- 1Department of Cardiac Surgery, Union Hospital, Fujian Medical University, Fuzhou, China
- 2Department of Nursing, Union Hospital, Fujian Medical University, Fuzhou, China
Background: Medication adherence is crucial for patients with mechanical heart valve replacement. Although families functioning is positively associated with medication adherence, little is known about the underlying mechanisms.
Objective: To test whether family functioning affects medication adherence through illness perceptions and whether this mediating effect was moderated by medication literacy.
Methods: 319 patients after mechanical heart valve replacement were included in this cross-sectional study from June 2021 to October 2021. Data regarding family functioning, illness perceptions, medication adherence, and medication literacy were collected through questionnaires. The moderated mediation model was examined by Hayes’s PROCESS macro, based on the bootstrapping method.
Results: The results revealed illness perceptions partially mediated the association of family functioning on medication adherence [β = 0.08, 95% confidence intervals: (0.04, 0.12)], and this effect was stronger for patients with low medication literacy than those with high literacy [β = −0.36, 95% CI: (−0.50, −0.22)]. Furthermore, the relationship between family functioning and medication adherence was only significant in patients with low medication literacy [β = 0.36, 95% CI: (0.23, 0.50)].
Conclusion: The mediating effect of illness perceptions between family functioning and medication adherence was moderated by medication literacy. Efforts to improve medication adherence by targeting at improving family functioning may be more effective when considering illness perceptions, especially for patients with limited medication literacy.
1 Introduction
Mechanical heart valve replacement (MHVR) is still one of the most common surgeries to reduce the mortality of patients with advanced valvular disease (van Geemen et al., 2016). Every year, more than 200,000 heart valve surgeries are performed in China (Chen et al., 2015). However, patients after mechanical heart valve replacement (MHVR) require life-long anticoagulant treatment. The use of anticoagulants is complicated, and the therapeutic range is narrow. Incorrect medication use can lead to thromboembolism or bleeding and even death (da Silva Praxedes et al., 2019). Medication adherence is considered as the extent to which patients take medications as recommendations by healthcare providers (Huang et al., 2020). Stringent adherence to anticoagulants can reduce the duration of hospitalizations and mortality (Smet et al., 2018). However, according to the World Health Organization, the average adherence rate for long-term medications is only 50% and even lower in low-and middle-income countries. (Thomson Mangnall et al., 2016).
Family is regarded as a critical factor in promoting the health of patients with cardiovascular disease (Vedanthan et al., 2016). Family functioning is the main concept exploring the effect of family in illness and is defined as how family members communicate with each other, fulfill family roles, cope with and adjust family stress, and relate to other members (Zhang 2018). Family functioning played an integral role in long-term self-management and adherence, especially in Chinese families (Luo et al., 2019). Patients with adequate family functioning, that is, receiving considerable support and care, were proved to have better medication-taking behaviors (Psihogios et al., 2019; Sun et al., 2019). However, the research exploring the potential mechanisms underlying the relationship between family functioning and medication adherence is still limited.
Family functioning is closely related to the emotions of individuals living in their families (Sullivan et al., 2012). There is evidence that patients with poor family functioning suffer from more emotional problems (Zhang et al., 2019). Illness perceptions are identified as the emotions and thoughts individuals formed about their illnesses (Alyami et al., 2021). Maintaining or developing negative illness perceptions can lead to worse health status and poorer quality of life after valve replacement (Kohlmann et al., 2012). According to the Common Sense Model, illness perceptions could activate individuals to change their behaviors (Gibbons et al., 2013). Prior research has also found that illness perception was a predictor of adherence behavior in patients with cardiovascular disease (Mosleh and Almalik 2016). Patients with negative illness perceptions were more likely to be non-adherent to receive anticoagulation as prescribed (Miyazaki et al., 2018). Therefore, based on the findings of previous studies, illness perceptions may play the mediating role in the association between family functioning and medication adherence such that sufficient family functioning may associate with less threatening illness perceptions, which in turn led to better medication adherence.
Medication literacy is health literacy in the context of medication use, which refers to the ability of individuals to obtain, understand, calculate, and process information to the appropriate use of medication (Lee et al., 2017; Cordina et al., 2018). Ostini et al. found that there was not always a linear but U-shaped relationship between health literacy and medication adherence, affected by factors like education, social support, or cognitive functioning (Ostini and Kairuz 2014). Although, a study carried out in Chinese patients initially revealed the connection between medication literacy and medication adherence (Shi et al., 2019). It is still uncertain whether medication literacy has interactions with other influencing factors on adherence. Furthermore, a previous study revealed that negative illness perceptions can lead to poor medication adherence, however, not all patients were equally affected by perceptions because of different levels of literacy (Shiyanbola et al., 2018). In other word, literacy played a moderating role in the relationship between illness perceptions and medication adherence. On the other hand, for patients with limited literacy, family functioning promote skills to access, share and evaluate information to enhance medication adherence (Kraenbring et al., 2019; Wong et al., 2020). However, patients with adequate literacy have the ability to process information independently to improve medication adherence (Shen et al., 2020). Thus, literacy may also be a potential moderator in the association between family functioning and medication adherence. However, no research has examined the moderating effect of medication literacy.
