- 1Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
- 2The First Hospital of Hebei Medical University, Shijiazhuang, China
- 3Institute of Cardiovascular Diseases, Beijing University of Chinese Medicine, Beijing, China
Aims: The objective of this study was to assess the efficacy and potential mechanisms of Chinese herbal medicine (CHM) for treating coronary heart disease (CHD) patients with anxiety or depression.
Methods: A systematic literature search was performed. Screening studies, extracting data, and assessing article quality were carried out independently by two researchers. The active ingredients of CHM for the treatment of CHD with anxiety or depression were analyzed by the network pharmacology, and the main potential mechanisms were summarized by the database of Web of Science.
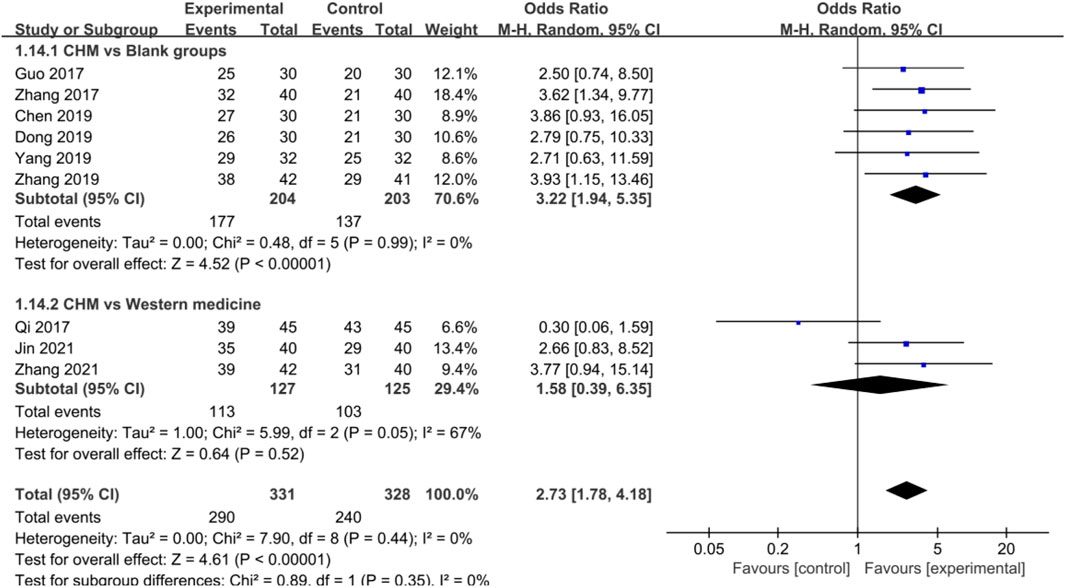
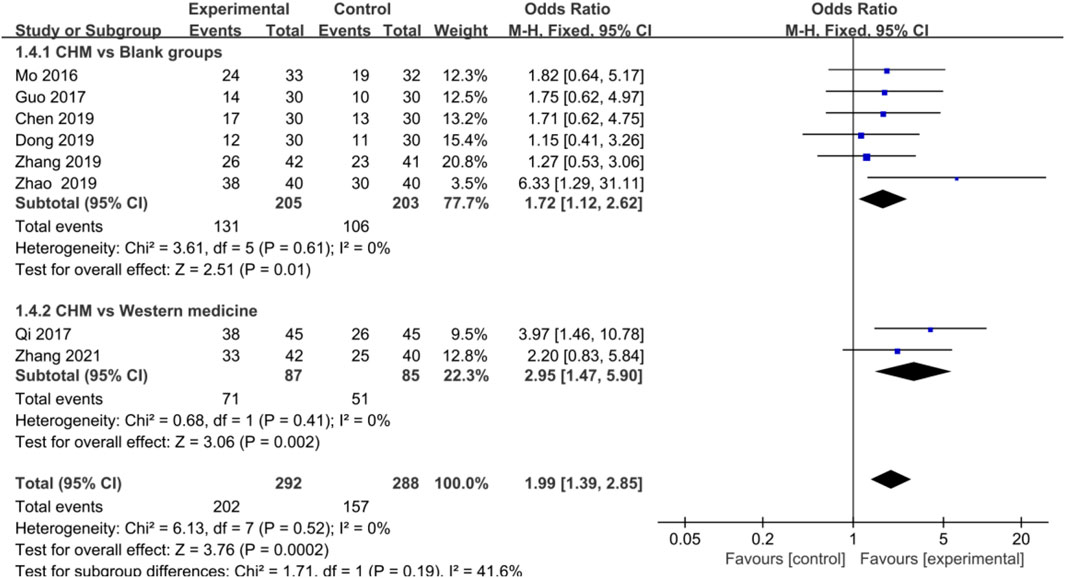
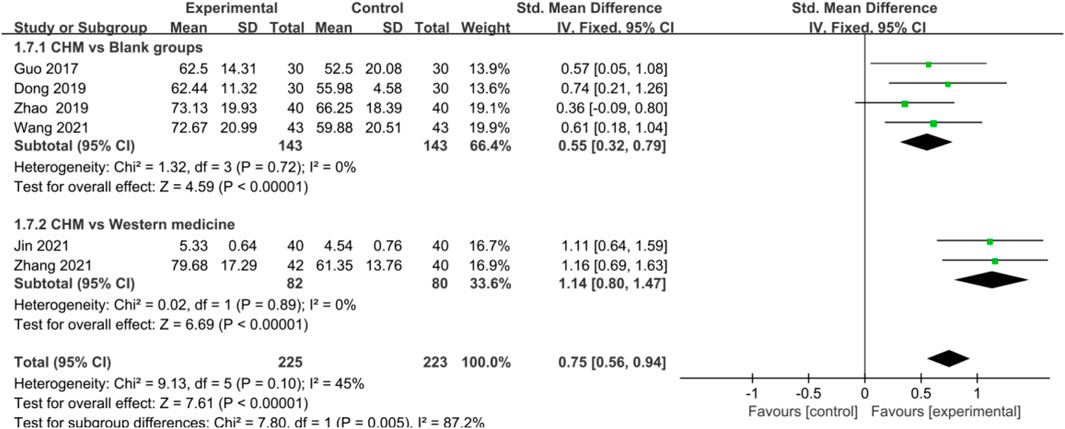
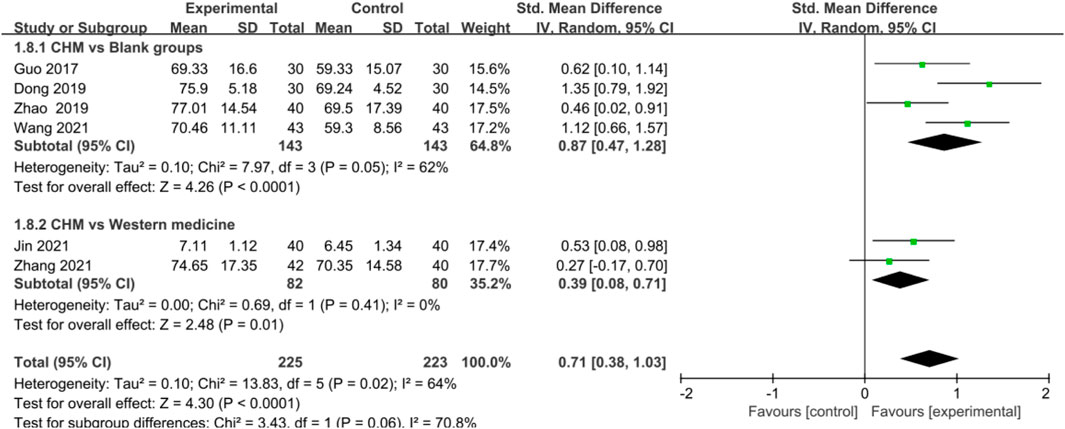
Results: A total of 32 studies were included. The results showed that compared with the blank control groups, CHM was more beneficial in treating anxiety or depression in patients with CHD [anxiety: OR = 3.22, 95% CI (1.94, 5.35), p < 0.00001, I2 = 0%; depression: OR = 3.27, 95% CI (1.67, 6.40), p = 0.0005, I2 = 0%], and the efficacy of CHM was not inferior to that of Western medicine (WM) [anxiety: OR = 1.58, 95%CI (0.39, 6.35), p = 0.52, I2 = 67%; depression: OR = 1.97, 95%CI (0.73, 5.28), p = 0.18, I2 = 33%,]. Additionally, CHM also showed a significant advantage in improving angina stability (AS) in CHD patients with anxiety or depression compared with blank groups [anxiety: SMD = 0.55, 95%CI (0.32, 0.79), p < 0.00001, I2 = 0%; depression: p = 0.004] and WM groups [anxiety: SMD = 1.14, 95%CI (0.80, 1.47), p < 0.00001, I2 = 0%; depression: SMD = 12.15, 95%CI (6.07, 18.23), p < 0.0001, I2 = 0%]. Angina frequency (AF) and electrocardiogram (ECG) analysis after using CHM demonstrated similar trends. Based on the network pharmacology, quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, stigmasterol, isorhamnetin, baicalein, tanshinone IIa, and nobiletin were most closely and simultaneously related to the pathological targets of CHD, anxiety, and depression. The main underlying mechanisms might involve anti-damage/apoptosis, anti-inflammation, antioxidative stress, and maintaining neurotransmitter homeostasis.
Conclusion: CHM exhibited an obvious efficacy in treating CHD patients with anxiety or depression, especially for improving the symptom of angina pectoris. The most active compounds of CHM could simultaneously act on the pathological targets of CHD, anxiety, and depression. Multiple effective components and multiple targets were the advantages of CHM compared with WM.
Introduction
Anxiety and depression are commonly found in patients with coronary heart disease (CHD), and the prevalence of CHD complicated with anxiety or depression is 21 and 13%, respectively (Daniel et al., 2018). Percutaneous coronary intervention (PCI) treatment increases the prevalence of anxiety and depression symptoms in CHD patients (Gu et al., 2016). Accumulating evidence has demonstrated that anxiety and depression are associated with the increased risk of CHD (Roest et al., 2010; Lederbogen and Ströhle, 2012; Giannarelli et al., 2017), and the use of anxiolytics or antidepressants is necessary for CHD patients with anxiety or depression. However, current drugs for emotional disorders, such as serotonin-specific reuptake inhibitors (SSRIs) and benzodiazepines, usually exert their effects after several weeks of treatment, with some unwanted side effects (Lakhan and Vieira, 2010; Ko et al., 2020). Thus, a more optimized treatment option is needed.
As an important treatment strategy, Chinese herbal medicine (CHM) is characterized by multiple components, multiple targets, and multiple channels. It has been verified that CHM had a satisfactory efficacy and fewer adverse effects on CHD with anxiety or depression (Liu and Qin, 2016; Ma et al., 2019). However, due to poor methodological quality and limited sample size, the evidence to support the effect of CHM on CHD with anxiety or depression is still weak. Moreover, the possible underlying mechanisms via which CHM treats CHD patients with anxiety or depression is still needed to be clarified. Therefore, by comprehensively analyzing published studies, a meta-analysis and systematic review were performed to assess the efficacy of CHM and the underlying mechanisms in the treatment of CHD patients with anxiety or depression, which might provide an essential clinical value for the disease management in the future.
Methods
This meta-analysis and systematic review were performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines (Moher et al., 2009).
Information Source and Search Strategy
Published articles were searched comprehensively in electronic databases (PubMed, Web of Science, Embase, Cochrane, China National Knowledge Infrastructure, WanFang Data, VIP Database, and SinoMed) up to October 2021. “Coronary disease OR coronary artery disease OR myocardial infarction OR acute coronary syndrome” AND “anxiety OR depression OR depressive disorder” AND “traditional Chinese medicine OR herbal medicine” AND “randomized controlled trial” and their common synonyms were used for the searching strategy. The detailed searching strategy was shown in supplementary material.
