- 1Jilin Provincial Key Laboratory on Molecular and Chemical Genetic, Second Hospital of Jilin University, Changchun, China
- 2Department of Pharmacy, The Eastern Division of First Hospital of Jilin University, Changchun, China
- 3Department of Breast Surgery, The Affiliated Hospital Changchun University of Chinese Medicine, Changchun, China
A major type of serious mood disorder, depression is currently a widespread and easily overlooked psychological illness. With the low side effects of natural products in the treatment of diseases becoming the pursuit of new antidepressants, natural Chinese medicine products have been paid more and more attention for their unique efficacy in improving depression. In a view from the current study, the positive antidepressant effects of berberine are encouraging. There is a lot of work that needs to be done to accurately elucidate the efficacy and mechanism of berberine in depression. In this review, the relevant literature reports on the treatment of depression and anxiety by berberine are updated, and the potential pharmacological mechanism of berberine in relieving depression has also been discussed.
Introduction
Depressive disorder is a heterogeneous disease based on symptoms forming a syndrome and causing bodily dysfunction, which has the characteristics of multiple phenotypes, biological and psychological susceptibilities, and indirect incidence (Kim 2021). The cardinal symptoms of patient include emotional instability, anhedonia, poor concentration, and tendency to commit suicide (Yang et al., 2015). With the increasing number of patients, depression has become a serious illness that threatens human health, and increases burden on families and society. A lot of research reports have made some breakthroughs in elucidating the underlying pathogenesis of depression, mainly including the widely accepted monoamine hypothesis, hypothalamic–pituitary–adrenal axis disorder hypothesis, neuroinflammation hypothesis, and neuroplasticity and neurogenesis hypothesis (Malhi and Mann 2018). These hypotheses show that depression is a rather complex medical disease caused by a combination of genetic and environmental factors, involving a variety of neurobiological substrates, brain regions, and circuits (Wang et al., 2019). Although multiple antidepressants are available, most patients do not respond with the desired effect to these treatments and even induced paradoxical effects, such as deterioration of symptoms and withdrawal symptoms (Chouinard and Chouinard 2015). In the search for better antidepressants, the lower side effects of drugs have become a pursuit of new antidepressants. Therefore, natural Chinese medicine products have been widely a concern by medical workers for their unique efficacy in improving depression. In particular, the research of safe and effective antidepressants in traditional herbal medicine has become a hot spot in the current medical field.
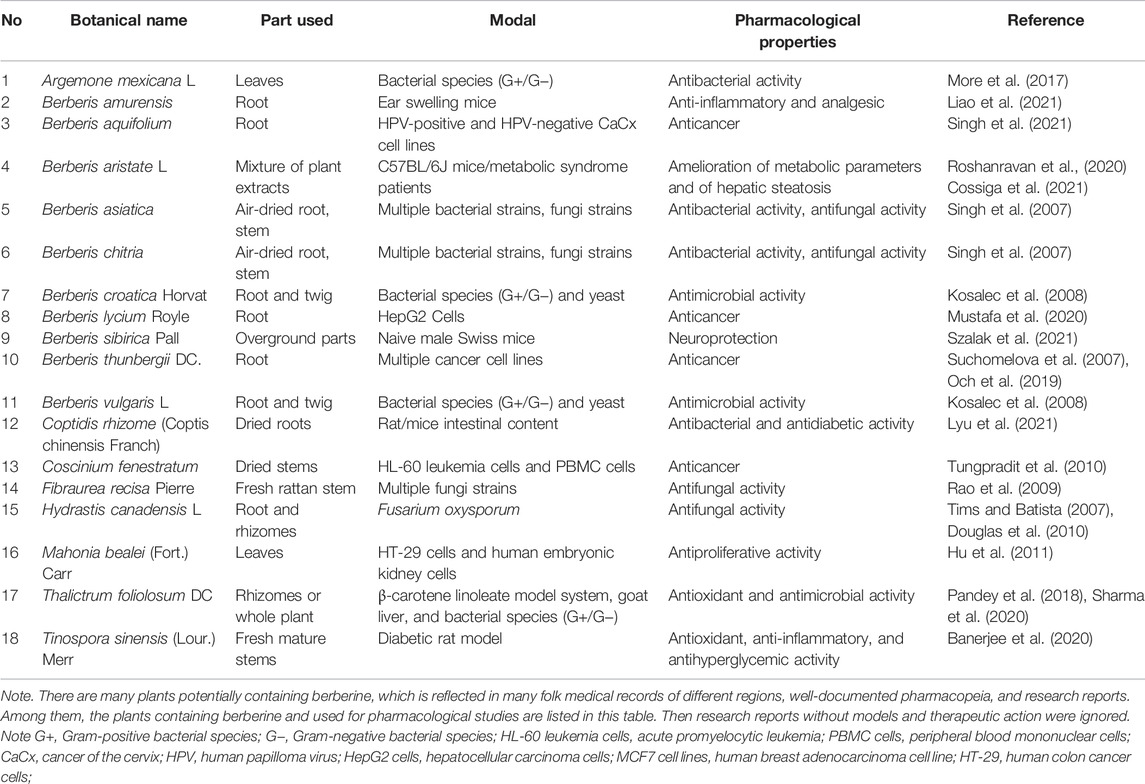
The naturally effective ingredients tested in most studies were selected based on their multiple pharmacological actions, medicinal value, or as antidepressants. Berberine, an isoquinoline alkaloid, was extracted from the roots and aboveground parts of plants (Table 1), which are readily available from Berberidaceae, Papaveraceae, Menispermaceae, Ranunculaceae, and other botanical families (Kulkarni and Dhir 2010; Liu et al., 2016). Clinical studies of berberine have revealed multiple therapeutic actions, including anti-inflammatory, anticancer, relieving depression, hypolipidemic, and hypoglycemic actions, which indicate that berberine is a drug with multispectral activities (Mujtaba et al., 2021). Therefore, it is also a noteworthy candidate drug for the treatment of depression, which has been studied in several animal models of depression (Figure 1). The purpose of this review was to investigate the mechanism of berberine and its traditional Chinese medicine prescription in the treatment of depression in recent literature reports, combined with the pathogenesis of depression. Meanwhile, we sought to present a summary of the current problems and feasible solutions of berberine in the clinical treatment of depression.