Family plays an important role in medication adherence of patients receiving life-long anticoagulant treatment, especially in domestic life after discharge. However, the underlying mechanisms of the association remain unknown. To fill the gaps in the literature, this study 1) examined the mediating effect of illness perceptions between family functioning and medication adherence, and 2) tested the moderating effect of medication literacy on the relationship between family functioning and medication adherence, and the relationship between illness perceptions and adherence. Knowledge about the mediating and moderating mechanisms between family functioning and medication adherence could elucidate the mean of improving medication adherence to develop more effective strategies.
2 Methods
2.1 Design and Setting
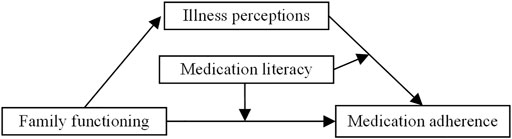
A cross-sectional study was conducted in the department of cardiac surgery at a tertiary hospital in Fuzhou, which is located in southeast China, from June 2021 to October 2021. A convenience sampling method was used to recruit participants. In this study, a moderated mediation model was constructed, integrated both mediation and moderation (Bolin, 2014), to examine the role of illness perceptions and medication literacy on the relationship between family functioning and medication adherence (Figure 1). The study was approved by the Research Ethics Committee of Fujian Medical University Union Hospital (No: 2020KY0127).
2.2 Participants and Procedures
Inclusion criteria were: 1) aged 18 years or older; 2) persisted with oral anticoagulants for at least 3 months after MHVR; 3) were able to read and understand the questionnaires. Patients with mental illness or cognitive impairment were excluded. Eligible patients were informed about the purpose, content, and investigation procedures of this study, and signed informed consent before the study began. All paper-based questionnaires were completed by patients on-site. The time of filling out the questionnaires was approximately 15 min. In this process, trained research assistants were present to resolve possible doubts. All questionnaires were reclaimed on the spot after completion, and collected questionnaires were checked for missing items.
2.3 Data Collection Tools
2.3.1 Participant Characteristics
The general information questionnaire was designed to obtain characteristics, including age, gender, education level, marital status, the burden of medical costs, side effects of anticoagulants, number of daily medications, and time of anticoagulants application.
2.3.2 Medication Adherence
Medication adherence was assessed using the 12-items Medication Adherence Scale (MAS) developed by Ueno et al. (2018) Responses are on a 5-point Likert scale (1 = never to 5 = always). The total score of MAS ranges from 12 to 60, with a higher score indicating better medication adherence. The Chinese version of the MAS has been tested with good reliability and validity in patients receiving anticoagulant therapy. (Zhang et al., 2021) In this study, Cronbach’s alpha of the scale was 0.79.
2.3.3 Family Functioning
Family functioning was measured by the Family APGAR Index, developed by Smilkstein et al. (1982) It is a self-report scale composed of five parameters: adaptation, partnership, growth, affection, and resolve. The items are rated on a 3-point Likert scale ranging from 0 to 2 (“hardly ever” = 0, “sometimes” = 1, “always” = 2). The total score on this scale ranges from 0 to 10. A Higher score reflects greater satisfaction of family functioning. The Chinese version of the scale has demonstrated good reliability with a Cronbach’s alpha of 0.89 (Wang et al., 2020). In this study, Cronbach’s alpha coefficient was 0.88.
2.3.4 Illness Perceptions
The Brief Illness Perception Questionnaire (BIPQ) was used to measure illness perceptions. BIPQ is a simple instrument to assess the individual’s emotional and cognitive representations of disease. The scale consists of the following domains: consequences, timeline, personal control, treatment control, identity, concerns, understanding, and emotional response. Each item was assessed on a scale of 0–10, and the overall score of the scale ranges from 0 to 80. Higher scores reflect more threatening and negative illness perceptions. Cronbach’s alpha for the Chinese version of BIPQ was 0.79, and test-retest reliability was 0.7 (Du et al., 2021). In the present study, Cronbach’s alpha was 0.87.
2.3.5 Medication Literacy
Maniaci developed the Medication Literacy Questionnaire (Maniaci et al., 2008). The Chinese version of the scale was modified and applied with good reliability (Zheng et al., 2015). It involves the evaluation of the ability to comprehend, calculate and process medication-related information. Each patient was required to answer the questions like “What is the recommended dose of each medication?”. The scale is scored one point for the correct answer and no point for the wrong answer. The highest score possible is 7. A higher score indicates a higher level of medication literacy. The value of Cronbach’s alpha in this study was 0.80.