Inclusion and Exclusion Criteria
The inclusion criteria of the articles were as follows: 1) all participants met the diagnostic criteria of CHD with anxiety or depression; 2) the number of subjects in each group was not less than 30; 3) CHD patients in control and trial groups received basic treatments, with antianxiety or antidepressant Western medicine (WM) used (WM groups) or not (blank control groups) in control groups, and oral CHM was used in trial groups; 4) Hamilton anxiety scale (HAMA) and Hamilton depression scale (HAMD) were used to evaluate patients’ anxiety and depression, respectively; and 5) the efficacy index of CHD included one of the following: ① electrocardiogram (ECG); ② angina stability (AS) and angina frequency (AF) come from Seattle Angina Questionnaire; and ③ traditional Chinese medicine syndrome (TCMS) score.
The exclusion criteria of the studies were as follows: 1) Nonclinical study and irrelevant research; 2) CHM was used in control groups, antianxiety or antidepressant WM was used in trial groups; 3) articles with incomplete data; 4) articles more than one high-risk item; and 5) review, meta-analysis, and conference abstracts.
Study Selection and Data Extraction
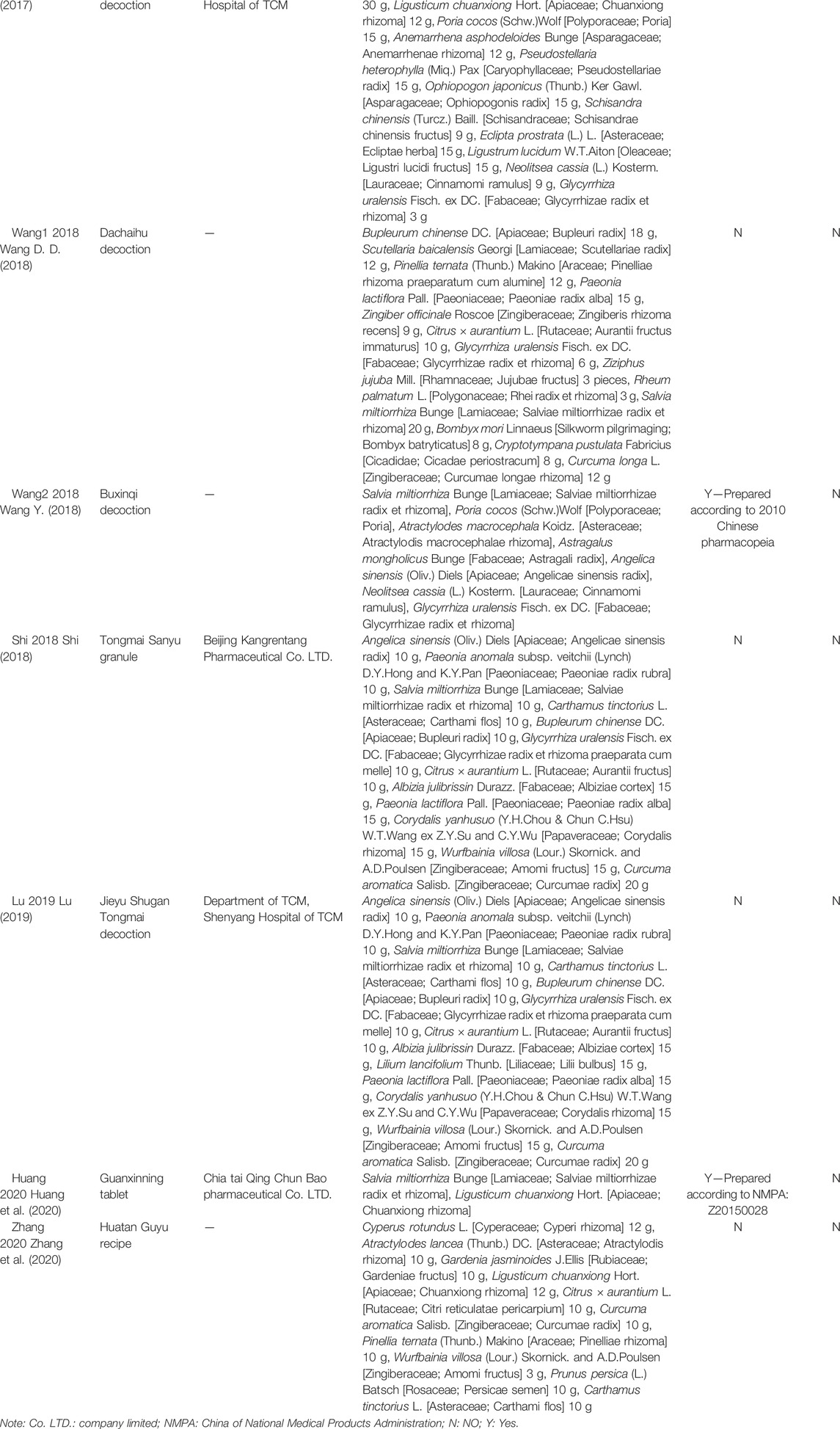
Retrieved articles were assessed independently by two researchers (YT and SL) according to the inclusion and exclusion criteria. Data, including first authors’ name, year of publication, sample size, age, gender, diseases, therapeutic regimen, final duration of treatment, dosage form and compositions of TCM, and the outcome index, were extracted from the included studies. The CHM was reported in scientific name, not the Latin name in pharmacopeia to avoid confusion (Table 1) (Rivera et al., 2014). Any disagreements were resolved by discussing and consulting with corresponding authors (MZ and XW).
Study Quality Assessment
Two authors (YL and YT) independently assessed the methodological quality according to the Cochrane risk-of-bias tool (Zhang K. J. et al., 2019). Sufficient domain information in relevant studies was considered as low risk, inadequate information was regarded as unclear risk, and no related information was regarded as high risk.
Data Analysis and Synthesis
RevMan 5.3 software provided by the Cochrane Collaboration was used for meta-analysis. The odds ratio (OR) and standard mean difference (SMD) were used to analyze the pooled effects of dichotomous outcomes and continuous variable, respectively. When the heterogeneity of included studies was low (I2 < 50%), the fixed effect model was selected to analyze the data; otherwise, a random-effects model was applied. The subgroups analysis was based on whether control groups used WM or not. Sensitivity analysis was performed to explore potential effect modification. Also, funnel plots were used to assess publication bias. p < 0.05 was considered statistically significant.
Chinese Herbal Medicine Compositions and Potential Mechanisms
The frequency statistics of single CHM was performed to identify the commonly used drugs, and CHM with frequency not less than three were selected for network pharmacology to find the primary active ingredients and the disease targets. The targets of the active ingredient of CHM were extracted from the Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform, while the targets of CHD, anxiety, and depression were collected from the GeneCards database. The networks of active ingredients-disease targets were acquired according to the Cytoscape 3.6.1. The active ingredients that most related with CHD, anxiety, and depression simultaneously were acquired by matching ingredients-disease targets. Also, the main potential mechanisms of the primary active compounds (top 10) were summarized by the database of Web of Science.
Results
Literature Search Results
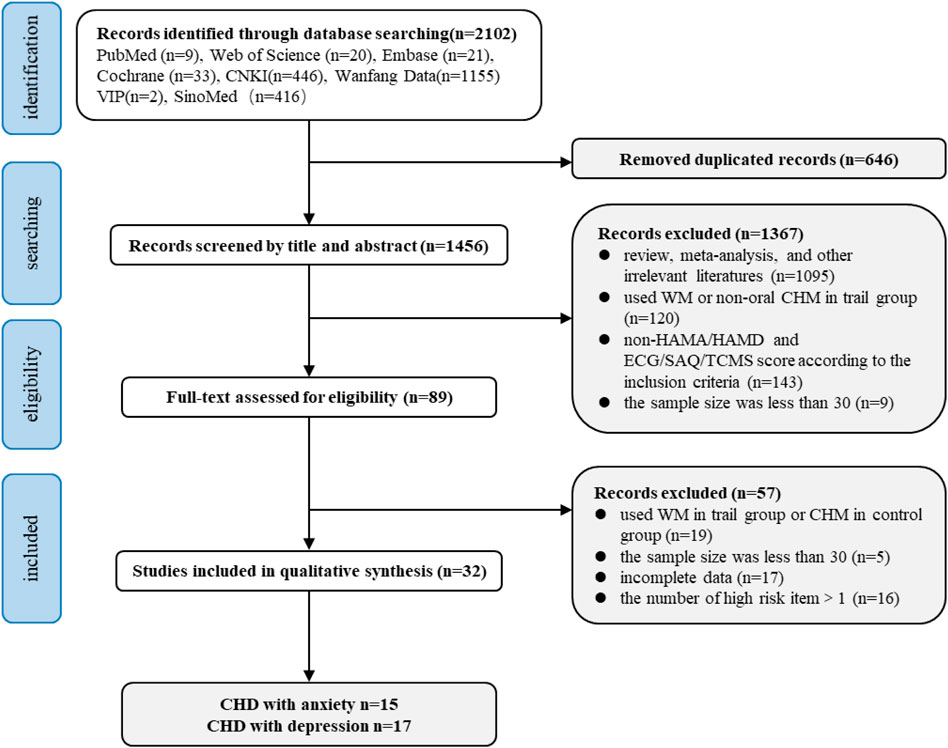
A total of 2,102 records were identified from eight electronic databases. Thirty-two studies met the inclusion criteria, and 2070 studies were excluded due to 1) irrelevant studies; 2) nonclinical studies; 3) review, meta-analysis, and conference abstracts; 4) sample size was less than 30; 5) using WM in trial groups; 6) non-HAMA or HAMD for evaluating the efficacy of anxiety or depression; 7) non-ECG or AS or AF or TCMS score for evaluating the efficacy of CHD; and 8) articles with incomplete data or more than one high-risk item. The specific screening process is illustrated in Figure 1.