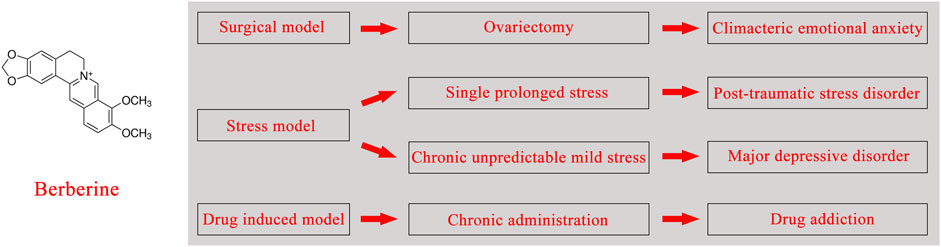
FIGURE 1. Chemical structural formula of berberine, associated depression models, and clinical diseases.
The effect of berberine on symptom clusters of depression
The multi-angle regulatory mechanism of berberine may confer positive therapeutic effects against depression, due to its extensive range of biological effects. Many potential factors that are well known to increase the risk of depression, including the influence of sex hormones, a dulled response to stress in the hypothalamic–pituitary–adrenal axis, and a higher tendency to introspection, might boost the chances of women suffering from depression (Riecher-Rossler 2017). Moreover, findings from a Chinese woman-based cohort study showed that symptoms of anxiety and depression are more common during and after menopause than in premenopausal women (Tang et al., 2019). Therefore, the ovariectomized (OVX) mice model was used to mimic clinical postmenopausal condition (Rana et al., 2022). Researchers have found that after gavage administration of berberine (100 mg/kg), the increased content of equol (a chemical structure similar to the hormone estrogen that binds to estrogen receptors) in the OVX rat model transplanted with fecal microbiota, enriched the taxa involved in isoflavone biotransformation and significantly reduced anxiety-like behavior. The results suggest that berberine may alleviate anxiety-like behavior in perimenopausal rat partly through the microbiota–gut–brain axis system (Fang et al., 2021). In addition, our previous study showed that ovariectomy reduced the brain-derived neurotrophic factor (BDNF) protein expression levels in the hippocampus and phosphorylated cyclase adenosine monophosphate response element-binding protein (pCREB)/CREB ratio in the frontal cortex, but this change was reversed in the short term by berberine, considering that the rapid-onset antidepressant-like behavior is mediated by the decreased phosphorylation of eukaryotic elongation factor 2 (eEF2) and the increased translation of BDNF. In this case, we suggest that berberine may produce antidepressant-like effects in OVX mice via the BDNF-CREB and eEF2 pathways (Fan et al., 2017).
Depression is closely related to a decrease in neuronal plasticity. BDNF is associated with changes in neuroplasticity in certain areas, such as the amygdala and hippocampus (Camuso et al., 2021), and is deemed to be beneficial in neurogenesis, neural survival, and growth (Shen et al., 2020). A recent study showed that berberine was involved in the regulation of depression progression through miRNA and BDNF. Berberine treatment could effectively reverse the promotion effect of overexpression of miR-34b-5p/miR-470-5p on the depressive-like behavior of chronic unpredicted mild stress (CUMS) mice and regulate the growth of hippocampal neurons by mediating the expression of BDNF(Zhan et al., 2021). Clinical studies on major depression patients showed that their hippocampus was seriously damaged, and their neurogenesis function was impaired (Park 2019; Huang et al., 2020). The above pathologic phenomenon was reversed by antidepressant treatment, suggesting that neurogenesis is associated with the altered course of depression (Zeng et al., 2022). Neurogenesis, an important focus of hippocampal structural plasticity, produces full neural function that involves the proliferation and differentiation of neural stem cells (Li et al., 2020). Berberine was able to protect C17.2 neural stem cells from the 2,2′-azobis(2-amidinopropane)dihydrochloride-induced oxidative damage; to be more specific, it lowered the cellular reactive oxygen species level in C17.2 cells via the nuclear factor erythroid 2-related factor 1/2 (NRF1/2)-NAD(P)H quinone dehydrogenase 1–heme oxygenase 1 pathway. Besides, berberine enhanced the viability of C17.2 cells by upregulating the expression of extracellular signal-related kinase (ERK) and phosphor-ERK, which contributed to the activation of the WNT/β catenin pathway in C17.2 cells to promote neuronal differentiation (Shou et al., 2019).