2.4 Statistical Analyses
Data were analyzed using SPSS version 25.0. Frequencies (percentages) or means (standard deviations) were calculated to describe the baseline characteristics. Pearson correlation was employed to evaluate the correlation between explanatory variables (family functioning, illness perceptions, and medication literacy) and the outcome variable (medication adherence). p values < 0.05 were considered statistically significant. Mediation and moderated mediation was carried out by the PROCESS macro for SPSS, which was developed especially to do computations by the fundamentals of mediation and moderation analysis (Bolin, 2014). According to the analytic framework developed by Baron and Kenny (1986), a series of regression were conducted to test the mediating effect of illness perceptions. In this study, the mediating effect was established if 1) family functioning significantly directly predicted medication adherence (in Model 1), 2) family functioning significantly predicted illness perceptions (in Model 2), and 3) illness perceptions predicted medication adherence after controlling family functioning (in Model 3). The bootstrapping method with 5,000 iterations produces 95% confidence intervals (CI), and the effect was established if the interval does not contain 0. The moderated mediation is used to test whether the mediation effect was differed by the level of moderator. According to the hypothesized model, we calculated the moderating effect of medication literacy in the relationship between family functioning and medication adherence (in Model 1), and the relationship between illness perceptions and medication adherence (in Model 3). In these processes, 95% CI of the interaction term did not contain 0, representing a significant moderating effect. Furthermore, simple slope analyses were used to calculate the moderated direct and indirect effects of family functioning on medication adherence. The results of simple slope were presented according to the high (one standard above the mean) and low (one standard below the mean) levels of variables. The patient’s characteristics, including age, gender, educational level, marital status, the burden of medical costs, side effects of anticoagulants, number of daily medications, and time of anticoagulants application were all treated as covariates throughout the analyses. All continuous variables were standardized before analyses.
3 Results
3.1 Characteristics of Patients
335 questionnaires were distributed, and 319 valid questionnaires were finally included, yielding a response rate of 95.22%. A total of 152 patients underwent mitral valve replacement, 90 patients underwent aortic valve replacement, and 77 patients received double valve replacement.
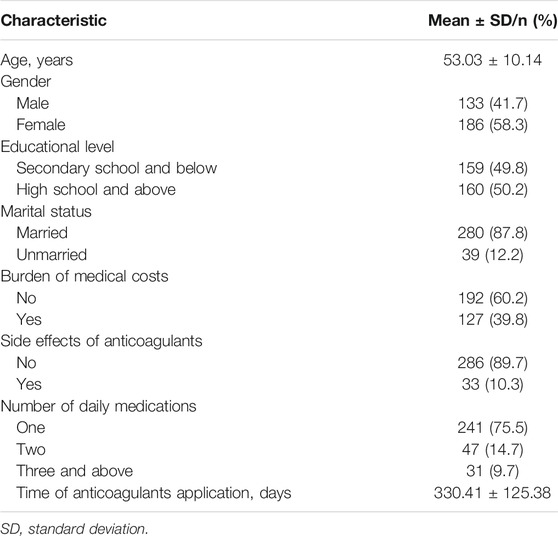
The mean age of the participants was 53.03 ± 10.14 years. The male accounted for 41.7% of the participants (n = 133). Nearly half of the cases were educated secondary school and below (49.8%, n = 159), and most were married (87.8%). 39.8% of the participants had the financial burden of paying medical costs. The average time of anticoagulants application was 330.41 ± 125.38 days after valve replacement (Table 1).
3.2 Mean Scores and Correlation Matrix of the Study Variables
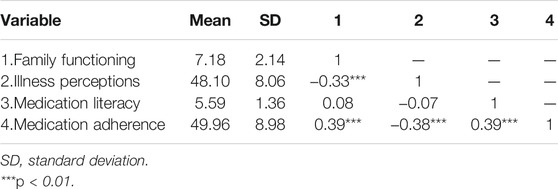
The means and standard deviations of family functioning, illness perceptions, medication literacy, and medication adherence are presented in Table 2. Family functioning was negatively associated with illness perceptions (r = −0.33, p < 0.001), and the relationship between family functioning and medication adherence was also statistically significant (r = 0.39, p < 0.001). Illness perceptions correlated negatively with medication adherence (r = −0.38, p < 0.001). In addition, medication literacy had positive correlations with medication adherence (r = 0.39, p < 0.001).