Study and Patient Characteristics
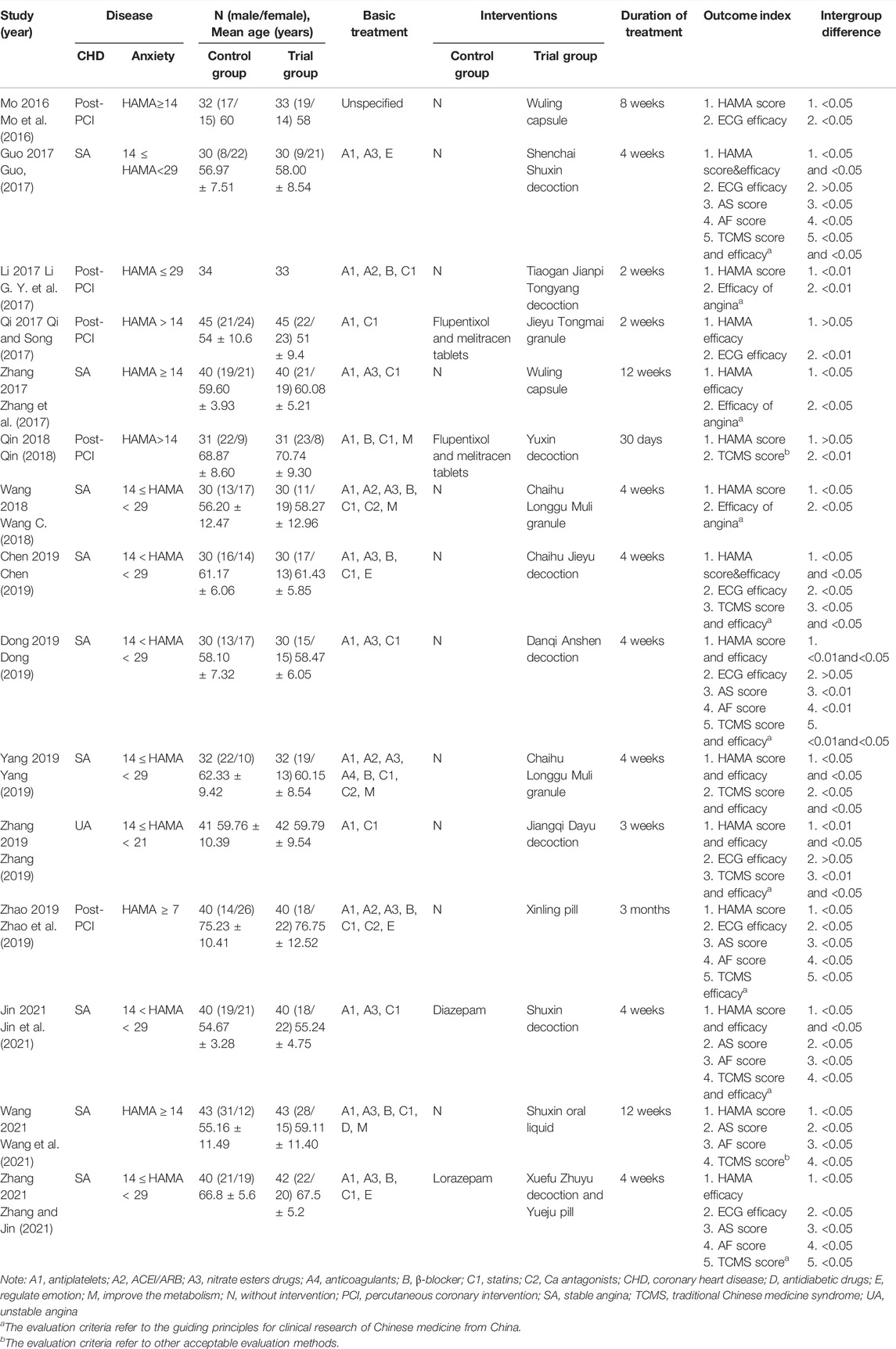
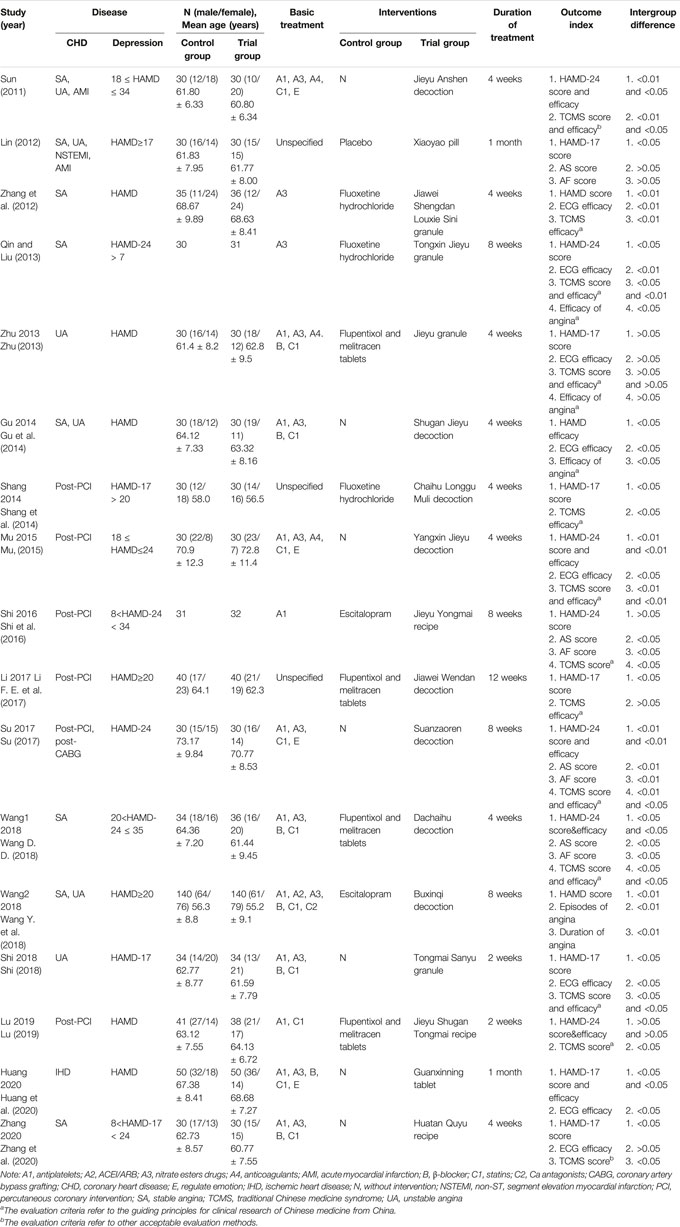
Thirty-two studies included 15 studies on CHD with anxiety (Mo et al., 2016; Li G. Y. et al., 2017; Guo, 2017; Qi and Song, 2017; Zhang et al., 2017; Qin, 2018; Wang C., 2018; Chen, 2019; Dong, 2019; Yang, 2019; Zhang, 2019; Zhao et al., 2019; Jin et al., 2021; Wang et al., 2021; Zhang and Jin, 2021) and 17 studies on CHD with depression (Sun, 2011; Lin, 2012; Zhang et al., 2012; Qin and Liu, 2013; Zhu, 2013; Gu et al., 2014; Shang et al., 2014; Mu, 2015; Shi et al., 2016; Li F. E. et al., 2017; Su, 2017; Shi, 2018; Wang Y. et al., 2018; Wang D. D., 2018; Lu, 2019; Huang et al., 2020; Zhang et al., 2020). All studies accounted for baseline comparability, and the patients’ overall characteristics are summarized in Tables 2A,B. Subjects of CHD who were diagnosed as stable angina (SA), unstable angina (UA), acute myocardial infarction (AMI), non-ST segment elevation myocardial infarction (NSTEMI), or post-percutaneous coronary intervention (post-PCI) were also evaluated by HAMA (Mo et al., 2016; Li G. Y. et al., 2017; Guo, 2017; Qi and Song, 2017; Zhang et al., 2017; Qin, 2018; Wang C., 2018; Chen, 2019; Dong, 2019; Yang, 2019; Zhang, 2019; Zhao et al., 2019; Jin et al., 2021; Wang et al., 2021; Zhang and Jin, 2021) and HAMD (Sun, 2011; Lin, 2012; Zhang et al., 2012; Qin and Liu, 2013; Zhu, 2013; Gu et al., 2014; Shang et al., 2014; Mu, 2015; Shi et al., 2016; Li F. E. et al., 2017; Su, 2017; Shi, 2018; Wang Y. et al., 2018; Wang D. D., 2018; Lu, 2019; Huang et al., 2020; Zhang et al., 2020). Secondary prevention drugs for CHD were used in all studies.
For control groups of CHD with anxiety, four studies used flupentixol and melitracen tablets (Qi and Song, 2017; Qin, 2018), diazepam (Jin et al., 2021), and lorazepam (Zhang and Jin, 2021), while nine studies used fluoxetine hydrochloride (Zhang et al., 2012; Qin and Liu, 2013; Shang et al., 2014), flupentixol and melitracen tablets (Zhu, 2013; Li F. E. et al., 2017; Wang D. D., 2018; Lu, 2019), and escitalopram (Shi et al., 2016; Wang Y. et al., 2018) in the CHD with depression. No WM were used in control groups in the remaining researches except for the study by Lin et al. who used a placebo (Lin, 2012). CHM was used in trial groups and the details are shown in Table 1. The treatment course in all studies varied from 2 weeks to 3 months. The primary efficacy endpoints, including the score and efficacy of HAMA and HAMD, ECG efficacy, AS score, and AF score, were extracted for this meta-analysis and systematic review. The score and efficacy of TCMS were also extracted for the evaluation as the secondary efficacy endpoint.
Quality Assessment of Included Studies
The study methodological quality is concluded in Supplementary Table S1. Random allocation was used in all included studies. Five studies performed blind method (Lin, 2012; Mo et al., 2016; Li G. Y. et al., 2017; Wang C., 2018; Su, 2017), and blinded outcome assessment was conducted in two studies (Qi and Song, 2017; Zhang and Jin, 2021). Additionally, allocation concealment was used in three studies (Sun, 2011; Mo et al., 2016; Wang C., 2018).
Efficacy of Chinese Herbal Medicine in Coronary Heart Disease With Anxiety
As shown in Table 2A, the score and efficacy of HAMA, ECG, AS, AF, and TCMS in trial groups in most studies possessed a significant improvement. However, there were also some different results. Two studies showed that there was no significant difference in the score or efficacy of HAMA between trial groups and flupentixol and melitracen tablet-treated groups (Qi and Song, 2017; Qin, 2018). Three studies reported that the efficacy of ECG in trial groups was not significantly different compared with blank control groups (Mo et al., 2016; Chen, 2019; Zhang, 2019). Thus, the primary endpoint results were pooled to further confirm the efficacy of CHM.
Efficacy of Chinese Herbal Medicine in Anxiety
In Supplementary Figure S1, the HAMA score displayed significant heterogeneity due to scoring bias in different studies. Therefore, the efficacy of CHM for treating anxiety was further analyzed. Meta-analysis of nine studies showed a significant efficiency of CHM for improving anxiety [OR = 2.73, 95%CI (1.78, 4.18), p < 0.00001, I2 = 0%] (Figure 2), and the subgroup analysis based on whether the control group used WM or not was also performed. As shown in Figure 2, the results of subgroup analysis showed a favor for CHM in curing anxiety in CHD patients compared with blank control groups [OR = 3.22, 95%CI (1.94, 5.35), p < 0.00001, I2 = 0%], whereas the efficacy of CHM in treating anxiety was not inferior to that of WM [OR = 1.58, 95%CI (0.39, 6.35), p = 0.52, I2 = 67%]. Moreover, a repetitive meta-analysis by consecutively excluding each study in WM groups was performed. The study by Qi et al. was the main source of heterogeneous, but it was not removed because of reasonable research design.
Efficacy of Chinese Herbal Medicine in Coronary Heart Disease
Meta-analysis of eight studies showed that the improvement of ECG in CHD patients was significantly associated with CHM treatment [OR = 1.99, 95%CI (1.39, 2.85), p = 0.0002, I2 = 0%] (Figure 3). In addition, subgroup analysis showed a consistent result favoring CHM in improving CHD compared with blank [OR = 1.72, 95%CI (1.12, 2.62), p = 0.01, I2 = 0%] and WM groups [OR = 2.95, 95%CI (1.47, 5.90), p = 0.002, I2 = 0%] (Figure 3).
In terms of improving AS and AF, CHM also showed a significant advantage in trial groups compared with control groups [AS: SMD = 0.75, 95%CI (0.56, 0.94), p < 0.00001, I2 = 45%; AF: SMD = 0.71, 95%CI (0.38, 1.03), p < 0.0001, I2 = 64%] (Figures 4, 5), blank groups [AS: SMD = 0.55, 95%CI (0.32, 0.79), p < 0.00001, I2 = 0%; AF: SMD = 0.87, 95%CI (0.47, 1.28), p < 0.0001, I2 = 62%], and WM groups [AS: SMD = 1.14, 95%CI (0.80, 1.47), p < 0.00001, I2 = 0%; AF: SMD = 0.39, 95%CI (0.08, 0.71), p = 0.01, I2 = 0%] (Figures 4, 5).
Efficacy of Traditional Chinese Medicine in Coronary Heart Disease With Depression
As shown in Table 2B, most included studies showed a significant improvement in the score and efficacy of HAMD, ECG, AS, AF, and TCMS in treatment groups. However, some studies showed different results. Three studies reported that the score or efficacy of HAMD in CHM groups was no statistical difference between treatment and control groups using antidepressants (Zhu, 2013; Shi et al., 2016; Lu, 2019). Similarly, for the score or efficacy of ECG, angina, and TCMS, there were also no statistical differences between treatment and control groups (Zhu, 2013; Gu et al., 2014; Shang et al., 2014; Li F. E. et al., 2017; Zhang et al., 2020). Additionally, the study by Lin et al. was the only study that used placebo (Lin, 2012). The scores of AS and AF were not significantly different between the CHM and placebo group, but the result of the 36-item short form survey showed a superior benefit of CHM compared with placebo. In the study by Wang Y. et al. (2018), antidepressants and CHM both possessed obvious efficacy for treating CHD with depression, and antidepressants exhibited even more efficiency. Therefore, the primary endpoint results were pooled to further confirm the efficacy of CHM.