In addition, berberine plays an antidepressant role by regulating brain neurotransmitters, especially biogenic amines. It has high affinity for dopamine receptors (Lee et al., 2018), and regulates hypothalamic corticotrophin-releasing factor and central norepinephrine systems (Lee et al., 2012). There is evidence that berberine increases the level of dopa/dopamine in blood, in which dopa enters the brain through the circulation and is converted into dopamine, so as to improve brain function. Generally, the increase in dopamine is closely related to positive emotions (Hamon and Blier 2013). Lee et al. found that single prolonged stress induced DAergic dysfunction in rats, leading to depression-like behavior. The concentration of dopamine in the hippocampus and striatum were significantly increased after intraperitoneal injection of berberine, which may alleviate anxiety to some extent (Lee et al., 2018). A recent study showed that oral berberine could promote the production of dopa/dopamine by improving the synthetic pathway of Phe–Tyr–dopa–dopamine in the gut flora, and the active compound produced by dopa/dopamine is dihydroberberine (an intestinal metabolite). In other words, dopa/dopamine in brain tissue was increased by dihydroberberine, but not berberine (Wang et al., 2021). These advances may lead to a deeper understanding of the role of berberine in regulating biogenic amines, gut–brain dialogue, and curing depression.
It is also well recognized that inflammation and weakened immunity are also key factors in the pathogenesis of depression (Chen et al., 2022). A line of evidence demonstrated that a significant proportion of patients with emotional-related diseases exhibit characteristics of chronic low-grade inflammation involving increased concentrations of peripheral and central inflammatory cytokines, inflammatory mediators, and acute-phase reactants (Felger 2018). For example, the levels of TNF-α, IL-1β, IL-6, IL-8 and other inflammatory cytokines in the serum of patients with depression is upregulated (Fan et al., 2017). Moreover, the study indicated that chronic methamphetamines (METH) induced anxiety-like behavior in rats, at least in part, by activating the immune Toll-like receptor 4 (TLR4) signaling pathway, which leads to the upregulation of the expression of several inflammatory agents, such as NF-κB and α-actin in the hippocampus (Wang et al., 2019; Rezaeian et al., 2020). Coincidentally, activation of NF-κB by proinflammatory mediators creates a positive feedback loop that amplifies inflammatory signals (Azam et al., 2019). Based on the above research results, Rezaeian et al. suggested that oral berberine (100 mg/kg) modulated neuroinflammation and reduced anxiety behavior via suppressing the activation of TLR4 and NF-κB in METH-addicted rats (Rezaeian et al., 2020).
The effect of Chinese medicine prescription of berberine on depression
The diversity of bioactive compounds contributes to prescriptions of traditional herbal medicines to perform multiple pharmacological effects. From this perspective, a simple theoretical conjecture is that herbal formula with several phytochemical components have more action targets than a single-compound Chinese medicine preparation. Although the action pathway or mechanism of Chinese medicine prescriptions with an antidepressant effect is relatively obscure owing to their multi-active ingredients or complexes and non-additivity, we cannot ignore the potential of prescriptions in antidepressants. Huang-Lian Jie-Du Decoction (HLJDD) is an ancient Chinese medicine prescription composed of Coptis chinensis Franch, Scutellaria baicalensis Georgi, Phellodendron chinense Schneid, and Gardenia fructus Ellis, which can ameliorate multiple central nervous system diseases, such as cerebral ischemia (Wang et al., 2013), Alzheimer’s disease (Liu et al., 2019), and mental disorders (Qu et al., 2021). A study reported that the protective mechanism of HLJDD against neurotoxicity may be due to the protective effect of berberine, an important component of the formula, in alleviating the decrease in paraquat-induced mitochondrial membrane potential in human SH-SY5Y cells (Lee et al., 2021). In addition, previous studies on pharmacological properties of berberine have shown that it could reduce NADPH oxidase activity, attenuate mitochondrial defects and redox imbalance, and induce mitochondrial biogenesis, which may partially support the viewpoints mentioned above. The network pharmacology and metabolomics study showed that the main target of HLJDD-ameliorated depressive-like behaviors in CUMS mice was tryptophan metabolism, in which sodium-dependent serotonin transporter (SLC6A4) and monoamine oxidase A (MAOA) were regulated by active ingredients such as berberine (Qu et al., 2021).
