinical studies have shown that nutraceuticals are able to reduce cancer and cardiovascular risk factors through anti-inflammatory activities (Barbarisi et al., 2019; Balakrishna and Kumar, 2015). However, their use must always be encouraged with the supervision of clinicians, avoiding self-administration, for possible drug-plant interactions that can reduce the anticancer efficacy and cancer outcomes (Yeung et al., 2018).
In conclusion, the extended clinical and instrumental response documented in the two patients with MM and the improved HR-QoL and good ST tolerance observed in all cases support the value of administering IM to patients whose oncological therapies have failed but who have a good PS.
Sometimes the patients themselves answer the question, choosing an alternative, and/or complementary treatment to obtain better results also in terms of HR-QoL and we firmly believing that this assessment is up to the healthcare staff.
CAM, adopted as an ST by a multidisciplinary team, is a major care opportunity for patients with cancer and for frail (elderly, HIV-positive) individuals (Berretta et al., 2010; Di Benedetto et al., 2011; Zanet et al., 2011). Clearly, our data need to be confirmed in a well-designed prospective clinical trial.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author Contributions
Conceptualization: MB, RT, LM, VQ, and MM; data curation: MB, VQ, FF, AM, LM, and MM; investigation: MB, VQ, LM, and MM; writing-original draft: MB, RT, VQ, LM, and MM; writing-review and editing: MB, VQ, LM, and MM. All authors have read and agreed to the published version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer MC declared a shared affiliation, with no collaboration, with two of the authors, NM and VQ to the handling editor at the time of the review.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank: Carmelo Iuculano, MD, for his clinical support to one of the patients and to Dr. Silvia Modena (www.silviamodena.com) for editorial and language revision.
References
Balakrishna, A., and Kumar, M. H. (2015). Evaluation of Synergetic Anticancer Activity of Berberine and Curcumin on Different Models of A549, Hep-G2, MCF-7, Jurkat, and K562 Cell Lines. Biomed. Res. Int. 2015, 354614. doi:10.1155/2015/354614
Barbarisi, M., Barbarisi, A., De Sena, G., Armenia, E., Aurilio, C., Libutti, M., et al. (2019). Boswellic Acid Has Anti-inflammatory Effects and Enhances the Anticancer Activities of Temozolomide and Afatinib, an Irreversible ErbB Family Blocker, in Human Glioblastoma Cells. Phytother. Res. 33 (6), 1670–1682. doi:10.1002/ptr.6354
Barbieri, A., Quagliariello, V., Del Vecchio, V., Falco, M., Luciano, A., Amruthraj, N. J., et al. (2017). Anticancer and Anti-inflammatory Properties of Ganoderma Lucidum Extract Effects on Melanoma and Triple-Negative Breast Cancer Treatment. Nutrients 9 (3), 210. doi:10.3390/nu9030210
Bearz, A., Garassino, I., Cavina, R., Favaretto, A., Boccalon, M., Talamini, R., et al. (2008). Pemetrexed Single Agent in Previously Treated Non-small Cell Lung Cancer: a Multi-Institutional Observational Study. Lung Cancer 60 (2), 240–245. doi:10.1016/j.lungcan.2007.10.008
Berretta, M., Bignucolo, A., Di Francia, R., Comello, F., Facchini, G., Ceccarelli, M., et al. (2020a). Resveratrol in Cancer Patients: From Bench to Bedside. Int. J. Mol. Sci. 21 (8), 2945. doi:10.3390/ijms21082945
Berretta, M., Della Pepa, C., TralongoP, P., Fulvi, A., Martellotta, F., Lleshi, A., et al. (2017). Use of Complementary and Alternative Medicine (CAM) in Cancer Patients: An Italian Multicenter Survey. Oncotarget 8 (15), 24401–24414. doi:10.18632/oncotarget.14224
Berretta, M., Lleshi, A., Cappellani, A., Bearz, A., Spina, M., Talamini, R., et al. (2010). Oxaliplatin Based Chemotherapy and Concomitant Highly Active Antiretroviral Therapy in the Treatment of 24 Patients with Colorectal Cancer and HIV Infection. Curr. HIV Res. 8 (3), 218–222. doi:10.2174/157016210791111061
Berretta, M., Quagliariello, V., Maurea, N., Di Francia, R., Sharifi, S., Facchini, G., et al. (2020b). Multiple Effects of Ascorbic Acid against Chronic Diseases: Updated Evidence from Preclinical and Clinical Studies. Antioxidants (Basel) 9 (12), 1182. doi:10.3390/antiox9121182
Berretta, M., Rinaldi, L., Taibi, R., Tralongo, P., Fulvi, A., Montesarchio, V., et al. (2020c). Physician Attitudes and Perceptions of Complementary and Alternative Medicine (CAM): A Multicentre Italian Study. Front. Oncol. 10, 594. doi:10.3389/fonc.2020.00594
Berretta, S., Fisichella, R., Spartà, D., Lleshi, A., and Nasti, G. (2015). Primary Liver Cancer: Clinical Aspects, Prognostic Factors and Predictive Response to Therapy. WCRJ 2 (3), e561.