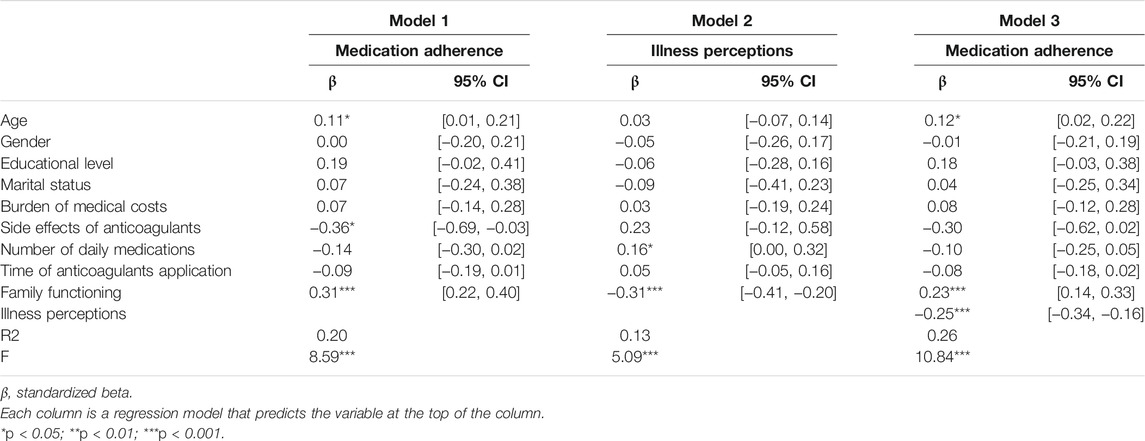
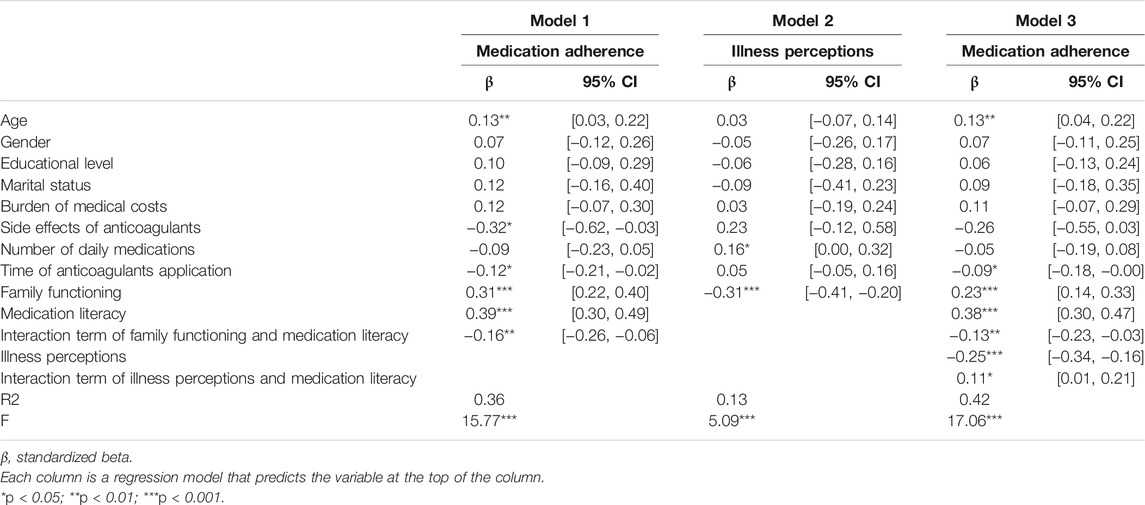
3.3 Mediation of Illness Perceptions
The results of the mediation test are presented in Table 3. In Model 1, family functioning was positively correlated with medication adherence [β = 0.31, 95%CI: (0.22, 0.40), p < 0.001]. In Model 2, the effect of family functioning on illness perceptions was significant [β = −0.31, 95%CI: (−0.41, −0.20), p < 0.001]. In Model 3, illness perceptions were negatively associated with medication adherence [β = -0.25, 95%CI: (−0.34, −0.16), p < 0.001]. The coefficient for the indirect path between family functioning and medication adherence through illness perceptions was significant [β = 0.08, 95%CI: (0.04, 0.12), p < 0.001]. The indirect effect accounted for 23.4% of the total effect, indicating a partial mediation. Results of mediation analyses revealed that illness perceptions played a mediating role in the relationship between family functioning and medication adherence.
3.4 Moderation of Mediation Literacy
The results of the moderation test are shown in Table 4. In Model 1, family functioning and medication literacy were both positively related to medication adherence (p < 0.001). The interaction term was negatively correlated with medication adherence [β = −0.16, 95% CI: (−0.26, −0.06), p < 0.01], which indicated that medication literacy moderated the relationship between family functioning and medication adherence. In Model 2, the effect of family functioning on illness perceptions was significant (p < 0.001). In Model 3, medication literacy positively predicted medication adherence (p < 0.001), while illness perceptions had a negative correlation with adherence (p < 0.001). The interaction term of illness perceptions and medication literacy positively affected medication adherence [β = 0.11, 95% CI: (0.01, 0.21), p < 0.05], which demonstrated a moderating role of medication literacy between illness perceptions and medication adherence. The index of moderated mediation was −0.04 [SE: 0.02, 95% CI: (−0.08, −0.00)]. Results revealed that medication literacy played a moderating role.
Further simple slope revealed, for patients with low medication literacy, family functioning was associated with medication adherence [β = 0.36, 95% CI: (0.23, 0.50), p < 0.001]. However, this relationship became non-significant in patients with high medication literacy [β = 0.10, 95%CI: (−0.03, 0.24), p > 0.05]. Under the condition of high medication literacy, the association of illness perceptions and medication adherence was significant [β = −0.13, 95% CI: (−0.27, −0.01), p < 0.05]. This relationship was much stronger for patients with low medication literacy [β = −0.36, 95% CI: (−0.50, −0.22), p < 0.001]. The moderation plot of medication literacy is shown in Figure 2.
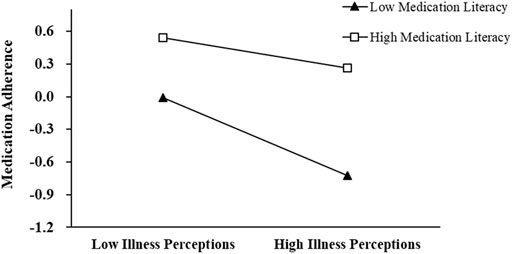
FIGURE 2. The moderator role of medication literacy on the relationship between illness perceptions and medication adherence. Y-axis is the standardized score of the MAS.