Challenges and possible solutions
In normal conditions, oral delivery and parenteral administration are relatively ideal routes of administration in treating chronic diseases. Although berberine has been researched for many years and received positive therapeutic feedback in an animal model of depression, there is poor bioavailability of oral or parenteral administration due to low absorption and intestinal first-pass effect, restricting its utilization in the treatment of depression (Fan et al., 2019). Therefore, it is necessary to overcome the problem of bioavailability and improve its therapeutic effects before it can be applied to clinical treatment. Nanotechnology-based drug delivery strategies constitute a potential approach to enhance the poor bioavailability of berberine. Many studies have demonstrated that topical delivery has the characteristics of targeting and performance release controllability, which plays an important role in medical treatment (Dare et al., 2020). Among them, intranasal delivery, as a form of topical delivery, bypasses the blood–brain barrier through the olfactory pathway and trigeminal nerve pathway, directly transporting drugs to the brain (Dhuria et al., 2010). Recent studies have shown that intranasal delivery of berberine was effective in the treatment of depression through a pre-prepared self-assembled thermosensitive in situ hydrogel (Wang et al., 2020; Xu et al., 2021). It is noteworthy that intranasal administration of hydrogel increased the bioavailability of berberine by approximately 135-fold, compared with intragastric administration of drug solution, which is probably the positive result of the synergistic effect of hydrogels in drug delivery.
Discussion
Depression is essentially a disease of the brain. Once its mechanisms of action with antidepressants are fully known, this disorder is likely to be effectively prevented and treated through some targets. In actual clinical treatment, antidepressants, such as selective serotonin reuptake inhibitor (SSRIs) or serotonin–noradrenaline reuptake inhibitors (SNRIs), are often applied to relieve symptoms. Actually, studies demonstrated that up to more than half of depression patients treated with SSRIs or SNRIs showed multiple common and well-documented adverse effects, such as some degree of emotional blunting (Christensen et al., 2021). For these reasons, while developing multitarget chemicals to reduce adverse reactions and long-term intolerance and improve the efficacy of depression drugs, a whole lot of attention is paid to the positive effects of active ingredients in natural products on depression. As a promising medicine ingredient candidate for the treatment of emotional disorders, berberine needs to be studied in substantive and long-term clinical practice with the help of neuroscience, genomics, and technologies. It exerts antidepressant effects through regulating monoamines, alleviating the dysfunction of nerve injury, ameliorating the dysregulation of immune and inflammation, and other regulatory mechanisms. Besides, it can also relieve depression-related complications, such as insomnia and cognitive impairment. Therefore, programs are necessary to increase knowledge on the use of natural antidepressants, formulate a treatment strategy for individual needs to reduce the adverse reactions of patients, as well as enhance the public’s confidence in traditional Chinese medicine to cure emotional diseases, so as to improve the public’s lack of trust in the health care system.
Conclusion
We have reviewed the latest research progress of berberine in the treatment of depression, which may provide a reference for the search of natural antidepressants. Although berberine has been revealed with multiple therapeutic actions, and it may be a potential drug for mood disorders, transformation research is needed to further address its safety concerns, poor bioavailability, and solubility.
Author Contributions
W-QZ wrote the manuscript. T-TG provided the critical revisions. H-Y W, Z-H S, Y G, B-J L, X L and R-J C provided supervision of entire manuscript. All authors approved the final version of the manuscript for submission.
Funding