Borchers, A. T., Keen, C. L., and Gershwin, M. E. (2004). Mushrooms, Tumors, and Immunity: an Update. Exp. Biol. Med. (Maywood). 229(5), 393–406. doi:10.1177/153537020422900507
Caputo, R., Cianniello, D., Giordano, A., Piezzo, M., Riemma, M., Trovò, M., et al. (2020). Gene Expression Assay in the Management of Early Breast Cancer. Curr. Med. Chem. 27 (17), 2826–2839. doi:10.2174/0929867326666191205163329
de Mejia, E. G., and Dia, V. P. (2010). The Role of Nutraceutical Proteins and Peptides in Apoptosis, Angiogenesis, and Metastasis of Cancer Cells. Cancer Metastasis Rev. 29(3), 511–528. doi:10.1007/s10555-010-9241-4
Del Buono, A., Bonucci, M., Pugliese, S., D’Orta, A., and Fioranelli, M. (2016). Polysaccharide from Lentinus Edodes for Integrative Cancer Treatment: Immunomodulatory Effects on Lymphocyte Population. WCRJ 3 (1), e652.
Deleemans, J. M., Gajtani, Z., Baydoun, M., Reimer, R. A., Piedalue, K. A., and Carlson, L. E. (2021). The Use of Prebiotic and Probiotic Interventions for Treating Gastrointestinal and Psychosocial Health Symptoms in Cancer Patients and Survivors: A Systematic Review. Integr. Cancer Ther. 20, 15347354211061733. doi:10.1177/15347354211061733
Di Benedetto, F., Berretta, M., D'Amico, G., Montalti, R., De Ruvo, N., Cautero, N., et al. (2021). Liver Resection for Colorectal Metastases in Older Adults: a Paired Matched Analysis. J. Am. Geriatr. Soc. 59(12), 2282–2290. doi:10.1111/j.1532-5415.2011.03734.x
Faermann, R., Nissan, N., Halshtok-Neiman, O., Shalmon, A., Gotlieb, M., Yagil, Y., et al. (2021). COVID-19 Vaccination Induced Lymphadenopathy in a Specialized Breast Imaging Clinic in Israel: Analysis of 163 Cases. Acad. Radiol. 28 (9), 1191–1197. doi:10.1016/j.acra.2021.06.003
Gao, Y., Zhou, S., Jiang, W., Huang, M., and Dai, X. (2003). Effects of Ganopoly (A Ganoderma Lucidum Polysaccharide Extract) on the Immune Functions in Advanced-Stage Cancer Patients. Immunol. Invest. 32 (3), 201–215. doi:10.1081/imm-120022979
Garau, V., Casu, C., Nardi, G. M., Denotti, G., and Orrù, G. (2021). Letter to the Editor – Oral Microbiota, Health and Cancer: the Dual Face of the Same Coin in the Field of the Host-Microbe Interactome. WCRJ 8, e2075. doi:10.32113/wcrj_20218_2075
Giacalone, A., Quitadamo, D., Zanet, E., Berretta, M., Spina, M., and Tirelli, U. (2013). Cancer-related Fatigue in the Elderly. Support Care Cancer 21 (10), 2899–2911. doi:10.1007/s00520-013-1897-1
Giacalone, A., Spina, M., Berretta, M., and Tirelli, U. (2012). Two Types of Fatigue in Cancer Patients. Br. J. Cancer 106 (2), 424–425. doi:10.1038/bjc.2011.528
Gnagnarella, P., Muzio, V., Caini, S., Raimondi, S., Martinoli, C., Chiocca, S., et al. (2021). Vitamin D Supplementation and Cancer Mortality: Narrative Review of Observational Studies and Clinical Trials. Nutrients. 13(9), 3285. doi:10.3390/nu13093285
Guggenheim, A. G., Wright, K. M., and Zwickey, H. L. (2014). Immune Modulation from Five Major Mushrooms: Application to Integrative Oncology. Integr. Med. (Encinitas) 13 (1), 32–44.