4 Discussion
The medication adherence of MHVR patients is closely related to adverse events (Smet et al., 2018). Therefore, paying attention to medication adherence and its influence mechanisms is of great significance to improving patients’ long-term survival. In this study, we examined the mediating effect of illness perceptions on the relationship between family function and medication adherence, and the moderating role that medication literacy played in the relationship. To the best of our knowledge, this is the first study to reveal the underlying mechanisms between family functioning and medication adherence, which provides a basis for further targeted intervention.
In a previous study, family functioning was found to be closely correlated with medication adherence in Chinese patients (Sun et al., 2019). Consistent with the prior study, our results also showed that good family functioning was a positive predictor of medication adherence in patients with MHVR. Family is the main source of support in the management of disease, for paying attention to members’ needs and having a profound impact on the behavior of the individual nested in it (Pereira et al., 2014; Barnes et al., 2020; Yeom and Lee 2020). Good family functioning provides adequate family cohesion and sufficient family coping ability to give practical support, including reading medication labels, picking up medications, and supervising medication-adverse reactions timely to improve medication adherence (Pereira et al., 2014; Zhang 2018). Early detection of risks caused by medications may also reduce the patients’ worries to improve adherence to oral anticoagulation therapy (Hwong et al., 2017).
In addition, the effect of family functioning on medication adherence was partially mediated by illness perceptions in this study. In other words, good family functioning helps to improve patients’ illness perceptions, which in turn impacts medication adherence. Family members provide emotional and appraisal support, bringing social interaction and relieving negative emotions including fear of illness (Mayberry and Osborn 2012; Ao et al., 2020). It was also mentioned in McMaster’s Family Functioning Model that sufficient family functioning helps improve the individual emotional response (Pires et al., 2016). Patients whose families act openly, express emotions directly, solve problems effectively, and communicate information directly, have lower negative illness perceptions (Postolica et al., 2017). In Common Sense Model, individuals’ emotional representations of illness are also precursors of behavioral change like adhering to medication (Shiyanbola et al., 2018). Thus, healthcare professionals should value the family status of patients with MHVR, and could integrate family involvement into the medication guidance and management.
In recent years, medication literacy has received increasing attention. A cross-sectional study conducted on 420 Chinese hypertension patients reported that medication literacy was an important predictor of medication adherence (Shi et al., 2019). Same as the previous study, a high level of medication literacy was also closely associated with medication adherence in patients with MHVR. In addition, medication literacy also played a moderating role. Specifically, the relationship between family functioning and medication adherence of patients with limited medication literacy was significant, but this relationship does not hold for patients with adequate medication literacy. Medication literacy contains elements including knowledge, attitude, skill, and behavior (Shen et al., 2020). Patients with limited literacy have difficulty in obtaining drug information actively, understanding drug label information correctly, and calculating drug dosage exactly (Soones et al., 2017). Moreover, patients may have skeptical perceptions about oral anticoagulants, resulting in prolonged duration of medication, adjustment of drug dose, or even unauthorized discontinuation (Lee et al., 2017). Limited literacy also increases doctor-patient communication barriers, resulting in patients being less involved in medical decision-making (Cordina et al., 2018). Therefore, patients with poor literacy are more likely to seek assistance and supervision from their families about how to use the medication correctly. Conversely, medication intervention with family involvement may not be effective for patients with adequate literacy. Therefore, medication literacy may be regarded as a promising indicator to distinguish whether people require family involvement in promoting adherence. For healthcare providers, they should also evaluate the level of medication literacy before guiding self-management of medication and pay more attention to patients with marginal literacy.
Literacy was reported as a moderator in a study conducted on 174 patients with diabetes in the United States (Shiyanbola et al., 2018). Similarly, our results also showed that medication literacy buffered the negative impact of illness perceptions on medication adherence. In other words, an increase in threatening illness perceptions may not always be associated with a sharp decrease in medication adherence for individuals with adequate literacy. Negative illness perceptions are independent of the surgery or medical changes and result in negative attitudes or actions for a long time after valve replacement (Kohlmann et al., 2012). Patients with adequate medication literacy increase their self-efficacy and sense of mastery during the process of actively acquiring and correctly utilizing information (Shen et al., 2020). This allows them to participate in their treatment more actively. On the other hand, in obtaining information, patients may also have a deeper understanding of the necessity and importance of receiving anticoagulants after MHVR. Thus, patients with high medication literacy can show better medication adherence even if they perceive a severe illness threat. However, for patients with limited literacy, improving negative illness perceptions may also contribute to medication adherence. Overall, our findings suggest that in focusing on medication use, it is necessary not only to understand the severity of patients’ illness perceptions but also to consider differences in individual literacy levels.
5 Limitations
There are still several limitations. First, we cannot infer any causal relationships from the cross-sectional design, nor can we observe the dynamic relationships between variables over time. Future research may apply longitudinal or experimental designs to validate relationships assumed among these variables. Second, a convenience sampling method was applied in this study, resulting in selection bias. Third, the data of this study were collected from patients’ self-reports. Multiple sources of information (such as family reports) can provide more rigorous tests for research hypotheses. Finally, the model of this study was developed for patients after MHVR. The results of this study may not be generalizable to other populations. Future research may also benefit from testing this model in other samples.