Efficacy of Chinese Herbal Medicine in Depression
Meta-analysis of seven studies showed that CHM had a significant effect on treating depression compared with control groups [OR = 2.79, 95%CI (1.61, 4.86), p = 0.0003, I2 = 0%] (Figure 6). The results of subgroup analysis also revealed that the antidepressive effect was improved significantly compared with blank control groups [OR = 3.27, 95%CI (1.67, 6.40), p = 0.0005, I2 = 0%] but was the same as WM groups [OR = 1.97, 95%CI (0.73, 5.28), p = 0.18, I2 = 33%] (Figure 6).
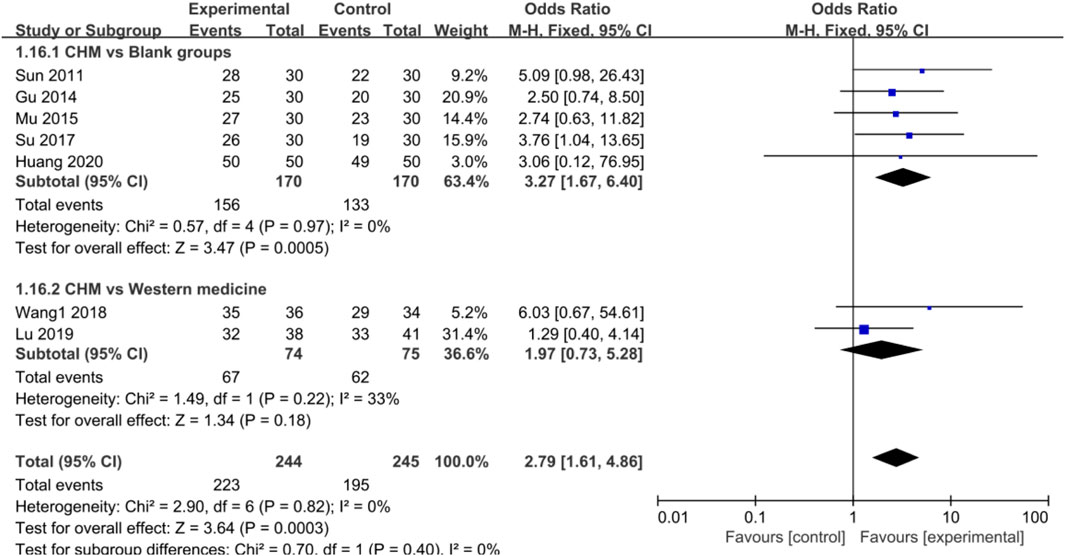
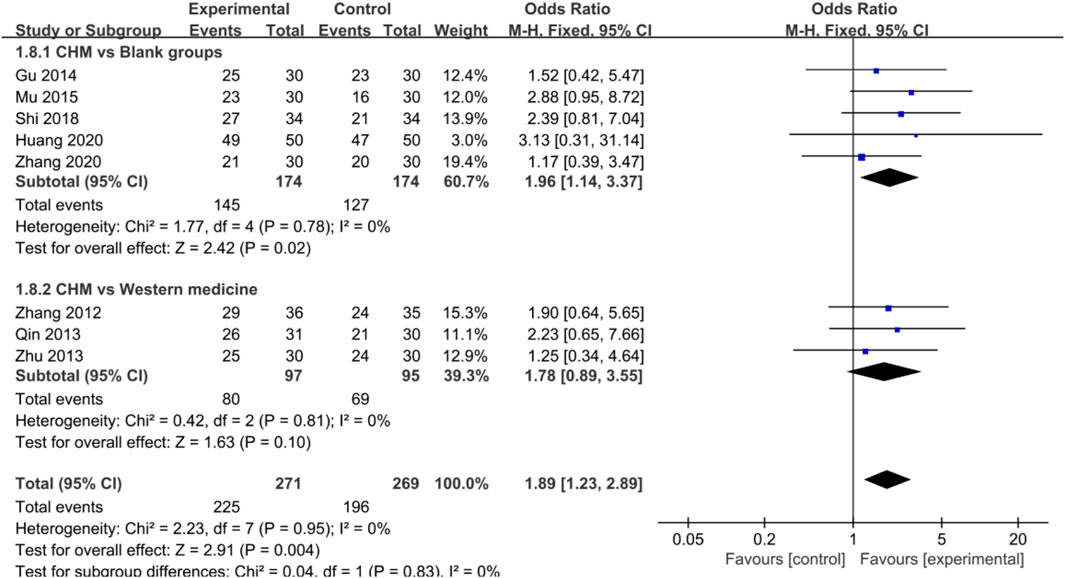
FIGURE 6. Forest plot: CHM improved HAMD efficacy in CHD with depression compared with control groups.
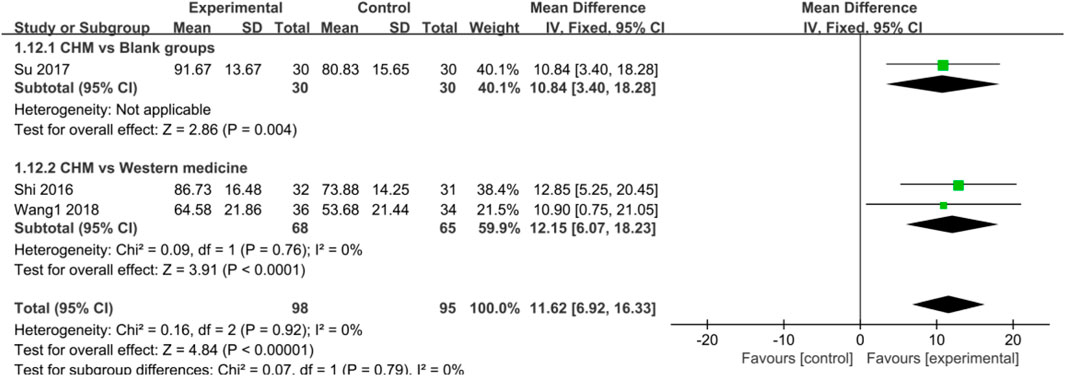
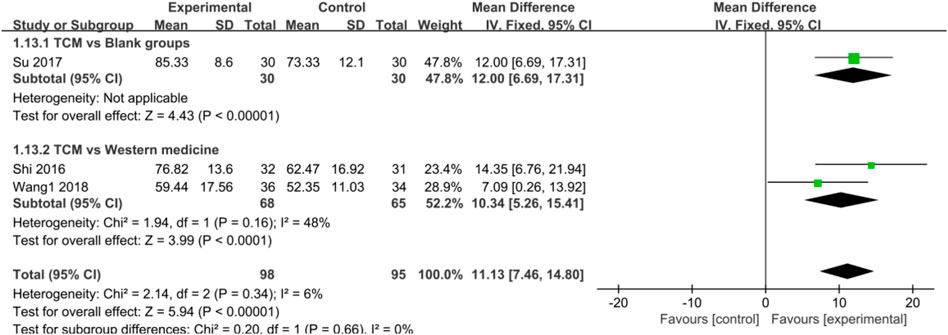
Efficacy of Chinese Herbal Medicine in Coronary Heart Disease
Eight studies reported that CHM significantly improved ECG in CHD patients [OR = 1.89, 95%CI (1.23, 2.89), p = 0.004, I2 = 0%] (Figure 7). In addition, subgroup analysis showed a similar result favoring CHM in improving CHD compared with blank groups [OR = 1.96, 95%CI (1.14, 3.37), p = 0.02, I2 = 0%], but no statistical difference was found when comparing CHM with WM groups [OR = 1.78, 95%CI (0.89, 3.55), p = 0.10, I2 = 0%] (Figure 7).
Regarding the efficacy of CHM in AS and AF, CHM also provided a more significant advantage compared with control groups [AS: SMD = 11.62, 95%CI (6.92, 16.33), p < 0.00001, I2 = 0%; AF: SMD = 11.13, 95%CI (7.46, 14.80), p < 0.00001, I2 = 6%] (Figures 8, 9), blank groups [AS: p = 0.004; AF: p < 0.00001], and WM [AS: SMD = 12.15, 95%CI (6.07, 18.23), p < 0.0001, I2 = 0%; AF: SMD = 10.34, 95%CI (5.26, 15.41), p < 0.0001, I2 = 48%] (Figures 8, 9).
Comparisons of the Characteristics of Chinese Herbal Medicine in Coronary Heart Disease With Anxiety or Depression
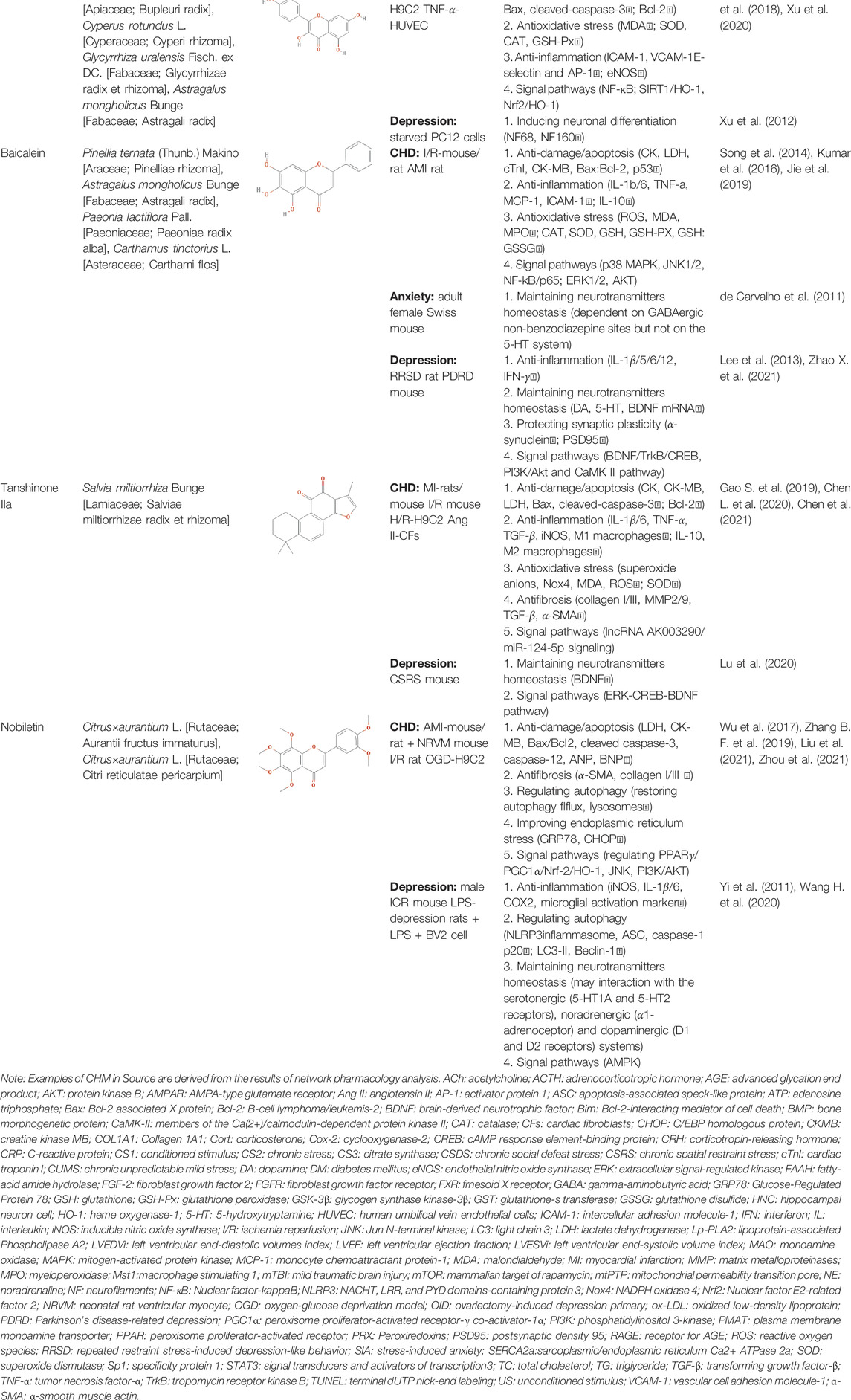
Due to the promising results of CHM treatment observed in most included studies, the frequency statistics of CHM was analyzed to identify the commonly used drugs among different groups. The results showed that Bupleurum chinense DC. [Apiaceae; Bupleuri radix], Glycyrrhiza uralensis Fisch. ex DC. [Fabaceae; Glycyrrhizae radix et rhizoma], Ligusticum chuanxiong Hort. [Apiaceae; Chuanxiong rhizoma], Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae radix et rhizoma], Angelica sinensis (Oliv.) Diels [Apiaceae; Angelicae sinensis radix], Paeonia lactiflora Pall. [Paeoniaceae; Paeoniae radix alba], Pinellia ternata (Thunb.) Makino [Araceae; Pinelliae rhizoma], Curcuma aromatica Salisb. [Zingiberaceae; Curcumae radix], and Citrus×aurantium L. [Rutaceae; Aurantii fructus] were commonly used for treating CHD with anxiety or depression (Supplementary Table S2). Also, the CHM with a frequency not less than three were selected for the networks of active ingredients-disease targets, and the results demonstrated the efficacy of CHM for CHD with anxiety or depression (Supplementary Figure S2). Furthermore, the primary active ingredients of these CHM that could act on the targets of CHD, anxiety, and depression simultaneously were analyzed by matching ingredients disease targets. The results showed the active ingredients including quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, stigmasterol, isorhamnetin, baicalein, tanshinone IIa, and nobiletin were most closely related to the targets of CHD, anxiety, and depression based on degree centrality, and the top 10 ingredients are shown in Table 3. These active compounds could either act on the targets of CHD, anxiety, and depression simultaneously or be extracted from varieties CHM.