Halil Güneş, İ., Karadağ, G., and Kul, S. (2020). Effect of Breathing Relaxation Exercise Training on the Self-Care Agency and Functional Life of the Lung Cancer Patients: a Randomized Controlled Trial. WCRJ 7, e1619. doi:10.32113/wcrj_20207_1619
Imran Ali Shah, S. (2020). Beneficial Role of Vitamin D in Common Cancers: Is the Evidence Compelling Enough? WCRJ 7, e1574. doi:10.32113/wcrj_20205_1574
İnci, F., İnci, H., Karataş, F., and Adahan, D. (2020). Is Low Serum Vitamin D Level Associated with Cancer? WCRJ 7, e1683. doi:10.32113/wcrj_20209_1683
İnci, H., and İnci, F. (2020). Complementary and Alternative Medicine Awareness in Cancer Patients Receiving Chemotherapy. WCRJ 7, e1752. doi:10.32113/wcrj_202011_1752
Ito, K., Masuda, Y., Yamasaki, Y., Yokota, Y., and Nanba, H. (2009). Maitake Beta-Glucan Enhances Granulopoiesis and Mobilization of Granulocytes by Increasing G-CSF Production and Modulating CXCR4/SDF-1 Expression. Int. Immunopharmacol. 9 (10), 1189–1196. doi:10.1016/j.intimp.2009.06.007
Jiang, Y., Chang, Y., Liu, Y., Zhang, M., Luo, H., Hao, C., et al. (2017). Overview of Ganoderma Sinense Polysaccharide-An Adjunctive Drug Used during Concurrent Chemo/Radiation Therapy for Cancer Treatment in China. Biomed. Pharmacother. 96, 865–870. doi:10.1016/j.biopha.2017.09.060
Kar Mahapatra, S., Bhattacharjee, S., Chakraborty, S. P., Majumdar, S., and Roy, S. (2011). Alteration of Immune Functions and Th1/Th2 Cytokine Balance in Nicotine-Induced Murine Macrophages: Immunomodulatory Role of Eugenol and N-Acetylcysteine. Int. Immunopharmacol. 11 (4), 485–495. doi:10.1016/j.intimp.2010.12.020
Khazaei, M., Khazaei, M. R., and Pazhouhi, M. (2020). An Overview of Therapeutic Potentials of Rosa Canina: a Traditionally Valuable Herb. WCRJ 7, e1580. doi:10.32113/wcrj_20205_1580
Lei, X., Zhi, C., Huang, W., Sun, X., Gao, W., Yin, X., et al. (2020). Recombinant Ganoderma Lucidum Immunomodulatory Protein Improves the Treatment for Chemotherapy-Induced Neutropenia. Front. Pharmacol. 11, 956. doi:10.3389/fphar.2020.00956
Liu, W. C., Chuang, W. L., Tsai, M. L., Hong, J. H., McBride, W. H., and Chiang, C. S. (2008). Cordyceps Sinensis Health Supplement Enhances Recovery from Taxol-Induced Leukopenia. Exp. Biol. Med. (Maywood) 233 (4), 447–455. doi:10.3181/0708-RM-230
Mallet, A., Lusque, A., Levy, C., Pistilli, B., Brain, E., Pasquier, D., et al. (2022). Real-world Evidence of the Management and Prognosis of Young Women (⩽40 Years) with De Novo Metastatic Breast Cancer. Ther. Adv. Med. Oncol. 14, 17588359211070362. doi:10.1177/17588359211070362
Martin, O (2021). Eastern Cooperative Oncology Group (ECOG) Performance Status. MDCALC. Availableat: Eastern Cooperative Oncology Group (ECOG) Performance Status - MDCalc.