6 Conclusion
This study indicated illness perceptions can be one possible mediating mechanism underlying the relationship between family functioning and medication adherence. Moreover, medication literacy moderated the direct and indirect relationship between family functioning and medication adherence, with the relation being more significant for patients with low level of medication literacy. Efforts to improve medication adherence by targeting at improving family functioning may be more effective when considering illness perceptions, especially for patients with limited medication literacy.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Research Ethics Committee, Union Hospital, Fujian Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YL and LC conceived the whole study. HN and YP drafted the manuscript and analyzed the data. HN, SL, and XH were in charge of data collecting. All authors provided an important revision of this manuscript.
Funding
This research was funded by the Guiding Project of Science and Technology, Fujian province (grant number 2021Y0023), the Fujian Provincial Finance Special Project (grant number 2020CZ011), and Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University), Fujian Province University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors appreciate all patients who participated in this study. We would also like to thank the hospital for supporting the data collection of this study.
References
Alyami, M., Serlachius, A., O'Donovan, C. E., van der Werf, B., and Broadbent, E. (2021). A Systematic Review of Illness Perception Interventions in Type 2 Diabetes: Effects on Glycaemic Control and Illness Perceptions. Diabet Med. 38 (3), e14495. doi:10.1111/dme.14495
Ao, Y., Zhu, H., Meng, F., Wang, Y., Ye, G., Yang, L., et al. (2020). The Impact of Social Support on Public Anxiety amidst the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 17 (23), 9097. doi:10.3390/ijerph17239097
Barnes, M. D., Hanson, C. L., Novilla, L. B., Magnusson, B. M., Crandall, A. C., and Bradford, G. (2020). Family-Centered Health Promotion: Perspectives for Engaging Families and Achieving Better Health Outcomes. Inquiry 57, 46958020923537. doi:10.1177/0046958020923537
Baron, R. M., and Kenny, D. A. (1986). The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers Soc. Psychol. 51 (6), 1173–1182. doi:10.1037//0022-3514.51.6.1173
Bolin, J. H. (2014). Hayes, Andrew F. (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press. J. Educ. Meas. 51 (3), 335–337. doi:10.1111/jedm.12050
Chen, Q. L., Dong, L., Dong, Y. J., Zhao, S. L., Fu, B., Wang, Y. Q., et al. (2015). Security and Cost Comparison of INR Self-Testing and Conventional Hospital INR Testing in Patients with Mechanical Heart Valve Replacement. J. Cardiothorac. Surg. 10, 4. doi:10.1186/s13019-015-0205-1
Cordina, M., Hämeen-Anttila, K., Lauri, J., Tabone, S., and Enlund, H. (2018). Health and Medication Literacy and the Desire to Participate in Pharmacotherapy Decision Making - Comparison of Two Countries. Res. Soc. Adm Pharm 14 (9), 817–823. doi:10.1016/j.sapharm.2018.06.009
da Silva Praxedes, M. F., Sousa Vianna, M., Freitas Nunes de Sousa, W. J., Bartolazzi, F., de Araújo, V. E., and Parreiras Martins, M. A. (2019). Instruments for the Assessment of Patient Adherence to Oral Anticoagulation with Warfarin Protocol for a Systematic Review. Medicine (Baltimore) 98 (42), e17323. doi:10.1097/md.0000000000017323
Du, Y., Zhang, Q., Liu, S., and Wang, L. (2021). Mediating Role of Coping Style in Illness Perceptions and Symptom burden of Elderly Patients with COPD. Nurs. Res. 35 (09), 1662–1666. doi:10.12102/j.issn.1009-6493.2021.09.029
Gibbons, C. J., Kenning, C., Coventry, P. A., Bee, P., Bundy, C., Fisher, L., et al. (2013). Development of a Multimorbidity Illness Perceptions Scale (MULTIPleS). PLoS One 8 (12), e81852. doi:10.1371/journal.pone.0081852
Huang, Y. M., Shiyanbola, O. O., Chan, H. Y., and Smith, P. D. (2020). Patient Factors Associated with Diabetes Medication Adherence at Different Health Literacy Levels: a Cross-Sectional Study at a Family Medicine Clinic. Postgrad. Med. 132 (4), 328–336. doi:10.1080/00325481.2020.1749499
Hwong, W. Y., Abdul Aziz, Z., Sidek, N. N., Bots, M. L., Selvarajah, S., Kappelle, L. J., et al. (2017). Prescription of Secondary Preventive Drugs after Ischemic Stroke: Results from the Malaysian National Stroke Registry. BMC Neurol. 17 (1), 203. doi:10.1186/s12883-017-0984-1