Potential Relevant Mechanisms
The effects and mechanisms of the primary active compounds (top 10) were searched in the Web of Science database. As shown in Table 3, the experimental research of quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, and baicalein covered CHD, anxiety, and depression. Models of myocardial infarction or ischemia reperfusion were commonly used in the study of CHD, while the ICR mice and multiple stress-stimulated rats were selected for anxiety and depression research.
The related mechanisms of these top 10 active ingredients in CHD, anxiety, and depression are summarized in Table 3, which mainly includes anti damage/apoptosis, anti-inflammation, antioxidative stress, antifibrosis, maintaining neurotransmitters homeostasis, and regulating autophagy. In addition, myocardial injure biomarkers (lactate dehydrogenase, creatine kinase MB, cardiac troponin I) and the damage/apoptosis biomarkers (Bcl-2 associated X protein, cleaved caspase-3, p53, B-cell lymphoma/leukemis-2) could be regulated by quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, isorhamnetin, baicalein, tanshinone IIa, and nobiletin. These phytochemicals were also reported to exert an anti-inflammatory effect by reducing the levels of interleukin (IL) -1β/6, tumor necrosis factor-α, vascular cell adhesion molecule-1, intercellular adhesion molecule-1, E-selectin, or elevating the IL-10 level in CHD patients. The anti-inflammatory role of quercetin, puerarin, or nobiletin was reported in anxiety or depression. Additionally, almost all active ingredients except stigmasterol and nobiletin possessed the functions of antioxidative stress and balancing level of reactive oxygen species, malondialdehyde, myeloperoxidase, and catalase, superoxide dismutase, glutathione. Quercetin, tanshinone IIa, and nobiletin were reported to reduce the levels of α-smooth muscle actin, angiotensin II, collagen I/III, matrix metalloproteinases 2/9, transforming growth factor (TGF)-β, and Smad7 to prevent myocardial fibrosis, which was one of the complications associated with myocardial infarction. Besides, the imbalance of adrenocorticotropic hormone, 5-hydroxytryptamine, brain-derived neurotrophic factor (BDNF), acetylcholine, noradrenaline, dopamine, and gamma-aminobutyric acid, which caused anxiety or depression, could be regulated by quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, stigmasterol, baicalein, tanshinone IIa, or nobiletin. Isorhamnetin and baicalein could improve the depression by inducing neuronal differentiation and protecting synaptic plasticity, respectively. The roles of active compounds in regulating autophagy and improving mitochondria were also reported. Overall, the related mechanisms of TCM-active compounds in treating CHD with anxiety or depression contained a variety of signaling pathways, such as nuclear factor-kappa B, mitogen-activated protein kinase, Jun N-terminal kinase, extracellular signal-regulated kinase1/2, signal transducers and activators of transcription3, TGF-β1/Smad3, phosphatidylinositol 3-kinase/protein kinase B, and BDNF.
Discussion
There is accumulating evidence showing high prevalence of anxiety and depression comorbidities in patients with CHD. SSRIs and benzodiazepines are frequently used for treating depression or anxiety disorders, and the effectiveness of these drugs on psychiatric disorders has also been acknowledged (Davies et al., 2004). However, the side effects, such as suicidal ideation, sexual dysfunction, and dependency, have not been resolved (Lakhan and Vieira, 2010; Ko et al., 2020). In addition, it is a common clinical phenomenon that CHD patients show subsyndromal anxiety or depression-like symptoms that do not meet the diagnostic criteria of anxiety or depression (Cohen et al., 2006; Kasckow et al., 2013). The issue of treatment for these patients still deserves much attention.
TCM has been reported to be effective in treating CHD, anxiety, and depression with a less adverse effect, and might be a potential therapeutic option for patients with subsyndromal anxiety or depression. However, the efficacy and benefit of CHM in treating CHD with anxiety or depression still need to be further verified due to poor methodological quality and potential confounding factors. This meta-analysis and systematic review was performed to provide the evidence for the application of CHM in CHD patients with anxiety or depression. Thirty-two studies (15 CHD with anxiety, and 17 CHD with depression) were included for the evaluation of the efficacy of CHM. The results showed that CHM had a significant benefit on anxiety and depression in CHD patients, and its efficacy was not inferior to that of WM. Importantly, CHM also had a significant advantage to alleviate the angina symptom compared with blank control and WM groups. Besides that, there were no obvious adverse effects of CHM in the included studies (Zhang et al., 2012; Qin and Liu, 2013; Zhu, 2013; Mo et al., 2016; Shi et al., 2016; Guo, 2017; Wang Y. et al., 2018; Wang C., 2018; Wang D. D., 2018; Chen, 2019; Lu, 2019; Yang, 2019; Huang et al., 2020).
Furthermore, the frequency of CHM used in the included studies was analyzed, and the commonly used drugs were analyzed by network pharmacology. The results concluded that the CHM regulating Qi and promoting blood circulation, including Bupleurum chinense DC. [Apiaceae; Bupleuri radix], Glycyrrhiza uralensis Fisch. ex DC. [Fabaceae; Glycyrrhizae radix et rhizoma], Ligusticum chuanxiong Hort. [Apiaceae; Chuanxiong rhizoma], Salvia miltiorrhiza Bunge [Lamiaceae; Salviae miltiorrhizae radix et rhizoma], Angelica sinensis (Oliv.) Diels [Apiaceae; Angelicae sinensis radix], Paeonia lactiflora Pall. [Paeoniaceae; Paeoniae radix alba], Pinellia ternata (Thunb.) Makino [Araceae; Pinelliae rhizoma], Curcuma aromatica Salisb. [Zingiberaceae; Curcumae radix], and Citrus×aurantium L. [Rutaceae; Aurantii fructus] were commonly used for CHD with anxiety and depression. The phytochemicals identified in the CHM could act on the pathological targets of CHD, anxiety, and depression simultaneously.
Inflammatory response to vascular injury participates in the pathological processes of the atherosclerosis and CHD, and is associated with the increased risk of cardiovascular events and recurrent myocardial infarction (Fioranelli et al., 2018; Zhang K. J. et al., 2019). Oxidative stress is also an important factor involved in myocardial cell injury and apoptosis caused by ischemia reperfusion, which is followed by heart failure and myocardial fibrosis (Li et al., 2018; Yang et al., 2019). The effectiveness of CHM ingredients including quercetin, kaempferol, luteolin, beta-sitosterol, puerarin, and baicalein was reported in the experimental research on CHD. Puerarin, quercetin, and tanshinone IIa were also shown to have a satisfactory efficacy in improving clinical prognosis (Mao et al., 2019; Zhang S. et al., 2019; Dehghani et al., 2021). Additionally, inflammation and oxidative stress could cause neuron damage and neurotransmitter disorder, leading to anxiety and depression (Bankier et al., 2009; Liu et al., 2015; van Dooren et al., 2016; Salim, 2017; Wang Y. L. et al., 2018). Quercetin, kaempferol, luteolin, and puerarin also showed a positive effect in curing anxiety and depression.
Overall, these findings reveal that the CHM has a satisfactory efficacy for CHD with anxiety and depression, especially for improving the symptom of angina pectoris. Of importance, CHM itself contains multiple components that play critical functions in a large number of signaling pathways involved in distinct biological processes of CHD with anxiety or depression mainly including anti-damage/apoptosis, anti-inflammation, antioxidative stress, and maintaining neurotransmitters homeostasis. Compared with WM’s single effect on the nervous system, CHM may extert its functions in multiple places and systems by targeting distinct factors in CHD with anxiety or depression to improve both CHD and anxiety/depression syndromes.
Limitations
First, the sample size in each group of included studies was not more than 50, except the study by Wang Y. L. et al. (2018), and the sample size needs to be expanded in future studies. Second, it is difficult to perform double blind due to the special smell and taste of TCM decoction. Also, the characteristics of TCM treatment affect the implementation of double blind. Additionally, the blinding of outcome assessment was conducted in 2 of 32 studies (Qi and Song, 2017; Zhang and Jin, 2021). Therefore, the strict trial design is also necessary to further verify the efficacy of CHM.
Conclusion
CHM had a significant efficacy for the treatment of CHD patients with anxiety or depression. Particularly, CHM could improve the symptoms of angina pectoris while alleviating anxiety and depression. The main mechanisms underlying the functions of these CHM-active ingredients might involve anti-damage/apoptosis, anti-inflammation, antioxidative stress, antifibrosis, maintaining neurotransmitters homeostasis, and regulating autophagy.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
BW, YT, and YL are co-first authors. Theme and design of the research: BW, YT, and YL. Extract data: YL, YT, and SL. Network pharmacology: YW. Statistical analysis: SC, YL, and XH. Data handling of mechanisms: HZ, YW, ZL, HL, YD, and LM. Writing of the manuscript: BW, YT, and YL. Critical revision of the manuscript for intellectual content: MZ and XW. Obtaining funding: MZ and XW.
Funding
This study was supported by the National Natural Science Foundation of China (81973787) and the key research projects of Beijing University of Chinese Medicine (2020-JYB-ZDGG-113).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.854292/full#supplementary-material
Abbreviations
AF, angina frequency; AS, angina stability; CHD, coronary heart disease; CHM, Chinese herbal medicine; ECG, electrocardiogram; HAMA, Hamilton anxiety scale; HAMD, Hamilton depression scale; TCM, traditional Chinese medicine; WM, Western medicine.