Martínez-Montemayor, M. M., Acevedo, R. R., Otero-Franqui, E., Cubano, L. A., and Dharmawardhane, S. F. (2011). Ganoderma Lucidum (Reishi) Inhibits Cancer Cell Growth and Expression of Key Molecules in Inflammatory Breast Cancer. Nutr. Cancer 63 (7), 1085–1094. doi:10.1080/01635581.2011.601845
Mavros, M. N., Economopoulos, K. P., Alexiou, V. G., and Pawlik, T. M. (2014). Treatment and Prognosis for Patients with Intrahepatic Cholangiocarcinoma: Systematic Review and Meta-Analysis. JAMA Surg. 149, 565–574. doi:10.1001/jamasurg.2013.5137
Moradali, M. F., Mostafavi, H., Ghods, S., and Hedjaroude, G. A. (2007). Immunomodulating and Anticancer Agents in the Realm of Macromycetes Fungi (Macrofungi). Int. Immunopharmacol. 7 (6), 701–724. doi:10.1016/j.intimp.2007.01.008
Nowakowski, P., Markiewicz-Żukowska, R., Bielecka, J., Mielcarek, K., Grabia, M., and Socha, K. (2021). Treasures from the Forest: Evaluation of Mushroom Extracts as Anti-cancer Agents. Biomed. Pharmacother. 143, 112106. doi:10.1016/j.biopha.2021.112106
Olçar, Z., and Karadağ, G. (2020). Effect of Individual Training on the Quality of Life and the Reduction of Chemotherapy Symptoms Hematologic Cancer Patients. WCRJ 7, e1578.
Paprottka, K. J., Galiè, F., Ingrisch, M., Geith, T., Ilhan, H., Todica, A., et al. (2021). Outcome and Safety after 103 Radioembolizations with Yttrium-90 Resin Microspheres in 73 Patients with Unresectable Intrahepatic Cholangiocarcinoma-An Evaluation of Predictors. Cancers (Basel) 13 (21), 5399. doi:10.3390/cancers13215399
PDQ Integrative, Alternative, and Complementary Therapies Editorial Board. Medicinal Mushrooms (2002). (PDQ®): Health Professional Version in: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute US. Availableat: https://pubmed.ncbi.nlm.nih.gov/27929633/.
Pino, A., De Angelis, M., Chieppa, M., Caggia, C., and Randazzo, C. L. (2020). Gut microbiota, probiotics colorectal cancer a tight Relat. WCRJ 7, e1456. doi:10.32113/wcrj_20201_1456
Quagliariello, V., Vecchione, R., Coppola, C., Di Cicco, C., De Capua, A., Piscopo, G., et al. (2018). Cardioprotective Effects of Nanoemulsions Loaded with Anti-inflammatory Nutraceuticals against Doxorubicin-Induced Cardiotoxicity. Nutrients. 10(9), 1304. doi:10.3390/nu10091304
Rizzetto, L., Fava, F., Tuohy, K. M., and Selmi, C. (2018). Connecting the Immune System, Systemic Chronic Inflammation and the Gut Microbiome: The Role of Sex. J. Autoimmun. 92, 12–34. doi:10.1016/j.jaut.2018.05.008
Roda, E., Luca, F., Iorio, C. D., Ratto, D., Siciliani, S., Ferrari, B., et al. (2020). Novel Medicinal Mushroom Blend as a Promising Supplement in Integrative Oncology: A Multi-Tiered Study Using 4T1 Triple-Negative Mouse Breast Cancer Model. Int. J. Mol. Sci. 21 (10), 3479. doi:10.3390/ijms21103479
Romeo, M. (2021). Oncobiome and Personalized Cancer Medicine: Myth or Reality? WCRJ 8, e2055. doi:10.32113/wcrj_20217_2055
Rossi, P., Difrancia, R., Quagliariello, V., Savino, E., Tralongo, P., Randazzo, C. L., et al. (2018). B-glucans from Grifola Frondosa and Ganoderma Lucidum in Breast Cancer: an Example of Complementary and Integrative Medicine. Oncotarget 9 (37), 24837–24856. doi:10.18632/oncotarget.24984