Kohlmann, S., Rimington, H., and Weinman, J. (2012). Profiling Illness Perceptions to Identify Patients At-Risk for Decline in Health Status after Heart Valve Replacement. J. Psychosom Res. 72 (6), 427–433. doi:10.1016/j.jpsychores.2012.03.002
Kraenbring, M. M., Zelikovsky, N., and Meyers, K. E. C. (2019). Medication Adherence in Pediatric Renal Transplant Patients: The Role of Family Functioning and Parent Health Locus of Control. Pediatr. Transpl. 23 (2), e13346. doi:10.1111/petr.13346
Lee, C. H., Chang, F. C., Hsu, S. D., Chi, H. Y., Huang, L. J., and Yeh, M. K. (2017). Inappropriate Self-Medication Among Adolescents and its Association with Lower Medication Literacy and Substance Use. PLoS One 12 (12), e0189199. doi:10.1371/journal.pone.0189199
Luo, D., Xu, J. J., Cai, X., Zhu, M., Wang, H., Yan, D., et al. (2019). The Effects of Family Functioning and Resilience on Self-Management and Glycaemic Control Among Youth with Type 1 Diabetes. J. Clin. Nurs. 28 (23-24), 4478–4487. doi:10.1111/jocn.15033
Maniaci, M. J., Heckman, M. G., and Dawson, N. L. (2008). Functional Health Literacy and Understanding of Medications at Discharge. Mayo Clin. Proc. 83 (5), 554–558. doi:10.4065/83.5.554
Mayberry, L. S., and Osborn, C. Y. (2012). Family Support, Medication Adherence, and Glycemic Control Among Adults with Type 2 Diabetes. Diabetes Care 35 (6), 1239–1245. doi:10.2337/dc11-2103
Miyazaki, M., Nakashima, A., Nakamura, Y., Sakamoto, Y., Matsuo, K., Goto, M., et al. (2018). Association between Medication Adherence and Illness Perceptions in Atrial Fibrillation Patients Treated with Direct Oral Anticoagulants: An Observational Cross-Sectional Pilot Study. PLoS One 13 (9), e0204814. doi:10.1371/journal.pone.0204814
Mosleh, S. M., and Almalik, M. M. (2016). Illness Perception and Adherence to Healthy Behaviour in Jordanian Coronary Heart Disease Patients. Eur. J. Cardiovasc. Nurs. 15 (4), 223–230. doi:10.1177/1474515114563885
Ostini, R., and Kairuz, T. (2014). Investigating the Association between Health Literacy and Non-adherence. Int. J. Clin. Pharm. 36 (1), 36–44. doi:10.1007/s11096-013-9895-4
Pereira, M. G., Pedras, S., and Machado, J. C. (2014). Family Variables as Moderators between Beliefs towards Medicines and Adherence to Self-Care Behaviors and Medication in Type 2 Diabetes. Fam. Syst. Health 32 (2), 198–206. doi:10.1037/fsh0000029
Pires, T., Assis, S. G., Avanci, J. Q., and Pesce, R. P. (2016). Cross-Cultural Adaptation of the General Functioning Scale of the Family. Rev. Saude Publica 50, 32. doi:10.1590/s1518-8787.2016050005832
Postolica, R., Iorga, M., Petrariu, F. D., and Azoicai, D. (2017). Cognitive-Behavioral Coping, Illness Perception, and Family Adaptability in Oncological Patients with a Family History of Cancer. Biomed. Res. Int. 2017, 8104397. doi:10.1155/2017/8104397
Psihogios, A. M., Fellmeth, H., Schwartz, L. A., and Barakat, L. P. (2019). Family Functioning and Medical Adherence across Children and Adolescents with Chronic Health Conditions: A Meta-Analysis. J. Pediatr. Psychol. 44 (1), 84–97. doi:10.1093/jpepsy/jsy044
Shen, Z., Shi, S., Ding, S., and Zhong, Z. (2020). Mediating Effect of Self-Efficacy on the Relationship between Medication Literacy and Medication Adherence Among Patients with Hypertension. Front. Pharmacol. 11, 569092. doi:10.3389/fphar.2020.569092
Shi, S., Shen, Z., Duan, Y., Ding, S., and Zhong, Z. (2019). Association between Medication Literacy and Medication Adherence Among Patients with Hypertension. Front. Pharmacol. 10, 822. doi:10.3389/fphar.2019.00822
Shiyanbola, O. O., Unni, E., Huang, Y. M., and Lanier, C. (2018). The Association of Health Literacy with Illness Perceptions, Medication Beliefs, and Medication Adherence Among Individuals with Type 2 Diabetes. Res. Soc. Adm Pharm 14 (9), 824–830. doi:10.1016/j.sapharm.2017.12.005
Smet, L., Heggermont, W. A., Goossens, E., Eeckloo, K., Vander Stichele, R., De Potter, T., et al. (2018). Adherence, Knowledge, and Perception about Oral Anticoagulants in Patients with Atrial Fibrillation at High Risk for Thromboembolic Events after Radiofrequency Ablation. J. Adv. Nurs. 74 (11), 2577–2587. doi:10.1111/jan.13780
Smilkstein, G., Ashworth, C., and Montano, D. (1982). Validity and Reliability of the Family APGAR as a Test of Family Function. J. Fam. Pract. 15 (2), 303–311. doi:10.1016/0021-9681(82)90122-9