References
Aguirre-Hernández, E., Rosas-Acevedo, H., Soto-Hernández, M., Martínez, A. L., Moreno, J., and González-Trujano, M. E. (2007). Bioactivity-guided Isolation of Beta-Sitosterol and Some Fatty Acids as Active Compounds in the Anxiolytic and Sedative Effects of Tilia Americana Var. Mexicana. Planta Med. 73, 1148–1155. doi:10.1055/s-2007-981593
Ahmad, H., Rauf, K., Zada, W., McCarthy, M., Abbas, G., Anwar, F., et al. (2020). Kaempferol Facilitated Extinction Learning in Contextual Fear Conditioned Rats via Inhibition of Fatty-Acid Amide Hydrolase. Molecules 25, 4683. doi:10.3390/molecules25204683
Albadrani, G. M., Binmowyna, M. N., Bin-Jumah, M. N., El-Akabawy, G., Aldera, H., and Al-Farga, A. M. (2020). Quercetin Protects against Experimentally-Induced Myocardial Infarction in Rats by an Antioxidant Potential and Concomitant Activation of Signal Transducer and Activator of Transcription 3. J. Physiol. Pharmacol. official J. Polish Physiol. Soc. 71, 875–890. doi:10.26402/jpp.2020.6.11
Albadrani, G. M., BinMowyna, M. N., Bin-Jumah, M. N., El–Akabawy, G., Aldera, H., and AL-Farga, A. M. (2021). Quercetin Prevents Myocardial Infarction Adverse Remodeling in Rats by Attenuating TGF-β1/Smad3 Signaling: Different Mechanisms of Action. Saudi J. Biol. Sci. 28, 2772–2782. doi:10.1016/j.sjbs.2021.02.007
Bankier, B., Barajas, J., Martinez-Rumayor, A., and Januzzi, J. L. (2009). Association between Anxiety and C-Reactive Protein Levels in Stable Coronary Heart Disease Patients. Psychosomatics 50, 347–353. doi:10.1176/appi.psy.50.4.347
Chen, L., Wei, L., Yu, Q., Shi, H., and Liu, G. (2020). Tanshinone IIA Alleviates Hypoxia/reoxygenation Induced Cardiomyocyte Injury via lncRNA AK003290/miR-124-5p Signaling. BMC Mol. Cell Biol 21, 20. doi:10.1186/s12860-020-00264-3
Chen, R., Chen, W., Huang, X., and Rui, Q. (2021). Tanshinone IIA Attenuates Heart Failure via Inhibiting Oxidative Stress in Myocardial Infarction Rats. Mol. Med. Rep. 23, 404. doi:10.3892/mmr.2021.12043
Chen, T., Zhang, X., Zhu, G., Liu, H., Chen, J., Wang, Y., et al. (2020). Quercetin Inhibits TNF-α Induced HUVECs Apoptosis and Inflammation via Downregulating NF-kB and AP-1 Signaling Pathway In Vitro. Medicine (Baltimore) 99, e22241. doi:10.1097/MD.0000000000022241
Chen, T. L., Zhu, G. L., Wang, J. A., Zhang, G. D., Liu, H. F., Chen, J. R., et al. (2015). Protective Effects of Isorhamnetin on Apoptosis and Inflammation in TNF-α-Induced HUVECs Injury. Int. J. Clin. Exp. Pathol. 8, 2311–2320.
Chen, Y. N. (2019). Clinical Observation of Chaihu Jieyu Decoction in the Treatment of Coronary Heart Disease Stable Angina Pectoris (Qi Stagnation, Blood Stasis and Phlegm Turbidity) with Anxiety (Heilongjiang, China: Heilongjiang University of Chinese Medicine). master’s thesis.
Cheng, J., Chen, M., Zhu, J. X., Li, C. F., Zhang, Q. P., Geng, D., et al. (2019). FGF-2 Signaling Activation in the hippocampus Contributes to the Behavioral and Cellular Responses to Puerarin. Biochem. Pharmacol. 168, 91–99. doi:10.1016/j.bcp.2019.06.025
Cohen, C. I., Magai, C., Yaffee, R., and Walcott-Brown, L. (2006). The Prevalence of Anxiety and Associated Factors in a Multiracial Sample of Older Adults. Psychiatr. Serv. 57, 1719–1725. doi:10.1176/ps.2006.57.12.1719
Coleta, M., Campos, M. G., Cotrim, M. D., Lima, T. C., and Cunha, A. P. (2008). Assessment of Luteolin (3',4',5,7-tetrahydroxyflavone) Neuropharmacological Activity. Behav. Brain Res. 189, 75–82. doi:10.1016/j.bbr.2007.12.010
Daniel, M., Agewall, S., Berglund, F., Caidahl, K., Collste, O., Ekenbäck, C., et al. (2018). Prevalence of Anxiety and Depression Symptoms in Patients with Myocardial Infarction with Non-obstructive Coronary Arteries. Am. J. Med. 131, 1118–1124. doi:10.1016/j.amjmed.2018.04.040
Davies, S. J., Jackson, P. R., Potokar, J., and Nutt, D. J. (2004). Treatment of Anxiety and Depressive Disorders in Patients with Cardiovascular Disease. BMJ 328, 939–943. doi:10.1136/bmj.328.7445.939
de Carvalho, R. S., Duarte, F. S., and de Lima, T. C. (2011). Involvement of GABAergic Non-benzodiazepine Sites in the Anxiolytic-like and Sedative Effects of the Flavonoid Baicalein in Mice. Behav. Brain Res. 221, 75–82. doi:10.1016/j.bbr.2011.02.038
de la Peña, J. B., Kim, C. A., Lee, H. L., Yoon, S. Y., Kim, H. J., Hong, E. Y., et al. (2014). Luteolin Mediates the Antidepressant-like Effects of Cirsium Japonicum in Mice, Possibly through Modulation of the GABAA Receptor. Arch. Pharm. Res. 37, 263–269. doi:10.1007/s12272-013-0229-9
Dehghani, F., Sezavar Seyedi Jandaghi, S. H., Janani, L., Sarebanhassanabadi, M., Emamat, H., and Vafa, M. (2021). Effects of Quercetin Supplementation on Inflammatory Factors and Quality of Life in post-myocardial Infarction Patients: A Double Blind, Placebo-Controlled, Randomized Clinical Trial. Phytother Res. 35, 2085–2098. doi:10.1002/ptr.6955
Dong, X. (2019). Clinical Observation of Danqi Anshen Decoction in Treating Coronary Heart Disease Stable Angina Pectoris (Qi Deficiency and Blood Stasis Type) with Anxiety (Heilongjiang, China: Heilongjiang University of Chinese Medicine). master’s thesis.
Fioranelli, M., Bottaccioli, A. G., Bottaccioli, F., Bianchi, M., Rovesti, M., and Roccia, M. G. (2018). Stress and Inflammation in Coronary Artery Disease: A Review Psychoneuroendocrineimmunology-Based. Front Immunol. 9, 2031. doi:10.3389/fimmu.2018.02031
Gao, S., Li, L., Li, L., Ni, J., Guo, R., Mao, J., et al. (2019). Effects of the Combination of Tanshinone IIA and Puerarin on Cardiac Function and Inflammatory Response in Myocardial Ischemia Mice. J. Mol. Cell. Cardiol. 137, 59–70. doi:10.1016/j.yjmcc.2019.09.012
Gao, W., Wang, W., Peng, Y., and Deng, Z. (2019). Antidepressive Effects of Kaempferol Mediated by Reduction of Oxidative Stress, Proinflammatory Cytokines and Up-Regulation of AKT/β-catenin cascade. Metab. Brain Dis. 34, 485–494. doi:10.1007/s11011-019-0389-5
Giannarelli, C., Rodriguez, D. T., Zafar, M. U., Christoffel, D., Vialou, V., Peña, C., et al. (2017). Susceptibility to Chronic Social Stress Increases Plaque Progression, Vulnerability and Platelet Activation. Thromb. Haemost. 117, 816–818. doi:10.1160/TH16-10-0817
Gu, G., Zhou, Y., Zhang, Y., and Cui, W. (2016). Increased Prevalence of Anxiety and Depression Symptoms in Patients with Coronary Artery Disease before and after Percutaneous Coronary Intervention Treatment. BMC psychiatry 16, 259. doi:10.1186/s12888-016-0972-9
Gu, Y. Q., Li, X. Q., and Yao, Z. P. (2014). Clinical Study of Shugan Jieyu Decoction on Coronary Heart Disease Complicated with Depression. Chin. J. Integr. Med. Cardio-/Cerebrovascuiar Dis. 12, 1435–1437.
Guan, T., Cao, C., Hou, Y., Li, Y., Wei, X., Li, S., et al. (2021). Effects of Quercetin on the Alterations of Serum Elements in Chronic Unpredictable Mild Stress-Induced Depressed Rats. Biometals 34, 589–602. doi:10.1007/s10534-021-00298-w
Guan, Y., Wang, J., Wu, X., Song, L., Wang, Y., Gong, M., et al. (2021). Quercetin Reverses Chronic Unpredictable Mild Stress-Induced Depression-like Behavior In Vivo by Involving Nuclear Factor-E2-Related Factor 2. Brain Res. 1772, 147661. doi:10.1016/j.brainres.2021.147661
Guo, J. L. (2017). Clinical Observation of Shenchai Shuxin Decoction on Angina Pectoris Complicated with Anxiety of Coronary Heart Disease (Heilongjiang, China: Heilongjiang University of Chinese Medicine). master’s thesis.
Hu, J., Man, W., Shen, M., Zhang, M., Lin, J., Wang, T., et al. (2016). Luteolin Alleviates post-infarction Cardiac Dysfunction by Up-Regulating Autophagy through Mst1 Inhibition. J. Cell. Mol. Med. 20, 147–156. doi:10.1111/jcmm.12714
Hu, Y., Zhang, C., Zhu, H., Wang, S., Zhou, Y., Zhao, J., et al. (2020). Luteolin Modulates SERCA2a via Sp1 Upregulation to Attenuate Myocardial Ischemia/reperfusion Injury in Mice. Sci. Rep. 10, 15407. doi:10.1038/s41598-020-72325-8
Huang, C. C., Tsai, M. H., Wu, Y. C., Chen, K. T., Chuang, H. W., Chen, Y., et al. (2018). Activity Dependent Mammalian Target of Rapamycin Pathway and Brain Derived Neurotrophic Factor Release Is Required for the Rapid Antidepressant Effects of Puerarin. Am. J. Chin. Med. 1, 1–16. doi:10.1142/S0192415X18500787
Huang, X. C., Jiang, R. L., Li, L., Hua, Y., and Chen, W. J. (2020). Clinical Study on Guanxinning Tablets for Coronary Heart Disease Complicated with Depression. JOURNAL NEW CHINESE MEDICINE 52, 72–75. doi:10.13457/j.cnki.jncm.2020.18.021
Jie, Z., Xiujian, W., and Jin, L. (2019). Pharmacological Mechanism and Apoptosis Effect of Baicalein in Protecting Myocardial Ischemia Reperfusion Injury in Rats. Pak J. Pharm. Sci. 32, 407–412.