This project was funded by the National Key R&D Program of China, China (#2018YFC1311600), the National Natural Science Foundation of China, China (81871070), the National Natural Science Foundation of China, China (31971078), the National Natural Science Foundation of China, China (81971276), the Jilin Science and Technology Agency funds in China, China (20200301005RQ), The Jilin Science and Technology Agency funds in China, China (20190701078GH, 20210402003GH), and the Scientific Research Foundation of the Education Department of Jilin Province (JJKH20201032KJ). Jilin Provincial Finance Department, China(2020SCZT091, JLSCZ b2019051).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Azam, S., Jakaria, M., Kim, I. S., Kim, J., Haque, M. E., and Choi, D. K. (2019). Regulation of Toll-like Receptor (TLR) Signaling Pathway by Polyphenols in the Treatment of Age-Linked Neurodegenerative Diseases: Focus on TLR4 Signaling. Front. Immunol. 10, 1000. doi:10.3389/fimmu.2019.01000
Banerjee, A., Singh, S., Prasad, S. K., Kumar, S., Banerjee, O., Seal, T., et al. (2020). Protective Efficacy of Tinospora Sinensis against Streptozotocin Induced Pancreatic Islet Cell Injuries of Diabetic Rats and its Correlation to its Phytochemical Profiles. J. Ethnopharmacol. 248, 112356. doi:10.1016/j.jep.2019.112356
Camuso, S., La Rosa, P., Fiorenza, M. T., and Canterini, S. (2021). Pleiotropic Effects of BDNF on the Cerebellum and hippocampus: Implications for Neurodevelopmental Disorders. Neurobiol. Dis. 163, 105606. doi:10.1016/j.nbd.2021.105606
Chen, X., Chen, Y., Qi, D., and Cui, D. (2022). Multifaceted Interconnections between Macrophage Migration Inhibitory Factor and Psychiatric Disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 112, 110422. doi:10.1016/j.pnpbp.2021.110422
Chouinard, G., and Chouinard, V. A. (2015). New Classification of Selective Serotonin Reuptake Inhibitor Withdrawal. Psychother. Psychosom. 84, 63–71. doi:10.1159/000371865
Christensen, M. C., Fagiolini, A., Florea, I., Loft, H., Cuomo, A., and Goodwin, G. M. (2021). Validation of the Oxford Depression Questionnaire: Sensitivity to Change, Minimal Clinically Important Difference, and Response Threshold for the Assessment of Emotional Blunting. J. Affect Disord. 294, 924–931. doi:10.1016/j.jad.2021.07.099
Cossiga, V., Lembo, V., Nigro, C., Mirra, P., Miele, C., D'Argenio, V., et al. (2021). The Combination of Berberine, Tocotrienols and Coffee Extracts Improves Metabolic Profile and Liver Steatosis by the Modulation of Gut Microbiota and Hepatic miR-122 and miR-34a Expression in Mice. Nutrients 13, 1281. doi:10.3390/nu13041281
Daré, R. G., Costa, A., Nakamura, C. V., Truiti, M. C. T., Ximenes, V. F., Lautenschlager, S. O. S., et al. (2020). Evaluation of Lipid Nanoparticles for Topical Delivery of Protocatechuic Acid and Ethyl Protocatechuate as a New Photoprotection Strategy. Int. J. Pharm. 582, 119336. doi:10.1016/j.ijpharm.2020.119336
Dhuria, S. V., Hanson, L. R., and Frey, W. H. (2010). Intranasal Delivery to the central Nervous System: Mechanisms and Experimental Considerations. J. Pharm. Sci. 99, 1654–1673. doi:10.1002/jps.21924
Douglas, J. A., Follett, J. M., Parmenter, G. A., Sansom, C. E., Perry, N. B., and Littler, R. A. (2010). Seasonal Variation of Biomass and Bioactive Alkaloid Content of Goldenseal, Hydrastis canadensis. Fitoterapia 81, 925–928. doi:10.1016/j.fitote.2010.06.006
Fan, J., Li, B., Ge, T., Zhang, Z., Lv, J., Zhao, J., et al. (2017). Berberine Produces Antidepressant-like Effects in Ovariectomized Mice. Sci. Rep. 7, 1310. doi:10.1038/s41598-017-01035-5
Fan, J., Zhang, K., Jin, Y., Li, B., Gao, S., Zhu, J., et al. (2019). Pharmacological Effects of Berberine on Mood Disorders. J. Cel. Mol. Med. 23, 21–28. doi:10.1111/jcmm.13930
Fan, Ni, N., Luo, Y., Ou, Y., and He, H. (2017). Altered Serum Levels of TNF-α, IL-6, and IL-18 in Depressive Disorder Patients. Hum. Psychopharmacol. 32. doi:10.1002/hup.2588
Fang, Y., Zhang, J., Zhu, S., He, M., Ma, S., Jia, Q., et al. (2021). Berberine Ameliorates Ovariectomy-Induced Anxiety-like Behaviors by Enrichment in Equol Generating Gut Microbiota. Pharmacol. Res. 165, 105439. doi:10.1016/j.phrs.2021.105439
Felger, J. C. (2018). Imaging the Role of Inflammation in Mood and Anxiety-Related Disorders. Curr. Neuropharmacol. 16, 533–558. doi:10.2174/1570159X15666171123201142
Hamon, M., and Blier, P. (2013). Monoamine Neurocircuitry in Depression and Strategies for New Treatments. Prog. Neuropsychopharmacol. Biol. Psychiatry 45, 54–63. doi:10.1016/j.pnpbp.2013.04.009