Soones, T. N., Lin, J. L., Wolf, M. S., O'Conor, R., Martynenko, M., Wisnivesky, J. P., et al. (2017). Pathways Linking Health Literacy, Health Beliefs, and Cognition to Medication Adherence in Older Adults with Asthma. J. Allergy Clin. Immunol. 139 (3), 804–809. doi:10.1016/j.jaci.2016.05.043
Sullivan, A. E., Judd, C. M., Axelson, D. A., and Miklowitz, D. J. (2012). Family Functioning and the Course of Adolescent Bipolar Disorder. Behav. Ther. 43 (4), 837–847. doi:10.1016/j.beth.2012.04.005
Sun, Y., Wang, M., Zhou, Y., Wang, L., Zhang, H., Lv, Y., et al. (2019). The Mediating Effect of Family Function and Medication Adherence between Symptoms and Mental Disability Among Chinese Patients with Schizophrenia: a Cross-Sectional Study. Psychol. Health Med. 24 (5), 559–569. doi:10.1080/13548506.2018.1533248
Thomson Mangnall, L. J., Sibbritt, D. W., Al-Sheyab, N., and Gallagher, R. D. (2016). Predictors of Warfarin Non-adherence in Younger Adults after Valve Replacement Surgery in the South Pacific. Heart Asia 8 (2), 18–23. doi:10.1136/heartasia-2016-010751
Ueno, H., Yamazaki, Y., Yonekura, Y., Park, M. J., Ishikawa, H., and Kiuchi, T. (2018). Reliability and Validity of a 12-item Medication Adherence Scale for Patients with Chronic Disease in Japan. BMC Health Serv. Res. 18 (1), 592. doi:10.1186/s12913-018-3380-7
van Geemen, D., Soares, A. L., Oomen, P. J., Driessen-Mol, A., Janssen-van den Broek, M. W., van den Bogaerdt, A. J., et al. (2016). Age-Dependent Changes in Geometry, Tissue Composition and Mechanical Properties of Fetal to Adult Cryopreserved Human Heart Valves. PLoS One 11 (2), e0149020. doi:10.1371/journal.pone.0149020
Vedanthan, R., Bansilal, S., Soto, A. V., Kovacic, J. C., Latina, J., Jaslow, R., et al. (2016). Family-Based Approaches to Cardiovascular Health Promotion. J. Am. Coll. Cardiol. 67 (14), 1725–1737. doi:10.1016/j.jacc.2016.01.036
Wang, Q., Liu, H., Ren, Z., Xiong, W., He, M., Li, N., et al. (2020). The Associations of Family Functioning, General Well-Being, and Exercise with Mental Health Among End-Stage Renal Disease Patients. Psychiatry Investig. 17 (4), 356–365. doi:10.30773/pi.2019.0204
Wong, J. Y. H., Wai, A. K. C., Zhao, S., Yip, F., Lee, J. J., Wong, C. K. H., et al. (2020). Association of Individual Health Literacy with Preventive Behaviours and Family Well-Being during COVID-19 Pandemic: Mediating Role of Family Information Sharing. Int. J. Environ. Res. Public Health 17 (23), 8838. doi:10.3390/ijerph17238838
Yeom, H. E., and Lee, J. (2020). Gender Difference in the Relationship Among Family Function, Health Behavior, and Stress in Midlife. Int. J. Aging Hum. Dev. 91 (4), 476–500. doi:10.1177/0091415019896225
Zhang, X., Zhao, M., Li, J., Shi, L., Xu, X., Dai, Q., et al. (2019). Associations between Family Cohesion, Adaptability, and Functioning of Patients with Bipolar Disorder with Clinical Syndromes in Hebei, China. J. Int. Med. Res. 47 (12), 6004–6015. doi:10.1177/0300060519877030
Zhang, L., Ma, L., Zhou, X., and Zhan., L. (2021). Reliability and Validity of 12-item Medication Adherence Scale. Cent. South Pharm. 19 (02), 302–308. doi:10.7539/j.issn.1672-2981.2021.02.023
Zhang, Y. (2018). Family Functioning in the Context of an Adult Family Member with Illness: A Concept Analysis. J. Clin. Nurs. 27 (15-16), 3205–3224. doi:10.1111/jocn.14500
Keywords: medication adherence (MeSH), family functioning, illness perceptions, medication literacy, moderated mediation analyses, valve replacement
Citation: Ni H, Lin Y, Peng Y, Li S, Huang X and Chen L (2022) Relationship Between Family Functioning and Medication Adherence in Chinese Patients With Mechanical Heart Valve Replacement: A Moderated Mediation Model. Front. Pharmacol. 13:817406. doi: 10.3389/fphar.2022.817406
Received: 18 November 2021; Accepted: 27 January 2022;
Published: 22 February 2022.
Edited by:
Tais Freire Galvao, State University of Campinas, BrazilReviewed by:
Chung-Ying Lin, National Cheng Kung University, TaiwanDushad Ram, Shaqra University, Saudi Arabia
Gustavo Magno Baldin Tiguman, State University of Campinas, Brazil
Copyright © 2022 Ni, Lin, Peng, Li, Huang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanjuan Lin, Zmp4aHlqbEAxNjMuY29t; Liangwan Chen, Y2hlbmxpYW5nd2FuQHRvbS5jb20=
†These authors have contributed equally to this work and share first authorship
 Hong Ni1†
Hong Ni1† Yanjuan Lin
Yanjuan Lin Liangwan Chen
Liangwan Chen