Jin, L., Ji, C. H., Mi, D., and Lu, S. S. (2021). Clinical Effect of Shuxin Decoction on Angina Pectoris Complicated with Anxiety. J. Liaoning Univ. Traditional Chin. Med. 23, 183–187. doi:10.13194/j.issn.1673-842x.2021.03.042
Karim, N., Khan, I., Abdelhalim, A., Halim, S. A., Khan, A., and Al-Harrasi, A. (2021). Stigmasterol Can Be New Steroidal Drug for Neurological Disorders: Evidence of the GABAergic Mechanism via Receptor Modulation. Phytomedicine 90, 153646. doi:10.1016/j.phymed.2021.153646
Kasckow, J. W., Karp, J. F., Whyte, E., Butters, M., Brown, C., Begley, A., et al. (2013). Subsyndromal Depression and Anxiety in Older Adults: Health Related, Functional, Cognitive and Diagnostic Implications. J. Psychiatr. Res. 47, 599–603. doi:10.1016/j.jpsychires.2013.01.017
Ko, Y. H., Kim, S. K., Lee, S. Y., and Jang, C. G. (2020). Flavonoids as Therapeutic Candidates for Emotional Disorders Such as Anxiety and Depression. Arch. Pharm. Res. 43, 1128–1143. doi:10.1007/s12272-020-01292-5
Kosari-Nasab, M., Shokouhi, G., Ghorbanihaghjo, A., Mesgari-Abbasi, M., and Salari, A. A. (2019). Quercetin Mitigates Anxiety-like Behavior and Normalizes Hypothalamus-Pituitary-Adrenal axis Function in a Mouse Model of Mild Traumatic Brain Injury. Behav. Pharmacol. 30, 282–289. doi:10.1097/FBP.0000000000000480
Kumar, M., Kasala, E. R., Bodduluru, L. N., Dahiya, V., and Lahkar, M. (2016). Baicalein Protects Isoproterenol Induced Myocardial Ischemic Injury in Male Wistar Rats by Mitigating Oxidative Stress and Inflammation. Inflamm. Res. 65, 613–622. doi:10.1007/s00011-016-0944-z
Lakhan, S. E., and Vieira, K. F. (2010). Nutritional and Herbal Supplements for Anxiety and Anxiety-Related Disorders: Systematic Review. Nutr. J. 9, 42. doi:10.1186/1475-2891-9-42
Lederbogen, F., and Ströhle, A. (2012). [Stress, Mental Disorders and Coronary Heart Disease]. Nervenarzt 83, 1448–1457. doi:10.1007/s00115-012-3666-7
Lee, B., Sur, B., Park, J., Kim, S. H., Kwon, S., Yeom, M., et al. (2013). Chronic Administration of Baicalein Decreases Depression-like Behavior Induced by Repeated Restraint Stress in Rats. Korean J. Physiol. Pharmacol. 17, 393–403. doi:10.4196/kjpp.2013.17.5.393
Lee, B., Yeom, M., Shim, I., Lee, H., and Hahm, D. H. (2020). Protective Effects of Quercetin on Anxiety-like Symptoms and Neuroinflammation Induced by Lipopolysaccharide in Rats. Evid. Based Complement Alternat Med. 2020, 4892415. doi:10.1155/2020/4892415
Li, D., Wang, X., Huang, Q., Li, S., Zhou, Y., and Li, Z. (2018). Cardioprotection of CAPE-oNO2 against Myocardial Ischemia/reperfusion Induced ROS Generation via Regulating the SIRT1/eNOS/NF-Κb Pathway In Vivo and In Vitro. Redox Biol. 15, 62–73. doi:10.1016/j.redox.2017.11.023
Li, F. E., Qiang, L. X., Sun, C. Y., and Wang, Q. X. (2017). Clinical Observation of 40 Cases of Coronary Heart Disease with Depression after PCI Treated by Liu Yujie with Modified Wendan Decoction. Chin. J. Integr. Med. Cardio-/Cerebrovascuiar Dis. 15, 2766–2768. doi:10.3969/j.issn.1672-1349.2017.21.033
Li, G. Y., Wu, H. Q., Zhang, Y. X., and Qian, R. (2017). Clinical Observation of Tiaogan Jianpi Tongyang Prescription in the Treatment of Anxiety State after PCI for Coronary Heart Disease. Heilongjiang Sci. Technology Inf. 23, 67–68. doi:10.3969/j.issn.1673-1328.2017.23.041
Li, S., Hao, M., Wu, T., Wang, Z., Wang, X., Zhang, J., et al. (2021). Kaempferol Alleviates Human Endothelial Cell Injury through circNOL12/miR-6873-3p/FRS2 axis. Biomed. Pharmacother. 137, 111419. doi:10.1016/j.biopha.2021.111419
Lin, C. X. (2012). Xiaoyaowan on Coronary Heart Disease with Major Depression Patients Qua Lity of Life (Gansu, China: Gansu University of Chinese Medicine). master’s thesis.
Lin, F., Xu, L., Huang, M., Deng, B., Zhang, W., Zeng, Z., et al. (2020). β-Sitosterol Protects against Myocardial Ischemia/Reperfusion Injury via Targeting PPARγ/NF-Κb Signalling. Evid. Based Complement Alternat Med. 2020, 2679409. doi:10.1155/2020/2679409
Liu, L., Liu, C., Wang, Y., Wang, P., Li, Y., and Li, B. (2015). Herbal Medicine for Anxiety, Depression and Insomnia. Curr. Neuropharmacol 13, 481–493. doi:10.2174/1570159x1304150831122734
Liu, W., and Qin, J. (2016). Clinical Efficacy and Safety of the Shugan Jieyu Capsule in Patients with Acute Myocardial Infarction and Depression. Int. J. Psychiatry Med. 51, 534–543. doi:10.1177/0091217417696740
Liu, Z., Gao, Z., Zeng, L., Liang, Z., Zheng, D., and Wu, X. (2021). Nobiletin Ameliorates Cardiac Impairment and Alleviates Cardiac Remodeling after Acute Myocardial Infarction in Rats via JNK Regulation. Pharmacol. Res. Perspect. 9, e00728. doi:10.1002/prp2.728
Lu, J., Zhou, H., Meng, D., Zhang, J., Pan, K., Wan, B., et al. (2020). Tanshinone IIA Improves Depression-like Behavior in Mice by Activating the ERK-CREB-BDNF Signaling Pathway. Neuroscience 430, 1–11. doi:10.1016/j.neuroscience.2020.01.026
Lu, X. R. (2019). Observation on Curative Effect of Jieyu Shugan Tongmai Decoction in Treating Depression after PCI (Syndrome of Liver Stagnation and Qi Stagnation) (Liaoning, China: Liaoning University of Traditional Chinese Medicine). master’s thesis.
Ma, H., Wang, Y., Xue, Y., Huang, D., Kong, Y., Zhao, X., et al. (2019). The Effect of Xinkeshu Tablets on Depression and Anxiety Symptoms in Patients with Coronary Artery Disease: Results from a Double-Blind, Randomized, Placebo-Controlled Study. Biomed. Pharmacother. 112, 108639. doi:10.1016/j.biopha.2019.108639
Ma, Z. X., Zhang, R. Y., Rui, W. J., Wang, Z. Q., and Feng, X. (2021). Quercetin Alleviates Chronic Unpredictable Mild Stress-Induced Depressive-like Behaviors by Promoting Adult Hippocampal Neurogenesis via FoxG1/CREB/BDNF Signaling Pathway. Behav. Brain Res. 406, 113245. doi:10.1016/j.bbr.2021.113245
Mao, S., Taylor, S., Chen, Q., Zhang, M., and Hinek, A. (2019). Sodium Tanshinone IIA Sulfonate Prevents the Adverse Left Ventricular Remodelling: Focus on Polymorphonuclear Neutrophil-Derived Granule Components. J. Cell Mol Med 23, 4592–4600. doi:10.1111/jcmm.14306
Mo, W. Y., Wang, J. X., and Sun, S. L. (2016). Clinical Study on Anxiety State of Patients after Percutaneous Coronary Intervention. Chin. J. Cardiovasc. Res. 14, 706–708. doi:10.3969/j.issn.1672-5301.2016.08.009
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. BMJ 339, b2535. doi:10.1371/journal.pmed.100009710.1136/bmj.b2535
Mu, L. Y. (2015). The Clinical Research of YangXinJieYu Soup to Treat Mild Depression Disorder in the Elderly after Percutaneous Coronary Intervention (Shandong, China: Shandong University of Traditional Chinese Medicine). master’s thesis.
Qi, F., and Song, B. Q. (2017). A Clinical Study on Treating Anxiety Disorder after Coronary Heart Disease Intervention with the Jieyu Tongmai Granule. Clin. J. Chin. Med. 9, 76–78. doi:10.3969/j.issn.1674-7860.2017.08.039
Qin, H. W., and Liu, P. (2013). “Observation on the Curative Effect of Invigorating Qi and Activating Blood to Relieve Stagnation in the Treatment of Depression Related to Coronary Heart Disease,” in The 3rd Cross-Strait Chinese Medicine Psychology Forum and the 2013 China Chinese Medicine Psychology Summit Forum. Editors M. Q. Wang, K. Q. Wang, and W. D. Wang (Nanjing, China, 101–107.
Qin, S. Y. (2018). The Clinical Research Based on the Principle of “ZhiQi” in the Treatment of Anxiety Disorder with Coronary Heart Disease after Percutaneous Coronary Intervention (Guangxi, China: Guangxi University of Chinese Medicine). master’s thesis.
Qiu, Z. K., Zhang, G. H., Zhong, D. S., He, J. L., Liu, X., Chen, J. S., et al. (2017). Puerarin Ameliorated the Behavioral Deficits Induced by Chronic Stress in Rats. Sci. Rep. 7, 6266. doi:10.1038/s41598-017-06552-x
Qiu, Z. K., Zhong, D. S., He, J. L., Liu, X., Chen, J. S., and Nie, H. (2018). The Anxiolytic-like Effects of Puerarin Are Associated with the Changes of Monoaminergic Neurotransmitters and Biosynthesis of Allopregnanolone in the Brain. Metab. Brain Dis. 33, 167–175. doi:10.1007/s11011-017-0127-9
Rivera, D., Allkin, R., Obón, C., Alcaraz, F., Verpoorte, R., and Heinrich, M. (2014). What Is in a Name? the Need for Accurate Scientific Nomenclature for Plants. J. Ethnopharmacol 152, 393–402. doi:10.1016/j.jep.2013.12.022
Roest, A. M., Martens, E. J., de Jonge, P., and Denollet, J. (2010). Anxiety and Risk of Incident Coronary Heart Disease: a Meta-Analysis. J. Am. Coll. Cardiol. 56, 38–46. doi:10.1016/j.jacc.2010.03.034
Salim, S. (2017). Oxidative Stress and the Central Nervous System. J. Pharmacol. Exp. Ther. 360, 201–205. doi:10.1124/jpet.116.237503
Samad, N., Saleem, A., Yasmin, F., and Shehzad, M. A. (2018). Quercetin Protects against Stress-Induced Anxiety- and Depression-like Behavior and Improves Memory in Male Mice. Physiol. Res. 67, 795–808. doi:10.33549/physiolres.933776
Shang, X. P., Zeng, Q. M., Jing, G. G., Jiang, L. F., and Wang, H. (2014). Clinical Observation on 30 Cases of Depression after PCI Treated with Bupleurum Plus Longgu Oyster Decoction. Guid J. Tradit Chin Med. Pharm. 20, 43–44. doi:10.13862/j.cnki.cn43-1446/r.2014.01.035
Shi, J. B. (2018). Clinical Study of Tongmai Sanyu Decoction on Unstable Angina Pectoris (Blood Stasis Type) with Depression (Liaoning, China: Liaoning University of Traditional Chinese Medicine). master’s thesis.
Shi, J. J., Shen, L., Li, H. N., Gao, Y., and Yan, H. (2016). Clinical Observation of Jieyu Tongmai Decoction on 68 Cases of Depression after Coronary Stenting. Tianjin J. Traditional Chin. Med. 33, 139–143. doi:10.11656/j.issn.1672-1519.2016.03.04
Song, L., Yang, H., Wang, H. X., Tian, C., Liu, Y., Zeng, X. J., et al. (2014). Inhibition of 12/15 Lipoxygenase by Baicalein Reduces Myocardial Ischemia/reperfusion Injury via Modulation of Multiple Signaling Pathways. Apoptosis 19, 567–580. doi:10.1007/s10495-013-0946-z
Su, X. P. (2017). Clinical Observation of Jiaweisuanzaoren Decoction in the Treatment of Revascularization in Senile Patients with CHD Coexisting Depressive Symptoms (Shandong, China: Shandong University of Traditional Chinese Medicine). master’s thesis.
Suchal, K., Malik, S., Khan, S. I., Malhotra, R. K., Goyal, S. N., Bhatia, J., et al. (2017). Molecular Pathways Involved in the Amelioration of Myocardial Injury in Diabetic Rats by Kaempferol. Int. J. Mol. Sci. 18, 1001. doi:10.3390/ijms18051001
Sun, Y. Y. (2011). Clinical Study of Jieyuhuoxue Anshen Method in Treatment of CHD with Depression (Shandong, China: Shandong University Of Traditional Chinese Medicine). master’s thesis.
Tao, J., Cui, Y., Duan, Y., Zhang, N., Wang, C., and Zhang, F. (2017). Puerarin Attenuates Locomotor and Cognitive Deficits as Well as Hippocampal Neuronal Injury through the PI3K/Akt1/GSK-3β Signaling Pathway in an In Vivo Model of Cerebral Ischemia. Oncotarget 8, 106283–106295. doi:10.18632/oncotarget.22290
van Dooren, F. E., Schram, M. T., Schalkwijk, C. G., Stehouwer, C. D., Henry, R. M., Dagnelie, P. C., et al. (2016). Associations of Low Grade Inflammation and Endothelial Dysfunction with Depression - the Maastricht Study. Brain Behav. Immun. 56, 390–396. doi:10.1016/j.bbi.2016.03.004
Wang, C. (2018). Double Heart Effect and Partial Mechanism of Bupleurum Plus Longguoyasu Decoction in Treating Coronary Heart Disease Complicated with Anxiety ([Beijing, China]: Beijing University of Chinese Medicine). dissertation.