Hu, W., Yu, L., and Wang, M. H. (2011). Antioxidant and Antiproliferative Properties of Water Extract from Mahonia Bealei (Fort.) Carr. Leaves. Food Chem. Toxicol. 49, 799–806. doi:10.1016/j.fct.2010.12.001
Huang, Y. L., Zeng, N. X., Chen, J., Niu, J., Luo, W. L., Liu, P., et al. (2020). Dynamic Changes of Behaviors, Dentate Gyrus Neurogenesis and Hippocampal miR-124 Expression in Rats with Depression Induced by Chronic Unpredictable Mild Stress. Neural Regen. Res. 15, 1150–1159. doi:10.4103/1673-5374.270414
Kim, Y. K. (2021). Recent Advances and Challenges in Major Depressive Disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 111, 110403. doi:10.1016/j.pnpbp.2021.110403
Kosalec, I., Gregurek, B., Kremer, D., Zovko, M., Sanković, K., and Karlović, K. (2008). Croatian Barberry (Berberis Croatica Horvat): a New Source of Berberine-Analysis and Antimicrobial Activity. World J. Microbiol. Biotechnol. 25, 145–150. doi:10.1007/s11274-008-9860-x
Kulkarni, S. K., and Dhir, A. (2010). Berberine: a Plant Alkaloid with Therapeutic Potential for central Nervous System Disorders. Phytother Res. 24, 317–324. doi:10.1002/ptr.2968
Lee, B., Shim, I., Lee, H., and Hahm, D. H. (2018). Berberine Alleviates Symptoms of Anxiety by Enhancing Dopamine Expression in Rats with post-traumatic Stress Disorder. Korean J. Physiol. Pharmacol. 22, 183–192. doi:10.4196/kjpp.2018.22.2.183
Lee, B., Sur, B., Yeom, M., Shim, I., Lee, H., and Hahm, D. H. (2012). Effect of Berberine on Depression- and Anxiety-like Behaviors and Activation of the Noradrenergic System Induced by Development of Morphine Dependence in Rats. Korean J. Physiol. Pharmacol. 16, 379–386. doi:10.4196/kjpp.2012.16.6.379
Lee, I. J., Chao, C. Y., Yang, Y. C., Cheng, J. J., Huang, C. L., Chiou, C. T., et al. (2021). Huang Lian Jie Du Tang Attenuates Paraquat-Induced Mitophagy in Human SH-Sy5y Cells: A Traditional Decoction with a Novel Therapeutic Potential in Treating Parkinson's Disease. Biomed. Pharmacother. 134, 111170. doi:10.1016/j.biopha.2020.111170
Li, H., Li, X., Liu, Z., Wu, S., Guo, J., Shi, R., et al. (2020). Resveratrol Reserved Hypoxia-Ischemia Induced Childhood Hippocampal Dysfunction and Neurogenesis via Improving Mitochondrial Dynamics. Neurosci. Res. 161, 51–58. doi:10.1016/j.neures.2019.11.012
Liao, C.-P., Liu, X.-C., Dong, S.-Q., An, M., Zhao, L., Zhang, A.-J., et al. (2021). Investigation of the Metabolites of Five Major Constituents from Berberis Amurensis in normal and Pseudo Germ-free Rats. Chin. J. Nat. Medicines 19, 758–771. doi:10.1016/S1875-5364(21)60082-1
Liu, C. S., Zheng, Y. R., Zhang, Y. F., and Long, X. Y. (2016). Research Progress on Berberine with a Special Focus on its Oral Bioavailability. Fitoterapia 109, 274–282. doi:10.1016/j.fitote.2016.02.001
Liu, Y., Du, T., Zhang, W., Lu, W., Peng, Z., Huang, S., et al. (2019). Modified Huang-Lian-Jie-Du Decoction Ameliorates Aβ Synaptotoxicity in a Murine Model of Alzheimer's Disease. Oxid Med. Cel. Longev. 2019, 8340192. doi:10.1155/2019/8340192
Lyu, Y. F., Lin, L., Xie, Y. N., Li, D., Xiao, M., Zhang, Y. F., et al. (2021). Blood-Glucose-Lowering Effect of Coptidis Rhizoma Extracts from Different Origins via Gut Microbiota Modulation in Db/db Mice. Front. Pharmacol. 12, 684358. doi:10.3389/fphar.2021.684358
Malhi, G. S., and Mann, J. J. (2018). Depression. Lancet 392, 2299–2312. doi:10.1016/S0140-6736(18)31948-2
More, N. V., Kharat, K. R., and Kharat, A. S. (2017). Berberine from Argemone Mexicana L Exhibits a Broadspectrum Antibacterial Activity. Acta Biochim. Pol. 64, 653–660. doi:10.18388/abp.2017_1621
Mujtaba, M. A., Akhter, M. H., Alam, M. S., Ali, M. D., and Hussain, A. (2022). An Updated Review on Therapeutic Potential and Recent Advances in Drug Delivery of Berberine: Current Status and Future prospect. Cpb 23, 60–71. doi:10.2174/1389201022666210208152113
Mustafa, K., Mohamed, H., Shah, A. M., Yu, S. X., Akhlaq, M., Xiao, H. F., et al. (2020). In Vitro Anticancer Potential of Berberis Lycium Royle Extracts against Human Hepatocarcinoma (HepG2) Cells. Biomed. Res. Int., 8256809. doi:10.1155/2020/8256809
Och, A., Zalewski, D., Komsta, Ł., Kołodziej, P., Kocki, J., and Bogucka-Kocka, A. (2019). Cytotoxic and Proapoptotic Activity of Sanguinarine, Berberine, and Extracts of Chelidonium Majus L. And Berberis Thunbergii DC. toward Hematopoietic Cancer Cell Lines. Toxins (Basel) 11, 485. doi:10.3390/toxins11090485