Seban, R.-D., Richard, C., Nascimento-Leite, C., Ghidaglia, J., Provost, C., Gonin, J., et al. (2021). Absolute Lymphocyte Count after COVID-19 Vaccination Is Associated with Vaccine-Induced Hypermetabolic Lymph Nodes on 18F-FDG PET/CT: a Focus in Breast Cancer Care. J. Nucl. Med. 121, jnumed.121.263082. doi:10.2967/jnumed.121.263082
Serio, G., Pezzuto, F., Marzullo, A., Scattone, A., Cavone, D., Punzi, A., et al. (2017). Peritoneal Mesothelioma with Residential Asbestos Exposure. Report of a Case with Long Survival (Seventeen Years) Analyzed by Cgh-Array. Int. J. Mol. Sci. 18, 1818. doi:10.3390/ijms18081818
Toor, D., Wsson, M. K., Kumar, P., Karthikeyan, G., Kaushik, N. K., Goel, C., et al. (2019). Dysbiosis Disrupts Gut Immune Homeostasis and Promotes Gastric Diseases. Int. J. Mol. Sci. 20(10), 2432. doi:10.3390/ijms20102432
Vanneman, M., and Dranoff, G. (2012). Combining Immunotherapy and Targeted Therapies in Cancer Treatment. Nat. Rev. Cancer 12 (4), 237–251. doi:10.1038/nrc3237
Vita, E., Stefani, A., Di Salvatore, M., Chiappetta, M., Lococo, F., Margaritora, S., et al. (2021). Oncological Frontiers in the Treatment of Malignant Pleural Mesothelioma. J. Clin. Med. 10 (11), 2290. doi:10.3390/jcm10112290
Xiaopei, H., Kunfu, D., Lianyuan, T., Zhen, L., Mei, X., and Haibo, Y. (2019). Tumor Invasion Front Morphology: a Novel Prognostic Factor for Intrahepatic Cholangiocarcinoma. Eur. Rev. Med. Pharmacol. Sci. 23 (22), 9821–9828. doi:10.26355/eurrev_201911_19545
Yeung, K. S., Gubili, J., and Mao, J. J. (2018). Herb-Drug Interactions in Cancer Care. Oncol. Willist. Park. 32(10), 516–520. PMID: 30334243.
Zanet, E., Berretta, M., Martellotta, F., Cacopardo, B., Fisichella, R., Tavio, M., et al. (2011). Anal Cancer: Focus on HIV-Positive Patients in the HAART-Era. Curr. HIV Res.9(2), 70–81. doi:10.2174/157016211795569087
Keywords: malignant mesothelioma, cholangiocarcinoma, breast cancer, treatment, cancer, integrative medicine, personalized medicine, medicinal mushrooms
Citation: Berretta M, Morra A, Taibi R, Monari F, Maurea N, Ippolito M, Tirelli U, Fiorica F, Montella L, Facchini G, Quagliariello V and Montopoli M (2022) Improved Survival and Quality of Life Through an Integrative, Multidisciplinary Oncological Approach: Pathophysiological Analysis of Four Clinical Cancer Cases and Review of the Literature. Front. Pharmacol. 13:867907. doi: 10.3389/fphar.2022.867907
Received: 01 February 2022; Accepted: 03 03 May 20222022;
Published: 16 June 2022.
Edited by:
Jiang-Jiang Qin, Institute of Cancer and Basic Medicine (CAS), ChinaReviewed by:
Marco Cascella, G. Pascale National Cancer Institute Foundation (IRCCS), ItalyCarla Paola Sanchez Rios, Instituto Nacional de Enfermedades Respiratorias-México (INER), Mexico
Massimo Ambroggi, Guglielmo da Saliceto Hospital, Italy
Copyright © 2022 Berretta, Morra, Taibi, Monari, Maurea, Ippolito, Tirelli, Fiorica, Montella, Facchini, Quagliariello and Montopoli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. Berretta, YmVycmV0dGFtYUBnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 M. Berretta
M. Berretta A. Morra3
A. Morra3 N. Maurea
N. Maurea U. Tirelli
U. Tirelli L. Montella
L. Montella G. Facchini
G. Facchini V. Quagliariello
V. Quagliariello M. Montopoli
M. Montopoli