Wang, D. D. (2018). Clinical Study of Jiawei Dachaihu Decoction on Stable Angina Pectoris of Coronary Heart Disease with Depression (Henan, China: Henan University of Chinese Medicine). master’s thesis.
Wang, H., Guo, Y., Qiao, Y., Zhang, J., and Jiang, P. (2020). Nobiletin Ameliorates NLRP3 Inflammasome-Mediated Inflammation through Promoting Autophagy via the AMPK Pathway. Mol. Neurobiol. 57, 5056–5068. doi:10.1007/s12035-020-02071-5
Wang, J. L., Li, L. W., Tian, Q. Q., Zhang, B. B., Gong, X., Xu, J. M., et al. (2021). Clinical Efficacy of Shuxin Oral Liquid Combined with Conventional Western Medicine in the Treatment of Stable Coronary Heart Disease with Anxiety Based on “Psycho-cardiology Disease” Theory. J. Shanghai Univ. Traditional Chin. Med. 35, 14–19. doi:10.16306/j.1008-861x.2021.05.003
Wang, Y. L., Han, Q. Q., Gong, W. Q., Pan, D. H., Wang, L. Z., Hu, W., et al. (2018). Microglial Activation Mediates Chronic Mild Stress-Induced Depressive- and Anxiety-like Behavior in Adult Rats. J. Neuroinflammation 15, 21. doi:10.1186/s12974-018-1054-3
Wang, Y., Liu, Y.-J., Li, F.-E., Guo, Z., and Wang, J. (2018). A Chinese Herbal Formula Shows Beneficial Effects on Comorbid Depression and Coronary Heart Disease Based on the Philosophy of Psycho-Cardiology. J. Herbal Med. 19, 100303. doi:10.1016/j.hermed.2019.100303
Wang, Z. K., Chen, R. R., Li, J. H., Chen, J. Y., Li, W., Niu, X. L., et al. (2020). Puerarin Protects against Myocardial Ischemia/reperfusion Injury by Inhibiting Inflammation and the NLRP3 Inflammasome: The Role of the SIRT1/NF-Κb Pathway. Int. Immunopharmacol. 89, 107086. doi:10.1016/j.intimp.2020.107086
Wei, B., Lin, Q., Ji, Y. G., Zhao, Y. C., Ding, L. N., Zhou, W. J., et al. (2018). Luteolin Ameliorates Rat Myocardial Ischaemia-Reperfusion Injury through Activation of Peroxiredoxin II. Br. J. Pharmacol. 175, 3315–3332. doi:10.1111/bph.14367
Wu, X., Zheng, D., Qin, Y., Liu, Z., Zhang, G., Zhu, X., et al. (2017). Nobiletin Attenuates Adverse Cardiac Remodeling after Acute Myocardial Infarction in Rats via Restoring Autophagy Flux. Biochem. Biophys. Res. Commun. 492, 262–268. doi:10.1016/j.bbrc.2017.08.064
Xu, S. L., Choi, R. C., Zhu, K. Y., Leung, K. W., Guo, A. J., Bi, D., et al. (2012). Isorhamnetin, A Flavonol Aglycone from Ginkgo Biloba L., Induces Neuronal Differentiation of Cultured PC12 Cells: Potentiating the Effect of Nerve Growth Factor. Evid. Based Complement Alternat Med. 2012, 278273. doi:10.1155/2012/278273
Xu, Y., Tang, C., Tan, S., Duan, J., Tian, H., and Yang, Y. (2020). Cardioprotective Effect of Isorhamnetin against Myocardial Ischemia Reperfusion (I/R) Injury in Isolated Rat Heart through Attenuation of Apoptosis. J. Cell. Mol. Med. 24, 6253–6262. doi:10.1111/jcmm.15267
Yang, J. J. (2019). Clinical Intervention Effect of Chaihu Plus Longgu Oyster Decoction on Coronary Heart Disease Complicated with Anxiety (Beijing, China: Beijing University of Chinese Medicine). master’s thesis.
Yang, X., He, T., Han, S., Zhang, X., Sun, Y., Xing, Y., et al. (2019). The Role of Traditional Chinese Medicine in the Regulation of Oxidative Stress in Treating Coronary Heart Disease. Oxid Med. Cell Longev 2019, 3231424. doi:10.1155/2019/3231424
Yi, L. T., Xu, H. L., Feng, J., Zhan, X., Zhou, L. P., and Cui, C. C. (2011). Involvement of Monoaminergic Systems in the Antidepressant-like Effect of Nobiletin. Physiol. Behav. 102, 1–6. doi:10.1016/j.physbeh.2010.10.008
Yin, Y., Liu, X., Liu, J., Cai, E., Zhao, Y., Li, H., et al. (2018). The Effect of Beta-Sitosterol and its Derivatives on Depression by the Modification of 5-HT, DA and GABA-Ergic Systems in Mice. RSC Adv. 8, 671–680. doi:10.1039/c7ra11364a
Yu, D., Li, M., Tian, Y., Liu, J., and Shang, J. (2015). Luteolin Inhibits ROS-Activated MAPK Pathway in Myocardial Ischemia/reperfusion Injury. Life Sci. 122, 15–25. doi:10.1016/j.lfs.2014.11.014
Zhang, B. F., Jiang, H., Chen, J., Guo, X., Li, Y., Hu, Q., et al. (2019). Nobiletin Ameliorates Myocardial Ischemia and Reperfusion Injury by Attenuating Endoplasmic Reticulum Stress-Associated Apoptosis through Regulation of the PI3K/AKT Signal Pathway. Int. Immunopharmacol. 73, 98–107. doi:10.1016/j.intimp.2019.04.060
Zhang, J. (2019). Effect of Jiangqi Dayu Decoction on Unstable Angina Pectoris Complicated with Anxiety (Liaoning, China: Liaoning University Of Traditional Chinese Medicine). master’s thesis.
Zhang, J., and Jin, M. (2021). Clinical Effect of Xuefu Zhuyu Decoction Combined with Yueju Pill on Coronary Heart Disease with Stable Angina Pectoris Due to Qi Stagnation and Blood Stasis Type, Accompanied with Anxiety. Beijing J. Traditional Chin. Med. 40, 765–769. doi:10.16025/j.1674-1307.2021.07.022
Zhang, J. S., Chen, Q., Cai, Z. B., Zhang, W. J., Zhang, N., Gu, N. F., et al. (2020). Clinical Observation on the Treatment of Coronary Heart Disease Complicated with Depression by Removing Phlegm and Stasis. YI YAO QIAN YAN 10, 215–216.
Zhang, K. J., Zheng, Q., Zhu, P. C., Tong, Q., Zhuang, Z., Zhu, J. Z., et al. (2019). Traditional Chinese Medicine for Coronary Heart Disease: Clinical Evidence and Possible Mechanisms. Front Pharmacol. 10, 844. doi:10.3389/fphar.2019.00844
Zhang, L. F., Wang, J., and Wang, Z. J. (2012). [Study on Clinical Intervention of Jiawei Shengdan Louxie Sini Fang on Coronary Heart Disease with Depression]. Zhongguo Zhong Yao Za Zhi 37, 3150–3154. doi:10.4268/cjcmm20122030
Zhang, Q. J., Wang, W. H., Xu, Y., Zhao, Y., and Jiao, M. X. (2017). Clinical Effect of Dual Heart Mode on Angina Pectoris with Anxiety of Coronary Heart Disease. Acta Chin. Med. Pharmacol. 45, 129–130. doi:10.3969/j.issn.1002-2392.2017.03.040
Zhang, S., Chen, L., Zhou, Z., Fan, W., and Liu, S. (2019). Effects of Puerarin on Clinical Parameters, Vascular Endothelial Function, and Inflammatory Factors in Patients with Coronary Artery Disease. Med. Sci. Monit. 25, 402–408. doi:10.12659/MSM.911108
Zhao, D., Zheng, L., Qi, L., Wang, S., Guan, L., Xia, Y., et al. (2016). Structural Features and Potent Antidepressant Effects of Total Sterols and β-sitosterol Extracted from Sargassum Horneri. Mar. Drugs 14. doi:10.3390/md14070123
Zhao, L., Wang, L., Zhang, D., Chen, Y., and Jin, F. (2021). Puerarin Alleviates Coronary Heart Disease via Suppressing Inflammation in a Rat Model. Gene 771, 145354. doi:10.1016/j.gene.2020.145354
Zhao, L., Zhou, Z., Zhu, C., Fu, Z., and Yu, D. (2020). Luteolin Alleviates Myocardial Ischemia Reperfusion Injury in Rats via Siti1/NLRP3/NF-Κb Pathway. Int. Immunopharmacol. 85, 106680. doi:10.1016/j.intimp.2020.106680
Zhao, T. T., Yang, T. L., Gong, L., and Wu, P. (2018). Isorhamnetin Protects against Hypoxia/reoxygenation-Induced Injure by Attenuating Apoptosis and Oxidative Stress in H9c2 Cardiomyocytes. Gene 666, 92–99. doi:10.1016/j.gene.2018.05.009
Zhao, X., Kong, D., Zhou, Q., Wei, G., Song, J., Liang, Y., et al. (2021). Baicalein Alleviates Depression-like Behavior in Rotenone- Induced Parkinson's Disease Model in Mice through Activating the BDNF/TrkB/CREB Pathway. Biomed. Pharmacother. 140, 111556. doi:10.1016/j.biopha.2021.111556
Zhao, X. J., Li, R., and Wan, Y. (2019). Clinical Observation of Xinling Pills in the Teatment of Coronary Heart Disease after PCI Complicated with Anxiety Based on Dual Heart Therapy. Chin. J. Integr. Med. Cardio-/Cerebrovascuiar Dis. 17, 432–435. doi:10.12102/j.issn.1672-1349.2019.03.032
Zhou, Y., Yin, T., Shi, M., Chen, M., Wu, X., Wang, K., et al. (2021). Nobiletin Attenuates Pathological Cardiac Remodeling after Myocardial Infarction via Activating PPARγ and PGC1α. PPAR Res. 2021, 9947656. doi:10.1155/2021/9947656
Zhu, F. (2013). The Clinical Research of Jieyu Particle in Treatment of Unstable Angina Patients with Depression Status (Shandong, China: Shandong University Of Traditional Chinese Medicine). master’s thesis.
Keywords: coronary heart disease, anxiety, depression, Chinese herbal medicine, efficacy
Citation: Wang B, Teng Y, Li Y, Lai S, Wu Y, Chen S, Li T, Han X, Zhou H, Wang Y, Lu Z, Li H, Ding Y, Ma L, Zhao M and Wang X (2022) Evidence and Characteristics of Traditional Chinese Medicine for Coronary Heart Disease Patients With Anxiety or Depression: A Meta-Analysis and Systematic Review. Front. Pharmacol. 13:854292. doi: 10.3389/fphar.2022.854292
Received: 13 January 2022; Accepted: 29 March 2022;
Published: 05 May 2022.
Edited by:
Yusof Kamisah, Universiti Kebangaan Malaysia, MalaysiaCopyright © 2022 Wang, Teng, Li, Lai, Wu, Chen, Li, Han, Zhou, Wang, Lu, Li, Ding, Ma, Zhao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingjing Zhao, bWpneDIwMDRAMTYzLmNvbQ==; Xian Wang, d3g2NTA1MTVAMTYzLmNvbQ==
†These authors shares co-first authorship
 Baofu Wang
Baofu Wang Yu Teng
Yu Teng Yang Li1†
Yang Li1† Shiqi Chen
Shiqi Chen Tong Li
Tong Li Hufang Zhou
Hufang Zhou Haiyan Li
Haiyan Li Mingjing Zhao
Mingjing Zhao