Pandey, G., Khatoon, S., Pandey, M. M., and Rawat, A. K. S. (2018). Altitudinal Variation of Berberine, Total Phenolics and Flavonoid Content in Thalictrum Foliolosum and Their Correlation with Antimicrobial and Antioxidant Activities. J. Ayurveda Integr. Med. 9, 169–176. doi:10.1016/j.jaim.2017.02.010
Park, S. C. (2019). Neurogenesis and Antidepressant Action. Cell Tissue Res. 377, 95–106. doi:10.1007/s00441-019-03043-5
Qu, S. Y., Li, X. Y., Heng, X., Qi, Y. Y., Ge, P. Y., Ni, S. J., et al. (2021). Analysis of Antidepressant Activity of Huang-Lian Jie-Du Decoction through Network Pharmacology and Metabolomics. Front. Pharmacol. 12, 619288. doi:10.3389/fphar.2021.619288
Rana, A. K., Sharma, S., Patial, V., and Singh, D. (2022). Lithium Therapy Subdues Neuroinflammation to Maintain Pyramidal Cells Arborization and Rescues Neurobehavioural Impairments in Ovariectomized Rats. Mol. Neurobiol. doi:10.1007/s12035-021-02719-w
Rao, G. X., Zhang, S., Wang, H. M., Li, Z. M., Gao, S., and Xu, G. L. (2009). Antifungal Alkaloids from the Fresh rattan Stem of Fibraurea Recisa Pierre. J. Ethnopharmacol. 123, 1–5. doi:10.1016/j.jep.2009.02.046
Rezaeian, L., Kalalian-Moghaddam, H., Mohseni, F., Khaksari, M., and Rafaiee, R. (2020). Effects of Berberine Hydrochloride on Methamphetamine-Induced Anxiety Behaviors and Relapse in Rats. Iran J. Basic Med. Sci. 23, 1480–1488. doi:10.22038/ijbms.2020.47285.10884
Riecher-Rössler, A. (2017). Sex and Gender Differences in Mental Disorders. Lancet Psychiatry 4, 8–9. doi:10.1016/S2215-0366(16)30348-0
Roshanravan, B., Yousefizadeh, S., Apaydin Yildirim, B., Farkhondeh, T., Amirabadizadeh, A., Ashrafizadeh, M., et al. (2020). The Effects of Berberis Vulgaris L. And Berberis Aristata L. in Metabolic Syndrome Patients: a Systematic and Meta-Analysis Study. Arch. Physiol. Biochem., 1–12. doi:10.1080/13813455.2020.1828482
Sharma, N., Kumar, V., Chopra, M. P., Sourirajan, A., Dev, K., and El-Shazly, M. (2020). Thalictrum Foliolosum: A Lesser Unexplored Medicinal Herb from the Himalayan Region as a Source of Valuable Benzyl Isoquinoline Alkaloids. J. Ethnopharmacol. 255, 112736. doi:10.1016/j.jep.2020.112736
Shen, X., Hui, R., Luo, Y., Yu, H., Feng, S., Xie, B., et al. (2020). Berberine Facilitates Extinction of Drug-Associated Behavior and Inhibits Reinstatement of Drug Seeking. Front. Pharmacol. 11, 476. doi:10.3389/fphar.2020.00476
Shou, J. W., Cheung, C. K., Gao, J., Shi, W. W., and Shaw, P. C. (2019). Berberine Protects C17.2 Neural Stem Cells from Oxidative Damage Followed by Inducing Neuronal Differentiation. Front. Cel. Neurosci. 13, 3955. doi:10.3389/fncel.2019.00395
Singh, M., Srivastava, S., and Rawat, A. K. (2007). Antimicrobial Activities of Indian Berberis Species. Fitoterapia 78, 574–576. doi:10.1016/j.fitote.2007.03.021
Singh, T., Chhokar, A., Thakur, K., Aggarwal, N., Pragya, P., Yadav, J., et al. (2021). Targeting Aberrant Expression of STAT3 and AP-1 Oncogenic Transcription Factors and HPV Oncoproteins in Cervical Cancer by Berberis Aquifolium. Front. Pharmacol. 12, 757414. doi:10.3389/fphar.2021.757414
Suchomelová, J., Bochoráková, H., Paulová, H., Musil, P., and Táborská, E. (2007). HPLC Quantification of Seven Quaternary Benzo[c]phenanthridine Alkaloids in Six Species of the Family Papaveraceae. J. Pharm. Biomed. Anal. 44, 283–287. doi:10.1016/j.jpba.2007.02.005
Szalak, R., Kukula-Koch, W., Matysek, M., Kruk-Słomka, M., Koch, W., Czernicka, L., et al. (2021). Effect of Berberine Isolated from Barberry Species by Centrifugal Partition Chromatography on Memory and the Expression of Parvalbumin in the Mouse Hippocampus Proper. Int. J. Mol. Sci. 22, 4487. doi:10.3390/ijms22094487
Tang, R., Luo, M., Li, J., Peng, Y., Wang, Y., Liu, B., et al. (2019). Symptoms of Anxiety and Depression Among Chinese Women Transitioning through Menopause: Findings from a Prospective Community-Based Cohort Study. Fertil. Steril. 112, 1160–1171. doi:10.1016/j.fertnstert.2019.08.005
Tims, Mc., and Batista, C. (2007). Effects of Root Isoquinoline Alkaloids from Hydrastis canadensis on Fusarium Oxysporum Isolated from Hydrastis Root Tissue. J. Chem. Ecol. 33, 1449–1455. doi:10.1007/s10886-007-9319-9
Tungpradit, R., Sinchaikul, S., Phutrakul, S., Wongkham, W., and Chen, S. T. (2010). Anti-Cancer Compound Screening and Isolation: Coscinium Fenestratum, Tinospora Crispa and Tinospora Cordifolia. Chiang Mai J. Sci. 37, 476–488.
Wang, P. R., Wang, J. S., Zhang, C., Song, X. F., Tian, N., and Kong, L. Y. (2013). Huang-Lian-Jie-Du-Decotion Induced Protective Autophagy against the Injury of Cerebral Ischemia/reperfusion via MAPK-mTOR Signaling Pathway. J. Ethnopharmacol. 149, 270–280. doi:10.1016/j.jep.2013.06.035
Wang, Q. S., Li, K., Gao, L. N., Zhang, Y., Lin, K. M., and Cui, Y. L. (2020). Intranasal Delivery of Berberine via In Situ Thermoresponsive Hydrogels with Non-invasive Therapy Exhibits Better Antidepressant-like Effects. Biomater. Sci. 8, 2853–2865. doi:10.1039/c9bm02006c
Wang, Y., Tong, Q., Ma, S. R., Zhao, Z. X., Pan, L. B., Cong, L., et al. (2021). Oral Berberine Improves Brain Dopa/dopamine Levels to Ameliorate Parkinson's Disease by Regulating Gut Microbiota. Signal. Transduct Target. Ther. 6, 77. doi:10.1038/s41392-020-00456-5
Wang, Xiaohui, X., Northcutt, A. L., Cochran, T. A., Zhang, X., Fabisiak, T. J., Haas, M. E., et al. (2019). Methamphetamine Activates Toll-like Receptor 4 to Induce Central Immune Signaling within the Ventral Tegmental Area and Contributes to Extracellular Dopamine Increase in the Nucleus Accumbens Shell. ACS Chem. Neurosci. 10, 3622–3634. doi:10.1021/acschemneuro.9b00225
Wang, Y. S., Shen, C. Y., and Jiang, J. G. (2019). Antidepressant Active Ingredients from Herbs and Nutraceuticals Used in TCM: Pharmacological Mechanisms and Prospects for Drug Discovery. Pharmacol. Res. 150, 104520. doi:10.1016/j.phrs.2019.104520
Xu, D., Qiu, C., Wang, Y., Qiao, T., and Cui, Y. L. (2021). Intranasal Co-delivery of Berberine and Evodiamine by Self-Assembled Thermosensitive In-Situ Hydrogels for Improving Depressive Disorder. Int. J. Pharm. 603, 120667. doi:10.1016/j.ijpharm.2021.120667
Yang, L., Zhao, Y., Wang, Y., Liu, L., Zhang, X., Li, B., et al. (2015). The Effects of Psychological Stress on Depression. Curr. Neuropharmacol. 13, 494–504. doi:10.2174/1570159x1304150831150507
Zeng, N. X., Li, H. Z., Wang, H. Z., Liu, K. G., Gong, X. Y., Luo, W. L., et al. (2022). Exploration of the Mechanism by Which Icariin Modulates Hippocampal Neurogenesis in a Rat Model of Depression. Neural Regen. Res. 17, 632, doi:10.4103/1673-5374.320993
Keywords: berberine, bioamine, depression, natural active ingredients, neuroplasticity
Citation: Zhu W-Q, Wu H-Y, Sun Z-H, Guo Y, Ge T-T, Li B-J, Li X and Cui R-J (2022) Current Evidence and Future Directions of Berberine Intervention in Depression. Front. Pharmacol. 13:824420. doi: 10.3389/fphar.2022.824420
Received: 29 November 2021; Accepted: 01 February 2022;
Published: 23 May 2022.
Edited by:
Fushun Wang, Nanjing University of Chinese Medicine, ChinaReviewed by:
Malcolm Hopwood, The University of Melbourne, AustraliaQi Xu, Anhui Medical University, China
Copyright © 2022 Zhu, Wu, Sun, Guo, Ge, Li, Li and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Li, WGlubGlAamx1LmVkdS5jbg==; Ran-Ji Cui, Y3VpcmFuamlAamx1LmVkdS5jbg==
 Wen-Qian Zhu1
Wen-Qian Zhu1 Bing-Jin Li
Bing-Jin Li Ran-Ji Cui
Ran-Ji Cui